- 1Department of Global Health and Social Medicine, Faculty of Social Science and Public Policy, King’s College London, London, United Kingdom
- 2Population Health Sciences Institute, Faculty of Medical Sciences, Newcastle University, Newcastle Upon Tyne, United Kingdom
- 3School of Public Health, Imperial College London, London, United Kingdom
- 4Population Health Sciences, King’s College London, London, United Kingdom
Objective: To synthesise evidence on the effectiveness of frailty interventions among prefrail and frail community-dwelling older adults living in low and middle-income countries (LMICs).
Methods: The four electronic databases, Embase, Ovid MEDLINE, Global Health, and APA PsycINFO, were searched until 25 September 2023. This review’s protocol was registered on PROSPERO (CRD42022309998). There was no publication time or language restriction. Inclusion criteria included randomised controlled trials and other intervention types of frailty interventions that focussed on community-dwelling older adults (mean age of at least 60 years) with prefrail or frail living in LMICs. The meta-analysis could not be conducted because of the heterogeneity of frailty interventions.
Results: This systematic review included fifteen studies: eleven were single-domain interventions (exercise, nutritional supplementation, and nurse home visits), and four were multidomain interventions (exercise plus nutrition and exercise plus mindfulness). Some evidence from high-quality studies showed that physical exercise interventions successfully addressed frailty.
Conclusion: This systematic review highlights the scarcity of evidence on frailty interventions in LMICs, making it difficult to evaluate their effectiveness. Additional research is needed to focus on specific types of interventions.
Introduction
The World Health Organization (WHO) predicts that by 2030, there will be 1.7 billion older people aged over 60, and this will increase to 2 billion by 2050, with an annual growth rate of 3%. As populations age, the prevalence of multiple chronic conditions also rises [1]. Health systems in low- and middle-income countries (LMICs) are poor-prepared for these changes, as aging is occurring rapidly in these regions, with resources stretched between large youthful populations and a growing elderly minority [2].
Frailty, a common syndrome in older adults, is associated with age-related physiological changes, reduced body reserves, and diminished ability to cope with stressors [3]. Pre-frailty represents the early stages of these changes [4]. According to a systematic review of 62 countries, the prevalence of frailty and prefrailty were 12% and 46% using physical frailty measures [5]. Whilst there is a deficit in terms of research, far from being a condition present only in wealthy countries, evidence suggests frailty is common among older people in resource-poor settings: according to another systematic review, the pooled prevalence of frailty in LMICs was 17.4%, and prefrailty was 49.3%, which is higher than in HICs [6].
The most common clinical presentations of frailty include fatigue, unintentional weight loss, recurrent infections, falls due to impaired gait and balance, and spontaneous falls in severe cases [7]. Factors contributing to frailty include biological elements such as sarcopenia, malnutrition, inflammation, and infection, as well as psychosocial factors like poverty and social isolation [8].
In clinical settings, frailty is typically diagnosed using either Fried’s Frailty Phenotype, which includes five criteria (weak grip strength, slow gait, unintentional weight loss, exhaustion, and low physical activity), or the Frailty Index (FI), which includes 30 or more signs, symptoms, co-morbidities, and laboratory findings [8]. Frailty is dynamic, with individuals moving between robust/non-frailty, pre-frailty, and frailty states [6]. Those meeting one or two of Fried’s criteria are considered pre-frail, while those scoring between 0.25 and 0.8 on the Rockwood’s Accumulation of Deficits Model or Frailty Index (FI) are classified as pre-frail [9].
Frailty has significant consequences. Physically, it is linked to chronic diseases, complications like falls and fractures, hospitalisations, and disability [7]. A meta-analysis by Fan et al. [10] found frailty increased mortality risk: the pooled risk ratio of all-cause mortality was 2.41 (95% CI 2.07–2.80) for frail women and 2.94 (95% CI 2.12–4.09) for frail men (as defined by using the frailty phenotype) [10]. Muscle mass loss can lead to reduced mobility, dependency, and limitations in daily life [11]. Additionally, frailty is associated with mental health issues such as depression, anxiety, and social isolation [12]. The broader societal consequences of frailty include increased healthcare costs and financial strain on families and communities [13].
Several systematic reviews from HICs suggest that frailty and pre-frailty can be reversed through interventions targeting different aspects of the syndrome. For example, multi-component exercise programs that include resistance, balance, and flexibility exercises have proven effective in improving health outcomes for frail older adults [14, 15]. These programs are also beneficial in improving cognitive function. Multidomain programs combining exercise, nutrition, and other interventions, such as health education and home visits, are particularly effective [16, 17]. A meta-analysis by Macdonald et al. [18] found that resistance-based exercise, particularly when combined with nutritional supplementation, is the most effective strategy for preserving functional capacity in ageing adults [18].
Despite the growing number of older adults in LMICs and the increasing prevalence of frailty, there is a need for more studies, and systematic reviews focused on frailty interventions in these countries. Findings from HICs may is not directly applicable to LMICs due to differences in healthcare systems, cultural perceptions, and resource availability. For instance, access to protein-rich foods and the acceptability of physical activity programs may vary significantly across different regions [19]. Healthcare systems in LMICs are often under-resourced, with limited clinical guidelines for chronic diseases, few specialists in geriatrics, and poorly trained healthcare workers in primary care [20]. Economic pressures and social perceptions about ageing can further discourage older adults from seeking medical help [21, 22].
There is a need to synthesise evidence from LMICs to identify effective frailty interventions in these settings. Interventions for older adults living in community rather than institutional settings are a particular priority, given that residential long-term care remains rare: the vast majority of older prefrail and frail older adults in LMIC live in communities, supported by family members. Research is required to determine recommended interventions’ feasibility, access, and acceptability within resource-limited environments, including dietary changes and exercise programs. Healthcare providers, policymakers, and advocates need relevant evidence to rapidly develop targeted interventions and services to address the unmet needs of older populations in these regions [23].
Methods
Search Strategy
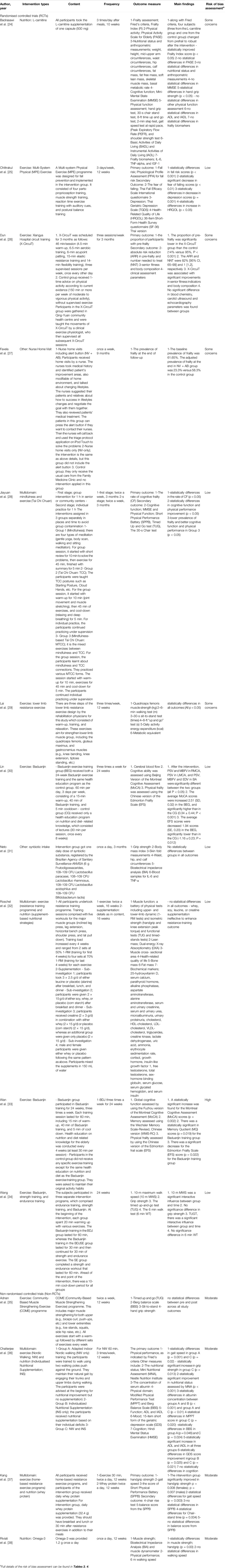
The systematic review protocol was registered on PROSPERO (CRD42022309998). The Preferred Reporting Items for a Systematic Review and Meta-Analysis (PRISMA) guidelines were followed, as shown in Figure 1. Literature searches were conducted using OVID, which includes Embase, Ovid MEDLINE, Global Health, and APA PsycINFO. Search terms included (frail* OR prefrail*) AND (intervention* OR physical exercise OR physical activity OR nutri* OR nutri* supplement* OR brain exercise OR brain stimulation OR cognitive stimulation OR randomised controlled trial* OR random allocation OR double blind method OR single blind method OR clinical trial* OR controlled clinical trial* OR multicenter stud* OR experimental stud*) AND the list of LMICs (per World Bank criteria). The search covered literature up to September 25, 2023.
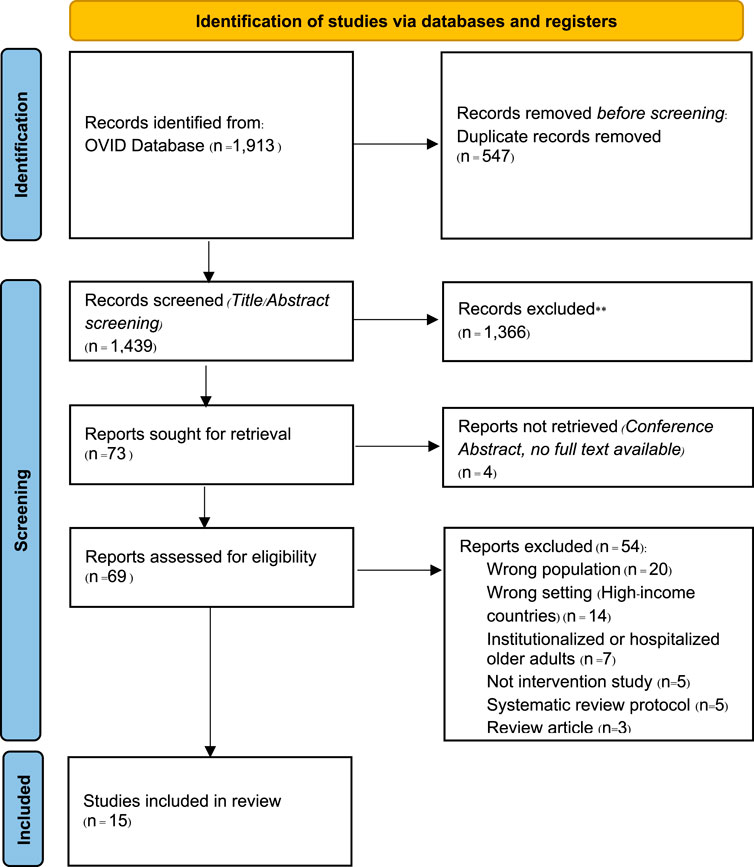
Figure 1. The Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) Diagram (London, United Kingdom. 2024).
Inclusion and Exclusion Criteria
Inclusion criteria were: 1) full-text peer-reviewed publications, 2) randomised controlled trials or other intervention studies (e.g., quasi-experimental, pre-post test studies, and non-randomised controlled trials) conducted in LMICs, 3) community-based interventions delivered in primary care settings, outpatient clinics, homes, or other community locations (e.g., day centres, churches), 4) participants identified as prefrail or frail using any frailty screening tool, 5) community-dwelling older adults in LMICs with a mean age of at least 60. Exclusions were hospitalised or institutionalised individuals, including those living in nursing homes and those with terminal illnesses. There were no language or time restrictions. Deduplicated references from OVID were screened using Rayyan.
Data Extraction and Quality Assessment
Two reviewers (FK and SA) independently screened titles and abstracts, followed by full-text assessments for eligibility. Disagreements were resolved through discussion. A third reviewer (RM) was available to resolve any disagreements. Extracted data included author(s), year, study design, participants (number and gender), frailty criteria, study inclusion criteria, intervention characteristics (type, content, frequency), outcomes, findings, statistical significance (P-values), and risk of bias assessment. Primary outcomes were frailty status/prevalence. The secondary outcomes were characteristics associated with different aspects of frailty: muscle strength, gait speed, mobility, balance, falls, functional ability, mood, cognitive function, and quality of life.
The risk of bias was assessed by two reviewers (FK and QA) using the Cochrane Risk of Bias tool (RoB 2) for randomised controlled trials and the Risk of Bias In Non-randomized Studies-of Interventions (ROBINS-I) for non-randomized controlled trials. Any disagreements were solved through discussion.
Data Synthesis
Narrative synthesis was conducted on study characteristics, participants, interventions, and outcomes. Meta-analysis was not performed due to intervention and outcome heterogeneity.
Results
Study Characteristics and Participants
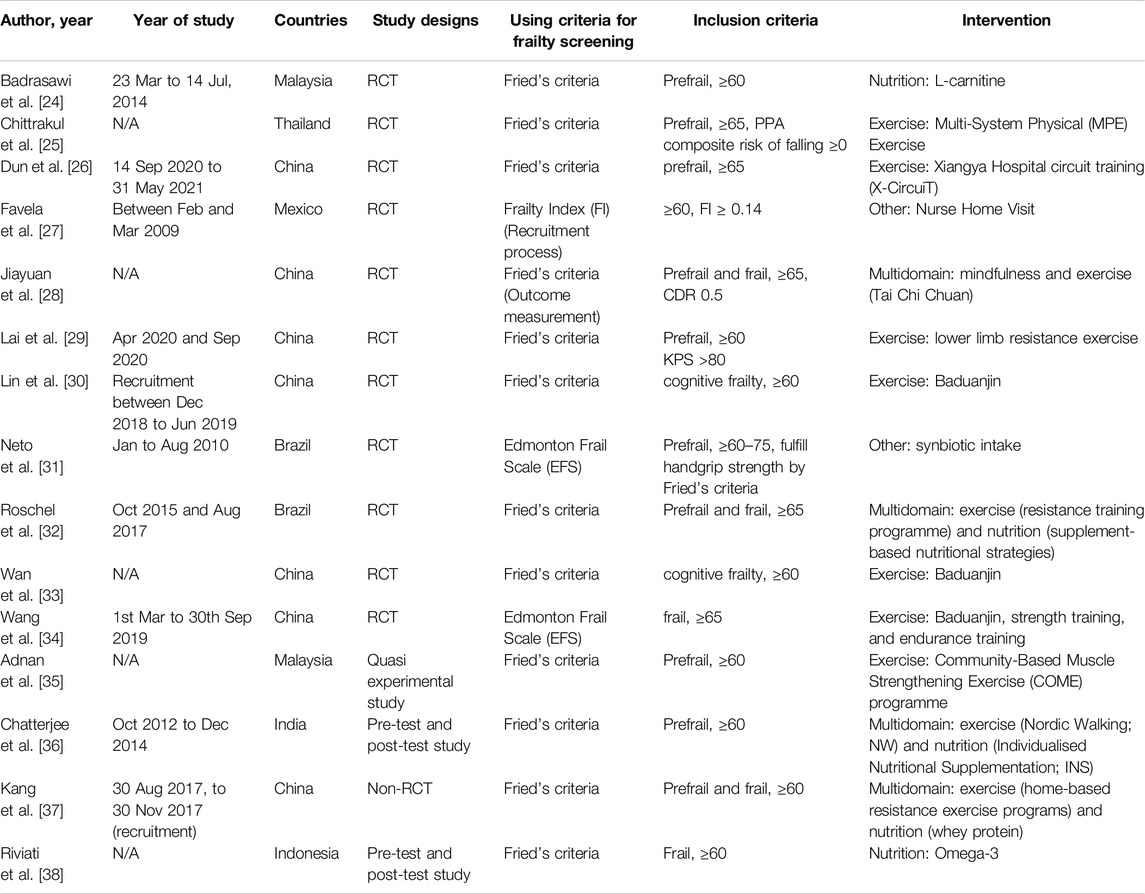
Table 1 summarises included studies’ characteristics. Studies were published in peer-reviewed journals between 2013 and 2022. We included fifteen studies in this review. Studies were conducted in 7 countries: China (n = 7), Malaysia (n = 2), Thailand (n = 1), India (n = 1), Indonesia (n = 1), Brazil (n = 2), and Mexico (n = 1). Eleven studies were randomised controlled trials (RCTs). Two were pre- and post-test designs. The other two studies were non-randomised controlled trials and quasi-experimental studies. The sample size ranged from 17 to 203. The total of participants included in all studies was 1,335. Most studies (n = 12) used Fried’s criteria to define frailty. Seven studies recruited prefrailty, while four recruited frailty or cognitive frailty. Four studies enrolled both prefrailty and frailty.
Intervention Characteristic
Table 2 summarises the intervention characteristics. There were eleven single domain intervention studies. Three intervention types were identified: exercise (n = 7), nutritional supplementation (n = 3), and home visit (n = 1). There were four multidomain intervention studies: exercise plus nutrition (n = 3) and exercise plus mindfulness (n = 1).
Exercise
All physical exercise intervention studies were conducted in Asian countries. In terms of intervention delivery: in one Chinese study, lower limb resistance exercises designed by rehabilitation physicians were initiated in rehabilitation centre (and then on ward) and after discharge, patients and families were taught by nurses to continue the exercise at home with 12 weeks of follow-up [29]; professional instructors delivered two interventions; physiotherapists delivered all other interventions. All but one of the interventions were delivered in group format in community halls [29]. Interventions included two multicomponent exercise programmes: multi-system physical exercise (MPE) programme covering proprioception, muscle strengthening, reaction time, postural sway, and lower limb resistance exercises-conducted in primary care centre in Thailand [25] and multicomponent exercise intervention delivered in urban China consisting of five stages: warm-up, aerobic training, Traditional Chinese Medicine (TCM)-acupoint patting, elastic band resistance, and flexibility training [26]. There were three single component programmes: a community-based muscle strengthening exercises (COME) intervention conducted at a community hall in Malaysia [35]. Two studies conducted in China were based on Baduanjin Exercise, one of China’s most popular mind-body exercises. It consists of eight movements with low-medium intensity characterised by symmetrical body postures and movements, breathing control, a meditative state of mind, and mental focus [30, 33]. The last exercise intervention, called a Hybrid Exercise Programme by Wang et al. [34], is a combination of Baduanjin exercise and strength and endurance training exercise [34].
Nutrition
Three studies conducted nutritional supplementation interventions. In Malaysia, Badrasawi et al. [24] conducted randomised, double-blind, placebo-controlled clinical trial of L-carnitine supplementation among prefrail older people ≥60 years old [24]. Riviati et al. [38] explored the effect of omega-3 supplementation in frail older people ≥60 years old in Indonesia [38]. Lastly, using a small sample (n = 17), Neto et al. [31] conducted 3-month double-blind RCT to evaluate the effect of synbiotic supplementation on frailty markers and body compositions of prefrail older people 60–75 years old in Brazil: synbiotics combine prebiotic-and probiotic-substances which are hypothesised to confer benefits to frail older adults via improvements to gut health and functioning [31, 39].
Nurse Home Visit
Favela et al. [27] evaluated the effects of nurse home visit intervention on frailty, conducting an unblinded RCT in Mexico to evaluate the effects of nurse home visits, including alert buttons (NV + AV) in reducing frailty; participants received home visits by a nurse [27]. The nurses took medical history and identified patient’s improvement areas, home environment, and lifestyle changes. The nurses made recommendations on how to make lifestyle changes and devise effective goal. They also reviewed patients’ medical treatment. The patients in this group can press the alert button to contact their nurses. Then, the nurses will call back and use the follow guidelines to resolve the problems.
Exercise Plus Nutrition
Three multi-domain interventions combined nutritional advice and/or supplementation and exercise. Chatterjee et al. [36] conducted a pre-and post-test study in India, which randomly allocated prefrail older people ≥60 years old into three groups: group A Nordic walking (NW) only, group B individualised nutritional supplementation (INS) only, and group C (NW and INS). Nordic walking engages upper and lower body muscles in a constant and alternating motion, increasing cardiovascular and respiratory demands while enhancing endurance, flexibility, and balance [36]. Kang et al. [37] conducted a case-control study in China to evaluate the effect of whey protein supplements on muscle function and frailty status of prefrail and frail older people ≥60 years old in addition to home-based resistance exercise programme [37]. Roschel et al. [32] conducted a 16-week, double-blind, randomised, placebo-controlled trial in prefrail and frail older people ≥65 [32]. All participants undertook a resistance training programme and were randomised into four sub-groups to compare different types of nutritional supplementation: either leucine or placebo (alanine), either soy, whey or placebo (corn starch), creatine combined with either whey or placebo (corn starch) or only placebo, and either whey or placebo.
Exercise Plus Mindfulness
One study combined mindfulness and exercise (Tai Chi Chuan). Jiayuan et al. [28] recruited prefrail and frail older people ≥65 years old for a 6-month single-blind, three-arm randomised controlled trial in China to compare the effects of mindfulness intervention only, Tai-Chi Chuan intervention only and mindfulness-based plus Tai-Chi Chuan (MTCC) intervention [28].
Quality Assessment
Table 3 (ROB2) and Table 4 (ROBINS-I) show the risk of bias assessment. Of the fifteen included studies, eleven were evaluated using the ROB2 for quality assessment and four using the ROBINS-I for quality assessment. Six studies were low-risk, and five had some concerns. From the ROBINS-I assessment, all studies (n = 4) were moderate risk. Therefore, only six studies had a low risk of bias.
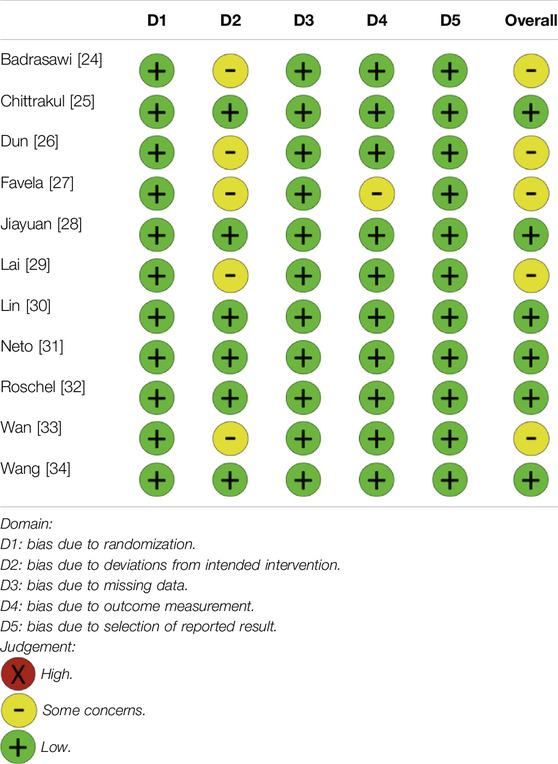
Table 3. Quality assessment using the Cochrane Risk of Bias tool (RoB 2) for randomised controlled trials (London, United Kingdom. 2024).
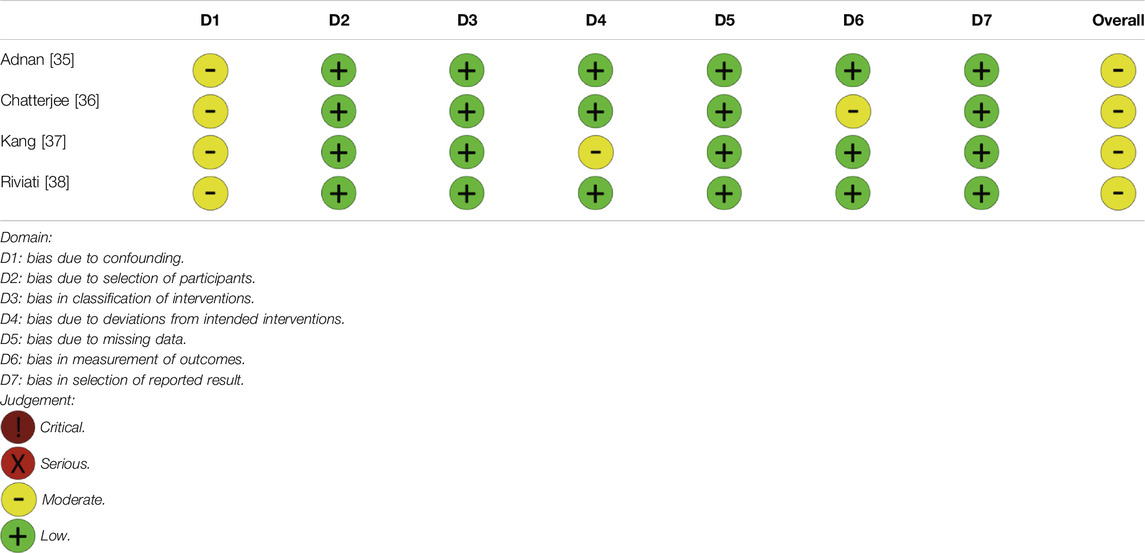
Table 4. Quality assessment using the Risk of Bias In Non-randomized Studies-of Interventions (ROBINS-I) for non-randomized controlled trials (London, United Kingdom. 2024).
Outcomes
Outcomes are summarised in Table 2.
Exercise
All but one of the exercise intervention studies reported positive effects on frailty-related variables after 12 weeks of intervention [35]. The COME programme resulted in small positive differences in some frailty-related outcomes: time up and go (TUG) = −0.25 (95%CI –0.89, 0.39), sit-to-stand duration = −0.41 (95%CI –1.17, 0.34), and handgrip strength 0.68 (95%CI –0.92, 2.30). The sit-to-stand duration showed the most significant benefit from the intervention, recording the highest effect size among the outcome measures (0.20). Chittrakul et al. [25] reported decreased risk of fall scores (p < 0.01) as well as decreased fear of falling scores (p < 0.01), depression scores (p = 0.001), and increased Health-Related Quality of Life (HRQOL) (p < 0.05) after 12 weeks of MPE programme [25]. Dun et al. [26] aimed to reverse prefrailty; they found significantly lower proportion of prefrailty in the 3-month X-Circuit intervention group than in the control (14% VS 95%, P < 0.01) [26]. The ARR and NNT were 82% (95% CI, 65–99) and 1 (1-2), respectively. Also, among pre-frail older people, Lai et al. [29] found that 12-week lower limb resistance exercise had a positive effect on mobility measured by 6-min walking test, 30-s sit-to-stand test, 8-ft “up&go” test with statistically significant results (all p < 0.05) [29]. Both studies, which assessed the effects of the 24-week Baduanjin programme, reported that this exercise significantly decreased the Edmonton Frailty Score (p = 0.01 from Lin et al.’s study [30] and p = 0.02 from Wan et al.’s study [33]). A significant increase in Montreal Cognitive Assessment (MoCA) scores (p < 0.001 and p < 0.01respectively) was also found. Another study on 24-week Baduanjin exercise by Wang et al. [34], found statistically significant changes in mobility, measured by a 10-m maximum walk speed (p < 0.01) and timed up and go test (TUGT) (p = 0.04) [34]. However, no differences were found in hand grip strength and the 6-min walking test.
Nutrition
In 10-week L-carnitine group, frailty index scores and hand grip strength were significantly improved (p < 0.05 for both parameters) [24]. However, there was no difference in frailty biomarkers (interleukin-6 (IL-6), tumour necrosis factor-alpha (TNF-alpha), and insulin-like growth factor-1 (IGF-1), physical function, cognitive function, and nutritional status [24]. Riviati et al. [38] claimed a significant improvement in hand grip strength from omega-3 supplementation for 12 weeks, but the reported data do not support that conclusion, the reported p-value 0.00 is erroreous [38].
The third nutritional study, by Neto et al. [31] found that 3 months of synbiotic supplementation did not benefit body composition or inflammatory cytokines [31].
Nurse Home Visit
Favela et al. [27] found that Nurse Home Visit for 9 months decreased the prevalence of frailty from 61.65% at baseline to 23.3% (p < 0.05) when an alert button was included (NV + AB) [27].
Exercise Plus Nutrition
Of the three studies examining exercise combined with nutrition interventions, Chatterjee et al. [36] found statistical differences in gait speed in the NW group (p < 0.01) and NW and INS group (p = 0.02) and statistically significant increase in hand grip strength in the NW and INS group (p = 0.013) after 12 weeks of follow-up. Mood measured by the Geriatric Depression Scale (GDS) was significantly improved in the INS group (p = 0.025) and the NW and INS group (p = 0.021) [36]. There was no significant difference in cognitive status. Kang et al. [37] found that 12-week whey protein supplements improved hand grip strength (p < 0.01), gait speed (p < 0.01) [37], and chair-stand time (<0.01). Roschel et al. [32] found no difference in muscle mass and function according to 16-week nutritional supplementation [32].
Exercise Plus Mindfulness
Among cognitively frail older people, Jiayuan et al. [28] found lower prevalence of frailty and improvement in physical performance (measured by Short physical performance battery: SPPB and TUGT) and cognitive function (Mini-Mental State Examination: MMSE) among the group receiving mindfulness plus Tai-Chi Chuan intervention (p < 0.05) for 3 months. The intervention also decreased frailty prevalence; 9 participants (30%) reversed to no cognitive frailty [28].
Discussion
Frailty is a significant global health issue, potentially affecting more older people in LMICs than in HICs. Our systematic review revealed limited evidence on frailty interventions in LMICs, identifying 15 studies, of which only six offered robust evidence (low risk of bias). Methodological concerns in studies with some concerns risk of bias included unblinded study, non-randomisation, or many drop-offs in per-protocol analysis studies. The small number of high-quality studies makes it difficult to draw definitive conclusions.
Unlike findings from HICs, two studies examining nutritional supplementation in LMICs (e.g., synbiotics, whey, creatine, leucine) showed no benefits. Conversely, other reviews from HICs reported modest improvements in physical function and mobility with protein supplementation [40]. According to the systematic review by Yan et al. [41], protein supplementation intervention remarkably improved body weight, muscle mass, muscle strength, and physical performance among frail older adults [41]. Consistent with HICs evidence, our findings suggest physical exercise can improve frailty-related outcomes, including cognitive and physical function, falls, depression, and quality of life [25, 30, 33]. Multi-component exercise programmes (resistance, balance, flexibility) were particularly effective in improving muscle strength [14, 15]. One high-quality LMICs study showed that such interventions reduced fall risk, fear of falling, and depression while improving health-related quality of life [25]. However, more research is needed to understand these effects fully.
Notably, two effective physical activity interventions incorporated mindful movement elements, bridging the mind-body divide often reinforced by biomedicine. These interventions address the psychological aspects of frailty, such as the “frailty identity crisis,” which reflects feelings of despair during the transition to frailty [42]. Psychological challenges, including depression, can worsen frailty and act as barriers to participation in interventions. Research from LMICs highlights that older people often view health decline as a natural part of ageing, face stigma around mental health, and perceive healthcare as inaccessible due to poorly equipped systems, limited old-age specialists, and insufficient insurance coverage.
Interventions addressing psychological, social, and spiritual aspects of frailty are essential. Successful interventions must also consider cultural appropriateness. For example, two reviewed interventions in China incorporated popular cultural practices like Tai Chi and Baduanjin, highlighting the importance of integrating traditional activities. This approach, widely debated in global mental health [43], has yet to become a topic for research in gerontology, where cultural appropriateness is, perhaps, equally important. Given this context, adopting or adapting traditional and/or popular practices as health promotion interventions (where locally relevant ones exist) is a promising line of inquiry in frailty and global ageing research.
Asian governments have invested in health systems and welfare reform to support changing demographics. In China, for example, policy changes target older people living with multimorbidity in terms of increased inputs from the government to the health and social system for older people [23]. In Thailand, National Policies on Ageing exist, such as the National Long-Term Plan for Older Persons [44]. Thailand is prepared for old-age security, including income security, housing and environment, health and healthcare, dependence care, and rights and safety [45].
The demographic and socioeconomic context in LMICs must be addressed. Notably, all the studies we identified were conducted in upper-middle-income countries. All but one of the exercise interventions included in this review were led by physiotherapists or professional instructors (in the case of Baduanjin). This resource is unlikely to be available in low-income countries, where health systems are more stretched and lack specialist health workers and training opportunities. Developing task-shared interventions where non-specialists deliver physical activity programmes could address these gaps. WHO’s Integrated Care for Older People (ICOPE) programme exemplifies this approach. A recent randomised controlled trial of this intervention revealed promising results, with improvements in mobility, vitality and psychological health [46].
Limitations
We adopted a comprehensive search strategy using four databases. However, it is possible that we missed article due to different language between search terms and language of publication (e.g., search terms were in English, maybe publications were in Thai and could only be found with Thai search terms). The search strategy we adopted has resulted in a small number of studies from which it is difficult to draw strong conclusions. However, this is more likely a finding rather than an artefact per se of our approach. The concept of frailty is derived from studies carried out in the West. Using this as a primary search term, we may have missed studies that addressed conditions, states, or symptoms linked to frailty (e.g., depression) but were not labelled as such by researchers. In particular contexts, specific health problems linked to older age may be considered necessary but not covered within the frailty construct. In addition, the validity of frailty measures in other cultural contexts has generally yet to be investigated [47]. Additionally, our last search was conducted in September 2023- it is possible that new studies have been published since then which are not included in this review.
We deliberately focused upon studies carried out among community-dwelling older adults. Even in countries with the largest numbers of older people, residential long-term care, whilst growing rapidly, remains rare and fraught with challenges-including shortages of workers, weak quality regulations [48]: there is a lack of studies carried out in these settings LMICs, despite positive findings from HICs [49]. Rates of frailty among hospitalised older adults in LMICs are high-a recent systematic review estimated the pooled prevalence to be 39% [50]. However, given that the vast majority of older people live in communities and primary healthcare is designed to be accessible to all [51], prioritising the integration of frailty interventions in primary healthcare settings perhaps has the greatest potential for impact.
Conclusion
Frailty interventions focused on physical activity show promise in addressing frailty among prefrail and frail older adults. However, the small number of high-quality studies and limited sample sizes hinder robust conclusions. Different from the wealth of research in HICs, LMICs face unique cultural, health system, demographic, and socioeconomic challenges, making findings from HICs less transferable.
Future research should investigate intervention feasibility, including delivery methods, implementers, and locations. Community-based delivery may be necessary to address feasibility, cultural appropriateness, and acceptability issues, as well as to maximise impact. Efforts should also focus on raising awareness of older adults’ health challenges as equity issues. Governments must prioritise ageing as a development issue, particularly in regions with rapidly growing older populations.
Author Contributions
All authors contributed to the responsibility for the following: study conception and design. Abstract and full text screening performed by FK and SA. Quality assessment performed by FK and QG. FK and RM wrote the first draft of the manuscript, and all authors commented on previous versions.
Funding
The author(s) declare that financial support was received for the research, and/or publication of this article. MP was partially funded by MR/T037423/1.
Conflict of Interest
The authors declare that they do not have any conflicts of interest.
Generative AI Statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
References
1. Chang, AY, Skirbekk, VF, Tyrovolas, S, Kassebaum, NJ, and Dieleman, JL. Measuring Population Ageing: An Analysis of the Global Burden of Disease Study 2017. Lancet Public Health (2019) 4(3):e159–67. doi:10.1016/S2468-2667(19)30019-2
2. He, W, Aboderin, I, and Adjaye-Gbewonyo, D. Africa Aging: 2020. U.S. Census Bureau, International Population Reports, P95/20-1. Washington, DC, USA: U.S. Government Printing Office (2020).
3. Fried, LP, Tangen, CM, Walston, J, Newman, AB, Hirsch, C, Gottdiener, J, et al. Frailty in Older Adults: Evidence for a Phenotype. J Gerontol A Biol Sci Med Sci (2001) 56(3):M146–M156. doi:10.1093/gerona/56.3.m146
4. Segar, MW, Singh, S, Goyal, P, Hummel, SL, Maurer, MS, Forman, DE, et al. Prefrailty, Impairment in Physical Function, and Risk of Incident Heart Failure Among Older Adults. J Am Geriatr Soc (2021) 69(9):2486–97. doi:10.1111/jgs.17218
5. O'Caoimh, R, Sezgin, D, O'Donovan, MR, Molloy, DW, Clegg, A, Rockwood, K, et al. Prevalence of Frailty in 62 Countries Across the World: A Systematic Review and Meta-Analysis of Population-Level Studies. Age Ageing (2021) 50(1):96–104. doi:10.1093/ageing/afaa219
6. Siriwardhana, DD, Hardoon, S, Rait, G, Weerasinghe, MC, and Walters, K. Prevalence of Frailty and Prefrailty Among Community-Dwelling Older Adults in Low-Income and Middle-Income Countries: A Systematic Review and Meta-Analysis. BMJ Open (2018) 8(3):e018195. doi:10.1136/bmjopen-2017-018195
7. Clegg, A, Young, J, Iliffe, S, Rikkert, MO, and Rockwood, K. Frailty in Elderly People. Lancet (2013) 381(9868):752–62. doi:10.1016/S0140-6736(12)62167-9
8. Dent, E, Lien, C, Lim, WS, Wong, WC, Wong, CH, Ng, TP, et al. The Asia-Pacific Clinical Practice Guidelines for the Management of Frailty. J Am Med Dir Assoc (2017) 18(7):564–75. doi:10.1016/j.jamda.2017.04.018
9. Mitnitski, AB, Mogilner, AJ, and Rockwood, K. Accumulation of Deficits as a Proxy Measure of Aging. TheScientificWorld (2001) 1:323–36. doi:10.1100/tsw.2001.58
10. Fan, L, Tian, Y, Wang, J, Ding, Y, Wang, S, Xue, H, et al. Frailty Predicts Increased Health Care Utilization Among Community-Dwelling Older Adults: A Longitudinal Study in China. J Am Med Dir Assoc (2021) 22(9):1819–24. doi:10.1016/j.jamda.2021.01.082
11. Ferrucci, L, Guralnik, JM, Studenski, S, Fried, LP, Cutler, GB, Walston, JD, et al. Designing Randomized, Controlled Trials Aimed at Preventing or Delaying Functional Decline and Disability in Frail, Older Persons: A Consensus Report. J Am Geriatr Soc (2004) 52(4):625–34. doi:10.1111/j.1532-5415.2004.52174.x
12. Soysal, P, Veronese, N, Thompson, T, Kahl, KG, Fernandes, BS, Prina, AM, et al. Relationship Between Depression and Frailty in Older Adults: A Systematic Review and Meta-Analysis. Ageing Res Rev (2017) 36:78–87. doi:10.1016/j.arr.2017.03.005
13. Fried, LP, Ferrucci, L, Darer, J, Williamson, JD, and Anderson, G. Untangling the Concepts of Disability, Frailty, and Comorbidity: Implications for Improved Targeting and Care. J Gerontol A Biol Sci Med Sci (2004) 59(3):255–63. doi:10.1093/gerona/59.3.M255
14. de Labra, C, Guimaraes-Pinheiro, C, Maseda, A, Lorenzo, T, and Millán-Calenti, JC. Effects of Physical Exercise Interventions in Frail Older Adults: A Systematic Review of Randomized Controlled Trials. BMC Geriatr (2015) 15(1):154. doi:10.1186/s12877-015-0155-4
15. Theou, O, Stathokostas, L, Roland, KP, Jakobi, JM, Patterson, C, Vandervoort, AA, et al. The Effectiveness of Exercise Interventions for the Management of Frailty: A Systematic Review. J Aging Res (2011) 2011:569194. doi:10.4061/2011/569194
16. Dedeyne, L, Deschodt, M, Verschueren, S, Tournoy, J, and Gielen, E. Effects of Multi-Domain Interventions in (Pre)frail Elderly on Frailty, Functional, and Cognitive Status: A Systematic Review. Clin Interv Aging (2017) 12:873–96. doi:10.2147/CIA.S130794
17. Travers, J, Romero-Ortuno, R, Bailey, J, and Cooney, MT. Delaying and Reversing Frailty: A Systematic Review of Primary Care Interventions. Br J Gen Pract (2019) 69(678):e61–9. doi:10.3399/bjgp18X700241
18. Macdonald, SHF, Travers, J, Ní Shé, É, Bailey, J, Romero-Ortuno, R, Keyes, M, et al. Primary Care Interventions to Address Physical Frailty Among Community-Dwelling Adults Aged 60 Years or Older: A Meta-Analysis. PLoS One (2020) 15(2):e0228821. doi:10.1371/journal.pone.0228821
19. Vijayakumaran, RK, Daly, RM, and Tan, VPS. We Want More: Perspectives of Sarcopenic Older Women on the Feasibility of High-Intensity Progressive Resistance Exercises and a Whey-Protein Nutrition Intervention. Front Nutr (2023) 10:1176523. doi:10.3389/fnut.2023.1176523
20. Mohd Rosnu, NS, Singh, DKA, Mat Ludin, AF, Ishak, WS, Abd Rahman, MH, and Shahar, S. Enablers and Barriers of Accessing Healthcare Services Among Older Adults in South-East Asia: A Scoping Review. Int J Environ Res Public Health (2022) 19(12):7351. doi:10.3390/ijerph19127351
21. Agyeman, N, Guerchet, M, Nyame, S, Tawiah, C, Owusu-Agyei, S, Prince, MJ, et al. When Someone Becomes Old Then Every Part of the Body Too Becomes Old: Experiences of Living With Dementia in Kintampo, Rural Ghana. Transcult Psychiatry (2019) 56(5):895–917. doi:10.1177/1363461519847054
22. Gao, Q, Chua, KC, Mayston, R, and Prina, M. Longitudinal Associations of Loneliness and Social Isolation With Care Dependence Among Older Adults in Latin America and China: A 10/66 Dementia Research Group Population-Based Cohort Study. Int J Geriatr Psychiatry (2024) 39(7):e6115. doi:10.1002/gps.6115
23. Gao, Q, Prina, M, Wu, YT, and Mayston, R. Unmet Healthcare Needs Among Middle-Aged and Older Adults in China. Age Ageing (2022) 51(1):afab235–9. doi:10.1093/ageing/afab235
24. Badrasawi, M, Shahar, S, Zahara, AM, Nor Fadilah, R, and Devinder Kaur Ajit Singh, D. Efficacy of L-Carnitine Supplementation on Frailty Status and its Biomarkers, Nutritional Status, and Physical and Cognitive Function Among Prefrail Older Adults: A Double-Blind, Randomized, Placebo-Controlled Clinical Trial. Clin Interv Aging (2016) 11:1675–86. doi:10.2147/CIA.S113287
25. Chittrakul, J, Siviroj, P, Sungkarat, S, and Sapbamrer, R. Multi-System Physical Exercise Intervention for Fall Prevention and Quality of Life in Pre-frail Older Adults: A Randomized Controlled Trial. Int J Environ Res Public Health (2020) 17(9):3102. doi:10.3390/ijerph17093102
26. Dun, Y, Hu, P, Ripley-Gonzalez, JW, Zhou, N, Li, H, Zhang, W, et al. Effectiveness of a Multicomponent Exercise Program to Reverse Pre-Frailty in Community-Dwelling Chinese Older Adults: A Randomised Controlled Trial. Age Ageing (2022) 51(3):afac026. doi:10.1093/ageing/afac026
27. Favela, J, Castro, LA, Franco-Marina, F, Sánchez-García, S, Juárez-Cedillo, T, Bermudez, CE, et al. Nurse Home Visits With or Without Alert Buttons Versus Usual Care in the Frail Elderly: A Randomized Controlled Trial. Clin Interv Aging (2013) 8:85–95. doi:10.2147/CIA.S38618
28. Jiayuan, Z, Xiang-Zi, J, Li-Na, M, Jin-Wei, Y, and Xue, Y. Effects of Mindfulness-Based Tai Chi Chuan on Physical Performance and Cognitive Function Among Cognitive Frailty Older Adults: A Six-Month Follow-Up of a Randomized Controlled Trial. J Prev Alzheimers Dis (2022) 9(1):104–12. doi:10.14283/jpad.2021.40
29. Lai, X, Bo, L, Zhu, H, Chen, B, Wu, Z, Du, H, et al. Effects of Lower Limb Resistance Exercise on Muscle Strength, Physical Fitness, and Metabolism in Pre-Frail Elderly Patients: A Randomized Controlled Trial. BMC Geriatr (2021) 21(1):447. doi:10.1186/s12877-021-02386-5
30. Lin, H, Ye, Y, Wan, M, Qiu, P, Xia, R, and Zheng, G. Effect of Baduanjin Exercise on Cerebral Blood Flow and Cognitive Frailty in the Community Older Adults With Cognitive Frailty: A Randomized Controlled Trial. J Exerc Sci Fit (2022) 21(2):131–7. doi:10.1016/j.jesf.2022.12.001
31. Valentini Neto, J, de Melo, CM, and Lima Ribeiro, SM. Effects of Three-Month Intake of Synbiotic on Inflammation and Body Composition in the Elderly: A Pilot Study. Nutrients (2013) 5(4):1276–86. doi:10.3390/nu5041276
32. Roschel, H, Hayashi, AP, Fernandes, AL, Jambassi-Filho, JC, Hevia-Larraín, V, de Capitani, M, et al. Supplement-based Nutritional Strategies to Tackle Frailty: A Multifactorial, Double-Blind, Randomized Placebo-Controlled Trial. Clin Nutr (2021) 40(11):4849–58. doi:10.1016/j.clnu.2021.06.024
33. Wan, M, Xia, R, Lin, H, Ye, Y, Qiu, P, and Zheng, G. Baduanjin Exercise Modulates the Hippocampal Subregion Structure in Community-Dwelling Older Adults With Cognitive Frailty. Front Aging Neurosci (2022) 14:956273. doi:10.3389/fnagi.2022.956273
34. Wang, Z, Meng, D, He, S, Guo, H, Tian, Z, Wei, M, et al. The Effectiveness of a Hybrid Exercise Program on the Physical Fitness of Frail Elderly. Int J Environ Res Public Health (2022) 19(17):11063. doi:10.3390/ijerph191711063
35. Raja Adnan, RNE, Mat Din, H, Ashari, A, and Minhat, HS. Effectiveness of a Community-Based Muscle Strengthening Exercise Program to Increase Muscle Strength Among Pre-Frail Older Persons in Malaysia: A Pilot Study. Front Public Health (2021) 9:610184. doi:10.3389/fpubh.2021.610184
36. Chatterjee, P, Kumar, P, Kandel, R, Madan, R, Tyagi, M, Kumar, DA, et al. Nordic Walking Training and Nutritional Supplementation in Pre-Frail Older Indians: An Open-Labelled Experimental Pre-Test and Post-Test Pilot Study to Develop Intervention Model. BMC Geriatr (2018) 18:212. doi:10.1186/s12877-018-0890-4
37. Kang, L, Gao, Y, Liu, X, Liang, Y, Chen, Y, Liang, Y, et al. Effects of Whey Protein Nutritional Supplement on Muscle Function Among Community-Dwelling Frail Older People: A Multicenter Study in China. Arch Gerontol Geriatr (2019) 83:7–12. doi:10.1016/j.archger.2019.03.012
38. Riviati, N, Indrajaya, T, Bahar, E, and Burni, DS. Potential of Omega-3 Supplementation on Muscle Mass, Muscle Strength, and Physical Performance in Elderly Community. Open Access Maced J Med Sci (2021) 9(B):55–9. doi:10.3889/oamjms.2021.5601
39. Tiihonen, K, Ouwehand, AC, and Rautonen, N. Human Intestinal Microbiota and Healthy Ageing. Ageing Res Rev (2010) 9(2):107–16. doi:10.1016/j.arr.2009.10.004
40. Racey, M, Ali, MU, Sherifali, D, Fitzpatrick-Lewis, D, Lewis, R, Jovkovic, M, et al. Effectiveness of Nutrition Interventions and Combined Nutrition and Physical Activity Interventions in Older Adults With Frailty or Prefrailty: A Systematic Review and Meta-Analysis. CMAJ Open (2021) 9(3):E744–56. doi:10.9778/cmajo.20200248
41. Yan, LC, Yu, F, Wang, XY, Yuan, P, Xiao, G, Cheng, QQ, et al. The Effect of Dietary Supplements on Frailty in Older Persons: A Meta-Analysis and Systematic Review of Randomized Controlled Trials. Food Sci Technol (2022) 42:e65222. doi:10.1590/fst.65222
42. Fillit, H, and Butler, RN. The Frailty Identity Crisis. J Am Geriatr Soc (2009) 57(2):348–52. doi:10.1111/j.1532-5415.2008.02104.x
43. Burgess, RA. The Struggle for the Social: Rejecting the False Separation of 'social' Worlds in Mental Health Spaces. Soc Psychiatry Psychiatr Epidemiol (2024) 59(3):409–16. doi:10.1007/s00127-023-02510-3
44. Jitapunkul, S, and Chayovan, N. National Policies on Ageing in Thailand: 2001-2020. Bangkok, Thailand: Chulalongkorn University (2001).
45. Asian Development Bank. Country Diagnostic Study on Long-Term Care in Thailand. Manila, Philippines: Asian Development Bank (2020).
46. Wang, NY, Liu, X, Kong, X, Sumi, Y, Chhetri, JK, Hu, L, et al. Implementation and Impact of the World Health Organization Integrated Care for Older People (ICOPE) Program in China: A Randomised Controlled Trial. Age Ageing (2024) 53:1–10. doi:10.1093/ageing/afad249
47. Sobhani, A, Fadayevatan, R, Sharifi, F, Akbari Kamrani, A, Ejtahed, HS, Hosseini, RS, et al. The Conceptual and Practical Definitions of Frailty in Older Adults: A Systematic Review. J Diabetes Metab Disord (2021) 20:1975–2013. doi:10.1007/s40200-021-00897-x
48. Feng, Z, Glinskaya, E, Chen, H, Gong, S, Qiu, Y, Xu, J, et al. Long-Term Care System for Older Adults in China: Policy Landscape, Challenges, and Future Prospects. Lancet (2020) 396(10259):1362–72. doi:10.1016/S0140-6736(20)32136-X
49. Valenzuela, PL, Saco-Ledo, G, Morales, JS, Gallardo-Gómez, D, Morales-Palomo, F, López-Ortiz, S, et al. Effects of Physical Exercise on Physical Function in Older Adults in Residential Care: A Systematic Review and Network Meta-Analysis of Randomised Controlled Trials. Lancet Healthy Longev (2023) 4(6):e247–56. doi:10.1016/S2666-7568(23)00057-0
50. Davidson, SL, Lee, J, Emmence, L, Bickerstaff, E, Rayers, G, Davidson, E, et al. Systematic Review and Meta-Analysis of the Prevalence of Frailty and Pre-Frailty Amongst Older Hospital Inpatients in Low- and Middle-Income Countries. Age Ageing (2025) 54:afae279. doi:10.1093/ageing/afae279
Keywords: systematic review, older people, frail, prefrail, frailty intervention
Citation: Kongngern F, Prina M, Akhter-Khan SC, Gao Q, Prince M and Mayston R (2025) A Systematic Review of Frailty Interventions in Community-Based Low and Middle-Income Settings. Int. J. Public Health 70:1608089. doi: 10.3389/ijph.2025.1608089
Received: 25 October 2024; Accepted: 03 March 2025;
Published: 16 April 2025.
Edited by:
Saverio Stranges, Western University, CanadaCopyright © 2025 Kongngern, Prina, Akhter-Khan, Gao, Prince and Mayston. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: F. Kongngern, ZnVhbmdmYS5rb25nbmdlcm5Aa2NsLmFjLnVr
 F. Kongngern
F. Kongngern M. Prina2
M. Prina2 S. C. Akhter-Khan
S. C. Akhter-Khan Q. Gao
Q. Gao R. Mayston
R. Mayston