Abstract
Objective: The rural northern region of Thailand exhibits the highest rate of hypertension. This study explored hypertensive-related food choices between normotensive and hypertensive people residing in rural northern Thailand to determine which food attributes influence their choices.
Methods: The study conducted a discrete choice experiment (DCE) survey among Thai adults residing in rural northern Thailand (n = 403) to estimate the relative importance of four food attributes, including food preparation, price, taste, and amount of salt. A mixed logit model was used to analyze the data from the DCE.
Results: The first and second most important attributes in both hypertensive and normotensive groups were the amount of salt and food preparation at home, respectively, followed by price and taste. Specifically, the normotensive group was more attentive to the amount of salt in their food than their hypertensive counterparts.
Conclusion: Intervention programs in rural communities may benefit from focusing their attention on embracing low-salt cultural foods and providing guidance on how to add flavor without additional salt or reduce high sodium seasonings without losing flavor when cooking.
Introduction
Hypertension, also known as high blood pressure, is a major public health concern and one of the most contributing risk factors for cardiovascular diseases (CVDs). About half of the world’s CVD burden occurs in the Asia Pacific region [1], and 30% of adults in Southeast Asia have elevated blood pressure [2]. As of 2019, one out of four Thai adults have hypertension, equating to 13.2 million people, and only 3.9 million have their blood pressure under control; more than 50,000 deaths annually are attributed to hypertension, where CVDs account for a quarter of all deaths [3]. A study on CVD patients in the northern region of Thailand found that 84% of hypertensive individuals did not know they had hypertension, and 73% of pre-hypertensive individuals did not think they were at risk [4]. Particularly, evidence indicates that the northern region of Thailand exhibits the highest rate of hypertension (33%) [3], where people living in this region consume a considerable amount of salt (3,044 mg/day) compared to those living in other regions [5].
Sodium consumption associated with hypertension in the Thai population has been extensively studied [6–8]. Thai adults consume, on average, 10.8 g of salt a day (4,320 mg of sodium), which is more than double the WHO recommended amount of daily salt (5 g/day ∼2,000 mg of sodium) [9]. Popular food choices such as one-plate meals, meat products, snacks, beverages, and fast food [10] are common sources of high sodium intake among Thai people. According to Nielsen’s global eating trend survey [11], Asia-Pacific people are avid out-of-home diners. In fact, 22% of Thai respondents, compared to 9% of global respondents, reported eating away from home at least once a day [12]. Moreover, 38% of Thai respondents who eat away from home reported eating street foods [12], which are a popular choice for out-of-home dining in Thailand and are commonly high in sodium [13].
Theoretical Framework and Hypotheses
Although the pathophysiological link between hypertension and sodium intake has been debated [14, 15], the strong association between these two has been widely recognized and supported in the literature [16]. A reduction in sodium intake can have a favorable effect on the cardiovascular system, inducing a reduction in blood pressure, particularly in hypertensive patients [14]. Furthermore, food choices can be an indicator of nutrient intake, leading to overall health status [17]. Thus, understanding individuals’ food choices and encouraging behavioral changes to promote healthier decisions can reduce the burden of hypertension-related complications [18]. However, the theoretical framework and methodologies in the literature do not account for the complexity in understanding the factors that underpin individual food choices.
The theory of planned behavior (TPB) [19], a psychological theory to predict an individual’s intention to engage in a specific behavior, has shown that food choices are complex and involve a combination of three fundamental components: 1) attitude, an overall favorable or unfavorable evaluation of the behavior; 2) personal and social norm, an individual’s sense of self obligation and accepted standard of behavior in specific situations, respectively; and 3) perceived behavioral control (PBC), a perception of the ease or difficulty of enacting the behavior [5, 20]. Mørk et al. [5] applied the TPB to food choices and found that positive salt-related attitudes (i.e., awareness of hypertension consequences), strong personal norms toward salt reduction, together with knowledge of salt-related diseases and diets can exert the strongest influence on the willingness to purchase food products low in salt.
While several studies have examined individual’s salt-related dietary knowledge, attitudes, and practices [
6,
21–
23], the results have been inconclusive. To complement the literature on TBP related to food choice behaviors, this study investigates individuals’ intention of selecting hypertension-related food between normotensive and hypertensive people in rural Thailand by constructing a choice-based survey. As food choices involve a complexity of conscious trade-offs such as money, nutrition, taste, etc. [
24], this study utilizes a discrete choice experiment (DCE), which closely resembles real-world decision-making processes [
25], to answer the following hypotheses (H1-H3):
H1: In foods that contain high salt, people with hypertension will make different trade-offs in their food choices than normotensive people.
H2: The relative importance of the attribute, amount of salt, will be lower among people with hypertension than normotensive people.
H3: People with hypertension will have different food choices than normotensive people.
Methods
Discrete Choice Experiment Design
In a DCE, subjects are presented with several questions known as choice sets, made up of several options that are constructed from different combinations of attributes [26]. Subjects are asked to select a single option. While existing survey methods such as rating, ranking, or focus group discussions, have been widely used to assess the attributes that influence food choices and health status [11, 12, 27, 28], they are unable to assess the interaction effect between two attributes. With a DCE, the interactions between attributes, and the relative importance of attributes can be identified and quantified [29], which captures the complexity of the trade-offs in decision making.
The design of the DCE refers to the selection of different combinations of attributes and levels to form the corresponding options and choice sets. It is critical in determining which attributes and interactions can be estimated. This study used an experimental design technique known as a block factorial design (BFD), which was utilized to design the DCEs in Rusmevichientong et al. 2021, 2020 [30, 31], and is based on the foundational work of Jaynes et al. 2016 [32].
The relationship between BFDs and DCEs is as follows. First, the number of blocks in a BFD refers to the number of choice sets. Second, the size of the blocks in a BFD refers to the number of options within each choice set. To construct a DCE using a BFD, start with either a full or fractional factorial block design, such that each block represents a choice set, and the number of combinations in the blocks represent the number of options within each choice set [30]. A couple of advantages of using a BFD for a DCE include 1) potentially reducing the number of choice sets while still answering the research question, and 2) estimating all individual effects and some interactions between two attributes.
This study considers four attributes denoted as A, B, C, and D, each with two levels. A full factorial design for four two-level attributes consists of 16 (24) possible combinations, which are divided into four blocks, each with four combinations [33], representing a DCE with four choice sets, each with four options. With this design, all four attributes (A, B, C, D) plus five interactions between two attributes (AC, AD, BC, BD, CD) can be estimated unbiasedly.
In addition to the four options in each choice set, a none option was also included. If subjects are unsatisfied with any of the available options, they may choose the opt-out option. By including an opt-out option, this prevents subjects from being forced to make a choice. As forcing subjects to make a choice induces bias, as they may not always make that same choice in real life [34]. An example choice set from the DCE is presented in Figure 1.
FIGURE 1
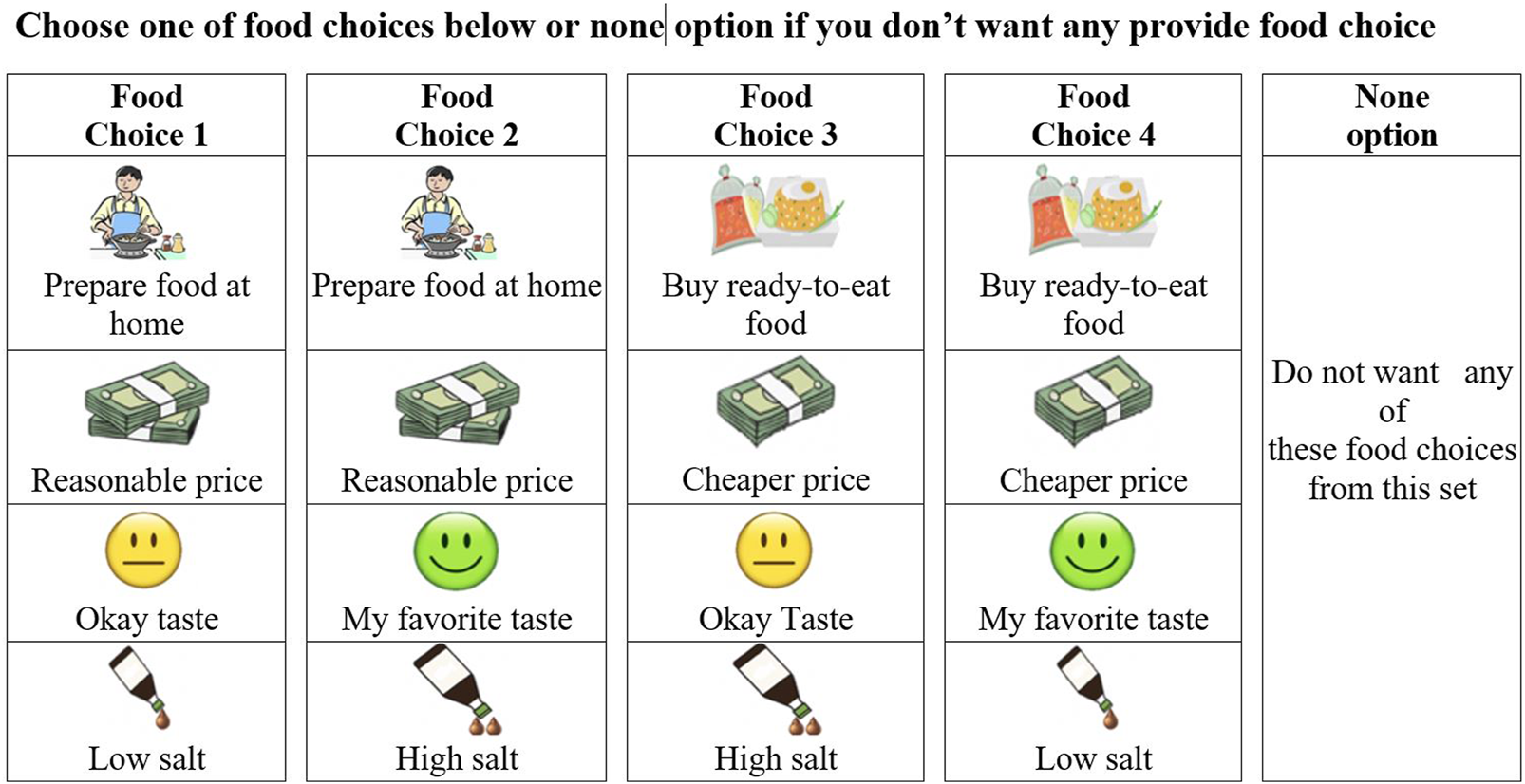
An example of a food choice set in a Discrete Choice Experiment (Chiang Mai, Thailand, 2019).
Attribute Selection and Attribute Levels
Various attributes can influence consumer choices and should be considered in a DCE; however, some attributes may need to be excluded so that the choice sets are appropriate for the subjects’ cognitive ability [35]. As the number of attributes and levels increase, the number of possible choice sets increase, which can be overwhelming for subjects [24], potentially creating cognitive overload. This study considered a limited number of attributes and levels for each attribute to keep the complexity of the DCE simple.
Based on the literature, the major drivers of food choices are perceptions of convenience, cost, taste, and nutritional values [12, 30, 36, 37]. Convenience refers to the ease of physical access to food sources and the time spent buying and preparing food [36, 37]. Ready-to-eat foods require less cooking time, energy, and space, and therefore are considered more convenient than cooking food at home [17]. Food costs, such as food prices and the relative affordability of alternative food patterns [36, 38] also strongly influence food choices. Food taste is not only the taste of the food but also the aroma, texture, and pleasure response to foods [36]. Preferences for certain tastes, such as salty tastes, can strongly affect eating habits and are highly associated with hypertension [39].
The attribute and attribute levels were carefully selected after several extensive discussions among a multi-disciplinary team of experts, consisting of health economists, epidemiologists, physicians, and public health experts. To ensure theoretical validity and cultural appropriateness, the research team pre-tested each of the DCE choice sets and the symbols representing the attributes with college students and staff at Chiang Mai University. In this study, four food attributes each with two levels were selected: convenience (preparing food at home and buying ready-to-eat food), price (reasonable price and cheaper price), taste (favorite taste and okay taste), and the amount of salt (low and high). The levels of these attributes were chosen to be qualitative as subjects may have a hard time quantifying exact values for some of these attributes, such as the amount of salt in milligrams or a taste test scale. The four attributes, levels, and symbols used in the DCE are presented in Figure 2.
FIGURE 2
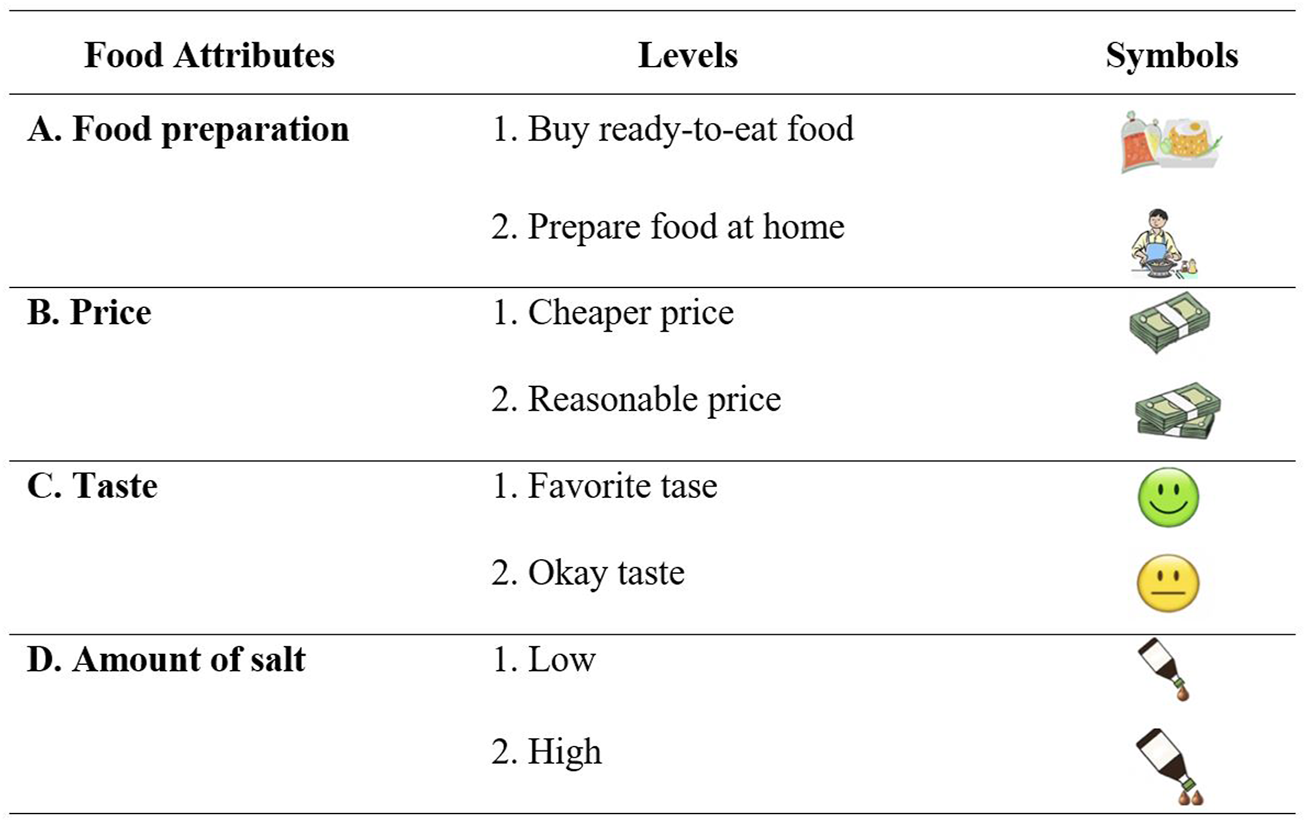
Food attributes for Discrete Choice Experiment (Chiang Mai, Thailand, 2019).
Furthermore, several nutritional values could also influence an individual’s food choice and are associated with hypertension, e.g., saturated fat, trans fat, sugar, and salt. The amount of salt was specifically selected as an attribute because it has been estimated that dietary sodium consumption in Thai adults is nearly twice as high as recommended levels [40] and significantly elevated in rural northern Thailand [5, 6]. Specifically, sodium sources are predominately from the use of flavor enhancers such as fish sauce, soybean sauce, monosodium glutamate, and table salt added during consumption [6, 41] or cooking preparation [6, 10].
Data Collection
The target population for this study was rural northern Thailand, particularly Chiang Mai province with the largest population in the northern region. Within Chiang Mai province, Bang Klang Subdistrict was chosen as it is located in the rural area of San Pa Tong District, not too far from the Muang District (City of Chiang Mai), where the research team was stationed, it has a well-established community network, which is beneficial to obtain representative data and a reasonable sample size, and lastly, hypertension is the main health concern in this area as it is the leading cause of illness, followed by respiratory tract infections, diabetes mellitus, kidney disease, and musculoskeletal diseases. In the Bang Klang Subdistrict, five of the largest villages out of eleven were selected. Subjects were residents from these villages and over the age of 18. A minimum sample size of 356 subjects was calculated using Taro Yamane’s formula [42] [n = N/(1+Ne2), n = 3,257/(1+ (3,257 x 0.052)], where n is the sample size; N is the largest sample population; e is the margin of error. In total, 407 Thai adults were sampled from the five villages: 1) Sieo Village (N = 1462), 2) Tong Fai Village (N = 722), 3) Phra Chao Thong Thip Village (N = 429), 4) Ton Kok Village (N = 390), and 5) Pa Sak Village (N = 254), of which 403 completed the survey questionnaire and received an incentive gift valued $1.00 (30 THB).
The paper-based survey questionnaire was created in the Thai language and pilot tested by volunteer college students prior to data collection. The English version of the survey questionnaire was created using the repeated forward-backward translation procedure to preserve the original meaning [43]. In June 2019, the research team conducted 20-min face-to-face, one-on-one interviews with each of the subjects in the Thai language at each of the participating village community centers. Before the DCE questions were presented to the subjects, the interviewer carefully explained the symbols in this study. Following this, the interviewer performed an assessment to ensure subjects clearly understood the meaning of the symbols before proceeding to the DCE questions. For every DCE question, the interviewer described the various combinations of attributes and the opt-out option to the subject until they had no further questions before asking them to select one option. The research study was reviewed and approved by an affiliated Institutional Review Board (#HSR-18-19-712, 21 June 2019). All subjects provided informed consent.
Hypertension Measurement
Trained health care professionals collected each subject’s blood pressure (BP) twice, once before and another 5 minutes after the interview. The average systolic and diastolic BPs of each subject were calculated. The BP measurement criteria used in this study were the 2017 AHA/ACC guideline [44] for the prevention, detection, evaluation, and management of high blood pressure in adults. The criteria recommend a blood pressure management goal of less than or equal to 130/80, rather than 140/90, for adults with diagnosed hypertension or heart disease. This recommendation promotes healthy blood pressure among Asian populations, in which high BP can contribute to more adverse cardiovascular health outcomes than in Western populations [45]. Hypertension at the time of measurement was considered if a subject’s average systolic BP was greater than or equal to 130 mmHg or their average diastolic BP was greater than or equal to 80 mmHg; otherwise, subjects have normotension. In Table 1, approximately 58% of the subjects (n = 234) have hypertension, and 42% have normotension.
TABLE 1
| Characteristics | Overall | Normotensive Groupa | Hypertensive Groupb | p-value |
|---|---|---|---|---|
| Age (mean ± s.d.) | 59.64 ± 11.93 | 59.18 ± 12.12 | 59.97 ± 11.78 | 0.003c** |
| Gender n (%) | ||||
| Male | 108 (26.80%) | 36 (21.30%) | 72 (30.77%) | <0.001d*** |
| Female | 295 (73.20%) | 133 (78.70%) | 162 (69.23%) | |
| Elderly (y ≥ 60) n (%) | ||||
| years ≥60 | 222 (55.09%) | 89 (52.66%) | 133 (56.84%) | <0.001d*** |
| years <60 | 181(44.91%) | 80 (47.34%) | 101 (43.16%) | |
| Education n (%) | ||||
| Junior high school degree or above | 111 (27.54%) | 45 (26.63%) | 66 (28.21%) | 0.118d |
| Less than junior high school degree | 292 (72.46%) | 124 (73.37%) | 168 (71.79%) | |
| Individual Monthly Income | ||||
| <5,000 Thai Baths (<150 US Dollars) | 242 (60.05%) | 103 (60.95%) | 139 (59.40%) | <0.001d*** |
| ≥5,000 That Baths (≥150 US Dollars) | 161 (39.95%) | 66 (39.05%) | 95 (40.60%) | |
| Occupation | ||||
| Daily Labor | 154 (38.21%) | 65 (38.46%) | 89 (38.03%) | <0.001d*** |
| Business | 83 (20.6%) | 29 (17.16%) | 54 (23.08%) | |
| Government officer | 13 (3.23%) | 10 (5.92%) | 3 (1.28%) | |
| Private employee | 1 (0.25%) | 0 (0.00%) | 1 (0.43%) | |
| Farmer | 40 (9.93%) | 17 (10.06%) | 23 (9.83%) | |
| Unemployed | 107 (26.55%) | 44 (26.04%) | 63 (26.92%) | |
| Other | 5 (1.24%) | 4 (2.37%) | 1 (0.43%) | |
| High Blood Pressure in Family History n (%) | ||||
| No | 217 (53.85%) | 96 (56.80%) | 121 (51.71%) | 0.001d*** |
| Yes | 186 (46.15%) | 73 (43.20%) | 113 (48.29%) | |
| Total observation | 403 | 169 (41.93%) | 234 (58.07%) | |
Sociodemographic characteristics of subjects associated with hypertension (Chiang Mai, Thailand, 2019).
Normotensive Group (NG): Systolic BP <130 and Diastolic BP <80.
Hypertensive Group (HG): Systolic BP ≥130 or Diastolic BP ≥80.
Two-Samples t-test for differences between normotensive and hypertensive groups.
Chi-Square test for differences between normotensive and hypertensive groups.
*Statistically significant for p ≤ 0.05; ** statistically significant for p ≤ 0.01; *** statistically significant for p ≤ 0.001.
Statistical Analysis
The results from the DCE were analyzed separately in normotensive and hypertensive groups using a Mixed Logit (MXL) model. Based on the BFD, four individual attributes (food preparation, price, taste, and amount of salt) and five interactions between two attributes (food preparation X taste, food preparation X amount of salt, price X taste, price X amount of salt, and taste X amount of salt) were estimated in the MXL model. Furthermore, an alternative specific constant (ASC) variable for the none option was included as a fixed effect in the model to examine the opt-out effect.
The relative importance of each attribute was estimated to compare the explanatory power of each attribute on food choices. The partial log-likelihood method was used to calculate the relative importance based on how much each attribute contributed to the overall log-likelihood in the choice model [46]. The reduced model log-likelihood values were calculated when one attribute and any of its estimable interactions were excluded from the full model. Then, the partial effect of each attribute was calculated as the change in the reduced model log-likelihood from the full model log-likelihood. The relative effect was calculated as the percent change in the log likelihood. Thus, attributes that subjects consider more important in their choices will contribute more to the relative effect and have higher relative importance. It is noted that the statistical analysis used in this study can be found in greater detail in our previous study [30].
Significance was measured at p-value ≤ 0.05; however, there were a couple of variables that were marginally significant with p-value slightly greater than 0.05 (0.05 < p ≤ 0.1) that are worth mentioning. The individual attributes in the DCE were coded using effects coding to ensure that the systematic observed utility effects are uncorrelated with the intercept [47].
Results
The sociodemographic characteristics of the subjects are presented in Table 1. The average age of the subjects was approximately 60 years old. About 73% were female, and 27% were male. Most subjects were elderly (55%), had an education level less than junior high school (72.46%), earned less than 5,000 Thai Bahts per month (∼<$150/month) (60.5%), and were daily laborers or unemployed (64.76%). More than half of the subjects had hypertension (58.07%) and reported having at least one family member with hypertension (53.85%). Among the sociodemographic characteristics, there were statistically significant differences between the NG and HG, except for the education characteristic.
The results from the Mixed Logit models for the DCE are presented in Table 2. Subjects in both the NG and HG were less likely to purchase ready-to-eat food (NG: = –1.981; p < 0.001; HG: = –1.807; p < 0.001). In other words, they preferred to prepare food at home. Furthermore, subjects in both the NG and HG were less likely to purchase food high in salt (NG: = –1.931; p < 0.001; HG: = –2.096; p < 0.001).
TABLE 2
| Food attributes | Normotensive Groupa | Hypertensive Groupb | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Estimate ( | Std.error | p-value | Estimate ( | Std.error | p-value | ||||
| Individual effects | |||||||||
| Food preparation | Buy ready-to-eat food | −1.981 | *** | 0.345 | <0.001 | −1.807 | *** | 0.256 | <0.001 |
| Prepare food at home (References) | |||||||||
| Price | Cheaper price | −0.066 | 0.109 | 0.545 | −0.092 | 0.095 | 0.336 | ||
| Reasonable price (References) | |||||||||
| Taste | My favorite taste | −0.152 | 0.115 | 0.302 | 0.118 | 0.098 | 0.255 | ||
| Okay taste (References) | |||||||||
| Amount of salt | High salt | −1.931 | *** | 0.269 | <0.001 | −2.096 | *** | 0.251 | <0.001 |
| Low salt (References) | |||||||||
| Interaction effects between attributes | |||||||||
| Ready-to-eat food X Favorite taste | 0.078 | 0.114 | 0.491 | −0.171 | 0.100 | 0.089 | |||
| Ready-to-eat food X High salt | 0.076 | 0.126 | 0.545 | 0.109 | 0.107 | 0.306 | |||
| Cheaper price X Favorite taste | −0.128 | 0.083 | 0.121 | −0.161 | ** | 0.081 | 0.047 | ||
| Cheaper price X High salt | 0.215 | 0.080 | 0.788 | 0.157 | ** | 0.078 | 0.043 | ||
| Favorite taste X High salt | −0.251 | ** | 0.123 | 0.040 | 0.052 | 0.104 | 0.619 | ||
| ASC for opt-out (none option) | −1.016 | ** | 0.499 | 0.042 | −0.620 | ** | 0.310 | 0.050 | |
| N | 169 | 234 | |||||||
| Log-likelihood | −440.86 | −564.85 | |||||||
Estimation of the mixed logit models (Chiang Mai, Thailand 2019).
Normotensive Group (NG): Systolic BP <130 and Diastolic BP <80.
Hypertensive Group (HG): Systolic BP ≥130 or Diastolic BP ≥80.
Statistically significant for p ≤ 0.05; ** statistically significant for p ≤ 0.01; *** statistically significant for p ≤ 0.001.
The interactions between attributes in the NG and HG varied and are presented in the bottom portion of Table 2. In the NG, the interaction between favorite taste and high salt had a significant negative impact on subjects’ food choices ( = –0.251; p = 0.040); NG subjects were less likely to purchase food high in salt despite their favorite taste. In the HG, two interactions between attributes had a significant negative impact on subjects’ food choices. HG subjects were less likely to purchase food that was cheaper priced and their favorite taste ( = –0.161; p < 0.047). In other words, they preferred food with a reasonable price and okay taste. HG subjects were less likely to purchase ready-to-eat food despite their favorite taste ( = –0.171; p < 0.089). Instead, they preferred to prepare food at home with okay taste. Moreover, in the HG, the interaction between cheaper price and high salt had a significant positive impact on subjects’ food choices; HG subjects were more likely to purchase cheaper food despite high salt ( = 0.157; p < 0.043). Hence, in foods that contain high salt, the subjects in the HG and NG made different trade-offs in their food choices (H1). Lastly, the estimate of the ASC variable for the none option indicated subjects in both the NG and HG groups were more likely to purchase food rather than opt out (NG: = –1.061; p < 0.042; HG: = –0.620; p < 0.05).
Table 3 presents the relative importance of the four attributes for the normotensive and hypertensive groups. The attribute, amount of salt, accounted for more than 50% of the log-likelihood in both the NG (50.55%) and HG (54.52%). Hence, the amount of salt significantly affected the subject’s food choices in both groups and thus had the highest relative importance in both NG and HG (H2). Further, the attribute, food preparation, added to 47.14% of the log-likelihood in the NG and 43.09% of the log-likelihood in the HG. The relative importance of the NG and HG differed in price and taste. Among the subjects in the HG, price had the third-highest relative importance (1.21%), and taste was the least relative important attribute (1.19%). However, taste (1.53%) and price (0.78%) were the third and fourth relative important attributes among subjects in the NG. Overall, subjects in the HG and NG had different food choices (H3).
TABLE 3
| Food attributes | Normotensive Group a | Hypertensive Group b | ||||||
|---|---|---|---|---|---|---|---|---|
| Log-likelihood | Partial effect | Relative effect (%) | Relative importance | Log-likelihood | Partial effect | Relative effect (%) | Relative importance | |
| Full model | −440.86 | −564.86 | ||||||
| Food Preparation | −694.91 | −254.05 | 47.14 | 2 | −907.53 | −342.68 | 43.09 | 2 |
| Price | −445.07 | −4.21 | 0.78 | 4 | −574.44 | −9.58 | 1.21 | 3 |
| Taste | −449.13 | −8.27 | 1.53 | 3 | −574.32 | −9.46 | 1.19 | 4 |
| Amount of salt | −731.28 | −272.42 | 50.55 | 1 | −998.46 | −433.61 | 54.52 | 1 |
Estimation of the relative importance of food attributes (Chiang Mai, Thailand, 2019).
Normotensive Group: Systolic BP <130 and Diastolic BP <80.
Hypertensive Group: Systolic BP ≥ 130 or Diastolic BP ≥80.
Discussion
This study used a DCE survey method to examine food choices associated with hypertension among people living in the rural northern region of Thailand. With the unique design of a DCE, the study quantified the relative importance of the food attributes and interaction effects between the food attributes. The amount of salt was considered the most important attribute in both normotensive and hypertensive groups, accounting for more than 50% of the relative effect. Both groups of subjects in our study were likely to purchase low-salt food, which may infer that they had similar attitudes, beliefs, and knowledge about salt reduction. Based on the TPB, individuals with a greater awareness of the negative consequences of salt consumption, stronger personal and social norms, and higher salt-related knowledge, had an increased likelihood of purchasing low-salt food [5]. Even though our study found normotensive and hypertensive individuals valued the amount of salt as the most important attribute and were willing to purchase low-salt food, it is worth noting that the willingness to purchase may not be translated to the consumption. Studies suggest that both in Thailand, as well as in other countries, individuals generally have a reasonable knowledge of salt and its adverse effects in addition to favorable attitudes toward low-salt food; most individuals are less likely to take action to reduce salt consumption, and their blood pressure was still uncontrolled [6, 48–50].
Notably, when analyzing the interaction between the amount of salt and taste attributes, foods high in salt could also be confounded with an individual’s favorite taste. However, the interaction between these two attributes was not significant in the hypertensive group. In the normotensive group, subjects instead were less likely to purchase foods high in salt despite their favorite taste. The findings from the latter group are interesting as previous studies [51, 52] found that consumers typically choose taste over health and are not willing to accept poor taste in exchange for healthier foods. This counterintuitive finding may be explained from the distinction between hedonic choices (i.e., enjoyable and pleasurable foods) and utilitarian choices (i.e., functional and practical foods) [41]. According to Kahn et al. [51], consumers may be more inclined to choose foods with less salt if they predominately perceive the foods as utilitarian products. Therefore, their purchase decision is dominated by health rather than immediate pleasure. Whereas, when analyzing the interaction between the amount of salt and price attributes, subjects in the hypertension group were more likely to purchase foods high in salt at a cheaper price. Thus, it is hard to determine if their purchase decision is based on immediate pleasure or economic factors.
Food preparation was considered the second most important attribute in both normotensive and hypertensive groups. Both groups preferred cooking or preparing food at home over purchased ready-to-eat food. It is noted that due to the labor-intensive nature of Thai cooking [53], a food preparation at home has been decreased within urban Thai households. Instead, the high pressure to work longer hours and hurried lifestyles in urban cities have promoted ready-to-eat food [17, 54]. However, recent data suggest that ready-to-eat food consumption is relatively low among individuals residing in rural areas and the northern region of Thailand [55]. Specifically, people living in rural northern Thailand reported cooking or preparing food at home at least once in the past 3 months (98.40%); on average, they cooked or prepared food at home almost every day [6].
Regarding the sociodemographic characteristics, most of the subjects were married females. This supports the traditional culture of women’s role in relation to cooking for their families in rural Thailand [56]. In fact, most subjects were daily laborers or unemployed, and thus, their schedules may be more flexible with more time to make home-cooked food. The primary source of sodium intake among Thais, like many other Southeast Asian countries, comes from condiments added while cooking at home [57]. In rural northern Thailand, the main seasoning ingredients used when cooking are salt, followed by 1-2 teaspoons of monosodium glutamate (MSG) and seasoning cubes [6, 58].
The taste attribute was ranked third in the normotensive group and ranked the least important by the hypertensive group. While this finding is surprising, it may be explained by the socioeconomic status of the study sample that most of the subjects had an education level less than junior high school and were classified as low-income. The study on factors affecting food choices of older adults [59] found that higher-income individuals rated a meal that has a very good taste to be more important than did low-income individuals. The more educated individuals tended to rate lower price foods more important than the less-educated individuals.
In rural Thailand, extended families are common in which three generations often live together [60], and thus dietary habits are likely to be shared within the family [61]. Cooking, eating, and sharing a combination of dishes among family members and relatives are typical practices among Thais [62], leading to unawareness of overconsumption of sodium. Therefore, public health educational programs may pivot to consider cultural sensitivity focusing on daily habits. Individualized salt-reduction intervention programs should be aimed at the family level, such as identifying the traditional high-salt food the family often cooks, giving advice for low-salt cooking ideas for their traditional food, and monitoring daily food consumption.
Limitations
There are some limitations to this study. The sample was small and lacking in demographic and socioeconomic diversity. A larger diverse sample could have provided more representation of the population. Furthermore, while DCEs closely reflect real-life decision-making in which people simultaneously make choices, each of which consists of several options, they are based on hypothetical choices as subjects do not actually choose the food, which may lead to hypothetical bias. As with any survey method, this limitation is common in DCE applications when choice tasks do not fully reflect reality in the characteristics of the choices [63]. In addition, the choice task of the DCE may become too cognitively challenging for subjects [64].
Moreover, since the interview was conducted at the village community center during midday, most of the sample were elderly females, as younger or male adults may have been at work during this time. This may have led to age-related factors (hearing, vision, memory loss) that could have affected the ability to obtain valid information [65], as well as age-related increases in blood pressure that could have influenced the proportion of hypertensive individuals in the sample. Future data collection should be gathered at various times throughout the day to obtain a more diverse range of ages and genders.
Conclusion
This study aimed to contribute to the gap in the literature on understanding food choices associated with hypertension and determine the attributes that influence the food choices of rural northern Thais. The use of a DCE quantified the relative importance of attributes and the interactions between the attributes for normotensive and hypertensive groups. The most and second most important attributes in both groups were the amount of salt and food preparation at home, respectively. The interactions between the attributes revealed that normotensive people are more attentive to the amount of salt in their food than their hypertensive counterparts. The findings revealed that people in the rural areas of Thailand are aware of the amount of salt in their food choices and prefer home-cooked meals. As eating habits are concentrated at home and foods are commonly shared within the family, this study suggests that intervention programs for this population may benefit from focusing their attention on embracing low-salt cultural foods and providing guidance on low-salt cooking, especially for households with hypertensive members. Local health agencies and village health volunteers can play an essential role in educating, guiding, and training people in rural communities on how to add flavor without additional salt or reduce high sodium seasonings without losing flavor when cooking.
Statements
Ethics statement
The studies involving human participants were reviewed and approved by the California State University Fullerton Review Board (#HSR-18-19-712, 21 June 2019). The patients/participants provided their written informed consent to participate in this study.
Author contributions
Conceptualization, PR, CM, and MW; data curation, PR and CM; methodology, PR and JJ; data analysis, PR, HN, CM, and JJ; writing original draft, PR, HN, and CM; writing-review and editing, PR, HN, CM, JJ, and MW; supervision, PR and MW. All authors have read, revised, and agreed to the published version of the manuscript.
Funding
This research was supported by grant MHRT 2T37MD001368 from the National Institute on Minority Health and Health Disparities, National Institutes of Health.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1.
Lawes CM Rodgers A Bennett DA Parag V Suh I Ueshima H et al Blood Pressure and Cardiovascular Disease in the Asia Pacific Region. J Hypertens (2003) 21(4):707–16. 10.1097/00004872-200304000-00013
2.
Castillo R . SSA 03-1 Prevalence and Management of Hypertension in Southeast Asia. J Hypertens (2016) 34:e4. 10.1097/01.hjh.0000499881.98439.59
3.
World Health Organization. Hypertension Care in Thailand: Best Practices and Challenges (2019). https://apps.who.int/iris/handle/10665/330488 (Accessed October 5, 2021).
4.
Aung MN Yuasa M Moolphate S Nedsuwan S Yokokawa H Kitajima T et al Reducing Salt Intake for Prevention of Cardiovascular Diseases in High-Risk Patients by Advanced Health Education Intervention (RESIP-CVD Study), Northern Thailand: Study Protocol for a Cluster Randomized Trial. Trials (2012) 13:158. 10.1186/1745-6215-13-158
5.
Mørk T Lähteenmäki L Grunert KG . Determinants of Intention to Reduce Salt Intake and Willingness to purchase Salt-Reduced Food Products: Evidence from a Web Survey. Appetite (2019) 139:110–8. 10.1016/J.APPET.2019.04.018
6.
Rusmevichientong P Morales C Castorena G Sapbamrer R Seesen M Siviroj P . Dietary Salt-Related Determinants of Hypertension in Rural Northern Thailand. Ijerph (2021) 18(2):377. 10.3390/ijerph18020377
7.
Chailimpamontree W Kantachuvesiri S Aekplakorn W Lappichetpaiboon R Sripaiboonkij Thokanit N Vathesatogkit P et al Estimated Dietary Sodium Intake in Thailand: A Nationwide Population Survey with 24‐hour Urine Collections. J Clin Hypertens (2021) 23(4):744–54. 10.1111/jch.14147
8.
Meelab S Bunupuradah I Suttiruang J Sakulrojanawong S Thongkua N Chantawiboonchai C et al Prevalence and Associated Factors of Uncontrolled Blood Pressure Among Hypertensive Patients in the Rural Communities in the central Areas in Thailand: A Cross-Sectional Study. PLoS One (2019) 14(2):e0212572. 10.1371/journal.pone.0212572
9.
World Health Organization. Reducing Cardiovascular Disease (Hypertension and Sodium) (2021). https://www.who.int/thailand/activities/reducing-cardiovascular-disease (Accessed October 5, 2021).
10.
Pavadhgul P Sunthonwaraluk S Srisorachatr S Temcharoen P . Dietary Sodium Intake by Semi-quantitative Food Frequency Questionnaire Among Undergraduate Students of Mahidol University. J Med Assoc Thai (2009) 92 Suppl 7:S75–82.
11.
Nielsen. We Are what We Eat: Healthy Eating Trends Around the World. New York: The Nielsen Company (2015).
12.
Nielsen. What’s in Our Food and on Our Mind: Ingredient and Dining-Out Trends Around the World. New York: The Nielsen Company (2016).
13.
Kanchanachitra M Chamchan C Kanchanachitra C Suttikasem K Gunn L Vlaev I . Nudge Interventions to Reduce Fish Sauce Consumption in Thailand. PLOS ONE (2020) 15(9):e0238642. 10.1371/journal.pone.0238642
14.
Grillo A Salvi L Coruzzi P Salvi P Parati G . Sodium Intake and Hypertension. Nutrients (2019) 11(9):1970. 10.3390/nu11091970
15.
Elijovich F Weinberger MH Anderson CAM Appel LJ Bursztyn M Cook NR et al Salt Sensitivity of Blood Pressure. Hypertension (2016) 68:e7–e46. 10.1161/HYP.0000000000000047
16.
Patience S . Understanding the Relationship between Salt Intake and Hypertension. Nurs Stand (2013) 27(18):45–7. 10.7748/ns2013.01.27.18.45.c9487
17.
Chalermsri C Herzig van Wees S Ziaei S Ekström E-C Muangpaisan W Rahman SM . Exploring the Experience and Determinants of the Food Choices and Eating Practices of Elderly Thai People: A Qualitative Study. Nutrients (2020) 12(11):3497. 10.3390/nu12113497
18.
Bazzano LA Green T Harrison TN Reynolds K . Dietary Approaches to Prevent Hypertension. Curr Hypertens Rep (2013) 15(6):694–702. 10.1007/s11906-013-0390-z
19.
Ajzen I . The Theory of Planned Behavior. Organizational Behav Hum Decis Process (1991) 50(2):179–211. 10.1016/0749-5978(91)90020-T
20.
McDermott MS Oliver M Svenson A Simnadis T Beck EJ Coltman T et al The Theory of Planned Behaviour and Discrete Food Choices: a Systematic Review and Meta-Analysis. Int J Behav Nutr Phys Act (2015) 12(12):162. 10.1186/s12966-015-0324-z
21.
Garg V Shivashankar R Kondal D Ghosh S Khandelwal S Gupta R et al Knowledge, Attitudes and Practices Related to Dietary Salt Intake Among Adults in North India. Public Health Nutr (2019) 22:1606–14. 10.1017/S1368980018003518
22.
Ghimire K Adhikari TB Rijal A Kallestrup P Henry ME Neupane D . Knowledge, Attitudes, and Practices Related to Salt Consumption in Nepal: Findings from the Community‐based Management of Non‐communicable Diseases Project in Nepal (COBIN). J Clin Hypertens (2019) 21:739–48. 10.1111/jch.13544
23.
Zhang J Xu A-q. Ma J-x. Shi X-m. Guo X-l. Engelgau M et al Dietary Sodium Intake: Knowledge, Attitudes and Practices in Shandong Province, China, 2011. PLoS ONE (2013) 8:e58973. 10.1371/journal.pone.0058973
24.
Blake CE Frongillo EA Warren AM Constantinides SV Rampalli KK Bhandari S . Elaborating the Science of Food Choice for Rapidly Changing Food Systems in Low-And Middle-Income Countries. Glob Food Security (2021) 28:100503. 10.1016/j.gfs.2021.100503
25.
Mangham LJ Hanson K McPake B . How to Do (Or Not to Do) … Designing a Discrete Choice experiment for Application in a Low-Income Country Designing a Discrete Choice experiment for Application in a Low-Income Country. Health Policy Plan (2009) 24(2):151–8. 10.1093/heapol/czn047
26.
Veldwijk J Lambooij MS de Bekker-Grob EW Smit HA de Wit GA . The Effect of Including an Opt-Out Option in Discrete Choice Experiments. PLoS One (2014) 9(11):e111805. 10.1371/journal.pone.0111805
27.
Gong Y Li J Xie J Tan Y . Relationship between Types of Food Choice Motives and Well‐being Among Young and Middle‐aged Chinese Adults. Int J Consum Stud (2020) 44(4):369–78. 10.1111/ijcs.12573
28.
Vorage L Wiseman N Graca J Harris N . The Association of Demographic Characteristics and Food Choice Motives with the Consumption of Functional Foods in Emerging Adults. Nutrients (2020) 12(9):2582. 10.3389/ijph.2021.59102710.3390/nu12092582
29.
de Bekker-Grob EW Ryan M Gerard K . Discrete Choice Experiments in Health Economics: A Review of the Literature. Health Econ (2012) 21(2):145–72. 10.1002/hec.1697
30.
Rusmevichientong P Jaynes J Chandler L . Understanding Influencing Attributes of Adolescent Snack Choices: Evidence from a Discrete Choice experiment. Food Qual Preference (2021) 92:104171. 10.1016/j.foodqual.2020.104171
31.
Rusmevichientong P Jaynes J Kazemi S . Which Snack Factors and Nutritional Ingredients Influence College Students' Snack Choices? Evidence from Discrete Choice Experiments. J Am Coll Health (2020) 68(2):192–9. 10.1080/07448481.2018.1538149
32.
Jaynes J Wong WK Xu H . Using Blocked Fractional Factorial Designs to Construct Discrete Choice Experiments for Healthcare Studies. Statist Med (2016) 35(15):2543–60. 10.1002/sim.6882
33.
Wu CFJ Hamada MS . Experiments: Planning, Analysis, and Optimization. New Jersey: John Wiley & Sons (2009).
34.
Dhar R Simonson I . The Effect of Forced Choice on Choice. J Marketing Res (2003) 40(2):146–60. 10.1509/jmkr.40.2.146.19229
35.
Kelly B Halford JCG Boyland EJ Chapman K Bautista-Castaño I Berg C et al Television Food Advertising to Children: A Global Perspective. Am J Public Health (2010) 100(9):1730–6. 10.2105/AJPH.2009.179267
36.
Drewnowski A Monsivais P . Taste, Cost, Convenience, and Food Choices. In: MarriotBPBirtDFStallingsVAYatesAA, editors. Present Knowledge in Nutrition. Cambridge, MA: Academic Press (2020). p. 185–200. 10.1016/B978-0-12-818460-8.00010-1
37.
Aggarwal A Rehm CD Monsivais P Drewnowski A . Importance of Taste, Nutrition, Cost and Convenience in Relation to Diet Quality: Evidence of Nutrition Resilience Among US Adults Using National Health and Nutrition Examination Survey (NHANES) 2007-2010. Prev Med (2016) 90:184–92. 10.1016/j.ypmed.2016.06.030
38.
French SA Tangney CC Crane MM Wang Y Appelhans BM . Nutrition Quality of Food Purchases Varies by Household Income: the SHoPPER Study. BMC Public Health (2019) 19(1):1–7. 10.1186/s12889-019-6546-2
39.
Villela PTM de-Oliveira EB Villela PTM Bonardi JMT Bertani RF Moriguti JC et al Salt Preference Is Linked to Hypertension and Not to Aging. Arq Bras Cardiol (2019) 113(3):392–9. 10.5935/abc.20190157
40.
Chailimpamontree W Kantachuvesiri S Aekplakorn W Lappichetpaiboon R Sripaiboonkij Thokanit N Vathesatogkit P et al Estimated Dietary Sodium Intake in Thailand: A Nationwide Population Survey with 24‐hour Urine Collections. J Clin Hypertens (2021) 23(4):744–54. 10.1111/jch.14147
41.
Satheannoppakao W Kasemsup R Inthawong R Chariyalertsak S Sangthong R Taneepanichskul S et al Sodium Intake and Socio-Demographic Determinants of the Non-compliance with Daily Sodium Intake Recommendations: Thai NHES IV. J Med Assoc Thai (2013) 96 Suppl 5(12):S161–70.
42.
Yamane T . Statistics: An Introduction Analysis. New York: Harper & Row (1973).
43.
World Health Organization . Management of Substance Abuse: Process of Translation and Adaptation of Instruments (2020).
44.
Whelton PK Carey RM Aronow WS Casey DE Jr Collins KJ Dennison Himmelfarb C et al 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol (20172018) 71:2199–269. 10.1016/j.jacc.2017.11.005
45.
Kario K Wang J-G . Could 130/80 Mm Hg Be Adopted as the Diagnostic Threshold and Management Goal of Hypertension in Consideration of the Characteristics of Asian Populations?Hypertension (2018) 71(6):979–84. 10.1161/HYPERTENSIONAHA.118.11203
46.
Crouch GI Louviere JJ . The Determinants of Convention Site Selection: A Logistic Choice Model from Experimental Data. J Trav Res (2004) 43(2):118–30. 10.1177/0047287504268233
47.
Louviere JJ Hensher DA Swait JD . Stated Choice Methods: Analysis and Applications. Cambridge: Cambridge University Press (2000).
48.
Buranakitjaroen P Phoojaroenchanachai M . The Prevalence of High Sodium Intake Among Hypertensive Patients at Hypertension Clinic, Siriraj Hospital. J Med Assoc Thai (2013) 96 Suppl 2:S1–8.
49.
Shim JS Heo JE Kim HC . Factors Associated with Dietary Adherence to the Guidelines for Prevention and Treatment of Hypertension Among Korean Adults with and without Hypertension. Clin Hypertens (2020) 26:5–11. 10.1186/s40885-020-00138-y
50.
Bagale A . Awareness of Hypertensive Patients about Disease, Self-Care and Complication. Saudi J Med Pharm Sci (2016) 2:65–8.
51.
Kahn U Dahr R Wertenbroch K . A Behavioral Decision Theory Perspective on Hedonic and. Utilitarian Choice. In: RatneshwarSMickDG, editors. Consumption: Frontiers of Research on Consumer Motives, Goals, and Desires. Abingdon, Oxon: Routledge (2004).
52.
Verbeke W . Functional Foods: Consumer Willingness to Compromise on Taste for Health?Food Qual Preference (2006)) 17(1-2):126–31. 10.1016/j.foodqual.2005.03.003
53.
Yasmeen G . "Plastic-bag Housewives" and Postmodern Restaurants?: Public and Private in Bangkok's Foodscape. Urban Geogr (1996) 17(6):526–44. 10.2747/0272-3638.17.6.526
54.
Vinijjakul P Kosalwat W . Food and Nutrition in Review and Revision of Strategic Plan for Health Research in Thailand. In: WibulpolprasertS, editor. Thailand Health Profile 2001–2004. Bangkok, Thailand: Printing Press of the Express Transportation Organization of Thailand (2003). p. 124.
55.
NHES Office, Health System Research Institute. Report of the Food Consumption Survey Among the Thai Population: The Thailand National Health Examination Survey V, 2012–2013. Nonthaburi, Thailand: The Graphico System Ltd (2014).
56.
Coyle S Kwong J . Women's Work and Social Reproduction in Thailand. J Contemp Asia (2000) 30(4):92–506. 10.1080/00472330080000471
57.
Amarra MS Khor GL . Sodium Consumption in Southeast Asia: An Updated Review of Intake Levels and Dietary Sources in Six Countries. In: BendichADeckelbaumRJ, editors. Preventive Nutrition: The Comprehensive Guide for Health Professionals. New York, NY: Springer International Publishing (2015). p. 765–92. 10.1007/978-3-319-22431-2_36
58.
Theingburanathum P Thiengburanathum P . Capitalistic Transition in Food System and Food Consumption in Mae Cham District, Chiang Mai, Thailand. ajarcde (2019) 3(1):41–4. 10.29165/ajarcde.v3i1.23
59.
Kamphuis CB de Bekker-Grob EW van Lenthe FJ . Factors Affecting Food Choices of Older Adults from High and Low Socioeconomic Groups: a Discrete Choice experiment. Am J Clin Nutr (2015) 101(4):768–74. 10.3945/ajcn.114.096776
60.
Tapanya S . Attributions and Attitudes of Mothers and Fathers in Thailand. Parenting (2011) 11(2-3):190–8. 10.1080/15295192.2011.585566
61.
Yokokawa H Yuasa M Nedsuwan S Moolphate S Fukuda H Kitajima T et al Daily Salt Intake Estimated by Overnight Urine Collections Indicates a High Cardiovascular Disease Risk in Thailand. Asia Pac J Clin Nutr (2016) 25(1):39–45. 10.3316/ielapa.9082310479885110.6133/apjcn.2016.25.1.22
62.
Phimpraphai W Tangkawattana S Kasemsuwan S Sripa B . Social Influence in Liver Fluke Transmission. Adv Parasitol (2018) 101:97–124. 10.1016/bs.apar.2018.05.004
63.
Quaife M Terris-Prestholt F Di Tanna GL Vickerman P . How Well Do Discrete Choice Experiments Predict Health Choices? A Systematic Review and Meta-Analysis of External Validity. Eur J Health Econ (2018) 19(8):1053–66. 10.1007/s10198-018-0954-6
64.
Buttorff C Trujillo AJ Diez-Canseco F Bernabe-Ortiz A Miranda JJ . Evaluating Consumer Preferences for Healthy Eating from Community Kitchens in Low-Income Urban Areas: A Discrete Choice experiment of Comedores Populares in Peru. Soc Sci Med (2015) 140:1–8. 10.1016/j.socscimed.2015.06.033
65.
Eysteinsdottir T Thorsdottir I Gunnarsdottir I Steingrimsdottir L . Assessing Validity of a Short Food Frequency Questionnaire on Present Dietary Intake of Elderly Icelanders. Nutr J (2012) 11(1):1–8. 10.1186/1475-2891-11-12
Summary
Keywords
hypertension, food choices, rural Thailand, discrete choice experiment (DCE), salt
Citation
Rusmevichientong P, Nguyen H, Morales C, Jaynes J and Wood MM (2022) Food Choices and Hypertension Among Rural Thais: Evidence From a Discrete Choice Experiment. Int J Public Health 67:1604850. doi: 10.3389/ijph.2022.1604850
Received
17 February 2022
Accepted
15 June 2022
Published
15 July 2022
Volume
67 - 2022
Edited by
L. Suzanne Suggs, University of Italian Switzerland, Switzerland
Reviewed by
Derya Dikmen, Hacettepe University, Turkey
Sedef Akgungor, Dokuz Eylul University, Turkey
Updates
Copyright
© 2022 Rusmevichientong, Nguyen, Morales, Jaynes and Wood.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Pimbucha Rusmevichientong, prusmevichientong@fullerton.edu
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.