- 1End-of-Life Care Research Group, Department of Family Medicine and Chronic Care, Vrije Universiteit Brussel, Brussels, Belgium
- 2End-of-Life Care Research Group, Department of Public Health and Primary Care, Universiteit Gent, Ghent, Belgium
- 3Department of Philosophy and Moral Sciences, Bioethics Institute Ghent, Universiteit Gent, Ghent, Belgium
Objectives: To explore the support needs that patients and relatives experience throughout their medical aid in dying (MAID) trajectories.
Methods: A qualitative study in Belgium in 2022 using 1) semi-structured interviews with and personal written narratives of patients requesting MAID and 2) semi-structured interviews with relatives of patients requesting MAID. We performed a qualitative content analysis.
Results: We included in our analysis the lived experiences of 15 patients and 21 of their relatives. We identified eight types of support needs: support for 1) maximizing daily functioning (only reported by patients), 2) making sense of the unbearable suffering (only reported by relatives), 3) managing meaningful activities, 4) navigating existential questions, 5) psycho-emotional regulation, 6) facilitating social interaction, 7) understanding the process toward MAID, 8) and handling organizational and practical matters.
Conclusion: Patients and relatives might experience multidimensional support needs throughout their MAID trajectories. Our findings suggest that they experience these trajectories more as social/existential pathways than as medical ones. A palliative care approach may be an effective way to fulfill the support needs of patients and relatives throughout their MAID trajectories.
Introduction
Medical aid in dying (MAID), including euthanasia and physician-assisted suicide, has become an increasingly important legal and medical issue. Euthanasia involves the practice in which a health practitioner ends a person’s life at their voluntary request by administering lethal drugs. Physician-assisted suicide involves the practice in which a health practitioner provides or prescribes to a patient, at his or her voluntary request, a lethal medication which the patient subsequently self-administers to end their own life [1]. At present, jurisdictions with MAID legislation cover about 300 million people across the globe [1]. Furthermore, prevalence rates of MAID continue to rise in jurisdictions where the practice is lawful [2–4]. Several jurisdictions are currently debating a possible enactment of MAID legislation.
MAID entails a complex process as patients requesting it and their relatives may experience a range of challenges, difficulties and undesired outcomes throughout their MAID trajectories [5]. These trajectories include the moment when the patient expresses an explicit desire for MAID, the assessment of the request, the performance of MAID, and the period following the performance of MAID [5, 6]. Patients, for example, sometimes feel that their autonomy and values are not respected, and may feel that healthcare professionals and relatives minimize their unbearable suffering [5, 7, 8]. Relatives, for example, may feel unprepared for the performance of MAID, can experience post-traumatic stress after the performance, and may feel excluded by healthcare professionals during the assessment of the MAID request [9–14]. These challenges, difficulties, and undesired outcomes may indicate that the support needs of patients and relatives are not adequately fulfilled, for instance, because their healthcare professionals do not know their support needs or have not assessed them properly [6, 7, 9, 15].
The existing scientific literature provides little direction on the specific support needs of patients and relatives throughout their MAID trajectories. Studies have primarily focused on describing their general experiences with MAID practice, their attitudes towards MAID, problems and difficulties they encounter in MAID practice, and their interactions with healthcare professionals [8, 16]. A better understanding of the support needs of patients and relatives in MAID practice could guide healthcare professionals in anticipating undesired outcomes and improving the quality of life of patients and relatives [17]. We sought to answer the following research question: what support needs do patients requesting MAID and their relatives experience throughout their MAID trajectories?
Methods
Research Paradigm and Study Design
We took on a social constructionist lens, assuming that support needs are social and dynamic constructs [18]. Due to the explorative nature of our research aim, we employed a qualitative design capturing the lived experiences of MAID practice among patients and relatives, using 1) semi-structured interviews with patients and relatives and 2) personal written narratives from patients through qualitative questionnaires.
In this study, we defined the medical aid in dying trajectory as beginning when the patient expresses an explicit desire for medical aid in dying, followed by the assessment of the request, the performance of medical aid in dying, and the period following the performance of medical aid in dying [5, 6].
Study Context
We conducted this study from December 2021 to September 2022 in Flanders and Brussels (Belgium). For a patient to be eligible for MAID, specific criteria must be met which are stipulated in the Belgian Act on Euthanasia [19]. In Belgium, medical aid in dying is mainly performed in the home setting (54% of all registered cases in 2020–2021), in hospitals (30%), and in nursing homes (13%) [20].
Research Participants, Recruitment, and Data Collection
We included patients and relatives having lived experiences with MAID practice. Eligibility criteria for patients were: 1) having expressed a desire for MAID to relatives (friends or family members) or healthcare professionals, or having formally requested MAID to an attending physician, or having received the formal approval from an attending physician to receive MAID; 2) being comfortable with being interviewed in Dutch; 3) residence in Flanders or Brussels, Belgium; and 4) being 18 years or older. Eligibility criteria for relatives of patients were: 1) being a family member or friend of a person who has expressed a desire for MAID or has formally requested MAID, or who has received the formal approval to receive MAID, or who received MAID prior to the interview (between 3 months and 3 years), 2) fluency in Dutch; 3) residence in Flanders or Brussels, Belgium; and 4) being 18 years or older.
We recruited participants between December 2021 and June 2022 using purposive and snowball sampling. We aimed to recruit a heterogeneous study sample in terms of sociodemographic characteristics, health conditions and principal care settings. More specifically, purposive sampling occurred through healthcare and patient organizations and associations, stakeholders, and the professional network of the End-of-Life Care Research Group in Flanders (Belgium). Snowball sampling was applied by inviting potential participants who were identified by those already included for participation in the study. Interested participants could register on a website or contact the research team. We conducted an eligibility assessment before inviting them to participate in the study. Eligible patients were allowed to participate via a semi-structured interview or a personal written narrative using an online qualitative questionnaire (LimeSurvey). We ensured that the interviewer was unfamiliar to the participants. Prior to study participation, we disclosed the identity of the interviewer to participants. Moreover, we offered participants the opportunity to get in touch with the interviewer for any questions or concerns regarding the study.
For the semi-structured interviews, we used a topic guide consisting of the following topics: 1) general experiences with MAID practice; 2) experienced practices regarding MAID; 3) experienced good practices regarding MAID, and 4) experienced support needs regarding MAID. The specific questions in the topic guide were iteratively refined throughout the data collection process. Support needs were conceptualized as the support or guidance a participant experienced as essential to meet his or her basic needs or to achieve a desired outcome in MAID practice [21]. Participants could choose whether the interview would be performed online by Whereby (http://Whereby.com) or in person at a location of their choice. XX (second author, M.Sc. in Social work, Ph.D. in Health Sciences, senior researcher, female) conducted one interview, while XX (first author, M.Sc. in Sociology, Ph.D. candidate, male) conducted the other interviews. Both are researchers with previous experience in conducting qualitative health research. Interviews were recorded and transcribed verbatim. After every interview, field notes were made to document unique observations and contextual information. For the personal written narratives, we sent an online qualitative questionnaire (LimeSurvey) to eligible patients who preferred this method of study participation [22]. The questionnaire included open-ended questions reflecting the themes of the semi-structured topic guide. We requested patients to respond to these questions by writing down their narratives and experiences, which we converted into transcripts for data analysis [22]. Data collection was informed by inductive thematic saturation in which we defined the saturation point as the stage at which no new meaning related to support needs emerges across the narratives of patients and relatives [23].
Data Analysis
We used a qualitative content analytic approach [24, 25]. In the first phase, XX and XX (last author, M.Sc. in Sociology, Ph.D. in Health Sciences, senior researcher, female) applied open inductive coding and categorization of the raw data, analyzing patients’ and relatives’ experiences separately. We linked initial codes to text fragments, aiming at identifying initial codes describing participants’ lived experiences of support needs regarding medical aid in dying. Support needs were conceptualized following the definition used during data collection [21]. XX and XX independently created a coding framework based on seven transcripts. These frameworks were then compared; inconsistencies and differences were discussed until a preliminary coding framework was reached. Next, XX used the coding framework to analyze the remaining transcripts, modifying it when new codes emerged. We used Nvivo 12 for the coding process. In the second phase, XX merged codes similar in understanding into meaningful clusters to identify types of support needs. Moreover, we concluded that saturation was reached after the 11th interview for patients and the 18th for relatives, as no new meaning in relation to support needs had arisen [23]. In the third phase, the identified clusters were discussed in group meetings with all co-authors. In this third phase, we also concluded that most types of support needs of patients are identical to those of relatives, with only a few different types. For clarity in reporting, the latter are described separately in the results section of this article. Again, inconsistencies were addressed until an agreement on final meaningful clusters, i.e., types of support needs, was reached. The field notes were used to help us organize the codes and identify meaningful clusters.
In terms of reflexivity, the research team included four health sociologists (SV, SD, KC, JC, and LD), one social worker (JG), and one bioethicist (FM), all with prior experience in qualitative methods related to end-of-life practices. None of the researchers hold strong normative positions for or against medical aid in dying. Each team member adopted a critical perspective, advocating for rigorous evaluation of medical aid in dying legislation and practices. To uphold objectivity in data interpretation, the research team convened regular discussion sessions.
Ethical Considerations
The Ethics Committee of the XX and XX approved our study (XX; 15 September 2021). We utilized pseudonyms for all participants in the transcripts and removed any identifying information. All participants provided written or oral informed consent to participate in the study.
Results
Study Sample
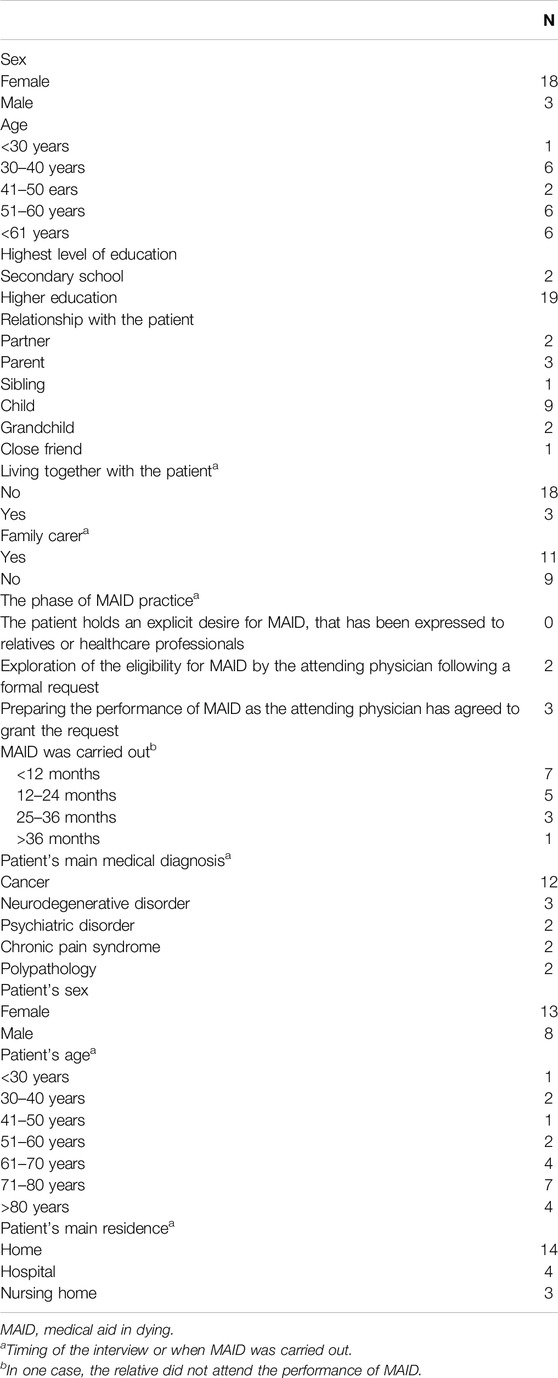
We identified 18 patients and 23 relatives as eligible for study participation, all of whom were invited to participate. 15 patients and 21 relatives (n = 36) eventually participated, whereas the other invited individuals chose not to participate or to drop out without providing their motives. We conducted nine semi-structured interviews with patients (five online interviews and four in person at the patient’s main residence), one dyadic semi-structured interview with a patient and a relative (in person at the main residence of the patient), and 20 semi-structured interviews with relatives (11 online interviews and 9 interviews in person at the main residence of the relative), and included five written narratives from patients. The mean length of the semi-structured interviews with patients was 78 min (range: 28–130 min), and with relatives 82 min (range: 54–127 min). The main characteristics of the participants are listed in Tables 1, 2.
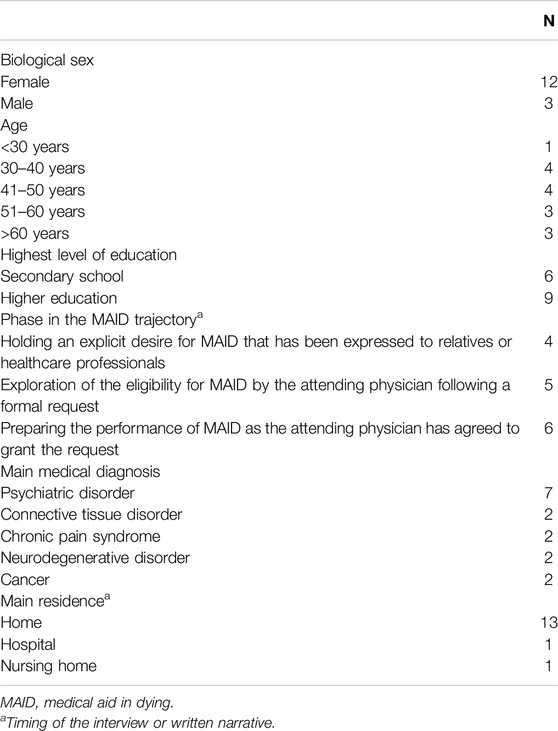
Table 1. Participant characteristics of patients requesting medical aid in dying (N = 15) (Belgium, 2021–2022).
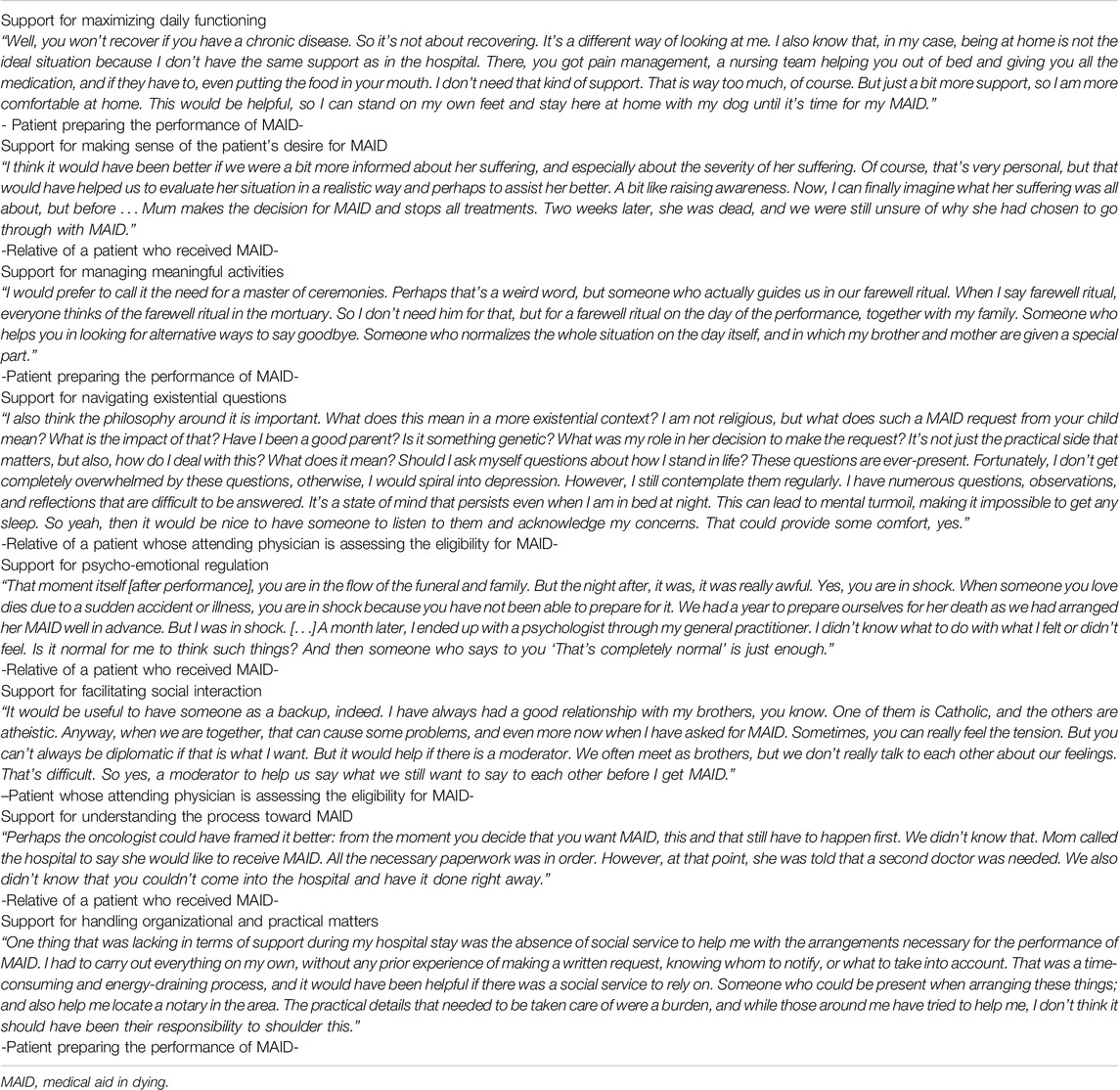
Support Needs Experienced Throughout the Medical Aid in Dying Trajectory
We identified eight types of support needs experienced by patients and relatives throughout their MAID trajectories (Figure 1). Identified support needs appeared to differ in their intensity of experience and seemed to be partially linked to a specific phase of the MAID trajectory, e.g., assessment or day of performance. We discuss each theme or type of support need separately for analytic clarity. However, they are interconnected in practice. In the following paragraphs, references to “participants” include both patients and relatives. Furthermore, some exemplary quotes are provided in Table 3.
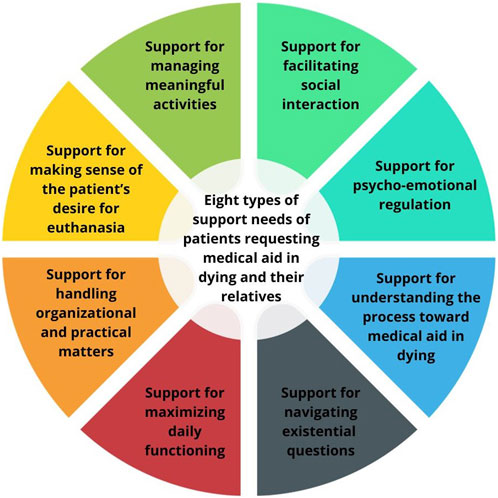
Figure 1. Eight types of support needs were identified that patients and their relatives might experience throughout their medical aid in dying trajectories. Support for maximizing daily functioning was only reported by patients, while support for making sense of the patient’s desire for medical aid in dying only in relatives. (Belgium, 2021–2022).
Support for Maximizing Daily Functioning
This support need was only found in patients. Patients repeatedly spoke of their unbearable suffering as a daily reality around which they had organized their lives. They described in many ways their ongoing struggle with accepting this suffering. Although patients recognized that no practical support could eradicate their suffering, some felt that support could ease their struggle by maximizing their daily functioning throughout their MAID trajectories. They favored practical support in carrying out daily activities and tasks, e.g., aid to travel to healthcare facilities. Some patients experienced such support as essential to maintaining a sense of self-worth. On the other hand, others experienced such support as pivotal to being able to stay at home independently and to receive MAID in their familiar environment.
Support for Making Sense of the Patient’s Desire for MAID
This support need was only identified in relatives. Relatives needed support for making sense of the patient’s desire for MAID and its broader context, such as the nature of the unbearable suffering. Most relatives needed this to 1) facilitate closure and accept the patient’s desire and 2) evaluate their potential role in alleviating the suffering. Relatives stated that this support need partially stemmed from their limited understanding of the desire for MAID as patients and healthcare professionals often reduced the desire to the patient’s medical condition. Moreover, relatives indicated that this support need was particularly strong in the early phases of the MAID trajectory, when they first learned of the patient’s desire or had just become involved in the process.
Support for Managing Meaningful Activities
Patients and relatives (hereafter referred to as participants) felt the need to experience moments and activities that gave purpose and meaning to their MAID trajectories as ways to make the most of the remaining time prior to the performance. In practice, these meaningful moments and activities reflected participants’ values, passions, lives, roles, and identities, particularly those of patients. These included, for example, preparing memorials, sharing (life) stories and memories, and participating in rituals and traditions. Participants particularly experienced a farewell ritual as one of the most meaningful activities. Moreover, relatives also identified being a family carer for the patient in his or her MAID trajectory as a meaningful activity. However, participants needed support to manage meaningful activities as they often faced difficulties and challenges. Additionally, patients with a non-terminal condition most often found their MAID trajectories to be long and purposeless and stipulated that they required support in finding meaningful activities prior to the performance.
Support for Navigating Existential Questions
Participants expressed having many existential questions and contemplating life and death throughout their MAID trajectories. This involved questioning and reflecting upon, for example, the value of life, when it is justified to request MAID, what will come after death, whether requesting MAID equals failing relatives (experienced by patients), or when one is ready to die. Consequently, participants emphasized their support need for navigating existential questions as like having a sounding board since these questions sometimes led to feelings of loneliness and distress. Furthermore, this support need appeared more acute in patients than in relatives.
Support for Psycho-Emotional Regulation
A rapid succession of negative and positive emotions characterized participants’ MAID trajectories. They particularly stressed the need for guidance in controlling and coping with negative emotions. Participants often felt overwhelmed by the intensity of their emotions and faced difficulties processing them individually. Patients’ negative emotions included anxiety due to the uncertain outcome of the MAID request, distress caused by the unpredictable progression of the unbearable suffering, and fear of death and the unknown afterlife. Negative emotions of relatives included feelings of loss and anticipatory grief throughout their MAID trajectories, stress when the request was being assessed, and tension upon receiving the news of the patient’s request.
The need for psycho-emotional regulation seemed to differ in intensity among participants. In their accounts, participants experiencing adverse events in their MAID trajectory emphasized their need for psycho-emotional regulation more strongly compared to those not experiencing adverse events. Examples of adverse events included witnessing the patient’s discomfort, complications or delays in accessing MAID, and communication issues with providers. Additionally, family carers or relatives very close to the patient also stressed their need for psycho-emotional regulation more firmly in their accounts compared with others. These relatives attributed this need in part to the fact that they neglected their emotions due to prioritizing the patient’s emotions as the focal point throughout the MAID trajectories.
Support for Facilitating Social Interaction
Participants felt a strong need for social connection and sharing their MAID trajectories with those close to them, who were often indicated as the most important individuals in their trajectories. However, many participants reported problems establishing and maintaining social interactions, and wished for support to facilitate this.
The support need for facilitating social interaction was materialized by participants in several ways. First, some participants required support to resolve social conflicts and to improve social bonds, e.g., conflict resolution through moderated family conversations. This support need was partly related to obtaining peace of mind before the performance. Moreover, some patients considered postponing the performance if social conflicts were not resolved. Second, a few patients needed social support in communicating their MAID desires or requests to relatives. Third, some relatives perceived this support as facilitating family engagement in the MAID trajectories. These relatives experienced family engagement as necessary to adequately support patients themselves in their MAID trajectories. Relatives who were at times not being engaged, experienced frustration or anger, sometimes resulting in psychological problems.
Support for Understanding the Process Toward MAID
In their MAID trajectories, participants required support for understanding the process toward MAID regarding 1) the MAID legislation and procedure, and 2) the attending physician’s decision-making regarding MAID. First, participants found it challenging to comprehend the legal modalities of MAID, especially the eligibility criteria. These difficulties led to confusion and ambiguity, such as whether patients with advanced dementia have access to MAID via an advance directive. In addition, participants wanted guidance in understanding the MAID procedure, including the formal steps one must complete before the performance. Second, participants required guidance in understanding the attending physician’s decision-making process for granting or rejecting the MAID request. Participants wanted to know the specific motives or reasoning behind the decision, partly due to their experiences of vagueness from attending physicians.
Support for Handling Organizational and Practical Matters
Participants required assistance with various organizational and practical matters throughout their MAID trajectories, such as deciding on the ideal location and timing of performance or arranging the patient’s funeral. They also needed help with administrative tasks, e.g., completing a written MAID request to meet the legal requirement.
Participants explained that this support need partly stemmed from their desire to focus on issues that mattered more to them than organization and practical matters, such as social activities. Organizational and practical support was perceived as a way to reduce the administrative burden often experienced in MAID practice. On the other hand, some patients wished for this support to be in order with all administrative requirements as a sense of control or relief. That was more acute in relatives than patients because handling organizational and practical matters was perceived as one of their important roles since patients often lacked strength due to their general deterioration.
Discussion
Using semi-structured interviews and written narratives, we identified various support needs among patients and relatives across their MAID trajectories i.e., from the moment when the patient conceives an explicit desire for MAID till the period following the performance of MAID. Participants needed support for maximizing daily functioning (only reported by patients), making sense of the patient’s desire for MAID (only reported by relatives), managing meaningful activities, navigating existential questions, psycho-emotional regulation, facilitating social interaction, understanding the process toward MAID, and handling organizational and practical matters.
Our study suggests that MAID constitutes a multidimensional practice for patients and relatives involving various support needs throughout their MAID trajectories. These support needs essentially reflect a much broader aspiration of patients and families for definition and experience of the conditions for a good death [26–29]. Although echoing some degree of specificity in terms of context and practice – e.g., making sense of the patient’s desire for MAID and understanding the process toward MAID-most identified support needs seem to correspond to the multidimensional support needs of patients and relatives in other end-of-life trajectories [30–32]. Our findings could be seen to align with Manfred Max-Neef’s theory which states that (support) needs across individuals and practices are highly similar, as opposed to traditional theories asserting considerable variation in (support) needs [33]. Hence, an inter-professional approach can be warranted to meet the multidimensional support needs throughout the MAID trajectory as it can be challenging for a single professional to address all of these needs alone.
Our study illustrates that, in line with other dying experiences, patients and relatives experience their MAID trajectory less as a medical practice and more as a social and personal process [34, 35]. This is substantiated by our finding that participants needed support for facilitating social interaction while emphasizing their intense need for social connection and sharing their final moments throughout their MAID trajectories. The social character of MAID practice is also evident in relatives’ need for support to be engaged in the MAID trajectories, making them active participants. These results build on previous studies indicating that MAID should be equally understood and approached as a social and relational phenomenon [8, 12, 36]. This implies that the MAID trajectories of patients and relatives are partly nurtured by the dynamics and quality of their relationships, which may influence their MAID experiences considerably [12, 36]. In that way, our findings provide empirical evidence for the suggestions of Canadian scholars that MAID support would benefit from both a patient- and family-centered approach [7, 13, 37]. Furthermore, “MAID as an existential practice” is substantiated by the fact that participants needed support for navigating existential questions, managing meaningful activities, and making sense of unbearable suffering in the case of relatives. This is in keeping with the study of Tuva et al., which found that patients near the end of life longed for care focusing on “living a meaningful life” [30]. Furthermore, these support needs may result from the typical existential experiences that are often reported among patients and relatives when death is imminent [38–40]. Moreover, our participants experienced farewell rituals in their medical aid in dying trajectories as particularly meaningful. That corroborates previous research, in which relatives perceived these farewell rituals as an advantage of medical aid in dying practice as they experienced that in other end-of-life practices, they would have less room to organize them due to the unpredictable nature of the moment of death [12, 41]. Successful farewell rituals may provide individuals with emotional energy and facilitate closure [41, 42]. Furthermore, our study suggests that patients and their relatives struggle to organize and manage meaningful and meaning-making activities. A plausible reason is that such tasks might come with an emotional burden and some unfamiliarity [5].
Our study further raises the interesting question about which support model would be best suited to meet the support needs of patients and relatives in medical aid in dying practice. In line with others [7, 43, 44], we argue that a palliative care approach seems to be highly suitable, based on our findings’ alignment with the principles and goals of palliative care: 1) patients requesting medical aid in dying and relatives require support for the multidimensional needs they experience with a strong emphasis on psychological, social and existential needs; 2) an inter-professional approach is advisable to fulfill the multitude of these support needs adequately; and 3) patient-and-family centeredness appears the most appropriate approach. These requirements mean that palliative care professionals and services are well suited to address the support needs of patients and relatives in medical aid in dying practice. Thus, palliative care and medical aid in dying practice should not necessarily be viewed as opposing options but might be integrated, as in Belgium [45]. The integration of palliative care and medical aid in dying practice continues to be the subject of intense international debate [46, 47]. Our study provides empirical support in favor of this integration. We suggest that jurisdictions with (proposed) assisted dying legislation should consider in earnest to what extent and how palliative care professionals can be engaged, and organizations can be strengthened, to support patients and relatives throughout their medical aid in dying trajectories.
Limitations and Strengths
With regard to study limitations, first, some psychological adjustments and recall bias regarding earlier experiences in the medical aid in dying trajectories may be possible (e.g., because of memory limitations and emotional influences), resulting in reporting predominantly positive or negative experiences. Recall bias, may have been possible, for example, for those relatives who were included in the study during their bereaved phase or after the administration of medical aid in dying. Second, we could have missed some specific support needs of patients with terminal conditions as we mainly recruited patients with non-terminal conditions. We mitigated this by including numerous medical aid in dying experiences from relatives of patients with terminal conditions. On the other hand, various study strengths can be acknowledged. We used several strategies to enhance the rigor and trustworthiness of our findings: method triangulation, investigator triangulation, and ongoing reflection [48]. We also used a combination of semi-structured interviews and written narratives. The latter method of data collection was presented at initial contact with patients to include those more difficult to engage with an interview format, aiding inclusivity and reducing potential recruitment bias. We obtained a saturation of types of support needs arising from the lived experiences of both patients and relatives.
Implications for Clinical Practice and Future Research
First, our findings offer valuable insights that can inform healthcare professionals, educational curricula, practice tools –e.g. guidelines for medical aid in dying- and training-programs about which support needs can improve the medical aid in dying experiences and outcomes of patients and relatives. Secondly, our study provides empirical evidence for key components that should be included in a needs-oriented approach to care for or support medical aid in dying practice, such as a person-centered approach. Thirdly, healthcare professionals should pay attention to the non-medical support needs of patients and relatives, with particular attention to their social and existential needs. In this regard, promising approaches to facilitating social interaction between patients and relatives throughout their medical aid in dying trajectories may include family therapeutic methods, family group discussions, and nurse-delivered dyadic interventions [49–53]. Following this, future research could investigate the most effective type of support to fulfill the social and existential support needs of patients and relatives in medical aid in dying practice, given the current lack of research on this topic.
Conclusion
Our study reveals that patients and relatives might experience multidimensional support needs throughout their medical aid in dying trajectories. Our findings suggest that they experience their medical aid in dying trajectories as explicitly social/existential in nature. As their support needs essentially correspond with those experienced in other trajectories at the end of life, support for patients and relatives in medical aid in dying practice might benefit from a palliative care approach.
Ethics Statement
The studies involving humans were approved by the Ethics Committee of the Brussels University Hospital and Vrije Universiteit Brussel. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author Contributions
Conceptualization: SV, JC, LD, FM, KC, and SD. Methodology: SV, JG, JC, LD, FM, KC, and SD. Software: SV. Formal analysis: SV, JG, JC, LD, FM, KC, and SD. Investigation: SV, JG, JC, LD, FM, KC, and SD. Data Curation: SV. Writing–original draft: SV. Visualization: SV. Writing–review and editing: SV, JG, JC, LD, FM, KC, and SD. Supervision: JC, LD, KC, and SD. Funding acquisition: SV, JC, LD, KC, and SD. All authors contributed to the article and approved the submitted version.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. The study was funded with internal funding (Vrije Universiteit Brussel, Ghent University and Ghent University Hospital) and with funding from deMens.nu, a Flemish Humanist Organisation.
Conflict of Interest
The authors declare that they do not have any conflicts of interest.
References
1. Mroz, S, Dierickx, S, Deliens, L, Cohen, J, and Chambaere, K. Assisted Dying Around the World: A Status Quaestionis. Ann Palliat Med (2020) 9(6):3540–53. doi:10.21037/apm-20-637
2. Dierickx, S, Deliens, L, Cohen, J, and Chambaere, K. Euthanasia in Belgium: Trends in Reported Cases Between 2003 and 2013. Cmaj (2016) 188(16):E407-E414–14. doi:10.1503/cmaj.160202
3. Onwuteaka-Philipsen, BD, Brinkman-Stoppelenburg, A, Gwen, CP, De Jong-Krul, JF, Van Delden, JJM, and Van Der Heide, A. Trends in End-Of-Life Practices Before and After the Enactment of the Euthanasia Law in the Netherlands From 1990 to 2010: A Repeated Cross-Sectional Survey. Lancet (2012) 380(9845):908–15. doi:10.1016/S0140-6736(12)61034-4
4. Al, RL, Leblanc, M, Bucy, T, Ellis, LM, Hershman, DL, Meyskens, FL, et al. Trends in Medical Aid in Dying in Oregon and Washington. JAMA Netw Open (2019) 2(8):1–7. doi:10.1001/jamanetworkopen.2019.8648
5. Dees, MK, Vernooij-Dassen, MJ, Dekkers, WJ, Elwyn, G, Vissers, KC, and Van Weel, C. Perspectives of Decision-Making in Requests for Euthanasia: A Qualitative Research Among Patients, Relatives and Treating Physicians in the Netherlands. Palliat Med (2013) 27(1):27–37. doi:10.1177/0269216312463259
6. Gamondi, C, Pott, M, Preston, N, and Payne, S. Family Caregivers’ Reflections on Experiences of Assisted Suicide in Switzerland: A Qualitative Interview Study. J Pain Symptom Manage (2018) 55(4):1085–94. doi:10.1016/j.jpainsymman.2017.12.482
7. Oczkowski, SJW, Crawshaw, DE, Austin, P, Versluis, D, Kalles-Chan, G, Kekewich, M, et al. How Can We Improve the Experiences of Patients and Families Who Request Medical Assistance in Dying? A Multi-Centre Qualitative Study. BMC Palliat Care (2021) 20(1):185–12. doi:10.1186/s12904-021-00882-4
8. Martin, T, Freeman, S, Lalani, N, and Banner, D. Qualities of the Dying Experience of Persons Who Access Medical Assistance in Dying: A Scoping Review. Death Stud (2022) 0(0):1033–43. doi:10.1080/07481187.2022.2160033
9. Goldberg, R, Nissim, R, An, E, and Hales, S. Impact of Medical Assistance in Dying (MAiD) on Family Caregivers. BMJ Support Palliat Care (2019) 11:107–14. doi:10.1136/bmjspcare-2018-001686
10. Andriessen, K, Krysinska, K, Castelli Dransart, DA, Dargis, L, and Mishara, BL. Grief after Euthanasia and Physician-Assisted Suicide: A Systematic Review. Crisis (2020) 41(4):255–72. doi:10.1027/0227-5910/a000630
11. Roest, B, Trappenburg, M, and Leget, C. The Involvement of Family in the Dutch Practice of Euthanasia and Physician Assisted Suicide: A Systematic Mixed Studies Review. BMC Med Ethics (2019) 20(1):23–1. doi:10.1186/s12910-019-0361-2
12. Gamondi, C, Fusi-Schmidhauser, T, Oriani, A, Payne, S, and Preston, N. Family Members’ Experiences of Assisted Dying: A Systematic Literature Review with Thematic Synthesis. Palliat Med (2019) 33(8):1091–105. doi:10.1177/0269216319857630
13. Hales, BM, Bean, S, Isenberg-Grzeda, E, Ford, B, and Selby, D. Improving the Medical Assistance in Dying (MAID) Process: A Qualitative Study of Family Caregiver Perspectives. Palliat Support Care (2019) 17(5):590–5. doi:10.1017/S147895151900004X
14. Beuthin, R, Bruce, A, Thompson, M, Andersen, AEB, and Lundy, S. Experiences of Grief-Bereavement after a Medically Assisted Death in Canada: Bringing Death to Life. Death Stud 2021/02/05 (2021) 46:1982–91. doi:10.1080/07481187.2021.1876790
15. Smolej, E, Diab, K, Reel, K, Cameron, JI, Daubert, C, Farnum, A, et al. A Qualitative Study Exploring Family Caregivers ’ Support Needs in the Context of Medical Assistance in Dying. Palliat Support Care (2022) 1–7. doi:10.1017/S1478951522000116
16. Brooks, L. Health Care Provider Experiences of and Perspectives on Medical Assistance in Dying: A Scoping Review of Qualitative Studies. Can J Aging (2019) 38(3):384–96. doi:10.1017/S0714980818000600
17. Oczkowski, SJW, Crawshaw, D, Austin, P, Versluis, D, Kalles-Chan, G, Kekewich, M, et al. How We Can Improve the Quality of Care for Patients Requesting Medical Assistance in Dying: A Qualitative Study of Health Care Providers. J Pain Symptom Manage (2020) 61:513–21.e8. doi:10.1016/j.jpainsymman.2020.08.018
19. The Belgian Act on Euthanasia of May, 28th 2002. Eur J Health L (2003) 10(3):329–35. doi:10.2143/ep.9.2.503856
20. Federale Controle-en Evaluatiecommissie Euthanasie F. EUTHANASIE – Cijfers van 2020. (2021) Available from: https://overlegorganen.gezondheid.belgie.be/sites/default/files/documents/fcee-cijfers-2020_persbericht.pdf (Accessed November 23, 2024).
21. Asadi-Lari, M, Tamburini, M, and Gray, D. Patients’ Needs, Satisfaction, and Health Related Quality of Life: Towards a Comprehensive Model. Health Qual Life Outcomes (2004) 2:32–15. doi:10.1186/1477-7525-2-32
22. Popping, R. Analyzing Open-Ended Questions by Means of Text Analysis Procedures. BMS Bull Sociol Methodol (2015) 128(1):23–39. doi:10.1177/0759106315597389
23. Saunders, B, Sim, J, Kingstone, T, Baker, S, Waterfield, J, Bartlam, B, et al. Saturation in Qualitative Research: Exploring its Conceptualization and Operationalization. Qual Quant (2018) 52(4):1893–907. doi:10.1007/s11135-017-0574-8
24. Elo, S, and Kyngäs, H. The Qualitative Content Analysis Process. J Adv Nurs (2008) 62(1):107–15. doi:10.1111/j.1365-2648.2007.04569.x
25. Hsieh, HF, and Shannon, SE. Three Approaches to Qualitative Content Analysis. Qual Health Res (2005) 15(9):1277–88. doi:10.1177/1049732305276687
26. Zaman, M, Espinal-Arango, S, Mohapatra, A, and Jadad, AR. What Would It Take To Die Well? A Systematic Review of Systematic Reviews on The Conditions For a Good Death. Lancet Heal Longev (2021) 2(9):e593–600. doi:10.1016/S2666-7568(21)00097-0
27. Lang, A, Frankus, E, and Heimerl, K. The Perspective of Professional Caregivers Working in Generalist Palliative Care on ‘Good Dying’: An Integrative Review. Soc Sci Med (2022) 293:114647. doi:10.1016/j.socscimed.2021.114647
28. Cottrell, L, and Duggleby, W. The Good Death: An Integrative Literature Review. Palliat Support Care (2016) 14(6):686–712. doi:10.1017/S1478951515001285
29. Krikorian, A, Maldonado, C, and Pastrana, T. Patient’s Perspectives on the Notion of a Good Death: A Systematic Review of the Literature. J Pain Symptom Manage (2020) 59(1):152–64. doi:10.1016/j.jpainsymman.2019.07.033
30. Sandsdalen, T, Hov, R, Høye, S, Rystedt, I, and Wilde-Larsson, B. Patients’ Preferences in Palliative Care: A Systematic Mixed Studies Review. Palliat Med (2015) 29(5):399–419. doi:10.1177/0269216314557882
31. Higginson, IJ, Hart, S, Koffman, J, Selman, L, and Harding, R. Needs Assessments in Palliative Care: An Appraisal of Definitions and Approaches Used. J Pain Symptom Manage (2007) 33(5):500–5. doi:10.1016/j.jpainsymman.2007.02.007
32. Afolabi, OA, Nkhoma, K, Maddocks, M, and Harding, R. What Constitutes a Palliative Care Need in People with Serious Illnesses across Africa? A Mixed-Methods Systematic Review of the Concept and Evidence. Palliat Med (2021) 35(6):1052–70. doi:10.1177/02692163211008784
33. Jorge, M. Patients’ Needs and Satisfiers: Applying Human Scale Development Theory on End-Of-Life Care. Curr Opin Support Palliat Care (2010) 4(3):163–9. doi:10.1097/SPC.0b013e32833b286d
34. Patrick, DL, Engelberg, RA, and Curtis, JR. Evaluating the Quality of Dying and Death. J Pain Symptom Manage (2001) 22(3):717–26. doi:10.1016/s0885-3924(01)00333-5
35. Fernandes, CS, and Angelo, M. Family Caregivers: What Do They Need? An Integrative Review. Rev da Esc Enferm (2016) 50(4):675–82. doi:10.1590/S0080-623420160000500019
36. Variath, C, Peter, E, Cranley, L, Godkin, D, and Just, D. Relational Influences on Experiences With Assisted Dying: A Scoping Review. Nurs Ethics (2020) 27:1501–16. doi:10.1177/0969733020921493
37. Brown, J, Goodridge, D, Harrison, A, Kemp, J, Thorpe, L, and Weiler, R. Medical Assistance in Dying: Patients’, Families’, and Health Care Providers’ Perspectives on Access and Care Delivery. J Palliat Med (2020) 23(11):1468–77. doi:10.1089/jpm.2019.0509
38. Simmons, JG, Reynolds, G, Kekewich, M, Downar, J, Isenberg, SR, and Kobewka, D. Enduring Physical or Mental Suffering of People Requesting Medical Assistance in Dying. J Pain Symptom Manage (2021) 63:244–50.e2. doi:10.1016/j.jpainsymman.2021.08.010
39. Gaignard, ME, and Hurst, S. A Qualitative Study on Existential Suffering and Assisted Suicide in Switzerland. BMC Med Ethics (2019) 20(1):34–8. doi:10.1186/s12910-019-0367-9
40. Wang, T, Molassiotis, A, Chung, BPM, and Tan, JY. Unmet Care Needs of Advanced Cancer Patients and Their Informal Caregivers: A Systematic Review. BMC Palliat Care (2018) 17(1):96–29. doi:10.1186/s12904-018-0346-9
41. Buchbinder, M. Choreographing Death: A Social Phenomenology of Medical Aid-In-Dying in the United States. Med Anthr Q (2018/07/18. 2018) 32(4):481–97. doi:10.1111/maq.12468
42. Rietjens, JAC, van der Heide, A, Onwuteaka-Philipsen, BD, van der Maas, PJ, and van der Wal, G. Preferences of the Dutch General Public for a Good Death and Associations With Attitudes towards End-Of-Life Decision-Making. Palliat Med (2006) 20(7):685–92. doi:10.1177/0269216306070241
43. Wales, J, Isenberg, SR, Wegier, P, Shapiro, J, Cellarius, V, Buchman, S, et al. Providing Medical Assistance in Dying Within a Home Palliative Care Program in Toronto, Canada: An Observational Study of the First Year of Experience. J Palliat Med (2018) 21(11):1573–9. doi:10.1089/jpm.2018.0175
44. Mathews, JJ, Hausner, D, Avery, J, Hannon, B, Zimmermann, C, and Al-Awamer, A. Impact of Medical Assistance in Dying on Palliative Care: A Qualitative Study. Palliat Med (2020) 35:447–54. doi:10.1177/0269216320968517
45. Bernheim, JL, Deschepper, R, Distelmans, W, Mullie, A, Bilsen, J, and Deliens, L. Development of Palliative Care and Legalisation of Euthanasia: Antagonism or Synergy? Bmj (2008) 336(7649):864–7. doi:10.1136/bmj.39497.397257.AD
46. Bernheim, JL, and Raus, K. Euthanasia Embedded in Palliative Care. Responses to Essentialistic Criticisms of the Belgian Model of Integral End-Of-Life Care. J Med Ethics (2017) 43(8):489–94. doi:10.1136/medethics-2016-103511
47. Gerson, SM, Koksvik, GH, Richards, N, Materstvedt, LJ, and Clark, D. The Relationship of Palliative Care With Assisted Dying where Assisted Dying Is Lawful: A Systematic Scoping Review of the Literature. J Pain Symptom Manage (2020) 59(6):1287–303. doi:10.1016/j.jpainsymman.2019.12.361
48. Lincoln, YS. Emerging Criteria for Quality in Qualitative and Interpretive Research. Qual Inq (1995) 1(3):275–89. doi:10.1177/107780049500100301
49. Areia, NP, Góngora, JN, Major, S, Oliveira, VD, and Relvas, AP. Support Interventions for Families of People With Terminal Cancer in Palliative Care. Palliat Support Care (2020) 18(5):580–8. doi:10.1017/S1478951520000127
50. Northouse, LL, Mood, DW, Schafenacker, A, Kalemkerian, G, Zalupski, M, Lorusso, P, et al. Randomized Clinical Trial of a Brief and Extensive Dyadic Intervention for Advanced Cancer Patients and Their Family Caregivers. Psychooncology (2013) 22(3):555–63. doi:10.1002/pon.3036
51. Bradley, N, Lloyd-Williams, M, and Dowrick, C. Effectiveness of Palliative Care Interventions Offering Social Support to People with Life-Limiting Illness—A Systematic Review. Eur J Cancer Care (Engl) (2018) 27(3):e12837–12. doi:10.1111/ecc.12837
52. Cahill, PJ, Lobb, EA, Sanderson, C, and Phillips, JL. What Is the Evidence for Conducting Palliative Care Family Meetings? A Systematic Review. Palliat Med (2017) 31(3):197–211. doi:10.1177/0269216316658833
Keywords: euthanasia, assisted dying, support needs, patients, relatives
Citation: Vissers S, Gilissen J, Cohen J, Deliens L, Mortier F, Chambaere K and Dierickx S (2024) The Support Needs of Patients Requesting Medical Aid in Dying and Their Relatives: A Qualitative Study Using Semi-Structured Interviews and Written Narratives. Int J Public Health 69:1606878. doi: 10.3389/ijph.2024.1606878
Received: 21 November 2023; Accepted: 08 November 2024;
Published: 28 November 2024.
Edited by:
Uwe Güth, University of Basel, SwitzerlandReviewed by:
Iris Hartog, Leiden University Medical Center (LUMC), NetherlandsOne reviewer who chose to remain anonymous
Copyright © 2024 Vissers, Gilissen, Cohen, Deliens, Mortier, Chambaere and Dierickx. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kenneth Chambaere, a2VubmV0aC5jaGFtYmFlcmVAdWdlbnQuYmU=
This Original Article is part of the IJPH Special Issue “Medical Aid in Dying: A Societal Challenge”
†These authors have contributed equally to this work and share last authorship
 Stijn Vissers
Stijn Vissers Joni Gilissen1,2
Joni Gilissen1,2 Kenneth Chambaere
Kenneth Chambaere