Abstract
Objectives: Some people do not fully recover from an acute viral infection and experience persistent symptoms or incomplete recovery for months or even years. This is not unique to the SARS-CoV-2 virus and history shows that post-viral conditions like post COVID-19 condition, also referred to as Long Covid, are not new. In particular, during and after pandemics caused by respiratory viruses in which large parts of the population were infected or exposed, professional and public attention was increased, not least because of the large number of people affected.
Methods: Given the current relevance of the topic, this article aims to narratively review and summarize the literature on post-viral symptoms during past pandemics and to supplement and illustrate it with Swiss examples from the pandemics of 1890, 1918–1920 and later.
Results: Post-viral diseases were an increasingly emphasised health topic during and after past pandemics triggered by respiratory infections over the last 150 years.
Conclusion: In the next pandemic, it should not be surprising that post-viral conditions will again play a role, and pandemic plans should reflect this.
Introduction
Some people do not fully recover from an acute viral infection and experience persistent symptoms or incomplete recovery for months or even years [1–3]. In the medical literature, these postviral conditions or late effects (sequelae) are collectively referred to as postviral symptoms or syndromes (PVS). The spectrum of possible symptoms is broad and often includes debilitating fatigue (postinfectious fatigue), physical weakness and exhaustion, musculo-skeletal complaints, mood swings, neurocognitive disorders (including “brain fog,” lack of concentration, etc.) or cardiovascular disturbances known to occur after acute infections with e.g., coronaviruses, influenza, Epstein-Barr, Ebola, polio or other viruses [3–5]. In analogy to post COVID-19 condition or Long Covid, post-viral disorders have the common feature that their causes are still incompletely understood and therefore therapeutic options are still limited.
A look at the past shows that PVS is not a new condition. For example, postviral fatigue syndromes have been reported in the medical literature for 100–200 years [6]. Particularly during and after pandemics caused by respiratory viruses, in which large parts of the population were infected or exposed, professional and public attention was heightened, not least because of the accumulation of affected individuals. In parallel, research on current and even past pandemics has increasingly begun to look beyond the mortality effects of pandemics to the longer-term health effects on the vast majority of survivors [7]. If historical experiences were more widely recognised, it would be apparent that the indirect effects of viruses such as influenza, polio or even SARS-CoV-2 can lead to drastic life changes, including disability, far beyond single cases [8].
Many of the post-viral symptoms mentioned above, such as incomplete or prolonged recovery or persistent symptoms such as chronic fatigue or even brain fog, have already been described in some of the survivors of previous pandemics and epidemics of the last 200 years, including the “Russian flu” of 1889/90, as well as the SARS pandemic of 2003 or the “Swine flu” of 2009. This is one of the reasons why some experts warned very early on during the COVID-19 pandemic that PVS would also play a role in this pandemic [9]. It is also known from previous long-term studies that many infections, especially those with severe courses, increase the risk of stroke, coronary heart disease or Parkinson’s disease later in life [10–15].
Methods
There are still not many historical review articles on the history of post-viral symptoms [5, 6, 16, 17]. Given the current relevance of the topic of postviral phenomenon, this narrative and selective review article aims to contribute to this incomplete puzzle. For this purpose, we identified and narratively reviewed the international literature on the history of PVS during past pandemics. Additionally, we incorporated examples from Switzerland that we have encountered in the past 10 years of archival research on past pandemics.
Results
Forgotten Pandemic Experiences in Switzerland
Over the past 150 years, the world, Europe and Switzerland have been hit by various epidemics and pandemics of respiratory infections: the “Russian flu” 1889–1894, the “Spanish flu” 1918–1920, the “Asian flu” 1957–1958, the “Hong Kong flu” 1969–1970, the “Russian flu” 1977, the SARS epidemic 2003, the “Swine flu” 2009, the MERS epidemic 2012 and COVID-19 2020–2023 [18, 19]. Prior to COVID-19, the 1889, 1918, and 1957 outbreaks were the pandemics with the greatest impact on health and/or mortality, with large differences between world regions.
In Switzerland, the “Spanish flu” of 1918–1920 remains the greatest demographic catastrophe of the 20th century [20]. It is estimated that about 25,000 people died in Switzerland from this pandemic, with the long wave in the autumn and winter of 1918 being particularly deadly. Why, as elsewhere, the 1918–1920 pandemic virus killed so many young people compared with other influenza pandemics is not yet fully understood. Comparing the various pandemics in Switzerland since the late 19th century in terms of annual (excess) mortality from all causes of death, the “Russian flu” of 1890 caused about 3000 or 10% more deaths and the “Spanish flu” of 1918 caused about 25,000 or 50% more deaths than what would be expected based on the preceeding 5 years [21]. Subsequently, however, none of the global pandemics between 1920 and 2020 reached the severity of the “Russian” or “Spanish flu” in Switzerland (Figure 1). The lack of mortality impact of recent pandemics in Switzerland and the decline in influenza-related mortality in the second half of the 20th century probably led to a loss of experiential knowledge and collective memory of pandemic disasters, which in turn led to an increasing neglect of immediate pandemic risks in the general population [22].
FIGURE 1
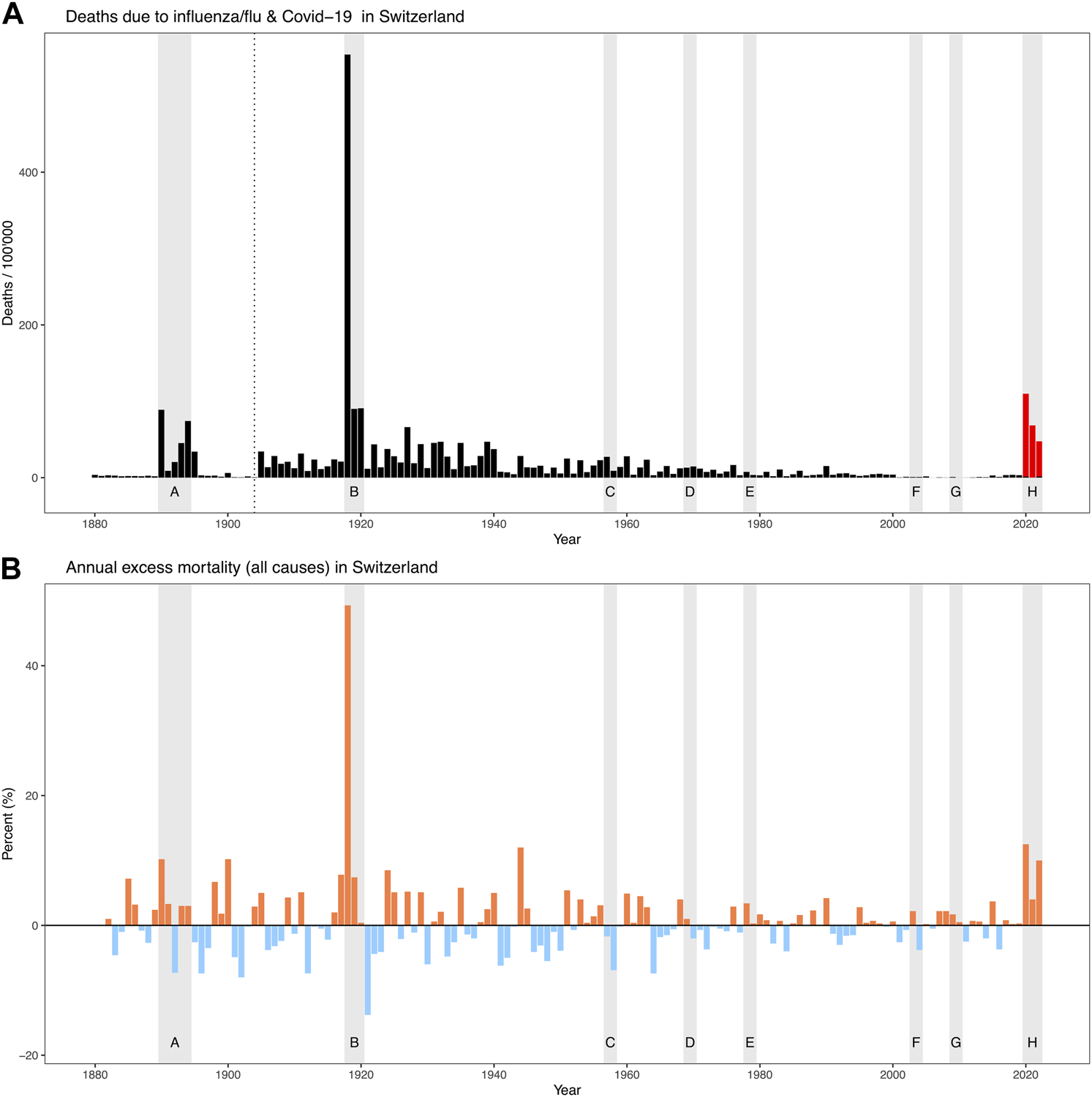
The eight pandemics/epidemic outbreaks since 1880 (gray shaded bars) and their impact on mortality: (A) Officially reported deaths per 100,000 population due to influenza (updated cause-of-death nomenclature as of 1904, data 1890–1894 from Schmid 1895 [28]) as well as COVID-19 (only 2020–2022 according to the Federal Statistical Office [72]); (B) Annual excess mortality (all causes of death) in percent (red = excess mortality, blue = lower mortality) according to [21] (figures 2021 and 2022 according to the Federal Statistical Office [73]). Pandemics/epidemics: A) “Russian flu” ca. 1889–1894, B) “Spanish flu” ca. 1918–1920, C) “Asian flu” 1957, D) “Hong Kong flu” ca. 1968–1970, E) “Russian flu” 1977, F) SARS 2003, G) “Swine flu” 2009, H) “COVID-19” 2020–2023. (Zurich, Switzerland, 2024).
Where does COVID-19 rank in the history of pandemics? The recent pandemic is a historic event and led to an excess mortality in Switzerland not seen since the “Spanish flu” of 1918–1920. As in 1918, the second wave in the autumn and winter of 2020 was particularly deadly. In total, COVID-19 caused about 9,000 or 12% more deaths than expected in 2020 alone [21]. The fact that shortly afterwards, in 2022, there was again a significant increase in excess mortality of about 10% (which is at least partly caused by COVID-19) has not been observed in this way for a long time. By the end of 2022, a total of about 19,000 people had officially died from COVID-19 in Switzerland. In absolute terms, this is not far from the number of victims of the “Spanish flu” (around 25,000 deaths). However, in relative terms, as a proportion of the population, there is still a large difference (220 deaths per 100,000 inhabitants in 2020–2022 compared with 670 deaths per 100,000 inhabitants in 1918–1920). It has recently been estimated that coronavirus vaccination may have prevented about 50,000 deaths in Switzerland in 2020–2022. Thus, there is at least a theoretical possibility that, even relative to the population, COVID-19 would have had the potential to reach the level of “Spanish flu” in terms of mortality in the absence of vaccination [23].
In pandemic research, the severity of a pandemic is often measured by the number of deaths or excess mortality [19]. However, it is the nature of pandemics caused by respiratory infections that a large proportion of the population becomes ill and the vast majority survives. However, the overall burden of disease and the long-term consequences of the infections survived during previous pandemics are not well understood. There is evidence that long-term effects may not become apparent for decades. In Switzerland, for example, mortality of the 1919 birth cohort, who were in utero during the 1918 pandemic, showed increased mortality from the age of 50 compared with birth cohorts immediately before and after the pandemic [24, 25].
Post-Viral Symptoms After the “Russian Flu” of 1889/90
The “Russian flu” was the first truly global pandemic in a world just connected by rail and covered by the mass media [26]. It probably originated in the Russian Empire and spread rapidly across Europe along trade routes in a matter of weeks from early December 1889. The pandemic killed around 1 million people (0.07% of the world’s population at the time) [27]. Depending on whether one assumes a single- or multi-wave pandemic, between 3,000 and 7,000 people died of influenza in Switzerland in 1889–1894, and depending on the region, up to 80% of the population fell ill [28]. The first and strongest wave swept through Switzerland between December 1889 and February 1890, but smaller to medium waves occurred repeatedly in subsequent winters until 1894. Due to the lack of human samples from this period, it has not been possible to identify the pathogen genetically. For decades, it was thought to be an influenza A virus (H2N2 or H3N8) [29, 30]. More recently, particularly in the context of COVID-19, it has been hypothesised that it may also have been a coronavirus. This theory is indirectly supported by temporal correlations of the common ancestors of today’s coronaviruses dating back to about 1890 [31] and by specific symptoms reported by physicians [32, 33]. This question will remain open until genetic evidence is available [34].
The literature contains a relatively large number of references to post-viral symptoms during and after “Russian flu,” such as persistent fatigue, cardiac problems, anxiety, neurological disorders, and so forth [35]. As early as October 2020, medical historians Mark Honigsbaum and Lakshmi Krishnan drew parallels between post-infectious neurological disorders at the time of the “Russian flu” and Long Covid based on symptom descriptions [16]. As an example of a sufferer, they cited Josephine Butler, an English campaigner for women’s rights, who fell ill with “Russian flu” during the Christmas period of 1891 and suffered from pneumonia for several days. Although her fever had subsided, she reported 3 months later that her general condition had hardly improved. In January 1892 she wrote to her son (quoted from Honigsbaum and Krishnan [16]): “I don’t think I ever remember being so weak, not even after the malaria fever at Genoa”[16]. And 3 months later, still weakened, she wrote: “I am so weak that if I read or write for half an hour I become so tired and faint that I have to lie down” [16].
In Switzerland, too, physicians and health authorities were concerned about the duration of the disease, its long-term implications and the sometimes long and incomplete recovery. In the aftermath of the pandemic, the Swiss Federal Office of Public Health conducted a pandemic survey among about 700 physicians in Switzerland. The result was a report of over 300 pages, written by the then director of the office, Dr Friedrich Schmid, and published in 1895 [28]. This report not only reconstructed the course of the pandemic, but also described the disease in detail on the basis of the physicians’ reports. A separate subchapter was devoted to the sequelae. It states, among other things (translated from German): “Above all, the generally slow and incomplete recovery of many people, not only of those who had suffered from severe influenza, but also of those who had suffered from mild cases, should be mentioned. Often there remained for a long time a striking physical and mental weakness, which disappeared only very very slowly, sometimes after many weeks and months.” (Figure 2).
FIGURE 2
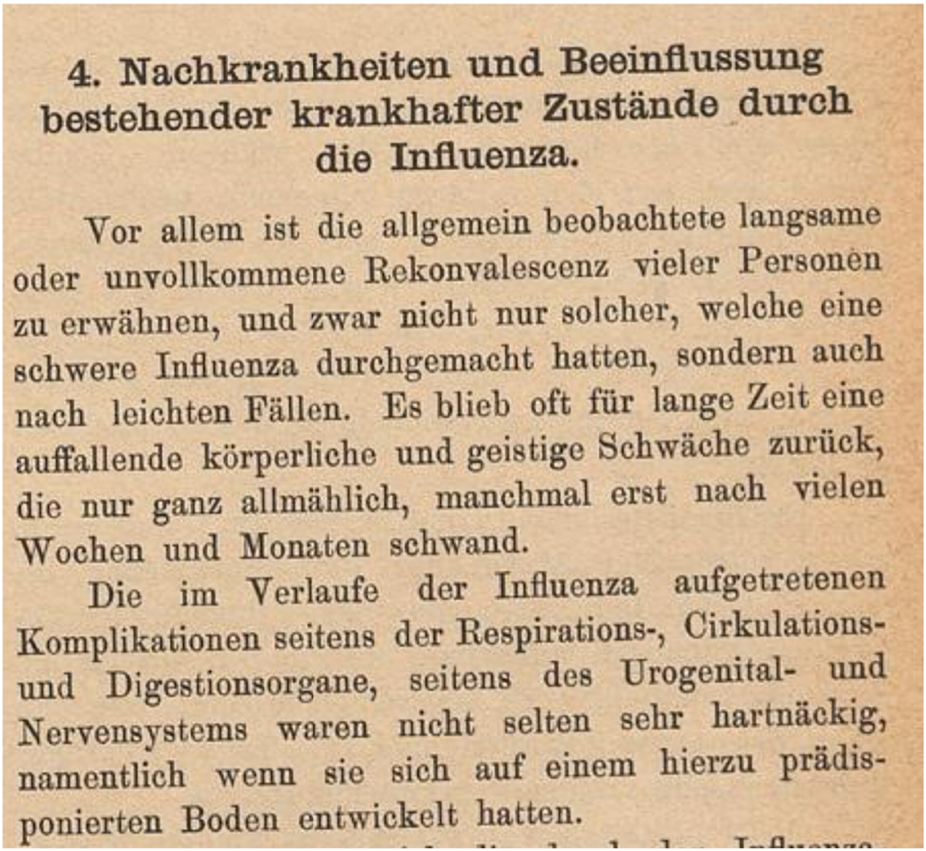
The beginning of the subchapter “secondary illnesses” in the more than 300-page report of the Swiss Health Office after the “Russian flu” of 1889–1894 [28]. (translated: Sequelae and the influence of influenza on existing pathological conditions—Above all, the generally slow and incomplete recovery of many people, not only of those who had suffered from severe influenza, but also of those who had suffered from mild cases, should be mentioned. Often there remained for a long time a striking physical and mental weakness, which disappeared only very very slowly, sometimes after many weeks and months.) (Bern, Switzerland, 1895).
The list of sequelae mentioned in the report was extensive, including nervous system disorders, neuralgia, insomnia, psychosis, hysteria, amnesia, lung disease, myocarditis, heart failure, etc. (loss of taste is not mentioned). Pre-existing conditions were often worsened by the flu. Children and schools were also affected by reduced cognitive performance after the flu. As a large proportion of the population was ill, the many absences caused by illness, e.g., in the railways and the post office, led to considerable disruptions and restrictions [36]. For example, the medical records of a spinning mill in Mollis (Glarus) showed that of 480 workers, 86 were ill with influenza for more than 3 days and 15 workers (about 3%) were absent from work for 30–55 days (almost 8 weeks or 2 months) because of the flu [28].
In the early 1890 s, several cases were also reported in Switzerland of people falling into a deep sleep, sometimes lasting for days, shortly after having contracted the flu (see the section on sleeping sickness below) [37]. As this phenomenon seemed to be spreading at the same time as an epidemic in some regions of Italy (the disease was called “Nona”) [38], Swiss newspapers feared that Switzerland might also be affected by this next epidemic (which apparently did not happen to the same extent) (Figure 3). Because of the temporal association between cases of the flu and cases of sleeping sickness, contemporaries suspected a link between the two diseases.
FIGURE 3
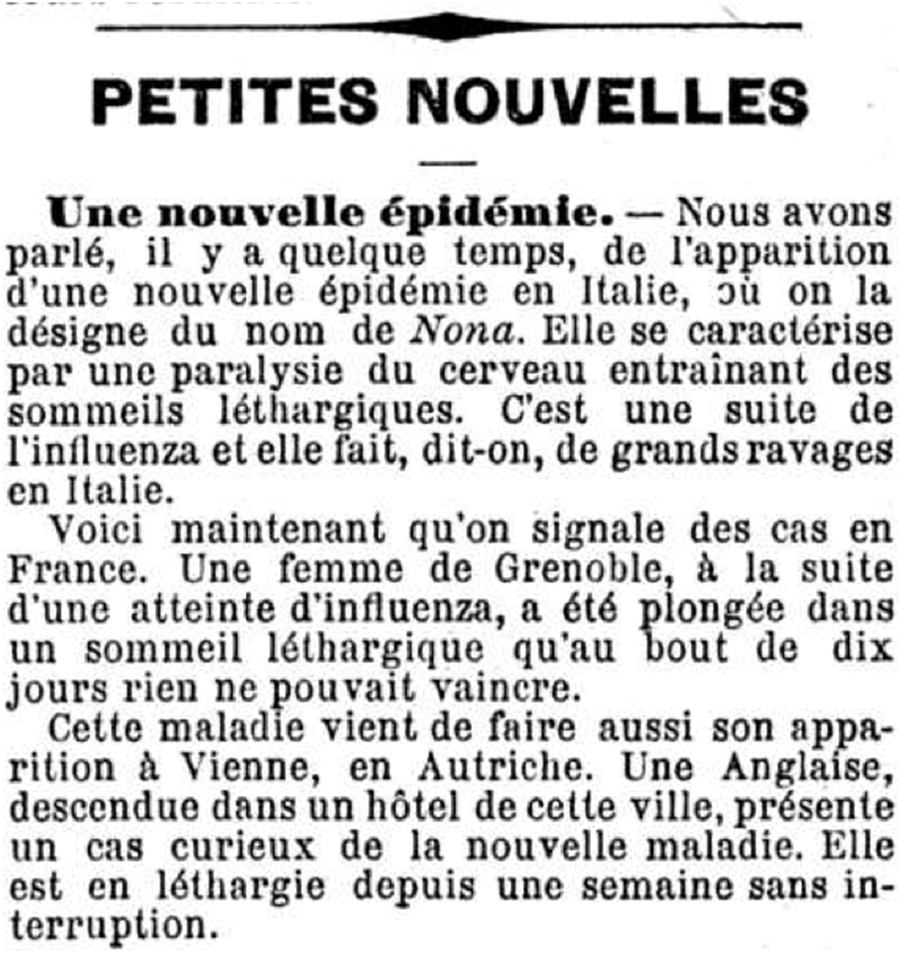
Report in the Valais newspaper “L’ami du peuple” of 12 March 1890 (page 3), on cases of sleeping sickness following the flu, a phenomenon known at the time as “Nona” (translated: A new epidemic.—Some time ago, we reported on the appearance of a new epidemic in Italy, where it is known as Nona. It is characterised by paralysis of the brain, leading to lethargic sleep. It is a sequel to influenza and is said to be wreaking great damage in Italy. Cases have now been reported in France. A woman in Grenoble, following an attack of influenza, was plunged into a lethargic sleep that after 10 days nothing could overcome. This disease has also just appeared in Vienna, Austria. An Englishwoman, staying in a hotel in this city, presented a strange case of the new disease. She had been lethargic for a week without interruption). (source:www.e-newspaperarchives.ch/?a=d&d=AMI18900312-01.2.13). (Valais, Switzerland, 1890).
Post-Viral Symptoms After the “Spanish Flu” 1918–1920
The 1918 influenza pandemic is the best-documented and researched historical pandemic and caused the most deaths, about 2.6 million in Europe alone. As the “Spanish flu” killed between 20 and 100 million people worldwide, including many young people, it is considered the “mother of all pandemics” and a worst-case scenario [39, 40]. Unlike the “Russian flu,” the pathogen causing the “Spanish flu” has been genetically identified as an influenza A/H1N1 virus [41, 42]. Although deaths were highest in this pandemic, especially among young adults, the majority of those who fell ill survived. Switzerland was hit by a total of four waves between the summer of 1918 and the spring of 1920, before the virus adopted a seasonal pattern [43, 44]. At least two-thirds of the Swiss population have fallen ill, in some cases several times, with reinfections often at least as severe as the initial illness [45].
Again, there are numerous reports in the literature of the prolonged convalescence and post-viral symptoms of survivors. One possible source is interviews with older people who survived the pandemic as children. This has been done for Ireland, among other countries, where one of the interviewees recalled (cited from Milne [46]): “I was 5 years of age. We all got it, all the households, there was no one moving, even the doctor who was attending us got it. … We were stricken down for 3 weeks maybe, and recovering afterwards was the most trying time of it. [A long pause.] The health services weren’t too good at the time. It was a terrible disaster.” [46] In collections of memoirs from South Africa and New Zealand compiled by historians Howard Phillips [47] and Geoffrey Rice [48], there are also reports of post-viral symptoms such as loss of muscle strength, nervous complications, depression, apathy, tremors, restlessness or insomnia. As early as 1990 [49], Phillips described how the inability to work as a result of influenza had a considerable impact on South Africa’s economy for some time. To the north, in what is now Tanzania, influenza has even been blamed for the worst famine in a century, after a debilitating lethargy prevented flu survivors from planting when the rains came in late 1918.
It is difficult to quantify the number of people who suffered sequelae after the “Spanish flu.” According to contemporary estimates from England, out of 1,000 cases of influenza, about 800 people suffered from normal influenza with no sequelae. Of the remaining 200 people, about 70 died and about 130 did not fully recover or suffered sequelae [5, 50]. Health consequences can also occur in the medium term. In recent decades, epidemiological research has shown through long-term studies that people who survived the “Spanish flu” in utero, as a child or as a young adult have an increased risk of all-cause mortality later in life, as well as an increased risk of Parkinson’s disease and cardiovascular disease [15, 24, 25, 35]. There is now increasing evidence that such an association with later cardiovascular disease may also exist for COVID-19 [51].
In Switzerland, too, there are various traces of post-viral symptoms following the “Spanish flu” of 1918–1920. Once again, the health authorities attempted to reconstruct what had happened after the first waves. A survey of physicians has been preserved, this time in the canton of Vaud, where in mid-1919 the 170 physicians in the canton were surveyed with a long questionnaire about the epidemic. One of the 20 questions again concerned recovery. Questions were asked about the duration of convalescence in the treated patient group, about the frequency of prolonged and incomplete convalescence, and about symptoms and late complications. Both the individual answer sheets of the physicians and a summary report of the cantonal health authorities have been preserved in the archives [52]. The report states (translated from French: “The duration of recovery varied considerably among influenza patients and was often desperately slow, even in mild cases. Patients suffered from general weakness, exhaustion, sometimes neurasthenia, acute psychosis or severe nervous depression, which delayed recovery. In addition, persistent heart problems were the main cause of long recovery times in a very large number of cases” (Figure 4). Of the 118 physicians answering to the recovery questions, 8 reported convalescence periods of several months to a year for some of their patients, and another 38, without giving a time, said their patients sometimes had long and slow recoveries. The report also quotes selected responses from individual physicians. For example, Dr Décombaz of Le Sentier said that he had observed that about 15% of convalescences were long-lasting. For Dr Zbinden of Lausanne, prolonged convalescence was even more the rule. The reply of Dr Wintsch from Lausanne is shown in Figure 5 (translated from French): “From a cardiological point of view, recovery often takes a very long time; after a year, some patients have heart insufficiency at a young age.”
FIGURE 4
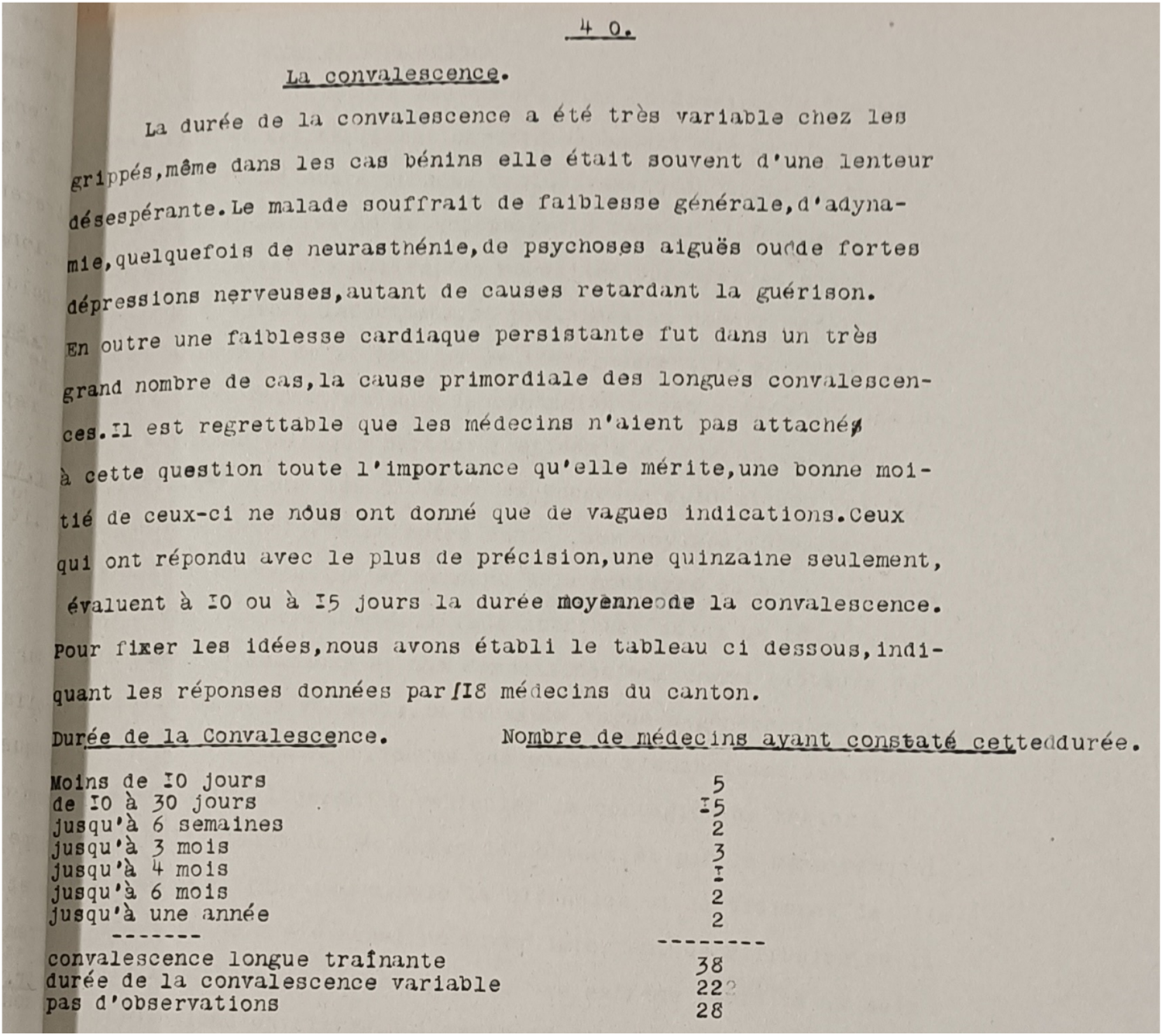
Subchapter on convalescence in the report of the Vaudois health authorities as a result of a survey of physicians after the “Spanish flu” of 1918–1919 (translated: The duration of recovery varied considerably among influenza patients and was often desperately slow, even in mild cases. Patients suffered from general weakness, exhaustion, sometimes neurasthenia, acute psychosis or severe nervous depression, which delayed recovery. In addition, persistent heart problems were the main cause of long recovery times in a very large number of cases.) (source: Archives Cantonal Vaudoise ARC KVIIIb 27/1 & 27/2) [52]. (Lausanne, Switzerland, 1919).
FIGURE 5
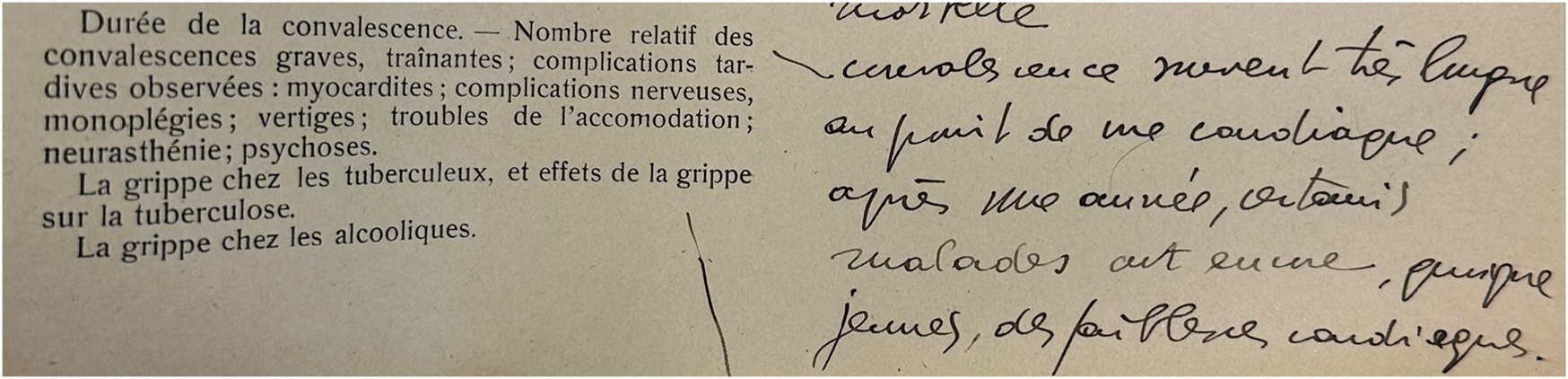
Original answer of the physician Dr. Wintsch from Lausanne to the questionnaire question about the duration of convalescence in his patient collective, the frequency of prolonged convalescence and postviral symptoms after the “Spanish flu” 1918–1920 (answer translated: “From a cardiological point of view, convalescence often takes a very long time; after 1 year, some patients already have heart weakness at a young age”) (source: Archives Cantonal Vaudoise ARC KVIIIb 27/1 & 27/2). (Lausanne, Switzerland, 1919).
Another case study goes back to school, to the Muristalden Teacher Training College in the city of Bern, where young men were trained to be teachers [53, 54]. The Teachers’ Training College was fortunate in that it was only marginally affected by mortality from influenza in 1918 and 1919, but it was all the more affected by the burden of disease. When, at the beginning of 1919, the authorities allowed regular schooling to resume after the heavy wave of influenza in the autumn/winter of 1918, all the young men in Muristalden who had not yet contracted the disease fell ill within a few days. For four to five weeks in January and February 1919, only half the students were able to attend. About a dozen seminarians missed six to eight weeks of school because of the flu and its sequelae. The actual epidemic was over by the end of February 1919, but the health consequences were still being felt. The house chronicle states (translated from German): “However, many of the students still needed rest and an extended holiday, and in some cases all the consequences of the flu, such as fatigue, heart palpitations, cardiac weakness and nervous phenomena, did not disappear completely until this spring, so that they had to miss some classes again.” In addition, seminarians who had been ill with influenza for a longer period of time performed significantly worse in the intermediate exams that followed in March 1919, and the difference was still evident in the final exams 2 years later. In April 1919, the house chronicle reported (translated from German): “In the seminary, the state of health still was not good ... For most of the term we had between two and seven inmates who were in bed. There were also heart weaknesses and all kind of relapses. One has to wonder whether these were the consequences of the flu [...].”
Influenza and Sleeping Sickness in the 1920 s
In addition to Parkinson’s disease (see above), the long-term neurological consequences of the “Spanish flu” of 1918–1920 also included so-called “encephalitis lethargica” or “sleeping sickness” (ICD-10 A85.8 and therefore not the same as ME/CFS) [35]. The involvement of the central nervous system can manifest as encephalitis during or after an influenza illness, whereby the symptoms usually subside without neurological consequences [55]. Post-influenza encephalitis has been described after many historical influenza epidemics, including the “Russian flu” (see above) [55].
However, in the wake of the “Spanish flu,” an encephalitis epidemic unprecedented in its frequency, virulence and consequences occurred in many countries from about 1918. The term encephalitis lethargica was first used in 1917 to describe an increasing number of patients with acute mental confusion, lethargy, fever, eye muscle movements, headache, tremors, delirium and convulsions. The lethargy that gave the disease its name lasted from days to months and in some cases led to coma and death from respiratory failure [12, 55]. In most countries, the epidemic peaked in the early 1920 s. The epidemic of encephalitis lethargica is closely associated with “Spanish flu” because of its concurrent occurrence [56]. However the exact aetiology remains unclear [12] and a causal link has not been established to this day with no influenza RNA having yet been isolated from historical brain tissue of patients [57, 58]. Because of the suspected link between encephalitis lethargica and the “Spanish flu,” it was feared at the beginning of COVID-19 that sleeping sickness might also play a role [59], but this has not yet been confirmed.
In the first months of 1920, many countries, including Switzerland, were affected by a so-called late wave of the “Spanish flu,” which did not reach the extent of the earlier waves, but again resulted in numerous cases of illness and deaths. At the beginning of 1920, when cases of encephalitis lethargica began to appear in Switzerland and a connection with influenza was suspected, the Federal Council ordered the compulsory reporting of this disease on 14 February 1920, and from then on the disease was systematically monitored together with influenza. In 1920 and 1921, the Federal Office of Public Health published several lengthy reports on the data generated by compulsory registration. From one of these reports in 1920, the reported cases of both diseases can be plotted by week (Figure 6). The two curves show a close temporal correspondence, with the wave of encephalitis lethargica appearing and disappearing with a delay of one to 2 weeks. In total, about 140,000 cases of influenza and 960 cases of sleeping sickness were reported between 4 January and 3 July 1920. In the 1921 report, the Federal Health Office wrote of encephalitis lethargica (translated from German): “The coincidence of its occurrence with that of influenza—for the year 1920 the curves of the two diseases in Switzerland coincide almost completely—has led to the opinion that encephalitis is a complication of influenza. This question is still open.” This is still true today, also because there has been no similar epidemic since.
FIGURE 6
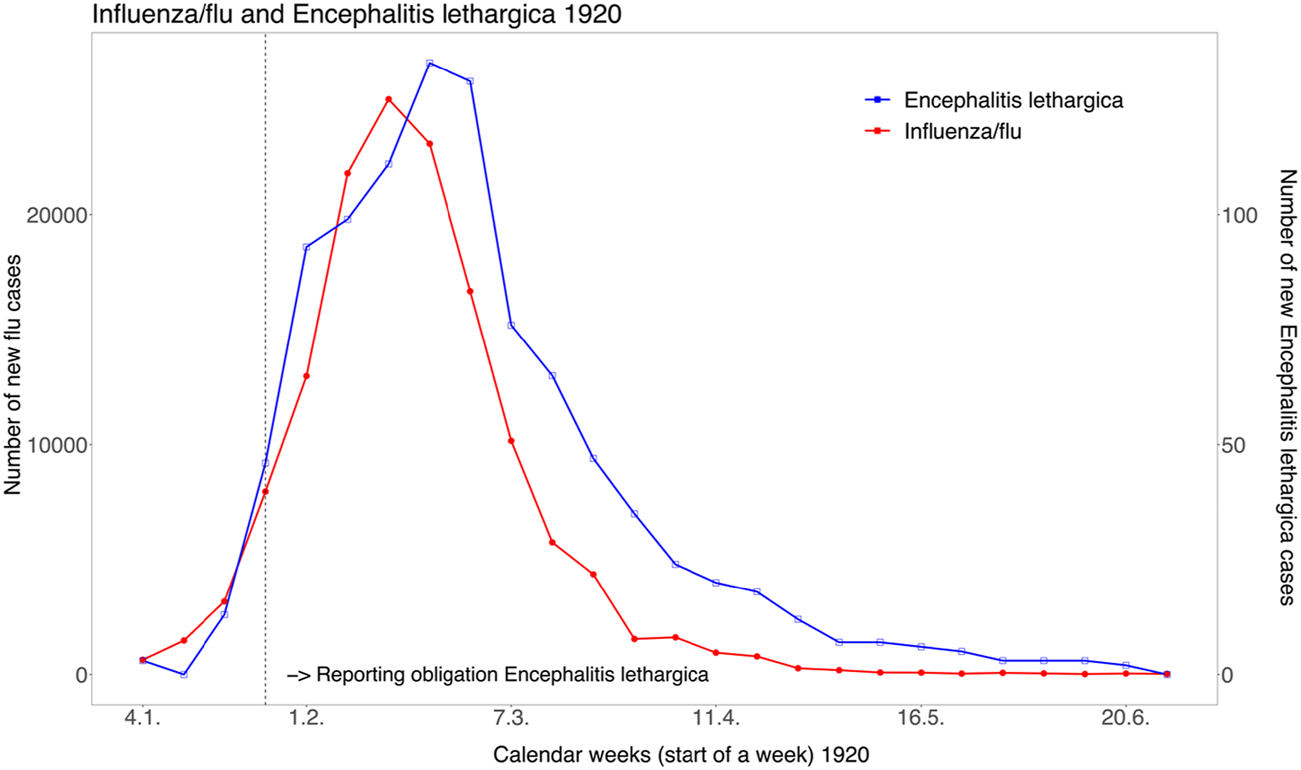
The concurrence of officially reported influenza cases and cases of encephalitis lethargica in the first half of 1920 in Switzerland (source: Bulletin des Eidgenössischen Gesundheitsamtes, 38, 1920, p. 398). (Zurich, Switzerland, 2024).
Post-Viral Symptoms After Other Pandemics or Epidemics Since 1920
Postviral diseases have also played a role in subsequent pandemics since 1920. This was the case, for example, after the influenza A H2N2 pandemic in the autumn of 1957, which was characterised primarily by high morbidity rather than mortality. Worldwide, the “Asian flu” in 1957 caused an estimated 1.1 million additional deaths [60]. As large parts of the Swiss population were infected or fell ill, hospitals stopped admitting visitors and schools were closed [61]. Due to the high number of cases, many companies and public institutions, such as the post office, telephone and public services, were severely affected and in some cases were only able to provide a limited service. Pensioners and auxiliary staff were deployed to make up for the lack of staff. Daily newspapers also reported major disruptions to events such as soccer championships and cycling races, where many athletes fell ill, and trade fairs such as the Olma, which attracted fewer visitors than expected. Neurological effects were also reported in Switzerland for some of those who recovered [61].
In late 2002 and throughout 2003, the SARS epidemic, the first global outbreak of severe acute respiratory syndrome (SARS) caused by the SARS-CoV virus, spread from Asia. There was only one officially confirmed case in Switzerland, but other regions of the world were much more severely affected. Again, studies show that some people have had to deal with post-viral symptoms after contracting SARS. For example, the health of recovered SARS patients was monitored after discharge from hospital, and more than half of the patients still reported severe fatigue at 3, 6, and 12 months [5, 62]. Another study followed SARS patients in Hong Kong for 4 years. 40% reported persistent chronic fatigue and 27% were diagnosed with encephalomyelitis/chronic fatigue syndrome (CFS) [63]. Based on this experience with SARS, experts warned already in 2020, relatively early in the COVID-19 pandemic, that post-viral illness would also play a role this time [9].
In 2009, the A/H1N1 influenza virus once again caused a pandemic, known as “Swine flu.” In Switzerland, an estimated 1 to 1.5 million people fell ill during the wave at the end of 2009, which lasted about 12 weeks. Not all cases were without complications; officially, there were about 600 hospitalisations and 18 deaths in Switzerland due to the pandemic virus [64, 65]. In Switzerland, there are few studies on post-viral diseases after the swine flu pandemic. In Norway, however, a study found an increased incidence of ME/CFS after influenza infection, especially in younger people, suggesting a direct link with the influenza virus [66].
Discussion
Given this previous experience with pandemics triggered by respiratory infections over the last 150 years or so, it is not surprising that post-viral diseases are also an important issue in the context of the COVID-19 pandemic, especially after the acute phase of the pandemic, in which the vast majority of the population is likely to have fallen ill at some point. In retrospect, parallels between pandemics are not difficult to identify (and systematic archive research would probably rediscover many more past examples). However, the knowledge gained from past pandemics has been forgotten over time and was therefore too little known by health authorities and physicians at the start of the COVID-19 pandemic. Another constant over time is that although the links between the viral disease and post-viral symptoms have often been recognized, the causal mechanisms are difficult to understand and a certain degree of uncertainty remains. It should be noted that the similarities and differences in post-viral symptoms after past pandemics have not yet been fully and only unsystematically researched. It is also important to emphasise that the causative pathogens of pandemics, usually influenza viruses or coronaviruses, differ in terms of their biological characteristics, and a comparison must always take these differences into account [39].
With regard to COVID-19, it can be stated that no pandemic has ever been so well documented from a medical and biological point of view, thanks to extensive diagnostic testing, established serosurveillance programs and longitudinal cohorts set up to study and estimate the burden of Long Covid [67–69]. Pandemics will very likely continue to happen, and in the next pandemic, it should come as no surprise if post-viral diseases play a role again. In this context, the COVID-19 pandemic has underscored the importance of considering the post-acute phase also in future pandemic preparedness. This includes investing in research to further understand these conditions, planning and allocating resources to enhance post-infectious care such as the development of multidisciplinary clinics or through self-management platforms (e.g., Altea Network in Switzerland or Your Covid Recovery in the UK), implementing policies to support affected individuals to return to work or school, and developing systematic assessments and documentation to aid in social insurance and assistance when necessary (e.g., EPOCA tool of Swiss Insurance Medicine [70, 71]). Taking the lessons we learned from COVID-19 and incorporating them into our pandemic preparedness plans will be extremely crucial in reducing the long-term impacts of future pandemics on individuals and societies worldwide.
Statements
Author contributions
KS has written a first draft of the manuscript. All authors contributed to the conception of the article and revised and expanded the first draft.
Acknowledgments
The authors would like to thank Antoine Flahault and Andreas Seibert for their valuable comments.
Conflict of interest
The authors declare that they do not have any conflicts of interest.
References
1.
Choutka J Jansari V Hornig M Iwasaki A . Unexplained Post-Acute Infection Syndromes. Nat Med (2022) 28(5):911–23. 10.1038/s41591-022-01810-6
2.
Ballouz T Menges D Anagnostopoulos A Domenghino A Aschmann HE Frei A et al Recovery and Symptom Trajectories up to Two Years After SARS-CoV-2 Infection: Population Based, Longitudinal Cohort Study. BMJ (2023) 381:e074425. 10.1136/bmj-2022-074425
3.
Willi S Lüthold R Hunt A Hänggi NV Sejdiu D Scaff C et al COVID-19 Sequelae in Adults Aged Less Than 50 Years: A Systematic Review. Trav Med Infect Dis (2021) 40:101995. 10.1016/j.tmaid.2021.101995
4.
Chandan JS Brown K Simms-Williams N Camaradou J Bashir N Heining D et al Non-Pharmacological Therapies for Postviral Syndromes, Including Long COVID: A Systematic Review and Meta-Analysis Protocol. BMJ Open (2022) 12(4):e057885. 10.1136/bmjopen-2021-057885
5.
Islam MF Cotler J Jason LA . Post-Viral Fatigue and COVID-19: Lessons From Past Epidemics. Fatigue Biomed Heal Behav (2020) 8(2):61–9. 10.1080/21641846.2020.1778227
6.
Wessely S . History of Postviral Fatigue Syndrome. Br Med Bull (1991) 47(4):919–41. 10.1093/oxfordjournals.bmb.a072521
7.
Briggs A Vassall A . Count the Cost of Disability Caused by COVID-19. Nature (2021) 593(7860):502–5. 10.1038/d41586-021-01392-2
8.
Spinney L . Pandemics Disable People — The History Lesson that Policymakers Ignore. Nature (2022) 602(7897):383–5. 10.1038/d41586-022-00414-x
9.
Perrin R Riste L Hann M Walther A Mukherjee A Heald A . Into the Looking Glass: Post-Viral Syndrome Post COVID-19. Med Hypotheses (2020) 144:110055. 10.1016/j.mehy.2020.110055
10.
Jang H Boltz DA Webster RG Smeyne RJ . Viral Parkinsonism. Biochim Biophys Acta - Mol Basis Dis (2009) 1792(7):714–21. 10.1016/j.bbadis.2008.08.001
11.
Martyn CN . Infection in Childhood and Neurological Diseases in Adult Life. Br Med Bull (1997) 53(1):24–39. 10.1093/oxfordjournals.bmb.a011603
12.
Henry J Smeyne RJ Jang H Miller B Okun MS . Parkinsonism and Neurological Manifestations of Influenza Throughout the 20th and 21st Centuries. Parkinsonism Relat Disord (2010) 16(9):566–71. 10.1016/j.parkreldis.2010.06.012
13.
Elkind MSV Boehme AK Smith CJ Meisel A Buckwalter MS . Infection as a Stroke Risk Factor and Determinant of Outcome After Stroke. Stroke (2020) 51:3156–68. 10.1161/STROKEAHA.120.030429
14.
Elkind MSV Carty CL O’Meara ES Lumley T Lefkowitz D Kronmal RA et al Hospitalization for Infection and Risk of Acute Ischemic Stroke: The Cardiovascular Health Study. Stroke (2011) 42(7):1851–6. 10.1161/STROKEAHA.110.608588
15.
Azambuja MIR Duncan BB . Similarities in Mortality Patterns From Influenza in the First Half of the 20th Century and the Rise and Fall of Ischemic Heart Disease in the United States: A New Hypothesis Concerning the Coronary Heart Disease Epidemic. Cad Saude Publica (2002) 18(3):557–66. 10.1590/s0102-311x2002000300002
16.
Honigsbaum M Krishnan L . Taking Pandemic Sequelae Seriously: From the Russian Influenza to COVID-19 Long-Haulers. Lancet (2020) 396(10260):1389–91. 10.1016/S0140-6736(20)32134-6
17.
Dimka JL Schneider BM Mamelund S-E . Protocol for a Systematic Review to Understand the Long-Term Mental-Health Effects of Influenza Pandemics in the Pre-COVID-19 Era. Scand J Public Health (2023) 0(0):1–6. 10.1177/14034948231217362
18.
Vuilleumier C Kaiser L . Les pandémies à travers les âges. Le cas suisse. Lausanne: Infolio (2020).
19.
Miller MA Viboud C Balinska M Simonsen L . The Signature Features of Influenza Pandemics — Implications for Policy. N Engl J Med (2009) 360(25):2595–8. 10.1056/NEJMp0903906
20.
Sonderegger C Tscherrig A . Die Grippepandemie 1918-1919 in der Schweiz. In: KrämerDPfisterCSegesserD, editors. Woche Fur Woche neue Preisaufschlage Nahrungsmittel, Energie- und Ressourcenkonflikte in der Schweiz des Ersten Weltkrieges. Basel: Schwabe (2016). p. 259–84.
21.
Staub K Panczak R Matthes KL Floris J Berlin C Junker C et al Historically High Excess Mortality During the COVID-19 Pandemic in Switzerland, Sweden, and Spain. Ann Intern Med (2022) 175(4):523–32. 10.7326/M21-3824
22.
Staub K Rühli F Floris J . The “Pandemic Gap” in Switzerland Across the 20th century, and the Necessity of Increased Science Communication of Past Pandemic Experiences. Swiss Med Wkly (2020). Available from: https://smw.ch/op-eds/post/the-pandemic-gap (Accessed March 28, 2024).
23.
Staub K Zwahlen M . What Would Have Happened if We Would Not Have Had the Covid Vaccination? Could the Pandemic Death Toll 2020/2021 Have Reached the Dimensions of the 1918/1919 Pandemic?Swiss Med Wkly (2022). Available from: https://smw.ch/index.php/smw/announcement/view/54 (Accessed March 28, 2024).
24.
Matthes KL . Long-Term Mortality Effects of Century Crises: A Warning From the Past for the Decades After COVID-19?Swiss Med Wkly (2023) 153(3):40057. 10.57187/smw.2023.40057
25.
Neelsen S Stratmann T . Long-Run Effects of Fetal Influenza Exposure: Evidence From Switzerland. Soc Sci Med (2012) 74(1):58–66. 10.1016/j.socscimed.2011.09.039
26.
Patterson KD . Pandemic Influenza, 1700-1900: A Study in Historical Epidemiology (1986). p. 118. Available from: file://catalog.hathitrust.org/Record/000812404 (Accessed March 28, 2024).
27.
Valleron A-J Cori A Valtat S Meurisse S Carrat F Boelle P-Y . Transmissibility and Geographic Spread of the 1889 Influenza Pandemic. Proc Natl Acad Sci (2010) 107(19):8778–81. 10.1073/pnas.1000886107
28.
Schmid FU . Die Influenza in der Schweiz in den Jahren 1889-1894, auf Grund amtlicher Berichte und sonstigen Materials. Bern: OCLC (1895).
29.
Berche P . The Enigma of the 1889 Russian Flu Pandemic: A Coronavirus?Presse Med (2022) 51(3):104111. 10.1016/j.lpm.2022.104111
30.
Gagnon A Acosta JE Madrenas J Miller MS . Is Antigenic Sin Always “Original?” Re-Examining the Evidence Regarding Circulation of a Human H1 Influenza Virus Immediately Prior to the 1918 Spanish Flu. PLOS Pathog (2015) 11(3):e1004615. 10.1371/journal.ppat.1004615
31.
Vijgen L Keyaerts E Moes E Thoelen I Wollants E Lemey P et al Complete Genomic Sequence of Human Coronavirus OC43: Molecular Clock Analysis Suggests a Relatively Recent Zoonotic Coronavirus Transmission Event. J Virol (2005) 79(3):1595–604. 10.1128/JVI.79.3.1595-1604.2005
32.
Brüssow H Brüssow L . Clinical Evidence That the Pandemic From 1889 to 1891 Commonly Called the Russian Flu Might Have Been an Earlier Coronavirus Pandemic. Microb Biotechnol (2021) 14(5):1860–70. 10.1111/1751-7915.13889
33.
Brüssow H . What We Can Learn From the Dynamics of the 1889 ‘Russian Flu’ Pandemic for the Future Trajectory of COVID-19. Microb Biotechnol (2021) 14(6):2244–53. 10.1111/1751-7915.13916
34.
Erkoreka A Hernando-Pérez J Ayllon J . Coronavirus as the Possible Causative Agent of the 1889–1894 Pandemic. Infect Dis Rep (2022) 14(3):453–69. 10.3390/idr14030049
35.
Stefano GB . Historical Insight into Infections and Disorders Associated With Neurological and Psychiatric Sequelae Similar to Long COVID. Med Sci Monit (2021) 27:e931447. 10.12659/MSM.931447
36.
Goff J-ML . Diffusion of Influenza During the Winter of 1889-1890 in Switzerland. Genus (2011) 67(2):77–99. Available from: http://www.jstor.org/stable/genus.67.2.77 (Accessed March 28, 2024).
37.
Di Vito A Donato A Bria J Donato F Donato G . Encephalitis Lethargica What Is Still Wrong?Int J Immunopathol Pharmacol (2023) 37:039463202311549. 10.1177/03946320231154997
38.
Klieneberger C . Schlafkrankheit, Grippe-Enzephalitis, Encephalitis Comatosa. Dtsch Med Wochenschr (1920) 46(24):654–5. 10.1055/s-0029-1192705
39.
Morens DM Taubenberger JK Fauci AS . A Centenary Tale of Two Pandemics: The 1918 Influenza Pandemic and COVID-19, Part I. Am J Public Health (2021) 111(6):1086–94. 10.2105/AJPH.2021.306310
40.
Morens DM Taubenberger JK . The Mother of All Pandemics Is 100 Years Old (And Going Strong). Am J Public Health (2018) 108(11):1449–54. 10.2105/AJPH.2018.304631
41.
Patrono LV Vrancken B Budt M Düx A Lequime S Boral S et al Archival Influenza Virus Genomes From Europe Reveal Genomic Variability During the 1918 Pandemic. Nat Commun (2022) 13(1):2314. 10.1038/s41467-022-29614-9
42.
Taubenberger JK . The Origin and Virulence of the 1918 “Spanish” Influenza Virus. Proc Am Philos Soc (2006) 150(1):86–112. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=17526158 (Accessed March 28, 2024).
43.
Staub K . If Immunisation Is Too Low, Dropping Temperatures in Fall 2021 May Lead to Epidemic Resurgence – As in 1918, 1957 and 2020. Swiss Med Wkly (2021) 151(31–32):w30014. 10.4414/SMW.2021.w30014
44.
Bernhard M Leuch C Kordi M Gruebner O Matthes KL Floris J et al From Pandemic to Endemic: Spatial-Temporal Patterns of Influenza-Like Illness Incidence in a Swiss Canton, 1918–1924. Econ Hum Biol (2023) 50:101271. 10.1016/j.ehb.2023.101271
45.
Matthes KL Le Vu M Bhattacharyya U Galliker A Kordi M Floris J et al Reinfections and Cross-Protection in the 1918/19 Influenza Pandemic: Revisiting a Survey Among Male and Female Factory Workers. Int J Public Health (2023) 68:1605777. 10.3389/ijph.2023.1605777
46.
Milne I . Through the Eyes of a Child - Spanish Influenza Remembered by Survivors. In: LellanAMMaugerA, editors. Growing Pains. Irish Academic Press (2012). p. 159–74.
47.
Dehner GHP . Howard Phillips, in a Time of Plague: Memories of the ‘Spanish’ Flu Epidemic of 1918 in South Africa. Soc Hist Med (2019) 33(1):343–4. 10.1093/shm/hkz093
48.
Rice G . Black November: The 1918 Influenza Pandemic in New Zealand. Christchurch, NZ: Canterbury University Press (2005).
49.
Phillips H . Black October: The Impact of the Spanish Influenza Epidemic of 1918 on South Africa. Pretoria: Government Printer (1990).
50.
Abrahams A Hallows N French H . A Further Investigation Into Influenzo-Pneumococcal and Influenzo-Streptococcal Septicæmia: Epidemic Influenzal “Pneumonia” of Highly FataL Type and its Relation to “Purulent Bronchitis.”. Lancet (1919) 193(4975):1–11. 10.1016/s0140-6736(01)22115-1
51.
Xie Y Xu E Bowe B Al-Aly Z . Long-Term Cardiovascular Outcomes of COVID-19. Nat Med (2022) 28(3):583–90. 10.1038/s41591-022-01689-3
52.
Autorités de la santé du canton de Vaud. Rapport sur l’épidémie de grippe 1918. Lausanne: Archives Cantonal Vaudoise ARC KVIIIb 27/1 (1919). p. 27.
53.
Boser L Staub K . How the Influenza Pandemic 1918/19 Affected Teacher Education and Schools in Several Ways − A Case Study From Switzerland. Paedagog Hist (2023) 1–18. 10.1080/00309230.2023.2238623
54.
Staub K . Die Influenza-Pandemie 1918/19 in Bern und ihre Auswirkungen am Lehrerseminar Muristalden. Berner Z für Geschichte (2023) 23(2):37–53.
55.
Cunha BA . Influenza: Historical Aspects of Epidemics and Pandemics. Infect Dis Clin North Am (2004) 18(1):141–55. 10.1016/S0891-5520(03)00095-3
56.
Müller T . Im Schatten der Pandemie. DNP - Der Neurol Psychiater (2020) 21(5):8–9. 10.1007/s15202-020-2873-5
57.
Unwin RJ . The 1918 Influenza Pandemic: Back to the Future?Kidney Blood Press Res (2021) 46(5):639–46. 10.1159/000519288
58.
Dale RC Church AJ Surtees RAH Lees AJ Adcock JE Harding B et al Encephalitis Lethargica Syndrome: 20 New Cases and Evidence of Basal Ganglia Autoimmunity. Brain (2004) 127(1):21–33. 10.1093/brain/awh008
59.
Giordano A Schwarz G Cacciaguerra L Esposito F Filippi M . COVID-19: Can We Learn From Encephalitis Lethargica?Lancet Neurol (2020) 19(7):570. 10.1016/S1474-4422(20)30189-7
60.
Viboud C Simonsen L Fuentes R Flores J Miller MA Chowell G . Global Mortality Impact of the 1957–1959 Influenza Pandemic. J Infect Dis (2016) 213(5):738–45. 10.1093/infdis/jiv534
61.
Bürgi H . Zur Frage der Enzephalitis bei Influenza. Bern: Arnaud Druck (1960).
62.
Tansey CM Louie M Loeb M Gold WL Muller MP de Jager J et al One-Year Outcomes and Health Care Utilization in Survivors of Severe Acute Respiratory Syndrome. Arch Intern Med (2007) 167(12):1312–20. 10.1001/archinte.167.12.1312
63.
Lam MH-B Wing YK Yu MWM Leung CM Ma RCW Kong APS et al Mental Morbidities and Chronic Fatigue in Severe Acute Respiratory Syndrome Survivors: Long-Term Follow-Up. Arch Intern Med (2009) 169(22):2142–7. 10.1001/archinternmed.2009.384
64.
Bundesamt für Gesundheit (BAG). Pandemische Grippe H1N1 2009 in der Schweiz, Wochen 17 (2009) bsi 8 (2010). Bull Des Bundesamtes für Gesundh (2010) 20:534–43.
65.
Lücker L Kherad O Iten A Wagner N Descombes M Camus V et al Clinical Features and Outcome of Hospitalised Adults and Children With the 2009 Influenza A H1N1 Infection at Geneva’s University Hospital. Swiss Med Wkly (2011) 141:w13177. 10.4414/smw.2011.13177
66.
Magnus P Gunnes N Tveito K Bakken IJ Ghaderi S Stoltenberg C et al Chronic Fatigue Syndrome/Myalgic Encephalomyelitis (CFS/ME) Is Associated With Pandemic Influenza Infection, But Not With an Adjuvanted Pandemic Influenza Vaccine. Vaccin (2015) 33(46):6173–7. 10.1016/j.vaccine.2015.10.018
67.
West EA Anker D Amati R Richard A Wisniak A Butty A et al Corona Immunitas: Study Protocol of a Nationwide Program of SARS-CoV-2 Seroprevalence and Seroepidemiologic Studies in Switzerland. Int J Public Health (2020) 65(9):1529–48. 10.1007/s00038-020-01494-0
68.
Frei A Kaufmann M Amati R Butty Dettwiler A von Wyl V Annoni AM et al Development of Hybrid Immunity During a Period of High Incidence of Omicron Infections. Int J Epidemiol (2023) 52:1696–707. 10.1093/ije/dyad098/7219995
69.
Wulf HS Abbafati C Aerts JG Al-Aly Z Ashbaugh C Estimated Global Proportions of Individuals With Persistent Fatigue, Cognitive, and Respiratory Symptom Clusters Following Symptomatic COVID-19 in 2020 and 2021. JAMA (2022) 328(16):1604–15. 10.1001/jama.2022.18931
70.
Kerksieck P Ballouz T Haile SR Schumacher C Lacy J Domenghino A et al Post COVID-19 Condition, Work Ability and Occupational Changes in a Population-Based Cohort. Lancet Reg Heal - Eur (2023) 31:100671. 10.1016/j.lanepe.2023.100671
71.
SIM Swiss Insurance Medicine. Empfehlungen für die versicherungsmedizinische Abklärung in der Schweiz bei Post-Covid-19-Erkrankung (Version 2.0) Basel (2023). Available from: https://www.swiss-insurance-medicine.ch/storage/app/media/Downloads/Dokumente/covid-19_aktuelle_Meldungen/230823_RevidierteEmpfehlungen_Final.pdf (Accessed March 28, 2024).
72.
Bundesamt für Statistik. Spezifische Todesursachen (2023). Available from: https://www.bfs.admin.ch/bfs/de/home/statistiken/gesundheit/gesundheitszustand/sterblichkeit-todesursachen/spezifische.html#:∼:text=DieMehrzahlderTodesfällelässt,TodesursachebeiMännernundFrauen (Accessed March 28, 2024).
73.
Bundesamt für Statistik. Sterblichkeit, Todesursachen (2023). Available from: https://www.bfs.admin.ch/bfs/de/home/statistiken/gesundheit/gesundheitszustand/sterblichkeit-todesursachen.html#:∼:text=ImHerbst2020kames,einerdrittenPeriodemitÜbersterblichkeit (Accessed March 28, 2024).
Summary
Keywords
historical epidemiology, long COVID, historical trends, pandemic, influenza
Citation
Staub K, Ballouz T and Puhan M (2024) An Unwanted but Long-Known Company: Post-Viral Symptoms in the Context of Past Pandemics in Switzerland (and Beyond). Public Health Rev 45:1606966. doi: 10.3389/phrs.2024.1606966
Received
12 December 2023
Accepted
22 March 2024
Published
08 April 2024
Volume
45 - 2024
Edited by
Paula Meireles, University Porto, Portugal
Reviewed by
Two reviewers who chose to remain anonymous
Updates
Copyright
© 2024 Staub, Ballouz and Puhan.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms. PHR is edited by the Swiss School of Public Health (SSPH+) in a partnership with the Association of Schools of Public Health of the European Region (ASPHER)+
*Correspondence: Kaspar Staub, kaspar.staub@iem.uzh.ch
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.