Abstract
Objectives: Adolescents exposed to alcohol have increased risky sexual behaviors (RSBs); however, the association between alcohol consumption and RSBs has to be systematically and quantitatively reviewed. We conducted a meta-analysis of the literature to systematically and quantitatively review the association between alcohol consumption and RSBs in adolescents and young adults.
Methods: We searched for qualified articles published from 2000 to 2020 and calculated pooled odds ratios (ORs) using the random-effect model. We also conducted meta-regression and sensitivity analyses to identify potential heterogeneity moderators.
Results: The meta-analysis of 50 studies involving 465,595 adolescents and young adults indicated that alcohol consumption was significantly associated with early sexual initiation (OR = 1.958, 95% confidence interval (CI) = 1.635–2.346), inconsistent condom use (OR = 1.228, 95% CI = 1.114–1.354), and having multiple sexual partners (OR = 1.722, 95% CI = 1.525–1.945).
Conclusion: Alcohol consumption is strongly associated with RSBs, including early sexual initiation, inconsistent condom use, and multiple sexual partners among adolescents and young adults. To prevent the adverse consequences of alcohol consumption, drinking prevention programs should be initiated at an early age and supported by homes, schools, and communities.
Introduction
Alcohol consumption in adolescence can affect hormone secretion and the brain, disrupting secondary sex characteristics and damaging brain cells (1). Alcohol consumption at an early age causes disability and accounts for 13.5% of deaths among those aged 20 to 39, causing social and economic losses across our society along with health issues (2). According to the World Health Organization (WHO), 26.5% of all adolescents aged 15–19 years of age worldwide are current drinkers, which is approximately 155 million adolescents. The highest prevalence rates of current drinking are in the WHO European Region (43.8%), followed by the Region of the Americas (38.2%) and the Western Pacific Region (37.9%). While heavy episodic drinking (HED) is less common among adolescents than in the total population, it peaks at the age of 20–24 years, with prevalence rates among drinkers in this age group higher than in the total population, except in the Eastern Mediterranean Region. Among current drinkers aged 15–24 years, prevalence of HED is high among men, with some studies reporting rates as high as 54.2% (3).
Alcohol consumption during adolescence is one of the factors that increase risky sexual behaviors (RSBs) (4, 5). Adolescents with substance abuse issues, specifically alcohol abuse, had approximately twice as many sexual partners and were 70% more likely to be diagnosed with sexually transmitted diseases (STDs) than adolescents without substance abuse issues (6). According to the literature on the relationship between alcohol consumption and early sexual experience in middle school students: Yu et al (7) reported a 2.35-fold increase in early sexual initiation when drinking alcohol, Hong et al (8) reported a 1.43-fold increase, Ayhan et al (9) reported a 2.13-fold increase, and Bersamin et al. (10) reported a 7.4-fold increase.
Depending on the study, the age of first sexual experience among adolescents varies, with Korean adolescents having their first sexual experience at 13.2 years old on average (11), specifically 12.1 years for boys and 13.9 years for girls. Ayhan et al (9) indicated that the first sexual experience occurred before the age of 14 in most studies. In particular, 13.4% of female adolescents had their first sexual experience after drinking alcohol (5). This early sexual debut increases the risk of unwanted pregnancy and STDs (12). Adolescents not using a condom during sexual experiences was reported at 34.4% in a study by Wilson, Asbridge et al (13), 46.9% in a study by Rios-Zertuche et al (14), and 41.1% in a study by Mlunde et al (15), thereby demonstrating that the rate of condom use among adolescents is very low. Alcohol consumption in adolescents is one of the factors for increasing inconsistent condom use, and Sanchez et al (16) reported that 57.1% of adolescents with drinking alcohol experience did not use condoms during sexual intercourse. The most used definition of binge drinking in research is based on the National Institute on Alcohol Abuse and Alcoholism (NIAAA)’s definition of a pattern of drinking that brings a person’s blood alcohol concentration (BAC) to 0.08 g/dL or higher, which is typically reached after consuming 4 drinks for women or 5 drinks for men within 2 h (17). This definition is consistent with that used by Wilson et al (13) who found that binge drinking, as defined by the NIAAA, increased inconsistent condom use by 1.1 times among adolescents, and Sanchez et al (16) reported this to be 1.27 times. Inconsistent condom use in adolescents can increase the prevalence of STDs and lead to teenage pregnancies (18).
Alcohol consumption in adolescents increases the probability of having more than three sexual partners by 3.37 times (19). Particularly, compared to female adolescents, male adolescents have a 2.9-fold increase in the likelihood of having multiple sexual partners (13). Moreover, the number of sexual partners increased by 2.41 times in current binge drinkers compared to current light drinkers. Drinking alcohol during adolescence increases the likelihood of regretting having sexual intercourse (19), and if they continue to abuse alcohol after adolescence, these sexual behaviors will likely continue into adulthood (20).
Therefore, alcohol consumption during sexual intercourse reduces sexual inhibition and increases RSBs by impacting adolescents’ judgment. However, studies analyzing the relationship between alcohol consumption and RSBs among adolescents have measured alcohol consumption in various ways according to fragmentary questions, amount of alcohol consumption (glass) or frequency of alcohol consumption, and time point (past alcohol consumption and current alcohol consumption). As the results differ by sex, it is difficult to synthesize and summarize the factors affecting alcohol consumption. Additionally, no meta-analysis has integrated each sex behavior by separating early sexual debut, inconsistent condom use, and multiple sexual partners for RSBs, which has a higher risk of STDs and teenage pregnancies—rather than integrating alcohol consumption and sexual experience. Thus, this study conducted a meta-analysis to identify the integrated effect of alcohol consumption in adolescents and young adults on the three types of RSBs and to determine whether the effect differs according to sex (male and female). Additionally, this study focused on analyzing the relationship between early sexual initiation, inconsistent condom use, and multiple sexual partners among RSBs due to alcohol consumption, and aimed to provide the derived results as fundamental data for health education and program development for safe sexual behaviors and prevention of alcohol consumption among adolescents and young adults.
Methods
Design
We conducted a systematic review and meta-analysis, following the protocol reported in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) Statement (21). The study protocol was registered with the PROSPERO database under the registration number CRD42022301637.
Search Strategy
Eight electronic bibliographic databases were used: Cumulative Index to Nursing and Allied Health Literature (CINAHL), Cochrane Library, EBSCO, PubMed, PsycINFO, Web of Science, Database Periodical Information Academic (DBpia, Korea), and Research Information Sharing Service (RISS, Korea). These were chosen since they comprehensively covered relevant literature in our field of study. Additionally, CINAHL, Cochrane Library, and PsycINFO are well-known and widely used databases in healthcare and psychology research, respectively. Korean databases, DBpia and RISS, allowed us to retrieve relevant studies published in the Korean language.
We conducted a comprehensive literature review using two search strategies. The first strategy was to select studies that investigated the relationship between alcohol consumption and RSBs and included alcohol consumption as an independent variable affecting RSBs from large systematic reviews of RSB-related factors in individuals, peers, schools, and communities. We used the general keywords “factor(s) AND sexual behavior” or “risky sexual behavior” and “adolescent(s) or young adult(s)” through the title and abstract fields to identify relevant articles published between January 2000 and July 2020. The process of literature search, screening, and selection is presented in a separate research article (Ahn and Yang, 2022) for more detailed information. In the systematic review (Ahn and Yang, 2022), we included studies that examined the relationship between self-esteem and RSBs. However, for this meta-analysis, we selected studies that investigated the association between alcohol consumption and RSBs. This distinction is highlighted in the study inclusion criteria and is further explained in Figure 1.
FIGURE 1
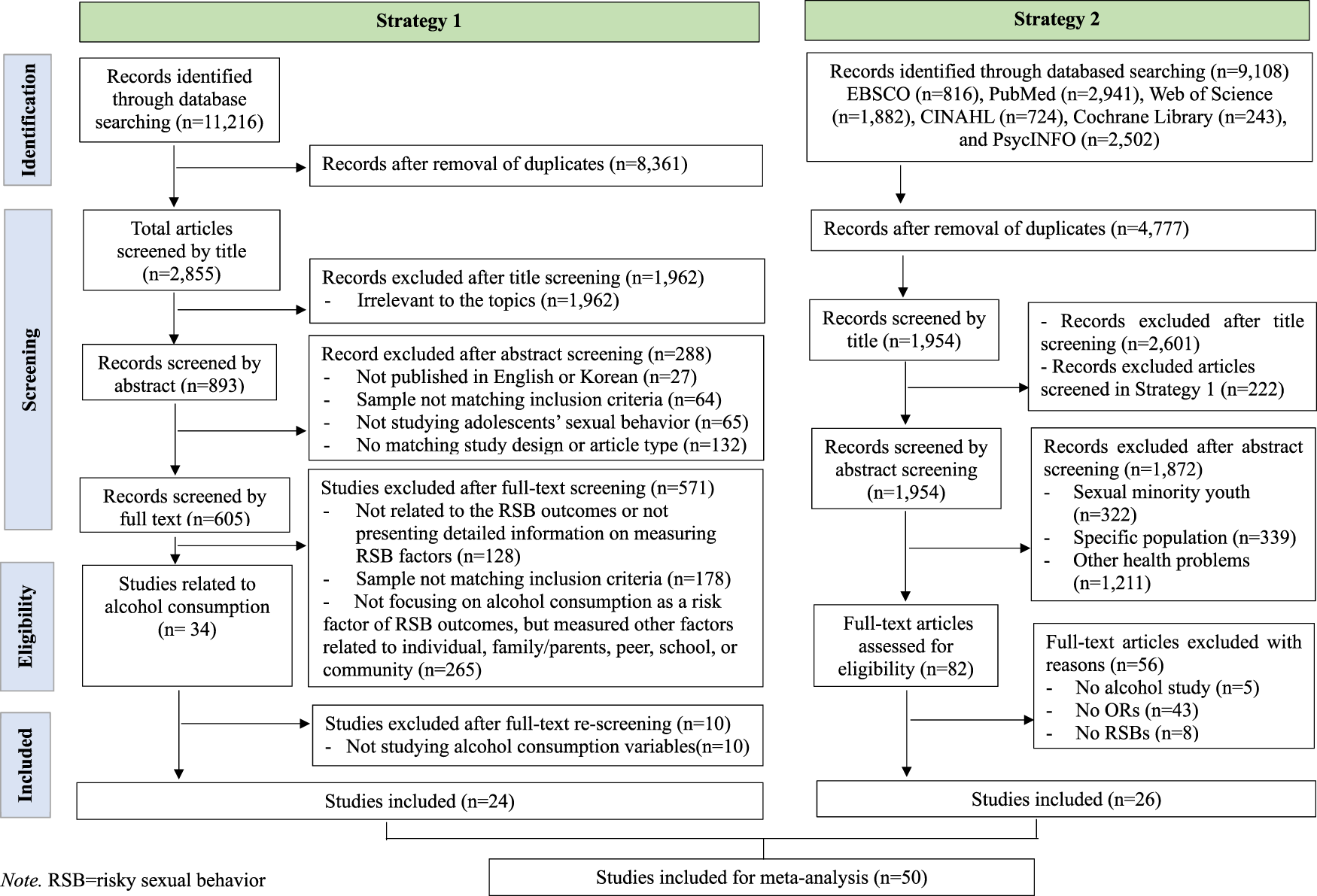
Flow chart of the selection process of studies included in the meta-analysis (Worldwide, 2001–2021).
The second search strategy used specific keywords to identify relevant articles. For example, in PubMed, we searched for articles using the following search terms: “Young Adult” [Mesh] OR “young adult*” OR “Adolescent” [Mesh] OR “adolescent*” OR “teen*” OR “youth*”), AND condom use (“Unsafe Sex” [Mesh] OR “unsafe sex” OR “unprotected sex” OR “high-risk sex” OR “unprotected intercourse” OR “condomless sex” OR “condom use” OR “condom compliance”) OR early sexual initiation (“Coitus” [Mesh] OR “Coitus” OR “First intercourse” OR “Sexual intercourse” OR “early sexual debut” OR “early sex*” OR “early sexual initiation”) OR multiple sexual partner (“Sexual Partners” [Mesh] OR “sexual partner*” OR “sex partner*” OR “multiple sexual partner*” OR “multiple sex partner*”).
Inclusion/Exclusion Criteria
Full-text versions of the retrieved articles were screened based on the pre-specified inclusion and exclusion criteria. The inclusion criteria were as follows: 1) target population aged 15–24; 2) investigating the association between alcohol consumption and RSBs; and 3) defined early sexual debut as initiation before the age of 14 years. The exclusion criteria were: 1) if the target populations were sexual minority youth (e.g., gay, bisexual, lesbian, homosexual, men who have sex with men, or transgender); specific population (homeless, juvenile, or military); 2) focusing on HIV (human immunodeficiency virus), STI (Sexually transmitted infections), or other mental health problems; 3) did not report the odds ratio of early sexual debut, inconsistent condom use, multiple sexual partners separately; 4) did not report direct alcohol consumption association; and 5) insufficient information to calculate effect size or insufficient effect size to convert to odd ratio. We excluded studies that focused on sexual minority youth because our primary focus was on the general adolescent population. While we acknowledge the importance of understanding the relationship between alcohol consumption and risky sexual behavior among sexual minority youth, we considered that the sexual behavior of sexual minority individuals might differ from that of heterosexual individuals.
Finally, we identified 50 articles through the two search strategies, with 24 and 26 articles selected through the first and second strategies, respectively. This comprehensive approach enabled us to identify all relevant studies published between January 2000 and July 2020 that investigated the relationship between alcohol consumption and RSB.
Data Extraction
Two independent researchers (CS and TK) conducted data extraction and study quality assessment, with a third researcher (YY) providing oversight to ensure accuracy and consistency. Any discrepancies between the two researchers were resolved through discussion and consensus. A standardized form was used to extract the following information: first author, year of publication, study country, total sample size, participant characteristics (e.g., mean age, gender distribution), measurements of alcohol consumption, and RSBs. OR and 95% CI for each type of RSB were abstracted by three researchers using a structured coding sheet. To reduce potential confounding variables and observational bias, adjusted estimates that controlled for demographic, individual, peer, school, and community variables were extracted if available. If multiple models were presented, we selected estimates from the last model that controlled for the most variables. This meta-analysis adhered to the Meta-Analysis of Observational Studies in Epidemiology Checklist, and the study selection flowchart was adapted from the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement (22, 23).
Quality Assessment
The methodological quality of the primary studies in this meta-analysis was assessed using the Newcastle-Ottawa Scale (NOS) adapted for cross-sectional studies (24). The assessment tool consisted of seven items: selection (representativeness of the sample, sample size, non-respondents, ascertainment of the exposure (risk factor), comparability, and outcome (assessment of the outcome and statistical test). For each item criterion, a maximum of five points for selection, two points for comparability, and three points for outcome could be given and then summed to a maximum of 10 points. Quality assessment results were evaluated as “good” if the NOS score was 7 points or higher, “fair” if the score was 5 points or higher or less than 7 points, and “poor” if the score was less than 5 points. Each of the two researchers independently conducted the quality assessment of the studies included in the analysis, and the final assessment scores were obtained after discussing a few discrepancy items.
Data Analysis
The data analysis was conducted using Comprehensive Meta-Analysis (CMA) Version 3 software (Biostat, Englewood, NJ, United States). Odds ratios and corresponding 95% confidence intervals were used to estimate the association between alcohol consumption and RSBs (early sexual initiation, inconsistent condom use, and multiple sexual partners). The extent of heterogeneity among the primary studies was assessed using Cochrane’s Q test (reported with x2 and p values) and Higgins I2 value (25). An I2 value of up to 25% indicated low heterogeneity, 50% indicated moderate heterogeneity, and ≥75% indicated high heterogeneity (25). Publication bias was evaluated using a funnel plot, trim-fill analysis, and Egger’s regression test. Sensitivity analysis was conducted by removing each study and examining the effect size (26). The random effects model was used for the meta-analysis, and a meta-regression analysis was performed with sex as a control variable. The level of significance for all analyses in this study was determined using a two-tailed p value of <0.05 with 95% confidence intervals.
Results
Characteristics of Primary Studies
Fifty studies were included in the meta-analysis based on the selection criteria of this study and the Newcastle-Ottawa Scale (NOS) assessment (Table 1). These studies were published between 2002 and 2021, and among the included studies, most were published in 2009, 2013 (n = 6 studies), followed by 2010 (n = 5 studies), 2017 (n = 4 studies), 2018 (n = 4 studies), and 2021 (n = 4 studies). Most published studies were written in English (n = 47 studies), and three were written in Korean; among the 50 articles, most studies were conducted in the United States (n = 23 studies), and seven were conducted in Europe (Croatia, Finland, Ireland, and the United Kingdom) and Asia (South Korea, China, Hong Kong, and Japan).
TABLE 1
| # of Reference | Author (year) | Country | Sample (N) | Study design/Data source | Mean age (range) | % of gender (M/F) | Measurement of alcohol consumption | Measurement of RSBs | Type of RSB | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| (27) | Mo et al. (2007) | Canada | N = 44,430 | A cross-sectional study | Mean age = Not presented (12–19 years) | M (47.7%) F (52.3%) |
Ever drink alcohol (yes/no) | 2. Inconsistent condom use: - Have not always used a condom during sexual intercourse in the past 12 months 3. Multiple sexual partners: Two or more sexual partners in the past 12 months |
2, 3 | ||
| (28) | Lepusic et al. (2013) | Croatia | N = 715 | A longitudinal study | Mean age = 17.9 (15–21 years) | F (100.0%) | Alcohol use -“How many alcoholic drinks do you usually have at the time?” |
2. Inconsistent condom use | 2, 3 | ||
| 3. Multiple sexual partners during the past 60 days (yes/no) | |||||||||||
| (14) | Rios-Zertuche et al. (2017) | Croatia | N = 919 | A cross-sectional study | Mean age = 14.7 (12–19 years) | M (41.5%) | Excessive alcohol consumption | 2. Used a condom when you last had sex | 2 | ||
| F (58.5%) | |||||||||||
| (29) | Scott-Sheldon et al. (2010) | United States | N = 221 | A cross-sectional study | Mean age = 19 (18–25 years) | F (67.0%) | Alcohol consumption | 2. Condom use during vaginal or anal sex | 2 | ||
| M(33.0%) | |||||||||||
| (30) | Mola et al. (2017) | Brazil | N = 1,275 | A cross-sectional study | Mean age = Not presented (12–24 years) | Not presented | Alcohol consumption during lifetime -non-user ∼ never drank alcohol during lifetime |
3. Number of sexual partners in lifetime -“with how many different people have you had sexual intercourse during your lifetime?” |
3 | ||
| (13) | Wilson et al. (2010) | Canada | N = 2,297 | A cross-sectional study | Mean age = 16.6 (9–12 Grade) | F (51.0%) M(49.0%) |
Alcohol use -having had 5 or more drinks on 2 or more occasions in the past month |
2. Condom non-use: Not using a condom during last vaginal intercourse | 2 | ||
| (15) | Mlunde et al. (2012) | Tanzania | N = 2,217 | A cross-sectional study | Mean age = Not presented (15–24 years) | F (39.8%) M (60.2%) |
Alcohol use in the past 1 year (yes/no) | 2. Condom use during last sexual intercourse | 2 | ||
| (31) | Kang et al. (2013) | Jamaica | N = 330 | A longitudinal study | Mean age = 14.7 (13–17 years) | F (100.0%) | Alcohol use -“In the past 3 months, how often did you drink beer, wine or liquor?” |
2. Condom use during last sexual intercourse (no vs. yes) -“did you use a condom?” |
2 | ||
| (32) | Kaltiala et al. (2015) | Finland | N = 2,070 | Prospective cohort study | Mean age = 17.6 (All ninth graders) | F (56.6%) M (43.4%) |
Frequent alcohol use -“How often do you drink alcoholic beverages?” |
3. Intercourse with five or more partners -“With how many partners have you had sexual intercourse?” (one/two/three/four/five or more) |
3 | ||
| (33) | Ramisetty et al. (2004) | United States | N = 2,657 | A three-stage cluster sample design | Mean age = Not presented (9–12 grade) | Not presented | Alcohol use and drinking pattern | 3. Multiple partners (lifetime and recent) - Number of people they had sex with in their lifetime and during the past 3 months (recent) |
3 | ||
| (34) | Kugbey et al. (2018) | Ghana | N = 1,648 | A secondary analysis of data from GSHS | Mean age = Not presented (11–18 years) | F (47.5%) M (52.5%) |
Alcohol use | 2. Condom use during last sexual intercourse -The last time you had sexual intercourse, did you or your partner use a condom or rubber? 3. Multiple sexual partners - during your life, how many people have you had sexual intercourse with? |
2, 3 | ||
| (35) | Ronis et al. (2011) | Canada | N = 1,100 | A cross-sectional study | Mean age = 14.8 (grades 9–11; 13–16 years) | F (64.7%) M (35.3%) |
Lifetime use of alcohol | 1. Age of first sexual intercourse (13–16 years) | 1 | ||
| (9) | Ayhan et al. (2015) | South America | N = 1,603 | A cross-sectional study | Mean age = 15 (13–18 years) | F (48%) M (52%) |
Alcohol | 1. Early first SI (sexual intercourse) - SI at the age of 15 years or before was defined as premature |
1 | ||
| (18) | Menna et al. (2014) | Ethiopia | N = 1,948 | A cross-sectional study | Mean age = Not presented (15–24 years) | F (60.7%) M (39.3%) |
Drinking alcohol (yes/no) | 3. Number of sexual partners -Number of sexual partners in previous year -Two or more |
3 | ||
| (36) | Peltzer et al. (2016) | Oceania (Fiji, Kiribati, Samoa, and Vanuatu) | N = 6,792 | A cross-sectional study | Mean age = Not presented (13–16 years) | F (50.3%) M (49.7%) |
Alcohol use -“During the past 30 days, how many days did you have at least one drink containing alcohol?” - 1 = 0 days to 7 = All 30 days |
1. Age of sexual debut - “How old were you when you had sexual intercourse for the first time?” - Early Sexual Debut (<14 Years) 2. Condom use -“The last time you had sexual intercourse, did you or your partner use a condom?” - Condom during last Sexual intercourse 3. Number of sexual partners - “During your life, how many people have you had sexual intercourse with?” - Two or more sexual partners |
1, 2, 3 | ||
| (37) | Kogan et al. (2010) | United States | N = 292 | A cross-sectional study | Mean age = Not presented (18–21 years) | F (59.9%) M (40.1%) |
Binge drinking -Four or more drinks at one sitting |
2. Unprotected intercourse -condom use at sexual intercourse during the past 3 months |
2 | ||
| (8) | Hong et al. (2018) | Republic of Korea | N = 68,043 | A secondary analysis of data from KYRBWS | Mean age = 13.56 (14–16 years) | Not presented | Alcohol consumption | 1. Coital experience (14–16) | 1 | ||
| (38) | Connor et al. (2013) | New Zealand | N = 2,921 | A cross sectional web-based survey | Mean age = Not presented (17–25 years) | F (61.0%) M (39.0%) |
Alcohol consumption - Questionnaire (Bohn et al., 1995) were used to assess alcohol consumption in the previous 4-week period on a scale of 0–12 (AUDIT-C) - 1. How often do you have a drink containing alcohol? −2. How many drinks do you have on a typical day when you are drinking? - 3. How often have you had 6 or more drinks on one occasion? |
2. Condom use at last sexual intercourse Did you use a condom the last time you had sex? (yes, no) |
2 | ||
| (39) | Seidu et al. (2021) | Namibia | N = 4,531 | A secondary analysis of data from GSHS | Mean age = Not presented (grade 6–12) | Not presented | Alcohol use -During the past 30 days, on how many days did you have at least one drink containing alcohol? |
3. Multiple sexual partners - During your life, how many people have you had sexual intercourse with? |
3 | ||
| (40) | Yarber et al. (2002) | United States | N = 1,130 | A secondary analysis of data from YRBS | Mean age = M (15.5 years) F (15.4 years) (14–18 or older) |
F (50.4%) M (49.6%) |
Binge drank past 30 days | 3. Multiple sexual partners during one’s lifetime - having two or more sexual partners during one’s lifetime |
3 | ||
| (41) | Benotsch et al. (2013) | United States | N = 763 | A cross-sectional study | Mean age = 18.9 years (18–25 years) | Not presented | Alcohol use - The frequency of use of alcohol in the previous 3 months |
2. Total number of unprotected sex (no condom used) - Vaginal or anal sex acts in the past 3 months 3. Number of sexual partners during one’s lifetime |
2, 3 | ||
| (16) | Sanchez et al. (2013) | Brazil | N = 17,371 | A cross sectional study | Mean age = Not presented (13–18 years) | Not presented | Alcohol use | 2. Sexual intercourse without condom use -Sexual intercourse without condom use during the past month (30 days) |
2 | ||
| (42) | Lee et al. (2010) | United States | N = 1,073 | National longitudinal study of Add Health | Mean age = Not presented (18–27 years) | Not presented | Binge drinking - “Over the past 12 months, how many days did you drink alcohol (five or more drinks in a row?)” |
2. Not using condom during recent sexual intercourse - “The most recent time you had vaginal intercourse—did you/your partner use a condom?’’ 3. Four or more sexual partners during one’s lifetime - “How many partners have you ever had vaginal intercourse with? Even if only once.” |
2, 3 | ||
| (43) | Agu et al. (2018) | Jamaica | N = 3,365 | A secondary analysis of data from NSS | Mean age = = Not presented (grade 8, 10, 11, 12) | Not presented | 1. Lifetime alcohol consumption 2. Alcohol consumption: past 12 months 3. Alcohol consumption: past 30 days |
2. Non-condom use -non-condom use during sex |
2 | ||
| (44) | Bartholomew et al. (2021) | London | N = 509 | A cross sectional study | Mean age = 17 M (18.1 years) F (17.8 years) (16–24 years) |
F (53.0%) M (47.0%) |
At least one episode of being drunk in the past month | 3. ≥2 sexual partners in the past year | 3 | ||
| (45) | Brown et al. (2007) | United States | N = 547 | A cross-sectional study | Mean age = Not presented (18 or older) | Not Presented | Alcohol use - Consumed alcohol: number of drinks consumed |
2. Unprotected vaginal sex during the most recent sexual encounter -Their most recent sexual experience, including items assessing which sexual behaviors occurred (i.e., oral, vaginal, and anal sex) -Respondents also indicated if a condom was used |
2 | ||
| (46) | Kiene et al. (2009) | United States | N = 116 | A longitudinal cohort daily diary study | Mean age = 19.15 | F (57.8%) M (42.2%) |
Daily alcohol consumption (number of drinks) - The number of drinks 30 consumed “last night.” |
2. Unprotected sex - Unavailability of condoms |
2 | ||
| (47) | Adhikari (2010) | Nepal | N = 1,137 | A cross sectional study | Mean age = Not presented (Grades 11 and 12; 15–19 or 20 and above | F (49.6%) M (50.4%) |
Alcohol consumption | 2. Condom use - Condom use during first sexual intercourse |
2 | ||
| (10) | Bersamin et al. (2006) | United States | N = 1,105 | A longitudinal study | Mean age = 14.1 (12–16 years) | F (48.2%) M (51.8%) |
Heavy drinking - How often, during the past 30 days, had the respondents had five or more alcoholic drinks within a 2-h period |
1. Sexual activity (sexual intercourse) -Vaginal sex (“Have you ever had sexual intercourse?”) -Yes/no |
1 | ||
| (48) | Nkansah-Amankra et al. (2011) | United States | N = 1,474 | A cross sectional data from the YRBS | Mean age = Not presented (grade 9–12) | F (49.1%) M (50.9%) |
1. Alcohol use - Non-drinkers (no alcohol in the past 30-day period), current light drinkers (1 drink in the past 30 days but 5 drinks in a row), and current binge drinkers (5 or more drinks in a row) |
1. Age at first sexual intercourse - Young adolescents (11–14 years) 3. Number of current sexual partners - Number of sexual partners in the past 3 months - >2 Sexual partners |
1, 3 | ||
| (56) | Page and Hall (2009) | Africa | N = 22,949 | A secondary analysis of data from GSHS | Mean age = Not presented (13–15 years) | Not presented | Alcohol use -“During the past 30 days, on how many days did you have at least 1 drink containing alcohol? | 1. “How old were you when you had sexual intercourse for the first time?” (had sex before age 13) | 1 | ||
| (7) | Yu et al. (2014) | Korea | N = 37,297 | A cross sectional study | Mean age = Not presented (12–15 years) | F (48.3%) M (51.7%) |
Present alcohol consumption -”In the past 30 days, on how many days did you drink at least one drink?” |
1. Sexual debut - Sexual intercourse with same or opposite sex |
1 | ||
| (50) | Gwon et al. (2015) | Korea | N = 74,186 | A secondary analysis of data from Korea Youth Risk Behavior Web-based Survey | Mean age = Not presented (12–15 years) | F (47.9%) M (52.1%) |
Ever drinking | 1. Sexual debut - Sexual intercourse with same or opposite sex |
1 | ||
| (51) | Brouwer et al. (2019) | United States | N = 241 | A cross-sectional study | Mean age = 18.9 (18–22 years) | F (69.7%) M (30.3%) |
Alcohol use | 3. Number of sexual partners - Sexual contact as vaginal intercourse, oral sex, or anal sex and defines a sexual partner as an individual with whom one engages in one or more of these acts |
3 | ||
| (52) | Choi et al. (2016) | HongKong | N = 666 | A cross sectional study | Mean age = 20.03 | F (54.1%) M (44.4%) [*did not answer (1.5%)] |
Drinking habit | 2. Condom use - Consistent vs. inconsistent - Condom use during the last sexual intercourse |
2 | ||
| (53) | Lewis et al. (2012) | United States | N = 1,468 | A cross-sectional study | Mean age = 19.9 (18–25 years) | F (56.4%) M (43.6%) |
Drinking during hookup - Number of drinks they had directly prior to or during the most recent hookup |
2. Condom use - “During this hookup, did you or your partner use a condom?” |
2 | ||
| (54) | Kuortti et al. (2009) | Finland | N = 247 | A cross sectional study | Mean age = 17.27 (15–18 years) | F (100.0%) | Binge drinking | 3. Multiple sexual partners | 3 | ||
| (55) | Lavikainen et al. (2009) | Finland | N = 100,790 | A secondary analysis of data from SHPS | Grade 8 (50,569) -Mean age = 14.8 Grade 9 (48,132) Mean age = 15.8 |
Grade 8 -F (49.6%) -M (50.4%) Grade 9 -F (48.9%) -M (51.1%) |
Drinking style 1) Frequency of drinking alcohol: “How often do you use alcohol?” 2) Drunkenness related drinking: frequency of drunkenness: “How often do you use alcohol until you are really drunk?” |
3. Three or more sexual partners -“How many different partners have you had sexual intercourse with?” |
3 | ||
| (5) | Young et al. (2018) | Ireland | N = 4,494 | A cross-sectional study | Mean age = Not presented (15–18 years) | F (46.2%) M (53.8%) |
Alcohol involvement | 1. Sexual initiation (very early sexual initiation (<14 years) - “Have you ever had sexual intercourse?” -“How old were you when you had sexual intercourse for the first time?” |
1 | ||
| (4) | Pengpid et al. (2021) | Africa (Mozambique) | N = 1,918 | A secondary analysis of data from GSHS | Mean age = Not presented (11–18 years) | Not presented | Current alcohol use - “During the past 30 days, on how many days did you have at least one drink containing alcohol?” |
2. Condom use - “The last time you had sexual intercourse, did you or your partner use a condom?” 3. Number of sexual partners - “During your life, how many people have you had sexual intercourse with?” |
2, 3 | ||
| (49) | Patrick et al. (2009) | United States | N = 218 | A cross-sectional study | Mean age = 18.85 (18.12–20.74 years) | Not presented | Alcohol use, - Number of standard drinks consumed the day prior |
2. Condom use with penetrative sex - Condom use was coded only for days with penetrative sex as 0 = no and 1 = yes |
2 | ||
| (57) | Woodrome et al. (2006) | United States | N = 117 | A cross-sectional study | Mean age = 16.2 (14–17 years) | F (100.0%) | Alcohol use concordance | 2. Condom non-use | 2 | ||
| (19) | Agius et al. (2013) | Australia | N = 450 | A secondary analysis of data from IYDS | Mean age = 17.0 (Grade 5, 7 and 9) | F (56.0%) M (44.0%) |
Drinking 1) Binge drinking: -”Think back over the past 2 weeks, how many times have you had five or more drinks in a row?” 2) Compulsive drinking -“When drinking alcohol over the past year, have you ever found that you were not able to stop drinking once you had started?” |
2. Condom non-use at last sexual encounter - “The last time you had sex, did you or your partner use a condom or another latex barrier?” 3. Three or more sexual partners in the past year - “In the past year, how many males and/or females have you had sex with?” |
2, 3 | ||
| (58) | Guo et al. (2017) | China | N = 22,288 | A secondary analysis of data from YARHC | Mean age = 19.0 (15–24 years) | F (49.7%) M (50.3%) |
Only alcohol use (OAU) | 2. Condom non-use during first sexual experience 2. Condom non-use during most recent sexual encounter 3. Sexual activity with multiple partners |
2, 3 | ||
| (59) | Seth et al. (2011) | United States | N = 393 | A cross-sectional study | Mean age = 17.9 (15–21 years) | F (100.0%) | Alcohol Use -“How many alcoholic drinks do you usually have at one time?” |
2. Inconsistent condom use 3. Multiple sexual partners during the past 60 days |
2, 3 | ||
| (60) | Cavazos-Rehg et al. (2007) | United States | N = 601 | A cross-sectional study | Mean age = 21.0 (18–25 years) | F (50.4%) M (49.6%) |
Alcohol involvement | 3. Number of Sexual Partners in lifetime >10 - “How many sexual partners have you had in your life?” |
3 | ||
| (61) | Thompson et al. (2005) | United States | N = 17,264 | A secondary analysis of data from Department of Defense Survey of Health | Mean age = Not presented (18 ∼ >46 years) | F (14.0%) M (86.0%) |
Frequency of alcohol intoxication - How often they got drunk or very high from drinking in the past 12 months |
2. Frequency of condom use with casual and one-time sexual partners in the past 12 months 3. Number of sexual partners in the past 12 months |
2, 3 | ||
| (62) | Hurley et al. (2017) | Republic of the Congo | N = 1,396 | A cross-sectional study | Mean age = 18 (15–24 years) | F (57.3%) M (42.7%) |
Alcohol use | 1. Sexual debut under age 15 | 1, 2, 3 | ||
| 2. Unprotected sex | |||||||||||
| - Inconsistent or no condom use with one or more partners in the last 12 months | |||||||||||
| 3. Multiple sexual partners | |||||||||||
| -Two or more sexual partners in the last 12 months | |||||||||||
| (63) | Scroggins et al. (2021) | US Cross-sectional analysis: utilized data from the 2017 National Youth Risk Behavioral Survey (YRBS) | N = 3,732 | A secondary analysis of data from Department of Defense Survey of YRBS | Mean age = Not presented (US high school students) | F (51.0%), M (49.0%) | Alcohol use pattern (past 30 days) | 2. Condom utilization— “The last time you had sexual intercourse, did you or your partner use a condom?” | 2 | ||
| (64) | Izutsu et al. (2009) | Japan | N = 281 | A cross-sectional study | Mean age = 16.88 (13–20 years) | M (100.0%) | AAIS (Adolescent Alcohol Involvement Scale) | 3. Number of sexual partners (0 = less than 2 and 1 = more than 3 | 3 | ||
Characteristics of the included studies on the relationship between alcohol consumption and RSB (Worldwide, 2001–2021).
The number of participants in 50 studies was 442,909, with sample sizes ranging from 116 to 100,790; whereas others used large-scale data from the School Health Promotion Study (SHPS) in Finland or the Youth Risk Behavior Surveillance (YRBS) developed by the Centers for Disease Control and Prevention (CDC) of the United States (55, 63). SHPS is a nationally representative sample of adolescents born between 1987 and 1989, with 374 municipalities out of 448 participating in Finnish municipalities. The YRBS is weighted by respondents to be nationally representative data from the 2017 National YRBS cross-sectional data developed by the US CDC for US high school students (n = 3,732).
The overall mean age of the participants was 17.24 years, and most studies were conducted with both males and females (n = 34 studies). However, some studies focused on a specific sex, such only females (n = 5 studies) and only males (n = 1 study).
Exploring the characteristics of the responses used in the measurement of alcohol consumption, the most common response was a “yes” or “no” for alcohol drinking (n = 28 studies), and the measurement methods of alcohol use were different for each study, such as frequency of alcohol consumption (n = 6 studies), amount of alcohol consumption (glass) (n = 4 studies), alcohol involvement (n = 2 studies), drinking pattern (n = 2 studies), and others (n = 6 studies). Some studies used the Alcohol Use Disorders Identification Test (AUDIT-C) to assess alcohol consumption in the previous 4-week period on a scale of 0–12 (AUDIT-C) (38), while another study used the Adolescent Alcohol Involvement Scale (AAIS) tool (64).
Quality of the Included Studies
Based on the Newcastle-Ottawa Scale assessment, 31 articles were rated as “good” while the remaining studies were rated as “fair” in terms of methodological quality (Table 2).
TABLE 2
| # of Reference | Author(s) (year) | Selection | Comparability | Outcome | Quality Score | ||||
|---|---|---|---|---|---|---|---|---|---|
| Representativeness of the sample | Sample size | Non-respondents | Ascertainment of the exposure | Based on design and analysis | Assessment of the outcome | Statistical test | |||
| (27) | Mo et al. (2007) | * | * | * | * | * | * | 6 | |
| (28) | Lepusić et al. (2013) | * | * | * | * | * | * | * | 7 |
| (14) | Rios-Zertuche et al. (2017) | * | * | * | * | * | * | 6 | |
| (29) | Scott-Sheldon et al. (2010) | * | * | * | * | * | * | * | 7 |
| (30) | Mola et al. (2017) | * | * | ** | * | * | * | 7 | |
| (13) | Wilson et al. (2010) | * | * | * | * | * | * | * | 7 |
| (15) | Mlunde et al. (2012) | * | * | ** | * | * | * | 7 | |
| (31) | Kang et al. (2013) | * | * | * | * | * | * | 6 | |
| (32) | Kaltiala et al. (2015) | * | * | * | * | * | * | * | 7 |
| (33) | Ramisetty et al. (2004) | * | * | * | * | * | * | * | 7 |
| (34) | Kugbey et al. (2018) | ** | * | * | ** | * | * | * | 9 |
| (35) | Ronis et al. (2011) | * | * | * | * | * | * | * | 7 |
| (9) | Ayhan et al. (2015) | ** | * | * | * | * | 6 | ||
| (18) | Menna et al. (2014) | * | * | * | * | * | * | * | 7 |
| (36) | Peltzer et al. (2016) | ** | * | * | ** | * | * | * | 9 |
| (37) | Kogan et al. (2010) | * | * | * | * | * | 5 | ||
| (8) | Hong et al. (2018) | * | * | * | * | * | * | * | 7 |
| (38) | Connor et al. (2013) | * | * | ** | * | * | * | 7 | |
| (39) | Seidu et al. (2021) | * | * | * | * | * | * | * | 7 |
| (40) | Yarber et al. (2002) | * | * | * | * | * | * | * | 7 |
| (41) | Benotsch et al. (2013) | * | * | * | * | * | * | * | 7 |
| (16) | Sanchez et al. (2013) | * | * | * | ** | * | * | * | 8 |
| (42) | Lee et al. (2010) | * | * | * | * | * | * | 6 | |
| (43) | Agu et al. (2018) | * | * | * | * | * | 5 | ||
| (44) | Bartholomew et al. (2021) | * | * | * | * | * | * | 6 | |
| (45) | Brown et al. (2007) | * | * | * | * | * | * | 6 | |
| (46) | Kiene et al. (2009) | * | * | * | * | * | * | 6 | |
| (47) | Adhikari. (2010) | * | * | ** | * | * | * | 7 | |
| (19) | Bersamin et al. (2006) | * | * | * | * | * | * | * | 7 |
| (48) | Nkansah-Amankra et al. (2011) | * | * | * | * | * | * | * | 7 |
| (49) | Patrick et al. (2009) | * | * | * | * | * | * | * | 7 |
| (7) | Yu et al. (2014) | ** | * | * | * | * | * | * | 8 |
| (50) | Gwon et al. (2015) | ** | * | * | * | * | * | * | 8 |
| (51) | Brouwer et al. (2019) | * | * | * | * | * | * | 6 | |
| (52) | Choi et al. (2016) | * | * | * | * | * | 5 | ||
| (53) | Lewis et al. (2012) | * | * | * | * | * | * | 6 | |
| (54) | Kuortti et al. (2009) | * | * | * | * | * | * | * | 7 |
| (55) | Lavikainen et al. (2009) | * | * | * | * | * | * | 6 | |
| (5) | Young et al. (2018) | * | * | * | * | * | * | * | 7 |
| (4) | Pengpid et al. (2021) | ** | * | * | * | * | * | * | 8 |
| (56) | Page and Hall (2009) | ** | * | * | * | ** | * | * | 9 |
| (57) | Woodrome et al. (2006) | * | * | * | * | * | * | 6 | |
| (19) | Agius et al. (2013) | ** | * | * | * | * | * | * | 8 |
| (58) | Guo et al. (2017) | * | * | * | * | * | * | * | 7 |
| (59) | Seth et al. (2011) | * | * | * | * | * | * | * | 7 |
| (60) | Cavazos-Rehg et al. (2007) | * | * | * | * | * | 5 | ||
| (61) | Thompson et al. (2005) | * | * | * | * | * | 5 | ||
| (62) | Hurley et al. (2017) | * | * | * | * | * | * | 6 | |
| (63) | Scroggins and Shacham (2021) | * | * | ** | * | * | * | 7 | |
| (64) | Izutsu et al. (2009) | * | ** | * | * | * | 6 | ||
Quality of the included studies (Newcastle-Ottawa Scale) (Worldwide, 2001–2021).
Results of Meta-Analysis
Early Sexual Initiation
After analyzing 11 articles studying early sexual initiation in adolescents, the incidence of sexual experience at an early age was found to be 1.958 times higher in the group that consumed alcohol compared to the group that did not (OR = 1.958, 95% CI = 1.635–2.346) (Figure 2). The analysis was based on 220,439 adolescents across the studies. The homogeneity test resulted in a Q statistic of 38.278 (p < 0.001) and an I2 statistic of 73.88%, demonstrating relatively high heterogeneity. Hence, the effect size was analyzed using a random-effects model.
FIGURE 2
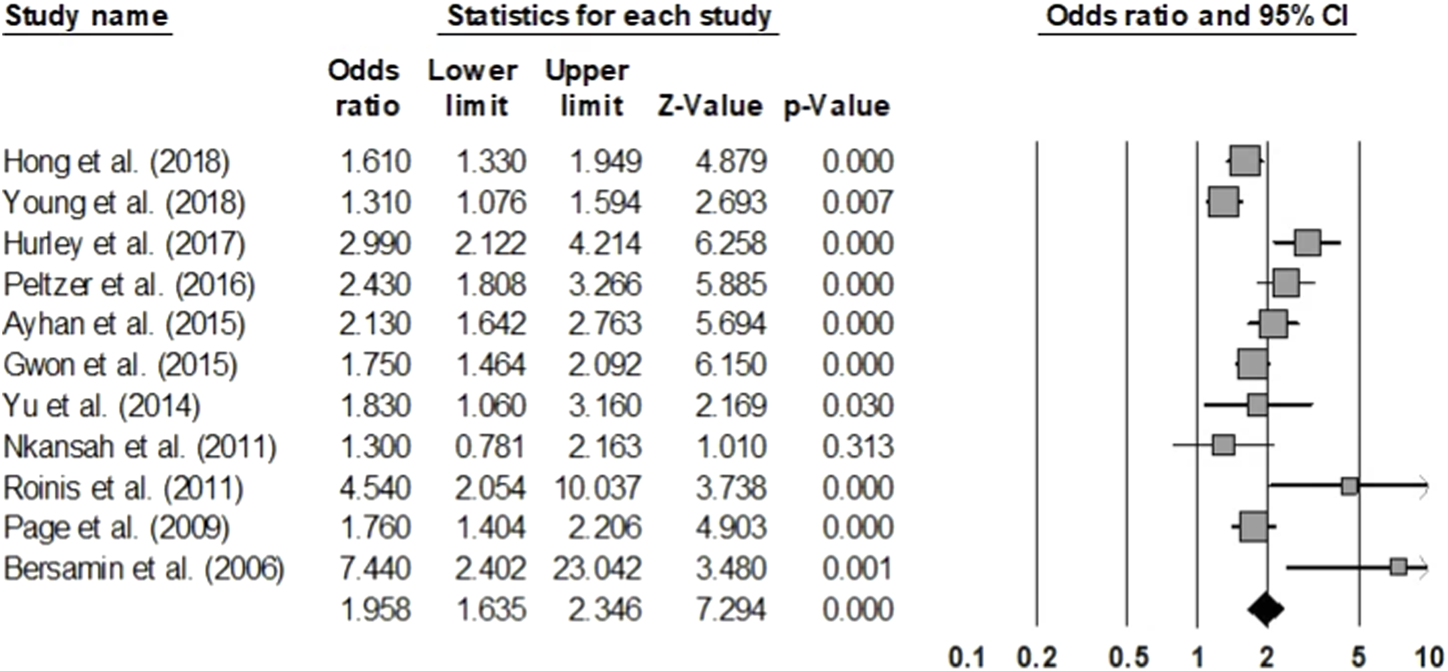
Forest plot (Early sexual initiation) (Worldwide, 2001–2021).
The publication bias test showed that some studies were omitted to the left of the mean effect size in the funnel plot, which seemed to be asymmetric, and Egger’s regression test showed a publication error (t = 2.272, p = 0.049). When the publication error is corrected using the trim-and-fill method, it is still statistically significant even if one more study is added (OR = 1.906, 95% CI = 1.581–2.298). Additionally, the sensitivity analysis showed that there was no substantial difference in the range of the mean effect size even after removing each individual article (1.854–2.056); and all were significant. To explain the heterogeneity of the effect size, a meta-regression analysis with sex as a moderating variable was conducted, indicating that it was statistically insignificant (Z = 0.600, p = 0.548) (Table 3).
TABLE 3
| Gender | Subgroup analysis | Meta-regression | ||||
|---|---|---|---|---|---|---|
| OR (95% CI) | Covariate | B | SE | 95% CI | Z (p) | |
| Intercept | 0.480 | 0.145 | (0.195, 0.764) | 3.300 (<0.001) | ||
| Females | 1.615 (1.214, 2.149) | Females | 1.000 | |||
| Males | 1.814 (1.412, 2.332) | Males | 0.116 | 0.194 | (−0.263, 0.496) | 0.600 (0.548) |
Results of meta-regression (Early sexual initiation) (Worldwide, 2001–2021).
Notes: 6 articles included in the subgroup analysis.
Inconsistent Condom Use
After analyzing 29 articles that investigated inconsistent condom use among adolescents and young adults, the rate of condom non-use during sexual intercourse was found to be 1.228 times higher in the group that consumed alcohol compared to the group that did not consume alcohol (OR = 1.228, 95% CI = 1.114–1.354) (Figure 3). The analysis included 137,064 individuals across the studies. The homogeneity test resulted in a Q statistic of 474.933 (p < 0.001), and an I2 statistic of 94.10%, demonstrating high heterogeneity. Hence, the effect size was analyzed using a random-effects model.
FIGURE 3
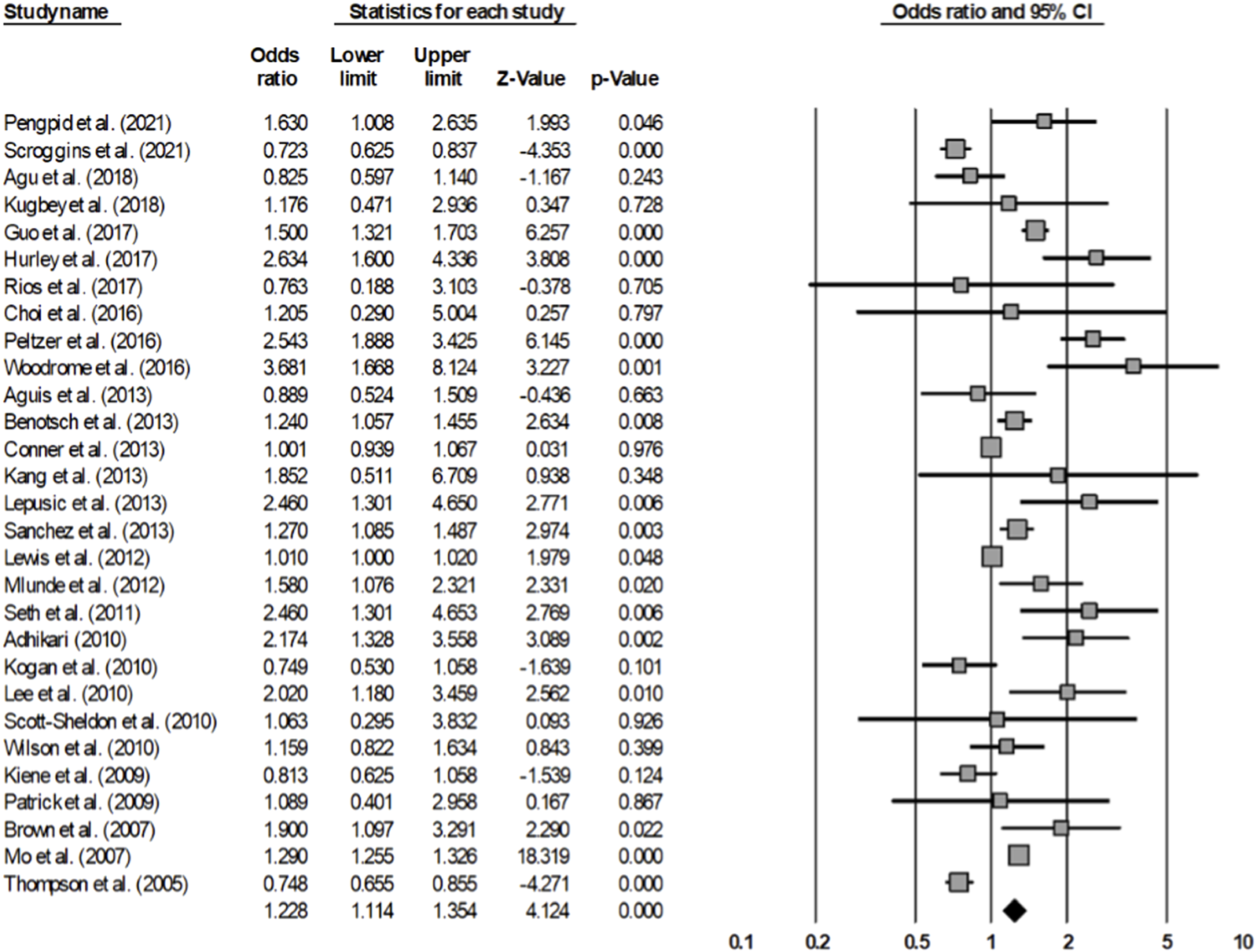
Forest plot (Inconsistent condom use) (Worldwide, 2001–2021).
The publication bias test showed that some studies were omitted to the left direction of the mean effect size in the funnel plot, which seemed to be asymmetric; however, it can be determined that there was no publication error according to Egger’s regression test (t = 1.732, p = 0.095). Additionally, the sensitivity analysis showed that there was no substantial difference in the range of the mean effect size, even after removing each article (1.184–1.283); and all were significant. To explain the heterogeneity of the effect size, a meta-regression analysis with sex as a moderating variable was conducted, which indicated that it was statistically insignificant (Z = −0.700, p = 0.4817) (Table 4).
TABLE 4
| Gender | Subgroup analysis | Meta-regression | ||||
|---|---|---|---|---|---|---|
| OR (95% CI) | Covariate | B | SE | 95% CI | Z (p) | |
| Intercept | 0.302 | 0.190 | (-0.070, 0.675) | 1.590 (0.112) | ||
| Females | 1.353 (0.938, 1.950) | Females | 1.000 | |||
| Males | 1.134 (0.820, 1.567) | Males | −0.177 | 0.251 | (-0.670, 0.316) | −0.700 (0.482) |
Results of meta-regression (Inconsistent condom use) (Worldwide, 2001–2021).
Notes: 7 articles included in the subgroup analysis.
Multiple Sexual Partners
Upon analyzing 25 articles, based on a total of 216,884 adolescents and young adults, that studied multiple sexual partners, the rate of having multiple sexual partners was 1.722 times higher in the group that consumed alcohol than in the group that did not (OR = 1.722, 95% CI = 1.525–1.945) (Figure 4). The homogeneity test resulted in a Q statistic of 253.151 (p < 0.001) and an I2 statistic of 90.52%, demonstrating high heterogeneity. Hence, the effect size was analyzed using a random-effects model.
FIGURE 4
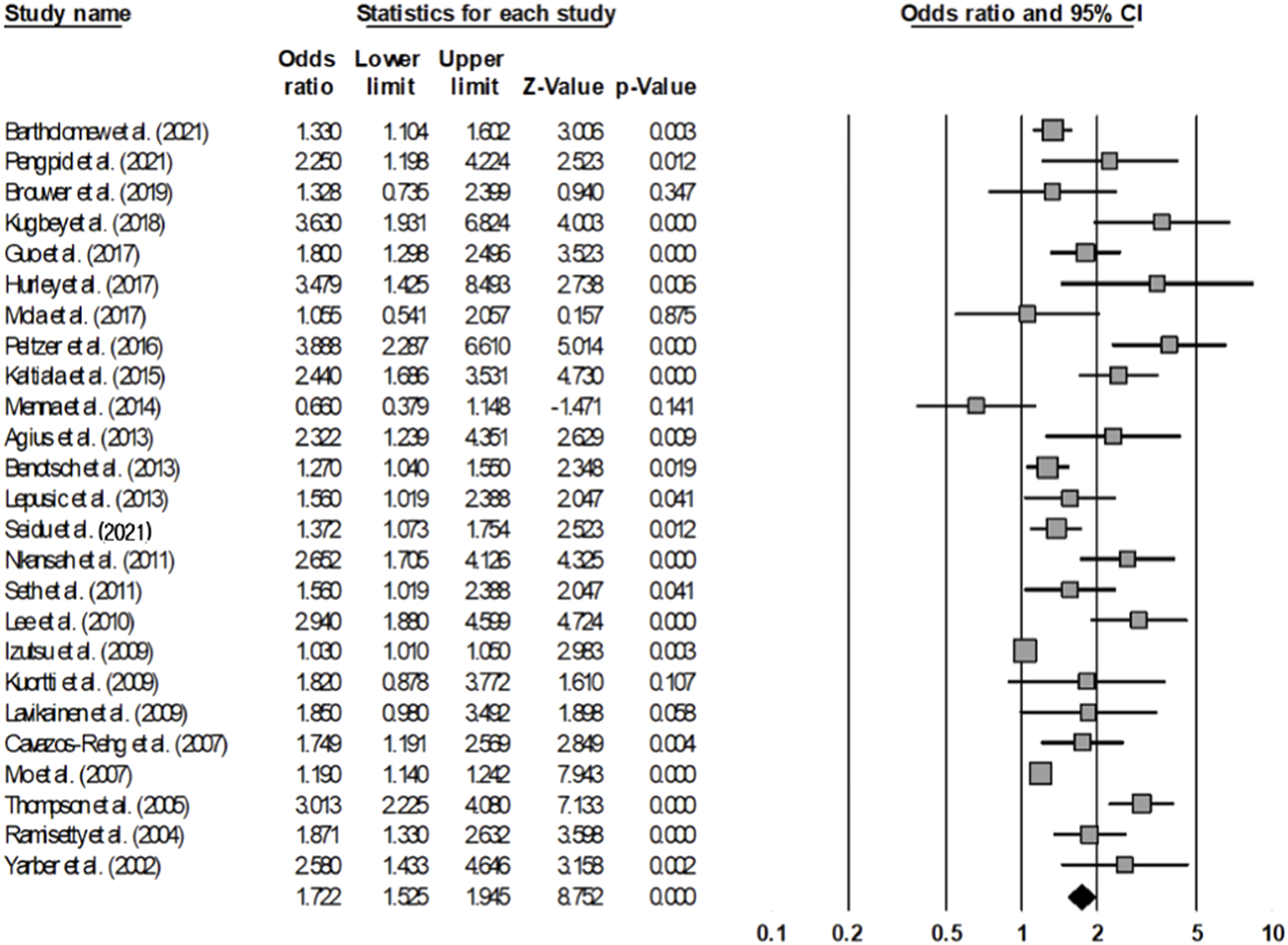
Forest plot (Multiple sexual partners) (Worldwide, 2001–2021).
The publication bias test showed that some studies were omitted to the left direction of the mean effect size in the funnel plot, which seemed to be asymmetric, and there was a publication error according to Egger’s regression test (t = 6.518, p < 0.001). When the publication error is corrected using the trim-and-fill method, it can be seen that it is still statistically significant even if nine more studies are added (OR = 1.367, 95% CI = 1.224–1.527). In addition, the sensitivity analysis showed that there was no substantial difference in the range of the mean effect size even after removing each article (1.653–1.838); and all were significant.
To explain the heterogeneity of the effect size, a meta-regression analysis with sex as a moderating variable was conducted, indicating that it was statistically insignificant (Z = −0.340, p = 0.732) (Table 5).
TABLE 5
| Gender | Subgroup analysis | Meta-regression | ||||
|---|---|---|---|---|---|---|
| OR (95% CI) | Covariate | B | SE | 95% CI | Z (p) | |
| Intercept | 0.913 | 0.194 | (0.532, 1.294) | 4.700 (<0.001) | ||
| Females | 2.590 (2.022, 3.317) | Females | 1.000 | |||
| Males | 2.262 (1.405, 3.640) | Males | 0.094 | 0.275 | (-0.633, 0.445) | −0.340 (0.732) |
Results of meta-regression (Having multiple sexual partners) (Worldwide, 2001–2021).
Notes: 6 articles included in the subgroup analysis.
Discussion
This meta-analysis included 50 independent studies that investigated the relationship between alcohol consumption and RSBs in adolescents and young adults. The RSBs considered in this study were early sexual initiation, inconsistent condom use, and multiple sexual partners. The odds ratio (OR) was used as the effect size measure, with OR = 1.958 for early sexual initiation, OR = 1.228 for inconsistent condom use, and OR = 1.722 for multiple sexual partners among adolescents and young adults who consumed alcohol, compared to those who did not. No sex-based differences were observed. These findings are consistent with the Alcohol Myopia Theory (65), which posits that alcohol consumption can impair cognitive processing and narrow individuals’ focus of attention rather than long-term goals or consequences, leading to a myopic view of the immediate environment and an over-reliance on cues that are immediately present, which may make individuals less likely to consider the potential consequences of their actions and more likely to engage in risky behaviors (66). By understanding the mechanisms underlying the association between alcohol consumption and RSBs, we can develop more effective prevention and intervention strategies to reduce the negative health outcomes associated with these behaviors.
The age of early sexual initiation among adolescents can vary within and between countries and cultures, but the mean age of sexual intercourse among sexually-experienced adolescents is typically between the ages of 14 and 15 (9, 10, 35). Some studies define early sexual experience as occurring at 14 years of age or younger (5, 36), but it is notable that the trend of sexual initiation age is rising in many countries. For example, a study conducted in the United States found that the proportion of adolescents who have had sexual intercourse before the age of 13 has declined over time from 10.2% in 1991% to 3.4% in 2017 (67). Similarly, a recent study on sub-Saharan Africa found that the age at first sexual intercourse among birth cohorts entering adulthood between 1985 and 2020 had increased over time, with the median age at first sex rising from 17.1 to 18.7 years for men and from 17.6 to 19.1 years for women (68).
The odds ratio of alcohol consumption and early sexual initiation was the highest at 1.958. This phenomenon of early alcohol consumption and risky behaviors seems to be particularly prominent in the United States, where the minimum legal drinking age (MLDA) is 21 years old (69). Despite this, a significant number of high school students under the age of 21 still report drinking alcohol, with one study finding that 29% of high school students reported consuming alcohol (67). Mo et al (27) also reported that 43.4% of adolescents between the ages of 14 and 16 had consumed alcohol and were 1.13 times more likely to engage in early sexual initiation. Early alcohol consumption during adolescence can lead to other risky behaviors, such as smoking, substance abuse, and RSBs (17, 69). Thus, implementing policies and strategies to increase the age at which alcohol is initiated, and measures like designating the MLDA and requiring ID for alcohol purchases, could be effective in reducing alcohol consumption among young people. However, it is notable that further research is needed to better understand the complex relationship between alcohol consumption and risky behaviors among adolescents and young adults.
Of the 50 studies analyzed in the meta-analysis, 29 studies examined the relationship between inconsistent condom use and alcohol consumption among adolescents. The results showed that adolescents and young adults who drank were 1.228 times more likely to engage in inconsistent condom use during sexual intercourse that those who did not.
These findings are consistent with the Inhibition Conflict Theory, which suggests that alcohol consumption can lead to a conflict between an individual’s desires and their inhibitions, resulting in a failure to inhibit inappropriate or risky behaviors (70). Dermen and Cooper (70) provides further support for this theory, showing that the quantity of alcohol consumed was negatively associated with condom use only among high-conflict individuals. In sexual behavior, this conflict could result in a failure to use condoms consistently, despite knowledge of the potential risks associated with unprotected sex. Adolescents who consume alcohol may be more likely to prioritize their immediate desires over their long-term health and wellbeing, leading to a failure to use condoms consistently during sexual activity. By understanding the role of inhibition conflict and alcohol expectancy in the association between alcohol consumption and inconsistent condom use, we can develop more targeted prevention and intervention strategies to reduce the gap of desires and conflict.
Although the rate of sexual experience among adolescents aged 13–18 years is increasing, only 65.5% of adolescents who have experienced sexual intercourse reported using condoms for contraception, with 64.6% being male and 67.0% female (11). This indicates that male adolescents are more passive in the practice of contraception compared to female adolescents. However, it is notable that alcohol consumption has a negative impact on condom use during sexual intercourse. The rate of condom use during sexual intercourse is already low at 57.9%, and drops to 51.2% when alcohol is involved (16). RSBs without condom use result in burden and responsibility due to unintended pregnancy among female adolescents. The integrative model of behavioral prediction (71) suggests that female adolescents may find it difficult to ask their partners to use condoms due to the influence of perceived normative pressure, lack of self-efficacy, and perceived control skill (14). To increase condom use among adolescents and prevent unwanted pregnancies or STDs after risky sexual intercourse, sex education should be provided in elementary schools regarding the consequences of not using condoms and how to use them correctly. Such education should be delivered not only within the school system but also at community centers and related institutions. Condoms should be universalized to enable youth to easily purchase them at pharmacies and convenience stores. Additionally, various programs should be implemented to strengthen communication, self-efficacy, and control skills so that female adolescents can confidently demand the use of condoms from their male partners.
The meta-analysis that examined the relationship between alcohol consumption and having multiple sexual partners included 25 studies and found that the risk of having two or more sexual partners was approximately 1.722 times higher for adolescents and young adults who drank alcohol. Among studies that examined the number of sexual partners by sex, Kugbey et al (34) and Mo et al (27) found that 61.1% of male adolescents had multiple sexual partners. However, some studies have reported no significant sex-related differences in the number of sexual partners (27). This study also found no significant sex-related differences depending on sex (male and female). The age at which alcohol consumption is initiated also affects the number of sexual partners. For example, a study found that females and males who began drinking alcohol at the age of 15 had a higher likelihood of having multiple sexual partners compared to those who began drinking at a later age (72). Such risky sexual behavior may expose adolescents to sexually transmitted diseases (STDs) through sexual contact with strangers. Therefore, it is important to educate adolescents and young adults on the dangers of having multiple sexual partners while drinking alcohol due to precocious puberty and open sexual culture. This could be accomplished through comprehensive sex education that covers the risks of unprotected sex, the importance of safe sex practices, and strategies for avoiding risky situations. It is also crucial to promote responsible drinking behaviors and discourage underage drinking, as early initiation of alcohol use is associated with a higher risk of engaging in risky sexual behavior. The Integrative Model of Behavioral Prediction (73) can be applied to understand the relationship between the intention to engage in RSBs and the actual practice of such behavior. This model may help in the development of a behavioral strategy to promote healthy sexual behavior. As alcohol negatively impacts all forms of RSBs, intervention for controlling adolescent drinking is necessary. However, since the level of risk associated with alcohol consumption varies depending on individual characteristics such as age and gender, it is difficult to apply the same guidelines for developing and implementing alcohol control programs from adolescents to young adults. Therefore, we propose developing intervention guidelines for each age group, considering factors such as age, gender, and educational methods, to develop the most effective guidelines. We also suggest using a tool called AUDIT (Alcohol Use Disorders Identification Test) to screen and assess risky drinkers among adolescents and young adults and provide different types of intervention based on their risk zone: alcohol education for low-risk drinkers, simple advice for hazardous drinkers, brief counselling for harmful drinkers, and referral for probable dependent drinkers (32).
Limitations and Strengths
The study has several limitations, and we suggest some areas for future research. Firstly, the study did not take into account the frequency and amount of alcohol consumption, which varied among adolescents and young adults in each study. Additionally, the definition of variables such as the number of sexual partners and condom use varied across studies, with some studies measuring over a lifetime, and others measuring within a certain time frame (e.g., the last 60 days or the past 12 months). Therefore, we suggest that future meta-analyses should consider these variations in measurement when examining the relationship between alcohol consumption and risky sexual behaviors. Secondly, although the results indicate a positive association between alcohol consumption and RSBs in this population, it is notable that this association does not necessarily imply causality, as other factors may contribute to both behaviors. To address this limitation and better understand the causal relationship between alcohol consumption and RSBs, we recommend further research using longitudinal cohort studies or experimental designs. By following adolescents and young adults over time and controlling for potential confounding variables, these types of studies could help to establish the temporal sequence of alcohol consumption and RSBs and provide stronger evidence for causality. Finally, we only focused on three RSBs: early sexual initiation, inconsistent condom use, and multiple partners. However, there are other RSBs that can be influenced by alcohol consumption, such as casual sex, sex against the will, and sexual violence. Previous studies have suggested that alcohol can impair judgment and decision-making, increase sexual arousal and desire, and reduce inhibitions and self-control (74, 75). These effects can lead to engaging in sex with unfamiliar or untrusted partners, having unwanted or coerced sex, or being involved in sexual aggression or assault (76). Future research should examine how alcohol consumption affects these other RSBs among adolescents and young adults.
Despite these limitations, this study had several strengths. First, 20,000 articles were screened for studies on alcohol use and RSBs that reported odds ratios using two search strategies, and a large number of articles were comprehensively meta-analyzed. Three types of RSBs were analyzed to provide fundamental data for developing and implementing specific programs by comparing and discussing the risks of alcohol consumption among adolescents and young adults in early sexual initiation, which leads to inconsistent condom use and multiple sexual partners.
Conclusion
This meta-analysis highlights the significant association between alcohol consumption and early sexual initiation, inconsistent condom use, and multiple sexual partners among adolescents and young adults. The findings suggest that alcohol consumption among adolescents and young adults may lead to exposure to unwanted pregnancy and STDs. Therefore, preventive interventions such as education and monitoring to prevent alcohol consumption and increasing the age criteria for drinking alcohol should be implemented. School- and community-based preventive interventions are required, such as education and monitoring to prevent alcohol consumption, and the age criteria for drinking alcohol in each country should be increased. Parents and guardians can provide guidance and support to help their children make healthy choices and avoid risky behaviors. Healthcare providers can also play an important role in preventing alcohol use among adolescents and young adults by screening for alcohol use, providing education on the harmful effects of alcohol, and referring adolescents and young adults to appropriate resources for prevention and treatment. Overall, it is crucial to raise awareness about the risks of alcohol consumption among adolescents and young adults and implement effective prevention measures to promote healthy behaviors and prevent the negative consequences of alcohol use.
Statements
Author contributions
YY conceived the study, participated in its design and coordination, and drafted the manuscript. H-SC participated in the design and interpretation of the data, and drafted the manuscript. All the authors have read and approved the final manuscript.
Funding
This study was supported by the Ministry of Education of the Republic of Korea and National Research Foundation of Korea (NRF-2020S1A5A2A03047080).
Conflict of interest
The authors declare that they do not have any conflicts of interest.
References
1.
Bonnie RJ Cook PJ Cushing JA Grube JW Halpern-Felsher BL Hansen WB et al Reducing Underage Drinking; a Collective Responsibility. In: Commiitte on Developing a Strategy to Reduce and Prevent Underage Drinking. Washington, DC: National Academies Press (2004). 58–9P.
2.
WHO. Alcohol (2022). Available at: https://www.who.int/health-topics/alcohol#tab=tab_1 (Accessed on August 24, 2022).
3.
WHO. Global Status Report on Alcohol and Health 2018 (2018). Available at: https://apps.who.int/iris/bitstream/handle/10665/274603/9789241565639-eng.pdf (Accessed on March 7, 2023).
4.
Pengpid S Peltzer K . Sexual Risk Behaviour and its Correlates Among Adolescents in Mozambique: Results from a National School Survey in 2015. SAHARA-J: Soc Aspects HIV/AIDS (2021) 18(1):26–32. 10.1080/17290376.2020.1858947
5.
Young H Burke L Gabhainn SN . Sexual intercourse, Age of Initiation and Contraception Among Adolescents in Ireland: Findings from the Health Behaviour in School-Aged Children (HBSC) Ireland Study. BMC Public Health (2018) 18:1–17. 10.1186/s12889-018-5217-z
6.
Cook RL Comer DM Wiesenfeld HC Chang C-CH Tarter R Lave JR et al Alcohol and Drug Use and Related Disorders: An Underrecognized Health Issue Among Adolescents and Young Adults Attending Sexually Transmitted Disease Clinics. Sex Transm Dis (2006) 33(9):565–70. 10.1097/01.olq.0000206422.40319.54
7.
Yu J-O Kim H-H Kim J-S . Factors Associated with Sexual Debut Among Korean Middle School Students. Child Health Nurs Res (2014) 20(3):159–67. 10.4094/chnr.2014.20.3.159
8.
Hong SW Suh YS Kim DH . The Risk Factors of Sexual Behavior Among Middle School Students in South Korea. Int J Sex Health (2018) 30(1):72–80. 10.1080/19317611.2018.1429513
9.
Ayhan G Martin L Levy-Loeb M Thomas S Euzet G Van Melle A et al Prevalence and Risk Factors of Early Onset of Sexual intercourse in a Random Sample of a Multiethnic Adolescent Population in French Guiana. AIDS Care Psychol Socio-medical Aspects AIDS/HIV (2015) 27(8):1025–30. 10.1080/09540121.2015.1020282
10.
Bersamin MM Walker S Fisher DA Grube JW . Correlates of Oral Sex and Vaginal Intercourse in Early and Middle Adolescence. J Res Adolesc (2006) 16(1):59–68. 10.1111/j.1532-7795.2006.00120.x
11.
Korea Disease Control and Prevention Agency (KDCA). Report of 2021 Adolescent Health Behavior Survey. Cheongju: KDCA (2021). 66–71. Available at: https://www.kdca.go.kr/yhs/home.jsp (Accessed on Feb 9, 2022).
12.
Pettifor A Brien KO Macphail C Miller WC Rees H . Early Coital Debut and Associated HIV Risk Factors Among Young Women and Men in South Africa. Int Perspect Sex Reprod Health (2009) 35(2):82–90. 10.1363/ifpp.35.082.09
13.
Wilson K Asbridge M Kisely S Langille D . Associations of Risk of Depression with Sexual Risk Taking Among Adolescents in Nova Scotia High Schools. Can J Psychiatry (2010) 55(9):577–85. 10.1177/070674371005500906
14.
Rios-Zertuche D Cuchilla J Zúñiga-Brenes P Hernández B Jara P Mokdad AH et al Alcohol Abuse and Other Factors Associated with Risky Sexual Behaviors Among Adolescent Students from the Poorest Areas in Costa Rica. Int J Public Health (2017) 62(2):271–82. 10.1007/s00038-016-0859-z
15.
Mlunde LB Poudel KC Sunguya BF Mbwambo JK Yasuoka J Otsuka K et al A Call for Parental Monitoring to Improve Condom Use Among Secondary School Students in Dares Salaam, Tanzania. BMC Public Health (2012) 12(1):1061–11. 10.1186/1471-2458-12-1061
16.
Sanchez ZM Nappo SA Cruz JI Carlini EA Carlini CM Martins SS . Sexual Behavior Among High School Students in Brazil: Alcohol Consumption and Legal and Illegal Drug Use Associated with Unprotected Sex. Clinics (2013) 68:489–94. 10.6061/clinics/2013(04)09
17.
National Institute on Alcohol Abuse and Alcoholism(NIAAA). Alcohol Intervention for Young Adults (2022). Available at: https://www.niaaa.nih.gov/alcohols-effects-health/alcohol-interventions-young-adults (Accessed on Sep 09, 2022).
18.
Menna T Ali A Worku A . Prevalence of “HIV/AIDS Related” Parental Death and its Association with Sexual Behavior of Secondary School Youth in Addis Ababa, Ethiopia: a Cross Sectional Study. BMC Public Health (2014) 14(1):1120–8. 10.1186/1471-2458-14-1120
19.
Agius P Taft A Hemphill S Toumbourou J McMorris B . Excessive Alcohol Use and its Association with Risky Sexual Behaviour: a Cross‐sectional Analysis of Data from Victorian Secondary School Students. Aust N Z J Public Health (2013) 37(1):76–82. 10.1111/1753-6405.12014
20.
Tapert SE Aarons GA Sedlar GR Brown SA . Adolescent Substance Use and Sexual Risk-Taking Behavior. Adolesc Health (2000) 28(3):181–9. 10.1016/S1054-139X(00)00169-5
21.
Moher D Liberati A Tetzlaff J Altman DG PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Plos Med (2009) 6(7):e1000097. 10.1371/journal.pmed.1000097
22.
Liberati A Altman DG Tetzlaff J Mulrow C Gøtzsche PC Ioannidis JPA et al The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies that Evaluate Healthcare Interventions: Explanation and Elaboration. BMJ (2009) 339:b2700. 10.1136/bmj.b2700
23.
Stroup DF Berlin JA Morton SC Olkin I Williamson GD Rennie D et al Meta-analysis of Observational Studies in Epidemiology: a Proposal for Reporting. Meta-Analysis of Observational Studies in Epidemiology (MOOSE) Group. JAMA (2000) 283(15):2008–12. 10.1001/jama.283.15.2008
24.
Herzog R Álvarez-Pasquin M Díaz C Del Barrio JL Estrada JM Gil Á . Are Healthcare Workers’ Intentions to Vaccinate Related to Their Knowledge, Beliefs and Attitudes? A Systematic Review. BMC public health (2013) 13(1):154–17. 10.1186/1471-2458-13-154
25.
Hwang SD Shim SR . Meta-analysis: From a forest Plot to a Network Meta-Analysis. Seoul: Hannarae Publishing Company (2018). p. 128–34.
26.
Egger M Smith GD Schneider M Minder C . Bias in Meta-Analysis Detected by a Simple, Graphical Test. Br Med J (1997) 315(7109):629–34. 10.1136/bmj.315.7109.629
27.
Mo F Wong T Merrick J . Adolescent Lifestyle, Sexual Behavior and Sexually Transmitted Infections (STI) in Canada. Int J Disabil Hum Dev (2007) 6(1):53–60. 10.1515/ijdhd.2007.6.1.53
28.
Lepušić D Radović-Radovčić S . Alcohol–a Predictor of Risky Sexual Behavior Among Female Adolescents. Acta Clin Croat (2013) 52(1):3–8.
29.
Scott-Sheldon LAJ Carey MP Carey KB . Alcohol and Risky Sexual Behavior Among Heavy Drinking College Students. AIDS Behav (2010) 14(4):845–53. 10.1007/s10461-008-9426-9
30.
Mola R Araújo RC Oliveira JVB Cunha SB Souza GF Ribeiro LP et al Association between the Number of Sexual Partners and Alcohol Consumption Among Schoolchildren. J Pediatr (2017) 93:192–9. 10.1016/j.jped.2016.05.003
31.
Kang SY Hutchinson MK Waldron N . Characteristics Related to Sexual Experience and Condom Use Among Jamaican Female Adolescents. J Health Care Poor Underserved (2013) 24(1):220–32. 10.1353/hpu.2013.0023
32.
Babor TF Higgins-Biddle JC Saunders JB Monteiro MG . The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Care. 2nd ed.Geneva, Switzerland: World Health Organization (2001).
33.
Ramisetty‐Mikler S Caetano R Goebert D Nishimura S . Ethnic Variation in Drinking, Drug Use, and Sexual Behavior Among Adolescents in Hawaii. J Sch Health (2004) 74(1):16–22. 10.1111/j.1746-1561.2004.tb06596.x
34.
Kugbey N Ayanore MA Amu H Asante KO Adam A . International Note: Analysis of Risk and Protective Factors for Risky Sexual Behaviours Among School-Aged Adolescents. J adolescence (2018) 68:66–9. 10.1016/j.adolescence.2018.06.013
35.
Ronis ST O'Sullivan LF . A Longitudinal Analysis of Predictors of Male and Female Adolescents' Transitions to Intimate Sexual Behavior. J Adolesc Health (2011) 49(3):321–3. 10.1016/j.jadohealth.2010.12.010
36.
Peltzer K Pengpid S . Risk and Protective Factors Affecting Sexual Risk Behavior Among School-Aged Adolescents in Fiji, Kiribati, Samoa, and Vanuatu. Asia Pac J Public Health (2016) 28(5):404–15. 10.1177/1010539516650725
37.
Kogan SM Brody GH Chen Y-f Grange CM Slater LM DiClemente RJ . Risk and Protective Factors for Unprotected intercourse Among Rural African American Young Adults. Public Health Rep (2010) 125(5):709–17. 10.1177/003335491012500513
38.
Connor J Psutka R Cousins K Gray A Kypri K . Risky Drinking, Risky Sex: a National Study of New Zealand university Students. Alcohol Clin Exp Res (2013) 37(11):1971–8. 10.1111/acer.12175
39.
Seidu AA Ahinkorah BO Ameyaw EK Darteh EKM Budu E Iddrisu H et al Risky Sexual Behaviours Among School-Aged Adolescents in Namibia: Secondary Data Analyses of the 2013 Global School-Based Health Survey. J Public Health (2021) 29:451–61. 10.1007/s10389-019-01140-x
40.
Yarber WL Milhausen R Crosby RA DiClemente RJ . Selected Risk and Protective Factors Associated with Two or More Lifetime Sexual intercourse Partners and Non-condom Use during Last Coitus Among US Rural High School Students. Am J Health Education (2002) 33(4):206–15. 10.1080/19325037.2002.10603509
41.
Benotsch EG Snipes DJ Martin AM Bull SS . Sexting, Substance Use, and Sexual Risk Behavior in Young Adults. J Adolesc Health (2013) 52(3):307–13. 10.1016/j.jadohealth.2012.06.011
42.
Lee J Hahm HC . Acculturation and Sexual Risk Behaviors Among Latina Adolescents Transitioning to Young Adulthood. J Youth Adolescence (2010) 39(4):414–27. 10.1007/s10964-009-9495-8
43.
Agu CF Oshi DC Abel WD Rae T Oshi SN Ricketts-Roomes T et al Alcohol Consumption and Sexual Risk Behaviour Among Jamaican Adolescents. Asian Pac J Cancer Prev (2018) 19(1):1–6. 10.22034/APJCP.2018.19.S1.1
44.
Bartholomew R Kerry‐Barnard S Beckley‐Hoelscher N Phillips R Reid F Fleming C et al Alcohol Use, Cigarette Smoking, Vaping and Number of Sexual Partners: A Cross‐sectional Study of Sexually Active, Ethnically Diverse, Inner City Adolescents. Health Expect (2021) 24(3):1009–14. 10.1111/hex.13248
45.
Brown JL Vanable PA . Alcohol Use, Partner Type, and Risky Sexual Behavior Among College Students: Findings from an Event-Level Study. Addict behaviors (2007) 32(12):2940–52. 10.1016/j.addbeh.2007.06.011
46.
Kiene SM Barta WD Tennen H Armeli S . Alcohol, Helping Young Adults to Have Unprotected Sex with Casual Partners: Findings from a Daily Diary Study of Alcohol Use and Sexual Behavior. J Adolesc Health (2009) 44(1):73–80. 10.1016/j.jadohealth.2008.05.008
47.
Adhikari R . Are Nepali Students at Risk of HIV? A Cross-Sectional Study of Condom Use at First Sexual intercourse Among College Students in Kathmandu. J Int AIDS Soc (2010) 13(1):7. 10.1186/1758-2652-13-7
48.
Nkansah-Amankra S Diedhiou A Agbanu HL Harrod C Dhawan A . Correlates of Sexual Risk Behaviors Among High School Students in Colorado: Analysis and Implications for School-Based HIV/AIDS Programs. Matern Child Health J (2011) 15(6):730–41. 10.1007/s10995-010-0634-3
49.
Patrick ME Maggs JL . Does Drinking lead to Sex? Daily Alcohol–Sex Behaviors and Expectancies Among College Students. Psychol Addict behaviors (2009) 23(3):472–81. 10.1037/a0016097
50.
Gwon SH Lee CY . Factors that Influence Sexual intercourse Among Middle School Students: Using Data from the 8th (2012) Korea Youth Risk Behavior Web-Based Survey. J Korean Acad Nurs (2015) 45(1):76–83. 10.4040/jkan.2015.45.1.76
51.
Brouwer AF Delinger RL Eisenberg MC Campredon LP Walline HM Carey TE et al HPV Vaccination Has Not Increased Sexual Activity or Accelerated Sexual Debut in a College-Aged Cohort of Men and Women. BMC Public Health (2019) 19(1):821–8. 10.1186/s12889-019-7134-1
52.
Choi EP-H Wong JY-H Lo HH-M Wong W Chio JH-M Fong DY-T . The Impacts of Using Smartphone Dating Applications on Sexual Risk Behaviours in College Students in Hong Kong. PLoS One (2016) 11(11):e0165394–15. 10.1371/journal.pone.0165394
53.
Lewis MA Granato H Blayney JA Lostutter TW Kilmer JR . Predictors of Hooking up Sexual Behaviors and Emotional Reactions Among US College Students. Arch Sex Behav (2012) 41(5):1219–29. 10.10.1007/s10508-011-9817-2
54.
Kuortti M Kosunen E . Risk-taking Behaviour Is More Frequent in Teenage Girls with Multiple Sexual Partners. Scand J Prim Health Care (2009) 27(1):47–52. 10.1080/02813430802691933
55.
Lavikainen HM Lintonen T Kosunen E . Sexual Behavior and Drinking Style Among Teenagers: a Population-Based Study in Finland. Health Promot Int (2009) 24(2):108–19. 10.1093/heapro/dap007
56.
Page RM Hall CP . Psychosocial Distress and Alcohol Use as Factors in Adolescent Sexual Behavior Among Sub-Saharan Africa Adolescents. School Health (2009) 79(8):369–79. 10.1111/j.1746-1561.2009.00423.x
57.
Woodrome SE Zimet GD Orr DP Fortenberry JD . Dyadic Alcohol Use and Relationship Quality as Predictors of Condom Non-use Among Adolescent Females. J Adolesc Health (2006) 38(3):305–6. 10.1016/j.jadohealth.2005.03.018
58.
Guo C Wen X Li N Wang Z Chen G Zheng X . Is Cigarette and Alcohol Use Associated with High-Risk Sexual Behaviors Among Youth in China?J Sex Med (2017) 14(5):659–65. 10.1016/j.jsxm.2017.03.249
59.
Seth P Sales JM DiClemente RJ Wingood GM Rose E Patel SN . Longitudinal Examination of Alcohol Use: a Predictor of Risky Sexual Behavior and Trichomonas Vaginalis Among African-American Female Adolescents. Sex Transm Dis (2011) 38(2):96–101. 10.1097/OLQ.0b013e3181f07abe
60.
Cavazos-Rehg PA Spitznagel EL Bucholz KK Norberg K Reich W Nurnberger J et al The Relationship between Alcohol Problems and Dependence, Conduct Problems and Diagnosis, and Number of Sex Partners in a Sample of Young Adults. Alcohol Clin Exp Res (2007) 31(12):2046–52. 10.1111/j.1530-0277.2007.00537.x
61.
Thompson JC Kao TC Thomas RJ . The Relationship between Alcohol Use and Risk-Taking Sexual Behaviors in a Large Behavioral Study. Prev Med (2005) 41(1):247–52. 10.1016/j.ypmed.2004.11.008
62.
Hurley EA Brahmbhatt H Kayembe PK Busangu M-AF Mabiala M-U Kerrigan D . The Role of Alcohol Expectancies in Sexual Risk Behaviors Among Adolescents and Young Adults in the Democratic Republic of the Congo. J Adolesc Health (2017) 60(1):79–86. 10.1016/j.jadohealth.2016.08.023
63.
Scroggins S Shacham E . What a Difference a Drink Makes: Determining Associations between Alcohol-Use Patterns and Condom Utilization Among Adolescents. Alcohol Alcohol (2021) 56(1):34–7. 10.1093/alcalc/agaa032
64.
Izutsu T Tsutsumi A Matsumoto T . Association between Sexual Risk Behaviors and Drug and Alcohol Use Among Young People with Delinquent Behaviors. Nihon Arukoru Yakubutsu Igakkai Zasshi= Jpn J Alcohol Stud Drug Dependence (2009) 44(5):547–53.
65.
Griffin JA Renée Umstattd M Usdan SL . Alcohol Use and High-Risk Sexual Behavior Among Collegiate Women: a Review of Research on Alcohol Myopia Theory. Am Coll Health (2010) 58(6):523–32. 10.1080/07448481003621718
66.
Cooper ML . Alcohol Use and Risky Sexual Behavior Among College Students and Youth: Evaluating the Evidence. Stud Alcohol (2002)(14) 101–17. 10.15288/jsas.2002.s14.101
67.
Kann L McManus T Harris WA Shanklin SL Flint KH Hawkins J et al Youth Risk Behavior surveillance-United States, 2017. MMWR Surveill Summ (2018) 67(8):1–114. 10.15585/mmwr.ss6708a1
68.
Nguyen VK Eaton JW Devi AP Poonsukkho P Sangvichien E Tran TN et al Eumitrins F-H: Three New Xanthone Dimers from the Lichen Usnea Baileyi and Their Biological Activities. BMC Public Health (2022) 22(1):1–11. 10.1080/14786419.2021.2023143
69.
CDC. Age 21 Minimum Legal Drinking Age (2022). Available at: https://www.cdc.gov/alcohol/fact-sheets/minimum-legal-drinking-age.htm (Accessed on Sep 1, 2022).
70.
Dermen KH Cooper ML . Inhibition Conflict and Alcohol Expectancy as Moderators of Alcohol's Relationship to Condom Use. Exp Clin Psychopharmacol (2000) 8(2):198–206. 10.1037/1064-1297.8.2.198
71.
Fishbein M Yzer MC . Using Theory to Design Effective Health Behavior Interventions. Commun Theor (2003) 13(2):164–83. 10.1111/j.1468-2885.2003.tb00287.x
72.
Kaltiala-Heino R Fröjd S Marttunen M . Depression, Conduct Disorder, Smoking and Alcohol Use as Predictors of Sexual Activity in Middle Adolescence: a Longitudinal Study. Health Psychol Behav Med (2015) 3(1):25–39. 10.1080/21642850.2014.996887
73.
Ajzen I Albarracín D . Predicting and Changing Behavior: A Reasoned Action Approach. In: AjzenIAlbarracínDHornikR, editors. Prediction and Change of Health Behavior: Applying the Reasoned Action Approach. Lawrence Erlbaum Associates Publishers (2007). 3–21.
74.
Lorenz K Ullman SE . Alcohol and Sexual Assault Victimization: Research Findings and Future Directions. Aggression Violent Behav (2016) 31:82–94. 10.1016/j.avb.2016.08.001
75.
George WH Stoner SA . Understanding Acute Alcohol Effects on Sexual Behavior. Annu Rev sex Res (2000) 11(1):92–124. 10.1080/10532528.2000.10559785
76.
CDC. Substance Use and Sexual Risk Behaviors Among Youth (2019). Available at: https://www.cdc.gov/healthyyouth/substance-use/dash-substance-use-fact-sheet.htm (Accessed on Mar 7, 2023).
Summary
Keywords
meta-analysis, risky sexual behavior, alcohol consumption, adolescent, young adult
Citation
Cho H-S and Yang Y (2023) Relationship Between Alcohol Consumption and Risky Sexual Behaviors Among Adolescents and Young Adults: A Meta-Analysis. Int J Public Health 68:1605669. doi: 10.3389/ijph.2023.1605669
Received
08 December 2022
Accepted
30 March 2023
Published
19 April 2023
Volume
68 - 2023
Edited by
Gabriel Gulis, University of Southern Denmark, Denmark
Updates
Copyright
© 2023 Cho and Yang.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Youngran Yang, youngran13@jbnu.ac.kr
This Review is part of the IJPH Special Issue “Public Health and Primary Care, is 1+1=1?”
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.