Abstract
Objectives:
Underweight remains the primary public health concern among under-five-year-old children in Ethiopia, despite numerous government-implemented nutrition-specific and sensitive interventions. Therefore, this study aimed to assess underweight and associated factors among children in South Ethiopia.
Methods:
Between March and April 2021, 717 children in the South Ari district who were between the ages of 6 and 59 months participated in a cross-sectional study. To choose a sample of households containing a minimum of one child between the ages of 6 and 59 months, a multi-stage sampling procedure was used. Data were collected by interviewer-administered structured questionnaires from the mothers of the children. To determine the factors associated with being underweight, a binary logistic regression analysis was built. All variables with a p-value <0.25 in the bivariable analysis were entered into a multivariable logistic regression analysis. To assess the strength of the association, an adjusted odds ratio (AOR) with a 95% confidence interval was used. With a p-value below 0.05, statistical significance was declared.
Results:
The prevalence of underweight was determined to be 29.7% (95% CI: 26.5%, 33.2%). Child age 6–23 months [adjusted odds ratio (AOR) = 0.28; 95% confidence interval (CI): 0.18, 0.44], food insecurity (AOR = 1.48; 95% CI: 1.04, 2.10), sub-optimal child dietary diversity (AOR = 1.44; 95% CI: 1.01, 2.03), birth interval <24 months (AOR = 2.49; 95% CI: 1.75, 3.54), and common childhood illness (AOR = 2.21; 95% CI: 1.52, 3.21) were associated with being underweight.
Conclusion:
Underweight among children is predicted by household food insecurity, suboptimal dietary diversity, and common childhood illnesses, necessitating further efforts to improve food security and manage common illnesses.
Introduction
Undernutrition is a type of malnutrition that results from deficiencies in an individual’s intake of energy and deficiencies in vitamins and minerals, and it includes being underweight, stunting, and wasting. Undernutrition makes under-five children much more susceptible to morbidity and mortality [1]. Being undernourished during childhood may continue up to preschool age and adulthood and result in poor school performance and weak immune systems [2]. Underweight is characterized as a lower weight-for-age, an indicator of the overall population’s nutritional status, and is a combination of both stunting and wasting [3].
Even though the prevalence of underweight among children less than 5 years of age decreased globally between 1990 and 2019, from 24.8% to 13%, it remained a significant public health issue [4]. Globally, 149 million children under five were projected to be stunted and forty-five million to be wasted in 2020 [1]. In Sub-Saharan African countries about 39.9% of children under 5 years who are affected by undernutrition are underweight and this is the highest burden of underweight among these age groups [5]. Evidence from Ethiopian Demographic and Health Surveys (EDHS) revealed that the occurrence of underweight decreased from 33% in 2011 to 21% in 2019 [6]. In Ethiopia, different previous studies revealed different proportions for underweight extending from 5 percent to 32 percent [7, 8].
Underweight has a substantial effect on the health, development, and wellbeing of children whose age is less than 5 years [9]. Children, who experienced undernutrition, were at high risk of reduced cognitive development which leads to poor academic performance, reduced school admission, and absenteeism; this in turn results in abridged productivity during the time of adulthood [10]. According to evidence from the World Health Organization (WHO), malnutrition is considered the single most important risk to the health of the world’s population [11].
Evidence from previous studies revealed that several factors contributed to being underweight among 6–59 months-aged children. Factors including child age, maternal education, family size, gender, maternal occupation, household wealth index, food insecurity, and poor child dietary diversity were associated with being underweight [12–16].
To alleviate this significant public health problem, different interventions were applied. Ethiopia’s government aspires to guarantee that all people have year-round access to safe, nutritious foods and to eradicate all types of malnutrition. Ethiopia has adopted some Nutrition-Sensitive Agriculture [17] measures to enhance children’s and women’s nutritional status by improving the quality and quantity of available, accessible, and inexpensive food and promoting the use of nutritious, diverse, and safe foods for all citizens every time [18]. South Ari Zone is a home to pastoralists, semi-pastoralists, and agrarians. South Ari district is among the areas where agrarians live. According to the zone’s report, malnutrition (acute and chronic) among children was the leading cause of admission to health facilities in the district even though the district was known for having a high vegetable, fruit, and crop production when compared to the zone’s semi-pastoralist and pastoralist districts [19, 20].
Despite the solutions tried, the problem is still evident and studies recommended frequent research to understand the trend of the prevalence of underweight and associated factors [21]. Therefore, the purpose of this study was to determine the prevalence of underweight among children between the ages of six and 59 months in the South Ari district, South Ethiopia, as well as the associated factors.
Methods
Study Area, Period, and Design
A community-based cross-sectional survey was conducted in the South Ari district from 11 March 2021 to 11 April 2021. South Ari district is 767 km from Addis Abeba, the country’s capital, and 17 km from Jinka, the administrative center of the South Ari hub. The district has 31 kebeles (small administrative units or neighbourhoods), out of which 2 are Kolla (lowland), 23 are Woina dega (mid-highland), and 6 are Dega (highland) [20]. The Kolla represents areas below 1,500 m, the Dega includes highlands over 2,300 m, and the Woina-Dega includes areas between 1,500 and 2,300 m. The district’s predicted population for 2020 is 160,896, with 25,121 children under the age of five, according to the Ethiopian Census 2007. There are 22,429 children aged between six and 59 months among the under-five population. The district is primarily rural and economically dependent on agriculture, with important crops including grains, pulses, cassava, fruits, sweet potatoes, and false banana. The main cash crops in the area are teff, maize, and fruits [20].
Population
All of the South Ari district’s households with children between the ages of 6 and 59 months were included as the source population. All the households in the district that were randomly selected and had children between the ages of 6 and 59 months and who had lived in the study setting for at least 6 months were included in the study. Children diagnosed with severe acute malnutrition, those enrolled in a therapeutic feeding program, and mothers and other primary caregivers who were unable to participate in an interview owing to illness were all excluded from the study.
Sample Size Determination and Sampling Procedure
The sample size was determined using the single population proportion formula by considering the following assumptions: a 95% level of confidence with a confidence level of Za/2 = 1.96, a prevalence of underweight of 27.6% taken from a study done in Dessie, Northwest Ethiopia [22], and a 4% margin of error. Using the above assumptions and a 1.5 design effect, the sample size was calculated to be 720, and after adding a 5% non-response rate, the final determined sample size used to conduct the study was 756.
The study subjects were chosen using a multi-stage sampling process. First, 31 kebeles in the district were classified as Kolla (n = 2), Woina Dega (n = 23), and Dega (n = 6) agroecological zones. Then, using the lottery approach, ten kebeles (one from Kolla, seven from Woina Dega as well as two from Dega) were chosen for the study. The family folder was used to obtain information on households having children aged six up to 59 months. A list of eligible households was created for each of the kebeles and then exported into the Emergency Nutrition Assessment software for random selection. The number of households from each kebele that were included in the study was determined by a proportional allocation to size based on the total number of eligible households living in the kebele. Only one child was chosen using the lottery procedure in selected households with more than one eligible child (Figure 1).
FIGURE 1
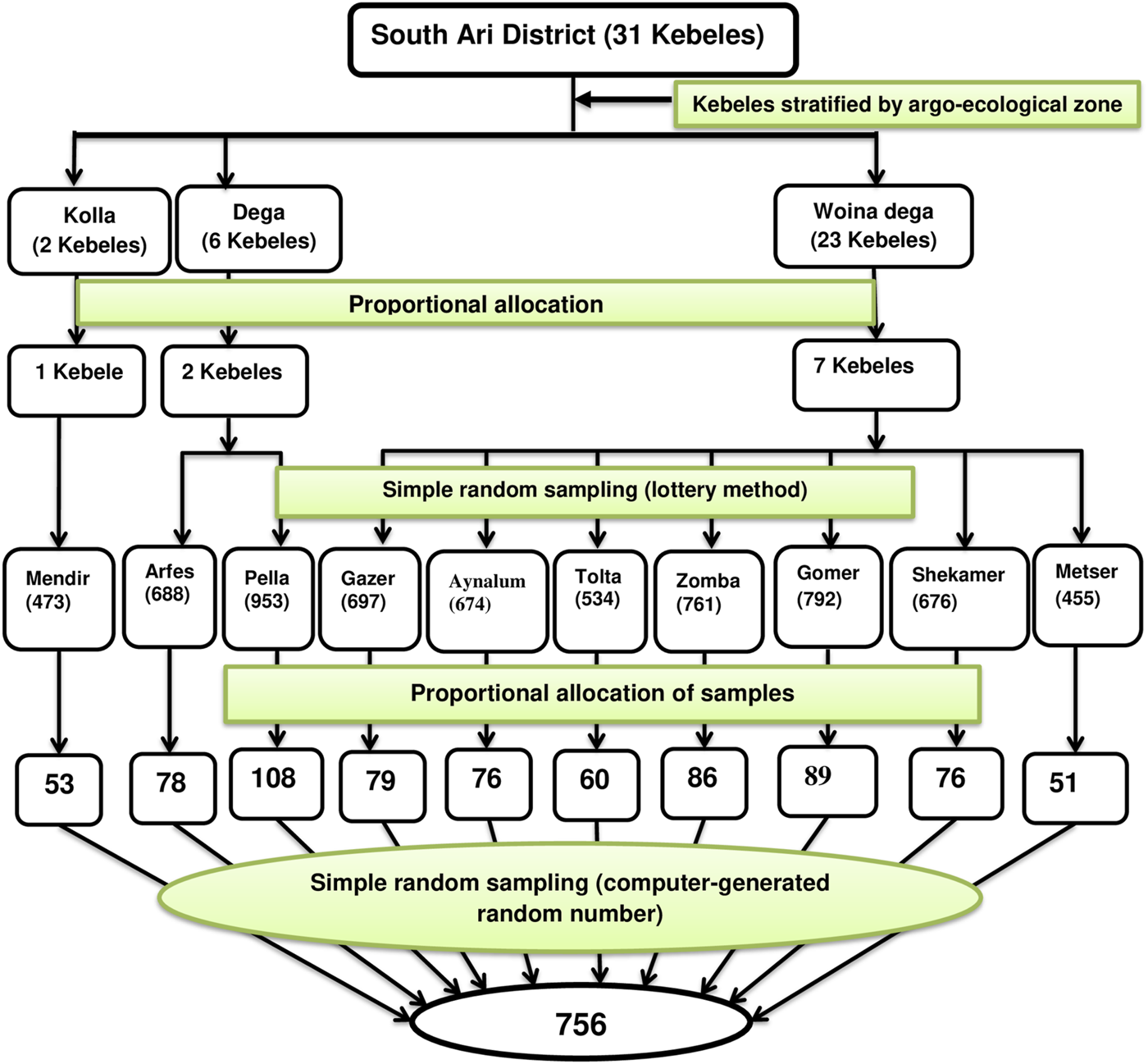
Schematic representation of the sampling procedure to assess underweight and associated factors among children aged 6–59 months in South Ari District, South Ethiopia, 2021: A community-based cross-sectional study.
Study Variables
Underweight among 6–59 month-old children was the dependent variable. Socio-demographic and socio-economic variables such as sex, age, family size, marital status, household wealth index, mother’s employment status, mother’s educational status, household food security status, and father’s education; maternal characteristics like maternal knowledge on child feeding, antenatal care visit, and place of delivery; and child factors like colostrum feeding, complementary feeding initiation age, time of breastfeeding initiation, bottle feeding, pre-lacteal feeding, dietary diversity, non-exclusive breastfeeding, immunization, birth order, birth interval, common childhood illness (fever, diarrhoea, cough) were independent variables.
Data Collection Procedure and Instrument
A structured tool was developed first in English before being translated into Amharic, and finally back into English by many translators to check consistency. The data collection tool contains socio-economic, socio-demographic, household food insecurity, maternal and child factors, and anthropometric measurements. Training for data collectors and supervisors included a demonstration of anthropometric measurements for 2 days. Data collection including anthropometric measurements was conducted by ten experienced diploma nurses and one health extension practitioner from each selected Kebele. The data collection process was supervised by 2 health officers. Data were collected from the mothers of the children but if the child had no mother then the head of the households were interviewed.
Measurements and Operational Definitions
Household Food Insecurity Measurement
Food security status: Was measured using the Household Food Insecurity Access Scale and categorized as food secure or food insecure. Food secure: If the household experienced none of the food insecurity (access) conditions or just experienced worry, but rarely, whereas food insecure if households are mildly, moderately, or severely food insecure. Households are categorized as mildly food insecure if they worry about not having enough food sometimes or often, and/or households are unable to eat preferred foods, and/or they eat a more monotonous diet than desired, and/or some foods are considered undesirable, but only rarely, and they do not experience the three most severe conditions (running out of food, going to bed hungry, or going a whole day and night without eating), while households with moderate food insecurity tend to compromise quality more frequently by eating uninteresting foods or a monotonous diet sometimes or often, as well as by beginning to reduce their meal size or frequency, rarely or sometimes. But it does not experience one of the three severe conditions. Severely food insecure: any household that experiences one of these three conditions even once in the last 4 weeks (30 days) is considered severely food insecure or has experienced cutting back on meal size or the number of meals often, and/or experiences any of the three most severe conditions (running out of food, going to bed hungry, or going a whole day and night without eating), even as infrequently as rarely [23, 24].
Anthropometric Measurement
Children were dressed simply and without shoes while having their weight measured using a portable Seca digital balance to the nearest 0.1 kg. For younger children (6–23 months), the mother and kid were weighed together, the mother individually, and then the child’s weight was calculated by using the tare function to deduct the mother’s weight from the total weight. Before weighing each infant, the scale was adjusted by turning it to zero. Additionally, a known-weight object was used every day to check the weighing scale’s accuracy. The technical error of measures was calculated to reduce anthropometric measurement mistakes. Ten children’s weights were measured twice each to determine the technical error of measurement (TEM) by the primary investigator, who also allowed the data collectors to measure each child twice. Then, a computer program called Emergency Nutrition Assessment (ENA for SMART) was employed.
Underweight was measured by weight-for-age and if children’s weight-for-age is < −2 standard deviations of the WHO Child Growth Standards median the child was classified as underweight [25].
Child Dietary Diversity
A 24-h dietary recall method was employed to assess child dietary diversity score (DDS) by using a standardized tool containing seven food groups (grains, roots, and tubers, legumes and nuts, dairy products, flesh foods, eggs, vitamin A rich fruits and vegetables, and other fruits and vegetables). Accordingly, the mothers of the children were asked to report the food types consumed by the child in the last 24 h before the data collection date. If the child consumed four or more of the seven food groups, it was regarded as optimal DDS; otherwise, the child was considered to have sub-optimal DDS [26].
Maternal Dietary Diversity
Standardized tool containing ten defined food groups (grains, white roots, and tubers, plantains, pulses, nuts and seeds, dairy, meat, poultry, fish, eggs, dark green leafy vegetables, other vitamin A-rich fruits and vegetables, other vegetables, and other fruits) using 24-h recall method. Accordingly, the mother was asked to report the consumed food group in the previous 24 h. If the mother consumed a minimum of five out of ten defined food groups in the earlier day or night, then the mother was considered to have a high diversity score; otherwise, the mother was considered to have Low DDS [27].
Wealth Index
Using easily obtainable information on a household’s possession of a certain 26 types of assets, the wealth index was created [28]. It was produced using principle components analysis (PCA), a statistical technique. The wealth index measures the relative wealth of households, with each asset scored using a factor from PCA. Asset scores normalized to a mean of 0 and standard deviation of 1 were used to create breakpoints to divide the wealth index into poor, medium, and rich categories.
Maternal Knowledge of Child Feeding
Assessed using 12-item questions having yes/no responses. A score of one was given for each correctly answered question and a score of zero for each wrong one. Mothers who scored beyond the mean (six) were categorized as having “adequate knowledge,” while, those who scored the mean and lower were categorized as having “inadequate knowledge” [29, 30].
Data Processing and Analysis
The collected data were checked, entered into Epi-Data 3.1, and then exported to STATA version 14.0 for further management and analysis. According to each variable’s kind, descriptive statistics like; frequency, proportion, mean, median, and standard deviations were computed. After checking the assumptions, the wealth index was computed using PCA and ranked by tertile. To determine underweight status, anthropometric measurements were converted to weight-for-age z-score (WFA) by WHO Anthro software version 3.2.2 using the WHO 2006 child growth standard.
To determine the association between underweight and independent variables, a binary logistic regression analysis model was fitted. All variables with a p-value <0.25 in the bivariable analysis were entered into a multivariable logistic regression analysis. Multicollinearity was checked using the variance inflation factor and tolerance. The maximum observed value of the variance inflation factor was 1.03, showing no risk of collinearity. A backward stepwise method was used to fit the final multivariable logistic regression model. At a p-value below 0.05, statistical significance was declared. To assess the significance of the association, a 95% confidence interval and an adjusted odds ratio (AOR) were used. To check the goodness of fit of the model, the Hosmer-Lemeshow test statistics (p-value = 0.21) were used.
Results
Socio-Demographic and Economic Characteristics
A 95% response rate was attained from the 717 respondents who were successfully questioned. Of the study participants, 385 (53.7%) children were male, and 499 (69.6%) children were between the ages of 24 and 59 months. In terms of wealth index, nearly one-third of children came from low-wealth index households. Regarding food security status, 55.2% of children came from food-secure households while 8.6%, 16.3%, and 19.8% of the children who participated in the study were from households with severe, moderate, and mild food insecurity, respectively. More half (55.1%) of the household heads were aged 25–34 years, and 406 (56.6%) of the household heads were men. Among household heads, 164 (22.9%) had not attended formal education. The majority of the mothers, 624 (87%), were married, and 525 of them—or 73.2%—were protestant. Regarding ethnicity, 650 (90.7%) of the participants were Ari by ethnicity, and nearly 42% of the mothers did not attend formal education. Three hundred-seventeen (44.2%) of the mothers were farmers as well as 241 (33.6%) mothers aged 25- to 29-year-old. The majority of the male respondents were farmers 485 (67.9%), and 155 (21.7%) of the fathers had not attended formal education. Ninety (12.6%) of the respondents had families with eight or more members (Table 1).
TABLE 1
| Variables | Frequency (N) | Percent (%) | |
|---|---|---|---|
| Child Age | 6–23 months | 218 | 30.4 |
| 24–59 months | 499 | 69.6 | |
| Sex of child | Male | 385 | 53.7 |
| Female | 332 | 46.3 | |
| Household head age (in years) | 15–24 | 32 | 4.5 |
| 25–34 | 395 | 55.1 | |
| ≥35 | 290 | 40.4 | |
| Household head educational status | No formal education | 164 | 22.9 |
| Primary education | 335 | 46.7 | |
| Secondary education and above | 218 | 30.4 | |
| Maternal Age (in years) | 15–19 | 2 | 0.3 |
| 20–24 | 151 | 21.1 | |
| 25–29 | 241 | 33.6 | |
| 30–34 | 140 | 19.5 | |
| ≥35 | 183 | 25.5 | |
| Marital status | Single | 70 | 9.8 |
| Married | 624 | 87.0 | |
| Widowed | 8 | 1.1 | |
| Divorced | 15 | 2.1 | |
| Religion | Orthodox | 171 | 23.8 |
| Protestant | 525 | 73.2 | |
| Muslim | 10 | 1.4 | |
| Catholic | 7 | 1.0 | |
| Others* | 6 | 0.6 | |
| Ethnicity | Ari | 650 | 90.6 |
| Amhara | 63 | 8.8 | |
| Woliata | 2 | 0.3 | |
| Goffa | 2 | 0.3 | |
| Maternal education | No formal education | 300 | 41.8 |
| Primary education | 286 | 39.9 | |
| Secondary education and above | 131 | 18.3 | |
| Maternal occupation | Farmer | 317 | 44.2 |
| Government employee | 278 | 38.8 | |
| Daily labourer | 34 | 4.7 | |
| Merchant | 51 | 7.1 | |
| No work | 30 | 4.2 | |
| Others** | 7 | 1.0 | |
| Father’s education (n = 714) | No formal education | 155 | 21.7 |
| Primary education | 332 | 46.5 | |
| Secondary education and above | 227 | 31.8 | |
| Father’s occupation (n = 714) | Farmer | 485 | 67.9 |
| Government employee | 94 | 13.2 | |
| Daily labourer | 60 | 8.4 | |
| Merchant | 63 | 8.8 | |
| No work | 12 | 1.7 | |
| Family size | 2–4 | 309 | 43.0 |
| 5–7 | 318 | 44.4 | |
| ≥8 | 90 | 12.6 | |
| Household Wealth Index | Poor | 239 | 33.3 |
| Medium | 261 | 36.4 | |
| Rich | 217 | 30.3 | |
| Food security status | Food secure | 396 | 55.2 |
| Food insecure | 321 | 44.8 | |
| Degree of food security status | Food secure | 396 | 55.2 |
| Mildly food insecure | 142 | 19.8 | |
| Moderately food insecure | 117 | 16.3 | |
| Severely food insecure | 62 | 8.7 | |
Socio-demographic and economic characteristics of children (6–59 months) in South Ari District, South Ari Zone, South Ethiopia, 2021: A community-based cross-sectional study (N = 717).
Note: *Only Jesus, Pagan; **Housewife, Student.
Nutrition-Related Characteristics
Of the children, 128 (17.9%), 136 (19.0%), and 112 (15.6%) reported having diarrhoea, cough, and fever in the 2 weeks before the study, respectively. More than ninety percent of children (660 – or – 92.1%) and (684 – or – 95.4%), began to breastfeed timely and were given colostrum, respectively. About one-third of children (27.9%) received non-exclusive breastfeeding, whereas 118 (16.5%) received pre-lacteal feeding. More than nine in ten children, 668 (93.3%), started complementary feeding 6 months and above, while 238 (33.2%) of them were still breastfeeding. More than ninety percent of children (659 – or – 91.9%), were vaccinated, and 351 (49.0%) of the mothers bottle-fed their infants. More than half of the children—384 (53.6%)—had birth intervals of 24 months or longer, and more than a quarter—193 (26.9%)—had birth orders of 4 or higher. Nearly two-fifths (42.8%) of the children had suboptimal dietary diversity scores, according to the study. The majority of mothers—654 or 91.2%—had delivered their child at a healthcare facility, and about eighty percent of them got four or more antenatal care checkups. Out of the respondents, 613 (85.5%) mothers had adequate knowledge of child-feeding practices. A high dietary diversity score of the mother was achieved by 532 (74.2%) of the participants or nearly three-fourths of them (Table 2).
TABLE 2
| Variables | Frequency (N) | Percent (%) | |
|---|---|---|---|
| Antenatal care follow-up | No | 30 | 4.2 |
| 1–3 | 116 | 16.2 | |
| ≥4 | 571 | 79.6 | |
| Place of delivery | Home | 63 | 8.8 |
| Health institution | 654 | 91.2 | |
| Maternal knowledge on child feeding practice | Adequate | 613 | 85.5 |
| Inadequate | 104 | 14.5 | |
| Maternal dietary diversity score (MDDS) | High MDDS | 532 | 74.2 |
| Low MDDS | 185 | 25.8 | |
| Cough in the past 2 weeks | Yes | 136 | 19.0 |
| No | 581 | 81.0 | |
| Diarrhea in the past 2 weeks | Yes | 128 | 17.9 |
| No | 589 | 82.1 | |
| Fever in the past 2 weeks | Yes | 112 | 15.6 |
| No | 605 | 84.4 | |
| Early initiation of breastfeeding | Yes | 660 | 92.1 |
| No | 57 | 7.9 | |
| Colostrum feeding | Yes | 684 | 95.4 |
| No | 33 | 4.6 | |
| Non-exclusive breastfeeding | Yes | 200 | 27.9 |
| No | 517 | 72.1 | |
| Currently on breastfeeding | Yes | 238 | 33.2 |
| No | 479 | 66.8 | |
| Age at initiation of complementary feeding (n = 716) | Before 6 months | 48 | 6.7 |
| 6 months and above | 668 | 93.3 | |
| Immunization status | Vaccinated | 659 | 91.9 |
| Unvaccinated | 58 | 8.1 | |
| Birth interval | <24 months | 333 | 46.4 |
| ≥24 months | 384 | 53.6 | |
| Birth order | First | 220 | 30.7 |
| 2–3 | 304 | 42.4 | |
| 4 and above | 193 | 26.9 | |
| Child dietary diversity score (DDS) | Optimal | 410 | 57.2 |
| Sub-optimal | 307 | 42.8 | |
Maternal and child nutrition-related characteristics in South Ari District, South Ethiopia, 2021: A community-based cross-sectional study (N = 717).
Abbreviations: MDDS, maternal dietary diversity score; DDS, Child Dietary Diversity Score.
Prevalence of Underweight
This study attested that the prevalence of underweight among children aged six up to 59 months in the study setting was 29.7% (95% CI: 26.5%, 33.2%) (Figure 2).
FIGURE 2
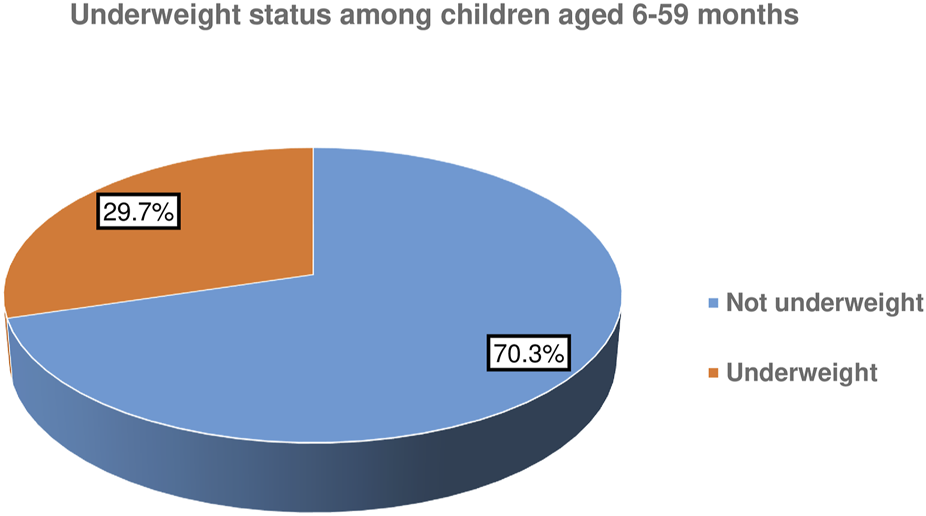
Underweight status of children aged 6–59 months in South Ari district, South Ethiopia, 2021: A community-based cross-sectional study.
Factors Associated With Underweight
In the bivariable logistic regression analysis, the age of the child, sex of the child, marital status, family size, wealth index, food security status, Maternal DDS, antenatal care visit, child DDS, birth interval, age of complementary feeding initiation, bottle feeding, early breastfeeding initiation, immunization status, and common childhood illnesses history were associated with being underweight. In the multivariable logistic regression model, after controlling confounding variables, child sex, age of the child, child DDS, food security status, birth interval, and common childhood illness were factors associated with underweight at p-value<0.05. Children residing in food-insecure households have 1.48 times increased odds of being underweight compared to their counterparts (AOR = 1.48; 95% CI: 1.04, 2.10). The likelihood of being underweight among children with sub-optimal dietary diversity is 1.44 times higher compared to those with optimal dietary diversity (AOR = 1.44; 95% CI: 1.01, 2.03). Children with a history of at least one of the common childhood illnesses in the earlier 2 weeks were two times more at risk of being underweight compared to their complements (AOR = 2.21; 95% CI: 1.52, 3.21) (Table 3).
TABLE 3
| Variables | Underweight status | COR (95% CI) | AOR (95% CI) | p-value | ||
|---|---|---|---|---|---|---|
| Yes (%) | No (%) | |||||
| Age of the household head (in years) | 15–24 | 7 (1.0) | 25 (3.5) | 0.83 (0.35, 2.00) | 0.82 (0.30, 2.24) | 0.69 |
| 25–34 | 133 (18.6) | 262 (36.5) | 1.51 (1.08, 2.11) | 1.32 (0.91, 1.93) | 0.14 | |
| ≥35 | 73 (10.2) | 217 (30.3) | 1 | 1 | ||
| Age of the child (in Months) | 6–23 | 30 (4.2) | 188 (26.2) | 0.28 (0.18, 0.42) | 0.28 (0.18, 0.44) | <0.001 |
| 24–59 | 183 (25.5) | 316 (44.1) | 1 | 1 | ||
| Sex of the child | Male | 105 (14.6) | 280 (39.1) | 1 | 1 | |
| Female | 108 (15.1) | 224 (31.2) | 1.29 (0.93, 1.77) | 1.43 (1.01, 2.02) | 0.04 | |
| Marital status | In union | 192 (26.8) | 432 (60.3) | 1 | 1 | |
| Not in union | 21 (2.9) | 72 (10.0) | 0.66 (0.39, 1.10) | 0.72 (0.41, 1.24) | 0.23 | |
| Family size (in number) | 2–4 | 95 (13.3) | 214 (29.9) | 1 | 1 | |
| 5–7 | 97 (13.5) | 221 (30.8) | 0.99 (0.70, 1.39) | 1.34 (0.89, 2.02) | 0.16 | |
| ≥8 | 21 (2.9) | 69 (9.6) | 0.69 (0.40, 1.18) | 0.98 (0.52, 1.85) | 0.94 | |
| Wealth index | Poor | 87 (12.1) | 152 (21.2) | 1.86 (1.24, 2.81) | 1.30 (0.81, 2.08) | 0.28 |
| Medium | 75 (10.5) | 186 (25.9) | 1.31 (0.87, 1.98) | 0.97 (0.62, 1.52) | 0.89 | |
| Rich | 51 (7.1) | 166 (23.2) | 1 | 1 | ||
| Food security status | Food secure | 103 (14.4) | 293 (40.9) | 1 | 1 | |
| Food insecure | 110 (15.3) | 211 (29.4) | 1.49 (1.07, 2.05) | 1.48 (1.04, 2.10) | 0.03 | |
| Maternal dietary diversity score | Low | 65 (9.1) | 120 (16.7) | 1.41 (0.98, 2.01) | 1.14 (0.74, 1.75) | 0.55 |
| High | 148 (20.6) | 384 (53.6) | 1 | 1 | ||
| Antenatal care follow-up | <4 times | 55 (7.7) | 91 (12.7) | 1.58 (1.08, 2.31) | 1.47 (0.96, 2.24) | 0.07 |
| ≥4 times | 158 (22.0) | 413 (57.6) | 1 | 1 | ||
| Child dietary diversity score | Sub-optimal | 108 (15.1) | 199 (27.8) | 1.58 (1.14, 2.18) | 1.44 (1.01, 2.03) | 0.04 |
| Optimal | 105 (14.6) | 305 (42.5) | 1 | 1 | ||
| Birth interval | <24 months | 132 (18.4) | 201 (28.0) | 2.46 (1.77, 3.41) | 2.49 (1.75, 3.54) | <0.001 |
| ≥24 months | 81 (11.3) | 303 (42.3) | 1 | 1 | ||
| Age of complementary feeding initiation | Before 6 months | 8 (1.1) | 40 (5.6) | 0.45 (0.21, 0.98) | 0.61 (0.27, 1.40) | 0.24 |
| 6 months and above | 205 (28.6) | 463 (64.7) | 1 | 1 | ||
| Bottle feeding | Yes | 94 (13.1) | 257 (35.8) | 0.76 (0.55, 1.05) | 0.79 (0.55, 1.12) | 0.18 |
| No | 119 (16.6) | 247 (34.5) | 1 | 1 | ||
| Early initiation of breastfeeding | Yes | 201 (28.0) | 459 (64.0) | 1 | 1 | |
| No | 12 (1.7) | 45 (6.3) | 0.61 (0.32, 1.18) | 0.81 (0.39, 1.69) | 0.58 | |
| Non-exclusive breastfeeding | Yes | 46 (6.4) | 154 (21.5) | 0.63 (0.43, 0.91) | 0.74 (0.49, 1.12) | 0.15 |
| No | 167 (23.3) | 350 (48.8) | 1 | 1 | ||
| Immunization status | Vaccinated | 190 (26.5) | 469 (65.4) | 1 | 1 | |
| Unvaccinated | 23 (3.2) | 35 (4.9) | 1.62 (0.93, 2.82) | 1.46 (0.77, 2.75) | 0.24 | |
| Common childhood illness | Yes | 84 (11.7) | 105 (14.6) | 2.47 (1.75, 3.51) | 2.21 (1.52, 3.21) | <0.001 |
| No | 129 (18.0) | 399 (55.7) | 1 | 1 | ||
Bivariable and multivariable regression analysis to assess factors associated with underweight among children aged 6–59 months in South Ari district, South Ethiopia, 2021: A community-based cross-sectional study (n = 717).
Discussion
The prevalence of underweight was 29.7% among children aged 6 upto 59 months in the District. Child age, being female, household food insecurity, children’s sub-optimal dietary diversity, <24 months birth interval, and having common childhood illness were the identified predictors of being underweight.
The prevalence of underweight was determined to be 29.7% by this study. This finding is in line with previously conducted studies in Ethiopia, which reported a prevalence of underweight ranging from 21.7% to 27.6% [15, 22, 31]. This finding is lower than studies done in Bangladesh (43%) [32] and Yemen (46.2%) [33]. On the contrary, the finding of the current study is higher than studies conducted in different regions of Ethiopia, which reported an underweight prevalence ranging from 13.5% to 19.95% [13, 16, 34, 35]. In addition, evidence from the current study is higher than studies done in Vietnam (11.4%) [36], Khyber Pakhtunkhwa (8.4%) [37], and Sub-Saharan Africa (16.3%) [5]. The possible reasons for the disparities between studies might be due to variations in study settings, socio-demographic and economic characteristics, topography as well as cultural differences in the caring and feeding practice of children, and developmental differences. Another likely reason might be that nearly half participants from the current study setting lived in a food-insecure area with a sub-optimal dietary diversity score among children, minimizing the frequency of feeding and making it difficult to provide diversified food. This finding implies that much work is needed to attain the SDG target 2.2 of ending all forms of malnutrition including underweight by 2030.
In this study, it was identified that children aged six upto 23 months had a reduced risk of being underweight compared to those aged 24–59 months. This may be explained by the reason that, as a child gets older they might be put on a family diet and may experience inadequate dietary intake (poor diet), despite increased caloric need for growth and development. Furthermore, as the child gets older, they might be prone to poor sanitation and hygiene and increased risk of infections including intestinal parasites, which might result in the vicious cycle of malnutrition. On the other hand, children aged 6 up to 23 months might be on complementary feeding, and this can help them get a chance to consume more vitamin-A-rich fruits, dairy products, and vegetables which can significantly lower the likelihood of being underweight.
As revealed by this study, sex is another socio-demographic factor that is significantly associated with being underweight. The risk of being underweight is higher among female children than males. The possible reason may be due to the fact that in the current study, there is a higher preference for male sex and families are highly concerned about their male child’s health and nutrition. This might prone female children to be more underweight when compared to their complement.
In this study, household food insecurity is associated with being underweight is household food insecurity. Children from food insecure households had an increased risk of being underweight than their counterparts. This finding is supported by evidence from studies conducted in different parts of Ethiopia: Northern Shewa Zone [16], Sekela District, Western Ethiopia [38], East Badawacho District [39], Semen Bench District [12], Nepal [40], Bangladesh and Vietnam [41]. Furthermore, sub-optimal dietary diversity of children is significantly associated with being underweight. The finding of this study is in line with studies conducted in the Semen Bench district, Ethiopia [12], Tanzania [42], and India [43] which stated that children who consumed less than four of the major food groups from seven food groups were more likely to develop underweight when compared to their complements. Children from food-insecure households might have insufficient access to diversified daily food intakes, which could result in an increased risk of being underweight. Moreover, household food insecurity might affect the availability and utilization of optimal dietary intake and might expose to increased risk of both macro- and micronutrient deficiencies, resulting in malnutrition (underweight).
The current study identified that birth interval is significantly associated with being underweight. This is supported by findings from India [44], China [45], and Sub-Saharan Africa [46]. This finding might be explained by having fewer birth intervals could increase the sharing of food among siblings and affect the quality care and duration of breastfeeding for the index child. Besides, fever birth interval might lead to decreased nutrient reserve for the mother, which exposes to intrauterine growth restriction and being underweight after birth because of the intergenerational effect of malnutrition.
Moreover, having at least one common childhood illness history is associated with being underweight as revealed by this study. The possible reason could be that children with illnesses like diarrhoea, pneumonia, and fever can have reduced apatite, which results in inadequate dietary intake, weight loss, lowered immunity, mucosal damage, and impaired growth and development, which exposes them to being underweight. Malnutrition, in general, can increase a person’s vulnerability to illness, and infection can also contribute to malnutrition, implying a vicious cycle of malnutrition and infection [47].
The finding of this study highlights that policymakers and programmers should give due emphasis to the reduction of malnutrition especially underweight for attaining SDG 3 through comprehensive implementation of interventions addressing identified factors.
The study has some limitations. It might be difficult to see the cause-effect relationship because of the character of the cross-sectional study design. Even though the due emphasis was given to reminding past events by linking them with usual events, there might be some recall bias among participants when assessing common childhood illness, twenty-four-child dietary diversity recall, 1-month household food security recall, and breastfeeding patterns. The standard tools used to assess food insecurity and dietary diversity cannot indicate the seasonal difference that happened over a year. The effect of some important variables like father’s knowledge on child feeding practice. Though emphasis like intensive practical training on anthropometric measurement, pretesting, calibration of instruments, standardizing measurement, computing TEM, and active supervision of field data collection to minimize bias was given, there might be measurement error.
Policy and Program Implication
The Ethiopian government launched the Seqota Declaration, a high-level commitment to end malnutrition among children by 2030 [48]. Despite this major collaborative platform, the present study finding indicated that the prevalence of underweight was high among children aged 6–59 months due to different factors. The findings of the current study are important for policy, program, and practice in the district, aligning with the second goal of the SDGs, which focuses on nutrition [49] and the World Health Assembly’s (WHA) six global nutrition targets focus on maternal, infant, and young children nutrition to be achieved between 2012 and 2025 [50]. Hence, the finding highlights that policymakers and programmers should give due emphasis to the reduction of malnutrition, especially underweight, for attaining SDG 2 and WHA targets through comprehensive implementation of nutrition-sensitive and specific interventions addressing identified factors. In addition, this public health problem requires integrated and consistent interventions from the district, zonal, regional health bureau, and other stakeholders to achieve the Ethiopian national commitment to end undernutrition among children. Non-governmental organizations need to give due attention to malnutrition screening to detect the underweight as early as possible, and intervention programs to control the prevalence of underweight among children aged 6–59 months. Furthermore, designing health policy should be considered to improve household food security status, ensure consumption of diversified diet among under-five children, and prevent common childhood illnesses that are contributors of underweight to enhance the normal growth of the children.
Conclusion
In this study, underweight was determined to be a significant public health concern in the district. Child age, being female, household food insecurity, children’s sub-optimal dietary diversity, fewer birth intervals, and having common childhood illnesses were the identified factors of being underweight. Hence, additional effort to improve household food security and feed children a diversified diet is required with due attention given to female children and children 24–59 months. Moreover, strengthening integrated management of common childhood illnesses and child care is highly demanding. More well-designed longitudinal studies are needed to guide efficient interventions that address food insecurity and underweight.
Statements
Ethics statement
Ethical clearance was obtained from the Arba Minch College of Health Sciences Institutional Review Board (reference number=AMCHS/01/20/7028). The South Ari District Health Office, the South Ari Zone Health Department, and other relevant organizations provided formal official letters. Informed consent was obtained from the mothers or the head of the household (other primary caregivers of the children). The study was conducted in a private, anonymous, and confidential manner at all times. Mothers or caregivers were made aware of their freedom to refuse consent at any moment and to leave the study. Underweight children were referred to the closest health facility, while families experiencing food insecurity were referred to the Agricultural and Rural Development Office. All of the study’s operations were carried out in compliance with the Helsinki Declaration’s ethical declaration.
Author contributions
TT conceived the study and contributed to the work in study design, execution, data analysis, interpretation, report writing, and drafting of the manuscript. KA, RA, BK, and KT were involved in the conception, design, data analysis, and revising of the manuscript. TG contributed to the work in study design, execution, data analysis, interpretation, report writing, and drafting of the manuscript. All authors contributed to the article and approved the submitted version.
Acknowledgments
We express gratitude to Arba Minch College of Health Sciences for sponsoring the study, South Ari Zone Health Department and South Ari District Health Office for providing information, and study participants, data collectors, and supervisors for their willingness and participation.
Conflict of interest
The authors declare that they do not have any conflicts of interest.
References
1.
WHO. Malnutrition Fact-Sheet (2021). Available from: https://www.who.int/news-room/fact-sheets/detail/malnutrition (Accessed on July 9, 2023).
2.
PFAN Wadhwani. Mother, Infant and Young Child Nutrition and Malnutrition (2019). Available from: https://motherchildnutrition.org/malnutrition/about-malnutrition/impact-of-malnutrition.html (Accessed July 12, 2023).
3.
Achadi E Ahuja A Bendech MA Bhutta ZA De-Regil LM Fanzo J et al Global Nutrition Report 2016: From Promise to Impact: Ending Malnutrition by 2030. Washington, D.C., USA: International Food Policy Research Institute (2016).
4.
UNICEF World Bank Levels and Trends in Child Malnutrition: Key Findings of the 2020 Edition of the Joint Child Malnutrition Estimates. Geneva: WHO (2020).
5.
Akombi BJ Agho KE Merom D Renzaho AM Hall JJ . Child Malnutrition in Sub-Saharan Africa: A Meta-Analysis of Demographic and Health Surveys (2006-2016). PloS one (2017) 12(5):e0177338. 10.1371/journal.pone.0177338
6.
Fenta HM Tesfaw LM Derebe MA . Trends and Determinants of Underweight Among Under-Five Children in Ethiopia: Data From EDHS. Int J Pediatr (2020) 2020:3291654. 10.1155/2020/3291654
7.
EPHI I. Ethiopian Public Health Institute (EPHI)[Ethiopia] and ICF. Ethiopia Mini Demographic and Health Survey 2019: Key Indicators (2019).
8.
Tariku B Mulugeta A Tsadik M Azene G . Prevalence and Risk Factors of Child Malnutrition in Community-Based Nutrition Program Implementing and Non-Implementing Districts From South East Amhara, Ethiopia. Open Access Libr J. (2014) 1(03):1–17. 10.4236/oalib.1100425
9.
Schönbeck Y Van Dommelen P HiraSing RA Van Buuren S . Thinness in the Era of Obesity: Trends in Children and Adolescents in The Netherlands Since 1980. Eur J Public Health (2015) 25(2):268–73. 10.1093/eurpub/cku130
10.
Aguayo VM Nair R Badgaiyan N Krishna V . Determinants of Stunting and Poor Linear Growth in Children Under 2 Years of Age in India: An In‐Depth Analysis of Maharashtra's Comprehensive Nutrition Survey. Matern child Nutr (2016) 12:121–40. 10.1111/mcn.12259
11.
WHO. Turning the Tide of Malnutrition: Responding to the Challenge of the 21st Century. Geneva, Switzerland: World Health Organization (2000).
12.
Fufa DA Laloto TD . Factors Associated With Undernutrition Among Children Aged Between 6–36 Months in Semien Bench District, Ethiopia. Heliyon (2021) 7(5):e07072. 10.1016/j.heliyon.2021.e07072
13.
Halala DDGEY. Prevalence of Underweight and Associated Factors Among Children Aged 6 to 59 Months in Areka Town. Wolaita Zone, South. Ethiopia Prevalence (2016) 25.
14.
Hossain MM Abdulla F Rahman A . Prevalence and Risk Factors of Underweight Among Under-5 Children in Bangladesh: Evidence From a Countrywide Cross-Sectional Study. Plos one (2023) 18(4):e0284797. 10.1371/journal.pone.0284797
15.
Tosheno D Mehretie Adinew Y Thangavel T Bitew Workie S . Risk Factors of Underweight in Children Aged 6–59 Months in Ethiopia. J Nutr Metab (2017) 2017:6368746. 10.1155/2017/6368746
16.
Yehuala GK Orcho AH Gebresilassie MH Meshesha HA Amera TG Tariku EZ . Undernutrition and Associated Factors Among Children Aged 6-59 Months in Nutrition-Sensitive Agriculture Intervention Implemented Basona District, North Shewa Zone, Amhara Region, Ethiopia. Plos one (2023) 18(4):e0284682. 10.1371/journal.pone.0284682
17.
Swaminathan S Hemalatha R Pandey A Kassebaum NJ Laxmaiah A Longvah T et al The Burden of Child and Maternal Malnutrition and Trends in its Indicators in the States of India: The Global Burden of Disease Study 1990–2017. Lancet Child Adolesc Health (2019) 3(12):855–70. 10.1016/S2352-4642(19)30273-1
18.
Ministry of Agriculture and Natural Resource (MoANR); Ministry of Livestock and Fisheries (MoLF). Nutrition Sensitive Agriculture Strategy (2016). p. 1–31.
19.
South Ari District Health Office. Health Report (2020).
20.
South Ari District Agriculture and Rural Development Office. Agricultural Report (2020).
21.
Abdulahi A Shab-Bidar S Rezaei S Djafarian K . Nutritional Status of Under-Five Children in Ethiopia: A Systematic Review and Meta-Analysis. Ethiopian J Health Sci (2017) 27(2):175–88. 10.4314/ejhs.v27i2.10
22.
Sewenet T Zenebe Y Yimam W Woretaw L . Undernutrition and Associated Factors Among Children Aged 6–23 Months in Dessie Town, Northeastern Ethiopia, 2021: A Community-Based Cross-Sectional Study. Front Pediatr (2022) 10:916726. 10.3389/fped.2022.916726
23.
FAO. Nutrition Technical Assistance Project, Academy for Educational Development (2007). Available from: http://www.fao.org/fileadmin/user_upload/eufaofsi4dm/doc-training/hfias.pdf (Accessed on July 17, 2023).
24.
Coates J Swindale A Bilinsky P . Household Food Insecurity Access Scale (HFIAS) for Measurement of Food Access: Indicator Guide (2007). version 3.
25.
WHO. Multicentre Growth Reference Study Group. WHO Child Growth Standards: Length/Height-For-Age, Weight-For-Age, Weight-For-Length, Weight-For-Height and Body Mass Index-for-Age. Methods Dev (2006).
26.
INDDEX Project. Data4Diets: Building Blocks for Diet-Related Food Security Analysis. Boston, MA: Tufts University (2018). p. 2006–8.
27.
FAO. Minimum Dietary Diversity for Women: A Guide for Measurement. Rome: FAO (2016).
28.
Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia Demographic and Health Survey 2016. Addis Ababa, Ethiopia, and Rockville, Maryland, USA: CSA and ICF (2016). Available from: https://dhsprogram.com/pubs/pdf/FR328/FR328.pdf (Accessed on July 17, 2023).
29.
Egata G Berhane Y Worku A . Predictors of Non-Exclusive Breastfeeding at 6 Months Among Rural Mothers in East Ethiopia: A Community-Based Analytical Cross-Sectional Study. Int Breastfeed J (2013) 8:8. 10.1186/1746-4358-8-8
30.
Wu Q Scherpbier RW Van Velthoven MH Chen L Wang W Li Y et al Poor Infant and Young Child Feeding Practices and Sources of Caregivers Feeding Knowledge in Rural Hebei Province, China: Findings From a Cross-Sectional Survey. BMJ open (2014) 4(7):e005108. 10.1136/bmjopen-2014-005108
31.
Feleke S Egata G Mesfin F Yilak G Molla A . Undernutrition and Associated Factors in Orphan Children Aged 6–59 Months in Gambella Southwest, Ethiopia: A Community-Based Cross-Sectional Study. BMJ open (2021) 11(7):e045892. 10.1136/bmjopen-2020-045892
32.
Ahsan KZ Arifeen SE Al-Mamun MA Khan SH Chakraborty N . Effects of Individual, Household and Community Characteristics on Child Nutritional Status in the Slums of Urban Bangladesh. Arch Public Health (2017) 75(1):9–13. 10.1186/s13690-017-0176-x
33.
Al-Sobaihi S Nakamura K Kizuki M . Undernutrition Among Children Under 5 Years of Age in Yemen: Role of Adequate Childcare Provided by Adults Under Conditions of Food Insecurity. J Rural Med (2016) 11(2):47–57. 10.2185/jrm.2915
34.
Nigatu G Assefa Woreta S Akalu TY Yenit MK . Prevalence and Associated Factors of Underweight Among Children 6–59 Months of Age in Takusa District, Northwest Ethiopia. Int J equity Health (2018) 17(1):106–8. 10.1186/s12939-018-0816-y
35.
Tibebu NS Emiru TD Tiruneh CM Getu BD Azanaw KA . Underweight and Its Associated Factors Among Children 6–59 Months of Age in Debre Tabor Town, Amhara Region of Ethiopia, 2019: A Community-Based Cross-Sectional Study. Pediatr Health Med Ther (2020) 11:469–76. 10.2147/PHMT.S288071
36.
Huynh G Huynh QHN Nguyen NHT Do QT Van Tran K . Malnutrition Among 6–59-Month-Old Children at District 2 Hospital, Ho Chi Minh City, Vietnam: Prevalence and Associated Factors. Biomed Res Int (2019) 2019:1–8. 10.1155/2019/6921312
37.
Ali W Ayub A Hussain H . Prevalence and Associated Risk Factors of Undernutrition Among Children Aged 6 to 59 Months in Internally Displaced Persons of Jalozai Camp, District Nowshera, Khyber Pakhtunkhwa. J Ayub Med Coll Abbottabad (2015) 27(3):556–9.
38.
Mulu E Mengistie B . Household Food Insecurity and Its Association With Nutritional Status of Under-Five Children in Sekela District, Western Ethiopia: A Comparative Cross-Sectional Study. BMC Nutr (2017) 3(1):35–9. 10.1186/s40795-017-0149-z
39.
Betebo B Ejajo T Alemseged F Massa D . Household Food Insecurity and Its Association With Nutritional Status of Children 6–59 Months of Age in East Badawacho District, South Ethiopia. J Environ Public Health (2017) 2017:6373595. 10.1155/2017/6373595
40.
Sreeramareddy CT Ramakrishnareddy N Subramaniam M . Association Between Household Food Access Insecurity and Nutritional Status Indicators Among Children Aged< 5 Years in Nepal: Results From a National, Cross-Sectional Household Survey. Public Health Nutr (2015) 18(16):2906–14. 10.1017/S1368980014002729
41.
Ali D Saha KK Nguyen PH Diressie MT Ruel MT Menon P et al Household Food Insecurity Is Associated With Higher Child Undernutrition in Bangladesh, Ethiopia, and Vietnam, But the Effect Is Not Mediated by Child Dietary Diversity. J Nutr (2013) 143(12):2015–21. 10.3945/jn.113.175182
42.
Khamis AG Mwanri AW Ntwenya JE Kreppel K . The Influence of Dietary Diversity on the Nutritional Status of Children Between 6 and 23 Months of Age in Tanzania. BMC paediatrics (2019) 19(1):518–9. 10.1186/s12887-019-1897-5
43.
Jain A Kalliyil M Agnihotri S . Minimum Diet Diversity and Minimum Meal Frequency–Do They Matter Equally? Understanding IYCF Practices in India. Curr Dev Nutr (2020) 4(2):nzaa054_084. 10.1093/cdn/nzaa054_084
44.
Chungkham HS Sahoo H Marbaniang SP . Birth Interval and Childhood Undernutrition: Evidence From a Large Scale Survey in India. Clin Epidemiol Glob Health (2020) 8(4):1189–94. 10.1016/j.cegh.2020.04.012
45.
Ntambara J Zhang W Qiu A Cheng Z Chu M . Optimum Birth Interval (36–48 Months) May Reduce the Risk of Undernutrition in Children: A Meta-Analysis. Front Nutr (2023) 9:939747. 10.3389/fnut.2022.939747
46.
Yaya S Uthman OA Ekholuenetale M Bishwajit G Adjiwanou V . Effects of Birth Spacing on Adverse Childhood Health Outcomes: Evidence From 34 Countries in Sub-Saharan Africa. J Maternal-Fetal Neonatal Med (2020) 33(20):3501–8. 10.1080/14767058.2019.1576623
47.
Katona P Katona-Apte J . The Interaction Between Nutrition and Infection. Clin Infect Dis (2008) 46(10):1582–8. 10.1086/587658
48.
Health FMo. Ethiopian Health Sector Transformation Plan II: 2020/21-2024/25 (2015). Available from: https://faolex.fao.org/docs/pdf/eth208376.pdf (Accessed on February 14, 2024).
49.
United Nation. Sustainable Development Goals - Goal 2: Zero Hunger (2024). Available from: https://www.un.org/sustainabledevelopment/hunger/ (Accessed on February 13, 2024).
50.
World Health Organization. Global Nutrition Targets 2025: Policy Brief Series. Geneva, Switzerland: World Health Organization (2014).
Summary
Keywords
underweight, predictors, children, south Ari district, South Ethiopia
Citation
Toma TM, Andargie KT, Alula RA, Kebede BM, Temesgen K and Guyo TG (2024) Underweight and Predictors Among Children Aged 6–59 Months in South Ethiopia. Int J Public Health 69:1606837. doi: 10.3389/ijph.2024.1606837
Received
09 November 2023
Accepted
06 May 2024
Published
21 May 2024
Volume
69 - 2024
Edited by
Rebecca Nantanda, Makerere University, Uganda
Reviewed by
Damalie Nalwanga, Makerere University, Uganda
Rebecca Nantanda, Makerere University, Uganda
Updates
Copyright
© 2024 Toma, Andargie, Alula, Kebede, Temesgen and Guyo.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tamirat Gezahegn Guyo, tamiratgezahegn7st@gmail.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.