- 1National Research Institute for Family Planning, Chinese Academy of Medical Sciences, Beijing, China
- 2School of Population Medicine and Public Health, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing, China
Objectives: This study aimed to systematically review the effectiveness of service interventions for improving postpartum contraception, including contraceptive use, prevention of repeat pregnancies and induced abortions.
Methods: A systematic literature search was conducted in three databases until June 2022 (PROSPERO registration CRD42022328349). Estimates of intervention effects from meta-analyses were represented as odds ratios (OR) with 95% confidence intervals (CI).
Results: 16 studies with 14,289 participants were included, with four kinds of interventions recognized. Interventions effect in increasing use of contraceptives and decreasing rates of repeated pregnancy for up to 6 months postpartum (OR = 2.24, 0.06, 95% CI = 1.46–3.44, 0.02–0.22, respectively), with no significant associations with contraceptive use at 12 months postpartum, prevention of postpartum repeat pregnancies and induced abortions during 1 year after childbirth.
Conclusion: We concluded that interventions impact the initiation of postpartum contraceptive use and prevention of repeat pregnancy with an overall certainty from low to moderate. These findings highlight the need for additional studies to integrate the beneficial effect of several interventions and then design more feasible strategies, which is important for the maternal and child healthcare systems.
Introduction
Although a rapid increase in the effectiveness of contraceptives has been achieved worldwide, the rates of perfect or typical use have not shown similar improvements. Moreover, the percentage of pregnancies considered to be unintended remains substantially higher in some regions (1, 2). According to a study that evaluated data from nationally published studies and official statistics, there were an average of approximately 121.0 million unintended pregnancies each year globally, which translates to a rate of 64 unintended pregnancies per 1,000 women aged 15–49 years in 2015–19 (3, 4). Studies also revealed that many unintended pregnancies are terminated, with more than half of the procedures performed unsafely (3, 5, 6).
Postpartum women are among those with the higher risk of unintended and closely spaced pregnancies and the greatest need for limiting birth. The extended postpartum period is the first year after childbirth (7). Maternal healthcare, through family planning services and via modern contraceptive methods, can allow postpartum women to prevent unintended pregnancies and determine their pregnancies’ spacing during this period (8–10). This kind of prevention of unintended pregnancies also helps to lower maternal ill-health and the number of pregnancy-related deaths (11). Previous studies (12, 13) suggested that at least 30% of maternal deaths and 10% of neonatal deaths can be avoided when the next pregnancies of mothers are delayed for 2 years after delivery. Given that, abundant interventions and strategies of services were applied internationally as vital components of comprehensive maternal healthcare to available postpartum family planning (PPFP) uptake.
Relevant interventions include counselling, education, reminding massages, etc., which may be provided to individuals or groups in a hospital/clinic or during home visits at prenatal care or postnatal care. The counselling strategies consist of a single component or multiple components delivered in a single session or multiple sessions at various contact points (including the prenatal care clinic, during delivery, postnatal care, etc.). The educational interventions used to be provided through oral/written materials, mobile phones, or multiple media to disseminate maternal care and family planning information in person or through a group discussion. The reminder messages may be sent daily to remind women to take their pills or may be sent reminders when their next injection or medical visit is due. Although these interventions were internationally implemented, the Royal College of Obstetricians & Gynecologists (RCOG) still believes that PPFP is often ignored, and many biases and misconceptions have limited its availability (14).
Several non-randomized trials (NRs) have shown that interventions delivered in maternal care settings may improve adherence to contraceptive use and reduce repeat pregnancy and induced abortion during the postpartum period (15–17). Furthermore, a systematic review assessed the impact of educational interventions based on these NRs, which concluded that education might increase postpartum contraceptive use. However, the quality of evidence was moderate to low, and interventions must be improved by strengthening the program design and implementation (18). Despite existing research, there is a lack of randomized controlled trials (RCTs), and systematic reviews assessing the evidence from RCTs are limited (4, 19, 20). And more is known about the appropriateness of specific contraceptive methods for postpartum women than how to help women use certain contraceptives. To address this gap, the current systematic review was conducted to reach consensus opinions about the impact of service interventions from RCTs and guide future research and clinical practices on the appropriate strategies for improving postpartum contraceptive use to make future maternal healthcare more valid and reliable.
Methods
This study followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (21), and its protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO) database: CRD42022328349.
Eligibility Criteria
Population
For the present review, studies that recruited postpartum women 18 years or older without being infected with human immunodeficiency virus (HIV) and another special pregnant status were eligible for inclusion.
Intervention
Service interventions scoping to improve postpartum contraception were included. For the purpose of this review, the intervention could start at any point in maternal healthcare, including prenatal care, postnatal care, or child healthcare.
Comparisons
Any comparison group without specific PPFP interventions was acceptable, including local routine maternal care or no interventions.
Outcomes
The primary outcome was rates of contraceptive use among postpartum women during 1 year after childbirth, compared to control groups. The secondary outcomes were the rates of repeat pregnancies and induced abortions during the postpartum period.
Study Design
Only randomized controlled trials and cluster-randomized trials in full-text published in English were eligible for inclusion. Studies whose follow-up time was less than 6 months after delivery; master’s or doctoral thesis or research report; studies that did not report health-related outcomes; multiple submissions and duplicate publications were excluded.
Search Strategy
English electronic databases (PubMed, EMBASE, and Web of Science) were comprehensively and systematically searched from their inception until June 2022. In-progress trials were searched for on the clinical trials register. Finally, bibliographies of the retrieved articles were also hand-searched to identify any relevant articles for our review. The search terms used were reported in Supplementary Tables S1–S3.
Data Screening and Extraction Process
Two authors (DH and YT) were assigned to independently screen the titles and abstracts among the records organized in Endnote X9 to retrieve relevant records. Then, they were also assigned to independently perform the second screening of the full text based on the predefined inclusion criteria, and independently extracted data from included studies using a format prepared in a Microsoft Excel spreadsheet. Detailed information was extracted, including author, publication year, location, study design, sample size, intervention details, comparison condition, service opportunities, and outcomes. Discrepancies and disagreements during the entire process were resolved by the third author (KP). Eligibility for inclusion in the meta-analysis was also determined for each study.
Risk of Bias
We evaluated the quality of the studies based on the Cochrane “risk of bias” assessment tool and using criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (22). Based on the rating obtained from 5 domains, each study was classified as having “Low risk,” “High risk,” and “Some Concerns.” The risk of bias was assessed by two authors (DH and KP) independently. Any discrepancies were discussed until a consensus was reached. A summary figure of the assessed bias of the included studies was created using Microsoft Excel (Microsoft Corp, Redmond, WA, USA).
Publication Bias and Heterogeneity
Rigorous searches (electronic/database search and manual search) have been used to minimize the risk of bias. With recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomized controlled trials (23), we could not construct funnel plots to test for publication bias as there were insufficient studies for any one comparison. According to the Cochrane handbook criteria, the Higgins I2 test measured heterogeneity among studies with its corresponding p-value. I2 test statistics values of 0, 25, 50, and 75% were considered no, low, moderate, and high degrees of heterogeneity, respectively (24). In this study, when I2 > 50%, there is an obvious heterogeneity and the random effect model will be used, otherwise, the fixed effect model will be applied.
Data Synthesis
Rates of postpartum contraceptive use, repeat pregnancy, and induced abortion during 1 year after childbirth were expressed as odds ratio (OR) and 95% confidence interval (CI). Where studies measured the same outcomes (including rates of contraceptive use, rates of repeat pregnancy, and rates of induced abortion during the postpartum period), we included them in a meta-analysis. Three random-effects models were applied to pool the ORs of interventions on contraceptive use at 6/8/12 months postpartum compared with local routine care or no interventions. Two fixed-effects models were applied to calculate the pooled OR for impact on repeat pregnancy. The results were presented using texts and forest plots. Sensitivity analysis was conducted using leave-one-out influence analyses with a p-value of less than 0.05 declaring the statistical significance. The data syntheses were done using R-studio Version 1.1.383 (1999 Free Software Foundation, Boston, Massachusetts, MA, USA: RStudio, PBC).
Results
Literature Search
782 citations were identified through database searches and reference lists of relevant articles. 152 duplicates were removed electronically, and we removed 4 by hand, leaving 626 unduplicated citations. After discarding 576 for not meeting the eligibility criteria according to titles and abstracts, we reviewed the full text of 50 articles for eligibility. Then, we excluded 34 and included 16 articles. 12 of 16 studies reported the outcomes of interest were included in the meta-analysis, and 4 eligible articles, excluded from the meta-analysis since they did not report any outcome of interest but other health-related outcomes, were included as part of the systematic review. A PRISMA flowchart was reported in Figure 1.
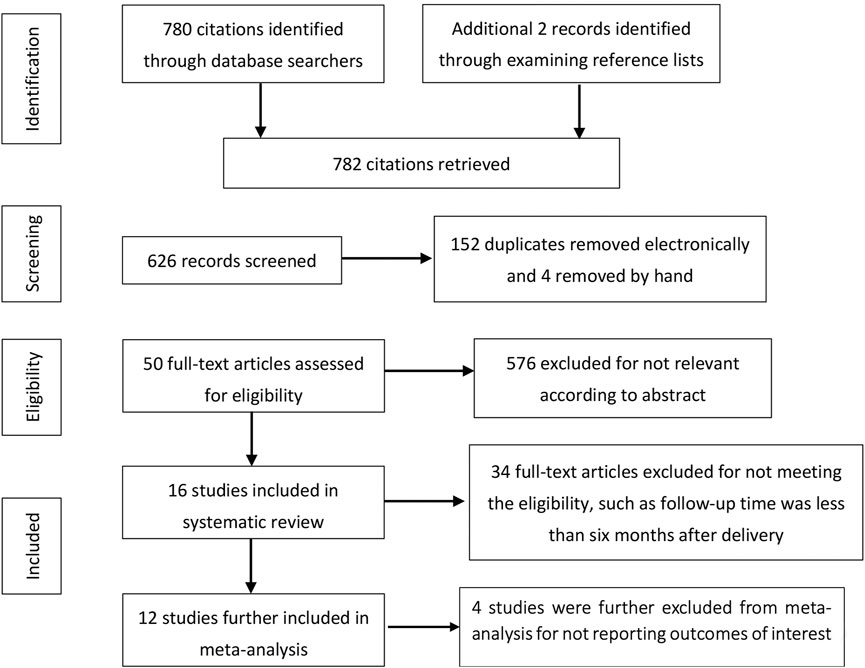
FIGURE 1. Flowchart of literature search (Beijing, China. 2022). Notes: The flow diagram was based on PRISMA.
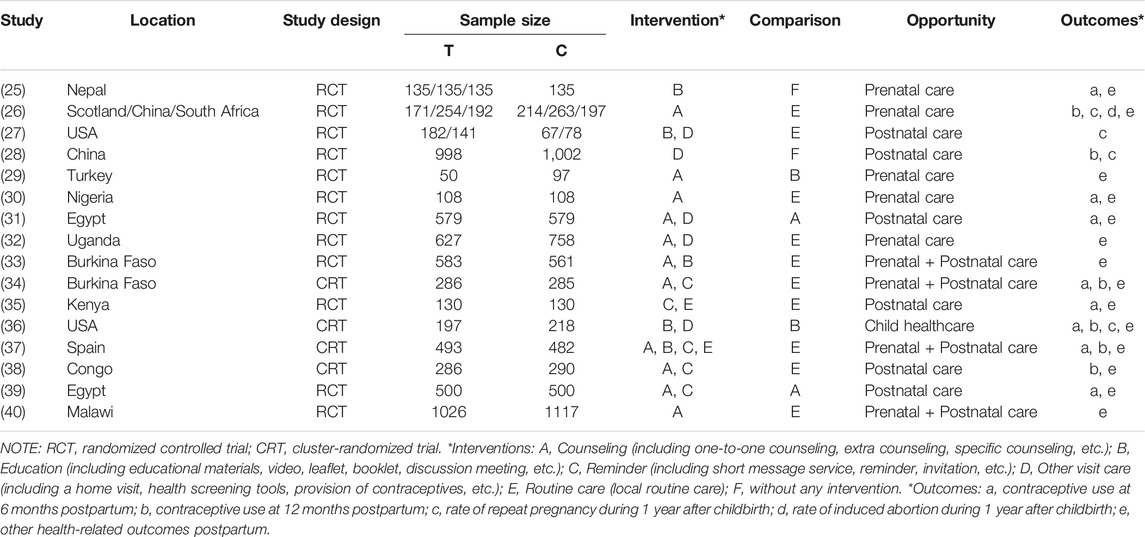
Characteristics of Included Studies
The characteristics of included studies are summarized in Table 1. Of the 16 studies, 12 were randomized controlled trials, and 4 were cluster-randomized trials. A total of 4 kinds of intervention strategies were included. Ten studies, including 8,463 women, provided direct in-person counselling, including one-to-one counselling, counselling sessions, and specific counselling meeting. Five trials provided written educational materials or videos and included 3,137 women. Five (N = 3,382) provided intensive reminders of appointments or dosing through sending a short message, phone call, or self-developed system. Studies also provided other healthcare services such as home visits, health screening tools, and free contraceptives.
Of these eligible studies, ten compared a compound strategy with the local routine healthcare of impact on the adoption of postpartum contraceptives. In contrast, others (n = 6) only provided a simple intervention such as counselling, educational materials, or screening tools, respectively. Only one study provided educational interventions and health screening tools for service opportunities in child healthcare clinics. Others (including 15 articles) were conducted in prenatal clinics, postnatal clinics, or both.
Risk of Bias Assessment
We found that 5 out of 16 studies had high risk or some concerns over the randomization process, all studies had high risk or some concerns over the blinding process, all studies had low risk over the outcome assessment and 5 studies had a high risk or some concerns over the missing of outcome data. Only 1 study had some concerns over other potential biases. Overall, 4 out of 16 studies had a high risk of bias and the other 12 studies had some concerns, and the quality of evidence was moderate to low (Figure 2).
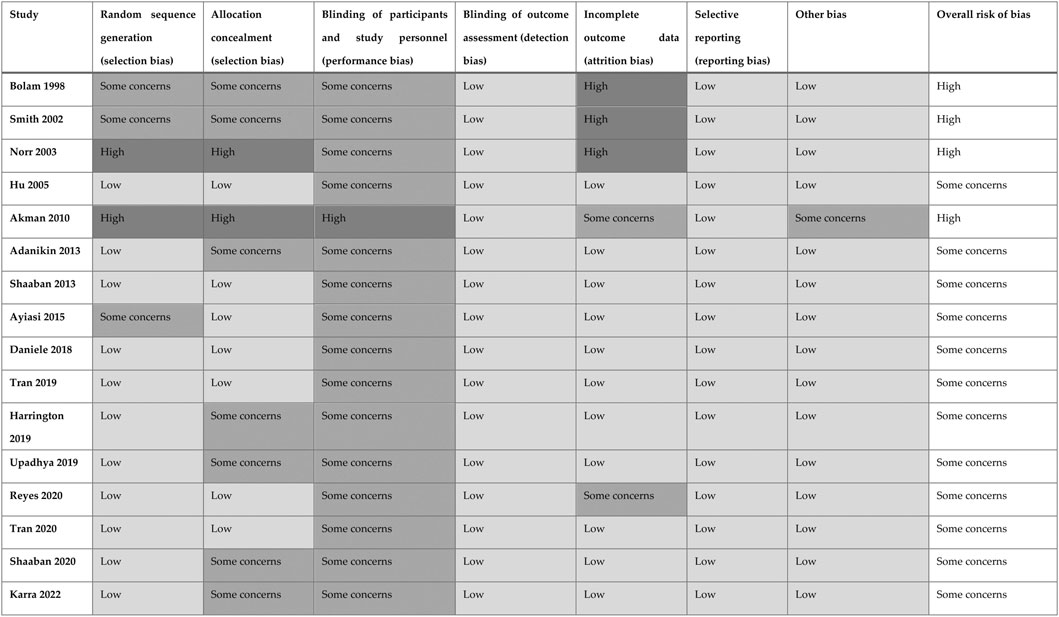
FIGURE 2. Risk of bias ratings (Beijing, China. 2022). Notes: low, low risk of bias; high, high risk of bias.
Outcomes
Contraceptive Use
Eight studies examined the impact of interventions on contraceptive use at 6 months postpartum compared with routine healthcare or no intervention. Three showed a statistically significant increase in contraceptive uptake among those who revived services. The remaining did not show a significant difference in contraceptive use. In the meta-analysis, it appears that interventions are significantly associated with increased rates of contraceptive use at 6 months postpartum (Figure 3A; OR = 2.24, 95% CI = 1.46–3.44, I2 = 83%, N = 4,679), based on the random effect model. Leave-one-out influence analyses indicated that the findings of the meta-analysis did not rely on a particular study.
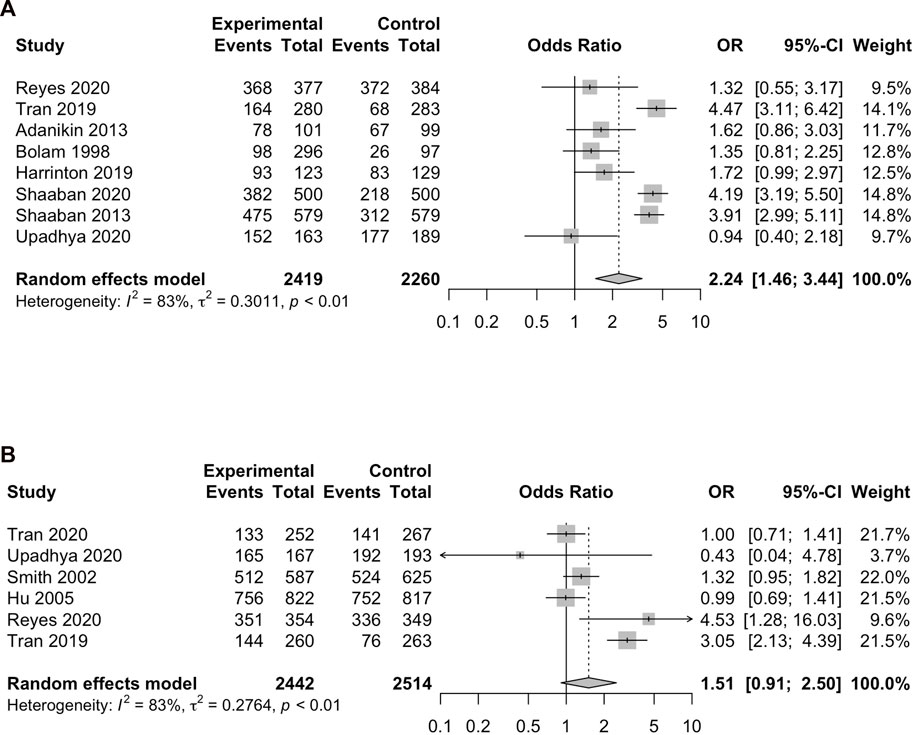
FIGURE 3. Forest plots of rates of contraceptive use (A) at 6 months postpartum, (B) at 12 months postpartum (Beijing, China. 2022). Notes: The squares depict individual study point estimates of OR. Horizontal lines display the 95% CI for point estimates.
Six studies (N = 4,956) compared interventions versus routine healthcare on contraceptive use at 12 months postpartum. Based on the random effect model (I2 = 83%, p < 0.01), the pooled results gave an OR of 1.51, favouring more chosen contraceptives. However, the 95% CIs were 0.91–2.50, indicating no significant influence of interventions on postpartum contraceptive uptake in Figure 3B. Leave-one-out influence analyses indicated that the findings of the meta-analysis did not rely on a particular study.
In addition, Hu and Daniele (28, 33) reported conflicting findings on contraceptive use at 8 months postpartum. After combining these two studies, the meta-analysis showed no significant associations with interventions (OR = 0.97, 95% CI = 0.52–1.81, I2 = 91%, N = 2,919) based on a random effect model. Karra et al. (40) found that contraceptive use after 2 years of intervention exposure increased by 5.9 percentage points compared with the control group. Of the two remaining articles that reported postpartum contraception, neither showed a statistically significant difference in interventions associated with any contraceptive uptake at 6–9 months or 12–14 months postpartum.
Repeat Pregnancy
Two articles evaluating the repeat pregnancy rates during 6 months postpartum reported a significant association. The meta-analysis also showed a statistically significant decrease in repeat pregnancy (Figure 4A. OR = 0.06, 95% CI = 0.02–0.22, I2 = 0%, N = 2,158) after receiving services. Four articles evaluated repeat pregnancy or unintended pregnancy 1 year after childbirth. However, none illustrated a statistically significant difference between the intervention groups and routine care or no intervention groups in Figure 4. Based on a fixed-effect model, the results also showed no statistically significant association between repeat pregnancy and interventions (Figure 4B. OR = 0.99, 95% CI = 0.79–1.24, I2 = 0%, N = 3,768). Leave-one-out influence analyses indicated that the findings of the meta-analysis did not rely on a particular study. However, one study in Malawi (40) reported the intervention group’s hazard of repeat pregnancy was significantly lower during 24 months postpartum.
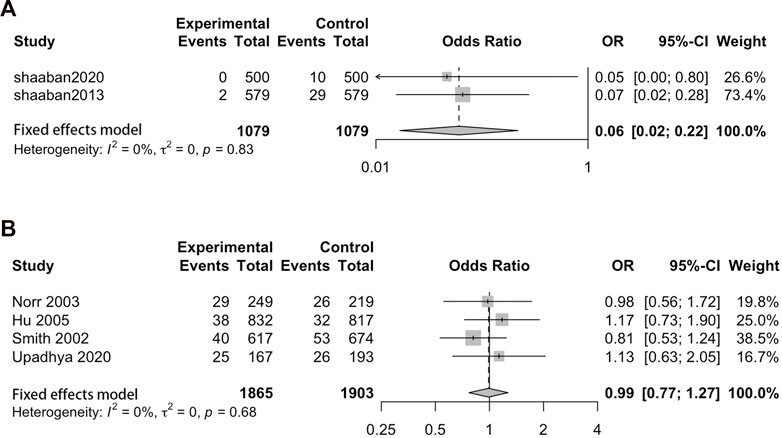
FIGURE 4. Forest plots of the rate of repeat pregnancy (A) during 6 months postpartum, (B) 1 year after delivery (Beijing, China. 2022). Notes: The squares depict individual study point estimates of OR. Horizontal lines display the 95% CI for point estimates.
Induced Abortion
Only one study reported the rate of induced abortion 1 year after delivery. The study was simultaneously conducted in Edinburgh, Cape town, and Shanghai. Only 2 participants and 1 control in Edinburgh and 29 participants and 27 controls in Shanghai experienced induced abortion. And the results showed no significant influence of interventions on rates of induced abortion during 12 months after childbirth.
Discussion
This systematic review summarizes the strategies adopted by previous RCTs, provides a synthesis of family planning services on the impact on postpartum contraception and finds that implementing interventions significantly impacts the use of contraceptives and prevention of repeat pregnancy for up to 6 months postpartum compared with local routine healthcare. These findings may offer significant recommendations for improving postpartum care and childcare systems.
Despite variations in strategies, half of the studies that reported rates of contraceptive use indicated an improved initiation of contraception, especially modern contraceptive uptake. Family planning services delivered via counselling (one-to-one, session and et al.), education, reminder and health visit during the prenatal and postpartum period were associated with increased contraceptive use. The meta-analysis shows a significantly positive association with contraceptive use at 6 months after childbirth. In addition, two studies reported a significant decrease in the repeat pregnancy rate 6 months after delivery as well as the result of the meta-analysis indicates a significantly negative association.
Although 2 of 6 studies reported a significantly increasing association with contraceptive use at 12 months postpartum, the meta-analysis shows no significant associations. The results of the prevention of repeat pregnancy and induced abortions 1 year after childbirth were also insignificant, regardless of the individual or meta-analysis.
Therefore, there are observed associations that indicated family planning services improve the initiation of postpartum contraception, without impacting on prevention of repeat pregnancy and induced abortion 1 year after childbirth. But there is a caveat that a certain degree of heterogeneity among the studies, and due to the limitation of the number of studies included, we have not well distinguished the causes of heterogeneity and impossible to conduct subgroup analysis. Another warning is that these estimates are inaccurate for these studies, with about half, being conducted with small samples (n<200). Thus, more studies with an adequate sample on the effects of family planning services on postpartum contraceptive uptake among postpartum women are needed.
Whether the goals are short-term or long-term will vary according to population differences, for example, the women’s age and number of children. Similarly, differences in the design among studies will also affect the goals. But included studies did not always consider the age differences and provide essential information, such as the frequency, theories and other details of interventions. Therefore, it may be unreasonable to evaluate the long-term effect (such as prevention of repeat pregnancies and induced abortions during 12 months postpartum) of intervention based on existing evidence and more clarity is also needed for future studies to consider the difference in the study design, intervention details and population.
In addition, RCOG believes family planning should be discussed from the beginning of pregnancy until the end of the postpartum. The current study includes three opportunities including prenatal care, postnatal care and child healthcare. However, there was also a lack of studies conducted during delivery and in child healthcare clinics, for which we were unable to obtain more evidence on the impact of the different contact points. Hence, we recommend more rigorous studies are needed to explore the feasibility and effectiveness of postpartum family planning services at different opportunities, and also an integrated delivery system or strategy of maternal healthcare, family planning services, and child healthcare during the whole postpartum period is needed to provide evidence-based guidance for future clinical postpartum contraceptive services and maternal and child healthcare practices.
Overall, this systematic review comprehensively synthesizes the available evidence, mainly on family planning services’ effects on postpartum contraception. This systematic review strengthens the recommendations that women receive family planning services integrated with routine maternal health services in prenatal care clinics, postnatal clinics and child healthcare clinics. In addition, this review will have significant implications for designing strategies to enhance family planning services to improve contraceptive uptake and maternal and child health.
Limitations
Several limitations of our systematic review should be highlighted. First, the primary studies included in this review were limited to some regions of the country, and others might be underrepresented. Second, only articles published in English were considered to conduct this review, which may result in missing studies that could have been published in other languages. Meanwhile, another strong limitation of the meta-analysis is that only 3 academic search systems were used, which greatly limited the application of evidence. And then, we did not distinguish interventions between different kinds under the same category, which makes we were not entirely certain which intervention or interventions were responsible for the significant differences observed in the meta-analysis. Few primary studies with a small sample size were included and we did not include grey literature in the review, which might influence the estimated magnitude of postpartum modern contraceptive use. Because the limited number of included studies leads the further subgroup analysis not being possible in each group. In addition, differing time frames likely influenced the design, intervention content, and outcome measures.
Conclusion
Counselling, education, reminders, and other related interventions in prenatal care clinics, postnatal care clinics, or both were significantly associated with improving postpartum contraception for up to 6 months, although the certainty of evidence was low to moderate. Considering the uptake of postpartum contraceptive methods is critical to reducing maternal and neonatal mortality and morbidity. It should be promoted and strengthened that family planning services to all women in prenatal care, during delivery, postnatal care, child healthcare or all. Furthermore, further investigation of detailed family planning services’ effects in different contact points on contraception among women within the 12 months postpartum period is needed.
Author Contributions
Conceptualization, DH, YT, and KP; Methodology, YT; Software, DH; Formal analysis, DH; Writing—original draft preparation, DH and YT; Writing—review and editing, KP; Visualization, DH; Supervision, KP; Project administration, KP; Funding acquisition, KP. All authors have read and agreed to the published version of the manuscript. KP had full access to all study data and took responsibility for the integrity of the data and the accuracy of the data analysis.
Funding
Open access funding provided by a project “Improving Sexual and Reproductive Health among Vulnerable Populations in Qinghai and Shanxi Provinces in China” under the United Nations Population Fund-Government of China Ninth Country Programme (2020–2025).
Author Disclaimer
The views expressed in this report are those of the authors alone and do not necessarily reflect the policies or views of the United Nations Population Fund.
Conflict of Interest
The authors declare that they do not have any conflicts of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/ijph.2023.1605564/full#supplementary-material
References
1. Bearak, J, Popinchalk, A, Alkema, L, and Sedgh, G. Global, Regional, and Subregional Trends in Unintended Pregnancy and its Outcomes from 1990 to 2014: Estimates from a Bayesian Hierarchical Model. Lancet Glob Health (2018) 6(4):e380–e389. doi:10.1016/s2214-109x(18)30029-9
2. Teal, S, and Edelman, A. Contraception Selection, Effectiveness, and Adverse Effects: A Review. Jama (2021) 326(24):2507–18. doi:10.1001/jama.2021.21392
3. Bearak, J, Popinchalk, A, Ganatra, B, Moller, AB, Tunçalp, Ö, Beavin, C, et al. Unintended Pregnancy and Abortion by Income, Region, and the Legal Status of Abortion: Estimates from a Comprehensive Model for 1990-2019. Lancet Glob Health (2020) 8(9):e1152–e1161. doi:10.1016/s2214-109x(20)30315-6
4. Mruts, KB, Tessema, GA, Gebremedhin, AT, Scott, J, and Pereira, G. The Effect of Family Planning Counselling on Postpartum Modern Contraceptive Uptake in Sub-saharan Africa: a Systematic Review. Public Health (2022) 206:46–56. doi:10.1016/j.puhe.2022.02.017
5. Shah, I, and Ahman, E. Unsafe Abortion: Global and Regional Incidence, Trends, Consequences, and Challenges. J Obstet Gynaecol Can (2009) 31(12):1149–58. doi:10.1016/s1701-2163(16)34376-6
6. Fathalla, MF. Safe Abortion: The Public Health Rationale. Best Pract Res Clin Obstet Gynaecol (2020) 63:2–12. doi:10.1016/j.bpobgyn.2019.03.010
7. Bakamjian, L. Programming Strategies for Postpartum Family Planning. Geneva, Switzerland: WHO Press, World Health Organization (2013). p. 1–39.
8. Fuller, WE. Family Planning in the Postpartum Period. Clin Obstet Gynecol (1980) 23(4):1081–6. doi:10.1097/00003081-198012000-00011
9. Sober, S, and Schreiber, CA. Postpartum Contraception. Clin Obstet Gynecol (2014) 57(4):763–76. doi:10.1097/grf.0000000000000055
10. Vieira, CS, Brito, MB, and Yazlle, ME. Contracepção No Puerpério. Rev Bras Ginecol Obstet (2008) 30(9):470–9. doi:10.1590/s0100-72032008000900008
11. Dehingia, N, Dixit, A, Atmavilas, Y, Chandurkar, D, Singh, K, Silverman, J, et al. Unintended Pregnancy and Maternal Health Complications: Cross-Sectional Analysis of Data from Rural Uttar Pradesh, India. BMC Pregnancy Childbirth (2020) 20(1):188. doi:10.1186/s12884-020-2848-8
12. Cleland, J, Conde-Agudelo, A, Peterson, H, Ross, J, and Tsui, A. Contraception and Health. Lancet (2012) 380(9837):149–56. doi:10.1016/s0140-6736(12)60609-6
13. Cleland, J, Bernstein, S, Ezeh, A, Faundes, A, Glasier, A, and Innis, J. Family Planning: the Unfinished Agenda. Lancet (2006) 368(9549):1810–27. doi:10.1016/s0140-6736(06)69480-4
15. Kassa, BG, Ayele, AD, Belay, HG, Tefera, AG, Tiruneh, GA, Ayenew, NT, et al. Postpartum Intrauterine Contraceptive Device Use and its Associated Factors in Ethiopia: Systematic Review and Meta-Analysis. Reprod Health (2021) 18(1):225. doi:10.1186/s12978-021-01273-x
16. Qureshey, EJ, Chauhan, SP, Wagner, SM, Batiste, O, Chen, HY, Ross, PJ, et al. Postpartum LARC Uptake in High-Risk Pregnancies with Decision Aid versus Routine Care: A Randomized Trial. Am J Obstet Gynecol (2022) 226(1):S265–6. doi:10.1016/j.ajog.2021.11.451
17. Hofler, L, Cordes, S, Cwiak, C, Goedken, P, Jamieson, D, and Kottke, M. Implementation of Immediate Postpartum Larc in Georgia. Contraception (2016) 94(4):425–6. doi:10.1016/j.contraception.2016.07.155
18. Lopez, LM, Grey, TW, Chen, M, and Hiller, JE. Strategies for Improving Postpartum Contraceptive Use: Evidence from Non-randomized Studies. Cochrane Database Syst Rev (2014) 2014(9). doi:10.1002/14651858.CD011298
19. Wakuma, B, Mosisa, G, Etafa, W, Mulisa, D, Tolossa, T, Fetensa, G, et al. Postpartum Modern Contraception Utilization and its Determinants in Ethiopia: A Systematic Review and Meta-Analysis. PLoS One (2020) 15(12):e0243776. doi:10.1371/journal.pone.0243776
20. Lopez, LM, Hiller, JE, and Grimes, DA. Postpartum Education for Contraception: A Systematic Review. Obstetrical Gynecol Surv (2010) 65(5):325–31. doi:10.1097/OGX.0b013e3181e57127
21. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The PRISMA 2020 Statement: an Updated Guideline for Reporting Systematic Reviews. BMJ (Clinical research ed) (2021) 372:n71. doi:10.1136/bmj.n71
22. Higgins, JP, Altman, DG, Gøtzsche, PC, Jüni, P, Moher, D, Oxman, AD, et al. The Cochrane Collaboration's Tool for Assessing Risk of Bias in Randomised Trials. BMJ (Clinical research ed) (2011) 343:d5928. doi:10.1136/bmj.d5928
23. Sterne, JA, Sutton, AJ, Ioannidis, JP, Terrin, N, Jones, DR, Lau, J, et al. Recommendations for Examining and Interpreting Funnel Plot Asymmetry in Meta-Analyses of Randomised Controlled Trials. BMJ (Clinical research ed) (2011) 343:d4002. doi:10.1136/bmj.d4002
24. Higgins, JP, and Thompson, SG. Quantifying Heterogeneity in a Meta-Analysis. Stat Med (2002) 21(11):1539–58. doi:10.1002/sim.1186
25. Bolam, A, Manandhar, DS, Shrestha, P, Ellis, M, and Costello, AM. The Effects of Postnatal Health Education for Mothers on Infant Care and Family Planning Practices in Nepal: a Randomised Controlled Trial. BMJ (Clinical research ed) (1998) 316(7134):805–11. doi:10.1136/bmj.316.7134.805
26. Smith, KB, Van Der Spuy, ZM, Cheng, L, Elton, R, and Glasier, AF. Is Postpartum Contraceptive Advice Given Antenatally of Value? Contraception (2002) 65(3):237–43. doi:10.1016/S0010-7824(01)00308-0
27. Norr, KF, Crittenden, KS, Lehrer, EL, Reyes, O, Boyd, CB, Nacion, KW, et al. Maternal and Infant Outcomes at One Year for a Nurse-Health Advocate home Visiting Program Serving African Americans and Mexican Americans. Public Health Nurs (2003) 20(3):190–203. doi:10.1046/j.0737-1209.2003.20306.x
28. Hu, X, Cheng, L, Hua, X, and Glasier, A. Advanced Provision of Emergency Contraception to Postnatal Women in China Makes No Difference in Abortion Rates: a Randomized Controlled Trial. Contraception (2005) 72(2):111–6. doi:10.1016/j.contraception.2005.02.004
29. Akman, M, Tuzun, S, Uzuner, A, Basgul, A, and Kavak, Z. The Influence of Prenatal Counselling on Postpartum Contraceptive Choice. J Int Med Res (2010) 38(4):1243–9. doi:10.1177/147323001003800405
30. Adanikin, AI, Onwudiegwu, U, and Loto, OM. Influence of Multiple Antenatal Counselling Sessions on Modern Contraceptive Uptake in Nigeria. Eur J Contracept Reprod Health Care (2013) 18(5):381–7. doi:10.3109/13625187.2013.816672
31. Shaaban, OM, Hassen, SG, Nour, SA, Kames, MA, and Yones, EM. Emergency Contraceptive Pills as a Backup for Lactational Amenorrhea Method (LAM) of Contraception: A Randomized Controlled Trial. Contraception (2013) 87(3):363–9. doi:10.1016/j.contraception.2012.07.013
32. Ayiasi, RM, Muhumuza, C, Bukenya, J, and Orach, CG. The Effect of Prenatal Counselling on Postpartum Family Planning Use Among Early Postpartum Women in Masindi and Kiryandongo Districts, Uganda. Pan Afr Med J (2015) 21:138. doi:10.11604/pamj.2015.21.138.7026
33. Daniele, MAS, Ganaba, R, Sarrassat, S, Cousens, S, Rossier, C, Drabo, S, et al. Involving Male Partners in Maternity Care in burkina faso: A Randomized Controlled Trial. Bull World Health Organ (2018) 96(7):450–61. doi:10.2471/BLT.17.206466
34. Tran, NT, Seuc, A, Coulibaly, A, Landoulsi, S, Millogo, T, Sissoko, F, et al. Post-Partum Family Planning in Burkina Faso (Yam Daabo): a Two Group, Multi-Intervention, Single-Blinded, Cluster-Randomised Controlled Trial. Lancet Glob Health (2019) 7(8):e1109–e1117. doi:10.1016/S2214-109X(19)30202-5
35. Harrington, EK, Drake, AL, Matemo, D, Ronen, K, Osoti, AO, John-Stewart, G, et al. An mHealth SMS Intervention on Postpartum Contraceptive Use Among Women and Couples in Kenya: A Randomized Controlled Trial. Am J Public Health (2019) 109(6):934–41. doi:10.2105/AJPH.2019.305051
36. Upadhya, KK, Psoter, KJ, Connor, KA, Mistry, KB, Levy, DJ, and Cheng, TL. Cluster Randomized Trial of a Pre/Interconception Health Intervention for Mothers in Pediatric Visits. Acad Pediatr (2020) 20(5):660–9. doi:10.1016/j.acap.2019.10.003
37. Reyes-Lacalle, A, Montero-Pons, L, Manresa-Domínguez, JM, Cabedo-Ferreiro, R, Seguranyes, G, and Falguera-Puig, G. Perinatal Contraceptive Counselling: Effectiveness of a Reinforcement Intervention on Top of Standard Clinical Practice. Midwifery (2020) 83:102631. doi:10.1016/j.midw.2020.102631
38. Tran, NT, Seuc, A, Tshikaya, B, Mutuale, M, Landoulsi, S, Kini, B, et al. Effectiveness of post-partum Family Planning Interventions on Contraceptive Use and Method Mix at 1 Year after Childbirth in Kinshasa, DR Congo (Yam Daabo): a Single-Blind, Cluster-Randomised Controlled Trial. Lancet Glob Health (2020) 8(3):e399–e410. doi:10.1016/S2214-109X(19)30546-7
39. Shaaban, OM, Saber, T, Youness, E, Farouk, M, and Abbas, AM. Effect of a mobile Phone-Assisted Postpartum Family Planning Service on the Use of Long-Acting Reversible Contraception: a Randomised Controlled Trial. Eur J Contraception Reprod Health Care (2020) 25(4):264–8. doi:10.1080/13625187.2020.1764528
Keywords: systematic review, family planning, contraception, postpartum, maternal care, meta-analysis
Citation: Hu D, Tang Y and Pei K (2023) Strategies for Improving Postpartum Contraception Compared With Routine Maternal Care: A Systematic Review and Meta-Analysis. Int J Public Health 68:1605564. doi: 10.3389/ijph.2023.1605564
Received: 06 November 2022; Accepted: 02 April 2023;
Published: 13 April 2023.
Edited by:
Seyma Karaketir, Istanbul University, TürkiyeReviewed by:
Ankit Anand, Institute for Social and Economic Change, IndiaMeryem Merve Oren, Istanbul University, Türkiye
Copyright © 2023 Hu, Tang and Pei. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kaiyan Pei, MTU4MTA0NzExOThAMTYzLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Denghui Hu
Denghui Hu Yuxiang Tang2†
Yuxiang Tang2†