- 1School of Health and Biomedical Sciences, STEM College, RMIT University, Bundoora, VIC, Australia
- 2Department of Health and Biostatistics, Swinburne University of Technology, Hawthorn, VIC, Australia
- 3School of Economics, Finance and Marketing, College of Business, RMIT University, Melbourne, VIC, Australia
- 4Northern Health Australia, Epping, VIC, Australia
- 5School of Media and Communication, College of Design and Social Context, RMIT University, Melbourne, VIC, Australia
- 6Institute of Health and Wellbeing, Federation University Australia, Ballarat, VIC, Australia
- 7Institute for Design Informatics, University of Edinburgh, Edinburgh, United Kingdom
Objective: To identify gaps among Australian Long COVID support services and guidelines alongside recommendations for future health programs.
Methods: Electronic databases and seven government health websites were searched for Long COVID-specific programs or clinics available in Australia as well as international and Australian management guidelines.
Results: Five Long COVID specific guidelines and sixteen Australian services were reviewed. The majority of Australian services provided multidisciplinary rehabilitation programs with service models generally consistent with international and national guidelines. Most services included physiotherapists and psychologists. While early investigation at week 4 after contraction of COVID-19 is recommended by the Australian, UK and US guidelines, this was not consistently implemented.
Conclusion: Besides Long COVID clinics, future solutions should focus on early identification that can be delivered by General Practitioners and all credentialed allied health professions. Study findings highlight an urgent need for innovative care models that address individual patient needs at an affordable cost. We propose a model that focuses on patient-led self-care with further enhancement via multi-disciplinary care tools.
Introduction
Since its outbreak in January 2020, the COVID-19 pandemic has resulted in an estimated 642 million cases and over 6.6 million deaths globally [1, 2]. In Australia, more than 11 million cases have been confirmed and over 19,000 deaths recorded [3].
While the majority of those infected recover fully, up to 40% of individuals may experience lingering symptoms including fatigue, shortness of breath, persistent cough, joint pain, brain fog, cognitive dysfunction, anxiety, depression, loss of smell or taste, and insomnia [4]. These symptoms may fluctuate, relapse over time and persist for several months. When symptoms persist beyond 12 weeks [4] the condition is deemed chronic and termed Long COVID or Post COVID-19 condition by the World Health Organization (WHO) [5]. In addition to these terms, several terms have been referenced including “long haulers,” “post-acute COVID-19,” “post COVID-19 syndrome” and “post-acute sequelae of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection” [6, 7]. For the purposes of this review, we have adopted the term “Long COVID” to describe this condition.
Long COVID poses a significant challenge as an emerging health condition for several reasons. Firstly, the underlying pathology of this condition is still being examined and effective treatments are not yet available [8]. Secondly, the emergence of Long COVID is occurring amidst an ongoing struggle of healthcare systems worldwide to manage the demands associated with the continued presence of COVID-19 [8]. Thirdly, Long COVID is a complex and heterogeneous health condition, with more than 50 different clinical symptoms affecting 10 different body systems [9]. [10], and its duration is still uncertain. Long COVID is a “major health challenge for the coming couple of years at least” [10].
Health authorities and services have responded to the needs of those affected by Long COVID by developing guidelines and providing services to assist recovery. To evaluate if the current status of services offered meets the needs of people affected by Long COVID, this review aims to present:
(i) A critical summary of national and international Long COVID guidelines;
(ii) A summary of the Long COVID support services currently being delivered in Australia;
(iii) An evaluation on whether the characteristics of these services are in accordance with national/international guides and identification of gaps; and
(iv) Recommend a care model for future services.
Methods
Search Strategy
To identify Long COVID guidelines, the following databases and websites were searched; Google Scholar, PDQ-Evidence, WHO, Centers for Disease Control and Prevention (CDC), National Institutes of Health (NIH), The Australian Royal Australian College of General Practitioners (RACGP), The National Institute for Health and Care Excellence (NICE), Public Health Agency of Canada and Ministry of Health NZ. Search terms included “Long COVID guidelines,” “Post COVID conditions guidelines” AND “Post COVID-19 condition” between 10 August to 23 September 2022 to obtain articles from 2020 onwards. Follow up searches were conducted on 26 January 2023 and 22 March 2023, respectively. The Guidelines International Network (GIN) repository was searched using the same search terms on 12 July 2023.
To identify Long COVID services in Australia, Google searches were undertaken using the terms “Long COVID service OR clinic Australia,” “Long COVID service OR clinic Victoria,” “Long COVID service OR clinic New South Wales,” “Long COVID service OR clinic Australian Capital Territory,” “Long COVID service OR clinic Queensland,” “Long COVID service OR clinic South Australia,” “Long COVID service OR clinic Western Australia,” “Long COVID service OR clinic Tasmania.” “Long COVID service OR clinic Northern Territory,” “Post covid service OR clinic Australia” between 10 August and 23 September 2022. Follow up searches were conducted on 26 January 2023 and 22 March 2023, respectively.
Selection Criteria
The following inclusion criteria to guidelines for Long COVID were utilized: 1) provide comprehensive information such as care principles, care models, and patient education on Long COVID and 2) developed in English-speaking countries. Clinical guidelines were excluded if they did not state the process of the guideline development as indicated in AGREE II assessment tool [11].
In regard to Long COVID services, only those: 1) Were located in Australia; 2) Offered Long COVID-specific services; 3) Provided information on the services offered.; 4) The information was available to the public were included.
Data Extraction and Synthesis
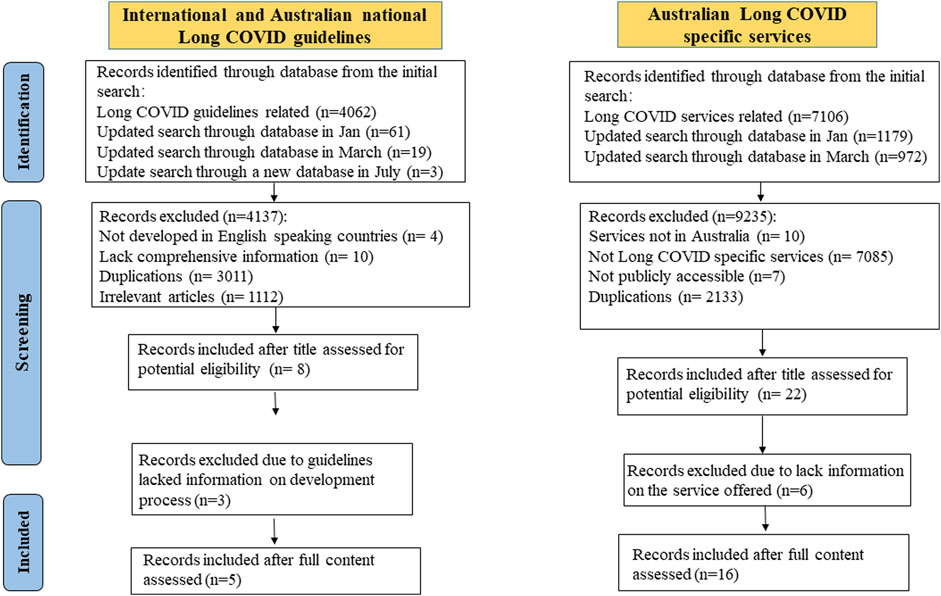
Data selection was conducted by one author (SL) and extracted and verified by two authors (SL and ZZ). The key data extraction items were developed from our aims and previewing of the content, then presented in tables or figures in a narrative format (Supplementary Appendix S1 and Figure 1).
Quality Assessment
Guidelines were evaluated by two independent appraisers (SL and ZZ) using the AGREE II assessment tool [11], covering six domains (scope and purpose, stakeholder involvement, rigor of development, clarity of presentation, applicability, and editorial independence) with 23 items rated on a 7-point scale (1 = strongly disagree; 7 = strongly agree). Domain scores were calculated following the recommended formula [11]. Guidelines scored below 50% were rated low-quality, 50%–70% moderate, and >70% high-quality [11].
Consumer Engagement
Three individuals with lived experience of COVID-19 or Long COVID and who had sought medical advice for management reviewed the manuscript and provided feedback.
Results
The search identified 8 Long COVID specific guidelines and 16 Long COVID specific services in Australia. Three out of eight guidelines were excluded (two from Canada and one from Australia) as they summarised existing guidelines without providing information about their development process. Five guidelines and 16 associated services were included in this review. Figure 1 illustrates the study selection process.
A Critical Summary of National and International Guidelines
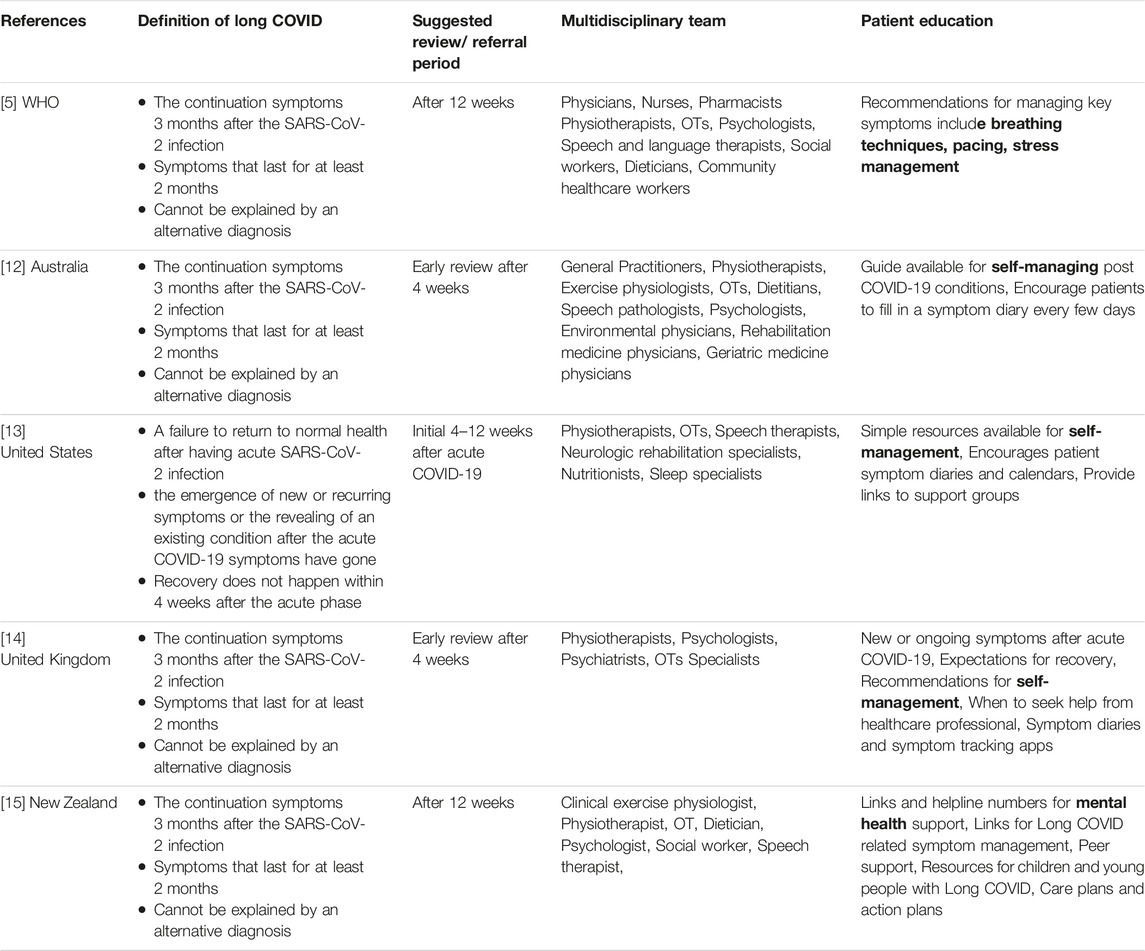
Table 1 is a summary of the guideline characteristics, including the definition of Long COVID, suggested review period, multidisciplinary team and patient education.
Five international guidelines were developed by the WHO [5], the United States (US) Centres for disease control and prevention (CDC) [13], a collation of the United Kingdom (UK) guidelines [The National Institute for Health and Care Excellence (NICE); the Scottish Intercollegiate Guidelines Network (SIGN), and the Royal College of General Practitioners (RCGP)] [14, 16], the Australian Royal Australian College of General Practitioners (RACGP) [12] and New Zealand Ministry of Health [15]. The WHO guidelines serve as the cornerstone for post-COVID care, while the Australian, United Kingdom, United States, and New Zealand guidelines complement and provide detailed information on patient care. While no guidelines met our selection criteria from the Public Health Agency of Canada, two excellent patient resources on Long COVID recovery care were provided [17–19].
The definition of Long COVID used in the guidelines have similarities and differences. Four guidelines, including WHO, Australian, New Zealand and UK guidelines define Long COVID as post COVID-19 condition that occurs in individuals with a history of probable or confirmed SARS-CoV-2 infection 3 months from the onset of COVID-19 with symptoms that last for at least 2 months and cannot be explained by an alternative diagnosis [5, 12, 14, 16]. Common symptoms include fatigue, persistent cough, shortness of breath, cognitive dysfunction which generally have an impact on everyday functioning. Symptoms may be new onset, following initial recovery from an acute COVID-19 episode, or persist from the initial illness. Symptoms may also fluctuate or relapse over time [5, 12, 14, 16] A separate definition is given for children, which is not included here as it is beyond the scope of this review [5].
In contrast, the US guidelines use both the term “Post-COVID Conditions” and “Long COVID.” They define Long COVID as signs, symptoms, and conditions that continue or develop 4 weeks or more after the acute phase of COVID-19 infection [13]. Moreover, the US guidelines are the sole source that consider exacerbation of the pre-existing symptoms as part of Long COVID presentation [13].
The US guidelines have assigned the code “U09.9 Post COVID-19 condition, unspecified” in the International Classification of Disease, 10th Revision (ICD-10) activated by WHO to allow the establishment of a link with COVID-19. The code is separate from cases with acute COVID-19 [13]. Similarly, the New Zealand guidelines also applied an ICD code for Long COVID [15].
All guidelines stress the importance of a person-centered approach and multidisciplinary interventions that address various physical, cognitive, psychological, and psychiatric symptoms, as well as functional disabilities, alongside screening for red flags [5, 13, 14, 16]. Patient education is emphasized across all guidelines, with a focus on mental health, symptom management, and keeping a symptom diary. Importantly, all guidelines lack step-by-step approaches to skills training and interactive or visual patient education materials [5, 12–14, 16].
The UK and US guidelines recommend early investigation within 4 weeks or between 4 and 12 weeks of contracting COVID, rather than waiting for 12 weeks as implied in the WHO guidelines [5, 13, 14, 16] The Australian and UK guidelines also suggest early review after the acute phase of COVID-19 and recommend patient assessment based on various factors such as the severity and duration of symptoms, mental health and worsening of pre-existing conditions [12, 14, 16].
In addition, what sets the US guidelines apart from other guidelines is their incorporation of trauma-informed approaches, which are based on six key principles (Supplementary Appendix S2). These principles include creating a safe environment, training staff to be trauma-informed, providing peer support, involving patients in organizational planning, empowering patients to make choices, and addressing cultural, historical, and gender-related issues [13].
Furthermore, although the New Zealand guidelines may not include specific details regarding interventions and referral timelines, they do provide recommendations for a variety of population groups, including children, the elderly, indigenous peoples, and individuals with disabilities. In addition, they address vocational rehabilitation for working individuals, particularly women. This work-related specific rehabilitation has not been mentioned in other guidelines (Supplementary Appendix S2) [15].
Quality Appraisal of the Guidelines
Table 2 presents the AGREE II scores of included guidelines. One of five (25%) guidelines (UK) was high-quality, three (75%) (US, WHO, New Zealand) were moderate-quality, and the remaining one (Australia) was low-quality.
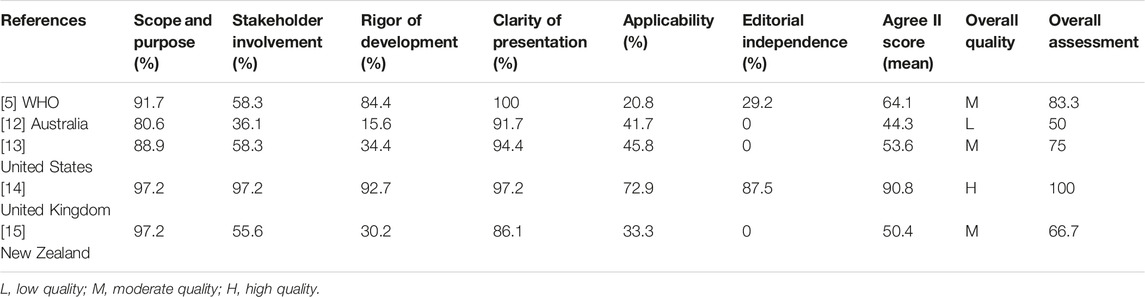
TABLE 2. Methodological quality of each guideline appraised by the AGREE II instrument (Australia, 2023).
All guidelines scored high in the domains of Scope and Purposes, and Clarity of Presentation, but poorly in Applicability, particularly lacking information on auditing criteria and facilitators/barriers to recommendation implementation, except for the UK guidelines. Editorial Independence was also a weak area, with four guidelines (Australia, WHO, US, New Zealand) failing to declare the funding body, or disclose panel members’ conflict interests. The quality of Stakeholder Involvement varied. Only two (WHO and United Kingdom) clearly stated they included Long COVID/COVID-19 survivors in the advisory committee, and one (United Kingdom) outlined the composition of the development panel. As for the Rigor of Development, three guidelines (Australia, New Zealand, United States) did not explain clearly the systematic search, evidence selection, external review, and update plans. Overall, the guidelines’ quality ranged from moderate to high.
Long COVID Services in Australia
Among the identified services, nine are located in Victoria (VIC), two in Queensland (QLD), and one each in New South Wales (NSW), Australian Capital Territory (ACT), South Australia (SA), Western Australia (WA), and Tasmania (TAS), respectively. Unfortunately, no Long COVID service could be identified in the Northern Territory. In our 2nd updated search conducted in March 2023, a few new GP-led or allied health-led clinics designed for Long COVID management were identified in NSW [20–22] and QLD [23, 24]. However, we did not incorporate them into this review because they did not provide detailed information on the services they offer, and the health professionals involved. Table 3 provides a summary of all 16 services, including three Victorian services that have been terminated due to a lack of funding.
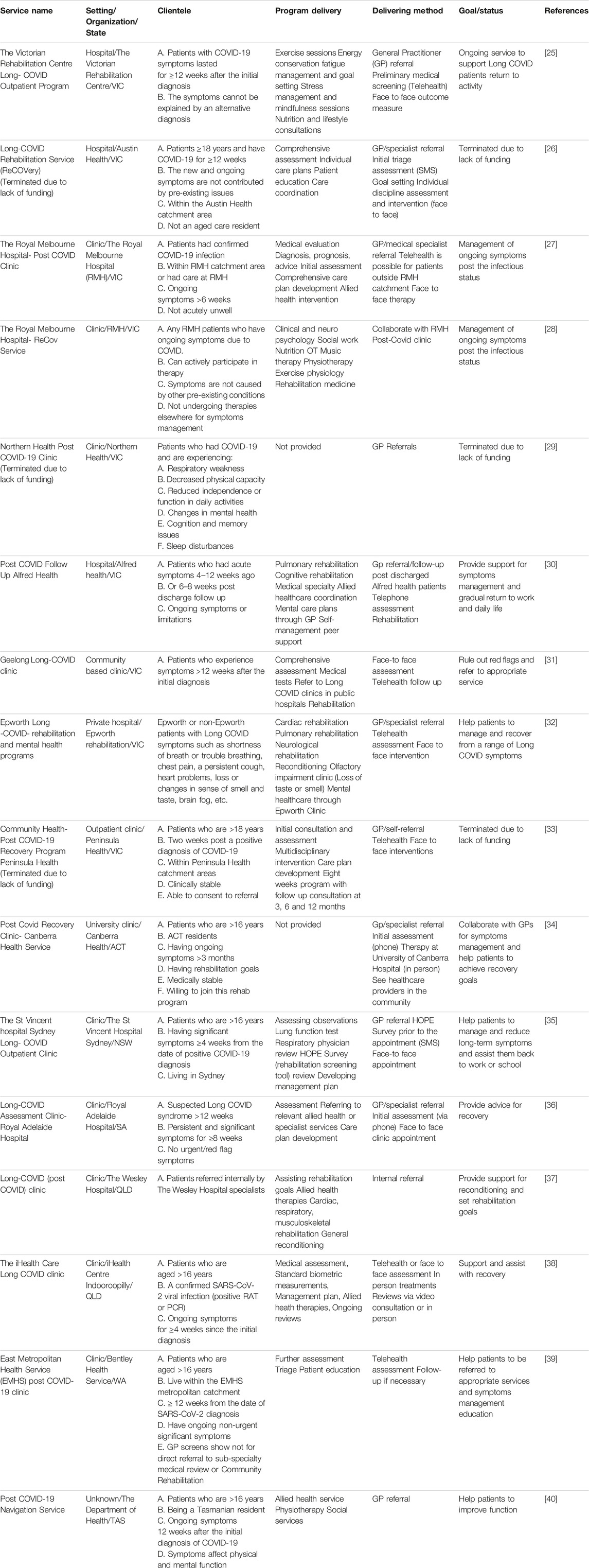
TABLE 3. Content, delivery and targeted population of long COVID service in Australia (n = 16) (Australia, 2023).
Most of the active services are publicly funded, with no extra charges to patients, while three are privately funded using a mixed funding with Medicare payment and gap payments by patients either personally or through private insurance. Fourteen services require a referral from general practitioners (GP) or other medical specialties and adopt a hybrid approach of in-person and remote models. Four services include follow-up for hospital admitted patients, while one service accepts inpatient referral only, and the remaining nine services are designed for patients living with the condition in the community.
The majority of services did not specify the age of the target population, so we assumed they accept people of all ages. Several services (in WA, ACT, NSW, QLD and TAS) provide support to patients as young as 17 years old. While older people can access these services, there are no specific services for either people over 65 or children as these populations may require different support [8, 41]. Two Victorian services specifically exclude aged care residents. Furthermore, no service is available specifically for people with mental or physical disabilities, who are already disadvantaged due to their increased vulnerability to Long COVID [8].
In addition, the majority of the Long COVID services focus on providing rehabilitation programs to address specific signs and symptoms of Long COVID, such as fatigue and shortness of breath. The common features of these services include: 1) support for the delivery of rehabilitation services; 2) multidisciplinary rehabilitation; 3) continuity and coordination of care teams; 4) hybrid care delivery methods.
Based on the service information provided by the Long COVID clinics, we calculated the percentage distribution of multidisciplinary management team members across the identified services (Supplementary Appendix S3). Physiotherapists and Psychologists are the most commonly included professionals (63% each), whereas Neurologists, Liaison Psychiatrists, and Pain Specialists are less common. Surprisingly, only 19% of multidisciplinary care teams included GPs (if we exclude referral from GP).
Moreover, out of all 16 services, the Post-COVID Follow Up Service provided by Alfred Health is the only one that has explicitly described the rationale for their service design. Their approach is based on a systematic review of care models for Long COVID conducted by a group of Canadian researchers [9]. Figure 2 illustrates the four key elements of their approach, with each element working as a network to prioritize the needs of each individual living with Long COVID. The coordination unit receives referrals from both hospitalized and community-based patients and assesses and triages cases according to individual needs. Some cases are referred to multidisciplinary rehabilitation teams, medical specialty clinics (such as pulmonary, cardiovascular, psychology/psychiatry, neurology, etc.) for advanced testing and diagnoses, and others to primary care teams for screening and support. The goal is to achieve positive outcomes for patients and assisting them back to work and daily life [9].
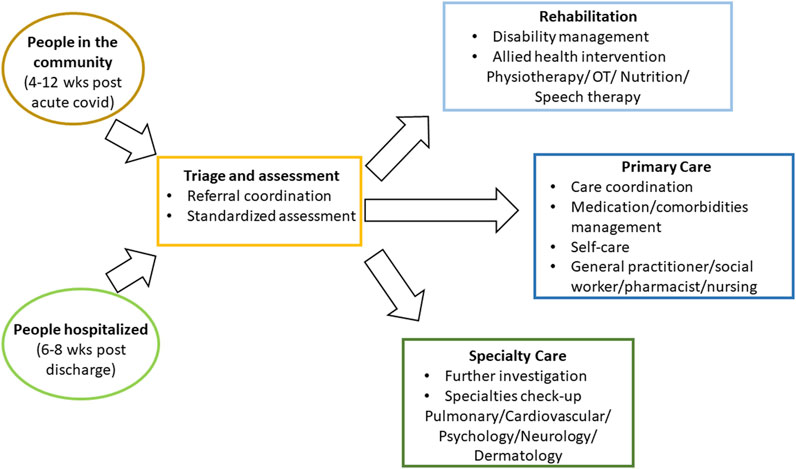
FIGURE 2. A proposed care pathway for Long COVID by a Canadian study (modified with permission [9]) (Canada, 2021).
Gaps Between Service and Guidelines
Service models in Australia are generally align with the international and national guidelines, consisting of 1) assessment of red flags, 2) support for the delivery of rehabilitation services; 3) multidisciplinary rehabilitation; 4) coordinated care and 5) a hybrid care delivery method. It is not clear how recommendations in the guidelines are carried out in clinical practice, including assessment, patient-centred care, shared-decision making and patient education. Even though the Australian, UK and US guidelines have developed patient resources for education and self-care strategies [12–14, 16], patient education and empowerment are not clearly described in any of the identified Long COVID services.
In addition, early investigation and review of individuals who have Long COVID or who could potentially develop it are recommended by the United States, Australia and United Kingdom. However, it is unclear how this recommendation could be implemented in clinical practice.
Considerations for Future Care Models
Based on the gaps between guidelines and current service models, future care models must consider the following aspects:
1) Early Investigation: When symptoms are persistent more than 4 weeks from the time of contracting virus, it is crucial to initiate investigations as this reduces the risk of developing persistent illness [13].
2) Self-Care Engagement: Self-care is a crucial aspect of the recovery process [12, 42]. Emphasising the importance of self-care practices empowers patients to take charge of their wellbeing and supports the healing process.
3) Seek Professional Assistance: If symptoms persist beyond 8 weeks, it is essential for individuals with Long COVID to seek prompt assistance from their general practitioners and specialists. This step is vital as it allows for thorough evaluation and, if deemed appropriate, referral to specialised Long COVID clinics [12, 14].
Discussion
Our review identifies five international guidelines, with four rated as moderate to high quality and one as low quality. WHO guidelines are the cornerstone of the definition and care for Long COVID whereas the Australian, UK, US, and New Zealand guidelines complement it on patient care. Long COVID is defined as signs and symptoms persisting 4 week (United States) or 12 weeks (WHO, United Kingdom, Australian and New Zealand) after the initial confirmed or probable infection of SARS-CoV-2. All guidelines promote the importance of screening for red flags, a person-centered approach, self-care and multidisciplinary interventions. Both US and New Zealand guidelines formally recognized Long COVID through using an ICD code. The latter also acknowledges the impact of Long COVID on work capacity and recommends vocational rehabilitation.
We have identified limited Long COVID services available in Australia, with 9 out of 16 clinics in Victoria, the state that had the earliest outbreaks of COVID-19 in Australia. Among the 16 services, three have since been terminated due to lack of funding. Most services promote multidisciplinary rehabilitation programs, which are often costly to operate and can only accommodate a small number of patients. This may explain why it has not been possible to sustain some service provision. However, considering the intermittent trend of worldwide COVID-19 cases [43], introducing more or reactivating of the long covid services will be necessary.
The significant gaps identified are the early identification and referral of individuals with Long COVID at 4 weeks after initial contraction of SARS-CoV-2 and patient education and engagement in self-care for managing the symptoms. With the discrepancy in the definition of Long COVID and limited educational information in the credible public domain, neither the public nor healthcare practitioners know how best to help individuals who are infected with SARS-CoV-2 to prevent the development of Long COVID.
Currently information of patient education and self-care strategies are placed on government or relevant health organizations’ website in written form and mainly in English. There are multiple disadvantages to this practice. Firstly, access to trustworthy internet sites is not readily available or widely publicized. Secondly, the information is all in English makes it non-accessible to people who have low health literacy skills or those from non-English speaking backgrounds. Finally, and most importantly, information provision alone does not activate people to do something for their own health [44, 45]. We propose a sustainable care model that could effectively address those gaps.
Proposed Sustainable Care Model
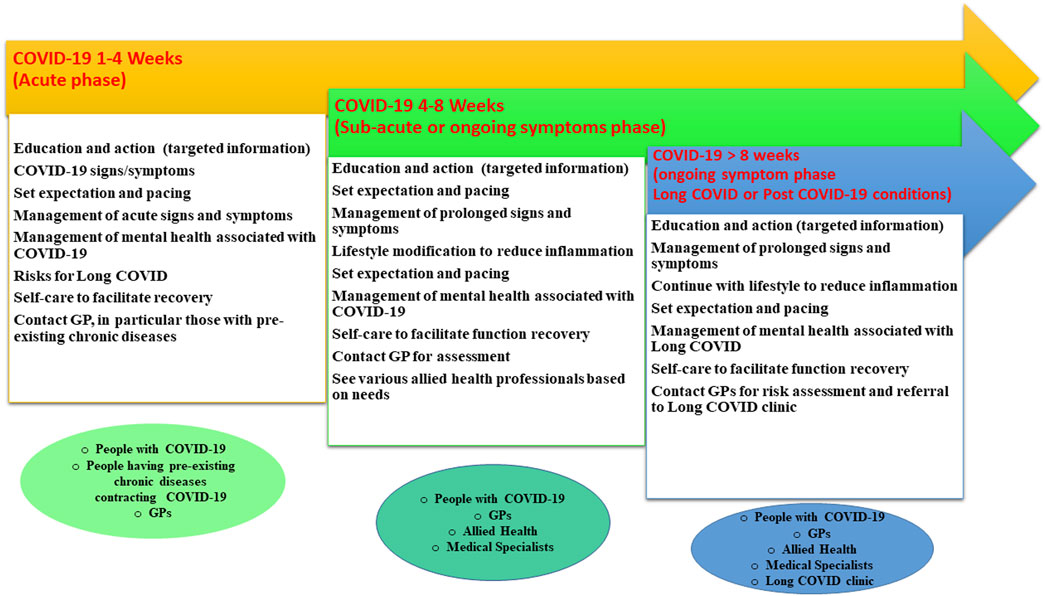
This proposed model is built on US, UK and Australian guidelines [12–14] that recommend early investigation, and coupled with insights from the Australian National Strategic Framework for Chronic Conditions [46] to bridge the gaps in Long COVID services through patient self-care, coordinated care and multidisciplinary collaboration with a strong focus on prevention, and patient engagement and empowerment.
Our proposed Long COVID care model/pathway is outlined in Figure 3. After contracting the SARS-CoV-2 virus, individuals should be informed that the recovery period typically ranges from 10 to 120 days [47], allowing them to pace their activities accordingly. Australian data show that 90% of COVID-19 cases recovered within 8 weeks with some continuing to recover between 8 and 12 weeks [48]. In addition, people with pre-existing conditions, such as chronic fatigue, mental illness, arthritis and/or diabetes, may experience exacerbations due to COVID-19 [48, 49]. Those conditions are potential risk factors for the presentations of Long COVID [13]. This cohort is vulnerable and should be better informed and prepared. Early monitoring, intervention and prevention are essential.
Furthermore, mental health is a significant concern during the acute phase of COVID-19 and up to 3 months after infection with reports indicating up to one in three people experiencing depression or sleep problems and up to one in two facing anxiety [50]. A multicounty study demonstrates the presence of depression can be exacerbated by physical symptoms resembling COVID-19 and health information [51]. Any care model needs to include strategies to minimize the impact on mental health from the acute stage.
From 4 to 8 weeks after initial SARS-CoV-2 contraction, the sub-acute phase, individuals should contact or continue to work closely with GPs or medical specialists to investigate any ongoing symptoms of the illness [12–14, 16]. Patients are encouraged to make lifestyle changes [52, 53] aimed at reducing persistent inflammation, which is linked to Long COVID symptoms [54], and decreasing risk of developing Long COVID [52]. Self-care practices should be encouraged to facilitate recovery [12–14, 16]. Additionally, at this stage, individuals may begin seeking treatments from allied health professionals [55, 56] to help address ongoing symptoms such as shortness of breath and fatigue as well as prevent long-term complications [57].
If symptoms persist for more than 8 weeks, it is important they continue with all the components mentioned above and request their GPs or medical specialists for a risk assessment and a possible referral to a Long COVID clinic, where they can receive multidisciplinary care [12–14, 16, 47].
To promote adoption of this care model, a few critical issues, including diagnosis, workforce training, and patient education and engagement barriers, will be discussed further in the following paragraphs.
How to Identify Long COVID and When to Treat
The diagnosis of Long COVID is based on a confirmed COVID-19 polymerase chain reaction (PCR) or rapid antigen test (RAT) positive test or suspected COVID-19 infection, and the persistence of various signs and symptoms that develop after COVID-19 where these symptoms cannot be explained by other causes or a pre-existing condition [5]. There is currently no confirmed laboratory or other forms of objective tests available globally for the diagnosis of Long COVID. So, relying on PCR or RAT and the persisting symptoms are the key strategies for the potential diagnosis of Long-COVID.
A number of guidelines advocate early review, starting within 4–12 weeks of contracting SARS-CoV-2, rather than delaying until 12 weeks as recommended by WHO. We adopt this recommendation in the proposed model. Early action and prevention of chronic conditions is prioritized in the Australian National Strategic Framework for Chronic Conditions [46] due to the substantial and growing cost of chronic diseases, both in direct medical expenses and indirect impacts. Limited data about Long COVID shows a twofold increase in direct medical costs within 12 months of contracting SARS-CoV-2 for those affected, while those without developing Long COVID experienced only a 7.5% cost increase during the same period [58]. Additionally, an analysis of New York State Workers’ Compensation Data over a 27 month period (2020–2022) during the pandemic revealed that one-third of workers’ compensation claims were attributed to Long COVID. Among claimants with Long COVID, 18% did not return to work after 12 months, and 40% of those who returned to work within 60 days continued to receive medical treatment [59].
The implementation of coordinated and multi-disciplinary programs poses however cost challenges [60], potentially burdening the healthcare system when advocating early review and intervention. So far, pulmonary rehabilitation delivered via telemedicine [61] and a tailored and multidisciplinary rehabilitation program [62] have been found to have long-term benefit for Long COVID.
We, however, could not identify any cost-effectiveness studies of treatments for Long COVID. To alleviate the potential financial burden, funding for medical investigations and Long COVID-specific programs could be sourced from various channels including a combination of resources from the government-funded programs for chronic diseases, aged care, and disability support, private health insurance, patient contributions, and philanthropic services [45]. According to Greco’s (2020) estimation, integrating enhanced self-care practices could foster sustainable healthcare outcomes [45].
The Workforce and Workforce Training
This review finds that nearly 1/2 to 2/3 of the Australian multi-disciplinary rehabilitation services have employed allied health practitioners including physiotherapists, psychologists, exercise physiologists, dietitians and occupational therapists. Only one in 16 services included medical specialists.
A few other credentialed health professions are not included in the current services, such as practitioners of Chinese medicine, chiropractic, osteopathy, pharmacists and community nursing. These practitioners operating at the primary care level are very likely to be approached for care by impacted individuals. Not including them in potential care models may be a missed opportunity for patient education and workforce training [63, 64].
Indeed, until today, many health professionals remain uninformed about Long COVID about its diagnosis, prevention and management, thus there is an urgent need for workforce training. In addition, there is room for a multi-skilled healthcare workforce. For example, healthcare workers could be trained to conduct quick screenings for mental health symptoms and undertake centralized process for referral as required [65, 66].
Patient Education and Engagement Barriers
Recent multi-country research showed that 90% of Long COVID cases developed from mild cases of COVID-19 [67] means that detecting the risks for Long COVID early becomes very difficult due to mild signs and symptoms. To prevent Long COVID, the most effective and immediate strategies are to educate people about the condition and provide evidence-based strategies for symptom management. This is perhaps why most guidelines encourage self-management and offer online supporting resources, which is mainly in text. This form of communication creates barriers as information does not translate into action readily.
The uptake and use of the existing Long COVID educational sites remain unclear. It will not be surprising if the resource is under-utilized. Previous research on patient activation show that given the same information, only a quarter of the population may act on the advice consistently, 40% may act on the advice initially but cannot sustain the practice, and the remaining 35% would not be able to either comprehend the information or not have the capacity to act on the advice [44, 45]. Research shows that 36% of health outcomes are due to individual behaviors, in comparison to 11% being determined by medical care [68]. It is paramount that future care models include a special section on measuring the level of patient engagement or activation so as to provide tailored information to individual needs.
Limitations
We reviewed Australian services only and the information might not be applicable to countries not having similar healthcare services. We only accessed information in the public domain and did not survey each service for their detailed operation. To compensate for this, we invited people who have attended some of the Long COVID services to provide their feedback. Furthermore, as most of the services and guidelines are for Long COVID patients at the primary care level, this review does not address the needs of patients who were hospitalized or had been in intensive care unit due to COVID-19. We also did not discuss the government, workplace and insurance companies’ recognition of the disability associated with Long COVID [69] or the funding model of our proposed service, which are beyond the scope of this review.
Conclusion
COVID-19 and Long COVID present a significant burden of disease and challenge to the healthcare system in Australia. In addition to Long COVID clinics, future solutions should focus on early identification and interventions that can be delivered at the primary care level by GPs and allied health practitioners. We propose a sustainable model that engages patients, with people-led self-care, further enhanced with multi-disciplinary care. COVID-19 and Long COVID present a one-in-a-century opportunity to enhance the public awareness of self-care through engaging individuals in managing the personal and societal consequence of the pandemic.
Author Contributions
ZZ, SB, BF, and JR developed the concept of this review. SL conduced the database search. SL and ZZ performed the data extraction, analysis and synthesis. SL, ZZ, and SB drafted the manuscript. ZZ, SB, MP, BF, RJ, WS, JR, SX, MO, DW, JS, and CI provided critical comments and revised the manuscript. All authors contributed to the article and approved the submitted version.
Funding
The project “EAT, MOVE, HEAL for Long-COVID” (Project ID: PRJ00000010) was funded by a 2022 Strategic Capability Deployment Fund, RMIT University, Victoria, Australia.
Conflict of Interest
The authors declare that they do not have any conflicts of interest.
Acknowledgments
We would like to thank Professors Sonja Cleary, Doa El-Ansary, Kerryn Butler-Henderson, and Donald Campbell and Ms. Mary Goodman for providing feedback to this review. This review is part of the project outcomes.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/phrs.2023.1606084/full#supplementary-material
References
1. Franc, J, Garegnani, L, Oltra, G, Metzendorf, M, Trivisonno, L, Sgarbossa, N, et al. Long-Term Health Symptoms and Sequelae Following SARS-CoV-2 Infection: An Evidence Map. Int J Environ Res Public Health (2022) 19(16):9915. doi:10.3390/ijerph19169915
2. Senefeld, J, Franchini, M, Mengoli, C, Cruciani, M, Zani, M, Gorman, E, et al. COVID-19 Convalescent Plasma for the Treatment of Immunocompromised Patients: A Systematic Review and Meta-Analysis. JAMA Netw Open (2023) 6(1):e2250647. doi:10.1001/jamanetworkopen.2022.50647
3. World Health Organization (WHO). WHO Coronavirus (COVID-19) Dashboard-Australia (2023). Available From: https://covid19.who.int/region/wpro/country/au (Accessed February 25, 2023).
4. Jarrott, B, Head, R, Pringle, K, Lumbers, E, and Martin, J. “LONG COVID”-A Hypothesis for Understanding the Biological Basis and Pharmacological Treatment Strategy. Pharmacol Res Perspect (2022) 10(1):e00911. doi:10.1002/prp2.911
5. World Health Organization (WHO). Clinical Management of COVID-19: Living Guideline (2023). Available From: https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2023.2 (Accessed February 28, 2023).
6. Akbarialiabad, H, Taghrir, MH, Abdollahi, A, Ghahramani, N, Kumar, M, Paydar, S, et al. Long COVID, a Comprehensive Systematic Scoping Review. Infection (2021) 49(6):1163–86. doi:10.1007/s15010-021-01666-x
7. Nittas, V, Gao, M, West, EA, Ballouz, T, Menges, D, Wulf Hanson, S, et al. Long COVID Through a Public Health Lens: An Umbrella Review. Public Health Rev (2022) 43:1604501. doi:10.3389/phrs.2022.1604501
8. Slimings, C, Harvey, N, and Jones, S. Long COVID in Australia – A Review of the Literature. Canberra: Australian Institute of Health and Welfare (2022).
9. Décary, S, Dugas, M, Stefan, T, Langlois, L, Skidmore, B, Bhéreur, A, et al. Care Models for Long COVID: A Rapid Systematic Review. medRxiv (2021).
10. McMillan, A. Long COVID a ‘Major Health Challenge’ for Australia in Next Few Years: Health Minister. The Age (2022).
11. Brouwers, M, Kho, M, Browman, G, Burgers, J, Cluzeau, F, Feder, G, et al. AGREE II: Advancing Guideline Development, Reporting and Evaluation in Healthcare. CMAJ (2010) 182:E839–42. doi:10.1503/cmaj.090449
12. RACGP. Australia Guideline Caring for Patients With Post COVID-19-Conditions (2022). Available From: https://www.racgp.org.au/clinical-resources/covid-19-resources/clinical-care/caring-for-patients-with-post-covid-19-conditions/introduction (Accessed February 28, 2023).
13. CDC. Long COVID or Post-COVID Conditions (2022). Available From: https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html (Accessed February 28, 2023).
14. NICE, SIGN, RCGP. COVID-19 Rapid Guideline: Managing the Long-Term Effects of COVID-19 (2022). Available From: https://www.nice.org.uk/guidance/ng188/resources/covid19-rapid-guideline-managing-the-longterm-effects-of-covid19-pdf-51035515742 (Accessed March 15, 2023).
15. Ministry of Health. Clinical Rehabilitation Guideline for People With Long COVID (Coronavirus Disease) in Aotearoa New Zealand (2022). Available From: https://www.health.govt.nz/publication/clinical-rehabilitation-guideline-people-long-covid-coronavirus-disease-aotearoa-new-zealand (Accessed March 22, 2023).
16. Shah, W, Hillman, T, Playford, E, and Hishmeh, L. Managing the Long Term Effects of Covid-19: Summary of NICE, SIGN, and RCGP Rapid Guideline. BMJ (2021) 372:n136. doi:10.1136/bmj.n136
17. Ontario Health. Post-COVID-19 Condition: Guidance for Primary Care (2022). Available From: https://www.ontariohealth.ca/sites/ontariohealth/files/2021-12/PostCovidConditionsClinicalGuidance_EN.pdf (Accessed March 15, 2023).
18. Provincial Health Services Authority. Post-COVID Recovery Care (2023). Available From: http://www.phsa.ca/health-professionals/clinical-resources/post-covid-19-care (Accessed March 22, 2023).
19. CanCov. Patient Resources (2020). Available From: https://cancov.net/patient-resources/ (Accessed March 22, 2023).
20. HealthPathways Sydney. SLHD Ambulatory & Specialist Services Accepting HealthLink E-Referrals (2023). Available From: https://sydneyproject.healthpathways.org.au/SLHDe-ReferralProgram.aspx (Accessed March 22, 2023).
21. Pearce, C. How Nepean Hospital Is at the ForeFront of Tackling ‘Long COVID’. The Western Weekender (2022).
22. Shire Family Medical. Our Doctor Dr. James Zhang (2023). Available from: https://www.shirefamilymedical.com/our-doctors/dr-james-zhang/ (Accessed March 22, 2023).
23. Alliance Rehabilitation. Long Covid Services for Townsville & North Queensland (2023). Available From: https://alliancerehab.com.au/current-programs/long-covid/ (Accessed March 22, 2023).
24. Mermaid Central Medical Clinic. Service-Long Covid Clinic (2023). Available From: https://mermaidcentralmedicalclinic.com.au/services/ (Accessed March 22, 2023).
25. The Victorian Rehabilitation Centre. Long COVID Rehabilitation Program Now Available Glen Waverley (2023). Available From: https://thevictorianrehabilitationcentre.com.au/services/long-covid-rehabilitation (Accessed March 2, 2023).
26. Austin Health. Long COVID Rehabilitation Service (ReCOVery) (2022). Available From: https://www.austin.org.au/recovery/ (Accessed March 2, 2023).
27. The Royal Melbourne Hospital. Post-Covid Clinic (2023). Available From: https://www.thermh.org.au/services/respiratory-medicine-sleep-disorders/post-covid-clinic (Accessed March 2, 2023).
28. The Royal Melbourne Hospital. ReCov Program (2023). Available From: https://www.thermh.org.au/services/respiratory-medicine-sleep-disorders/recov-program/ (Accessed March 2, 2023).
29. Northern Health. Northern Health Post COVID-19 Clinic and Rehabilitation (2022). Available From: https://www.nh.org.au/wp-content/uploads/2020/12/Post-Covid-Rehab-Patient-and-Referrer-Information-Sheet.pdf (Accessed March 2, 2023).
30. Janet, B. Post COVID Follow up Alfred Health Model of Care (2022). Available From: https://www.safercare.vic.gov.au/sites/default/files/2021-12/Webinar%2011%20-%20COVID%20%2B%20Pathway%20Learning%20Network.pdf (Accessed March 2, 2023).
31. Geelong Long Covid Clinic. Our Services (2023). Available From: https://www.geelonglongcovidclinic.com.au/services/ (Accessed March 2, 2023).
32. Epworth. Long COVID and Rehabilitation (2023). Available From: https://www.epworth.org.au/who-we-are/our-services/rehabilitation/covid-19-after-effects-and-rehabilitation (Accessed March 2, 2023).
33. Peninsula Health. Community Health: Post Covid-19 Recovery Program (2022). Available From: https://www.peninsulahealth.org.au/wp-content/uploads/Community-Health-Post-Covid-19-Recovery-Program-1.pdf (Accessed March 2, 2023).
34. Canberra Health Services. Post-COVID Recovery Clinic (2023). Available From: https://www.canberrahealthservices.act.gov.au/services-and-clinics/services/post-covid-recovery-clinic#:∼:text=Phone%3A%20(02)%205124%200200 (Accessed March 2, 2023).
35. The St Vincent Hospital Sydney. Post-Acute & Long COVID Clinic (2023). Available From: https://www.svhs.org.au/patients-visitors/covid-19 (Accessed March 2, 2023).
36. Royal Adelaide Hospital. Long COVID Assessment Clinic (2023). Available From: https://s3-ap-southeast-2.amazonaws.com/sahealth-rah-assets/general-downloads/Long-COVID-Clinic-consumer-information-sheet.pdf (Accessed March 2, 2023).
37. The Wesley Hospital. Long COVID (Post-COVID) Clinic (2023). Available From: https://www.wesley.com.au/services/long-covid-clinic (Accessed March 2, 2023).
38. iHealth Centre. Long COVID Clinic (2023). Available From: https://www.ihealthcentre.com.au/indooroopilly/about-our-practice/long-covid-clinic/ (Accessed March 23, 2023).
39. East Metropolitan Health Service. EMHS Post COVID-19 Clinic (2023). Available From: https://emhs.health.wa.gov.au/Hospitals-and-Services/Services/EMHS-Post-COVID-19-Clinic (Accessed March 2, 2023).
40. Post COVID-19 Navigation Service. Post COVID-19 Navigation Service Fact Sheet (2022). Available From: https://www.health.tas.gov.au/sites/default/files/2022-12/Fact-sheet-Post-COVID-19-Navigation-Service.pdf (Accessed March 2, 2023).
41. Nalbandian, A, Desai, A, and Wan, E. Post-COVID-19 Condition. Annu Rev Med (2022) 74:55–64. doi:10.1146/annurev-med-043021-030635
42. RACGP. Patient Resource: Managing Post–COVID-19 Symptoms-Managing Common Symptoms (2022). Available From: https://www.racgp.org.au/clinical-resources/covid-19-resources/patient-resources/patient-resource-managing-post-covid-19-symptoms/managing-common-symptoms (Accessed July 24, 2023).
43. John Hopkins University and Medicine. New COVID-19 Cases Worldwide (2023). Available From: https://coronavirus.jhu.edu/data/new-cases (Accessed July 24, 2023).
44. Ansell, J, and Root, J. Patient Activation (2019). Available From: https://www.choosingwisely.org.au/assets/PatientActivation_PRINT2.pdf (Accessed March 22, 2023).
45. Greco, M. Patient Activation Measure®: A Vital Sign for Value-Based Care (2020). Available From: https://view.officeapps.live.com/op/view.aspx?src=https%3A%2F%2Fvaluebasedcareaustralia.com.au%2Fwp-content%2Fuploads%2F2020%2F06%2FAHHA-webinar-3rd-June-2020-Greco.pptx&wdOrigin=BROWSELINK (Accessed March 2, 2023).
46. Australian Health Minister s’ Advisory Council. National Strategic Framework for Chronic Conditions (2017). In: Government A, editor Canberra. Canberra: Australian Government.
47. Liu, B, Jayasundara, D, Pye, V, Dobbins, T, Dore, GJ, Matthews, G, et al. Whole of Population-Based Cohort Study of Recovery Time From COVID-19 in New South Wales Australia. Lancet Reg Health West Pac (2021) 12:100193. doi:10.1016/j.lanwpc.2021.100193
48. Sakibuzzaman, M, Hassan, A, Hayee, S, Haque, FA, Bushra, SS, Maliha, M, et al. Exacerbation of Pre-Existing Neurological Symptoms With COVID-19 in Patients With Chronic Neurological Diseases: An Updated Systematic Review. Cureus (2022) 14(9):e29297. doi:10.7759/cureus.29297
49. Schofield, J, Leelarathna, L, and Thabit, H. COVID-19: Impact of and on Diabetes. Diabetes Ther (2020) 11(7):1429–35. doi:10.1007/s13300-020-00847-5
50. Shanbehzadeh, S, Tavahomi, M, Zanjari, N, Ebrahimi-Takamjani, I, and Amiri-Arimi, S. Physical and Mental Health Complications Post-COVID-19: Scoping Review. J Psychosom Res (2021) 147:110525. doi:10.1016/j.jpsychores.2021.110525
51. Wang, C, Chudzicka-Czupala, A, Tee, ML, Nunez, MIL, Tripp, C, Fardin, MA, et al. A Chain Mediation Model on COVID-19 Symptoms and Mental Health Outcomes in Americans, Asians and Europeans. Sci Rep (2021) 11(1):6481. doi:10.1038/s41598-021-85943-7
52. Wang, S, Li, Y, Yue, Y, Yuan, C, Kang, JH, Chavarro, JE, et al. Adherence to Healthy Lifestyle Prior to Infection and Risk of Post-COVID-19 Condition. JAMA Intern Med (2023) 183(3):232–41. doi:10.1001/jamainternmed.2022.6555
53. Storz, MA. Lifestyle Adjustments in Long-COVID Management: Potential Benefits of Plant-Based Diets. Curr Nutr Rep (2021) 10(4):352–63. doi:10.1007/s13668-021-00369-x
54. National Institutes of Health. Long COVID Symptoms Linked to Inflammation (2022). Avaliable from: https://www.nih.gov/news-events/nih-research-matters/long-covid-symptoms-linked-inflammation (Accessed July 24, 2023).
55. Adidharma, NC, Dharma, BDI, Negara, KNDP, and Sudewa, IGA. Breathing Exercise and Chest Physiotherapy in Post-Acute COVID-19 Patient: A Case Report. Intisari Sains Medis (2022) 13(1):293–6. doi:10.15562/ism.v13i1.1300
56. Hersche, R, and Weise, A. Occupational Therapy-Based Energy Management Education in People With Post-COVID-19 Condition-Related Fatigue: Results From a Focus Group Discussion. Occup Ther Int (2022) 2022:4590154. doi:10.1155/2022/4590154
57. Estebanez-Perez, MJ, Pastora-Bernal, JM, and Martin-Valero, R. The Effectiveness of a Four-Week Digital Physiotherapy Intervention to Improve Functional Capacity and Adherence to Intervention in Patients With Long COVID-19. Int J Environ Res Public Health (2022) 19(15):9566. doi:10.3390/ijerph19159566
58. Koumpias, AM, Schwartzman, D, and Fleming, O. Long-Haul COVID: Healthcare Utilization and Medical Expenditures 6 Months Post-Diagnosis. BMC Health Serv Res (2022) 22(1):1010. doi:10.1186/s12913-022-08387-3
59. NYSIF. Shining a Light on Long Covid: An Analysis of Workers' Compensation Data (2023). Available From: https://ww3.nysif.com/Home/FooterPages/Column1/Initiatives/LongCOVID (Accessed July 24, 2023).
60. National Health Service. The NHS Plan for Improving Long COVID Services (2022). Available From: https://www.england.nhs.uk/wp-content/uploads/2022/07/C1607_The-NHS-plan-for-improving-long-COVID-services_July-2022.pdf (Accessed July 24, 2023).
61. Pescaru, CC, Crisan, AF, Marc, M, Trusculescu, AA, Maritescu, A, Pescaru, A, et al. A Systematic Review of Telemedicine-Driven Pulmonary Rehabilitation After the Acute Phase of COVID-19. J Clin Med (2023) 12(14):4854. doi:10.3390/jcm12144854
62. Grishechkina, IA, Lobanov, AA, Andronov, SV, Rachin, AP, Fesyun, AD, Ivanova, EP, et al. Long-Term Outcomes of Different Rehabilitation Programs in Patients With Long COVID Syndrome: A Cohort Prospective Study. Eur J Transl Myol (2023) 33(2):11063. doi:10.4081/ejtm.2023.11063
63. Dehghan, M, Ghanbari, A, Ghaedi Heidari, F, Mangolian Shahrbabaki, P, and Zakeri, MA. Use of Complementary and Alternative Medicine in General Population During COVID-19 Outbreak: A Survey in Iran. J Integr Med (2022) 20(1):45–51. doi:10.1016/j.joim.2021.11.004
64. Green, BN, Pence, TV, Kwan, L, and Rokicki-Parashar, J. Rapid Deployment of Chiropractic Telehealth at 2 Worksite Health Centers in Response to the COVID-19 Pandemic: Observations From the Field. J Manipulative Physiol Ther (2020) 43(5):404 e1–404 e10. doi:10.1016/j.jmpt.2020.05.008
65. Giorgi, G, Lecca, LI, Alessio, F, Finstad, GL, Bondanini, G, Lulli, LG, et al. COVID-19-Related Mental Health Effects in the Workplace: A Narrative Review. Int J Environ Res Public Health (2020) 17(21):7857. doi:10.3390/ijerph17217857
66. Shamsi, A, and Peyravi, H. Nursing Shortage, a Different challenge in Iran: A Systematic Review. Med J Islam Repub Iran (2020) 34:8. doi:10.34171/mjiri.34.8
67. Hanson, S, Abbafati, C, Aerts, J, Al-Aly, Z, Ashbaugh, C, Ballouz, T, et al. Estimated Global Proportions of Individuals With Persistent Fatigue, Cognitive, and Respiratory Symptom Clusters Following Symptomatic COVID-19 in 2020 and 2021. JAMA (2022) 328(16):1604–15. doi:10.1001/jama.2022.18931
68. Goinvo. Determinants of Health (2020). Available From: https://www.goinvo.com/vision/determinants-of-health/ (Accessed February 28, 2023).
Keywords: long COVID, care model, guidelines, long COVID services, post COVID-19 condition, multidisciplinary
Citation: Luo S, Zheng Z, Bird SR, Plebanski M, Figueiredo B, Jessup R, Stelmach W, Robinson JA, Xenos S, Olasoji M, Wan DWL, Sheahan J and Itsiopoulos C (2023) An Overview of Long COVID Support Services in Australia and International Clinical Guidelines, With a Proposed Care Model in a Global Context. Public Health Rev 44:1606084. doi: 10.3389/phrs.2023.1606084
Received: 14 April 2023; Accepted: 23 August 2023;
Published: 22 September 2023.
Edited by:
Milena Maule, University of Turin, ItalyReviewed by:
Eva Pagano, Azienda Ospedaliero Universitaria Città della Salute e della Scienza di Torino, ItalyCopyright © 2023 Luo, Zheng, Bird, Plebanski, Figueiredo, Jessup, Stelmach, Robinson, Xenos, Olasoji, Wan, Sheahan and Itsiopoulos. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
PHR is edited by the Swiss School of Public Health (SSPH+) in a partnership with the Association of Schools of Public Health of the European Region (ASPHER)+
*Correspondence: Zhen Zheng, emhlbi56aGVuZ0BybWl0LmVkdS5hdQ==
†These authors have contributed equally to this work and share first authorship
 Shiqi Luo
Shiqi Luo Zhen Zheng
Zhen Zheng Stephen Richard Bird2
Stephen Richard Bird2 Magdalena Plebanski
Magdalena Plebanski Jennifer A. Robinson
Jennifer A. Robinson Jacob Sheahan
Jacob Sheahan