- 1Department of Health Administration and Management, College of Medicine, University of Nigeria, Enugu, Nigeria
- 2Department of Health Systems and Policy, Sustainable Impact Resource Agency, Enugu, Nigeria
Objectives: This study validated a person-centred maternity care (PCMC) scale and assessed perception of PCMC and its associated factors among post-partum women.
Methods: A cross-sectional study was conducted among 450 post-partum women in two districts in Enugu State, Nigeria, using a 30-item PCMC scale. Exploratory and confirmatory factor analyses, descriptive, bivariate and Generalized Linear Models analyses were conducted.
Results: Twenty-two items were retained in the PCMC scale with high internal reliability and goodness-of-fit indices. About 25% of women received high PCMC. Marrying at 20–29 years (β = 3.46, ρ = 0.017) and 30–49 years (β = −5.56, ρ = 0.020); self-employment (β = −7.50, ρ = 0.005); marrying government worker (β = 7.12, ρ = 0.020); starting antenatal care in the third trimester (β = −6.78, ρ = 0.003); high participation in decision-making (β = −10.41, ρ < 0.001); domestic violence experience (β = 3.60, ρ = 0.007); delivery at health centre (β = 18.10, ρ < 0.001), private/mission hospital (β = 4.01, ρ = 0.003), by non-skilled attendant (β = −16.55, ρ < 0.001) and community health worker (β = −10.30, ρ < 0.001); and pregnancy complication (β = 4.37, ρ = 0.043) influenced PCMC.
Conclusion: The PCMC scale is valid and reliable in Nigeria. PCMC requires improvement in Enugu State. This study identified factors that may be considered for inclusion in intervention strategies.
Introduction
Person-centred maternity care (PCMC), defined as “maternity care that is respectful of and responsive to individual women and their families’ preferences, needs, and values” [1], is an effective strategy for improving quality of care experienced by women during facility-based childbirth in low- and middle-income countries (LMICs) [2, 3]. Improvements in quality of maternity care contribute to a reduction in maternal mortality ratio [2]. PCMC, comprising autonomy and communication, respect and dignity, and supportive care, aims at reducing mistreatment, abuse, disrespect and neglect of women during facility-based childbirth; and promoting positive childbirth experiences [1, 4]. Prior studies indicate that women are not getting adequate PCMC in LMICs [1, 4–6]. Perception of PCMC ranged from low in Ghana to moderately high in Kenya and India [1, 4–6]. Women’s perception of dignity and respect was high; communication and autonomy, low to moderately high; and supportive care, moderately high to high [1, 4–6]. Neglect of PCMC leads to disparities in use of skilled birth attendance and maternal and neonatal outcomes [7].
Broadly, patient characteristics, facility characteristics, and service types affect PCMC [3]. Patient characteristics include socio-demographic characteristics, clinical history and prior health care-seeking behaviour [3]. Perception of PCMC varied with socio-economic status and education in Kenya, India and Ghana [5, 7]. Women with high socio-economic status are usually personally empowered; live in areas with high quality of care; tend to have relationships with healthcare providers, narrow social power between women and providers, higher expectation of care, and capacity to advocate for high quality care [7, 8]. Higher incidents of disrespectful and abusive care were reported from women from lower socio-economic strata in Ethiopia and Pakistan [9–11], and younger and less educated women in other LMICs [12]. Employment, marital status and absence of domestic violence experience predicted higher PCMC among childbearing women [7]. In this study, we hypothesize that low socio-economic status, experience of domestic violence and low participation in household decisions will be associated with low PCMC.
Facility characteristics such as type of facilities and types of providers may modify women’s experiences of maternity care [3]. Whereas indices of clinical quality of maternal health were higher in hospitals than health centres [13, 14], interpersonal quality was higher in private than public hospitals [13, 15]. Women who delivered in health centres and private hospitals reported higher PCMC than those who were delivered in public hospitals in Kenya and India, but no significant differences were observed in Ghana [5, 7]. Disrespect and abuse were more likely in hospitals than health centres in Ethiopia [10], and in public health facilities than private health facilities in Pakistan [9]. In this study, we hypothesize that PCMC will be lower in public hospitals than health centres and private hospitals.
Evidence that type of services influences PCMC are mixed. In Pakistan, type of delivery service did not influence women’s experiences of disrespect and abuse [9]. Pregnancy complications was related to high perception of PCMC in Ghana, but not in Kenya and India [5]. However, severe pregnancy complication significantly predicted higher PCMC in Kenya [7]. Also, In Gambia, normal vaginal delivery was associated with a higher perception of autonomy and supportive care than instrumental delivery [16]. Conversely, higher incidents of disrespectful and abusive care were reported from women who had complications, longer labour durations and Caesarean birth [11, 17–19]. Our proposition is that women with pregnancy complications will have significantly lower PCMC than those without complications.
In Nigeria, mistreatment of women during childbirth are common and not only undermine utilization of health facilities for delivery but also create psychological distance between women and health providers [20, 21]. Yet, respectful and responsive maternity care has not been comprehensively studied in Nigerian health system [20, 22]. Also, PCMC scale has not been validated nor has any study investigated women’s perception and determinants of PCMC in Nigeria. This study, therefore, validated the PCMC scale, assessed perception of PCMC and its associated factors among post-partum women in Enugu State, Nigeria. This evidence will help decision-makers, providers, and service users identify gaps, design interventions to promote positive childbirth experiences, and evaluate changes in quality of maternity care.
Methods
Study Setting
The study took place in two districts of Enugu State, South-east Nigeria. Enugu state was delineated into seven health districts. We categorised the seven health districts into two groups of three well-performing and four less-performing districts using maternal healthcare utilisation data [23]. Enugu Metropolis and Isi-Uzo districts were randomly selected from the well-performing and less-performing districts, respectively. The two districts have, each a general hospital and a network of cottage hospitals and primary health facilities. In 2019, the estimated population of Enugu State was about 4.8 million people. Enugu Metropolis and Isi-Uzo had 1,061,256 and 217,952 populations respectively, out of which women of childbearing age constitute 47.2 and 43.1% respectively [24]. Skill birth attendance is about 93% [24]. However, the maternal mortality ratio in Enugu is 1,252/100, 000 live births [25], higher than the national ratio of 512/100,000 live births [24].
Research Design
The study adopted a facility-based cross-sectional survey design using an interviewer administered questionnaire.
Study Population and Sampling Strategy
Post-partum women aged 15–49 years, who delivered in 9 weeks preceding the study constituted the study population. To detect mean differences between post-partum women in the two districts (alpha level = 0.05, 95% power, allocation ratio of 3:1, GPower 3.1.9.7), we required a minimum sample size of 280 (70 in Isi-Uzo and 210 in Enugu metropolis). We, however, sampled 450 eligible post-partum women equally allocated to the two districts.
In each district, we purposively selected the general hospital and four primary health centres (one facility per local health authority) with the highest maternal and child healthcare attendance based on routine health management information system. Additionally, the sample in Enugu metropolis purposively included the state teaching hospital because of its central location which made it very accessible. Eligible post-partum women were recruited by convenience as they leave immunisation clinics using healthcare providers as gatekeepers.
Data Collection
Data was collected from January to March 2019 using an interviewer-administered PCMC scale made up of 30 items measuring three domains of PCMC: dignity and respect (6 items), communication and autonomy (9 items), and supportive care (15 items) [1]. The PCMC scale has been validated in similar low-resource context with good reliability coefficients for the total PCMC scale and sub-scales [1, 4]. The Cronbach alpha coefficients for full PCMC scale, dignity and respect (DR), autonomy and communication (AC), and supportive care (SC) sub-scales in Kenya were 0.86, 0.63, 0.73, and 0.72 correspondingly [1]. In India, the Cronbach alpha coefficients for full PCMC scale (27 items), DR (6 items), AC (9 items), and SC (12 items) sub-scales were 0.85, 0.70, 0.67, and 0.73, respectively [4]. Each item is on a 4-point response scale—0: “no, never,” 1: “yes, a few times,” 2: “yes, most of the time,” and 3: “yes, all the time.” For each respondent, responses from the PCMC scale were summed up into one composite PCMC score. The possible score on the PCMC scale range from 0 to 90, with a lower score implying poorer PCMC. The range of possible scores on the sub-PCMC scales are: 0–18, 0–27, and 0–45 for respect and dignity, communication and autonomy, and supportive care correspondingly.
The questionnaire also included information on socio-demographic characteristics such as age, marital status, residence, religion, age at marriage, education, literacy, occupation, partner’s education, partner’s occupation, and maternal health care-seeking behaviour. Other information collected include facility characteristics (facility type and provider type), service types, household wealth index, women’s participation in household decisions, domestic violence tolerance, and experience as well as a question on overall satisfaction with maternity care. Household wealth index was measured using 11 questions on Nigeria equity tool and its accompanying syntax used to create wealth quintiles [26]. Participation in household decision-making was assessed using questions on five household decisions [27]. Each question was assigned the following scores: 0—if the decision was made by husband/partner alone, someone else or other; 1—if the decision was jointly made by respondent and husband/partner; and 2—if the respondent alone made the decision. Participation score ranged from 0–10. Also, attitudes towards domestic violence were measured using five variables describing whether beating was justified if the wife: goes out without telling her husband; neglects the children; argues with her husband; refuses sex with her husband; and burns food [27]. Women who answered “Yes” and “Don’t know” were scored 0 while women who responded “No” were scored 1. Domestic violence tolerance score ranged from 0–5. The value of either the participation score or domestic violence tolerance was transformed into 0–1 interval [27]. The median values were used to dichotomise the scores into low and high participation as well as domestic violence tolerant and intolerant categories. Five trained research assistants administered the questionnaires, while the authors supervised the data collection.
Data Analysis
We conducted exploratory and confirmatory factor analyses using EViews version 11 and all other analyses using SPSS (version 26, IBM, NY, United States). Data were assessed for sampling adequacy using Kaiser-Meyer-Olkin measure. We conducted exploratory factor analysis with maximum likelihood estimation. Items that yield communalities ≥0.4 were deemed adequate [28]. A rotated factor loading of 0.32 on Promax rotation with Kaiser Normalization was considered significant [28]. The goodness of fit of the final factor structure of the 22-item scale was assessed using Chi-square goodness of fit test with confirmatory factor analysis. Additionally, a series of goodness-of-fit indices (root mean square residual, generalized fit index, adjusted generalized fit index, root mean square error of approximation, normed fit index, non-normed fit index, incremental fit index, and comparative fit index) were used to evaluate the quality of model fit. Cronbach alpha, inter-item correlation and intraclass correlation were used to report the reliability coefficients of the PCMC scale and sub-scales.
Characteristics of respondents were presented using frequencies and percentages. Mean PCMC scores and standard deviation were calculated and compared across various socio-demographic characteristics of respondents, facility characteristics and service type using t-tests and analysis of variance (ANOVA). Parametric tests were deemed appropriate since the single composite PCMC scores have interval-like properties. We categorized full PCMC and each sub-scale into “low, medium, and high.” Low was defined as scores in the approximate lower 25th percentile and scores in the top 75th percentile defined as high [29]. Pearson correlation was used to test association of total PCMC scores with overall satisfaction with maternity care. Generalized Linear Models was used to test relationship between PCMC and the parameters that were significant on bivariate analysis. Statistical significance was set at alpha 0.05 level.
Ethical Consideration
The study was approved by the Health Research Ethics Committee of University of Nigeria Teaching Hospital, Enugu, Nigeria (NHREC/05/01/2008B-FWA00002458-IRB00002323). Written, informed consent was obtained from all respondents.
Results
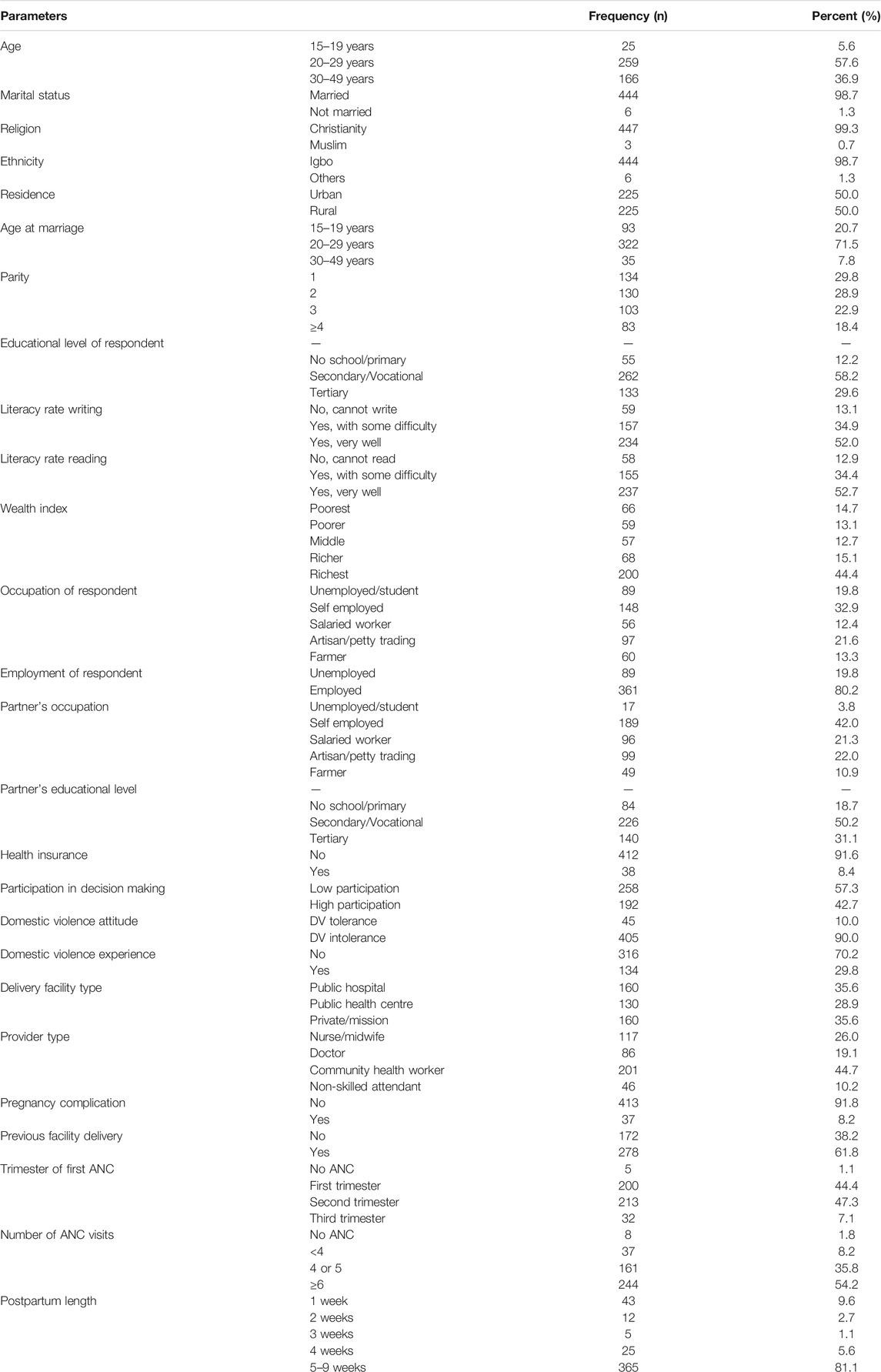
Characteristics of Respondent
The response rate was 100%. Table 1 shows the characteristics of respondents. Most women were married, Christians, Igbo, married in their 20 s and educated to at least secondary or vocational school. About a fifth of women were unemployed. While 57% of women had low participation in household decisions, about 30% had experienced domestic violence. About 54% of women started antenatal care late. About 8% reported pregnancy complications.
Factor Analysis
The PCMC scale was found to be valid. The Kaiser-Meyer-Olkin measure of sampling adequacy was 0.9507 (X2 = 1886, ρ < 0.001). Eight items yielded communalities ≤0.4, which were deemed inadequate (Table 2). Promax rotation with Kaiser Normalization showed that the remaining 22 items loaded ≥0.32 and were retained. Twenty items loaded on factor 1 (87.8% variance), while only two items loaded on factor 2 (12.2% variance). The goodness of fit Chi-square statistic was 1150.305 (ρ < 0.001). Goodness-of-fit indices suggested adequate fitness as shown in Table 3. PCMC scores correlated strongly with women’s overall satisfaction with quality of maternity care (r = 0.910, ρ < 0.001) indicating high criterion validity. The possible score on our 22-item PCMC scale range from 0 to 66. The range of possible scores on the sub-PCMC scales are: 0–12, 0–21, and 0–33 for respect and dignity (n = 4), communication and autonomy (n = 7), and supportive care (n = 11) correspondingly. Full PCMC scores correlated strongly with women’s overall satisfaction with quality of maternity care (r = 0.910, ρ < 0.001) indicating high criterion validity. The reliability indices of the full PCMC scale and sub-scales were high as shown in Table 3.
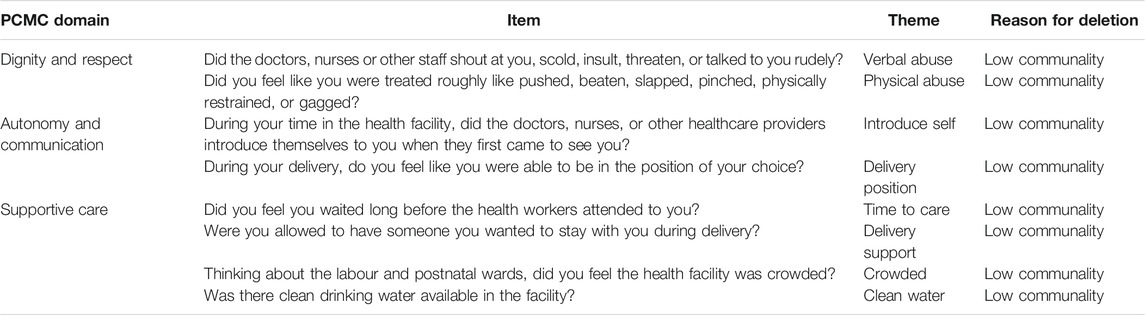
TABLE 2. Items deleted from person-centred maternity care scale during factor analysis for different reasons, Enugu State, Nigeria, 2019.
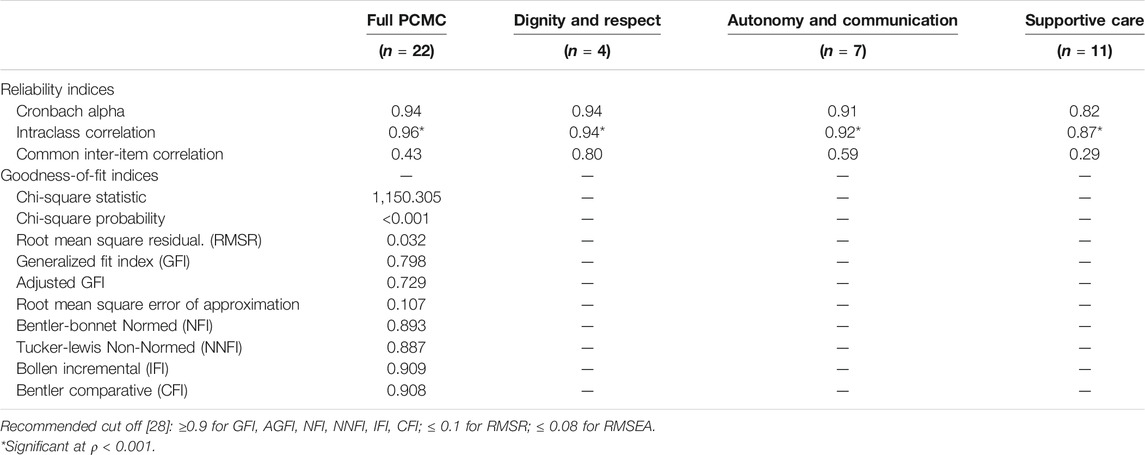
TABLE 3. Reliability and goodness-of-fit indices of person-centred maternity care scale in Enugu State, Nigeria, 2019.
Distribution of Individual PCMC Items Among Women (N = 450)
As shown in Table 4, most women were treated with respect and in a friendly manner Most women also reported good visual privacy and record confidentiality.
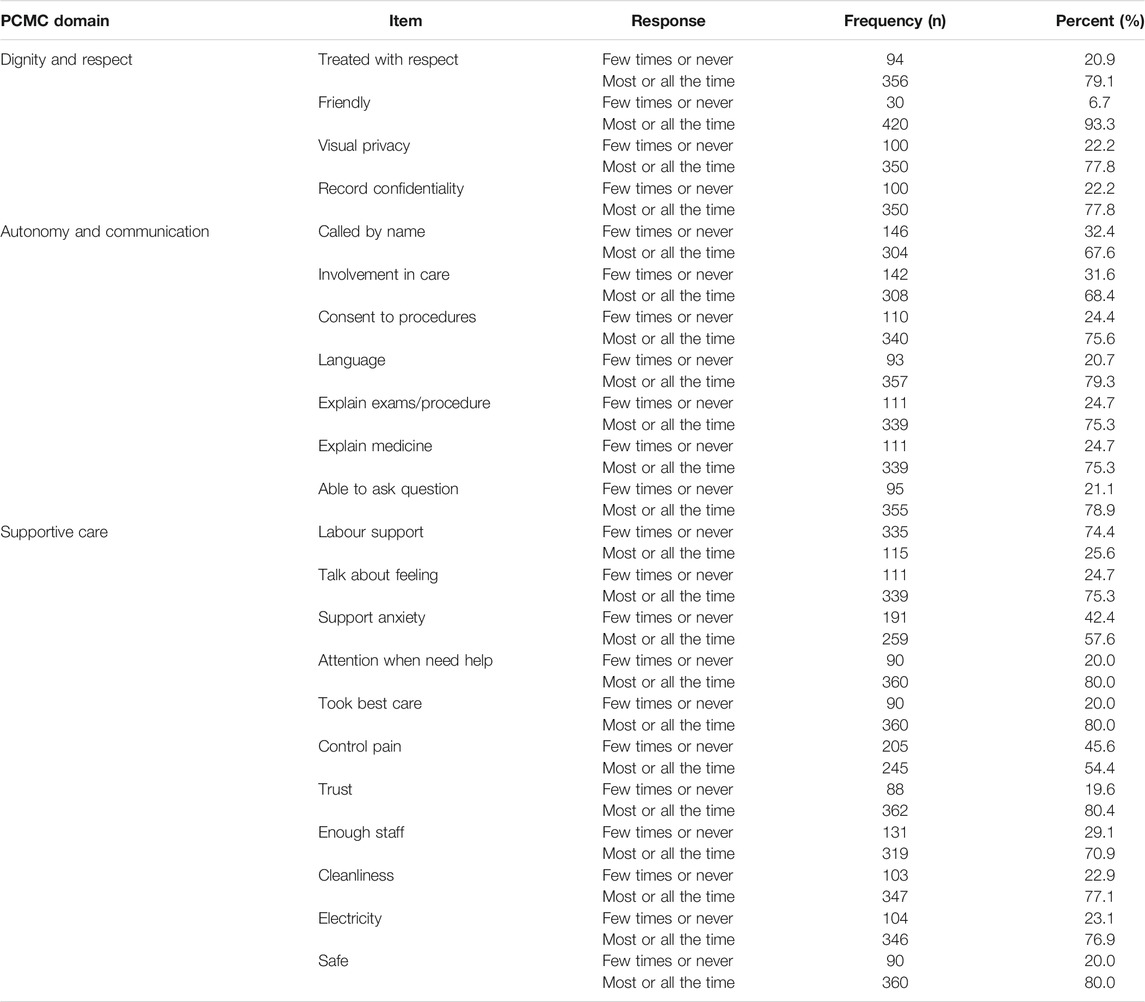
TABLE 4. Distribution of individual person-centred maternity care items (n = 22) among post-partum women in Enugu State, Nigeria, 2019.
Most women reported that providers called women by their names, involved women in care decisions, sought consent to procedures, talked to women in language that women understood, explained examinations and medicines (Table 4). Likewise, most women were able to ask their service providers questions.
Most women indicated that providers paid attention when needed, talked to women about their feeling, took the best care of them and could be trusted (Table 4). Most women also reported that health facilities were safe, clean, had electricity but had few staff. A quarter of women indicated that health facilities did not allow labour support (Table 4).
Distribution of Full PCMC Scale and Sub-Scales
Overall, women had medium scores on full PCMC scale and sub-scales, but a quarter of women perceived PCMC as high (Table 5). Over 60% of women perceived respect and dignity as high. While less than a quarter of women perceived communication and autonomy as high, just over a quarter perceived supportive care as high.
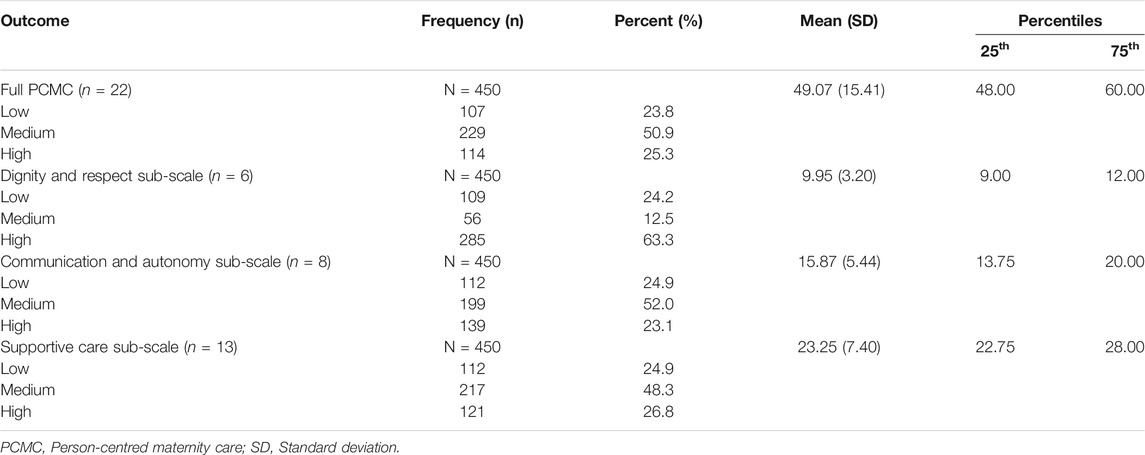
TABLE 5. Descriptive statistics of person-centred maternity care scale and sub-scales in Enugu State, Nigeria, 2019.
Bivariate Analysis
Table 6 shows mean score differences in PCMC disaggregated by patient characteristics, facility characteristics, and service types. Women who married at age 20–29 years had significantly higher mean PCMC score than women in other age groups (ρ < 0.001). Self-employed women (ρ < 0.001) and women married to unemployed partners (ρ = 0.008) had significantly low PCMC scores among occupational categories. High participation in household decision-making (ρ < 0.001), domestic violence experience (ρ < 0.001) and starting antenatal care during the third trimester (ρ< 0.001) were associated with lower PCMC scores. Delivery in health centres (ρ < 0.001), delivery by CHEW (ρ < 0.001), and pregnancy complications (ρ = 0.030) were associated with higher PCMC scores.
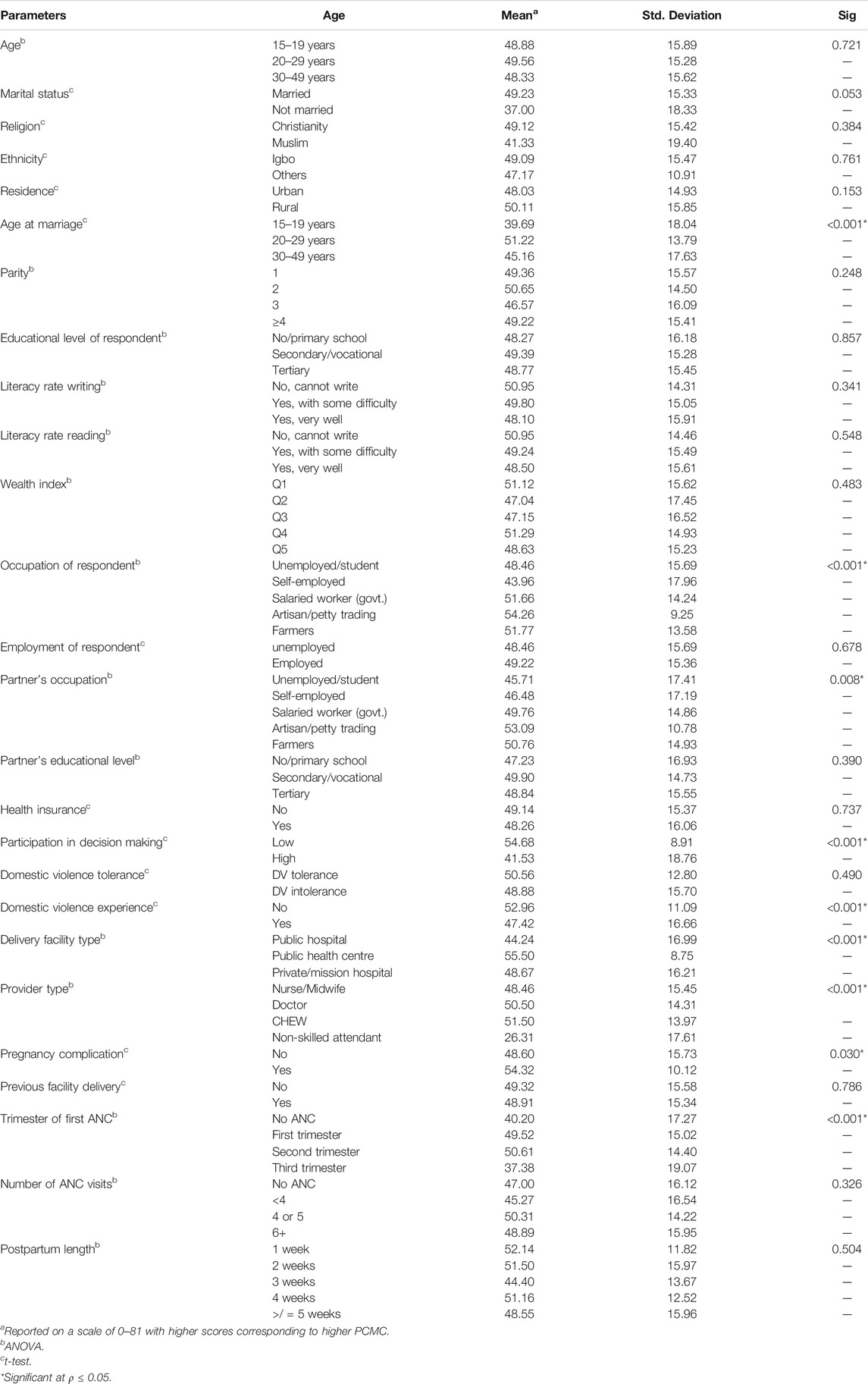
TABLE 6. Mean perception of person-centred maternity care disaggregated by respondents’ characteristics in Enugu State, Nigeria, 2019.
Factors Influencing Person-Centred Maternity Care
Table 7 shows the parameters that influenced perceived PCMC among women in this study. Marrying at age 20–29 years (β = 3.46, ρ = 0.017) and 30–49 years (β = −5.56, ρ = 0.020), self-employed women (β = −7.50, ρ = 0.005), married to a government worker (β = 7.12, ρ = 0.020), starting antenatal care in the third trimester (β = −6.78, ρ = 0.003), high participation in household decisions (β = −10.41, ρ ≤ 0.001), domestic violence experience (β = 3.60, ρ = 0.007), delivery at health centre (β = 18.10, ρ < 0.001), delivery at private/mission hospital (β = 4.01, ρ = 0.003), delivery by non-skilled attendant (β = −16.55, ρ < 0.001); and delivery by community health worker (β = −10.30, ρ < 0.001) and experience of pregnancy complication (β = 4.37, ρ = 0.043) influenced PCMC.
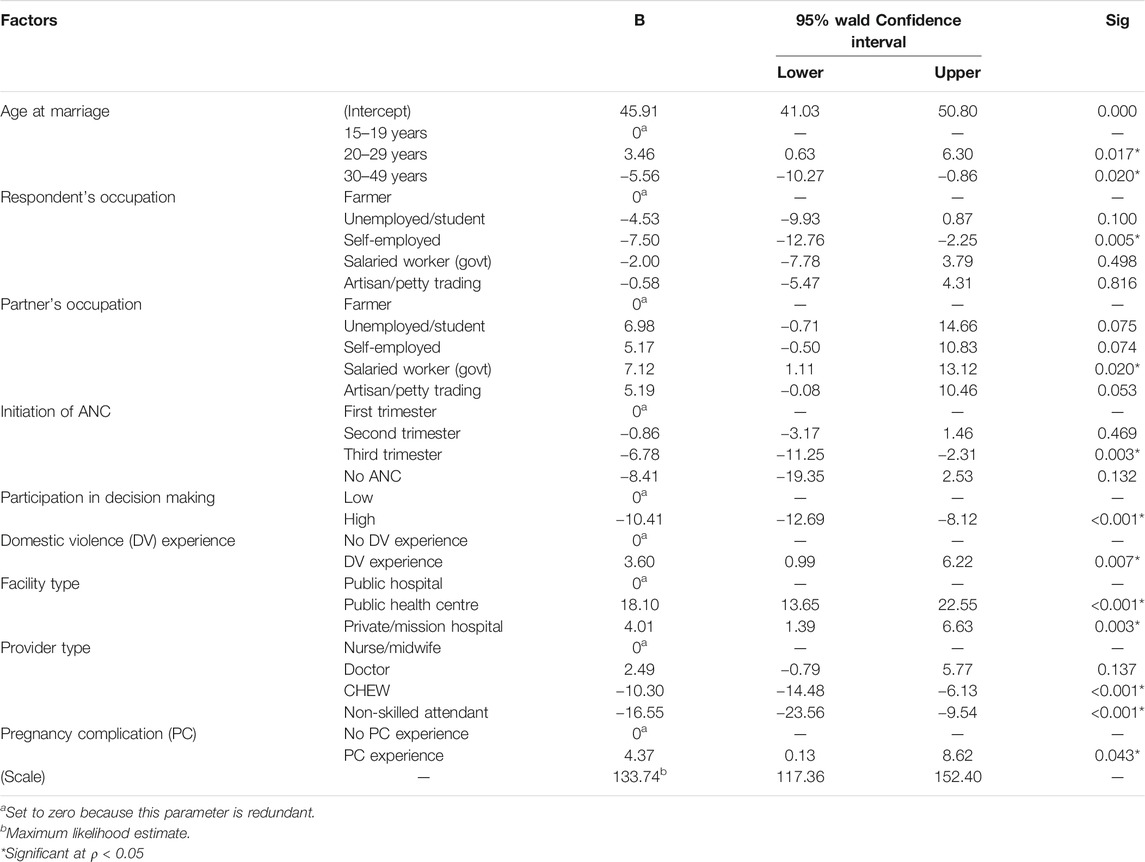
TABLE 7. Factors associated with perception of person-centred maternity care among post-partum women in Enugu State, Nigeria, 2019.
Discussion
The purpose of this study was to assess the perception of PCMC and its associated factors among post-partum women in Enugu State, Southeast Nigeria. Analysis of the findings reveals three areas that need to be explored further. The first is the psychometric properties of the PCMC scale. The second is the fact that PCMC is generally inadequate. The third relates to the factors associated with PCMC that can be considered for inclusion in intervention strategies to improve PCMC in Enugu State, Nigeria.
We found the PCMC scale to be a valid and reliable instrument for measuring women’s experiences of responsive and respectful care in the study population. The construct validity was high for the 22 items with adequate communalities and high rotated factor loading. The goodness-of-fit indices were generally adequate. The criterion validity was also high because total PCMC scores correlated strongly with women’s satisfaction with quality of maternal health services. Nonetheless, the two-factor solution for our data did not represent clear conceptual domains. For instance, factor 1 was dominant and included 20 items from the three domains. Consistent with evidence from Indian PCMC validation [4], we regrouped the retained items into three conceptual domains to provide the sub-scales for Dignity and respect, Autonomy and communication, and Supportive care. The full PCMC scale and its sub-scales had high reliability. Although our 22-item PCMC scale is shorter than the Kenyan and Indian PCMC scales their psychometric properties are consistent confirming that our PCMC scale has high construct validity, criterion validity, and reliability [1, 4]. Furthermore, our PCMC scale did not retain any factor with low communality and inadequate loading as were the case in previous studies [1, 4]. For instance, despite being theoretically relevant to PCMC, verbal and physical abuse are culturally accepted as normal and helpful to ensure positive childbirth outcomes in Nigeria and are underreported [20, 30]; and might not represent a good measure for women’s experiences with maternity care.
The study found that most women had low to medium scores on full PCMC scale and sub-scales, which are comparable to evidence from previous studies [1, 4–6]. The least proportion of women with high perception was communication and autonomy sub-scale, while highest proportion was respect and dignity dimension. However, there were considerable variations in individual PCMC items. Most women had high perceptions of respectful care, friendly care, visual privacy, and record confidentiality which are similar to existing evidence [4–6]. Lower score on communication and autonomy resulted from limited consented care, inadequate explanation of procedure and medicines, low involvement in decisions about women’s care, and not calling of women by their names. Our findings regarding these items of autonomy and communication were much lower than findings from previous studies [4–6]. Supportive care was constrained by restrictive labour companionship, inadequate support of anxious women, poor control of pain, dirty environment, and inadequate staffing. Evidence on these supportive care variables from previous studies are mixed suggesting that PCMC varies with context [4–6]. Improving PCMC would involve strengthening respectful care, visual privacy, and record confidentiality, informed consent, and interpersonal communication, and addressing gaps in facility-level drivers of low PCMC.
This study revealed that marriage at 20–29 years had a significant positive relationship with women’s perception of PCMC, similar to findings of a previous study [11]. Yet, marriage at 30–49 years had a significant inverse relationship with women’s perception of PCMC. The influence of age at marriage on PCMC might not simply reflect age, but also economic and educational empowerment given that nearly 60% of women in our sample belong to rich quintiles and most women have a minimum of secondary education. In Nigeria, women with no education marry 6 years earlier than women with secondary education, whereas women in the lowest wealth quintile marry eight years earlier than women in the highest quintile [24]. We argue that women, who marry at age 20–29 years, are better empowered, have higher expectation of care and can recognise low-quality care and advocate for improved care. However, women at age 30–49 years are better empowered than at age 20–29, giving them more freedom to take decisions and make personal choices [31], and as such, they tend to have a poorer perception of PCMC.
We found that self-employment had significant, but an inverse relationship with women’s perception of PCMC. An increase in self-employment would result in decrease in PCMC among self-employed women. This finding is comparable with evidence in Kenya which found that employment status predicted women’s perception of PCMC [7]. However, while the study in Kenya dichotomized occupation into unemployed and employed, our study used five occupational categories. Two factors could explain our findings. First self-employment could enhance women’s participation in household decision-making for their own healthcare [32]. Secondly, self-employment increases women’s economic empowerment, which means that women can effectively demand better maternity care [8, 32]. The empowered state makes the women more demanding of better PCMC, and as such, they tend to have a poorer perception than those who are less empowered, who might be more grateful for whatever PCMC they might get. As perception of PCMC varies with socio-economic status [5, 7], an increase in women’s labour participation that promotes self-employment is needed to improve person-centred maternity care.
Marriage to government workers had a significant positive relationship with women’s perception of PCMC. In Kenya, women’s perception of PCMC were associated with marrying petty traders but not government workers [7]. Prior studies indicate that men can provide substantial practical, financial, and emotional support to overcome demand-side barriers to accessing maternal health services and improve positive childbirth experiences [33]. It might be that in this study, government workers cared more for their pregnant partners and provided support during pregnancy and childbirth, which improved their perception of PCMC. Also, high cost is an important barrier to respectful maternity care and skilled delivery service in Nigeria [20]. It might be the case that women who are married to government workers are covered by formal sector health insurance scheme [34], or free maternal healthcare programme since evidence of public sector employment of a partner guaranteed women’s access to free care [35].
High participation in household decision-making was found to have an inverse relationship with women’s perception of PCMC in this study. Our results contrast findings of a prior study in Kenya which found that PCMC was not significantly related to participation in household decision-making [7]. In Nigeria, healthcare decisions for women are mostly made by their husbands/partners without women’s involvement [36]. It might be that low women’s decision-making autonomy limits women’s expectation of quality of maternity care, social power between women and providers, and women’s capacity to demand better care in Nigeria. Conversely, women who participate highly in household decisions are better aware of their rights to person-centred care and tend to have increased self-confidence thereby reducing power differential between health providers and women [20].
This study further revealed that women who had no domestic violence experience had significantly higher perception of PCMC than those who experienced domestic violence. Our finding, which is consistent with evidence from a prior study in Kenya [7], is expected because women who experience gender-based violence are disempowered and more vulnerable to dominance by providers [37]. Women who experience domestic violence are emotionally challenged. Women even when receiving technically sound care but lacking in emotional support perceive it as low-quality care [9]. Also, domestic violence limits women’s decision-making power regarding their reproductive health and have been associated with poor maternal health outcomes [38].
Trimester of commencing antenatal care predicted women’s perception of PCMC in this study. Women who commenced antenatal care during the third trimester were more likely to have a lower perception of person-centred maternity care than women who started antenatal care in their first trimester. Our findings are inconsistent with results of a previous Kenyan study [7]. Failure to initiate antenatal care early is a potential risk for complications during pregnancy and childbirth [39]. Tailored group educational activities and peer support motivates behaviour change among pregnant women and increases women’s satisfaction with maternity care [39]. In this study, late initiation of antenatal care meant that women are not familiar with the health system and might not have the benefit of psychological support and sharing of experiences which help women feel more empowered as decision makers during childbirth [40].
Moreover, women who were delivered in health centres and private/mission hospitals had higher PCMC scores than those delivered in public hospitals. Similar findings of higher PCMC were also found in health centres and private hospitals in Kenya [7]. Our findings support the evidence of higher interpersonal quality of maternal healthcare in health centres and private than public hospitals [9, 13, 15]. Conversely, indices of clinical quality of maternal health were higher in public hospitals than private hospitals and health centres [13, 14]. In this study, higher PCMC scores in health centres and private hospitals may be due to low provider-patient ratio which reduces the strain on provider-patient interaction [7]. Equally, higher PCMC scores in health centres might reflect closer ties between providers and women in closely knitted communities that health centres serve [7] and effect of citizen participation in governance of health centres [41]. In Nigeria, users have better perception of health workers in private facilities because private facilities greatly emphasize interpersonal quality [42].
Type of birth attendant was also found to predict women’s perception of PCMC in this study. PCMC was inversely and significantly related to delivery by community health workers and non-skilled attendants, although we expected a direct relationship given that negative attitudes and behaviours are commonly ascribed to trained professionals especially doctors and nurses [43]. Although women who were delivered by doctors received higher PCMC than those delivered by nurses, delivery by doctors was not significantly predictive. By contrast, PCMC was directly and significantly related to delivery by doctors in Kenya [7]. Higher perception of PCMC among women delivered by doctors than nurses is consistent with a Nigerian study showing that healthcare users have a better perception of doctors than nurses [42]. It could be that negative attitudes and behaviours are more common among nurses than doctors as hostile and impersonal behaviour from nurses and midwives are common reasons for dissatisfaction with quality of maternal health services in South-east Nigeria [44].
Furthermore, our study revealed that women who had pregnancy complications had higher PCMC scores than those without pregnancy complications; and experience of pregnancy complication significantly predicted perception of PCMC. Comparable results were found in Kenya, where women with severe pregnancy complication reported higher PCMC than other women [7]. By contrast, we expected that women with pregnancy complications will have significantly lower PCMC than those without complications. Our expectation is consistent with findings in previous studies showing that there were higher incidents of disrespectful care among women who experience pregnancy complications and longer labour durations requiring instrumental delivery and caesarean birth [11, 16–19]. It could be that survivors of pregnancy complication are more satisfied with their positive pregnancy outcomes and tend to report exaggerated positive patient experiences.
This study builds on current literature by adding validating PCMC scale in a Nigerian population and identifying factors that may be considered for inclusion in intervention strategies to improve PCMC in Nigeria. However, this study could have recall bias, though our respondents seemed to recall their childbirth experiences vividly. While women recall childbirth experiences accurately within twenty years [45], we adopted 9 weeks post-partum following a previous study [1] and because we thought that women would have the best chances of recall in the first few weeks following the post-partum period. Secondly, sampling bias is possible as only women who gave birth to live babies and attended immunization clinics were included. The study, therefore, potentially excluded women with stillbirths and neonatal deaths who may have had negative childbirth experiences. Finally, demographics of women attending immunization clinics in our study sites may not completely reflect demographics of post-partum women in Nigeria, possibly limiting generalizability of the study.
Conclusion
Evidence from this study indicate that PCMC scale is a valid and reliable instrument for measuring responsive and respectful maternity care. The study also reveal that PCMC is generally inadequate and associated with six patient characteristics (age at marriage, self-employment, married to government worker, high participation in household decisions, domestic violence experience, and initiation of antenatal care in the third trimester); two facility characteristics (facility type and provider type); and service type (pregnancy complication). This information should inform the design of interventions to promote positive childbirth experiences and evaluation of changes in the quality of maternity care.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by the Health Research Ethics Committee, University of Nigeria Teaching Hospital, Enugu, Nigeria. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
DO and CN conceptualised the study. DO and CN supervised the field work. DO analysed the data and drafted the manuscript. DO and CN contributed to the intellectual content of the article. DO finalised the article. All authors read and approved the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Afulani, PA, Diamond-Smith, N, Golub, G, and Sudhinaraset, M. Development of a Tool to Measure Person-Centered Maternity Care in Developing Settings: Validation in a Rural and Urban Kenyan Population. Reprod Health (2017). 14:118. doi:10.1186/s12978-017-0381-7
2. Downe, S, Lawrie, TA, Finlayson, K, and Oladapo, OT. Effectiveness of Respectful Care Policies for Women Using Routine Intrapartum Services: a Systematic Review. Reprod Health (2018). 15:23. doi:10.1186/s12978-018-0466-y
3. Larson, E, Sharma, J, Bohren, MA, and Tunçalp, Ö. When the Patient Is the Expert: Measuring Patient Experience and Satisfaction with Care. Bull World Health Organ (2019). 97:563–9. doi:10.2471/BLT.18.225201
4. Afulani, PA, Diamond-Smith, N, Phillips, B, Singhal, S, and Sudhinaraset, M. Validation of the Person-Centered Maternity Care Scale in India. Reprod Health (2018a). 15:147. doi:10.1186/s12978-018-0591-7
5. Afulani, PA, Phillips, B, Aborigo, RA, and Moyer, CA. Person-centred Maternity Care in Low-Income and Middle-Income Countries: Analysis of Data from Kenya, Ghana, and India. Lancet Glob Health (2019). 7:e96–e109. doi:10.1016/S2214-109X(18)30403-0
6. Sudhinaraset, M, Giessler, K, Golub, G, and Afulani, P. Providers and Women's Perspectives on Person-Centered Maternity Care: a Mixed Methods Study in Kenya. Int J Equity Health (2019a). 18:83. doi:10.1186/s12939-019-0980-8
7. Afulani, PA, Sayi, TS, and Montagu, D. Predictors of Person-Centered Maternity Care: the Role of Socioeconomic Status, Empowerment, and Facility Type. BMC Health Serv Res (2018b). 18:360. doi:10.1186/s12913-018-3183-x
8. Afulani, PA, Altman, M, Musana, J, and Sudhinaraset, M. Conceptualizing Pathways Linking Women's Empowerment and Prematurity in Developing Countries. BMC Pregnancy Childbirth (2017). 17:338. doi:10.1186/s12884-017-1502-6
9. Azhar, Z, Oyebode, O, and Masud, H. Disrespect and Abuse during Childbirth in District Gujrat, Pakistan: A Quest for Respectful Maternity Care. PLoS One (2018). 13:e0200318. doi:10.1371/journal.pone.0200318
10. Bobo, FT, Kasaye, HK, Etana, B, Woldie, M, and Feyissa, TR. Disrespect and Abuse during Childbirth in Western Ethiopia: Should Women Continue to Tolerate? PLoS One (2019). 14:e0217216. doi:10.1371/journal.pone.0217126
11. Gebremichael, MW, Worku, A, Medhanyie, AA, and Berhane, Y. Mothers' Experience of Disrespect and Abuse during Maternity Care in Northern Ethiopia. Glob Health Action (2018). 11:1465215. doi:10.1080/16549716.2018.1465215
12. Bohren, MA, Mehrtash, H, Fawole, B, Maung, TM, Balde, MD, Maya, E, et al. How Women Are Treated during Facility-Based Childbirth in Four Countries: a Cross-Sectional Study with Labour Observations and Community-Based Surveys. Lancet (2019). 394:1750–63. doi:10.1016/S0140-6736(19)31992-0
13. Diamond-Smith, N, Sudhinaraset, M, and Montagu, D. Clinical and Perceived Quality of Care for Maternal, Neonatal and Antenatal Care in Kenya and Namibia: the Service Provision Assessment. Reprod Health (2016). 13:92. doi:10.1186/s12978-016-0208-y
14. Hutchinson, PL, Do, M, and Agha, S. Measuring Client Satisfaction and the Quality of Family Planning Services: A Comparative Analysis of Public and Private Health Facilities in Tanzania, Kenya and Ghana. BMC Health Serv Res (2011). 11:203. doi:10.1186/1472-6963-11-203
15. Afulani, PA. Rural/Urban and Socioeconomic Differentials in Quality of Antenatal Care in Ghana. PLoS One (2015). 10:e117996. doi:10.1371/journal.pone.0117996
16. Colley, S, Kao, C-H, Gau, M, and Cheng, S-F. Women's Perception of Support and Control during Childbirth in the Gambia, a Quantitative Study on Dignified Facility-Based Intrapartum Care. BMC Pregnancy Childbirth (2018). 18:413. doi:10.1186/s12884-018-2025-5
17. Banks, KP, Karim, AM, Ratcliffe, HL, Betemariam, W, and Langer, A. Jeopardizing Quality at the Frontline of Healthcare: Prevalence and Risk Factors for Disrespect and Abuse during Facility-Based Childbirth in Ethiopia. Policy Plann (2018). 33:317–27. doi:10.1093/heapol/czx180
18. Galle, A, Manaharlal, H, Cumbane, E, Picardo, J, Griffin, S, Osman, N, et al. Disrespect and Abuse during Facility-Based Childbirth in Southern Mozambique: a Cross-Sectional Study. BMC Pregnancy Childbirth (2019). 19:369. doi:10.1186/s12884-019-2532-z
19. Wassihun, B, and Zeleke, S. Compassionate and Respectful Maternity Care during Facility Based Child Birth and Women's Intent to Use Maternity Service in Bahir Dar, Ethiopia. BMC Pregnancy Childbirth (2018). 18:294. doi:10.1186/s12884-018-1909-8
20. Ishola, F, Owolabi, O, and Filippi, V. Disrespect and Abuse of Women during Childbirth in Nigeria: A Systematic Review. PLoS One (2017). 12:e0174084. doi:10.1371/journal.pone.0174084
21. Ijadunola, MY, Olotu, EA, Oyedun, OO, Eferakeya, SO, Ilesanmi, FI, Fagbemi, AT, et al. Lifting the Veil on Disrespect and Abuse in Facility-Based Child Birth Care: Findings from South West Nigeria. BMC Pregnancy Childbirth (2019). 19:39. doi:10.1186/s12884-019-2188-8
22. Okafor, , Ugwu, EO, and Obi, SN. Disrespect and Abuse during Facility-Based Childbirth in a Low-Income Country. Int J Gynecol Obstet (2015). 128:110–3. doi:10.1016/j.ijgo.2014.08.015
23. Ogbuabor, DC, and Onwujekwe, OE. Implementation of Free Maternal and Child Healthcare Policies: Assessment of Influence of Context and Institutional Capacity of Health Facilities in South-East Nigeria. Glob Health Action (2018c). 11:1535031. doi:10.1080/16549716.2018.1535031
24.NPC NigeriaICF. Nigeria Demographic and Health Survey 2018. Abuja, Nigeria, and Rockville, Maryland, USA: National Population Commission and ICF (2019).
25. Ugwu, GO, Iyoke, C, Ezugwu, E, Ajah, L, Onah, H, and Ozumba, B. A Comparison of the Characteristics of Maternal Near-Misses and Maternal Deaths in Enugu, Southeast Nigeria: A 3-Year Prospective Study. Ijwh (2020). 12:207–11. doi:10.2147/IJWH.S237221
26.Metrics for Management. Nigeria Equity Tool. Metric for Measurement (2015). Available at: https://www.equitytool.org/nigeria/ (Accessed October 27, 2018).
27. Musonera, A, and Heshmati, A. Measuring Women's Empowerment in Rwanda. Institute for the Study of Labour (IZA) (2016).
28. Pituch, KA, and Stevens, JP. Applied Multivariate Statistics for the Social Sciences. 6th edn. New York and London: Routledge/Taylor & Francis Group (2016).
29. Sudhinaraset, M, Landrian, A, Afulani, PA, Diamond‐Smith, N, and Golub, G. Association between Person‐centered Maternity Care and Newborn Complications in Kenya. Int J Gynecol Obstet (2019b). 148:27–34. doi:10.1002/ijgo.12978
30. Bohren, MA, Vogel, JP, Tunçalp, Ö, Fawole, B, Titiloye, MA, Olutayo, AO, et al. Mistreatment of Women during Childbirth in Abuja, Nigeria: a Qualitative Study on Perceptions and Experiences of Women and Healthcare Providers. Reprod Health (2017). 14:9. doi:10.1186/s12978-016-0265-2
31. Agunwa, CC, Obi, IE, Ndu, AC, Omotowo, IB, Idoko, CA, Umeobieri, AK, et al. Determinants of Patterns of Maternal and Child Health Service Utilization in a Rural Community in South Eastern Nigeria. BMC Health Serv Res (2017). 17:715. doi:10.1186/s12913-017-2653-x
32. Asaolu, IO, Alaofè, H, Gunn, LKJ, Adu, KA, Monroy, JA, Ehiri, EJ, et al. Measuring Women's Empowerment in Sub-saharan Africa: Exploratory and Confirmatory Factor Analysis of the Demographic and Health Surveys. Front Psychol (2018). 9:994. doi:10.3389/fpsyg.2018.00994
33. Tokhi, M, Comrie-Thomson, L, Davis, J, Portela, A, Chersich, M, and Luchters, S. Involving Men to Improve Maternal and Newborn Health: A Systematic Review of the Effectiveness of Interventions. PLoS ONE (2018). 13:e0191620. doi:10.1371/journal.pone.0191620
34. Etiaba, E, Onwujekwe, O, Honda, A, Ibe, O, Uzochukwu, B, and Hanson, K. Strategic Purchasing for Universal Health Coverage: Examining the Purchaser-Provider Relationship within a Social Health Insurance Scheme in Nigeria. BMJ Glob Health (2018). 3:e000917. doi:10.1136/bmjgh-2018-000917
35. Ogbuabor, DC, and Onwujekwe, OE. Scaling-up Strategic Purchasing: Analysis of Health System Governance Imperatives for Strategic Purchasing in a Free Maternal and Child Healthcare Programme in Enugu State, Nigeria. BMC Health Serv Res (2018a). 18:245. doi:10.1186/s12913-018-3078-x
36. Osamor, P, and Grady, C. Factors Associated with Women's Health Care Decision-Making Autonomy: Empirical Evidence from Nigeria. J Biosoc Sci (2017). 50:70–85. doi:10.1017/S0021932017000037
37. Jewkes, R, and Penn-Kekana, L. Mistreatment of Women in Childbirth: Time for Action on This Important Dimension of Violence against Women. PLoSMed (2015). 12:e1001849. doi:10.1371/journal.pmed.1001849
38. Benebo, FO, Schumann, B, and Vaezghasemi, M. Intimate Partner Violence against Women in Nigeria: a Multilevel Study Investigating the Effect of Women's Status and Community Norms. BMC Women's Health (2018). 18:136. doi:10.1186/s12905-018-0628-7
39. Manyeh, AK, Amu, A, Williams, J, and Gyapong, M. Factors Associated with the Timing of Antenatal Clinic Attendance Among First-Time Mothers in Rural Southern Ghana. BMC Pregnancy Childbirth (2020). 20:47. doi:10.1186/s12884-020-2738-0
40. Rubashkin, N, Warnock, R, and Diamond-Smith, N. A Systematic Review of Person-Centered Care Interventions to Improve Quality of Facility-Based Delivery. Reprod Health (2018). 15:169. doi:10.1186/s12978-018-0588-2
41. Ogbuabor, DC, and Onwujekwe, OE. The Community Is Just a Small circle: Citizen Participation in the Free Maternal and Child Healthcare Programme of Enugu State, Nigeria. Glob Health Action (2018b). 11:1421002. doi:10.1080/16549716.2017.1421002
42. Odusanya, OO, Akinyinka, MR, Oluwole, EO, Odugbemi, BA, Bakare, OQ, and Adeniran, A. How Does the Public Perceive Healthcare Workers in Lagos? A Comparison of Health Workers in Public and Private Health Facilities. Niger Postgrad Med J (2018). 25:177–85. doi:10.4103/npmj.npmj_102_18
43. Mannava, P, Durrant, K, Fisher, J, Chersich, M, and Luchters, S. Attitudes and Behaviours of Maternal Health Care Providers in Interactions with Clients: a Systematic Review. Glob Health (2015). 11:36. doi:10.1186/s12992-015-0117-9
44. Uzochukwu, B, Onwujekwe, O, and Akpala, C. Community Satisfaction with the Quality of Maternal and Child Health Services in Southeast Nigeria. E Af Med Jrnl (2004). 81:293–9. doi:10.4314/eamj.v81i6.9178
Keywords: person-centred care, maternity care, respectful maternity care, responsive care, facility-based childbirth, Nigeria
Citation: Ogbuabor DC and Nwankwor C (2021) Perception of Person-Centred Maternity Care and Its Associated Factors Among Post-Partum Women: Evidence From a Cross-Sectional Study in Enugu State, Nigeria. Int J Public Health 66:612894. doi: 10.3389/ijph.2021.612894
Received: 01 October 2020; Accepted: 07 May 2021;
Published: 17 June 2021.
Edited by:
Lyda Osorio, University of Valle, ColombiaCopyright © 2021 Ogbuabor and Nwankwor. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Daniel C. Ogbuabor, ZGFuaWVsLm9nYnVhYm9yQHVubi5lZHUubmc=
 Daniel C. Ogbuabor1,2*
Daniel C. Ogbuabor1,2*