- 1Department of General Medicine and Geriatrics, Shenzhen Qianhai Shekou Free Trade Zone Hospital, Shenzhen, China
- 2Department of Pediatrics, Shenzhen Qianhai Shekou Free Trade Zone Hospital, Shenzhen, China
Objective: To investigate the status and influential factors of depression, anxiety, and insomnia among people in quarantine during COVID-19.
Methods: Data was collected from August 2020 to November 2021 through an online survey of 1,360 people in a quarantined hotel. The Patient Health Questionnaire-9 (PHQ-9), Generalized Anxiety Disorder-7 (GAD-7), and Insomnia Severity Index (ISI) were used to assess different mental symptoms.
Results: 19.9% (n = 270), 17.6% (n = 239) and 7.1% (n = 97) of participants had depression, anxiety and insomnia. Married (OR = 0.641, 95% CI = 0.450–0.915) was a protective factor for depression. Chronic disease (OR = 2.579, 95% CI = 1.416–4.698) was a risk factor for insomnia. No psychiatric medication history was a protective factor for depression (OR = 0.227, 95% CI = 0.068–0.757) and insomnia (OR = 0.240, 95%CI = 0.078–0.736). Female, history of mental illness, low moods at check-in, and partial/cannot understand the quarantine policies were risk factors for anxiety, depression, and insomnia.
Conclusion: People in quarantine had problems with depression, anxiety, and insomnia. Female, low moods at check-in, and partial/cannot understand the quarantine policies had significant impacts. It is necessary to help quarantined people understand quarantine policies, reduce negative emotions and improve sleep quality.
Introduction
COVID-19 is the infectious disease of the world’s pandemic. As of 16 December 2021, the virus spread rapidly, leading to 271,376,643 confirmed infections and 5,324,969 deaths worldwide [1]. Quarantine is one of the effective ways to control the spread of COVID-19. WHO issued guidelines for quarantine measures to strengthen epidemic prevention and control. Mandatory mass quarantines inevitably have a marked psychological impact on the public, with the media reporting the number of new cases every day, resulting in panic and psychological stress [2]. Past experiences of quarantine [3], from SARS to Ebola, have shown that it can take a toll on a person’s mental health, including separation from loved ones, losing freedom, enduring illness, and feeling bored are among the most common problems. Anxiety and mood disorders are also prevalent [4]. A US study [5] reported an increased incidence of first psychiatric diagnosis (HR = 1.6–2.1) in COVID-19 patients within 14–90 days of COVID-19 diagnosis. Studies [6] linked quarantine to negative emotions and increased psychological stress, PTSD, and depression. A meta-analysis [7] of COVID-19’s effects on mental health among 33,062 participants noted that depression prevalence reached 22.8%, anxiety prevalence reached 23.2%, and insomnia prevalence reached 38.9%. The lack of data is a global problem. Only one study [8] conducted in the Czech Republic used structured diagnostic interviews (MINI) to assess prevalence in repeated cross-sectional surveys before and during the pandemic (2017 and 2020). A two—to three-fold increase in point prevalence of anxiety and depression has been reported. The Chinese government instituted an unprecedented nationwide public health home quarantine measure to control the spread of the pandemic. Some unique features of China’s COVID-19 epidemic pattern and its management policies contribute to the public mental health crisis [9]. Many people returning or leaving China were forced to stay in quarantined hotels due to local quarantine policies in cities across China. COVID-19 patients and healthy citizens unaffected have suffered from stress and anxiety caused by these massive quarantine policies. Unfavourable news can cause mental panic and negative emotions in people who are isolated for a long time [10]. In terms of policy, recognizing the epidemic’s impact on public mental health and life satisfaction and illuminating issues related to public mental health is crucial in large-scale quarantine measures to prevent infection in countries with high levels of COVID-19 [6].
Methods
Subjects
The subjects were in a quarantined hotel in Shenzhen from August 2020 to November 2021, all of whom were inbound from Hong Kong. After finishing the first nucleic acid testing at the customs, they would stay 14 days in the quarantine hotel. Inclusion criteria: 1) Occupancy date from August 2020 to November 2021; 2) Good cognitive ability, good reading comprehension ability, and able to complete the answers normally; 3) Complete the questionnaire survey on the day of check-in; 4) Informed consent to the questionnaire survey and voluntary participation. Exclusion criteria: 1) infants and illiterate persons; 2) Unable to understand the questionnaire’s content or incapable of completing the questionnaire due to cognitive impairment.
Measures
The questionnaire was divided into two parts. The first part collected sociodemographic data, including gender, age, education, marital status, whether quarantine alone, history of physical illness, history of mental illness, history of psychiatric medication, moods at check-in, and attitude towards quarantine policies. Another part of the study focused on standard scales to measure depression, anxiety, and insomnia symptoms, such as PHQ-9, GAD-7, and ISI. There were nine questions on the PHQ-9 scale, and each question was scored 0–3 points, a total of 28 points. 0 to 4 points were for normal. In this paper, subjects were divided into 0 to 4 points for the normal group and >4 points for the depression group. There were seven questions on the GAD-7 scale, and each question was scored 0–3 points out of 21 points. 0 to 4 points were for normal people. This paper divided subjects into 0 to 4 points for the normal group and >4 points for the anxiety group. There were seven questions on the ISI scale, each graded on a scale of 0–4 points out of 28. 0–7 points for normal and 8–14 points for subclinical insomnia. In this paper, subjects were divided into 0–14 points for the normal group and >14 points for the insomnia group. An invalid questionnaire would be marked if the response time was less than 1 min or if there were more than 20% incomplete responses.
Statistical Analysis
The statistical analysis was performed using SPSS 20.0. Continuous variables were expressed as mean ± standard deviation. Continuous variables were expressed by mean ± standard deviation. Classified variable data were expressed by numerical value or percentage. To compare the count data between groups, we used the Chi-square test. Fisher’s exact test was adopted when the expected frequency of grouped variables was less than 5. The correlation of data was analyzed using Spearman correlation analysis. Multivariate analysis was performed by binary logistic regression. Odds ratios (OR) and 95% confidence intervals (95% CI) of independent variables were calculated. p < 0.05 was considered statistically significant.
Results
Characteristics of the Participants
A total of 1,360 valid questionnaires were collected for data analysis. 639 were female (47.0%), and 721 were male (53.0%). The average age was 41.82 ± 11.4 years old. 77.7% were quarantined alone. Most of them were well educated, married, had no history of chronic physical illness, mental illness, psychiatric medication history, good moods at check-in, and fully understood the quarantine policies, as shown in Table 1.
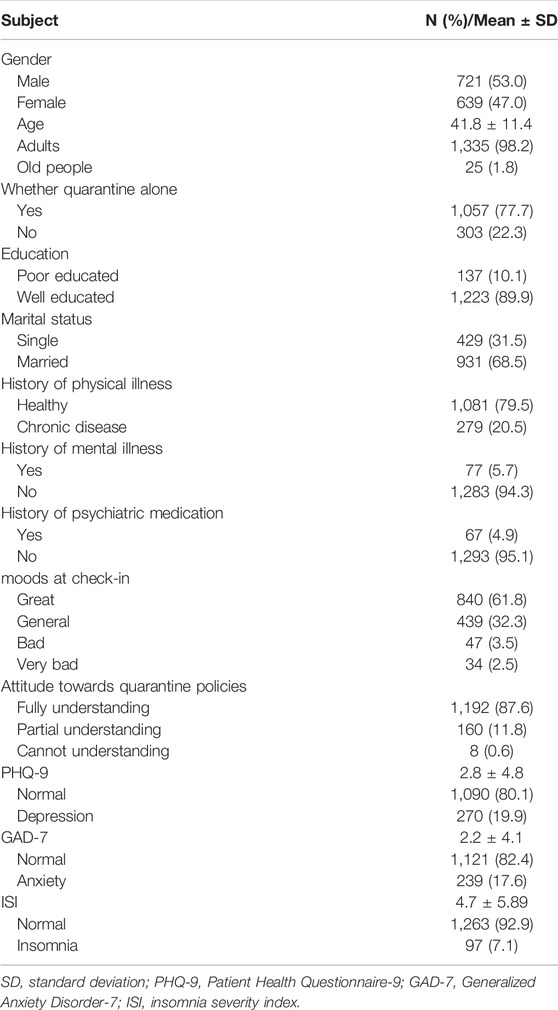
TABLE 1. Descriptive statistics outcomes of difference factors of depression, anxiety and insomnia symptoms among people in quarantine during COVID-19 epidemic study. China, 2020–2021.
Status of Depression, Anxiety, and Insomnia Among People in Quarantine
The mean PHQ-9 score was 2.8 ± 4.8. 270 (19.9%) of them were screened for depression. The average score of GAD-7 was 2.2 ± 4.1, and 239 (17.6%) of them were screened for anxiety. The average ISI score was 4.7 ± 5.9. Ninety-seven of them (7.1%) with insomnia were screened out, as shown in Table 1.
Difference Analysis of Depression, Anxiety, and Insomnia Among People in Quarantine
Age, education, and whether quarantine alone showed no significant difference in the risk of depression, anxiety, and insomnia among people in quarantine (p > 0.05). Gender, history of physical illness, history of mental illness, history of psychiatric medication, moods at check-in, and attitude towards quarantine policies had statistical significance in the risk of depression, anxiety, and insomnia (p < 0.05). Marital status had no difference in the risk of anxiety and insomnia (p > 0.05) but had statistical significance in the risk of depression (p < 0.05). See Table 2.
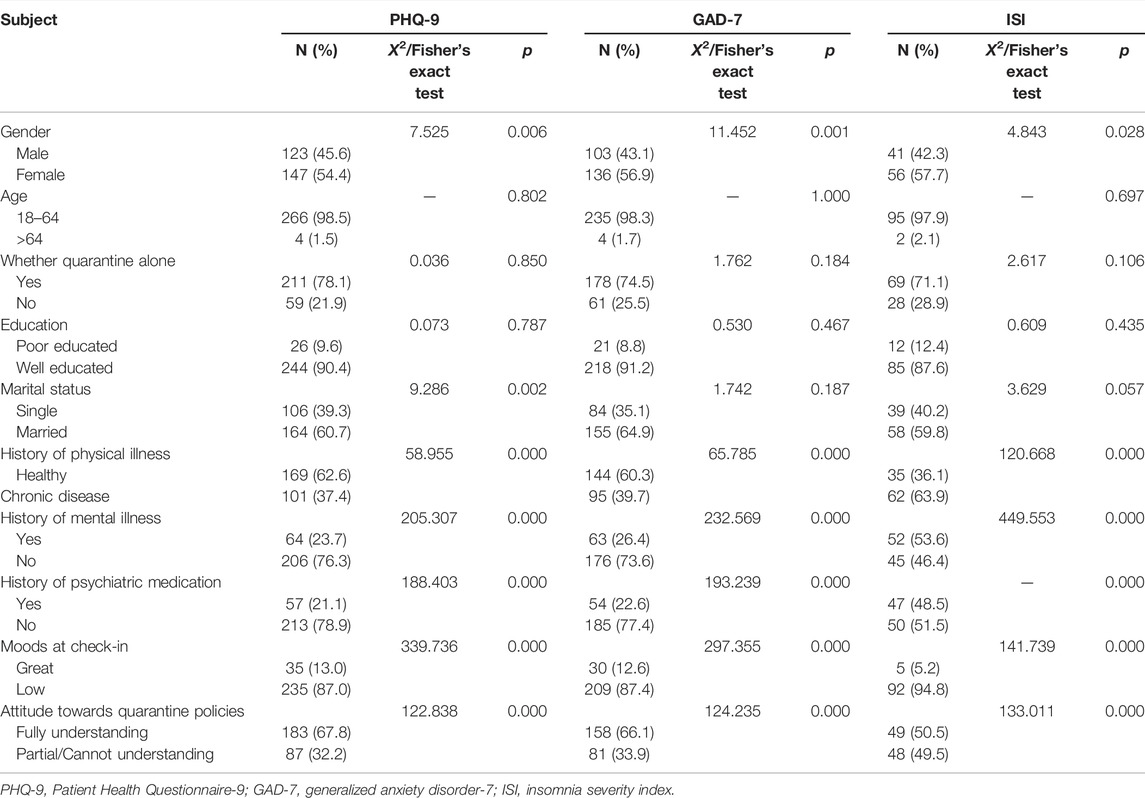
TABLE 2. Chi-square test or Fisher’s exact test of difference factors of depression, anxiety and insomnia symptoms among people in quarantine during COVID-19 epidemic study. China, 2020–2021.
Correlation Between PHQ-9, GAD-7, and ISI Scores Among People in Quarantine
Spearman correlation analysis showed that the PHQ-9 score was positively correlated with the GAD-7 score (r = 0.705, p < 0.0001). PHQ-9 score was positively correlated with the ISI score (r = 0.528, p < 0.0001). GAD-7 score was positively correlated with ISI score (r = 0.533, p < 0.0001).
Influential Factors of Depression, Anxiety, and Insomnia Among People in Quarantine
Multivariate logistic regression analysis showed that being married (OR = 0.614, 95% CI = 0.450–0.915) was a protective factor for depression. Chronic disease (OR = 2.579, 95% CI = 1.416–4.698) was a risk factor for insomnia. No psychiatric medication history was a protective factor for depression (OR = 0.227, 95% CI = 0.068–0.757) and insomnia (OR = 0.240, 95% CI = 0.078–0.736). Female, history of mental illness, low moods at check-in, and partial/cannot understand the quarantine policies were risk factors for anxiety, depression, and insomnia. See Tables 3–5.
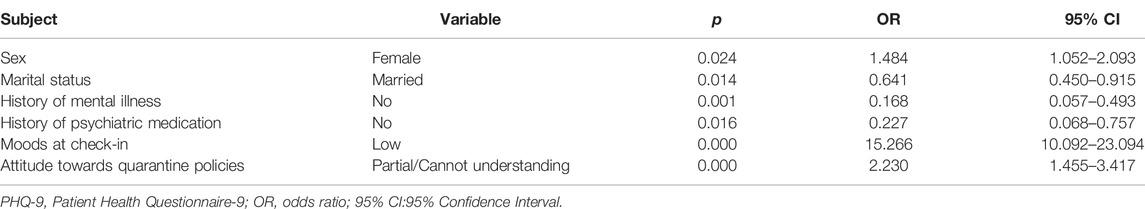
TABLE 3. Multivariate logistic regression analysis outcomes for influential factors of depression symptoms among people in quarantine during COVID-19 epidemic study. China, 2020–2021.
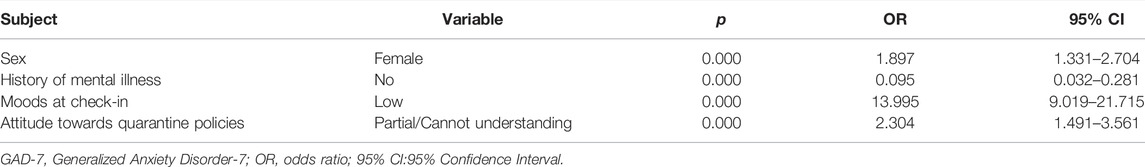
TABLE 4. Multivariate logistic regression analysis outcomes for influential factors of anxiety symptoms among people in quarantine during COVID-19 epidemic study. China, 2020–2021.
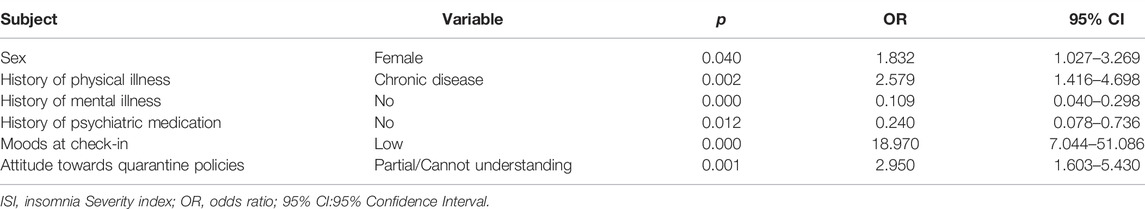
TABLE 5. Multivariate logistic regression analysis outcomes for influential factors of insomnia symptoms among people in quarantine during COVID-19 epidemic study. China, 2020–2021.
Discussion
There was no large-scale epidemiological data to show the central psychological problems of the current epidemic and the main psychological problems in different populations. While the neurological effects of COVID-19 are still unknown, adverse effects of COVID-19 on physical and mental health are well documented [6]. United Nations Secretary-General Antonio Guterres released a policy brief on COVID-19 and mental health [11]. COVID-19 was not only affecting people’s physical health. Bereavement, unemployment, isolation, and movement restrictions lead to tremendous stress and mental health problems. A meta-analysis [12] of 134,061 patients revealed that COVID-19 quarantine was associated with anxiety, depression, and psychological stress. Quarantine and mental health are moderated differently by different groups. The country of origin had no significant effect on quarantine and mental health. Another meta-analysis [13] of 189,159 sample sizes revealed a prevalence of depression at 15.97%, anxiety at 15.15%, insomnia at 23.87%, PTSD at 21.94%, and psychological distress at 13.29%. Many studies [14–20] have shown that the outbreak of highly infectious diseases would bring about related mental symptoms, indicating that COVID-19 is an extremely stressful life event and a leading cause of physical and mental disorders.
Depression, Anxiety, and Insomnia Were Positively Correlated
In COVID-19, the mental health study results varied significantly among countries [13]. A meta-analysis [21] indicates that depression, anxiety, and insomnia are prevalent among people in quarantine during the COVID-19 period. Those rates ranged from 0.9 to 48%, 0.7%–64%, and 0.9%–37.6%, respectively. Based on systematic reviews and meta-analyses [15] of coronaviruses (SARS, MERS, and SARS-CoV2), 14%–61% of those infected experience mental health complications, and 14.8%–76.9% experienced these problems after their illness. Our data showed a positive correlation between PHQ-9, GAD-7, and ISI scores. This positive correlation indicates that depression, anxiety, and insomnia were closely related and might have a high co-morbidity rate. Stress affects the internal state of balance between the body and mind, leading to physical and mental reactions such as tension, depression, anxiety, insomnia, or various physical problems [19]. Even if the pandemic is over, it to the general public health professionals and the influence on the vulnerable groups of mental health and well-being will continue for a long time. We want to be able to care for patients in a more personalized way [22].
Multiple Regression Analysis on the Influential Factors of Depression, Anxiety, and Insomnia Among People in Quarantine
This study suggests that being married was a protective factor for depression. Single people increased the risk of depression by 35.9% compared with married people, consistent with existing research. Wang et al. [23] found that unmarried people suffered higher psychological stress during the pandemic. Tian et al. [24] showed that married people showed fewer psychological symptoms than unmarried people. Others reported more somatization, paranoid ideas, obsessiveness, depression, anxiety, phobias, and psychosis than married people.
Chronic disease increases the risk of insomnia, and psychiatric medication history contributes to depression and insomnia. Additionally, the risk of anxiety, depression, and insomnia increases with a mental illness history. Available evidence suggests that some of the measures taken to contain the pandemic may harm vulnerable populations, including those with mental or physical health problems and those with mental illness [6, 25, 26]. Due to the loss of access to mental health support and active activities, COVID-19 isolation can increase anxiety and depression in people coping with it.
Female, lack of understanding of quarantine policies (including partial and cannot understand at all) and low moods (including general, bad, and very bad moods) at check-in would significantly increase the risk of depression, anxiety, and insomnia. This study showed that females were 1.484, 1.897, and 1.832 times more than males to experience the risk of depression, anxiety, and insomnia, respectively. When previous trends are considered, mental distress is higher than expected, especially among women. Consistent with many existing studies [27–29]. In an earlier cross-sectional study of COVID-19 in Spain (n = 3,480), the female was a strong predictor of anxiety. A meta-analysis [7] also noted a higher prevalence of anxiety among women during the pandemic. According to a Greek study [30], women were more likely to have sleep problems, reflecting an existing gender difference in anxiety and insomnia symptoms.
China continued to implement the most stringent prevention and control measures globally [31], including nucleic acid testing, tracking, self-isolation, quarantine, and broader population measures, including travel bans, school closures, assembly restrictions, curfews, and total lockdown. Entry quarantine was an essential means of preventing imported cases of COVID-19. However, some people still did not fully understand and agree with the quarantine policies. This study showed a positive correlation between the attitude towards quarantine policies and the moods at check-in (r = 0.361, p < 0.0001). The psychological resistance to quarantine policies would be reflected in the emotion during quarantine, resulting in adverse effects. More obvious negative emotions were observed for people in quarantine as a particular group. The low moods at check-in reflected the negative coping emotion of people in the face of the epidemic and quarantine policies. The psychological stress level of people with negative coping emotions was higher [23]. Negative coping emotions might be related to psychological stress or mental illness such as anxiety and depression [32, 33]. Considering the positive correlation between the attitude towards quarantine policies and the moods at check-in, people would have more pronounced negative emotions under quarantine measures [34]. In the study [35] of psychological interventions for people in quarantine, members of the psychological support team mentioned the experience of communicating with people in an equal manner, explaining the importance of quarantine measures, and acknowledging their contribution to social security. On 26 January 2020, China’s National Health Commission released guidelines for emergency psychological crisis intervention during the COVID-19 epidemic [36]. The notice provisions, psychological crisis intervention should be part of the public health response, by the municipal city and provincial levels organize joint prevention and control mechanism, interventions should be distinguished according to the group intervention staff. With the implementation of crisis interventions in China to reduce the negative psychosocial impacts on public mental health, there are challenges to mobilizing an effective mental health care system [22], which should provide which type of intervention, which groups need help, and in what way. In addition to emergency psychological crisis intervention measures afterward, this study suggests how to allow the public to understand different policies during different pandemic periods, which may significantly reduce various emotional and spiritual problems in quarantine. This involves official media must be authoritative and credible, rather than simply creating information panic to attract traffic. There is a risk that fake news can spread faster than the virus itself and create uncertainty and fear. This should be regulated through constant interaction with the media and national regulations.
Limitations
This study is a single-center study without considering the impact of the difference in living environments and medical conditions from other quarantine sites on mental health problems. The research results might be biased. In addition, due to the limitation of conditions, there was no comparative investigation of mental health before and after quarantine and psychological intervention research.
Conclusion
People in quarantine had problems with depression, anxiety, and insomnia. Depression, anxiety, and insomnia are closely related and positively correlated. Being married was a protective factor for depression. Chronic disease was a risk factor for insomnia. No psychiatric medication history was a protective factor for depression and insomnia. Female, history of mental illness, low moods at check-in, and partial/cannot understand the quarantine policies were risk factors for anxiety, depression, and insomnia. Positive correlations were found between attitudes towards quarantine policies and moods at check-in. In the face of public emergencies such as COVID-19, the psychological status of quarantined people will constantly change with the epidemic’s progress. Quarantine is part of our public health, but side effects must be weighed against alternatives like every medical intervention [2]. For example, voluntary isolation may be associated with good compliance and less psychological impact, especially when clearly explained and advertised as altruism. Therefore, timely monitoring and intervention of psychological status should be carried out during quarantine, but how to make the public understand quarantine policies during different periods deserve further studies.
Ethics Statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
CL: Responsible for data analysis and article writing. XF: Responsible for data collection and proofreading.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1.World Health Organization. WHO Coronavirus (COVID-19) Dashboard Data (2021). Available at: https://covid19.who.int/(Accessed December 18, 2021).
2. Rubin, GJ, and Wessely, S. The Psychological Effects of Quarantining a City. BMJ (2020) 368:m313. doi:10.1136/bmj.m313
3. Barbisch, D, Koenig, KL, and Shih, F-Y. Is There a Case for Quarantine? Perspectives from SARS to Ebola. Disaster Med Public Health Prep (2015) 9(5):547–53. doi:10.1017/dmp.2015.38
4. Prince, M, Patel, V, Saxena, S, Maj, M, Maselko, J, Phillips, MR, et al. No Health without Mental Health. Lancet (2007) 370(9590):859–77. doi:10.1016/s0140-6736(07)61238-0
5. Taquet, M, Luciano, S, Geddes, JR, and Harrison, PJ. Bidirectional Associations between COVID-19 and Psychiatric Disorder: Retrospective Cohort Studies of 62 354 COVID-19 Cases in the USA. Lancet Psychiatry (2021) 8(2):130–40. doi:10.1016/s2215-0366(20)30462-4
6. Brooks, SK, Webster, RK, Smith, LE, Woodland, L, Wessely, S, Greenberg, N, et al. The Psychological Impact of Quarantine and How to Reduce it: Rapid Review of the Evidence. Lancet (2020) 395(10227):912–20. doi:10.1016/s0140-6736(20)30460-8
7. Pappa, S, Ntella, V, Giannakas, T, Giannakoulis, VG, Papoutsi, E, and Katsaounou, P. Prevalence of Depression, Anxiety, and Insomnia Among Healthcare Workers during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. Brain Behav Immun (2020) 88:901–7. doi:10.1016/j.bbi.2020.05.026
8. Winkler, P, Formanek, T, Mlada, K, Kagstrom, A, Mohrova, Z, Mohr, P, et al. Increase in Prevalence of Current Mental Disorders in the Context of COVID-19: Analysis of Repeated Nationwide Cross-Sectional Surveys. Epidemiol Psychiatr Sci (2020) 29:e173. doi:10.1017/S2045796020000888
9. Dong, L, and Bouey, J. Public Mental Health Crisis during COVID-19 Pandemic, China. Emerg Infect Dis (2020) 26(7):1616–8. doi:10.3201/eid2607.200407
10. Duan, L, and Zhu, G. Psychological Interventions for People Affected by the COVID-19 Epidemic. The Lancet Psychiatry (2020) 7(4):300–2. doi:10.1016/s2215-0366(20)30073-0
11.United Nations. Policy Brief:COVID-19 and the Need for Action on Mental Health (2020). Available at: https://www.un.org/en/coronavirus/mental-health-services-are-essential-part-all-government-responses-covid-19 (Accessed December 18, 2021).
12. Jin, Y, Sun, T, Zheng, P, and An, J. Mass Quarantine and Mental Health during COVID-19: A Meta-Analysis. J Affective Disord (2021) 295:1335–46. doi:10.1016/j.jad.2021.08.067
13. Cénat, JM, Blais-Rochette, C, Kokou-Kpolou, CK, Noorishad, P-G, Mukunzi, JN, McIntee, S-E, et al. Prevalence of Symptoms of Depression, Anxiety, Insomnia, Posttraumatic Stress Disorder, and Psychological Distress Among Populations Affected by the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. Psychiatry Res (2021) 295:113599. doi:10.1016/j.psychres.2020.113599
14. Kisely, S, Warren, N, McMahon, L, Dalais, C, Henry, I, and Siskind, D. Occurrence, Prevention, and Management of the Psychological Effects of Emerging Virus Outbreaks on Healthcare Workers: Rapid Review and Meta-Analysis. BMJ (2020) 369:m1642. doi:10.1136/bmj.m1642
15. Rogers, JP, Chesney, E, Oliver, D, Pollak, TA, McGuire, P, Fusar-Poli, P, et al. Psychiatric and Neuropsychiatric Presentations Associated with Severe Coronavirus Infections: A Systematic Review and Meta-Analysis with Comparison to the COVID-19 Pandemic. Lancet Psychiatry (2020) 7(7):611–27. doi:10.1016/s2215-0366(20)30203-0
16. da Silva Neto, RM, Benjamim, CJR, de Medeiros Carvalho, PM, and Neto, MLR. Psychological Effects Caused by the COVID-19 Pandemic in Health Professionals: A Systematic Review with Meta-Analysis. Prog Neuro-Psychopharmacol Biol Psychiatry (2021) 104:110062. doi:10.1016/j.pnpbp.2020.110062
17. Xiong, J, Lipsitz, O, Nasri, F, Lui, LMW, Gill, H, Phan, L, et al. Impact of COVID-19 Pandemic on Mental Health in the General Population: A Systematic Review. J Affective Disord (2020) 277:55–64. doi:10.1016/j.jad.2020.08.001
18. Vindegaard, N, and Benros, ME. COVID-19 Pandemic and Mental Health Consequences: Systematic Review of the Current Evidence. Brain Behav Immun (2020) 89:531–42. doi:10.1016/j.bbi.2020.05.048
19. Krishnamoorthy, Y, Nagarajan, R, Saya, GK, and Menon, V. Prevalence of Psychological Morbidities Among General Population, Healthcare Workers and COVID-19 Patients amidst the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. Psychiatry Res (2020) 293:113382. doi:10.1016/j.psychres.2020.113382
20. Luo, M, Guo, L, Yu, M, Jiang, W, and Wang, H. The Psychological and Mental Impact of Coronavirus Disease 2019 (COVID-19) on Medical Staff and General Public - A Systematic Review and Meta-Analysis. Psychiatry Res (2020) 291:113190. doi:10.1016/j.psychres.2020.113190
21. Kunzler, AM, Röthke, N, Günthner, L, Stoffers-Winterling, J, Tüscher, O, Coenen, M, et al. Mental burden and its Risk and Protective Factors during the Early Phase of the SARS-CoV-2 Pandemic: Systematic Review and Meta-Analyses. Glob Health (2021) 17(1):34. doi:10.1186/s12992-021-00670-y
22. Fiorillo, A, and Gorwood, P. The Consequences of the COVID-19 Pandemic on Mental Health and Implications for Clinical Practice. Eur Psychiatr (2020) 63(1):e32. doi:10.1192/j.eurpsy.2020.35
23. Wang, H, Xia, Q, Xiong, Z, Li, Z, Xiang, W, Yuan, Y, et al. The Psychological Distress and Coping Styles in the Early Stages of the 2019 Coronavirus Disease (COVID-19) Epidemic in the General mainland Chinese Population: A Web-Based Survey. PLoS One (2020) 15(5):e0233410. doi:10.1371/journal.pone.0233410
24. Tian, F, Li, H, Tian, S, Yang, J, Shao, J, and Tian, C. Psychological Symptoms of Ordinary Chinese Citizens Based on SCL-90 during the Level I Emergency Response to COVID-19. Psychiatry Res (2020) 288:112992. doi:10.1016/j.psychres.2020.112992
25. Wang, J, Lloyd-Evans, B, Giacco, D, Forsyth, R, Nebo, C, Mann, F, et al. Social Isolation in Mental Health: A Conceptual and Methodological Review. Soc Psychiatry Psychiatr Epidemiol (2017) 52(12):1451–61. doi:10.1007/s00127-017-1446-1
26. Cacioppo, JT, Hughes, ME, Waite, LJ, Hawkley, LC, and Thisted, RA. Loneliness as a Specific Risk Factor for Depressive Symptoms: Cross-Sectional and Longitudinal Analyses. Psychol Aging (2006) 21(1):140–51. doi:10.1037/0882-7974.21.1.140
27. González-Sanguino, C, Ausín, B, Castellanos, MÁ, Saiz, J, López-Gómez, A, Ugidos, C, et al. Mental Health Consequences during the Initial Stage of the 2020 Coronavirus Pandemic (COVID-19) in Spain. Brain Behav Immun (2020) 87:172–6. doi:10.1016/j.bbi.2020.05.040
28. Mazza, C, Ricci, E, Biondi, S, Colasanti, M, Ferracuti, S, Napoli, C, et al. A Nationwide Survey of Psychological Distress Among Italian People during the COVID-19 Pandemic: Immediate Psychological Responses and Associated Factors. Int J Environ Res Public Health (2020) 17(9):3165. doi:10.3390/ijerph17093165
29. Chang, J, Yuan, Y, and Wang, D. Mental Health Status and its Influencing Factors Among College Students during the Epidemic of COVID-19. Nan Fang Yi Ke Da Xue Xue Bao (2020) 40(2):171–6. doi:10.12122/j.issn.1673-4254.2020.02.06
30. Voitsidis, P, Gliatas, I, Bairachtari, V, Papadopoulou, K, Papageorgiou, G, Parlapani, E, et al. Insomnia during the COVID-19 Pandemic in a Greek Population. Psychiatry Res (2020) 289:113076. doi:10.1016/j.psychres.2020.113076
31.Government of the People’s Republic of China. Epidemic Prevention and Control (2021). Available at: http://www.gov.cn/fuwu/zt/yqfwzq/yqfkblt.html (Accessed December 18, 2021).
32. Huang, J, Liu, Q, Li, J, Li, X, You, J, Zhang, L, et al. Post-Traumatic Stress Disorder Status in a rescue Group after the Wenchuan Earthquake Relief. Neural Regen Res (2013) 8(20):1898–906. doi:10.3969/j.issn.1673-5374.2013.20.009
33. Hollifield, M, Hewage, C, Gunawardena, CN, Kodituwakku, P, Bopagoda, K, and Weerarathnege, K. Symptoms and Coping in Sri Lanka 20-21 Months after the 2004 Tsunami. Br J Psychiatry (2008) 192(1):39–44. doi:10.1192/bjp.bp.107.038422
34. Qianyi, L, Chan, Y, Shaomin, D, Liang, Z, Weiyang, M, Yuping, N, et al. An Online Investigation of Mental Health Status of 857 Different Status Identities in Guangdong Province during the Outbreak of COVID-19. Chin J Psychiatrys (2020) 53(3):190–7. doi:10.3760/cma.j.cn113661-20200212-00026
35. Shuyue, W, Wenhua, Z, Sailing, G, Zhensong, G, Haoran, D, and Ting, Z. Investigation and Intervention on the Psychological Status of the Quarantined Observation Staff during the COVID-19. Compr Med Investig Reports (2021) 41:266–9.
36.National Health Commission of China. Principles of the Emergency Psychological Crisis Interventions for the New Coronavirus Pneumonia (2020). Available at: http://www.nhc.gov.cn/jkj/s3577/202001/6adc08b966594253b2b791be5c3b9467 (Accessed December 18, 2021).
Keywords: anxiety, COVID-19, quarantine, depression, cross-sectional study, insomnia
Citation: Lin C and Fu X (2022) A Cross-Sectional Study of Depression, Anxiety, and Insomnia Symptoms in People in Quarantine During the COVID-19 Epidemic. Int J Public Health 67:1604723. doi: 10.3389/ijph.2022.1604723
Received: 23 December 2021; Accepted: 27 June 2022;
Published: 20 July 2022.
Edited by:
Gonzalo Martinez-Ales, Columbia University, United StatesReviewed by:
Ziqiang Han, Shandong University, ChinaCopyright © 2022 Lin and Fu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chun Lin, NzgxNjY0OTA1QHFxLmNvbQ==
This Original Article is part of the IJPH Special Issue “The Impact of the COVID-19 Pandemic on Mental Health.”
 Chun Lin
Chun Lin Xiaohong Fu2
Xiaohong Fu2