- 1London School of Hygiene and Tropical Medicine, University of London, London, United Kingdom
- 2Medical Research Council (MRC)/Uganda Virus Research Institute (UVRI) and London School of Hygiene and Tropical Medicine (LSHTM) Uganda Research Unit, Entebbe, Uganda
- 3Institut National de Recherche Biomédicale (République démocratique du Congo), Kinshasa, Democratic Republic of Congo
- 4College of Medicine and Allied Health Sciences, University of Sierra Leone, Freetown, Sierra Leone
- 5Ministry of Health and Sanitation (Sierra Leone), Freetown, Sierra Leone
- 6KEMRI Wellcome Trust Research Programme, Kilifi, Kenya
- 7Mwanza Intervention Trials Unit, Mwanza, Tanzania
Objectives: This cross-sectional survey explored COVID-19 vaccine acceptability among public healthcare facility workers in Kambia (Sierra Leone), Goma (Democratic Republic of Congo) and Masaka (Uganda).
Methods: Questionnaire-based interviews conducted between April–October 2021 explored participants’ knowledge and perceptions of, and attitudes towards, the COVID-19 pandemic and COVID-19 vaccines, as well as COVID-19 vaccine acceptability (defined as uptake of ≥1 dose or intent to get vaccinated).
Results: Whilst most (n = 444; 81.8%) of the 543 participants had one or more concerns about COVID-19 vaccines, 487 (89.7%) nonetheless perceived that they were important for pandemic control. Most participants from Kambia or Masaka either were vaccinated (n = 137/355; 38.6%) or intended to get vaccinated (n = 211/355; 59.4%) against COVID-19. In Goma, all 188 participants were unvaccinated; only 81 (43.1%) participants intended to get vaccinated, and this was associated with positive perceptions about COVID-19 vaccines. In Goma, the most common reasons for not wanting a COVID-19 vaccine were concerns that the vaccines were new (n = 75/107; 70.1%) and fear of side effects (n = 74/107; 69.2%).
Conclusion: Reported COVID-19 vaccine acceptability was high among healthcare facility workers in Kambia and Masaka. The lower vaccine acceptability in Goma may highlight the importance of social mobilisation and accurate, accessible information that addresses specific concerns.
Introduction
The development, licensing and implementation of prophylactic COVID-19 vaccines was an immense global accomplishment. Up to May 2022, over 66% of the global population had received at least 1 COVID-19 vaccine dose, but vaccine uptake varied considerably across regions and countries, ranging from just 0.1% in Burundi to 99% in the United Arab Emirates [1, 2]. Whilst funding constraints and inequitable vaccine access have undoubtedly resulted in slower vaccine distribution in many low and middle income countries (LMIC) [3, 4], vaccine hesitancy has presented a separate challenge in both high income countries (HIC) and LMIC [5, 6]. Some countries in Sub-Saharan Africa (SSA) have come under the spotlight with reported widespread reluctance to be vaccinated that has led to COVID-19 vaccines expiring and being destroyed [7, 8].
Until recently, the scientific community’s assumption was that vaccine hesitancy arises from misinformation and lack of access to correct information; however, an important role of institutional and social mistrust is increasingly recognised [6, 9], which has been particularly evident during the COVID-19 pandemic [10–12]. Healthcare workers are often trusted figureheads within communities and thus have an integral role in promoting vaccine uptake [6, 13, 14]. Furthermore, healthcare workers are widely considered as a priority group for COVID-19 vaccination due to their high risk of exposure to SARS-CoV-2, their contact with vulnerable individuals, and the burden on healthcare services if they are off work due to sickness.
Few studies have evaluated COVID-19 vaccine acceptability among healthcare workers in SSA and the sparse data available have demonstrated variable acceptability in this group, though some of the studies were conducted before COVID-19 vaccines were actually available to participants [15, 16]. This was a multi-centre cross-sectional survey to evaluate COVID-19 vaccine acceptability (inclusive of vaccine uptake or intent to get vaccinated) among public healthcare facility workers in three countries spanning West, Central and East Africa—Sierra Leone, Democratic Republic of Congo (DRC) and Uganda—in the months following vaccine introduction in these countries. The study explored participants’ knowledge and perceptions of, and attitudes towards, COVID-19 vaccines in order to better understand drivers of vaccine acceptability, and evaluated factors specifically associated with COVID-19 vaccine uptake or intent to get vaccinated.
Methods
Study Design
This was a cross-sectional survey nested within the serosurvey component of a study assessing the impact of COVID-19 on primary health care service provision and utilisation in Kambia (Sierra Leone), Goma (DRC) and Masaka (Uganda): the “COVID-19 HWI study.” The COVID-19 HWI study has been described elsewhere [17]. In the serosurvey component, repeated SARS-CoV-2 serology was conducted among staff with patient contact roles at participating healthcare facilities to estimate their exposure to SARS-CoV-2, the incidence of infection during the study period, and the rate of antibody waning following infection. The vaccine acceptability survey described in this paper was conducted among healthcare facility workers when they were participating in the second or third serosurvey.
Study Setting
Kambia district, located in the northern province of Sierra Leone, covers an area of ∼3,100 km2 and has ∼345,000 residents and 69 public health facilities (1 hospital, 15 community health centres, 16 community health posts, and 37 maternal child health posts). Goma, the capital of the North Kivu province of the DRC, covers an area of ∼76 km2 and has ∼707,000 residents and 39 public health facilities (13 tertiary care hospitals and 26 health centres). Masaka, located in southern Uganda, covers an area of ∼1,603 km2 and has ∼336,000 residents and 36 health facilities (2 hospitals, 25 public health centres and 9 private not-for-profit health centres). Twenty-nine public health facilities in Kambia were selected for participation in the COVID-19 HWI study through stratified random sampling to ensure proportional representation of health posts and health facilities [17]. All 25 public health centres in Masaka and 21 accessible health centres in Goma were selected for participation.
Details of the COVID-19 pandemic situation and COVID-19 vaccine introductions in the 3 study countries are shown in Table 1.
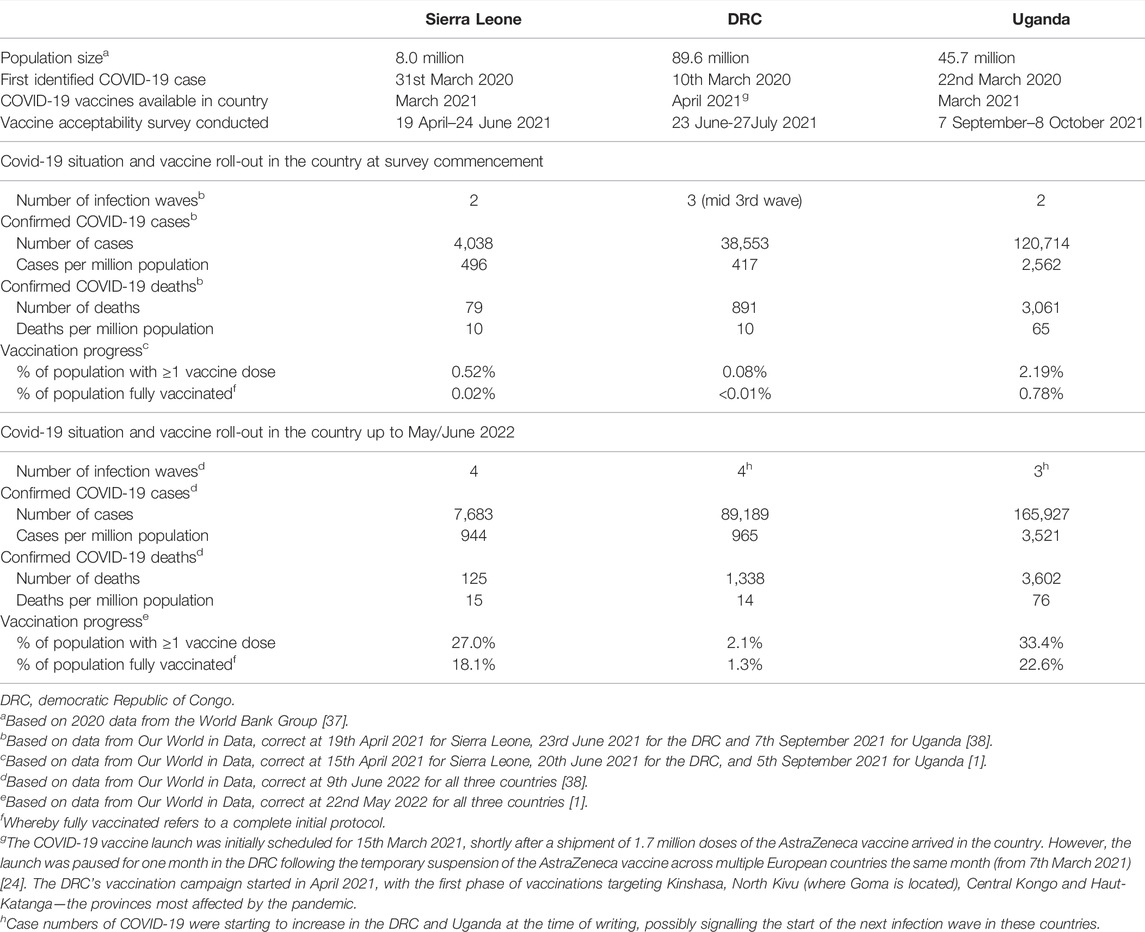
TABLE 1. Details on the COVID-19 pandemic situation and COVID-19 vaccine roll-out in Sierra Leone, Democratic Republic of Congo and Uganda at the time when the survey was conducted and up to May/June 2022. (COVID-19 vaccination in health workers; Sierra Leone, Democratic Republic of Congo and Uganda; 2021).
Vaccine Survey Participants
Selection of participants for the COVID-19 HWI serosurvey has been described previously [17]. Healthcare facility workers aged ≥18 years who were enrolled in the COVID-19 HWI serosurvey and available at the time that the vaccine acceptability survey was conducted were eligible for inclusion. Potential participants were provided with an information sheet about the study, and written informed consent was obtained from all individual participants included in the study.
Data Collection and Study Variables
Data were collected through structured, face-to-face questionnaire-based interviews conducted by trained study staff members. The questionnaire, which was developed by the study team specifically for this survey, was pre-programmed into computer tablets. Participants were asked about their knowledge and perceptions of, and attitudes towards, the COVID-19 pandemic and COVID-19 vaccines, their COVID-19 vaccination status and, if unvaccinated, whether they would accept COVID-19 vaccination if it were offered to them. The interviewer read each question to the participant and pre-coded answers were recorded in the electronic case report form.
Statistical Analysis
Data were analysed using STATA version 16.0. Data were summarised descriptively and tabulated, stratified by country. Primary analyses were conducted among all healthcare facility roles combined. Secondary analyses were stratified by role, considering level and proximity of patient contact as follows [1]: doctors, clinical officers, nurses and midwives—highest contact [2]; clinical support staff (such as health attendants, antenatal care workers and community health workers)—medium contact; and [3] pharmacy and laboratory staff and non-clinical support staff (such as ambulance drivers, porters and receptionists)—lowest contact.
Multivariable logistic regression was used to examine factors associated with COVID-19 vaccine uptake or intent to get vaccinated. Regression analyses first evaluated associations with age, sex, education level and role in the healthcare facility. Second, adjusted for these variables, analyses examined whether vaccine uptake or intent to get vaccinated was associated with specific perceptions on the impact of the COVID-19 pandemic and the COVID-19 response in the country, as well as understanding and views of COVID-19 vaccines.
Ethics
The study was reviewed and approved by the London School of Hygiene and Tropical Medicine Research Ethics Committee (Ref: 22726), the Uganda Virus Research Institute Research Ethics Committee (Ref: GC/127/821), the Uganda National Council for Science and Technology (Ref: H1430ES), the Comité National d’Ethique de la Santé, and the Sierra Leone Ethics and Scientific Review committee. All study procedures were performed in accordance with the ethical standards of the institutional and national research committees, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Results
The vaccine acceptability survey was conducted from 19th April to 24th June 2021 in Kambia (1–3 months after COVID-19 vaccine introduction in Sierra Leone), 23rd June to 27th July 2021 in Goma (2-3 months after vaccine introduction in the DRC), and 7th September to 8th October 2021 in Masaka (6–7 months after vaccine introduction in Uganda) (Table 1). In total, 543 healthcare facility staff participated, 124 (22.8%) from Kambia, 188 (34.6%) from Goma and 231 (42.5%) from Masaka. Brief demographics and characteristics of the interviewees are shown in Table 2.
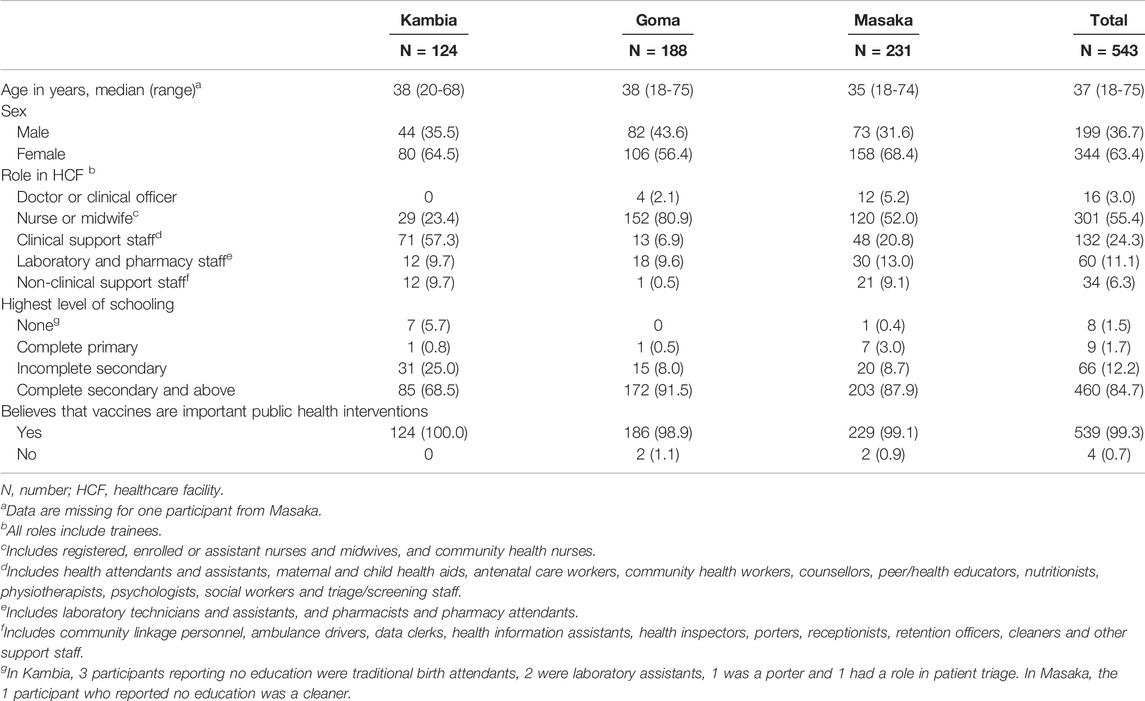
TABLE 2. Participant demographics and characteristics. (COVID-19 vaccination in health workers; Sierra Leone, Democratic Republic of Congo and Uganda; 2021).
Overall, 99.3% of participants agreed that vaccines in general (i.e., not only COVID-19 vaccines) are important public health interventions. Most agreed that vaccines can prevent infections (n = 433/539; 80.3%) and severe illness or death from some diseases (n = 490/539; 90.9%), and that they can reduce the burden on healthcare services (414/539; 76.8%) and healthcare costs (389/539; 72.2%). The few participants (2 registered nurses in Goma and 1 counsellor and a health information assistant from Masaka) who did not agree that vaccines, in general, are important public health interventions had concerns over vaccine safety (n = 3) and efficacy (n = 2) and/or considered vaccine manufacturers to be untrustworthy (n = 3).
Knowledge and Perceptions About the COVID-19 Pandemic and COVID-19 Vaccines
All participants in Kambia, 185 (98.4%) from Goma and 225 (97.4%) from Masaka agreed that COVID-19 was an important public health problem in their country (Table 3). Results were similar when stratifying by role in the healthcare facility (Supplementary Tables S1–S3). Most participants perceived that many healthcare workers were getting sick (337/543; 62.1%), and that many people generally were becoming unwell (n = 455/543; 83.8%) and dying (n = 365/545; 67.2%), from COVID-19 in their country. However, 2 registered nurses from Goma and a training nurse from Masaka believed that COVID-19 was not a real disease (n = 2), or that there was no SARS-CoV-2 or COVID-19 in their country (n = 2).
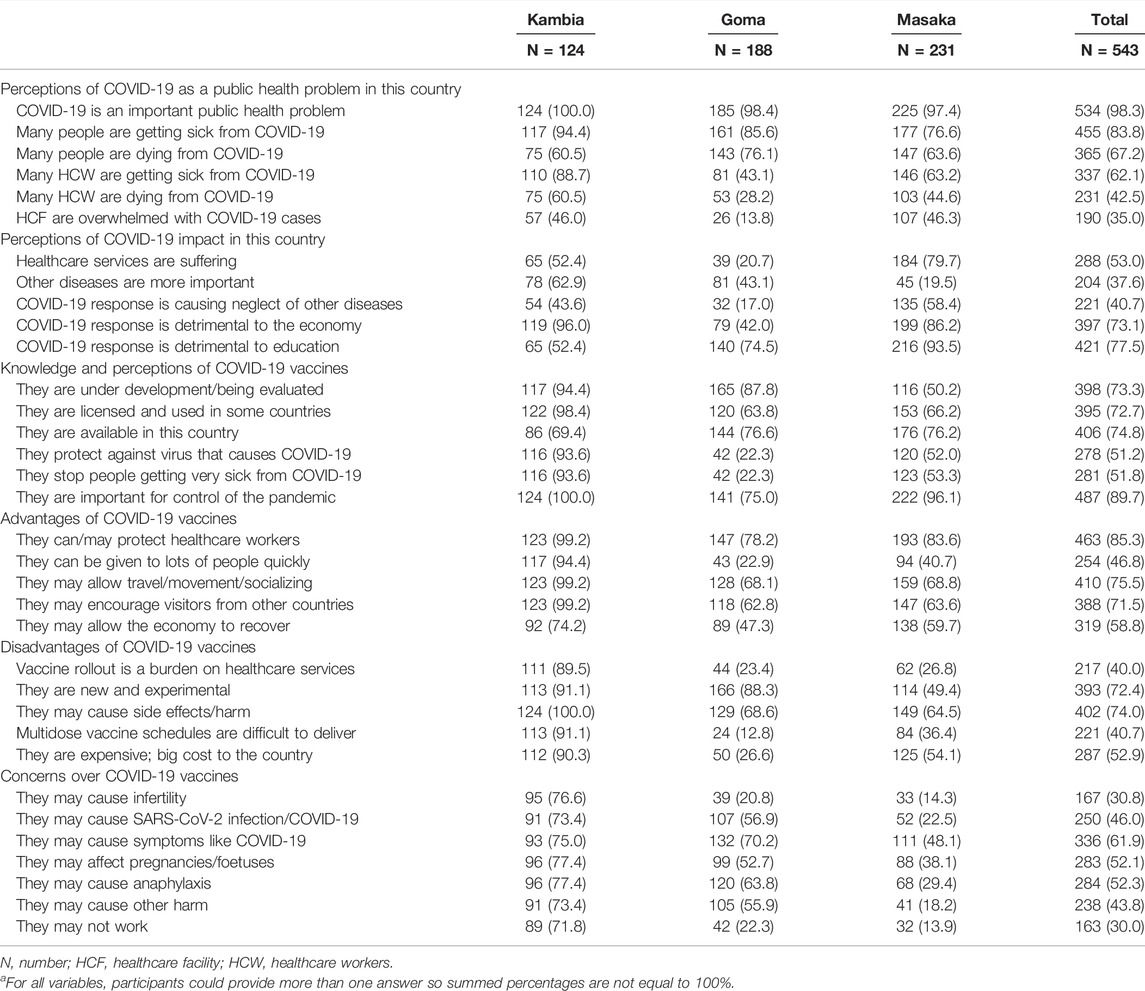
TABLE 3. Knowledge and perceptions of the COVID-19 pandemic and COVID-19 vaccines.a (COVID-19 vaccination in health workers; Sierra Leone, Democratic Republic of Congo and Uganda; 2021).
Views on the impact of the COVID-19 pandemic varied considerably across the 3 study sites (Table 3). For example, 184 (79.7%) participants in Masaka believed that healthcare services in their country were suffering because of the pandemic, compared with just 39 (20.7%) from Goma. Most (n = 119; 96.0%) participants from Kambia considered that the COVID-19 response was detrimental to their country’s economy, compared to just 79 (42.0%) from Goma.
Most participants (89.7% overall; 86.4% of clinicians, nurses and midwives) considered that COVID-19 vaccines were important to control the pandemic; this ranged from 75.0% of participants in Goma to 100.0% in Kambia (Table 3; Supplementary Tables S1–S3). Among the participants who did not agree that COVID-19 vaccines were important for control of the pandemic, the most commonly cited reasons were that there were other priorities that were more important for the country (n = 15), that COVID-19 could be controlled with other measures (n = 15) and that COVID-19 vaccines might not work (n = 15). Overall, 58 (46.8%) participants from Kambia, 21 (11.2%) from Goma and 154 (66.7%) from Masaka believed that COVID-19 vaccination should be compulsory in their country.
Whilst the results above indicate that overall support for COVID-19 vaccines was high (albeit lower in Goma compared to the other study sites), 393 (72.4%) participants (ranging from 49.4% in Masaka to 91.1% in Kambia) had concerns that the vaccines were new and experimental (Table 3). Findings were similar when restricted to clinicians, nurses and midwives (Supplementary Tables S1–S3). Overall, 250 (46.0%) participants had concerns that COVID-19 vaccines could cause SARS-CoV-2 infection or COVID-19, 167 (30.8%) had concerns that they could cause infertility and 283 (52.1%) had concerns that they could be harmful in pregnancy; all of these concerns were more common in Kambia than in Goma or Masaka (Table 3). Findings were similar when restricted to clinicians, nurses and midwives (Supplementary Tables S1–S3). Only 174 (54.9%) participants from this restricted group considered that COVID-19 vaccines could cause anaphylaxis, despite this being a known risk associated with vaccines.
COVID-19 Vaccine Uptake and Acceptability
At the time of the survey, 48 (38.7%) participants from Kambia and 89 (38.5%) from Masaka had received ≥1 COVID-19 vaccine dose (Table 4; Figure 1). In Kambia, vaccine uptake (≥1 dose) was highest among clinicians, nurses and midwives (n = 17/29; 58.6%), followed by clinical support workers (n = 25/71; 35.2%), followed by other workers (n = 6/24; 25.0%) (37.9%) (Chi2 = 7.1, p = 0.029; Supplementary Table S1). There was no difference in uptake between different roles in Masaka (Supplementary Table S3). Most unvaccinated participants from Kambia (n = 75/76; 98.7%) and Masaka (n = 136/142; 95.8%) said that they would accept a COVID-19 vaccine if offered it, meaning that reported willingness to accept the vaccine—including either uptake of ≥1 dose by the time of the survey or intent to get vaccinated—was very high (99.2% in Kambia; 97.4% in Masaka). In Goma, no study participant was vaccinated against COVID-19 at the time of the survey (despite the vaccine being available to healthcare facility workers at that time) and only 81 (43.1%) participants (and 43.6% of clinicians, nurses and midwives) said that they would accept the vaccine if offered it.
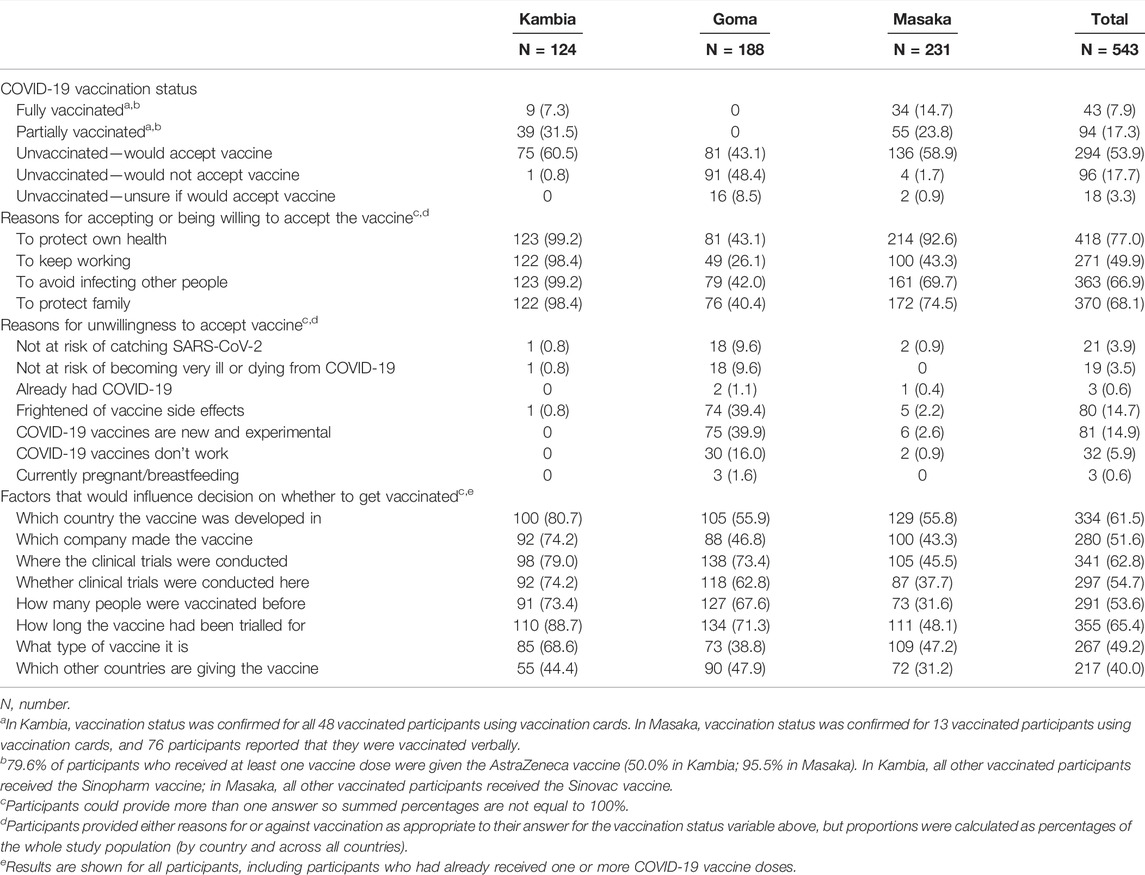
TABLE 4. COVID-19 vaccine uptake and acceptability. (COVID-19 vaccination in health workers; Sierra Leone, Democratic Republic of Congo and Uganda; 2021).
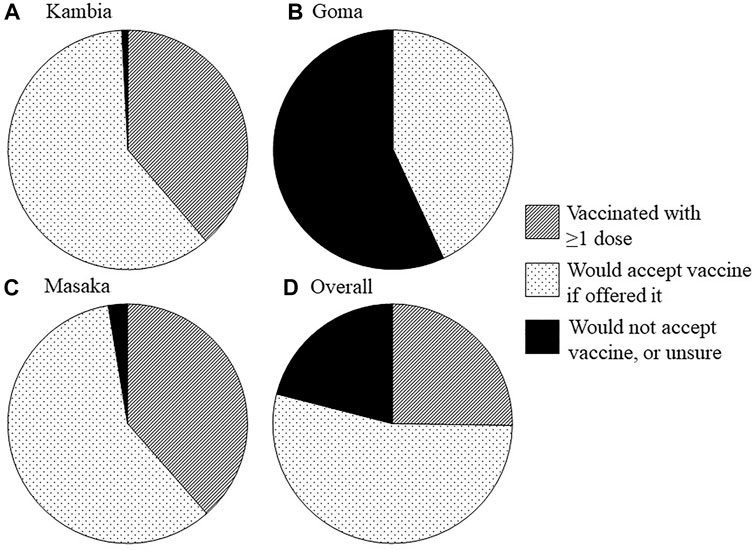
FIGURE 1. COVID-19 vaccine uptake, intent to get vaccinated and vaccine hesitancy/declining vaccination among healthcare facility workers. Pie charts show, by study site [(A) Kambia, (B): Goma, (C): Masaka, and (D): overall], the proportion of participants who had already received at least one dose of the vaccine by the time of the survey, who would accept the vaccine if offered it and who would not accept the vaccine or did not know if they would accept the vaccine. (COVID-19 vaccination in health workers; Sierra Leone, Democratic Republic of Congo and Uganda; 2021).
Reasons for accepting or not accepting the COVID-19 vaccine (with “acceptance” referring to either vaccine uptake or intent to get vaccinated) are shown in Table 4. Among the 96 participants from the 3 study sites who reported that they would not accept the vaccine, the most common reasons were fear of side effects (n = 80; 83.3%) and concerns that the vaccines were new and experimental (n = 81; 84.4%). Approximately one fifth of participants who would not accept the vaccine believed that they were not at risk of catching SARS-CoV-2 (n = 21; 21.9%) or becoming seriously ill or dying from COVID-19 (n = 19; 19.8%), and almost a third believed that the vaccines did not work (n = 32; 33.3%).
When asked, hypothetically, what factors might influence participants’ decisions on whether or not to receive a COVID-19 vaccine, the most commonly selected factors included which country the vaccine was developed in (n = 334; 61.5%) and where and for how long the clinical vaccine trials to evaluate it were conducted (n = 341; 62.8% and n = 355; 65.4%, respectively), although results varied slightly across the 3 study sites (Table 4). Among the 114 unvaccinated participants who said that they would not accept a COVID-19 vaccine or were unsure if they would accept one, most said that, hypothetically, their decision on whether to get vaccinated might be influenced by where and for how long the clinical vaccine trials were conducted (n = 78; 68.4% and n = 74; 64.9%, respectively), and how many people had been vaccinated before them (n = 69; 60.5%).
In Kambia, theoretical willingness to be vaccinated against COVID-19 was high for vaccines developed in the United States (n = 119; 96.0%), the United Kingdom (n = 122; 98.4%), Europe (n = 112; 90.3%) or Russia (n = 113; 91.1%), but was lower for vaccines developed in China (n = 80; 64.5%) (Supplementary Figure S1). A similar pattern was observed in Goma (the United States: n = 95; 50.5%, United Kingdom: n = 92; 48.9%, Europe: n = 86; 45.7%, China: n = 57; 30.3%, Russia: n = 69; 36.7%). In Masaka, willingness to be vaccinated against COVID-19 was highest for vaccines developed in the United States (n = 192; 83.1%) and the United Kingdom (n = 185; 80.1%), and lower for those developed in Europe (n = 114; 49.4%), China (n = 97; 42.0%) or Russia (n = 100; 43.3%).
Factors Associated With Intent to Get Vaccinated in Goma
Since almost all participants in Kambia and Masaka had either received ≥1 COVID-19 vaccine dose or reported their intention to receive the vaccine, analyses of factors associated with willingness to receive a COVID-19 vaccine were limited to participants from Goma (Table 5). Adjusted for age, sex and type of role within the healthcare facility, participants with lower education level were more likely to report intent to receive the COVID-19 vaccine than those with higher education level (OR 3.17, 95%CI 1.01–9.96; p = 0.040) (Table 5). Adjusted for age, sex, education and type of role within the healthcare facility, intention to get vaccinated was associated with participant perceptions that the COVID-19 pandemic, or the country’s response to the pandemic, was having a negative or detrimental affect on healthcare services (OR 5.69, 95%CI 2.45–13.21; p < 0.001), that the COVID-19 response was resulting in the neglect of other diseases (OR 8.61, 95%CI 3.24–22.89; p < 0.001), and that the COVID-19 response was detrimental to the economy (OR 2.24, 95%CI 1.21–4.17; p = 0.010). Intent to be vaccinated was also associated with participants’ perceptions/knowledge that COVID-19 vaccines protect against SARS-CoV-2 infection or can stop people from getting very ill from COVID-19 (for each, OR 3.69, 95%CI 1.73–7.87; p < 0.001), and that the vaccines are important for control of the pandemic (OR 18.19, 95%CI 5.23–63.30; p < 0.001).
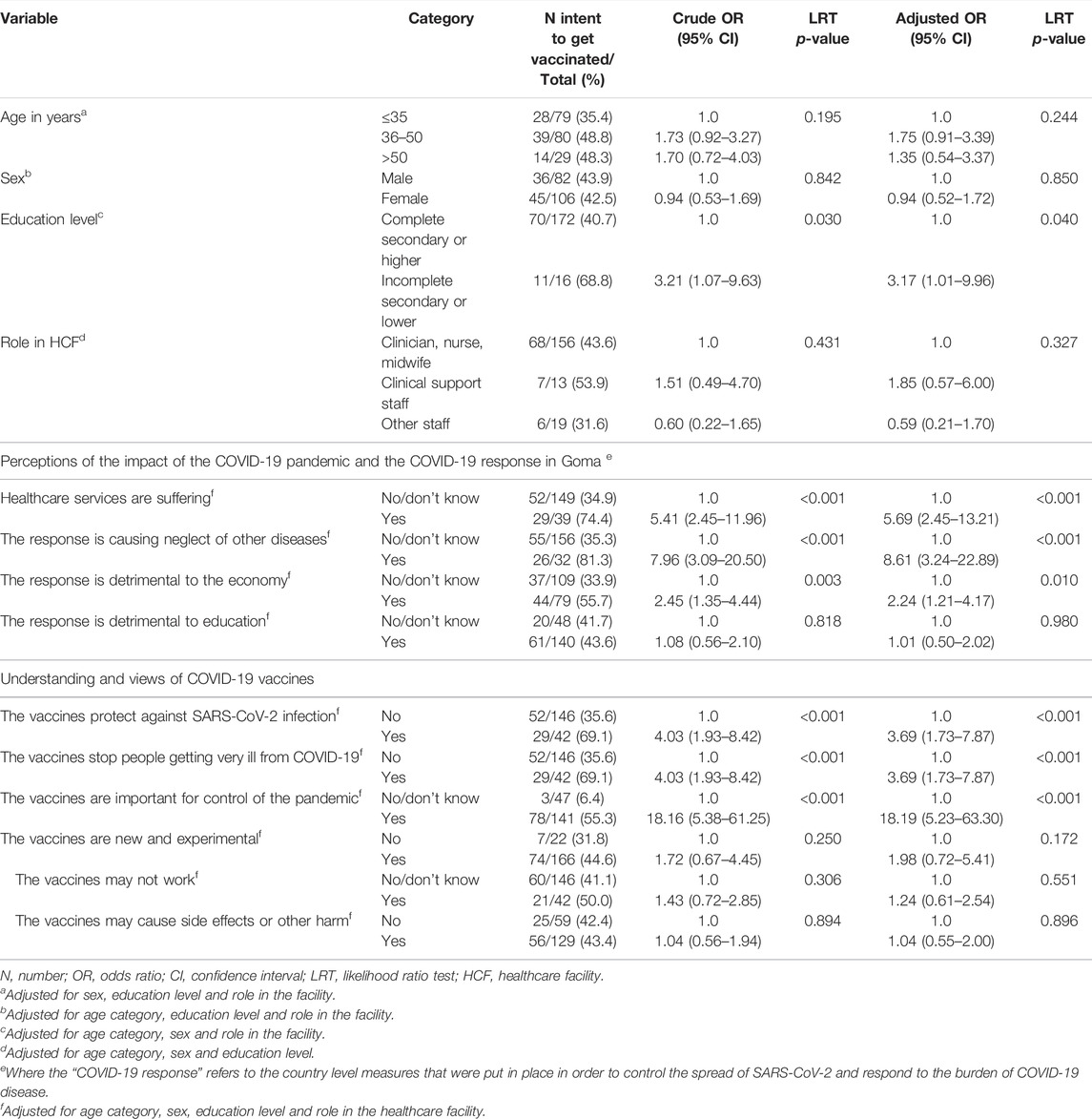
TABLE 5. Factors associated with intent to get vaccinated against COVID-19 in Goma. (COVID-19 vaccination in health workers; Sierra Leone, Democratic Republic of Congo and Uganda; 2021).
Whilst many participants from Goma had concerns that COVID-19 vaccines were new and experimental (n = 166; 88.3%), that they might not work (n = 42; 22.3%), and that they may cause side effects or harm (n = 129; 68.6%), these concerns were not associated with lower intention to get vaccinated in multivariable analyses (Table 5). Thus, whilst these concerns may have played an integral role in decision making among participants who did not intend to get vaccinated, the concerns were similarly prevalent among participants who reported intent to get vaccinated (i.e., with the latter group intending to get vaccinated despite these concerns).
Additional exploratory analyses evaluated factors associated with uptake of ≥1 vaccine dose in Masaka, with the hypothesis that unvaccinated participants may be those who had delayed getting vaccinated (as the survey was conducted 6–7 months after vaccine introduction); none of the variables evaluated were associated with uptake (Supplementary Table S4).
Discussion
To our knowledge, this was the first study in SSA to evaluate acceptability of COVID-19 vaccines (alongside participants’ knowledge and perceptions of, and attitudes towards, the vaccines) in a diverse range of healthcare facility workers with varying levels of patient contact, and to stratify findings across cadres. Consistent with earlier studies from SSA [16], reported COVID-19 vaccine acceptability was high in Kambia and Masaka, with most participants having already received ≥1 vaccine dose or reporting that they would have the vaccine if offered it.
Accounting for the timing of the survey, COVID-19 vaccine uptake (of ≥1 dose) was greatest in Kambia (where the survey was conducted 1–3 months after vaccine introduction), possibly reflecting high country-wide willingness to get vaccinated following the devastation of the 2014–2015 West African Ebola outbreak. In 2015, research infrastructure was rapidly set up in Kambia for conduct of clinical trials of novel Ebola vaccines [18, 19]; a programme of these trials continues to date. Thus, the high COVID-19 vaccine acceptability observed among healthcare facility workers in Kambia may additionally be motivated by 7 years of research teams’ engagement, communication and building trust with and between local authorities, communities and healthcare personnel [20, 21]. Whilst concerns about adverse effects of COVID-19 vaccines were common across all 3 study sites, they were most common in Kambia. Thus, the high vaccine acceptability observed despite these concerns suggests a high level of trust in authorities, vaccine manufacturers and other relevant institutions.
It is notable that many participants from Masaka were reportedly willing to have a COVID-19 vaccine but not yet vaccinated at the time of the survey (conducted 6–7 months after vaccine introduction) given that healthcare workers were prioritized for vaccination. For comparison, a study conducted in Malawi between 0.5 and 2 months after COVID-19 vaccine introduction in the country found that 83% of surveyed healthcare workers had already received the first COVID-19 vaccine dose [22]. Whilst the slower uptake in Masaka may reflect logistical constraints and delays in vaccine roll-out and challenges in vaccine access, it may also be due to participants delaying vaccination or decision-making on whether to get vaccinated. In Masaka, the main COVID-19 vaccine available to participants at the time of the survey was the Covishield AstraZeneca vaccine (produced by the Serum Institute of India), and there was extensive media attention surrounding a small risk of thrombotic events associated with the AstraZeneca COVID-19 vaccine around that time [23, 24]. Furthermore, there were long and heavily publicised delays in the European Medicines Agency (EMA) issuing approval of the Covishield vaccine, with ensuing challenges to entering Europe for travellers who had received it [25]. Anecdotally, many people in Uganda reported waiting for “better” or “safer” COVID-19 vaccines to become available before getting vaccinated. Nonetheless, our results are consistent with earlier research from Uganda that showed high acceptability of COVID-19 vaccines in general among eye healthcare workers [26] and high willingness of healthcare workers to participate in COVID-19 vaccine trials [27].
COVID-19 vaccine introduction in the DRC met with several challenges. The vaccine launch was initially scheduled for March 2021 but postponed following the temporary suspensions in roll-out of the AstraZeneca vaccine in Europe (due to the small risk of thrombotic events described above) [24]. Whilst the vaccination campaign in the DRC started just a month later, rapid and extensive spread of vaccine-related rumours across the country and the president’s vociferous mistrust in the vaccines meant that uptake was very slow [28, 29]. This is reflected in the results of this study, with no study participants from Goma having received a COVID-19 vaccine by the time of the survey (conducted 2–3 months after vaccinations started), and less than half reporting willingness to be vaccinated. A public health official from the DRC expressed concerns that distrust in the vaccines was amplified by the “unfortunate communication around AstraZeneca in Europe” [30]. Nonetheless, the poor uptake of COVID-19 vaccines in the DRC follows a history of multiple outbreaks of measles and yellow fever occurring in the country over the past decade due to inadequate coverage of the respective vaccines, partly resulting from low vaccine acceptability [28].
In earlier studies, female gender, lower age and being in a nursing role were associated with COVID-19 vaccine hesitancy among healthcare workers, and being older, male and a doctor were associated with higher vaccine acceptability [31–34]. These associations were not observed in this study. However, reported intent to get vaccinated in Goma was associated with perceptions that the COVID-19 pandemic and the country’s response to the pandemic were having negative impacts on the country (for example, on healthcare services or the economy) and, as seen in previous studies of healthcare workers in Malawi, South Africa and Ethiopia [22, 34, 35], with positive perceptions of the vaccines’ efficacy/effectiveness and impact against SARS-CoV-2 infection or COVID-19 disease.
A major strength of this study is that it was conducted in sites from 3 countries spanning East, Central and West Africa, and that it included participants from a range of healthcare facilities in each of the study locations. Furthermore, the study included a wide variety of healthcare facility workers with patient contact roles and results were stratified by cadre. The survey was conducted at an important time within the context of vaccine roll-out in SSA; the vaccines were newly available in the countries and, given that healthcare workers were prioritized for vaccination, most participants should have had access to the vaccine or would be given access within the near future. Several earlier studies of healthcare workers were conducted before the COVID-19 vaccines became available in their country [15], and thus reported acceptability was hypothetical.
The cross-sectional study design was a limitation as results represent participant views at just one point in time. Vaccine decision-making is a dynamic process and vaccination status or intent to get vaccinated may change over time. This is particularly relevant for a newly available vaccine as many people may be reassured as more populations are vaccinated and as more safety/efficacy data become available. Second, it was not always possible to verify vaccination status using vaccination cards. The risk of recall bias with self-reporting of vaccination status is likely to be low in this study, but social desirability bias is possible. Finally, due to the quantitative study design, it was not possible to explore the in-depth nuances of participants’ views and perceptions and rationale behind their decision-making. There were also several inconsistencies in participants’ responses that could not be further explored and elucidated. Nonetheless, the study highlights interesting and important topics that could be further explored through employment of qualitative methods.
Conclusion
In 2019, the WHO declared vaccine hesitancy as one of the ten greatest threats to global health [36]. With the recent development, trialling and roll-out of COVID-19 vaccines, topics surrounding vaccine decision-making, misinformation and ‘anti-vax’ movements have gained even greater prominence in both the scientific literature and the media. This survey provides important results on COVID-19 vaccine acceptability among healthcare facility workers in the months following vaccine introduction in study sites from 3 SSA countries, which may be informative for future vaccine introductions in the region, particularly within the context of an outbreak or pandemic. The results demonstrate the importance of educating healthcare staff on vaccine development processes, and on evidence surrounding vaccine efficacy/effectiveness and safety, both to promote vaccine uptake in this group and to ensure appropriate and accurate communication regarding vaccines between healthcare staff and their patients or the wider communities. Results also demonstrate the importance of careful and accurate messaging surrounding vaccines and vaccine introductions at a global level.
Ethics Statement
The studies involving human participants were reviewed and approved by the London School of Hygiene and Tropical Medicine Research Ethics Committee, the Uganda Virus Research Institute Research Ethics Committee, the Uganda National Council for Science and Technology, the Comité National d’Ethique de la Santé, and the Sierra Leone Ethics and Scientific Review committee. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
HSW, DW-J, and KEG conceptualised the study, wrote the study protocol and designed the data collection tools, with input from all co-authors. JK, KK, DT, and JB coordinated or contributed to data collection, with oversight from ER, HK-M, BL, HSW, KEG, DW-J, and BG. PK, YN, and DT were responsible for data management. HSW performed data analyses and created the data tables and figures. HSW and JK wrote the manuscript, with input from all co-authors.
Funding
This research was funded through a UKRI (MRC), DHSC (NIHR) research grant (GEC1017, MR/V029363/1).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We would like to acknowledge Dr. Myfanwy James, who contributed to planning of data collection in the DRC.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/ijph.2022.1605113/full#supplementary-material
References
1.Our World In Data. Coronavirus (COVID-19) Vaccinations (2022). Available from: https://ourworldindata.org/covid-vaccinations (Last accessed Jun 10, 2022).
2. Mathieu, E, Ritchie, H, Ortiz-Ospina, E, Roser, M, Hasell, J, Appel, C, et al. A Global Database of COVID-19 Vaccinations. Nat Hum Behav (2021) 5(7):947–53. doi:10.1038/s41562-021-01122-8
3. Ariyo, OE, Oladipo, EK, Osasona, OG, Obe, O, and Olomojobi, F. COVID-19 Vaccines and Vaccination: How Prepared Is Africa? Pan Afr Med J (2021) 39:107. doi:10.11604/pamj.2021.39.107.27912
4. Lawal, L, Aminu Bello, M, Murwira, T, Avoka, C, Yusuf Ma'aruf, S, Harrison Omonhinmin, I, et al. Low Coverage of COVID-19 Vaccines in Africa: Current Evidence and the Way Forward. Hum Vaccin Immunother (2022) 18(1):2034457. doi:10.1080/21645515.2022.2034457
5. Idris, IO, Ayeni, GO, and Adebisi, YA. Why many African Countries May Not Achieve the 2022 COVID-19 Vaccination Coverage Target. Trop Med Health (2022) 50(1):15. doi:10.1186/s41182-022-00407-6
6. Mutombo, PN, Fallah, MP, Munodawafa, D, Kabel, A, Houeto, D, Goronga, T, et al. COVID-19 Vaccine Hesitancy in Africa: a Call to Action. Lancet Glob Health (2022) 10(3):e320–e321. doi:10.1016/S2214-109X(21)00563-5
7. Adidja, A, Boum, Y, and Ongolo-Zogo, P. Cameroon: Doubt Could Mean Vaccine Doses Expire. Nature (2021) 595(7865):30. doi:10.1038/d41586-021-01784-4
8. Murewanhema, G, Musuka, G, Mukwenha, S, Chingombe, I, Mapingure, MP, and Dzinamarira, T. Hesitancy, Ignorance or Uncertainty? the Need for Effective Communication Strategies as Zimbabwe's Uptake of COVID-19 Vaccine Booster Doses Remains Poor. Public Health Pract (Oxf) (2022) 3:100244. doi:10.1016/j.puhip.2022.100244
9. Stoop, N, Hirvonen, K, and Maystadt, JF. Institutional Mistrust and Child Vaccination Coverage in Africa. BMJ Glob Health (2021) 6(4):e004595. doi:10.1136/bmjgh-2020-004595
10. Katoto, P, Parker, S, Coulson, N, Pillay, N, Cooper, S, Jaca, A, et al. Predictors of COVID-19 Vaccine Hesitancy in South African Local Communities: The VaxScenes Study. Vaccines (Basel) (2022) 10(3):353. doi:10.3390/vaccines10030353
11. Roy, DN, Biswas, M, Islam, E, and Azam, MS. Potential Factors Influencing COVID-19 Vaccine Acceptance and Hesitancy: A Systematic Review. PLoS One (2022) 17(3):e0265496. doi:10.1371/journal.pone.0265496
12. Jennings, W, Stoker, G, Bunting, H, Valgarðsson, VO, Gaskell, J, Devine, D, et al. Lack of Trust, Conspiracy Beliefs, and Social Media Use Predict COVID-19 Vaccine Hesitancy. Vaccines (Basel) (2021) 9(6):593. doi:10.3390/vaccines9060593
13. Solís Arce, JS, Warren, SS, Meriggi, NF, Scacco, A, McMurry, N, Voors, M, et al. COVID-19 Vaccine Acceptance and Hesitancy in Low- and Middle-Income Countries. Nat Med (2021) 27(8):1385–94. doi:10.1038/s41591-021-01454-y
14. Ekwebelem, OC, Yunusa, I, Onyeaka, H, Ekwebelem, NC, and Nnorom-Dike, O. COVID-19 Vaccine Rollout: Will it Affect the Rates of Vaccine Hesitancy in Africa? Public Health (2021) 197:e18–e19. doi:10.1016/j.puhe.2021.01.010
15. Sallam, M. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines (Basel) (2021) 9(2):160. doi:10.3390/vaccines9020160
16. Sallam, M, Al-Sanafi, M, and Sallam, M. A Global Map of COVID-19 Vaccine Acceptance Rates Per Country: An Updated Concise Narrative Review. J Multidiscip Healthc (2022) 15:21–45. doi:10.2147/JMDH.S347669
17. Kasonia, K, Tindanbil, D, Kitonsa, J, Baisley, K, Zalwango, F, Enria, L, et al. The Impact of the COVID-19 Pandemic on the Provision & Utilisation of Primary Health Care Services in Goma, Democratic Republic of the Congo, Kambia District, Sierra Leone & Masaka District, Uganda. medRxiv (2022). doi:10.1101/2022.04.28.22274416
18. Afolabi, MO, Ishola, D, Manno, D, Keshinro, B, Bockstal, V, Rogers, B, et al. Safety and Immunogenicity of the Two-Dose Heterologous Ad26.ZEBOV and MVA-BN-Filo Ebola Vaccine Regimen in Children in Sierra Leone: a Randomised, Double-Blind, Controlled Trial. Lancet Infect Dis (2022) 22(1):110–22. doi:10.1016/S1473-3099(21)00128-6
19. Ishola, D, Manno, D, Afolabi, MO, Keshinro, B, Bockstal, V, Rogers, B, et al. Safety and Long-Term Immunogenicity of the Two-Dose Heterologous Ad26.ZEBOV and MVA-BN-Filo Ebola Vaccine Regimen in Adults in Sierra Leone: a Combined Open-Label, Non-randomised Stage 1, and a Randomised, Double-Blind, Controlled Stage 2 Trial. Lancet Infect Dis (2022) 22(1):97–109. doi:10.1016/S1473-3099(21)00125-0
20. Dada, S, McKay, G, Mateus, A, and Lees, S. Lessons Learned from Engaging Communities for Ebola Vaccine Trials in Sierra Leone: Reciprocity, Relatability, Relationships and Respect (The Four R's). BMC Public Health (2019) 19(1):1665. doi:10.1186/s12889-019-7978-4
21. Enria, L, Lees, S, Smout, E, Mooney, T, Tengbeh, AF, Leigh, B, et al. Power, Fairness and Trust: Understanding and Engaging with Vaccine Trial Participants and Communities in the Setting up the EBOVAC-Salone Vaccine Trial in Sierra Leone. BMC Public Health (2016) 16(1):1140. doi:10.1186/s12889-016-3799-x
22. Moucheraud, C, Phiri, K, Whitehead, HS, Songo, J, Lungu, E, Chikuse, E, et al. Uptake of the COVID-19 Vaccine Among Healthcare Workers in Malawi. Int Health (2022) ihac007. doi:10.1093/inthealth/ihac007
23. Faranda, D, Alberti, T, Arutkin, M, Lembo, V, and Lucarini, V. Interrupting Vaccination Policies Can Greatly Spread SARS-CoV-2 and Enhance Mortality from COVID-19 Disease: The AstraZeneca Case for France and Italy. Chaos (2021) 31(4):041105. doi:10.1063/5.0050887
24. Wise, J. Covid-19: European Countries Suspend Use of Oxford-AstraZeneca Vaccine after Reports of Blood Clots. BMJ (2021) 372:n699. doi:10.1136/bmj.n699
25.Author Anonymous. Many Covid Vaccine Doses Donated to African Countries Are Not Recognized by EU Travel Certificate. CNN (2021). Available from: https://edition.cnn.com/2021/06/29/africa/africa-eu-vaccine-passport-intl/index.html (Last Accessed September 14, 2022).
26. Otiti-Sengeri, J, Andrew, OB, Lusobya, RC, Atukunda, I, Nalukenge, C, Kalinaki, A, et al. High COVID-19 Vaccine Acceptance Among Eye Healthcare Workers in Uganda. Vaccines (2022) 10(4):609. doi:10.3390/vaccines10040609
27. Kitonsa, J, Kamacooko, O, Bahemuka, UM, Kibengo, F, Kakande, A, Wajja, A, et al. Willingness to Participate in COVID-19 Vaccine Trials; a Survey Among a Population of Healthcare Workers in Uganda. PLoS One (2021) 16(5):e0251992. doi:10.1371/journal.pone.0251992
28. Rackimuthu, S, Hunain, R, Uday, U, Muzzamil, M, Rehman, MU, Okonji, OC, et al. COVID-19, Measles, and Yellow Fever: The Need to Reinforce Vaccination in the Democratic Republic of Congo. Clin Epidemiol Glob Health (2022) 13:100956. doi:10.1016/j.cegh.2021.100956
29. Nachega, JB, Sam-Agudu, NA, Masekela, R, van der Zalm, MM, Nsanzimana, S, Condo, J, et al. Addressing Challenges to Rolling Out COVID-19 Vaccines in African Countries. Lancet Glob Health (2021) 9(6):e746–e748. doi:10.1016/S2214-109X(21)00097-8
30.Africa News. DRC Launches Covid Vaccination in Kinshasa (2021). Available from: https://www.africanews.com/2021/04/19/drc-launches-covid-vaccination-in-kinshasa// (Last Accessed September 14, 2022).
31. Li, M, Luo, Y, Watson, R, Zheng, Y, Ren, J, Tang, J, et al. Healthcare Workers' (HCWs) Attitudes and Related Factors towards COVID-19 Vaccination: a Rapid Systematic Review. Postgrad Med J (2021)–140195. doi:10.1136/postgradmedj-2021-140195
32. Kabamba Nzaji, M, Kabamba Ngombe, L, Ngoie Mwamba, G, Banza Ndala, DB, Mbidi Miema, J, Luhata Lungoyo, C, et al. Acceptability of Vaccination against COVID-19 Among Healthcare Workers in the Democratic Republic of the Congo. Pragmat Obs Res (2020) 11:103–9. doi:10.2147/POR.S271096
33. Yilma, D, Mohammed, R, Abdela, SG, Enbiale, W, Seifu, F, Pareyn, M, et al. COVID-19 Vaccine Acceptability Among Healthcare Workers in Ethiopia: Do We Practice what We Preach? Trop Med Int Health (2022) 27(4):418–25. doi:10.1111/tmi.13742
34. Wiysonge, CS, Alobwede, SM, de Marie Ckp, , Kidzeru, EB, Lumngwena, EN, Cooper, S, et al. COVID-19 Vaccine Acceptance and Hesitancy Among Healthcare Workers in South Africa. Expert Rev Vaccin (2022) 21(4):549–59. doi:10.1080/14760584.2022.2023355
35. Boche, B, Kebede, O, Damessa, M, Gudeta, T, and Wakjira, D. Health Professionals' COVID-19 Vaccine Acceptance and Associated Factors in Tertiary Hospitals of South-West Ethiopia: A Multi-Center Cross- Sectional Study. Inquiry (2022) 59:469580221083181. doi:10.1177/00469580221083181
36.World Health Organisation. Newsroom. Ten Threats to Global Health in (2019). Available from: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (Last accessed Jun 10, 2022).
37.World Bank Group. Data. Population, Total (2022). Available from: https://data.worldbank.org/indicator/SP.POP.TOTL (Last accessed May 04, 2022).
38.Our World in Data. Coronavirus Data Explorer (2022). Available from: https://ourworldindata.org/explorers/coronavirus-data-explorer (Last accessed Jun 10, 2022).
Keywords: healthcare workers, sub-Saharan Africa, COVID-19 pandemic, COVID-19 vaccines, vaccine uptake, vaccine acceptability
Citation: Whitworth HS, Kitonsa J, Kasonia K, Tindanbil D, Kafeero P, Bangura J, Nije Y, Tetsa Teta D, Greenwood B, Kavunga-Membo H, Leigh B, Ruzagira E, Gallagher KE and Watson-Jones D (2022) COVID-19 Vaccine Acceptability Among Healthcare Facility Workers in Sierra Leone, the Democratic Republic of Congo and Uganda: A Multi-Centre Cross-Sectional Survey. Int J Public Health 67:1605113. doi: 10.3389/ijph.2022.1605113
Received: 10 June 2022; Accepted: 08 September 2022;
Published: 23 September 2022.
Edited by:
Jean Tenena Coulibaly, Félix Houphouët-Boigny University, Côte d’IvoireCopyright © 2022 Whitworth, Kitonsa, Kasonia, Tindanbil, Kafeero, Bangura, Nije, Tetsa Teta, Greenwood, Kavunga-Membo, Leigh, Ruzagira, Gallagher and Watson-Jones. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hilary S. Whitworth, aGlsYXJ5LndoaXR3b3J0aEBsc2h0bS5hYy51aw==
†These authors share first authorship
 Hilary S. Whitworth
Hilary S. Whitworth Jonathan Kitonsa
Jonathan Kitonsa Kambale Kasonia1,3
Kambale Kasonia1,3