Abstract
Objectives:
To synthesize qualitative evidence on the experience of lay responders performing cardiopulmonary resuscitation (CPR).
Methods:
Qualitative evidence synthesis was performed using the Thomas and Harden method. The PubMed, Cochrane Library, Web of Science, OVID Medline, Embase, CINAHL, CNKI, and WanFang databases were systematically searched. The quality of the research was assessed by the Critical Assessment Skills Program Tool (CASP).
Results:
A total of 5,610 studies were identified, and 9 studies were included in the analysis. Four analytical themes were generated: emotional ambivalence before CPR, psychological tolerance during CPR, perceived experience after CPR, and enhancing psychological resilience.
Conclusion:
Lay responders face complicated psychological experience during CPR, which may be susceptible to psychological effects such as “loss aversion,” “bystander effects” and “knowledge curse.” In addition to the timely retraining of CPR, lay responders should be instructed to manage psychological distress and improve psychological resilience. More importantly, the psychological sequelae may be long-lasting, requiring ongoing psychological intervention and follow-up based on valuing transdisciplinarity across endeavours.
Introduction
Out-of-hospital cardiac arrest (OHCA) is a critical public health concern characterized by high mortality and morbidity and has been identified as contributing factors, including congenital heart disease [1], acute coronary syndrome [2], air pollution [3], viral infections [4], drug abuse [5], etc. Given that cardiac arrest often occurs outside of a medical setting, but the golden time for resuscitation is only 4 min, bystander cardiopulmonary resuscitation (CPR) is essential to save patients’ lives [6]. Ample evidence [7–10] suggests that bystander CPR significantly increases patients’ chances of survival, but without timely and effective CPR and defibrillation, survival rates are less than half, and neurological outcomes are worse [11]. Given these concerns, there is wide consensus on disseminating education on bystander CPR among the general public and even incorporating it into the curriculum for school-aged children [12] to rapidly recognize signs of cardiac arrest and perform immediate and effective CPR.
However, it is of note that the percentage of OHCA patients receiving bystander CPR is significantly low worldwide, ranging between 35% and 45% [13], notwithstanding a myriad of CPR-related training for lay responders [14]. Towards this end, extensive public education has been conducted to encourage lay responders to initiate CPR for unconscious victims who are not breathing [15], but this still cannot adequately prepare lay responders for OHCA patients. There is a growing appreciation that psychological factors may play important roles throughout CPR and even affect future psychological and behavioral performance [16, 17], as lay responders have to face great psychological stress and fear during the whole process of CPR [18], which impacts the decision-making and execution of CPR [19]. In addition, caution is needed after CPR due to the reason that lay responders may experience psychological sequelae for a long time (e.g., self-blame for not providing effective CPR, guilt from fear of poor patient prognosis) and even progressively suffer from posttraumatic stress disorder (PTSD) [20].
There is a critical need for lay responders to overcome fear in the actual rescue process [21] and be equipped with courage, self-confidence and positive attitudinal beliefs [14, 22]. In this regard, stress coping strategies [23] or virtual reality-based CPR simulation training [24] are increasingly being used throughout the CPR training process, and these strategies have been proven to be effective in reducing the attitude, intention and perception of stress among lay responders. Despite this, considering the complexity of the psychological experience of CPR, including the duration of CPR, the prognosis of patients and the attitudes of professional rescuers may have important impacts on the psychological experience of lay responders [17]. It is necessary to expand the training of CPR to include the psychological experience of lay responders [25, 26], which may have important reference value for improving the attitudes and willingness of lay responders toward CPR.
To reduce the incidence of psychological sequelae, improve self-perception of the implementation of CPR and increase the response rate, qualitative studies [26–28] have been conducted to explore the feelings, experience, and coping strategies of lay responders performing CPR in recent years. By gaining a deeper understanding of the challenges and experience faced by lay responders, healthcare providers can better equip them with the mental health support and training needed to provide effective CPR in OHCA patients, save lives and reduce the risk of brain injury. However, individual primary studies involve different cultural backgrounds, methodologies, and values, which may not comprehensively reflect the psychological experience of this population. Furthermore, caution is needed when extrapolating these findings and guiding optimal behaviors, given that a systematic evaluation to integrate and summarize the related research findings is lacking. To overcome this hurdle, a qualitative systematic synthesis is needed by summarizing the real perceptions and elucidating the feelings of lay responders performing CPR, which touch on the potential importance of providing more contextualized training based on the experience of actual responders, implementing targeted psychological interventions, and informing policy development for healthcare providers.
Methods
Study Design
The review was based on a synthesis of thematic findings from qualitative studies (PROSPERO ID: CRD42022360427). In this meta-synthesis, we performed thematic synthesis following the steps outlined by Sandelowski and Barroso. This review used the ENTREQ statement, which enhances the transparency framework for qualitative research reporting, to ensure the normative and transparent nature of the research findings [29].
Search Strategy
We searched the following eight databases in September 2023: PubMed, Cochrane Library, Web of Science, OVID Medline, Embase, CINAHL, CNKI, and Wanfang. The search terms used were “qualitative research,” “Cardiopulmonary resuscitation,” and “First responder.” The search strategy for each database is described in Supplementary Appendix S1.
Inclusion and Exclusion Criteria
We developed a sensitive and comprehensive search strategy based on the SPIDER tool (sample, phenomenon of interest, design, evaluation, research type) [30]. The inclusion criteria were as follows: lay responders who performed CPR; lay responders who had real experience performing CPR; original research published in English or Chinese; journal articles; and qualitative research. The exclusion criteria were as follows: quantitative studies, mixed studies, or reviews.
Study Selection and Data Extraction
The search results were imported into Endnote X9, and duplicate studies were removed. Two reviewers independently screened the title, abstract, and full text (NL and CS), and disagreements were discussed and resolved by a third reviewer for inclusion (ZPC). We ultimately included nine studies with the following PRISMA flow chart (Figure 1). Two authors used Microsoft Excel to independently extract key information from the articles, including authors, year, country, sample, methods, study aims, and main findings. Disagreements were resolved through consultation and discussion. In addition, we independently extracted quotations from the articles for qualitative integration analysis.
FIGURE 1
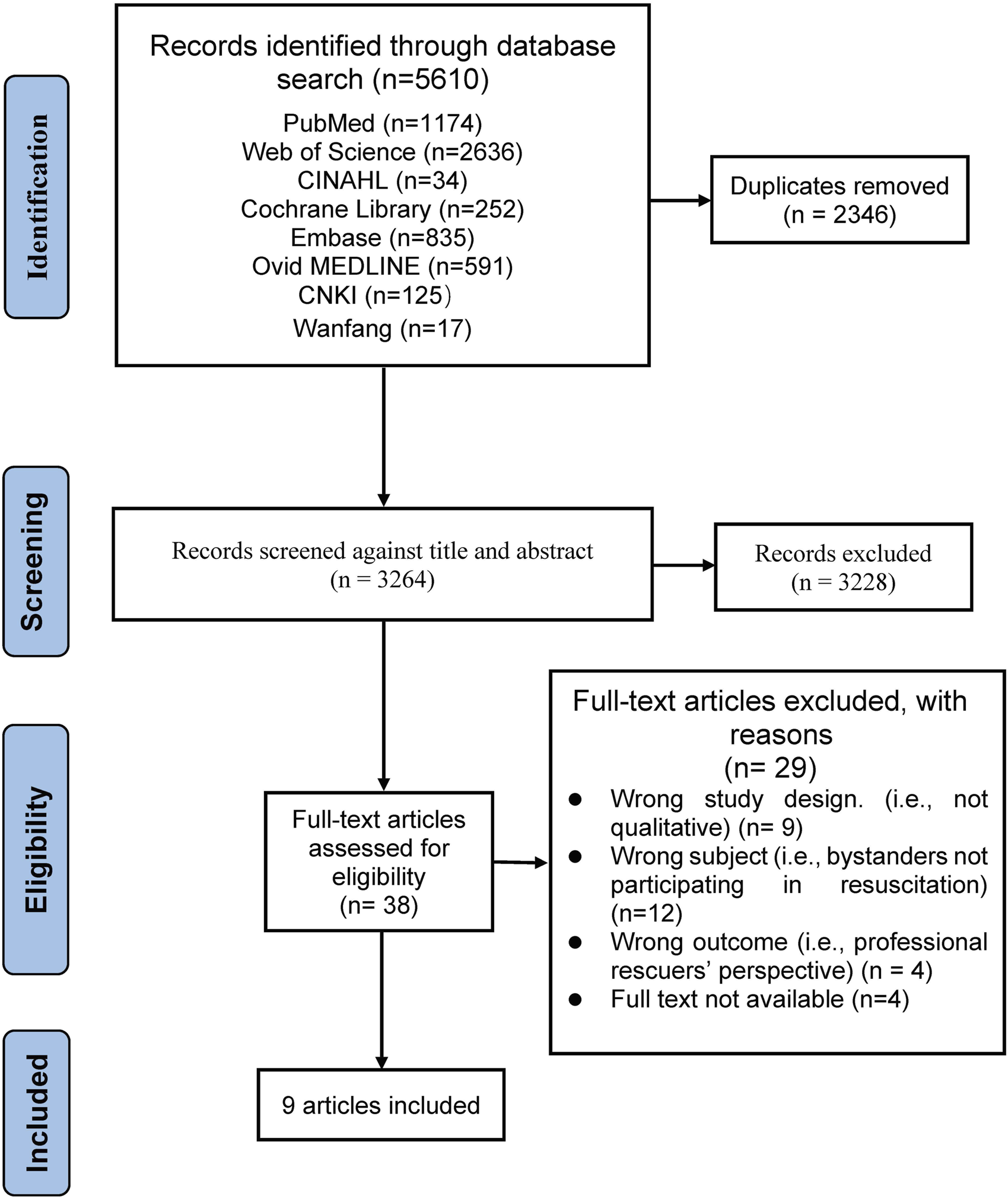
PRISMA flow chart of the search strategy results (China, 2023).
Appraisal of Methodological Quality
To ensure the quality of the study results, all studies were methodologically measured through the Critical Appraisal Skills Programme (CASP) [31]. Two researchers (NL and CS) independently measured the quality of each article, and disagreements were resolved through discussion with a third reviewer (WZ). The grade of quality assessment was not used as an inclusion or exclusion criterion for the literature in this study. The quality appraisal process is shown in Table 1.
TABLE 1
| Axelsson [26] (2000) | Chen [32] (2020) | Hasselqvist [33] (2018) | Moller [16] (2014) | Mathiesen [34] (2016) | Mathiesen [35] (2017) | Mausz [27] (2018) | Skora [28] (2001) | Yang [36] (2022) | |
|---|---|---|---|---|---|---|---|---|---|
| Item 1 | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Item 2 | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Item 3 | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Item 4 | Y | U | N | Y | Y | Y | Y | Y | Y |
| Item 5 | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Item 6 | N | U | U | U | U | N | N | U | N |
| Item 7 | U | U | Y | Y | Y | Y | U | Y | Y |
| Item 8 | Y | Y | Y | Y | Y | Y | Y | Y | U |
| Item 9 | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Item 10 | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Overall scores | 8.5 | 8 | 8.5 | 9.5 | 9.5 | 9 | 8.5 | 9.5 | 8.5 |
| Quality grade | Moderate to High | Moderate to High | Moderate to high | High | High | High | Moderate to High | High | Moderate to High |
Results of the critical appraisal of the included studies (China, 2023).
Noted: Y = Yes (1 point); N = No (0 points); U = Unclear (0.5 points). Item 1, Was there a clear statement of the aims of the research?; Item 2, Is a qualitative methodology appropriate?; Item 3, Was the research design appropriate to address the aims of the research?; Item 4. Was the recruitment strategy appropriate to the aims of the research?; Item 5, Was the data collected in a way that addressed the research issue?; Item 6, Has the relationship between the researcher and participants been adequately considered?; Item 7, Have ethical issues been taken into consideration?; Item 8, Was the data analysis sufficiently rigorous?; Item 9, Is there a clear statement of findings?; Item 10, Was this research valuable?
Data Synthesis and Assessment
We used a three-stage thematic synthesis approach for the analysis, a process that was carried out by two researchers [37]: 1) using Microsoft Excel to code all quotes; 2) generating descriptive topics; and 3) developing analytical themes. We used the GRADE‐CERQual (Confidence in the Evidence from Reviews of Qualitative Research) approach to assess our confidence in each finding [38]. We assessed four components of methodological limitations [39], adequacy [40], coherence [41], and relevance [42]. All disagreements were resolved by discussion and confirmed by a third author (ZPC). The credibility assessment of the study results is presented in Supplementary Appendix S2 [43].
Rigor, Trustworthiness, and Reflexivity
Our study illustrates this point by analysing the quotes from the original study. The research team members included nurses, librarians, research assistants and Red Cross members. Nurses and librarians were trained in qualitative research methods. During the study, team members communicated regularly in online meetings, and all disagreements were resolved through discussions. Finally, we presented the findings to lay responders who had experienced OHCA rescue and incorporated their recommendations into the final analytical themes.
Results
Characteristics of the Included Studies
These nine qualitative studies included 150 participants from six countries (Sweden, China, Norway, Denmark, Canada, United States) who participated in OHCA resuscitation. The characteristics of this study are shown in Table 2. We extracted a total of 207 quotes from the 9 included articles, synthesized 24 new findings according to the meaning of the introductions, and integrated 24 findings into 8 new categories and 4 integrated outcomes. All key supporting quotes per theme are shown in Supplementary Appendix S3.
TABLE 2
| Authors/(Year) | Country | Participants | Methods | Study aims | Main findings |
|---|---|---|---|---|---|
| Axelsson et al., 2000 [26] | Sweden | N = 19, Aged 22–64, F/M, 11/8), Outcome: (S/D/U, 5/12/2) | Purposive sampling; focus group and in- dividual interviews; content analysis | To know more about the bystanders’ perceptions of their intervention |
Theme 1) To have a sense of humanity Theme 2) To have competence Theme 3) To feel an obligation Theme 4) To have courage Theme 5) To feel exposed |
| Chen et al., 2020 [32] | China | N = 9, Aged 28–40, (F/M, 4/5), Outcome: (S, 9) | Semistructured interview; Grounded theory | Explore the experience of lay rescuers who had performed CPR and AED in public locations in Taiwan |
Theme 1) Motivation Theme 2) Training reality discrepancy Theme 3) Psychological influence |
| Hasselqvist et al., 2018 [33] | Sweden | N = 22, Aged 23–54, (F/M, 5/17), Outcome: not reported | Purposive sampling; semistructured in-depth interviews; critical incident technique (CIT) and inductive qualitative content analysis | To explore firefighters’ and police officers’ experience of responding to OHCA in a dual dispatch |
Theme 1) Preparedness Theme 2) Managing the scene Theme 3) The aftermath caring for rescuers |
| Moller et al., 2014 [16] | Danish | N = 33, (F/M, 16/17) Outcome: not reported |
Semistructured interview; phenomenological method | To explore the concept of debriefing bystanders after participating in an OHCA resuscitation |
Theme 1) Identification of OHCA. Theme 2) Emotional and perceptual experience with OHCA. Theme 3) Collaboration with healthcare professionals Theme 4) Patient outcome Theme 5) Reflexions |
| Mathiesen et al., 2016 [34] | Norway | N = 20, Aged 24–69, Outcome: (S/D/U, 14/5/1) | Snowball sampling; Semi structured in-depth interviews; content analysis | To explore reactions and coping strategies in lay rescuers who have provided CPR to OHCA. |
Theme 1) Concern Theme 2) Uncertainty Theme 3) Coping strategies |
| Mathiesen et al., 2017 [35] | Norway | N = 10, Aged 24–69, (F/M, 4/6) Outcome: not reported |
Semistructured interviews; content analysis | To gain a better understanding of why barriers to providing CPR are overcome |
Theme 1) Valuing life itself Theme 2) Comprehension Theme 3) Normative obligation Theme 4) Confidence Theme 5) Context-specific CPR. |
| Mausz et al., 2018 [27] | Canada | N = 12, Aged 24–65, (F/M, 4/8) Outcome: not reported |
Semistructured in-depth interviews and focus group; constructivist grounded theory | What is the experience of bystanders who have attempted to resuscitate the victim of a sudden, out-of- hospital cardiac arrest? |
Theme 1) Being called to act Theme 2) Taking action Theme 3) Making sense of the experience |
| Skora et al., 2001 [28] | United States | N = 12 Average age 45, (F/M, 2/10) Outcome: not reported |
Purposive sampling | To examine the thoughts, feelings, and motivations of laypersons who have attempted to resuscitate a stranger |
Theme 1) Description of the resuscitation attempt Theme 2) Thoughts and feelings on first seeing the person who required resuscitation Theme 3) Thoughts and feelings during the course of the resuscitation event Theme 4) Thoughts and feelings immediately after the resuscitation event Theme 5) Discussion of feelings after the resuscitation event Theme 6) What motivated providing lifesaving measures to a stranger Theme 7) Hesitations, barriers, and obstacles to providing lifesaving measures Theme 8) Responses of prehospital providers to the respondents Theme 9) Recommendations for future CPR classes |
| Yang et al., 2022 [36] | China | N = 10, Aged 26–40, (F/M, 5/5) Outcome: not reported |
Purposive sampling; semistructured in-depth interviews; content analysis | To explore the first responder experience of CPR. |
Theme 1) First responders had a sense of responsibility and empathy Theme 2) First aid literacy of first responder needed to be improved Theme 3) First responder lacked professional first aid knowledge Theme 4) The first responder had heavy psychological pressure load during CPR, which was difficult to adjust Theme 5) The outcome of CPR will have far-reaching impact on the career achievement of the first responder |
Characteristics of the included studies (China, 2023).
Noted: OHCA: out-of-hospital cardiac arrest; CPR: cardiopulmonary resuscitation; EMS: emergency medical services; BLS: basic life support; AED: automated external defibrillator; M/F: Male/Female; S/D/U: Survived/Died/Unknown.
Emotional Ambivalence Before Cardiopulmonary Resuscitation
When faced with OHCA, lay responders may experience a variety of reactions, such as stress and panic in the face of unknown events, ambivalence about the need for help, and helplessness when unable to judge the patient’s condition, which are closely related to the respondents’ proficiency in CPR, previous experience performing CPR, and awareness of the importance of CPR. Of course, strong psychological quality and self-confidence, as well as encouragement and support from people around them, are also indispensable.
Pre-resuscitation Reaction
OHCA is sudden and unprepared, which may create panic among lay responders who do not know what is going on and who feel overwhelmed, especially for people who have not previously been involved in CPR.
“Having somebody go down like that, it’s the first time I have ever seen something like that. It was like “Oh [expletive]! What is going on?” [27]
“She was lying on her back. And was not well, that was obvious. She was not conscious, but there was a sort of breathing. It was quite obvious she was really not well.” [16]
When other people are present at the scene of an accident, lay responders may think that someone else may be able to help instead. The main reason may be the lack of self-confidence of lay responders, who are worried that their irregular rescue measures may cause greater harm to patients.
“I wondered if I should get involved and was there a possibility that I could make the situation worse. I looked around to see if anyone was making a move to help him no one was.” [28]
Of course, there are some lay responders who know the importance of racing against the clock to save patients’ lives. They help patients as much as they can by shouting for help, calling 911, or conducting a pre-CPR assessment.
“[I thought] this guy needs help; activate 911. He's unconscious and pale. Check for breathing and pulse.” [28]
Factors Influencing Cardiopulmonary Resuscitation Implementation
Factors such as lay responders’ knowledge, psychological readiness, values, and perceptions of outcomes can influence their behaviors. For responders who have attended training, training can be methodical. In addition, the family and friends of lay responders can affect their decisions in the face of patients’ need for CPR.
“At the time, I felt really calm. I knew exactly what to do. It was very fortunate, because first I had done the course and after that the revision course, which I had done quite recently, only a few months earlier.” [26]
“When I was young, my family and friends affected my thought and behavior very much.” [32]
Psychological Tolerance During Cardiopulmonary Resuscitation
For lay responders, after overcoming the fear of starting resuscitation, there are still many difficulties in the process of resuscitation, which mainly include unreliable knowledge of CPR, learning theoretical knowledge without actual participation, or affecting the operation of resuscitation due to stress and tension. In addition, because of possible blood or body fluid exposure and the unknown condition of the patient’s disease, bystander respondents also considered their own safety or prevention of infection. In this case, support from professional rescue workers, respiratory balloon assistance instead of mouth-to-mouth artificial respiration or performing hands-only CPR can help lay responders better complete the rescue of patients.
Psychological Conflicts in Complex Situations
The respondents were confused about chest compressions. Most respondents were confused about the location and intensity of the compressions.
“But I figured anywhere around the chest is a good thing.” [27]
In particular, if an accident occurs during compressions, such as a broken rib, this can leave the responder uncertain about his or her actions and unsure of the next step to take.
“When I heard a rib crack, then I wondered if I was doing it correctly, but still I went on.” [26]
The automated external defibrillator (AED) has a built-in voice prompting system, so it is only necessary to follow the step-by-step instructions in the use of the AED, but there are still problems in the use of the AED by lay responders.
“Others tended to misinterpret the prompts from the defibrillator, thinking the beeping metronome meant that they were performing compressions incorrectly.” [27]
Some responders are concerned about spreading infectious diseases after artificial respiration to strangers, and they consider cleaning their own mouths to be a necessary protective behavior.
“When we arrived at the hospital, I cleaned my mouth in the washroom because he was a stranger. Cleaning the mouth is a necessary behavior.” [32]
Desire to Be Assisted by Others
Lay responders crave support and assistance in delivering life-saving treatment. The online dispatcher directing the lay responders to perform the operation made them feel in control, overcoming inner fears and calming down.
“For one thing, you do not feel so alone; and you have a voice that gives you instructions without increasing the intensity by even a small amount.”(42)
At the same time, lay respondents also said that support from people around them would give them strength.
“One person told me that I ought to compress the chest continuously. I had the courage to keep chest compressions.” [32]
The respondents were eager to receive support from medical personnel and positive comments about their behaviors, which would alleviate their internal uncertainty.
“It was very nice that the physician calmly talked to the people involved, while the other staff was packing up the patient.” [16]
Perceived Experience After Cardiopulmonary Resuscitation
After lay responders perform CPR, they may try to understand the patient’s prognosis to express their concern for the patients and assess the quality of their CPR. This may have different impacts. On the one hand, the successful rescue of patients will increase the self-confidence of lay responders and strengthen the courage to carry out CPR again; on the other hand, the experience of failure rescue may increase the likelihood of long-standing psychological sequelae, such as self-doubt, guilt, and psychological fear in lay responders.
Post-resuscitation Perceptions
Regardless of whether the results were good or bad, lay respondents were eager to obtain results, believing it was their right. Lay responders were happy that the patients survived and were confident about performing bystander CPR next time.
“I wondered about the outcome. I looked in the newspaper … …. Did we manage this, or did we not?” [34]
However, if the patient has a poor prognosis or dies, they will doubt their own ability, wonder why they failed, and experience negative emotions as a result.
“When I heard word [that] he passed, that was hard … …. Is it because I did not run fast enough? Was I supposed to start the process?” [27]
Responders feel confident about helping again after experiencing real-life resuscitation, and they will be more confident and quicker to initiate resuscitation procedures in similar scenarios.
“I believe I can make a quicker decision to start CPR next time.” [32]
Subsequent Impact
Because OHCA usually occurs when the respondent is unprepared, it is an unexpected and frightening experience for the respondent, who may experience physiological reactions such as nightmares, vomiting, and loss of appetite following the rescue.
“I felt terrible. Plus, I was throwing up. I probably saw the victim’s face in my dreams for a month.” [28]
Of course, some respondents experienced psychological problems, such as depression, anxiety, and situational flashbacks. These psychological problems are especially prominent when they pass through the place of the incident.
“I cannot go in the room [where the incident occurred]; I cannot even look at that door because my anxiety goes through the roof.” [27]
Enhancing Psychological Resilience
After providing CPR, some lay responders choose to ease psychological stress after OHCA through self-adjustment, self-relaxation or increased communication with family and friends. Of course, some lay responders consulted medical staff or psychological counsellors to seek more systematic guidance and help. In addition, empathy from other lay responders who have the same experience is also important. Psychotherapy is not achieved overnight and requires long-term maintenance and enhancement of the psychological resilience of lay responders.
Coping Strategies
Lay responders experience different physical and psychological reactions after performing CPR. They will adopt different coping strategies to return their lives to normal. In general, talking with others can make them feel calm and understood.
“I spoke to my mother-in-law about it. I just told her what happened. I just had to calm down and so on.” [16]
Some respondents opted for a self-acceptance approach to self-adaptation, and they began to think positively about the relationship between life and death.
“I’ve got the answers. I’ve got the information I needed. I’ve had the rest, now it’s time to move forward.” [27]
At the same time, respondents expressed the desire for psychological support after recovery and the idea of receiving medical staff consultation, whether in the short term or long term, which seems to be crucial for respondents.
“It was a kind of first aid to me, and I liked that. Because when standing in the middle of it all and experiencing all that, the ambulance crew have to help other people. But no one helped me.” [16]
The respondents expressed the importance of communicating with healthcare professionals, and this communication can enhance lay responders’ skills, increase confidence in potentially performing CPR in the future, and increase positive perceptions of their own performance.
“I think it was nice to talk to a professional who knows what it is about 100 percent.” [16]
Previous Experience Performing Cardiopulmonary Resuscitation
Lay responders offer some suggestions: bridging the gap between training and the reality of recovery, focusing on the physical and mental health of the respondent. In addition, Lay responders suggested adding the importance of sharing the real-life experience of rescuers to training, as this experience may help trainees mentally prepare for the actual implementation of CPR and enhance coping strategies.
“If you are trained but cannot use your skills, then the training is meaningless. You could consider preparing people on how surrealistic a situation it is.” [16]
After resuscitation, it is important to provide appropriate support to lay responders. This can include actively communicating with them after they have provided first aid, paying attention to their mental health, and taking steps to prevent psychological distress.
“Stressing the spiritual and philosophical nature of death and the importance of speaking with someone after the experience.” [28]
Lay responders also expressed their views on the training courses. The frequency of courses should be increased, sufficient practice and feedback opportunities for trainees should be provided, and workplace employee training should be increased.
“Lower student-to-teacher ratio, lots of practice time and feedback opportunities.” [28]
Discussion
This study identified, reviewed, and synthesized nine qualitative articles that systematically explored the experience of lay responders performing CPR, and 4 analytical themes were generated: emotional ambivalence before CPR; psychological tolerance during CPR; perceived experience after CPR; and enhancing psychological resilience. Our findings highlight the importance of improved CPR training and follow-up social support for lay responders. The results of this study show that lay responders experience a series of emotional reactions before CPR and make complex decisions immediately under stressful conditions, which is consistent with the findings of previous studies [44, 45]. Our review suggested that the most common emotional reaction of lay responders to CPR was panic. Therefore, patients exhibit certain characteristics that may exacerbate the emotional reactions of lay responders. This can be attributed to the lack of experience and psychological preparation for lay responders performing CPR, as some emergency responders may experience psychological stress reactions due to past traumatic events, which can also affect their performance in CPR [46]. There is often discomfort associated with initiating CPR due to concerns about inappropriate or unethical resuscitation attempts. This can affect individuals’ willingness to perform CPR even after receiving training.
In addition to the emotional reactions of lay responders, the results also showed the “bystander effect,” where the presence of others makes lay responders hesitate to provide assistance, and they experience conflicting psychological reactions [47]. Interestingly, some responders perceive the presence of others as moral support, especially when people know each other, which reduces the indifferent attitude of lay responders [48]. In a study designed to investigate bystander witness type and receipt of bystander CPR [49], the investigators included 10,016 OHCA patients and showed that nonfamily witnessed OHCA patients were less likely to receive bystander CPR, confirming that witness type may have a potential impact. Indeed, the majority of OHCAs occur in residential areas or at home [50, 51]. Based on this, capitalizing on the bystander effect and conducting home-centered CPR training would be beneficial for improving the response rate of lay responders to family members in potential cardiac arrest and promoting survival from OHCA in residences. In addition, bystander indifference is caused by reflexive emotional reactions depending on the personality of the bystander [52]. This indicates that current training courses focus on skills and may not adequately prepare lay responders psychologically. It is worth noting that personality is also influenced by factors in the cultural environment of the East and West. Based on the results of the literature we included, it was shown that Easterners have conservative personalities, which may influence them to initiate bystander CPR in cases of uncertainty or lack of confidence [34], whereas Westerners are bold, enthusiastic and risk-taking, and are more likely to take action when they have some knowledge base [16]. Future training courses should consider the cognitive and complex emotional processes based on diverse cultural settings that occur during OHCA and expand the design of integrated emotional, motivational, and personality training interventions.
In the same vein, the possible knowledge curse in CPR training should not be ignored [53]. The curse of knowledge refers to the tendency for individuals to be influenced by their own knowledge and experience, which can lead to biases when attempting to understand or appreciate perspectives that are more naive or uninformed [54]. The reason for the “curse of knowledge” among CPR trainers is based on the tendency of others to share the same level of understanding and skills as oneself. Actually, the complexity and technical nature of CPR training require a high level of proficiency from instructors, whereas there is a significant gap between theoretical knowledge and practical skills retention among lay responders. First, lay responders find it difficult to identify signs of cardiac arrest, which may lead to delayed CPR. Studies have shown that the inability to identify a patient’s blueness, abnormal breathing, and vital signs may be obstacles for lay responders [55]. This is consistent with our integration results. In addition, lay responders reported various difficulties during the resuscitation process, such as problems with the location and force of chest compressions. The reasons for these difficulties may be the lack of proficiency of the trainer, which causes excessive tension in real situations and leads to the failure of technical points, or the inability of simulation training to simulate multiple emergency situations, resulting in the inability to respond to various emergencies. The key to maintaining skills depends on the frequency and timing of retraining, and regular CPR training every 6 months is recommended to ensure that lay responders maintain their practical CPR skills [56]. In simplified terms, the knowledge curse in CPR training can be mitigated by ensuring regular and timely retraining, employing effective teaching methods that focus on practical skills, and addressing attitudes towards CPR to encourage its use in emergency situations.
During CPR, strong psychological tolerance plays a pivotal role in effective resuscitation, which is susceptible to theoretical knowledge, practice, patient condition and surroundings. In addition, loss aversion may touch on the potential importance of performing CPR. Loss aversion, as discussed in the provided evidence, refers to the psychological phenomenon where individuals exhibit a strong dislike or fear of loss, particularly when it involves significant aspects of their identity or wellbeing [57]. The psychological impact of loss aversion can affect how lay responders perceive and manage their own reactions to CPR scenarios. For instance, the fear of losing a patient can lead to increased stress and anxiety among clinicians, which might affect their performance during CPR. This internal conflict between the desire to save lives and the fear of causing unnecessary harm or loss can complicate the resuscitation process. Loss aversion in the context of CPR involves a complex interplay of psychological factors that influence patient and provider behaviors and decisions. Understanding these dynamics is crucial for improving communication strategies and providing more effective support during critical care situations. It also highlights the need for comprehensive training and support systems for healthcare providers to help lay responders manage their reactions to potential losses and make informed decisions that align with both ethical standards and patient safety [58].
Of note, early defibrillation during CPR is one of the key factors in improving the prognosis of patients with OHCA [59, 60]. The results of an observational study based on 8,269 patients with OHCA showed that for OHCA occurring in public, patients had the highest probability of surviving to hospital discharge if they received both bystander-initiated CPR and defibrillation performed by a bystander (OR 4.33, 95% CI 2.11–8.87) [61]. However, many lay responders seem to have some psychological fear and lack experience using AEDs. In the included literature, two papers elucidated the barriers to the use of AEDs among lay responders, highlighting the potential importance of AED training in basic life support courses [62]. Previous studies have shown that the correct use of AEDs does not require specific skills [63], only following voice prompts. This encourages untrained lay responders to use AEDs [64]. Cardiac arrest is a rapidly evolving crisis situation in a dynamic environment that requires emergency personnel to perform highly technical interventions to save lives under emotional stress [65]. Current CPR training seems unable to cope with real-life resuscitation, and lay responders need more support in terms of both psychological preparation and technical training. It is recommended that contextualized CPR training be developed based on the real experience of lay responders, specifically by incorporating descriptions of the difficulties experienced by lay responders who prepare them for realistic recovery.
More importantly, after CPR, lay responders face diverse perceived experience, which should be prioritized in future studies. According to our integrated results, most lay responders actively adjusted their cognition and took positive action, whereas a proportion of lay responders have to face short-term psychological stress and self-doubt [27]. Moreover, the psychological impact of witnessing such a life-threatening event can lead to long-term psychological distress, including symptoms of PTSD, anxiety, and depression [66]. Social support plays a crucial role in mitigating these psychological impacts. Studies have shown that perceived social support is strongly associated with better recovery outcomes following trauma or illness [67]. In the context of cardiac events, both the presence of social support and the quality of this support are critical factors that influence the psychological wellbeing of individuals involved [68]. An alternative approach is that the coping strategies of lay responders are in line with stress coping theory [69]. Coping theory defines coping as an effort by an individual to deal with demands from the environment, with the aim of making these demands tolerable and reducing stress and conflict [69]. This theory provides guidance and a reference for individuals to cope with stressful events, including the psychological stress experienced by lay responders after performing CPR. According to this theory, individuals can take the following measures to cope with such stress: first, they can actively adjust their cognition by practicing positive thinking and reinterpreting the event to reduce the impact of negative emotions; second, they can seek external information and professional support and help, such as communicating with family, friends, and professionals for advice and support; and finally, they can take positive actions, such as participating in psychological counselling, physical exercise, and relaxation training activities, to alleviate psychological stress. Taken together, we need to pay more attention to the life status of lay responders and provide them with personalized psychological counselling services and follow-up system support.
Limitations
Some limitations of this study should not be ignored. First, selection bias is unavoidable due to the reason that not all lay CPR rescuers are willing to recall and participate in research, and usually, the subjects who can be interviewed are those who have succeeded in rescue or who have a positive attitude. These biases can influence the integrity of the integrated findings. Second, we did not account for the interaction between lay responders and professional medical responders, which may potentially influence the performance and response of lay responders. Future research should consider incorporating variables that reflect the relationship dynamics between these groups to better understand their impact on emergency response outcomes. In addition, few studies included in our analysis noted the time interval between performing CPR and collecting qualitative data, which may have introduced recall bias and affected the results. Finally, qualitative research is deeply embedded in specific cultural and contextual settings. Integrating findings across different cultures or contexts can be challenging due to varying social norms, values, and behaviors.
Conclusion
This study systematically assessed real experience of lay responders performing CPR. Our results emphasize that, in addition to attaching importance to CPR training, healthcare professionals should fully understand the real experience of lay responders and promptly intervene in possible psychological sequelae to improve the response rate of lay responders and promote public health. As noted, our knowledge of lay responders’ perceptions of performing CPR can compensate for biases in medical research regarding treatment outcomes, clinical providers, and decision-making by reflecting the true perspective of lay responders’ experience performing CPR. Additionally, the emotional and psychological impacts of CPR, which are susceptible to “loss aversion” and “bystander effects,” as well as the “knowledge curse” during CPR implement and training, can also affect the enthusiasm of lay responders to perform effectively in future incidents. Not surprisingly, these findings support the emerging consensus that incorporating these factors into our analysis could provide a more comprehensive understanding of the psychological dynamics of lay responders throughout the CPR process.
Statements
Author contributions
NL: Conceptualization; Methodology; Formal analysis; Supervision; Writing - original draft; Writing - review and editing; Project administration. CS: Conceptualization; Methodology; Data curation; Formal analysis; Investigation; Writing review and editing; Writing original draft. RW: Conceptualization; Supervision; Writing original draft; Writing review and editing. XY: Conceptualization; Visualization; Writing - original draft. LG: Conceptualization; Data curation; Formal analysis; Writing original draft; Methodology; Investigation; Project administration; Writing review and editing. WZ: Conceptualization; Formal analysis; Methodology; Supervision; Validation; Writing - original draft; Writing review and editing. ZC: Conceptualization; Formal analysis; Methodology; Supervision; Validation; Writing original draft; Writing review and editing. All authors contributed to the article and approved the submitted version.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that they do not have any conflicts of interest.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/phrs.2024.1606650/full#supplementary-material
References
1.
Barcella CA Christensen DM Idorn L Mudalige N Malmborg M Folke F et al Outcomes of Out-Of-Hospital Cardiac Arrest in Adult Congenital Heart Disease: A Danish Nationwide Study. Eur Heart J (2023) 44:3264–74. 10.1093/eurheartj/ehad358
2.
Paratz ED van Heusden A Smith K Brennan A Dinh D Ball J et al Factors Predicting Cardiac Arrest in Acute Coronary Syndrome Patients Under 50: A State-Wide Angiographic and Forensic Evaluation of Outcomes. Resuscitation (2022) 179:124–30. 10.1016/j.resuscitation.2022.08.016
3.
Pan C Xu C Zheng J Song R Lv C Zhang G et al Fine and Coarse Particulate Air Pollution and Out-Of-Hospital Cardiac Arrest Onset: A Nationwide Case-Crossover Study in China. J Hazard Mater (2023) 457:131829. 10.1016/j.jhazmat.2023.131829
4.
Garcia R Warming PE Hansen CJ Rajan D Torp-Pedersen C Benfield T et al Out-of-Hospital Cardiac Arrest in Individuals With Human Immunodeficiency Virus: A Nationwide Population-Based Cohort Study. Clin Infect Dis (2023) 77:1578–84. 10.1093/cid/ciad422
5.
Trytell A Osekowski M Zentner D Nehme Z James P Pflaumer A et al Prevalence of Illicit Drug Use in Young Patients With Sudden Cardiac Death. Heart Rhythm (2023) 20:1349–55. 10.1016/j.hrthm.2023.06.004
6.
Tian L Qiu H . Environmental Factors and Out-Of-Hospital Cardiac Arrest. Eur Heart J Qual Care Clin Outcomes (2017) 3(2):97–8. 10.1093/ehjqcco/qcw061
7.
Riva G Ringh M Jonsson M Svensson L Herlitz J Claesson A et al Survival in Out-Of-Hospital Cardiac Arrest After Standard Cardiopulmonary Resuscitation or Chest Compressions Only Before Arrival of Emergency Medical Services: Nationwide Study During Three Guideline Periods. Circulation (2019) 139:2600–9. 10.1161/CIRCULATIONAHA.118.038179
8.
Park GJ Song KJ Shin SD Lee KW Ahn KO Lee EJ et al Timely Bystander CPR Improves Outcomes Despite Longer EMS Times. Am J Emerg Med (2017) 35(8):1049–55. 10.1016/j.ajem.2017.02.033
9.
Hawkes C Booth S Ji C Brace-McDonnell SJ Whittington A Mapstone J et al Epidemiology and Outcomes From Out-Of-Hospital Cardiac Arrests in England. Resuscitation (2017) 110:133–40. 10.1016/j.resuscitation.2016.10.030
10.
Adielsson A Hollenberg J Karlsson T Lindqvist J Lundin S Silfverstolpe J et al Increase in Survival and Bystander CPR in Out-Of-Hospital Shockable Arrhythmia: Bystander CPR and Female Gender Are Predictors of Improved Outcome. Experiences From Sweden in an 18-Year Perspective. Heart (2011) 97(17):1391–6. 10.1136/hrt.2011.222711
11.
Grunau B Kime N Leroux B Rea T Van Belle G Menegazzi JJ et al Association of Intra-Arrest Transport vs Continued On-Scene Resuscitation With Survival to Hospital Discharge Among Patients With Out-Of-Hospital Cardiac Arrest. Jama (2020) 324(11):1058–67. 10.1001/jama.2020.14185
12.
Fodale V Angileri FF Antonuccio P Basile G Benedetto F Leonetti D et al The Dramatic Increase in Sudden Cardiac Deaths and the Alarming Low Survival: A Global Call to Action to Improve Outcome With the Engagement of Tertiary Education System. J Educ Health Promot (2023) 12:164. 10.4103/jehp.jehp_1385_22
13.
White AE Ho AF Shahidah N Asyikin N Liew LX Pek PP et al An Essential Review of Singapore's Response to Out-Of-Hospital Cardiac Arrests: Improvements Over a Ten-Year Period. Singapore Med J (2021) 62(8):438–43. 10.11622/smedj.2021114
14.
Farquharson B Dixon D Williams B Torrens C Philpott M Laidlaw H et al The Psychological and Behavioural Factors Associated With Laypeople Initiating CPR for Out-Of-Hospital Cardiac Arrest: A Systematic Review. BMC Cardiovasc Disord (2023) 23(1):19. 10.1186/s12872-022-02904-2
15.
Brooks SC Simmons G Worthington H Bobrow BJ Morrison LJ . The PulsePoint Respond mobile Device Application to Crowdsource Basic Life Support for Patients With Out-Of-Hospital Cardiac Arrest: Challenges for Optimal Implementation. Resuscitation (2016) 98:20–6. 10.1016/j.resuscitation.2015.09.392
16.
Møller TP Hansen CM Fjordholt M Pedersen BD Østergaard D Lippert FK . Debriefing Bystanders of Out-Of-Hospital Cardiac Arrest Is Valuable. Resuscitation (2014) 85(11):1504–11. 10.1016/j.resuscitation.2014.08.006
17.
Axelsson A Herlitz J Karlsson T Lindqvist J Reid Graves J Ekström L et al Factors Surrounding Cardiopulmonary Resuscitation Influencing Bystanders' Psychological Reactions. Resuscitation (1998) 37(1):13–20. 10.1016/s0300-9572(98)00027-6
18.
Krage R Zwaan L Tjon Soei Len L Kolenbrander MW van Groeningen D Loer SA et al Relationship Between Non-Technical Skills and Technical Performance During Cardiopulmonary Resuscitation: Does Stress Have an Influence? Emerg Med J (2017) 34(11):728–33. 10.1136/emermed-2016-205754
19.
Hunziker S Pagani S Fasler K Tschan F Semmer NK Marsch S . Impact of a Stress Coping Strategy on Perceived Stress Levels and Performance during a Simulated Cardiopulmonary Resuscitation: A Randomized Controlled Trial. BMC Emerg Med (2013) 13:8. 10.1186/1471-227X-13-8
20.
Zijlstra JA Beesems SG De Haan RJ Koster RW . Psychological Impact on Dispatched Local Lay Rescuers Performing Bystander Cardiopulmonary Resuscitation. Resuscitation (2015) 92:115–21. 10.1016/j.resuscitation.2015.04.028
21.
Perman SM . Overcoming Fears to Save Lives: COVID-19 and the Threat to Bystander CPR in Out-Of-Hospital Cardiac Arrest. Circulation (2020) 142(13):1233–5. 10.1161/CIRCULATIONAHA.120.048909
22.
Vaillancourt C Kasaboski A Charette M Islam R Osmond M Wells GA et al Barriers and Facilitators to CPR Training and Performing CPR in an Older Population Most Likely to Witness Cardiac Arrest: A National Survey. Resuscitation (2013) 84(12):1747–52. 10.1016/j.resuscitation.2013.08.001
23.
Hunziker S Laschinger L Portmann-Schwarz S Semmer NK Tschan F Marsch S . Perceived Stress and Team Performance During a Simulated Resuscitation. Intensive Care Med (2011) 37(9):1473–9. 10.1007/s00134-011-2277-2
24.
Chang YT Wu KC Yang HW Lin CY Huang TF Yu YC et al Effects of Different Cardiopulmonary Resuscitation Education Interventions Among University Students: A Randomized Controlled Trial. PLoS One (2023) 18(3):e0283099. 10.1371/journal.pone.0283099
25.
Lu C Jin YH Shi XT Ma WJ Wang YY Wang W et al Factors Influencing Chinese University Students' Willingness to Performing Bystander Cardiopulmonary Resuscitation. Int Emerg Nurs (2017) 32:3–8. 10.1016/j.ienj.2016.04.001
26.
Axelsson A Herlitz J Fridlund B . How Bystanders Perceive Their Cardiopulmonary Resuscitation Intervention; a Qualitative Study. Resuscitation (2000) 47(1):71–81. 10.1016/s0300-9572(00)00209-4
27.
Mausz J Snobelen P Tavares W . Please. Don't. Die.": A Grounded Theory Study of Bystander Cardiopulmonary Resuscitation. Circ Cardiovasc Qual Outcomes (2018) 11(2):e004035. 10.1161/CIRCOUTCOMES.117.004035
28.
Skora J Riegel B . Thoughts, Feelings, and Motivations of Bystanders Who Attempt to Resuscitate a Stranger: A Pilot Study. Am J Crit Care (2001) 10(6):408–16. 10.4037/ajcc2001.10.6.408
29.
Tong A Flemming K McInnes E Oliver S Craig J . Enhancing Transparency in Reporting the Synthesis of Qualitative Research: ENTREQ. BMC Med Res Methodol (2012) 12:181. 10.1186/1471-2288-12-181
30.
Methley AM Campbell S Chew-Graham C McNally R Cheraghi-Sohi S . PICO, PICOS and SPIDER: A Comparison Study of Specificity and Sensitivity in Three Search Tools for Qualitative Systematic Reviews. BMC Health Serv Res (2014) 14:579. 10.1186/s12913-014-0579-0
31.
Critical Appraisal Skills Programme. CASP Qualitative Checklist (2018). Available from: https://casp-uknet/wp-content/uploads/2018/01/CASP-Qualitative-Checklist-2018pdf (Accessed January 10, 2022).
32.
Chen HH Chiang WC Hsieh MJ Lee CH Yuan ZF Lin HY et al Experiences and Psychological Influences in Lay Rescuers Performing Bystander Cardiopulmonary Resuscitation: A Qualitative Study. J Acute Med (2020) 10(4):138–48. 10.6705/j.jacme.202012_10(4).0002
33.
Hasselqvist-Ax I Nordberg P Svensson L Hollenberg J Joelsson-Alm E . Experiences Among Firefighters and Police Officers of Responding to Out-Of-Hospital Cardiac Arrest in a Dual Dispatch Programme in Sweden: An Interview Study. BMJ Open (2019) 9(11):e030895. 10.1136/bmjopen-2019-030895
34.
Mathiesen WT Bjørshol CA Braut GS Søreide E . Reactions and Coping Strategies in Lay Rescuers Who Have Provided CPR to Out-Of-Hospital Cardiac Arrest Victims: A Qualitative Study. BMJ Open (2016) 6(5):e010671. 10.1136/bmjopen-2015-010671
35.
Mathiesen WT Bjørshol CA Høyland S Braut GS Søreide E . Exploring How Lay Rescuers Overcome Barriers to Provide Cardiopulmonary Resuscitation: A Qualitative Study. Prehosp Disaster Med (2017) 32(1):27–32. 10.1017/S1049023X16001278
36.
Lu Y Bin L Yan Z Shaoqing C Ming Z Hua Z . Qualitative Study on the rescue Experience of the First Responder of Cardiopulmonary Resuscitation. Chin J Emerg Resusc Disaster Med (2022) 17(04):430–4. 10.3969/j.issn.1673-6966.2022.04.003
37.
Thomas J Harden A . Methods for the Thematic Synthesis of Qualitative Research in Systematic Reviews. BMC Med Res Methodol (2008) 8:45. 10.1186/1471-2288-8-45
38.
Lewin S Glenton C Munthe-Kaas H Carlsen B Colvin CJ Gülmezoglu M et al Using Qualitative Evidence in Decision Making for Health and Social Interventions: An Approach to Assess Confidence in Findings from Qualitative Evidence Syntheses (GRADE-CERQual). Plos Med (2015) 12(10):e1001895. 10.1371/journal.pmed.1001895
39.
Munthe-Kaas H Bohren MA Glenton C Lewin S Noyes J Tunçalp Ö et al Applying GRADE-CERQual to Qualitative Evidence Synthesis Findings-Paper 3: How to Assess Methodological Limitations. Implement Sci (2018) 13(Suppl. 1):9. 10.1186/s13012-017-0690-9
40.
Glenton C Carlsen B Lewin S Munthe-Kaas H Colvin CJ Tunçalp Ö et al Applying GRADE-CERQual to Qualitative Evidence Synthesis Findings-Paper 5: How to Assess Adequacy of Data. Implement Sci (2018) 13(Suppl. 1):14. 10.1186/s13012-017-0692-7
41.
Colvin CJ Garside R Wainwright M Munthe-Kaas H Glenton C Bohren MA et al Applying GRADE-CERQual to Qualitative Evidence Synthesis Findings-Paper 4: How to Assess Coherence. Implement Sci (2018) 13(Suppl. 1):13. 10.1186/s13012-017-0691-8
42.
Noyes J Booth A Lewin S Carlsen B Glenton C Colvin CJ et al Applying GRADE-CERQual to Qualitative Evidence Synthesis Findings-Paper 6: How to Assess Relevance of the Data. Implement Sci (2018) 13(Suppl. 1):4. 10.1186/s13012-017-0693-6
43.
Lewin S Bohren M Rashidian A Munthe-Kaas H Glenton C Colvin CJ et al Applying GRADE-CERQual to Qualitative Evidence Synthesis Findings-Paper 2: How to Make an Overall CERQual Assessment of Confidence and Create a Summary of Qualitative Findings Table. Implement Sci (2018) 13(Suppl. 1):10. 10.1186/s13012-017-0689-2
44.
Barry T Guerin S Bury G . Motivation, Challenges and Realities of Volunteer Community Cardiac Arrest Response: A Qualitative Study of 'lay' Community First Responders. BMJ Open (2019) 9(8):e029015. 10.1136/bmjopen-2019-029015
45.
Case R Cartledge S Siedenburg J Smith K Straney L Barger B et al Identifying Barriers to the Provision of Bystander Cardiopulmonary Resuscitation (CPR) in High-Risk Regions: A Qualitative Review of Emergency Calls. Resuscitation (2018) 129:43–7. 10.1016/j.resuscitation.2018.06.001
46.
Berger W Coutinho ES Figueira I Marques-Portella C Luz MP Neylan TC et al Rescuers at Risk: A Systematic Review and Meta-Regression Analysis of the Worldwide Current Prevalence and Correlates of PTSD in Rescue Workers. Soc Psychiatry Psychiatr Epidemiol (2012) 47(6):1001–11. 10.1007/s00127-011-0408-2
47.
Davies E Maybury B Colquhoun M Whitfield R Rossetti T Vetter N . Public Access Defibrillation: Psychological Consequences in Responders. Resuscitation (2008) 77(2):201–6. 10.1016/j.resuscitation.2007.11.012
48.
Fischer P Krueger JI Greitemeyer T Vogrincic C Kastenmüller A Frey D et al The Bystander-Effect: A Meta-Analytic Review on Bystander Intervention in Dangerous and Non-Dangerous Emergencies. Psychol Bull (2011) 137(4):517–37. 10.1037/a0023304
49.
Lo CYZ Fook-Chong S Shahidah N White AE Tan CK Ng YY et al Does Witness Type Affect the Chance of Receiving Bystander CPR in Out-Of-Hospital Cardiac Arrest? Resuscitation (2023) 189:109873. 10.1016/j.resuscitation.2023.109873
50.
Stieglis R Zijlstra JA Riedijk F Smeekes M van der Worp WE Tijssen JGP et al Alert System-Supported Lay Defibrillation and Basic Life-Support for Cardiac Arrest at Home. Eur Heart J (2022) 43(15):1465–74. 10.1093/eurheartj/ehab802
51.
Stieglis R Zijlstra JA Riedijk F Smeekes M van der Worp WE Koster RW . AED and Text Message Responders Density in Residential Areas for Rapid Response in Out-Of-Hospital Cardiac Arrest. Resuscitation (2020) 150:170–7. 10.1016/j.resuscitation.2020.01.031
52.
Babaie J Barati M Azizi M Ephtekhari A Sadat SJ . A Systematic Evidence Review of the Effect of Climate Change on Malaria in Iran. J Parasit Dis (2018) 42(3):331–40. 10.1007/s12639-018-1017-8
53.
Swor R Khan I Domeier R Honeycutt L Chu K Compton S . CPR Training and CPR Performance: Do CPR-Trained Bystanders Perform CPR?Acad Emerg Med (2006) 13(6):596–601. 10.1197/j.aem.2005.12.021
54.
Birch SAJ Brosseau-Liard PE Haddock T Ghrear SE . A 'curse of Knowledge' in the Absence of Knowledge? People Misattribute Fluency when Judging How Common Knowledge Is Among Their Peers. Cognition (2017) 166:447–58. 10.1016/j.cognition.2017.04.015
55.
Breckwoldt J Schloesser S Arntz HR . Perceptions of Collapse and Assessment of Cardiac Arrest by Bystanders of Out-Of-Hospital Cardiac Arrest (OOHCA). Resuscitation (2009) 80(10):1108–13. 10.1016/j.resuscitation.2009.06.028
56.
Goodwin AP . Cardiopulmonary Resuscitation Training Revisited. J R Soc Med (1992) 85(8):452–3. 10.1177/014107689208500809
57.
McGraw AP Larsen JT Kahneman D Schkade D . Comparing Gains and Losses. Psychol Sci (2010) 21(10):1438–45. 10.1177/0956797610381504
58.
Chittenden EH Clark ST Pantilat SZ . Discussing Resuscitation Preferences With Patients: Challenges and Rewards. J Hosp Med (2006) 1(4):231–40. 10.1002/jhm.110
59.
Zhang L Li B Zhao X Zhang Y Deng Y Zhao A et al Public Access of Automated External Defibrillators in a Metropolitan City of China. Resuscitation (2019) 140:120–6. 10.1016/j.resuscitation.2019.05.015
60.
Travers AH Perkins GD Berg RA Castren M Considine J Escalante R et al Part 3: Adult Basic Life Support and Automated External Defibrillation: 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation (2015) 132(16 Suppl. 1):S51–83. 10.1161/CIR.0000000000000272
61.
Fordyce CB Hansen CM Kragholm K Dupre ME Jollis JG Roettig ML et al Association of Public Health Initiatives With Outcomes for Out-Of-Hospital Cardiac Arrest at Home and in Public Locations. JAMA Cardiol (2017) 2(11):1226–35. 10.1001/jamacardio.2017.3471
62.
Malta Hansen C Rosenkranz SM Folke F Zinckernagel L Tjørnhøj-Thomsen T Torp-Pedersen C et al Lay Bystanders' Perspectives on What Facilitates Cardiopulmonary Resuscitation and Use of Automated External Defibrillators in Real Cardiac Arrests. J Am Heart Assoc (2017) 6(3):e004572. 10.1161/JAHA.116.004572
63.
Yeung J Okamoto D Soar J Perkins GD . AED Training and its Impact on Skill Acquisition, Retention and Performance--a Systematic Review of Alternative Training Methods. Resuscitation (2011) 82(6):657–64. 10.1016/j.resuscitation.2011.02.035
64.
Perkins GD Graesner JT Semeraro F Olasveengen T Soar J Lott C et al European Resuscitation Council Guidelines 2021: Executive Summary. Resuscitation (2021) 161:1–60. 10.1016/j.resuscitation.2021.02.003
65.
Dukes K Girotra S . Are Lay Rescuers Adequately Prepared for Cardiopulmonary Resuscitation and its Aftermath?Circ Cardiovasc Qual Outcomes (2018) 11(2):e004465. 10.1161/CIRCOUTCOMES.118.004465
66.
Afzali Rubin M Svensson TL Herling SF Jabre P Møller AM . Family Presence During Resuscitation. Cochrane Database Syst Rev (2023) 5(5):Cd013619. 10.1002/14651858.CD013619.pub2
67.
Orlas CP Herrera-Escobar JP Hau KM Velmahos A Patel N Sanchez S et al Perceived Social Support Is Strongly Associated With Recovery after Injury. J Trauma Acute Care Surg (2021) 91(3):552–8. 10.1097/TA.0000000000003230
68.
Thompson DR Pedersen SS . Psychosocial Assessment and Psychological Interventions Following a Cardiac Event. Heart (2023) 109(5):405–10. 10.1136/heartjnl-2022-321607
69.
Braun-Lewensohn O Mayer CH . Salutogenesis and Coping: Ways to Overcome Stress and Conflict. Int J Environ Res Public Health (2020) 17(18):6667. 10.3390/ijerph17186667
Summary
Keywords
cardiopulmonary resuscitation, lay responder, real experience, qualitative synthesis, psychological intervention
Citation
Li N, Shen C, Yang X, Wang R, Gu LQ, Zhao W and Chu ZP (2024) The Real Experience of Lay Responders Performing Cardiopulmonary Resuscitation: A Synthesis of Qualitative Evidence. Public Health Rev 45:1606650. doi: 10.3389/phrs.2024.1606650
Received
20 September 2023
Accepted
24 May 2024
Published
05 June 2024
Volume
45 - 2024
Edited by
Raquel Lucas, University Porto, Portugal
Reviewed by
Justin Sempsrott, Independent Researcher, Kuna, Idaho, United States
Xuejie Dong, Peking University, China
Stefanie Beck, University Medical Center Hamburg-Eppendorf, Germany
Updates
Copyright
© 2024 Li, Shen, Yang, Wang, Gu, Zhao and Chu.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms. PHR is edited by the Swiss School of Public Health (SSPH+) in a partnership with the Association of Schools of Public Health of the European Region (ASPHER)+
*Correspondence: Wei Zhao, 450502687@qq.com; Zhi Ping Chu, 2289598516@qq.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.