- 1Jacobs Center for Productive Youth Development, University of Zurich, Zurich, Switzerland
- 2Department of Sociology, Utrecht University, Utrecht, Netherlands
- 3Department of Psychology, School of Philosophy, Psychology and Language Sciences, University of Edinburgh, Edinburgh, United Kingdom
- 4Integrated Psychiatric Services Winterthur-Zurcher Unterland, Winterthur, Switzerland
- 5Experimental and Clinical Pharmacopsychology, Department of Psychiatry, Psychotherapy and Psychosomatics, Psychiatric Hospital of the University of Zurich, Zurich, Switzerland
- 6Neuroscience Center Zurich, University of Zurich and Swiss Federal Institute of Technology, Zurich, Switzerland
- 7Institute of Criminology, University of Cambridge, Cambridge, United Kingdom
- 8Department of Psychology, University of Zurich, Zurich, Switzerland
Objectives: Young adults are essential to the effective mitigation of the novel coronavirus (SARS-CoV-2/COVID-19) given their tendency toward greater frequency of social interactions. Little is known about vaccine willingness during pandemics in European populations. This study examined young people’s attitudes toward COVID-19 vaccines in Fall 2020.
Methods: Data came from an ongoing longitudinal study’s online COVID-19-focused supplement among young adults aged 22 in Zurich, Switzerland (N = 499) in September 2020. Logistic regressions examined young adults’ likelihood of participating in COVID-19 immunization programs.
Results: Approximately half of respondents reported being unlikely to get vaccinated against COVID-19. Compared to males, females were more likely to oppose COVID-19 vaccination (p < 0.05). In multivariate models, Sri Lankan maternal background and higher socioeconomic status were associated with a greater likelihood of getting vaccinated against COVID-19 (p < 0.05). Respondents were more likely to report a willingness to get vaccinated against COVID-19 when they perceived 1) an effective government response (p < 0.05) and 2) their information sources to be objective (p < 0.05).
Conclusion: This study communicates aspects important to the development of targeted information campaigns to promote engagement in COVID-19 immunization efforts.
Introduction
COVID-19, the disease caused by severe acute respiratory virus 2 (SARS-CoV-2), has demonstrated capabilities of rapid transmission across populations [1]. First reported in 2019, more than 2.4 million deaths and upward of 117 million cases have been attributed to the virus as of March 2021 worldwide [2]. There have been extensive challenges in responding to the COVID-19 pandemic due to a lack of knowledge of the natural history of the disease profiles it produces as well as rampant misinformation, skepticism and conspiracies related to the virus and its mitigation efforts [3, 4].
In November 2020, Switzerland had among the highest laboratory-confirmed COVID-19 cases per capita in the world [5]. Young people aged 20 to 29 in Switzerland had the highest infection rates across all age groups, posing a considerable threat to vulnerable populations [5]. Although younger people are less likely to experience serious negative health outcomes as a result of a COVID-19 infection, their tendency toward greater frequency of social interactions made them an essential group to consider in controlling the spread of the virus [6–10]. In December 2020, vaccine variants started to become available. As of March 2021, Switzerland had not completed vaccinations of the eldest and most at-risk groups of the population or published strategies to vaccinate the rest of the population, including young people [11]. Thus, it is urgent to better understand vaccine hesitancy among young adults as they are important disease vectors to address in order to mount an effective immunization campaign [12–15]. It remains unclear whether COVID-19 vaccination limits further transmission, however, it is understood to protect vulnerable populations. According to the Strategic Advisory Group of Experts (SAGE) on Immunization, vaccine hesitancy is a behavior influenced by a number of factors including issues of confidence (trust in vaccine provider), complacency (perceptions of need and/or value of a vaccine), and convenience (access) [16].
Switzerland has among the lowest levels of vaccine confidence internationally [17]. In Switzerland, vaccinations are not compulsory and a national vaccination registry does not exist [18, 19]. This strategy was designed to provide autonomy in local governance but has led to suboptimal vaccine coverage among the general population [18, 20]. Coverage between cantons is variable, for example, measles vaccination coverage is lower in German- (71.3%) than French-speaking (85.0%) cantons [21]. Similarly, individuals in French-speaking cantons report greater influenza vaccine coverage than those in German-speaking cantons across all age groups [22]. Vaccine hesitancy and refusal leads to under-immunization, reduction in potential for reaching herd immunity, and increases the risk of preventable illness and mortality. The success of mitigating outbreaks is dependent on the public’s willingness to engage with preventive public health programs including immunization.
Reasons for accepting or declining preventive measures in pandemic situations include uncertainties of the severity of a disease agent, perceptions that vaccines are rushed to market, among others [23–27]. Emerging work on COVID-19 vaccine acceptance demonstrates that these attitudes are highly variable worldwide. Among European populations, approximately 7 in 10 (73.9%) reported a willingness to get vaccinated against COVID-19 in early April 2020 [28]. Over time, vaccine acceptance has been reported to be as low as 53.7% in Italy and as high as 80% in Denmark according to more recent data [27, 29, 30]. Decreases in vaccine acceptance were observed in Europe throughout the pandemic which is thought to be associated with lower perceived confidence in vaccine safety and effectiveness among populations [29]. Public perceptions of vaccines in Switzerland are poorly understood; existing research suggests a great influence of local socio-cultural contexts as determinants of vaccination decisions which may be distinct by Swiss region [31, 32]. More recent public opinion polls and peer-reviewed literature from around the world have noted a decreased willingness. For example, among adults in the United Kingdom and United States, approximately half responded that they would likely get vaccinated; in Switzerland, only 16% had the same response [3, 33–35]. These attitudes are not fixed and may change as nations report on successes.
Young people form risk perceptions related to health issues, in part, based on their perceptions of susceptibility and seriousness of a particular disease as well as social patterning from respected peers’ behavior [36]. Higher participation in immunization programs may occur when individuals believe that effective protections exist and when they are directed or enabled to engage in such activities [37]. Young people may base personal vaccine uptake decisions on misinformed or shortsighted heuristics whereby they perceive the side-effects related to a vaccine to be more likely than the disease it may prevent [38, 39]. These perceptions are informed by their physical and social environment which includes mass public health information campaigns. Successful campaigns create enabling conditions to seek reliable information on prevention and other services to help mitigate a diseased state. For example, human papilloma virus (HPV) vaccination rates among adolescent young Swiss women aged 16 years were 51% if they attended schools with a vaccination program and 37% if their school did not have such a program [39]. In Switzerland, there have been limited public attempts to actively engage and educate young people about their role in combatting the COVID-19 pandemic. The most high profile appeal for limiting social contact among young people came from the WHO in March 2020 [40]. It is unclear if and how this message was disseminated or tailored to young people in Switzerland. In the absence of reliable information campaigns, young adults may turn to the internet as a primary source of information about COVID-19 where there is little information quality control [41]. Scientific journals, media outlets and other respected sources of information were not immune to baseless claims during this pandemic, including conspiracy theories related to COVID-19 vaccine development and trials [42–48]. Perceptions of this media landscape and their associations with vaccine uptake are currently unknown among young people living in Switzerland in the context of the COVID-19 pandemic.
Sociodemographic characteristics have been observed to influence behavior and shape differences in cultural norms around vaccine uptake. For example, women tend to be more averse to vaccine uptake than males [49, 50]. Existing literature suggests differences in immune responses between the sexes, however, sex is not considered in the design or dosing of recommended immunizations, which may lead to undocumented adverse effects disproportionately affecting females [51]. Women also report more influenza vaccination concerns in terms of its efficacy and safety, and report more adverse reactions to vaccines in general which may explain their relatively lower uptake than men and greater hesitancy to participate in immunization programs [49, 50]. Higher education has also been associated with increased uptake of vaccines over the life course [52]. Differences in national background have been observed in vaccine willingness in Switzerland; non-Swiss children have higher vaccine coverage levels than Swiss children [53]. Relatively greater household economic resources has also been observed to affect vaccination attitudes and behaviors although this has been a confounder in some studies [32, 54].
To optimize COVID-19 vaccine utility, it is essential that national health authorities have an evidence base to inform the (re)allocation of resources to key and strategic subpopulations and to develop strategies to combat deficiencies in health literacy related to the COVID-19 pandemic. These activities should include the development of mass communication campaigns related to vaccination and clarifications of prevalent misinformation.
The current prospective, community-based study took place in Switzerland’s largest city, Zurich, over the course of the first 6 months of the COVID-19 outbreak in Europe and collected data specific to young people’s perceptions of the COVID-19 virus and their opinions on a hypothetical vaccine compliance strategy implemented by the Swiss government. The study sought to characterize its respondents along sociodemographic factors and provide perspectives important to the development of an evidence base for Swiss-specific pandemic responses targeting young people.
We expect that H1: there will be significant associations between female sex and lower vaccine willingness, H2: significant associations between perceptions of a favorable government response and media coverage and vaccine willingness, and that H3: experience with COVID-19 will be significantly associated with agreement to a mandatory COVID-19 vaccine.
Methods
Design
Data came from a supplement to the Zurich Project on the Social Development from Childhood to Adulthood (z-proso), an ongoing prospective longitudinal study on the development of prosocial and problem behavior (e.g., antisocial behavior) from childhood to adulthood. A total of eight waves of data, at ages 7, 8, 9, 11, 13, 15, 17, and 20, were collected from children who, in 2004, entered first grade in one of 56 public primary schools in Zurich. Stratified random sampling procedures used in the initial target sample of schools oversampled less resourced school districts. Details on original sample selection and attrition have been detailed elsewhere [55, 56]. Respondents who had participated in the age-20 assessment (2018, N = 1,180) were invited to participate in four data collections after Switzerland went into its first home semi-confinement period which were conducted in German: Supplement 1 (8–14 April 2020, N = 786), Supplement 2 (30 April–5 May 2020, N = 650), Supplement 3 (21–26 May 2020, N = 569), and Supplement 4 (10–15 September 2020, N = 525). The current analyses primarily use data from Supplement 4, when data on vaccination willingness was collected, as well as assessments from ages 13 and 15 when the most complete records for socioeconomic indicators were collected.
At ages 13 and 15, participants completed a paper questionnaire in classrooms outside of regular class times. At age 20, the questionnaire was conducted on a computer at a Decision Science Laboratory of the Swiss Federal Institute of Technology (ETH) in Zurich which typically lasted 90 min. At ages 13 and 15, respondents were compensated with 50 Swiss Francs for their time. Those who had participated in the age-20 z-proso data collection were invited by SMS and e-mail to participate in the supplementary COVID-19 data collection through a personalized link. Respondents of the z-proso COVID-19 Supplements, 1–4, were entered into a lottery with the opportunity to win one of 50 prizes of 100 Swiss Francs each. At each of the four Supplement waves, participants were given 7 days to complete the survey. The study was reviewed by and received ethics clearance from the Ethics Committee of the Faculty of Arts and Social Sciences of the University of Zurich.
Measures
Sociodemographic variables included: sex (female, male), education level (compulsory school, vocational/technical training, higher education), and household International Socio-Economic Index of Occupational Status (ISEI) Quartile at age 13/15 [57]. Preliminary analyses of the data revealed no significant differences between respondents with Swiss or Northwestern European maternal backgrounds; therefore, we coded these participants into one Western European group. Thus, categories presented include: Western European, Southern European, Sri Lankan, Middle East and African, and American and other maternal background.
Perceptions of Swiss authorities ‘response, politicians’ views, and media coverage were assessed with the following question and statements: “What are your opinions and attitudes toward the measures against the coronavirus? How much truth do the following statements have for you?”; “The measures taken by the Swiss authorities to deal with the coronavirus are effective.”; “I agree with the measures taken by the Swiss authorities to combat the coronavirus”; “Politicians and the media exaggerate the threat”; “The media provides balanced and objective information about the coronavirus.” Answer options included: 1 = Not true at all, 2 = Not really true, 3 = Somewhat true, and 4 = Completely true; these were dichotomized to: 0 = Not true at all/not really true, and 1 = Somewhat true/completely true.
Personal health experiences with COVID-19. Exposure of a family member, partner, or other close person to COVID-19 was assessed with the probe, “A family member, partner or other close person…” where 1 = has tested positive for COVID-19, but did not have to go to the hospital because of it, 2 = is/was sick with COVID-19 and therefore had to go to the hospital, 3 = died as a result of the coronavirus illness. Each of these three items had answer options 1 = Yes, 2 = No. A positive indication to any of the three items probed across the four waves of data collection that occurred during the pandemic was coded as: 0 = Family member, partner or related person’s health not affected by COVID-19, alternatively 1 = Family member, partner or related person’s health affected by COVID-19 if there were positive responses to the probes. Next, a respondent’s personal health affected by the COVID-19 was assessed using the probe, “I myself…” where 1 = had symptoms that could be attributed to the coronavirus with answer options 1 = Yes, 2 = No. If respondents indicated a positive response to the probe in any of the four data collection waves that were conducted during the pandemic, they were coded as 1 = Personal health affected by COVID-19 pandemic, 0 = Personal health not affected by the COVID-19 pandemic. Initially, Swiss authorities established regulations that barred asymptomatic and subclinical suspected cases from testing which is the most common presentation of a COVID-19 infection among young people, thus, self-reported data may provide a better estimate of prevalence of disease among this population [58].
Attitudes toward vaccination were assessed with the following hypothetical: “Imagine that Switzerland has officially approved a vaccine against the coronavirus.” “Would you get vaccinated?”; answer options: 1 = Yes, for sure, 2 = Yes, probably, 3 = Undecided, 4 = No, probably not, and 5 = Definitely not. A binary variable was created to assess respondents’ reported likelihood of getting vaccinated coded as 1 = Likely to get vaccinated and 0 = Not likely to get vaccinated or undecided should a vaccine become available. Delving deeper, undecided about vaccination was coded as 1 = Undecided and 0 = Decided either way. Participants were also asked, “Would you agree to an obligatory vaccination if the public health authorities mandated it?” with answer options, 1 = Completely agree, 2 = Somewhat agree, 3 = Somewhat disagree, and 4 = Completely disagree. To assess whether respondents would be agreeable to a mandatory vaccine, a binary variable was created coded as 1 = Agree and 0 = Disagree.
Analysis
All analyses were conducted using SPSS (Version 26.0, Armonk, NY: IBM Corp.). Survey weights were used to allow for generalization back to the original recruitment population (see Nivette et al. 2021). Logistic regression models examined whether personal and peripheral experiences with COVID-19 and perceptions of the Swiss government response and media portrayal of the pandemic were associated with attitudes toward vaccination including likelihood of vaccine uptake, being undecided about vaccination, and agreeableness to a compulsory vaccination. Final models included sex, maternal national background, respondents’ education level, household ISEI quartile, perceptions of governmental response, perceptions of media portrayal of the pandemic, and personal experiences with COVID-19. Sample weights were applied to all analyses.
Results
Sample characteristics are displayed in Table 1. Overall, 525 respondents completed the fourth z-proso COVID-19 supplement survey which included the questions on vaccination. However, respondents who reported being outside of Switzerland at the time that the survey was administered were excluded; hence the analytic sample of 499. Perceptions of Swiss authorities’ response, politicians’ views, and media coverage are presented in Figure 1.
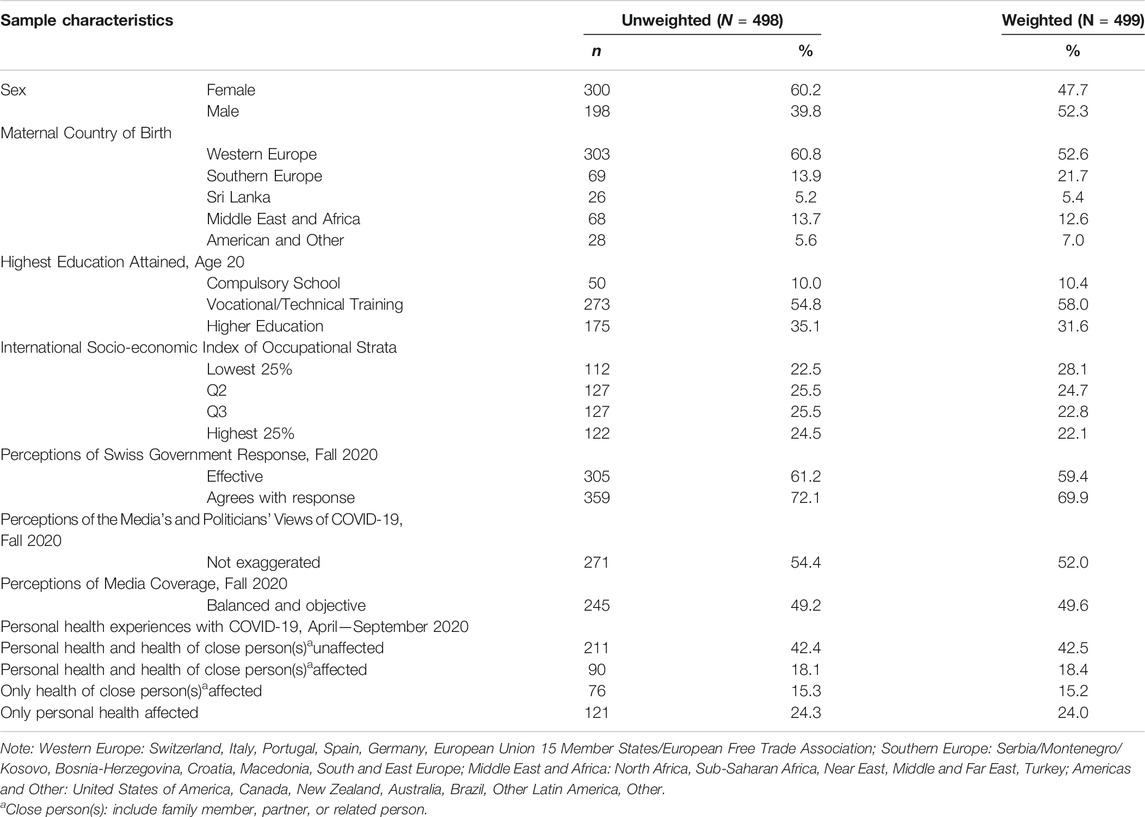
TABLE 1. Sample characteristics; Zurich Project on the Social Development from Childhood to Adulthood, Zurich, Switzerland, September 2020.
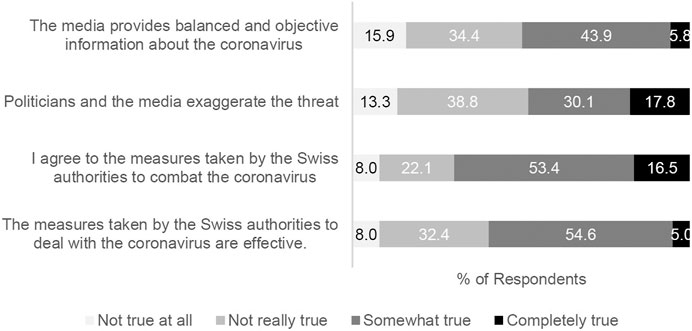
FIGURE 1. Perceptions of Swiss authorities ‘response, politicians’ views, and media coverage (N = 499); Zurich Project on the Social Development from Childhood to Adulthood, Zurich, Switzerland, September 2020.
Vaccination Willingness
Table 2 shows that approximately half (46.9%) of young people surveyed reported that they would likely get vaccinated if a vaccine became available. Final adjusted logistic regression analyses indicated that females were less likely than males to indicate vaccination willingness (p < 0.001, OR = 0.46, 95%CI = 0.30–0.71). Respondents with a Sri Lankan maternal background were more likely to report that they would get vaccinated than respondents of other cultural backgrounds (p < 0.01); this Sri Lankan maternal background became significant and stronger from the bivariate models (Table A1) to the adjusted models (in Table 2), with the adjustment of socioeconomic status. Thus, when SES is held equal, participants with a Sri Lankan background are more likely to report a higher likelihood of getting vaccinated. Lower educational attainment was associated with lower likelihood of vaccine willingness. Individuals with vocational or technical training were less likely to report vaccine willingness than those with higher education (p = 0.015, OR = 0.55, 95%CI = 0.34–0.89). Compared to respondents in the lowest ISEI quartile, all others were more likely to be willing to get vaccinated against COVID-19 (p < 0.01).
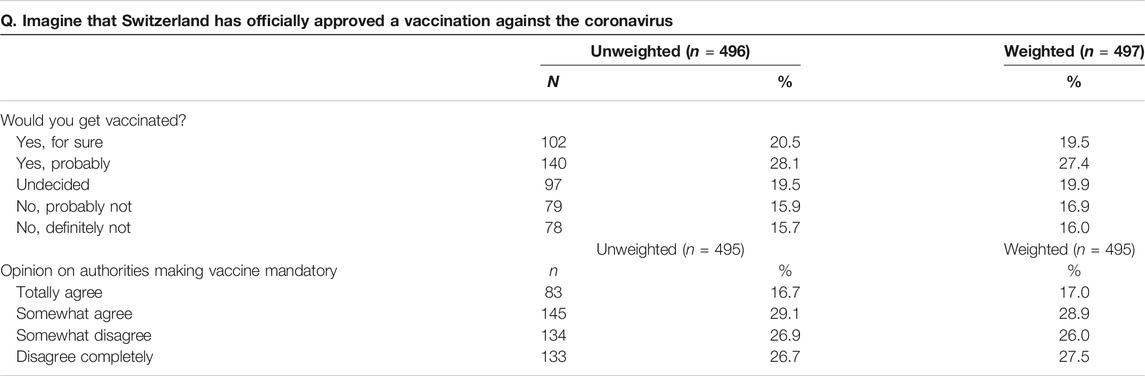
TABLE 2. Attitudes toward a COVID-19 vaccination among young people in; Zurich Project on the Social Development from Childhood to Adulthood, Zurich, Switzerland, September 2020.
Table 3 shows that respondents who perceived that the Swiss national response was effective and that politicians provided non-exaggerated views of the COVID-19 situation were more likely to report a greater likelihood of getting vaccinated than those who reported otherwise (p = 0.048, OR = 1.64, 95%CI = 1.00–2.68 and p < 0.001, OR = 3.93, 95%CI = 2.49–6.21 respectively). Finally, personal experience with COVID-19 was not significantly associated with greater likelihood of vaccination willingness. One exception was that respondents whose own health and the health of close ones was reportedly affected by COVID-19 were less likely to report vaccination willingness than when only they themselves had been affected (p = 0.026, OR = 0.49, 0.26–0.92).
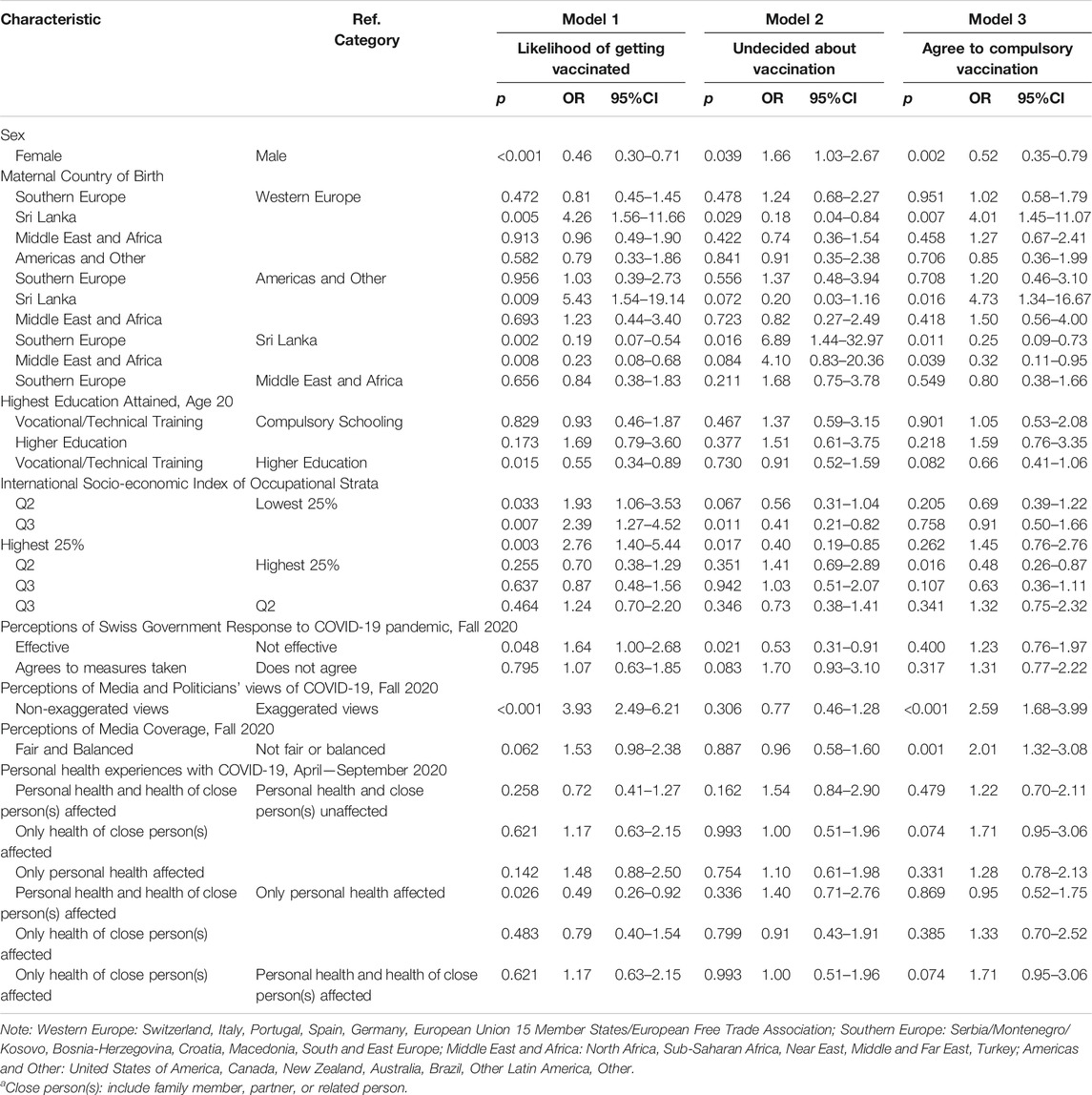
TABLE 3. Multivariate logistic regression analyses examining likelihood of getting vaccinated, vaccine hesitancy, and opinion to compulsory vaccination, weighted analyses; Zurich Project on the Social Development from Childhood to Adulthood, Zurich, Switzerland, September 2020.
Undecided About Vaccination
A significant minority of respondents, approximately 1 in 5 (19.9%), reported being undecided about getting vaccinated. Table 3 shows that female respondents were more likely to be undecided than males (p = 0.039, OR = 1.66, 95%CI = 1.03–2.67). In final adjusted models, Sri Lankans were less likely than those with Western European backgrounds to report being undecided about vaccination (p = 0.029, OR = 0.18, 95%CI = 0.04–0.84). Conversely, Southern Europeans were much more likely to report being undecided than those with Sri Lankan backgrounds (p = 0.016, OR = 6.89, 95%CI = 1.44–32.97). Respondents in the top two socioeconomic quartiles (Q3 and Q4) were less likely to be undecided than those in the lowest quartile (p = 0.011, OR = 0.41, 95%CI = 0.21–0.82 and p = 0.017, OR = 0.40, 95%CI = 0.19–0.85 respectively). Finally, those who believed that the Swiss government had responded effectively were less likely to be undecided (p = 0.021, OR = 0.53, 95%CI = 0.31–0.91).
Agreement to Compulsory Vaccination
When asked about their opinion on a situation whereby the authorities implemented a compulsory vaccination mandate, approximately half (45.9%) of young people surveyed were agreeable to this strategy. However, female respondents were less likely to agree than males (p = 0.002, OR = 0.52, 95%CI = 0.35–0.79). Respondents with a maternal Sri Lankan background were more likely to agree than those who identified any other national background (p < 0.05). Differences in responses by ISEI were limited to those in Q2 being less likely than those in the highest ISEI quartile to agree to such a mandate (p = 0.016, OR = 0.48, 95%CI = 0.26–0.87). Finally, when respondents perceived that politicians provided non-exaggerated views and that the media provided fair and balanced coverage of the pandemic, they were more likely to agree to compulsory, health authority-mandated vaccinations (p < 0.001, OR = 2.59, 95%CI = 1.68–3.99 and p = 0.001, OR = 2.01, 95%CI = 1.32–3.08).
Discussion
In September 2020, before any COVID-19 vaccine was approved worldwide, almost half of young adults in Zurich were either undecided or unlikely to get vaccinated against COVID-19 and also would not agree with coercive vaccine mandates. This is generally consistent with recent Swiss general population surveys, which reported that COVID-19 vaccine willingness has eroded as the pandemic and social restrictions have been prolonged [34, 59]. These low rates of vaccine willingness among youth and young adults is concerning; their cooperation with mitigation efforts such as vaccinations are essential to combatting COVID-19 at a national level [5]. To date, no information campaigns have yet been tailored to or systematically deployed specifically to young people in Swiss settings that expound on their importance to COVID-19 eradication efforts and the collective interest in their participation in immunization programs.
Historically, vaccination rates in Switzerland have not always been high enough to protect the population (18). Arguably, parts of the population do not sufficiently endorse vaccines as an acceptable and effective strategy to prevent disease or mortality. Coercive immunization programs in certain countries have proven to be effective in reducing morbidity and mortality of vaccine preventable diseases, however, they are ethically fraught, and may lead to further resistance [60, 61]. Switzerland values plurality and policy diversity among its different cantons; this is reflected in the cantons’ different immunization programs and outcomes. Deficiencies in vaccine compliance among cantons have been attributed to differing priorities and practices of policy makers and attitudes of vaccine gate-keepers (e.g., nurses, general practitioners) and engagement in alternative health care and education pedagogies [32, 53, 62]. Swiss communities report an openness to public programs if their autonomous decision-making is respected [62–66].
The findings of the current study suggest that in Fall 2020, young women in Switzerland were less willing to get vaccinated against COVID-19, more undecided about vaccination, and unlikely to agree to a mandatory vaccine. These findings are consistent with existing research on sex differences in vaccine acceptance and uptake.
In final adjusted models, Sri Lankan maternal background was associated with greater vaccination willingness, lower vaccine undecidedness, and more agreement to mandated immunization than all other national groups in the sample. These findings only emerged when socioeconomic background, which is a considerable social determinant of health and health behaviors, was adjusted for. Sri Lanka has vaccine coverage approaching 99% for most vaccine-preventable diseases [67]; thus, young adults with a Sri Lankan background may have stronger cultural norms of participating in vaccination programs compared to young adults from other nationalities with comparable socioeconomic status [68].
Young adults in the current study in higher ISEI quartiles were more likely to report vaccine willingness and being decided about vaccination. In other studies, socioeconomic status has been a confounder to vaccine willingness, as it has been associated with greater likelihood of an acceptance of alternative medicines that are not based on a biomedical model of health [69]. Future studies should continue to untangle the mechanisms that drive these alternative attitudes in order to identify intervention points that optimize local public health strategy.
Finally, the current study provides concrete evidence that while the population of young adults in Switzerland does not necessarily have to agree with the extraordinary measures that the Swiss government took in order to perceive that the national response was effective. When presented with what young people perceive to be balanced views from politicians, decision makers, and media, young adults are more open to participating in immunization programs and become more open to paternalistic strategies to mitigate the spread of COVID-19. These findings provide an evidence base on which to build mass information campaigns dedicated to subpopulations of young adults that adequately inform and build resilience against misinformation that may otherwise dissuade them from immunization efforts. Furthermore, it identifies women, those with relatively lower educational achievement, and socioeconomically disadvantaged groups as priorities for immunization information campaigns. Any public health effort should tailor messaging that is relevant to the target group, contains clear guidelines, and is easily understandable to improve health literacy specific to COVID-19 or any other contagion. When information is too complex, it fails to lead to disambiguation, increases feelings of despair and panic, and further confuses an already stressed population [70].
The current study used a broad and diverse sample that is representative of young adults living in Zurich during the time of the COVID-19 pandemic. While it may not be representative of French- or Italian-speaking Switzerland, it provides a measure that may be standardized that informs willingness to participate in vaccination programs. The findings may be useful during times of epidemics but also generally inform the Swiss National Vaccination Strategy and related public health activities. The substantial attrition across survey waves is a limitation mitigated with the development and application of survey weights to reflect the original sample in all analyses; it may have been further mitigated with a longer data collection period. The original target sample was generally representative of first-graders in Zurich in 2004. In the current study, we used sampling weights that allowed us to generalize findings back to this original sample, which consisted of a balanced sample of males and females. The use of non-validated scales is a potential limitation, but also a necessity during times of novel stressors for which we may not have well-established scales. The current study identifies groups that may have strong vaccine-adherence practices based on their national background that should be leveraged to inform public health practice in Swiss settings—specifically, factors that sustain and maintain strong immunization compliance. Furthermore, we emphasize the importance of including sex-based considerations in vaccine messaging development and identify populations that may be at risk of future immunization deficiencies.
Overall, our findings suggest that approximately half of young people living in Switzerland’s largest city report being unlikely to participate in COVID-19 immunization programs. However, when young adults perceived information in their media landscape to be balanced and objective, they were more likely to report a willingness to get vaccinated and even participate in a health authority-mandated vaccination program. In order to create and sustain these attitudes, targeted public information campaigns relatable to young adults, delivered at an appropriate language level that are easy to understand are essential to creating enabling conditions for participation in improving immunization coverage efforts.
Data Availability Statement
Publicly available datasets were analyzed in this study. This data can be found here: Anonymized individual participant data and data dictionaries that underlie the results reported in this article are available to other researchers upon request. Requests including a brief proposal should be sent to DR. As a research infrastructure supported by the SNSF, the z-proso study is committed to an open data access policy. Anonymized data, protocols, and other metadata from earlier data collections of the study are generally available to the scientific community. Please contact DR to this purpose.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethics Committee of the Faculty of Arts and Sciences of the University of Zurich (Approval Nr. 2018.2.12; 2020.4.3). Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author Contributions
MPE, LS, DR, UH, and AM co-developed and co-led the study. AS, MPE, LS, UH, DR, AM, and LB contributed to the design of the questionnaire. DR organized the data collection. CL-T conducted the analyses and wrote up the results. CL-T and LS drafted and wrote the article. AN, AS, LB, MPE, LS, DR, UH, AM, BQ, and CL-T contributed to the interpretation of the data, and critically revised the article for important intellectual content.
Funding
The research reported in this article is currently financially supported by the Swiss National Science Foundation as a research infrastructure (SNF; Grants 10531C_189008; 10FI14_170409; 1310FI14_170402/2; 189008 10FI14_198052) and by the Jacobs Foundation (JF). The Zurich Project on Social Development from Childhood to Adulthood is a long-term study set up by MPE and DR. Earlier phases of the study (2003–2016) were funded by the SNF, the JC, the Swiss Federal Office of Public Health, the Department of Education of the Canton of Zurich, the Swiss State Secretariat of Migration and its predecessors, the Julius Bär Foundation, and the Visana Plus Foundation.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/ijph.2021.643486/full#supplementary-material
Appendix
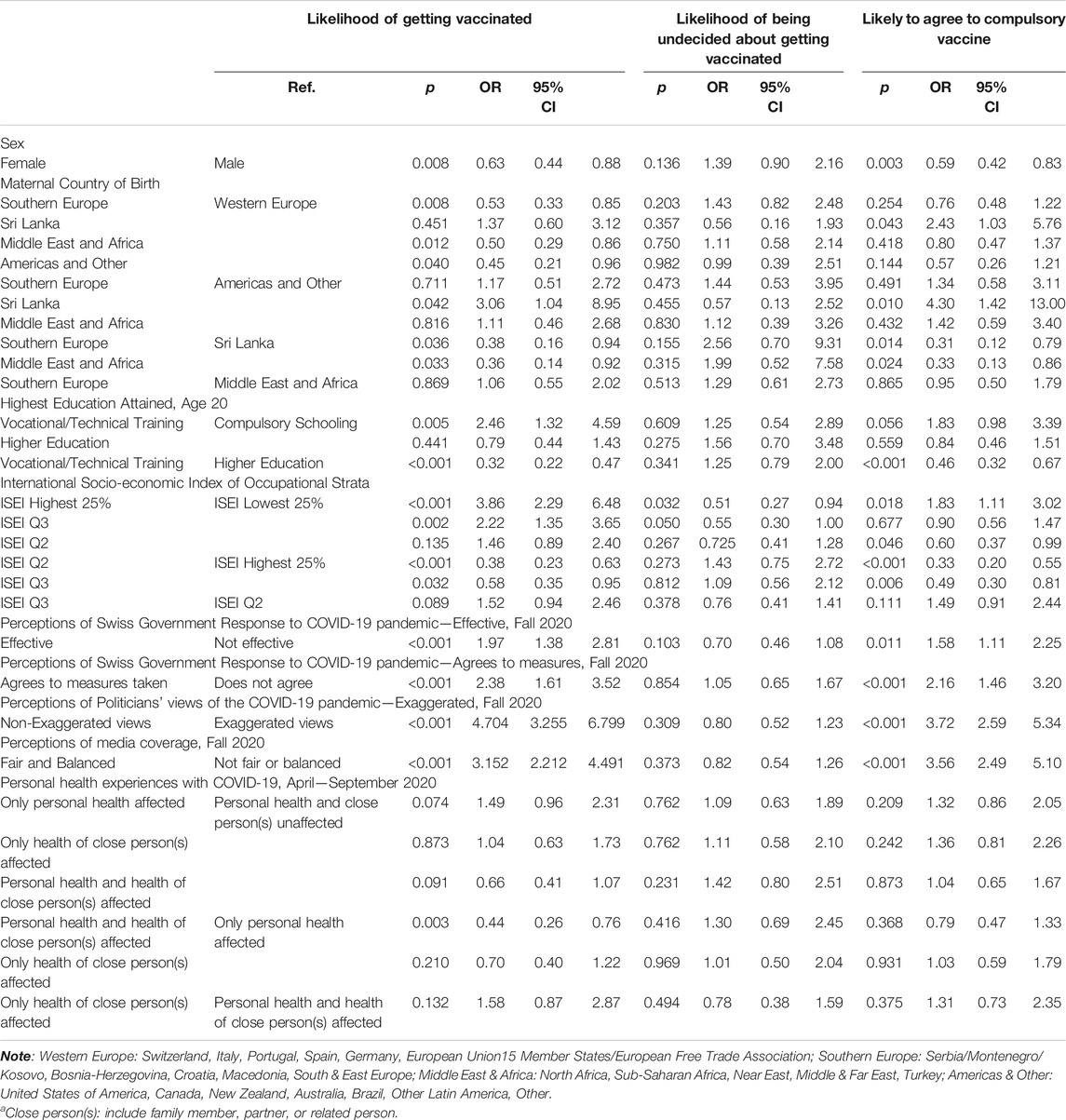
TABLE A1. Bivariate logistic regression analyses examining likelihood of getting vaccinated, vaccine hesitancy, and opinion to compulsory vaccination, weighted analyse; Zurich Project on the Social Development from Childhood to Adulthood, Zurich, Switzerland, September 2020.
References
1. Lu, R, Zhao, X, Li, J, Niu, P, Yang, B, Wu, H, et al. Genomic Characterisation and Epidemiology Of 2019 Novel Coronavirus: Implications for Virus Origins And Receptor Binding. Lancet (2020). 395(10224):565–74. doi:10.1016/s0140-6736(20)30251-8
2.European Centre for Disease Prevention and Control. COVID-19 Situation Update Worldwide as of 23 February 2021 (2021). Available from: https://www.ecdc.europa.eu/en/geographical-distribution-2019-ncov-cases. (accessed March 11, 2021).
3. Wang, B, Allington, D, Beaver, K, Meyer, C, Moxham-Hall, V, Murkin, G, et al. Coronavirus Uncertainties: Vaccines, Symptoms and Contested Claims. London, UK: King's College London - The Policy Institute (2020). Available from: https://www.kcl.ac.uk/policy-institute/assets/coronavirus-uncertainties.pdf. (accessed March 11, 2021).
4. V’Kovski, P, Kratzel, A, Steiner, S, Stalder, H, and Thiel, V. Coronavirus Biology and Replication: Implications for SARS-CoV-2. Nat Rev Microbiol (2020).
5.Federal Office of Public Health. COVID-19 Switzerland: information on the Current Situation, as of 19 November 2020 (2020). Available from: https://www.covid19.admin.ch/en/overview?detTime=total (accessed November 19, 2020).
6. Dong, Y, Mo, X, Hu, Y, Qi, X, Jiang, F, Jiang, Z, et al. Epidemiology of COVID-19 Among Children in China. Pediatrics (2020). 145(6):e20200702. doi:10.1542/peds.2020-0702
7. Gruszecka, J, and Filip, R. Preliminary Information on Prevention of Infections Caused by SARS-COV-2 Virus in Endoscopic Laboratories. Ann Agric Environ Med (2020). 27(2):171–4. doi:10.26444/aaem/122137
8. Pastor-Barriuso, R, Perez-Gomez, B, Hernan, MA, Perez-Olmeda, M, Yotti, R, Oteo-Iglesia, J, et al. Infection Fatality Risk for SARS-CoV-2: a Nationwide Seroepidemiological Study In The Non-Institutionalized Population of Spain. BMJ (2020). 371:m4509. doi:10.1136/bmj.m4509
9. Perez-Saez, J, Lauer, SA, Kaiser, L, Regard, S, Delaporte, E, Guessous, I, et al. Serology-Informed Estimates of SARS-CoV-2 Infection Fatality Risk in Geneva, Switzerland. Lancet Infect Dis (2021). 21:e69–e70. doi:10.1016/S1473-3099(20)30584-3
10. Ward, H, Atchison, C, Whitaker, M, Ainslie, KEC, Elliott, J, Okell, L, et al. Antibody Prevalence for SARS-CoV-2 following the Peak of the Pandemic in England: REACT2 Study in 100,000 Adults. medRxiv (2020). doi:10.1101/2020.08.12.20173690
11.Federal Office of Public Health. COVID-19: Switzerland Can Start Vaccinating Already in December [Federal Office of Public Health Current News] (2020). Available from: https://www.bag.admin.ch/bag/en/home/das-bag/aktuell/news/news-17-12-2020.html (Accessed December 19, 2020).
12. Thomas, K. New Pfizer Results: Coronavirus Vaccine is safe and 95% Effective (2020). Available from: https://www.nytimes.com/2020/11/18/health/pfizer-covid-vaccine.html (Accessed November 20, 2020).
13. McGinley, L, and Johnson, CY. Experimental Drug Given to Trump to Treat Covid-19 Wins FDA Clearance: The Washington Post (2020). Available from: https://www.washingtonpost.com/health/2020/11/21/regeneron-fda-clearance/ (accessed November 22, 2020).
14. Chen, P, Nirula, A, Heller, B, Gottlieb, RL, Boscia, J, Morris, J, et al. SARS-CoV-2 Neutralizing Antibody LY-CoV555 in Outpatients with Covid-19. N Engl J Med (2021). 384(3):229–37. doi:10.1056/nejmoa2029849
15.National Health Service. Coronavirus vaccine UK (2020). [cited 2020 4/12/2020]. Available from: https://www.nhs.uk/conditions/coronavirus-covid-19/coronavirus-vaccination/coronavirus-vaccine/.
16.World Health Organization. SAGE Working Group Dealing with Vaccine Hesitancy (March 2012 to November 2014) (2014). Available from: https://www.who.int/immunization/sage/sage_wg_vaccine_hesitancy_apr12/en/. (Accessed March 11, 2021)
17. Huhn, A, Simas, C, Karafillakis, E, Paterson, P, and Larson, HJ. Mapping Global Trends In Vaccine Confidence And Investigating Barriers To Vaccine Uptake: A Large-Scale Retrospective Temporal Modelling Study. Lancet (2020). 396(10255):898–908. doi:10.1016/s0140-6736(20)31558-0
18.Federal Office of Public Health. National Vaccination Strategy (2017). Available from: www.bag.admin.ch/bag/en/home/strategie-und-politik/nationale-gesundheitsstrategien/nationale-strategie-impfungen-nsi.html. (Accessed December 19, 2020)
19.Federal Office of Public Health. Schweizerischer Impfplan. in: FCV Issues, editor. Bern2020 (2020). p. 48.
20. Valeri, F, Hatz, C, Jordan, D, Leuthold, C, Czock, A, and Lang, P. Immunisation Coverage of Adults: a Vaccination Counselling Campaign in the Pharmacies in Switzerland. Swiss Med Wkly (2014). 144:w13955. doi:10.4414/smw.2014.13955
21. Lang, P, Zimmermann, H, Piller, U, Steffen, R, and Hatz, C. The Swiss National Vaccination Coverage Survey, 2005-2007. Public Health Rep (2011). 126 Suppl 2(Suppl. 2):97–108. doi:10.1177/00333549111260s212
22. Zürcher, K, Zwahlen, M, Berlin, C, Egger, M, and Fenner, L. Trends in Influenza Vaccination Uptake in Switzerland: Swiss Health Survey 2007 and 2012. Swiss Med Weekly (2019). 149:14705. doi:10.4414/smw.2019.14705
23. Henrich, N, and Holmes, B. The Public's Acceptance of Novel Vaccines during a Pandemic: a Focus Group Study and its Application to Influenza H1N1. Emerging Health Threats J (2009). 2(1):7088. doi:10.3402/ehtj.v2i0.7088
24. Morrison, LG, and Yardley, L. What Infection Control Measures Will People Carry Out to Reduce Transmission of Pandemic Influenza? A Focus Group Study. BMC Public Health (2009). 9(1):258. doi:10.1186/1471-2458-9-258
25. Bish, A, Yardley, L, Nicoll, A, and Michie, S. Factors Associated with Uptake of Vaccination against Pandemic Influenza: A Systematic Review. Vaccine (2011). 29(38):6472–84. doi:10.1016/j.vaccine.2011.06.107
26. Wilson, K, Nguyen, , Holdt, H, Brehaut, , and Hoe, . Acceptance of a Pandemic Influenza Vaccine: a Systematic Review of Surveys of the General Public. Infect Drug Resist (2011). 197. doi:10.2147/idr.s23174
27. Determann, D, De Bekker-Grob, EW, French, J, Voeten, HA, Richardus, JH, Das, E, et al. Future Pandemics and Vaccination: Public Opinion and Attitudes across Three European Countries. Vaccine (2016). 34(6):803–8. doi:10.1016/j.vaccine.2015.12.035
28. Korfage, S, Varghese, NE, Sabat, I, Barros, PP, Brouwer, W, Van Exel, J, et al. Once We Have it, Will We Use it? A European Survey on Willingness to Be Vaccinated against COVID-19. Eur J Health Econ (2020). 21(7):977–82. doi:10.1007/s10198-020-01208-6
29. Schreyögg, M. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines (2021). 9(2):160. doi:10.3390/vaccines9020160
30. Barello, S, Nania, T, Dellafiore, F, Graffigna, G, and Caruso, R. ‘Vaccine Hesitancy' Among University Students in Italy during the COVID-19 Pandemic. Eur J Epidemiol (2020). 35(8):781–3. doi:10.1007/s10654-020-00670-z
31. Siegrist, C-A, and Balinska Peroutkova, MA. The Public Perception of the Value of Vaccines - the Case of Switzerland. J Public Health (2008). 16(4):247–52. doi:10.1007/s10389-008-0201-1
32. Deml, MJ, Jafflin, K, Merten, S, Huber, B, Buhl, A, Frau, E, et al. Determinants of Vaccine Hesitancy in Switzerland: Study Protocol of a Mixed-Methods National Research Programme. BMJ Open (2019). 9(11):e032218. doi:10.1136/bmjopen-2019-032218
34. Perricone, M. Corona Pandemic: Only 16 Percent Want to Get Vaccinated Immediately (2020). Available from: https://www.srf.ch/news/schweiz/corona-pandemie-nur-16-prozent-wollen-sich-sofort-impfen-lassen. (Accessed November 9, 2020).
35. Robinson, E, Jones, A, Lesser, I, and Daly, M. International Estimates of Intended Uptake and Refusal of COVID-19 Vaccines: A Rapid Systematic Review and Meta-Analysis of Large Nationally Representative Samples. Vaccine (2021). 39(15):2024–34. doi:10.1016/j.vaccine.2021.02.005
37. Rimal, RN, and Real, K. Perceived Risk and Efficacy Beliefs as Motivators of Change: Use of the Risk Perception Attitude (RPA) Framework to Understand Health Behaviors. Hum Commun Res (2003). 29(3):370–99. doi:10.1093/hcr/29.3.370
38.World Health Organization ROfE. Vaccination and Trust. How Concerns Arise and the Role of Communication in Mitigating Crises (2017). Available from: https://www.euro.who.int/__data/assets/pdf_file/0004/329647/Vaccines-and-trust.PDF. (Accessed November 9, 2020)
39. Tarr, PE, Deml, MJ, and Huber, BM. Measles in Switzerland – Progress Made, but Communication Challenges Lie Ahead. Swiss Med Weekly (2019). 149:w20105. doi:10.4414/smw.2019.20105
40. Nebehay, S. WHO Message to Youth on Coronavirus: 'You Are Not Invincible. Geneva, Switzerland: Reuters (2020). Available from: https://www.reuters.com/article/us-health-coronavirus-who/who-message-to-youth-on-coronavirus-you-are-not-invincible-idUSKBN21733O (updated 03 20, 2020). (Accessed November 9, 2020)
41. Ioannidis, JPA. Coronavirus Disease 2019: The Harms of Exaggerated Information and Non‐evidence‐based Measures. Eur J Clin Invest (2020). 50(4):e13222. doi:10.1111/eci.13222
42. Bhagavathula, AS, Aldhaleei, WA, Rahmani, J, Mahabadi, MA, and Bandari, DK. Knowledge and Perceptions of COVID-19 Among Health Care Workers: Cross-Sectional Study. JMIR Public Health Surveill (2020). 6(2):e19160. doi:10.2196/19160
43. Mian, A, and Khan, S. Coronavirus: the Spread of Misinformation. BMC Med (2020). 18(1):89. doi:10.1186/s12916-020-01556-3
44. Cuan-Baltazar, JY, Muñoz-Perez, MJ, Robledo-Vega, C, Pérez-Zepeda, MF, and Soto-Vega, E. Misinformation of COVID-19 on the Internet: Infodemiology Study. JMIR Public Health Surveill (2020). 6(2):e18444. doi:10.2196/18444
45. Pradhan, P, Pandey, AK, Mishra, A, Gupta, P, Tripathi, PK, Menon, MB, et al. Uncanny Similarity of Unique Inserts in the 2019-nCoV Spike Protein to HIV-1 Gp120 and Gag. bioRxiv (2020). doi:10.1101/2020.01.30.927871
46. Gomes, C, Schunk, M, Sothmann, P, Bretzel, G, Froeschl, G, Wallrauch, C, et al. Transmission of 2019-nCoV Infection from an Asymptomatic Contact in Germany. N Engl J Med (2020). 382(10):970–1. doi:10.1056/nejmc2001468
47. Zimmer, K. Study Claiming New Coronavirus Can Be Transmitted by People without Symptoms Was Flawed. Berlin, Germany: Science (2020). Available from: https://www.sciencemag.org/news/2020/02/paper-non-symptomatic-patient-transmitting-coronavirus-wrong (updated 07 14, 2020). (Accessed November 9, 2020)
48. Devine, D, Gaskell, J, Jennings, W, and Stoker, G. Trust and the Coronavirus Pandemic: What Are the Consequences of and for Trust? an Early Review of the Literature. Polit Stud Rev (2020). 147892992094868. doi:10.1177/1478929920948684
49. Mesch, GS, and Schwirian, KP. Social and Political Determinants of Vaccine Hesitancy: Lessons Learned from the H1N1 Pandemic of 2009-2010. Am J Infect Control (2015). 43(11):1161–5. doi:10.1016/j.ajic.2015.06.031
50. Flanagan, KL, Fink, AL, Plebanski, M, and Klein, SL. Sex and Gender Differences in the Outcomes of Vaccination over the Life Course. Annu Rev Cel Dev. Biol (2017). 33:577–99. doi:10.1146/annurev-cellbio-100616-060718
51. Fink, AL, and Klein, SL. Sex and Gender Impact Immune Responses to Vaccines Among the Elderly. Physiology (2015). 30(6):408–16. doi:10.1152/physiol.00035.2015
52. Forshaw, J, Gerver, SM, Gill, M, Cooper, E, Manikam, L, and Ward, H. The Global Effect of Maternal Education on Complete Childhood Vaccination: a Systematic Review and Meta-Analysis. BMC Infect Dis (2017). 17(1):801. doi:10.1186/s12879-017-2890-y
54. Richard, JL, and Spicher, VM. Large Measles Epidemic in Switzerland from 2006 to 2009: Consequences for the Elimination of Measles in Europe. Eurosurveillance (2009). 14(50). doi:10.2807/ese.14.50.19443-en
55. Eisner, NL, Murray, AL, Eisner, M, and Ribeaud, D. A Practical Guide to the Analysis of Non-response and Attrition in Longitudinal Research Using a Real Data Example. Int J Behav Develop (2019). 43(1):24–34. doi:10.1177/0165025418797004
56. Eisner, M, Malti, T, and Ribeaud, D. Large-scale Criminological Field Experiments: the Zurich Project on the Social Development of Children. In: D Gadd, D Karstedt, and S Messner, editors. The SAGE Handbook of Criminological Research Methods. London, UK: SAGE (2011). p. 410–24.
57. Ganzeboom, HBG, De Graaf, PM, and Treiman, DJ. A Standard International Socio-Economic Index of Occupational Status. Soc Sci Res (1992). 21(1):1–56. doi:10.1016/0049-089x(92)90017-b
58. Davies, NG, Klepac, P, Klepac, P, Liu, Y, Prem, K, Jit, M, et al. Age-dependent Effects in the Transmission and Control of COVID-19 Epidemics. Nat Med (2020). 26(8):1205–11. doi:10.1038/s41591-020-0962-9
59. Eggo, M. COVID-19-Präventionsmassnahmen: Informationsstand, Einstellungen und Verhalten -- Bericht zur Wirkungsmessung von Ende Oktober 2020 im Auftrag des Bundesamts für Gesundheit BAG. Bern: Forschungsstelle sotomo (2020).
60. Attwell, K, Navin, MC, Lopalco, PL, Jestin, C, Reiter, S, and Omer, SB. Recent Vaccine Mandates in the United States, Europe and Australia: A Comparative Study. Vaccine (2018). 36(48):7377–84. doi:10.1016/j.vaccine.2018.10.019
61. Savulescu, J. Good Reasons to Vaccinate: Mandatory or Payment for Risk?. J Med Ethics (2021). 47(2):78–85. doi:10.1136/medethics-2020-106821
62. Masserey Spicher, V, and Weiss, MG. Policy and Socio-Cultural Differences between Cantons in Switzerland with High and Low Adolescent Vaccination Coverage for Hepatitis B and HPV. Vaccine (2019). 37(52):7539–46. doi:10.1016/j.vaccine.2019.09.085
63. Browne, M, Thomson, P, Rockloff, MJ, and Pennycook, G. Going against the Herd: Psychological and Cultural Factors Underlying the ‘Vaccination Confidence Gap’. PLOS ONE (2015). 10(9):e0132562. doi:10.1371/journal.pone.0132562
64. Klein, SD, Torchetti, L, Frei-Erb, M, and Wolf, U. Usage of Complementary Medicine in Switzerland: Results of the Swiss Health Survey 2012 and Development since 2007. PLOS ONE (2015). 10(10):e0141985. doi:10.1371/journal.pone.0141985
65. Simões-Wüst, AP, Rist, L, and Dettling, M. Self-Reported Health Characteristics and Medication Consumption by CAM Users and Nonusers: A Swiss Cross-Sectional Survey. J Altern Complement Med (2014). 20(1):40–7. doi:10.1089/acm.2012.0762
66. Wolf, U, Maxion-Bergemann, S, Bornhöft, G, Matthiessen, PF, and Wolf, M. Use of Complementary Medicine in Switzerland. Forsch Komplementärmed (2006). 13(2):4–6. doi:10.1159/000093488
67.World Health Organization. WHO Vaccine-Preventable Diseases: Monitoring System. 2020 Global Summary (2020). Available from: https://apps.who.int/immunization_monitoring/globalsummary/countries?countrycriteria%5Bcountry%5D%5B%5D=LKA&commit=OK. (Accessed November 9, 2020)
68. Braveman, P, and Gottlieb, L. The Social Determinants of Health: It's Time to Consider the Causes of the Causes. Public Health Rep (2014). 129(1_Suppl. 2):19–31. doi:10.1177/00333549141291s206
69. Wardle, J, Frawley, J, Steel, A, and Sullivan, E. Complementary Medicine and Childhood Immunisation: A Critical Review. Vaccine (2016). 34(38):4484–500. doi:10.1016/j.vaccine.2016.07.026
Keywords: vaccine willingness, COVID-19, pandemic health communication, evidence-based health messaging, vaccine acceptance, vaccine hesitancy
Citation: Leos-Toro C, Ribeaud D, Bechtiger L, Steinhoff A, Nivette A, Murray AL, Hepp U, Quednow BB, Eisner MP and Shanahan L (2021) Attitudes Toward COVID-19 Vaccination Among Young Adults in Zurich, Switzerland, September 2020. Int J Public Health 66:643486. doi: 10.3389/ijph.2021.643486
Received: 18 December 2020; Accepted: 01 April 2021;
Published: 06 May 2021.
Edited by:
Luca Crivelli, University of Applied Sciences and Arts of Southern Switzerland (SUPSI), SwitzerlandCopyright © 2021 Leos-Toro, Ribeaud, Bechtiger, Steinhoff, Nivette, Murray, Hepp, Quednow, Eisner and Shanahan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Cesar Leos-Toro, Y2VzYXIubGVvc3Rvcm9AdXpoLmNo
 Cesar Leos-Toro1*
Cesar Leos-Toro1*