- 1Department of Outpatient, Felege Meles Health Center, Addis Ababa, Ethiopia
- 2Department of Public Health, Unity University, Addis Ababa, Ethiopia
Objective: This study aimed to assess the dietary diversity and its associated factors among pregnant women in Addis Ababa, Ethiopia, 2021.
Methods: An institution-based Cross-sectional was conducted among 320 participants from four health facilities in Addis Ababa selected based on a simple random sampling method from 01 September to 30 December 2021. An Interviewer-administered structured questionnaire was used, following informed consent. Binary (Bivariate and multivariate) logistics regression was applied for the identification factors associated with dietary diversity with their respective 95% confidence interval and less than 5% p-value.
Results: The prevalence of inadequate dietary diversity during pregnancy was 51.6% (95% CI: 46.1%–57.0%). Being illiterate (AOR: 0.591; 95% CI: 1.88–1.901; p < 0.05) and primary education (AOR: 0.347; 95% CI: 0.166–0.728; p < 0.05), having poor knowledge (AOR: 0.437; 95% CI: 0.252–0.757; p < 0.05) and lower monthly income (AOR: 0.395; 95% CI: 0.184–0.845; p < 0.05) were factors associated with inadequate dietary diversity.
Conclusion: A higher level of inadequate dietary diversity was reported. Being illiterate, having primary education, having poor knowledge, and having lower monthly income were associated with inadequate dietary diversity during pregnancy. Concerned bodies were suggested to work on the identified factors.
Introduction
A healthy diet is essential throughout one’s life, but especially during pregnancy. Pregnant women are nutritionally vulnerable due to their increased nutrient demand. Consumption of a variety of dietary sources is important for ensuring optimal maternal and child nutrition, as it prevents nutritional deficiencies and negative consequences [1, 2].
Dietary diversity is about taking varieties of food item and reflected as a proxy measure of micronutrient adequacy [1, 3]. Evidence suggests that dietary diversity promotes nutrient adequacy in women and lowers the risk of a negative birth outcome [4–7]. Dietary diversification is an appealing approach to addressing nutrient deficiency [1].
Micronutrient deficiency remains a major public health concern in low to middle-income countries commonly in reproductive-age women. [1–5], Thus pregnancy augments an additional burden of nutritional requirements for the women and fetus [6–8].
Malnutrition during pregnancy has a long-lasting effect on the physiological development of the fetus through increasing the risk of low birth weight, maternal morbidity and mortality, preterm delivery, and intrauterine growth retardation [9–12].
Optimal nutrient intake during pregnancy reduces the risk of preterm baby, low birth weight, infant mortality, and small for gestational age [13–15]. Moreover, in women who are underweight during their pregnancy supplementation of multiple micronutrients before 20 weeks of gestation reduces the risk of a preterm baby [16–18].
Understanding the enormous benefits of a healthy diet and adequate micronutrient supplementation during pregnancy [19, 20], dietary diversity is one of the best-recommended strategies for the improvement of dietary adequacy and increased food groups in their daily consumption [21]. Thus, dietary diversity refers to the number of different groups of food consumed over some time [22, 23].
Though evidence suggests that the prevalence of nutritional deficiency during pregnancy was higher in Africa [24–26], including Ethiopia, dietary diversification is an essential tool to reduce nutritional deficiencies [27].
To the best of the researcher’s knowledge, the level of dietary diversity and its associated factors during pregnancy was not well investigated in the study settings. Therefore; this study would hopefully fill the existing gap in the literature.
Methods
Participants and Study Design
The institutional-based cross-sectional study design was conducted among 320 participants from the selected health facilities at Addis Ketema Sub-City of Addis Ababa from 01 September to 30 December 2021. The study received Ethical approval from Santé Medical College; a research review ethics committee and applied to the respective Health Facilities. All the participants were provided written informed consent.
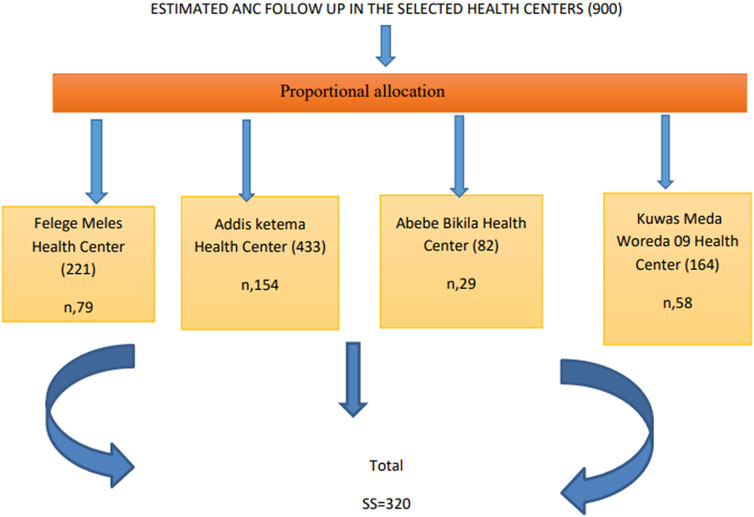
The source population was all pregnant women in Addis Ketema Sub-City, whereas the study population was pregnant women having had ANC follow-up at the selected health facilities; namely; Addis Ketema, Abebe Bikila, Kuwas Meda, and Felege Meles health centers, during the study period. Pregnant women who were available, willing, and free from any severe medical conditions were included in the study. The researcher selected the health facilities by simple random sampling method, after list of all health facilities was determined from the sub city likewise simple random sampling techniques was employed for the selection of the study participants ones their lists were identified from their medical records at respective facilities. Proportional allocation was made based on the health centers monthly follow-up (Figure 1).
The sample size was determined based on a single population proportion, with the premise that the magnitude of dietary diversity from Shashemene was 25.4% [28], 95% confidence interval of 1.96, and a 5% margin of error. The final sample was 320 inclusive of a 10% non-response rate.
Data were gathered with a pre-tested interviewer-administered questionnaire. The questionnaire was developed by reviewing related pieces of literature [29–32] and then given for two senior researchers working in academic institutions and their inputs were incorporated into the final tool.
Definitions of Concepts
The outcome variable (Dietary diversity) was measured as adquate and inadequate. A minimum dietary diversity score (MDD-W) was used to calculate the sum of the number of different food groups consumed by the pregnant women in the 24 Hours before the assessment. The MDD-W indicator was based on the 10-food group’s women’s dietary diversity score (MDDW-10). These food groups are starch staples (grains, white roots and tubers, and plantains); vitamin A-rich vegetables and fruits; dark green leafy vegetables; other vegetables; other fruits; flesh foods (meat, fish, poultry, and liver/organ meats); eggs; pulses/legumes; nuts and seeds; and dairy products. MDD-W is based on a 24-h dietary recall period [33]. The women were asked to recall all foods consumed from the above food groups on the previous day. Responses were recorded as “yes” or “no.”A “yes” response was scored as “1,” and a “no” response was scored as ‘0’. The scores summed up to yield the women’s MDD-W score. The dietary diversity scores were then classified as inadequate and adequate dietary diversity based on the MDD-W. Women having a diversity score of less than 5 were classified as having low dietary diversity and scores of 5–10 are classified as the high/good dietary diversity scores [34]. Knowledge was measured as true and false questions and categorized as poor versus good knowledge based on median score after constructs forming knowledge were once computed.
Statistical Analysis
Descriptive statistics were used for the summarization of data. For the identification factors associated with dietary diversity, binary (Bi-variable and multivariable) logistics regression was used, with their respective 95% Confidence Interval (CI) and p-value of less than 0.05 as a statistically significant level.
Results
Socio Demographic Characteristics
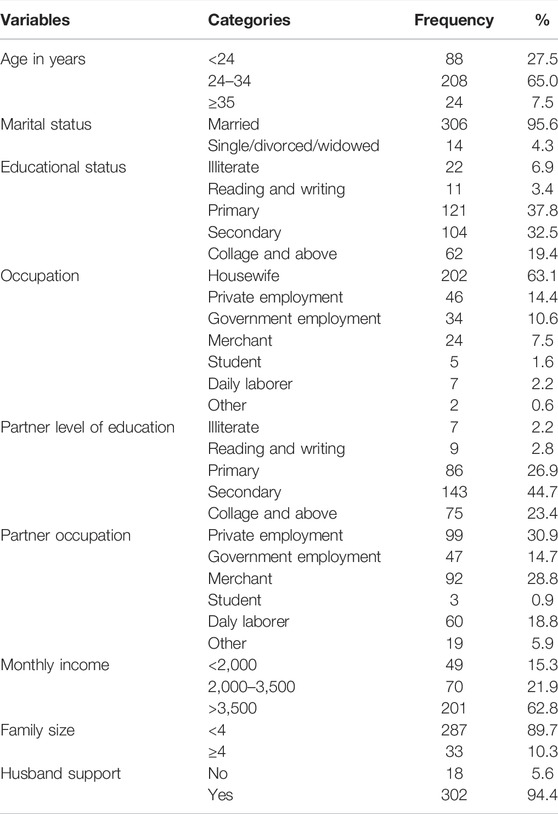
A total of 320 pregnant women participated in this study making a response rate of 100%. The mean age of study participants was 26.98 with a standard deviation of 4.468. The majority (95%) of the participants were married and more than one-third (37.8%) of their husbands attended primary school. Regarding occupation, most (63.1%) of the study participants were housewives. Almost all (94.4%) of the participants got support from their husband (Table 1).
Maternal Characteristics
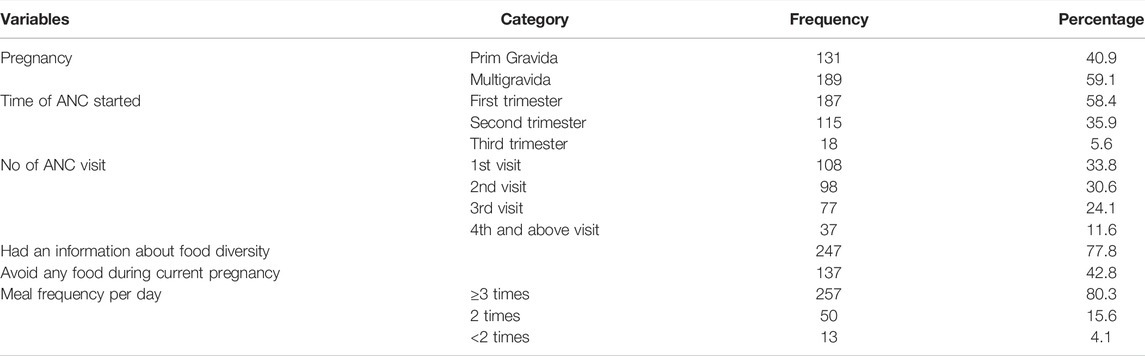
Most (59.1%) and (58.4%) were multigravidas and started ANC in their first trimester of pregnancy respectively. About three-fourths (77.8%) of the study participants had information about the importance of dietary diversity during pregnancy whereas less than half (42.8%) of respondents had avoided some kind of food during pregnancy. Most (80.3%) of respondents had a meal frequency of three and above per day (Table 2).
Pregnant Women Knowledge of Dietary Diversity
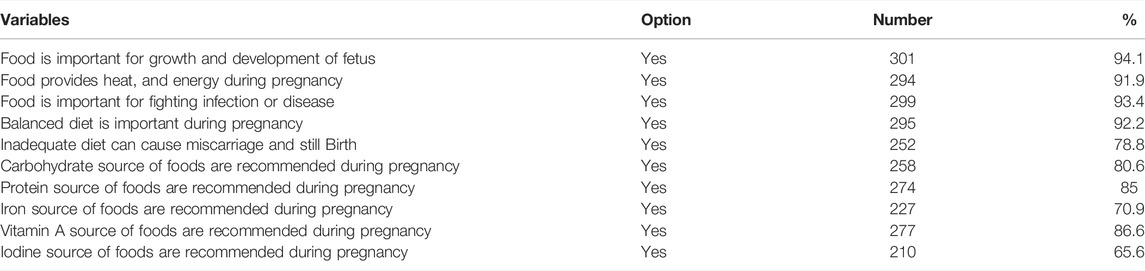
The proportion of women having had a good dietary diversity knowledge during pregnancy was 69.1% (95% CI: 63.7%–74.1%). A large majority of pregnant women (94.1%) knew the importance of food for the growth and development of the fetus during pregnancy, and (93.4%) perceived food is important for fighting infection. More than three fourth (78.8%) of the study participants reported that inadequate diet can cause miscarriage and stillbirth (Table 3).
Prevalence of Inadequate Dietary Diversity
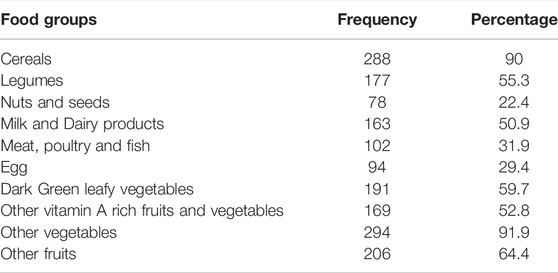
The prevalence of inadequate dietary diversity during pregnancy was 51.6% (95% CI: 46.1%–57.0%). Most (90%) of the study participants reported that they consumed cereal-based crops (maize, sorghum, millet, wheat, barley, and teff) before the survey. Dark green leafy vegetables (kale, swiss chard, and green pepper) and legumes were consumed by 59.7% and 55.3% of the subjects respectively 1 day before the survey. More than half (52.8%) of the study participants reported that they consumed other vitamins A-rich vegetables (pumpkin, carrot, and orange-fleshed sweet potato). Among animal products, milk and milk products were consumed by (50.9%) of the study group whereas meat, poultry, fish, and egg were consumed by 31.9% and 29.4%, respectively (Table 4).
Factors Associated With Dietary Diversity Practice
The bivariate logistics regression identified the age of the mother, educational status, knowledge, attitude, and monthly incomes to be the candidate variables for the multivariate logistics regression at a p-value of <0.25. The multivariable logistics regression identified maternal educational status, knowledge and monthly income were factors statistically associated with dietary diversity of the mother.
The odds of having had inadequate dietary diversity was higher by 40.9% among illiterates compared to those of college and above (AOR: 0.591; 95% CI: 1.88–1.901; p < 0.05). The odds of having inadequate dietary diversity was higher by 65.3% among mothers who had completed primary schooling compared to those of college and above (AOR: 0.347; 95% CI: 0.166–0.728; p < 0.05).
The odds of having inadequate dietary diversity was higher by 56.3% among mothers who had poor knowledge compared to good knowledge (AOR: 0.437; 95% CI: 0.252–0.757; p < 0.05). The odds of having inadequate dietary diversity was higher by 65.5% among mothers who had monthly income <2000 compared to >3500monthly income (AOR: 0.395; 95% CI: 0.184–0.845; p < 0.05) (Table 5).
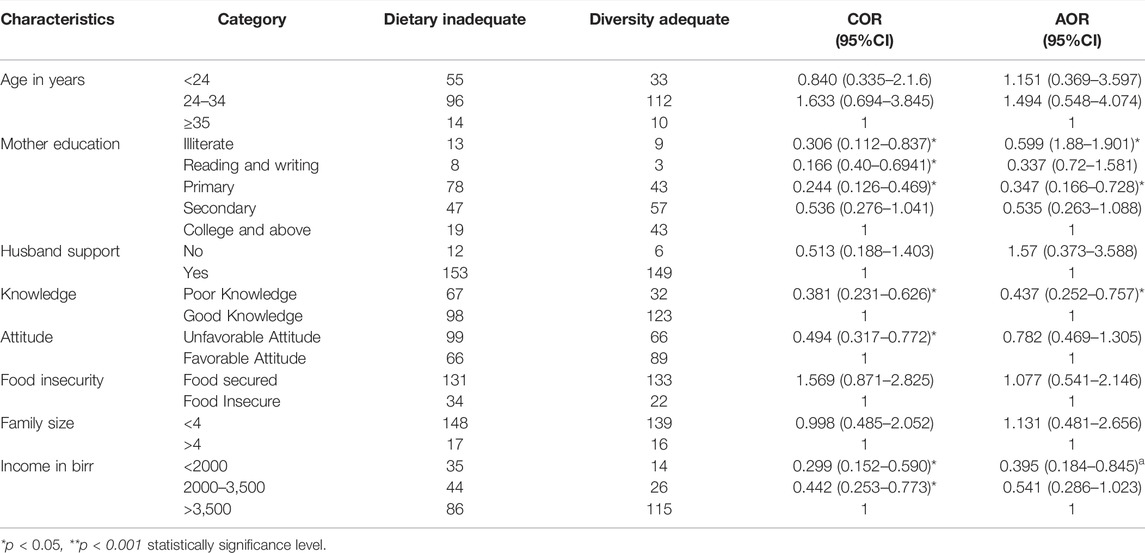
TABLE 5. Factors affecting dietary diversity of the study participants (Addis Ababa, Ethiopia, 2021).
Discussion
In this study, the prevalence of inadequate dietary diversity practice during pregnancy was 51.6%, which was in agreement with 57.4% in Southern Ethiopia [35] and 57% in Dire Dewa, Eastern Ethiopia [36]. A study from the United States reported that 46% of pregnant women had inadequate dietary practice [37], this was also consistent with current findings.
Studies from Gondar; Northwest of Ethiopia reported that about 60% of pregnant women had inadequate dietary diversity [38]. Another study from Shashemene, South Western Ethiopia also reported a dietary diversity practice of 74.6% [28]. In these cases, a lower proportion was reported. The observed difference might be due to differences in sample size and time of the investigation across the studies.
Much lower dietary diversity scores were reported by studies 19.6% in Kenya [6]and 19.9% in Gojjam, Northwest Ethiopia [39]. The dietary diversity practice in this study was much higher than in those studies. Such variations might be associated with differences in time of investigation and population.
A study from Malaysia [40] reported a much higher 74% dietary practice than the current study reported. Such variations might be due to differences in population demographics and access to various dietary sources across the population.
In this study, maternal education was statistically associated with dietary diversity, which was supported by the studies from Ghana [41], Kenya [7], Tanzania [42], and Ethiopia [28]. People that are more educated had good dietary diversity compared to those of uneducated in that the more they had an exposure to different nutritional knowledge and information, the higher they tend to use it.
The other factor statistically associated with dietary diversity was maternal knowledge about dietary diversity during pregnancy. Knowledge can affect positively or negatively the practice, through shaping the attitude of people. This was evidently observed in this study that mothers who had poor dietary diversity knowledge had inadequate dietary diversity, which thus was supported by the studies from Malawi [43], and Ethiopia [29].
Additionally, the other factor statistically associated with dietary diversity was monthly income. Those pregnant women who had higher monthly income were more likely to have had adequate dietary diversity compared to their counterparts. This was supported by the studies from Iran [44] and Kenya [7]. This study has the following limitations; The 24 h dietary might not indicate the usual dietary diversity of the pregnant women as the cross sectional nature of the study. The study might have recall and social desirability bias. Moreover, the study used a lower proportion to compute the sample size.
Conclusion
A higher prevalence of inadequate dietary diversity practice during pregnancy was observed in the study settings. Educational status, knowledge, and monthly income were factors identified to affect the dietary diversity during pregnancy. Being illiterate, primary education, poor dietary knowledge, and lower monthly incomes were associated with inadequate dietary diversity during pregnancy in the study settings.
Data Availability Statement
A finding of this study was generated from the data collected and analyzed on the basis of stated methods and materials hence all data were already available in the article.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethics and review board of Sante Medical College. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors thank study participants for their willingness in taking part in the study.
Abbreviations
AOR, Adjusted Odds Ratio; COR, Crude Odds Ratio; DDS, Dietary Diversity Score; WHO, World Health Organization
References
1. Darnton-Hill, I, and Mkparu, UC. Micronutrients in Pregnancy in Low-And Middle-Income Countries. Nutrients (2015) 7(3):1744–68. doi:10.3390/nu7031744
2. Pasricha, S-R, Drakesmith, H, Black, J, Hipgrave, D, and Biggs, B-A. Control of Iron Deficiency Anemia in Low-And Middle-Income Countries. Blood (2013) 121(14):2607–17. doi:10.1182/blood-2012-09-453522
3. Victora, CG, Christian, P, Vidaletti, LP, Gatica-Domínguez, G, Menon, P, and Black, RE. Revisiting Maternal and Child Undernutrition in Low-Income and Middle-Income Countries: Variable Progress towards an Unfinished Agenda. Lancet (2021) 397(10282):1388–99. doi:10.1016/S0140-6736(21)00394-9
4. Gernand, AD, Schulze, KJ, Stewart, CP, West, KP, and Christian, P. Micronutrient Deficiencies in Pregnancy Worldwide: Health Effects and Prevention. Nat Rev Endocrinol (2016) 12(5):274–89. doi:10.1038/nrendo.2016.37
5. Chaparro, CM, and Suchdev, PS. Anemia Epidemiology, Pathophysiology, and Etiology in Low‐and Middle‐income Countries. Ann N Y Acad Sci (2019) 1450(1):15–31. doi:10.1111/nyas.14092
6. Kiboi, W, Kimiywe, J, and Chege, P. Dietary Diversity, Nutrient Intake and Nutritional Status Among Pregnant Women in Laikipia County, Kenya. Int J Health Sci Res (2016) 6:378–9.
7. Kiboi, W, Kimiywe, J, and Chege, P. Determinants of Dietary Diversity Among Pregnant Women in Laikipia County, Kenya: a Cross-Sectional Study. BMC Nutr (2017) 3(1):12–8. doi:10.1186/s40795-017-0126-6
8. Kemunto, ML. Dietary Diversity and Nutritional Status of Pregnant Women Aged 15-49 Years Attending Kapenguria District Hospital West Pokot County. Nairobi, Kenya: Kenya kenayatta University Institutional Repository (2013).
9. Muthayya, S. Maternal Nutrition & Low Birth Weight-What Is Really Important. Indian J Med Res (2009) 130(5):600–8.
10. Grote, NK, Bridge, JA, Gavin, AR, Melville, JL, Iyengar, S, and Katon, WJ. A Meta-Analysis of Depression during Pregnancy and the Risk of Preterm Birth, Low Birth Weight, and Intrauterine Growth Restriction. Arch Gen Psychiatry (2010) 67(10):1012–24. doi:10.1001/archgenpsychiatry.2010.111
11. King, JC. The Risk of Maternal Nutritional Depletion and Poor Outcomes Increases in Early or Closely Spaced Pregnancies. J Nutr (2003) 133(5):1732S–1736S. doi:10.1093/jn/133.5.1732S
12. Suhag, A, and Berghella, V. Intrauterine Growth Restriction (IUGR): Etiology and Diagnosis. Curr Obstet Gynecol Rep (2013) 2(2):102–11. doi:10.1007/s13669-013-0041-z
13. Tudehope, D, Vento, M, Bhutta, Z, and Pachi, P. Nutritional Requirements and Feeding Recommendations for Small for Gestational Age Infants. J Pediatr (2013) 162(3):S81–S9. doi:10.1016/j.jpeds.2012.11.057
14. De Jesus, LC, Pappas, A, Shankaran, S, Li, L, Das, A, Bell, EF, et al. Outcomes of Small for Gestational Age Infants Born at <27 Weeks' Gestation. J Pediatr (2013) 163(1):55–60. e3. doi:10.1016/j.jpeds.2012.12.097
15. Ehrenkranz, RA. Nutrition, Growth and Clinical Outcomes. World Rev Nutr Diet (2014) 110:11–26. doi:10.1159/000358455
16. Abu-Saad, K, and Fraser, D. Maternal Nutrition and Birth Outcomes. Epidemiol Rev (2010) 32(1):5–25. doi:10.1093/epirev/mxq001
17. Ramakrishnan, U, Grant, F, Goldenberg, T, Zongrone, A, and Martorell, R. Effect of Women's Nutrition before and during Early Pregnancy on Maternal and Infant Outcomes: a Systematic Review. Paediatr Perinat Epidemiol (2012) 26:285–301. doi:10.1111/j.1365-3016.2012.01281.x
18. Wu, G, Imhoff‐Kunsch, B, and Girard, AW. Biological Mechanisms for Nutritional Regulation of Maternal Health and Fetal Development. Paediatr Perinat Epidemiol (2012) 26:4–26. doi:10.1111/j.1365-3016.2012.01291.x
19. Jolivet, RR, Moran, AC, O’Connor, M, Chou, D, Bhardwaj, N, Newby, H, et al. Ending Preventable Maternal Mortality: Phase II of a Multi-step Process to Develop a Monitoring Framework. BMC Pregnancy Childbirth (2016–20302018) 18(1):258–13. doi:10.1186/s12884-018-1763-8
20.WHO. Strategies towards Ending Preventable Maternal Mortality (EPMM). Geneva, Switzerland: World Health Organization (2015).
21. Kennedy, GL, Pedro, MR, Seghieri, C, Nantel, G, and Brouwer, I. Dietary Diversity Score Is a Useful Indicator of Micronutrient Intake in Non-breast-feeding Filipino Children. J Nutr (2007) 137(2):472–7. doi:10.1093/jn/137.2.472
22. Chakona, G, and Shackleton, C. Minimum Dietary Diversity Scores for Women Indicate Micronutrient Adequacy and Food Insecurity Status in South African Towns. Nutrients (2017) 9(8):812. doi:10.3390/nu9080812
23. Kennedy, G, Fanou-Fogny, N, Seghieri, C, and Brouwer, ID. Dietary Diversity as a Measure of the Micronutrient Adequacy of Women's Diets: Results from Bamako, Mali Site (2009).
24. Lartey, A. Maternal and Child Nutrition in Sub-saharan Africa: Challenges and Interventions. Proc Nutr Soc (2008) 67(1):105–8. doi:10.1017/S0029665108006083
25. Baumgartner, J. Antenatal Multiple Micronutrient Supplementation: Benefits beyond Iron-Folic Acid Alone. Lancet Glob Health (2017) 5(11):e1050–1. doi:10.1016/S2214-109X(17)30389-3
26. Persson, LÅ. Prenatal Nutrition, Socioenvironmental Conditions, and Child Development. Lancet Glob Health (2017) 5(2):e127–8. doi:10.1016/S2214-109X(16)30356-4
27. Weerasekara, PC, Withanachchi, CR, Ginigaddara, G, and Ploeger, A. Understanding Dietary Diversity, Dietary Practices and Changes in Food Patterns in Marginalised Societies in Sri Lanka. Foods (2020) 9(11):1659. doi:10.3390/foods9111659
28. Desta, M, Akibu, M, Tadese, M, and Tesfaye, M. Dietary Diversity and Associated Factors Among Pregnant Women Attending Antenatal Clinic in Shashemane, Oromia, Central Ethiopia: a Cross-Sectional Study. J Nutr Metab (2019) 2019:3916864. doi:10.1155/2019/3916864
29. Zerfu, TA, and Biadgilign, S. Pregnant Mothers Have Limited Knowledge and Poor Dietary Diversity Practices, but Favorable Attitude towards Nutritional Recommendations in Rural Ethiopia: Evidence from Community-Based Study. BMC Nutr (2018) 4(1):43–9. doi:10.1186/s40795-018-0251-x
30. Yeneabat, T, Adugna, H, Asmamaw, T, Wubetu, M, Admas, M, Hailu, G, et al. Maternal Dietary Diversity and Micronutrient Adequacy during Pregnancy and Related Factors in East Gojjam Zone, Northwest Ethiopia, 2016. BMC Pregnancy Childbirth (2019) 19(1):173–9. doi:10.1186/s12884-019-2299-2
31. Weldehaweria, NB, Misgina, KH, Weldu, MG, Gebregiorgis, YS, Gebrezgi, BH, Zewdie, SW, et al. Dietary Diversity and Related Factors Among Lactating Women Visiting Public Health Facilities in Aksum Town, Tigray, Northern Ethiopia. BMC Nutr (2016) 2(1):38–9. doi:10.1186/s40795-016-0077-3
32. Fite, MB, Tura, AK, Yadeta, TA, Oljira, L, and Roba, KT. Prevalence and Determinants of Dietary Practices Among Pregnant Women in Eastern Ethiopia. BMC Nutr (2022) 8(1):3–10. doi:10.1186/s40795-021-00494-4
33. Idf, DAG. Update of Mortality Attributable to Diabetes for the IDF Diabetes Atlas: Estimates for the Year 2013. Diabetes Res Clin Pract (2015) 109(3):461–5. doi:10.1016/j.diabres.2015.05.037
34. Saaka, M, Mutaru, S, and Osman, SM. Determinants of Dietary Diversity and its Relationship with the Nutritional Status of Pregnant Women. J Nutr Sci (2021) 10:e14. doi:10.1017/jns.2021.6
35. Delil, R, Zinab, B, Mosa, H, Ahmed, R, and Hassen, H. Determinants of Dietary Diversity Practice Among Pregnant Women Attending Antenatal Clinic at Wachemo University Nigist Eleni Mohammed Memorial Referral Hospital, Southern Ethiopia. PloS one (2021) 16(4):e0250037. doi:10.1371/journal.pone.0250037
36. Shenka, A, Damena, M, Abdo, M, and Roba, KT. Dietary Diversity and Nutritional Status of Pregnant Women Attending Public Hospitals in Dire Dawa City Administration, Eastern Ethiopia. East Afr J Health Biomed Sci (2018) 2(1):10–7.
38. Alemayehu, MS, and Tesema, EM. Dietary Practice and Associated Factors Among Pregnant Women in Gondar Town north West, Ethiopia, 2014. Int J Nutr Food Sci (2015) 4(6):707–12. doi:10.11648/j.ijnfs.20150406.27
39. Demilew, YM, Alene, GD, and Belachew, T. Dietary Practices and Associated Factors Among Pregnant Women in West Gojjam Zone, Northwest Ethiopia. BMC Pregnancy Childbirth (2020) 20(1):18–1. doi:10.1186/s12884-019-2702-z
40. Mirsanjari, M, Muda, W, Ahmad, A, Othman, MS, and Mosavat, M. Does Nutritional Knowledge Have Relationship with Healthy Dietary Attitude and Practices during Pregnancy. ICNFS (2012) 39:159–63.
41. Amugsi, DA, Lartey, A, Kimani-Murage, E, and Mberu, BU. Women’s Participation in Household Decision-Making and Higher Dietary Diversity: Findings from Nationally Representative Data from Ghana. J Health Popul Nutr (2016) 35(1):16–8. doi:10.1186/s41043-016-0053-1
42. Ochieng, J, Afari-Sefa, V, Lukumay, PJ, and Dubois, T. Determinants of Dietary Diversity and the Potential Role of Men in Improving Household Nutrition in Tanzania. PloS one (2017) 12(12):e0189022. doi:10.1371/journal.pone.0189022
43. Katenga-Kaunda, LZ, Kamudoni, PR, Holmboe-Ottesen, G, Fjeld, HE, Mdala, I, Shi, Z, et al. Enhancing Nutrition Knowledge and Dietary Diversity Among Rural Pregnant Women in Malawi: a Randomized Controlled Trial. BMC Pregnancy Childbirth (2021) 21(1):644–11. doi:10.1186/s12884-021-04117-5
Keywords: Ethiopia, women, associated factors, dietary practice, Addis Ababa
Citation: Kebede AN, Sahile AT and Kelile BC (2022) Dietary Diversity and Associated Factors Among Pregnant Women in Addis Ababa, Ethiopia, 2021. Int J Public Health 67:1605377. doi: 10.3389/ijph.2022.1605377
Received: 06 September 2022; Accepted: 25 October 2022;
Published: 03 November 2022.
Edited by:
Vittorio Krogh, National Cancer Institute Foundation (IRCCS), ItalyReviewed by:
Teshome Geta, Wolkite University, EthiopiaAnkit Anand, Institute for Social and Economic Change, India
Copyright © 2022 Kebede, Sahile and Kelile. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Addisu Tadesse Sahile, c2FoZGlzOTFAZ21haWwuY29t
 Aynshet Nega Kebede1
Aynshet Nega Kebede1 Addisu Tadesse Sahile
Addisu Tadesse Sahile