- 1Department of Public Health, Medical University of Warsaw, Warsaw, Poland
- 2Department of Urology, Mazovia Hospital Warsaw, Warsaw, Poland
- 3School of Public Health, Centre of Postgraduate Medical Education, Warsaw, Poland
Objective: This study aimed to assess the awareness of genitourinary cancers risk factors among adults in Poland and to identify factors associated with public awareness of risk factors for genitourinary cancers.
Methods: This cross-sectional survey was carried out between 1 and 4 March 2024 in a nationwide sample of 2,165 adults in Poland. Quota sampling was used. Data were collected using computer-assisted web interview (CAWI) method.
Results: Regardless of the type of cancer (kidney, bladder, or prostate cancer), a family history of cancer was the most recognized risk factor indicated by over half of respondents. Over one-third were aware that chemical exposure increases the risk for bladder cancer (39.4%) or prostate cancer (34.2%). Smoking was recognized as a risk factor for kidney cancer by 40.6% of respondents. Female gender, having higher education, being occupationally active and the presence of chronic diseases were the most important factors (p < 0.05) associated with a higher level of awareness of genitourinary cancers risk factors.
Conclusion: This study revealed gaps in public awareness of genitourinary cancers risk factors among adults in Poland, especially lifestyle-related and workplace-related risk factors.
Introduction
Genitourinary cancers include cancers of the urinary system, as well as the reproductive tract [1]. Kidney, bladder, and prostate cancers are the most common genitourinary cancers posing significant health burden [1–3]. Between 1990 and 2019, the global incidence of kidney cancer increased by 155%, bladder cancer by 123%, and prostate cancer by 169% [2]. Population aging will increase the burden of genitourinary cancers [4]. Regular screening is a key preventive measure for early detection of genitourinary cancer [5]. Symptoms differ by type of genitourinary cancer, but most of them include trouble urinating, haematuria, and pain (mostly located in the back, lumps, or abdomen) [6, 7]. However, prostate cancer is often asymptomatic making early detection difficult [7].
Public awareness of genitourinary cancer risk factors is necessary to assess individual health risks and implement regular screening. Smoking is the most important lifestyle-related risk factor for genitourinary cancer [8]. Obesity and some types of diet may also increase the risk of genitourinary cancer [9]. Smoking prevalence in Poland is estimated at 28.8% of the adult population [10] and the prevalence of overweight or obesity is 42.2% and 16.4% respectively [11], so lifestyle-related risk factors significantly contribute to the genitourinary cancer burden in Poland. Chemical exposures, especially environmental and occupational exposures are also well-documented risk factors for genitourinary cancers [12]. Patients with arterial hypertension are also at higher risk of some types of genitourinary cancers, like kidney cancer [13]. Scientific data confirmed the link between chronic use of analgesics, history of chemotherapy or radiation therapy as well as long-term dialysis treatment, and increased risk for genitourinary cancers [14–16]. Genetic predisposition (family history of genitourinary cancers), male gender, and older age also increase the risk for genitourinary cancers [17].
There is a high burden of genitourinary cancers in Poland [18, 19]. Prostate cancer is the most common cancer in men, accounting for 20.6% of all cancer cases in men [18]. Bladder cancer is the fourth most common cancer in men [18]. Kidney cancer accounts for 5% of cancer in men and 3% in women [19]. Moreover, in Poland, the prevalence of genitourinary cancer risk factors, such as smoking [10] and obesity [20] is high. Population aging observed in Poland may also contribute to the growing genitourinary cancer burden. In Poland, educational campaigns on genitourinary cancer are mostly limited to those focused on prostate cancer during the “Movember” annual event, supported by national public health institutions [21]. Moreover, education on different types of cancers (including kidney and bladder cancer) is carried out by non-governmental organizations (NGOs), including those run by patient representatives [22]. Physicians, including general practitioners, are encouraged to provide basic education on cancer risk factors as a part of preventive services, but the involvement of physicians in health education is limited [23]. Nationwide data on public awareness of genitourinary cancer risk factors may inform policymakers and healthcare professionals on current needs for the prevention and control of genitourinary cancers [22, 23].
This study aimed to assess the awareness of genitourinary cancers risk factors among adults in Poland as well as to identify factors associated with public awareness of risk factors for genitourinary cancers.
Methods
Study Design and Population
This population-based cross-sectional study was carried out in Poland, between 1 and 4 March 2024 on a nationwide sample of 2,165 adults in Poland. Data were collected using the computer-assisted web interview (CAWI) technique. A professional public opinion research agency (Nationwide Research Panel Ariadna in Warsaw) was contracted to collect data on behalf of the authors [24]. An online panel of more than 100,000 verified persons managed by the research agency was used to recruit participants to form a nationwide sample of the Polish adult population concerning demographic characteristics (gender, age, and place of residence). The population was first divided into subgroups based on mutual exclusivity. Then, respondents were chosen using a stratification model and quota sampling. Demographic data on the age, gender, and place of residence from the Population Yearbook of the Central Statistical Office of the Republic of Poland [25], were used in the stratification model. Every participant received a unique URL to the research website via e-mail that granted a single access to the survey. A text message reminder was also sent. Participation in the study was voluntary and informed consent was collected from all participants. If the selected respondent refused to participate in the survey, the next participant from the list was invited in line with the demographic criteria. The overall response rate was estimated at 22%.
The same methodology was used in previous population-based cross-sectional studies in Poland [26, 27].
This study was approved on 05 February 2024, by the Ethical Board at the Medical University of Warsaw, document signature AKBE/43/2024. All procedures followed the followed the Declaration of Helsinki.
Study Questionnaire
The study questionnaire was based on a review of the literature on public awareness of genitourinary cancers and their risk factors, including data published by the American Cancer Society [28, 29]. The study questionnaire included 8 questions (5 multiple-choice, 3 single-choice) on genitourinary cancer risk factors and prevention methods. Moreover, a set of questions on the health status of respondents, and sociodemographic characteristics was addressed. A pilot study was carried out, and 8 adults filled the questionnaire twice, 7 days apart. After the pilot study, one question and three answers in multiple-choice questions were revised to improve the clarity of the text.
Respondents were asked about risk factors for genitourinary cancers using the following multiple-choice questions: “What do you think are the risk factors for (1) kidney cancer; (2) bladder cancer; (3) prostate cancer?” With 6–8 answers. Each risk factor was required to answer yes or no. As the study aim was the assessment of risk factors for a group of diseases (genitourinary cancers), questions were focused directly on this group of cancers rather than general cancer knowledge. A similar type of question was used in the study by Luryi et al. in the study on public awareness of head and neck cancers and their risk factors [30]. The list of risk factors for genitourinary cancers included in the multi-choice questions was based on the most common genitourinary cancer risk factors listed by the American Cancer Society [28].
The presence of chronic diseases was self-reported and based on the following question “Do you have chronic diseases or long-term health problems lasting at least 6 months? (yes or no).”
Questions on sociodemographic characteristics addressed: gender, age, marital status, having higher education (yes/no), having children (yes/no), place of residence, and occupational activity (active—currently employed or self-employed; passive—unemployed, retired, or student).
Statistics
Statistical testing was completed using procedures available in SPSS v.29 (IBM, Armonk, NY, United States). The distribution of categorical variables was presented with frequencies and proportions. Cross-tabulations and chi-square tests were used for the comparison of categorical variables. Multivariable logistic regression analyses were used to identify factors associated with public awareness of genitourinary cancers risk factors. Five best-documented risk factors for genitourinary cancers—(1) smoking, (2) family history of genitourinary cancers, (3) male gender, (4) obesity; and (5) chemical exposures were considered separately as dependent variables in the model. For multivariable logistic regression, it was assumed that if the respondent indicated a given factor as a risk factor for any of the analyzed genitourinary cancers (kidney, bladder, or prostate cancer), the respondent was aware that the given factor increased the risk of genitourinary cancer. The strength of the association was measured by the odds ratio (OR) and 95% confidence intervals (CI). Statistical significance was based on the criterion p < 0.05.
Results
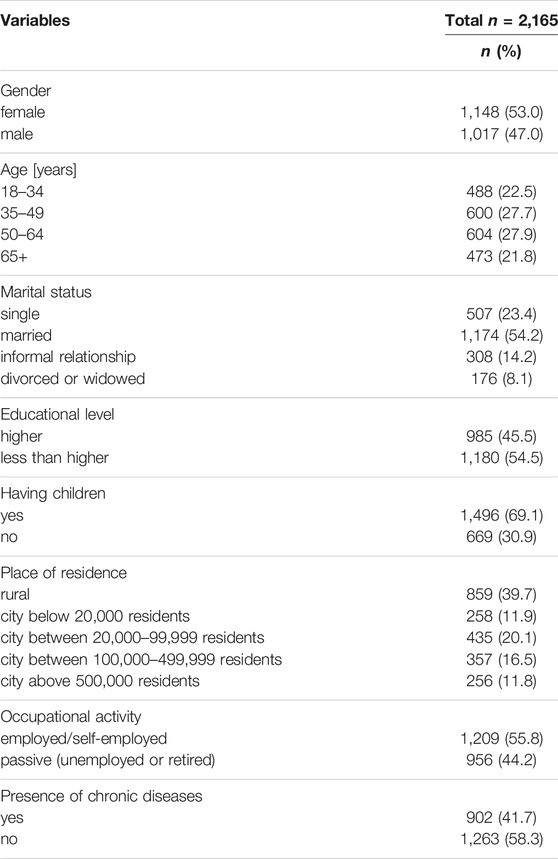
The mean age of respondents was 49.2 ± 16.2 years, 53% of respondents were females, and 41.7% had chronic diseases (Table 1).
Public Awareness of Genitourinary Cancers Risk Factors
Public awareness of genitourinary cancers risk factors is presented in Table 2. Regardless of the type of cancer (kidney, bladder, or prostate cancer), a family history of cancer was the most recognized risk factor indicated by over half of respondents. Over half of the respondents were aware that chemical exposure increases the risk for kidney cancer (50.1%). However, approximately one-third were aware that chemical exposure increases the risk for bladder cancer (39.4%) or prostate cancer (34.2%). Smoking was recognized as a risk factor for kidney cancer by 40.6% of respondents and only 35.3% of respondents indicated smoking as a risk factor for bladder cancer. Less than 30% of respondents were aware that chronic use of analgesics or long-term dialysis treatment increases the risk for kidney cancer (Table 2). Over half of the respondents (51.9%) were aware that chronic bladder irritation and infections increase the risk for bladder cancer. Older age was recognized as a risk factor for prostate cancer by 53.4% of respondents.
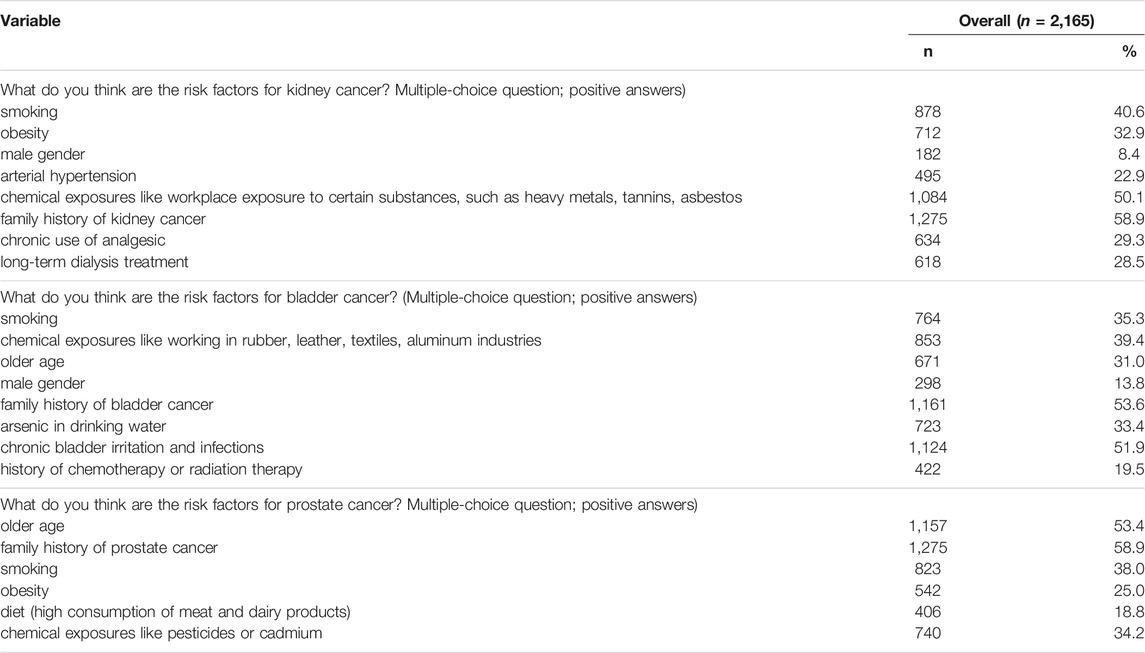
Table 2. Public awareness of genitourinary cancers risk factors, Poland, 2024 (n = 2,165) (Warsaw, Poland, 2024).
Sociodemographic Differences in Public Awareness of Genitourinary Cancers Risk Factors
There were sociodemographic differences in public awareness of risk factors for kidney cancer (Table 3), bladder cancer (Table 4), and prostate cancer (Table 5). In general, respondents with chronic diseases as well as those with higher education more often correctly indicated risk factors for genitourinary cancers (p < 0.05). Females more often correctly indicated risk factors for kidney cancer when compared to males (Table 3). There were gender differences in the percentage of patients who correctly indicated risk factors for bladder cancer (Table 4). Moreover, awareness of risk factors for prostate cancer differed by age (Table 5).
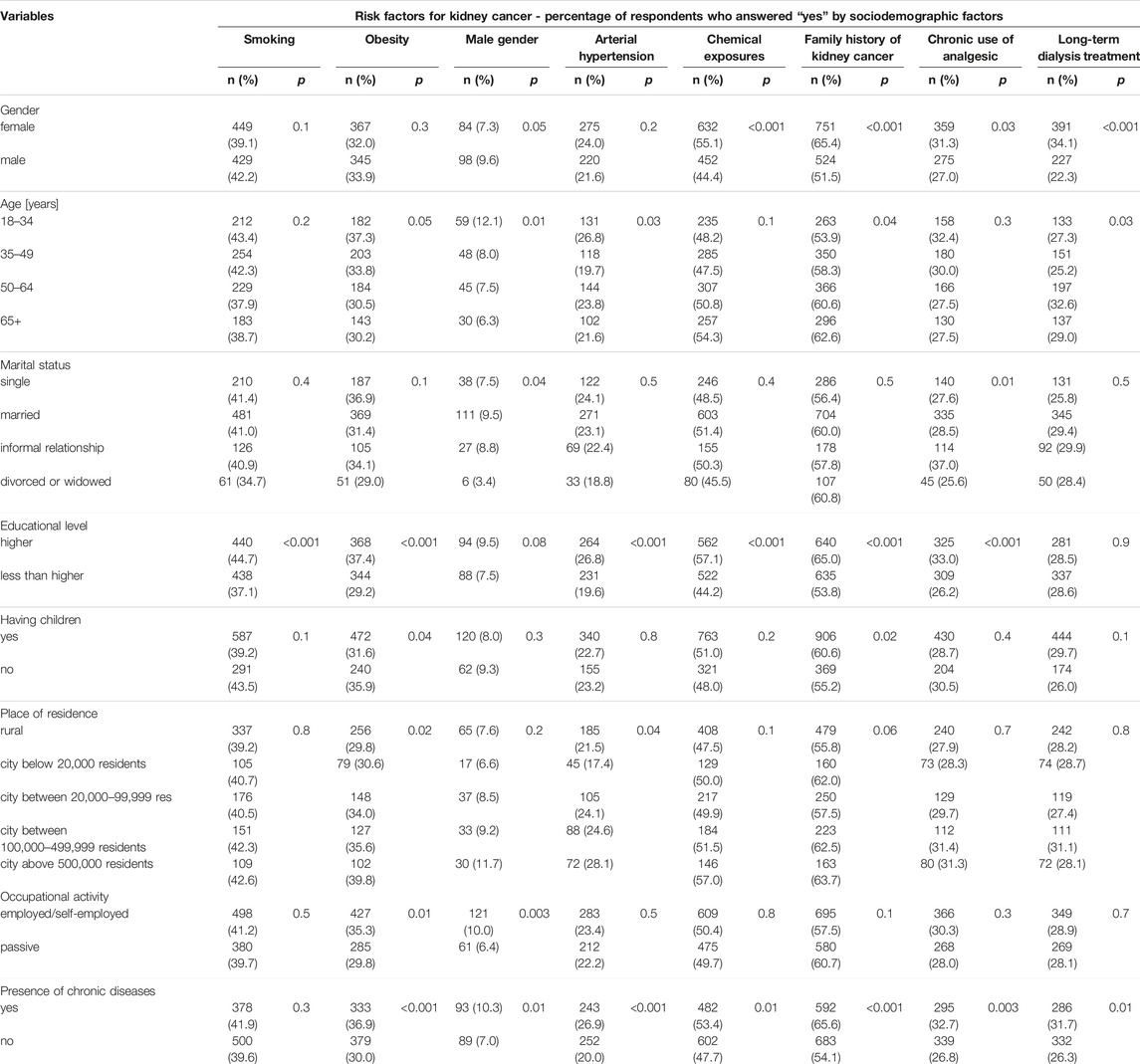
Table 3. Awareness of risk factors for kidney cancer by sociodemographic factors (n = 2,165) (Warsaw, Poland, 2024).
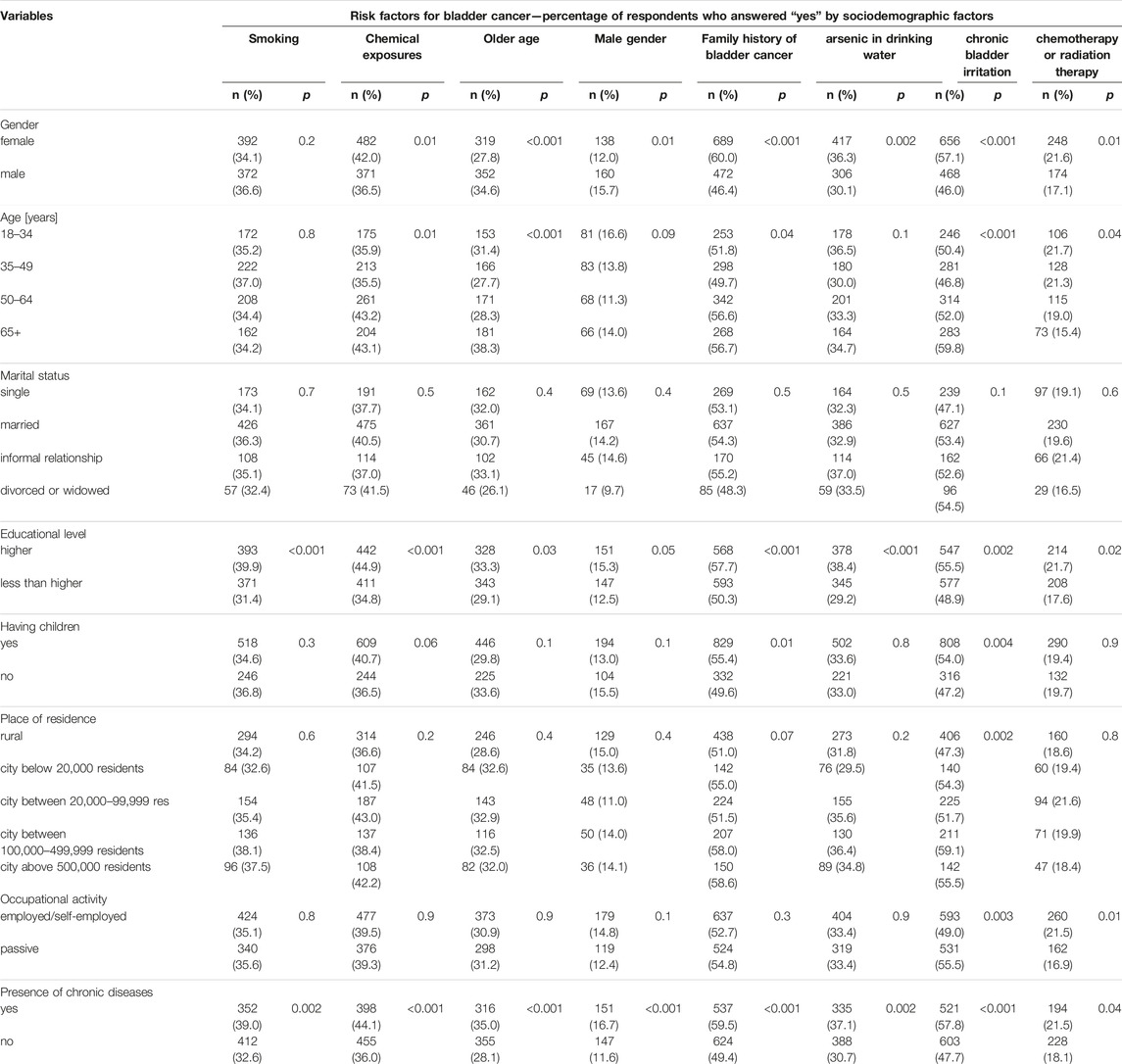
Table 4. Awareness of risk factors for bladder cancer by sociodemographic factors (n = 2,165) (Warsaw, Poland, 2024).
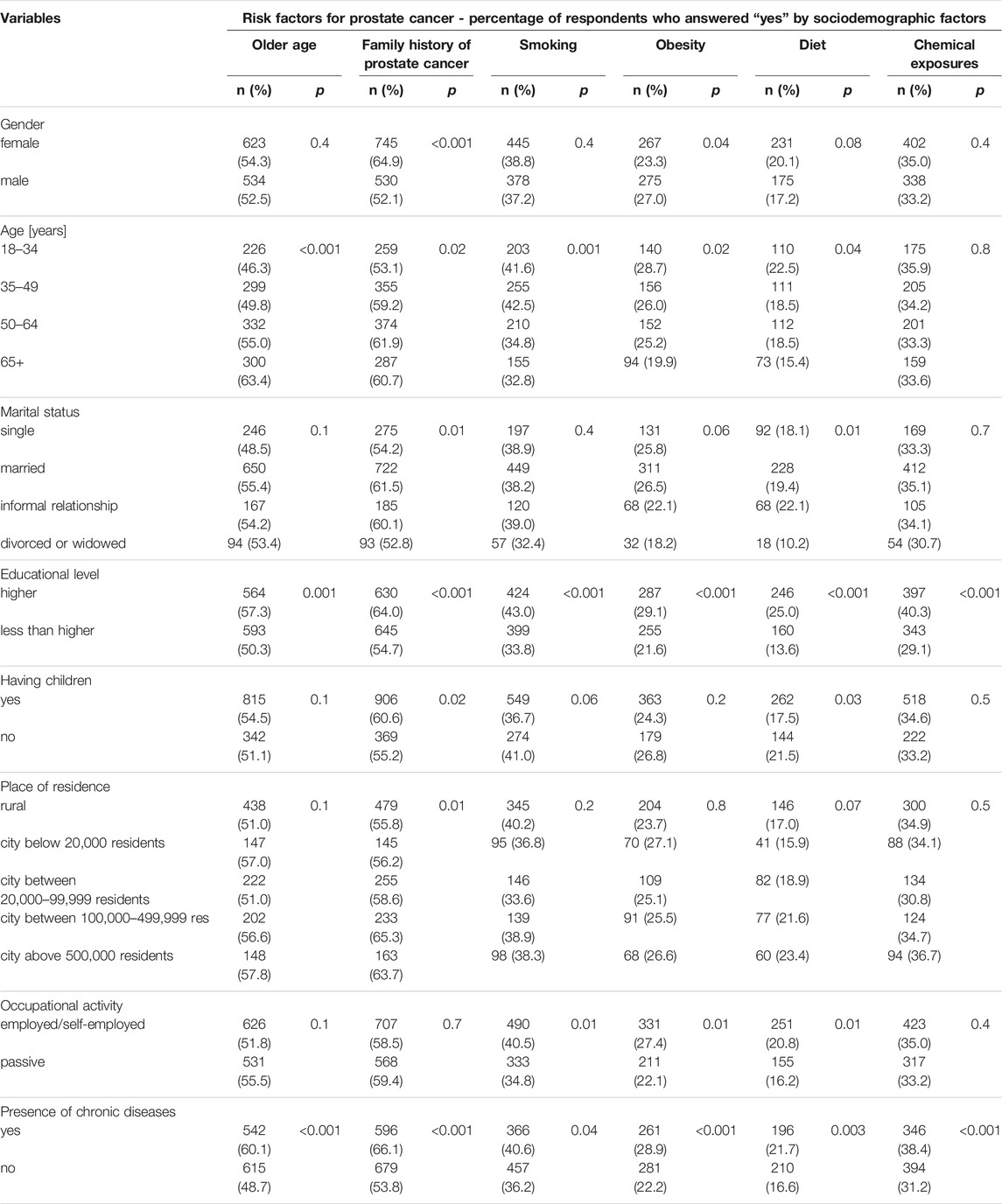
Table 5. Awareness of risk factors for prostate cancer by sociodemographic factors (n = 2,165) (Warsaw, Poland, 2024).
Factors Associated With Public Awareness of Genitourinary Cancers Risk Factors
In multivariable logistic regression, awareness of 5 different risk factors for genitourinary cancers was analyzed (Table 6). Age 18–49 (p < 0.05), having higher education (p < 0.001), having children (p < 0.001) as well as the presence of chronic diseases (p = 0.02) were associated with higher awareness of smoking as a risk factor for genitourinary cancers. Female gender (p < 0.001), marital status (p < 0.05), having higher education (p = 0.03), and the presence of chronic diseases (p < 0.001) were associated with higher awareness of family history of genitourinary cancers as a risk factor for genitourinary cancers. Male gender (p = 0.04), being employed or self-employed (p = 0.03), and the presence of chronic diseases (p < 0.001) were associated with higher awareness of male gender as a risk factor for genitourinary cancers. Age 18–34 years (p < 0.003), having higher education (p = 0.002), being employed or self-employed (p = 0.02), and the presence of chronic diseases (p < 0.001) were associated with higher awareness of obesity as a risk factor for genitourinary cancers. Female gender (p = 0.001), having higher education (p < 0.001), being employed or self-employed (p = 0.04), and the presence of chronic diseases (p = 0.01) were associated with higher awareness of chemical exposures as a risk factor for genitourinary cancers (Table 6).
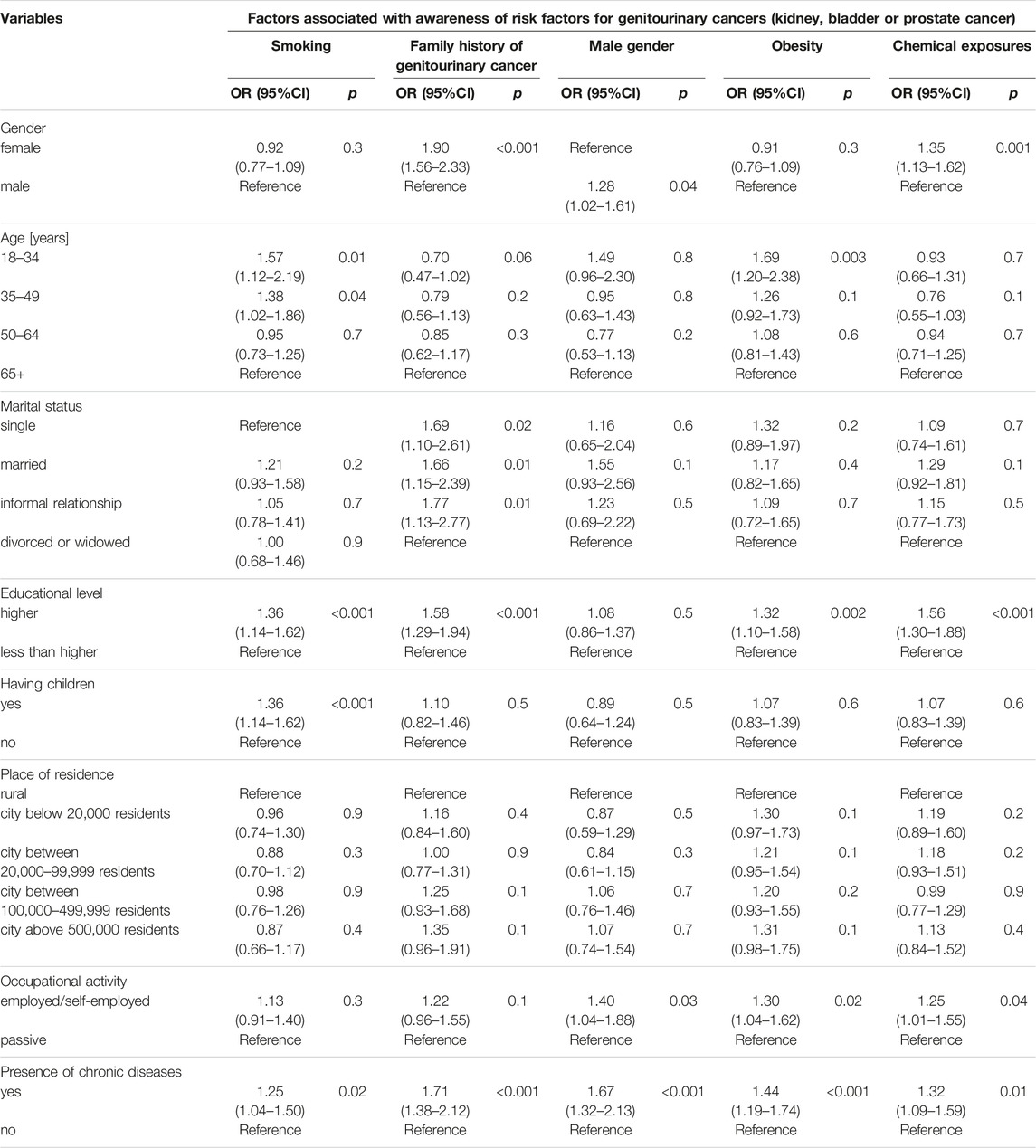
Table 6. Factors associated with awareness of genitourinary cancers risk factors (n = 2,165) (Warsaw, Poland, 2024).
Discussion
This population-based cross-sectional study provided data on public awareness of genitourinary (kidney, bladder, and prostate) cancers risk factors among adults in Poland. There was relatively low public awareness of genitourinary cancers risk factors, especially lifestyle-related and workplace-related risk factors. There were significant sociodemographic differences in awareness of particular risk factors for genitourinary cancer. Female gender, having higher education, being occupationally active and the presence of chronic diseases were the most important factors associated with a higher level of awareness of genitourinary cancers risk factors.
Awareness of genitourinary cancers risk factors may impact individuals’ behaviors related to cancer screening and prevention, including the prevalence of testing as well as lifestyle changes [8, 9]. It is estimated that one-quarter of adults in Poland are smokers [10]. Smoking increases the risk for most of the genitourinary cancers [8]. In this study, over 60% of adults in Poland were not aware of the link between smoking and kidney, bladder, or prostate cancer. This finding is in line with previously published data on insufficient counseling and knowledge of genitourinary cancers as tobacco-related diseases [31]. Urologists may play an important role in tobacco counseling, as patients who receive smoking cessation advice from their urologist are over 2 times more likely to attempt to quit [32].
Obesity is a significant risk factor for numerous cancers, including genitourinary cancers [9]. In this study majority (approximately 70%) of respondents were not aware of obesity as a risk factor for genitourinary cancers. Education on obesity-related cancers is difficult due to the reality of obesity stigma [33]. Nevertheless, there is a need to educate people on health consequences of obesity, especially in countries with high overweight and obesity prevalence, like Poland [23].
Chemical exposures, especially workplace-related exposures to heavy metals, tannins, and asbestos, working in agriculture where pesticides are used, or working in rubber, leather, textiles, or aluminum industries may increase risks of genitourinary cancers [12]. Workplace-related health risks are controlled within occupational medicine screening and surveillance [34]. However, public awareness of chemical exposures that increase cancer risks may motivate workers to comply with rules on security measures in the workplace or to change industries [12, 34]. Occupational medicine professionals may be involved in workers’ education on genitourinary cancers.
Family history of cancers is important data that influences the frequency of cancer screening [35]. Out of all genitourinary cancers risk factors analyzed in this study, a family history of cancer was the most recognized risk factor indicated by over half of respondents. Patients with a family history of genitourinary cancers should be educated on the importance of cancer screening [36].
Genitourinary cancers are more prevalent among men [2]. However, in this study, approximately 10% of respondents were aware of gender differences in the prevalence and risk of genitourinary cancers. Older age was correctly indicated as a risk factor for prostate cancer by over half of respondents, whereas only one-third of respondents indicated older age as a risk factor for bladder cancer. Education on genitourinary cancers risk factors should include activities targeted to older adults, especially older males, who are at higher risk for genitourinary diseases [17].
In this study, less than 30% of respondents were aware of genitourinary cancer risk factors related to healthcare procedures and treatment methods, including analgesics use, long-term dialysis treatment, and chemotherapy or radiation therapy [14–16]. Clinical guidelines should be regularly revised and updated to reduce the risk of genitourinary cancers related to healthcare procedures [14–16].
Sociodemographic differences in public awareness of different risk factors for genitourinary cancers indicated health inequalities in the knowledge of cancers in Poland. This finding suggests the need to prepare tailored activities, including those addressed to local communities [37]. Out of 8 different factors analyzed in this study, the presence of chronic diseases was associated with awareness of all 5 risk factors analyzed in multivariable logistic regression analyses. Health status and personal experience related to visits to healthcare facilities, as well as health education by physicians during these visits, may shape individuals’ knowledge of cancer [38]. Education is a well-reported factor associated with knowledge of health and health literacy levels [39]. In this study, having higher education was significantly associated with higher awareness of risk factors for genitourinary cancers. Occupationally active respondents were also more aware of genitourinary disease risk factors, which may result from the fact that they are covered by occupational medicine services and health education in the workplace [40]. Female gender was associated with higher awareness of gender and chemical exposures as risk factors for genitourinary cancers, whereas male gender was associated with higher awareness of gender differences in the risk of genitourinary diseases. There is a need for further education on genitourinary cancers targeted to males.
This study revealed gaps in public awareness of genitourinary cancers risk factors among adults in Poland. Educational campaigns on genitourinary cancers risk factors (especially those lifestyle-related) should be implemented. Public interventions on genitourinary cancers should be targeted to populations with the lowest awareness of genitourinary cancers, including those without higher education, males, and pensioners. Improvement of public knowledge on genitourinary cancers should be one of the targets of cancer policy in Poland. Findings from this study may pose a basis for international comparisons, especially between European countries.
The study questionnaire was limited to the most common risk factors for genitourinary diseases. There was no direct face-to-face interaction with the respondents, so there was no possibility to judge the respondents’ abilities and capacity to comprehend the questions posed. The cross-sectional design limiting some casual inferences and the nature of self-reported findings are also limitations of this study. Data on chronic conditions were self-reported and medical records were not verified. This study was carried out in a nationwide sample of adults in Poland and further studies in high-risk populations are needed.
Conclusion
Findings from this study revealed gaps in public awareness of genitourinary cancers risk factors among adults in Poland. Education on lifestyle-related and workplace-related risk factors for genitourinary cancers should be implemented. Gender, educational level, and health status (presence of chronic diseases) were the most important factors associated with public awareness of genitourinary cancers risk factors. National cancer strategies should pay more attention to education on genitourinary cancers risk factors.
Data Availability Statement
The dataset used to conduct the analyses is available from corresponding author upon reasonable request.
Ethics Statement
The studies involving humans were approved on 05 February 2024, by the Ethical Board at the Medical University of Warsaw, document signature AKBE/43/2024. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author Contributions
All authors GM, MJ, AD-Z, and MG have contributed to this work, have seen the contents of the manuscript, and agreed to its submission. GM was the leading author of this manuscript with the highest contribution. All authors contributed to the article and approved the submitted version.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of Interest
The authors declare that they do not have any conflicts of interest.
References
1. Guo, CC, Shen, SS, and Ro, JY. Pathogenesis and Diagnosis of Genitourinary Cancer. Cancers (Basel) (2021) 13(2):347. doi:10.3390/cancers13020347
2. Zi, H, He, SH, Leng, XY, Xu, XF, Huang, Q, Weng, H, et al. Global, Regional, and National burden of Kidney, Bladder, and Prostate Cancers and Their Attributable Risk Factors, 1990-2019. Mil Med Res (2021) 8(1):60. doi:10.1186/s40779-021-00354-z
3. Tian, YQ, Yang, JC, Hu, JJ, Ding, R, Ye, DW, and Shang, JW. Trends and Risk Factors of Global Incidence, Mortality, and Disability of Genitourinary Cancers from 1990 to 2019: Systematic Analysis for the Global Burden of Disease Study 2019. Front Public Health (2023) 11:1119374. doi:10.3389/fpubh.2023.1119374
4. Berben, L, Floris, G, Wildiers, H, and Hatse, S. Cancer and Aging: Two Tightly Interconnected Biological Processes. Cancers (Basel) (2021) 13(6):1400. doi:10.3390/cancers13061400
5. Thompson, IM, and Basler, J. Screening and Early Detection for Genitourinary Cancer. In: JM Potts, editor. Essential Urology. Current Clinical Urology. Totowa, NJ: Humana Press (2004). doi:10.1007/978-1-59259-737-6_4
6. Hippisley-Cox, J, and Coupland, C. Predicting the Risk of Prostate Cancer in Asymptomatic Men: A Cohort Study to Develop and Validate a Novel Algorithm. Br J Gen Pract (2021) 71(706):e364–e371. doi:10.3399/bjgp20X714137
7. Qin, Q, Sheffield, H, Taasan, SM, Wang, AZ, and Zhang, T. Genitourinary Cancers Updates: Highlights from ASCO 2023. J Hematol Oncol (2023) 16(1):112. doi:10.1186/s13045-023-01511-8
8. Gottlieb, J, Higley, C, Sosnowski, R, and Bjurlin, MA. Smoking-related Genitourinary Cancers: A Global Call to Action in Smoking Cessation. Rev Urol (2016) 18(4):194–204. doi:10.3909/riu0729
9. Santoni, M, Cimadamore, A, Massari, F, Piva, F, Aurilio, G, Martignetti, A, et al. Key Role of Obesity in Genitourinary Tumors with Emphasis on Urothelial and Prostate Cancers. Cancers (Basel) (2019) 11(9):1225. doi:10.3390/cancers11091225
10. Jankowski, M, Ostrowska, A, Sierpiński, R, Skowron, A, Sytnik-Czetwertyński, J, Giermaziak, W, et al. The Prevalence of Tobacco, Heated Tobacco, and E-Cigarette Use in Poland: A 2022 Web-Based Cross-Sectional Survey. Int J Environ Res Public Health (2022) 19(8):4904. doi:10.3390/ijerph19084904
11. Stoś, K, Rychlik, E, Woźniak, A, Ołtarzewski, M, Jankowski, M, Gujski, M, et al. Prevalence and Sociodemographic Factors Associated with Overweight and Obesity Among Adults in Poland: A 2019/2020 Nationwide Cross-Sectional Survey. Int J Environ Res Public Health (2022) 19(3):1502. doi:10.3390/ijerph19031502
12. Cani, M, Turco, F, Butticè, S, Vogl, UM, Buttigliero, C, Novello, S, et al. How Does Environmental and Occupational Exposure Contribute to Carcinogenesis in Genitourinary and Lung Cancers? Cancers (Basel) (2023) 15(10):2836. doi:10.3390/cancers15102836
13. Kim, CS, Han, KD, Choi, HS, Bae, EH, Ma, SK, and Kim, SW. Association of Hypertension and Blood Pressure with Kidney Cancer Risk: A Nationwide Population-Based Cohort Study. Hypertension (2020) 75(6):1439–46. doi:10.1161/HYPERTENSIONAHA.120.14820
14. Bruinsma, FJ, Jordan, S, Bassett, JK, Severi, G, MacInnis, RJ, Walsh, J, et al. Analgesic Use and the Risk of Renal Cell Carcinoma - Findings from the Consortium for the Investigation of Renal Malignancies (CONFIRM) Study. Cancer Epidemiol (2021) 75:102036. doi:10.1016/j.canep.2021.102036
15. Kamran, SC, and Efstathiou, JA. Current State of Personalized Genitourinary Cancer Radiotherapy in the Era of Precision Medicine. Front Oncol (2021) 11:675311. doi:10.3389/fonc.2021.675311
16. Lin, MY, Kuo, MC, Hung, CC, Wu, WJ, Chen, LT, Yu, ML, et al. Association of Dialysis with the Risks of Cancers. PLoS One (2015) 10(4):e0122856. doi:10.1371/journal.pone.0122856
17. Tang, CH, Chen, YC, Hsieh, WT, and Sue, YM. Gender and Age Differences of Genitourinary Cancers Among Chronic Dialysis Patients in Taiwan. Clin Genitourin Cancer (2022) 20(2):e126–e134. doi:10.1016/j.clgc.2021.11.013
18. Didkowska, J, Wojciechowska, U, Michalek, IM, and Caetano Dos Santos, FL. Cancer Incidence and Mortality in Poland in 2019. Sci Rep (2022) 12(1):10875. doi:10.1038/s41598-022-14779-6
19. Wysocki, PJ, Chłosta, P, Chrzan, R, Czech, A, Gronostaj, K, Konopka, K, et al. Polish Society of Clinical Oncology and Polish Urological Association Guidelines for the Diagnosis and Treatment of Renal Cell Cancer. Oncol Clin Pract (2020) 16(6):301–30. doi:10.5603/OCP.2020.0029
20. Krzysztoszek, J, Wierzejska, E, and Zielińska, A. Obesity. An Analysis of Epidemiological and Prognostic Research. Arch Med Sci (2015) 11(1):24–33. doi:10.5114/aoms.2013.37343
21. Ryszawy, J, Kowalik, M, Wojnarowicz, J, Rempega, G, Kępiński, M, Burzyński, B, et al. Awareness of Testicular Cancer Among Adult Polish Men and Their Tendency for Prophylactic Self-Examination: Conclusions from Movember 2020 Event. BMC Urol (2022) 22(1):149. doi:10.1186/s12894-022-01098-1
22. Wawryka, J, Ziobro, P, and Tyszko, M. Cancer Education in Poland: Current Status and Suggestions for Improvement. J Cancer Educ (2017) 32(3):669–75. doi:10.1007/s13187-016-1033-2
23. Mańczuk, M, Przepiórka, I, Cedzyńska, M, Przewoźniak, K, Gliwska, E, Ciuba, A, et al. Actual and Potential Role of Primary Care Physicians in Cancer Prevention. Cancers (Basel) (2023) 15(2):427. doi:10.3390/cancers15020427
24. The Nationwide Research Panel Ariadna. About the Panel (2024). Available from: https://panelariadna.com/(accessed on March 08, 2024).
25. Statistics of Poland. Demographic Yearbook of Poland 2023 (2023). Available from: https://stat.gov.pl/en/topics/statistical-yearbooks/statistical-yearbooks/demographic-yearbook-of-poland-2023,3,17.html (accessed on March 08, 2024).
26. Kamińska, A, Pinkas, J, and Jankowski, M. Factors Associated with the Frequency of Eye Examinations Among Adults in Poland – A Nationwide Cross-Sectional Survey, December 2022. Ann Agric Environ Med (2023) 30(2):287–95. doi:10.26444/aaem/159152
27. Grudziąż-Sękowska, J, Sękowski, K, Pinkas, J, and Jankowski, M. Public Expectations and Needs Related to Type 2 Diabetes Prevention: A Population-Based Cross-Sectional Study in Poland. Int J Public Health (2024) 69:1606790. doi:10.3389/ijph.2024.1606790
28. American Cancer Society. Risk Factors for Kidney Cancer (2024). Available from: https://www.cancer.org/cancer/types/kidney-cancer/causes-risks-prevention/risk-factors.html (accessed on March 08, 2024).
29. Fitzpatrick, JM, Kirby, RS, Brough, CL, and Saggerson, AL. Awareness of Prostate Cancer Among Patients and the General Public: Results of an International Survey. Prostate Cancer Prostatic Dis (2009) 12(4):347–54. doi:10.1038/pcan.2009.30
30. Luryi, AL, Yarbrough, WG, Niccolai, LM, Roser, S, Reed, SG, Nathan, CA, et al. Public Awareness of Head and Neck Cancers: A Cross-Sectional Survey. JAMA Otolaryngol Head Neck Surg (2014) 140(7):639–46. doi:10.1001/jamaoto.2014.867
31. Mori, K, Mostafaei, H, Abufaraj, M, Yang, L, Egawa, S, and Shariat, SF. Smoking and Bladder Cancer: Review of the Recent Literature. Curr Opin Urol (2020) 30(5):720–5. doi:10.1097/MOU.0000000000000804
32. Sosnowski, R, Bjurlin, MA, Verze, P, De Nunzio, C, Shariat, SF, Brausi, M, et al. Role of Cigarette Smoking in Urological Malignancies and Clinical Interventions for Smoking Cessation. Cent Eur J Urol (2016) 69(4):366–9. doi:10.5173/ceju.2016.883
33. Mojtahedi, Z, and Farjadian, S. Awareness of Obesity-Related Cancers: A Complex Issue. Int J Environ Res Public Health (2022) 19(11):6617. doi:10.3390/ijerph19116617
34. Cherrie, JW. Reducing Occupational Exposure to Chemical Carcinogens. Occup Med (Lond) (2009) 59(2):96–100. doi:10.1093/occmed/kqn172
35. Krakow, M, Rising, CJ, Trivedi, N, Yoon, DC, and Vanderpool, RC. Prevalence and Correlates of Family Cancer History Knowledge and Communication Among US Adults. Prev Chronic Dis (2020) 17:E146. doi:10.5888/pcd17.200257
36. Koutros, S, Decker, KL, Baris, D, Pardo, LA, Johnson, A, Hosain, GMM, et al. Bladder Cancer Risk Associated with Family History of Cancer. Int J Cancer (2021) 148(12):2915–23. doi:10.1002/ijc.33486
37. Kale, S, Hirani, S, Vardhan, S, Mishra, A, Ghode, DB, Prasad, R, et al. Addressing Cancer Disparities through Community Engagement: Lessons and Best Practices. Cureus (2023) 15(8):e43445. doi:10.7759/cureus.43445
38. Liu, C, Wang, D, Liu, C, Jiang, J, Wang, X, Chen, H, et al. What Is the Meaning of Health Literacy? A Systematic Review and Qualitative Synthesis. Fam Med Community Health (2020) 8(2):e000351. doi:10.1136/fmch-2020-000351
39. van der Heide, I, Wang, J, Droomers, M, Spreeuwenberg, P, Rademakers, J, and Uiters, E. The Relationship between Health, Education, and Health Literacy: Results from the Dutch Adult Literacy and Life Skills Survey. J Health Commun (2013) 18(Suppl. 1):172–84. doi:10.1080/10810730.2013.825668
Keywords: genitourinary diseases, cancer, preventive health services, public awareness, risk factors
Citation: Moczeniat G, Jankowski M, Duda-Zalewska A and Gujski M (2024) Awareness of Genitourinary Cancers Risk Factors—A 2024 Population-Based Cross-Sectional Study in Poland. Int J Public Health 69:1607264. doi: 10.3389/ijph.2024.1607264
Received: 10 March 2024; Accepted: 10 June 2024;
Published: 21 June 2024.
Edited by:
Paolo Chiodini, University of Campania Luigi Vanvitelli, ItalyReviewed by:
Sina Azadnajafabad, University of Leeds, United KingdomOne reviewer who chose to remain anonymous
Copyright © 2024 Moczeniat, Jankowski, Duda-Zalewska and Gujski. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gabriela Moczeniat, bmF1a2FAZ3J1cGFtYXpvdmlhLnBs
 Gabriela Moczeniat1,2*
Gabriela Moczeniat1,2* Mateusz Jankowski
Mateusz Jankowski