Abstract
Objective: This study aims to investigate the level of knowledge, attitude and self-management behaviors of diabetic patients, to explore the mediating role of attitude in the relationship between knowledge and self-management behaviors.
Methods: 900 diabetes patients were randomly selected from the eastern, central and western regions of Shandong Province, China, and recovered 863 valid questionnaires. Path analysis was used to examine the mediating role of attitude in the relationship between knowledge and self-management behaviors in patients with diabetes.
Results: The mean score (SD) of the diabetes self-management questionnaire (DSMQ) in this study was 35.01 (6.87). The direct effect value of knowledge level on self-management behaviors was 0.357, accounting for 62.09% of the total effect. The indirect effect value of knowledge on self-management behaviors through attitude was 0.218, accounting for 37.91%.
Conclusion: Level of knowledge has a significant direct impact on self-management behaviors and an indirect impact on self-management behaviors through attitude. Therefore, it is necessary to strengthen health education on diabetes to improve awareness, ameliorate attitudes toward diabetes, and change self-management behaviors.
Introduction
With the rapid development of social economy and the aggravation of population aging, the prevalence of diabetes is gradually increasing [1]. According to the 10th edition of the Diabetes Atlas released by the International Diabetes Federation [2], the number of patients with diabetes aged 20–79 in the world has reached 536.6 million in 2021, and is estimated to reach 783.2 million by 2045. China is one of the countries with the most significant increase in the prevalence of diabetes in the world [3]. The number of patients with diabetes in China was about 140.9 million in 2021, ranking the first in the world, and is estimated to reach 174.4 million by 2045 [2]. Diabetes is one of the main drivers of global mortality, about 6.7 million adults aged 20–79 will die of diabetes or its complications in 2021, and China has the highest number of deaths from diabetes, at approximately 1.4 million [2]. Unstable blood glucose control may cause a series of serious complications, such as retinopathy, nephropathy, and neuropathy [4], which seriously threat the quality of life in patients with diabetes and bring a huge disease burden to individuals, families, and society. Therefore, it is particularly important to control the blood glucose in patients with diabetes and prevent the onset of complications.
Diabetes management is reported to help control blood glucose and effectively prevent complications [5]. In recent years, research on diabetes management focuses on community management and self-management [6]. Diabetes community management refers to health education, guidance, and intervention implemented for diabetic patients performed by community medical staff, and regular health monitoring and follow-up visits with the aim of treatment compliance improvement [7]. Worldwide practical experience shows that extensive community-based population intervention and health management is an effective strategy for preventing and controlling diabetes [8, 9]. In addition, a large amount of research demonstrates that active engagement in diabetes community management assists in controlling the level of blood glucose, promoting individual mental health and further improving the quality of life [10–12].
Moreover, the community management of diabetes also emphasizes the self-management of patients [13–15]. From the experience at home and abroad, the community is an important base for self-management and prevention of diabetes, and also the most effective choice to prevent and control chronic diseases. Based on community management, community health workers help improve the self-management ability of patients with diabetes through health education, and combine community management with self-management to comprehensively and systematically manage the health status. Therefore, the self-management of patients with diabetes has received more and more attention. It is considered to be one of the most cost-effective health management measures, and is described as the basis for controlling blood glucose, preventing complications, and improving health status and quality of life [15, 16]. Diabetes self-management refers to the diabetes patients, with the assistance of medical staff, managing their daily behaviors and lifestyle by adopting scientific self-management skills. It is conducive to stabilizing the condition, promoting health and improving the quality of life [15, 17].
Prior studies have found that the self-management level of patients with diabetes still needs to be improved [18, 19]. A study in Oman found that only 1% of patients regularly self-monitored their blood glucose, 9.5% of them did exercise regularly, and 18% of them maintained healthy diet habits [18]. A study from China showed that only 9.2% of patients with diabetes had a good level of self-management [19]. Numerous studies have explored the factors associated with self-management. A systematic review has reported that longer time living with diabetes, financial difficulties, and low self-efficacy were the main obstacles to diabetes self-management [20]. Another study found that males, being old, married, duration of diabetes, the COVID-19 pandemic, reduced support from health professionals, and increased levels of anxiety and stress were associated with the self-management level of patients with diabetes [21].
Previous studies on diabetes self-management mainly focus on the level of self-management [18, 19], influencing factors [22, 23], and the effect of intervention strategies [24]. Some studies have also discussed the impact of the knowledge level or attitude on self-management behaviors in patients with diabetes [25–28]. However, little is known about the correlation and path relationship between knowledge, attitude, and self-management behaviors in patients with diabetes. Reliable evidence is warranted to provide further insight for decision-makers to evaluate management strategies designed for the prevention and treatment of diabetes. Knowledge, Attitude, and Practice (KAP) model was first proposed by Dr. Gcust in the 1960s and has been widely used in the field of public health [29]. KAP model suggests that knowledge is the basis of behaviors change, attitude is the driving force for behaviors change [30]. This study aims to investigate the level of knowledge, attitude and self-management behaviors in patients with diabetes based on KAP model. The relationship between knowledge, attitude and self-management behavior of diabetes patients was explored through path analysis.
Methods
Study Design and Setting
This cross-sectional study was conducted in Shandong Province from August to September 2019. Shandong is a major province in east China with a vast area and large population [31]. This study used a multi-stage stratified sampling method. First, three prefectures (Qingdao, Weifang, and Liaocheng) were selected based on their geographical location and socio-economic status. Second, one urban district and one rural county were selected in each prefecture. Third, three streets and three townships were selected in each district and each county, respectively. Fourth, three communities and three villages were selected in each street and each township, respectively. Finally, a total of 27 urban community health stations (CHSs) and 27 rural village clinics (VCs) were selected as sample areas.
Study Sample and Data Collection
This study is a cross-sectional study on knowledge, attitude and self-management behaviors of patients with diabetes. All the tests were double-tailed, α Value is 0.05, and the allowable error value is 0.05. The sample size calculated according to the formula “” should be 385 cases [32]. Considering the 20% loss rate, at least 482 patients with diabetes need to be included in this study.
A total of 900 diabetic patients who were included in the basic public health services, which is a long-term strategic deployment to address China’s public health problems and improve the health level of residents [33], were randomly selected as the participants from the sample areas. The inclusion criteria of diabetic patients were diagnosis of diabetes mellitus by the clinician. Diabetes patients with mental illness, communication difficulties and cognitive impairment were excluded. This study has been approved by the ethics committee of the School of Healthcare Management, Shandong University, China (ID: ECSHCMSDU20170401). All participants were voluntary to join the survey and provided written informed consent at the beginning of the study.
In this study, a questionnaire survey was used to collect data. A total of 863 valid questionnaires were collected from August to September 2019 with a response rate of 95.89% (863/900). Participants were convened in community health service stations or village clinics for one-on-one questioning by trained investigators. All questions in the questionnaire are filled out by the investigators, and both questioning and questionnaire filling were conducted simultaneously.
Measures and Variables
The diabetes self-management questionnaire (DSMQ) was used to measure the self-management level of the participants [34]. DSMQ is a reliable and effective instrument to effectively evaluate self-management behaviors associated with blood glucose control. This study used a self-designed scale based on the diabetes prevention and treatment guidelines as well as the existing literature to measure the knowledge and attitude among patients with diabetes mellitus [35, 36]. There were 16 items in the knowledge scale of diabetic patients, with 1 point for a correct answer, and the total score ranged from 0 to 16. The diabetic attitude scale had 11 five-point Likert scale questions with options including very agreed, agreed, moderate, disagreed, very disagreed, and was successively assigned points of 1, 2, 3, 4, and 5. For items 1, 2, 3, and 11, the points were assigned on a reverse scale. The total score was calculated as the sum of the points in 11 items, ranging from 0 to 55. Less than 34 refers to a poor attitude, 34–46 refers to a moderate attitude, and higher than 46 refers to a good attitude.
In addition, we also collected some risk factors that contribute to the outcome variables through the questionnaire survey. Social-demographic variables included age (years), gender (male, female), residence area (rural, unban), marital status (unmarried, married), and educational level (illiteracy, primary school, junior school, high school or above). Diabetes-related variables included family medical history (yes, no), diabetes complication (yes, no), blood glucose level (normal, abnormal), and duration of diabetes (years). The duration of diabetes refers to years from diagnosis of diabetes to investigation.
Statistical Analysis
IBM SPSS Statistics 25.0 was used to analyze the data. We used frequency (N), percentage (%), and mean (standard deviation [SD]) to show the socio-demographic and diabetes-related characteristics of the participants. One-way ANOVA and linear correlation analysis were used to analyze the categorical and continuous factors associated with self-management behaviors, respectively. Multiple linear regression analysis was carried out on the factors associated with self-management behaviors, and dummy variables were set for the categorical variables with more than two groups, including educational level. Path analysis was used to examine the mediation effect of attitude on the relationships between knowledge and self-management behaviors. All the tests were double-tailed and a p values ≤ 0.05 was considered to be statistically significant.
Results
A total of 863 patients with diabetes (male 33.2% and female 65.8%) were enrolled in this study. The mean age (SD) was 51.21 (8.53) years, and the mean duration of diabetes (SD) was 8.69 (6.24) years. The mean score (SD) of diabetes knowledge was 11.32 (3.28), and the mean score (SD) of diabetes attitude was 44.48 (6.17). Diabetes patients from rural areas accounted for 45% (388/863), 10.3% of the patients were unmarried, only 16.2% had a high school education or above, nearly 1/3 of the patients had a family history of diabetes, 36.1% had diabetic complications, and 34.3% of the patients had abnormal blood glucose levels. Better diabetes self-management behavior was more likely to be observed in participants living in urban areas (F = 13.678, p < 0.001), with no diabetes complication (F = 6.914, p < 0.001), higher diabetes knowledge level (r = 0.242, p < 0.001) and higher diabetes attitude (r = 0.464, p < 0.001) (Table 1).
TABLE 1
| Variate | Mean ± SD/n (%) | Diabetes self-management behaviors | ||
|---|---|---|---|---|
| Mean | SD | F/r | ||
| All | 863 (100.0) | 35.01 | 6.87 | |
| Gender | 0.01 | |||
| Male | 286 (33.2) | 35.04 | 7.53 | |
| Female | 576 (65.8) | 35.01 | 6.53 | |
| Residence area | 13.68*** | |||
| Rural | 388 (45.0) | 34.06 | 7.28 | |
| Urban | 475 (55.0) | 35.79 | 6.42 | |
| Marital status | 3.03 | |||
| Unmarried | 89 (10.3) | 33.82 | 6.48 | |
| Married | 772 (89.7) | 35.16 | 6.91 | |
| Educational level | 2.13 | |||
| Illiteracy | 217 (25.2) | 34.36 | 6.52 | |
| Primary school | 278 (32.3) | 34.75 | 6.85 | |
| Junior school | 227 (26.3) | 35.34 | 6.93 | |
| High school or above | 140 (16.2) | 36.09 | 7.21 | |
| Family medical history | 0.19 | |||
| Yes | 285 (33.1) | 35.17 | 6.64 | |
| No | 576 (66.9) | 34.95 | 6.96 | |
| Diabetes complication | 6.91** | |||
| No | 546 (63.9) | 35.47 | 6.92 | |
| Yes | 309 (36.1) | 34.19 | 6.73 | |
| Blood glucose level | 0.12 | |||
| Normal | 294 (34.3) | 35.17 | 6.67 | |
| Abnormal | 564 (65.7) | 34.99 | 6.86 | |
| Age (years) | 55.21 ± 8.53 | 35.01 | 6.87 | −0.05 |
| Duration of diabetes (years) | 8.69 ± 6.24 | 35.01 | 6.87 | 0.04 |
| Diabetes knowledge | 11.32 ± 3.28 | 35.01 | 6.87 | 0.24*** |
| Diabetes attitude | 44.48 ± 6.17 | 35.01 | 6.87 | 0.46*** |
Characteristics and the single analysis of diabetes self-management behaviors (China, 2019).
Abbreviation: SD, standard deviation.
Notes: *p < 0.05. **p < 0.01. ***p < 0.001. “F” refers to the variance value in one-way ANOVA. “r” refers to the correlation coefficient value in linear correlation analysis. The last four independent variables report “r”, and the remaining independent variables report “F”.
Table 2 presents the factors associated with diabetes self-management behaviors. In Model 1, after adjusting for the covariates, higher diabetes knowledge level (β = 0.272, p < 0.001) was associated with better diabetes self-management behaviors. In Model 2, after additionally adjusting for diabetes attitude, both diabetes knowledge (β = 0.174, p < 0.001) and diabetes attitude (β = 0.428, p < 0.001) were positively associated with diabetes self-management. However, the partial regression coefficients of diabetes knowledge decreased, indicating a mediation effect of diabetes attitude on the association between diabetes knowledge and self-management behaviors. Being younger (β = −0.071, p < 0.05), living in urban areas (β = 0.091, p < 0.01) and having less diabetes complication (β = −0.077, p < 0.05) were independently associated with greater self-management behaviors.
TABLE 2
| Model 1 | Model 2 | |
|---|---|---|
| Gender (Ref. = Male) | ||
| Female | 0.015 (−0.786, 1.226) | −0.016 (−1.155, 0.690) |
| Residence area (Ref. = Rural) | ||
| Urban | 0.079 (0.100, 2.032)* | 0.091 (0.361, 2.125)** |
| Marital status (Ref. = Unmarried) | ||
| Married | 0.044 (−0.520, 2.443) | −0.001 (−1.372, 1.326) |
| Educational level (Ref. = Illiteracy) | ||
| Primary school | −0.054 (−1.999, 0.442) | −0.068 (−2.097, 0.137) |
| Junior school | −0.018 (−1.679, 1.127) | −0.045 (−1.970, 0.596) |
| High school or above | −0.002 (−1.684, 1.612) | 0.021 (−1.115, 1.900) |
| Family medical history (Ref. = Yes) | ||
| No | −0.022 (−1.290, 0.649) | −0.028 (−1.290, 0.477) |
| Diabetes complication (Ref. = No) | ||
| Yes | −0.121 (−2.648, −0.746)*** | −0.077 (−1.954, −0.208)* |
| Blood glucose level (Ref. = Normal) | ||
| Abnormal | −0.054 (−1.722, 0.195) | −0.018 (−1.132, 0.624) |
| Age (years) | −0.104 (−0.141, −0.023)** | −0.071 (−0.109, −0.002)* |
| Duration of diabetes (years) | −0.004 (−0.083, 0.073) | −0.040 (−0.115, 0.029) |
| Diabetes knowledge | 0.272 (0.409, 0.715)*** | 0.174 (0.214, 0.500)*** |
| Diabetes attitude | — | 0.428 (0.404, 0.543)*** |
| Constant | 33.395 (29.624, 37.165)*** | 14.153 (9.697, 18.610)*** |
| R 2 | 0.10 | 0.27 |
Factors associated with self-management behaviors in diabetes patients by linear regression [β (95% CI)] (China, 2019).
Abbreviation: Ref., reference. Notes: *p < 0.05. **p < 0.01. ***p < 0.001.
Notes: Model 1 adjusted for all covariates associated with diabetes self-management behaviors without “Diabetes attitude.” Model 2 additionally included “Diabetes attitude.”
We further examined the mediation effect of attitude between their knowledge and self-management behaviors in patients with diabetes in Table 3. The findings indicate a partially mediation effect of attitude, since 95% CI in both direct effect (0.214, 0.500) and indirect effect (0.142, 0.299) were above 0. In addition, the direct effect of knowledge on self-management behaviors was 0.357, accounting for 62.09% of the total effect. The indirect effect of knowledge on self-management behaviors through attitude was 0.218, accounting for 37.91% (Table 3). The standardized path coefficients were shown in Figure 1.
TABLE 3
| Effect | SE | t | p | 95% CI | |
|---|---|---|---|---|---|
| Total effect of X on Y | 0.575 | 0.079 | 7.320 | 0.000 | (0.421∼0.730) |
| Direct effect of X on Y (c’) | 0.357 | 0.073 | 4.902 | 0.000 | (0.214∼0.500) |
| Indirect effect of X on Y (a × b) | 0.218 | 0.040 | — | — | (0.142∼0.299) |
Mediation effect of attitude between knowledge and self-management behaviors in diabetes patients (China, 2019).
FIGURE 1
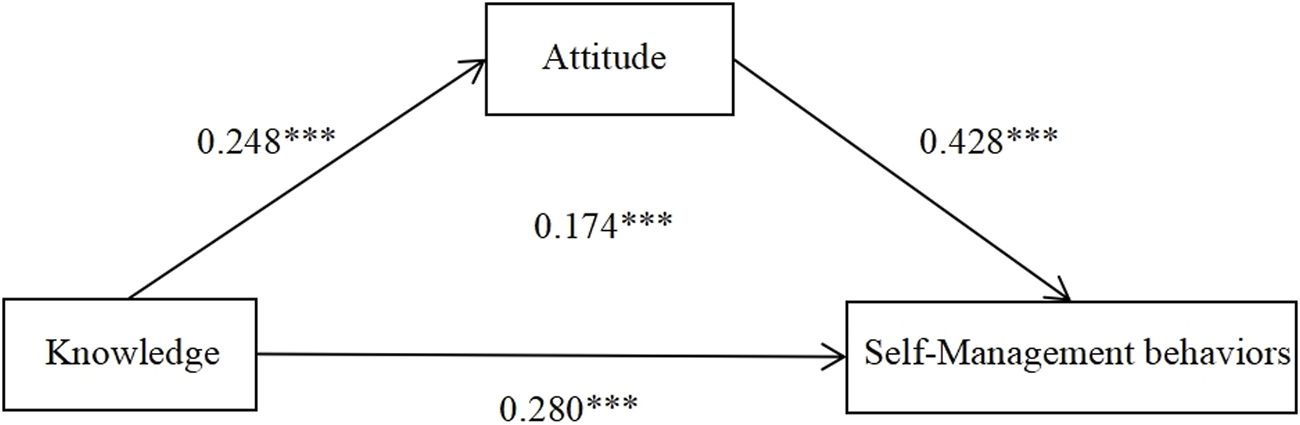
Mediation model with standardized path (β) coefficients of attitude as the mediator in the relationship between knowledge and self-management behaviors in patients with diabetes (China, 2019).
Discussion
This study described the status of knowledge, attitude, and behaviors of self-management, and innovatively revealed their interrelationships in 863 Chinese patients with diabetes. Our study reported a moderate level of self-management behaviors in patients with diabetes. The level of diabetes knowledge has a significant direct impact on their self-management behaviors, and the attitude exerted a mediation effect on the association between diabetes knowledge and self-management behaviors. Findings from this study contributed to doctors understand the relationship between knowledge, attitude and self-management behaviors of diabetes patients. And these findings provide a basis for improving the self-management behaviors of diabetes patients.
The mean score of the diabetes self-management questionnaire (DSMQ) in this study was 35.01 out of 48, which was higher than that of some other countries such as Pakistan (23.04) and Iran (33.1) [37, 38], and was ameliorated compared with previous studies (30.89) in China [39], but the self-management level still lower than that of some developed countries, such as such as Germany (37.44) and Hungary (36.72) [40, 41]. The self-management level of diabetes patients varies in different studies. This may result from the differences in the socio-economic status, the access to medical and health services and diabetes self-management education in different countries and regions [37–39]. It may also be related to the different definitions of self-management behaviors in patients with diabetes, the study design and the subject factors in different studies [40–42]. Our study reported that t the self-management of diabetic patients in China is at a moderate level. Good self-management of diabetes can reduce or delay the occurrence of complications, which is conducive to the control of diabetes [43]. It is urgent to design and implement tailored approaches to improving the self-management behaviors in diabetic patients.
Our study observed that the knowledge level was positively associated with their self-management behaviors in patients with diabetes. This is consistent with the results of previous studies [44, 45]. The higher the knowledge level of diabetes patients, the better their self-management behaviors. This may be because the higher the level of diabetes knowledge of patients, the easier it is to accept opinions about changing self-management behaviors [43]. Some studies have shown that health education on diabetes has a direct impact on self-management in patients [17]. Strengthening the health education of diabetes self-management and improving the knowledge level of patients is one effective measure to improve the self-management behaviors of diabetes patients [46]. Therefore, healthcare providers should carry out health education for patients with diabetes, and actively teach patients self-management knowledge such as eating habits and physical exercise [47]. This is beneficial to change the poor self-management behavior of diabetes patients, develop good living habits, and improve the condition of diabetes.
Our study also found that attitudes toward diabetes were partially mediating the association between knowledge and self-management behaviors. It indicated that the impact of diabetes patients’ knowledge on their self-management behaviors was partly through attitude. In other words, diabetes patients with a higher level of knowledge on health were easier to form a more positive health attitude, which was conducive to developing healthy diabetes self-management behaviors. Studies have reported that a positive attitude is the basis for improving self-management behaviors in patients with diabetes [48]. Therefore, diabetes patients not only need to improve their knowledge level, but also should maintain a positive attitude, which will help improve their self-management behaviors. Some studies have shown that support received from family and friends can help diabetes patients to have an optimistic and positive attitude [49]. Therefore, the future interventions to promote good self-management behaviors among patients should involve the companionship and support of family and friends. In addition, some studies also found that patients’ attitudes towards diabetes were affected by their knowledge level [45]. Thus, in the future diabetes health education, healthcare providers should also pay attention to patients’ attitudes towards diabetes. Enhance patients’ awareness of the importance of self-management, promote patients’ positive attitude towards diabetes, and then have good self-management behaviors.
In addition, this study demonstrated significant associations between some socio-demographic characteristics and diabetes self-management behaviors. We observed that the level of self-management was better in diabetic patients living in urban areas compared to those living in rural areas. This may result from the fact that urban areas have more opportunities to access information about diabetes self-management through media, books, and the internet [50]. We also found that older patients had lower levels of diabetes self-management. The self-management level of patients with longer diabetes duration was poor. And the diabetes patients with severe complications had worse self-management behaviors. Therefore, healthcare providers should pay more attention to the above types of diabetes patients, and prevent them from worsening their diabetes due to poor self-management.
Limitations
This study is subject to several limitations. First, this is a cross-sectional study, which can most appropriately reveal the associations of the variables observed at a single time point, instead of causality. Therefore, longitudinal datasets are warranted to identify the causality relationships in future research. Second, the knowledge and attitude scales of diabetic patients used in this study were self-designed according to previous studies, but they were proved to have acceptable Cronbach’s Alpha (0.781 and 0.701). Third, the investigators collected clinical covariates such as diabetes complication, blood glucose level, and duration of diabetes through questionnaires, which may lead to recall bias. Finally, the samples in this study were only from three prefectures in Shandong Province, which may affect the representativeness of the research samples. However, we have obtained samples from different urban districts and rural counties according to geographical location and economic development level with similar demographic characteristics to the national average, so our results still provide insights into self-management in Chinese patients with diabetes.
Conclusion
The diabetes knowledge and attitude were positively correlated with self-management behaviors in patients with diabetes. Good self-management behaviors were based on the good knowledge level and positive attitude of patients with diabetes. The attitude toward diabetes plays a partial mediation role in the association between knowledge and self-management behaviors. These findings provide practical evidence and policy implications for diabetes-related healthcare services. Therefore, it is warranted to tailor health education programs for patients with diabetes to improve health awareness, attitudes, and self-management behaviors, and control blood glucose levels throughout all stages of diabetes.
Statements
Data availability statement
The data used and analyzed during the study are available from the corresponding author on reasonable request.
Ethics statement
The studies involving human participants were reviewed and approved by the institutional review board of Shandong University School of Public Health (Theory No.: ECSHCMSDU20170401). The patients/participants provided their written informed consent to participate in this study.
Author contributions
HW and YZ designed the study. HW, YZ, BZ, CC, and XF conducted the data collection. YZ performed statistical analysis of data and wrote the first draft. SS and HW revised and edited the manuscript. All authors contributed to the article and approved the submitted version.
Funding
The research was supported by the Shandong Provincial Natural Science Foundation Youth Project (ZR2016HQ02) and the National Key Research and Development Program of China (2020YFC2006505).
Acknowledgments
Our thanks go to all the participants of the study for their valuable cooperation.
Conflict of interest
The authors declare that they do not have any conflicts of interest.
References
1.
Raoufi AM Tang X Jing Z Zhang X Xu Q Zhou C . Blood Glucose Monitoring and Its Determinants in Diabetic Patients: A Cross-Sectional Study in Shandong, China. Diabetes Ther (2018) 9:2055–66. 10.1007/s13300-018-0499-9
2.
Sun H Saeedi P Karuranga S Pinkepank M Ogurtsova K Duncan BB et al IDF Diabetes Atlas: Global, Regional and Country-Level Diabetes Prevalence Estimates for 2021 and Projections for 2045. Diabetes Res Clin Pract (2022) 183:109119. 10.1016/j.diabres.2021.109119
3.
Ma RCW . Epidemiology of Diabetes and Diabetic Complications in China. Diabetologia (2018) 61:1249–60. 10.1007/s00125-018-4557-7
4.
Lau DC . Are Diabetes Care Providers Too Glucocentric?Can J Diabetes (2016) 40:479–81. 10.1016/j.jcjd.2016.10.004
5.
Zhao Y . Research on the Present Situation, Problems and Countermeasures of Diabetes Management Under the K Medical Union in Suzhou. China: Soochow University (2020).
6.
Stellefson M Dipnarine K Stopka C . The Chronic Care Model and Diabetes Management in US Primary Care Settings: A Systematic Review. Prev Chronic Dis (2013) 10:E26. 10.5888/pcd10.120180
7.
Peng C Qiu W . Research Progress in Community Management of Diabetes Mellitus. China Med Innovation (2017) 14:145–8. 10.3969/j.issn.1674-4985.2017.24.044
8.
Gofin J Gofin R Abramson JH Ban R . Ten-Year Evaluation of Hypertension, Overweight, Cholesterol, and Smoking Control: The Chad Program in Jerusalem. Community Syndrome of Hypertension, Atherosclerosis and Diabetes. Prev Med (1986) 15:304–12. 10.1016/0091-7435(86)90049-6
9.
Nissinen A Berrios X Puska P . Community-Based Noncommunicable Disease Interventions: Lessons From Developed Countries for Developing Ones. Bull World Health Organ (2001) 79:963–70. 10.1590/S0042-96862001001000010
10.
Grady PA Gough LL . Self-Management: A Comprehensive Approach to Management of Chronic Conditions. Am J Public Health (2014) 104:E25–31. 10.2105/ajph.2014.302041
11.
Vadiee M . The UK “Expert Patient Program” and Self-Care in Chronic Disease Management: An Analysis. Eur Geriatr Med (2012) 3:201–5. 10.1016/j.eurger.2012.02.003
12.
Horsburgh MP Bycroft JJ Goodyear-Smith FA Roy DE Mahony FM Donnell EC et al The Flinders Programme of Chronic Condition Self-Management in New Zealand: Survey Findings. J Prim Health Care (2010) 2:288–93. 10.1071/hc10288
13.
Sugiyama T Steers WN Wenger NS Duru OK Mangione CM . Effect of a Community-Based Diabetes Self-Management Empowerment Program on Mental Health-Related Quality of Life: A Causal Mediation Analysis From a Randomized Controlled Trial. BMC Health Serv Res (2015) 15:115. 10.1186/s12913-015-0779-2
14.
Werfalli M Raubenheimer P Engel M Peer N Kalula S Kengne AP et al Effectiveness of Community-Based Peer-Led Diabetes Self-Management Programmes (Comp-Dsmp) for Improving Clinical Outcomes and Quality of Life of Adults With Diabetes in Primary Care Settings in Low and Middle-Income Countries (Lmic): A Systematic Review and Meta-Analysis. BMJ Open (2015) 5:e007635. 10.1136/bmjopen-2015-007635
15.
Jiang Y Mao F Dong W Zhang X Dong J . Lasting Effects of a Community-Based Self-Management Intervention for Patients With Type 2 Diabetes in China: Outcomes at 2-Year Follow-Up of a Randomized Trial. Asia Pac J Public Health (2021) 33:30–8. 10.1177/1010539520975266
16.
Alexandre K Campbell J Bugnon M Henry C Schaub C Serex M et al Factors Influencing Diabetes Self-Management in Adults: An Umbrella Review of Systematic Reviews. JBI Evid Synth (2021) 19:1003–118. 10.11124/jbies-20-00020
17.
Adam L O'Connor C Garcia AC . Evaluating the Impact of Diabetes Self-Management Education Methods on Knowledge, Attitudes and Behaviours of Adult Patients With Type 2 Diabetes Mellitus. Can J Diabetes (2018) 42:470–7. 10.1016/j.jcjd.2017.11.003
18.
Alrahbi H . Diabetes Self-Management (Dsm) in Omani With Type-2 Diabetes. Int J Nurs Sci (2014) 1:352–9. 10.1016/j.ijnss.2014.09.002
19.
Ji J Liu L Lou Q Yuan X Yao P Zhang D . Self-Management Behaviors and Glycemic Control in Patients With Type 2 Diabetes Mellitus. Chin J Nurs (2014) 49:617–20. 10.3761/j.issn.0254-1769.2014.05.026
20.
Schmidt-Busby J Wiles J Exeter D Kenealy T . Understanding 'Context' in the Self-Management of Type 2 Diabetes With Comorbidities: A Systematic Review and Realist Evaluation. Diabetes Res Clin Pract (2018) 142:321–34. 10.1016/j.diabres.2018.06.003
21.
Utli H Vural Dogru B . The Effect of the COVID-19 Pandemic on Self-Management in Patients With Type 2 Diabetics. Prim Care Diabetes (2021) 15:799–805. 10.1016/j.pcd.2021.07.009
22.
Luo X Liu T Yuan X Ge S Yang J Li C et al Factors Influencing Self-Management in Chinese Adults With Type 2 Diabetes: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health (2015) 12:11304–27. 10.3390/ijerph120911304
23.
Peng X Guo X Li H Wang D Liu C Du Y . A Qualitative Exploration of Self-Management Behaviors and Influencing Factors in Patients With Type 2 Diabetes. Front Endocrinol (Lausanne) (2022) 13:771293. 10.3389/fendo.2022.771293
24.
Chrvala CA Sherr D Lipman RD . Diabetes Self-Management Education for Adults With Type 2 Diabetes Mellitus: A Systematic Review of the Effect on Glycemic Control. Patient Educ Couns (2016) 99:926–43. 10.1016/j.pec.2015.11.003
25.
Coates VE Boore JRP . Knowledge and Diabetes Self-Management. Patient Educ Couns (1996) 29:99–108. 10.1016/0738-3991(96)00938-x
26.
von Arx LB Gydesen H Skovlund S . Treatment Beliefs, Health Behaviors and Their Association With Treatment Outcome in Type 2 Diabetes. BMJ Open Diabetes Res Care (2016) 4:e000166. 10.1136/bmjdrc-2015-000166
27.
Wang Q Zhang X Fang L Guan Q Guan L Li Q . Prevalence, Awareness, Treatment and Control of Diabetes Mellitus Among Middle-Aged and Elderly People in a Rural Chinese Population: A Cross-Sectional Study. PLoS One (2018) 13:e0198343. 10.1371/journal.pone.0198343
28.
van Smoorenburg AN Hertroijs DFL Dekkers T Elissen AMJ Melles M . Patients' Perspective on Self-Management: Type 2 Diabetes in Daily Life. BMC Health Serv Res (2019) 19:605. 10.1186/s12913-019-4384-7
29.
Hu W Li T Cao S Gu Y Chen L . Influence of Nurse-Led Health Education on Self-Management Ability, Satisfaction, and Compliance of Elderly Patients With Chronic Obstructive Pulmonary Disease Based on Knowledge, Belief, and Practice Model. Comput Math Methods Med (2022) 2022:1782955. 10.1155/2022/1782955
30.
Alzghoul BI Abdullah NA . Pain Management Practices by Nurses: An Application of the Knowledge, Attitude and Practices (Kap) Model. Glob J Health Sci (2015) 8:154–60. 10.5539/gjhs.v8n6p154
31.
Wang H Zhang Y Sun L . The Effect of Workplace Violence on Depression Among Medical Staff in China: The Mediating Role of Interpersonal Distrust. Int Arch Occup Environ Health (2021) 94:557–64. 10.1007/s00420-020-01607-5
32.
Zheng W He F . Sample Size Calculation Method for Current Situation Investigation. Prev Med (2020) 32:647–8. 10.19485/j.cnki.issn2096-
33.
Qin J . Progress in Basic Public Health Service Project in China. Chin J Public Health (2017) 33:1289–97. 10.11847/zgggws2017-33-09-01
34.
Schmitt A Gahr A Hermanns N Kulzer B Huber J Haak T . The Diabetes Self-Management Questionnaire (Dsmq): Development and Evaluation of an Instrument to Assess Diabetes Self-Care Activities Associated With Glycaemic Control. Health Qual Life Outcomes (2013) 11:138. 10.1186/1477-7525-11-138
35.
Wang W Liu X Chen B Li C Feng N . Development on the Diabetes Self-Management Knowledge, Attitude, and Behavior Assessment Scale (Dskab). Chin J Prev Med (2016) 50:40–9. 10.3760/cma.j.issn.0253-9624.2016.01.008
36.
Society CD . Guideline for the Prevention and Treatment of Type 2 Diabetes Mellitus in China (2020 Edition) (Part 1). Chin J Pract Intern Med (2021) 41:668–95. 10.19538/j.nk2021080106
37.
Bukhsh A Lee SWH Pusparajah P Schmitt A Khan TM . Psychometric Properties of the Diabetes Self-Management Questionnaire (Dsmq) in Urdu. Health Qual Life Outcomes (2017) 15:200. 10.1186/s12955-017-0776-8
38.
Nakhaeizadeh M Khalooei A . Psychometric Properties of the Persian Version of the Diabetes Self-Management Questionnaire for Patients With Type 2 Diabetes in Iran. Int J Prev Med (2021) 12:120. 10.4103/ijpvm.IJPVM_241_19
39.
Ma Q Jing K Guo Y . Self-Management Status and Influencing Factors of Diabetes Mellitus. Mod Prev Med (2019) 46:915–20.
40.
Brenk-Franz K Strauss B Tiesler F Fleischhauer C Ciechanowski P Schneider N et al The Influence of Adult Attachment on Patient Self-Management in Primary Care-The Need for a Personalized Approach and Patient-Centred Care. PLoS One (2015) 10:e0136723. 10.1371/journal.pone.0136723
41.
Vincze A Losonczi A Stauder A . The Validity of the Diabetes Self-Management Questionnaire (Dsmq) in Hungarian Patients With Type 2 Diabetes. Health Qual Life Outcomes (2020) 18:344. 10.1186/s12955-020-01595-7
42.
Ghannadi S Amouzegar A Amiri P Karbalaeifar R Tahmasebinejad Z Kazempour-Ardebili S . Evaluating the Effect of Knowledge, Attitude, and Practice on Self-Management in Type 2 Diabetic Patients on Dialysis. J Diabetes Res (2016) 2016:3730875. 10.1155/2016/3730875
43.
Yin X . Analysis of Self-Management Behavior and Its Influencing Factors in Patients With Type 2 Diabetes. Mod Nurse (2023) 30(02):47–50. 10.19791/j.cnki.1006-6411.2023.04.012
44.
Kueh YC Morris T Borkoles E Shee H . Modelling of Diabetes Knowledge, Attitudes, Self-Management, and Quality of Life: A Cross-Sectional Study With an Australian Sample. Health Qual Life Outcomes (2015) 13:129. 10.1186/s12955-015-0303-8
45.
Karbalaeifar R Kazempour-Ardebili S Amiri P Ghannadi S Tahmasebinejad Z Amouzegar A . Evaluating the Effect of Knowledge, Attitude and Practice on Self-Management in Patients With Type 2 Diabetes. Acta Diabetol (2016) 53:1015–23. 10.1007/s00592-016-0905-6
46.
Chatterjee S Davies MJ Heller S Speight J Snoek FJ Khunti K . Diabetes Structured Self-Management Education Programmes: A Narrative Review and Current Innovations. Lancet Diabetes Endocrinol (2018) 6(2):130–42. 10.1016/s2213-8587(17)30239-5
47.
ALSharit BA Alhalal EA . Effects of Health Literacy on Type 2 Diabetic Patients' Glycemic Control, Self-Management, and Quality of Life. Saudi Med J (2022) 43:465–72. 10.15537/smj.2022.43.5.20210917
48.
Cao D Yin W Bao L Zhang H Li X . Correlation Between Personality Traits, Attitudes and Self-Management Behavior in Patients With Type 2 Diabetes. Guangxi Med J (2019) 41(17):2262–5. 10.11675/j.issn.0253-4304.2019.17.32
49.
Shawon MS Hossain FB Adhikary G Das Gupta R Hashan MR Rabbi MF et al Attitude Towards Diabetes and Social and Family Support Among Type 2 Diabetes Patients Attending a Tertiary-Care Hospital in Bangladesh: A Cross-Sectional Study. BMC Res Notes (2016) 9:286. 10.1186/s13104-016-2081-8
50.
Niguse H Belay G Fisseha G Desale T Gebremedhn G . Self-Care Related Knowledge, Attitude, Practice and Associated Factors Among Patients With Diabetes in Ayder Comprehensive Specialized Hospital, North Ethiopia. BMC Res Notes (2019) 12:34. 10.1186/s13104-019-4072-z
Summary
Keywords
diabetes, self-management, knowledge, attitudes, behaviors
Citation
Zhang Y, Zhang B, Chen C, Feng X, Song S and Wang H (2023) The Mediation Effect of Attitude on the Association Between Knowledge and Self-Management Behaviors in Chinese Patients With Diabetes. Int J Public Health 68:1606022. doi: 10.3389/ijph.2023.1606022
Received
24 March 2023
Accepted
03 September 2023
Published
13 September 2023
Volume
68 - 2023
Edited by
Gabriel Gulis, University of Southern Denmark, Denmark
Reviewed by
Natasha Sobers, The University of the West Indies, Cave Hill, Barbados
Wondimeneh Shiferaw, Debre Berhan University, Ethiopia
Updates
Copyright
© 2023 Zhang, Zhang, Chen, Feng, Song and Wang.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Haipeng Wang, wanghaipeng@sdu.edu.cn
This Original Article is part of the IJPH Special Issue “Public Health and Primary Care, is 1+1=1?”
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.