- Department of Family and Preventive Medicine, Faculty of Medicine, Prince of Songkla University, Songkhla, Thailand
Objective: To investigate clusters of students’ COVID-19 preventive behaviors and their associated factors.
Methods: We surveyed undergraduate students using an online questionnaire at a regional university in southern Thailand, between April and June 2022. Statistical analyses included latent class analysis and multinomial regression analysis.
Results: Three latent classes were identified: moderately consistent practitioner (7.5%), high compliance overall (48.9%), and good compliance with routine safeguards (43.6%). Females tended to have high compliance overall (RRR 2.46 95% CI 1.23–4.94), and higher academic performance was associated with high compliance overall and good routine safeguards. Perceived threats from COVID-19 were associated with good compliance with routine safeguards (RRR 4.21 95% CI 1.70–10.45). Benefits of actions and clear cues to action were associated with high overall compliance (RRR 5.24 95% CI 2.13–12.90). Students who perceived feasibility were more likely to be moderately consistent practitioners.
Conclusion: The common clusters of the students’ preventive behaviors were high compliance overall and good compliance with routine preventions. Female, academic performance, perceived threats, and perceived benefits and cues to action were associated with compliance.
Introduction
Between the recognition of COVID-19 in March 2020 and October 2021, the Coronavirus Disease of 2019 (COVID-19) pandemic had more than two hundred million cases and was attributed to more than four million deaths worldwide [1]. The pandemic had caused significant public health and economic impacts in many countries [2]. COVID-19 is caused by the SARS-CoV-2 virus which can be transmitted from human to human via droplets and aerosols. Transmission is possible despite a person being asymptomatic [3]. After COVID-19 was declared a pandemic, significant efforts were put into dealing with disruptions in health systems and other industries [4]. Global public health sections tackled the spread of COVID-19 by lifting countries’ capacities to screen, treat, and prevent new cases by manipulating population behavior through gradual encouragements and enforcing some new regulations, including wearing face mask in public places [5, 6], things for which it was believed that enforcement alone might not yield effective or sustainable compliance with COVID-19 preventive measures [7].
Since 2020, closures of schools and colleges have been reported worldwide due to pandemic [8]. Reopening universities during the COVID-19 epidemic was a significant challenge in many countries around the world. Israel’s and Korea’s experiences in reopening their universities showed that inadequate implementation of preventive measures could lead to peaks of new cases and reclosures [9, 10]. In Taiwan, there were seven confirmed cases reported from six colleges, of which one university experienced a reclosure 4 months after the pandemic was declared despite having had guidelines for disease surveillance, self-quarantine protocols, a guideline for hygiene practices, ventilation and sanitization control measures, regulations on school gatherings, policies for temporary school closures, and adaptive classes [11].
University students are mostly adolescents [12]. They pay more attention to rewards than to drawbacks and often overlook long-term consequences [13]. In this age group, students prioritize peer effects and behave similarly within their social groups, thus several behaviors can also be clustered [14]. These psychosocial features complicate campaigns which aim to encourage and manipulate the students’ compliance with preventive measures [15]. During COVID-19 pandemic, one study found that these young people were unlikely to report social distancing, washing hands, or avoiding touching faces (38%, 30%, and 30%, respectively) [16]. A Vietnamese study reported that only half (47.4%) had regular hand hygiene practice despite a prevalent favorable attitude to recommended hand hygiene practice (97.9%) [17]. Moreover, the students reported 2.3, 4.0, and 3.7 times lower concerns towards risk of infection, hospitalization, and death from COVID-19, respectively [16].
In late 2021, university teaching in Thailand had to be adapted to control the spread of COVID-19 and was modified to hybrid teaching where in-classroom and video teaching were scheduled alternately. The classes for the social sciences and liberal arts disciplines were held online while the universities tried to keep up with essential laboratory teaching in health science divisions. However, these urgent adaptations might not have sufficed to ensure safe university environments in Thailand during the pandemic. According to Thailand statistics [18], this age group was responsible for 20% of new cases although they had shown favorable attitudes and good compliance with preventive measures [19]. Thus, the Thailand health authorities put a lot of effort into ensuring high vaccine coverage for students before establishing on-site classes, enforcement of strict physical distancing measures, new classroom standards, high compliance with wards hygiene recommendations, and good self-monitoring methods [5, 20].
In the south of Thailand, teaching activities ceased due to the rise in COVID-19 cases in February 2022. Most of the universities decided to reopen their campuses in late June 2022 after the current study was conducted [21]. To control COVID-19 in the university campuses, health authorities demanded good understanding about patterns of behavior that made the students vulnerable to COVID-19. Earlier studies only described the university students’ compliance with individual behaviors and identified certain potential behavior modifiers. However, such simple descriptions might not be sufficient when the students’ preventive behaviors were potentially clustered and influenced by their close ones, including their friends and family members. Therefore, the current study aimed to investigate the underlying clusters of the students’ preventive behaviors in one university, and further identify potential behavioral modifiers of the underlying behavior clusters.
Methods
Study Design and Setting
The cross-sectional study was conducted at Prince of Songkla University (PSU), Hat Yai campus between 28 April and 15 June 2022. The data were collected via an online self-reported questionnaire which had been distributed via social media platforms (i.e., the university student affairs page and group emails) and in the form of posters for local advertising. The study did not provide any monetary or other compensation to the participants.
Study Population and Sample Size Calculation
The participants in our study were undergraduate students of PSU, Hat Yai campus, who could access the internet and understand the Thai language. To estimate required sample size, we calculated the proportions of COVID-19 prevention behaviors in undergraduate students by estimating a finite population proportion [22]. We assumed the compliance with preventive behaviors was 47% and determined the acceptable error at 4.7% [17], which we then adjusted with a design effect of 1.5. Finally, the minimum required sample size was 633 participants.
Measurements
Independent Variables
Demographic Characteristics
The study demographic data consisted of age, sex, religion, residence, number of co-residents, sufficiency of monthly budget, faculty group, academic year, academic performance (GPA), mode of study, medical conditions, source of COVID-19 information, source of COVID-19 recommendations, vaccination status, history of COVID-19 infection, and history COVID-19 infections in friends and family. Age was classified into two groups: 18–21 years, and over 21 years. Residence was defined as the students’ current place of living, categorized into two groups: dormitory, and home. The sufficiency of the monthly budget as perceived by the respondent was divided into three groups: insufficient, sufficient, and having savings. The faculty was divided into three groups based on their learning activities during the pandemic: health sciences (hospital-based), sciences and technology (laboratory-based), and social sciences and others (online-based). Academic performance was measured by grade point average (GPA) of the previous year, which was later categorized into three groups: high, moderate, and low.
Perceptions Related With COVID-19 and Preventive Measures
We developed the study questionnaires incorporating factors influencing youth behaviors from previous studies [14, 15]. Perceptions are important internal mechanisms that can influence one’s compliance with health recommendation [23], thus we hypothesized the perceptions were the main exposure in the study. The students’ perceptions were measured by a 4-point Likert scale questionnaire with responses ranging from strongly disagree to strongly agree. An item-objective congruency index (IOC) was used to evaluate the questions in the questionnaire by three experts. The IOC was 0.96–1.00 for each item, and 0.91 overall. We conducted exploratory factor analysis (EFA) to assess the latent constructs of the students’ perceptions. Principal axis factoring with varimax rotation was used, and we found three variables: perceptions towards threats from COVID-19 (including one’s own perceived susceptibility to develop COVID-19 and perceived severity of COVID-19), perceived benefits of following recommended measures and cues to the actions, and the feasibility of complying with the recommended actions (defined as the degree of confidence individuals felt in their ability to adopt and maintain the recommended preventive measures) [24]. The questionnaire was internally consistent (alpha = 0.61 to 0.89 for each domain, and 0.77 overall). The total scores in each perception domain were later categorized into low and high levels by the group median (25, 14, and 27 for perceived threats from COVID-19, perceived feasibility of compliance with recommended measures, and perceived benefits of following recommended measures and cues to the actions, respectively).
Dependent Variables – COVID-19 Preventive Behaviors
We formulated ten behavior measurement questions based on local guidelines and CDC recommendations [5]. The questions asked participants to rate their frequency of seven preventive measures: appropriate hand hygiene practices, cough etiquette, mask-wearing, avoiding crowds, social distancing, cleaning contact surfaces in daily life, and self-health monitoring. Responses were based on a 4-level frequency scale ranging from 1 to 4 (1 = never, 2 = rarely, 3 = sometimes, and 4 = often). Compliance with COVID-19 preventive behaviors was represented by the proportion of participants in each frequency category. The IOCs were acceptable (ranging from 0.67 to 1 for each item and 0.97 overall), and the items were internally consistent (alpha = 0.79).
Statistical Analysis
The compliance with each preventive behavior was described in frequency and percentage. We evaluated possible participant-centered clusters of behavior from the ten preventive behaviors by latent class analysis (LCA) following standard recommendations [25]. Our analysis evaluated one to six-classes model and incorporated social factor covariates: gender, sufficiency of monthly budget, year of study, and place of residence. Participants with incomplete covariate data were removed from the LCA. The Chi-square test was used to examine differences in the distributions of each factor among the classes. Subsequently, we chose variables with p < 0.05 to be factors for adjusting effect estimates in the regression analysis. Relative Risk Ratios (RRR) with 95% confidence intervals (95% CI) were acquired from multivariable multinomial regression. The Akaike information criterion (AIC), Bayesian information criterion (BIC), maximum log-likelihood, and entropy were used as diagnostic parameters for choosing a proper model in terms of the number of classes, together with its interpretability. R software version 4.2.0 with ggplot2, latticeExtra, poLCA, epicalc, and nnet were used in the analysis.
Results
Participant Characteristics
Of the 687 participants who had complete data (97.6% of the total sample), more than half were female (58.8%), with most aged between 18 and 21 years old (89.5%), and Buddhist (79.8%). The majority of the participants stayed at home (73.5%), the highest number had 4-6 members in the same residence (48.5%), and had sufficient monthly budget and had savings (42.6%). The majority of the participants were studying in the science and technology group (60.8%), almost half were studying in the 2nd academic year (49.3%), and had moderate grades (46.6%). Nearly ninety percent of the did all their academic work online. Only one-fifth of the participants had medical condition (23.3%), of which the most common was allergic rhinitis. Around half of the participants were feasible students, while less than half had high perceived threats from COVID-19 and had high perceptions of the benefits of following the recommended behaviors and cues to action. The baseline characteristics of the participants are reported in Table 1.
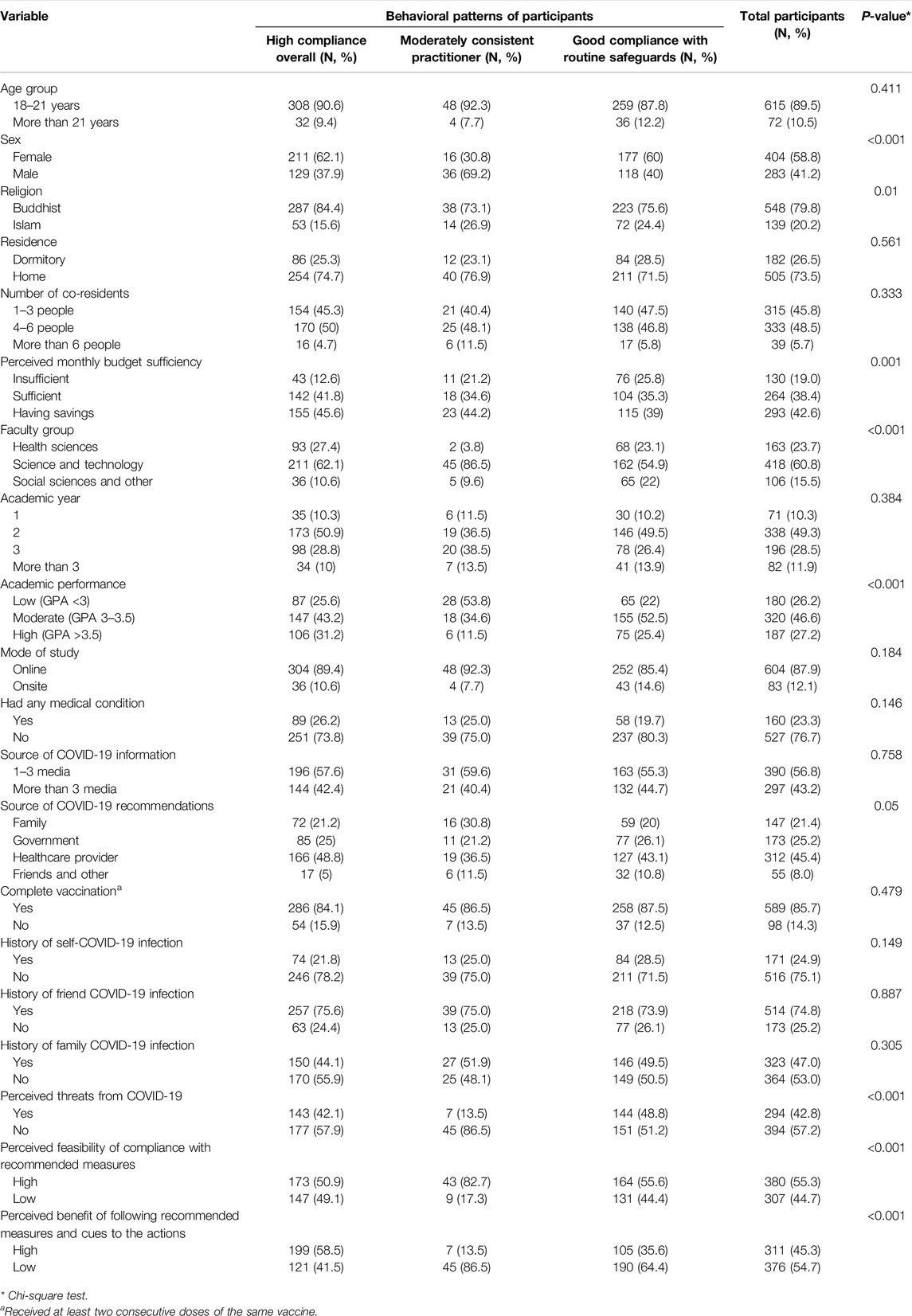
Table 1. The three behavioral classes with associated variables (participants who had complete data = 687) (Subgroup Behaviors and Factors Influencing Compliance With COVID-19 Preventive Measures Among Undergraduate Students in Southern Thailand, Thailand, 2022).
Most participants reported high compliance with wearing a mask in public settings or crowds (89.5%) and monitoring their health daily (72.3%). Over half of the participants often washed their hands during daily activities (59.1%), used public transportation only as needed (58.7%), covered their mouth when coughing or sneezing (54%), and avoided touching the front of their mask (52.8%). One-third of the participants often avoided crowds and poorly ventilated spaces (40.5%), washed their hand after coughing or sneezing (36.4%), cleaned high-touch surfaces before using public areas (34.2%), and maintained a 1–2 m distance from others (34.1%). The variations of the participants’ COVID-19 preventive behaviors are shown in Table 2.
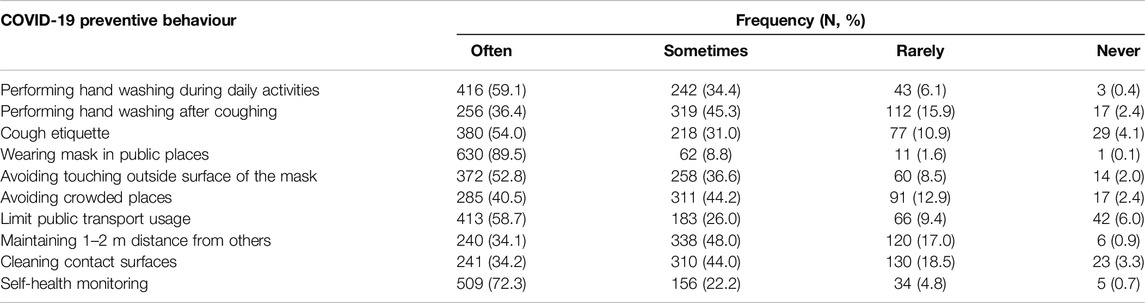
Table 2. Compliance with recommended COVID-19 preventive behaviours (Total participants = 704) (Subgroup Behaviors and Factors Influencing Compliance With COVID-19 Preventive Measures Among Undergraduate Students in Southern Thailand, Thailand, 2022).
We constructed a three-class model which was statistically and conceptually suitable to capture latent subpopulations (Figure 1). The details of the diagnostic statistics used in all the models and their values are provided in Supplementary Table S1. Figure 1 shows the conditional probability for each response (compliance score in each behavior) in each latent class. The model predicted that classes one, two and three would share 7.5%, 48.9%, and 43.6% probability of the study sample. The mean scores of each behavior in each latent class were also used to describe the features of the clusters (Figure 2). Moderately consistent practitioner (class 1) and high compliance overall (class 2) represented clusters of individuals who had moderately high and high mean scores across the ten behaviors, respectively, and good compliance with routine safeguards (class 3) referred to the cluster of people who had high compliance in only certain routine measures (often the measures applied in public places) while their compliances with some actions were relatively low.
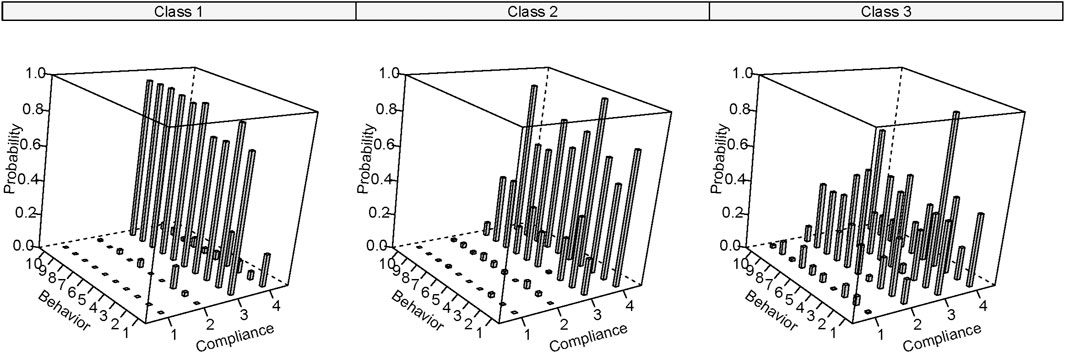
Figure 1. Latent classes of recommended coronavirus disease 2019 preventive measures in the participants (Subgroup Behaviors and Factors Influencing Compliance With COVID-19 Preventive Measures Among Undergraduate Students in Southern Thailand, Thailand, 2022). Remarks: class1 = moderately consistent practitioner, class 2 = high compliance overall, class 3 = good compliance with routine safeguards, compliance score 1 = rarely practiced, 2 = sometimes practiced, 3 = often practiced, 4 = regularly practiced, and probability represents conditional probability of levels of compliance based on the latent class, behavior numbers from one to ten represent performing hand washing in daily life (1), performing hand washing after coughing (2), cough etiquette (3), wearing mask in public places (4), avoiding touching outside surface of the mask (5), avoiding crowded places (6), limit public transport usage (7), maintaining 1–2 meter distance from others (8), cleaning contact surfaces (9), and self-health monitoring (10), respectively.
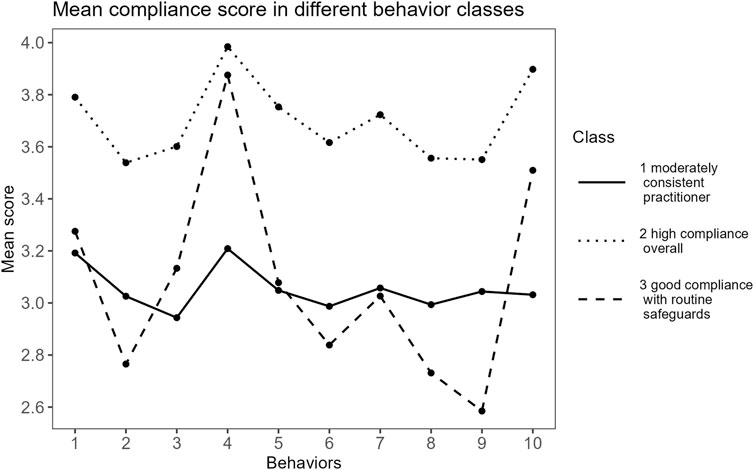
Figure 2. Mean compliance scores in different behavior classes (Subgroup Behaviors and Factors Influencing Compliance With COVID-19 Preventive Measures Among Undergraduate Students in Southern Thailand, Thailand, 2022). Remarks: y-axis is partly collapsed to illustrate variations of the score, behavior numbers from one to ten represent performing hand washing in daily life (1), performing hand washing after coughing (2), cough etiquette (3), wearing mask in public places (4), avoiding touching outside surface of the mask (5), avoiding crowded places (6), limit public transport usage (7), maintaining 1–2 m from others (8), cleaning contact surface (9), and self-health monitoring (10), respectively.
Table 1 illustrates the overall characteristics of the participants and across the latent classes. We found that sex, religion, sufficiency of monthly budget, faculty group, academic performance (GPA), high perceived threats from COVID-19, high perceived feasibility of compliance with recommended measures, and high perceived benefits of following recommended measures and cues to the actions significantly differed among the three classes (p < 0.05).
We used multinomial regression analysis to identify factors associated with COVID-19 preventive behaviors (Table 3). Our results showed that females were more likely to have high compliance overall compared with males (RRR 2.46, 95% CI 1.23–4.94). Participants with a moderate GPA were more likely to be categorized as good compliance with routine safeguards and high compliance overall (RRR 3.22, 95% CI 1.59–6.54 and RRR 2.05, 95% CI 1.01–4.16, respectively) while a high GPA was more likely to indicate a participant with high compliance overall (RRR 3.15, 95% CI 1.14–8.74). Participants with high perceived threats from COVID-19 were more likely to have good compliance with routine safeguards (RRR 4.21, 95% CI 1.70–10.45). Additionally, participants with a high perceived feasibility of compliance with recommended measures were less likely to have good compliance with routine safeguards and high compliance overall (RRR 0.28, 95% CI 0.12–0.62 and RRR 0.30, 95% CI 0.14–0.68, respectively). Individuals who highly perceived benefits of following recommended measures and cues to the actions were somewhat likely to have high compliance overall (RRR 5.24, 95% CI 2.13–12.90).
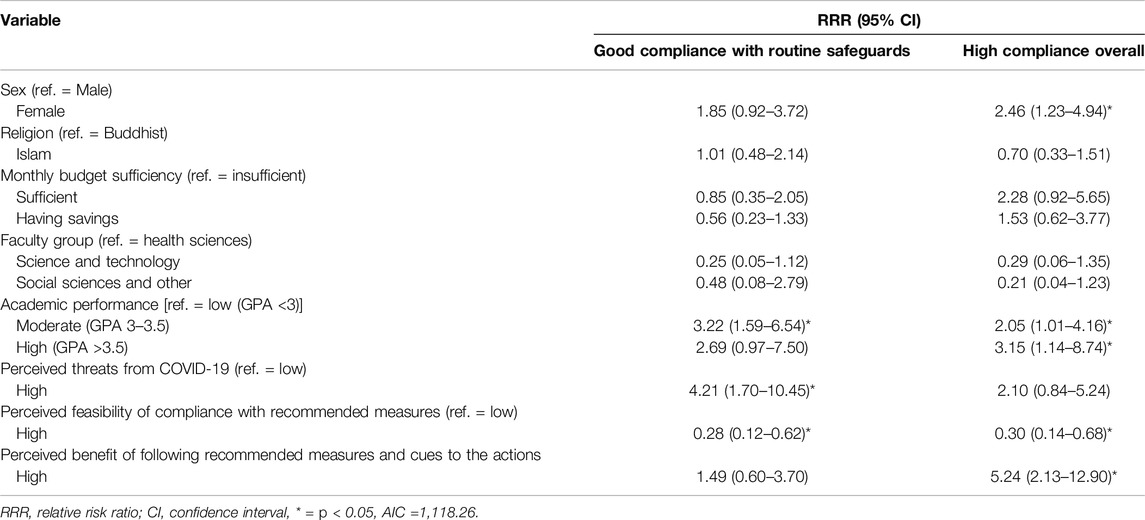
Table 3. Factors associated with COVID-19 preventive behaviors (reference = moderately consistent practitioner, N = 687) (Subgroup Behaviors and Factors Influencing Compliance With COVID-19 Preventive Measures Among Undergraduate Students in Southern Thailand, Thailand, 2022).
Discussion
Our study was exploratory research aimed at examining the prevalence of compliance with preventive measures and the factors associated with COVID-19 preventive behaviors among undergraduate students at a large university in Southern Thailand. At the time of the study, the university was emphasizing various COVID-19 preventive policies, including campaigning for students to adhere to several preventive measures, implementing electronic temperature checkpoints in most public areas, and conducting online surveillance of COVID-19 through daily self-reported symptoms [20]. Most of the study participants reported high compliance with wearing masks in public places and self-health monitoring. The high compliance with mask-wearing in our study was similar to findings from studies in Vietnam and Malaysia [26]. However, care is required to ensure good mask-wearing compliance during outdoor public activities. Previous studies of undergraduate students in the US showed that mask-wearing in outdoor spaces was relatively low compared with indoors [27, 28]. We also found that only one-third of the participants maintained good hand hygiene, regularly cleaned contact surfaces, and practiced proper physical distancing. These low compliance rates, however, were not uncommon. Similar findings have been reported at other universities in Asia and the United States [17, 29–31]. Therefore, university authorities should consider these commonly low compliance rates as areas for improvement when preparing for similar outbreaks in the future. Nevertheless, extra care should be taken to balance physical distancing with opportunities for healthy social interactions, as excessive distancing could negatively impact students’ mental health and increase the risk of depression [32].
For health behaviors, investigating multiple separate behaviors and trying to modify these behaviors separately might not be an efficient method for a university as the high risk students often present with a cluster of health-risk behaviors [14]. Latent class analysis is an approach to identify unmanifested groups of behaviors could provide insights into behavior modifications for an outbreak control for COVID-19 or other respiratory viral infections. We classified the COVID-19 preventive behaviors into three classes: moderately consistent practitioners (class 1), high overall compliance (class 2), and good compliance with routine safeguards (class 3). Classes 2 and 3 made up approximately 93 percent of the study sample. The behavior patterns in these two classes were similar in terms of having high mask wearing and self-monitoring compliances, which could further imply that a majority of the participants had relatively equivalent awareness towards these two behaviors compared to the other eight practices. However, the lower compliances in class 2 could reflect the needs for additional health promotion campaigns.
We identified several factors associated with good compliance, including female gender, a high GPA, a high perceived threat from COVID-19, a high perceived feasibility of compliance with preventive measures, and a high perceived benefit of following recommended measures and cues to action. Females were more likely to have high overall compliance. Several previous studies have shown that females exhibited higher adherence to COVID-19 preventive measures [33–35]. Studies explained that females had higher conscientiousness and agreeableness [36], and also had higher interests in health information, thus they were more compliant to the COVID-10 prevention [37]. Apart from gender, lower student GPAs were associated with an increased risk of low prevention compliances, similar to its association with other public health recommendations [38]. In addition, the extent to which students perceived threats was particularly associated with compliance with routine safeguards. Leveraging awareness of threats from COVID-19 could be an effective strategy to promote compliance with mask-wearing and self-monitoring. Furthermore, the perceived benefits of following recommended measures and cues to action were significant motivators for high overall compliance. Several studies have demonstrated a strong positive relationship between perceived benefits, cues to action, and the adoption of COVID-19 preventive behaviors among undergraduates in Thailand and many other countries [39–43]. Therefore, policy should aim at promoting awareness of the benefits of COVID-19 preventive measures and providing resources as cues to action, with a particular focus on male students and those with a low GPA.
Undergraduate students are mostly adolescents and study under structured coursework [44]. There are interventions to promote the student behaviors through persuasive techniques and social engineering [45]. The persuasive approach [46] utilizes simple, credible, relevant, and emotional messages connected to the actual pandemic situation and distributes these messages through student online social networks or coursework panels. Social engineering involves various socio-environmental modifications, such as rule enforcement or enhancing accessibility to face masks and hand sanitizers throughout the university [47]. Nevertheless, we identified perceived feasibility as a risk factor for poor routine (class 2) and overall (class 3) hygiene practices. This phenomenon could be due to a paradoxical effect: while perceiving abundant feasibility of carrying out preventive behaviors initially increases motivation to adhere to the measures, excessive resources can reverse this effect [48]. Thus, monitoring students’ behaviors should be conducted in parallel with these promotions.
Strengths
Our study had several strengths. We applied local COVID-19 prevention recommendations with world standards in our instrument’s design to enhance the study’s internal validity. The internet-based survey also helped us to achieve a good response rate during the pandemic time and reduce biased responses from students who were concerned about whether their behaviors were socially acceptable. In addition, we applied latent class analysis to further identify potential clusters of students’ preventive behaviors to illustrate the existence of clusters where students had similar behaviors rather than using simple descriptive statistics. This empirical evidence could help policymakers identify potential groups of students and prioritize actions to tackle certain behavioral risk factor issues.
Limitations and Further Study Suggestions
There were certain limitations in our study. First, we conducted the study during a period of stable pandemic situation and a small re-surge of COVID-19 case numbers. The dynamics of COVID-19 might have influenced the students’ awareness through surging pandemic information and a wide range of regulations at the participants’ residences. Thus, caveats should be considered that the presented associations might have been confounded by the intensity of the outbreak. Second, our latent class analysis was based on the behaviors of the study population. This could limit the generalizability of the classes and their associated factors to the other populations. Third, our data were based on a undergraduate students who had the capacity to access to the internet. Caution is advised when using the behavioral patterns for non-undergraduates and those who cannot access online resources, as perceptions could be altered significantly by the receipt of information showing individual’s susceptibility to the active infection.
Implications
During a respiratory virus outbreak, university authorities should consider campaigns to promote hand hygiene, cough etiquette, environment cleaning, and balanced physical distancing for the university students while routine safeguards are regulated. In addition, policy or campaign designs should pay special attention to groups less likely to follow the suggestions of authorities, including low GPA and male students. They should also increase awareness of the incoming threats, highlight the benefits of preventive actions, and exhibit clear cues to the suggested actions, to promote high compliance with preventive measures in their students.
Conclusion
The study highlighted a relatively low compliance with physical distancing among undergraduate university students. The most common clusters of the undergraduate students’ preventive behaviors were high compliance overall, and good compliance only to some routine preventions. Female students and participants who had better academic performance tended to have high compliance for prevention recommendations in general. The perceptions towards threats from COVID-19, and perceived benefits and cues to the preventive actions, were potential behavioral modifiers which require attention from the university.
Ethics Statement
The studies involving humans were approved by the Human Research Ethics Committee (HREC), Faculty of Medicine, Prince of Songkla University, REC. 65-128-9-4. The studies were conducted in accordance with the local legislation and institutional requirements. All the activities were performed in accordance with the principles and ethical standards of the declaration of Helsinki. The participants provided their action consent to participate in this study by clicking the consent button at the first page of our electronic questionnaire before participating in the research.
Author Contributions
SS, PN, and NA conceptualized and designed the study. NA participated in the acquisition of data. SS and PN supervised the data project. SS and NA analyzed the data. SS and NA are responsible for the integrity of data analysis. SS and NA wrote the original draft of the manuscript. NA acquired funding support. All authors contributed to the article and approved the submitted version.
Funding
The authors declare that financial support was received for the research, authorship, and/or publication of this article. This study was funded by the Faculty of Medicine, Prince of Songkla University (grant number 65-046-1). The funder did not participate in the design of the study design, data collection, analysis and interpretation, or manuscript preparation.
Conflict of Interest
The authors declare that they do not have any conflicts of interest.
Acknowledgments
The authors would like to thank all participants for their participation and the student affairs offices for their cooperation in distributing the online questionnaire. We would like to thank the International Affairs Department, Faculty of Medicine, Prince of Songkhla University, for the proofreading this manuscript.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/ijph.2024.1606788/full#supplementary-material
References
1. World Health Organization. Coronavirus Disease 2019 Dashboard (2021). Available from: https://covid19.who.int (Accessed October 31, 2021).
2. United Nations. Social Impact of Coronavirus Disease 2019 (2021). Available from: https://www.un.org/development/desa/dspd/everyone-included-covid-19.html (Accessed November 11, 2021).
3. Giri, S, Sen, S, Singh, R, Paul, P, Sahu, R, Nandi, G, et al. Current Challenges in Different Approaches to Control COVID-19: A Comprehensive Review. Bull Natl Res Cent (2022) 46:47. doi:10.1186/s42269-022-00730-2
4. World Health Organization. COVID-19 and the Social Determinants of Health and Health Equity: Evidence Brief (2021). Available from: https://apps.who.int/iris/handle/10665/348333 (Accessed September 3, 2023).
5. Centers for Disease Control and Prevention. COVID-19 Prevention Actions (2021). Available from: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html (Accessed October 27, 2021).
6. Centers for Disease Control and Prevention. CDC Strategy for Global Response to COVID-19 (2022). Available from: https://www.cdc.gov/coronavirus/2019-ncov/global-covid-19/global-response-strategy.html (Accessed September 23, 2023).
7. Mills, F, Symons, C, and Carter, H. Exploring the Role of Enforcement in Promoting Adherence With Protective Behaviours During COVID-19. Policing: J Pol Pract (2022) 16:580–90. doi:10.1093/police/paab079
8. United Nations Educational, Scientific and Cultural Organization. Dashboards on the Global Monitoring of School Closures Caused by the COVID-19 Pandemic (2020). Available from: https://covid19.uis.unesco.org/global-monitoring-school-closures-covid19/(Accessed October 11, 2022).
9. Klobucista, C, and Maizland, L. How Countries Are Reopening Schools During the Pandemic (2020). Available from: https://www.cfr.org/backgrounder/how-countries-are-reopening-schools-during-pandemic (Accessed November 24, 2021).
10. Kwon, J, and Jeong, S. Hundreds of South Korea Schools Close Again After Reopening (2020). Available from: https://edition.cnn.com/2020/05/29/asia/south-korea-coronavirus-shuts-down-again-intl/index.html (Accessed November 21, 2021).
11. Cheng, SY, Wang, CJ, Shen, ACT, and Chang, SC. How to Safely Reopen Colleges and Universities During COVID-19: Experiences From Taiwan. Ann Intern Med (2020) 173:638–41. doi:10.7326/M20-2927
12. Office of the Education Council. Higher Education Student Statistics 2000–2001. Bangkok: Secretariat Office of the Education Council of Thailand (2003). p. 39.
13. Colton, T, Allread, V, Abrams, E, Schoeneborn, A, Thome, B, and Fayorsey, R. The Nature of Adolescence and the Provision of Youth-Friendly Services. In: Adolescent HIV Care and Treatment. ICAP Columbia University (2012). p. 31–56.
14. Jessor, R. Risk Behavior in Adolescence: A Psychosocial Framework for Understanding and Action. J Adolesc Health (1991) 12:597–605. doi:10.1016/1054-139x(91)90007-k
15. World Health Organization. Young People and COVID-19: Behavioural Considerations for Promoting Safe Behaviours (2021). Available from: https://www.who.int/publications/i/item/978-92-4-002831-9 (Accessed November 20, 2021).
16. Bechard, LE, Bergelt, M, Neudorf, B, DeSouza, TC, and Middleton, LE. Using the Health Belief Model to Understand Age Differences in Perceptions and Responses to the COVID-19 Pandemic. Front Psychol (2021) 12:609893. doi:10.3389/fpsyg.2021.609893
17. Duong, MC, Nguyen, HT, Duong, BT, and Vu, MT. Assessment of Hand Hygiene Practices of University Students in Vietnam Amid the COVID-19 Pandemic: A Brief Report. Disaster Med Public Health Prep (2021) 16:1844–7. doi:10.1017/dmp.2021.256
18. Thai Department of Disease and Control. Coronavirus Disease 2019 Dashboard (2021). Available from: https://ddc.moph.go.th/covid19-dashboard/?dashboard=select-trend-line [Accessed December 2, 2021].
19. Singkun, A. Factors Associated With Social Responsibility Among University Students in Yala, Thailand During the COVID-19 Pandemic. J Health Res (2020) 35:265–75. doi:10.1108/JHR-05-2020-0142
20. Prince of Songkla University. Measures for Monitoring and Control of Coronavirus Disease 2019 Outbreak Among Staff and Students at Prince of Songkla University, Hat Yai Campus Issue no. 10 (2022). Available from: https://hatyai.psu.ac.th/th/node/9434 (Accessed March 4, 2022).
21. Ministry of Higher Education, Science, Research and Innovation. Preparations to Open Higher Education Institutions Nationwide in November 2021. Available from: https://www.mhesi.go.th/index.php/news/4490-2021-09-24-05-31-35.html (Accessed July 17, 2024).
22. Wayne, WD. Biostatistics: A Foundation of Analysis in the Health Sciences. 6th ed. United States: Malloy Lithographing, Inc. (1995). p. 794.
23. Rosenstock, IM. Historical Origins of the Health Belief Model. Health Educ Monogr (1974) 2:328–35. doi:10.1177/109019817400200403
24. Nguyen, C. Demographic Factors, Family Background and Prior Self-Employment on Entrepreneurial Intention - Vietnamese Business Students Are Different: Why? J Glob Entrepr Res (2018) 8:10. doi:10.1186/s40497-018-0097-3
25. Sinha, P, Calfee, CS, and Delucchi, KL. Practitioner’s Guide to Latent Class Analysis: Methodological Considerations and Common Pitfalls. Crit Care Med (2021) 49:e63–79. doi:10.1097/CCM.0000000000004710
26. Al Mamun, A, Hayat, N, Dieu, HTM, Zainol, NR, and Salameh, AA. COVID-19 Preventive Behavior Among University Students in Southeast Asia: Effects of Knowledge, Concern, Awareness, and Perceived Risk. Front Public Health (2022) 10:958021. doi:10.3389/fpubh.2022.958021
27. Burnell, K, Robbins, M, Kulali, S, and Wells, EM. Prevalence and Predictors of Mask Use on a Large US University Campus During the COVID-19 Pandemic: A Brief Report. Am J Infect Control (2022) 50:349–51. doi:10.1016/j.ajic.2021.11.028
28. Barrios, LC, Riggs, MA, Green, RF, Czarnik, M, Nett, RJ, Staples, JE, et al. Observed Face Mask Use at Six Universities - United States, September-November 2020. MMWR Morb Mortal Wkly Rep (2021) 70:208–11. doi:10.15585/mmwr.mm7006e1
29. Lee, K, Han, S, and Suh, HS. Early Impact of COVID-19 Social Distancing on Social Determinants of Health and Their Effects on Mental Health and Quality of Life of Korean Undergraduate Students. Front Public Health (2023) 11:1197143. doi:10.3389/fpubh.2023.1197143
30. Oosterhoff, B, and Palmer, CA. Attitudes and Psychological Factors Associated With News Monitoring, Social Distancing, Disinfecting, and Hoarding Behaviors Among US Adolescents During the Coronavirus Disease 2019 Pandemic. JAMA Pediatr (2020) 174(12):1184–90. doi:10.1001/jamapediatrics.2020.1876
31. Daniel, D, Kurniawan, A, Indah Pinawati, AR, Thohira, MC, and Annaduzzaman, M. The COVID-19 Health Protocol Among University Students: Case Studies in Three Cities in Indonesia. Int J Environ Res Public Health (2022) 19:10630. doi:10.3390/ijerph191710630
32. Pancani, L, Marinucci, M, Aureli, N, and Riva, P. Forced Social Isolation and Mental Health: A Study on 1,006 Italians Under COVID-19 Lockdown. Front Psychol (2021) 12:663799. doi:10.3389/fpsyg.2021.663799
33. Thanaphonganan, N, Yurayat, P, and Seechaliao, T. Health Literacy and Preventive Behaviors of Undergraduate University Students During the COVID-19 Pandemic. J Educ Learn (2022) 11:27–34. doi:10.5539/jel.v11n2p27
34. Gao, Z, Ying, S, Liu, J, Zhang, H, Li, J, and Ma, C. A Cross-Sectional Study: Comparing the Attitude and Knowledge of Medical and Non-Medical Students Toward 2019 Novel Coronavirus. J Infect Public Health (2020) 13:1419–23. doi:10.1016/j.jiph.2020.06.031
35. Potisopha, W, Saensom, D, Noonark, C, and Kabkumba, C. Factors Impacting COVID-19 Preventive Behaviors in Thai Adults During the Initial Phase of Vaccination. J Public Health Dev (2022) 20:236–48. doi:10.55131/jphd/2022/200319
36. Otterbring, T, and Festila, A. Pandemic Prevention and Personality Psychology: Gender Differences in Preventive Health Behaviors During COVID-19 and the Roles of Agreeableness and Conscientiousness. J Saf Sci Resil (2022) 3:87–91. doi:10.1016/j.jnlssr.2021.11.003
37. Deeks, A, Lombard, C, Michelmore, J, and Teede, H. The Effects of Gender and Age on Health Related Behaviors. BMC Public Health (2009) 9:213. doi:10.1186/1471-2458-9-213
38. Ong, CKY, Hutchesson, MJ, Patterson, AJ, and Whatnall, MC. Is There an Association Between Health Risk Behaviours and Academic Achievement Among University Students? Int J Environ Res Public Health (2021) 18:8314. doi:10.3390/ijerph18168314
39. Siramaneerat, I, Mungkhamanee, S, Chawajaroenpan, W, Choolert, P, Sirisabjanan, L, and Mangkalamanee, O. The Application of the Health Belief Model (HBM) for the Assessing Preventive Behavior Against COVID-19 Among Nursing Students in Thailand. J Med Assoc Thail (2022) 105:934–41. doi:10.35755/jmedassocthai.2022.10.13676
40. Alsulaiman, SA, and Rentner, TL. The Use of the Health Belief Model to Assess U.S. College Students’ Perceptions of COVID-19 and Adherence to Preventive Measures. J Public Health Res (2021) 10:2273. doi:10.4081/jphr.2021.2273
41. Karimy, M, Bastami, F, Sharifat, R, Heydarabadi, AB, Hatamzadeh, N, Pakpour, AH, et al. Factors Related to Preventive COVID-19 Behaviors Using Health Belief Model Among General Population: A Cross-Sectional Study in Iran. BMC Public Health (2021) 21:1934. doi:10.1186/s12889-021-11983-3
42. Shah, GH, Faraz, AA, Khan, H, and Waterfield, KC. Perceived Benefits Matter the Most in COVID-19 Preventive Behaviors: Empirical Evidence From Okara District, Pakistan. Int J Environ Res Public Health (2021) 18:6772. doi:10.3390/ijerph18136772
43. Tam, CC, Li, X, Li, X, Wang, Y, and Lin, D. Adherence to Preventive Behaviors Among College Students During COVID-19 Pandemic in China: The Role of Health Beliefs and COVID-19 Stressors. Curr Psychol (2021) 42:17280–90. doi:10.1007/s12144-021-01942-x
44. Education in Thailand. Office of the Education Council. Dusit Bangkok, Thailand: Ministry of Education, Kingdom of Thailand (2017). Available from: https://www.bic.moe.go.th/images/stories/pdf/EDUCATION_IN_THAILAND_2017.pdf (Accessed July 17, 2024).
45. Rosenstock, IM. The Health Belief Model and Preventive Health Behavior. Health Educ Monogr (1974) 2:354–86. doi:10.1177/109019817400200405
46. Atkin, CK, and Salmon, C. Persuasive Strategies in Health Campaigns. In: The SAGE Handbook of Persuasion: Developments in Theory and Practice. 2nd ed. Thousand Oaks, CA, United States: SAGE Publications (2013). p. 278–95.
47. Kumar, M. Changing Health Behaviour Through Social Engineering (2023). Available from: https://www.tutorialspoint.com/changing-health-behaviour-through-social-engineering (Accessed October 1, 2023).
Keywords: college health, COVID-19, preventive behaviors, latent class analysis, Thailand
Citation: Anujan N, Sripaew S and Ngamchaliew P (2024) Subgroup Behaviors and Factors Influencing Compliance With COVID-19 Preventive Measures Among Undergraduate Students in Southern Thailand. Int J Public Health 69:1606788. doi: 10.3389/ijph.2024.1606788
Received: 31 October 2023; Accepted: 26 August 2024;
Published: 06 September 2024.
Edited by:
Erica Di Ruggiero, University of Toronto, CanadaReviewed by:
Kanokwan Tharawan, Mahidol University, ThailandOne reviewer who chose to remain anonymous
Copyright © 2024 Anujan, Sripaew and Ngamchaliew. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Supakorn Sripaew, c3VwYWtvcm4uc0Bwc3UuYWMudGg=
 Nonlapan Anujan
Nonlapan Anujan Supakorn Sripaew
Supakorn Sripaew Pitchayanont Ngamchaliew
Pitchayanont Ngamchaliew