- 1Faculty I - Educational and Social Sciences, Institute for Social Sciences, Carl von Ossietzky University of Oldenburg, Oldenburg, Germany
- 2Population Research Centre, Faculty of Spatial Sciences, University of Groningen, Groningen, Netherlands
- 3Department of Economics, Econometrics and Finance, Faculty of Economics and Business, University of Groningen, Groningen, Netherlands
- 4Healthy Demography Centre, Prasanna School of Public Health, Manipal Academy for Higher Education, Manipal, India
Objective: This scoping review examines health outcome trends in European cross-border regions, identifies available evidence, and highlights research gaps. The European Union’s integration efforts aim to harmonise living standards and healthcare access. Removed border controls and freedom of movement enhanced service availability, benefiting populations in border regions with cross-border healthcare access. However, these populations are exposed to different institutional settings, highlighting health differences worth studying.
Methods: We employed the Joanna Briggs Institute methodology, using the PCC (Population-Concept-Context) framework to set eligibility criteria. The search covered literature databases and international governmental institution websites, yielding 785 studies, with 24 included in the final analysis.
Results: No comprehensive studies investigating longitudinal population health patterns were found. Instead, there are studies on specific diseases or health outcomes in particular border regions, especially around Germany. Most of these studies were cross-sectional. Five key research themes emerged: antibiotic resistance, COVID-19/SARS-CoV-2, other infectious diseases, cancer survival, and additional health outcomes.
Conclusion: The findings suggest that cross-border contexts have predominantly been used to study infectious disease spread, with little attention given to the broader impact of European integration on long-term health trends.
Introduction
Rationale
Europe has witnessed consistent improvements in living standards, working conditions, and cross-border collaborations [1, 2] over the past 30 years, in part thanks to the ongoing process of European integration aiming to promote unity and solidarity across the continent [3]. The Maastricht Treaty, signed in 1992, played a significant role in this integration by establishing the European Union (EU) and promoting the elimination of border controls. Member states have experienced economic growth since joining the EU [4, 5]. This economic growth, in turn, positively impacted population health, as an increase in GDP per capita is associated with an increase in life expectancy in the long run [6–9]. The removal of hard borders strengthened economic, political, and cultural exchange, contributing to the harmonisation of living conditions. The freedom to live and work in other member states and to use their infrastructure, such as healthcare, may have impacted overall life satisfaction, which in turn has a positive effect on health [10, 11].
Besides these potential indirect effects of European integration processes on health outcomes, reducing health inequalities within and between regions is also an explicit and central aim of the EU. With Directive 2011/24/EU [12], citizens can receive healthcare across member states without further costs, to converge health differences and synchronize healthcare among EU member states. Meanwhile, the EU provides structural funds, such as the European Regional Development Fund, to help disadvantaged regions address imbalances between them. Notably, the Interreg project is instrumental in fostering regional development, strengthening cohesion, and reducing economic disparities through cross-border collaboration [13]. Increased cooperation and the resulting knowledge exchange make border regions key contributors to European integration. Cross-border partnerships in the health sector exemplify the EU’s efforts toward harmonisation, as reflected in Directive 2011. However, despite these efforts, synchronising social and healthcare in the EU remains a challenge due to the fundamental differences between the systems in each state [14]. These differences are unlikely to change since the systems are deeply rooted in the fundamental structure of the states.
The COVID-19 pandemic has highlighted the critical need for improved cross-border health policies, revealing gaps in coordination and resource sharing [15]. In response, the EU introduced the European Health Union initiative [16], which aims to strengthen health coordination during crises and improve the resilience of healthcare systems across member states. These measures are designed to better prepare the EU for future cross-border health threats and pandemics while addressing disparities in healthcare provision. Cross-border regions offer a unique setting to explore health differences within the framework of European integration. These regions function as natural laboratories for studying the impact of varying policies and healthcare systems on health outcomes. Despite sharing cultural and historical similarities, populations on either side of a border operate within distinct institutional environments, including healthcare systems. Moreover, residents often benefit from access to infrastructure and services in neighboring countries.
Many European border regions are situated in rather remote and rural parts of the country, often far away from national central hubs of economic activity. This peripheral positioning is often characterised by limited development in terms of infrastructure, transportation, and overall accessibility. Consequently, these regions may have faced economic stagnation and a steady population decline, as residents migrated to urban centres in search of better opportunities [17]. Declining birth rates and high levels of out-migration have resulted in shrinking and ageing populations, leading to an uneven distribution of age groups and straining the local labour markets [18]. The impact of these dynamics is particularly evident in Eastern and Central Europe, where non-metropolitan regions have been experiencing pronounced population declines [19].
The core-periphery concept suggests that peripheral regions become dependent on central regions [20]; however, this can be reversible due to economic growth and the reorganization of activities in space [21–23]. Due to European integration and globalisation, cross-border areas might have shifted from those dependent peripheries to regions that now draw in new industries [24]. In fact, the opening of national borders has contributed to an increase in regional economic activity for border regions within Europe [25], particularly metropolitan border areas in Western Europe benefitted from better connectivity and economic prospect.
Insights on how these changes have impacted the health of cross-border populations over time remain limited in the literature. Existing research on health in Europe has conventionally emphasized within- or between-country comparisons, whereas these comparisons have rarely gone beyond national borders. While there is an ever-growing literature on health and morbidity at the sub-national level within the European Union [26–28], most of these studies are confined to provincial (NUTS-2) levels and do not specifically address (cross-) border regions. This limitation has hindered a comprehensive understanding of health outcomes on a regional scale across different countries. Therefore, it is imperative to broaden the scope of research to include cross-border comparisons that can provide insights into the drivers of the differences and similarities in health outcomes between regions. Such an approach would enable policymakers to develop more tailored and effective health policies that are better aligned with regional needs.
Objectives
Our scoping review seeks to systematically map the presence of empirical studies focusing on the differences and trends of health outcomes over time within various health policy frameworks for individuals residing in cross-border regions among EU and Schengen area member states. A comprehensive overview of health indicators in European cross-border areas since the establishment of the EU has not yet been conducted. We anticipate that such an overview could guide future research on health in EU cross-border regions by identifying evidence sources, cross-border data availability, and literature gaps. In our review, we focused on the following guiding questions:
a) Since the Maastricht Treaty was implemented in 1992, what is known regarding the differences and developments in health outcomes within EU cross-border regions?
b) What empirical evidence and data are available regarding differences in health across borders?
c) What gaps can be observed in the existing literature?
Methods
Due to the multidisciplinary and the diversity of the literature on health in cross-border regions, a scoping review is a suitable approach for this paper. We conducted an initial search of PubMed/MEDLINE, the Cochrane Database of Systematic Reviews, and Joanna Briggs Institute Evidence Synthesis. However, we did not discover any existing or ongoing systematic or scoping reviews related to the subject.
We followed the Joanna Briggs Institute methodology for scoping reviews [29, 30]. Additionally, we applied the Preferred Reporting Items for Systematic Reviews and Meta-Analysis extension for Scoping Reviews (PRISMA-ScR) as a framework to assist us in addressing the research question at hand [31]. The PRISMA-ScR checklist is provided in the Supplemental Material. In the following, we provide a summary of our inclusion criteria and methods for this scoping review. For more details, see our research protocol [32]. Following the suggestion of Pieper and colleagues, we reused text from our protocol in the introduction and method sections, as the research objectives and the methodology remained largely unchanged from the original plan [33].
Selection Criteria
We considered peer-reviewed articles as well as book chapters, policy reports, working papers, or organizational reports for inclusion in this review. Our search was limited to studies published exclusively in English. Furthermore, we disregarded studies published before 1992, that is, studies predating the Maastricht Treaty enactment in 1992 and its subsequent implementation in 1993. The selection criteria for inclusion and exclusion were developed under the Population, Concept, and Context (PCC) approach recommended by PRISMA-ScR.
First, the population of this scoping review encompassed all residents of varying age groups residing in cross-border regions of all EU member states and Schengen area countries. Second, the central concept was to explore disparities or similarities in health outcomes among the cross-border population in the European Union and how these outcomes have evolved. Health outcomes comprised mortality (e.g., life expectancy, survival rates), morbidity (e.g., disease prevalence, incidence rates), and measures of disease burden, which combine aspects of both morbidity and mortality. Third, our review focused on the context of European integration.
The Nomenclature of Territorial Units for Statistics (NUTS) classification, established by Eurostat and the European Commission, defines border regions as NUTS-3 areas that either share a land border or have more than half of their population living within 25 km of the border. However, limiting our search to a small scale would have excluded relevant studies that were conducted on a larger geographical scale. Therefore, we have also included studies that consider their study location as cross-border, even if it is at a larger regional scale, such as NUTS-2 level. The key requirement was that it must be at a subnational level so that a border region can be differentiated from the rest of the country.
Search Strategy and Data Management
We conducted a three-step search strategy in alignment with the PRISMA-ScR. After a preliminary search on PubMed and Scopus, we refined our search with updated keywords and index terms on the databases of PubMed, Scopus, Web of Science and SocIndex (EBSCOhost). We conducted a preliminary search in August 2022, followed by two updates in August 2023 and September 2024, to account for papers that have been published after our initial search. The search syntax was developed using three key terms based on the PCC framework: “cross-border” (Population), “European Union” (Context), and “health outcome” (Concept). For each key term, we included several related keywords and, when appropriate, relevant index terms. We also adapted the syntax for each database according to its specific syntax requirements. The complete search strategy syntax of all databases is provided in the Supplementary Material (See Supplementary Material S1 – Syntax and Key Terms). Furthermore, we examined reference lists of included articles and searched the publication websites of the World Health Organisation, the EU, and the Organization for Economic Co-operation and Development (OECD) for additional studies. Duplicates were identified and systematically removed with the help of the citation manager Zotero (V.6.0.29, 2023). Two independent reviewers assessed the titles and abstracts using the Rayyan software to ensure they met the eligibility criteria for this review. The full text of the selected articles was thoroughly assessed. Disagreements between the reviewers were resolved through joint discussion.
Data Analysis
After the selection process had been completed, we extracted the data from the final included studies. As proposed in our protocol, we extracted the following information: “Author,” “Location,” “Period (Year),” “Population,” “Method,” “Variable,” “Results,” “Data source,” and “Research Gaps.” We added the “Research Objective” to the table. The result chapter includes an abbreviated version of the table. Furthermore, we summarized evidence from the studies in the form of summary statistics, data visualisations (using R and Tableau Desktop), and narrative text.
Results
Study Selection
A comprehensive search was conducted across four databases, identifying a total of 1,535 records. After removing 750 duplicate records, the remaining 785 were screened based on their titles and abstracts. A total of 740 records were excluded based on our screening criteria. We then carefully analysed the full text of 45 articles and removed any records that did not meet our eligibility requirements. Reasons for exclusion included lack of regional focus, studies limited to one side of the border, and non-health-related outcome variables. To ensure a thorough search, we also examined websites, publication databases of European and health organizations, and reference lists of retrieved articles, which led to the inclusion of two additional records. The scoping review ultimately included 24 studies. Figure 1 displays the PRISMA-flow diagram, illustrating the sequential selection and exclusion of studies.
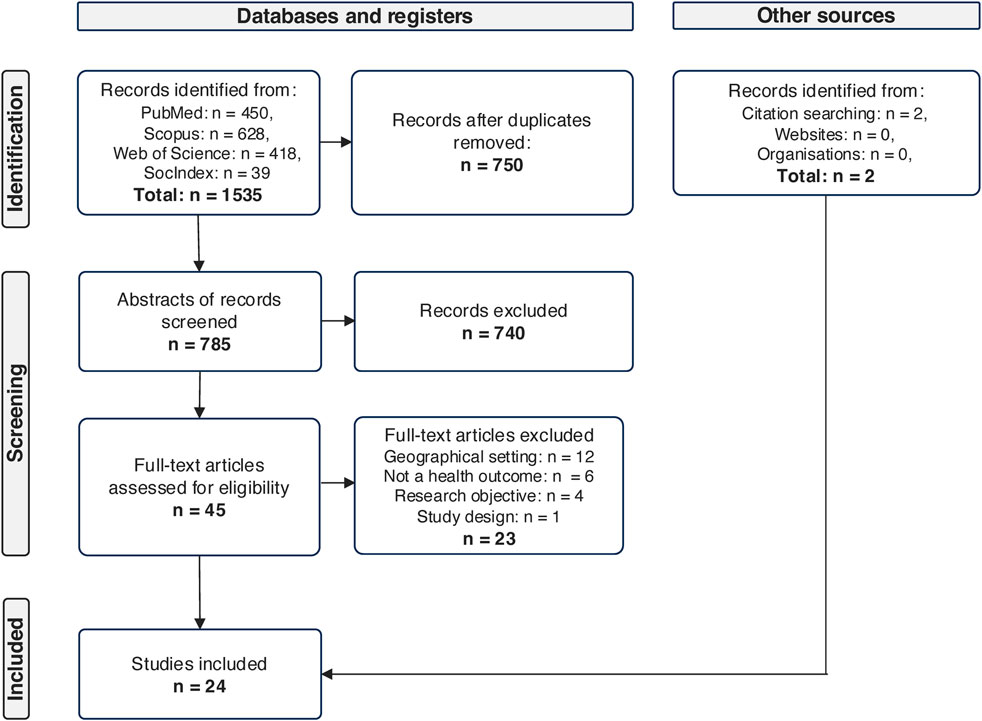
Figure 1. Flow diagram according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis extension for Scoping Reviews; based on Moher et al., 2009 (Netherlands, 2024).
Characteristics of the Articles
Most of the selected studies (n = 15) were cross-sectional epidemiological studies focusing on infectious diseases in a specific cross-border setting of two or three countries. Meanwhile, we did not detect comprehensive studies investigating health patterns over time on a macro level for several cross-border regions. Although we found studies that investigated differences in other health parameters such as cancer survival or physical health indicators, these were also limited temporally and geographically. We classified the results into five thematic groups based on the health parameters examined by the studies: Antibiotic resistance, COVID-19/SARS-CoV-2, other infectious diseases, cancer survival, and other health outcomes.
Year of Publication
The selected articles for review were published between 2005 and 2024. We did not find any article between the implementation of the Maastricht Treaty in 1992 and 2004. Only a few studies emerged in the 2000s and the number of studies published per year fluctuated. There were minor rises in 2015 and 2022, during which four and three studies were published, respectively. At the same time, we have seen an increase in studies since 2020, mainly due to the emergence of COVID-19 studies.
Temporal Coverage of the Data
Many of the eligible articles were cross-sectional epidemiological studies that focus on infectious diseases in a specific cross-border setting of two or three countries (see Figure 2 below for an overview of the respective observation windows). The earliest year of data utilization was in 1999 and the last in 2018 for studies on antibiotic resistance. Investigations on transnational cancer research were carried out during the interval spanning from 2004 to 2016. Subsequently, data commencing from the year 2020 were used in the context of studies about COVID-19 and SARS-CoV-2. Nine out of 24 used a longitudinal design with a diverse observation window. While COVID-19 studies use an observation period of up to 1 year, studies on cancer survival and other infectious diseases observe data for up to 9 years.
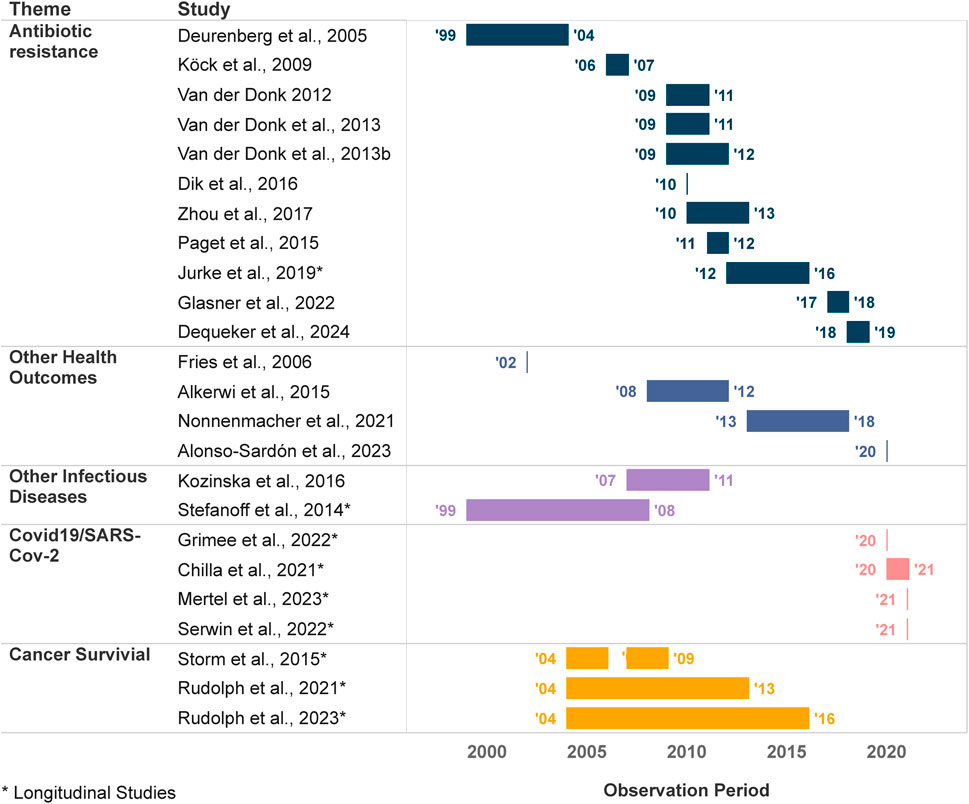
Figure 2. Temporal Coverage: Observation or data collection period of the selected articles (Netherlands, 2024).
Spatial Coverage of the Data
Figure 3 shows that the studies selected for analysis primarily focus on Western Europe. Of these, many studies (17 out of 24) cover research on Germany and its neighbouring countries only, with a particular clusteringin West-Germany, alongside the Dutch and Belgian border regions, of which the majority are studies on antibiotic resistance. Another regional cluster of research can be observed in the Fehmarn-Belt region, the border area between Denmark and Germany, where three cross-border studies on cancer survival were conducted. Studies in cross-border regions of Poland, Czechia, and Slovakia deal with the spread of other infectious diseases such as Mycobacterium tuberculosis and Tick-Borne Encephalitis and Lyme Borreliosis. One study on COVID-19 covered all German border regions, including those in neighbouring countries. Two additional COVID-19 studies were conducted in the Polish-German and Czech-German border regions, respectively, while one more study was conducted in Switzerland and Northern Italy. Other health outcomes have also been examined, such as the prevalence of neurodegenerative diseases in a Spanish-Portuguese cross-border region and the outcomes of cardiopulmonary resuscitation along the Dutch-Belgian-German border region.
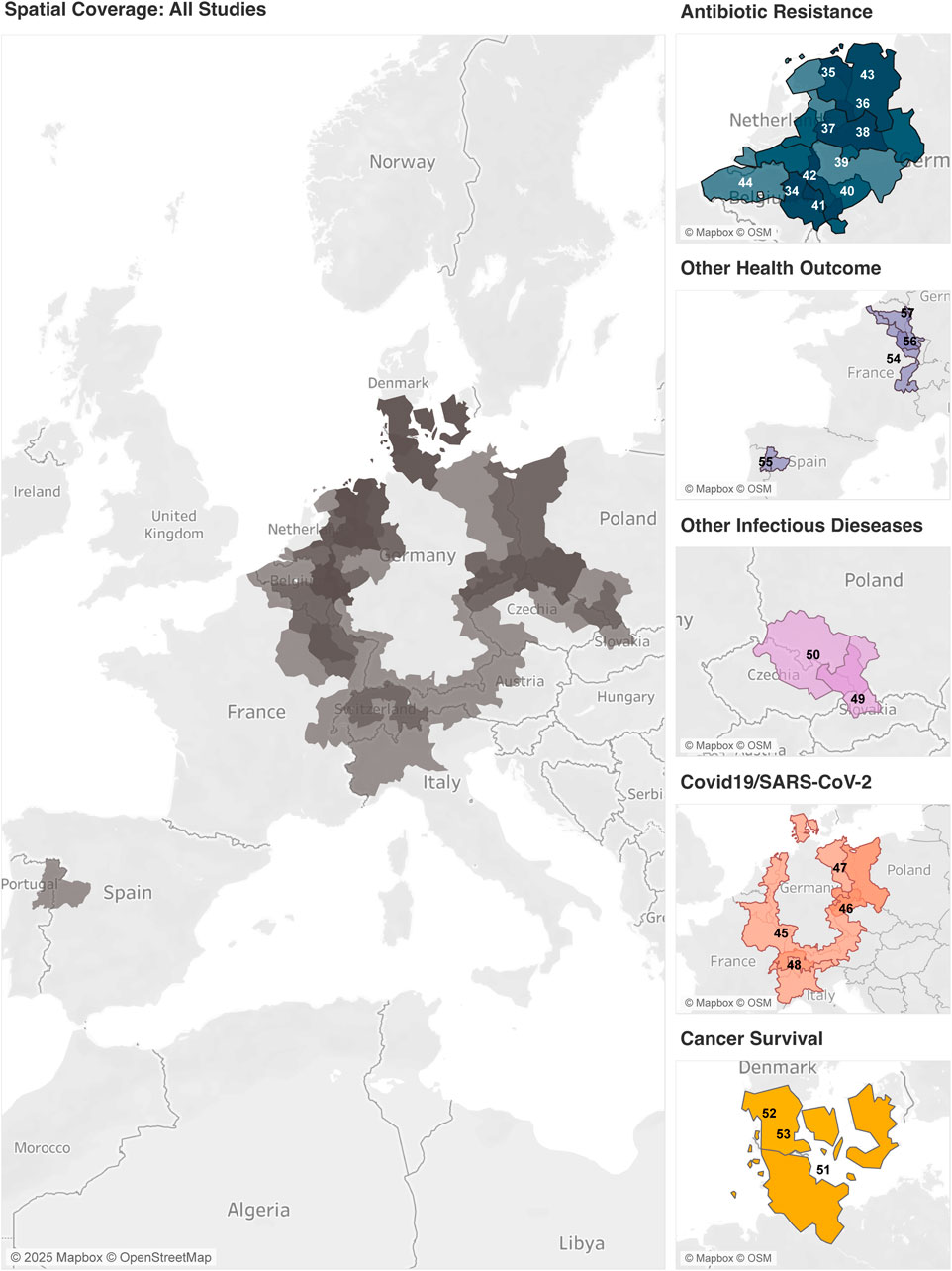
Figure 3. Geographical coverage of the selected studies. The map on the left summarises all studies in the scoping review. The maps on the right side are categorised according to the respective themes. The darker the shade, the more studies were conducted in the respective region. The numbers refer to the ID as indicated in Table 1 (Netherlands, 2024).
Data Sources
Microbiological data in many studies were collected through swabs taken from patients in participating healthcare institutions. This type of data collection was dominant in studies on antibiotic resistance. In some cases, questionnaires or patient documentation were used to supplement the data. Primary data was also collected through population-based surveys such as the European Labour Force Survey and the NESCaV (Nutrition, Environment and Cardiovascular Health) study. Secondary data was obtained from open and closed data sources, e.g., from health insurance companies, governments, national health ministries, and other institutions. This was particularly evident in studies on COVID-19/SARS-CoV-2 and cancer survival.
Synthesis of Results
A detailed summary of the results is presented in Table 1.
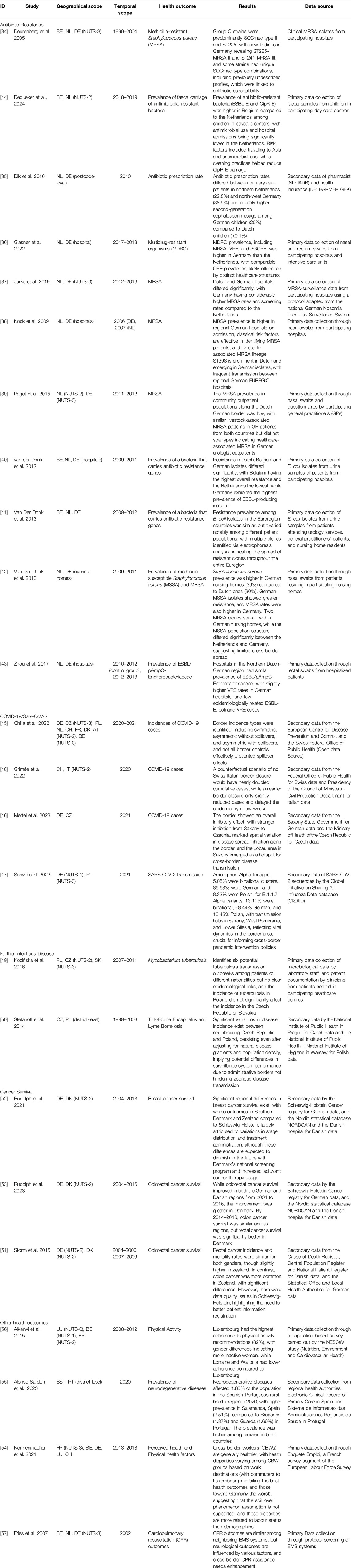
Table 1. A summarised overview of the selected studies and their characteristics (Netherlands, 2024).
Antibiotic Resistance
The selected studies on antibiotic resistance of our scoping review are clustered in the border region of Germany [34–43], Netherlands [34–44] and Belgium [34, 40, 41, 44]. These investigations delve into the epidemiology of various antibiotic-resistant pathogens, including Escherichia coli (E.coli) [40, 41, 43], methicillin-resistant Staphylococcus aureus (MRSA) [34, 36–39, 42], vancomycin-resistant Enterococcus faecium/E. faecalis (VRE) [36, 43, 44], ciprofloxacin-resistant Enterobacterales (CipR-E) [44], extended-spectrum beta-lactamase-producing Enterobacterales (ESBL-E) [40, 43, 44], third-generation cephalosporin-resistant (3GCRE) [36], carbapenemase-producing Enterobacterales (CPE) [44], and carbapenem-resistant Enterobacteriales (CRE) [36]. An additional paper [35] examined the prevalence of antibiotic prescriptions among primary care patients. It found that the proportion of German patients receiving at least one antibiotic was higher than that among Dutch patients, particularly among children. While one study finds similar MRSA prevalence and types among outpatients of general practitioners in Germany and the Netherlands [39], many studies show heterogeneities in multidrug resistance among the three countries. Germany shows a higher prevalence of resistance in MRSA [36–38, 42], VRE [36, 43] and CRE [36] compared to the Netherlands among intensive care patients [36], inpatients [37, 38, 43] and nursing home residents [42]. These differences can, among other things, be attributed to variations in healthcare structures and systems, such as higher antibiotic prescription rates [35], higher hospitalisation rates, and longer hospital stays [37]. Furthermore, variations in the examination of MRSA rates occurred within hospitals and even departments [38]. Additionally, the prevalence of multi-drug resistant E.coli isolates varied significantly in the German-Dutch-Belgian border region among different patient populations, with Belgium showing the highest prevalence and the Netherlands the lowest [40]. Another study in the same region reveals comparable E.coli resistance prevalence among the three countries but significant differences among various patient groups, with the highest prevalence observed in urology [41]. One study compares the border regions of the Netherlands and Belgium and finds a higher prevalence of ESBL-E and CipR-E in children attending daycare centres on the Belgian side [44]. Most of these studies lack additional clinical and patient information, primarily due to data availability issues, particularly concerning comorbidities.
COVID-19/SARS-CoV-2
Since 2020, studies examining COVID-19 with a focus on border-related aspects have emerged, primarily in the border regions of Germany and its neighbouring countries [45–47] and at the border regions of Switzerland and Italy [48]. These investigations aim to understand border incidence types and the effectiveness of border controls in mitigating spillover effects. The research findings reveal distinct patterns across different countries. A study establishes a typology by dividing neighbouring country pairs into symmetric and asymmetric pairs [45]. Symmetric pairs, such as DK-DE during the first wave, exhibit similar infection rates and trends on both sides of the border, suggesting that the border does not significantly impact infection dynamics. In contrast, asymmetric pairs without spillover effects, like BE-DE during the second wave, display significant differences in infection rates and their change over time, indicating the effectiveness of containment measures in preventing spillover. Furthermore, asymmetric pairs with spillover effects, exemplified by CZ-DE during the second wave, show varying infection rates that eventually converge over time, albeit with a time lag. This suggests the presence of spillover effects, particularly in German border regions [45]. Interestingly, an inhibitory effect of borders on COVID-19 transmission was observed in the German-Czech border region, although this effect is asymmetrical, with stronger inhibition from Germany to the Czech Republic than in the reverse direction [46]. Moreover, two specific hotspots for cross-border SARS-CoV-2 virus spread were identified. One hotspot encompassed the cross-border region including Saxony in Germany and West Pomerania as well as Lower Silesia in Poland, spanning the period from 2020 to 2021 [47]. Another hotspot was identified in the German-Czech border region [46]. Lastly, the impact of border closure on the prevalence of COVID-19 cases in the Swiss-Italian border region was quantified [48]. Counterfactual scenarios were modelled, revealing that the absence of border closure would have nearly doubled the cumulative cases of COVID-19 infections. An earlier border closure, although only slightly reducing cases, did manage to delay the epidemic by a few weeks.
Other Infectious Diseases
Beyond the extensive research on antibiotic resistance and COVID-19/SARS-CoV-2, additional studies have explored various infectious diseases [49, 50]. Notably, a transmission outbreak of Tuberculosis involving patients from different nationalities was detected in the Polish-Czech-Slovakian border region [50]. However, no epidemiological link was established, and incidences of tuberculosis in Poland did not significantly influence the incidence in neighbouring areas across the border. In a separate study encompassing the entire border region of the Czech Republic and Poland, the focus was on zoonotic diseases, specifically tick-borne encephalitis (TBE) and Lyme borreliosis (LB) [49]. Findings indicate persistent differences in disease incidence between these neighbouring countries. The Czech Republic exhibited a higher risk ratio for TBE and LB incidences, even after adjusting for epidemiological gradients and population density across the regions. This observation highlights the presence of substantial variations in surveillance systems between the two countries, suggesting that administrative borders alone do not fully account for the patterns of zoonotic diseases.
Cancer Survival
In cross-border research within the Fehmarn Belt region, which encompasses the state of Schleswig-Holstein in Germany and the region Zealand [51] in Denmark, along with the region of Southern Denmark [52, 53], two studies have illuminated regional disparities in cancer survival, with more favourable outcomes observed among German patients. This overarching theme of regional variations is particularly pronounced in cases of breast and colon cancer. Specifically, breast cancer patients in the Danish border region exhibited significantly lower overall cancer survival rates compared to their counterparts in the German border regions [52]. These differences appear to stem from variations in cancer screening and treatment protocols. Germany initiated breast cancer screening and adjuvant cancer therapy earlier than Denmark. However, the implementation of national cancer screening and therapy plans by Denmark is viewed as a potential means to narrow the cancer survival gap between the regions. Similar patterns emerged in the case of colon cancer patients [51], with Schleswig-Holstein showing a lower incidence rate, lower mortality rate, and higher survival rate compared to Zealand. However, the disparities were less pronounced among rectum cancer patients. The study was conducted again with updated data, which showed that the Danish border region caught up with and even surpassed the German border regions [53]. By the end of the observation period, survival rates for colon cancer were similar across the border, while survival rates for rectal cancer were higher in Danish border regions. Concerns were raised regarding data availability and, consequently, the comparability of cancer survival between the two countries. Notably, cases in Germany were primarily known from death certificates, and information regarding co-morbidities or socio-economic characteristics of the study population was lacking in both studies.
Other Health Outcomes
Studies focusing on other health outcomes were found in French [54], Spanish-Portuguese [55], Belgian-Luxembourgish-French [56] and Dutch-German-Belgian [57] border regions. Cross-border workers (CBWs) have better health outcomes and higher income compared to non-cross-border workers (NCBWs), showing a strong positive correlation between income and health [54]. In this paper, health is measured from five self-reported health variables, i.e., low perceived health, activity limitation, chronic diseases, disabilities, and lack of leisure activities. The disparities of these combined health outcomes among CBWs are linked to work destinations. Commuters to Luxembourg reported better self-reported health while commuters to Germany reported the worst. In another study, it was shown that individuals living in Luxembourg have a higher likelihood of meeting the physical activity recommendation, defined by the World Health Organisation, compared to the neighbouring regions, Wallonia in Belgium and Lorraine in France [56]. In the border regions between Spain and Portugal, variations in the prevalence of neurodegenerative diseases have been observed [55]. The prevalence is higher in the Spanish border region compared to the Portuguese counterpart. Furthermore, the prevalence in the entire cross-border region exceeds the European and global averages, presumably attributed to the rurality of the region and its significant elderly population. Lastly, outcomes of cardiopulmonary resuscitation were similar in Belgium, the Netherlands and Germany, even though medical and organisational differences among the three emergency medical services exist [57]. Furthermore, cross-border emergency assistance for cardiopulmonary resuscitation was hardly identified, which could be related to legal and communication obstacles.
Discussion
This scoping review searched for trends and differences in health outcomes in cross-border regions within the EU. It uncovered 785 distinct studies, of which only 24 met our eligibility criteria. Most of the studies were excluded due to wrong geographical settings, health outcomes, research objectives or study design. Based on the health outcomes analysed by the included studies, we identified five thematic and geographic clusters: Antibiotic resistance, COVID-19/SARS-CoV-2, other infectious diseases, cancer survival, and other health outcomes. While the setting of EU border regions is mainly used to investigate various infectious diseases transmitted from one country to another, macro health levels and trends, such as mortality and morbidity outcomes, are sparsely represented in the literature corpus.
We have discussed the health differences of cross-border regions that resulted from the selected studies. However, we know very little about how these differences in health outcomes developed over time. Moreover, no references are being made to how health trends relate to EU integration processes. This is due to two reasons; First, we did not find any study that started its observation period at the foundation of the EU in 1992 when the Maastricht Treaty was signed. The data collected only goes back to 1999. Second, most studies are cross-sectional rather than longitudinal, which means that the health parameters are rarely observed over multiple years. Studies on COVID-19 do examine the incidence rates and changes over time, but due to the recent emergence of the virus, the study period is rather short. As an exception, three studies are looking at the trends of health outcomes for a longer period [50, 52, 53].
In addition to the temporal limitations of the studies, we have identified gaps in the spatial coverage. Almost all studies are focused on a particular cross-border region of two or three countries. Only one study has compared the outcomes of German border regions with those of all its eight neighbouring countries. Moreover, the study regions of the articles are mainly clustered among Central and Western European countries. Specifically, German, Dutch, Belgian, and French border regions are well represented in this scoping review. However, we noticed a lack of studies on border regions from Eastern, Southern and Northern European countries, as well as a comprehensive overview of multiple, or even all member states.
Studies on infectious diseases mostly use the cross-border setting to detect their spread across borders, due to the high cross-border mobility of patients, workers, and tourists. Especially, studies on antibiotic resistance do address that the border region of Germany and the Netherlands may serve as a “living lab,” stressing the importance of the different healthcare systems, practices, protocols, and surveillance in the healthcare units on both sides of the border. Interestingly, although not its main focus, one study showed that living closer to the border seems to increase antibiotic consumption, which the authors explain by the fact that cross-border regions are further away from the medical centre of the respective countries and exhibit lower socioeconomic status, both of which are associated with antibiotic consumption [35]. This outcome is a minor side result, mentioned only briefly in the text and not listed as a main result. Yet, we do not know how opening the border affected the prevalence of different antibiotic resistance of the patients in those cross-border regions. Furthermore, in the studies on cancer survival [51–53] and adherence to physical activity recommendations [56], regional comparisons rarely yield anything specific about cross-border regions and their populations as such. Instead, it seems that they are used to compare countries, making border regions merely placeholders for the entire country. The only study that appears to directly address cross-border populations as distinct is by Nonnenmacher and colleagues [54] who compared several health outcomes of cross-border workers and non-cross-border workers.
A potential reason for the research gaps is the lack of cross-border data that is both available at a regional level and comparable across all member states. Countries may have different definitions and registration systems in their healthcare systems, making it challenging to gather comparable data. This was particularly evident in the studies on cancer survival [51–53] in Denmark and Germany, which addressed the different registrations of cancer in the respective countries. As a result, caution is required when interpreting the survival rates.
This review emphasises the need to strengthen infrastructure for data sharing and collaboration between border regions. There are some positive developments in this area, such as the establishment of a regional health atlas by Meuse-Rhine-Euroregion, which covers indicators on mortality and healthcare resources [58]. Additionally, the Cross-Border Institute of Healthcare Systems and Prevention is creating a health atlas and data inventory for the Ems-Dollard Region to facilitate cross-border research. While these initiatives demonstrate how localized efforts can inform broader policy frameworks, it is essential to scale such projects across all member states to ensure equitable and effective health interventions. Eurostat published an atlas on mortality statistics in the EU in 2002 [59], which was updated with new data in 2009 [60]. However, there have been no further updates since then. Although open data sources like Eurostat and the Atlas of Population Health in European Union Regions [61], provide useful overviews of regional health in the EU, they either date back 10 years or are limited to NUTS-2 regions, making it difficult to identify border regions. Robust cross-border policies are needed, similar to those envisioned in the European Health Union initiative, to mitigate these challenges. Such policies would foster standardised data collection and uniform reporting mechanisms, as well as facilitate the use of this data at a subnational level.
Limitations
This scoping review also comes with limitations. Since we restricted our search to English publications exclusively, there is a possibility that we might have left out pertinent studies that were published in a different language and could have been relevant to our research. This may be especially relevant for national reports published in the country’s official language. For example, publications regarding COVID-19 cases, such as the report on the impact of the COVID-19 crisis in German border regions by the Federal Office for Building and Regional Planning [62], or studies on cross-border infection threats in border areas, may have been excluded from this study. Furthermore, we limited our scope to published studies and reports. While this approach is common practice in literature reviews, it may result in a publication bias, as unpublished or grey literature was not considered. Ultimately, our review focused exclusively on health outcomes of the population. Consequently, we did not consider studies addressing socio-economic factors and determinants of health, which could additionally explain our lack of findings related to health trends and European integration. Including socio-economic factors in our search, however, was beyond the scope of our research. Our primary objective was to compile literature on the differences in health outcomes among European cross-border regions at a macro level. Moreover, focusing on population health determinants and contextual factors could be a promising addition to this work in the future, as they could provide deeper insights into the underlying mechanisms of cross-border health disparities and trends.
Conclusion
In this scoping review, we identified temporal, geographical, and thematic gaps in the literature. The studies found were predominantly epidemiological, cross-sectional studies covering a specific border region. Research on infectious diseases, such as antibiotic resistance and, more recently, on COVID-19, was particularly dominant. Meanwhile, studies on macro-level health trends in cross-border regions were lacking in the scanned literature. This is a significant shortcoming in the existing literature since cross-border regions could act as “living labs” for evaluating the effectiveness of European integration. Additionally, health profiles of cross-border regions can serve as benchmarks for measuring successful regional convergence of living standards. Therefore, more health-relevant data and research are needed on health trends and their underlying determinants to identify best practices that can aid policymaking, not just in the health domain but also for those concerned with European integration.
Author Contributions
TV initiated and conceptualised the study. SSt and TV developed the search strategy. SSt, VA, SSc, and TV designed the methods and participated in the data analysis. SSt wrote the draft of the manuscript. TV, VA, and SSc contributed to the drafting and editing of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This project was funded by the Ministry of Science and Culture of Lower Saxony (MWK) as part of the Niedersächsisches “Vorab” Program. (Grant Agreement No. ZN3730).
Conflict of Interest
The authors declare that they do not have any conflicts of interest.
Generative AI Statement
The author(s) declare that Generative AI was used in the creation of this manuscript. During the preparation of this work, we used Grammarly to improve language and readability. After using this tool, we reviewed and edited the content as needed. We take full responsibility for the content of the publication.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/phrs.2025.1608170/full#supplementary-material
References
1. Brandolini, A, and Rosolia, A. The Distribution of Well-Being Among Europeans. In: G Fischer, and R Strauss, editors. Europe’s Income, Wealth, Consumption, and Inequality. Oxford University Press (2021). 39–103. doi:10.1093/oso/9780197545706.003.0002
2. Medeiros, E. Should EU Cross-Border Cooperation Programmes Focus Mainly on Reducing Border Obstacles? Documents d’Anàlisi Geogràfica (2018) 64(3):467–91. doi:10.5565/rev/dag.517
3. Grosse Hüttmann, M, and Wehling, HG. Das Europalexikon. 2. In: überarbeitete und erweiterte. Dietz: Aufl. Bonn (2013).
4. Campos, NF, Coricelli, F, and Moretti, L. Institutional Integration and Economic Growth in Europe. J Monetary Econ (2019) 103:88–104. doi:10.1016/j.jmoneco.2018.08.001
5. Mann, K. The EU, a Growth Engine? The Impact of European Integration on Economic Growth in Central Eastern Europe. Vienna: FIW Research Centre International Economics (2015). Available from: https://www.econstor.eu/handle/10419/121136 (Accessed August 5, 2022).
6. Preston, SH. The Changing Relation between Mortality and Level of Economic Development. Bull World Health Organ (1975) 81(11):833–41. doi:10.1093/ije/dym075
7. Swift, R. The Relationship between Health and GDP in OECD Countries in the Very Long Run. Health Econ (2011) 20(3):306–22. doi:10.1002/hec.1590
8. Weil, DN. Health and Economic Growth. In: Handbook of Economic Growth. Elsevier (2014). 623–82. doi:10.1016/B978-0-444-53540-5.00003-3
9. Shkolnikov, VM, Andreev, EM, Tursun-zade, R, and Leon, DA. Patterns in the Relationship between Life Expectancy and Gross Domestic Product in Russia in 2005–15: A Cross-Sectional Analysis. Lancet Public Health (2019) 4(4):e181–8. doi:10.1016/S2468-2667(19)30036-2
10. Grant, N, Wardle, J, and Steptoe, A. The Relationship between Life Satisfaction and Health Behavior: A Cross-Cultural Analysis of Young Adults. Intj Behav Med (2009) 16(3):259–68. doi:10.1007/s12529-009-9032-x
11. Strine, TW, Chapman, DP, Balluz, LS, Moriarty, DG, and Mokdad, AH. The Associations between Life Satisfaction and Health-Related Quality of Life, Chronic Illness, and Health Behaviors Among U.S. Community-Dwelling Adults. J Community Health (2008) 33(1):40–50. doi:10.1007/s10900-007-9066-4
12. European Parliament, Council of the European Union. Directive 2011/24/EU of the European Parliament and of the Council of 9 March 2011 on the Application of Patients’ Rights in Cross-Border Healthcare. OJ L Mar (2011) 9. Available from: http://data.europa.eu/eli/dir/2011/24/oj/eng (Accessed March 21, 2022).
13. European Commission. Inforegio - European Regional Development Fund (2021). Available from: https://ec.europa.eu/regional_policy/funding/erdf_en (Accessed November 2, 2023).
14. Reibling, N. Healthcare Systems in Europe: Towards an Incorporation of Patient Access. J Eur Soc Pol (2010) 20(1):5–18. doi:10.1177/0958928709352406
15. Leloup, F. Research for REGI Committee - Cross-Border Cooperation in Healthcare. Brussels, Belgium (2021).
16. European Commission. Communication From the Commission to the European Parliament, the Council, the European Economic and Social Committee and the Committee of the Regions Building a European Health Union: Reinforcing the EU’s Resilience for Cross-Border Health Threats (2020). Available from: https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=celex:52020DC0724 (Accessed January 15, 2025).
17. Young, N. Globalization from the Edge: A Framework for Understanding How Small and Medium-Sized Firms in the Periphery Go Global. Environ Plan A (2010) 42(4):838–55. doi:10.1068/a42315
18. Pawlewicz, K, Senetra, A, Gwiaździńska-Goraj, M, and Krupickaitė, D. Differences in the Environmental, Social and Economic Development of Polish–Lithuanian Trans-Border Regions. Soc Indic Res (2020) 147(3):1015–38. doi:10.1007/s11205-019-02179-9
19. Sohn, C, and Stambolic, N. The Urban Development of European Border Regions: A Spatial Typology. Europa Reg (2013) 21:177–89.
21. Keim, KD. Peripherisierung ländlicher räume. aus Politik und Zeitgeschichte (2006) 37(2006):3–7.
22. Krugman, P. History and Industry Location: The Case of the Manufacturing Belt. Am Econ Rev (1991) 81(2):80–3.
23. Krugman, P. The Role of Geography in Development. Int Reg Sci Rev (1999) 22(2):142–61. doi:10.1177/016001799761012307
24. Şlusarciuc, M. The Economic Potential of Crossborder Areas. Opportunities and Threats. Proced Econ Finance (2015) 32:801–8. doi:10.1016/S2212-5671(15)01465-3
25. Basboga, K. The Role of Open Borders and Cross-Border Cooperation in Regional Growth across Europe. Reg Stud Reg Sci (2020) 7(1):532–49. doi:10.1080/21681376.2020.1842800
26. Shaw, M, Orford, S, Brimblecombe, N, and Dorling, D. Widening Inequality in Mortality between 160 Regions of 15 European Countries in the Early 1990s. Soc Sci and Med (2000) 50(7–8):1047–58. doi:10.1016/S0277-9536(99)00354-8
27. Maynou, L, Saez, M, Bacaria, J, and Lopez-Casasnovas, G. Health Inequalities in the European Union: An Empirical Analysis of the Dynamics of Regional Differences. Eur J Health Econ (2015) 16(5):543–59. doi:10.1007/s10198-014-0609-1
28. Hrzic, R, Vogt, T, Brand, H, and Janssen, F. The Short-Term Effects of European Integration on Mortality Convergence: A Case Study of European Union’s 2004 Enlargement. Eur J Popul (2021) 37(4–5):909–31. doi:10.1007/s10680-021-09596-y
29. Peters, MDJ, Godfrey, CM, Khalil, H, McInerney, P, Parker, D, and Soares, CB. Guidance for Conducting Systematic Scoping Reviews. Int J Evidence-Based Healthc (2015) 13(3):141–6. doi:10.1097/XEB.0000000000000050
30. Peters, MDJ, Marnie, C, Tricco, AC, Pollock, D, Munn, Z, Alexander, L, et al. Updated Methodological Guidance for the Conduct of Scoping Reviews. JBI Evid Synth (2020) 18(10):2119–26. doi:10.11124/JBIES-20-00167
31. Tricco, AC, Lillie, E, Zarin, W, O’Brien, KK, Colquhoun, H, Levac, D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med (2018) 169(7):467–73. doi:10.7326/M18-0850
32. Stroisch, S, Angelini, V, Schnettler, S, and Vogt, T. Population Health differences in Cross-Border Regions Within the European Union and Schengen Area: A protocol for a Scoping Review. BMJ Open (2023) 13(8):e068571. doi:10.1136/bmjopen-2022-068571
33. Pieper, D, Ge, L, and Abou-Setta, A. Is Reusing Text From a Protocol in the Completed Systematic Review Acceptable? Syst Rev (2021) 10(1):131. doi:10.1186/s13643-021-01675-9
34. Deurenberg, RH, Vink, C, Oudhuis, GJ, Mooij, JE, Driessen, C, Coppens, G, et al. Different Clonal Complexes of Methicillin-Resistant Staphylococcus aureus Are Disseminated in the Euregio Meuse-Rhine Region. Antimicrob Agents Chemother (2005) 49:4263–71. doi:10.1128/AAC.49.10.4263-4271.2005
35. Dik, JWH, Sinha, B, Friedrich, AW, Lo-Ten-Foe, JR, Hendrix, R, Köck, R, et al. Cross-Border Comparison of Antibiotic Prescriptions Among Children and Adolescents between the North of the Netherlands and the North-West of Germany. Antimicrob Resist Infect Control (2016) 5(1):14. doi:10.1186/s13756-016-0113-8
36. Glasner, C, Berends, MS, Becker, K, Esser, J, Gieffers, J, Jurke, A, et al. A Prospective Multicentre Screening Study on Multidrug-Resistant Organisms in Intensive Care Units in the Dutch–German Cross-Border Region, 2017 to 2018: The Importance of Healthcare Structures. Eurosurveillance (2022) 27(5):2001660. doi:10.2807/1560-7917.ES.2022.27.5.2001660
37. Jurke, A, Daniels-Haardt, I, Silvis, W, Berends, MS, Glasner, C, Becker, K, et al. Changing Epidemiology of Meticillin-Resistant Staphylococcus aureus in 42 Hospitals in the Dutch–German Border Region, 2012 to 2016: Results of the Search-And-Follow-Policy. Eurosurveillance (2019) 24(15):1800244. doi:10.2807/1560-7917.ES.2019.24.15.1800244
38. Köck, R, Brakensiek, L, Mellmann, A, Kipp, F, Henderikx, M, Harmsen, D, et al. Cross-Border Comparison of the Admission Prevalence and Clonal Structure of Meticillin-Resistant Staphylococcus aureus. J Hosp Infect (2009) 71:320–6. doi:10.1016/j.jhin.2008.12.001
39. Paget, J, Aangenend, H, Kühn, M, Hautvast, J, Van Oorschot, D, Olde Loohuis, A, et al. MRSA Carriage in Community Outpatients: A Cross-Sectional Prevalence Study in a High-Density Livestock Farming Area along the Dutch-German Border. PLoS One (2015) 10(11):e0139589. doi:10.1371/journal.pone.0139589
40. van der Donk, CFM, van de Bovenkamp, JHB, De Brauwer, EIGB, De Mol, P, Feldhoff, KH, Kalka-Moll, WM, et al. Antimicrobial Resistance and Spread of Multi Drug Resistant Escherichia coli Isolates Collected from Nine Urology Services in the Euregion Meuse-Rhine. PloS One (2012) 7:e47707. doi:10.1371/journal.pone.0047707
41. Van Der Donk, C, Van De Bovenkamp, J, Bamelis, H, Driessen, C, Feldhoff, KH, Kalka-Moll, W, et al. Prevalence and Spread of Multidrug-Resistant Escherichia coli Including ST131 in Different Patient Populations in the Euroregion Meuse-Rhine. Future Microbiol (2013) 8:1027–37. doi:10.2217/fmb.13.61
42. van der Donk, CFM, Schols, JMGA, Schneiders, V, Grimm, KH, and Stobberingh, EE. Antibiotic Resistance, Population Structure and Spread of Staphylococcus aureus in Nursing Homes in the Euregion Meuse-Rhine. Eur J Clin Microbiol Infect Dis (2013) 32(11):1483–9. doi:10.1007/s10096-013-1901-1
43. Zhou, X, García-Cobos, S, Ruijs, GJHM, Kampinga, GA, Arends, JP, Borst, DM, et al. Epidemiology of Extended-Spectrum β-Lactamase-Producing E. coli and Vancomycin-Resistant Enterococci in the Northern Dutch-German Cross-Border Region. Front Microbiol (2017) 8:1914. doi:10.3389/fmicb.2017.01914
44. Dequeker, S, Van Hensbergen, M, Den Heijer, CDJ, Dhaeze, W, Raven, SFH, Ewalts-Hakkoer, H, et al. Cross-Border Differences in the Prevalence and Risk Factors for Carriage of Antimicrobial Resistance in Children Attending Daycare Centers: A Point Prevalence Study in the Netherlands and Belgium. BMC Infect Dis (2024) 24(1):131. doi:10.1186/s12879-024-08996-9
45. Chilla, T, Große, T, Hippe, S, and Walker, BB. COVID-19 Incidence in Border Regions: Spatiotemporal Patterns and Border Control Measures. Public health (2022) 202:80–3. doi:10.1016/j.puhe.2021.11.006
46. Mertel, A, Vyskočil, J, Schüler, L, Schlechte-Wełnicz, W, and Calabrese, JM. Fine-Scale Variation in the Effect of National Border on COVID-19 Spread: A Case Study of the Saxon-Czech Border Region. Spat Spatiotemporal Epidemiol (2023) 44:100560. doi:10.1016/j.sste.2022.100560
47. Serwin, K, Aksak-Wąs, B, and Parczewski, M. Phylodynamic Dispersal of SARS-CoV-2 Lineages Circulating across Polish–German Border Provinces. Viruses (2022) 14(5):884. doi:10.3390/v14050884
48. Grimée, M, Bekker-Nielsen, DM, Hofmann, F, and Held, L, SUSPend Modelling Consortium. Modelling the Effect of a Border Closure between Switzerland and Italy on the Spatiotemporal Spread of COVID-19 in Switzerland. Spat Stat (2022) 49:100552. doi:10.1016/j.spasta.2021.100552
49. Kozińska, M, Zientek, J, Augustynowicz-Kopeć, E, Zwolska, Z, and Kozielski, J. Transmission of Tuberculosis Among People Living in the Border Areas of Poland, the Czech Republic, and Slovakia. Pol Arch Med Wewn (2016) 126:32–40. doi:10.20452/pamw.3263
50. Stefanoff, P, Orlíková, H, Príkazský, V, Beneš, Č, and Rosińska, M. Cross-Border Surveillance Differences: Tick-Borne Encephalitis and Lyme Borreliosis in the Czech Republic and Poland, 1999-2008. Cent Eur J Public Health (2014) 22:54–9. doi:10.21101/cejph.a3937
51. Storm, HH, Engholm, G, Pritzkuleit, R, Kejs, AMT, Katalinic, A, Dunst, J, et al. Less Pitfalls and Variation in Population Based Cancer Survival Comparisons Within the European Union: Lessons From Colorectal Cancer Patients in Neighbouring Regions in Denmark and Germany - the Fehmarn Belt Project. Eur J Cancer (2015) 51(9):1188–98. doi:10.1016/j.ejca.2014.11.006
52. Rudolph, CES, Engholm, G, Pritzkuleit, R, Storm, HH, and Katalinic, A. Survival of Breast Cancer Patients in German-Danish Border Regions - A Registry-Based Cohort Study. Cancer Epidemiol (2021) 74:102001. doi:10.1016/j.canep.2021.102001
53. Rudolph, C, Engholm, G, Pritzkuleit, R, Storm, HH, and Katalinic, A. Colorectal Cancer Survival in German–Danish Border Regions—A Registry-Based Cohort Study. Cancers (2023) 15(18):4474. doi:10.3390/cancers15184474
54. Nonnenmacher, L, Baumann, M, le Bihan, E, Askenazy, P, and Chauvel, L. Cross-Border Mobility in European Countries: Associations Between Cross-Border Worker Status and Health Outcomes. BMC Public Health (2021) 21(1):588. doi:10.1186/s12889-021-10564-8
55. Alonso-Sardón, M, Paulino, M, Fernandes, A, Martín-Delgado, MA, Pérez-Martín, RN, Magalhães, CP, et al. Epidemiological Impact of Neurodegenerative Diseases in the Rural Spanish-Portuguese Cross-Border Region. Neurodegener Dis (2023) 23(3–4):25–34. doi:10.1159/000535683
56. Alkerwi, A, Schuh, B, Sauvageot, N, Zannad, F, Olivier, A, Guillaume, M, et al. Adherence to Physical Activity Recommendations and Its Associated Factors: An Interregional Population-Based Study. J Public Health Res (2015) 4:406. doi:10.4081/jphr.2015.406
57. Fries, M, Beckers, S, Bickenbach, J, Skorning, M, Krug, S, Nilson, E, et al. Incidence of Cross-Border Emergency Care and Outcomes of Cardiopulmonary Resuscitation in a Unique European Region. Resuscitation (2007) 72:66–73. doi:10.1016/j.resuscitation.2006.06.001
58. Euregional Health Atlas. Available from: https://euregionalhealthatlas.eu/volwdashboard.html (Accessed November 30, 2023).
59. Eurostat. Health Statistics: Atlas on Mortality in the European Union: Data 1994-96. Luxembourg: Office for Official Publications of the European Communities (2002).
60. Eurostat. Health Statistics: Atlas on Mortality in the European Union. Luxembourg: Office for Official Publications of the European Communities (2009).
61. Santana, P. Atlas of Population Health in European Union Regions. Coimbra, Portugal: Imprensa da Universidade de Coimbra/Coimbra University Press (2017). 266. doi:10.14195/978-989-26-1463-2
62. Schwarze, S, Saad, H, and Joswowitz-Niemierski, D. Auswirkungen der COVID-19-Krise in den Grenzregionen. Bonn: Bundesinstitut für Bau-, Stadt- und Raumforschung (BBSR) (2023). Available from: https://www.bbsr.bund.de/BBSR/DE/veroeffentlichungen/bbsr-online/2023/bbsr-online-05-2023-dl.pdf;jsessionid=CA68088D2A5F52E1087978C8B175396A.live11314?__blob=publicationFile&v=5 (Accessed January 9, 2025).
Keywords: scoping review, European Union, public health, morbidity, mortality, cross-border
Citation: Stroisch S, Angelini V, Schnettler S and Vogt T (2025) Health Outcomes in EU Cross-Border Regions: A Scoping Review. Public Health Rev 46:1608170. doi: 10.3389/phrs.2025.1608170
Received: 18 November 2024; Accepted: 30 January 2025;
Published: 24 February 2025.
Edited by:
Ana Ribeiro, University Porto, PortugalReviewed by:
José Chen-Xu, Instituto Salud Global Barcelona (ISGlobal), SpainAngela Freitas, University of Coimbra, Portugal
Copyright © 2025 Stroisch, Angelini, Schnettler and Vogt. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
PHR is edited by the Swiss School of Public Health (SSPH+) in a partnership with the Association of Schools of Public Health of the European Region (ASPHER)+
*Correspondence: Sophie Stroisch, cy5zdHJvaXNjaEBydWcubmw=
 Sophie Stroisch
Sophie Stroisch Viola Angelini3
Viola Angelini3 Sebastian Schnettler
Sebastian Schnettler Tobias Vogt
Tobias Vogt