Abstract
Objectives: The purpose of this study was to explore the association between multiple chronic conditions (MCCs) and depressive symptoms among older adults in China.
Methods: We used the fourth round of data from the China Health and Retirement Longitudinal Study, and included 9789 older adults aged 60 years old and above.
Results: Compared with the older adults without chronic disease, older adults with MCCs and those with one chronic disease had a high risk of depression (MCCs: OR-adjusted: 1.55, 95% CI: 1.37 to 1.75; one chronic disease: OR-adjusted: 1.20, 95% CI: 1.05–1.37). In urban areas, the prevalence among older adults with MCCs was 2.01 times higher than that among older adults without chronic disease (OR-adjusted: 2.01, 95% CI: 1.56–2.60), while it was 1.44 times higher in rural areas (OR-adjusted:1.44, 95% CI: 1.25–1.65). Self-reported health, duration of sleep, social activities, and type of medical insurance were the influencing factors of depressive symptoms in older adults.
Conclusion: This study contributed to enriching the research on the relationship between MCCs and depressive symptoms in older adults in China.
Introduction
Depression is a mental health problem characterized by persistent sadness, a loss of interest in some enjoyable activities, disturbed sleep and appetite, poor concentration, and other symptoms (1, 2). Studies have shown that when people transition from middle adulthood to older age, depressive symptoms tend to increase, often together with worsening physical health, which will cause a large disease burden with the increasing growth of the global aging population. Depression has been increasingly recognized as a serious public health concern in older populations (2–5). The Global Health Estimates Report showed that the prevalence of depression among elderly people had peaked, and more than 10% of elderly people worldwide have experienced depression (6). In China, the prevalence of depression in elderly people is approximately 15%, making depression the fourth leading cause of disability in China (7, 8).
The risk of depression, a psychiatric disorder that is related to physical health, is significantly related to the number of chronic diseases of an individual, thus the risk of depression increases with the number of chronic diseases. Hua’s study found that older adults with multiple chronic diseases (MCCs) often have different degrees of depressive symptoms (9–12). Presently, MCCs and health loss due to MCCs among older adults in China are gradually increasing (13, 14). Individual with MCCs usually require a combination of linked medical institutions for disease management from the initial screening until death, and they may need to take multiple drugs for a long time to control their conditions, which could lead to a decline in quality of life and could have varying influences on the risk of depression in older adults (11, 12). Meanwhile, Lichtman’s study showed that depression affected the occurrence, development, and prognosis of cardiovascular diseases, and it was listed as a risk factor for poor prognosis of patients with acute coronary syndrome (15), while hypertension, coronary heart disease, diabetes, and other chronic diseases were shown to be accompanied by a high incidence of depression among elderly individuals (16, 17). Thus, the risk of depression in older adults not only increases with the prevalence of physical diseases but is also related to severe neck, chest, and abdominal pain and many other chronic diseases. Mieke et al. found that the prevalence of depression in patients with chronic disease is much higher than that in the general population (11). Patients with MCCs were shown to have a higher degree of depression than those without MCCs.
In addition, due to China’s urban-rural dual economic structure, economic and social environments are different between urban and rural areas, which may have varying influences on the physical or mental health level of older adults. It is well known that there is a link between socioeconomic status and the development of disease through various mechanisms (18, 19). Urbanization, as an important manifestation of current social and economic factors, and the imbalance in social and economic development between urban and rural areas affect the differences in people’s habits and lifestyles, which leads to the heterogeneity of depression symptoms in older adults. Hu’s study showed that the age trajectories of later-life depression caseness varied by urbanization level. For both men and women and across all ages, the crude predicted probability of depression caseness was the highest in the rural group, followed by the semiurban group, and it was the lowest in the urban group (20). A meta-analysis based on 32 studies showed that the prevalence of depressive symptoms was approximately 10% higher in rural older adults aged 60 and above (29.2%) than that in their urban counterparts (20.5%) (21). Due to significant differences in the social and psychological status of elderly individuals in urban and rural areas, the proportion of elderly individuals who were at risk of developing depression was higher in rural areas (32.6%) than in urban areas (30.4%) (22). Jokela and Li’s studies found that the depression prevalence among middle-aged and older adults is lower with a higher level of urbanization (23), which was consistent with the result of Yang’s study that the prevalence rate of depression among the urban elderly individuals was lower than that of rural elderly individuals (31.9%) (24).
Dahlgren’s model of social determinants of health also pointed out that age, sex, lifestyle, social interaction, social experience and national policy environment were influencing factors of individual health (25). Wu’s study indicated that sex, age, marital status, social activities, and sleeping time and quality had significant impacts on depression in elderly individuals (26). Additionally, differences in intergenerational support received from children between urban and rural older adults receiving different intergenerational supports will have different impacts on depression in older adults, especially for those who are floating outside from their hometown (27). Jiang’s study found that self-reported health, social activities, education level and life satisfaction were influencing factors of depression in the older adults. The prevalence of depression varies significantly among older adults by self-reported health and life satisfaction (28). Therefore, we pose the following questions: after controlling for the social and environmental factors, what is the relationship between MCCs and depressive symptoms in older adults in China? After controlling for the confounding factors of socioeconomic and individual characteristics, especially when considering the background of China’s urban-rural dual structure, is there any difference in depressive symptoms between older adults living in urban and rural settings? Are there any differences in the relationship between MCCs and depressive symptoms between older adults living in urban and rural settings? Based on these questions, we propose the following two hypotheses:
Hypothesis 1MCCs are an important influencing factor of depressive symptoms in older adults in China. The proportion of having a high risk of depression in older adults with MCCs is higher than that in older adults without MCCs.
Hypothesis 2The relationship between MCCs and depressive symptoms in older adults is different between those living in urban and rural areas.
Methods
Data and Sample
Data were obtained from the fourth-round investigation of the China Health and Retirement Longitudinal Study (CHARLS), a large Chinese community study based on a sample of households with members aged 45 years or above. The investigation was conducted between July 2018 and March 2019 and involved 19817 respondents aged 45 years and above in 150 counties/districts and 450 villages/urban communities (3, 29, 30). According to the definition of older adults in China, “All citizens of the People’s Republic of China who have reached the age of 60 years belong to the older adults population,” 11055 older adults aged 60 years and above were selected as the research objects (the actual age of the older adults was calculated according to the question “What is your actual date of birth?”). According to the response of the core dependent variable (Depressive symptoms: The Center for Epidemiologic Studies Depression Scale, CES-D-10), if the respondents did not complete or refused to answer to the CES-D-10, they were removed from the study. Finally, 1266 older adults were excluded, and 9789 older adults were included in our study (for the sample screening process, see Figure 1).
FIGURE 1
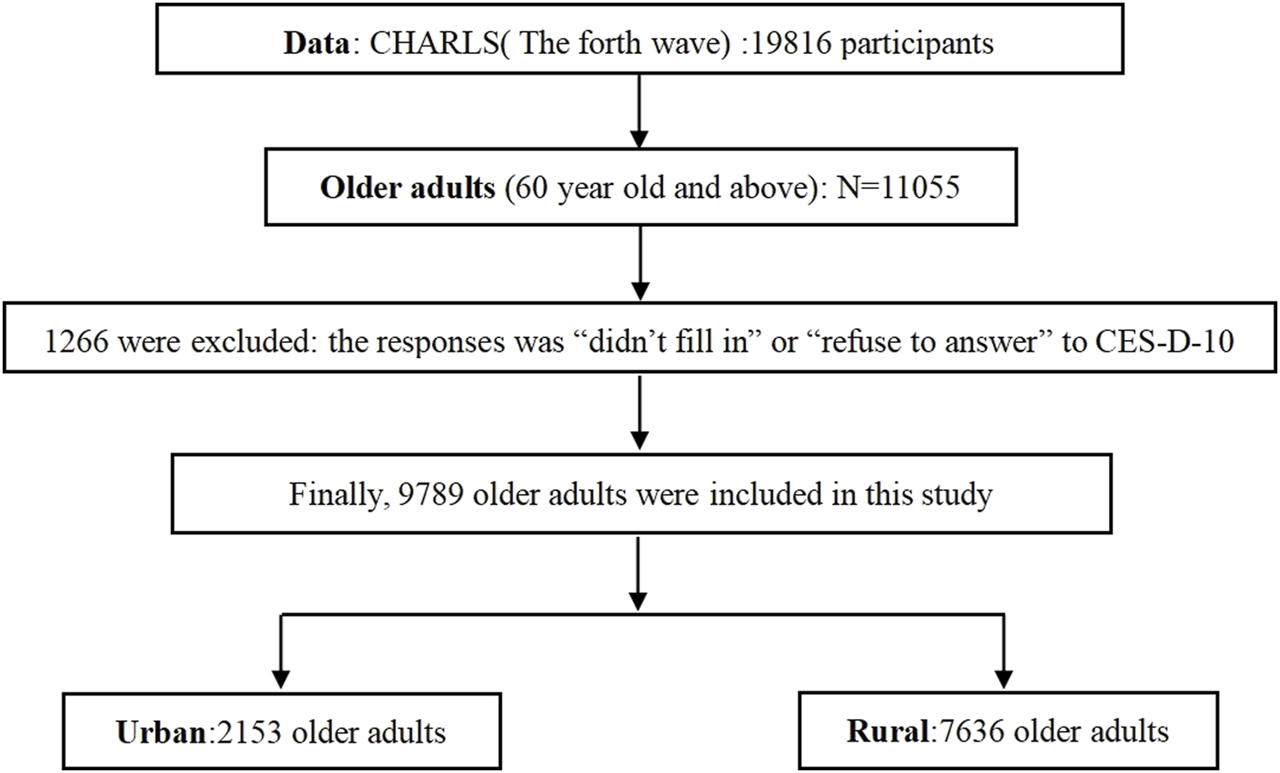
Study population screening process (China, 2018–2019).
Measures
Depressive Symptoms
Depressive symptoms of the participants were measured using the Center for Epidemiologic Studies Depression Scale (CES-D-10) (31, 32), which has been validated among the older adults and used in CHARLS (33). The CES-D-10 includes 10 questions regarding the participant’s experiences in the past week: feeling bothered, having trouble concentrating, feeling depressed, feeling as though everything required effort, feeling hopeful, feeling fearful, having restless sleep, feeling happy, feeling lonely, and having difficulty getting going (34). The total CES-D-10 score ranges from 0 to 30, with higher scores suggesting greater severity of depressive symptoms or a high risk of depression (35). In CHARLS, a cut-off score of 10 is usually used to distinguish participants (score≥ 10: high risk of depression, assigned to subgroup 1; score<10: low risk of depression, assigned to subgroup 0). In this study, the CES-D-10 had good reliability (Cronbach’s α = 0.799).
Criteria of Chronic Disease and Multiple Chronic Conditions
In CHARLS, older adults with chronic disease are those who have been diagnosed with chronic disease by a doctor up to the time of the investigation, and the question is “Have you been diagnosed with [conditions listed below, read one by one] by a doctor?”. A total of 12 chronic diseases were listed and included in this study, including hypertension, dyslipidemia (high or low), diabetes or hyperglycemia, cancer, malignant tumor, chronic lung disease, liver disease, heart disease (heart infarction, coronary heart disease, angina pectoris, congestive heart failure, etc.), stroke (including cerebral infarction and cerebral hemorrhage), kidney disease (excluding tumor or cancer), diseases of the stomach or digestive system (excluding tumor or cancer), arthritis or rheumatism, and asthma. Based on the collection of chronic disease data, the criteria for MCCs in this study were defined as follows: if the older adults had two or more chronic diseases, they were defined as MCC patients. The variable of “MCCs or not” was defined as follows: if the older adults had two or more chronic diseases, they were assigned to subgroup 3; if they had one chronic disease, they were assigned to subgroup 2; and if they have no chronic disease, they were assigned to subgroup 1.
Statistical Analysis
Descriptive analysis (N/%) was used to describe the status of MCCs and depressive symptoms of the older adults, and the chi-square test was used to compare the depressive symptoms between the older adults with MCCs and those without MCCs. Then, a generalized linear model (GLM) was employed to analyze the association between MCCs and depressive symptoms after controlling for other confounding factors, including analysis of urban and rural areas, and the results were expressed as adjusted odds ratios (OR-adjusted) and their 95% confidence intervals (95% CI).
GLM is an extension of the traditional linear model that allows the overall average to depend on a linear predictor through a non-linear link function and allows the response probability distribution to be any member of the exponential distribution family, including the logistic regression model. In this study, a binary logistic regression model was used to analyze the influence of MCCs on depressive symptoms in older adults in urban areas or rural areas after controlling for the confounding factors of sex, residence, education level, per capita household income, duration of sleep, social activities, self-reported health, type of medical insurance, life satisfaction, health satisfaction, marital satisfaction and child relationship satisfaction. A GLM always includes three components:
In our study, we chose as the link function; therefore, the form of the generalized linear model was:
In Eq. 4, is the prevalence rate of depressive symptoms in older adults, is a constant and is the regression coefficient, which represents the effect of on the predictive value of individual incidence (Y = 1).
All statistical analyses were performed using IBM SPSS Statistics V22.0, and a result with a p-value < 0.05 was considered statistically significant.
Results
The characteristics of the participants (9789 older adults) are displayed in Table 1. A total of 2,153 (22.0%) older adults lived in urban areas, and 7,636 (78.0%) lived in rural areas, including 4,933 (48.9%) male and 5,150 (51.1%) female older adults. A total of 30.7% of the older adults were aged 60–64 years old, 43.7% were aged 65–74 years old and 25.6% were aged over 75 years old. A total of 53.5% of the older adults had social activities, and 72.6% of the older adults stated that their self-reported health was “very good,” “good,” or “fair.” A total of 65.2% and 80.7% of the older adults were satisfied with their health and life, respectively. A total of 54.4% of the older adults suffered from MCCs, and 43.5% had a high risk of depression. There were significant differences in the prevalence of a high risk of depression between the older adults with or without MCCs, and the prevalence of a high risk of depression among the older adults with MCCs was higher than that of those with no chronic diseases or one chronic disease (χ2 = 399.59, p < 0.001). without controlling for other confounding factors, the prevalence of a high risk of depression among older adults with MCCs was 1.84 times higher than that of the older adults who had no chronic diseases without controlling for other factors. Meanwhile, the prevalence of a high risk of depression among older adults living in rural setting was higher than that among older adults living in an urban setting (χ2 = 5.88, p < 0.05). The prevalence of a high risk of depression among older adults with no social activities was higher than that among older adults who had social activities (χ2 = 40.41, p < 0.001). There were also significant differences in the prevalence of a high risk of depression among the older adults in different groups of self-reported health, duration of sleep, per capita household income, and medical insurance types (Table 2).
TABLE 1
| Variables | Options | N (%) | Variables | Options | N (%) |
|---|---|---|---|---|---|
| Residence | Urban | 2,153 (22.0) | Duration of sleep | ≤5 h | 3,317 (33.9) |
| Rural | 7,636 (78.0) | 6–9 h | 6,055 (61.9) | ||
| Sex | Male | 4,779 (48.8) | ≥10 h | 417 (4.3) | |
| Female | 5,010 (51.2) | Social activities | Yes | 5,237 (53.5) | |
| Age(year) | 60-64 | 3,009 (30.7) | No | 4,552 (46.5) | |
| 65-74 | 4,273 (43.7) | Per capita household income | Low income | 3,728 (38.1) | |
| ≥75 | 2,507 (25.6) | Middle income | 4,858 (49.6) | ||
| Marital status | Married and living with spouse | 7,287 (74.4) | High income | 1,203 (12.3) | |
| Married, not living with spouse | 365 (3.7) | Life satisfaction | Satisfied | 7,900 (80.7) | |
| Dissatisfied | 1889 (19.3) | ||||
| Divorced | 94 (1.0) | Health satisfaction | Satisfied | 6,387 (65.2) | |
| Widowed | 1974 (20.2) | Dissatisfied | 3,402 (34.8) | ||
| Marital satisfaction | Satisfied | 7,727 (78.9) | |||
| Never married | 69 (0.7) | Dissatisfied | 846 (8.6) | ||
| Education level | Illiterate | 3,103 (31.7) | Child relationship satisfaction | Satisfied | 9247 (94.5) |
| Primary school and below | 4,256 (43.5) | Dissatisfied | 453 (4.6) | ||
| Elementary school and above | 2,430 (24.8) | Type of medical insurance | Urban employees | 1,320 (13.5) | |
| Self-reported health | Very good | 1,068 (10.9) | Urban and rural residents | 7,504 (76.7) | |
| Good | 1,225 (12.5) | Free | 617 (6.3) | ||
| Fair | 4,812 (49.2) | Commercial insurance and others | 348 (3.6) | ||
| Poor | 2016 (20.6) | Chronic disease | Yes | 7,704 (78.7) | |
| Very poor | 653 (6.7) | No | 2085 (21.3) | ||
| Depression | High risk of depression | 4,258 (43.5) | MCCs | No chronic disease | 2088 (21.3) |
| Low risk of depression | 5,531 (56.5) | One chronic disease | 2,376 (24.3) | ||
| MCCs | 5,325 (54.4) |
The characteristics of the study participants (China, 2018–2019).
TABLE 2
| Variables | Option | High risk of depression (N/%) | Low risk of depression (N/%) | χ 2 -value |
|---|---|---|---|---|
| MCCs or not | No chronic disease | 592 (28.4) | 1,496 (71.6) | 399.59** |
| Having one chronic disease | 884 (37.2) | 1,492 (62.8) | ||
| Having MCCs | 2,783 (52.3) | 2,542 (47.7) | ||
| Sex | Male | 2058 (43.1) | 2,721 (56.9) | 0.75 |
| Female | 2,201 (43.9) | 2,809 (56.1) | ||
| Residence | Urban | 3,273 (42.9) | 4,363 (57.1) | 5.88* |
| Rural | 986 (45.8) | 1,167 (54.2) | ||
| Age (years) | 60–64 | 1,295 (43.0) | 1714 (57.0) | 0.46 |
| 65–74 | 1873 (43.8) | 2,400 (56.2) | ||
| ≥75 | 1,091 (43.5) | 1,416 (56.50 | ||
| Marital status | Married and living with spouse | 3,175 (43.6) | 4,112 (56.4) | 0.66 |
| Married, not living with spouse | 152 (41.6) | 213 (58.4) | ||
| Divorced | 40 (42.6) | 54 (57.4) | ||
| Widowed | 863 (43.7) | 1,111 (56.3) | ||
| Never married | 29 (42.0) | 40 (58.0) | ||
| Education level | Illiterate | 1,370 (44.2) | 1739 (55.8) | 2.68 |
| Primary school and below | 1866 (43.8) | 2,390 (56.2) | ||
| Elementary school and above | 1,023 (42.1) | 1,407 (57.9) | ||
| Self-reported health | Very good | 217 (20.3) | 851 (79.7) | 1,063.75** |
| Good | 312 (25.5) | 913 (74.5) | ||
| Fair | 1921 (39.9) | 2,891 (60.1) | ||
| Poor | 1,316 (65.3) | 700 (34.7) | ||
| Very poor | 486 (74.4) | 167 (5.6) | ||
| Per capita household income | Low income | 1739 (46.6) | 1989 (53.4) | 28.51** |
| Middle income | 2052 (42.2) | 2,806 (57.8) | ||
| High income | 468 (38.9) | 735 (61.1) | ||
| Duration of sleep | ≤5 h | 1955 (58.9) | 1,362 (41.1) | 487.42** |
| 6–9 h | 2,144 (35.4) | 3,911 (64.5) | ||
| ≥10 h | 160 (38.4) | 257 (61.6) | ||
| Social activities | No | 2,136 (46.9) | 2,416 (53.1) | 40.41** |
| Yes | 2,123 (40.5) | 3,114 (59.5) | ||
| Life satisfaction | Satisfied | 828 (43.8) | 1,061 (56.2) | 0.10 |
| Dissatisfied | 3,431 (43.4) | 4,469 (56.6) | ||
| Health satisfaction | Satisfied | 1,458 (42.9) | 1944 (57.1) | 0.90 |
| Dissatisfied | 2,801 (43.9) | 3,586 (56.1) | ||
| Marital satisfaction | Satisfied | 360 (42.6) | 486 (57.4) | 0.43 |
| Dissatisfied | 3,364 (43.5) | 4,363 (56.5) | ||
| Never married | 535 (44.0) | 681 (56.0) | ||
| Child relationship satisfaction | Satisfied | 185 (40.8) | 268 (59.2) | 1.75 |
| Dissatisfied | 4,038 (43.7) | 5,209 (56.3) | ||
| No child | 36 (40.4) | 53 (59.6) | ||
| Type of medical insurance | Urban employees | 471 (35.7) | 849 (64.3) | 40.83** |
| Urban and rural residents | 3,379(45.0) | 4,125 (55.0) | ||
| Free | 257 (41.7) | 360 (58.3) | ||
| Commercial insurance and others | 152 (43.7) | 196 (56.3) |
Comparison of the prevalence of depressive symptoms in older adults (China, 2018–2019).
Note: *p < 0.05; **p < 0.01.
After controlling for the variables of sex, residence, age, marital status, education level, self-reported health, per capita household income, duration of sleep, life satisfaction, health satisfaction, child relationship satisfaction, and type of medical insurance (Table 3), the prevalence of a high risk of depression among the older adults with MCCs was 1.55 times higher than that in the older adults without chronic disease (OR-adjusted: 1.55, 95% CI: 1.37–1.75), and the prevalence of high risk of depression among the older adults with one chronic disease was 1.20 times higher than that of the older adults without chronic disease (OR-adjusted: 1.20, 95% CI: 1.05–1.37), which supported the first hypothesis of our study (MCCs are an important influencing factor of depressive symptoms in older adults in China. The proportion of having high a risk of depression in older adults with MCCs is higher than that in older adults without MCCs).
TABLE 3
| Variables | Options | Model I | Model II | ||
|---|---|---|---|---|---|
| OR | OR (95% CI) | OR | OR (95% CI) | ||
| MCCs or not | No chronic disease | - | - | 1 | - |
| Having one chronic disease | - | - | 1.20** | 1.05, 1.37 | |
| Having MCCs | - | - | 1.55** | 1.37, 1.75 | |
| Sex | Male | 1 | - | 1 | - |
| Female | 1.01 | 0.92, 1.12 | 1.02 | 0.93, 1.23 | |
| Residence | Urban | 1 | - | 1 | - |
| Rural | 1.12* | 1.01, 1.24 | 1.13* | 1.01, 1.25 | |
| Age (years) | 60–64 | 1 | - | 1 | - |
| 65–74 | 1.05 | 0.94, 1.16 | 1.05 | 0.94, 1.16 | |
| ≥75 | 1.01 | 0.89, 1.14 | 1.01 | 0.89, 1.14 | |
| Marital status | Married and living with spouse | 1 | - | 1 | - |
| Married, not living with spouse | 1.01 | 0.80, 1.27 | 1.01 | 0.80, 1.28 | |
| Divorced | 0.98 | 0.62, 1.55 | 1.01 | 0.64, 1.60 | |
| Widowed | 1.01 | 0.87, 1.16 | 1.00 | 0.87, 1.16 | |
| Never married | 0.90 | 0.52, 1.55 | 0.90 | 0.52, 1.55 | |
| Education level | Illiterate | 1 | - | 1 | - |
| Primary school and below | 0.98 | 0.88, 1.10 | 0.98 | 0.88, 1.09 | |
| Elementary school and above | 0.91 | 0.80, 1.03 | 0.91 | 0.80, 1.03 | |
| Self-reported health | Very good | 1 | - | 1 | - |
| Good | 1.30** | 1.07, 1.59 | 1.25* | 1.03, 1.53 | |
| Fair | 2.40** | 2.04, 2.82 | 2.15** | 1.82, 2.53 | |
| Poor | 6.23** | 5.21, 7.44 | 5.13** | 4.26, 6.17 | |
| Very poor | 9.57** | 7.57, 12.10 | 7.68** | 6.03, 9.77 | |
| Per capita household income | Low income | 1 | - | 1 | - |
| Middle income | 0.92 | 0.84, 1.01 | 0.92 | 0.84, 1.01 | |
| High income | 0.91 | 0.78, 1.07 | 0.91 | 0.78, 1.07 | |
| Duration of sleep | ≤5 h | 1 | - | 1 | - |
| 6–9 h | 0.45** | 0.41, 0.49 | 0.46** | 0.42, 0.51 | |
| ≥10 h | 0.48** | 0.39, 0.60 | 0.49** | 0.39, 0.62 | |
| Social activities | No | 1 | - | 1 | - |
| Yes | 0.88** | 0.81, 0.96 | 0.87** | 0.80, 0.95 | |
| Life satisfaction | Dissatisfied | 1 | - | 1 | - |
| Satisfied | 0.95 | 0.84, 1.09 | 0.95 | 0.84,1.09 | |
| Health satisfaction | Dissatisfied | 1 | - | 1 | - |
| Satisfied | 1.03 | 0.92, 1.15 | 1.03 | 0.92, 1.15 | |
| Marital satisfaction | Dissatisfied | 1 | - | 1 | - |
| Satisfied | 1.04 | 0.92, 1.18 | 1.05 | 0.93, 1.18 | |
| Child relationship satisfaction | Dissatisfied | 1 | - | 1 | - |
| Satisfied | 1.12 | 0.91, 1.36 | 1.12 | 0.92, 1.37 | |
| Type of medical insurance | Urban employees | 1 | - | 1 | - |
| Urban and rural residents | 1.28** | 1.11, 1.47 | 1.29** | 1.12, 1.48 | |
| 0 | Free | 1.23 | 1.00, 1.52 | 1.23 | 0.99, 1.52 |
| Commercial insurance and others | 1.28 | 0.98, 1.67 | 1.29 | 0.99, 1.69 | |
Influence of having multiple chronic conditions on the risk of depression among older adults (China, 2018–2019).
Taking the first category as the reference category (the one with the minimum value).
OR: OR-adjusted odds ratio with other variables controlled; 95% CI: 95% confidence interval.
*p < 0.05, **p < 0.01.
Showcasing the impact of urban-rural difference on depression in older adults, after controlling for MCCs and other confounding factors the prevalence of a high risk of depression among older adults living in rural areas was 1.13 times higher than that among older adults living in urban areas (OR-adjusted: 1.13, 95% CI: 1.01–1.25), which indicated that there were differences in depressive symptoms between older adults in urban and rural settings. Meanwhile, whether in urban or rural areas, having MCCs was an influencing factor of depressive symptoms in older adults (Table 4). The prevalence of a high risk of depression in the older adults with MCCs was 2.01 times higher than that among older adults without chronic disease and living in urban areas (OR-adjusted = 2.01, 95% CI: 1.56–2.60), while it was 1.44 times higher than that of older adults living in rural areas (OR-adjusted = 1.44, 95% CI: 1.25–1.65), which supported hypothesis 2 of our study (The relationship between MCCs and depressive symptoms in older adults is different between those living in urban and rural areas). In rural areas, the prevalence of a high risk of depression in the older adults with one chronic disease was 1.18 times higher than that in older adults without chronic disease and living in urban areas (OR-adjusted = 1.18, 95% CI: 1.01–1.37). The variables of self-reported health, sleep duration, social activities, and type of medical insurance were influencing factors of depressive symptoms among older adults in both urban and rural areas.
TABLE 4
| Variables | Options | Urban | Rural | ||
|---|---|---|---|---|---|
| OR | OR (95% CI) | OR | OR (95% CI) | ||
| MCCs or not | No chronic disease | 1 | - | 1 | - |
| Having one chronic disease | 1.27 | 0.95, 1.68 | 1.18* | 1.01, 1.37 | |
| Having MCCs | 2.01** | 1.56, 2.60 | 1.44** | 1.25, 1.65 | |
| Sex | Male | 1 | - | 1 | - |
| Female | 0.94 | 0.76, 1.16 | 1.04 | 0.94, 1.16 | |
| Age | 60–64 | 1 | - | 1 | - |
| 65–74 | 1.02 | 0.82, 1.28 | 1.06 | 0.94, 1.19 | |
| ≥75 | 0.85 | 0.65, 1.11 | 1.06 | 0.92, 1.22 | |
| Marital status | Married and living with spouse | 1 | - | 1 | - |
| Married, not living with spouse | 1.04 | 0.65, 1.67 | 1.02 | 0.78, 1.33 | |
| Divorced | 1.61 | 0.60, 4.33 | 0.88 | 0.52, 1.49 | |
| Widowed | 1.09 | 0.80, 1.47 | 0.99 | 0.84, 1.17 | |
| Never married | 0.89 | 0.29, 2.74 | 0.93 | 0.50, 1.75 | |
| Education level | Illiterate | 1 | - | 1 | - |
| Primary school and below | 1.01 | 0.80, 1.28 | 0.97 | 0.86, 1.10 | |
| Elementary school and above | 0.82 | 0.62, 1.09 | 0.93 | 0.80, 1.07 | |
| Self-reported health | Very good | 1 | - | 1 | - |
| Good | 1.21 | 0.79, 1.86 | 1.28* | 1.02, 1.61 | |
| Fair | 2.23** | 1.56, 3.16 | 2.12** | 1.76, 2.56 | |
| Poor | 4.89** | 3.30, 7.26 | 5.23** | 4.24, 6.45 | |
| Very poor | 4.75** | 2.86, 7.88 | 8.82** | 6.70, 11.62 | |
| Per capita household income | Low income | 1 | - | 1 | - |
| Middle income | 0.98 | 0.80, 1.20 | 0.91 | 0.81, 1.01 | |
| High income | 1.18 | 0.84, 1.66 | 0.85 | 0.71, 1.01 | |
| Duration of sleep | ≤5 h | 1 | - | 1 | - |
| 6–9 h | 0.46** | 0.37, 0.56 | 0.46** | 0.42, 0.52 | |
| ≥10 h | 0.43** | 0.27, 0.67 | 0.51** | 0.40, 0.66 | |
| Social activities | No | 1 | - | 1 | - |
| Yes | 0.80* | 0.67, 0.97 | 0.90* | 0.82, 0.99 | |
| Life satisfaction | Dissatisfied | 1 | - | 1 | - |
| Satisfied | 0.99 | 0.75, 1.32 | 0.94 | 0.81, 1.10 | |
| Health satisfaction | Dissatisfied | 1 | - | 1 | - |
| Satisfied | 1.13 | 0.89, 1.42 | 1.00 | 0.89, 1.13 | |
| Marital satisfaction | Dissatisfied | 1 | - | 1 | - |
| Satisfied | 0.91 | 0.71, 1.18 | 1.09 | 0.94, 1.25 | |
| Child relationship satisfaction | Dissatisfied | 1 | - | 1 | - |
| Satisfied | 1.02 | 0.66, 1.58 | 1.13 | 0.90, 1.42 | |
| Type of medical insurance | Urban employees | 1 | - | 1 | - |
| Urban and rural residents | 1.61** | 1.14, 2.29 | 1.22* | 1.04, 1.43 | |
| Free | 1.55 | 0.94, 2.55 | 1.28 | 0.93, 1.49 | |
| Commercial insurance and others | 1.42 | 0.86, 2.34 | 1.30 | 0.93, 1.80 | |
Influence of having multiple chronic conditions on the risk of depression among older adults in urban and rural areas (China, 2018–2019).
Taking the first category as the reference category (the one with the minimum value).
OR: OR-adjusted, odds ratio with other variables controlled; 95% CI: 95% confidence interval.
*p < 0.05, **p < 0.01.
Discussion
These analyses added important information to understand the relationship between MCCs and depression among the older adults in China, using a nationally representative cross-sectional dataset of CHARLS. We found that there was a significant difference in the prevalence of a high risk of depression between older adults with MCCs and those without chronic disease, and the prevalence of a high risk of depression in older adults with MCCs was significantly higher than that in older adults without chronic disease. The results indicated that MCCs were an important influencing factor on depressive symptoms in older adults, which was consistent with the results of Meher’s study, which showed that the association between the number of chronic conditions and depression exhibited a linear trend with an increased odds ratio indicating a higher risk of depression among older adults with multiple chronic conditions (36). Our study found that 52.3% of the older adults with MCCs had a high risk of depression, and the prevalence of a high risk of depression among the older adults without chronic disease was 27.4%. Other studies also indicated that older adults with chronic diseases often have different degrees of depression, and the number of chronic diseases was positively related to the score of depressive symptoms: the more MCCs, the higher the score of depressive symptoms (37–40). Usually, MCCs among older adults have a long course, are difficult to cure, and easily recur. Some patients need long-term or even lifelong treatment, which aggravates the patient’s economic pressure, thus increasing the mental pressure and psychological disorder of older patients. The risk of depression in older adults with cerebrovascular disease, coronary heart disease, diabetes, and visual impairment is higher than that in older adults without those chronic diseases (39, 40). Depressive symptoms were associated with increased medical utilization and expenditure among chronic lung disease patients, which varies between urban and rural areas (41).
In particular, under the background of rapid urbanization, the proportion of the urban population increased from 26% in 1990% to 60.6% in 2019 in China. Moving to urban areas is viewed as a means of upwards social mobility in China, as it will lead to a better educational environment, more economic resources, more opportunities, and a sense of cultural and psychological preeminence (41). The difference between residing in urban and rural areas has different effects on depression symptoms in older adults. Our study showed that urban versus rural residences were the influencing factors of depression symptoms in older adults after controlling for other confounding factors. The prevalence of a high risk of depression among older adults living in rural areas was 1.13 times higher than that among older adults living in urban areas, which was consistent with the results of some previous studies (41–43).
Whether in urban or rural areas, the variables of self-reported health, duration of sleep, social activities, and type of medical insurance were the influencing factors of depressive symptoms in older adults; the worse their self-reported health, the higher the risk of depression in older adults, which was consistent with the results of Maier et al.’s study. In their meta-analysis, the results of the heterogeneity analysis indicated that self-reported health had a significant influence in several studies. Quality of physical activity, chronic disease, and difficulty initiating sleep increased the risk of depression (44). The risk of depression among older adults was also associated with the duration of sleep. Our study also found that the prevalence of a high risk of depression among older adults who slept 6–9 h every day was 0.46 times higher than that among the older adults who slept for less than 6 h, and the prevalence of a high risk of depression among older adults who slept 10 or more hours every day was 0.49 times higher than that among older adults who slept for less than 6 h. The prevalence of high a risk of depression among the older adults who slept less than or equal to 5 h was the highest, followed by those who slept more than or equal to 10 h, and the prevalence of high risk of depression among the older adults who slept for 6–9 h was the lowest. The results indicated that proper sleep time could reduce the risk of depression in elderly individuals, which was similar to the results of Zeo’s study to some extent. Compared with older adults who had less than 5 h sleep, those who had more sleep had a lower risk of depression (28, 45). The duration of sleep was a significant influencing factor against depressive symptoms in old people. Their study also pointed out that the quality of sleep affected the risk of depressive symptoms and moderated the relationship between pain interference and depressive symptoms among older adults with chronic pain, such that good sleep quality attenuated the effect of pain interference on depression, and poor sleep quality amplified the effect of pain interference on depression (45–47).
Meanwhile, we found that social activities could reduce the risk of depression in older adults. The prevalence of a high risk of depression among people who participated in social activities was lower than that among older adults who did not participate in social activities, whether in rural or urban areas. The results in Wang’s study indicated that for urban respondents, playing mah-jong or cards and joining sports or social clubs predicted a decline in depressive symptoms. For rural residents, interacting with friends regularly was associated with fewer depressive symptoms. In conclusion, a more diverse and higher frequency of social participation was associated with better mental health, while the social significance of social participation varied across different types of social participation and between rural and urban areas (48). Therefore, social activities play an important role in depressive symptoms among older adults. We can try to encourage and provide social opportunities for older adults based on their personal needs, preferences and abilities, actively build entertainment and leisure service facilities, and encourage older adults to participate in more social activities, which may reduce the risk of depression to some extent.
Conclusion
Our study found that whether they were living in urban or rural areas, MCCs were important factors influencing depressive symptoms among older adults. Compared with older adults without MCCs, older adults with MCCs have a higher risk of depression, and the influence of MCCs on depressive symptoms in older adults is different between urban and rural areas. This study added important information to help us understand the relationship between MCCs and depressive symptoms in older adults in China. However, there are also some limitations: (1) We analyzed the relationship between MCCs and depressive symptoms among older adults based on a cross-sectional study, not on a cohort study. Therefore, the evidence of this study was weak regarding the determination of a causal relationship. (2) This study only focused on the impact of MCCs on depressive symptoms in older adults, but did not consider the impact of different types of chronic disease and different combinations of chronic diseases. The impact of different types and combinations of chronic diseases on depressive symptoms needs in-depth study in the future. (3) Although the CES-D-10 has been widely used in the investigation of depressive symptoms and has good reliability, it was based on the subjective feelings of participants and not a diagnosis from a doctor. Therefore, the results from the screening tool may include some false-positives.
Statements
Ethics statement
Ethical approval for the China Health and Retirement Longitudinal Study (CHARLS) was granted by the Institutional Review Board (IRB) of Peking University. The IRB approval number for the main household survey including anthropometrics is IRB00001052-11015, and the IRB approval number for biomarker collection is IRB00001052-11014. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
Conceptualization: HL and ZZ; Methodology: XF and CS; Software: HS and HL; Formal analysis and writing the original draft preparation: HL and YM; Review and modification: HL, ZZ, YM, and CS. All authors have read and agreed to the published version of the manuscript and have no competing interests.
Funding
This work was supported by the Shandong Province Natural Science Foundation (grant number: ZR2021QG050) and Social Science Planning Project of Shandong Province (grant number: 21DRKJ02).
Acknowledgments
First, thanks the Institute of Social Science Survey of Peking University for their organization of the CHARLS and all the participants, investigators, and assistants of the CHARLS (Wave 4), especially Zhao YH, John S, Chen XX, Wang YF, Gong JQ, Meng QQ, Wang GW, and Wang HL. Second, we would like to thank ZZ, XF, and CS for their excellent writing suggestions, YM, HS, and ZX for providing assistance with data management and analysis. Finally, in order to communicate with peers more timely and improve our manuscript, the original version of this article has been uploaded to a preprint server of Research Square (https://www.researchsquare.com/article/rs-1740273/v1), but it has not previously been peer reviewed or published by any other journal.
Conflict of interest
The authors declare that they do not have any conflicts of interest.
References
1.
Andrade GE Martinez GD Rodriguez AF Garcia-Esquinas E . Sedentary Behaviors, Physical Activity, and Changes in Depression and Psychological Distress Symptoms in Older Adults. Depress Anxiety (2018) 35:884–97. 10.1002/da.22804
2.
Ouyang P Sun W . The Association between Depressive Symptoms and Fall Accidents Among Middle-Aged and Elderly People in China. Environ Health Prev Med (2018) 23(1):42. 10.1186/s12199-018-0735-y
3.
Zhao Y Atun R Oldenburg B McPake B Tang S Mercer SW et al Physical Multimorbidity, Health Service Use, and Catastrophic Health Expenditure by Socioeconomic Groups in China: an Analysis of Population-Based Panel Data. Lancet Glob Health (2020) 8:e840–9. 10.1016/S2214-109X(20)30127-3
4.
Zhao YW Haregu TN He L Lu S Katar A Wang H et al The Effect of Multi-Morbidity on Functional Limitations and Depression Amongst Middle-Aged and Older Population in China a Nationwide Longitudinal Study. Age Ageing (2020) 6(10):190–7. 10.1093/ageing/afaa117
5.
Wilkinson P Ruane C Tempest K . Depression in Older Adults. BMJ (2018) 363:k4922. 10.1136/bmj.k4922
6.
World Health Organization. Depression and Other Common Mental Disorders: Global Health Estimates. Geneva: World Health Organization (2017). p. 2.
7.
Li D Zhang DJ Shao JJ Qi X Tian L . A Meta-Analysis of the Prevalence of Depressive Symptoms in Chinese Older Adults. Arch Gerontol Geriatr (2014) 58(1):1–9. 10.1016/j.archger.2013.07.016
8.
GBD. Global, Regional, and National Incidence, Prevalence, and Years Lived with Disability for 328 Diseases and Injuries for 195 Countries, 1990-2016: a Systematic Analysis for the Global Burden of Disease Study 2016. Lancet (2017) 390(10100):1211–59. 10.1016/S0140-6736(17)32154-2
9.
Hua QZ Ni CP Xu QL . A Study on Relatioship between Chronic Diseases and Depressive Syptoms of Senile People in Community in Xi’an City. Chin Nurs Res (2009) 23(2):390–2. 10.3969/j.issn.1009-6493.2009.05.007
10.
Lai TT Ma TW Hou WK . Multimorbidity Is Associated with More Subsequent Depressive Symptoms in Three Months: a Prospective Study of Community-Dwelling Adults in Hong Kong. Int Psychogeriatr (2018) 31:1367–71. 10.1017/S1041610218001916
11.
Mieke BT . Multiple Chronic Conditions, Spouse’s Depressive Symptoms, and Gender within Marriage. J Health Soc Behav (2016) 57(1):59–76. 10.1177/0022146516628179
12.
Ecks S . Depression, Deprivation, and Dysbiosis: Polyiatrogenesis in Multiple Chronic Illnesses. Cult Med Psychiatry (2021) 45(4):507–24. 10.1007/s11013-020-09699-x
13.
Zhang R Lu Y Zhang SS . Prevalence Pattern and Component Correlation of Chronic Disease Comorbidity Among the Elderly People in China. Chin J Public Health (2019) 35(8):1003–5. 10.11847/zgggws1120351
14.
Li SS Zhang LW Lu QC . The Prevalence of Multi-Morbidity and Related Functional Limitation Among Middleaged and Senior Population in China: Nationally Evidence from CHARLS 2018. J Pract Med (2021) 37(4):518–24. 10.3969/j.issn.1006-5725.2021.04.020
15.
Lichtman JH Froelicher ES Blumenthal JA Carney RM Doering LV Frasure-Smith N et al Depression as a Risk Factor for Poor Prognosis Among Patients with Acute Coronary Syndrome: Systematic Review and Recommendations: a Scientific Statement from the American Heart Association. Circulation (2014) 129(12):1350–69. 10.1161/CIR.0000000000000019
16.
Zhang Y Chen Y Ma L . Depression and Cardiovascular Disease in Elderly: Current Understanding. J Clin Neurosci (2018) 47:1–5. 10.1016/j.jocn.2017.09.022
17.
Mittag O Meyer T . The Association of Depressive Symptoms and Ischemic Heart Disease in Older Adults Is Not Moderated by Gender, Marital Status or Education. Int J Public Health (2012) 57(1):79–85. 10.1007/s00038-011-0256-6
18.
Jonassen M Shaheen A Duraidi M Qalalwa K Jeune B Bronnum-Hansen H . Socio-economic Status and Chronic Disease in the West Bank and the Gaza Strip: in and outside Refugee Camps. Int J Public Health (2018) 63(7):875–82. 10.1007/s00038-018-1122-6
19.
World Health Organization. China Country Assessment Report on Ageing and Health. Geneva: Switzerland (2015) 3.
20.
Hu Y Li P Martikainen P . Rural-urban Disparities in Age Trajectories of Depression Caseness in Later Life: the china Health and Retirement Longitudinal Study. PLoS One (2019) 14:e0215907. 10.1371/journal.pone.0215907
21.
Yang GH Wang Y Zeng YX Gao GF Liang X Zhou M et al Rapid Health Transition in China, 1990-2010: Findings from the Global Burden of Disease Study 2010. Lancet (2013) 381(9882):1987–2015. 10.1016/S0140-6736(13)61097-1
22.
Akila GV Arvind BA Isaac A . Comparative Assessment of Psychosocial Status of Elderly in Urban and Rural Areas, Karnataka, India. J Fam Med Prim Care (2019) 8(9):2870–6. 10.4103/jfmpc.jfmpc_536_19_536_19
23.
Jokela M Batty GD Vahtera J Elovainio M Kivimaki M . Socioeconomic Inequalities in Common Mental Disorders and Psychotherapy Treatment in the UK between 1991 and 2009. Br J Psychiatry (2013) 202(2):115–20. 10.1192/bjp.bp.111.098863
24.
Yang Z Chen R Hu X Ren XH . Factors that Related to the Depressive Symptoms Among Elderly in Urban and Rural Areas of China. China J Epidemiol (2017) 38(08):1088–93. 10.3760/cma.j.issn.0254-6450.2017.08.018
25.
Escalante E Golden RL Mason DJ . Social Isolation and Loneliness Imperatives for Health Care in a Post—COVID World. JAMA (2020) 325(6):520–1. 10.1001/jama.2021.0100
26.
Wu S Zhang FY Zang ZY . Analysis on Depression and Life Satisfaction of the Elderly in China and Influencing Factors. J Zhengzhou Univ (2019) 54(1):88–92. 10.13705/j.issn.1671-6825.2018.06.157
27.
Ruan YH Zhu DM . Association of Chinese Drifting Elderly's Intergenerational Support Satisfaction with Expectation: A Mixed Method Study in Shanghai. Int J Health Plann Manage (2020) 36:173–88. 10.1002/hpm.3078
28.
Jiang CH Zhu F Qin TT . Relationships between Chronic Diseases and Depression Among Middle Aged and Elderly People in China: A Prospective Study from CHARLS. Curr Med Sci (2020) 40(05):858–70. 10.1007/s11596-020-2270-5
29.
Zhao YW Haregu TN He L Lu S Katar A Wang H et al The Effect of Multimorbidity on Functional Limitations and Depression Amongst Middle-Aged and Older Population in China: a Nationwide Longitudinal Study. Age Ageing (2021) 50(1):190–7. 10.1093/ageing/afaa117
30.
Zhao YH John S Chen XX Park A . Wave 4 User’s Guide China Health and Retirement Longitudinal StudyBeijing, China: National School of Development Peking University (2020).
31.
Shaffer K . Center for Epidemiologic Studies Depression (CES-D) Scale. In: MichalosAC editor. Encyclopedia of Quality of Life and Well-Being Research. Dordrecht: Springer (2014).
32.
Lewinsohn PM Seeley JR Roberts RE Allen NB . Center for Epidemiologic Studies Depression Scale (CES-D) as a Screening Instrument for Depression Among Community-Residing Older Adults. Psychol Aging (1997) 12(2):277–87. 10.1037//0882-7974.12.2.277
33.
Chen HJ Mui AC . Factorial Validity of the Center for Epidemiologic Studies Depression Scale Short Form in Older Population in China. Int Psychogeriatrics (2014) 26(1):49–57. 10.1017/S1041610213001701
34.
Qin T Liu W Yin M Shu C Yan M Zhang J et al Body Mass index Moderates the Relationship between C-Reactive Protein and Depressive Symptoms: Evidence from the China Health and Retirement Longitudinal Study. Sci Rep (2017) 7:39940. 10.1038/srep39940
35.
Baron EC Davies T Lund C . Validation of the 10-item Centre for Epidemiological Studies Depression Scale (CES-D-10) in Zulu, Xhosa and Afrikaans Populations in South Africa. BMC Psychiatry (2017) 17(1):6. 10.1186/s12888-016-1178-x
36.
Meher T Muhammad T Gharge S . The Association between Single and Multiple Chronic Conditions and Depression Among Older Population in India: A Comparative Study between Men and Women. Int J Geriatr Psychiatry (2022) 37:37. 10.1002/gps.5639
37.
Verhaak PF Dekker JH Waal MW . Depression, Disability and Somatic Diseases Among Elderly People. J Affective Disord (2014) 167:187–91. 10.1002/gps.5639
38.
Rachel AP Maureen WG Allison RH . Multiple Chronic Condition Combinations and Depression in Community-Welling Older Adults. The Gerontological Soc America (2016) 71(7):910–5. 10.1093/gerona/glw025
39.
Federico T Lisa HA Martino BM Calderon-Larranaga A Vetrano DL Sjoberg L et al The Complex Interplay between Depression and Multimorbidity in Late Life: Risks and Pathways. Mech Ageing Dev (2020) 192:111383. 10.1016/j.mad.2020.111383
40.
Katon WJ . Epidemiology and Treatment of Depression in Patients with Chronic Medical Illness. Dialogues Clin Neurosci (2011) 2011(13):7–23. 10.31887/DCNS.2011.13.1/wkaton
41.
Jin S Wu Y Chen S Zhao D Guo J Chen L et al The Additional Medical Expenditure Caused by Depressive Symptoms Among Middle-Aged and Elderly Patients with Chronic Lung Diseases in China. Int J Environ Res Public Health (2022) 19(13):7849. 10.3390/ijerph19137849
42.
Yang L Hu Y Silventoinen K Martikainen P . Childhood Adversity and Depressive Symptoms Among Middle-Aged and Older Chinese: Results from China Health and Retirement Longitudinal Study. Aging Ment Health (2020) 24(6):923–31. 10.1080/13607863.2019.1569589
43.
Hong C Xiong X Li J Ning X Qi D Yang Y et al Urbanization and Depressive Symptoms Among Middle-Aged and Older Adults in China. Front Public Health (2022) 10:1086248. 10.3389/fpubh.2022.1086248
44.
Maier A Riedel-Heller SG Pabst A . Risk Factors and Protective Factors of Depression in Older People 65+ A Systematic Review. PLoS One (2021) 16:e0251326. 10.1371/journal.pone.0251326
45.
Zoe Z Elizabeth J Antonio RF Dimitriou D . Good Sleep Quality Improves the Relationship between Pain and Depression Among Individuals with Chronic Pain. Front Psychol (2021) 12:668930. 10.3389/fpsyg.2021.668930
46.
Zhang J Zhang YY Luan ZG Zhang X Jiang H Wang A . A Study on Depression of the Elderly with Different Sleep Quality in Pension Institutions in Northeastern China. BMC Geriatr (2020) 20:374. 10.1186/s12877-020-01777-4
47.
Yu J Rawtaer I Fam J Jiang MJ Feng L Kua EH et al Sleep Correlates of Depression and Anxiety in an Elderly Asian Population. Psychogeriatrics (2016) 16(3):191–5. 10.1111/psyg.12138
48.
Wang R Chen Z Zhou Y Shen L Zhang Z Wu X . Melancholy or Mahjong? Diversity, Frequency, Type, and Rural-Urban divide of Social Participation and Depression in Middle- and Old-Aged Chinese: A Fixed-Effects Analysis. Soc Sci Med (2019) 238:112518. 10.1016/j.socscimed.2019.112518
Summary
Keywords
older adults in China, depressive symptoms, multiple chronic conditions (MCCs), comorbidity, urban and rural areas
Citation
Liu H, Zhou Z, Fan X, Shen C, Ma Y, Sun H and Xu Z (2023) Association Between Multiple Chronic Conditions and Depressive Symptoms Among Older Adults in China: Evidence From the China Health and Retirement Longitudinal Study (CHARLS). Int J Public Health 68:1605572. doi: 10.3389/ijph.2023.1605572
Received
10 November 2022
Accepted
15 February 2023
Published
03 March 2023
Volume
68 - 2023
Edited by
Nino Kuenzli, Swiss School of Public Health (SSPH+), Switzerland
Reviewed by
Dan Cao, Xi’an Jiaotong University, China
Updates
Copyright
© 2023 Liu, Zhou, Fan, Shen, Ma, Sun and Xu.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Haixia Liu, liuhaixia127@163.com
This Original Article is part of the IJPH Special Issue “Health in All Sustainable Development Goals.”
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.