Dear Editors,
We commend Luo et al. for their in-depth analysis of the current available services in Australia to support people with Long COVID [1]. This devastating illness affects over 10% of those after acute COVID-19 infection and is projected to affect over 200 million people in the next decade worldwide [2]. Many with Long COVID are severely impacted by physical symptoms to the extent that simple activities of daily living are extremely fatiguing, and the demands of travel to a healthcare appointment can trigger episodes of severe post-exertional malaise which has been found to affect over 80% of those with Long COVID [3]. Provision of healthcare should be available in a format that does not worsen symptoms nor impact upon them financially.
As Luo et al. describe, options for Long COVID specialist care in Australia are limited, particularly for people in rural or remote locations [1]. We note, however, that their summary did not review the option of telehealth as a model of care for Long COVID. Telehealth encompasses provision of medical assessment, diagnosis, treatment, and education through the use of technology, including video and telephone-based consultation [4]. Our Australian-based clinic, which was not included in Luo et al.’s review, uses a telehealth model of care and to date has provided care to over 500 people with Long COVID (including children) from all states and territories, including the Northern Territory, which has no other dedicated Long COVID services [1]. Of our cohort, 22% live outside of major metropolitan centres as measured by the Modified Monash model [5] (Figure 1).
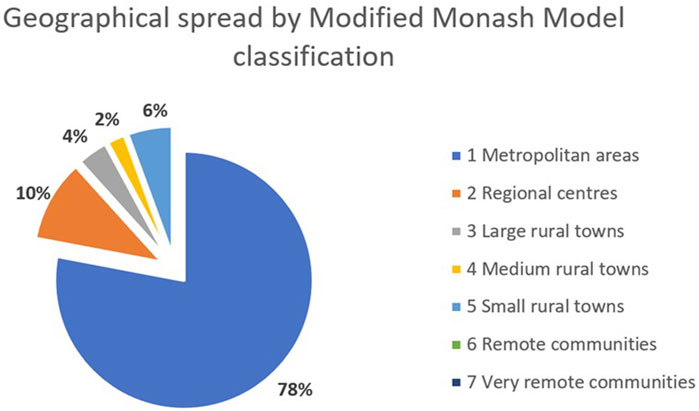
Figure 1. Geographical spread of cohort by Modified Monash Model [5] classification (unpublished data) (Footnote [1]) (Australia. 2023). *Modified Monash (MM) category 1: metropolitan areas in major cities accounting for 70% of Australia’s population; MM2: regional centres within 20 km road distance of town with population over 50,000; MM3: large rural town within 15 km of town with population 15,000 to 50,000; MM4: medium rural town within 10 km road distance of a town with population 5,000 to 15,000; MM5: small rural town, all other areas excluding MM6 and MM7 (remote and very remote communities).
This model of care provides an option for patients with physical [6] or other disability and geographical limitations [7] to equitably access healthcare without physical detriment or disproportionate financial penalty due to travel costs. The need, strengths, safety and limitations of telehealth services to provide rapid and accessible care has been highlighted throughout the COVID-19 pandemic. Systemic changes within the Australian health system provided funding of a wide-scale shift in the modality of care delivery [4], and which have been trialled elsewhere including Canada [8].
The use of telehealth, where service is otherwise limited, provides a real option for many patients to receive care they would not otherwise be able to access [6], and the inability to undertake a physical examination can often be mitigated through close collaboration with the person’s primary care provider. This approach has been successfully demonstrated in several settings including with rehabilitation [9], an important facet of long COVID care. Furthermore, formal and informal consumer feedback from our clinic indicates that this model of care is desired by many people with Long COVID, in keeping with published literature [10]. Luo et al. highlight the importance of consumer engagement and empowerment, and including consumers in discussion about models of care is of paramount importance to be able to provide optimal quality care.
Provision of care for Long COVID must be equitable, should not exacerbate symptoms, and should be designed with consumer needs and opinions at its heart. The benefits of telehealth are numerous for those with Long COVID and should be embedded within systemic strategies to enhance care.
Author Contributions
NW, ET, and MS wrote the manuscript. JM, LA, PH, and AL contributed to data analysis and review of the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors work at a telehealth-based clinic in Australia dedicated to provision of care to long COVID patients. This work was submitted separately to usual care and no payment or other services were received to undertake writing this letter.
References
1. Luo, S, Zheng, Z, Bird, SR, Plebanski, M, Figueiredo, B, Jessup, R, et al. An Overview of Long COVID Support Services in Australia and International Clinical Guidelines, With a Proposed Care Model in a Global Context. Public Health Rev (2023) 44:1606084. doi:10.3389/phrs.2023.1606084
2. Davis, HE, McCorkell, L, Vogel, JM, and Topol, EJ. Long COVID: Major Findings, Mechanisms and Recommendations. Nat Rev Microbiol (2023) 21:133–46. doi:10.1038/s41579-022-00846-2
3. Bonilla, H, Quach, TC, Tiwari, A, Bonilla, AE, Miglis, M, Yang, PC, et al. Myalgic Encephalomyelitis/Chronic Fatigue Syndrome Is Common in Post-Acute Sequelae of SARS-CoV-2 Infection (PASC): Results From a Post-COVID-19 Multidisciplinary Clinic. Front Neurol (2023) 14:1090747. doi:10.3389/fneur.2023.1090747
4. Caffery, LA, Muurlink, OT, and Taylor-Robinson, AW. Survival of Rural Telehealth Services Post-Pandemic in Australia: A Call to Retain the Gains in the ‘New Normal’. Aust J Rural Health (2022) 30(4):544–9. doi:10.1111/ajr.12877
5. Australian Government Department of Health and Aged Care. Modified Monash Model (2023). Available from: https://www.health.gov.au/topics/rural-health-workforce/classifications/mmm#about-the-modified-monash-model (Accessed December 1, 2023).
6. Valdez, RS, Rogers, CC, Claypool, H, Trieshmann, L, Frye, O, Wellbeloved-Stone, C, et al. Ensuring Full Participation of People With Disabilities in an Era of Telehealth. J Am Med Inform Assoc (2021) 28(2):389–92. doi:10.1093/jamia/ocaa297
7. Bradford, NK, Caffery, LK, and Smith, AC. Telehealth Services in Rural and Remote Australia: A Systematic Review of Models of Care and Factors Influencing Success and Sustainability. Rural Remote Health (2016) 16(4):4268–23. doi:10.22605/rrh4268
8. Alami, H, Lehoux, P, Attieh, R, Fortin, JP, Fleet, R, Niang, M, et al. A ‘Not So Quiet’ Revolution: Systemic Benefits and Challenges of Telehealth in the Context of COVID-19 in Quebec (Canada). Front Digit Health (2021) 3:3. doi:10.3389/fdgth.2021.721898
9. Tenforde, AS, Hefner, JE, Kodish-Wachs, JE, Iaccarino, MA, and Paganoni, S. Telehealth in Physical Medicine and Rehabilitation: A Narrative Review. PM R (2017) 9(5):S51–S58. doi:10.1016/j.pmrj.2017.02.013
Keywords: long COVID, telehealth, equity, care model, post COVID-19 condition
Citation: Whyler N, Atkins L, Hogg P, Leong A, Metcalfe J, Scoullar M and Tippett E (2024) Harnessing the Benefits of Telehealth in Long COVID Service Provision. Public Health Rev 45:1606948. doi: 10.3389/phrs.2024.1606948
Received: 08 December 2023; Accepted: 21 May 2024;
Published: 31 May 2024.
Edited by:
Sarah Mantwill, University of Lucerne, SwitzerlandCopyright © 2024 Whyler, Atkins, Hogg, Leong, Metcalfe, Scoullar and Tippett. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
PHR is edited by the Swiss School of Public Health (SSPH+) in a partnership with the Association of Schools of Public Health of the European Region (ASPHER)+
*Correspondence: Naomi Whyler, bmFvbWljYXdoeWxlckBkb2N0b3JzLm9yZy51aw==
 Naomi Whyler
Naomi Whyler Liz Atkins
Liz Atkins