- National Center for Chronic and Noncommunicable Disease Control and Prevention, Chinese Center for Disease Control and Prevention, Beijing, China
Cardiovascular disease (CVD), including stroke and acute myocardial infarction (AMI), is a leading cause of death in both urban and rural China (44.26% and 46.74% of total deaths) [1]. However, CVD mortality has been greater in rural than in urban areas in the last 10 years (up to 323.29 vs. 277.92 per 100,000 people) [1]. Reducing mortality from CVD in China therefore probably requires improvements in the chain of CVD care— a new concept (see Figure 1), including prevention, control, and treatment of both risk factors and disease. This chain will guide us to understand urban-rural differences, improve health services, and thereafter reduce CVD mortality in a broad perspective across the whole population, rather than simply hospital-based patients.
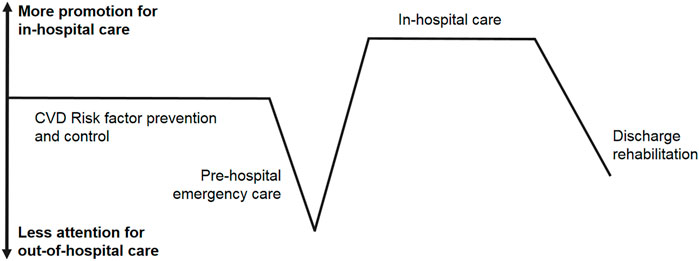
FIGURE 1. Current status of cardiovascular diseases prevention and control in China indicated by a chain of cardiovascular diseases care (Beijing, China. 2022). Note: CVD means cardiovascular diseases.
Hypertension accounts for 72.8% of the disease burden from stroke and 64.5% from other CVDs such as AMI and hypertensive heart disease, and is the most important risk factor for CVD [2]. There is a similar prevalence between urban and rural adult Chinese people (23.4% vs. 23.1%), but rural hypertensive patients have a worse rate of blood pressure control than urban patients (13.1% vs. 19.4%) [3]. This is despite improvements since 2012, when the overall rate in China was just 9.7%. These changes are probably associated with the National Primary Public Health Services (NPPHS) program of China, which was launched in 2009. Under this program, community doctors provide various free primary healthcare services for all registered citizens of China, including hypertension management. To date, the NPPHS has managed 100 million hypertensive patients, and this figure is expected to increase to 110 million by 2025. For most of the rural population, the main treatment for CVD is therefore village doctor-led usual care. A study has suggested that interventions led by village doctors, including both multifaceted interventions and enhanced usual care, result in significant improvements in blood pressure control among rural residents in China [4]. However, in less urbanized areas, drug use is still unsatisfactory in primary healthcare [5].
In the WHO MONICA Project, around 70% of patients with acute coronary heart disease died before reaching hospital. After over 30 years, this is still true in China. Only 18.9% of CVD deaths currently happen in hospital, and this falls to 14.0% in rural China [6]. This may be because of poorer emergency medical services in rural areas. Out-of-hospital cardiac arrest, which has an extremely low survival rate (generally lower than 1%) and contributes to half of heart deaths, keeps challenging the CVD care chain [7]. Ongoing improvements are related to bystander cardiopulmonary resuscitation (CPR), advanced life support provided by emergency medical services, and in-hospital care. Provision of basic life support by non-professional bystanders increases the survival chance of people who have a cardiac arrest outside hospitals. However, CPR training for the public and public provision of automatic external defibrillators are both insufficient.
In-hospital CVD care is generally better than other links of the chain. China has focused on improving in-hospital care quality. Recently, there have been several studies exploring differences in in-hospital mortality from AMI between urban and rural regions [8–10]. One study in particular suggested that the difference could be reduced by percutaneous coronary intervention (PCI) [10], but this is unlikely to be the only relevant factor. Urban and rural areas have different levels of social and economic development. This inevitably leads to divergence in population characteristics, demand for healthcare, provision of specific care, and patients screened by the chain of CVD care. The divergence is also linked to availability and effect of PCI. The urban–rural differences related to in-hospital mortality from AMI reflect all these factors, and not just a single intermediate factor such as PCI, but it remains important to enhance primary healthcare clinics and hospitals, especially in developing rural regions. Additionally, hierarchical analyses exploring the impact of particular factors such as PCI on the association between exposure and disease are indispensable to the development of a complex and conditioned statistical model adjusting for multiple factors.
CVD discharge rehabilitation needs more attention. China currently has 13 million people with stroke and 11 million with coronary heart disease. However, there is little high-quality research evidence to support the development of policies for rehabilitation after stroke and myocardial infarction. In rural regions, these patients may be more dependent on blood pressure and blood sugar management from the NPPHS than those living in cities where there are more medical resources.
In conclusion, out-of-hospital CVD care is the main area that needs attention in this care chain. Out-of-hospital links, including risk factor control, pre-hospital emergency care, and discharge rehabilitation, are much weaker than in-hospital care in the overall chain of CVD care. The difference between rural and urban regions is systemic, and both out-of-hospital and in-hospital care need to be enhanced in rural areas. However, the most cost-effective course of action in both urban and rural areas is undoubtedly to be controlling CVD risk factors such as hypertension, smoking, unhealthy diet, and lacking physical activity.
Author Contributions
LH developed the topic and wrote the article after invitation from Prof. Nino Kuenzli, Editor-in-chief of the IJPH.
Funding
This work was supported by the Science & Technology Fundamental Resources Investigation Program of China (2018FY100602).
Conflict of Interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
I thank Melissa Leffler, MBA, from Liwen Bianji (Edanz) (www.liwenbianji.cn) for editing the English text of a draft of this manuscript.
References
1.National Center for Cardiovascular Diseases, China. Annual Report on Cardiovascular Health and Diseases in China (2021). Beijing: Science Press (2022).
2. Hou, L, Chen, B, Ji, Y, Wang, B, and Wu, J. China CDC in Action—Hypertension Prevention and Control. China CDC Wkly (2020) 2(40):783–6. doi:10.46234/ccdcw2020.212
3. Wang, Z, Chen, Z, Zhang, L, Wang, X, Hao, G, Zhang, Z, et al. Status of Hypertension in China: Results from the China Hypertension Survey, 2012-2015. Circulation (2018) 137(22):2344–56. doi:10.1161/CIRCULATIONAHA.117.032380
4. Sun, Y, Mu, J, Wang, DW, Ouyang, N, Xing, L, Guo, X, et al. A Village Doctor-Led Multifaceted Intervention for Blood Pressure Control in Rural China: an Open, Cluster Randomised Trial. Lancet (2022) 399(10339):1964–75. doi:10.1016/S0140-6736(22)00325-7
5. Hou, L, Chen, X, Chen, B, Liu, L, Sun, X, Zou, Y, et al. Pharmacological Therapy and Blood Pressure Control in Primary Health Care Sites in China: Data from 254, 848 Hypertensive Patients. Clin Epidemiol (2018) 10:1467–78. doi:10.2147/CLEP.S172567
6. Wang, W, Liu, Y, Ye, P, Liu, J, Yin, P, Qi, J, et al. Trends and Associated Factors in Place of Death Among Individuals with Cardiovascular Disease in China, 2008-2020: a Population-Based Study. Lancet Reg Health West Pac (2022) 21:100383. doi:10.1016/j.lanwpc.2022.100383
7. Hou, L, Wang, Y, and Wang, W. Prevention and Control of Cardiac Arrest in Healthy China. China CDC Wkly (2021) 3(14):304–7. doi:10.46234/ccdcw2021.076
8. Zhong, Q, Gao, Y, Zheng, X, Chen, J, Masoudi, FA, Lu, Y, et al. Geographic Variation in Process and Outcomes of Care for Patients with Acute Myocardial Infarction in China from 2001 to 2015. JAMA Netw Open (2020) 3(10):e2021182. doi:10.1001/jamanetworkopen.2020.21182
9. Li, X, Murugiah, K, Li, J, Masoudi, FA, Chan, PS, Hu, S, et al. Urban-Rural Comparisons in Hospital Admission, Treatments, and Outcomes for ST-Segment-Elevation Myocardial Infarction in China from 2001 to 2011: a Retrospective Analysis from the China PEACE Study (Patient-Centered Evaluative Assessment of Cardiac Events). Circ Cardiovasc Qual Outcomes (2017) 10(11):e003905. doi:10.1161/CIRCOUTCOMES.117.003905
10. Cai, M, Liu, E, Bai, P, Zhang, N, Wang, S, Li, W, et al. The Chasm in Percutaneous Coronary Intervention and In-Hospital Mortality Rates Among Acute Myocardial Infarction Patients in Rural and Urban Hospitals in China: a Mediation Analysis. Int J Public Health (2022) 67:1604846. doi:10.3389/ijph.2022.1604846
Keywords: cardiovascular disease, chain, out-of-hospital, hypertension, cardiac arrest
Citation: Hou L (2022) A Call to Improve a Chain of Cardiovascular Disease Care. Int J Public Health 67:1605219. doi: 10.3389/ijph.2022.1605219
Received: 14 July 2022; Accepted: 21 July 2022;
Published: 24 August 2022.
Edited by:
Nino Kuenzli, Swiss Tropical and Public Health Institute (Swiss TPH), SwitzerlandCopyright © 2022 Hou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lei Hou, aG91bGVpQG5jbmNkLmNoaW5hY2RjLmNu
 Lei Hou
Lei Hou