- 1Department of Occupational Health Science, University of Wuppertal, Wuppertal, Germany
- 2Institute for Medical Research and Occupational Health, Zagreb, Croatia
- 3University of Zagreb, School of Medicine, Andrija Štampar School of Public Health, Zagreb, Croatia
- 4Department of Epidemiology, Center for Public Health, Medical University of Vienna, Vienna, Austria
- 5Research Group, Institute of Occupational Medicine, Edinburgh, United Kingdom
- 6Centre for Occupational and Environmental Health, University of Manchester, Manchester, United Kingdom
- 7Estonian University of Life Sciences, Tartu, Estonia
- 8Department of Occupational Medicine, Faculty of Medicine, University of Tuzla, Tuzla, Bosnia and Herzegovina
- 9Department of Occupational and Environmental Health, Unisanté, University of Lausanne, Lausanne, Switzerland
- 10Department of Primary Care and Public Health, University of Leuven, Leuven, Belgium
- 11IDEWE, External Service for Prevention and Protection at Work, Heverlee, Belgium
Objectives: Work-related stress is highly prevalent. Recent systematic reviews concluded on a significant association between common work-related stress measures and depression. Our scoping review aims to explore whether work-related psychosocial stress is generally associated with depression or depressiveness, the extent and methodology of the primary research undertaken on this topic and to elucidate inconsistencies or gaps in knowledge.
Methods: We searched for literature in Pubmed, PsycInfo and Web of Science including full reports in seven languages published between 1999 and 2022 and applied the PRISMA statement for scoping reviews criteria.
Results: Of 463 primarily identified articles, 125 were retained after abstract and full-text screening. The majority report significant associations between work-related stress and depression. Cross-sectional studies are most prevalent. Sufficient evidence exists only for job strain and effort-reward imbalance. Most studies are from Asia, North America and Europe. The health sector is the most studied. Several research gaps such as the lack of interventional studies were identified.
Conclusion: The consistency of most studies on the significant association between work-related stress and depression is remarkable. More studies are needed to improve evidence and to close research gaps.
Introduction
Work-related stress is highly prevalent. In 2019 38 percent of workers globally reported experiencing high daily stress [1]. Occupational stress can be associated with absenteeism, presenteeism, low productivity or early work exits [2–6]. Moreover, occupational injuries can be associated with work-related stress [7]. Approximately 363,000 occupational fatalities and 26 million DALYs were caused by occupational injuries worldwide in 2016 [8]. For Europe, Australia and North America the annual costs of work-related stress to society were estimated between 221 million to 187 billion U.S. dollars, 70%–90% of which was caused by loss of productivity [9].
Apart from physical load, psychosocial factors can be a considerable source of stress at work. Half the workers in industrialized countries judge their work to be “mentally demanding” [10]. The working environment and the individual characteristics are fundamental in the development of work-related psychosocial stress [11]. According to the transactional theory of stress, the reaction to an environmental stimulus depends on the individual’s appraisal of it as challenging or threatening [12, 13]. The individual response to a stressful event can be different depending on the person’s coping strategy [14]. Health-related risks associated with chronic stress exposure can vary with genetic predisposition, epigenetic changes due to stressful early life experiences, and medical preconditions [15–17]. Work stress can influence employees’ health via a primary stress reaction with mediators (e.g., cortisol) and allostatic load affecting the cardiovascular, metabolic and immune systems and the brain [18, 19] or can lead to risky health behaviours (e.g., smoking or alcohol consumption) [20, 21]. Work-related stress is a risk factor for coronary heart disease [22] and type 2 diabetes mellitus [23]. Moreover, chronic stress exposure can impair mental health, with mild to severe subjective symptoms, burnout, psychosomatic and psychiatric diseases such as depressive disorders [7, 24–27].
Depressive and anxiety disorders are by far the most common mental disorders [28]. Approximately 12 billion working days are lost annually due to depression and anxiety, associated with cost of US$ 1 trillion by loss of productivity, globally [29]. In 2019 there were worldwide 279.6 million people (95% CI: 251.6–310.3) suffering from depression, which was 1.56-fold more frequent in women than in men [28]. Apart from significantly reduced life expectancy in both men and women after early onset of the depression [30], the occurrence and persistence of depressive symptoms significantly impact working life and the working environment. The estimated number of future employment years at the age of 30 for workers experiencing high depression symptoms throughout their working life, is more than 15 years shorter than for workers experiencing persistent low depression symptoms [31].
An imbalance between work demands and resources can contribute to work-related psychosocial stress [32–34]. About 30% of workers are in jobs with higher job demands than job resources in Europe, with between-country variation [35]. Health (45%), transport (42%) and agriculture (40%) are the sectors with the highest proportions of stressful jobs [35]. While this sector-specific prevalence of work-related stress is known, an overview of studies investigating the association between work-related stress and depression in different occupations is missing. Furthermore, it would be interesting to know which measurements for work-related stress and depression were used in studies investigating their association.
Often stress measurements are based on theoretical models. Two of the most investigated stress models, the job demand-control (JDC) model of Karasek [32] and the effort-reward-imbalance (ERI) model of Siegrist [33], and extensions of these, such as the job-demands-resources-model of Bakker and Demerouti [34], assume an imbalance between job demands and resources. Definitions of the latter differ depending on the stress model used. For instance, job resources can be non-monetary like decision latitude, a part of the JDC model, or monetary like wages, a part of the ERI model. Systematic reviews and meta-analyses have provided epidemiological evidence that work-related stress measured with ERI [26] and JDC [25, 27, 36] is associated with depressive symptoms or clinical depression. Yet, a comprehensive overview of the current state of research on the association between any measure of work-related stress and depression or depressiveness including research gaps and inconsistencies in knowledge is missing.
The aim of this scoping review of studies including data from 1999 to 2019 is to explore whether work-related psychosocial stress is associated with depression or depressive symptoms in general and to elucidate the research questions mentioned above:
1. Which occupational groups were most frequently investigated in the included studies on the association between work-related stress and depression or depressiveness?
2. Which measuring instruments of work-related psychosocial stress, as a whole or by individual components, were used in the identified studies?
3. Which measuring instruments of depression or depressive symptoms were used in the identified studies?
4. What knowledge exists on the relationship between work-related psychosocial stress and depression or depressiveness, in the identified studies?
5. What are the inconsistencies or gaps in knowledge regarding the factors contributing to the relationship between work stress and depression or depressiveness?
Methods
Protocol and Registration
This scoping review performed in accordance with the PRISMA Extension for Scoping Reviews guidelines [37] is based on a protocol registered at the Open Science Framework under registration number hg7r4-v1 [38].
Databases Used
A literature search was performed by two independent search teams in PubMed, Web of Science Core Collection and PsycInfo using predefined search strings and filters (Supplementary Table S1).
Eligibility Criteria
Primary research articles published between January 1999 and April 2022 in the form of full reports, focusing on the association of psychosocial work-related stress as the exposure and depression or depressive symptoms as the outcome measured with a questionnaire or a diagnostic interview were included. Only studies which finished data collection before December 2019 were considered, to avoid bias by any changes in the work environment introduced by the ensuing SARS-CoV 2 pandemic. We considered all forms of interventional and observational studies but no reviews, qualitative studies, abstracts, letters to the editor or commentaries. Only studies with employees, but not employers or managers were included, to focus on harmonised study groups. Publications in English, German, Bosnian, Croatian, French, Italian, Serbian and Serbo-Croatian were included according to the researchers’ language fluencies. Excluded were pharmacological studies, studies with unemployed persons or those focusing on physical stressors. Studies with mental comorbidities (except anxiety as a symptom of depressiveness) were excluded to avoid erroneous appraisal of the work-related stress effect on depression or depressiveness. The electronic search strategy can be found in Supplementary Table S1 in the online Supplementary Material.
Study Selection
Duplicates found in different literature data basis were excluded. The screening of studies found in the literature research followed two steps (Figure 1). First, titles and abstracts were independently screened by two reviewers against the inclusion and exclusion criteria. Then, full texts of the remaining articles were screened for inclusion and exclusion criteria by two reviewers. In both steps a third reviewer helped get agreement about in- or exclusion of articles when necessary.
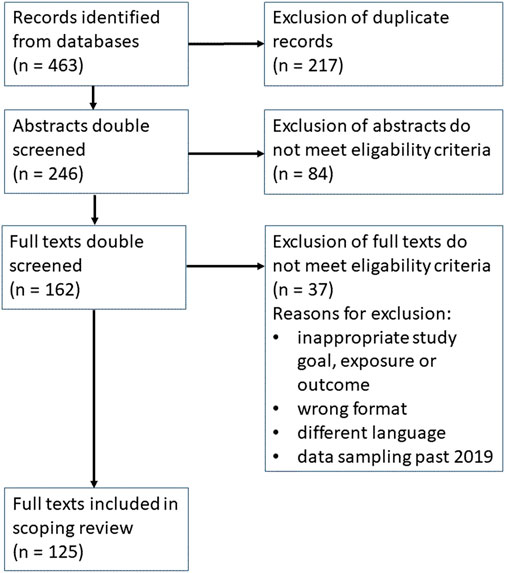
Figure 1. Identified studies in Pubmed, PsycInfo and Web of Science (scoping review on the relationship between work-related stress and depression, six continents, 1999–2022).
Data Extraction
A specially developed data extraction form was used by the reviewers to independently extract the data from eligible studies. Relevant information on key study characteristics and detailed information on all metrics used to estimate/describe work-related stress, depression/depressiveness and relevant information about covariates. The data-extraction process was conducted twice. Any inconsistencies and disagreements were resolved through discussion between the reviewers or with a third reviewer before transfer of results in Supplementary Table S2.
Finally, the study characteristics were reported in Supplementary Table S2, the number of studies per country and continent in Table 1 and the frequencies of the used exposure and outcome measurements in Supplementary Tables S3, S4.
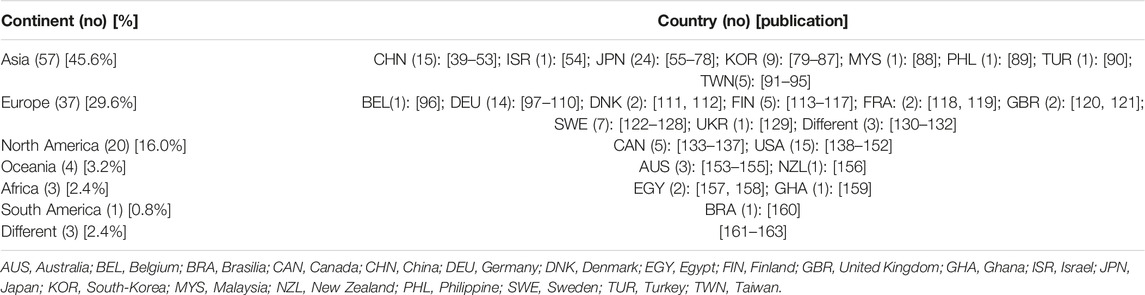
Table 1. Included studies per continent and country (scoping review on the relationship between work-related stress and depression, six continents, 1999–2022). (N = 125).
Synthesis of Results
Results were summarized narratively. We grouped the studies by 1) occupation, 2) types of stress measurement, 3) measurement of depression/depressiveness and 4) study type, and summarized the type of settings, populations and study designs for each group, along with the measurements used and broad findings.
Results
Of 463 articles identified in the literature searches after exclusion of duplicates and those not meeting the inclusion criteria in the title, abstract and full text screening, 125 studies [39–163] were included in the data extraction process (Figure 1).
The studies selected for analysis are charted in Supplementary Table S2. This provides information about study type and design (prospective or retrospective), continent and country, occupation, number of subjects, sociodemographic characteristics, occupational stress measure as the exposure, time of exposure measure, depression (categorized) or depressiveness (continuous) as the outcome, effect size of the association between exposure and outcome (incl. p-values and confidence intervals), factors adjusted for, a short summary of key findings and remarks when needed.
Study Characteristics
Among the articles included, 67.2% were cross-sectional studies, followed by cohort studies (20.0% prospective, 1.6% historical), other longitudinal studies (7.2%), interventional studies, including one RCT (2.4%), one case-control-study (0.8%) and one clinical non-interventional study (0.8%) (Supplementary Table S2).
Occupational Groups
Analysed studies included healthcare workers (24.0%), manufacturing workers (7.2%), education/teachers (4.0%), public servants (4.0%), emergency workers (2.4%), farmers and fishermen (2.4%), clergy (1.6%) and managers/executives (1.6%). Most studies (36.0%) included employees from different occupations (Supplementary Table S2).
Nurses, nearly all female, were the most common studied occupational group in 16 studies, with composite measurements or singular components of work stress showing a significant association with depression. Physicians (14 studies) were the second most frequent group, with the ERI questionnaire being the most frequently used stress measurement (42.9%). 85.7% of doctors’ studies found significant associations between work-related stress and depression or depressiveness. Support from co-workers, working shorter hours and not working at weekends may lead to a risk reduction [67, 109].
Manufacturing workers were represented with nine studies, all but one [138] conducted in Asia. Five studies focused on teachers and public servants, three studies on emergency workers and farmers/fishermen and two on clergy and managers/executives. The remaining 66 studies addressed occupations by only a single study (12), different occupations in one study (45) or the occupations were not stated (9).
Overall, beside nurses, physicians and manufacturing workers the number of studies investigating this association in other occupations is limited.
Measuring Instruments of Work-Related Psychosocial Stress
Measurement instruments of work-related psychosocial stress were most frequently based on Karasek’s JDC model [32]: seventeen studies used the JDC questionnaire, 10 of these without, and seven including the support component (JDC-S). Different versions of the Job Content Questionnaire (JCQ) were used in 22 studies, half of them with and half without the support component. Other instruments related to JDC were the Brief Job Stress Questionnaire (BJSQ) (7), the Child Care Worker Job Stress Inventory (CCW-JSI) (2), the Job Stress Scale (JSS) (1), the Brief Stress Scale (BSS) (1), the Work Stress Scale (1), the Copenhagen Psychosocial Questionnaire (2), the Shortened Stress Evaluation Tool (1), and the Psychosocial Leave-Behind Questionnaire (1) (Supplementary Table S3).
Second most common (26.4%) were stress measurements based on Siegrist’s ERI model [33]. Eight studies applied the original, 14 studies long and 11 studies short versions of the ERI-questionnaire. Twenty studies included measurements of the extrinsic (efforts and rewards) and the intrinsic component (overcommitment) of the ERI model and 13 studies the extrinsic component alone. Thirteen studies combined ERI components with other stress measurements. Furthermore, country-specific and modified versions of the ERI-instrument were often used.
7.2% of studies used the Generic Job Stress Questionnaire developed by the US National Institute for Occupational Safety and Health (NIOSH-GJSQ) [164]. The Korean Occupational Stress Scale (KOSS) [165] (6.4%) includes items from the JCQ, ERI and NIOSH-GJSQ. One study [47] applied the Job Burden-Capital Matching Model [166] which combines questions from the JCQ and ERI. Thirty-eight studies used a variety of stress assessment tools including perceived stress measures [167, 168], occupation specific instruments [169–173] and instruments focused on certain stressful aspects like workplace bullying [174]. One study [128] used a Job-exposure-Matrix (JEM), including job demand and control items to classify jobs, with respect to the stress prevalence and identify those corresponding to a stressful work environment. JEM is a widely used exposure assessment tool in occupational epidemiology, especially when individual exposure measurement data are unavailable [175].
Altogether, the majority of studies used stress measurements based on the JDC- and ERI-model or components of them followed by the NIOSH-GJSQ.
Measuring Instruments of Depression or Depressive Symptoms
The most common instrument to assess depression or depressive symptoms (n = 57) was the Center for Epidemiological Survey-Depression Scale (CES-D) [176], used in its original, or long, short, or modified version and in different languages. Sixteen studies used the Beck Depression Inventory (BDI) [177], and 12 studies the Patient Health Questionnaire (PHQ) [178]. Other commonly used tools include Zung’s Self-Rating Depression Scale [179], EURO-D depression scale [180] and the Hopkins Symptom Checklist [181], to name only a few. Five studies used ICD-9 or ICD-10 diagnoses; three studies relied on DSM-IV Diagnosis. Only three studies created ad hoc scales. One of them a 5-item scale assessed feelings over the past 4 weeks. Another one assessed two domains of depression in the past 2 months (Supplementary Table S4).
In summary, most of the studies applied validated measurements of depression or depressiveness. CES-D, BDI or PHQ were most commonly used.
Existing Knowledge on the Relationship Between Work-Related Psychosocial Stress and Depression or Depressive Symptoms
High job strain (high job demands, low control) as measured by JDC, JDC-S, JCQ, JSS, KOSS, BJSQ, CCW-JSI or Job Burden-Capital Matching Model was associated with depressiveness or depression in most of cross-sectional and longitudinal studies. Yet, in some studies only components of the JDC-model (e.g., control) were significantly associated with depression or depressiveness cross-sectionally [39, 76, 81, 97, 143, 151] or longitudinally [115, 117, 131, 138, 143, 152, 161, 162]. Social support was negatively associated with depressiveness in one cross-sectional study [141], but not in another [48] nor in two cohort studies [73, 126] (Supplementary Table S2).
Effort-reward ratio (ERI-R) [182], or components of the ERI-model were significantly associated with depressiveness or depression in most cross-sectional and all longitudinal studies. In one cross-sectional study the significant association disappeared after adjustment for burn-out [53]. Two studies found the strongest association either with personal [102] or organisational rewards [77]. Both found monetary rewards to be the weakest. The length of working hours was also found to affect the association [74, 109]. A longitudinal study found comparable strengths of association between ERI and depression for women and men [107], another observed a significant association between ERI and depressiveness over time in Europe, but not in the United States or Japan [162]. An interventional study found that reducing ERI-stress through interpersonal psychotherapy was more effective than standard therapy [108]. Overcommitment, independent of the extrinsic component of the ERI-model, has been linked to depression or depressiveness cross-sectionally [44, 46, 71, 74, 76, 98–100, 103, 155] and longitudinally [101, 107, 118]. Some studies found a significant bivariate association without controlling for confounders [40, 102, 119]. Studies combining components of ERI and JDC independently have shown an association with depressive symptoms or depression cross-sectionally [76, 98, 136] and longitudinally [130, 144, 161].
Most cross-sectional studies [55, 56, 65, 66, 69, 74, 78] and a longitudinal study [57] found dimensions of the NIOSH-GJSQ, such as role ambiguity or low job control associated with depression or depressive symptoms. Most studies using KOSS [79, 80, 82–85, 87] found at least one component significantly associated with depression or depressiveness. Less often used stress assessment tools were also significantly associated with depressiveness or depression in cross-sectional [41–43, 48–50, 52, 59, 60, 62, 80, 91, 92, 94, 110, 139–141, 145, 146, 148, 149, 157, 163] and longitudinal studies [137, 142, 150] (for effect strength of the association under review see Supplementary Table S2).
Region
The majority of studies were conducted in Asia, Europe and North America, less frequent were studies from Oceania, Africa, South America or transcontinental regions. Over half were conducted in Japan, United States, China and Germany (Table 1). A cross-country comparison between United States, Europe and Japan [162] found for ERI and low job control a significant cross-sectional link to depression except low control in Japan. Significant longitudinal associations were found for these stress measurements only in Europe (Supplementary Table S2).
Gender
A study found a stronger association between work-related stress (JCQ) and depression for female employees in public administration [96], while male automotive manufacture workers with higher socioeconomic status were more vulnerable to interpersonal conflict [56]. Job demands were significantly associated with depression only in men, both cross-sectionally [84, 127] and longitudinally [54]. Conversely, organizational injustice and low influence at work were risk factors and support from superiors and fellow workers protective factors only in females [84, 112, 127]. In other studies, job strain [72, 124] and demands [68, 87] were significantly associated with depressiveness or depression in both genders, with a stronger effect in men. Job control [87, 112] and job security [87] were significant risk factors for depression only in men and organizational injustice only in women [87]. The association between the ERI-ratio and depressive symptoms was stronger in men in Germany [100], but no significant gender-specific differences in this association has been observed in Europe longitudinally [107]. A bidirectional longitudinal association between work-related stress measured by workload and job control and depressiveness has been shown in men [54].
Age
In older employees (50+) significant longitudinal associations between ERI [130, 132, 144, 161, 162] and job strain [130, 144] or control [161, 162] and depression and depressiveness, and cross-sectional evidence of this association for some other stress measurements [50, 149] were found. However, no studies focused on employees younger than 25, and while two studies showed a higher risk for depression in employees under 30, no age stratified analysis was found.
Mediators
Work-related psychosocial stress and depressiveness are linked through various mediators: Job strain [32] and depressive symptoms were mediated by burn-out cross-sectionally [53, 95, 114, 139], while longitudinal evidence is limited to dentists and two study waves [113, 115]. Sleep quality was another mediator in this association among psychiatric nurses [95]. For ERI and depressiveness mediating effects of psychosocial capital [44] and work-family conflict have been found cross-sectionally [100]. Moreover, ERI can partly explain the social inequality in depressiveness [99, 130].
Moderators
Social support, job autonomy, job satisfaction and job security can moderate (“buffer”) the negative effect of different job stressors on depression [39, 43, 68, 137]. Furthermore, an interaction between hair cortisol level and work stress (MSIQ) on depression in fishermen was observed [51]. Severe work-related stress may curtail as a moderator the protective effect of spirituality on depression [89]. Moreover, a reduction of work stress has been reported when reducing working hours [109].
Overall, most studies (n = 115) found a statistically significant association between work-related stress and depression or depressiveness, at least for some measurements, regardless of study type, period and region, occupational group, sociodemographic differences and the measuring instruments and form (self-reported or doctor’s diagnosis). The majority of studies are from Asia, Europe and North America. Some studies indicate that organizational injustice increases the risk of depression in women and job insecurity in men.
Inconsistencies and Gaps in Knowledge
Sociodemographics
Studies on employees under the age of 25 on the association between work stress and depression are missing. Studies on gender-specific differences in this association are limited, with inconsistencies between studies using specific measures, e.g., regarding the protective effect of social support. More gender-specific or -stratified studies are needed to explain these differences.
Study Type
Only three interventional studies were identified: One was a stress-management programme [63] and another a workplace promotion programme [88], both for manufacturing workers. A third was a work-focused interpersonal psychotherapy programme for clinically diagnosed depression [108]. While all of these interventions were effective, interventional studies with more participants, different occupations and forms of stress interventions are needed.
Bias
One study concludes that reporting bias may inflate associations between high psychological demands and low decision latitude at work and the occurrence of depression [111]. Another suggests that there may be a substantial under-recognition and under-compensation of job strain-attributable depression [154].
Mediators and Moderators
More, especially longitudinal studies, are needed on factors mediating or moderating the association between work-related psychosocial stress and depressiveness or depression.
Measurement of Work-Related Psychosocial Stress
Studies show that various measures of work-related psychosocial stress contribute independently to depression [76, 98, 130, 136, 144, 161]. Reforms of mainstream models, like the job burden-capital model [155] integrate JDC, ERI and intrinsic personality factors. However, more investigation is needed to understand the independent influences of the different facets of psychosocial work-related stress on depression.
Altogether, gender specific inconsistencies exist in research on the association between certain work-related stress measures and depression. No studies were found for employees younger than 25. More interventional studies, research on bias, moderators and mediators of this association and studies on composite stress measurements are needed.
Discussion
This scoping review provides new insights on the relationship between work-related stress and depression or depressiveness by including 125 studies from five continents over more than two decades. However, study data were only considered until the end of 2019 to avoid bias through additional stress or mood disturbances introduced by the SARS-CoV-2-pandemic [183]. Since the SARS-CoV-2-pandemic may have caused enduring changes in working conditions, this ought to be addressed in future studies.
We found large geographical differences in the state of research on this topic: Most studies came from Asia, Europe and North America, but only few from Oceania, Africa and South America. Transcontinental and transnational studies were scarce. Results on the association between work stress and depression, however, were surprisingly consistent regardless of geographic location. The healthcare sector has been most frequently investigated on this topic.
Consistent with an earlier review [36] we found Karasek’s job strain model [32] including instruments derived from it, to be the most commonly applied measure of work-related psychosocial stress followed by measuring instruments based on Siegrist’s ERI model [33]. CES-D was the instrument most commonly used to measure depression or depressiveness, followed by the BDI and the PHQ. Studies with a clinical diagnosis of depression were rare. The evidence for the association between job strain and ERI and depression seems to be sufficient given the high percentage of longitudinal and cross-sectional studies which found significant associations in line with meta-analyses [25–27]. Interestingly, studies which included components of job strain and ERI to measure work stress, found independent associations of both, with depression/depressiveness [76, 98, 130, 144, 161] indicating that both models identify different aspects of stressful work conditions. Different stress measurements may also be more or less appropriate for certain job types [76]. Under the high number of studies using other instruments to measure work stress than job strain or ERI only four longitudinal studies were identified [57, 140, 142, 150]. Nevertheless, the prevailing congruence in significant associations between psychosocial work stress and depression or depressiveness in cross-sectional and longitudinal studies using a variety of instruments to measure work stress and depression or depressiveness is remarkable. However, heterogeneity in results was found regarding the association of social support and depression regarding study types [73, 126, 141] and gender aspects [54, 112, 127].
Many studies have focused on specific occupational groups. It is warranted to consider potential limitations of this approach: The JCQ, which derives its cut-offs based on the respective population means [184], will be of limited usefulness if the range of job stress in a given occupational population is narrow (e.g., if all participants are working in nursing, with similar job demands and control). Associations may appear inflated in such studies, and would not be comparable to other occupational groups with different work stress exposures. Likewise, comparisons of study results on specific occupational groups with others can be difficult when using ERI-tertiles or -quartiles derived from the population under study [182]. We recognize the necessity to focus on specific occupational sub-groups to investigate specific job-related aspects in the association between work-related stress and depression and also for practical reasons. However, scientists should be aware of these methodological limitations when using stress measurements related to the population under study.
Furthermore, we acknowledge the importance of considering individual differences and contextual factors in explaining heterogeneity. While our review primarily focuses on psychological and sociological responses, integrating biological markers like allostatic load and epigenetics can offer a comprehensive understanding of the mechanisms underlying diverse responses to the phenomenon under study. By incorporating these multidimensional perspectives, future research can better elucidate the complex interplay between psychological, sociological, and biological factors in shaping individual variations in response.
One limitation of our scoping review is that psychometric tools used in some studies to assess depression have not been previously validated. However, when comparing results from these studies with others using validated depression instruments, we found largely similar results. Thus, a strength of this scoping review is to demonstrate the utility of these studies which may otherwise have been discarded based on their potentially weak outcome assessments.
Similarly, measurements of work stress varied greatly in our scoping review though the majority centred around two well established instruments (JDC and ERI). An interesting outcome of our review is that the association between work-related stress and depression was apparent, regardless of which measure used and which study type applied. Even though random misclassification in these unvalidated exposure assessments and publication bias cannot be ruled out, the consistency of this association makes it generally more probable in terms of plausibility.
Several research gaps of note were identified: Firstly, there is a lack of interventional studies, to investigate the effect of work stress alleviating interventions on depression prevention. Secondly, improved work-related stress assessment tools are needed incorporating different known and potentially novel stressors (e.g., dissolving boundaries at home office) in future studies. Our review focused on the pre-pandemic period as it is conceivable that pandemic-related changes could impact the association between work stress and depression. Nonetheless, our review aims to provide a reference basis for future studies. Moreover, some groups, such as younger workers are severely under-investigated. Presumably, because available measuring instruments of work stress do not include important stressful aspects (conflicts between work and school or study) and are created for full-time employment which is often not the case for younger employees [185]. Therefore, assessment tools focusing on stress items relevant to younger adults are required.
The strengths of our scoping review relate to the assessment of the association of work-related stress as the exposure, and depression as the outcome, irrespective of measurements used, or study designs implemented—providing for the first time a comprehensive picture of the existing literature. Another strength is its focus on the pre-pandemic time, alleviating any concerns regarding how work-related changes during the pandemic might have changed the work-stress profile of workers.
In conclusion, our results will serve as guidance for employers and employees alike to pay more attention to work stress given its impact on workers’ depression risk and its potential long-lasting consequences for the work ability of our future workforce. Moreover, the research gaps identified in this scoping review should be addressed in future studies.
Authors Contributions
J-BdP and ES developed the research question and study concept. AKB, J-BdP, LH, and ZF created the search strings and performed the literature search. AKB, EM, J-BdP, LH, NP, and ZF were involved the abstract screening and AKB, DM, EM, ES, HB, J-BdP, LH, LG, NP, and ZF in the full text screening. J-BdP drafted the manuscript and all authors contributed in writing and improvement. All authors contributed to the preparation of tables and the graph and LH and J-BdP finalized them. All authors contributed to the article and approved the submitted version.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. The work of AB and ZF was partly funded by the European Union—Next-Generation EU (Program Contract of 8 December 2023, Class: 643-02/23-01/00016, Reg. no. 533-03-23-0006). All authors acknowledge support from the Open Access Publication Fund of the University of Wuppertal. The authors did not receive any further funding by a third party for this publication. The responsibility for the content of this publication lies with the authors.
Conflict of Interest
DM is employed by Research Group, Institute of Occupational Medicine.
The remaining authors declare that they do not have any conflicts of interest.
Acknowledgments
This publication is based upon work from COST Action CA16216 (OMEGA-NET), supported by COST (European Cooperation in Science and Technology). We want to thank the OMEGA.net core group, especially Ingrid Sivesind Mehlum and Maria Albin for their support.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/phrs.2024.1606968/full#supplementary-material
References
1. Gallup. State of the Global Workplace 2023 Report (2023). Available from: https://www.gallup.com/workplace/349484/state-of-the-global-workplace.aspx (Accessed March 20, 2024).
2. ILO. Stress Prevention at Work Checkpoints. Practical Improvements for Stress Prevention in the Workplace. Geneva: International Labour Office (2012). Available from: https://www.ilo.org/wcmsp5/groups/public/---dgreports/---dcomm/---publ/documents/publication/wcms_168053.pdf (Accessed May 24, 2023).
3. Du Prel, JB, March, S, Schröder, H, and Peter, R. Occupational Gratification Crisis and Sickness Absence in Germany: Cross-Sectional Results From the lidA-Study. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz (2015) 56:996–1004. doi:10.1007/s00103-015-2207-5
4. Levi, L. Bridging the Science-Policy and Policy-Implementation Gaps. In: CL Cooper, and J Campbell, editors. The Handbook of Stress and Health: A Guide to Research and Practice. West Sussex, UK: Wiley-Blackwell (2017). p. 7–23.
5. Brunner, B, Igic, I, Keller, AC, and Wiese, S. Who Gains the Most From Improving Working Conditions? Health-Related Absenteeism and Presenteeism Due to Stress at Work. Eur J Health Econ (2019) 20:1165–80. doi:10.1007/s10198-019-01084-9
6. Stengård, J, Leineweber, C, Virtanen, M, Westerlund, H, and Wang, HX. Do Good Psychosocial Working Conditions Prolong Working Lives? Findings From the Prospective Study in Sweden. Eur J Ageing (2021) 19:677–88. doi:10.1007/s10433-021-00672-0
7. J In: LaDou, and RJ Harrison, editors. CURRENT Diagnosis and Treatment: Occupational and Environmental Medicine, 6e. New York: McGraw Hill (2021). Available from: https://accessmedicine.mhmedical.com/content.aspx?bookid=3065§ionid=255628483 (Accessed November 18, 2023).
8. World Health Organization. WHO/ILO Joint Estimate of the Work-Related Burden of Disease and Injury, 2000-2016. Global Monitoring Report. Geneva: World Health Organization and International Labour Organization (2021). Available from: https://www.who.int/publications/i/item/9789240034945 (Accessed February 19, 2023).
9. Hassard, J, Teoh, KRH, Visockaite, G, Dewe, P, and Cox, T. The Cost of Work-Related Stress to Society: A Systematic Review. J Occup Health Psychol (2018) 23:1–17. doi:10.1037/ocp0000069
10. Houtman, I, and Jettinghoff, K. Raising Awareness of Stress at Work in Developing Countries. A Modern Hazard in a Traditional Working Environment. Netherlands: WHO (2007). Available from: https://www.who.int/publications/i/item/924159165X ([Accessed November 18, 2023).
11. Glazer, S, and Liu, C. Work, Stress, Coping, and Stress Management. Oxford: Oxford Research Encyclopedia of Psychology (2017). doi:10.1093/acrefore/9780190236557.013.30
12. Folkman, S, and Lazarus, RS. If It Changes It Must Be a Process: Study of Emotion and Coping During Three Stages of a College Examination. J Pers Soc Psychol (1985) 48:150–70. doi:10.1037/0022-3514.48.1.150
13. Cooper, CL, and Quick, JC. The Handbook of Stress and Health: A Guide to Research and Practice. Chichester: Whiley Blackwell (2017). p. 728.
14. Peter, R. Von Handlungs-Und Entscheidungsspielräumen, Belohnungen und Betrieblicher Gerechtigkeit: Die Modelle Demand-Control und Berufliche Gratifikationskrisen. In: G Faller, editor. Lehrbuch Betriebliche Gesundheitsförderung. Bern: Hogrefe Verlag (2016). p. 111–23.
15. Ising, M, and Holsboer, F. Genetics of Stress Response and Stress-Related Disorders. Dialogues Clin Neurosci (2006) 8:433–44. doi:10.31887/DCNS.2006.8.4/mising
16. Bakusic, J, Lavreysen, O, and Godderis, L. Genetics, Epigenetics, and Mental Health at Work. In: M Wahrendorf, T Chandola, and A Descatha, editors. Handbook of Life Course Occupational Health. Handbook Series in Occupational Health Sciences. Springer (2023). p. 157–74. doi:10.1007/978-3-030-94023-2_27-1
17. Cholesterol Treatment Trialists (CTT) Collaboration, Baigent, C, Blackwell, L, Emberson, J, Holland, LE, Reith, C, et al. Efficacy and Safety of More Intensive Lowering of LDL Cholesterol: A Meta-Analysis of Data From 170,000 Participants in 26 Randomised Trials. Lancet (2010) 376:1670–81. doi:10.1016/S0140-6736(10)61350-5
18. McEwen, BS, and Stellar, E. Stress and the Individual. Mechanisms Leading to Disease. Arch Intern Med (1993) 153:2093–101. PMID: 8379800. doi:10.1001/archinte.1993.00410180039004
19. McEwen, BS, and Gianaros, PJ. Stress- and Allostasis-Induced Brain Plasticity. Annu Rev Med (2011) 62:431–45. doi:10.1146/annurev-med-052209-100430
20. Kouvonen, A, Kivimäki, M, Virtanen, M, Pentti, J, and Vahtera, J. Work Stress, Smoking Status, and Smoking Intensity: An Observational Study of 46,190 Employees. J Epidemiol Community Health (2005) 59:63–9. doi:10.1136/jech.2004.019752
21. Kouvonen, A, Kivimäki, M, Elovainio, M, Väänänen, A, De Vogli, R, Heponiemi, T, et al. Low Organisational Justice and Heavy Drinking: A Prospective Cohort Study. Occup Environ Med (2008) 65:44–50. doi:10.1136/oem.2007.032755
22. Dragano, N, Siegrist, J, Nyberg, ST, Lunau, T, Fransson, EI, Alfredsson, L, et al. Effort–Reward Imbalance at Work and Incident Coronary Heart Disease. A Multicohort Study of 90,164 Individuals. Epidemiology (2017) 28:619–26. doi:10.1097/EDE.0000000000000666
23. Pena-Gralle, APB, Talbot, D, Duchaine, CS, Lavigne-Robichaud, M, Trudel, X, Aubé, K, et al. Job Strain and Effort-Reward Imbalance as Risk Factors for Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis of Prospective Studies. Scand J Work Environ Health (2022) 48:5–20. doi:10.5271/sjweh.3987
24. Lupien, SJ, Ouellet-Morin, I, Hupbach, A, Tu, MT, Buss, C, Walker, D, et al. Beyond the Stress Concept: Allostatic Load--a Developmental Biological and Cognitive Perspective. In: D Cicchetti, and DJ Cohen, editors. Developmental Psychopathology, Volume 2, Developmental Neuroscience. 2nd ed. Wiley (2006). p. 578–628.
25. Madsen, IEH, Nyberg, ST, Hanson, LM, Ferrie, JE, Ahola, K, Alfredsson, L, et al. Job Strain as a Risk Factor for Clinical Depression: Systematic Review and Metaanalysis With Additional Individual Participant Data. Psychol Med (2017) 47:1342–56. doi:10.1017/S003329171600355X
26. Rugulies, R, Aust, B, and Madsen, IEH. Effort-Reward Imbalance at Work and Risk of Depressive Disorders. A Systematic Review and Meta-Analysis of Prospective Cohort Studies. Scand J Work Environ Health (2017) 43:294–306. doi:10.5271/sjweh.3632
27. Seidler, A, Schubert, M, Freiberg, A, Drössler, S, Hussenoeder, FS, Conrad, I, et al. Psychosocial Occupational Exposures and Mental Illness. Dtsch Arztebl Int (2022) 119:709–15. doi:10.3238/arztebl.m2022.0295
28. GBD 2019 Mental Disorders Collaborators. Global, Regional, and National Burden of 12 Mental Disorders in 204 Countries and Territories, 1990–2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry (2022) 9:137–50. doi:10.1016/S2215-0366(21)00395-3
29. WHO. Mental Health at Work. Geneva. Switzerland: World Health Organization(2022). Available from: https://www.who.int/news-room/fact-sheets/detail/mental-health-at-work (Accessed November 18, 2023).
30. Laursen, TM, Musliner, KL, Benros, ME, Vestergaard, M, and Munk-Olsen, T. Mortality and Life Expectancy in Persons With Severe Unipolar Depression. J Affect Disord (2016) 193:203–7. doi:10.1016/j.jad.2015.12.067
31. Dobson, KG, Gignac, MAM, and Mustard, CA. The Working Life Expectancy of American Adults Experiencing Depression. Soc Psychiatry Psychiatr Epidemiol (2023). doi:10.1007/s00127-023-02547-4
32. Karasek, RA. Job Demands, Job Decision Latitude, and Mental Strain: Implications for Job Redesign. Adm Sci Q (1979) 24:285–308. doi:10.2307/2392498
33. Siegrist, J. Adverse Health Effects of High-Effort/low-Reward Conditions. J Occup Health Psychol (1996) 1:27–41. doi:10.1037/1076-8998.1.1.27
34. Bakker, AB, and Demerouti, E. The Job Demands-Resources Model: State of the Art. J Manag Psychol (2007) 22:309–28. doi:10.1108/02683940710733115
35. Eurofound. Working Conditions in the Time of COVID-19: Implications for the Future, European Working Conditions Telephone Survey 2021 Series. Luxembourg: Publications Office of the European Union (2022). Available from: https://www.eurofound.europa.eu/system/files/2023-01/ef22012en.pdf (Accessed November 18, 2023).
36. Theorell, T, Hammarström, A, Aronsson, G, Bendz, LT, Grape, T, Hogstedt, C, et al. A Systematic Review Including Meta-Analysis of Work Environment and Depressive Symptoms. BMC Public Health (2015) 15:738. doi:10.1186/s12889-015-1954-4
37. Tricco, AC, Lillie, E, Zarin, W, O'Brien, KK, Colquhoun, H, Levac, D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med (2018) 169:467–73. doi:10.7326/M18-0850
38. Du Prel, JB, Koscec Bjelajac, A, Franic, Z, Henftling, L, Brborovic, H, Schernhammer, E, et al. Relationship Between Work-Related Stress and Depression/Depressive Symptoms: A Scoping Review. Study Protoc (2020). Available from: https://osf.io/4z5js/?view_only=47b7263f1b83441d90651cf23a746af2 (Accessed January 17, 2024).
39. Chen, WQ, Siu, OL, Lu, J-F, Cooper, CL, and Phillips, DR. Work Stress and Depression: The Direct and Moderating Effects of Informal Social Support and Coping. Stress and Health (2009) 25:431–43. doi:10.1002/smi.1263
40. Han, X, Li, Q, Wang, C, and Li, Y. The Association of Occupational Stress and Depressive Symptoms Among Employed Persons With Benign Breast Disease: The Mediating Role of Psychological Capital. Psychopathology (2019) 52:205–11. doi:10.1159/000501164
41. He, SC, Wu, S, Wang, C, Du, XD, Yin, G, Jia, Q, et al. Interaction Between Job Stress and the BDNF Val66Met Polymorphism Affects Depressive Symptoms in Chinese Healthcare Workers. J Affect Disord (2018) 236:157–63. doi:10.1016/j.jad.2018.04.089
42. Jiang, H, Li, S, and Yang, J. Work Stress and Depressive Symptoms in Fishermen With a Smoking Habit: A Mediator Role of Nicotine Dependence and Possible Moderator Role of Expressive Suppression and Cognitive Reappraisal. Front Psychol (2018) 9:386. doi:10.3389/fpsyg.2018.00386
43. Li, Q, Chi, P, Hall, BJ, Wu, Q, and Du, H. Job Stress and Depressive Symptoms Among Migrant Workers in Macau: A Moderated Mediation Model of Self-Esteem and Perceived Social Support. Psych J (2019) 8:307–17. doi:10.1002/pchj.298
44. Liu, L, Chang, Y, Fu, J, Wang, J, and Wang, L. The Mediating Role of Psychological Capital on the Association Between Occupational Stress and Depressive Symptoms Among Chinese Physicians: A Cross-Sectional Study. BMC Public Health (2012) 12:219. doi:10.1186/1471-2458-12-219
45. Shang, L, Riedel, N, Loerbroks, A, Müller, A, Wege, N, Angerer, P, et al. The Association Between Effort-Reward Imbalance and Depressive Symptoms Is Modified by Selection, Optimization, and Compensation Strategy. J Occup Environ Med (2015) 57:1222–7. doi:10.1097/jom.0000000000000546
46. Shen, X, Yang, YL, Wang, Y, Liu, L, Wang, S, and Wang, L. The Association Between Occupational Stress and Depressive Symptoms and the Mediating Role of Psychological Capital Among Chinese University Teachers: A Cross-Sectional Study. BMC Psychiatry (2014) 14:329. doi:10.1186/s12888-014-0329-1
47. Wang, C, Li, S, Li, T, Yu, S, Dai, J, Liu, X, et al. Using the Job Burden-Capital Model of Occupational Stress to Predict Depression and Well-Being Among Electronic Manufacturing Service Employees in China. Int J Environ Res Public Health (2016) 13:819. doi:10.3390/ijerph13080819
48. Wu, H, Ge, CX, Sun, W, Wang, JN, and Wang, L. Depressive Symptoms and Occupational Stress Among Chinese Female Nurses: The Mediating Effects of Social Support and Rational Coping. Res Nurs Health (2011) 34:401–7. doi:10.1002/nur.20449
49. Li, W, Sun, F, Li, Y, and Durkin, DW. Work Stress and Depressive Symptoms in Chinese Migrant Workers: The Moderating Role of Community Factors. J Immigr Minor Health (2019) 21:1248–56. doi:10.1007/s10903-018-0843-1
50. Sun, F, Li, W, Jiang, L, and Lee, J. Depressive Symptoms in Three Chinese Older Workforce Groups: The Interplay of Work Stress With Family and Community Factors. Int Psychogeriatr (2020) 32:217–27. doi:10.1017/s1041610219000528
51. Wu, Y, Li, S, Hu, K, and Yang, J. Evidence of the Moderating Role of Hair Cortisol and Hair Cortisone in the Relationship Between Work Stress and Depression Symptoms Among Chinese Fishermen. J Affect Disord (2021) 294:868–75. doi:10.1016/j.jad.2021.06.023
52. Yang, X, Qiu, D, Lau, MCM, and Lau, JTF. The Mediation Role of Work-Life Balance Stress and Chronic Fatigue in the Relationship Between Workaholism and Depression Among Chinese Male Workers in Hong Kong. J Behav Addict (2020) 9:483–90. doi:10.1556/2006.2020.00026
53. Yong, X, Gao, X, Zhang, Z, Ge, H, Sun, X, Ma, X, et al. Associations of Occupational Stress With Job Burn-Out, Depression and Hypertension in Coal Miners of Xinjiang, China: A Cross-Sectional Study. BMJ Open (2020) 10:e036087. doi:10.1136/bmjopen-2019-036087
54. Armon, G, Shirom, A, Melamed, S, and Shapira, I. Gender Differences in the Across-Time Associations of the Job Demands-Control-Support Model and Depressive Symptoms: A Three-Wave Study. Appl Psychol Health Well-being (2010) 2:65–88. doi:10.1111/j.1758-0854.2009.01027.x
55. Hoshino, A, Amano, S, Suzuki, K, and Suwa, M. Relationships Between Depression and Stress Factors in Housework and Paid Work Among Japanese Women. Hong Kong J Occup Ther (2016) 27:35–41. doi:10.1016/j.hkjot.2016.03.001
56. Inoue, A, Kawakami, N, Haratani, T, Kobayashi, F, Ishizaki, M, Hayashi, T, et al. Job Stressors and Long-Term Sick Leave Due to Depressive Disorders Among Japanese Male Employees: Findings From the Japan Work Stress and Health Cohort Study. J Epidemiol Community Health (2009) 64:229–35. doi:10.1136/jech.2008.085548
57. Inoue, A, and Kawakami, N, Japan Work Stress and Health Cohort Study Group. Interpersonal Conflict and Depression Among Japanese Workers With High or Low Socioeconomic Status: Findings From the Japan Work Stress and Health Cohort Study. Soc Sci Med (2010) 71:173–80. doi:10.1016/j.socscimed.2010.02.047
58. Inoue, N, Otsui, K, Yoshioka, T, Suzuki, A, Ozawa, T, Iwata, S, et al. A Simultaneous Evaluation of Occupational Stress and Depression in Patients With Lifestyle-Related Diseases. J Intern Med (2016) 55:1071–5. doi:10.2169/internalmedicine.55.5920
59. Katsuyama, H, Tomita, M, Hidaka, K, Fushimi, S, Okuyama, T, Watanabe, Y, et al. Association Between Serotonin Transporter Gene Polymorphisms and Depressed Mood Caused by Job Stress in Japanese Workers. Int J Mol Med (2008) 21:499–505. doi:10.3892/ijmm.21.4.499
60. Kikuchi, Y, Nakaya, M, Ikeda, M, Okuzumi, S, Takeda, M, and Nishi, M. Relationship Between Job Stress, Temperament and Depressive Symptoms in Female Nurses. Int J Occup Med Environ Health (2014) 27:426–34. doi:10.2478/s13382-014-0270-z
61. Kitaoka-Higashiguchi, K, Nakagawa, H, Morikawa, Y, Ishizaki, M, Miura, K, Naruse, Y, et al. The Association Between Job Demand, Control and Depression in Workplaces in Japan. J Occup Health (2002) 44:427–8. doi:10.1539/joh.44.427
62. Koreki, A, Nakagawa, A, Abe, A, Ikeuchi, H, Okubo, J, Oguri, A, et al. Mental Health of Japanese Psychiatrists: The Relationship Among Level of Occupational Stress, Satisfaction and Depressive Symptoms. BMC Res Notes (2015) 8:96. doi:10.1186/s13104-015-1054-7
63. Mino, Y, Babazono, A, Tsuda, T, and Yasuda, N. Can Stress Management at the Workplace Prevent Depression? A Randomized Controlled Trial. Psychother Psychosom (2006) 75:177–82. doi:10.1159/000091775
64. Miyaki, K, Song, Y, Htun, NC, Tsutsumi, A, Hashimoto, H, Kawakami, N, et al. Folate Intake and Depressive Symptoms in Japanese Workers Considering SES and Job Stress Factors: J-HOPE Study. BMC Psychiatry (2012) 12:33. doi:10.1186/1471-244x-12-33
65. Nakada, A, Iwasaki, S, Kanchika, M, Nakao, T, Deguchi, Y, Konishi, A, et al. Relationship Between Depressive Symptoms and Perceived Individual Level Occupational Stress Among Japanese Schoolteachers. Ind Health (2016) 54:396–402. doi:10.2486/indhealth.2015-0195
66. Nitta, T, Deguchi, Y, Iwasaki, S, Kanchika, M, and Inoue, K. Depression and Occupational Stress in Japanese School Principals and Vice-Principals. Occup Med (2018) 69:39–46. doi:10.1093/occmed/kqy149
67. Saijo, Y, Chiba, S, Yoshioka, E, Kawanishi, Y, Nakagi, Y, Itoh, T, et al. Effects of Work Burden, Job Strain and Support on Depressive Symptoms and Burnout Among Japanese Physicians. Int J Occup Med Environ Health (2014) 27:980–92. doi:10.2478/s13382-014-0324-2
68. Saijo, Y, Chiba, S, Yoshioka, E, Nakagi, Y, Ito, T, Kitaoka-Higashiguchi, K, et al. Synergistic Interaction Between Job Control and Social Support at Work on Depression, Burnout, and Insomnia Among Japanese Civil Servants. Int Arch Occup Environ Health (2014) 88:143–52. doi:10.1007/s00420-014-0945-6
69. Saijo, Y, Ueno, T, and Hashimoto, Y. Job Stress and Depressive Symptoms Among Japanese Fire Fighters. Am J Ind Med (2007) 50:470–80. doi:10.1002/ajim.20460
70. Saijo, Y, Yoshioka, E, Kawaishi, Y, Nakagi, Y, Itoh, T, and Yoshida, T. Relationships of Job Demand, Job Control, and Social Support on Intention to Leave and Depressive Symptoms in Japanese Nurses. Ind Health (2016) 54:32–41. doi:10.2486/indhealth.2015-0083
71. Sakata, Y, Wada, K, Tsutsumi, A, Ishikawa, H, Aratake, Y, Watanabe, M, et al. Effort-Reward Imbalance and Depression in Japanese Medical Residents. J Occup Health (2008) 50:498–504. doi:10.1539/joh.l8043
72. Takaki, J, Taniguchi, T, Fukuoka, E, Fujii, Y, Tsutsumi, A, Nakajima, K, et al. Workplace Bullying Could Play Important Roles in the Relationships Between Job Strain and Symptoms of Depression and Sleep Disturbance. J Occup Health (2010) 52:367–74. doi:10.1539/joh.l10081
73. Tatsuse, T, Sekine, M, and Yamada, M. The Contributions Made by Job Satisfaction and Psychosocial Stress to the Development and Persistence of Depressive Symptoms: A 1-Year Prospective Study. J Occup Environ Med (2019) 61:190–6. doi:10.1097/jom.0000000000001491
74. Tomioka, K, Morita, N, Saeki, K, Okamoto, N, and Kurumatani, N. Working Hours, Occupational Stress and Depression Among Physicians. Occup Med (2011) 61:163–70. doi:10.1093/occmed/kqr004
75. Tsuboi, H, Tatsumi, A, Yamamoto, K, Kobayashi, F, Shimoi, K, and Kinae, N. Possible Connections Among Job Stress, Depressive Symptoms, Lipid Modulation and Antioxidants. J Affect Disord (2006) 91:63–70. doi:10.1016/j.jad.2005.12.010
76. Tsutsumi, A, Kayaba, K, Theorell, T, and Siegrist, J. Association Between Job Stress and Depression Among Japanese Employees Threatened by Job Loss in a Comparison Between Two Complementary Job-Stress Models. Scand J Work Environ Health (2001) 27:146–53. doi:10.5271/sjweh.602
77. Tsutsumi, A, Kawanami, S, and Horie, S. Effort-Reward Imbalance and Depression Among Private Practice Physicians. Int Arch Occup Environ Health (2011) 85:153–61. doi:10.1007/s00420-011-0656-1
78. Yoshizawa, K, Sugawara, N, Yasui-Furukori, N, Danjo, K, Furukori, H, Sato, Y, et al. Relationship Between Occupational Stress and Depression Among Psychiatric Nurses in Japan. Arch Environ Occup Health (2016) 71:10–5. doi:10.1080/19338244.2014.927345
79. Cho, JJ, Kim, JY, Chang, SJ, Fiedler, N, Koh, SB, Crabtree, BF, et al. Occupational Stress and Depression in Korean Employees. Int Arch Occup Environ Health (2008) 82:47–57. doi:10.1007/s00420-008-0306-4
80. Kim, JI, Park, H, and Kim, J-H. The Mediation Effect of PTSD, Perceived Job Stress and Resilience on the Relationship Between Trauma Exposure and the Development of Depression and Alcohol Use Problems in Korean Firefighters: A Cross-Sectional Study. J Affect Disord (2018) 229:450–5. doi:10.1016/j.jad.2017.12.055
81. Kim, YK, and Cha, NH. Correlations Among Occupational Stress, Fatigue, and Depression in Call Center Employees in Seoul. J Phys Ther Sci (2015) 27:3191–4. doi:10.1589/jpts.27.3191
82. Lee, JS, Joo, EJ, and Choi, KS. Perceived Stress and Self-Esteem Mediate the Effects of Work-Related Stress on Depression. Stress Health (2012) 29:75–81. doi:10.1002/smi.2428
83. Lee, H, Ahn, H, Miller, A, Park, CG, and Kim, SJ. Acculturative Stress, Work-Related Psychosocial Factors and Depression in Korean-Chinese Migrant Workers in Korea. J Occup Health (2012) 54:206–14. doi:10.1539/joh.11-0206-oa
84. Park, SG, Min, K-B, Chang, S-J, Kim, H-C, and Min, JY. Job Stress and Depressive Symptoms Among Korean Employees: The Effects of Culture on Work. Int Arch Occup Environ Health (2008) 82:397–405. doi:10.1007/s00420-008-0347-8
85. Yoon, SL, and Kim, JH. Job-Related Stress, Emotional Labor, and Depressive Symptoms Among Korean Nurses. J Nurs Scholarsh (2013) 45:169–76. doi:10.1111/jnu.12018
86. Jung, HS, and Baek, E. A Structural Equation Model Analysis of the Effects of Emotional Labor and Job Stress on Depression Among Nurses With Long Working Hours: Focusing on the Mediating Effects of Resilience and Social Support. Work (2020) 68:561–8. doi:10.3233/wor-203198
87. Kim, SSY, Shin, YC, Oh, KS, Shin, DW, Lim, WJ, Cho, SJ, et al. Gender and Age Differences in the Association Between Work Stress and Incident Depressive Symptoms Among Korean Employees: A Cohort Study. Int Arch Occup Environ Health (2020) 93:457–67. doi:10.1007/s00420-019-01487-4
88. Mohamed, AF, Isahak, M, Awg Isa, MZ, and Nordin, R. The Effectiveness of Workplace Health Promotion Program in Reducing Work-Related Depression, Anxiety and Stress Among Manufacturing Workers in Malaysia: Mixed-Model Intervention. Int Arch Occup Environ Health (2022) 95:1113–27. doi:10.1007/s00420-022-01836-w
89. Batalla, VRD, Barrameda, ALN, Basal, JMS, Bathan, ASJ, Bautista, JEG, Rebueno, MCDR, et al. Moderating Effect of Occupational Stress on Spirituality and Depression of Registered Nurses in Tertiary Hospital: A Structural Equation Model. J Adv Nurs (2018) 75:772–82. doi:10.1111/jan.13856
90. Keser, A, Li, J, and Siegrist, J. Examining Effort–Reward Imbalance and Depressive Symptoms Among Turkish University Workers. Workplace Health Saf (2018) 67:131–6. doi:10.1177/2165079918807227
91. Lin, HS, Probst, JC, and Hsu, YC. Depression Among Female Psychiatric Nurses in Southern Taiwan: Main and Moderating Effects of Job Stress, Coping Behaviour and Social Support. J Clin Nurs (2010) 19:2342–54. doi:10.1111/j.1365-2702.2010.03216.x
92. Lin, TC, Lin, HS, Cheng, SF, Wu, LM, and Ou-Yang, MC. Work Stress, Occupational Burnout and Depression Levels: A Clinical Study of Paediatric Intensive Care Unit Nurses in Taiwan. J Clin Nurs (2016) 25:1120–30. doi:10.1111/jocn.13119
93. Wang, LJ, Chen, CK, Hsu, SC, Lee, SY, Wang, CS, and Yeh, WY. Active Job, Healthy Job? Occupational Stress and Depression Among Hospital Physicians in Taiwan. Ind Health (2011) 49:173–84. doi:10.2486/indhealth.ms1209
94. Wang, SM, Lai, CY, Chang, YY, Huang, CY, Zauszniewski, JA, and Yu, CY. The Relationships Among Work Stress, Resourcefulness, and Depression Level in Psychiatric Nurses. Arch Psychiatr Nurs (2015) 29:64–70. doi:10.1016/j.apnu.2014.10.002
95. Hsieh, HF, Liu, Y, Hsu, HT, Ma, SC, Wang, HH, and Ko, CH. Relations Between Stress and Depressive Symptoms in Psychiatric Nurses: The Mediating Effects of Sleep Quality and Occupational Burnout. Int J Environ Res Public Health (2021) 18:7327. doi:10.3390/ijerph18147327
96. Clays, E, De Bacquer, D, Leynen, F, Kornitzer, M, Kittel, F, and De Backer, G. Job Stress and Depression Symptoms in Middle-Aged Workers—Prospective Results From the Belstress Study. Scand J Work Environ Health (2007) 33:252–9. doi:10.5271/sjweh.1140
97. Bernburg, M, Vitzthum, K, Groneberg, DA, and Mache, S. Physicians’ Occupational Stress, Depressive Symptoms and Work Ability in Relation to Their Working Environment: A Cross-Sectional Study of Differences Among Medical Residents With Various Specialties Working in German Hospitals. BMJ Open (2016) 6:e011369. doi:10.1136/bmjopen-2016-011369
98. Dragano, N, He, Y, Moebus, S, Jöckel, K-H, Erbel, R, Siegrist, J, et al. Two Models of Job Stress and Depressive Symptoms. Results From a Population-Based Study. Soc Psychiatry Psychiatr Epidemiol (2007) 43:72–8. doi:10.1007/s00127-007-0267-z
99. Du Prel, JB, Iskenius, M, and Peter, R. Are Effort–Reward Imbalance and Social Isolation Mediating the Association Between Education and Depressiveness? Baseline Findings From the LidA§-Study. Int J Public Health (2014) 59:945–55. doi:10.1007/s00038-014-0613-3
100. Du Prel, JB, and Peter, R. Work-Family Conflict as a Mediator in the Association Between Work Stress and Depressive Symptoms: Cross-Sectional Evidence From the German LidA-Cohort Study. Int Arch Occup Environ Health (2014) 88:359–68. doi:10.1007/s00420-014-0967-0
101. Li, J, Weigl, M, Glaser, J, Petru, R, Siegrist, J, and Angerer, P. Changes in Psychosocial Work Environment and Depressive Symptoms: A Prospective Study in Junior Physicians. Am J Ind Med (2013) 56:1414–22. doi:10.1002/ajim.22246
102. Kuhnke-Wagner, I-A, Heidenreich, J, and Brauchle, G. Psychosoziale Arbeitsbelastungen Und Depressive Symptome Bei Führungskräften. Psychotherapeut (Berl) (2010) 56:26–33. doi:10.1007/s00278-010-0794-z
103. Larisch, M, Joksimovic, L, von dem Knesebeck, O, Starke, D, and Siegrist, J. Berufliche Gratifikationskrisen Und Depressive Symptome. Ppmp Psychother Psychosom Med Psychol (2003) 53:223–8. doi:10.1055/s-2003-38867
104. Peter, R, March, S, and du Prel, JB. Are Status Inconsistency, Work Stress and Work-Family Conflict Associated With Depressive Symptoms? Testing Prospective Evidence in the LidA Study. Soc Sci Med (2016) 151:100–9. doi:10.1016/j.socscimed.2016.01.009
105. Rösler, U, Stephan, U, Hoffmann, K, Morling, K, Müller, A, and Rau, R. Psychosoziale Merkmale Der Arbeit, Überforderungserleben Und Depressivität. Z für Arbeits- Organisationspsychologie A&O (2008) 52:191–203. doi:10.1026/0932-4089.52.4.191
106. Santa, MA, Wörfel, F, Wolter, C, Gusy, B, Rotter, M, Stark, S, et al. The Role of Job Demands and Job Resources in the Development of Emotional Exhaustion, Depression, and Anxiety Among Police Officers. Police Q (2017) 21:109–34. doi:10.1177/1098611117743957
107. Wege, N, Li, J, and Siegrist, J. Are There Gender Differences in Associations of Effort–Reward Imbalance at Work With Self-Reported Doctor-Diagnosed Depression? Prospective Evidence From the German Socio-Economic Panel. Int Arch Occup Environ Health (2018) 91:435–43. doi:10.1007/s00420-018-1293-8
108. Schramm, E, Mack, S, Thiel, N, Jenkner, C, Elsaesser, M, and Fangmeier, T. Interpersonal Psychotherapy vs. Treatment as Usual for Major Depression Related to Work Stress: A Pilot Randomized Controlled Study. Front Psychiatry (2020) 11:193. doi:10.3389/fpsyt.2020.00193
109. Beschoner, P, von Wietersheim, J, Jarczok, MN, Braun, M, Schönfeldt-Lecuona, C, Viviani, R, et al. Effort-Reward-Imbalance, Burnout, and Depression Among Psychiatrists 2006 and 2016-Changes After a Legislative Intervention. Front Psychiatry (2021) 12:641912. doi:10.3389/fpsyt.2021.641912
110. Weigl, T, Tölle, AS, and Seppelfrick, T. Differential Aspects of Chronic Work-Related Stress Predict Depression in Registered and Geriatric Nurses. Pflege (2021) 34:133–40. doi:10.1024/1012-5302/a000802
111. Kolstad, HA, Hansen, AM, Kaergaard, A, Thomsen, JF, Kaerlev, L, Mikkelsen, S, et al. Job Strain and the Risk of Depression: Is Reporting Biased? Am J Epidemiol (2010) 173:94–102. doi:10.1093/aje/kwq318
112. Rugulies, R, Bültmann, U, Aust, B, and Burr, H. Psychosocial Work Environment and Incidence of Severe Depressive Symptoms: Prospective Findings From a 5-Year Follow-Up of the Danish Work Environment Cohort Study. Am J Epidemiol (2006) 163:877–87. doi:10.1093/aje/kwj119
113. Ahola, K, and Hakanen, J. Job Strain, Burnout, and Depressive Symptoms: A Prospective Study Among Dentists. J Affect Disord (2007) 104:103–10. doi:10.1016/j.jad.2007.03.004
114. Ahola, K, Honkonen, T, Kivimäki, M, Virtanen, M, Isometsä, E, Aromaa, A, et al. Contribution of Burnout to the Association Between Job Strain and Depression: The Health 2000 Study. J Occup Environ Med (2006) 48:1023–30. doi:10.1097/01.jom.0000237437.84513.92
115. Hakanen, JJ, Schaufeli, WB, and Ahola, K. The Job Demands-Resources Model: A Three-Year Cross-Lagged Study of Burnout, Depression, Commitment, and Work Engagement. Work and Stress (2008) 22:224–41. doi:10.1080/02678370802379432
116. Mäntyniemi, A, Oksanen, T, Salo, P, Virtanen, M, Sjösten, N, Pentti, J, et al. Job Strain and the Risk of Disability Pension Due to Musculoskeletal Disorders, Depression or Coronary Heart Disease: A Prospective Cohort Study of 69 842 Employees. J Occup Environ Med (2012) 69:574–81. doi:10.1136/oemed-2011-100411
117. Pulkki-Råback, L, Elovainio, M, Virtanen, M, Kivimäki, M, Hintsanen, M, Hintsa, T, et al. Job Demands and Job Control as Predictors of Depressive Symptoms: Moderating Effects of Negative Childhood Socioemotional Experiences. Stress Health (2015) 32:383–94. doi:10.1002/smi.2632
118. Jolivet, A, Caroly, S, Ehlinger, V, Kelly-Irving, M, Delpierre, C, Balducci, F, et al. Linking Hospital Workers’ Organisational Work Environment to Depressive Symptoms: A Mediating Effect of Effort–Reward Imbalance? The ORSOSA Study. Soc Sci Med (2010) 71:534–40. doi:10.1016/j.socscimed.2010.04.003
119. Nourry, N, Luc, A, Lefebvre, F, Sultan-Taïeb, H, and Béjean, S. Psychosocial and Organizational Work Environment of Nurse Managers and Self-Reported Depressive Symptoms: Cross-Sectional Analysis From a Cohort of Nurse Managers. Int J Occup Med Environ Health (2014) 27:252–69. doi:10.2478/s13382-014-0264-x
120. Looseley, A, Wainwright, E, Cook, TM, Bell, V, Hoskins, S, O’Connor, M, et al. Stress, Burnout, Depression and Work Satisfaction Among UK Anaesthetic Trainees; a Quantitative Analysis of the Satisfaction and Wellbeing in Anaesthetic Training Study. J Anesth (2019) 74:1231–9. doi:10.1111/anae.14681
121. Stansfeld, SA, Shipley, MJ, Head, J, and Fuhrer, R. Repeated Job Strain and the Risk of Depression: Longitudinal Analyses From the Whitehall II Study. Am J Public Health (2012) 102:2360–6. doi:10.2105/ajph.2011.300589
122. Balog, P, Janszky, I, Leineweber, C, Blom, M, Wamala, SP, and Orth-Gomé, K. Depressive Symptoms in Relation to Marital and Work Stress in Women With and Without Coronary Heart Disease: The Stockholm Female Coronary Risk Study. J Adv Nurs (2003) 54:113–9. doi:10.1016/s0022-3999(02)00485-3
123. Sandström, A, Säll, R, Peterson, J, Salami, A, Larsson, A, Olsson, T, et al. Brain Activation Patterns in Major Depressive Disorder and Work Stress-Related Long-Term Sick Leave Among Swedish Females. STRESS (2012) 15:503–13. doi:10.3109/10253890.2011.646347
124. Theorell, T, Hammarström, A, Gustafsson, PE, Magnusson Hanson, L, Janlert, U, and Westerlund, H. Job Strain and Depressive Symptoms in Men and Women: A Prospective Study of the Working Population in Sweden. J Epidemiol Community Health (2014) 68:78–82. doi:10.1136/jech-2012-202294
125. Åhlin, JK, Westerlund, H, Griep, Y, and Magnusson Hanson, LL. Trajectories of Job Demands and Control: Risk for Subsequent Symptoms of Major Depression in the Nationally Representative Swedish Longitudinal Occupational Survey of Health (SLOSH). Int Arch Occup Environ Health (2018) 91:263–72. doi:10.1007/s00420-017-1277-0
126. Magnusson Hanson, LL, Chungkham, HS, Åkerstedt, T, and Westerlund, H. The Role of Sleep Disturbances in the Longitudinal Relationship Between Psychosocial Working Conditions, Measured by Work Demands and Support, and Depression. Sleep (2014) 37:1977–85. doi:10.5665/sleep.4254
127. Magnusson Hanson, LL, Theorell, T, Bech, P, Rugulies, R, Burr, H, Hyde, M, et al. Psychosocial Working Conditions and Depressive Symptoms Among Swedish Employees. Int Arch Occup Environ Health (2009) 82:951–60. doi:10.1007/s00420-009-0406-9
128. Almroth, M, Hemmingsson, T, Sörberg Wallin, A, Kjellberg, K, Burström, B, and Falkstedt, D. Psychosocial Working Conditions and the Risk of Diagnosed Depression: A Swedish Register-Based Study. Psychol Med (2022) 52:1–9. doi:10.1017/s003329172100060x
129. Raskin, M, Kotake, C, Easterbrooks, MA, Ebert, M, and Miller, LC. Job-Related Stress and Depression in Orphanage and Preschool Caregivers in Ukraine. J Res Child Educ (2014) 29:130–45. doi:10.1080/02568543.2014.978516
130. Hoven, H, Wahrendorf, M, and Siegrist, J. Occupational Position, Work Stress and Depressive Symptoms: A Pathway Analysis of Longitudinal SHARE Data. J Epidemiol Community Health (2015) 69:447–52. doi:10.1136/jech-2014-205206
131. Åhlin, JK, Halonen, JI, Madsen, IEH, Rugulies, R, Sørensen, JK, and Magnusson Hanson, LL. Interrelationships Between Job Demands, Low Back Pain and Depression: A Four-Way Decomposition Analysis of Direct and Indirect Effects of Job Demands Through Mediation And/or Interaction. J Affect Disord (2021) 282:219–26. doi:10.1016/j.jad.2020.12.061
132. Mayerl, H, Stolz, E, Kowatz, U, and Freidl, W. Within- and Between-Person Effects in the Relationship Between Effort-Reward Imbalance and Depressive Symptoms. Adv Life Course Res (2020) 48:100394. doi:10.1016/j.alcr.2020.100394
133. Wallace, JE. Job Stress, Depression and Work-To-Family Conflict: A Test of the Strain and Buffer Hypotheses. Ind Relat J (2006) 60:510–39. doi:10.7202/012157ar
134. Wang, J, and Schmitz, N. Does Job Strain Interact With Psychosocial Factors Outside of the Workplace in Relation to the Risk of Major Depression? The Canadian National Population Health Survey. Soc Psychiatry Psychiatr Epidemiol (2010) 46:577–84. doi:10.1007/s00127-010-0224-0
135. Wang, J, Schmitz, N, Dewa, C, and Stansfeld, S. Changes in Perceived Job Strain and the Risk of Major Depression: Results From a Population-Based Longitudinal Study. Am J Epidemiol (2009) 169:1085–91. doi:10.1093/aje/kwp037
136. Wang, J, Smailes, E, Sareen, J, Schmitz, N, Fick, G, and Patten, S. Three Job-Related Stress Models and Depression: A Population-Based Study. Soc Psychiatry Psychiatr Epidemiol (2011) 47:185–93. doi:10.1007/s00127-011-0340-5
137. Kim, HR, Kim, SM, Han, DH, and Lee, YS. Protective and Risk Factors for Depressive Mood and Anxiety Against Occupational Stress: Examining Temperament Character and Coping Strategy Among Civil Servants. Arch Environ Occup Health (2020) 75:346–57. doi:10.1080/19338244.2019.1666789
138. DeSanto, IJ, Cullen, MR, Cantley, L, Slade, MD, Fiellin, M, and Kasl, SV. Effects of Externally Rated Job Demand and Control on Depression Diagnosis Claims in an Industrial Cohort. Am J Epidemiol (2009) 171:303–11. doi:10.1093/aje/kwp359
139. Gayman, MD, and Bradley, MS. Organizational Climate, Work Stress, and Depressive Symptoms Among Probation and Parole Officers. Crim Justice Stud (2012) 26:326–46. doi:10.1080/1478601x.2012.742436
140. Goodman, WB, and Crouter, AC, The Family Life Project Key Investigators. Longitudinal Associations Between Maternal Work Stress, Negative Work-Family Spillover, and Depressive Symptoms. Fam Relat (2009) 58:245–58. doi:10.1111/j.1741-3729.2009.00550.x
141. Gray-Stanley, JA, Muramatsu, N, Heller, T, Hughes, S, Johnson, TP, and Ramirez-Valles, J. Work Stress and Depression Among Direct Support Professionals: The Role of Work Support and Locus of Control. J Intellect Disab Res (2010) 54:749–61. doi:10.1111/j.1365-2788.2010.01303.x
142. Hybels, CF, Blazer, DG, and Proeschold-Bell, RJ. Persistent Depressive Symptoms in a Population With High Levels of Occupational Stress: Trajectories Offer Insights Into Both Chronicity and Resilience. J Psychiatr Pract (2018) 24:399–409. doi:10.1097/pra.0000000000000337
143. Jeon, HJ, Kwon, KA, Walsh, B, Burnham, MM, and Choi, YJ. Relations of Early Childhood Education Teachers’ Depressive Symptoms, Job-Related Stress, and Professional Motivation to Beliefs About Children and Teaching Practices. Early Educ Dev (2018) 30:131–44. doi:10.1080/10409289.2018.1539822
144. Lunau, T, Wahrendorf, M, Müller, A, Wright, B, and Dragano, N. Do Resources Buffer the Prospective Association of Psychosocial Work Stress With Depression? Longitudinal Evidence From Ageing Workers. Scand J Work Environ Health (2018) 44:183–91. doi:10.5271/sjweh.3694
145. Mackie, KS, Holahan, CK, and Gottlieb, NH. Employee Involvement Management Practices, Work Stress, and Depression in Employees of a Human Services Residential Care Facility. Hum Relations (2001) 54:1065–92. doi:10.1177/0018726701548004
146. McCleese, CS, Eby, LT, Scharlau, EA, and Hoffman, BH. Hierarchical, Job Content, and Double Plateaus: A Mixed-Method Study of Stress, Depression and Coping Responses. J Vocat Behav (2007) 71:282–99. doi:10.1016/j.jvb.2007.05.001
147. Mezuk, B, Bohnert, ASB, Ratliff, S, and Zivin, K. Job Strain, Depressive Symptoms, and Drinking Behavior Among Older Adults: Results From the Health and Retirement Study. J Gerontol B Psychol Sci Soc Sci (2011) 66B:426–34. doi:10.1093/geronb/gbr021
148. Proeschold-Bell, RJ, Miles, A, Toth, M, Adams, C, Smith, BW, and Toole, D. Using Effort-Reward Imbalance Theory to Understand High Rates of Depression and Anxiety Among Clergy. J Prim Prev (2013) 34:439–53. doi:10.1007/s10935-013-0321-4
149. Rayens, MK, and Reed, DB. Predictors of Depressive Symptoms in Older Rural Couples: The Impact of Work, Stress and Health. J Rural Health (2013) 30:59–68. doi:10.1111/jrh.12028
150. Shepherd-Banigan, M, Bell, JF, Basu, A, Booth-LaForce, C, and Harris, JR. Workplace Stress and Working From Home Influence Depressive Symptoms Among Employed Women With Young Children. Int J Behav Med (2016) 23:102–11. doi:10.1007/s12529-015-9482-2
151. Simmons, LA, and Swanberg, JE. Psychosocial Work Environment and Depressive Symptoms Among US Workers: Comparing Working Poor and Working Non-Poor. Soc Psychiatr Epidemiol (2009) 44:628–35. doi:10.1007/s00127-008-0479-x
152. Smith, PM, and Bielecky, A. The Impact of Changes in Job Strain and its Components on the Risk of Depression. Am J Public Health (2012) 102:352–8. doi:10.2105/AJPH.2011.300376
153. Hall, GB, Dollard, MF, Winefield, AH, Dormann, C, and Bakker, AB. Psychosocial Safety Climate Buffers Effects of Job Demands on Depression and Positive Organizational Behaviors. Anxiety, Stress and Coping (2013) 26:355–77. doi:10.1080/10615806.2012.700477
154. LaMontagne, AD, Keegel, T, Vallance, D, Ostry, A, and Wolfe, R. Job Strain — Attributable Depression in a Sample of Working Australians: Assessing the Contribution to Health Inequalities. BMC Public Health (2008) 8:181. doi:10.1186/1471-2458-8-181
155. Vearing, A, and Mak, AS. Big Five Personality and Effort–Reward Imbalance Factors in Employees’ Depressive Symptoms. Pers Individ Differ (2007) 43:1744–55. doi:10.1016/j.paid.2007.05.011
156. Bailey, TS, Dollard, MF, and Richards, PAM. A National Standard for Psychosocial Safety Climate (PSC): PSC 41 as the Benchmark for Low Risk of Job Strain and Depressive Symptoms. J Occup Health Psychol (2015) 20:15–26. doi:10.1037/a0038166
157. Elsayed, S, Hasan, AA, and Musleh, M. Work Stress, Coping Strategies and Levels of Depression Among Nurses Working in Mental Health Hospital in Port-Said City. Int J Cult Ment Health (2017) 11:157–70. doi:10.1080/17542863.2017.1343859
158. Mohamed, MY, Elbatrawy, AN, Mahmoud, DAM, Mohamed, MM, and Rabie, ES. Depression and Suicidal Ideations in Relation to Occupational Stress in a Sample of Egyptian Medical Residents. Int J Soc Psychiatry (2023) 69:14–22. doi:10.1177/00207640211061981
159. Kploanyi, EE, Dwomoh, D, and Dzodzomenyo, M. The Effect of Occupational Stress on Depression and Insomnia: A Cross-Sectional Study Among Employees in a Ghanaian Telecommunication Company. BMC Public Health (2020) 20:1045. doi:10.1186/s12889-020-08744-z
160. Gherardi-Donato, ECda S, Cardoso, L, Teixeira, CAB, Pereira, Sde S, and Reisdorfer, E. Association Between Depression and Work Stress in Nursing Professionals With Technical Education Level. Revista Latino-Americana de Enfermagem (2015) 23:733–40. doi:10.1590/0104-1169.0069.2610
161. Lunau, T, Wahrendorf, M, Dragano, N, and Siegrist, J. Work Stress and Depressive Symptoms in Older Employees: Impact of National Labour and Social Policies. BMC Public Health (2013) 13:1086. doi:10.1186/1471-2458-13-1086
162. Siegrist, J, Lunau, T, Wahrendorf, M, and Dragano, N. Depressive Symptoms and Psychosocial Stress at Work Among Older Employees in Three Continents. Glob Health (2012) 8:27. doi:10.1186/1744-8603-8-27
163. Steinhardt, MA, Smith Jaggars, SE, Faulk, KE, and Gloria, CT. Chronic Work Stress and Depressive Symptoms: Assessing the Mediating Role of Teacher Burnout. Stress Health (2011) 27:420–9. doi:10.1002/smi.1394
164. Hurrell, JJ, and McLaney, MA. Exposure to Job Stress--a New Psychometric Instrument. Scand J Work Environ Health (1988) 14(Suppl. 1):27–8.
165. Chang, SJ, Koh, SB, Kang, D, Kim, SA, Kang, MG, Lee, CG, et al. Developing an Occupational Stress Scale for Korean Employees. Korean J Occup Environ Med (2005) 17:297–317. doi:10.35371/kjoem.2005.17.4.297
166. Wang, C, Li, S, Li, T, Yu, SF, Dai, JM, Liu, XM, et al. Development of Job Burden-Capital Model of Occupational Stress: An Exploratory Study. Biomed Environ Sci (2016) 29:678–82. doi:10.3967/bes2016.090
167. Cohen, S, Kamarck, T, and Mermelstein, R. A Global Measure of Perceived Stress. J Health Soc Behav (1983) 24:385–96. doi:10.2307/2136404
168. Levenstein, S, Prantera, C, Varvo, V, Scribano, ML, Berto, E, Luzi, C, et al. Development of the Perceived Stress Questionnaire: A New Tool for Psychosomatic Research. J Psychosom Res (1993) 37:19–32. doi:10.1016/0022-3999(93)90120-5
169. Frenk, SM, Mustillo, SA, Hooten, EG, and Meador, KG. The Clergy Occupational Distress Index (CODI): Background and Findings From Two Samples of Clergy. J Relig Health (2013) 52:397–407. doi:10.1007/s10943-011-9486-4
170. Gorter, RC, Albrecht, G, Hoogstraten, J, and Eijkman, MA. Professional Burnout Among Dutch Dentists. Community Dent Oral Epidemiol (1999) 27:109–16. doi:10.1111/j.1600-0528.1999.tb01999.x
171. Fimian, MJ. The Development of an Instrument to Measure Occupational Stress in Teachers: The Teacher Stress Inventory. J Occup Psychol (1984) 57:277–93. doi:10.1111/j.2044-8325.1984.tb00169.x
172. Tsai, SL, and Chen, ML. A Test of the Reliability and Validity of Nurse Stress Checklist. Nurs Res (1996) 4:355–62.
173. French, SE, Lenton, R, Walters, V, and Eyles, J. An Empirical Evaluation of an Expanded Nursing Stress Scale. J Nurs Meas (2000) 8:161–78. doi:10.1891/1061-3749.8.2.161
174. Takaki, J, Tsutsumi, A, Fujii, Y, Taniguchi, T, Hirokawa, K, Hibino, Y, et al. Assessment of Workplace Bullying and Harassment: Reliability and Validity of a Japanese Version of the Negative Acts Questionnaire. J Occup Health (2010) 52:74–81. doi:10.1539/joh.o9011
175. Guseva Canu, I. Chemical Hazards at Work and Occupational Diseases Using Job-Exposure Matrices. In: M Wahrendorf, T Chandola, and A Descatha, editors. Handbook of Life Course Occupational Health. Handbook Series in Occupational Health Sciences. Cham: Springer (2023). p. 195–212. doi:10.1007/978-3-030-94023-2_4-1
176. Radloff, LS. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Appl Psychol Meas (1977) 1:385–401. doi:10.1177/014662167700100306
177. Beck, AT, and Beck, RW. Screening Depressed Patients in Family Practice. A Rapid Technic. Postgrad Med (1972) 52:81–5. doi:10.1080/00325481.1972.11713319
178. RAND Health. Depression Screener (1998). Available from: http://www.rand.org/health/surveys_tools/depression.html (Accessed December 01, 2023).
179. Zung, WWK. A Self-Rating Depression Scale. Arch Gen Psychiatry (1965) 12:63–70. doi:10.1001/archpsyc.1965.01720310065008
180. Prince, MJ, Reischies, F, Beekman, AT, Fuhrer, R, Jonker, C, Kivela, SL, et al. Development of the EURO-D Scale—A European, Union Initiative to Compare Symptoms of Depression in 14 Europeancentres. Br J Psychiatry (1999) 174:330–8. doi:10.1192/bjp.174.4.330
181. Montgomery, SA, and Asberg, M. A New Depression Scale Designed to Be Sensitive to Change. Br J Psychiatry (1979) 134:382–9. doi:10.1192/bjp.134.4.382
182. Siegrist, J, Starke, D, Chandola, T, Godin, I, Marmot, M, Niedhammer, I, et al. The Measurement of Effort-Reward Imbalance at Work: European Comparisons. Soc Sci Med (2004) 58:1483–99. doi:10.1016/S0277-9536(03)00351-4
183. Brym, S, Mack, JT, Weise, V, Kopp, M, Steudte-Schmiedgen, S, and Garthus-Niegel, S. Mental Health of Working Parents During the COVID-19 Pandemic: Can Resilience Buffer the Impact of Psychosocial Work Stress on Depressive Symptoms? BMC Public Health (2022) 22:2426. doi:10.1186/s12889-022-14582-y
184. Karasek, R, Brisson, C, Kawakami, N, Houtman, I, Bongers, P, and Amick, B. The Job Content Questionnaire (JCQ): An Instrument for Internationally Comparative Assessments of Psychosocial Job Characteristics. J Occup Health Psychol (1998) 3:322–55. doi:10.1037//1076-8998.3.4.322
185. Loughlin, C, and Lang, K. Young Workers. In: J Barling, EK Kelloway, and MR Frome, editors. Handbook of Work Stress. Thousand Oaks: Sage Publications Ltd (2004). p. 405–30.
186. Karasek, R, and Theorell, T. Healthy Work: Stress, Productivity and the Reconstruction of the Working Life. New York: Basic Books (1990).
187. Shimomitsu, T, Haratani, T, Nakamura, K, Kawakami, NH, Hiro, H, Arai, M, et al. The Final Development of the Brief Job Stress Questionnaire Mainly Used for Assessment of the Individuals. In: M Kato, editor. Ministry of Labour Sponsored Grant for the Prevention of Work-Related Illness: The 1999 Report. Tokyo: Tokyo Medical College (2000). p. 126–64. (in Japanese).
188. Curbow, B, Spratt, K, Ungarett, A, McDonnell, K, and Breckler, S. Development of the Child Care Worker Job Stress Inventory. Early Child Res Q (2000) 15:515–36. doi:10.1037/t60670-000
189. Kristensen, TS, Hannerz, H, Høgh, A, and Borg, V. The Copenhagen Psychosocial Questionnaire--a Tool for the Assessment and Improvement of the Psychosocial Work Environment. Scand J Work Environ Health (2005) 31:438–49. doi:10.5271/sjweh.948
190. Faragher, EB, Cooper, CL, and Cartwright, S. A Shortened Stress Evaluation Tool (ASSET). Stress and Health (2004) 20:189–201. doi:10.1002/smi.1010
191. Frone, M, Russell, M, and Cooper, L. Relation of Work-To-Family Conflict to Health Outcomes: A Four-Year Longitudinal Study of Employed Parents. J Occup Organ Psychol (1997) 70:325–35. doi:10.1111/j.2044-8325.1997.tb00652.x
192. Williams, S, and Cooper, CL. Measuring Occupational Stress: Development of the Pressure Management Indicator. J Occup Health Psychol (1998) 3:306–21. doi:10.1037//1076-8998.3.4.306
193. Osipow, SH. Occupational Stress Inventory Revised Edition (Professional Manual). Odessa,Ukraine: Psychological Assessment Resources, Inc (1998).
194. Wheaton, B. Sampling the Stress Universe. In: WR Avison, and IH Gotlib, editors. Stress and Mental Health. New York, NY: Plenum Press (1994). p. 77–115.
195. Moos, RH. Work Environment Scale Manual. 2nd ed. Palo Alto, CA: Consulting Psychologists Press (1986).
196. House, RJ, and Rizzo, JR. Role Conflict and Ambiguity as Critical Variables in a Model of Organizational Behavior. Organizational Behav Hum Perform (1972) 7:467–505. doi:10.1016/0030-5073(72)90030-X
197. Yu, H, Tao, YJ, Pan, HX, Jiang, NN, and Ma, HY. Development of Mental Stressor Investigation Questionnaire Among the Crew of Naval Ships. J Prev Med Chin Peoples Liberation Army (2014) 32:119–21.
198. Uehata, T, Yamasaki, Y, Sakano, J, Abe, N, Ishihara, N, Namikawa, S, et al. An Epidemiological Survey on Work Stress and Health in Various Kinds of Occupations of Japan: Fi Rst Report. Tokyo: Institute of Industrial Medicine (1991). (in Japanese).
199. Bagley, SC, Sirota, M, Chen, R, Butte, AJ, and Altman, RB. Constraints on Biological Mechanism From Disease Comorbidity Using Electronic Medical Records and Database of Genetic Variants. Plos Comput Biol (2016) 12:e1004885. doi:10.1371/journal.pcbi.1004885
200. Schulz, P, Schlotz, W, and Becker, P. Trierer Inventar Zum Chronischen Stress. Göttingen, Bern: Hogrefe (2004).
201. Cai, H, and Jiang, F. Work Stress of Urban Employees and Their Differences in Different Systems and Organizations. Learn Exploration (2017) 6:53–61.
202. Musa, R, Fadzil, MA, and Zain, Z. Translation, Validation and Psychometric Properties of Bahasa Malaysia Version of the Depression Anxiety and Stress Scales (DASS). ASEAN J Psychiatr (2007) 8:82–9.
203. Carson, J. The Stress Process in Mental Health Workers: Assessment and Intervention Studies (Dissertation). London: King's College, University of London (2005).
204. Caplan, RD, Cobb, S, French, JRP, Van Harrison, RV, and Pinneau, SR. Job Demands and Worker Health: Main Effects and Occupational Differences. Washington, DC: US Department of Health, Education, and Welfare (1975). p. 351. Monograph. doi:10.1037/e573842014-001
205. Lee, Y, Yang, MJ, Lai, TJ, Chiu, NM, and Chau, TT. Development of the Taiwanese Depression Questionnaire. Chang Gung Med J (2000) 23:688–94.
207. Christensen, KS, Fink, P, Toft, T, Frostholm, L, Ornbøl, E, and Olesen, F. A Brief Case-Finding Questionnaire for Common Mental Disorders: The CMDQ. Fam Pract (2005) 22:448–57. doi:10.1093/fampra/cmi025
208. Goldberg, D, and Williams, P. A User Guide to the General Health Questionnaire. Windsor: NFER-Nelson (1991).
209. Baer, L, Jacobs, DG, Meszler-Reizes, J, Blais, M, Fava, M, Kessler, R, et al. Development of a Brief Screening Instrument: The HANDS. Psychother Psychosom (2000) 69(1):35–41. doi:10.1159/000012364
210. Kessler, RC, Barker, PR, Colpe, LJ, Epstein, JF, Gfroerer, JC, Hiripi, E, et al. Screening for Serious Mental Illness in the General Population. Arch Gen Psychiatry (2003) 60:184–9. doi:10.1001/archpsyc.60.2.184
211. Berwick, DM, Murphy, JM, Goldman, PA, Ware, JE, Barsky, AJ, and Weinstein, MC. Performance of a Five-Item Mental Health Screening Test. Med Care (1991) 29:169–76. doi:10.1097/00005650-199102000-00008
212. Magnusson Hanson, LL, Westerlund, H, Leineweber, C, Rugulies, R, Osika, W, Theorell, T, et al. The Symptom Checklist-Core Depression (SCL-CD6) Scale: Psychometric Properties of a Brief Six Item Scale for the Assessment of Depression. Scand J Public Health (2014) 42:82–8. doi:10.1177/1403494813500591
213. Pearlin, LI, Lieberman, MA, Menaghan, EG, and Mullan, JT. The Stress Process. J Health Soc Behav (1981) 22:337–56. doi:10.2307/2136676
214. Spitzer, RL, Kroenke, K, and Williams, JB. Validation and Utility of a Self-Report Version of PRIME-MD: The PHQ Primary Care Study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA (1999) 282:1737–44. doi:10.1001/jama.282.18.1737
215. Fujisawa, D, Tanaka, E, Sakamoto, S, Neichi, K, Nakagawa, A, and Ono, Y. The Development of a Brief Screening Instrument for Depression and Suicidal Ideation for Elderly: The Depression and Suicide Screen. Psychiatry Clin Neurosci (2005) 59:634–8. doi:10.1111/j.1440-1819.2005.01429.x
216. Zhang, J, Wz, Y, Fang, G, Li, J, Han, BX, and Chen, ZY. Development of the Chinese Age Norms of CES-D in Urban Area. Chin Ment Health J (2010) 24:139–43.
217. Krohne, HW, Schmukle, SC, Spaderna, H, and Spielberger, CD. The State-Trait Depression Scales: An International Comparison. Anxiety Stress Coping (2002) 15:105–22. doi:10.1080/10615800290028422
Keywords: psychosocial work stress, work-related depression, depressive symptoms, effort-reward imbalance, job strain
Citation: du Prel J-B, Koscec Bjelajac A, Franić Z, Henftling L, Brborović H, Schernhammer E, McElvenny DM, Merisalu E, Pranjic N, Guseva Canu I and Godderis L (2024) The Relationship Between Work-Related Stress and Depression: A Scoping Review. Public Health Rev 45:1606968. doi: 10.3389/phrs.2024.1606968
Received: 12 December 2023; Accepted: 16 April 2024;
Published: 01 May 2024.
Edited by:
Gemma Castano-Vinyals, Instituto Salud Global Barcelona (ISGlobal), SpainReviewed by:
Vicent Villanueva, Generalitat Valenciana, SpainOne reviewer who chose to remain anonymous
Copyright © 2024 du Prel, Koscec Bjelajac, Franić, Henftling, Brborović, Schernhammer, McElvenny, Merisalu, Pranjic, Guseva Canu and Godderis. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
PHR is edited by the Swiss School of Public Health (SSPH+) in a partnership with the Association of Schools of Public Health of the European Region (ASPHER)+
*Correspondence: Jean-Baptist du Prel, ZHVwcmVsQHVuaS13dXBwZXJ0YWwuZGU=
†ORCID: Irina Guseva Canu, orcid.org/0000-0001-7059-8421
 Jean-Baptist du Prel
Jean-Baptist du Prel Adrijana Koscec Bjelajac
Adrijana Koscec Bjelajac Zrinka Franić2
Zrinka Franić2 Hana Brborović
Hana Brborović Nurka Pranjic
Nurka Pranjic Lode Godderis
Lode Godderis