- Research Centre for Palliative Care, Death and Dying, College of Nursing and Health Sciences, Flinders University, Adelaide, SA, Australia
Objectives: This scoping review identifies and details the scope of practice of health professionals who provide palliative care within the primary health setting in Australia.
Methods: A scoping review approach was conducted on the Cinahl (Ebsco), Scopus, Medline (Ovid) and PubMed databases to extract articles from 1 December 2015 to 1 December 2020. Broad text words and MeSH headings were used with relevance to palliative care, general practice, primary health, and community setting. Extracted journal articles were limited to those based on the Australian population or Australian health system.
Results: Eighty-four papers met the inclusion criteria and were included in the review. The review identified the following health professional roles within the Primary Health Care setting undertaking palliative care: General Practitioner, Nurse, Pharmacist, Paramedics, Carers, and Allied Health professionals.
Conclusion: This review offers a first understanding of the individual health professional roles and multidisciplinary team approach to actively providing palliative care within the Primary Health Care setting in Australia.
Introduction
In Australia, as in many other countries around the world, there is an increasing demand for palliative care services as a result of an aging population and an increase in the prevalence of cancer and chronic disease [1]. This has led to palliative care being provided in almost all health care settings within the Australian health care system, including hospital intensive care units, inpatient services, outpatient services, general practices, ambulatory services, pharmacies, and residential aged care facilities [2]. As a result, in Australia palliative care has become highly institutionalized [3]. However, recent survey data reveals that 60%–70% of Australians would prefer to die at home [4], which echoes the emerging trend of older Australian’s preferring to age in place. Though for this shift in the preferred place of death to occur within Australia, end-of-life care will have to change to provide more support for dying at home [3].
In response to the growing demand for palliative care at home, on the first of July 2021, the Australian Government provided funding (Greater Choice for At Home Palliative Care Measure) to the Primary Health Networks (PHNs), which are independent organizations focused on rationalizing health services to ensure equitable and appropriate health care provision [5]. The goals of the Greater Choice for At Home Palliative Care measure are to:
• improve your access to the best palliative care at home;
• support palliative care services in primary health and community care;
• make sure you get the right care, at the right time and in the right place to reduce unnecessary hospital visits;
• generate and use data to improve services;
• use technology to provide flexible and responsive care, including after-hours care [6].
PHNs are well placed to help coordinate at-home palliative care as their primary roles are to commission health services, work closely with health professionals to build health service capacity, integrate services at a local level, and ensure that health services meet the requirements of their region’s population [5].
While the Australian Government has provided financial incentive to develop palliative care within the Primary Health Care setting, many primary health care providers may not consider they have many palliative care patients even though they may provide care for people with progressive, chronic and/or life limiting illness and older people approaching the last years of life. This can make maintaining a depth of knowledge and acquiring new knowledge on palliative care difficult. In particular knowledge on recent trends in pharmaceutical management, new pain management, and approaches to using these medications are especially challenging [7]. Health professionals working in the Primary Health Care setting have also reported that their undergraduate education does not adequately cover palliative care and that they may not possess the skills required to manage palliative care patients [7]. This highlights the need by health professionals within the Primary Health Care setting for quality information and resources on palliative care management. Of high importance is the need for evidence and information to develop their professional knowledge, to enable clinical and service delivery of palliative care [8].
There is a growing body of evidence on providing Palliative care within the Primary Health Care setting and a need by Health Professionals to be able to access this evidence easily and quickly to provide best clinical practice and more generally for professional development [9]. However, providing access to appropriate information in a format that is feasible for health professionals is challenging [7]. There are several reasons for this, including the lack of time of health professionals have, as well as the volume of published research which makes specific evidence hard to find and manage [9].
The objective of this scoping literature review is to provide an overview of health professionals providing palliative care within the Primary Health Care setting within Australia. The results from this scoping review will then be developed into content for a new section within CareSearch, which provides health professionals, as well as those affected by the need for palliative care, with online evidence and information [10]. In this way, health professionals in the Primary Health Care setting are provided with information that will enable them to provide high-quality palliative care [11].
Methods
Search Strategy
We used a scoping review approach to collect and describe peer-reviewed journal articles from the last 5 years [12, 13]. Due to the relatively new field of palliative care within the Primary Health Care setting within Australia, a scoping review methodology was used rather than a systematic review, as it was better suited to clarifying key concepts and identifying available evidence.
Peer-reviewed journal articles were retrieved through searching electronic databases. The database search strategy (SupplementaryAppendix S1) was developed and tested in PubMed with the help of a health Librarian. Broad text words and MeSH headings were used: palliative care, general practice, primary health, Australia, allied health personnel, and community setting. Extracted journal articles were limited to those based on the Australian population or Australian health system. A date limit of the last 5 years was applied due to time and resource constraints. Once the search was finalised and run in PubMed, it was then translated and run in Cinahl (Ebsco), Scopus, and Medline (Ovid) on 1 December 2020.
Study Selection
The search results for each database were uploaded into Endnote X9.3 reference management software and deduplicated. Journal articles were then imported into the web-based software Covidence for screening and data extraction.
Two reviewers (DvG and KEA) independently assessed titles and abstracts against the priori inclusion criteria outlined in Table 1. Where eligibility was unclear based on the title and abstract screening, the full text article was retrieved and assessed.
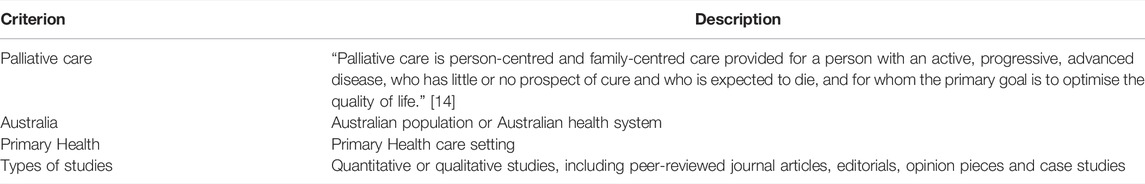
TABLE 1. Inclusion criteria for title and abstract screening of the included papers (Australia, 2022).
Criteria for inclusion were agreed upon by both reviewers (see Table 1.)
Two reviewers (DvG and KE-A) then defined exclusion criteria (Table 2) to exclude articles which were not relevant to the aim of the scoping review. Both reviewers then screened the full text against the exclusion criteria.
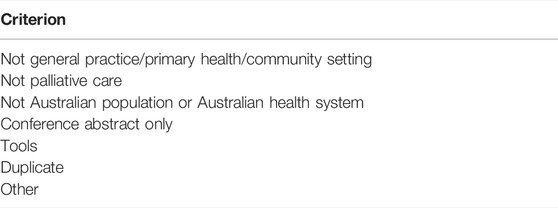
TABLE 2. Exclusion criteria for title and abstract screening of the included papers (Australia, 2022).
Results
The literature search strategy (Figure 1) highlights the systematic approach that was undertaken to select relevant publications from the initial 1,699 that were identified through the database searches. Covidence software [15] was then used to remove duplicate publications (n = 34) and review the publications title and abstracts against the inclusion criteria (Table 1) which resulted in the removal of 1289 publications. The full text of the remaining publications were then reviewed against the defined exclusion criteria and a further 292 publications were removed. The independent review process resulted in 84 publications being included in the scoping review (SupplementaryAppendix S2). Findings are presented for defined health professional roles.
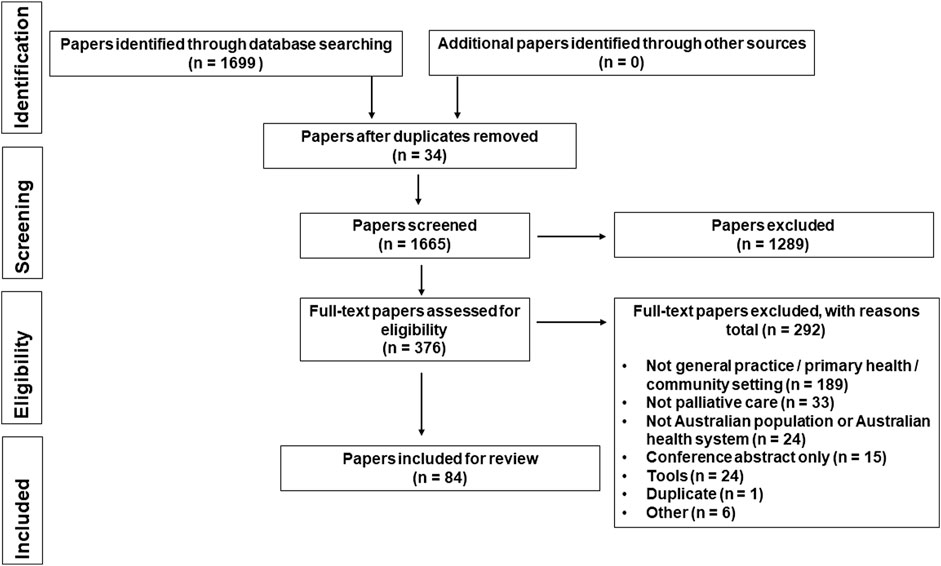
FIGURE 1. Search results in a PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) Flow Diagram (Australia, 2022).
General Practitioners
As the population ages, GPs and General Practice Nurses are increasingly expected to provide end-of-life care [16, 17]. As a natural extension of primary care, palliative care often includes GPs providing continuity of care by setting up an individualized care pathway from diagnosis to palliation, coordinating care across that pathway, and collaborating with other health care providers [18–22]. Hence, most General Practitioners are already practicing end-of-life care without recognising it [23]. Since GPs provide care throughout a patient’s lifetime they are well positioned to identify those with life-limiting illnesses and to address the needs of patients and caregivers [20, 24, 25].
The palliative care process is very complex and involves interactions between GPs and patients and their carers as well as other service providers both in the community and in acute care settings [20]. GPs are essential players in an integrated model of palliative care as they are often intimately familiar with patients and caregivers, expert in generalist care, and knowledgeable about health and social services in their local region [18, 26]. Team members vary depending on patients’ needs and local availability of health professionals, but in most cases, home-based palliative care teams are led and coordinated by the GP [27]. Health professional members include nurses, social workers, occupational therapists, other allied health professionals, and the local pharmacist, however if the patient is more complex, specialist palliative care services may be enlisted by the GP to complement the skills of the local team [27]. Therefore community based palliative care is often seen as a collaborative, integrative model incorporating generalist and specialist palliative care providers that is coordinated by a GP [28], often through interprofessional case conferences [16].
The GP role is diverse and includes symptom management, pain management and non-malignant disease management [16]. The GP is proactive in clinical care planning, anticipating and providing care as the person’s clinical condition deteriorates and as the goals of care shift from treating illness to comfort and death management [29]. Therefore, the GPs role also includes making referrals to specialist palliative care services [25, 30]. GPs are also often involved in end-of-life conversations, starting with establishing a strong doctor-patient relationship, gauging patients’ readiness to engage, and managing time availability [31]. Conversations usually start when a patient initiates them, when they are included in routine care, when they discuss prognosis or less directly inquire about the patients feelings about death [31]. GPs commit time and resource to assist their patients to create an end-of-life care plan [32], however, at times the end-of-life care plan is not explicitly articulated and discussed, so an informal care plan is developed gradually without discussing these plans with the patient [33].
With limited specialist palliative care resources available in the community, it is often GPs who provide and co-ordinate end-of-life care in collaboration with community-based support services [18]. This has resulted in the GP role differing slightly in urban versus rural settings due to resource limitations and lack of training [34]. Although inappropriate payment models discourage the involvement of GPs in certain end-of-life care aspects, such as case conferences and home visits, rural communities often indicate closer relationships between GPs and patients and better care integration and collaboration [34]. This points out the importance of providing GPs and rural/remote communities with support, education, incentives, better administrative tools, and options for advanced care planning [35].
Paramedics
Paramedics play an important role in community-based palliative care [36], their role is to treat patients who are experiencing health problems related to palliative care, such as pain and respiratory distress [37]. With Extended Care Paramedics responding to palliative care emergencies, and preventing unwanted and unnecessary hospitalisations [38]. In response to the increased use of Ambulance services in Australia to palliative care patients they are developing specific palliative care guidelines [37].
Carers
Patients’ caregivers usually know them best and are most motivated to help [27]. In the Primary Health Care setting, a palliative patient’s caregiver can provide assistance with activities of daily living, personal and domestic care, and shopping and household responsibilities [39]. Assistance may also include basic nursing care, as determined by the patient’s GP and the specialist palliative care team [39]. In addition, caregivers can have a role in managing medications for palliative care patients [40], and with training and support, can administer subcutaneous injections to relieve symptoms [41]. GP’s also play a role in supporting the carer, and as a result the Carer Supports Needs Assessment Tool is often integrated into palliative care within the Primary Health Care setting [42]. This tool facilitates support for family members and carers of adults with life-limiting conditions. In addition to indicating additional support they need, caregivers can also use this tool to indicate they need support for their own health and well-being in caring for a palliative care patient at home [42].
Pharmacists
For older populations, Pharmacists can provide comprehensive health care at the end of life [43]. The Pharmacist plays a key role in ensuring that palliative care patients receive the best possible medication management [44], with community pharmacies providing medication for managing symptoms of the terminal phase [45]. Medication management for long term palliative care occurs as an interdisciplinary collaboration between pharmacists, GP’s, carers and other health professionals [46, 47], with improved management occurring when pharmacists are engaged in anticipation of the terminal phase [45, 48, 49]. Tait and Cheung [50] identified six key themes to improve community access to terminal phase medicines in Australia: medication supply, education and training, caregiver burden, safety, funding and clinical governance.
Nurses
There are several well-defined nursing roles undertaking palliative care within the primary health setting. With adequate training and support, General Practice Nurses are able to initiate and facilitate advanced care planning conversations with patients [51]. In those cases where access to specialists is difficult, Advance Nurses provide specialized care [52]. With their knowledge of rural health resources available to patients, District Nurses are an expert advocate for implementing a person-centred goal plan for rural palliative patients [53]. Nurse practitioner coordinated palliative care appears to enable more integrated care which extends the potential for collaborative primary care and may be effective in reducing hospitalisations [54, 55]. Providing physical care to patients, managing symptoms and educating families are often roles undertaken by Specialist Nurses [56].
Allied Health Professionals
To a lesser extent, the review has also highlighted the importance of specific allied health professionals in the provision of physical care (optimising function and nonpharmacological symptom management), social, emotional, and spiritual care [57] of palliative care patients within the primary health setting. Having Advanced Care Planner Facilitators within general practices can positively impact end-of-life care experience by referring patients to supportive programs and facilitating advance care planning [58].
Discussion
This scoping review has identified a diverse range of individual health professional roles who work as a multidisciplinary team to meet the palliative care needs of people with life limiting illness within the Primary Health Care setting within Australia. The review has also identified that health professionals not only have a relationship to people with life-limiting illness but also their carers. While carers are not health professionals they have an important role to play in providing care for people with life limiting illness, and therefore they are often included as part of the multidisciplinary team. Carers enable care within the community through providing basic nursing, help with daily activities and with training can provide medication management and subcutaneous injections [39, 41].
The review has highlighted the pivotal role that GPs play as the patients first contact at various points along the care trajectory as a natural extension of primary care [20]. As GPs provide first-line services [59], and play an important role in engaging the multidisciplinary team of health professionals, including community services, allied health professionals, and palliative care physicians [20]. With the composition of the multidisciplinary team being determined by the patients’ palliative care needs and their accessibility to services. This multidisciplinary teamwork approach to address individual palliative care needs can be clearly seen in the work by Saurman et. al. 2019 [60] who mapped the delivery of palliative care in the Far West Local Health District in New South Wales, Australia. The Far West Local Health District network mapping has also highlighted the integration of services and care practice, identifying palliative care activities that can be undertaken by a number of health professional roles. Mapping palliative care pathways within the Primary Health Care setting provides examples to other health professionals new to palliative care and shows that policy makers and systems are currently active in this setting. The identified pathways provide Primary Health Care Networks in Australia with clear evidence on the health professionals, services and models of care that are required to meet palliative care needs within their regions.
The increase in the number of people preferring to undertake palliative care at home and the provision of financial incentives from the Australian Government through the Greater Choice for at Home Palliative Care Measure has provided momentum for increased positive end-of-life services for people with life limiting illness and their carers within the Primary Health Care setting within Australia [61]. However, there are currently obstacles to support people at home to have their symptoms well managed and to provide personal, social, and psychological support. Palliative care delivery in the Primary Health Care setting is currently challenged by meeting the needs of the increasing number of people requiring palliative care, the need to increase the workforce capacity and capability of health professionals [59]. The review findings suggest that for best practice palliative care to occur within this setting, there is a need to support those that actively provide palliative care with training, evidence to inform practice and tools.
The identification of these health professional roles and the palliative care activities that they undertake has provided the scope for developing an evidence base for continuing professional development and for clinical decision making to support palliative care within the Primary Health Care setting. The multidisciplinary team approach that has been acknowledged within several articles further extends the scope of evidence that is required to support health professionals working within the Primary Health Care setting to include referral triggers and pathways between not only health professionals but settings of care including primary care, aged care and acute care.
Strengths and Limitations
Our scoping review benefits from several strengths. Firstly, the scoping literature review search was undertaken by a professional health librarian. The study selection process was verified by a second reviewer to ensure the inclusion and exclusion criteria were applied accurately. The scoping literature review has been a useful way to synthesise a broad range of research evidence about palliative care within the Primary Health Care setting within Australia. However, this scoping literature review would have benefitted from a search of grey literature to yield insights into broader aspects of palliative care within the Primary Health Care setting.
A limitation of this review is that the literature surveyed was limited to Australia only. However, this provides a good national example of palliative care within the Primary Health Care setting which could be adopted by other countries.
Conclusion
This scoping review has identified health professional roles and their scope of practice in providing palliative care within the Primary Health Care setting within Australia. It has also provided examples of models of care which support people with life-limiting illness engage with other services and health professionals within the Primary Heath Care setting and across other health care settings.
Author Contributions
JT and KE-A initiated the concept for the scoping review. The literature was reviewed for inclusion by DvG and KE-A. DvG analysed the results and wrote the manuscript, JT and KE-A provided comments.
Funding
The CareSearch project is supported by the Australian Government Department of Health.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
All authors thank Ms. Sue Hammond for her assistance with the literature search.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/phrs.2022.1604856/full#supplementary-material
References
2.Welfare AIoHa. Palliative Care Services in Australia: Australian Government (2021). Available from: https://www.aihw.gov.au/reports/palliative-care-services/palliative-care-services-in-australia (Accessed November 20, 2021).
3. Swerissen, H, and Duckett, SJ. What can we Do to help Australians die the way they want to? Med J Aust (2015) 202(1):10–1. doi:10.5694/mja14.01580
4. Foreman, LM, Hunt, RW, Luke, CG, and Roder, DM. Factors Predictive of Preferred Place of Death in the General Population of South Australia. Palliat Med (2006) 20:447–53. doi:10.1191/0269216306pm1149oa
5.Health Do. Primary Health Networks: Australian Government; [updated 2/9/202124/11/2021] (2021). Available from: https://www.health.gov.au/initiatives-and-programs/phn (Accessed November 24, 2021).
6.Health Do. Greater Choice for at home Palliative Care Measure: Australian Government; [updated 12/05/2021; Cited 2021 20/11/2021] (2021). Available from: https://www.health.gov.au/initiatives-and-programs/greater-choice-for-at-home-palliative-care-measure (Accessed November 20, 2021).
7. White, K. Rural Palliative Care: Exploration of the Pivotal Role of Primary Healthcare Providers. CancerForum (2007) 31(1).
8. Tieman, J. Ensuring Quality in Online Palliative Care Resources. Cancers (2016) 8(12):E113. doi:10.3390/cancers8120113
9. Tieman, J. Ensuring Quality in Online Palliative Care Resources. Cancers (2016) 8(12):E113. doi:10.3390/cancers8120113
10. Tieman, J, and Lewis, V. Benefits of Structured Engagement with Target Audiences of a Health Website: Study Design for a Multi-Case Study. Healthcare (2021) 9:600. doi:10.3390/healthcare9050600
11.Welfare AIoHa. Review and Evaluation of Australian Information about Primary Health Care: A Focus on General Practice. Canberra, Australia: Australian Institute of Health and Welfare (2008).
12. Arksey, H, and O'Malley, L. Scoping Studies: Towards a Methodological Framework. Int J Soc Res Methodol (2005) 8(1):19–32. doi:10.1080/1364557032000119616
13. Rumrill, PD, Fitzgerald, SM, and Merchant, WR. Using Scoping Literature Reviews as a Means of Understanding and Interpreting Existing Literature. Work (2010) 35(3):399–404. doi:10.3233/WOR-2010-0998
14.Australia PC. What Is Palliative Care? [cited 2021 20/11/2021] (2021). Available from: https://palliativecare.org.au/what-is-palliative-care (Accessed November 20, 2021).
16. Senior, H, Grant, M, Rhee, JJ, Aubin, M, McVey, P, Johnson, C, et al. General Practice Physicians' and Nurses' Self-Reported Multidisciplinary End-Of-Life Care: a Systematic Review. BMJ support (2019) 29:29.
17. Reymond, L, Cooper, K, Parker, D, and Chapman, M. End-of-life Care: Proactive Clinical Management of Older Australians in the Community. Aust Fam Physician (2016) 45(1):76–8.
18. Johnson, CE, McVey, P, Rhee, JJ, Senior, H, Monterosso, L, Williams, B, et al. General Practice Palliative Care: Patient and Carer Expectations, advance Care Plans and Place of Death-A Systematic Review. BMJ support (2018) 25:25.
19. Mitchell, G, Aubin, M, Senior, H, Johnson, C, Fallon-Ferguson, J, Williams, B, et al. General Practice Nurses and Physicians and End of Life: a Systematic Review of Models of Care. BMJ support (2020) 27:27.
20. Herrmann, A, Carey, M, Zucca, A, Boyd, L, and Roberts, B. General Practitioners' Perceptions of Best Practice Care at the End of Life: a Qualitative Study. BJGP open (2019) 3(3):bjgpopen19X101660. doi:10.3399/bjgpopen19X101660
21. van de Mortel, TF, Marr, K, Burmeister, E, Koppe, H, Ahern, C, Walsh, R, et al. Reducing Avoidable Admissions in Rural Community Palliative Care: a Pilot Study of Care Coordination by General Practice Registrars. Aust J Rural Health (2017) 25(3):141–7. doi:10.1111/ajr.12309
22. Halkett, GK, Jiwa, M, and Lobb, EA. Patients' Perspectives on the Role of Their General Practitioner after Receiving an Advanced Cancer Diagnosis. Eur J Cancer Care (2015) 24(5):662–72. doi:10.1111/ecc.12224
23. Mitchell, GK, Senior, HE, Johnson, CE, Fallon-Ferguson, J, Williams, B, Monterosso, L, et al. Systematic Review of General Practice End-Of-Life Symptom Control. BMJ Support Palliat Care (2018) 8(4):411–20. doi:10.1136/bmjspcare-2017-001374
24. Johnson, CE, Senior, H, McVey, P, Team, V, Ives, A, and Mitchell, G. End-of-life Care in Rural and Regional Australia: Patients’, Carers’ and General Practitioners’ Expectations of the Role of General Practice, and the Degree to Which They Were Met. Health Soc Care Community (2020) 28(6):2160–71. doi:10.1111/hsc.13027
25. Rhee, JJ, Teo, PCK, Mitchell, GK, Senior, HE, Tan, AJH, and Clayton, JM. General Practitioners (GPs) and End-Of-Life Care: a Qualitative Study of Australian GPs and Specialist Palliative Care Clinicians. BMJ support (2018) 01:01.
26. Carmont, SA, Mitchell, G, Senior, H, and Foster, M. Systematic Review of the Effectiveness, Barriers and Facilitators to General Practitioner Engagement with Specialist Secondary Services in Integrated Palliative Care. BMJ Support Palliat Care (2017) 8(4):385–99. doi:10.1136/bmjspcare-2016-001125
27. Reymond, L, Parker, G, Gilles, L, and Cooper, K. Home-Based Palliative Care. Aust J Gen Pract (2018) 47(11):747–52. doi:10.31128/AJGP-06-18-4607
28. Le, B, Eastman, P, Vij, S, McCormack, F, Duong, C, and Philip, J. Palliative Care in General Practice: GP Integration in Caring for Patients with Advanced Cancer. Aust Fam Physician (2017) 46(1):51–5.
30. Sinclair, C, Davidson, C, and Auret, K. The Role of Mediation in advance Care Planning and End-Of-Life Care. Aust Fam Physician (2016) 45(1):69–73.
31. Deckx, L, Thomas, HR, Sieben, NA, Foster, MM, and Mitchell, GK. General Practitioners' Practical Approach to Initiating End-Of-Life Conversations: a Qualitative Study. Fam Pract (2020) 37(3):401–5. doi:10.1093/fampra/cmz074
32. Panozzo, L, Harvey, P, Adams, MJ, O'Connor, D, and Ward, B. Communication of advance Care Planning Decisions: a Retrospective Cohort Study of Documents in General Practice. BMC Palliat Care (2020) 19(1):108. doi:10.1186/s12904-020-00613-1
33. Deckx, L, Mitchell, G, Rosenberg, J, Kelly, M, Carmont, SA, and Yates, P. General Practitioners' Engagement in End-Of-Life Care: a Semi-structured Interview Study. BMJ support (2019) 03:03.
34. Ding, J, Saunders, C, Cook, A, and Johnson, CE. End-of-life Care in Rural General Practice: How Best to Support Commitment and Meet Challenges? BMC Palliat Care (2019) 18(1):51. doi:10.1186/s12904-019-0435-4
35. Littlewood, J, Hinchcliff, R, Lo, W, and Rhee, J. Advance Care Planning in Rural New South Wales from the Perspective of General Practice Registrars and Recently Fellowed General Practitioners. Aust J Rural Health (2019) 27(5):398–404. doi:10.1111/ajr.12525
36. Long, D. Paramedic Delivery of Community-Based Palliative Care: An Overlooked Resource? Prog Palliat Care (2019) 27(6):289–90. doi:10.1080/09699260.2019.1672414
37. Lord, B, Andrew, E, Henderson, A, Anderson, DJ, Smith, K, and Bernard, S. Palliative Care in Paramedic Practice: A Retrospective Cohort Study. Palliat Med (2019) 33(4):445–51. doi:10.1177/0269216319828278
38. Mills, J. Ambulance Wish: An Opportunity for Public Health Palliative Care Partnerships with Paramedics and Other Community Members. Prog Palliat Care (2020) 28(1):17–8. doi:10.1080/09699260.2020.1695335
39. MacLeod, R, Johnson, C, and Yule, S. Making it easier for people to die at home - an innovative programme in New South Wales, Australia. Eur J Palliat Care (2015) 22(1):26–9.
40. Tait, P, Cuthbertson, E, and Currow, DC. What Are the Factors Identifying Caregivers Who Need Help in Managing Medications for Palliative Care Patients at Home? J Palliat Med (2020) 23(8):1084–9. doi:10.1089/jpm.2019.0573
41. Healy, S, Israel, F, Charles, M, and Reymond, L. Laycarers Can Confidently Prepare and Administer Subcutaneous Injections for Palliative Care Patients at home: A Randomized Controlled Trial. Palliat Med (2018) 32(7):1208–15. doi:10.1177/0269216318773878
42. Aoun, S, Toye, C, Deas, K, Howting, D, Ewing, G, Grande, G, et al. Enabling a Family Caregiver-Led Assessment of Support Needs in home-based Palliative Care: Potential Translation into Practice. Palliat Med (2015) 29(10):929–38. doi:10.1177/0269216315583436
43. Tait, P, Chakraborty, A, and Tieman, J. The Roles and Responsibilities of Community Pharmacists Supporting Older People with Palliative Care Needs: A Rapid Review of the Literature. Pharmacy (2020) 8(3):E143. doi:10.3390/pharmacy8030143
44. Kuruvilla, L, Weeks, G, Eastman, P, and George, J. Medication Management for Community Palliative Care Patients and the Role of a Specialist Palliative Care Pharmacist: A Qualitative Exploration of Consumer and Health Care Professional Perspectives. Palliat Med (2018) 32(8):1369–77. doi:10.1177/0269216318777390
45. Tait, P, Sheehy, K, Sindhusake, D, and Muscillo, N. Factors Affecting Access to Subcutaneous Medicines for People Dying in the Community. Prog Palliat Care (2020) 28(5):326–33. doi:10.1080/09699260.2020.1746033
46. Disalvo, D, Luckett, T, Bennett, A, Davidson, P, and Agar, M. Pharmacists' Perspectives on Medication Reviews for Long-Term Care Residents with Advanced Dementia: a Qualitative Study. Int J Clin Pharm (2019) 41(4):950–62. doi:10.1007/s11096-019-00821-7
47. Cross, AJ, Etherton-Beer, CD, Clifford, RM, Potter, K, and Page, AT. Exploring Stakeholder Roles in Medication Management for People Living with Dementia. Res Soc Administrative Pharm (2020) 17:707. doi:10.1016/j.sapharm.2020.06.006
48. Tait, P, Horwood, C, Hakendorf, P, and To, T. Improving Community Access to Terminal Phase Medicines through the Implementation of a 'Core Medicines List' in South Australian Community Pharmacies. BMJ Support Palliat Care (2020) 10(1):e4. doi:10.1136/bmjspcare-2016-001191
49. Antoine, S, Glewis, S, Alexander, M, Lingaratnam, MS, Cherie, C, and Luetsch, K. Cancer Patients' Perspectives on Participating in a Community Pharmacy-Based Hyperglycaemia Screening Service - A Qualitative Exploration of Enablers and Barriers. Res Soc Adm Pharm (2020) 28:28.
50. Tait, PA, Cheung, WH, Wiese, M, and Staff, K. Improving Community Access to Terminal Phase Medicines in Australia: Identification of the Key Considerations for the Implementation of a 'core Medicines List. Aust J Prim Health (2017) 23(4):373–8. doi:10.1071/PY16153
51. Miller, H, Tan, J, Clayton, JM, Meller, A, Hermiz, O, Zwar, N, et al. Patient Experiences of Nurse-Facilitated advance Care Planning in a General Practice Setting: a Qualitative Study. BMC Palliat Care (2019) 18(1):25. doi:10.1186/s12904-019-0411-z
52. Khalil, H, Poon, P, Byrne, A, and Ristevski, E. Challenges Associated with Anticipatory Medications in Rural and Remote Settings. J Palliat Med (2019) 22(3):297–301. doi:10.1089/jpm.2018.0354
53. Reed, F, Fitzgerald, L, and Bish, MR. Advocating for End-Of-Life Choice at home: a Survey of Rural Australian Nurses. Rural Remote Health (2018) 18(3):4322. doi:10.22605/RRH4322
54. Mitchell, GK, Senior, HE, Bibo, MP, Makoni, B, Young, SN, Rosenberg, JP, et al. Evaluation of a Pilot of Nurse Practitioner Led, GP Supported Rural Palliative Care Provision. BMC Palliat Care (2016) 15(1):93. doi:10.1186/s12904-016-0163-y
55. Craswell, A, Wallis, M, Coates, K, Marsden, E, Taylor, A, Broadbent, M, et al. Enhanced Primary Care provided by a Nurse Practitioner Candidate to Aged Care Facility Residents: A Mixed Methods Study. Collegian (2020) 27(3):281–7. doi:10.1016/j.colegn.2019.08.009
56. Rabbetts, L, Harrington, A, and Breaden, K. Nurses' Experience of Providing home-based Palliative Care in the Country Setting: An Integrated Literature Review. Int J Nurs Pract (2020) 26(1). doi:10.1111/ijn.12773
57. Morgan, D, Rawlings, D, Button, E, and Tieman, J. Allied Health Clinicians' Understanding of Palliative Care as it Relates to Patients, Caregivers, and Health Clinicians: A Cross-Sectional Survey. J Allied Health (2019) 48(2):127–33.
58. Mann, J, Gill, SD, Mitchell, L, Rogers, MJ, Martin, P, Quirk, F, et al. Locating advance Care Planning Facilitators in General Practice Increases Consumer Participation. Aust Fam Physician (2017) 46(9):691–5.
60. Saurman, E, Lyle, D, Wenham, S, and Cumming, M. A Mapping Study to Guide a Palliative Approach to Care. Rural Remote Health (2019) 19(1):4625. doi:10.22605/RRH4625
61. Aoun, SM, Abel, J, Rumbold, B, Cross, K, Moore, J, Skeers, P, et al. The Compassionate Communities Connectors Model for End-Of-Life Care: A Community and Health Service Partnership in Western Australia. Palliat Care Soc Pract (2020) 14:2632352420935130. doi:10.1177/2632352420935130
62. Aoun, SM, Breen, LJ, and Skett, K. Supporting Palliative Care Clients Who Live Alone: Nurses' Perspectives on Improving Quality of Care. Collegian (2016) 23(1):13–8. doi:10.1016/j.colegn.2014.09.007
64. Bernardes, CM, Beesley, V, Martin, J, Sabesan, S, Baade, P, Meiklejohn, JA, et al. Unmet Supportive Care Needs Among People with Cancer: A Cross-Cultural Comparison between Indigenous and Non-indigenous Australians. Eur J Cancer Care (2019) 28(5):e13080. doi:10.1111/ecc.13080
65. Bernardes, CM, Martin, J, Cole, P, Kitchener, T, Cowburn, G, Garvey, G, et al. Lessons Learned from a Pilot Study of an Indigenous Patient Navigator Intervention in Queensland, Australia. Eur J Cancer Care (2018) 27(1):e12714. doi:10.1111/ecc.12714
66. Borthwick, A, and Higgs, P. The Medical Treatment Planning and Decisions Act 2016: what Is the Role for Allied Health Professionals? Aust J Prim Health (2020) 26(5):383–7. doi:10.1071/PY19212
67. Carey, ML, Zucca, AC, Freund, MA, Bryant, J, Herrmann, A, and Roberts, BJ. Systematic Review of Barriers and Enablers to the Delivery of Palliative Care by Primary Care Practitioners. Palliat Med (2019) 33(9):1131–45. doi:10.1177/0269216319865414
68. Carey, TA, Arundell, M, Schouten, K, Humphreys, JS, Miegel, F, Murphy, S, et al. Reducing Hospital Admissions in Remote Australia through the Establishment of a Palliative and Chronic Disease Respite Facility. BMC Palliat Care (2017) 16(1):54. doi:10.1186/s12904-017-0247-3
69. Carey, TA, Schouten, K, Wakerman, J, Humphreys, JS, Miegel, F, Murphy, S, et al. Improving the Quality of Life of Palliative and Chronic Disease Patients and Carers in Remote Australia with the Establishment of a Day Respite Facility. BMC Palliat Care (2016) 15:62. doi:10.1186/s12904-016-0136-1
70. Champion, N. Exploring why some terminally ill people die in hospital when home was their preferred choice. Aust J Adv Nurs (2015) 33(2):6–12.
71. Clark, K, Connolly, A, Clapham, S, Quinsey, K, Eagar, K, and Currow, DC. Physical Symptoms at the Time of Dying Was Diagnosed: A Consecutive Cohort Study to Describe the Prevalence and Intensity of Problems Experienced by Imminently Dying Palliative Care Patients by Diagnosis and Place of Care. J Palliat Med (2016) 19(12):1288–95. doi:10.1089/jpm.2016.0219
72. Collier, A, Hodgins, M, Crawford, G, Every, A, Womsley, K, Jeffs, C, et al. What Does it Take to Deliver Brilliant home-based Palliative Care? Using Positive Organisational Scholarship and Video Reflexive Ethnography to Explore the Complexities of Palliative Care at home. Palliat Med (2019) 33(1):91–101. doi:10.1177/0269216318807835
73. Collier, A, Rowett, D, Allcroft, P, Greene, A, and Currow, DC. Academic Detailing of General Practitioners by a Respiratory Physician for Diagnosis and Management of Refractory Breathlessness: a Randomised Pilot Study. BMC Health Serv Res (2015) 15:193. doi:10.1186/s12913-015-0861-9
74. Cross, J, Fischer, A, Shotton, D, Pollicino, C, May, A, Vora, R, et al. Supporting Choice: an Innovative Model of Integrated Palliative Care Funded by a Private Health Insurer. Intern Med J (2020) 50(8):931–7. doi:10.1111/imj.14615
75. Ding, J, Johnson, CE, and Cook, A. How We Should Assess the Delivery of End-Of-Life Care in General Practice? A Systematic Review. J Palliat Med (2018) 21:1790–805. doi:10.1089/jpm.2018.0194
76. Dong, ST, Butow, PN, Agar, M, Lovell, MR, Boyle, F, Stockler, M, et al. Clinicians' Perspectives on Managing Symptom Clusters in Advanced Cancer: A Semistructured Interview Study. J Pain Symptom Manage (2016) 51(4):706–17. e5. doi:10.1016/j.jpainsymman.2015.11.021
77. Dunning, T. Integrating Palliative Care with Usual Care of Diabetic Foot Wounds. Diabetes Metab Res Rev (2016) 32(1):303–10. doi:10.1002/dmrr.2758
78. Edwards, J, Hooper, D, Rothwell, G, Kneen, K, Watson, J, and Saurman, E. A Nurse Practitioner-Led Community Palliative Care Service in Australia. Int J Palliat Nurs (2019) 25(5):245–53. doi:10.12968/ijpn.2019.25.5.245
79. Ewald, D, Marr, K, and van de Mortel, T. Reducing Avoidable Admissions in Rural Palliative Care. Int J Integr Care (2018) 18:19–2. doi:10.5334/ijic.s1019
80. Fletcher, S, Sinclair, C, Rhee, J, Goh, D, and Auret, K. Rural Health Professionals' Experiences in Implementing advance Care Planning: a Focus Group Study. Aust J Prim Health (2016) 22(5):423–7. doi:10.1071/PY15004
81. Harvey, P, Panozzo, L, Adams, MJ, O'Connor, D, and Ward, B. Rural Health Services' Relationships with Patients: An Enabler and a Barrier to advance Care Planning. Aust J Rural Health (2019) 27(6):563–7. doi:10.1111/ajr.12542
82. Holloway, K, Toye, C, McConigley, R, Tieman, J, Currow, D, and Hegarty, M. National Consultation Informing Development of Guidelines for a Palliative Approach for Aged Care in the Community Setting. Australas J Ageing (2015) 34(1):21–6. doi:10.1111/ajag.12083
83. Hudson, P, Trauer, T, Kelly, B, O'Connor, M, Thomas, K, Zordan, R, et al. Reducing the Psychological Distress of Family Caregivers of home Based Palliative Care Patients: Longer Term Effects from a Randomised Controlled Trial. Psychooncology (2015) 24(1):19–24. doi:10.1002/pon.3610
84. Jiang, B, Bills, M, and Poon, P. Integrated Telehealth-Assisted home-based Specialist Palliative Care in Rural Australia: A Feasibility Study. J Telemed Telecare (2020) 2020:1357633X2096646. doi:10.1177/1357633X20966466
85. Johns, LL, McAuliffe, D, and Dorsett, P. Psychosocial Care Provision for Terminally Ill Clients in Rural Australian Communities: the Role of Social Work. Rural Remote Health (2019) 19(3):5285. doi:10.22605/RRH5285
86. Kirby, S, Barlow, V, Saurman, E, Lyle, D, Passey, M, and Currow, D. Are Rural and Remote Patients, Families and Caregivers Needs in Life-Limiting Illness Different from Those of Urban Dwellers? A Narrative Synthesis of the Evidence. Aust J Rural Health (2016) 24(5):289–99. doi:10.1111/ajr.12312
87. Leonard, R, Horsfall, D, Rosenberg, J, and Noonan, K. Carer Experience of End-Of-Life Service Provision: a Social Network Analysis. BMJ Support Palliat Care (2020) 10(2):e20. doi:10.1136/bmjspcare-2017-001344
88. Mounsey, L, Ferres, M, and Eastman, P. Palliative Care for the Patient without Cancer. Aust J Gen Pract (2018) 47(11):765–9. doi:10.31128/AJGP-07-18-4625
89. Politis, J, Eastman, P, Le, B, Furler, J, Irving, L, and Smallwood, N. Managing Severe Chronic Breathlessness in Chronic Obstructive Pulmonary Disease Is Challenging for General Practitioners. Am J Hosp Palliat Care (2020) 38:472–9. doi:10.1177/1049909120959061
90. Poulos, RG, Harkin, D, Poulos, CJ, Cole, A, and MacLeod, R. Can Specially Trained Community Care Workers Effectively Support Patients and Their Families in the home Setting at the End of Life? Health Soc Care Community (2018) 26(2):e270–9. doi:10.1111/hsc.12515
91. Rainsford, S, Phillips, CB, Glasgow, NJ, MacLeod, RD, and Wiles, RB. The 'safe Death': An Ethnographic Study Exploring the Perspectives of Rural Palliative Care Patients and Family Caregivers. Palliat Med (2018) 32(10):1575–83. doi:10.1177/0269216318800613
92. Reed, FM, Fitzgerald, L, and Bish, MR. District nurse advocacy for choice to live and die at home in rural Australia: a scoping study. Nurs Ethics (2015) 22(4):479–92. doi:10.1177/0969733014538889
93. Reed, FM, Fitzgerald, L, and Bish, MR. Rural District Nursing Experiences of Successful Advocacy for Person-Centered End-Of-Life Choice. J Holist Nurs (2017) 35(2):151–64. doi:10.1177/0898010116646643
94. Reed, FM, Fitzgerald, L, and Bish, MR. A Practice Model for Rural District Nursing success in End-Of-Life Advocacy Care. Scand J Caring Sci (2018) 32(2):746–55. doi:10.1111/scs.12505
95. Rosenberg, J. Working in Multidisciplinary Teams: Understanding Gp Clinical Practice in the End of Life Care. Aust Nurs Midwifery J (2017) 25(6):39.
96. Shahid, S, Taylor, EV, Cheetham, S, Woods, JA, Aoun, SM, and Thompson, SC. Key Features of Palliative Care Service Delivery to Indigenous Peoples in Australia, New Zealand, Canada and the United States: a Comprehensive Review. BMC Palliat Care (2018) 17(1):72. doi:10.1186/s12904-018-0325-1
97. Sinclair, C, Gates, K, Evans, S, and Auret, KA. Factors Influencing Australian General Practitioners' Clinical Decisions Regarding Advance Care Planning: A Factorial Survey. J Pain Symptom Manage (2016) 51(4):718–27. doi:10.1016/j.jpainsymman.2015.11.014
98. Spelten, E, Timmis, J, Heald, S, and Duijts, SFA. Rural Palliative Care to Support Dying at home Can Be Realised; Experiences of Family Members and Nurses with a New Model of Care. Aust J Rural Health (2019) 27(4):336–43. doi:10.1111/ajr.12518
99. Thomas, HR, Deckx, L, Sieben, NA, Foster, MM, and Mitchell, GK. General Practitioners' Considerations when Deciding whether to Initiate End-Of-Life Conversations: a Qualitative Study. Fam Pract (2020) 37(4):554–60. doi:10.1093/fampra/cmz088
100. To, THM, Tait, P, Morgan, DD, Tieman, JJ, Crawford, G, Michelmore, A, et al. Case Conferencing for Palliative Care Patients - a Survey of South Australian General Practitioners. Aust J Prim Health (2017) 23(5):458–63. doi:10.1071/PY16001
Keywords: public health, workforce, palliative care, primary healthcare, general practitioners
Citation: van Gaans D, Erny-Albrecht K and Tieman J (2022) Palliative Care Within the Primary Health Care Setting in Australia: A Scoping Review. Public Health Rev 43:1604856. doi: 10.3389/phrs.2022.1604856
Received: 21 February 2022; Accepted: 19 August 2022;
Published: 06 September 2022.
Edited by:
Daniela Gonçalves-Bradley, Independent Researcher, London, United KingdomCopyright © 2022 van Gaans, Erny-Albrecht and Tieman. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
PHR is edited by the Swiss School of Public Health (SSPH+) in a partnership with the Association of Schools of Public Health of the European Region (ASPHER)+
*Correspondence: Jennifer Tieman, amVubmlmZXIudGllbWFuQGZsaW5kZXJzLmVkdS5hdQ==
 Deborah van Gaans
Deborah van Gaans Katrina Erny-Albrecht
Katrina Erny-Albrecht Jennifer Tieman
Jennifer Tieman