Abstract
Objectives: We tested an adapted version of an effective U.S.-based peer-texting intervention to promote Quitline use and smoking cessation among rural participants in Vietnam.
Methods: We conducted a two-arm randomized trial with participants recruited at four rural community centers. The intervention included peer messages sent for six months that promoted Quitline use and smoking cessation. Additionally, biweekly two-way text messages assessed participants’ interest in Quitline referral and current smoking status. Comparison participants received only the bi-weekly text message assessment of their current smoking status. At six months, we assessed Quitline use and smoking cessation. Smoking cessation was assessed using the 7-day point prevalence question and verified with a carbon monoxide breath monitor (<=6 ppm).
Results: Among 750 participants, the intervention had higher Quitline verified use (18%, 95% CI 0.14, 0.22) than comparison (1%, 95% CI .2, 2, p < 0.0001). Carbon-monoxide-verified smoking cessation did not differ between the two groups. However, intervention (28.3%, 95% CI) and comparison (28.1%, 95% CI) participants had substantial rates of carbon monoxide cessation at 6 months (both 28%).
Conclusion: Our study highlighted the promise of texting interventions to extend tobacco control efforts in Vietnam.
Introduction
Tobacco use is associated with over 8 million yearly deaths [1, 2]. Mostly, these deaths occur in low- and middle-incomes countries (LMICs), where approximately 80% of people who smoke live [2]. Despite the World Health Organization (WHO) Framework Convention on Tobacco Control (FCTC) mandate for the treatment of tobacco use and dependence in LMICs, there is limited evidence for effective tobacco interventions, including texting interventions, in LMICs [3]. Texting interventions are valuable due to the widespread use of texting in LMICs. While systematic reviews in high-income countries have noted texting intervention effectiveness compared with no intervention or attention control [4, 5], the evidence for LIMCs is of low quality [3].
Vietnam is an LMIC with high smoking rates in men (44%) and lower in women (1%) [6]. It is estimated that over 85% of these men smoke daily [7]. Smoking-related diseases place a considerable economic burden on Vietnam (an estimated 0.97 of the total GDP in 2011) [8, 9]. Smoking cessation is emphasized in the Joint Annual Health Review (2014) published by the Vietnam Ministry of Health [10]. The country is a party to the World Health Organization (WHO) Framework Convention for Tobacco Control. Tobacco taxes were used to create a Tobacco Control fund and with these funds the Vietnam Ministry of Health has established two Quitlines (modeled after U.S. Quitlines) to support tobacco control. These Quitlines are staffed by certified tobacco treatment specialists (e.g., registered nurses and public health professionals) who have been trained in principles of motivational interviewing, tobacco risks, and evidence-based tobacco cessation strategies summarized in the 2008 U.S. Treating Tobacco Use and Dependence guidelines including the 5As (Ask, Advise, Assess, Assist, and Arrange) and the 5Rs (Relevance, Risks, Rewards, Roadblocks, and Repetition) [11]. Unfortunately, these Quitlines are underused, with one estimate suggesting they conduct as few as 25 daily calls. The Vietnam Ministry of Health is interested in methods to promote the use of these Quitlines in Vietnam. As texting is almost ubiquitous in Vietnam [12], it may be a viable option to promote Quitline use and smoking cessation. However, texting has not been tested in Vietnam for promoting Quitline use and smoking cessation.
Thus, we tested the M2Q2 texting intervention, an adaptation of an effective U.S.-based texting intervention for people in Vietnam who smoke [13–17]. The intervention used peer text messages that are pre-written advice messages written by other people in Vietnam who smoke [11]. Messages “in a smoker’s own words” enhance homophily, a feeling of similarity between the message writer and the message reader [15]. Peer messages, a form of vicarious learning, can influence self-efficacy [18]. The messages were motivational and promoted the use of the Bach Mai Quitline (one of the two Quitlines in Vietnam) and nicotine replacement therapy (NRT), which could be requested through the Quitline [11].
This paper presents the results of our randomized controlled trial that tested the M2Q2 intervention among rural Vietnamese people who smoke. We hypothesized that intervention would increase i) Quitline and NRT use, ii) smoking cessation self-efficacy, and iii) smoking cessation rates.
Methods
Study Design
We conducted a two-arm randomized controlled trial among participants in Hung Yen, a rural province northern Vietnam, between November 2018 and April 2021 (Figure 1). Participants were randomized and followed for 6 months [11].
FIGURE 1
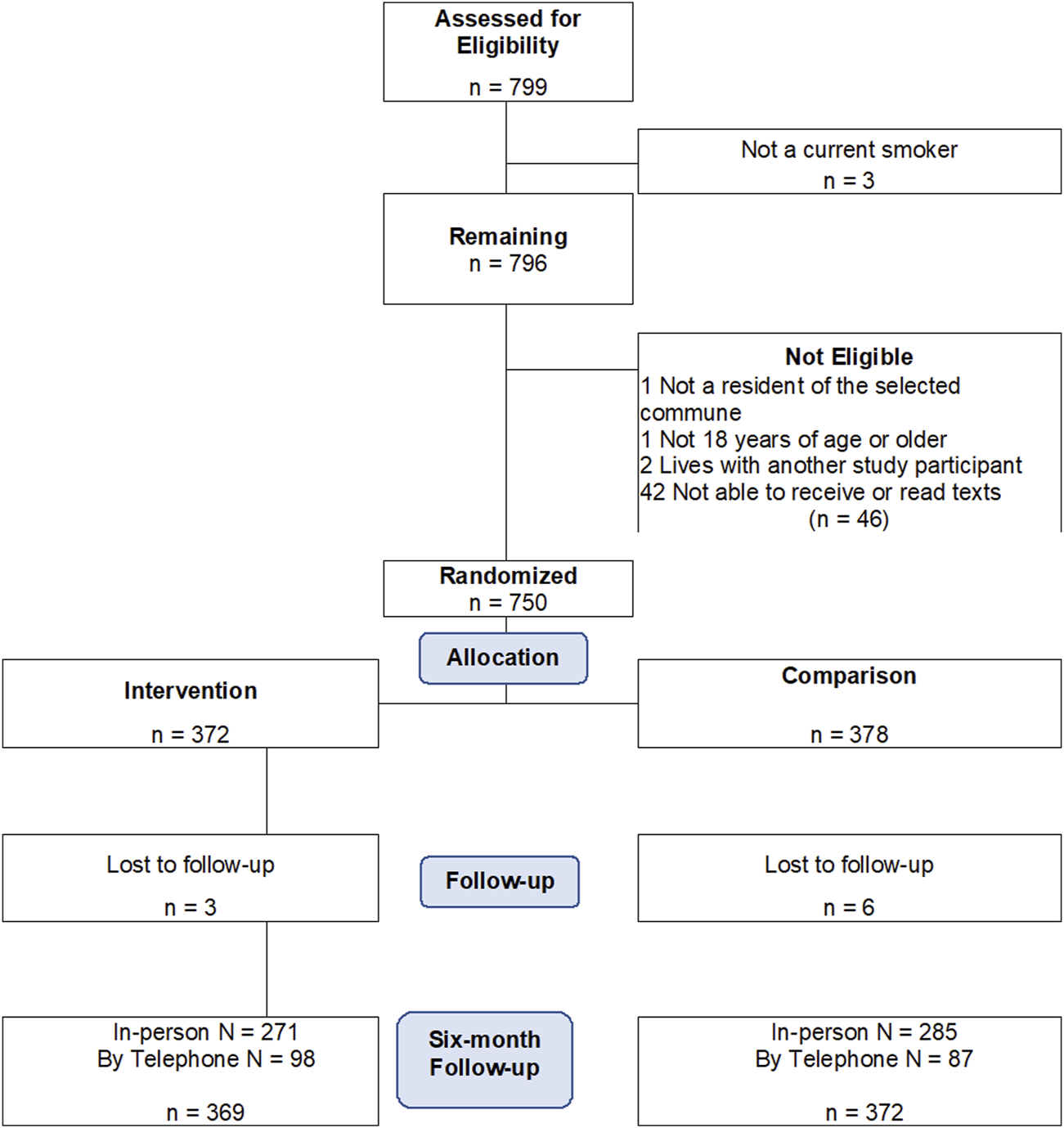
Flow diagram showing allocation of participants into study arms of a text based smoking cessation randomized intervention conducted among rural Vietnamese people who smoke (mHealth Messaging to Motivate Quitline Use and Quitting (M2Q2): RCT in rural Vietnam, Vietnam, 2017-2022).
Participants, Inclusion and Exclusion Criteria
In Vietnam, the healthcare system is organized into four levels. The lowest level (the communes) contains community health centers, responsible for primary healthcare, outpatient services, and routine health delivery services. The four communes selected for this study satisfied the following criteria: (1) had a community health center with a medical doctor; (2) were not currently participating in other smoking cessation studies; and (3) had a minimum distance of 12 km from the other study communes to minimize contamination. Participant inclusion criteria included: (1) a resident of the selected commune; (2) current smoker; (3) able to receive texts and read text (literate); (4) not cognitively impaired; (5) not a participant who helped develop the motivational texts used in the intervention; and (6) not a family member of another participant in the study.
Community Health Workers (CHWs) advertised the study at community health centers. During monthly recruitment events, study staff screened interested individuals for eligibility, obtained informed consent, and completed a baseline survey before randomization. Participants received a mobile telephone credit for participating or a basic phone that could be used for texting if they did not own a mobile phone.
Intervention and Comparison Arms
Intervention Condition
The intervention included text messaging and NRT provision. Participants received three types of text messages. The first type was one-way peer text messages sent daily in the first week and two messages per week for the next 25 weeks of their participation. We created new peer messages written by people who currently or recently smoked in Vietnam and had used the Bach Mai Quitline. We also adapted peer messages from those developed in U.S.-based texting studies by translating and having these same participants review and rewrite the messages to increase relevance to the target population [15]. The peer messages included motivational messages, tips, and strategies to quit smoking (e.g., tips to manage cravings) and encouraged Quitline use. The second type was a two-way message sent every 2 weeks asking participants whether they were interested in being referred to the Quitline. Quitline counselors then proactively called and enrolled interested participants in counseling sessions. We trained the Quitline counselors in best practices for counseling people who smoke (e.g., topics included motivational interviewing, pharmacotherapy, and behavioral interventions for smoking cessation). The third type was a two-way message assessing whether the participants had smoked recently, followed by tailored feedback encouraging the participants toward their smoking cessation goals, sent bi-weekly in alternate weeks to the Quitline messages. We have detailed our procedure for adapting the peer messages and the Quitline training protocol [11].
Both intervention and comparison participants could receive NRT at no cost from the communes by requesting NRT during their Quitline calls (although Quitline use was not promoted in comparison participants). However, due to high enthusiasm among the participants, many of the communes distributed the NRT among all the participants without adhering to the study protocol.
Comparison Condition
Participants did not receive peer messages. They received only the bi-weekly two-way assessment question assessing whether they had smoked recently. However, they did not receive tailored feedback based on their responses. We included these assessment messages to maximize blinding to the randomization group since we were promoting the study as a texting study. Quitline use was not promoted in comparison participants; however, participants were not restricted from Quitline use if they found it via other means.
Data Collection and Main Outcomes
All survey instruments were translated into Vietnamese by a certified translator. Baseline data included demographics and smoking-related behaviors (e.g., level of addiction and readiness to quit). At 6 months, Quitline and NRT use was assessed via Quitline and commune site-collected data respectively. Self-efficacy was assessed at baseline and follow-up using the Smoking Self-Efficacy Questionnaire (SEQ-12) [19]. We assessed the 7-day point prevalence smoking cessation using the question (Do you currently smoke tobacco [smoked even 1 puff of tobacco in the last 7 days].). We also assessed other forms of tobacco use by presenting popular options of tobacco as checkboxes and an open textbox. Biochemical verification was conducted for those who self-reported as quitters, and those with greater than 6 parts per million (ppm) of carbon monoxide were classified as smokers.
Qualitative Exit Interviews
We conducted qualitative interviews with participants (n = 30) who had completed the six-month follow-up and explored the use of text messages, Quitline, NRT, and the effect of COVID-19 on their tobacco use. Study staff generated a list of potential participants based on the commune of residence and smoking status and mailed them a fact sheet describing the qualitative interview. During phone calls, verbal consent was obtained, and interviews were scheduled. Participants were reimbursed for their interview participation (USD 15). Interviews were in-person, audio-recorded, transcribed, and translated into English.
Sample Size and Power
We calculate power with the comparison cessation rate at 10%. Based on our prior trials, we have detected a 9% difference in intervention and comparison, comparing the messaging system with a robust, website-only comparison (as we have a minimal control in this study, we estimated the difference may be greater). With a sample of 600 participants, we were powered to detect a 10% difference between groups (alpha at 0.05) with 91% power. We recruited 750 participants estimating 15%–20% attrition.
Randomization
Participant allocation to study arms was based on a permuted block scheme in which treatment assignments were made within blocks so that numbers assigned to each treatment arm are equal after filling a block. Blocks of various sizes (2, 4, and 6) were used in random order to facilitate allocation concealment. Randomization was stratified by commune site. Participants and the staff conducting the six-month outcome evaluation were also blinded to allocation condition.
Data Analysis
The independent variable was the randomization condition for all analyses. For assessing Quitline contact and NRT use, we reported proportions and tested the differences in proportions between groups using Fisher’s exact test. The comparison of mean SEQ-12 scores between groups was conducted using a linear mixed model accounting for clustering within commune. To calculate smoking cessation, we first conducted the analysis using the 7-day point prevalence question. Logistic regression accounting for clustering within commune using a random effects model was used to report the odds of smoking cessation. We report both self-report and biochemically verified odds. Since several participants reported waterpipe use, we repeated the smoking cessation assessment by including waterpipe use in addition to the 7-day point prevalence question. An alpha level of 0.05 was used as a criterion to determine statistical significance. All analyses were conducted using SAS software (version 9.4; SAS Institute, Cary, NC).
Qualitative Analysis
We used Rapid Qualitative Analysis, an efficient method of qualitative analysis when pre-set questions are being explored (e.g., acceptability of the texting system), to extract information from each interview and to compile findings across interviews in a series of domains [20–22], an efficient method of qualitative analysis when pre-set questions are being explored (e.g., acceptability for the texting system).
Results
The study was conducted among 750 current smokers recruited through four community health centers, with 372 being randomly assigned to the intervention group and 372 randomly assigned to the intervention group and 378 randomly assigned to the comparison group (Figure 1). Our overall follow-up rate was 98.8%. Carbon monoxide biochemical verification of smoking cessation had a lower follow-up rate (n = 178/365 of those who self-reported quitting smoking, 48.8%) due to COVID-19-related protocol changes, as it was deemed unsafe to use the carbon monoxide devices during the pandemic. In addition, a carbon monoxide device failure during one of the follow-up events affected the data collection of 19 participants.
Sex was not an eligibility criterion because rates of smoking among women are very low in Vietnam, and therefore, the sample was 100% male. There were no baseline differences in participant’s demographics (Table 1) or smoking-related behaviors (Table 2). There were no baseline differences in characteristics between those who completed the carbon monoxide verification and others.
TABLE 1
| Participant characteristics | Intervention | Comparison | p-value |
|---|---|---|---|
| N = 372 | N = 377a | ||
| Age, mean (SD) | 42.7 (12.5) | 42.7 (12.6) | 0.96 |
| Education Level | |||
| Primary school | 27 (7.3) | 28 (7.4) | 0.94 |
| Completed secondary school | 165 (44.4) | 175 (46.4) | |
| Vocational college/college/university or above | 65 (17.5) | 61 (16.2) | |
| Completed high school | 115 (30.9) | 113 (30.0) | |
| Marital Status | |||
| Divorced or widowed/Separated/Single | 49 (13.2) | 52 (13.8) | 0.80 |
| Married/A member of an unmarried couple | 323 (86.8) | 325 (86.2) | |
| Employment | |||
| Self-employed | 82 (22.0) | 95 (25.2) | 0.43 |
| Farmer | 95 (25.5) | 79 (21.0) | |
| Paid Work | 155 (41.7) | 165 (43.8) | |
| Other | 40 (10.8) | 38 (10.1) | |
| Number of adults in household, mean (SD) | 3.2 (1.2) | 3.3 (1.4) | 0.29 |
| Number of children in household, mean (SD) | 1.5 (1.3) | 1.3 (1.2) | 0.08 |
| Past 12 months: were worried or stressed about having enough money? | |||
| Never/Rarely | 195 (52.4) | 211 (56.0) | 0.22 |
| Sometimes | 84 (22.6) | 66 (17.5) | |
| Usually/Always | 93 (25.0) | 100 (26.5) | |
| Number of Comorbidities | |||
| None | 176 (47.3) | 173 (45.9) | 0.42 |
| One comorbidity | 104 (28.0) | 121 (32.1) | |
| Two or more comorbidity | 92 (24.7) | 83 (22.0) | |
| How would you describe your own health? | |||
| Excellent/Very Good | 87 (23.4) | 74 (19.6) | 0.61 |
| Good | 266 (71.5) | 281 (74.5) | |
| Fair | 17 (4.6) | 20 (5.3) | |
| Poor | 2 (0.54) | 2 (0.53) | |
| In the last 6 months, did you have to stay overnight in the hospital for any reason? | |||
| Yes | 20 (5.4) | 19 (5.0) | 0.84 |
| No | 352 (94.6) | 358 (95.0) | |
Demographic and socio-economic characteristics of participants randomized to a text-based smoking cessation intervention (mHealth Messaging to Motivate Quitline Use and Quitting (M2Q2): RCT in rural Vietnam, Vietnam, 2017-2022).
One participant did not complete the baseline survey and subsequently withdrew from the study.
TABLE 2
| Participant characteristics | Intervention | Comparison | p-value |
|---|---|---|---|
| N = 372 | N = 377a | ||
| Number of cigarettes consumed per day, mean (SD) | 13.5 (8.9) | 13.2 (11.2) | 0.71 |
| Age when first smoked tobacco; mean (SD) | 18.7 (6.1) | 18.6 (5.6) | 0.80 |
| Number of years: daily tobacco use: mean (SD) | 23.9 (13.4) | 23.7 (13.8) | 0.83 |
| How soon after you wake up do you first smoke tobacco? | |||
| Within 5 min | 153 (41.1) | 135 (35.8) | 0.30 |
| 6–30 min | 117 (31.5) | 116 (30.8) | |
| 31–60 min | 21 (5.6) | 25 (6.6) | |
| After 60 min | 81 (21.8) | 101 (26.8) | |
| Do you smoke other tobacco products? | |||
| Yes | 198 (53.2) | 202 (53.6) | 0.92 |
| No | 174 (46.8) | 175 (46.4) | |
| Other tobacco products smoke | |||
| Water pipes | 196 (52.7) | 202 (53.6) | 0.81 |
| Have you ever tried an “e-cigarette,” even just one time? | 0.16 | ||
| Yes | 77 (20.7) | 63 (16.7) | |
| No | 295 (79.3) | 314 (83.3) | |
| Does your workplace have any rules about smoking tobacco? | 0.62 | ||
| Yes | 88 (23.7) | 95 (25.2) | |
| No | 284 (76.3) | 282 (74.8) | |
| How much money per week do you currently spend on tobacco products? | |||
| 0–10,000 VND | 47 (12.6) | 66 (17.5) | 0.10 |
| 10,000–20,000 VND | 18 (4.8) | 30 (8.0) | |
| 20,000–30,000 VND | 46 (12.4) | 40 (10.6) | |
| 30,000–40,000 VND | 50 (13.4) | 41 (10.9) | |
| >40,000 VND | 211 (56.7) | 200 (53.1) | |
| Quit attempt in past 12 months | 0.57 | ||
| Yes | 210 (56.5) | 205 (54.4) | |
| No | 162 (43.6) | 172 (45.6) | |
| Before being contacted for this survey, had you ever heard of the Bach Mai Quitline? | 0.32 | ||
| Yes | 58 (15.6) | 69 (18.3) | |
| No | 314 (84.4) | 308 (81.7) | |
| Besides yourself, does anyone who lives in your home currently smoke tobacco? | 0.78 | ||
| Yes | 111 (29.8) | 109 (28.9) | |
| No | 261 (70.2) | 268 (71.1) | |
| Baseline smoking self-efficacy SEQ-12, mean (SD) | 32 (9.9) | 33 (9.9) | 0.10 |
Smoking characteristics of participants randomized to a text-based smoking cessation intervention (mHealth Messaging to Motivate Quitline Use and Quitting (M2Q2): RCT in rural Vietnam, Vietnam, 2017-2022).
One participant did not complete the baseline survey and subsequently withdrew from the study.
Quitline Use
The intervention group had a significantly higher proportion of Quitline-verified use than the comparison group (proportion: 0.18, 95% CI 0.14, 0.22 vs. proportion: 0.01, 95% C 0.002, 0.042, p < 0.0001; Table 3). Quitline users had a mean age of 43 (Standard Deviation SD = 12) years, most had completed secondary school (39%) or high school (33%), and the majority were married or in a relationship (92%). About 41% smoked their first cigarette within 5 min of waking up, and 35% smoked within 6–30 min of waking. About 27% of them lived with someone who also smoked tobacco. The mean number of cigarettes smoked per day was 14 (SD = 8.9). It took a mean of 9.4 (SD = 13.2) days from when participants indicated they were interested in talking with the Quitline to their first call. Quitline users completed a mean of 5.3 (SD = 3.4) calls.
TABLE 3
| Quitline use | Intervention (n = 369) | 95% CI of proportion | Comparison (n = 372) | 95% CI of proportion | p-Value |
|---|---|---|---|---|---|
| Proportion | Proportion | ||||
| Quitline verified use | 0.18 | (0.14, 0.22) | 0.01 | (0.002, 0.02) | <.0001a |
| Self-reported any Quitline use | 0.25 | (0.21, 0.3) | 0.02 | (0.009, 0.04) | <.0001a |
| Nicotine Replacement Therapy (NRT) use | proportion | 95% CI of proportion | proportion | 95% CI of proportion | p-value |
| Commune verified NRT use | 0.19 | (0.15, 0.23) | 0.18 | (0.14, 0.22) | 0.78 |
| Self-reported NRT use | 0.25 | (0.21, 0.3) | 0.24 | (0.20, 0.29) | 0.82 |
| Smoking Self-Efficacy SEQ-12 | mean (SD) | 95% CI of mean | mean (SD) | 95% CI of mean | p-value |
| 43 (10.6) | (42, 44) | 43 (10.2) | (42, 44) | 0.88b |
Quitline use and self-efficacy at six-month follow-up for participants randomized to a text-based smoking cessation intervention (mHealth Messaging to Motivate Quitline Use and Quitting (M2Q2): RCT in rural Vietnam, Vietnam, 2017-2022).
Fisher’s exact test for the p-value.
F-test p-value from linear regression model accounting for clustering within commune.
Nicotine Replacement Therapy (NRT) Use
There were no differences in NRT use between the two groups (Table 3).
Self-Efficacy
Smoking self-efficacy increased from baseline in both groups (32–43 in the intervention group, and 33 to 43 in the comparison group) with no significant difference between groups at 6 months (Table 3).
Smoking Cessation
Overall, 28% of participants had quit at 6 months. There were no differences in the odds of carbon monoxide-verified smoking cessation (Odds Ratio: 0.99, 95% CI 0.57, 1.7; Table 4). Waterpipe use was reported by 105 (28%) of intervention and 103 (28%) of comparison participants at follow-up. After including waterpipe use, we estimated that 23% of participants had quit at 6 months and the odds of carbon monoxide-verified smoking cessation was 0.92 (95% CI 0.51, 1.7).
TABLE 4
| Intervention | Comparison | OR (95% CI of proportion) for intervention vs. Comparisona | p-Value | |
|---|---|---|---|---|
| Proportion | Proportion | |||
| Carbon monoxide verified smoking cessation | (n = 326) | (n = 339) | ||
| 7-day point prevalence biochemically verified | 0.28 | 0.28 | 0.99 (0.57, 1.7) | 0.97 |
| 7-day point prevalence and waterpipe use biochemically verified | 0.22 | 0.24 | 0.92 (0.51, 1.7) | 0.68 |
| Self-report smoking cessation | (n = 369) | (n = 372) | ||
| 7-day point prevalence only | 0.52 | 0.50 | 1.1 (0.82, 1.5) | 0.58 |
| 7-day point prevalence and waterpipe use | 0.37 | 0.36 | 1.1 (0.65, 1.7) | 0.74 |
Smoking cessation at six-month follow-up for participants randomized to a text-based smoking cessation intervention (mHealth Messaging to Motivate Quitline Use and Quitting (M2Q2): RCT in rural Vietnam, Vietnam, 2017-2022).
Accounting for clustering within commune.
Qualitative Findings
Most participants endorsed that the text messages were understandable and acceptable in tone. While participants liked the frequency of the text messages, some reported that receiving them during work hours when they did not have their phone was inconvenient. Some participants reported ignoring or deleting texts because they thought they were spam.
Participants were positive about their Quitline counselors and found them caring and “friendly like a family member.” Other participants felt that they were able to quit on their own and did not need the Quitline or NRT. A community physician usually prescribed NRT. While most found the NRT helpful, some participants reported experiencing side effects from NRT (e.g., itchy throat, nausea, and gastrointestinal problems) but did not report stopping NRT for these reasons.
The COVID-19 pandemic occurred during the trial, and participants reported differing effects on their smoking habits. Some participants reported smoking less because they were at home more, had less money to spend on cigarettes, were wearing masks, or were more aware of the health effects of COVID-19 on people who smoke. Conversely, some participants reported smoking more during the pandemic, also because they were at home more, were bored, or because they believed that smoking would protect them against COVID-19. For example, one participant stated: “If I smoke, I think that COVID will be afraid of me.”
Discussion
The M2Q2 texting intervention significantly increased Quitline use among participants from a rural province in northern of Vietnam. While the intervention did not increase smoking cessation compared with the comparison group, the quit rates in both groups (28%) were remarkable. For comparison, the “Treating Tobacco Use and Dependence: 2008 Update” reported an estimated quit rate of 24.7% (21.0–28.4) for intensive in-person interventions greater than eight sessions [23]. A recent clinical trial that tested the efficacy of varenicline reported a 7-day point prevalence of 29.0% in the varenicline arm, compared to 6% in the placebo arm [24]. Our findings also revealed self-efficacy increased by greater than one standard deviation from baseline to follow-up for both groups, another remarkable temporal trend. Further, there were notable differences in cessation rates between the self-report and carbon-monoxide-verified cessation, which suggests that future trials in low- and middle-income countries like Vietnam should carefully consider how to measure cessation.
Our study findings pose important questions for Vietnam, a country that has only recently begun addressing tobacco use. The texting intervention increased Quitline use, showing it may be a viable option in Vietnam. People in rural parts of Vietnam may not have been exposed to messages promoting Quitline use and thus may have been more willing to accept the referral to the Quitline in our study. The two prior studies that tested the use of texting for increasing Quitline use were both conducted in the United States and reported varied results, possibly due to differences in the frequency of the messages promoting Quitline use [25, 26]. Future studies could experiment with the number and framing of messages to determine the optimal approach to motivate Quitline use.
It was remarkable that both groups achieved high quit rates and increased self-efficacy, suggesting that Vietnam may be at a pivotal transitional time in their fight against tobacco use. A high proportion of people in Vietnam who smoke have reported making recent quit attempts (37.5%) compared to other countries [27], but may simply not have had access to tobacco cessation programs given the low reach of current tobacco efforts. Our study suggests that even minimal exposure to a tobacco cessation program, such as our comparison (i.e., participating in a tobacco cessation study and text assessment of current smoking), could have a high impact on reducing the tobacco use rate in Vietnam. Investing in such tobacco programs that deliver minimal exposure to tobacco cessation and could be implemented to have a broad reach may considerably benefit Vietnam. These could include training providers or CHWs to deliver brief interventions (such as the 5As) or to continue to improve the texting program as discussed below.
In addition, despite its lack of success in increasing tobacco cessation rates in our study, we posit that Vietnam must continue to invest in more intensive forms of tobacco control, like Quitlines, to ensure that tobacco control services are distributed fairly and equitably. This is critical to avoid the challenges faced by the U.S. tobacco control efforts, which, although effective in reducing overall tobacco use, have led to segments of the population being left behind. Highlighted below are potential areas of improvement in the intervention components based on our results.
The Vietnam Quitline modeled on the U.S. (e.g., frequency and number of calls) may not be optimized for people in Vietnam. Another study that evaluated the Quitline services in Vietnam also reported high relapse rates despite high satisfaction among participants [28]. Additional research on the specific challenges of the people in Vietnam who smoke may be needed. We found the intervention did not increase self-efficacy compared to the comparison, and self-efficacy has been shown as a mediator of tobacco cessation [29]. Future studies could investigate additional approaches to increasing self-efficacy, such as supporting the practice of short-term quit attempts designed to help the participant succeed, which can lead to increased knowledge, self-efficacy, and potentially cessation [30].
Similar to another study, there were no additive effects of the combination of text messaging and Quitline use [31]. Our text messages were designed to be independent of Quitline use as we anticipated only a subset would use the Quitline. Text messages that reinforce the messages of the counselors may more effectively promote synergism between the Quitline and the text messages, and future trials should test this integrated approach. Participants’ feedback on our text messaging intervention was varied and suggested that further refinement of the messages, including providing choices for the timing of the messages, may increase the intervention’s effectiveness.
There is debate on whether light-touch interventions (such as M2Q2) with minimal direct contact with participants, as opposed to interventions such as individual counseling, needs biochemical verification of smoking cessation. Some argue that the social desirability in light-touch interventions is low and that needing biochemical verification may reduce the generalizability of the sample (as only the more motivated subset might participate) and the study’s feasibility [32, 33]. The high disagreement in our results between the self-report and the carbon-monoxide verified results may indicate that the social desirability in countries like Vietnam is higher and that even light touch interventions in these countries would benefit from biochemical verification.
Our study is the first trial to test a texting intervention among rural participants of a LMIC, as other such studies have been conducted in urban populations [3]. Our follow-up rate of 98% was also high. We recruited rural participants in northern Vietnam, who seldom have the chance to join research studies, through community health workers. This recruitment approach may have increased their appreciation and motivation for engaging with our study. However, we had limitations in our study. Although we did not exclude participants based on their motivation to quit smoking, we acknowledge that those who participated in the study may have had higher motivation levels than the general population. Despite informing the participants during the baseline session about the specific cell phone number that would send them text messages, we could not estimate how many ignored the messages as spam. As noted, a protocol deviation reduced our ability to detect differences in NRT use. We also did not collect additional details on NRT use, including dosage and duration. The COVID-19 pandemic reduced our ability to conduct biochemical verification with all participants. We also collected only minimal data about how the COVID-19 pandemic may have impacted our participants’ smoking behaviors.
Conclusion
Our trial adds to the growing literature on mobile interventions for tobacco cessation in LMICs. Our participants were from rural areas who were underrepresented in prior trials in LMICs. Our results showed that texting is a viable strategy to increase the use of Quitline services in Vietnam, while also raising important implications for future tobacco policy in Vietnam, such as whether an intervention that provides minimal exposure to tobacco cessation, like our comparison, could be used for increasing reach and impact of tobacco interventions. Our next steps are to explore additional ways to increase the effectiveness of the Quitline and the texting system, such as incorporating strategies to promote self-efficacy, closer integration of the text messages with the Quitline messages and providing additional flexibility in the timing of the messages.
Statements
Ethics statement
The studies involving humans were approved by the UMass Chan Institutional Review Board and monitored by a Data and Safety Monitoring Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Funding
This research was supported by John E Fogarty International Center of the National Institutes of Health under award number R01TW010647. JF was supported by the National Heart, Lung, and Blood Institute under award number 1K01HL163254. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funder had no role in the study design, data collection, analysis, writing, or decision to submit.
Acknowledgments
The authors gratefully acknowledge their partners at the community health centers, district health centers, the Bach Mai Quitline, the provincial department of health in the Hung Yen province, and the Tobacco Control Fund at Vietnam Ministry of Health.
Conflict of interest
The authors declare that they do not have any conflicts of interest.
References
1.
World Health Organization. Tobacco Key Facts (2020). Available at: https://www.who.int/news-room/fact-sheets/detail/tobacco (Accessed September 15, 2020).
2.
Akanbi MO Carroll AJ Achenbach C O'Dwyer LC Jordan N Hitsman B et al The Efficacy of Smoking Cessation Interventions in Low- and Middle-Income Countries: A Systematic Review and Meta-Analysis. Addiction (Abingdon, England) (2019) 114(4):620–35. 10.1111/add.14518
3.
Krishnan N Gu J Abroms LC . Mobile Phone-Based Messaging for Tobacco Cessation in Low and Middle-Income Countries: A Systematic Review. Addict behaviors (2021) 113:106676. 10.1016/j.addbeh.2020.106676
4.
Whittaker R McRobbie H Bullen C Rodgers A Gu Y Dobson R . Mobile Phone Text Messaging and App-Based Interventions for Smoking Cessation. Cochrane database Syst Rev (2019) 10(10):Cd006611. 10.1002/14651858.CD006611.pub5
5.
Scott-Sheldon LA Lantini R Jennings EG Thind H Rosen RK Salmoirago-Blotcher E et al Text Messaging-Based Interventions for Smoking Cessation: A Systematic Review and Meta-Analysis. JMIR mHealth and uHealth (2016) 4(2):e49. 10.2196/mhealth.5436
6.
CENTERS FOR DISEASE CONTROL AND PREVENTION WORLD HEALTH ORGANIZATION. Global Adult Tobacco Survey (GATS) Viet Nam 2010 (2010).
7.
Nguyen TNP Love J Hunsberger M Tran TPT Phan TH Luong NK et al Individual-Social- and Policy-Factors Associated With Smoking Cessation Among Adult Male Cigarette Smokers in Hanoi, Vietnam: A Longitudinal Study. BMC public health (2023) 23(1):1883. 10.1186/s12889-023-16781-7
8.
Luu NM Tran TTH Luong NK Phan TH Phan VC Khuong QL et al Smoking Cessation, Quit Attempts and Predictive Factors Among Vietnamese Adults in 2020. Asian Pac J Cancer Prev (2023) 24(5):1701–10. 10.31557/APJCP.2023.24.5.1701
9.
Hoang Anh PT Thu le T Ross H Quynh Anh N Linh BN Minh NT . Direct and Indirect Costs of Smoking in Vietnam. Tob Control (2016) 25(1):96–100. 10.1136/tobaccocontrol-2014-051821
10.
Vietnam Ministry of Health. Joint Annual Health Review- Strengthening Prevention and Control of Non-Communicable Diseases (2014).
11.
Larkin C Wijesundara J Nguyen HL Ha DA Vuong A Nguyen CK et al mHealth Messaging to Motivate Quitline Use and Quitting: Protocol for a Community-Based Randomized Controlled Trial in Rural Vietnam. JMIR Res Protoc (2021) 10(10):e30947. 10.2196/30947
12.
Tran BX Houston S . Mobile Phone-Based Antiretroviral Adherence Support in Vietnam: Feasibility, Patient's Preference, and Willingness-To-Pay. AIDS Behav (2012) 16(7):1988–92. 10.1007/s10461-012-0271-5
13.
Houston TK Chen J Amante DJ Blok AC Nagawa CS Wijesundara JG et al Effect of Technology-Assisted Brief Abstinence Game on Long-Term Smoking Cessation in Individuals Not yet Ready to Quit: A Randomized Clinical Trial. JAMA Intern Med (2022) 182(3):303–12. 10.1001/jamainternmed.2021.7866
14.
Houston TK Sadasivam RS Allison JJ Ash AS Ray MN English TM et al Evaluating the QUIT-PRIMO Clinical Practice ePortal to Increase Smoker Engagement With Online Cessation Interventions: A National Hybrid Type 2 Implementation Study. Implement Sci (2015) 10:154. 10.1186/s13012-015-0336-8
15.
Coley HL Sadasivam RS Williams JH Volkman JE Schoenberger YM Kohler CL et al Crowdsourced Peer-Versus Expert-Written Smoking-Cessation Messages. Am J Prev Med (2013) 45(5):543–50. 10.1016/j.amepre.2013.07.004
16.
Sadasivam RS Borglund E Adams R Marlin B Houston TK . Impact of a Collective Intelligence Tailored Messaging System on Smoking Cessation: The PERSPeCT Randomized Experiment. J Med Internet Res (2016) 18:e285. 10.2196/jmir.6465
17.
Faro JM Nagawa CS Allison JA Lemon SC Mazor KM Houston TK et al Comparison of a Collective Intelligence Tailored Messaging System on Smoking Cessation Between African American and White People Who Smoke: Quasi-Experimental Design. JMIR mHealth and uHealth (2020) 8(4):e18064. 10.2196/18064
18.
Bandura A . Social Foundation of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall (1986).
19.
Etter JF Bergman MM Humair JP Perneger TV . Development and Validation of a Scale Measuring Self‐Efficacy of Current and Former Smokers. Addiction (Abingdon, England) (2000) 95(6):901–13. 10.1046/j.1360-0443.2000.9569017.x
20.
Vindrola-Padros C Johnson GA . Rapid Techniques in Qualitative Research: A Critical Review of the Literature. Qual Health Res (2020) 30(10):1596–604. 10.1177/1049732320921835
21.
Nagawa CS Lane IA Davis M Wang B Pbert L Lemon SC et al Experiences Using Family or Peer Support for Smoking Cessation and Considerations for Support Interventions: A Qualitative Study in Persons With Mental Health Conditions. J Dual Diagn (2023) 19(1):40–8. 10.1080/15504263.2022.2159732
22.
Hamilton AB Finley EP . Qualitative Methods in Implementation Research: An Introduction. Psychiatry Res (2019) 280:112516. 10.1016/j.psychres.2019.112516
23.
Fiore M . Treating Tobacco Use and Dependence: 2008 Update. Rockville, Md: U.S. Dept. of Health and Human Services, Public Health Service (2008).
24.
Russo C Walicka M Caponnetto P Cibella F Maglia M Alamo A et al Efficacy and Safety of Varenicline for Smoking Cessation in Patients With Type 2 Diabetes: A Randomized Clinical Trial. JAMA Netw Open (2022) 5(6):e2217709. 10.1001/jamanetworkopen.2022.17709
25.
Hoeppner BB Hoeppner SS Abroms LC . How Do Text-Messaging Smoking Cessation Interventions Confer Benefit? A Multiple Mediation Analysis of Text2Quit. Addiction (Abingdon, England) (2017) 112(4):673–82. 10.1111/add.13685
26.
Krebs P Sherman SE Wilson H El-Shahawy O Abroms LL Zhao X et al Text2Connect: A Health System Approach to Engage Tobacco Users in Quitline Cessation Services Via Text Messaging. Translational Behav Med (2020) 10(1):292–301. 10.1093/tbm/ibz033
27.
Hoang LT Tuyet Hanh TT Khue LN Hai PT Can PV Long KQ et al Intention to Quit and Predictive Factors Among Current Smokers in Vietnam: Findings From Adult Tobacco Survey 2020. Tob use insights (2022) 15:1179173X221098460. 10.1177/1179173X221098460
28.
Ngo QC Doan LPT Vu GV Phan TP Chu HT Duong AT et al Telephone-Based Smoking Cessation Counseling Service: Satisfaction and Outcomes in Vietnamese Smokers. Healthcare (Basel, Switzerland) (2022) 11(1):135. 10.3390/healthcare11010135
29.
Elshatarat RA Yacoub MI Khraim FM Saleh ZT Afaneh TR . Self-Efficacy in Treating Tobacco Use: A Review Article. Proc Singapore Healthc (2016) 25(4):243–8. 10.1177/2010105816667137
30.
Burris JL Heckman BW Mathew AR Carpenter MJ . A Mechanistic Test of Nicotine Replacement Therapy Sampling for Smoking Cessation Induction. Psychol Addict behaviors (2015) 29(2):392–9. 10.1037/adb0000035
31.
Boal AL Abroms LC Simmens S Graham AL Carpenter KM . Combined Quitline Counseling and Text Messaging for Smoking Cessation: A Quasi-Experimental Evaluation. Nicotine Tob Res (2016) 18(5):1046–53. 10.1093/ntr/ntv249
32.
Heffner JL McClure JB . Commentary on Graham et al.: Biochemical Verification of Abstinence in Remotely Conducted Smoking Cessation Trials Should Not Be a Universal Design Requirement for Rigor. Addiction (Abingdon, England) (2022) 117(4):1047–8. 10.1111/add.15803
33.
Verification SSB . Biochemical Verification of Tobacco Use and Cessation. Nicotine Tob Res (2002) 4(2):149–59. 10.1080/14622200210123581
Summary
Keywords
smoking cessation, LMICs, texting, Quitlines, mhealth
Citation
Sadasivam RS, Nagawa CS, Wijesundara JG, Flahive J, Nguyen HL, Larkin C, Faro JM, Balakrishnan K, Ha DA, Nguyen CK, Vuong A, Phan PT, Pham QPL, Allison JJ and Houston TK (2024) Peer Texting to Promote Quitline Use and Smoking Cessation Among Rural Participants in Vietnam: Randomized Clinical Trial. Int J Public Health 69:1606941. doi: 10.3389/ijph.2024.1606941
Received
06 December 2023
Accepted
29 February 2024
Published
08 April 2024
Volume
69 - 2024
Edited by
Rana Charafeddine, Scientific Institute of Public Health (WIV-ISP), Belgium
Reviewed by
Elise Braekman, Sciensano, Belgium
One reviewer who chose to remain anonymous
Updates
Copyright
© 2024 Sadasivam, Nagawa, Wijesundara, Flahive, Nguyen, Larkin, Faro, Balakrishnan, Ha, Nguyen, Vuong, Phan, Pham, Allison and Houston.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rajani S. Sadasivam, rajani.sadasivam@umassmed.edu
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.