Abstract
Objectives:
To identify COVID-19 infectious disease models that accounted for social determinants of health (SDH).
Methods:
We searched MEDLINE, EMBASE, Cochrane Library, medRxiv, and the Web of Science from December 2019 to August 2020. We included mathematical modelling studies focused on humans investigating COVID-19 impact and including at least one SDH. We abstracted study characteristics (e.g., country, model type, social determinants of health) and appraised study quality using best practices guidelines.
Results:
83 studies were included. Most pertained to multiple countries (n = 15), the United States (n = 12), or China (n = 7). Most models were compartmental (n = 45) and agent-based (n = 7). Age was the most incorporated SDH (n = 74), followed by gender (n = 15), race/ethnicity (n = 7) and remote/rural location (n = 6). Most models reflected the dynamic nature of infectious disease spread (n = 51, 61%) but few reported on internal (n = 10, 12%) or external (n = 31, 37%) model validation.
Conclusion:
Few models published early in the pandemic accounted for SDH other than age. Neglect of SDH in mathematical models of disease spread may result in foregone opportunities to understand differential impacts of the pandemic and to assess targeted interventions.
Systematic Review Registration::
[https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020207706], PROSPERO, CRD42020207706.
Introduction
Infectious disease models are tools that help researchers simulate real-world possibilities in a virtual environment and inform public health policy decisions. Models use mathematical equations to anticipate the future course of an outbreak, aid public health planning, and support disease control efforts. The models describe “how infectious diseases progress in a given population depending on existing and counterfactual conditions/measures and a disease’s characteristic (e.g., transmission rate, incubation, asymptomatic case).” [1] To build these models, analysts synthesize information from a variety of sources, including epidemiological surveillance data, the published literature, and expert opinion. The validity of the models can be tested by changing the input parameters within plausible ranges, also known as uncertainty analysis, and by comparing the model predictions to epidemiological surveillance data.
Infectious disease models can be grouped into three types: compartmental, agent-based, and statistical models [1]. Each differs in the way the modelled population is conceptualized. Compartmental models divide the simulated population into groups, and changes in disease incidence over time are a function of interactions amongst the groups. In the simplest compartmental models, simulated groups are defined only by infection status (e.g., susceptible, infected), however the number of groups expands greatly if modelers wish to account for additional characteristics (for example, age group and gender). Agent-based models assign characteristics to simulated individuals, rather than groups, and changes in disease incidence over time are a function of interactions amongst simulated individuals. Statistical models predict infection risks in a simulated population without explicitly modelling interactions. Statistical models take different forms. Curve fitting models, sometimes called auto-regressive models, fit epidemic curves to historical data and extrapolate the curves to simulate and predict future incidence. Other statistical models use data on population or cohort characteristics to simulate and predict infection risk. Non-communicable disease models can be used to model COVID-19 risk or health system impacts for a simulated population, as a function of cohort or population characteristics [2]. Models have a range of complexities and there are often tradeoffs between developing tractable models that can inform policy decisions in a timely manner and accurately reflecting important sources of heterogeneity, such as social determinants of health.
The World Health Organization defines the social determinants of health as the “non-medical factors that influence health outcomes” and “the conditions in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life,” which include “economic policies and systems, development agendas, social norms, social policies and political systems” [3]. The WHO social determinants of health include income and social protection, education, unemployment, job insecurity, working life conditions, food insecurity, housing, basic amenities and the environment, early childhood development, social inclusion and non-discrimination, structural conflict, and access to affordable health services of decent quality [3]. Geography can also be considered a social determinant of health, when the aforementioned factors differ spatially, by neighborhood, county, country, or region [4, 5]. Gender, as a social construct, is a non-medical factor associated with the availability of care and is thus a social determinant of health [6, 7]. Sex, as a biological attribute is related to disease susceptibility and progression. We will report on gender as a social determinant, recognizing that modelling studies may have reported on sex, either conflating gender and sex in the conceptualization of the model, or intending to conceptualize sex differences in COVID-19 susceptibility and outcomes.
Early in the pandemic, empirical evidence identified significant variation in the epidemiology and impact of COVID-19 as a function of the social determinants of health. Counties in the United States with a higher proportion of African-Americans demonstrated significantly elevated rates of COVID-19 infection and death compared to other counties, even after controlling for demographic, clinical, social and environmental factors [8]. In England, Black and Asian ethnic minorities experienced elevated rates of COVID-19 diagnoses, compared to White residents [9]. Essential workers disproportionately came from low socioeconomic backgrounds (e.g., meat processing workers, temporary/migrant farm workers) and faced elevated COVID-19 occupational health and safety hazards [10]. These disparities are a symptom of deeper societal and health system inequities, including disproportionate exposure to infection risk, prevalence of comorbidities, and inequitable access to testing and treatment [11].
The goals of this systematic review of the literature were to identify COVID-19 infectious disease models that accounted for social determinants of health and characterize the extent to which COVID-19 models incorporate the social determinants of health. The systematic review is focused on models published early in the pandemic (during a period corresponding to the first two waves). Models published early in the pandemic reflect at least in part the preparedness of the modelling community to support responses to an emerging infectious disease threat. The early pandemic period represented an opportunity to reduce morbidity and mortality of COVID-19 impact through policies and interventions that were well informed and thoroughly evaluated. Incorporating social determinants of health into COVID-19 models can better support the development and appraisal of policies and targeted interventions than models based on an average population approach [12]. Including social determinants of health in models is also necessary to understand both the equity and efficiency of COVID-19 control efforts.
Methods
We conducted a systematic review of the literature according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [13]. The protocol is registered in the International Prospective Register of Systematic Reviews (PROSPERO) (Registration number CRD42020207706), and published in the peer-reviewed literature [14].
Search Strategy and Eligibility Criteria
We searched MEDLINE, EMBASE, Cochrane Library, medRxiv, and the Web of Science databases to identify all COVID-19 modelling studies published from December 2019 to August 14, 2020. Studies were deemed eligible if they: 1) focused on SARS-CoV-2 in a human population, 2) were a modelling study, 3) investigated one of the following outcomes: COVID-19 disease-related outcomes, non-COVID-19 disease-related outcomes (i.e., indirect impacts on other health conditions), impacts on health services, impact of policies or interventions on COVID-19 outcomes or its societal impact, and 4) included at least one social determinant of health. We excluded studies that focused on: 1) within-host biological studies, 2) non-human SARS-CoV-2 studies, 3) phylogenic/genetic studies, 4) environmental or meteorological studies without health impact analysis on humans, 5) epidemiological or statistical analyses without a model, 6) economic analyses without a model, and 7) COVID-19 infectious disease models that did not include a social determinant of health. A search strategy is provided in Supplementary File S1.
We made one amendment to the original systematic review protocol [14]. The original protocol included plans to assess social determinants of health in preprint models. Although our search strategy targeted preprints, we amended the protocol to exclude preprint models at the screening stage. Due to the poor quality of reporting in preprint models and the large volume of preprint models, we judged that the insights gleaned would not be worth the significant investment in systematic review resources that would be required to abstract data from preprint models.
Review Process
Using Covidence Software (v204501fd4fa9), duplicate citations were removed. Titles and abstracts were screened independently in duplicate (GC, FWA, LG, EP, CS) to identify studies that potentially met the inclusion criteria outlined above. Conflicts were resolved by a third independent reviewer (DEK, NM, MM, ZL). Full text articles were retrieved and independently assessed for eligibility in duplicate (GC, LG, FWA, EP, CS). Disagreements were resolved by a third reviewer (DEK, NM, MM, ZL).
Data Extraction and Quality Assessment
Data were extracted by one reviewer (GC, LG, FWA, EP, CS) and confirmed by a second (AJB, ZL). Data extracted from studies included: author, publication year, country, target population, modelling goals, type of model, social determinants of health, and approach to incorporating socioeconomic factors. We abstracted model type in the following categories: compartmental models, simulation models, multi-state life table models, comparative risk assessment models, regression models, autoregressive models, network or agent-based simulations, and other model types. Model type categories were based on systems for infectious disease models and non-communicable disease models, which distinguish between statistical models and non-statistical models, modelling of individuals or groups, and whether or not models incorporate interactions amongst modelled entities [1, 2]. Where relevant, we abstracted the interventions or policies appraised by the model. When multiple intervention options that differed only by the level of intensity or assumptions about adherence were compared, we did not record them as separate interventions. We assessed whether model results were reported by social determinants (e.g., age or race/ethnicity), and whether interventions were targeted according to social determinants, or varied by social determinants. We also recorded whether the goal of the modelling exercise was to evaluate the impact of COVID-19 by social determinants.
We developed a checklist for assessing the quality of infectious disease models (Supplementary File S2) based on the principles of best practices for models [15, 16]. Quality appraisal focused on justification of the model structure and assumptions, conduct of sensitivity analysis, internal validation (i.e., verifying that model equations have been accurately implemented and fit data used to develop the model, often referred to as model calibration), external validation (i.e., comparing model outputs to data that were not used to develop the model), completeness and transparency in model reporting, including the provision of model equations, code and initial values. Model appraisal was conducted by one reviewer (GC, LG, FWA, EP) and confirmed by a second (AJB, ZL), and was based on the analyses reported by the study authors. For example, study authors may have conducted internal validation of models, but if this was not reported in the manuscript, it was assumed that it was not performed.
Results
A total of 8,878 unique citations were identified and screened (Figure 1). Of these, 2,966 full-text manuscripts were assessed for eligibility (Figure 1). Only 83 studies were included in the review, reflecting that the vast majority of potentially eligible COVID-19 modelling studies did not include social determinants (Figure 1).
FIGURE 1
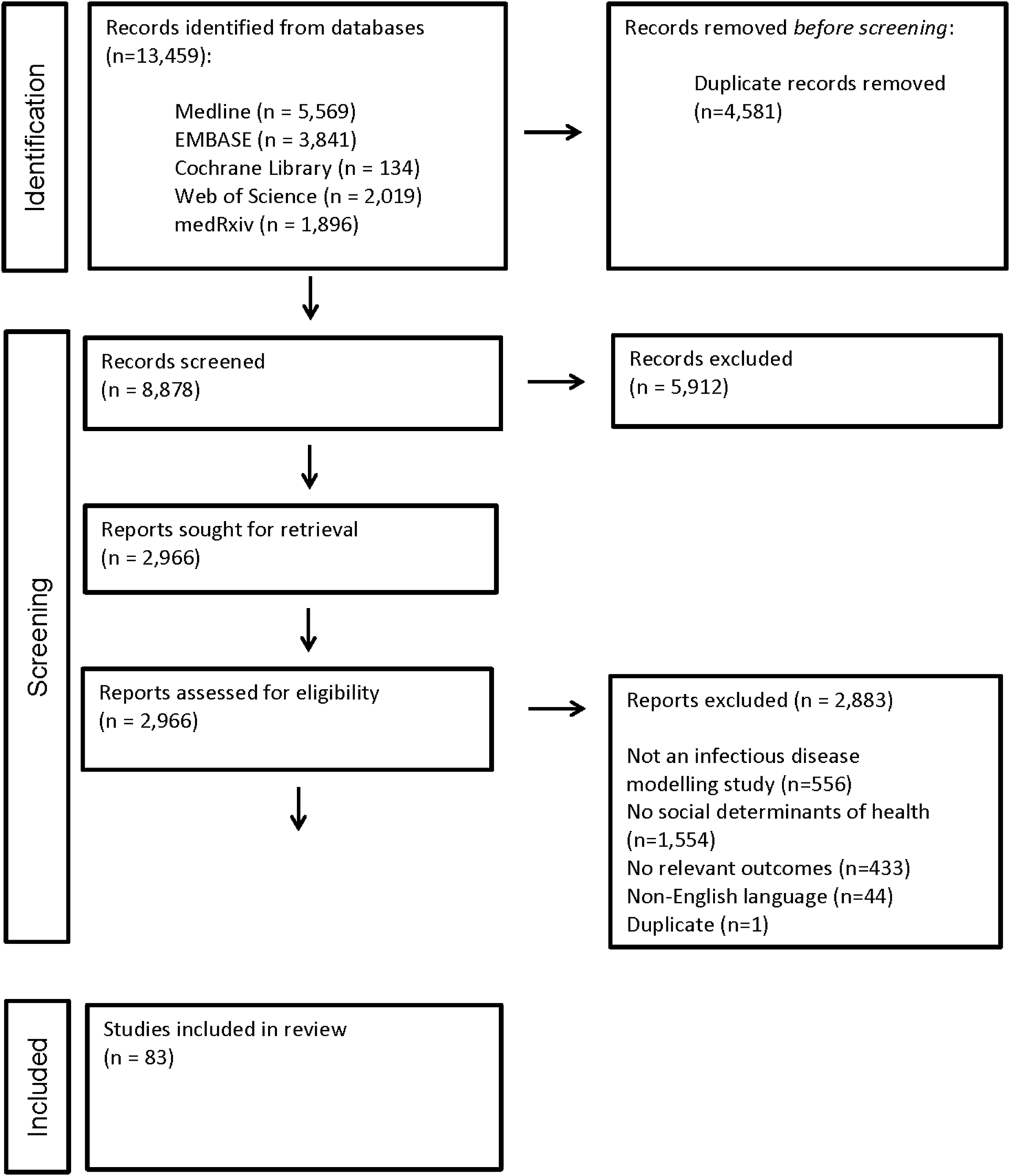
PRISMA flow diagram (Worldwide. 2020).
Of the studies included, most models pertained to multiple countries (n = 15, 18%), the United States (n = 12, 14%), or China (n = 7, 8%) (Figure 2A). The majority addressed two or more goals: (a) 24 studies focused on predicting the pandemic and assessing the impact of policies or interventions; (b) 21 studies focused on predicting the pandemic, assessing the impact on health services, and assessing the impact of policies or interventions; and (c) 17 studies focused only on predicting the pandemic (Figure 2B). The most common model types that incorporated interaction amongst modelled entities, included compartmental (n = 43, 52%) and agent-based (n = 7, 8%) models. Regression models, including those with regression analysis of area-level data (n = 6, 7%) and comparative risk assessment models (n = 6, 7%), were the next most common, followed by simulation models (n = 5, 6%), models with auto-regressive curve fitting (n = 5, 6%), and multi-state life table models (n = 5, 6%). Other model types included one of the following: Maxent ecological niche model, Bayesian hierarchical model, Bayesian spatiotemporal model, artificial neural networks, and a semi-parametric generalized additive model (Figure 2C).
FIGURE 2
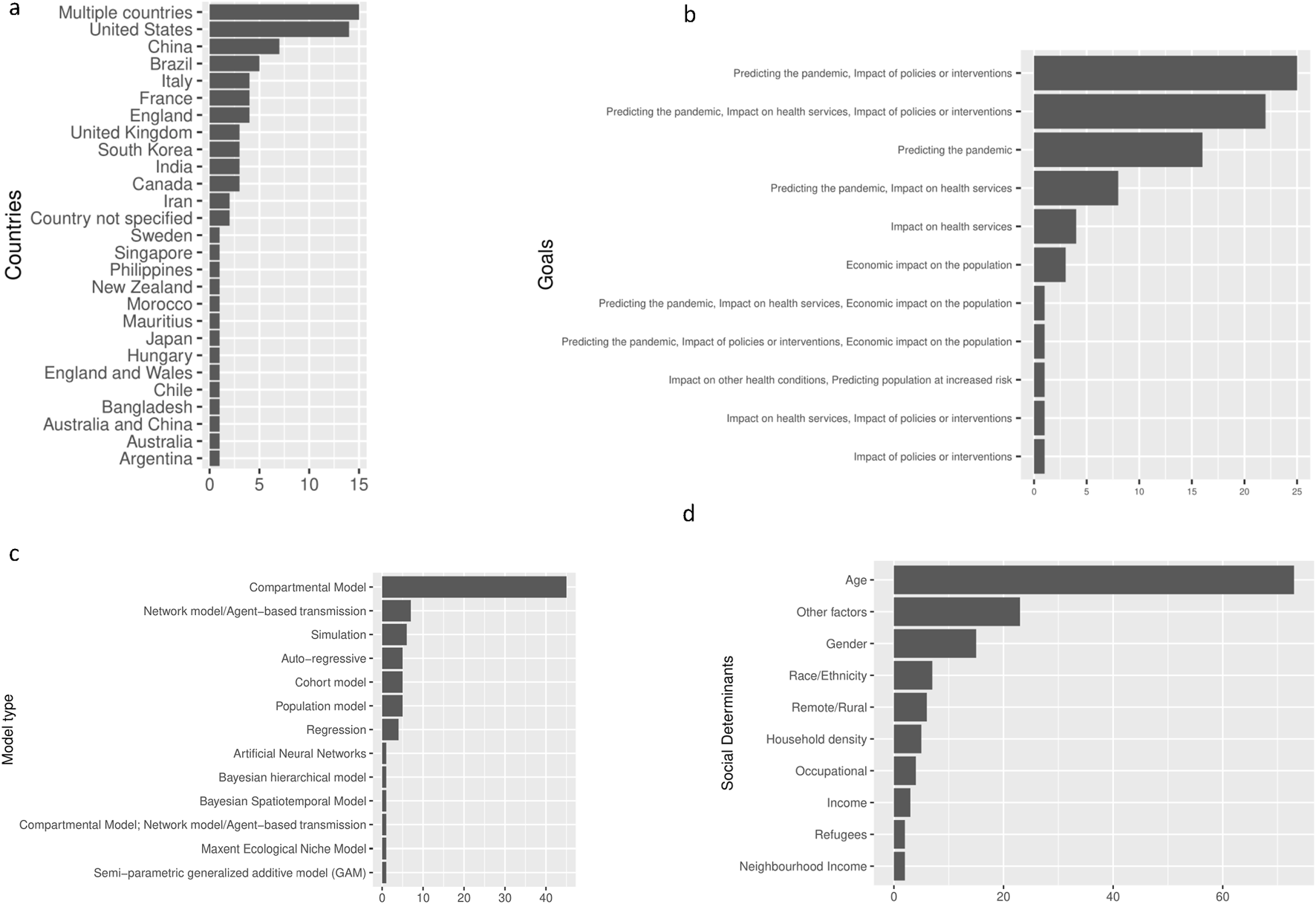
Characteristics of included studies (Worldwide. 2020). (A): Distribution of countries in the included studies (Worldwide. 2020). (B): Goals addressed by the studies (Worldwide. 2020). (C): Distribution of model types (Worldwide. 2020). (D): Social determinants included in the studies (Worldwide. 2020).
The most common social determinant included in the models was age (n = 74, 89%). Of the included studies, 36 (43%) incorporated non-age social determinants. The most common non-age social determinants included in the models were gender (n = 13, 16%), race/ethnicity (n = 7, 8%), remote/rural location (n = 6, 7%), and household density/size (n = 5, 6%) (Figure 2D). Overall, 26% of compartmental models and 43% of agent-based models incorporated non-age social determinants. All regression analyses, 83% of comparative risk assessment models, 60% of auto-regressive models and 60% of simulation models included non-age social determinants (Supplementary Table S1). Thus, regression analysis and comparative risk assessment models were more likely to include non-age social determinants.
The approach to incorporating social determinants differed by model type. Stratification was a common approach to incorporating social determinants in compartmental models, comparative risk assessment models and multi-state life table models. Compartmental models stratified the modelled population by the social factor, most commonly by age group, using age-group specific contact rates amongst age-groups [17–19]. Compartmental models also stratified the population according to income [20], gender [21, 22], household density [23] and occupational factors [24, 25]. For example, Laurio Dizon et al. modelled a separate compartment for those required to work during shutdowns (mobile workers) to capture the risk of COVID-19 spread associated with occupational factors [25]. In comparative risk assessment models, risks specific to strata defined by gender [26, 27], household density [26], and rural/urban divides [28], were used to predict COVID-19 related outcomes. Multi-state life table models also incorporated risk-specific strata, by age group, to estimate the present value of lives lost [29], and differences in the negative impacts of COVID-19 control policies on HIV-related mortality [30].
In auto-regressive modelling studies, social determinants were incorporated by fitting curves to incidence data from regions with varying levels of social determinants such as population density [31], gender ratio [32], and distance to public spaces [33]. Auto-regressive modelling studies also incorporated social determinants as a time-varying covariate reflecting changes in the age distribution of those infected with COVID-19 over time [34, 35]. Regression analyses that were not auto-regressive used area-level data to estimate the association between social determinants and COVID-19 risk at the ecological level [36–40]. For example, in one study, COVID-19 risk was modelled as a function of regional characteristics such as the percentage of black individuals in each state [37], while population density, mobility data, the number of restaurants, and the number of supermarkets were used in another [36]. In agent-based models and simulation models social determinants were person-level characteristics signifying different risk levels [41, 42].
Model type was also associated with modelling goals. All agent-based models (7/7, 100% and most compartmental models (37/45, 82%) assessed the impact of policies or interventions, whereas few regression (1/5, 20%) and auto-regressive models (1/4, 25%) assessed policies or interventions. Thus, the model types more likely to incorporate a broader range of social determinants were less frequently used to appraise the impact of policies or interventions.
Even though all the included studies incorporated at least one social factor into the COVID-19 model, a significant proportion did not report model findings according to social factor (n = 29, 35%). We identified some studies that assessed interventions that were either targeted by social factor or varied by social factor (n = 22, 27%). For example, Jamieson-Lane and colleagues evaluated targeted sequestration of older age groups [43], and Davies et al. examined school closures targeting individuals under age 20 [44].
Twelve studies (12%) explicitly stated that the goal of the modelling was to examine the impact of social determinants. Studies estimated age-standardized infection rates [20], age-specific fatality rates [45], rates of infection by race [37], intergenerational impacts of COVID-19 infection [35], and how variation in co-residence patterns across countries is associated with susceptibility to COVID-19 outbreaks [45]. Others compared the predictions of models with and without age structure [17, 31, 46–49], or with different assumptions about age distribution [50]. No studies examined the effect of including other social determinants on internal or external model validation.
The study by Koo et al. included the largest number of social determinants, incorporating parameters for age, gender, race/ethnicity, immigration status, income, occupational factors, employment status, hours worked, industry, religion, marital status, number of children, education, housing type, enrollment in the national service health insurance, transportation mode, transportation time, and mobility status into an agent-based model [51]. Thus, this study included both household-level and individual-level factors in an agent-based simulation.
Quality Appraisal
Appraisal of model quality revealed that most models included in the systematic review reflected the dynamic nature of infectious disease spread (n = 51, 61%) in which the risk of infection is a function of the number of infected individuals over time. Most authors provided justification of the model structure (n = 53, 64%), clearly specified model assumptions (n = 73, 88%), performed sensitivity analysis on key input parameters (n = 46, 55%), and conducted uncertainty analysis on key structural assumptions related to infectious disease spread (n = 50, 60%). Few studies considered thresholds for epidemic spread or extinction related to COVID-19 (n = 14, 17%), few reported performing internal model validation (n = 10, 12%), and fewer than half reported performing external validation of models (n = 31, 37%). Many study authors provided model equations (n = 41, 49%), however relatively few provided the code to reproduce the analysis (n = 23, 28%).
Discussion
In our systematic review of the literature on COVID-19 infectious disease models, we identified 83 studies that included social determinants of health, representing fewer than 3% of the full-text articles screened. Age was the most common social factor, incorporated into 89% of included studies. Some social determinants known to play an important role in COVID-19 spread were not represented well in models published early in the pandemic. We found only a few models that incorporated occupational factors despite the knowledge that essential workers were at increased risk of contracting COVID-19. We also found no models addressing substance users, sexual minorities, or incarcerated persons, which were particularly vulnerable populations.
Our study represents a unique contribution to the literature as we are unaware of any other systematic reviews focused on incorporation of social determinants of health in COVID-19 models. Gerlee et al performed a systematic review to identify Swedish COVID-19 modelling studies from the early pandemic period [52]. The goal of this research effort was to appraise the predictive accuracy of the models, and no information on inclusion of social determinants of health was abstracted [52]. Kimani et al conducted a systematic review identifying 74 COVID-19 modelling studies pertaining to the Africa region [53]. While no information on inclusion of social determinants of health was abstracted in this study, the finding that only 7% of the models were calibrated using demographic data, suggests that few of the identified models incorporated social determinants of health [53].
Infectious disease modelling guidelines stress the importance of reflecting significant sources of heterogeneity due to differences in risk behaviours, morbidity, mortality, and the rate of uptake of interventions to accurately reflect transmission dynamics and improve model accuracy and precision [1, 12, 54–56]. Social determinants represent potentially important sources of heterogeneity as COVID-19 risks vary for important groups. Incorporating social determinants into models may be hampered by inadequate data. A systematic review of peer-reviewed quantitative studies that was published early in the pandemic identified estimates of COVID-19 risk specific to sub-groups defined by race, ethnicity and socioeconomic deprivation, but limited evidence was found on other key determinants, including occupation, educational attainment, housing status and food security [57]. Quantitative estimates, even when available, may not be in the optimal format. Early in the pandemic, quantitative estimates of differential impacts were provided at the ecological level, pertaining to regions rather than individuals [8]. One of the benefits of modelling is that limited data, while not optimal, can still inform parameter estimates. For example, area-level estimates may still be useful for model validation even when individual data are unavailable.
Modellers are often required to make tradeoffs between model complexity and feasibility. Model types that provide the flexibility to facilitate incorporation of social determinants, such as agent-based models, require more computational power. Model types requiring less computing power limit flexibility for incorporating social determinants into models. For example, we found compartmental models, which are less computationally intensive, less likely to include non-age social determinants. On the other hand, agent-based models incorporated multiple social determinants. Implementation and analysis of agent-based models requires greater investments in resources, particularly computational power. Statistical models, such as regression analyses and auto-regressive approaches, were more likely to include social determinants, but many of these studies used an ecological approach. Applying an ecological approach to social determinants in regression models (e.g., neighbourhood deprivation, racial/ethnic concentration) is useful for using regional characteristics to identify pandemic hotspots, but does not provide the flexibility to evaluate the impact of policies or interventions at the individual-level. Models that do not incorporate social determinants may be adequate to inform general public health policies. We found some studies that assessed improvements in model validity derived from including age strata, however, none examined the effect of including other social determinants on model validity. The benefits of including social determinants in COVID-19 models were largely unexplored early in the pandemic.
Infectious disease models are one input into decision making processes. Other types of research evidence may have influenced the devising and implementation of COVID-19 control policies targeting vulnerable populations. Epidemiological analyses, news media reports, or advocacy efforts may have provided the impetus for addressing COVID-19 and targeting certain vulnerable populations. For example, evidence that incidence was highest in United States counties with a high percentage of African American residents, may have promoted policies targeting this high-risk group even if African American ethnicity was not accounted for in published models. In the absence of data, analysts, policymakers, and advocates may have promoted consideration of social determinants in decision-making processes. However, neglecting to represent social determinants in models means the opportunity to apply the power of mathematical modelling to forecast the potential effectiveness of targeted policies was foregone. Targeting can potentially be a more efficient mechanism of infectious disease control. For example, handing out masks to individuals in a low-income neighbourhood early in the pandemic might have reduced morbidity and mortality in low-income communities, and may have also decreased COVID-19 spread overall.
Decision makers are interested in models that address the social determinants of health. A qualitative investigation of North Carolina state policymakers revealed a desire for COVID-19 models “to show disease spread within subpopulations, including by race/ethnicity, to understand and predict how groups experiencing a higher burden of disease shifted over time” [58]. Making efforts to incorporate social determinants of health into mathematical models can be considered an ethical imperative to overcome historical injustices that lead to both the disparities in health outcomes associated with social determinants and the lack of available data to inform social determinants of health in mathematical models [59].
Limitations
Our study has several limitations. Published COVID-19 models may not be representative of all models. Modellers directly informing government decision-makers may not have published model findings. A systematic review of the grey literature to identify and appraise non-peer-reviewed models was beyond the scope of this study. However, our personal experience of policy models in Canada, the United States, and the United Kingdom, suggests these models infrequently included non-age determinants of health. Our systematic review covers a period early in the pandemic, corresponding to the first two waves. Because models incorporating social determinants of health are more complex, it is possible that these more complex models took more time to develop, validate and publish. As a result, the models published early in the pandemic could reflect a subset of simpler COVID-19 models that did not incorporate social determinants of health. It is also possible that modelers updated extant models to incorporate social determinants. More recently published models may have incorporated social determinants at a higher rate, particularly as attention to social determinants increased. However, making changes to models requires allocating resources to evidence synthesis, model programming and model validation. As the pandemic evolved, modelers adapted models to reflect new variants and to evaluate changing public health policies (e.g., vaccination and easing of public health measures). Adapting models to keep pace with changes in the pandemic may have taken priority over adapting models to incorporate social determinants, as this change would have been difficult to accomplish amidst competing priorities. Therefore, we hypothesize that a synthesis of models published in the later phases of the pandemic would produce similar findings. Future research should focus on the later phases of the pandemic, to determine if more models incorporated social determinants of health.
Conclusion
Our study provides an important overview and synthesis of modelling studies published early in the pandemic. Mathematical models have been, and remain, a critical tool in controlling COVID-19, forecasting the pandemic, estimating the potential impact of policies and interventions, and assessing potential impacts on other conditions. Critical synthesis of modelling studies is an important part of reflective practice, which can lead to improvements in the modelling profession and optimize the usefulness of model-based studies to inform decision-making. We found that few studies incorporated social determinants, and even fewer still incorporated non-age social determinants. The absence of social determinants is concerning for several reasons. Social determinants represent important areas of heterogeneity. Excluding social determinants can reduce modelling accuracy and forego the ability to account for differential uptake, acceptability, affordability, and effectiveness of COVID-19 interventions. Amidst calls to tackle growing health inequities, including social determinants in modelling efforts may provide an important contribution to this effort. Improved data are required to support inclusion of social determinants in models (for example, contact matrices should account for occupational risk, race/ethnicity, household density and income). However, limited availability of data can be partly overcome through modelling techniques. When inclusion of social determinants is a priority for modellers, they can design data collection initiatives to fill in the identified gaps. Modellers should work with stakeholders to formulate research questions reflecting disparities in health and non-health burden, differential access to care, heterogeneity in policy impact and values, and preferences of important social groups. Agent-based models incorporated a greater number of social determinants, but these models also require the most resources. Politicians should fund the infrastructure required to increase modelling complexity and facilitate incorporation of social determinants. Large modelling collaborations can pool intellectual capital and advocate for resources to develop complex models reflecting heterogeneity derived from social determinants. They can also advocate for better data collection efforts, supports for systematic reviews and meta-analyses, and model validation efforts. As countries continue to cope with COVID-19 and prepare for future pandemics, we should take advantage of lessons learned and build a global, coordinated modelling infrastructure that is equipped to account for important social determinants in infectious disease models.
Statements
Data availability statement
Study materials, including template data collection forms and extracted data, will be made available upon request.
Author contributions
AJ-B, KM, MA, DC, SM, LC, AP, SS, MH-B, AG, and SA were responsible for the design of systematic review. AJ-B, MM, ZL, DH, GC, DK, FA, LG, CS, EP, and NM contributed to acquisition of data. AJ-B wrote the first draft of the manuscript and prepared the tables and figures, while all authors were responsible for critically reviewing the content. All authors contributed to the article and approved the submitted version.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This project is funded by the Gordon and Betty Moore Foundation through Grant GBMF9634 to Johns Hopkins University to support the work of the Society for Medical Decision Making (SMDM) COVID-19 Decision Modeling Initiative (CDMI).
Conflict of interest
The authors declare that they do not have any conflicts of interest.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/phrs.2024.1607057/full#supplementary-material
References
1.
The COVID-19 Multi-Model Comparison Collaboration (CMCC) Policy Group. Guidance on Use of Modelling for Policy Responses to COVID-19. 2020.
2.
Briggs AD Wolstenholme J Blakely T Scarborough P . Choosing an Epidemiological Model Structure for the Economic Evaluation of Non-communicable Disease Public Health Interventions. Popul Health Metr (2016) 14:17. 10.1186/s12963-016-0085-1
3.
Social Determinants of Health. World Health Organization. 2023. Available from: https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1 (Accessed September 12, 2024).
4.
Dummer TJ . Health Geography: Supporting Public Health Policy and Planning. CMAJ (2008) 178(9):1177–80. 10.1503/cmaj.071783
5.
Agarwal S Wade AN Mbanya JC Yajnik C Thomas N Egede LE et al The Role of Structural Racism and Geographical Inequity in Diabetes Outcomes. Lancet (2023) 402(10397):235–49. 10.1016/S0140-6736(23)00909-1
6.
Phillips SP . Defining and Measuring Gender: A Social Determinant of Health Whose Time Has Come. Int J Equity Health (2005) 4:11. 10.1186/1475-9276-4-11
7.
Miani C Wandschneider L Niemann J Batram-Zantvoort S Razum O . Measurement of Gender as a Social Determinant of Health in Epidemiology-A Scoping Review. PLoS One (2021) 16(11):e0259223. 10.1371/journal.pone.0259223
8.
Millett GA Jones AT Benkeser D Baral S Mercer L Beyrer C et al Assessing Differential Impacts of COVID-19 on Black Communities. Ann Epidemiol (2020) 47:37–44. 10.1016/j.annepidem.2020.05.003
9.
Disparities in the Risk and Outcomes of COVID-19. London, England: Public Health England. 2020. Available from: https://www.gov.uk/government/publications/covid-19-review-of-disparities-in-risks-and-outcomes (Accessed September 12, 2024).
10.
The L . The Plight of Essential Workers during the COVID-19 Pandemic. Lancet (2020) 395(10237):1587. 10.1016/S0140-6736(20)31200-9
11.
Ali S Asaria M Stranges S . COVID-19 and Inequality: Are We All in This Together?Can J Public Health (2020) 111(3):415–6. 10.17269/s41997-020-00351-0
12.
Moghadas SM Haworth-Brockman M Isfeld-Kiely H Kettner J . Improving Public Health Policy through Infection Transmission Modelling: Guidelines for Creating a Community of Practice. Can J Infect Dis Med Microbiol (2015) 26(4):191–5. 10.1155/2015/274569
13.
Page MJ McKenzie JE Bossuyt PM Boutron I Hoffmann TC Mulrow CD et al The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. Syst Rev (2021) 10(1):89. 10.1186/s13643-021-01626-4
14.
John-Baptiste A Moulin MS Ali S . Are COVID-19 Models Blind to the Social Determinants of Health? A Systematic Review Protocol. BMJ Open (2021) 11(7):e048995. 10.1136/bmjopen-2021-048995
15.
Pitman R Fisman D Zaric GS Postma M Kretzschmar M Edmunds J et al Dynamic Transmission Modeling: A Report of the ISPOR-SMDM Modeling Good Research Practices Task Force Working Group-5. Med Decis Making (2012) 32(5):712–21. 10.1177/0272989X12454578
16.
Weinstein MC O'Brien B Hornberger J Jackson J Johannesson M McCabe C et al Principles of Good Practice for Decision Analytic Modeling in Health-Care Evaluation: Report of the ISPOR Task Force on Good Research Practices--Modeling Studies. Value Health (2003) 6(1):9–17. 10.1046/j.1524-4733.2003.00234.x
17.
Castilho C Gondim JAM Marchesin M Sabeti M . Assessing the Efficiency of Different Control Strategies For the COVID-19 Epidemic. Electron J Differ Equ (2020) 17. 10.58997/ejde.2020.64
18.
Chatterjee K Kumar A Shankar S . Healthcare Impact of COVID-19 Epidemic in India: A Stochastic Mathematical Model. Med J Armed Forces India (2020) 76:147–55. 10.1016/j.mjafi.2020.03.022
19.
Duczmal LH Almeida ACL Duczmal DB Alves CRL Magalhaes FCO Lima MS et al Vertical Social Distancing Policy Is Ineffective to Contain the COVID-19 Pandemic. Cadernos de saude publica (2020) 36(5):e00084420. 10.1590/0102-311x00084420
20.
Chowdhury R Heng K Shawon MSR Goh G Okonofua D Ochoa-Rosales C et al Dynamic Interventions to Control COVID-19 Pandemic: A Multivariate Prediction Modelling Study Comparing 16 Worldwide Countries. Eur J Epidemiol (2020) 35(5):389–99. 10.1007/s10654-020-00649-w
21.
Krishnamurthy K Ambikapathy B Kumar A Britto LD . Prediction of the Transition from Subexponential to the Exponential Transmission of SARS-CoV-2 in Chennai, India: Epidemic Nowcasting. JMIR Public Health Surveill (2020) 6:e21152. 10.2196/21152
22.
Salje H Tran Kiem C Lefrancq N Courtejoie N Bosetti P Paireau J et al Estimating the Burden of SARS-CoV-2 in France. Science (New York, NY) (2020) 369(6500):208–11. 10.1126/science.abc3517
23.
Sjodin H Wilder-Smith A Osman S Farooq Z Rocklov J . Only Strict Quarantine Measures Can Curb the Coronavirus Disease (COVID-19) Outbreak in Italy, 2020. Eurosurveillance (2020) 25(13):2000280. 10.2807/1560-7917.ES.2020.25.13.2000280
24.
Truelove S Abrahim O Altare C Lauer SA Grantz KH Azman AS et al The Potential Impact of COVID-19 in Refugee Camps in Bangladesh and Beyond: A Modeling Study. PLoS Med (2020) 17(6):e1003144. 10.1371/journal.pmed.1003144
25.
Dizon RL . The Heterogeneous Age-Mixing Model of Estimating the COVID Cases of Different Local Government Units in the National Capital Region, Philippines. Clin Epidemiol Glob Health (2020). 10.1016/j.cegh.2020.06.003
26.
Moser DA Glaus J Frangou S Schechter DS . Years of Life Lost Due to the Psychosocial Consequences of COVID-19 Mitigation Strategies Based on Swiss Data. Eur Psychiatry : J Assoc Eur Psychiatrists (2020) 63(1):e58. 10.1192/j.eurpsy.2020.56
27.
Clark A Jit M Warren-Gash C Guthrie B Wang HHX Mercer SW et al Global, Regional, and National Estimates of the Population at Increased Risk of Severe COVID-19 Due to Underlying Health Conditions in 2020: A Modelling Study. The Lancet Glob Health (2020) 8(8):e1003–e1017. 10.1016/S2214-109X(20)30264-3
28.
Li XZ Jin F Zhang JG Deng YF Shu W Qin JM et al Treatment of Coronavirus Disease 2019 in Shandong, China: A Cost and Affordability Analysis. Infect Dis poverty (2020) 9(1):78. 10.1186/s40249-020-00689-0
29.
Kirigia JM Muthuri RNDK . The Fiscal Value of Human Lives Lost From Coronavirus Disease (COVID-19) in China. BMC Res Notes (2020) 13(1):198. 10.1186/s13104-020-05044-y
30.
Jewell BL Mudimu E Stover J Ten Brink D Phillips AN Smith JA et al Potential Effects of Disruption to HIV Programmes in Sub-Saharan Africa Caused by COVID-19: Results from Multiple Mathematical Models. The lancet HIV (2020) 7:e629–e640. 10.1016/S2352-3018(20)30211-3
31.
Qiu Y Chen X Shi W . Impacts of Social and Economic Factors on the Transmission of Coronavirus Disease 2019 (COVID-19) in China. J Popul Econ (2020) 33:1127–72. 10.1007/s00148-020-00778-2
32.
Kumar A Rani P Kumar R Sharma V Purohit SR . Data-Driven Modelling and Prediction of COVID-19 Infection in India and Correlation Analysis of the Virus Transmission With Socio-Economic Factors. Diabetes & Metab Syndr (2020) 14(5):1231–40. 10.1016/j.dsx.2020.07.008
33.
Pourghasemi HR Pouyan S Heidari B Farajzadeh Z Fallah Shamsi SR Babaei S et al Spatial Modeling, Risk Mapping, Change Detection, and Outbreak Trend Analysis of Coronavirus (COVID-19) in Iran (Days between February 19 and June 14, 2020). Int J Infect Dis : IJID : official Publ Int Soc Infect Dis (2020) 98:90–108. 10.1016/j.ijid.2020.06.058
34.
Mamode Khan N Soobhug AD Heenaye-Mamode Khan M . Studying the Trend of the Novel Coronavirus Series in Mauritius and its Implications. PloS one (2020) 15(7):e0235730. 10.1371/journal.pone.0235730
35.
Yu X . Risk Interactions of Coronavirus Infection across Age Groups After the Peak of COVID-19 Epidemic. Int J Environ Res Public Health (2020) 17(14):5246. 10.3390/ijerph17145246
36.
Sangiorgio V Parisi F . A Multicriteria Approach for Risk Assessment of Covid-19 in Urban District Lockdown. Saf Sci (2020) 130:104862. 10.1016/j.ssci.2020.104862
37.
Holmes L Jr. Enwere M Williams J Ogundele B Chavan P Piccoli T et al Black-White Risk Differentials in COVID-19 (SARS-COV2) Transmission, Mortality and Case Fatality in the United States: Translational Epidemiologic Perspective and Challenges. Int J Environ Res Public Health (2020) 17(12):4322. 10.3390/ijerph17124322
38.
Stedman M Lunt M Davies M Gibson M Heald A . COVID-19: Generate and Apply Local Modelled Transmission and Morbidity Effects to Provide an Estimate of the Variation in Overall Relative Healthcare Resource Impact at General Practice Granularity. Int J Clin Pract (2020) 74:e13533. 10.1111/ijcp.13533
39.
Kozlovskyi S Bilenko D Kuzheliev M Lavrov R Kozlovskyi V Mazur H et al The System Dynamic Model of the Labor Migrant Policy in Economic Growth Affected by COVID-19. Glob J Environ Sci Manag (2020) 6:95–106. 10.22034/GJESM.2019.06.SI.09
40.
Verhagen MD Brazel DM Dowd JB Kashnitsky I Mills MC . Forecasting Spatial, Socioeconomic and Demographic Variation in COVID-19 Health Care Demand in England and Wales. BMC Med (2020) 18(1):203. 10.1186/s12916-020-01646-2
41.
Shoukat A Wells CR Langley JM Singer BH Galvani AP Moghadas SM . Projecting Demand for Critical Care Beds during COVID-19 Outbreaks in Canada. CMAJ: Can Med Assoc J = J de l'Association medicale canadienne (2020) 192(19):E489-E496–E96. 10.1503/cmaj.200457
42.
Ogden NH Fazil A Arino J Berthiaume P Fisman DN Greer AL et al Modelling Scenarios of the Epidemic of COVID-19 in Canada. Can Commun Dis Rep = Releve des maladies transmissibles au Can (2020) 46(8):198–204. 10.14745/ccdr.v46i06a08
43.
Jamieson-Lane A Cytrynbaum E . Effects of Age-Targeted Sequestration for COVID-19. J Biol Dyn (2020) 14(1):621–32. 10.1080/17513758.2020.1795285
44.
Davies NG Klepac P Liu Y Prem K Jit M CMMID COVID-19 working group et al Age-Dependent Effects in the Transmission and Control of COVID-19 Epidemics. Nat Med (2020) 26(8):1205–11. 10.1038/s41591-020-0962-9
45.
Esteve A Permanyer I Boertien D Vaupel JW . National Age and Coresidence Patterns Shape COVID-19 Vulnerability. Proc Natl Acad Sci USA (2020) 117(28):16118–20. 10.1073/pnas.2008764117
46.
Griette Q Liu Z magal p . Estimating the End of the First Wave of Epidemic for COVID-19 Outbreak in Mainland China. medRxiv. 2020:
47.
Britton T Ball F Trapman P . A Mathematical Model Reveals the Influence of Population Heterogeneity on Herd Immunity to SARS-CoV-2. Science (2020) 369:846–9. 10.1126/science.abc6810
48.
Yu X Duan J Jiang Y Zhang H . Distinctive Trajectories of the COVID-19 Epidemic by Age and Gender: A Retrospective Modeling of the Epidemic in South Korea. Int J Infect Dis: IJID: official Publ Int Soc Infect Dis (2020) 98:200–5. 10.1016/j.ijid.2020.06.101
49.
Gosce L Phillips PA Spinola P Gupta DRK Abubakar PI . Modelling SARS-COV2 Spread in London: Approaches to Lift the Lockdown. The J Infect (2020) 81(2):260–5. 10.1016/j.jinf.2020.05.037
50.
Chikina M Pegden W . Modeling Strict Age-Targeted Mitigation Strategies for COVID-19. PloS one (2020) 15(7):e0236237. 10.1371/journal.pone.0236237
51.
Koo JR Cook AR Park M Sun Y Sun H Lim JT et al Interventions to Mitigate Early Spread of SARS-CoV-2 in Singapore: A Modelling Study. The Lancet Infect Dis (2020) 20(6):678–88. 10.1016/S1473-3099(20)30162-6
52.
Gerlee P Joud A Spreco A Timpka T . Computational Models Predicting the Early Development of the COVID-19 Pandemic in Sweden: Systematic Review, Data Synthesis, and Secondary Validation of Accuracy. Sci Rep (2022) 12(1):13256. 10.1038/s41598-022-16159-6
53.
Kimani TN Nyamai M Owino L Makori A Ombajo LA Maritim M et al Infectious Disease Modelling for SARS-CoV-2 in Africa to Guide Policy: A Systematic Review. Epidemics (2022) 40:100610. 10.1016/j.epidem.2022.100610
54.
den Boon S Jit M Brisson M Medley G Beutels P White R et al Guidelines for Multi-Model Comparisons of the Impact of Infectious Disease Interventions. BMC Med (2019) 17(1):163. 10.1186/s12916-019-1403-9
55.
Caro JJ Briggs AH Siebert U Kuntz KM Force I-SMGRPT . Modeling Good Research Practices--Overview: A Report of the ISPOR-SMDM Modeling Good Research Practices Task Force-1. Med Decis Making (2012) 32(5):667–77. 10.1177/0272989X12454577
56.
Jit M Brisson M . Modelling the Epidemiology of Infectious Diseases for Decision Analysis: A Primer. Pharmacoeconomics (2011) 29(5):371–86. 10.2165/11539960-000000000-00000
57.
Upshaw TL Brown C Smith R Perri M Ziegler C Pinto AD . Social Determinants of COVID-19 Incidence and Outcomes: A Rapid Review. PLoS One (2021) 16(3):e0248336. 10.1371/journal.pone.0248336
58.
Johnson K Biddell CB Hassmiller Lich K Swann J Delamater P Mayorga M et al Use of Modeling to Inform Decision Making in North Carolina during the COVID-19 Pandemic: A Qualitative Study. MDM Policy Pract (2022) 7(2):23814683221116362. 10.1177/23814683221116362
59.
Abuelezam NN Michel I Marshall BD Galea S . Accounting for Historical Injustices in Mathematical Models of Infectious Disease Transmission: An Analytic Overview. Epidemics (2023) 43:100679. 10.1016/j.epidem.2023.100679
Summary
Keywords
COVID-19, infectious disease models, social determinants of health, public health, model validity
Citation
John-Baptiste AA, Moulin M, Li Z, Hamilton D, Crichlow G, Klein DE, Alemu FW, Ghattas L, McDonald K, Asaria M, Sharpe C, Pandya E, Moqueet N, Champredon D, Moghadas SM, Cooper LA, Pinto A, Stranges S, Haworth-Brockman MJ, Galvani A and Ali S (2024) Do COVID-19 Infectious Disease Models Incorporate the Social Determinants of Health? A Systematic Review. Public Health Rev 45:1607057. doi: 10.3389/phrs.2024.1607057
Received
05 January 2024
Accepted
30 August 2024
Published
10 October 2024
Volume
45 - 2024
Edited by
Peter Francis Raguindin, University of Lucerne, Switzerland
Reviewed by
Diana Buitrago-Garcia, University of Geneva, Switzerland
Chepkoech Buttia, Epistudia GmbH, Switzerland
Updates
Copyright
© 2024 John-Baptiste, Moulin, Li, Hamilton, Crichlow, Klein, Alemu, Ghattas, McDonald, Asaria, Sharpe, Pandya, Moqueet, Champredon, Moghadas, Cooper, Pinto, Stranges, Haworth-Brockman, Galvani and Ali.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms. PHR is edited by the Swiss School of Public Health (SSPH+) in a partnership with the Association of Schools of Public Health of the European Region (ASPHER)+
*Correspondence: Ava A. John-Baptiste, ajohnbap@uwo.ca
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.