Abstract
Objectives:
To examine trends in socioeconomic inequality in adolescent health over three decades, across fifteen health indicators: overweight, underweight, headache, stomachache, backpain, emotional symptoms, difficulties falling asleep, loneliness, low life satisfaction, low self-rated heath, smoking, drunkenness, physical inactivity, low vegetable intake, and inadequate toothbrushing.
Methods:
The Health Behaviour in School-aged Children (HBSC) study in Denmark included nine identical surveys of 11–15-year-olds from 1991 to 2022, n = 35,423. For each health indicator, we measured absolute and relative socioeconomic inequality by prevalence differences and odds ratios between low and high socioeconomic groups.
Results:
There was socioeconomic inequality in thirteen health indicators, e.g., the OR (95% CI) for overweight in low vs. high socioeconomic groups was 2.22 (1.95–2.49). This social inequality persisted across health indicators throughout the study period with two deviations: Underweight was not associated with socioeconomic background and drunkenness was persistently most prevalent in higher socioeconomic groups.
Conclusion:
The political efforts to reduce socioeconomic inequality in health seems to have failed. It is important to improve monitoring of adolescent health and implement improved policies to tackle socioeconomic inequality in adolescent health.
Introduction
Social inequality in health refers to systematic differences in health between socioeconomic groups. There is ample evidence that adolescents from lower socioeconomic groups have higher risk of poor health and harmful health behaviours [1, 2]. Social inequality in child and adolescent health is a public health concern because the full health potential of children and adolescents from lower socioeconomic groups are not fulfilled [2, 3]. In many countries there has been a strong political interest in reducing social inequalities in health in the past decades [4]. This paper addresses time trends in social inequality in adolescent health from 1991 to 2022 in a country with a strong political desire to reduce this inequality. The analyses include 15 indicators of physical health, mental health, and health behaviours to provide a comprehensive picture of social inequality in adolescent health.
Most indicators of poor physical and mental health show higher prevalence with lower socioeconomic status among adolescents. This is the case for overweight [5–8], pain [9–12], psychological distress [12–16], difficulties falling asleep [17], loneliness [18, 19], poor life satisfaction [20] and poor self-rated health [21, 22]. Adolescents in lower socioeconomic strata have higher prevalences of unhealthy behaviours [23] including smoking [24–26], low vegetable intake [6, 27], physical inactivity [6], and infrequent toothbrushing [28]. Two exceptions are observed. One is underweight, which is not associated with socioeconomic status in high-income countries [29–31]. The other is binge drinking or drunkenness, where the association with socioeconomic status varies across countries [32, 33].
Although social inequality in health is well documented, less is known about secular trends in social inequality in adolescent health. In many domains of adolescent health, the social inequality in health has been either widening or persistent during the past decades. Elgar et al. studied trends from 2002 to 2010 and found widening social inequality in several health indicators, but not life satisfaction [34]. Lampert et al. analysed trends from 2003 to 2017 in general health, mental health, physical activity, consumption of sugary soft drinks, and smoking [35]. They found persistent and, in some cases, widening health inequalities, although sometimes with different developments in absolute and relative social inequality. Moor et al. found a stable pattern of social inequality in life satisfaction, self-rated health, fruit and vegetable consumption, and physical activity from 2009 to 2022 in Germany [36]. Hammani et al. found widening social inequalities from 2002 to 2018 in overweight, physical symptoms, low life satisfaction, and poor self-rated health among Canadian adolescents [37]. Studies of trends in social inequality in weight status among adolescents show widening social inequality in overweight and obesity in the past decades [5, 6, 31, 38]. Social inequalities in underweight has not changed much in Western countries between the 1990s and 2018 [29]. There are few studies of trends in social inequality in pain, psychological distress, loneliness, difficulties in falling asleep, and poor self-rated health. The findings vary by country, but most of the studies covering parts of the period 1990–2018 found persistent or slightly increasing social inequality [1, 10, 13, 39]. Two exceptions show diminishing social inequality due to an increasing rate of health problems among students from higher socioeconomic strata: A study by Madsen et al. showed diminishing social inequality in loneliness 1991–2014 [18] and a study by Due et al. showed diminishing social inequality in emotional symptoms 1991–2014 [40].
Studies analysing trends in social inequality in adolescent smoking since 1990 showed mixed results. Findings indicate a widening gap [25, 41], persistent social inequality [42], a diminishing gap [35] or differening trends for absolute and relative social inequality [24]. Few studies address changes in social inequality for other health behaviours since 1990 and most of these studies report persistent social inequality, however often with differences across countries, sex- and age groups [6, 27, 43–46].
Most studies on trends in social inequality in adolescent health focus on one or few indicators of adolescent health and cover relatively short periods. There is a need for studies which cover a broad range of health indicators over extended periods. Such studies can give insights into the full picture of inequalities of adolescent health and may help determine the success of political efforts to reduce health inequality. Therefore, the objective of this study was to analyse secular trends in social inequality across numerous indicators of adolescent health over a 31-year period, from 1991 to 2022. The study focused on adolescents in Denmark, a country with high per capita income, a high human development index, a relatively low income inequality, a strong political desire to reduce social inequality in health, and a comprehensive tax-financed welfare system.
There are several studies on changes in social inequality in adolescent health from Denmark, and most of these studies show persistent social inequality [7, 10, 18, 20, 25, 27, 29, 40, 44]. This new study included five indicators of physical health, five on mental health, and five on health behaviours. This study is challenged by two competing hypotheses: First, that the political ambition to reduce social inequality in health in Denmark has been successful. Second, that macroeconomic conditions have resulted in increasing social inequality in health. In general, social inequality in health increases with increasing income disparities in the society [34, 47, 48] and there has been a substantial and continuous upward trend in income inequality in Denmark during the past 30 years with an increase in the Gini-coefficient from 22 in 1991 to 30 in 2022 [49].
Methods
Study Design and Study Population
Data stem from the Danish arm of the international Health Behaviour in School-aged Children (HBSC) study, which collected questionnaire data among nationally representative samples of 11-, 13- and 15-year-olds about health and health behaviours [50]. The study design was cross-sectional, and data collections was repeated every 4 years following a standard protocol for sampling, measurement, and data collection. This enabled comparison of data across survey waves. Students completed the questionnaire during a school class. This study used data from nine HBSC surveys in Denmark in 1991, 1994, 1998, 2002, 2006, 2010, 2014, 2018 and 2022.
Across all waves of data collection, participants were recruited from random samples of schools, a new sample in each wave, drawn from complete lists of public and private schools in Denmark. In each school we invited all students in the fifth, seventh and ninth grade (corresponding to the age groups 11, 13 and 15) to complete the internationally standardized HBSC questionnaire in the classroom [50]. Student participation rate across all nine waves was 84.9%, n = 41,143, ranging from 90.2% in 1991 to 70.1% in 2022. School participation rate across survey waves was 37.4%, with a decline from 82.6% in 1991 to 16.0% in 2022. The most common reason for declining participation was recent participation in similar surveys. The low participation rate in 2022 was also related to schools needing to prioritize issues related to COVID-19.
Outcome Measures
Table 1 displays the applied 15 indicators of health and health behaviours, the survey years in which they were included, their cutoff points, and validity. There were five indicators of physical health: 1) Overweight and 2) underweight based on self-reported height and weight classified by the method recommended by Cole and Lobstein [51]. 3) Headache more than once a week, 4) stomachache more than once a week, and 5) backpain more than once a week. The questions on pain originate from the HBSC Multiple Health Complaints Measure [53–56], and we used them as separate measures because pain is not only psychosomatic: these three kinds of pain may each reflect specific somatic health problems. We used the cut-off point more than once a week to separate students with severe burden of pain.
TABLE 1
| Measurement and item formulation | Response categories and cutoff points | Reliability and validity | |
|---|---|---|---|
| 1. Overweight (1998–2022) | Self-reported weight and height measured by the items: “How much do you weigh without clothes?” and “How tall are you without shoes?”a Calculation of BMI (kg/m2) |
Internationally standardized age- and sex-specific cutoff points [51] to categorize weight status into overweight and obese combined, normal weight, and underweight (thinness grade 2–3) | The difference in BMI calculated from self-reported and objective data are modest, on average by 0.8 kg for boys and 1.8 kg for girls [52] |
| 2. Underweight (1998–2022) | |||
| 3. Headache more than once a week (1998–2022) | “In the last 6 months, how often have you had headache?”a | Items from the HBSC Multiple Health Complaints Measure [53]. Cutoff points as in reference [11] Responses dichotomized into more than once a week (“about every day” and “more than once a week”) vs. less often (“about every week,” “about every month,” and “rarely or never”) |
Studies suggested that this measure is reliable assessed by consistent response patterns and valid assessed by qualitative interviews [53–56] |
| 4. Stomachache more than once a week (1998–2022) | “In the last 6 months, how often have you had stomach-ache?”a | ||
| 5. Backpain more than once a week (1998–2022) | “In the last 6 months, how often have you had backpain?”a | ||
| 6. Daily emotional symptoms (1998–2022) | Three items from the HBSC Multiple Health Complaints Measure [53],a “In the last 6 months, how often have you been … • feeling low • Irritability or • bad temper • feeling nervous |
Responses dichotomized into daily (“about every day”) vs. less often (“more than once a week,” “about every week,” “about every month,” and “rarely or never”) The index separated students who answered “about every day” to at least one of these items [57] |
Studies suggested that this measure is reliable assessed by consistent response patterns and valid assessed by qualitative interviews [53–56] |
| 7. Difficulties falling asleep daily (1998–2022) | Item from the HBSC Multiple Health Complaints Measure [53].a“In the last 6 months, how often have you had the following: … difficulties in getting to sleep?” | Responses dichotomized into daily (“about every day”) vs. less frequent (“more than once a week,” “about every week,” “about every month,” and “rarely or never”) | |
| 8. Loneliness often/very often (1991–1998, 2010–2022) | National item, not part of the HBSC protocol “Do you feel lonely?” |
Responses dichotomised in accordance with prior studies (18.57) into lonely (“Yes very often” + “yes often”) vs. not lonely (“sometimes” + “never”) | The measurement was valid assessed by qualitative interviews [58] and correspondence with other loneliness measures [59, 60] |
| 9. Low life satisfaction (2006–2022) | The Cantril Laddera [61] presents a ladder of 11 steps from 0 to 10 where 10 indicates the “best possible life” and 0 “the worst possible life” for you and asks: “Where on the ladder do you feel you stand at the moment?” | Cutoff points as in reference [20]: Cutoff point of 0–5 versus 6–10 to categorise low versus high score | This measure is reliable and valid for use with adolescents [61]. Responses were significantly associated with self-perception, psychological wellbeing, parent relations, mood and emotions among adolescents and therefore appears to be a useful indicator of adolescents’ life satisfaction [62] |
| 10. Poor self-rated health (1991, 2002–2022) | 1991: “What do you think about your health at present?” 2002–2022: “Would you say your health is … excellent, good, fair, poor?”a |
Cutoff points as in reference [21]: Responses dichotomised into poor (poor, fair) and good (good, excellent) | Self-rated health is valid for disparities research in large, population-based surveys of adolescents [63] |
| 11. Smoking, 15-year-olds (1998–2022) | “How often do you smoke?”a | Responses dichotomised into “every day” +“at least once a week, but not every day” vs. “less than once a week,” “I do not smoke” | Self-reported smoking among adolescents has acceptable agreement with objective measures, e.g., salivary cotinine [64, 65] |
| 12. Drunkenness, 15-year-olds (1998–2022) | “Have you ever had so much alcohol that you were really drunk?”a | Cutoff points as in reference [45]: Responses dichotomized into high (”4–10 times” and “more than 10 times”) vs less. [33] | Studies suggest that adolescents’ information about their alcohol use is valid and reliable [66, 67] |
| 13. Physical inactivity (1998–2022) | “OUTSIDE SCHOOL HOURS: How many hours a week do you usually exercise in your free time so much that you get out of breath or sweat?”a | Cutoff points as in reference [44]: We dichotomised the responses into “none” vs. “about half an hour” + “about 1 h” + “about 2–3 h” + “about 4–6 h” + “7 h or more” | This measure showed good reliability and a fair validity in the sense that adolescents who reported 0 h of vigorous physical activity also have low aerobic fitness [68, 69]. Toftager et al. showed that high level of self-reported vigorous physical activity corresponded with device-based measures [70] |
| 14. Low vegetable intake (2002–2022) | “How many days a week do you usually eat vegetables?”a Cutoff points as in reference [27] |
Responses dichotomized into low (“never” + “less than once a week”) vs. more often (“once a week,” “2-4 days a week,” “5-6 days a week,” “once a day every day” and “every day more than once”) | A validation study reported that this measure was reliable as assessed by test-retest agreement and valid as assessed by comparison with a seven-day food diary [71] |
| 15. Infrequent toothbrushing (1998–2022) | “How often do you brush your teeth?”a | Responses dichotomised according to official recommendations into frequent (“more than once a day”) vs infrequent (“once a day” + “at least once a week but not daily” + “less than once a week” + “never”) | Children’s self-reported toothbrushing habits was highly correlated with their clinically measured oral health [72] |
Measurement of health indicators (Denmark, 1991–2022).
Item from the internationally standardized HBSC questionnaire.
There were five indicators of mental health: 6) Daily emotional symptoms, an index based on three items from the HBSC Multiple Health Complaints Measure [56]. These items were so strongly intercorrelated that we suspected they measured the same aspects of emotional mental health. 7) Difficulties falling asleep every day measured by an item from the HBSC Multiple Health Complaints Measure [56]. 8) Loneliness measured by one validated item from the Danish HBSC questionnaire [58–60]; 9) low life satisfaction measured by the validated Cantril ladder [61, 62]; and 10) poor self-rated health, which is considered a valid measure encompassing aspects of both physical and mental health conditions [63]. We chose to categorize self-rated health as a mental health variable.
Finally, the study included five health compromising behaviours: 11) Smoking, only among 15-year-olds, measured by one item; 12) drunkenness, only among 15-year-olds, measured by one item. These two measurements were reported as valid at the population level [64, 66, 67]. 13) Physical inactivity measured by one item on vigorous physical activity which validly can identify a very low activity level [68–70]; 14) low vegetable intake measured by one item with acceptable validity [71], and 15) infrequent toothbrushing measured by one item with acceptable validity [72].
All outcome measures except loneliness used questions from the internationally standardized HBSC questionnaire [50]. Nine of the 15 health indicators were included in all nine survey years, and the remaining six indicators were included in most but not all survey years (Table 1). The formulation of the items and response categories in the questionnaire were similar across survey years except for a small deviation in the item about self-rated health (Table 1). Choice of cutoff points (see Table 1) was justified by two considerations, first to reflect a serious threat to adolescent health, and second to ensure enough students in the unfavourable category. Some of our cutoff points deviated from the practice within the HBSC project [50].
Socioeconomic Measure
We measured the students’ socioeconomic status by their parents’ occupational social class (OSC). The students answered the following questions: “Does your father/mother have a job?”, “If no, why does he/she not have a job?”, “If yes, please write in what place he/she works (for example,: hospital, bank, restaurant)” and “Please write down exactly what job he/she does there (for example: teacher, bus driver).” The research group coded the responses in accordance with the Danish Occupational Social Class measure [73], ranging from I (high) to V (low) and VI for economically inactive parents who received unemployment benefits, disability pension or other kinds of transfer income, similarly based on students’ responses. The questions and coding of occupations were identical across surveys. Job titles change over time, but the coding procedure was unaffected by such changes, because we assessed occupations by two universal characteristics: 1) required educational qualifications and 2) control (over capital or people) connected with the occupation. Each participant was categorized by the highest-ranking parent into three levels of OSC: High (I-II, e.g., professionals and managerial positions, large-scale business owners), middle (III-IV, e.g., technical and administrative staff, small-scale business owners, skilled workers), and low (V, unskilled workers and VI, economically inactive). Students with insufficient information about OSC (n = 5720, 13.9% of the participants) were excluded from the analyses. The study included sex and age group as covariates.
Statistical Procedures
This study included students with complete information about sex, age group, and the family’s OSC, n = 35,423. The analyses involved assessment of absolute social inequality estimated by prevalence differences between low and high OSC groups and relative social inequality estimated by logistic regression analyses.
We used SAS version 9.4 for the analyses. The first step was contingency tables to describe the prevalence of each health indicator by survey year and OSC. The second step was calculation of prevalence differences between low and high OSC and chi2-test of statistical significance of the differences between low and high OSC groups. The third step, time trends: We assessed time trends within each OSC group by the Cochran-Armitage test. This test aims to assess an association between a variable with two categories (here: each health indicator, one at the time) and an ordinal variable (here: survey year). The fourth step was logistic regression analyses to examine the sex- and age group adjusted association between the outcome variables (each health indicator, one at the time) and OSC group in each survey year. We report the results as odds ratios (OR) with 95% confidence interval (95% CI).
Finally, we investigated whether the social inequality changed during the study period. We conducted the logistic regression analyses for the entire period (all survey years) with inclusion of an interaction term (year*OSC) to assess if the effect of OSC on the health indicators was modified by year. Statistical interaction was reported by p-values (pint) to show whether this modification was statistically significant. The logistic regression analyses accounted for the applied cluster sampling by means of multilevel modelling (PROC GLIMMIX in SAS).
Results
Table 2 shows the characteristics of the study population. There was an equal share of boys and girls, and an almost equal share of students in the three age groups. The OSC distribution changed over the study period. The high OSC group constituted 28.2% of the students in 1991, increasing to 52.0% in 2022. The low OSC group constituted 20.0% of the students in 1991, decreasing to 10.2% in 2022.
TABLE 2
| 1991 | 1994 | 1998 | 2002 | 2006 | 2010 | 2014 | 2018 | 2022 | Total | |
|---|---|---|---|---|---|---|---|---|---|---|
| Invited schools, n | 23 | 50 | 64 | 78 | 100 | 137 | 168 | 200 | 588 | 1,408 |
| Participating schools, n | 19 | 45 | 55 | 68 | 80 | 73 | 48 | 45 | 94 | 527 |
| School participation rate % | 82.6 | 90.0 | 85.9 | 87.2 | 80.0 | 53.3 | 28.6 | 22.5 | 16.0 | 37.4 |
| Student response rate, % | 90.2 | 89.5 | 89.9 | 89.3 | 88.8 | 86.3 | 85.7 | 84.8 | 70.1 | 84.9 |
| Students in the data file | 1,860 | 4,046 | 5,205 | 4,824 | 6,269 | 4,922 | 4,534 | 3,660 | 5,823 | 41,143 |
| Study populationa | 1,696 | 3,683 | 4,810 | 4,306 | 5,041 | 4,171 | 3,946 | 3,015 | 4,749 | 35,423 |
| Pct. girls | 49.9 | 50.7 | 50.4 | 52.0 | 51.5 | 51.0 | 52.1 | 51.4 | 51.7 | 51.3 |
| Pct. 11-year-olds Pct. 13-year-olds Pct. 15year-olds |
30.1 34.7 35.3 |
30.7 34.6 34.7 |
33.6 35.5 30.9 |
35.4 33.1 31.4 |
36.3 36.0 27.7 |
35.5 34.5 30.0 |
30.5 35.4 34.1 |
39.2 34.4 27.4 |
33.9 36.7 29.4 |
34.1 35.1 30.8 |
| Pct. high OSC Pct. medium OSC Pct. low OSC |
28.2 51.8 20.0 |
33.0 48.6 18.4 |
27.9 49.6 22.5 |
24.7 54.3 21.0 |
27.6 49.6 22.8 |
38.7 42.2 19.2 |
42.2 41.5 16.4 |
42.8 44.7 12.4 |
52.0 37.8 10.2 |
36.4 46.4 18.2 |
School and student response rate and participants by sex, age group, and occupational social class (OSC) (Denmark, 1991–2022).
Students with information about occupational social class.
Figure 1 shows the prevalence (pct.) of each health indicator by OSC in each survey year from 1991 to 2022. There were fluctuations, but almost consistently across survey years the prevalence of health problems was higher in low than high OSC. There were two exceptions: underweight was not associated with OSC, and drunkenness was more prevalent in high than low OSC in most survey waves.
FIGURE 1
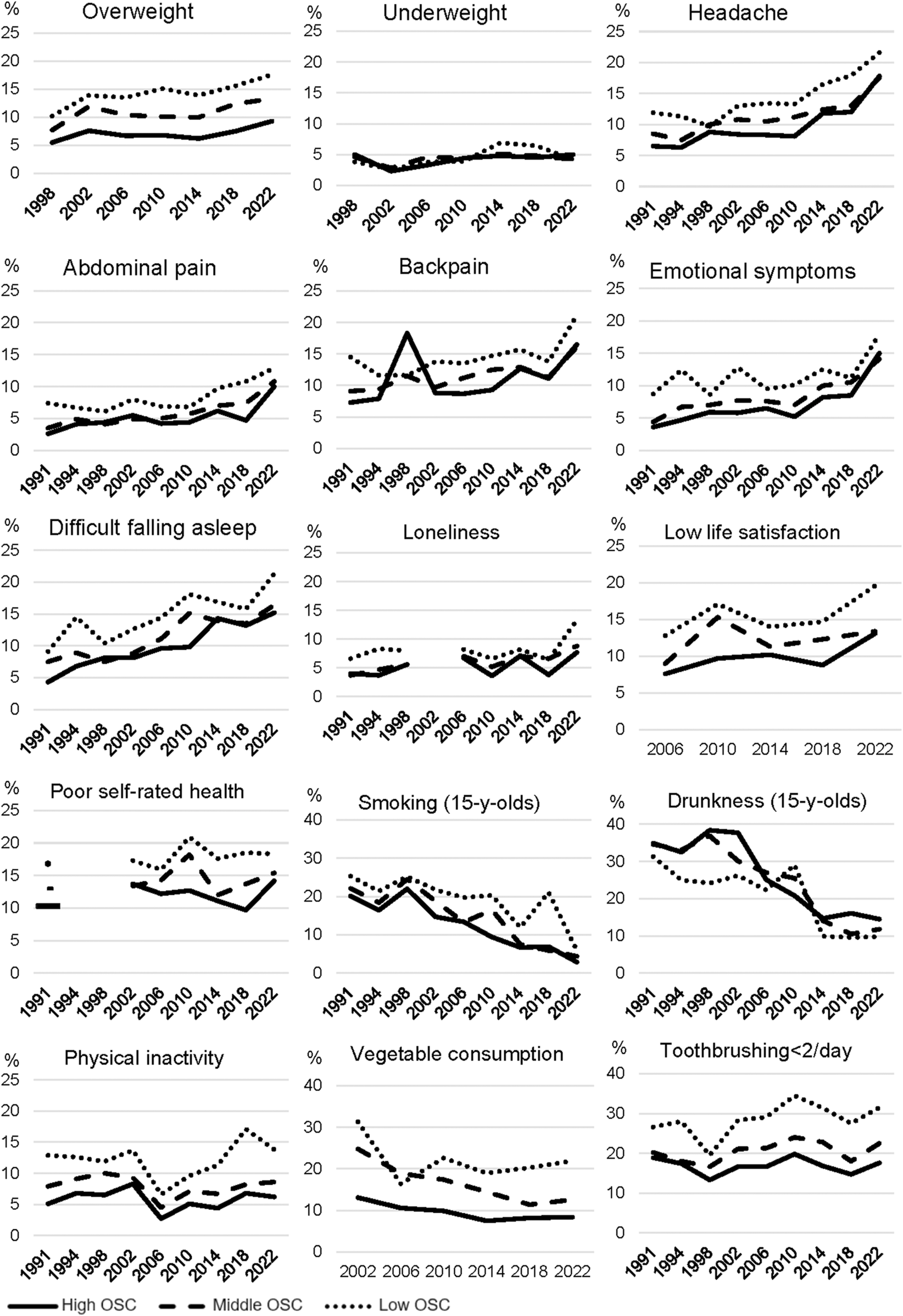
Prevalence of 15 health indicators by survey year and occupational social class (OSC) (Denmark, 1991–2022).
Tables 3–5 shows the prevalence of each health indicator in each year and in each OSC group. The columns “Prevalence Difference” shows the difference between low and high OSC group including a chi2-test for statistical difference. The lines “Time trend” shows the trend over time, tested by the Cochran-Armitage test.
TABLE 3
| Survey year | Absolute social inequality described by prevalence and prevalence difference (%) | Relative social inequality described by sex- and age adjusted OR (95% CI) | ||||||
|---|---|---|---|---|---|---|---|---|
| Occupational social class (OSC) | Occupational social class (OSC) | |||||||
| High | Middle | Low | Prev. Diffa | High | Middle | Low | ||
| Overweight | 1998 | 5.5 | 7.7 | 10.2 | 4.7*** | 1 | 1.43 (1.06–1.92) | 2.06 (1.48–2.86) |
| 2002 | 7.6 | 11.9 | 13.9 | 6.3*** | 1 | 1.69 (1.29–2.22) | 1.99 (1.45–2.72) | |
| 2006 | 6.7 | 10.4 | 13.5 | 6.8*** | 1 | 1.61 (1.23–2.10) | 2.20 (1.64–2.94) | |
| 2010 | 6.8 | 10.1 | 15.1 | 8.3*** | 1 | 1.55 (1.18–2.03) | 2.47 (1.82–3.36) | |
| 2014 | 6.2 | 10.0 | 13.9 | 7.7*** | 1 | 1.72 (1.32–2.24) | 2.56 (1.87–3.50) | |
| 2018 | 7.5 | 12.4 | 15.6 | 8.1*** | 1 | 1.77 (1.34–2.33) | 1.24 (1.66–2.48) | |
| 2022 | 9.3 | 13.3 | 17.6 | 8.3*** | 1 | 1.50 (1.23–1.83) | 2.11 (1.58–2.80) | |
| Years (1998–2022)b | 7.3 | 10.7 | 13.7 | 6.4*** | 1 | 1.60 (1.46–1.77) | 2.22 (1.95–2.49) | |
| Time trendc | Up** | Up*** | Up** | pint = 0.9618d | ||||
| Underweight | 1998 | 5.0 | 4.6 | 3.8 | −1.2 | 1 | 0.91 (0.65–1.27) | 0.69 (0.49–1.06) |
| 2002 | 2.3 | 2.8 | 2.6 | 0.3 | 1 | 0.93 (0.59–1.48) | 0.86 (0.48–1.54) | |
| 2006 | 3.3 | 4.6 | 3.8 | 0.5 | 1 | 1.41 (0.97–2.04) | 1.13 (0.72–1.79) | |
| 2010 | 4.4 | 4.4 | 3.9 | −0.5 | 1 | 0.97 (0.68–1.39) | 0.84 (0.52–1.36) | |
| 2014 | 4.8 | 5.1 | 6.9 | 2.1 | 1 | 0.99 (0.72–1.38) | 1.27 (0.85–1.89) | |
| 2018 | 4.5 | 4.8 | 6.4 | 1.9 | 1 | 1.05 (0.72–1.54) | 1.39 (0.82–2.35) | |
| 2022 | 5.0 | 4.2 | 4.2 | −0.8 | 1 | 0.84 (0.62–1.13) | 0.80 (0.48–1.33) | |
| Years (1998–2022)b | 5.0 | 4.6 | 3.8 | −1.2 | 1 | 1.00 (0.87–1.14) | 0.95 (0.80–1.13) | |
| Time trendc | Stable | Stable | Up* | pint = 0.5026d | ||||
| Headache | 1991 | 6.5 | 8.5 | 11.9 | 5.4** | 1 | 1.38 (0.89–2.14) | 1.97 (1.20–3.26) |
| 1994 | 6.3 | 7.5 | 11.3 | 5.0*** | 1 | 1.18 (0.88–1.59) | 1.82 (1.30–2.55) | |
| 1998 | 8.8 | 10.0 | 9.7 | 0.9 | 1 | 1.16 (0.91–1.46) | 1.09 (0.82–1.44) | |
| 2002 | 8.4 | 10.8 | 13.0 | 4.6** | 1 | 1.26 (0.98–1.63) | 1.58 (1.17–2.12) | |
| 2006 | 8.3 | 10.5 | 13.4 | 5.1*** | 1 | 1.27 (1.01–1.61) | 1.69 (1.30–2.18) | |
| 2010 | 8.1 | 11.2 | 13.3 | 5.2*** | 1 | 1.42 (1.12–1.79) | 1.74 (1.32–2.29) | |
| 2014 | 11.8 | 12.4 | 16.5 | 4.7** | 1 | 1.00 (0.81–1.24) | 1.41 (1.09–1.84) | |
| 2018 | 12.0 | 13.0 | 17.9 | 5.9** | 1 | 1.09 (0.86–1.38) | 1.66 (1.21–2.29) | |
| 2022 | 17.8 | 17.5 | 21.6 | 3.8 | 1 | 1.00 (0.85–1.18) | 1.35 (1.05–1.73) | |
| Years (1991–2022)b | 10.8 | 11.3 | 13.6 | 2.8*** | 1 | 1.14 (1.06–1.23) | 1.49 (1.35–1.63) | |
| Time trendc | Up*** | Up*** | Up*** | pint = 0.1842d | ||||
| Stomachache | 1991 | 2.6 | 3.5 | 7.4 | 4.8** | 1 | 1.43 (0.72–2.83) | 2.85 (1.39–5.83) |
| 1994 | 4.1 | 4.9 | 6.7 | 2.6* | 1 | 1.15 (0.80–1,65) | 1.53 (1.00–2.34) | |
| 1998 | 4.4 | 4.1 | 6.1 | 1.7 | 1 | 0.95 (0.69–1.33) | 1.31 (0.91–1.90) | |
| 2002 | 5.5 | 4.9 | 8.0 | 2.5* | 1 | 0.82 (0.59–1.14) | 1.38 (0.96–1.99) | |
| 2006 | 4.2 | 5.0 | 6.9 | 2.7* | 1 | 1.15 (0.83–1.58) | 1.65 (1.16–2.34) | |
| 2010 | 4.4 | 5.7 | 6.8 | 2.4* | 1 | 1.29 (0.94–1.77) | 1.54 (1.06–2.22) | |
| 2014 | 6.2 | 7.0 | 9.7 | 3.5* | 1 | 1.06 (0.80–1.41) | 1.50 (1.07–2.11) | |
| 2018 | 4.7 | 7.4 | 10.8 | 6.1*** | 1 | 1.59 (1.14–2.22) | 2.44 (1.60–3.72) | |
| 2022 | 10.0 | 10.8 | 12.9 | 2.9 | 1 | 1.12 (0.91–1.37) | 1.35 (1.00–1.84) | |
| Years (1991–2022)b | 5.7 | 5.9 | 7.9 | 2.0*** | 1 | 1.12 (1.01–1.24) | 1.59 (1.40–1.80) | |
| Time trendc | Up*** | Up*** | Up*** | pint = 0.3998d | ||||
| Backpain | 1991 | 7.3 | 9.1 | 14.5 | 7.2** | 1 | 1.24 (0.81–1.90) | 2.35 (1.46–3.77) |
| 1994 | 7.9 | 9.4 | 11.6 | 3.7* | 1 | 1.21 (0.92–1.58) | 1.53 (1.11–2.22) | |
| 1998 | 8.3 | 11.5 | 11.6 | 3.3* | 1 | 1.42 (1.12–1.79) | 1.55 (1.17–2.04) | |
| 2002 | 8.8 | 9.7 | 13.8 | 5.0** | 1 | 1.11 (0.86–1.43) | 1.68 (1.26–2.23) | |
| 2006 | 8.7 | 11.2 | 13.5 | 4.8*** | 1 | 1.31 (1.05–1.64) | 1.66 (1.29–2.14) | |
| 2010 | 9.3 | 12.5 | 14.7 | 5.4*** | 1 | 1.40 (1.12–1.75) | 1.73 (1.33–2.25) | |
| 2014 | 12.7 | 12.9 | 15.7 | 3.0 | 1 | 1.00 (0.81–1.23) | 1.27 (0.97–1.66) | |
| 2018 | 11.1 | 11.3 | 13.8 | 2.7 | 1 | 1.02 (0.80–1.31) | 1.33 (0.94–1.88) | |
| 2022 | 16.5 | 16.1 | 21.1 | 4.6* | 1 | 0.99 (0.84–1.18) | 1.45 (1.13–1.86) | |
| Years (1991–2022)b | 10.9 | 11.6 | 14.0 | 3.1*** | 1 | 1.15 (1.07–1.25) | 1.52 (1.39–1.67) | |
| Time trendc | Up*** | Up*** | Up*** | pint = 0.2842d | ||||
Physical health indicators by occupational social class; expressed as absolute and relative social inequality (Denmark, 1991–2022).
Prevalence in low OSC minus prevalence in high OSC.
Logistic regression analyses combining all survey years adjusted for sex, age group, and survey year.
Time trends assessed by Cochran-Armitage test. Statistical significance at the 95% level: *<0.05, **<0.001, **<0.0001.
pint is the p-value for statistical interaction between year and OSC.
Bold text indicating significant results.
TABLE 4
| Survey year | Absolute social inequality described by prevalence and prevalence difference (%) | Relative social inequality described by sex- and age adjusted OR (95% CI) | ||||||
|---|---|---|---|---|---|---|---|---|
| Occupational social class (OSC) | Occupational social class (OSC) | |||||||
| High | Middle | Low | Prev. Diffa | High | Middle | Low | ||
| Emotional symptoms | 1991 | 3.6 | 4.4 | 8.7 | 5.1* | 1 | 1.21 (0.67–2.17) | 2.53 (1.36–4.70) |
| 1994 | 4.7 | 6.7 | 12.4 | 7.7*** | 1 | 1.44 (1.04–2.00) | 2.79 (1.96–3.99) | |
| 1998 | 5.9 | 7.0 | 8.6 | 2.7* | 1 | 1.21 (0.92–1.60) | 1.49 (1.02–2.06) | |
| 2002 | 5.8 | 7.7 | 12.8 | 7.0*** | 1 | 1.29 (0.95–1.74) | 2.29 (1.65–3.18) | |
| 2006 | 6.5 | 7.6 | 9.5 | 3.0* | 1 | 1.16 (0.89–1.50) | 1.49 (1.11–1.99) | |
| 2010 | 5.2 | 7.0 | 10.1 | 4.9*** | 1 | 1.34 (1.01–1.80) | 1.86 (1.43–2.73) | |
| 2014 | 9.2 | 10.0 | 12.5 | 3.3*** | 1 | 1.03 (0.81–1.30) | 1.32 (0.98–1.77) | |
| 2018 | 8.5 | 10.5 | 11.2 | 2.7 | 1 | 1.24 (0.95–1.62) | 1.37 (0.94–2.00) | |
| 2022 | 15.0 | 14.1 | 17.9 | 2.9 | 1 | 1.09 (0.79–1.13) | 1.28 (0.98–1.67) | |
| Years (1991–2022)b | 8.2 | 8.4 | 11.2 | 3.0*** | 1 | 1.13 (1.04–1.23) | 1.63 (1.47–1.81) | |
| Time trendc | Up*** | Up*** | Up** | pint = 0.0122d | ||||
| Difficulties falling asleep | 1991 | 4.3 | 7.5 | 9.1 | 4.8* | 1 | 1.79 (1.07–3.00) | 2.15 (1.20–3.87) |
| 1994 | 6.8 | 8.9 | 14.5 | 7.7*** | 1 | 1.30 (0.98–1.72) | 2.22 (1.62–3.05) | |
| 1998 | 8.1 | 7.5 | 10.4 | 2.3 | 1 | 0.92 (0.72–1,19) | 1.22 (0.92–1.62) | |
| 2002 | 8.1 | 8.8 | 12.6 | 4.5*** | 1 | 1.07 (0.82–1.40) | 1.58 (1.17–2.14) | |
| 2006 | 9.6 | 11.1 | 14.4 | 4.8** | 1 | 1.15 (0.93–1.44) | 1.55 (1.21–1.98) | |
| 2010 | 9.8 | 15.1 | 18.1 | 8.3*** | 1 | 1.63 (1.32–2.01) | 2.00 (1.56–2.56) | |
| 2014 | 14.3 | 13.9 | 16.9 | 2.6 | 1 | 0.95 (0.77–1.16) | 1.17 (0.90–1.51) | |
| 2018 | 13.2 | 13.5 | 15.8 | 2.6 | 1 | 1.02 (0.81–1.27) | 1.21 (0.88–1.68) | |
| 2022 | 15.2 | 16.4 | 21.3 | 6.1* | 1 | 1.09 (0.93–1.30) | 1.49 (1.16–1.91) | |
| Years (1991–2022)b | 11.0 | 11.3 | 14.5 | 3.5*** | 1 | 1.33 (1.05–1.22) | 1.53 (1.39–1.67) | |
| Time trendc | Up*** | Up*** | Up*** | pint = 0.0081d | ||||
| Loneliness | 1991 | 4.0 | 3.7 | 6.6 | 2.6 | 1 | 0.93 (0.52–1.65) | 1.65 (0.88–3.12) |
| 1994 | 3.7 | 4.7 | 8.3 | 4.6*** | 1 | 1.26 (0.87–1.83) | 2.26 (1.51–3.39) | |
| 1998 | 5.6 | 5.6 | 8.0 | 2.4* | 1 | 1.00 (0.75–1.35) | 1.47 (1.06–2.03) | |
| 2010 | 3.6 | 5.2 | 6.6 | 3.0* | 1 | 1.47 (0.96–2.23) | 1.86 (1.15–3.02) | |
| 2014 | 7.1 | 7.0 | 8.2 | 1.1 | 1 | 0.98 (0.73–1.25) | 1.17 (0.83–1.65) | |
| 2018 | 3.8 | 6.6 | 6.4 | 2.6* | 1 | 1.75 (1.22–2.50) | 1.76 (1.06–2.93) | |
| 2022 | 7.7 | 8.8 | 13.3 | 5.6*** | 1 | 1.18 (0.94–1.48) | 1.94 (1.41–2.66) | |
| Years (1991–1998, 2010–2022)b | 5.8 | 6.3 | 8.2 | 3.4*** | 1 | 1.14 (1.02–1.27) | 1.57 (1.37–1.79) | |
| Time trendc | Up*** | Up*** | Up* | pint = 0.0401d | ||||
| Low life satisfaction | 2006 | 7.6 | 9.0 | 12.8 | 5.2*** | 1 | 1.18 (0.92–1.50) | 1.78 (1.37–2.33) |
| 2010 | 9.7 | 15.3 | 17.1 | 7.4*** | 1 | 1.65 (1.33–2.04) | 1.88 (1.47–2.42) | |
| 2014 | 10.2 | 11.3 | 13.7 | 2.5* | 1 | 1.07 (0.86–1.34) | 1.36 (1.03–1.80) | |
| 2018 | 8.8 | 12.3 | 14.7 | 5.9** | 1 | 1.44 (1.12–1.86) | 1.80 (1.26–2.55) | |
| 2022 | 13.1 | 13.4 | 19.6 | 6.5** | 1 | 1.05 (0.87–1.26) | 1.73 (1.33–2.24) | |
| Years (2006–2022)b | 10.4 | 11.9 | 15.2 | 4.8*** | 1 | 1.21 (1.02–1.33) | 1.66 (1.49–1.86) | |
| Time trendc | Up*** | Up** | Up* | pint = 0.0762d | ||||
| Poor self-rated health | 1991 | 10.6 | 13.1 | 16.6 | 6.0* | 1 | 1.28 (0.90–1.83) | 1.79 (1.19–2.71) |
| 2002 | 13.8 | 13.2 | 17.5 | 3.7* | 1 | 0.97 (0.78–1.20) | 1.34 (1.04–1.71) | |
| 2006 | 12.3 | 14.1 | 15.7 | 3.4* | 1 | 1.18 (0.97–1.43) | 1.35 (1.08–1.70) | |
| 2010 | 12.8 | 18.2 | 21.2 | 8.4*** | 1 | 1.52 (1.25–1.85) | 1.84 (1.46–2.31) | |
| 2014 | 11.1 | 12.2 | 18.2 | 7.1*** | 1 | 1.08 (0.87–1.34) | 1.74 (1.34–2.25) | |
| 2018 | 9.8 | 13.5 | 18.6 | 8.8*** | 1 | 1.47 (1.15–1.88) | 2.13 (1.54–2.84) | |
| 2022 | 14.2 | 15.2 | 18.5 | 4.3* | 1 | 1.12 (0.94–1.33) | 1.42 (1.09–1.84) | |
| Years (1991, 2002–2022)b | 12.4 | 14.3 | 17.9 | 5.5*** | 1 | 1.19 (1.14–1.29) | 1.54 (1.40–1.69) | |
| Time trendc | Stable | Stable | Stable | pint = 0.0176d | ||||
Mental health indicators by occupational social class; expressed as absolute and relative social inequality (Denmark, 1991–2022).
Prevalence in low OSC minus prevalence in high OSC.
Logistic regression analyses combining all survey years adjusted for sex, age group, and survey year.
Time trends assessed by Cochran-Armitage test. Statistical significance at the 95% level: *<0.05, **<0.001, **<0.0001.
pint is the p-value for statistical interaction between year and OSC.
Bold text indicating significant results.
TABLE 5
| Survey year | Absolute social inequality described by prevalence and prevalence difference (%) | Relative social inequality described by sex- and age adjusted OR (95% CI) | ||||||
|---|---|---|---|---|---|---|---|---|
| Occupational social class (OSC) | Occupational social class (OSC) | |||||||
| High | Middle | Low | Prev. Diffa | High | Middle | Low | ||
| Smoking weekly (15-year-olds) | 1991 | 20.1 | 22.1 | 25.3 | 5.2 | 1 | 1.14 (0.71–1.82) | 1.36 (0.74–2.48) |
| 1994 | 16.4 | 18.4 | 21.4 | 5.0 | 1 | 1.22 (0.78–1.82) | 0.93 (0.51–1.73) | |
| 1998 | 22.0 | 24.5 | 25.2 | 3.2 | 1 | 1.13 (0.86–1.49) | 1.18 (0.82–1.70) | |
| 2002 | 14.7 | 18.8 | 21.8 | 7.1* | 1 | 1.32 (0.94–1.86) | 1.60 (1.06–2.41) | |
| 2006 | 13.4 | 13.3 | 19.7 | 6.3* | 1 | 1.01 (0.70–1.45) | 1.62 (1.07–2.44) | |
| 2010 | 9.4 | 16.5 | 20.3 | 10.9*** | 1 | 2.14 (1.13–4.06) | 2.72 (1.31–5.65) | |
| 2014 | 6.7 | 7.5 | 11.9 | 5.1* | 1 | 1.14 (0.73–1.79) | 1.89 (1.10–3.26) | |
| 2018 | 6.9 | 5.9 | 21.1 | 14.2*** | 1 | 0.63 (0.17–2.97) | 3.87 (1.18–12.7) | |
| 2022 | 2.9 | 4.4 | 5.9 | 3.0 | 1 | 1.56 (0.86–2.83) | 2.17 (0.90–5.22) | |
| Years (1991–2022)b | 11.1 | 15.3 | 19.6 | 8.5*** | 1 | 1.22 (1.07–1.39) | 1.63 (1.39–1.91) | |
| Time trendc | Down*** | Down*** | Down*** | pint = 0.0764d | ||||
| Drunkenness (15-year-olds) | 1991 | 43.4 | 46.3 | 38.1 | −5.3 | 1 | 1.11 (0.76–1.63) | 0.79 (0.47–1.63) |
| 1994 | 45.3 | 41.3 | 33.3 | −12.0* | 1 | 0,86 (0.67–1.10) | 0.61 (0.42–0.86) | |
| 1998 | 50.2 | 48.2 | 39.3 | −10.9* | 1 | 0.84 (0.74–1.18) | 0.65 (0.47–0.89) | |
| 2002 | 47.5 | 44.1 | 39.3 | −8.2 | 1 | 0.89 (0.69–1.14) | 0.73 (0.53–1.00) | |
| 2006 | 37.5 | 36.3 | 32.9 | −6.6 | 1 | 0.96 (0.74–1.25) | 0.83 (0.60–1.14) | |
| 2010 | 36.8 | 40.8 | 38.2 | 2.2 | 1 | 1.19 (0.92–1.53) | 1.06 (0.76–1.49) | |
| 2014 | 23.1 | 21.5 | 14.4 | −8.7* | 1 | 0.93 (0.70–1.23) | 0.58 (0.37–0.90) | |
| 2018 | 27.5 | 21.9 | 25.3 | −2.2 | 1 | 0.77 (0.54–1.08) | 0–91 (0.51–1.61) | |
| 2022 | 25.0 | 26.5 | 18.6 | −6.1 | 1 | 1.08 (0.84–1.40) | 0.68 (0.42–1.11) | |
| Years (1991–2022)b | 35.5 | 37.3 | 32.4 | −1.1** | 1 | 0.96 (0.88–1.05) | 0.75 (0.66–0.84) | |
| Time trendc | Down*** | Down*** | Down*** | pint = 0.5245d | ||||
| Physical inactivity | 1991 | 5.1 | 7.9 | 12.9 | 7.8*** | 1 | 1.59 (0.99–2.58) | 2.78 (1.65–4.68) |
| 1994 | 6.8 | 9.1 | 12.6 | 5.8*** | 1 | 1.36 (1.03–1.80) | 1.98 (1.44–2.73) | |
| 1998 | 6.5 | 10.0 | 11.9 | 5.4*** | 1 | 1.60 (1.23–2.06) | 2.06 (1.54–2.74) | |
| 2002 | 8.3 | 9.3 | 13.7 | 5.4*** | 1 | 1.14 (0.88–1.48) | 1.80 (1.34–2.41) | |
| 2006 | 2.7 | 4.5 | 6.6 | 3.9*** | 1 | 1.70 (1.16–2.48) | 2.61 (1.74–3.90) | |
| 2010 | 5.1 | 7.1 | 9.6 | 4.5*** | 1 | 1.44 (1.07–1.92) | 2.09 (1.50–2.89) | |
| 2014 | 4.4 | 6.7 | 11.3 | 6.9*** | 1 | 1.56 (1.14–2.13) | 2.82 (1.98–4.01) | |
| 2018 | 6.8 | 8.2 | 17.1 | 10.3*** | 1 | 1.23 (0.91–1.66) | 2.83 (1.97–4.07) | |
| 2022 | 6.2 | 8.6 | 13.8 | 7.6*** | 1 | 1.44 (1.13–1.93) | 2.51 (1.83–3.46) | |
| Years (1991–2022)b | 5.7 | 7.9 | 11.4 | 5.7*** | 1 | 1.43 (1.29–1.57) | 2.34 (2.00–2.50) | |
| Time trendc | Stable | Down* | Stable | pint = 0.4134d | ||||
| Low vegetable intake | 2002 | 13.1 | 24.8 | 31.3 | 18.2*** | 1 | 2.24 (1.83–2.75) | 3.12 (2.48–3.92) |
| 2006 | 10.6 | 18.9 | 26.4 | 15.8*** | 1 | 2.02 (1.65–2.49) | 3.09 (2.49–3.84) | |
| 2010 | 9.9 | 17.4 | 22.6 | 12.7*** | 1 | 1.94 (1.58–2.39) | 2.75 (2.17–3.48) | |
| 2014 | 7.5 | 14.5 | 18.9 | 11.4*** | 1 | 2.17 (1.72–2.74) | 3.03 (2.30–3.98) | |
| 2018 | 8.2 | 11.4 | 20.3 | 12.1*** | 1 | 1.45 (1.12–1.89) | 2.83 (2.05–3.92) | |
| 2022 | 8.4 | 12.6 | 21.9 | 13.5*** | 1 | 1.57 (1.28–1.92) | 3.05 (2.35–3.96) | |
| Years (2002–2022)b | 9.3 | 17.0 | 24.6 | 15.3*** | 1 | 1.90 (1.74–2.07) | 2.91 (2.63–3.22) | |
| Time trendc | Down*** | Down*** | Down*** | pint = 0.1540d | ||||
| Infrequent toothbrushing | 1991 | 18.9 | 20.2 | 26.6 | 7.7* | 1 | 1.08 (0.82–1.45) | 1.58 (1.13–2.22) |
| 1994 | 17.4 | 18.0 | 28.0 | 10.6*** | 1 | 1.08 (0.89–1.31) | 1.97 (1.57–2.49) | |
| 1998 | 13.3 | 16.6 | 19.5 | 6.2*** | 1 | 1.29 (1.07–1.57) | 1.59 (1.28–1.99) | |
| 2002 | 16.6 | 21.1 | 28.3 | 11.7*** | 1 | 1.38 (1.14–1.67) | 2.04 (1.64–2.55) | |
| 2006 | 16.6 | 21.3 | 29.1 | 12.5*** | 1 | 1.40 (1.18–1.66) | 2.13 (1.76–2.57) | |
| 2010 | 19.8 | 24.0 | 34.5 | 14.7*** | 1 | 1.29 (1.09–1.52) | 2.17 (1.79–2.64) | |
| 2014 | 16.8 | 22.8 | 31.4 | 14.6*** | 1 | 1.49 (1.25–1.78) | 2.32 (1.88–2.87) | |
| 2018 | 14.7 | 18.0 | 27.5 | 12.8*** | 1 | 1.27 (1.03–1.57) | 2.21 (1.68–2.92) | |
| 2022 | 17.6 | 22.5 | 31.5 | 13.9*** | 1 | 1.36 (1.17–1.58) | 2.06 (1.65–2.57) | |
| Years (1991–2022)b | 16.9 | 20.5 | 28.0 | 11.1*** | 1 | 1.32 (1.24–1.40) | 2.02 (1.87–2.17) | |
| Time trendc | Stable | Up*** | Up*** | pint = 0.3338d | ||||
Health behaviours by occupational social class; expressed as absolute and relative social inequality (Denmark, 1991–2022).
Prevalence in low OSC minus prevalence in high OSC.
Logistic regression analyses combining all survey years adjusted for sex, age group, and survey year.
Time trends assessed by Cochran-Armitage test. Statistical significance at the 95% level: *<0.05, **<0.001, **<0.0001.
pint is the p-value for statistical interaction between year and OSC.
Bold text indicating significant results.
Overall Development in Health
There was a significant deterioration in physical health measured by overweight, headache, stomachache, and backpain in all OSC groups and for underweight in the low OSC group (Table 3). There was also a significant deterioration in mental health measured by daily emotional symptoms, loneliness, difficulties falling asleep, and poor life satisfaction in all OSC groups (Table 4). There was improvement in smoking and drunkenness behaviour and vegetable intake in all OSC groups and mixed developments in physical inactivity and infrequent toothbrushing (Table 5).
Social Inequality
There was an absolute social inequality (prevalence difference) in 13 of 15 health indicators in most survey years (Tables 3–5). There were two exceptions: Underweight was not associated with OSC and drunkenness was more prevalent in high than low OSC. Assessed by OR estimates, there was a relative social inequality in 13 of 15 health indicators in most survey years, again with the same two exceptions: Underweight was not associated with OSC and drunkenness was more common in high than low OSC. Two examples of the social inequality in health were the OR (95% CI) for overweight in low socioeconomic groups which was 2.22 (1.95–2.49) and for low vegetable intake, 2.91 (2.63–3.22).
Trends in Social Inequality
The absolute social inequality (prevalence difference) fluctuated across the study period without any consistent increasing or decreasing patterns (Tables 3–5). There was one exception: the prevalence difference for overweight increased from 4.7 in 1998 to 8.3 in 2022. The relative social inequality assessed by OR-estimates also fluctuated across survey years without any consistent patterns. Tests for statistical interaction suggested that survey year modified the social inequality in daily emotional symptoms (pint = 0.0122), in difficulties falling asleep (pint = 0.0081), in loneliness (pint = 0.0401), and in poor self-rated health (pint = 0.0176). The broad confidence intervals in the analyses of relative social inequality did not allow any conclusion about increasing or diminishing social inequality. Further, eyeballing of the trendlines in Figure 1 suggest that there might be a slight reduction in social inequality for these four health indicators but that the significant pint-values could as well reflect more random variations in trendlines.
Discussion
Main Findings
This is the first study of secular trends in social inequality in adolescents’ health which covers a period of more than three decades and a broad selection of health indicators. There were two main findings. First, there was persistent social inequality – meaning more problems in lower OSC-groups - in 13 of 15 health indicators from 1991 to 2022. The social inequality appeared in absolute terms (prevalence differences) as well as in relative terms (odds ratios). Drunkenness among 15-year-olds was persistently more prevalent in high than low OSC and underweight was persistently not associated with OSC. The observation of trends in social inequality in adolescents’ health aligns with many other studies covering overweight [6–8], pain [10, 12], mental health problems [12, 15, 17] and unhealthy behaviours [6, 24, 27].
Second, the magnitude of social inequality in health fluctuated from one survey year to the next but did not change in any systematic way over the past three decades. Test for statistical interaction suggested a slight reduction in social inequality in four mental health indicators (daily emotional symptoms, difficulties falling asleep, loneliness, poor self-rated health). This finding did not consistently support any of the two competing hypotheses: The health policy goal to reduce social inequality in health was not achieved, and the increasing income inequality in the past three decades did not result in increasing social inequality in health. Several studies show widening social inequality in physical inactivity, overweight, and smoking [6, 31, 34, 35, 38, 41] as well as slightly widening social inequality in pain, psychological distress, loneliness, difficulties in falling asleep, and poor self-rated health [1, 12, 13, 22, 39, 74]. From a health policy point of view, it is disappointing that the desired reduction of social inequality was unsuccessful. The efforts may have been insufficient, or other developments in the society may have facilitated increasing social inequality. It is a challenge to explain the almost universal and persistent pattern of social inequality in adolescent health, but the Theory of Fundamental Causes [75] provides a potential explanatory framework: According to this theory, the reason for persistent social inequality is that high socioeconomic status embodies a multitude of resources (material assets, knowledge, control, resourceful social networks, etc.) which protect health, no matter what mechanisms are at stake.
Methodological Issues
The strength of the HBSC study is that it covers many indicators of adolescent health, covers an extended period, and that the survey rounds are methodologically comparable [50, 76]. The included health indicators are important aspects of adolescent health as they either challenge the life quality of the individuals and/or increase the risk of future disease. Several other important indicators such as hospitalization, healthcare use, chronic illness, and diagnosed mental health problems were not included in the study.
There are important limitations as well. First, there may be problems related to comparability of socioeconomic status over time. We used occupational social class, a generic indicator of socioeconomic status which reflects the family’s position in the occupational structure [77]. We have reasons to believe that the data – although with a high level of missing data - are valid because most students in these age groups can report their parents’ occupation with a reasonable validity [76, 78–81]. Pförtner et al. showed that OSC is an appropriate variable for studies of social inequality in adolescents’ health [82]. The occupational structure in the country changed substantially from the 1990s to 2022 and so did the OSC distribution in the population. The traditional working classes shrieked, and the upper middle classes increased in size. Therefore, widening social inequality may reflect changes in the composition of the population. We decided not to use the socioeconomic indicator, which is often used in analyses of HBSC data, the Family Affluence Scale (FAS) [83] because FAS was not available for the two first surveys in 1991 and 1994, and FAS has relatively low correlations with two generic measures of socioeconomic status, parental education and parents’ occupational status [84].
A second limitation may be selection bias. We excluded 5,720 students with incomplete information about parents’ OSC, 13.9% of the sample. We also excluded students with missing data on each health indicator. In most cases the proportion of missing data on health indicators was < 5% but in the analyses of overweight and underweight we missed 12.9% of the applied study population. We have no way to investigate the magnitude or direction of the potential selection bias.
Implications
We need more insight into how socioeconomic health differences change over time. We need to know more about other health indicators; whether changes in social inequality vary by country; and whether these social inequalities are sensitive to health policy interventions. We may need other inequality methodologies. Although regression-based measures such as Slope Index of Inequality and Relative Index of Inequality are sensitive to changes in the distribution of the socioeconomic groups over time, they could still result in misleading conclusions regarding changes in the social inequality [85]. When it comes to health policy monitoring, we might consider total impact inequality measures such as Population Attributable Fraction and Index of Dissimilarity more relevant for future studies.
From a policy point of view, there is a desire to fight social inequalities in adolescent health, because they limit the full health potential of adolescents from lower socioeconomic groups. The substantial efforts in England over the past decades to reduce social inequality in child and adolescent health were disappointing [4, 86]. Mackenbach concluded that “Health inequalities can be reduced substantially only if governments have a democratic mandate to make the necessary policy changes, if demonstrably effective policies can be developed and if these policies are implemented on the scale needed to reach the overall targets.” [4]. Other scholars suggest that less radical ways to tackle social inequality in child and adolescent health may be successful. Diderichsen et al. suggest a combination of structural changes such as reducing child poverty, reducing early school drop-out, and fighting harmful health behaviours [87]. Law et al. suggest that child health professionals can contribute by ensuring that health services are accessible and equitable. They also emphasize that staff training could foster an understanding of the causes and solutions to child health inequalities [86].
Conclusion
There was significant social inequality in 13 of 15 specific indicators of adolescent health and this pattern did not change much in the period 1991–2022. There is a need for better monitoring of social inequalities in adolescent health and for strengthened policies to improve adolescent health across socioeconomic groups.
Statements
Ethics statement
The HBSC study complies with national guidelines and regulation regarding consent, data protection, and ethics approval. The legislation and guidelines changed over time. Considering our surveys from 2010 and 2014, the Danish Data Protection Authority granted acceptance (Case No. 2013-54-0576). The surveys from 2018 and 2022 were registered within the institution University of Southern Denmark (Case 10.622, University of Southern Denmark). All data has been pseudonymised and the research group had no access to information that can identify participants. According to section 14 in the Danish Scientific Ethical Committees Act, there is no request for ethics approval of population-based questionnaire surveys and there was no agency to provide approval (https://www.retsinformation.dk/eli/lta/2017/1083). In all surveys, we received approval from the school principal, the school board representing the parents, and the board of schoolchildren representing the schoolchildren in every participating school. We informed the participants orally and in writing about the purpose of the study, that data collection was pseudonymised and voluntary, that publication of data would be in a de-identified format, and that data could be used for research with similar purposes by approval of University of Southern Denmark. In 2018 and 2022, we also provided written information to the parents about the study. The parents also received an electronic link to a short video with information about the study and that participation was voluntary and confidential as well as an electronic link by which they could reject their child’s participation in the study. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
BH, MD, KR, TP, JR, MR, and MT acquired the data. BH analysed the data and drafted the first version of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The Nordea foundation (grant number 02-2011-0122) provided economic support for the Danish National HBSC Trend Datafile.
Conflict of interest
The authors declare that they do not have any conflicts of interest.
References
1.
Inchley JC Willis M Mabelis J Brown J Currie DB . Inequalities in Health Complaints: 20-Year Trends Among Adolescents in Scotland, 1998–2018. Front Psychol (2023) 14:1095117. 10.3389/fpsyg.2023.1095117
2.
Viner RM Ozer EM Denny S Marmot M Resnick M Fatusi A et al Adolescence and the Social Determinants of Health. The Lancet (2012) 379:1641–52. 10.1016/S0140-6736(12)60149-4
3.
Patton GCMD Sawyer SMMD Santelli JSMD Ross DAP Afifi RP Allen NBP et al Our Future: A Lancet Commission on Adolescent Health and Wellbeing. The Lancet (2016) 387:2423–78. 10.1016/S0140-6736(16)00579-1
4.
Mackenbach JP . Can We Reduce Health Inequalities? An Analysis of the English Strategy (1997–2010). J Epidemiol Community Health (2011) 65:568–75. 10.1136/jech.2010.128280
5.
Bann D Johnson W Li L Kuh D Hardy R . Socioeconomic Inequalities in Childhood and Adolescent Body-Mass Index, Weight, and Height From 1953 to 2015: An Analysis of Four Longitudinal, Observational, British Birth Cohort Studies. Lancet Public Health (2018) 3:e194–e203. 10.1016/S2468-2667(18)30045-8
6.
Inchley J Currie D Jewell J Breda J Barnekow V . Adolescent Obesity and Related Behaviours: Trends and Inequalities in the WHO European Region, 2002–2014: Observations From the Health Behaviour in School-Aged Children (HBSC) WHO Collaborative Cross-National Study. Copenhagen: World Health Organization. Regional Office for Europe (2017).
7.
Rasmussen M Damsgaard MT Morgen CS Kierkegaard L Toftager M Rosenwein SV et al Trends in Social Inequality in Overweight and Obesity Among Adolescents in Denmark 1998-2018. Int J Public Health (2020) 65:607–16. 10.1007/s00038-020-01342-1
8.
Wang Y Lim H . The Global Childhood Obesity Epidemic and the Association Between Socio-Economic Status and Childhood Obesity. Int Rev Psychiatry (2012) 24:176–88. 10.3109/09540261.2012.688195
9.
Ge R Chang J Cao Y . Headache Disorders and Relevant Sex and Socioeconomic Patterns in Adolescents and Young Adults Across 204 Countries and Territories: An Updated Global Analysis. The J Headache Pain (2023) 24:110. 10.1186/s10194-023-01648-4
10.
Holstein BE Damsgaard MT Madsen KR Pedersen TP Toftager M . Chronic Backpain Among Adolescents in Denmark: Trends 1991–2018 and Association With Socioeconomic Status. Eur J Pediatr (2022) 181:691–9. 10.1007/s00431-021-04255-0
11.
Madsen KM Holstein BE Madsen KR . Recurrent Headache, Stomachache, and Backpain Among Adolescents: Association With Exposure to Bullying and Parents’ Socioeconomic Status. Scand J Pain (2023) 23:563–70. 10.1515/sjpain-2022-0144
12.
Moor I Richter M Ravens-Sieberer U Ottová-Jordan V Elgar FJ Pförtner T-K . Trends in Social Inequalities in Adolescent Health Complaints From 1994 to 2010 in Europe, North America and Israel: The HBSC Study. Eur J Public Health (2015) 25:57–60. 10.1093/eurpub/ckv028
13.
Corell M Friberg P Petzold M Löfstedt P . Socioeconomic Inequalities in Adolescent Mental Health in the Nordic Countries in the 2000s - A Study Using Cross-Sectional Data From the Health Behaviour in School-Aged Children Study. Arch Public Health (2024) 82:20. 10.1186/s13690-024-01240-5
14.
Gautam N Rahman MM Hashmi R Lim A Khanam R . Socioeconomic Inequalities in Child and Adolescent Mental Health in Australia: The Role of Parenting Style and Parents’ Relationships. Child Adolesc Psychiatry Ment Health (2024) 18:28. 10.1186/s13034-024-00719-x
15.
Myhr A Anthun KS Lillefjell M Sund ER . Trends in Socioeconomic Inequalities in Norwegian Adolescents’ Mental Health From 2014 to 2018: A Repeated Cross-Sectional Study. Front Psychol (2020) 11:1472. 10.3389/fpsyg.2020.01472
16.
Reiss F . Socioeconomic Inequalities and Mental Health Problems in Children and Adolescents: A Systematic Review. Social Sci Med (2013) 90:24–31. 10.1016/j.socscimed.2013.04.026
17.
Papadopoulos D Sosso FAE . Socioeconomic Status and Sleep Health: A Narrative Synthesis of 3 Decades of Empirical Research. J Clin Sleep Med (2023) 19:605–20. 10.5664/jcsm.10336
18.
Madsen KR Holstein BE Damsgaard MT Rayce SB Jespersen LN Due P . Trends in Social Inequality in Loneliness Among Adolescents 1991–2014. J Public Health (2018) 41:e133–e140. 10.1093/pubmed/fdy133
19.
Qualter P Hennessey A Yang K Chester KL Klemera E Brooks F . Prevalence and Social Inequality in Youth Loneliness in the UK. Int J Environ Res Public Health (2021) 18:10420. 10.3390/ijerph181910420
20.
Holstein BE Trab Damsgaard M Rich Madsen K Rasmussen M . Persistent Social Inequality in Low Life Satisfaction Among Adolescents in Denmark 2002–2018. Child Youth Serv Rev (2020) 116:105097. 10.1016/j.childyouth.2020.105097
21.
Holstein BE Jørgensen SE Due P Damsgaard MT Rasmussen M . Short Report: Persistent Social Inequality in Poor Self-Rated Health Among Adolescents in Denmark 1991–2014. Eur J Public Health (2018) 28:1114–6. 10.1093/eurpub/cky234
22.
Torsheim T Nygren JM Rasmussen M Arnarsson AM Bendtsen P Schnohr CW et al Social Inequalities in Self-Rated Health: A Comparative Cross-National Study Among 32,560 Nordic Adolescents. Scand J Public Health (2018) 46:150–6. 10.1177/1403494817734733
23.
Gautam N Dessie G Rahman MM Khanam R . Socioeconomic Status and Health Behavior in Children and Adolescents: A Systematic Literature Review. Front Public Health (2023) 11:1228632. 10.3389/fpubh.2023.1228632
24.
de Looze M ter Bogt T Hublet A Kuntsche E Richter M Zsiros E et al Trends in Educational Differences in Adolescent Daily Smoking Across Europe, 2002–10. Eur J Public Health (2013) 23:846–52. 10.1093/eurpub/ckt022
25.
Holstein BE Andersen A Damsgaard MT Due P Bast LS Rasmussen M . Trends in Socioeconomic Differences in Daily Smoking Among 15-Year-Old Danes 1991–2014. Scand J Public Health (2020) 48:667–73. 10.1177/1403494819848284
26.
Moor I Rathmann K Lenzi M Pförtner T-K Nagelhout GE de Looze M et al Socioeconomic Inequalities in Adolescent Smoking Across 35 Countries: A Multilevel Analysis of the Role of Family, School and Peers. Eur J Public Health (2015) 25:457–63. 10.1093/eurpub/cku244
27.
Rasmussen M Pedersen TP Johnsen NF Krølner RF Holstein BE . Persistent Social Inequality in Low Intake of Vegetables Among Adolescents, 2002–2014. Public Health Nutr (2018) 21:1649–53. 10.1017/S136898001800040X
28.
da Mata LL Azevedo A Pereira ML . Socioeconomic Inequalities in Oral Health-Related Behaviors in 18-Year-Old Adolescents: A Cross-Sectional Study. J Int Soc Prev Community Dentistry (2021) 11:703–11. 10.4103/jispcd.JISPCD_184_21
29.
Holstein BE Andersen A Damsgaard MT Madsen KR Pedersen TP . Underweight Among Adolescents in Denmark: Prevalence, Trends (1998–2018), and Association of Underweight With Socioeconomic Status. Fam Pract (2021) 39:413–9. 10.1093/fampra/cmab134
30.
Martínez-Vizcaíno V Solera-Martínez M Cavero-Redondo I García-Prieto JC Arias-Palencia N Notario-Pacheco B et al Association Between Parental Socioeconomic Status With Underweight and Obesity in Children From Two Spanish Birth Cohorts: A Changing Relationship. BMC Public Health (2015) 15:1276. 10.1186/s12889-015-2569-5
31.
White J Rehkopf D Mortensen LH . Trends in Socioeconomic Inequalities in Body Mass Index, Underweight and Obesity Among English Children, 2007–2008 to 2011–2012. PLOS ONE (2016) 11:e0147614. 10.1371/journal.pone.0147614
32.
Inchley J Currie D Young T Samdal O Torsheim T Augustson L et al Growing Up Unequal: Gender and Socioeconomic Differences in Young People’s Health and Well-Being. In: Health Behaviour in School-Aged Children (HBSC) Study: International Report From the 2013/2014 Survey. Copenhagen: World Health Organization (2016).
33.
Bendtsen P Andersen A Damsgaard MT Due P Rasmussen M Holstein BE . Brief Report: Trends in Social Inequality in Drunkenness Among Danish Adolescents, 1991–2014. J Stud Alcohol Drugs (2018) 79:561–6. 10.15288/jsad.2018.79.561
34.
Elgar FJ Pförtner T-K Moor I De Clercq B Stevens GWJM Currie C . Socioeconomic Inequalities in Adolescent Health 2002-2010: A Time-Series Analysis of 34 Countries Participating in the Health Behaviour in School-Aged Children Study. The Lancet (2015) 385:2088–95. 10.1016/S0140-6736(14)61460-4
35.
Lampert T Hoebel J Kuntz B Finger JD Hölling H Lange M et al Health Inequalities Among Children and Adolescents in Germany. Developments Over Time and Trends From the KiGGS Study. J Health Monit (2019) 4:15–37. 10.25646/5871
36.
Moor I Herke M Markert J Böhm M Reiß F Bilz L et al Trends in Health Inequalities in Childhood and Adolescence in Germany: Results of the HBSC Study 2009/10 - 2022. J Health Monit (2024) 9:79–98. 10.25646/11876
37.
Hammami N Azevedo Da Silva M Elgar FJ . Trends in Gender and Socioeconomic Inequalities in Adolescent Health Over 16 Years (2002-2018): Findings From the Canadian Health Behaviour in School-Aged Children Study. Health Promot Chronic Dis Prev Can (2022) 42:68–78. 10.24095/hpcdp.42.2.03
38.
Broadbent P Shen Y Pearce A Katikireddi SV . Trends in Inequalities in Childhood Overweight and Obesity Prevalence: A Repeat Cross-Sectional Analysis of the Health Survey for England. Arch Dis Child (2024) 109:233–9. 10.1136/archdischild-2023-325844
39.
Lipari D Bocci BM Rivieri C Frongillo E Miserendino A Pammolli A et al Trend of Correlations Between Psychological Symptoms and Socioeconomic Inequalities Among Italian Adolescents: Cross-Sectional Study From 2006 to 2018 in Tuscany Region. Int J Environ Res Public Health (2023) 20:6473. 10.3390/ijerph20156473
40.
Due P Damsgaard MT Madsen KR Nielsen L Rayce SB Holstein BE . Increasing Prevalence of Emotional Symptoms in Higher Socioeconomic Strata: Trend Study Among Danish Schoolchildren 1991–2014. Scand J Public Health (2019) 47:690–4. 10.1177/1403494817752520
41.
Kuipers MAG Nagelhout GE Willemsen MC Kunst AE . Widening Educational Inequalities in Adolescent Smoking Following National Tobacco Control Policies in the Netherlands in 2003: A Time–Series Analysis. Addiction (2014) 109:1750–9. 10.1111/add.12637
42.
Kuntz B Waldhauer J Moor I Rathmann K Richter M Orth B et al Zeitliche Entwicklung von Bildungsunterschieden im Rauchverhalten von Jugendlichen in Deutschland. Bundesgesundheitsblatt - Gesundheitsforschung - Gesundheitsschutz (2017) 61:7–19. 10.1007/s00103-017-2636-4
43.
Fismen A-S Smith ORF Torsheim T Rasmussen M Pedersen Pagh T Augustine L et al Trends in Food Habits and Their Relation to Socioeconomic Status Among Nordic Adolescents 2001/2002-2009/2010. PLOS ONE (2016) 11:e0148541. 10.1371/journal.pone.0148541
44.
Johnsen NF Toftager M Melkevik O Holstein BE Rasmussen M . Trends in Social Inequality in Physical Inactivity Among Danish Adolescents 1991–2014. SSM - Popul Health (2017) 3:534–8. 10.1016/j.ssmph.2017.04.003
45.
Nicolas C Rouche M Dierckens M Kelly C Fismen A-S Nardone P et al Sixteen-Year Trends in Fruit Consumption and Related Socioeconomic Inequalities Among Adolescents in Western European Countries. Eur J Nutr (2023) 62:3287–96. 10.1007/s00394-023-03199-5
46.
Zaborskis A Kavaliauskienė A Levi S Tesler R Dimitrova E . Adolescent Toothbrushing and its Association With Sociodemographic Factors—Time Trends From 1994 to 2018 in Twenty Countries. Healthcare (2023) 11:3148. 10.3390/healthcare11243148
47.
Jutz R . The Role of Income Inequality and Social Policies on Income-Related Health Inequalities in Europe. Int J Equity Health (2015) 14:117. 10.1186/s12939-015-0247-y
48.
Rathmann K Ottova V Hurrelmann K de Looze M Levin K Molcho M et al Macro-Level Determinants of Young People’s Subjective Health and Health Inequalities: A Multilevel Analysis in 27 Welfare States. Maturitas (2015) 80:414–20. 10.1016/j.maturitas.2015.01.008
49.
Statistics Denmark. Income Inequality. Copenhagen: Statistics Denmark. Available from: https://www.dst.dk/da/Statistik/emner/arbejde-og-indkomst/indkomst-og-loen/indkomstulighed (Accessed June 25, 2024).
50.
Inchley J Currie D Cosma A Samdal O . Health Behaviour in School-Aged Children (HBSC) Study Protocol: Background, Methodology and Mandatory Items for the 2017/18 Survey. 2018.
51.
Cole TJ Lobstein T . Extended International (IOTF) Body Mass Index Cut‐Offs for Thinness, Overweight and Obesity. Pediatr Obes (2012) 7:284–94. 10.1111/j.2047-6310.2012.00064.x
52.
Rasmussen M Holstein BE Melkevik O Damsgaard MT . Validity of Self-Reported Height and Weight Among Adolescents: The Importance of Reporting Capability. BMC Med Res Methodol (2013) 13:85. 10.1186/1471-2288-13-85
53.
Haugland S Wold B . Subjective Health Complaints in Adolescence—Reliability and Validity of Survey Methods. J Adolescence (2001) 24:611–24. 10.1006/jado.2000.0393
54.
Haugland S Wold B Stevenson J Aaroe LE Barbara W . Subjective Health Complaints in Adolescence: A Cross-National Comparison of Prevalence and Dimensionality. Eur J Public Health (2001) 11:4–10. 10.1093/eurpub/11.1.4
55.
Hetland J Torsheim T Aarø LE . Subjective Health Complaints in Adolescence: Dimensional Structure and Variation across Gender and Age. Scand J Public Health (2002) 30:223–30. 10.1080/140349402320290953
56.
Ravens-Sieberer U Erhart M Torsheim T Hetland J Freeman J Danielson M et al An International Scoring System for Self-Reported Health Complaints in Adolescents. Eur J Public Health (2008) 18:294–9. 10.1093/eurpub/ckn001
57.
Damsgaard MT Holstein BE Koushede V Madsen KR Meilstrup C Nelausen MK et al Close Relations to Parents and Emotional Symptoms Among Adolescents: Beyond Socio-Economic Impact? Int J Public Health (2014) 59:721–6. 10.1007/s00038-014-0600-8
58.
Madsen KR Tjørnhøj-Thomsen T Jervelund SS Qualter P Holstein BE . Lonely, But Not Alone: Qualitative Study Among Immigrant and Native-Born Adolescents. Int J Environ Res Public Health (2021) 18:11425. 10.3390/ijerph182111425
59.
Eccles AM Qualter P Madsen KR Holstein BE . Loneliness in the Lives of Danish Adolescents: Associations With Health and Sleep. Scand J Public Health (2020) 48:877–87. 10.1177/1403494819865429
60.
Mund M Maes M Drewke PM Gutzeit A Jaki I Qualter P . Would the Real Loneliness Please Stand Up? The Validity of Loneliness Scores and the Reliability of Single-Item Scores. Assessment (2023) 30:1226–48. 10.1177/10731911221077227
61.
Levin KA Currie C . Reliability and Validity of an Adapted Version of the Cantril Ladder for Use With Adolescent Samples. Social Indicators Res (2014) 119:1047–63. 10.1007/s11205-013-0507-4
62.
Mazur J Szkultecka-Dębek M Dzielska A Drozd M Małkowska-Szkutnik A . What Does the Cantril Ladder Measure in Adolescence?Arch Med Sci (2018) 14:182–9. 10.5114/aoms.2016.60718
63.
Allen CD McNeely CA Orme JG . Self-Rated Health Across Race, Ethnicity, and Immigration Status for US Adolescents and Young Adults. J Adolesc Health (2016) 58:47–56. 10.1016/j.jadohealth.2015.09.006
64.
Dolcini MM Adler NE Lee P Bauman KE . An Assessment of the Validity of Adolescent Self-Reported Smoking Using Three Biological Indicators. Nicotine Tob Res (2003) 5:473–83. 10.1080/1462220031000118586
65.
Battista K Patte KA Wade TJ Cole AG Elton-Marshall T Lucibello KM et al Do Sociodemographic Risk Profiles for Adolescents Engaging in Weekly E-Cigarette, Cigarette, and Dual Product Use Differ? BMC Public Health (2024) 24:1558. 10.1186/s12889-024-18813-2
66.
Lintonen T Ahlström S Metso L . The Reliability of Self-Reported Drinking in Adolescence. Alcohol Alcohol (2004) 39:362–8. 10.1093/alcalc/agh071
67.
Brener ND Billy JOG Grady WR . Assessment of Factors Affecting the Validity of Self-Reported Health-Risk Behavior Among Adolescents: Evidence From the Scientific Literature. J Adolesc Health (2003) 33:436–57. 10.1016/S1054-139X(03)00052-1
68.
Booth ML Okely AD Chey T Bauman A . The Reliability and Validity of the Physical Activity Questions in the WHO Health Behaviour in Schoolchildren (HBSC) Survey: A Population Study. Br J Sports Med (2001) 35:263–7. 10.1136/bjsm.35.4.263
69.
Rangul V Holmen TL Kurtze N Cuypers K Midthjell K . Reliability and Validity of Two Frequently Used Self-Administered Physical Activity Questionnaires in Adolescents. BMC Med Res Methodol (2008) 8:47. 10.1186/1471-2288-8-47
70.
Toftager M Brønd JC Roman JEI Kristensen PL Damsgaard MT Grøntved A et al Måling Af Fysisk Aktivitet Blandt Elever I 5.-9. Klasse - Overensstemmelse Mellem Selvrapporteret Og Accelerometermålt Fysisk Aktivitet I Skolebørnsundersøgelsen. København: Statens Institut for Folkesundhed (2024).
71.
Vereecken CA Maes L . A Belgian Study on the Reliability and Relative Validity of the Health Behaviour in School-Aged Children Food-Frequency Questionnaire. Public Health Nutr (2003) 6:581–8. 10.1079/PHN2003466
72.
Jamieson LM Thomson WM McGee R . An Assessment of the Validity and Reliability of Dental Self-Report Items Used in a National Child Nutrition Survey. Community Dentistry Oral Epidemiol (2004) 32:49–54. 10.1111/j.1600-0528.2004.00126.x
73.
Christensen U Krølner R Nilsson CJ Lyngbye PW Hougaard CØ Nygaard E et al Addressing Social Inequality in Aging by the Danish Occupational Social Class Measurement. J Aging Health (2014) 26:106–27. 10.1177/0898264314522894
74.
Hu Y van Lenthe FJ Borsboom GJ Looman CWN Bopp M Burström B et al Trends in Socioeconomic Inequalities in Self-Assessed Health in 17 European Countries Between 1990 and 2010. J Epidemiol Community Health (2016) 70:644–52. 10.1136/jech-2015-206780
75.
Phelan JC Link BG Tehranifar P . Social Conditions as Fundamental Causes of Health Inequalities: Theory, Evidence, and Policy Implications. J Health Social Behav (2010) 51:S28–S40. 10.1177/0022146510383498
76.
Lien N Friestad C Klepp KI . Adolescents’ Proxy Reports of Parents’ Socioeconomic Status: How Valid Are They. J Epidemiol Community Health (2001) 55:731–7. 10.1136/jech.55.10.731
77.
Galobardes B Shaw M Lawlor DA Lynch JW Davey Smith G . Indicators of Socioeconomic Position (Part 1). J Epidemiol Community Health (2006) 60:7–12. 10.1136/jech.2004.023531
78.
Ensminger ME Forrest CB Riley AW Kang M Green BF Starfield B et al The Validity of Measures of Socioeconomic Status of Adolescents. J Adolesc Res (2000) 15:392–419. 10.1177/0743558400153005
79.
Pu C Huang N Chou Y-J . Do Agreements Between Adolescent and Parent Reports on Family Socioeconomic Status Vary With Household Financial Stress?BMC Med Res Methodol (2011) 11:50. 10.1186/1471-2288-11-50
80.
Pueyo M-J Serra-Sutton V Alonso J Starfield B Rajmil L . Self-Reported Social Class in Adolescents: Validity and Relationship With Gradients in Self-Reported Health. BMC Health Serv Res (2007) 7:151. 10.1186/1472-6963-7-151
81.
West P Sweeting H Speed E . We Really Do Know What You Do: A Comparison of Reports From 11 Year Olds and Their Parents in Respect of Parental Economic Activity and Occupation. Sociology (2001) 35:539–59. 10.1017/S0038038501000268
82.
Pförtner T-K Günther S Levin KA Torsheim T Richter M . The Use of Parental Occupation in Adolescent Health Surveys. An Application of ISCO-Based Measures of Occupational Status. J Epidemiol Community Health (2015) 69:177–84. 10.1136/jech-2014-204529
83.
Currie C Molcho M Boyce W Holstein B Torsheim T Richter M . Researching Health Inequalities in Adolescents: The Development of the Health Behaviour in School-Aged Children (HBSC) Family Affluence Scale. Social Sci & Med (2008) 66:1429–36. 10.1016/j.socscimed.2007.11.024
84.
Corell M Chen Y Friberg P Petzold M Löfstedt P . Does the Family Affluence Scale Reflect Actual Parental Earned Income, Level of Education and Occupational Status? A Validation Study Using Register Data in Sweden. BMC Public Health (2021) 21:1995. 10.1186/s12889-021-11968-2
85.
Renard F Devleesschauwer B Speybroeck N Deboosere P . Monitoring Health Inequalities When the Socio-Economic Composition Changes: Are the Slope and Relative Indices of Inequality Appropriate? Results of a Simulation Study. BMC Public Health (2019) 19:662. 10.1186/s12889-019-6980-1
86.
Law C Parkin C Lewis H . Policies to Tackle Inequalities in Child Health: Why Haven’t They Worked (Better)?Arch Dis Child (2012) 97:301–3. 10.1136/archdischild-2011-300827
87.
Diderichsen F Andersen I Manual C Andersen A-MN Bach E Baadsgaard M et al Summary. Scand J Public Health (2012) 40:6–8. 10.1177/1403494812457733
Summary
Keywords
adolescence, HBSC, physical health, mental health, health behaviour, social inequality, socioeconomic inequality, trend study
Citation
Holstein BE, Damsgaard MT, Pedersen TP, Rasmussen M, Román JEI, Toftager M and Rich Madsen K (2024) Persistent Social Inequality in Adolescent Health Indicators 1991–2022: Trend Study From Denmark. Int J Public Health 69:1607698. doi: 10.3389/ijph.2024.1607698
Received
26 June 2024
Accepted
20 November 2024
Published
28 November 2024
Volume
69 - 2024
Edited by
Irene Moor, Institute of Medical Sociology, Germany
Reviewed by
Joanna Mazur, University of Zielona Góra, Poland
Sven Bremberg, Karolinska Institutet (KI), Sweden
Updates
Copyright
© 2024 Holstein, Damsgaard, Pedersen, Rasmussen, Román, Toftager and Rich Madsen.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bjørn E. Holstein, bho@sdu.dk; Katrine Rich Madsen, krma@sdu.dk
This Original Article is part of the IJPH Special Issue “Trends in Adolescent Health and Wellbeing - 40 Years of the HBSC Study”
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.