- 1Parasitology and Epidemiology Unit, Department of Animal and Environmental Biology, Federal University Oye-Ekiti, Oye, Nigeria
- 2Clinical Psychology Unit, Department of Psychology, Federal University Oye-Ekiti, Oye, Nigeria
- 3Neglected Tropical Diseases Unit, Ekiti State Primary Healthcare and Development Agency, Ado Ekiti, Nigeria
- 4Mission to Save the Helpless (MITOSATH), Jos, Nigeria
- 5Parasitology and Epidemiology Unit, Department of Pure and Applied Zoology, Federal University of Agriculture, Abeokuta, Abeokuta, Nigeria
- 6Bioscience Research Programme, Institute of Food Security, Environmental Resource and Agricultural Research (IFSERAR), Federal University of Agriculture, Abeokuta, Nigeria
Objective: This study assessed the coverage of albendazole (ALB) in mass drug administration (MDA) programs implemented before (2019) and during the (2020 and 2021) COVID-19 pandemic in Ekiti State, Nigeria.
Methods: Standardized questionnaires were administered to 1,127 children across three peri-urban communities to ascertain if they received and swallowed ALB across the years. Reasons, why ALB was not received, were documented and analyzed in SPSS. 20.0.
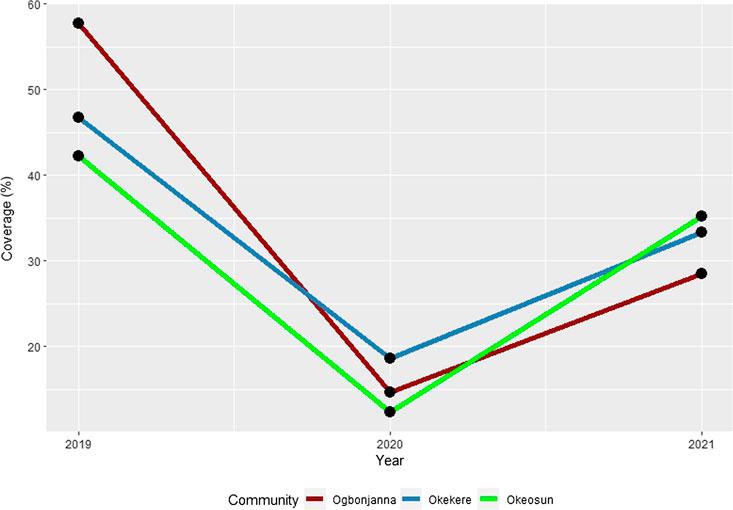
Results: In 2019, the medicine reach was between 42.2%–57.8%, however, during the pandemic, the reach significantly reduced to 12.3%–18.6%, and increased to 28.5%–35.2% in 2021 (p < 0.000). About 19.6%–27.2% of the participants have missed 1 MDA, while 26.9%–37.8% and 22.4%–32.8% have missed 2 and 3 MDAs, respectively. The majority who did not receive ALB (60.8%–75%) claimed drug distributors never came, while about 14.9%–20.3% mentioned they did not hear about MDA. However, individual compliance towards swallowing was above 94% across the study years (p < 0.00).
Conclusion: These results highlight the need to explore the perceptions of those who have consistently missed MDAs, and also understand the health-system-related issues including those imposed by the pandemic affecting MDA.
Introduction
Soil-Transmitted Helminthiasis (STH) is one of the most important neglected tropical diseases (NTDs) in sub-Saharan Africa (SSA) [1]. The global burden of STH is enormous, with over a billion people at risk, about 6300 deaths and 3.5 million disability-adjusted life years (DALYs) [2]. The disease is common in areas where water, sanitation and hygiene resources are limited, with school-aged children (SAC) between ages 5 and 14 years constituting the most vulnerable group, due to their increased mobility, developing immunity and poor hygiene practices [3, 4]. The cornerstone strategy for STH control has been through periodic mass administration of albendazole medicines (MDA) to SAC through teachers or community volunteers in schools and communities, respectively [3].
WHO recommends consistent MDA with albendazole to at least 75% of at-risk populations in endemic countries to achieve elimination [3] and has coordinated the annual distribution of over 400 million albendazoles to treat about 576.4 million children in 2019 [2, 5]. Successful MDA requires community participation and health workers’ commitment [6]. In areas with poor treatment coverage, and where a large segment of SAC is consistently not included or refuses to participate in MDA, a potential parasite reservoir is left untreated, thus risking continued transmission [7–9]. Research targeted at identifying these individuals, and understanding the individual, social, cultural, and health-system factors that interfere with MDA coverage is therefore important. Furthermore, with the advent of the COVID-19 pandemic, there have been severe disruptions in routine public health services [10], with concerns that accompanied shifts in policies such as restriction of movement, closure of schools and delay in MDA during the pandemic might have a negative impact on MDA implementation [11].
Nigeria shares over 25% of the NTDs burden in SSA, including those caused by STH. Since 2014, endemic States in the country have benefitted from the MDA program targeted at STH [12]. However, in 2020, MDA campaigns were temporarily suspended following the lockdown orders instituted by the government across all states in response to the COVID-19 pandemic [13, 14]. In October 2020, lockdown orders were lifted, and MDA resumed following standard operating guidelines stipulated by WHO [10]. MDAs were prioritized in selected states across the country. Ekiti was among the states to resume MDA with support from the state government and a non-governmental organization, Mission to Save The Helpless (MITOSATH). The state is located in the southwestern part of the country and has 16 local government areas (LGAs). Before the pandemic, there were speculations that a large reservoir of children who have consistently missed MDAs exist in some communities in Ikere, one of the peri-urban LGAs in the State. This speculation was reinforced by a recent analysis of MDA programmatic data in the LGA. This study, therefore, evaluated the coverage of albendazole medicines in MDA implemented before and during the pandemic (2019–2021) in Ogbonjanna, Okekere and Okeosun communities. In addition, the study evaluated the proportion of SAC that have consistently missed MDAs and established factors associated with their non-participation or refusals. This study was part of a larger implementation study aimed at understanding the effect of the COVID-19 pandemic on MDA campaigns, to support the design and implementation of context-fitting strategies to strengthen MDA.
Methods
Study Area
Ekiti is one of the rural and NTD endemic states in the southwestern part of Nigeria. The state has 16 LGAs, with its capital located in Ado-Ekiti. The majority of the LGAs are rural (n = 13), followed by peri-urban (n = 2) and urban LGA (n = 1). An estimated population of 2.2 million people live within the state, with an agrarian population mostly in rural communities. Ikere LGA is one of the peri-urban LGAs, with great proximity to the capital city. The MDA program targeted at STH commenced in the LGA in 2015, with a biennial mode of operation.
Study Design, Selection of Communities and Sample Size Estimations
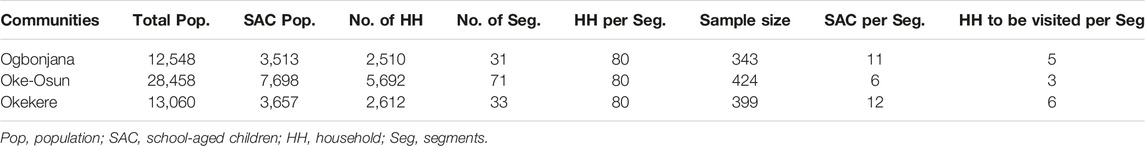
This study employed a cross-sectional sampling design involving questionnaire administration and household visitations across three communities in Ikere LGA i.e., Ogbonjana, Oke-Osun and Okekere. These communities were purposively selected based on their poor MDA coverage in 2019 (<75%). The methodology employed for estimating sample size followed the guidelines provided by WHO for coverage evaluation surveys with some modifications (WHO, 2016). As an initial step, the total population of school-aged children in each community was extracted from the 2022 updated village census register obtained from the NTDs control department. Sample size was calculated using the formula;
Estimation of Household Size, Segments, and Sample Size Per Segment
The WHO coverage evaluation survey guide was adopted in estimating household size and segmenting the communities [15]. In brief, the average number of households in each community was estimated using the formula; Average number of household =
Enumeration of Households and Selection of Study Participants
The survey team, with the help of a local guide visited each segment to identify a common walking path. All households along the identified walk path were enumerated and labelled using colored crayons. Households were marked sequentially, starting from 1 to n, irrespective of the condition of the house. A systematic sampling method was then employed to select households to be recruited in the study. A sampling interval (K) was determined using the formula; K =
Ethical Considerations
This study received ethical approval from Ekiti State Ethical Review Board (MOH/EKHREC/EA/P/33). Permissions and consents were also obtained from the NTD control unit in the state. Prior commencement of household visitation, consent was sought from the community leaders in each of the selected communities. Informed assent was also obtained from all children in addition to another written consent provided by their parent or legal guardian. In cases where the parents or legal guardian were not physically present, verbal consent through telephone were obtained. Unique identifiers and a password protected database were used to protect personal information of the study participant (Supplementary Material S2).
Data Collection and Tools
Data were collected using WHO standardized coverage evaluation survey questionnaire (Supplementary Material S3) designed into electronic forms and administered by a team of 8 research assistants (in a pair of 4). Each pair comprises of an interviewer and an assistant and was accompanied by a local guide during the period of the survey. The standardized questionnaire was used to collect information on demographics, program reach and coverage across the MDAs implemented before the pandemic (2019) and during the pandemic (2020 and 2021). Questions included were 1) if SAC were offered the medicine (program reach), 2) if SAC swallowed the medicine (survey coverage), and 3) reasons why medicines were either not offered and/or swallowed. SAC was shown the samples of the medicine administered to facilitate recall during the interviews. Interviews were also conducted in Yoruba and English languages (as appropriate). However, in areas where the targeted respondents were unavoidably absent, or too young to respond, the household head responded on their behalf.
Data Management and Analysis
Data collected were downloaded from cloud and imported into SPSS 20.0 statistical software (SPSS, United States) for analysis. Descriptive statistics such as frequencies, proportions, means, and standard deviations were used to summarize and present the proportions on background and socio-demographic characteristics of the respondents. Only children between age 5 and 14 across the survey years were considered eligible. As such, data of children below age 8 for year 2019, age 7 for year 2020 and age 6 for year 2021 were excluded from the analysis. Two percentage metrics; the self-reported “survey coverage,” which is the percentage of the eligible population who swallowed the medicine administered, and the “program reach,” which is the percentage of respondents who were offered the drug were estimated. The following formulas were used to calculate the survey coverage and program reach, respectively; Survey coverage =
Results
Demographic Characteristics of Study Participants
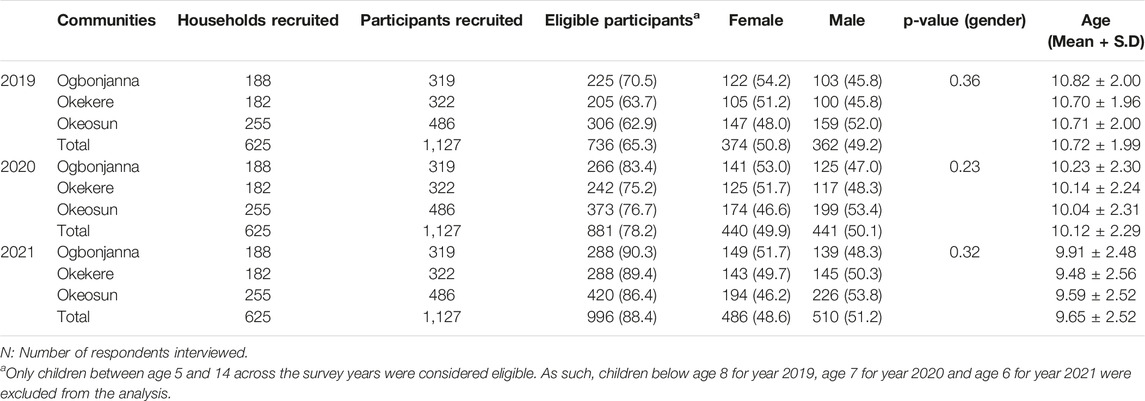
A total of 1,127 school-aged children across 625 households were recruited, with 736 (65.3%) of them being eligible for MDA in 2019, 881 (78.2%) in 2020 and 996 (88.4%) in 2021. The mean age of the respondents ranges from 9.48
Program Reach and Coverage Across the Study Communities (2019–2021)
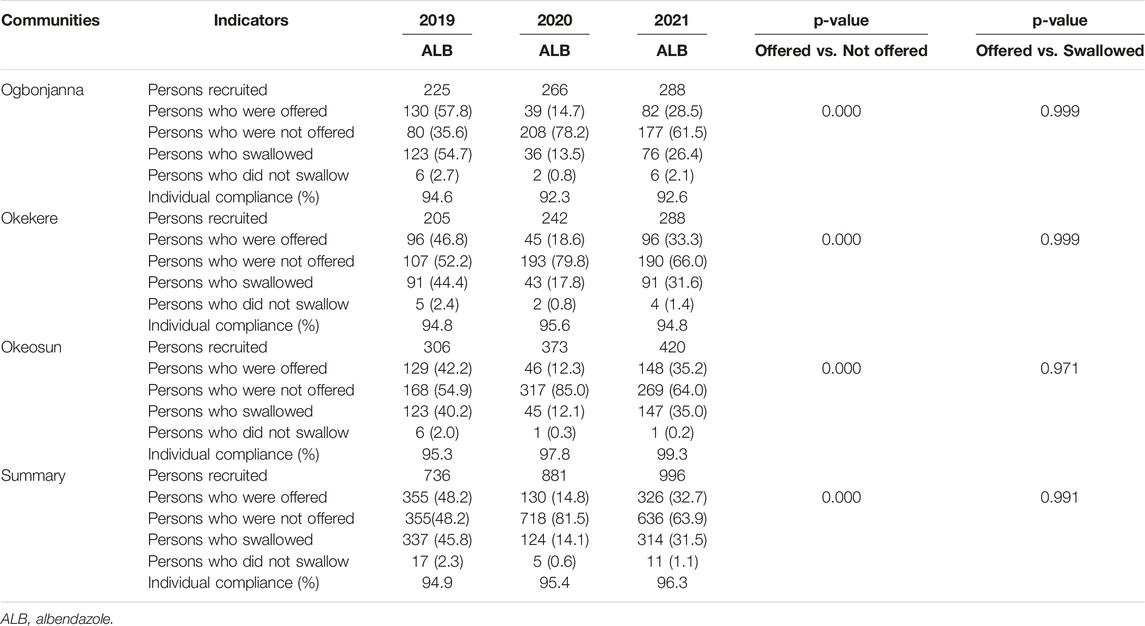
In Ogbonjana, about 57.8% (130/225) of those interviewed in 2019 were offered albendazole medicines, and compliance towards swallowing was 94.6%. However, in 2020, only 14.7% (39/266) were offered, with individual compliance of 92.3%. Furthermore in 2021, only 28.5% (82/288) were offered, with compliance of 92.6%. There were significant differences in the proportions of those offered albendazole across the study years (p = 0.000), with significant decline in 2020. However, there were no significant differences in the proportions of those swallowing albendazole across the study years (p = 0.999) (Table 3; Figure 1).
Similarly, in Okekere, about 46.8% (96/205) of those interviewed in 2019 were offered albendazole medicines, and compliance towards swallowing was 94.8%. However, in 2020, only 18.6% (45/242) were offered, with individual compliance of 95.6%. Furthermore in 2021, only 33.3% (96/288) were offered, with compliance of 94.8%. There were significant differences in the proportions of those offered albendazole across the study years (p = 0.000), with significant decline in 2020. However, there were no significant differences in the proportions of those swallowing albendazole across the study years (p = 0.999) (Table 3; Figure 1).
In Oke-osun, about 42.2% (129/306) of those interviewed in 2019 were offered albendazole medicines, and compliance towards swallowing was 95.3%. However, in 2020, only 12.3% (46/373) were offered, with individual compliance of 97.8%. Furthermore in 2021, only 35.2% (148/420) were offered, with compliance of 99.3%. There were also significant differences in the proportions of those offered albendazole across the study years (p = 0.000), with significant decline in 2020. However, there were no significant differences in the proportions of those swallowing albendazole across the study years (p = 0.971) (Table 3; Figure 1).
Profile of Participants Based on Participation in MDA Programs Across the Study Communities (2019–2021)
About 19.6%–27.2% of the participants have missed 1 MDA, while 26.9%–37.8% and 22.4%–32.8% have missed 2 and 3 MDAs, respectively. By communities, majority of the study participants in Ogbonjana (108, 37.8%) and Okekere (90, 31.9%) had missed 2 MDAs. However, in Oke-osun, majority had missed 3 MDAs (137, 32.9%) (Table 4).
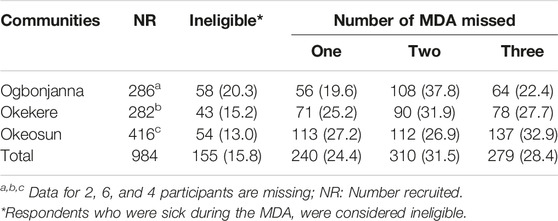
TABLE 4. Profile of participants based on participation in MDA programs across the study communities. Nigeria, 2019–2021.
Reasons Why Albendazoles Were Not Received Across the Study Years (2019–2021)
Of the 355 participants recruited before the pandemic, majority of them (216, 60.8%) mentioned that nobody (drug distributors) came to their house, while others (72, 20.3%) mentioned that they did not hear about MDA. Similarly, during the pandemic, more participants mentioned that nobody (drug distributors) came to their house, 534(74.4%) in 2020 and 477(75.0%) in 2021. However, the proportion of those who did not hear about MDA reduced during the pandemic, 123(17.1%) in 2020 and 95(14.9%) in 2021 (Table 5).
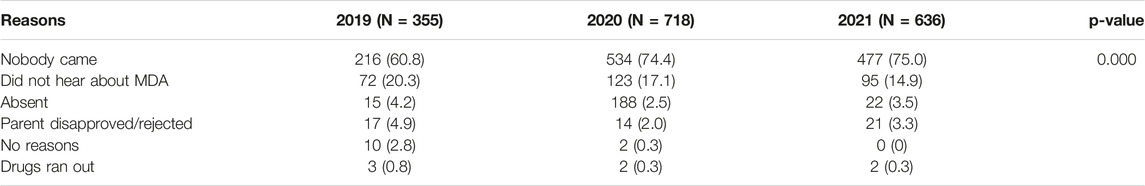
TABLE 5. Reasons why albendazole medicines were not received across the study years. Nigeria, 2019–2021.
Discussion
The advent of COVID-19 pandemic in 2020 disrupted routine public health service including implementation of mass drug administration (MDA) campaigns. In the year of the pandemic (2020–2021), school-based distribution of medicines was disallowed, and MDA for albendazole were implemented using community drug distributors as volunteers. In this study, we evaluated the coverage of albendazole (ALB) medicines in MDA programs implemented before and during the pandemic, as part of a larger study targeted at understanding the effect of pandemic on implementation of MDA programs. Our primary aim was to validate existing speculations that school-aged children have consistently missed MDAs, and secondarily, investigate if there were significant reductions in treatment coverage during the pandemic, and identify factors associated with such reductions. Following WHO recommended guidelines, we measured program reach as the proportion of individual who were offered/received ALB medicines [15], and our findings revealed unsatisfactory rates below the 75% threshold. The program reach was higher in 2019, compared to the pandemic years, and this trend was common across all the study communities. Our findings validated existing speculations as almost half of the eligible children interviewed had missed MDA in the year before the pandemic. The situation worsened during the pandemic with about 82% and 64% of them missing MDAs in 2020 and 2021, respectively. These findings are similar with the coverage report for MDA implemented during the pandemic in Guinea, with reservations that coverage was below what would have been expected under non-pandemic circumstances [16].
The degree of non-participation/compliance in MDA programs, and transmission intensity of parasites are important indicators in elimination programs. Whenever, transmission intensity is high, a consistently high treatment coverage (≥75%) will be required over at least 5 years to move towards transmission elimination [17]. As such, the high non-participation in MDA programs reported in this study is a critical issue that requires attention [7–9]. At the moment, MDA participation patterns are particularly understudied [18], as it is difficult to identify individual non-compliers after MDA programs. There are propositions to implement longitudinal components that document MDA participation patterns in monitoring and evaluation programs [17], however, the feasibility of this idea is yet to be assessed, as MDA programs have funding limitations, and combining a longitudinal component would incur additional costs beyond budget limits [17]. More importantly, such follow-up component would require a more refined data collection and curation methodology, which are currently missing. In addition, successive visits by distributors to administer medicines to those who has repeatedly missed annual treatment, will often be prohibitively time-consuming and hence costly [17]. It is therefore important to leverage on technological innovations incorporated into existing MDA implementation processes, to better document who is treated and when treatment was made, as well as who is not treated, and why treatment was not made.
To this end, our study, retrospectively analyzed data from children in three communities, across three implementation years. Although compliance to swallowing the medicines were high, we however, observed that about one-third of the population had missed 1, 2 and 3 MDAs, respectively. These persons were systematically selected and recruited for follow-up studies, particularly on factors associated with non-participation. Reasons attributed to non-participation were non-visitation of community volunteers, absenteeism of household members during MDA and not having enough information about the medicines. These reasons were frequently reported during the pandemic years and are consistent with other existing reports from India [19], Kenya [20], Ethiopia [21], Liberia [22] and Mali [23]. It is therefore important to reflect on these gaps and identify factors that might contribute to non-visitation of community volunteers and absenteeism of household members especially during the post-COVID lockdown era [11]. For instance, drug shortages, lack of motivation for the volunteers, poor timing of interventions might contribute to inability of drug distributors to visit the households, or even meet household members at home [22, 24]. It is therefore important to further invest efforts in understanding factors associated with non-visitation of community volunteers and absenteeism of household members during MDAs. These findings would be useful in optimizing participation and strengthening MDA delivery [25].
Conclusion
Our findings validate existing speculations that a group of eligible school-aged children had consistently missed MDAs targeted at controlling STH. The program reach was significantly lower during the pandemic compared to the year before the pandemic, with reasons attributed to non-visitation of community volunteers, absenteeism of household members and not having enough information about the medicines. It is therefore important to further explore perceptions of those who have consistently missed MDAs, and also understand how health-system related issues including those imposed by the pandemic have affected MDA.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethical Review Board at the Department of Planning, Research and Statistics, Ekiti State Ministry of Human Resources and Development (MOH/EKHREC/EA/P/33). Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author Contributions
HM conceptualized the study and prepared the protocol, while AM, UE, and FO improved the protocol. NA and AD coordinated field surveys involving data collection. HM, HO, AL, KO, and AM supervised the field surveys. HM performed all statistical analysis and HM prepared the first draft of the manuscript. All authors contributed to the development of the final manuscript and approved its submission.
Funding
This work received financial support from the Coalition for Operational Research on Neglected Tropical Diseases (COR-NTD), which is funded at The Task Force for Global Health primarily by the Bill & Melinda Gates Foundation, by the United States Agency for International Development through its Neglected Tropical Diseases Program, and with UKaid from the British government. The grant was administered by the African Research Network for Neglected Tropical Diseases (ARNTD). This project is registered with the following grant numbers; SGPV/0310.098 under ARNTD, and OPP1190754 under the Bill & Melinda Gates Foundation.
Conflict of Interest
The authors declare that they do not have any conflicts of interest.
Acknowledgments
We are grateful to the community leaders across the study communities, and all the health workers who facilitated the implementation process. We also acknowledge the efforts of Aladejana Abdulrahman, Olaide Rukayat, Oyewole Oluwasogo, Adebayo Boluwatife, Olowo Adejumoke, Ismail Happiness, and Fasakin Temidayo who served as research assistants during data collection process.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/ijph.2023.1605510/full#supplementary-material
References
1. Hotez, PJ, and Kamath, A. Neglected Tropical Diseases in Sub-saharan Africa: Review of Their Prevalence, Distribution, and Disease burden. Plos Negl Trop Dis (2009) 3(8):e412. doi:10.1371/journal.pntd.0000412
2.World Health Organization. Ending the Neglect to Attain the Sustainable Development Goals: A Road Map for Neglected Tropical Diseases 2021–2030. Geneva: World Health Organization (2020). Licence: CC BY-NC-SA 3.0 IGO.
3.World Health Organization. Helminth Control in School-Age Children: a Guide for Managers of Control Programmes (2011). Available from: https://www.who.int/neglected_diseases/resources/9789241548267/en/ (Accessed April 15, 2021).
4.World Health Organization. Soil Transmitted Helminthiasis. Fact Sheet (2022). Available from: https://www.who.int/news-room/fact-sheets/detail/soil-transmitted-helminth-infections (Accessed February 3, 2022).
5. Montresor, A, Mupfasoni, D, Mikhailov, A, Mwinzi, P, Lucianez, A, Jamsheed, M, et al. The Global Progress of Soil-Transmitted Helminthiases Control in 2020 and World Health Organization Targets for 2030. Plos Negl Trop Dis (2020) 4(8):e0008505. doi:10.1371/journal.pntd.0008505
6. Mogaji, HO, Odoh, IM, Iyeh, CI, Adeniran, AA, Oyedeji, SI, Okoh, HI, et al. Attendee's Awareness about Preventive Chemotherapy Neglected Tropical Diseases (PC-NTD) Control during the First World Neglected Tropical Diseases Day in Ekiti State, Nigeria. Plos Negl Trop Dis (2021) 15(3):e0009315. doi:10.1371/journal.pntd.0009315
7. Mathieu, E, Direny, AN, Rochars, MB, de Streit, TG, Addiss, DG, and Lammie, PJ. Participation in Three Consecutive Mass Drug Administrations in Leogane, Haiti. Trop Med Int Health (2006) 11(6):862–8. doi:10.1111/j.1365-3156.2006.01626.x
8. Krentel, A, Fischer, PU, and Weil, GJ. A Review of Factors that Influence Individual Compliance with Mass Drug Administration for Elimination of Lymphatic Filariasis. Plos Negl Trop Dis (2013) 7(11):e2447. doi:10.1371/journal.pntd.0002447
9. El-Setouhy, M, Abd Elaziz, KM, Helmy, H, Farid, HA, Kamal, HA, Ramzy, RM, et al. The Effect of Compliance on the Impact of Mass Drug Administration for Elimination of Lymphatic Filariasis in Egypt. Am J Trop Med Hyg (2007) 77(6):1069–73. doi:10.4269/ajtmh.2007.77.1069
10. Molyneux, D, Bush, S, Bannerman, R, Downs, P, Shu’aibu, J, Boko-Collins, P, et al. Neglected Tropical Diseases Activities in Africa in the COVID-19 Era: the Need for a "hybrid" Approach in COVID-Endemic Times. Infect Dis Poverty (2021) 10(1):1. doi:10.1186/s40249-020-00791-3
11.SightsaversMission to Save the Helpless. Implementing the Mass Treatment Programme for Neglected Tropical Diseases Following the COVID-19 Outbreak in Nigeria: A Mixed-Methods Study on Programme and Community Preparedness to Resume Routine Disease Control Activities in Ekiti, Kaduna and Taraba States. Kaduna, Nigeria: Sightsavers (2021). Available from: https://research.sightsavers.org/project/ntds-nigeria-following-covid-19/ (Accessed January 15, 2021).
12.Federal Ministry of Health (FMOH). Neglected Tropical Diseases: Nigeria Multi-Year Master Plan 2015–2020 (2015). Available from: https://espen.afro.who.int/system/files/content/resources/NIGERIA_NTD_Master_Plan_2015_2020.pdf (Accessed January 15, 2021).
13.National Centre for Disease Control (NCDC). Public Health Advisory on COVID-19 (2020). Available from: https://covid19.ncdc.gov.ng/advisory/ (Accessed February 2, 2021).
14. Warren, L. Community Directed Treatment for Neglected Tropical Diseases in a post COVID-19 Lockdown World (2020). Available from: https://end.org/community-directed-treatment-for-neglected-tropical-diseases-in-a-post-covid-19-lockdown-world/ (Accessed January 15, 2021).
15.World Health Organization. Coverage Evaluation Surveys for Preventive Chemotherapy: Field Guide for Implementation (2016). Available from: https://www.ntdenvision.org/sites/default/files/docs/who_coverage_evaluation_survey_guidance.docx (Accessed January 15, 2021).
16. Sakho, F, Badila, CF, Dembele, B, Diaby, A, Camara, AK, Lamah, L, et al. Implementation of Mass Drug Administration for Neglected Tropical Diseases in Guinea during the COVID-19 Pandemic. Plos Negl Trop Dis (2021) 15(9):e0009807. doi:10.1371/journal.pntd.0009807
17. Farrell, SH, Truscott, JE, and Anderson, RM. The Importance of Patient Compliance in Repeated Rounds of Mass Drug Administration (MDA) for the Elimination of Intestinal Helminth Transmission. Parasit Vectors (2017) 10:291. doi:10.1186/s13071-017-2206-5
18. Shuford, KV, Turner, HC, and Anderson, RM. Compliance with Anthelmintic Treatment in the Neglected Tropical Diseases Control Programmes: a Systematic Review. Parasit Vectors (2016) 9:29. doi:10.1186/s13071-016-1311-1
19. Nandha, B, Sadanandane, C, Jambulingam, P, and Das, P. Delivery Strategy of Mass Annual Single Dose DEC Administration to Eliminate Lymphatic Filariasis in the Urban Areas of Pondicherry, South India: 5 Years of Experience. Filaria J (2007) 6:7. doi:10.1186/1475-2883-6-7
20. Musuva, RM, Matey, E, Masaku, J, Odhiambo, G, Mwende, F, Thuita, I, et al. Lessons from Implementing Mass Drug Administration for Soil Transmitted Helminths Among Pre-school Aged Children during School-Based Deworming Program at the Kenyan Coast. BMC Public Health (2017) 17:575. doi:10.1186/s12889-017-4481-7
21. Asfaw, MA, Zerdo, Z, Churko, C, Seife, F, Yihune, M, Chisha, Y, et al. Preventive Chemotherapy Coverage against Soil-Transmitted Helminth Infection Among School Age Children: Implications from Coverage Validation Survey in Ethiopia, 2019. PloS one (2020) 15(6):e0235281. doi:10.1371/journal.pone.0235281
22. Agboraw, E, Sosu, F, Dean, L, Siakeh, A, Thomson, R, Kollie, K, et al. Factors Influencing Mass Drug Administration Adherence and Community Drug Distributor Opportunity Costs in Liberia: a Mixed-Methods Approach. Parasit Vectors (2021) 14:557. doi:10.1186/s13071-021-05058-w
23. Sangare, M, Berthe, A, Dolo, H, Diabaté, AF, Konipo, FDN, Soumaoro, L, et al. Evaluation of Mass Drug Administration for Schistosomiasis and Soil-Transmitted Helminths in School-Aged Children in Bankass, Mali. Int J Infect Dis (2021) 112:196–201. doi:10.1016/j.ijid.2021.08.063
24. Tuhebwe, D, Bagonza, J, Kiracho, EE, Yeka, A, Elliott, AM, and Nuwaha, F. Uptake of Mass Drug Administration Programme for Schistosomiasis Control in Koome Islands, Central Uganda. PLoS One (2015) 10(4):e0123673. doi:10.1371/journal.pone.0123673
25. Liyew, EF, Chernet, M, Belay, H, Maddren, R, Landeryou, T, Kalahasti, S, et al. Coverage Evaluation Surveys Following Soil-Transmitted Helminthiasis and Schistosomiasis Mass Drug Administration in Wolaita Zone of Ethiopia—The Geshiyaro Project. PLoS One (2021) 16(12):e0260722. doi:10.1371/journal.pone.0260722
Keywords: COVID-19, Nigeria, soil-transmitted helminthiasis, albendazole, mass drug administration
Citation: Mogaji HO, Okoh HI, Lawal AM, Ojo KH, Marcus AJ, Aaron NO, Adeleye DR, Olamiju FO and Ekpo UF (2023) A Post-Lockdown Assessment of Albendazole Treatment Coverage in Mass Drug Administration Campaigns Implemented Before and During COVID-19 Pandemic in Ekiti, Southwest Nigeria. Int J Public Health 68:1605510. doi: 10.3389/ijph.2023.1605510
Received: 20 October 2022; Accepted: 26 January 2023;
Published: 09 February 2023.
Edited by:
Jean Tenena Coulibaly, Félix Houphouët-Boigny University, Côte d'IvoireReviewed by:
Rufin Kouassi Assare, Félix Houphouët-Boigny University, Côte d'IvoireTah Yves-Nathan Tian Bi, Félix Houphouët-Boigny University, Côte d'Ivoire
Clémence Esse, Félix Houphouët-Boigny University, Côte d'Ivoire
Copyright © 2023 Mogaji, Okoh, Lawal, Ojo, Marcus, Aaron, Adeleye, Olamiju and Ekpo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hammed O. Mogaji, bW9nYWppaGFtbWVkQGdtYWlsLmNvbQ==
This Original Article is part of the IJPH Special Issue “Neglected Tropical Diseases During the COVID-19 Pandemic”
 Hammed O. Mogaji
Hammed O. Mogaji Hilary I. Okoh
Hilary I. Okoh Abiodun M. Lawal2
Abiodun M. Lawal2 Nwana O. Aaron
Nwana O. Aaron Uwem F. Ekpo
Uwem F. Ekpo