Abstract
Objective: Identify barriers and facilitators in access to medicines for diabetes, hypertension, and dyslipidemia, considering patient, health provider, and health system perspectives.
Methods: Scoping review based on Joanna Briggs methodology. The search considered PubMed, Cochrane Library, CINAHL, Academic Search Ultimate, Web of Science, SciELO Citation Index, and grey literature. Two researchers conducted screening and eligibility phases. Data were thematically analyzed.
Results: The review included 219 documents. Diabetes was the most studied condition; most of the evidence comes from patients and the United States. Affordability and availability of medicines were the most reported dimension and specific barrier respectively, both cross-cutting concerns. Among high- and middle-income countries, identified barriers were cost of medicines, accompaniment by professionals, long distances to facilities, and cultural aspects; cost of transportation emerges in low-income settings. Facilitators reported were financial accessibility, trained health workers, medicines closer to communities, and patients’ education.
Conclusion: Barriers and facilitators are determined by socioeconomic and cultural conditions, highlighting the role of health systems in regulatory and policy context (assuring financial coverage and free medicines); providers’ role bringing medicines closer; and patients’ health education and disease management.
Introduction
Cardiovascular diseases remain the first cause of death worldwide, representing 32% of all global deaths in 2019 [1]. Conditions such as hypertension [2], diabetes [3], and dyslipidemia [4] are among the most prevalent risk factors for their development.
The treatment of these three conditions provides a convenient entry point to control other non-communicable diseases (NCDs) [5]. They share commonalities in delivery of services and model of care (e.g., continuous monitoring, multidisciplinary treatment team, importance of diet), also share the importance of pharmacotherapy [6, 7] and achieving patient adherence to control them [8].
Equitable access to medicines for these risk factors is crucial to reduce the burden of NCD [9, 10]. For instance, providing medicines at primary care level [11] has shown as an effective approach to reduce blood-pressure-related NCDs deaths. Moreover, the universal health coverage Sustainable Development Goal requires access to safe, adequate quality, and affordable medicines [12, 13]. However, even when low-cost and generic drugs are available to treat NCDs, many patients cannot access [10].
Access to health care in general has been defined as “the opportunity to reach and obtain appropriate health care services in situations of perceived need for care” [14]. Following this framework, Koh et al. [7] frame access to medicines as the interaction of accessibility and ability (to perceive, seek, reach, pay, engage), in a process that goes from medication need to medication utilization. In long-term therapies, access to appropriate medicines affects patients’ adherence [7], which is key for successfully treating these types of conditions [15].
Access to medicines is a complex concept that includes the dimensions of availability, accessibility, accommodation, affordability, and acceptability [16, 17]. They can become barriers or facilitators, challenging the health system’s capacity, and hindering people’s ability to obtain the medication they need to maintain or improve their health [18]. Because these barriers are complex and interconnected, access to medicines should be tackled from a health system perspective, considering access constraints at different levels (individual, household and community; health service delivery; health sector; public policies cutting across sectors; and international and regional level), and both demand- and supply-side constraints [19].
Health policy would benefit from systematic information on the scope of common and specific barriers and facilitators in access to medicines for treating diabetes, hypertension, and dyslipidemia. Isolated evidence exists about barriers and facilitators faced by patients or from the perspective of health providers, but no evidence was identified that systematizes the findings [20–29]. In addition, no current or ongoing scoping or systematic reviews on the topic were identified. Considering the importance of these three conditions in the global disease burden, updated evidence that systematizes the various findings related to access to medicines to treat such conditions is essential to visualize the entire phenomenon comprehensively, to guide articulated strategies and effective health solutions.
The objective of this scoping review is to comprehensively map and summarize knowledge related to the identification of barriers and facilitators in access to medicines, worldwide, for diabetes, hypertension, and dyslipidemia, considering patient, health care provider, and health system perspectives.
Methods
The scoping review was conducted following the Joanna Briggs Institute (JBI) Guidance for conducting systematic scoping reviews [30] and reported according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) [31].
Review Question
What are the barriers and facilitators in access to medicines for the treatment of diabetes, hypertension, and dyslipidemia from the perspectives of patients, health care providers, and the health system?
Inclusion Criteria
The inclusion criteria were based on the components of the Population, Concept, and Context (PCC) method of JBI [30]. See Figure 1.
FIGURE 1
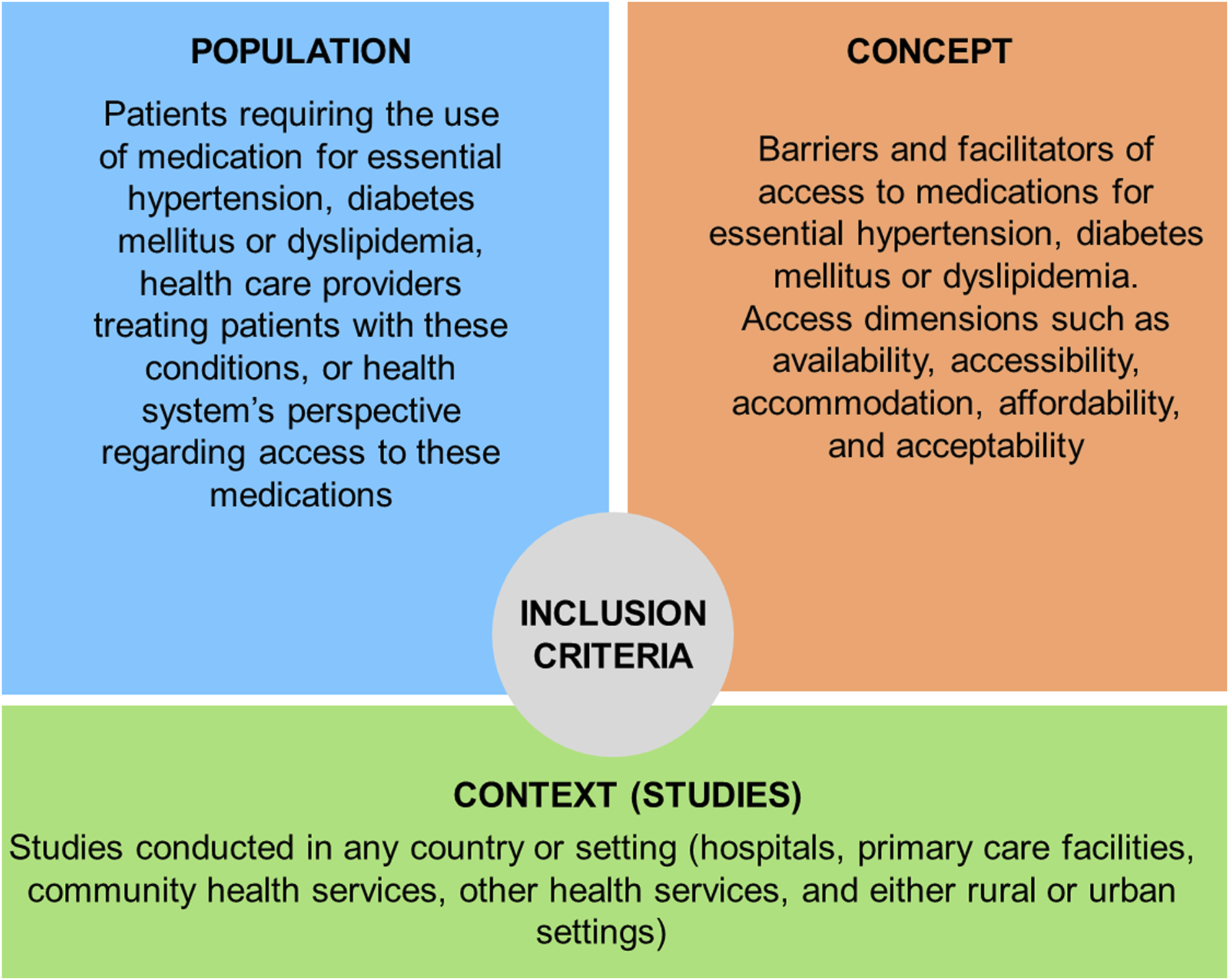
Inclusion criteria based on PCC method for scoping reviews (Chile, 2022).
Population
Focused on patients requiring medication for essential diabetes mellitus, hypertension, or dyslipidemia, health care providers treating patients with these conditions, or the health system’s perspective (health systems factors, interventions, policies, or programs) regarding access to these medications.
Concept
Barriers or facilitators to access to medicines for the treatment of essential diabetes mellitus, hypertension, or dyslipidemia were reviewed. Under the conceptual frameworks by Tanahashi [16], and Penchansky and Thomas [17], the access dimensions included were: availability, accessibility, accommodation, affordability, and acceptability. Studies related to recreational drugs and medications in animals were excluded since these topics are far from the focus of the study. Furthermore, adherence to medications was not included because patient adherence is related to disease management rather than to access to medicines.
Context
Studies conducted in any country or setting, including hospitals, primary care facilities, community health services, other health services, and either rural or urban settings.
Data Sources and Search Strategy
The following biomedical databases were consulted: PubMed (NCBI), Cochrane Library (free access by Ministry of Health, Chile), CINAHL Plus with Full Text (EBSCO), Academic Search Ultimate (EBSCO), Web of Science (Clarivate), and SciELO Citation Index (Clarivate). Grey literature was searched in the OpenGrey database and through homepages of the following international organizations: World Health Organization (WHO), Pan American Health Organization (PAHO), and the Organization for Economic Co-operation and Development (OECD). A hand search was also performed in the World Bank databases.
This review considered all types of scientific articles and grey literature (manuals, technical papers, scientific conferences reports, recommendations, reports, and policy briefs).
To identify relevant studies, an experienced biomedical librarian (AJS) and two researchers trained in public health/epidemiology (MH and OU) searched the literature based on the stages recommended by the JBI [32]. Firstly, an initial limited pilot study search was conducted in PubMed (MH and AJS) using keywords and Medical Subject Headings (MeSH) terms associated with “drugs,” “access barriers,” “access facilitators,” “diabetes,” “arterial hypertension,” “dyslipidemia,” “hypercholesterolemia,” and “metabolic syndrome.” This search strategy was conducted in the other databases, verifying the consistency of results to the research question. Secondly, the keywords identified in the relevant articles of the initial search were used to develop the complete planned search strategy (see Appendix).
A language filter was applied to exclude all studies or documents available in languages other than English, French, Portuguese, and Spanish, and only studies in humans were included. There was no restriction of publication year considered. Finally, a hand search of reference lists of relevant articles identified in the final search was conducted (Reference review or Backward citation).
The information search strategy for the full review was carried out on 27 January 2020, in the case of indexed literature, and 28 February, 12 March, and 29 April 2020, for grey literature.
Following the search, reference management software (Mendeley) was used to download and manage the reference database. Additionally, the search results were managed using Microsoft Excel, by creating separate sheets for the various stages of the search and review process.
The titles and abstracts resulting from the search (identification phase) were independently screened by two reviewers from the research team (CC-L, IM, MH-A, OU, XM, CA, CF-M, SP-L, FD-R, TR, and BP), selecting full-text articles or reports for the eligibility phase, in which the texts were reviewed by two independent reviewers. Disagreement, in any of these two phases, was resolved by consulting a third reviewer. It should be noted that five of the reviewers have extensive experience in public health research and epidemiology, as well as experience in literature reviews.
Once the titles and abstracts to be included were selected, the full text was searched and obtained through free access, requested from the head of the Biomedical Library of our University (AJS), or purchased. The entire selection process was diagrammed in a flow chart identifying each stage (identification, screening, and eligibility), the number of results and eliminations at each stage, and the reason for their exclusion.
Data Extraction
Relevant data extraction from selected studies was performed according to Peters et al. [32]. The research team piloted and executed the extraction process. The pilot allowed the researchers to test the designed matrix and adjust it according to the feedback obtained from this phase. In addition, it allowed the criteria to be standardized for the final data extraction. Once the extraction was completed, three researchers (CC-L, IM, MH-A) conducted a review of this stage, validating each of the barriers and facilitators extracted from the documents and adjusting when necessary.
Data were compiled in a single spreadsheet, containing the articles’ main characteristics, along with specific aspects of the research question of this review. Data extraction categories included: author(s), date, title, journal, volume, issue, pages, year of publication, country, aims/purpose, study population and sample size, methodology/methods, intervention type, comparison, outcomes, and key findings that relate to this scoping review question.
Analysis and Presentation of Results
Data from the selected studies and documents were synthesized by three researchers (CC-L, IM, MH-A) through an iterative process, according to the research question.
To summarize the data, descriptive statistics were calculated on the general aspects of the documents and on the barriers and facilitators identified. Also, a qualitative description and an analysis of these barriers and facilitators was included. Finally, the data characterization enabled gaps in knowledge to be identified [33].
Results
Overview
The search identified 1,844 studies, from which 219 records were finally included in the scoping review (198 indexed literature and 30 grey literature) (Figure 2).
FIGURE 2
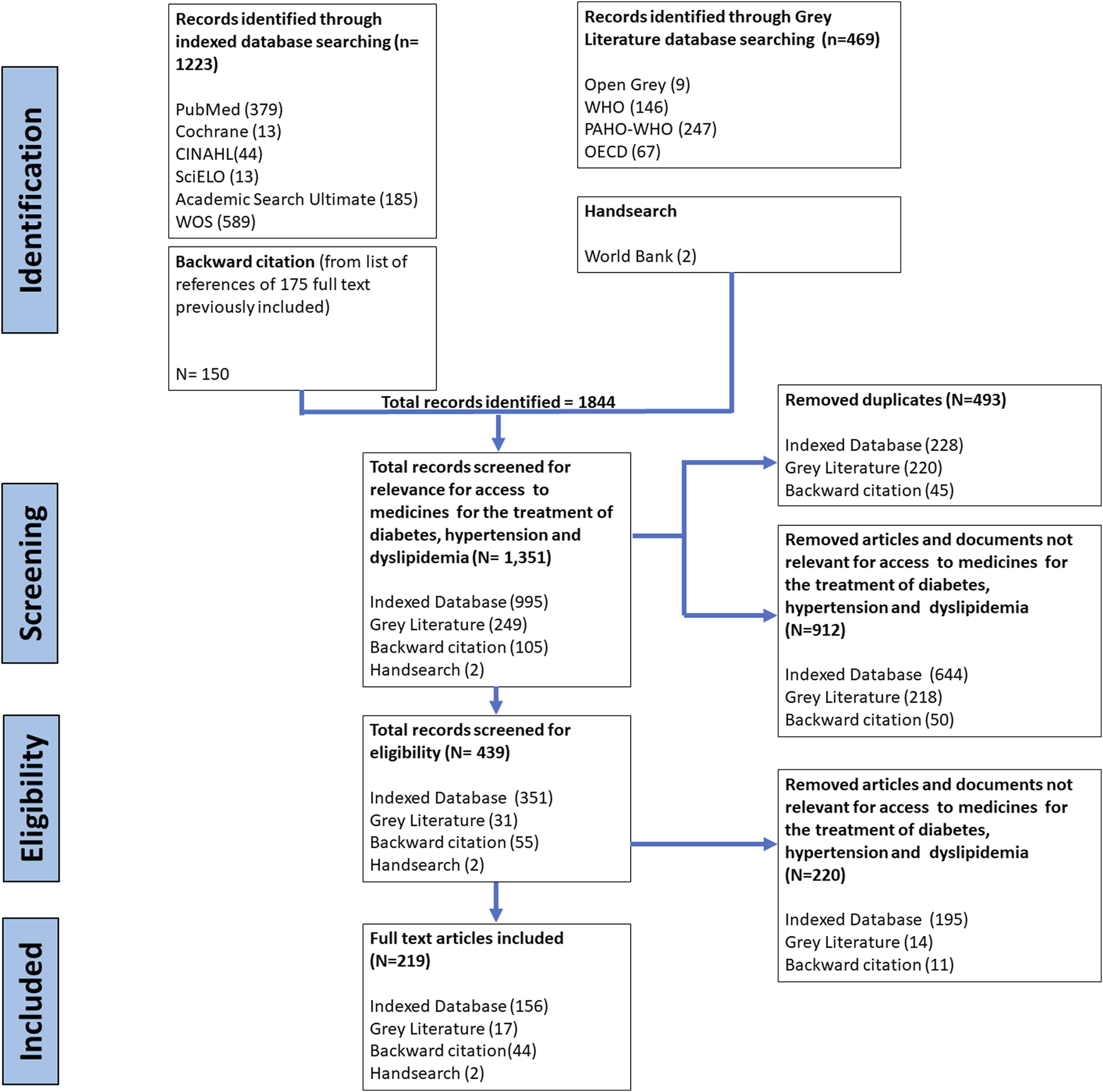
Flow chart of study selection for scoping review process (Chile, 2022). WOS, Web of Science; WHO, World Health Organization; PAHO, Pan American Health Organization; OECD, Organization for Economic Co-operation and Development.
Of the total publications with a study design (189 indexed literature, 1 grey literature), 32.1% were cross-sectional (n = 61), qualitative (n = 47, 24.7%), “report, review or discussion article” (16.3%, n = 31), cohort (6.3%, n = 12), mixed method (5.8%, n = 11) and literature review (4.7%, n = 9) (Table 1). Nine of the 30 selected grey literature documents (30%) were country reports, while eight and six were technical and regional reports respectively (26.7% and 20%), and the remaining documents were policy report, recommendations (10%, n = 3), and a PhD thesis (3.3%, n = 1).
TABLE 1
| Characteristics of included documents (n = 219) | ||
|---|---|---|
| Characteristic | n | % |
| Publication year | ||
| <2000 | 2 | 0.9 |
| 2000–2004 | 12 | 5.5 |
| 2005–2009 | 45 | 20.5 |
| 2010–2014 | 61 | 27.8 |
| 2015–2020 | 99 | 45.2 |
| Publication type | ||
| Indexed database | 189 | 86.3 |
| Grey literature | 30 | 13.6 |
| Country report | 9 | 30.0 |
| Technical report | 8 | 26.7 |
| Regional report | 6 | 20.0 |
| Policy report | 3 | 10.0 |
| Recommendation | 3 | 10.0 |
| PhD thesis | 1 | 3.3 |
| Study design (n = 190) | ||
| Cross sectional | 61 | 32.1 |
| Qualitative study | 47 | 24.7 |
| Report, review or discussion article | 31 | 16.3 |
| Cohort study | 12 | 6.3 |
| Mixed method | 11 | 5.8 |
| Literature review | 9 | 4.7 |
| Othera | 5 | 2.6 |
| Systematic literature review | 3 | 1.6 |
| Experimental design | 2 | 1.1 |
| Longitudinal and observational study | 2 | 1.1 |
| Systematic literature review and meta- analysis | 2 | 1.1 |
| Cohort and cross sectional | 1 | 0.5 |
| Quasi-experimental design | 1 | 0.5 |
| Experimental design (rationale and design) | 1 | 0.5 |
| Prospective study with survey | 1 | 0.5 |
| Qualitative study (multi-method) | 1 | 0.5 |
| Study population | ||
| Patients | 97 | 44.3 |
| Patients and Health providers | 34 | 15.5 |
| Patients, Health providers, Health system | 32 | 14.6 |
| Health system | 25 | 11.4 |
| Health providers | 16 | 7.3 |
| Health providers and Health system | 7 | 3.2 |
| Studied diseases | ||
| Diabetes | 105 | 47.95 |
| Diabetes and hypertension | 48 | 21.92 |
| Hypertension | 39 | 17.8 |
| Diabetes, hypertension, dyslipidemia | 19 | 8.67 |
| Dyslipidemia | 6 | 2.73 |
| Non-communicable diseases | 2 | 0.91 |
Summary of characteristics of the reviewed documents (Chile, 2022).
Participants
Based on the PCC model, the target populations of the 219 publications were: 44.3% patients only, 15.5% patients and health care providers, 14.6% patients, providers and the health care system, 11.4% only health system, 7.3% only health care providers, 3.2% health system and providers together. Regarding the conditions studied, of 219 results, 78.5% addressed diabetes, 48.4% hypertension and 11.4% dyslipidemia (Table 1).
Context
The studied countries classified by income and region respectively, according to the World Bank classification [34], are presented in Supplementary Tables S2, S3. Out of the 219 publications, 68% could be classified by income: 38% (n = 84) in the context of high-income countries (HIC), 13% (n = 29) in upper middle-income economies (UMIC), 14% in lower middle-income (LMIC), and 2% low-income (LIC). The most studied region was North America (31.5%) with 69 publications, of which the United States (US) had 60 and Canada nine records. Representing Latin America and the Caribbean (6.8%, n = 15), Brazil leads with six (2.7%) documents.
The first publication identified was an article from 1986, while the year with the highest number of publications was 2018 (n = 24) (Table 1).
Concept: Barriers and Facilitators in Access to Diabetes, Hypertension, and Dyslipidemia Medicines
The classification of barriers and facilitators presented below emerges from the in-depth review of the texts and the findings found in the review; and is based on the theoretical models of Tanahashi [16], and Penchansky and Thomas [17].
Of the 219 documents included in the review, reported barriers were identified in: affordability (79.5%, n = 174), availability (44.7%, n = 98), acceptability (44.3%, n = 97), accommodation (25.6%, n = 56), and accessibility (18.7%, n = 41). Facilitators were identified in: affordability (37%, n = 81), acceptability (21.9%, n = 48), availability (18.3%, n = 40), accommodation (8.7%, n = 19), and geographical accessibility (4.6%, n = 10). Details of sub-dimensions are found in Figure 3.
FIGURE 3
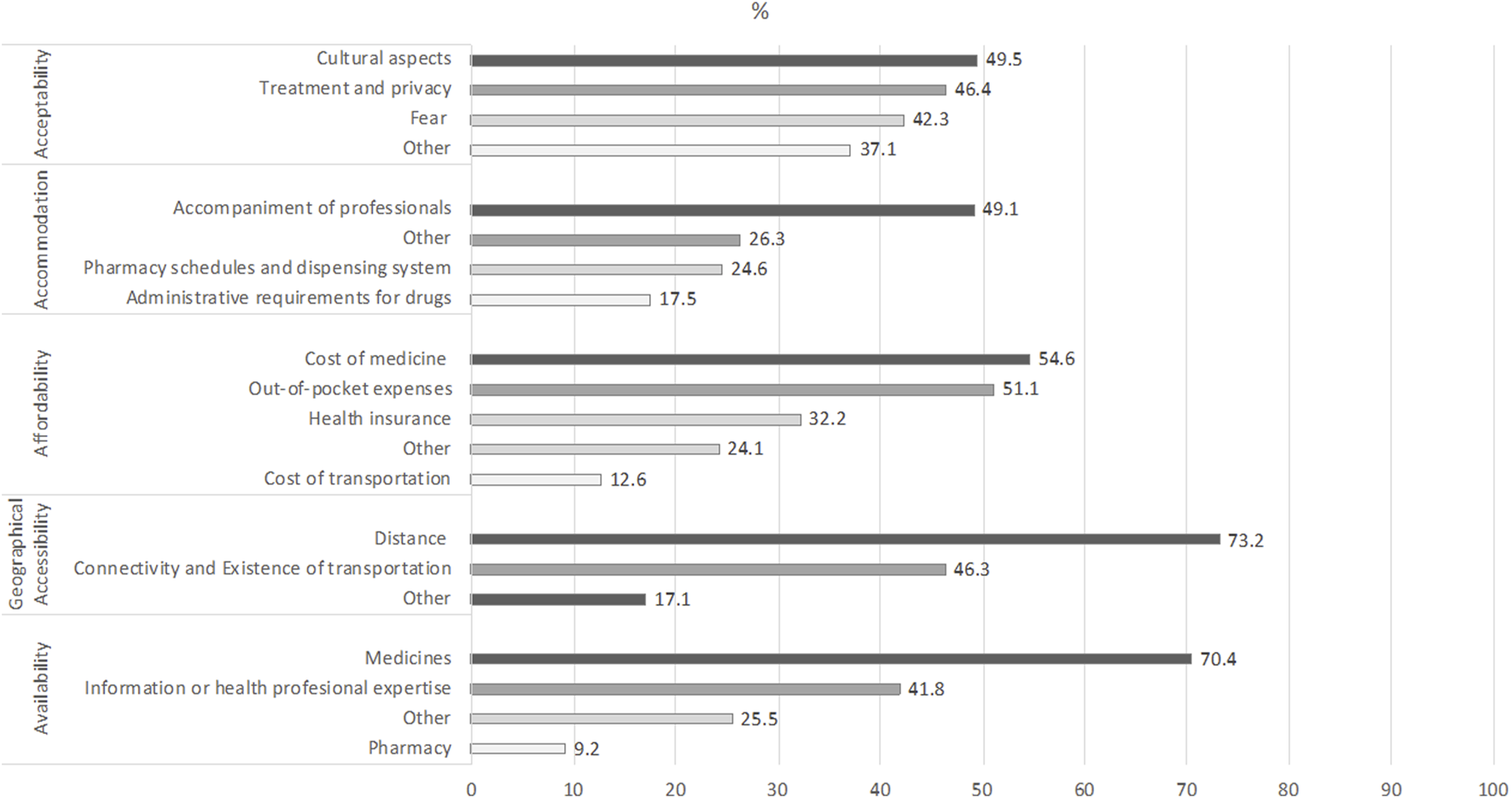
Barriers by sub-dimensions (Chile, 2022). Source: based on [4, 7, 9, 15, 16, 22–24, 26, 27, 35–245].
Following, the dimensions and their corresponding subdimensions are characterized and defined. Also, Table 2 presents a complementary analysis regarding the settings in which these barriers and facilitators were reported.
TABLE 2
| Dimension | Barrier/facilitators | Setting |
|---|---|---|
| Availability | Medicine | There are no major differences according to income in the countries studied. However, barriers stand out in vulnerable contexts such as rural health facilities, remote villages, in public health facilities, in poor urban areas and in poor communities |
| Pharmacy | These barriers predominate in UMIC and LMIC (n = 5), one was identified in a LIC (Rwanda), and the other three were worldwide | |
| Information or health professional expertise | Most of these barriers were identified in UMIC and LMIC (n = 16); followed by HIC (n = 11), especially in the United States (n = 8) and finally LIC (n = 2), Rwanda and Uganda | |
| Other | These barriers were identified mainly in UMIC and LMIC (n = 9); one in HIC and in LIC (United States and Uganda, respectively) | |
| Facilitators | Facilitators were identified most in UMIC and LMIC (n = 10), followed by HIC (n = 4), mostly in the United States (n = 3), and one in LIC (Uganda). At all income levels of the countries, training of health professionals, and free and easy access to medicines are relevant. At the global level, the strengthening of national policies, regulation, registration of generics and the drug market are recognized as facilitators | |
| Geographical accessibility | Distance | Most of these barriers were identified in UMIC and LMIC (n = 11), followed by HIC (n = 6), especially in the United States (n = 3) |
| Connectivity and existence of transportation | Most of these barriers were identified in UMIC and LMIC (n = 8), followed by HIC (n = 4) and finally LIC (n = 1) | |
| Other | This was found in HIC such as Singapore, United States and Australia (n = 3), followed by UMIC and LMIC (n = 2) such as Nepal and South Africa | |
| Facilitators | Facilitators were identified mainly in HIC (n = 5), especially in the United States (n = 4), followed by UMIC and LMIC (n = 2), India and South Africa. All recognized as facilitators the need for transportation and pharmacies close to the communities (less than 30 min); however, HIC also identified the use of mail order pharmacies | |
| Affordability | Cost of medicines | Although most of the studies are from HIC, and specially the United States (n = 25), there is evidence for the cost of medicines as a barrier from LMIC, such as India (n = 7) and from UMIC, such as China (n = 3) |
| Out-of-pocket expenditure | Having to pay for medications is a cross-cutting concern. Although it has been more studied in the context of HIC (19 documents just from the United States), it is also possible to find studies from LMIC, mainly from the north and Sub-Saharan region [e.g., Kenya (n = 4); Nigeria (n = 3), Ghana (n = 3)], and from UMIC, such as Brazil (n = 4) | |
| Cost of transportation | In this case, most of evidence comes from Sub-Saharan Africa (e.g., Kenya, n = 3) and South Asia (e.g., India, n = 3) | |
| Lack of financial coverage by the health system or private health insurance | Most of the studies coming from HIC, especially from the United States (n = 20) | |
| Other | Most of the studies from the United States (n = 15) | |
| Facilitators | While most of the studies are from HIC (e.g., United States, n = 15) mentioning medication assistance programs or Medicare Part D, there is a growing interest in programs such as “Health has no Price,” in Brazil (n = 3) | |
| Accommodation | Pharmacy hours and dispensing system | Although two of the studies regarding dispensing system are from the United States, the rest are from LMIC from the Sub-Saharan Africa (Kenya, Nigeria), and UMIC from Latin America (Brazil, Colombia) |
| Administrative requirements | All the studies that mentioned administrative requirements as a barrier are from HIC (n = 10), with six of them being from the United States (paperwork) | |
| Accompaniment | In this case all the studies are from HIC (n = 12), nine of them from the United States | |
| Other | Four studies form HIC, four from LMIC (all from South Asia) and three from UMIC [South Africa (n = 2) and Malaysia (n = 1)] | |
| Facilitators | Among evidence from high-income countries, five studies from the US present facilitators such as prescribing clinicians that considers patients’ preferences, translation services, services targeted to specific minority populations, while three studies from Canada mentioned the availability of advice over the phone (or by email), up to date staff, staff that provides support beyond the technical expertise, and interprofessional collaboration | |
| Acceptability | Cultural aspects | This type of barrier is mainly mentioned in HIC (n = 25), particularly in the United States (n = 21) where language barriers, and ethnic and racial disparities predominate. In UMIC (two studies in Malaysia and two in South Africa) and LMIC (four studies in: India, Bangladesh, Tunisia, and Tanzania), the use of alternative medicines instead of traditional ones is observed |
| Fear | Most of the studies mentioning this barrier come from HIC (n = 20), mainly the United States (n = 19), but the same fears are also identified in UMIC (n = 4), in LMIC (n = 4) and worldwide (n = 13) | |
| Treatment and privacy | Considerations on the quantity and way of taking medications appear in studies from HIC (n = 19), UMIC (n = 5) and LMIC (n = 7) | |
| Evidence regarding lack of trust and dissatisfaction with the treatment, as well as the perception of a lower quality of care in public services compared to private ones comes mainly from HIC | ||
| Other | These types of barriers are observed in countries with different income levels; however, most of the studies come from HIC (n = 17) | |
| Facilitators | Although most studies mentioning facilitators come from HIC (n = 19), the use of modern devices, such as insulin pens, or the combination of drugs that decrease intake are also identified in UMIC (n = 5) and LMIC (n = 9). In particular, bilingual care is highlighted in the United States | |
| Other | Other barriers | Most of the studies that mention these barriers are from HIC (n = 5) or include countries from different socioeconomic levels (n = 5) |
| Other facilitators | They are mentioned only in three studies (one in the United States and two worldwide) |
Dimensions, barriers and facilitators settings (Chile, 2022).
Availability
This dimension considers different aspects related to the physical existence of medications and health professional expertise. It was classified into four areas: 1) medicine, refers to the physical availability of medicines [4, 9, 21, 22, 35–99]. 2) Pharmacy, refers to the availability of medication dispensing establishments [35, 46, 54, 61, 62, 65, 94, 99, 100]. 3) Information or health professional expertise, understood, on one hand, as the information or training that professionals have about the disease and its treatment, which is materialized in the prescription of the medication needed [9, 21, 35, 40, 42, 65, 73, 81, 86, 90, 93, 96, 100–116], as well as the availability of professionals who issue the prescription [22, 35, 36, 41, 45, 51, 61, 72–74, 91, 107, 117–119]. 4) Other, considers regulatory, legal and market aspects, patents, regulatory and drug registration processes [4, 44, 57, 65, 73, 86, 120–125]. This last category also includes aspects related to the availability of supplies for the administration of medications (syringes, needles, or reagent strips); the availability of tests or glucometers [9, 15, 35, 46, 56, 91, 101, 102, 112, 126, 127]; and finally, sub diagnoses [99] and drug transport mechanisms [38, 46].
Facilitators in this dimension are related to the political and health system level, and include national regulations for medication purchasing, the definition of an essential list of medicines, evidence-based national strategies for control of chronic diseases, national drug policies, and the strengthening of health information systems, which make it possible to link health risks with the availability of drugs, efficient procurement, increased national supply of generic drugs, and distribution systems for pharmaceuticals and regular monitoring of medicine stocks [4, 9, 39, 44, 55, 56, 63, 65, 72, 73, 77, 80, 99, 102, 123, 124, 128–130]. Other aspects that facilitate availability are providing education, competencies, and training to health professionals [22, 35, 86, 102, 107, 111, 131–134]; easily-accessible medication dispensing facilities (people’s pharmacies, medicine delivered to home, mobile pharmacies in rural settings) [36, 43, 94, 99, 113, 134–136], and integrated health care programs, which optimize the resources allocated for private health care, to benefit other programs [122, 137]. Finally, medical innovation provides more individualized treatment options and treatments adapted to patients [51, 93, 95, 138].
Geographical Accessibility
This relates to geographical distance between medicines and the location of users who need them. Three areas were considered: 1) distance, refers to the physical distance that people must travel to obtain the medication they need [4, 7, 9, 35–37, 42, 45, 47, 50, 56, 64, 65, 69, 73, 76, 81, 86, 87, 91, 110, 122, 139–146]. 2) Connectivity and existence of transportation, related to the quality of roads, routes and difficulties related to inclement weather, presence of rivers, jungle areas or areas under socio-political conflict or occupation [35, 42, 61, 65, 67, 122]; furthermore, in this area, the presence of sufficient means of transportation and stops that cover the areas where people reside are considered [38, 45, 46, 56, 69, 93, 110, 112, 135, 139, 142, 146, 147]. 3) Other, considers age and physical disabilities as barriers to transportation [7, 43, 68, 117, 135, 140, 148, 149].
Facilitators identified in this dimension are related to the positive perception of the geographic accessibility of a public health facility, proximity to public and private health facilities, transportation availability, urban location of the household [9, 38, 69, 142, 146, 150, 151], services such as mobile pharmacy in rural settings, mail-order pharmacy and transportation assistance for patients (e.g., access to a vehicle, public transit discounts or medical transportation services) [99, 146, 151, 152].
Affordability
Is the relationship between price of medicines and the ability of patients to pay. This dimension was divided into five areas: 1) costs of medicines, in which the high price of medicines represents a barrier to access [9, 15, 21–23, 25, 35, 36, 43, 44, 47, 50–52, 54, 56, 58, 59, 62, 65, 66, 69, 73, 75, 77, 78, 82, 84, 86, 88, 92, 94, 95, 97, 99, 100, 107–109, 111, 112, 116, 121, 122, 124, 126, 128, 140, 142, 145, 147, 153–187], implying the postponement of the treatment initiation, interruption/discontinuity, the use of lower doses or only a part of the prescribed medicines [47, 74, 89, 113, 133, 150, 188–191]. 2) Out-of-pocket expenditure, understood as the direct payment for the medicines [4, 9, 21, 37, 41, 42, 44–46, 49, 51, 63, 65, 67, 68, 70, 71, 79, 86–88, 91, 93, 94, 100, 106, 109, 115, 117, 119, 120, 124, 129, 131, 136, 141, 142, 144, 147, 161, 163, 169, 192–203], which is associated with the ability of households to pay for those medicines; therefore, a lack of money is relevant in this context [43, 60, 69, 96, 146, 172, 186, 204–207], especially considering that paying for medicine can lead households to borrow, sell assets, disregard needs, or even fall into poverty [56, 61, 72, 138, 139, 189, 208, 209]. This goes beyond the price of the medicines or the financial coverage, since even low-cost medicines or a lack of full coverage for very expensive medicines could represent a significant proportion of the expenditure for low-income households, with medicines accounting for a considerable proportion of total health expenditure, both at the household and aggregate levels [7, 35, 47, 50, 53, 55, 62, 73, 99, 121, 122, 128, 157, 162, 168, 210]. 3) Cost of transportation, which considers the cost people must incur to travel to the place where they pick up or purchase their medicine; related to the cost of public or private transportation, and the frequency with which they must assume this cost [22, 25, 35, 36, 38, 42, 43, 47, 48, 50, 56, 62, 65, 72, 88, 96, 112, 122, 135, 144–146]. 4) Lack of financial coverage by the health system or private health insurance, which implies that the person must cover the full cost of the required medicines [7, 9, 15, 22, 25, 26, 35, 42, 43, 54, 57, 62, 64, 65, 69, 72, 81, 86, 99, 117, 119–122, 134, 136, 139, 141, 143–145, 157, 158, 160, 161, 164, 166–169, 172, 180, 186, 189, 199, 205, 209–218]. 5) Other considers: cost of elements required for administering the prescribed medicine (e.g., glucometers, strips, syringes) [56, 63, 74, 93, 127, 132, 219], lack of drug price regulation policies and inefficient purchasing by the public sector [35, 66, 97, 99, 112, 128], cost of consultation or check-up with doctors and specialists [86, 91, 113, 171, 191, 213], cost of travel time [36, 96], sociodemographic characteristics that make it more difficult to afford medications (socioeconomic status, unemployment, age, disability, ethnicity, food insecurity) [65, 115, 122, 133, 135, 140, 172, 180, 186, 195, 202, 212], among others [9, 58, 105, 121, 149, 166, 218, 220, 221].
Regarding facilitators, the following were identified: the provision of free-of-charge medicine and health insurance coverage for pharmaceuticals [7, 21, 35–37, 43, 45–47, 49, 50, 60, 66, 69, 72, 73, 75, 87, 97, 107, 112, 117, 119, 134, 139, 140, 142, 150, 154, 158, 161, 164, 177, 180, 181, 186, 191, 194, 201, 202, 204, 205, 208, 209, 222–225]; health policies such as efficiency in government procurement, price regulation, financial coverage of essential medicines, promoting the use of generic, reducing import duties and promoting local production [4, 44, 55, 56, 58, 59, 65, 99, 120, 122, 124, 137, 157, 162, 189]; global or regional initiatives such as the HEARTS Initiative, the Strategic Fund, WHO’s Model list of essential medicines [9, 65, 123, 129, 149]; among others [22, 71, 74, 82, 95, 96, 113, 121, 144, 169, 175, 188, 207, 226].
Accommodation
This refers to the relationship between how resources for delivering medicines to users are assigned and the users’ capability to adapt to these factors. It was divided into four areas: 1) pharmacy hours and dispensing system, considers scheduling issues (e.g., due to shortages or only 1 day per month) [46, 87], inconvenient operating hours (for instance, needing to depend on others or missing working time) [42, 48, 93, 139, 191, 227], inefficient dispensing processes (e.g., monthly prescribing instead of considering longer periods) [42, 110], and long wait times to collect the medicines [60, 71, 93, 191, 227]. 2) Administrative requirements, includes excessive paperwork needed for prescribing certain drugs (newer or more expensive) [110, 166, 215], confusion about how the system works [147], bureaucratic process for obtaining drugs or applying for coverage programs [79, 110, 228], among others [165, 229]. 3) Accompaniment area, considers the lack of support and communication from professionals towards to patients in their treatments [81, 91, 98, 102, 104, 113, 139, 159, 180, 187, 202, 206, 230], very short consultations (excessive workload, lack of adequate time to educate, answer questions, adjust doses, discuss possible adverse effects and the risks of not controlling their condition, inadequate counseling or lack thereof) [22, 40, 42, 74, 86, 103, 127, 159, 187, 202, 231, 232], clinical inertia (follow-up and treatment adjustment) [103, 159], lack of alignment in the prescribing behavior at the same center [102], lack of communication between health staff members (ambiguity regarding responsibilities, no team approach to care) [40, 145, 159], lack of concern by physicians about the cost of treatment [189], negative attitude or mistreatment by staff [71, 139], lack of continuity with the same health care professional [40, 213], and infrequent follow-up/monitoring [42, 127, 133, 179, 206]. 4) Other considers: inadequate staff incentives and training [35, 102, 133, 145], inadequate logistic systems [39], incorrect prescriptions or dispensing [128], legibility of prescriptions [43], inadequate infrastructure [101, 139, 233], long wait times to see the doctor [233], lack of coordination between different providers (e.g., public and private) [37, 145], lack of active community outreach for chronic patients [36, 159], inadequate information technologies (e.g., poor record-keeping) [145, 159], lack of recognition of circular migration [38], and different prescribing behavior of professionals depending on the size of the facility [221].
Among facilitators identified are: the development of multidisciplinary teams [103, 234], mentorship programs for primary care physicians [103], the expansion of nurse prescriber or manager role [22, 81, 103] (like in Vietnam), physicians effectively communicating their knowledge and addressing patient preferences for information [7, 84, 131, 156], patients directed to mail-order pharmacy services [150], community outreach [150], support programs (e.g., over the phone, by email, through disease associations) or medication counseling [35, 112, 131, 150], periodic reevaluation of medication efficacy for patients [218], diverse health care professionals that accommodate patients’ cultural and language background [150, 177], offering community venues to decongest clinics [135] and combining medicine collection with other appointments [38] (like in South Africa), exceptions on the restrictions to treatment duration or dispensing quantities for chronic diseases [35], reorganizing patients flow to facilitate dispensing [35], targeting specific minority populations [199], simplified and harmonized, online prior authorization process [215], logistic improvements [86], and extending clinic hours [42].
Acceptability
This refers to the degree to which population or specific social groups accept medicines and the factors that increase or decrease the likelihood of their use. This depends both on the attitudes of users towards the characteristics of providers and medicines, as well as on the attitudes of providers towards the characteristics of users. It was divided into four areas: 1) cultural aspects, such as preference for alternative medicines [25, 40, 42, 45, 86, 91, 102, 141, 147, 184, 227], social stigma, sense of failure and psychological resistance to insulin [54, 76, 102, 103, 108, 110, 114, 132, 133, 175, 183, 191, 228, 231, 235–239], language barriers [40, 118, 139, 150, 188, 196, 199, 206], and barriers associated with certain ethnic groups, low socioeconomic level and female gender, among others [9, 26, 118, 139, 140, 142, 150, 156, 171, 180, 200, 218, 240–242], and religious beliefs related to concerns about the purity of insulin [102]. 2) Fear, mainly of the use of injectable insulin (fear of needles), side effects of medications, weight gain and hypoglycemia [4, 15, 25, 40, 54, 68, 74, 84, 89, 98, 102–104, 108, 111, 114, 127, 132, 133, 150, 159, 160, 170, 175, 179, 183, 190, 191, 193, 200, 225, 230, 231, 235–239, 243–245], this fear faced by patients is also reported from the health care providers perspective [40, 103, 104, 114, 231, 238]. 3) Treatment and privacy such as the perception of over-prescription, distrust of patients regarding the correctness of the treatment, its complexity and effectiveness, preference for the use of oral medication and skepticism regarding generic drugs [15, 22, 43, 54, 68, 88, 89, 99, 103, 106, 108, 158, 159, 163, 179, 183, 190, 203, 206, 231, 235, 236, 239, 244, 245]. Furthermore, there is evidence of a lack of trust and dissatisfaction with the treatment provided by health care providers, as well as the perception of a lower quality of care in public services compared to private ones [7, 36, 69, 81, 85, 106, 109, 122, 140, 147, 156, 244]. Health care providers also have negative attitudes towards certain treatments and doubt the efficacy of certain medications and are distrustful of the compliance of patients with treatment [22, 51, 54, 101, 102, 118, 132, 155, 159, 193, 239]. 4) Other includes lack of knowledge of the disease, illiteracy and low schooling, which affects the understanding of the disease and the need for medication by patients and their families [4, 7, 25, 40, 42, 51, 56, 65, 69, 75, 81, 98, 118, 141, 159, 177, 180, 187, 191, 202, 206, 235]. In this area, the barriers are observed in the denial of the diagnosis [158, 159], the idea that medication is only necessary if the patient is symptomatic [36, 82, 179], and other misconceptions about the disease and its control [46, 61, 68, 84, 91, 106, 110, 180, 218, 236, 237].
Concerning the aspects that facilitate acceptability, one of the most reported refers to educating patients, the community, and schools about the pathologies through structured educational programs, innovative materials, and sustained campaigns [35, 41, 45, 74, 75, 91, 102, 103, 113, 130, 132, 133, 159, 179, 231, 232, 245]. Another relevant aspect is to consider the cultural context of the people and to use an integral approach centered on the patients, based on knowledge, and oriented to the improvement of the patients’ quality of life [63, 65, 85–87, 98, 124, 131, 150, 158, 179, 199, 231, 235, 238, 245]. Concerning this, bilingual health personnel are valued by patients [25, 69, 188, 199]. On the other hand, social and family support also emerges as a facilitator [45, 177], as well as trust in medications and healthcare personnel [7, 154], and some personal, clinical and social background of the patients [69, 141, 179, 208, 232]. Finally, facilitators related to the type of drug and its application include the use of analogs, flexible doses, pen devices, or inhalable insulin (for children and adolescents), as well as the combination of medications in the same drug [9, 35, 74, 99, 103, 132, 133, 160, 163, 174, 175, 231, 237–239]. Moreover, the importance of regulating the information and the marketing of medicines [35], and of focusing messages on the equivalence between brand name products and generics, when the quality of generic medicines is assured [99], are underlined.
Others
Other barriers that could not be included in the previous dimensions are mainly related to the socioeconomic context of the countries and populations, such as LIC, LMIC and UMIC [35, 55, 63, 109, 120] or poverty [109, 118, 120, 173]. Personal factors such as comorbidities [145], mental health problems [118, 145], disability [118], younger age [26, 140], and lack of time [228] are also included here.
Other facilitators included living in a HIC [55], improved social determinants of health [199], and using disaggregated data for vulnerable groups [35].
Discussion
Lack of access to medicines for chronic conditions, as the three studied in this review, continues to be a struggle for a significant part of the population worldwide. The present review identified 219 documents that discussed this issue in at least one of its dimensions.
The findings suggest that there are recurrent circumstances that hinder people with the studied conditions, to access their medicines. When analyzing the barriers according to the main dimensions, affordability is the most reported and it is present in all settings described. The most reported barriers were availability of medicines, which is a cross-cutting concern, and long distances to facilities, costs of medicines, accompaniment of professionals, and cultural aspects, most present in HIC, UMIC and LMIC.
Although socioeconomic disparities in access to medicines are present worldwide, especially in vulnerable populations, barriers identified in HIC are mostly related to the health system capacity to cover medicines, which, when segmented, generates, and maintains access gaps in the most vulnerable populations. Also, it seems to be an implicit hierarchical order among the barriers depending on socioeconomic status, were availability and affordability are the first two barriers to overcome, and then the other barriers start to play a role. This can be seen regarding accommodation and acceptability (apart from cultural barriers), that does not emerge as an issue in LIC, as seems to be in HIC.
The results show that the relevance of the barriers is determined by the socioeconomic and cultural conditions in which people live. This finding highlights the importance of the role of health systems in the regulatory and policy context, focusing to meet the needs of their population, and assuring financial coverage and access to free medicines when possible. On the other hand, providers can facilitate access through training their health workers, implementing multidisciplinary approach, bringing medicines closer to the people, having more flexible schedules, and having intercultural translators. At the patient level, health education and disease management are crucial.
Based on the results, three major gaps were identified. First, related to the studied conditions, diabetes was undisputedly the most studied; probably due to the need for positioning new forms of insulin administration [114, 160, 174, 175, 237]. Secondly, regarding the target population, most of the evidence is based on patients rather than providers and health systems. Finally, most of the evidence is from the US, with few specific studies from Latin America, Asia or Africa. This should be considered, as there may be underestimated barriers and facilitators related to the other two pathologies, settings, and actors involved.
The strengths of this study are related, on one hand, to its design, since as a scoping review, different types of barriers and facilitators from various perspectives are systematized, allowing for a broad understanding of the phenomenon. A second strength is the rigor of the methodology based on JBI and PRISMA standards.
However, a limitation of the study is that since reviewing the quality of the evidence is optional in this type of study, low-quality studies that report barriers or facilitators would not be identified. Moreover, as the findings originate from published studies and documents, other characteristics, barriers, and facilitators may exist that are not studied for not being published.
The Tanahasi [16], and Penchansky and Thomas [17] models identify a population that encounters health services and another that remains outside the system. For instance, during the review process, only two articles on diabetic homeless were identified [81, 202]. Future research should consider some groups who are excluded from health services, and who may face different barriers than those identified for the individuals who access them.
Statements
Author contributions
Conceptualization: CC-L, IM, and MH-A; Search: MH-A, AJ, and OU; Protocol: CC-L, MH-A, IM, AJ, OU, XM, and CA; Review, selection and extraction: CC-L, MH-A, IM, OU, XM, CA, CF-M, SP-L, FD-R, TR, and BP; Original manuscript: CC-L, MH-A, IM, AJ, OU, XM, CA, CF-M, SP-L, FD-R, TR, and BP. All authors approved the submitted manuscript.
Funding
The study was developed in the context of Project FONIS SA19|0174, financed by the Fondo Nacional de Investigación y Desarrollo en Salud (FONIS), Agencia Nacional de Investigación y Desarrollo (ANID), Chile.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/phrs.2022.1604796/full#supplementary-material
References
1.
World Health Organization. Cardiovascular diseases (CVDs) [internet] (2021). Available from: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds.) (Accessed June 5, 2022).
2.
World Health Organization. Hypertension - key facts [internet] (2019). Available from: https://www.who.int/news-room/fact-sheets/detail/hypertension (Accessed September 9, 2020).
3.
World Health Organization. Global report on diabetes [Internet] (2016). Available from: http://www.who.int/about/licensing/copyright_form/index.html (Accessed September 9, 2020).
4.
Murphy A Faria-Neto JR Al-Rasadi K Blom D Catapano A Cuevas A et al World heart federation cholesterol roadmap. Glob Heart (2017) 12(3):179–97.e5. 10.1016/j.gheart.2017.03.002
5.
Mendis S O’Brien E Seedat YK Yusuf S . Hypertension and diabetes: Entry points for prevention and control of the global cardiovascular epidemic. Int J Hypertens (2013) 2013:878460. 10.1155/2013/878460
6.
World Health Organization . World health statistics 2020: Monitoring health for the sustainable development goals. Geneva, Switzerland: World Health Organization (2020).
7.
Koh JJK Cheng RX Yap Y Haldane V Tan YG Teo KWQ et al Access and adherence to medications for the primary and secondary prevention of atherosclerotic cardiovascular disease in Singapore: A qualitative study. Patient Prefer Adherence (2018) 12:2481–98. 10.2147/PPA.S176256
8.
Grover A Joshi A . An overview of chronic disease models: A systematic literature review. Glob J Health Sci (2015) 7(2):210–27. 10.5539/gjhs.v7n2p210
9.
Wirtz VJ Kaplan WA Kwan GF Laing RO . Access to medications for cardiovascular diseases in low- and middle-income countries. Circulation (2016) 133(21):2076–85. 10.1161/CIRCULATIONAHA.115.008722
10.
Abegunde D . Essential medicines for non-communicable diseases (NCDs) (2011). Background paper.
11.
NCD Countdown Collaborators. NCD countdown 2030: Worldwide trends in non-communicable disease mortality and progress towards sustainable development goal target 3.4. Lancet (2018) 392:1072–88. 10.1016/s0140-6736(18)31992-5
12.
United Nations. The sustainable development goals report (2019). Available from: https://unstats.un.org/sdgs/report/2019/The-Sustainable-Development-Goals-Report-2019.pdf (Accessed September 9, 2020).
13.
Beran D Pedersen HB Robertson J . Noncommunicable diseases, access to essential medicines and universal health coverage. Glob Health Action (2019) 12:1670014. 10.1080/16549716.2019.1670014
14.
Levesque JF Harris M Russell G . Patient-centred access to health care: Conceptualising access at the interface of health systems and populations. Int J Equity Health (2013) 12(18):18–9. 10.1186/1475-9276-12-18
15.
Burkhart P Sabaté E . Adherence to long-term therapies. Geneva, Switzerland: Evidence for action (2003).
16.
Tanahashi T . Health service coverage and its evaluation. Bull World Health Organ (1978) 56(2):295–303.
17.
Penchansky R Thomas JW . The concept of access: Definition and relationship to consumer satisfaction. Med Care (1981) 19(2):127–40. 10.1097/00005650-198102000-00001
18.
Marangos PJ Okamoto LJ Caro JJ . Economic burden of the components of the metabolic syndrome. In: Handbook of disease burdens and quality of life measures. New York: Springer (2010). p. 1135–49.
19.
Bigdeli M Jacobs B Tomson G Laing R Ghaffar A Dujardin B et al Access to medicines from a health system perspective. Health Policy Plan (2013) 28(7):692–704. 10.1093/heapol/czs108
20.
Raaijmakers LGM Hamers FJM Martens MK Bagchus C Vries NKD Kremers SP . Perceived facilitators and barriers in diabetes care: A qualitative study among health care professionals in The Netherlands. BMC Fam Pract (2013) 14(114). 10.1186/1471-2296-14-114
21.
Mendis S Fukino K Cameron A Laing R Anthonio F Jr Khatib O et al The availability and affordability of selected essential medicines for chronic diseases in six low- and middle-income countries. Bull World Health Organ (2007) 85(4):279–88. 10.2471/blt.06.033647
22.
Beran D Higuchi M . Delivering diabetes care in the Philippines and Vietnam: Policy and practice issues.Asia Pac J Public Health (2013) 25(1):92–101. 10.1177/1010539511412177
23.
Beran D Ewen M Lepeska M Laing R . Access to insulin: Current challenges and constraints (2017).
24.
Brunton SA Renda SM Carolina N Davis SN . Overcoming psychological barriers to insulin use in type 2 diabetes. Clin Cornerstone (2006) 8(2):s19–s26. 10.1016/s1098-3597(06)80012-8
25.
Nam S Chesla C Stotts NA Kroon L Janson SL . Barriers to diabetes management: Patient and provider factors. Diabetes Res Clin Pract (2011) 93(1):1–9. 10.1016/j.diabres.2011.02.002
26.
Huttin C . The role of different types of health insurance on access and utilization of antihypertensive drugs. An empirical study in a US hypertensive population. Dis Management Health Outcomes (2002) 10(7):419–30. 10.2165/00115677-200210070-00003
27.
Evans DB Hsu J Boerma T . Universal health coverage and universal access. Bull World Health Organ (2013) 91(8):546–A. 10.2471/blt.13.125450
28.
World Health Organization. Roadmap for access to medicines, vaccines and health product 2019-2023. Comprehensive support for access to medicines, vaccines and other health products. Geneva, Switzerland: World Health Organization (2019).
29.
World Health Organization. Towards access 2030: WHO medicines and health products programme strategic framework 2016 - 2030. Geneva, Switzerland: World Health Organization (2017).
30.
Peters MDJ Godfrey C McInerney P Munn Z Tricco AC Khalil H . Chapter 11: Scoping reviews (2020 version). In: EAromatarisZMunn, editors. JBI manual for evidence synthesis. JBI (2020). 10.46658/JBIMES-20-12
31.
Tricco AC Lillie E Zarin W O’Brien KK Colquhoun H Levac D et al PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann Intern Med (2018) 169:467–73. 10.7326/M18-0850
32.
Peters MDJ Godfrey CM Khalil H McInerney P Parker D Soares CB . Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc (2015) 13:141–6. 10.1097/XEB.0000000000000050
33.
Nyanchoka L Tudur-smith C Thu VN Iversen V Tricco AC Porcher R . A scoping review describes methods used to identify, prioritize and display gaps in health research. J Clin Epidemiol (2019) 109:99–110. 10.1016/j.jclinepi.2019.01.005
34.
World Bank. Washington, DC: World Bank Country and Lending Groups (2020). Data: World Bank Country and Lending Groups [Internet].
35.
Management Sciences for Health. MDS-3: Managing access to medicines and health technologies. Arlington, Va: Management Sciences for Health (2012).
36.
Naheed A Haldane V Jafar TH Chakma N Legido-Quigley H Grp CBS . Patient pathways and perceptions of hypertension treatment, management, and control in rural Bangladesh: A qualitative study.Patient Prefer Adherence (2018) 12:1437–49. 10.2147/PPA.S163385
37.
Lall D Engel N Devadasan N Horstman K Criel B . Models of care for chronic conditions in low/middle-income countries: A ‘best fit’ framework synthesis. BMJ Glob Health (2018) 3(6):e001077. 10.1136/bmjgh-2018-001077
38.
Magadzire BP Budden A Ward K Jeffery R Sanders D . Frontline health workers as brokers: Provider perceptions, experiences and mitigating strategies to improve access to essential medicines in South Africa. BMC Health Serv Res (2014) 14:520. 10.1186/s12913-014-0520-6
39.
Bhuvan KC Heydon S Norris P . Access to and quality use of non-communicable diseases medicines in Nepal. J Pharm Pol Pract (2015) 8(1):21. 10.1186/s40545-015-0041-7
40.
Haque M Navsa M Emerson SH Dennison CR Levitt NS . Barriers to initiating insulin therapy in patients with type 2 diabetes mellitus in public-sector primary health care centres in Cape Town. J Endocrinol Metab Diabetes South Africa (2005) 10(3):94–9. 10.1080/22201009.2005.10872127
41.
Hendriks ME Bolarinwa OA Wit FWNW Brewster LM Odusola AO Rosendaal NTA et al Feasibility and quality of cardiovascular disease prevention within a community-based health insurance program in rural Nigeria: An operational cohort study. J Hypertens (2015) 33(2):366–75. 10.1097/HJH.0000000000000401
42.
Risso-Gill I Balabanova D Majid F Ng KK Yusoff K Mustapha F et al Understanding the modifiable health systems barriers to hypertension management in Malaysia: A multi-method health systems appraisal approach. BMC Health Serv Res (2015) 15:254. 10.1186/s12913-015-0916-y
43.
Williams AF Manias E Walker R . Adherence to multiple, prescribed medications in diabetic kidney disease: A qualitative study of consumers’ and health professionals’ perspectives. Int J Nurs Stud (2008) 45(12):1742–56. 10.1016/j.ijnurstu.2008.07.002
44.
Organization for Economic Co-operation and Development. Pharmaceutical innovation and access to medicines. Berlin, Germany: OECD (2018).
45.
Metta E Haisma H Kessy F Geubbels E Hutter I Bailey A . It is the medicines that keep us alive”: Lived experiences of diabetes medication use and continuity among adults in southeastern Tanzania. BMC Health Serv Res (2015) 15:111. 10.1186/s12913-015-0768-5
46.
Araujo JLO Pereira MD de Sá Del Fiol F Barberato-Filho S . Access to antihypertensive agents in Brazil: Evaluation of the “health has No price” program. Clin Ther (2014) 36(8):1191–5. 10.1016/j.clinthera.2014.06.003
47.
Ministry of Medical ServicesMinistry of Public Health and Sanitation. Access to essential medicines in Kenya: A health facility survey (2009).
48.
Iwelunmor J Plange-Rhule J Airhihenbuwa CO Ezepue C Ogedegbe O . A narrative synthesis of the health systems factors influencing optimal hypertension control in sub-saharan Africa. PLOS ONE (2015) 10(7):e0130193. 10.1371/journal.pone.0130193
49.
Organization for Economic Co-operation and DevelopmentWorld Health Organization. Health at a Glance Asia/Pacific 2014. Measuring progress towards universal health coverage. Berlin, Germany: OECD Publishing (2014).
50.
Beran D McCabe A Yudkin JS . Access to medicines versus access to treatment: The case of type 1 diabetes. Bull World Health Organ (2008) 86(8):648–9. 10.2471/blt.07.048710
51.
Attaei MW Khatib R McKee M Lear S Dagenais G Igumbor EU et al Availability and affordability of blood pressure-lowering medicines and the effect on blood pressure control in high-income, middle-income, and low-income countries: An analysis of the PURE study data. Lancet Public Health (2017) 2(9):e411–9. 10.1016/S2468-2667(17)30141-X
52.
Su M Zhang Q Bai X Wu C Li Y Mossialos E et al Availability, cost, and prescription patterns of antihypertensive medications in primary health care in China: A nationwide cross-sectional survey. Lancet (2017) 390(10112):2559–68. 10.1016/S0140-6736(17)32476-5
53.
van Mourik MSM Cameron A Ewen M Laing RO . Availability, price and affordability of cardiovascular medicines: A comparison across 36 countries using WHO/hai data. BMC Cardiovasc Disord (2010) 10:25. 10.1186/1471-2261-10-25
54.
Khatib R . Barriers to the management of cardiovascular disease: A focus on availability and affordability of medications in 17 countries. Hamilton, Canada: McMaster University (2014).
55.
Ewen M Zweekhorst M Regeer B Laing R . Baseline assessment of WHO's target for both availability and affordability of essential medicines to treat non-communicable diseases.PLOS ONE (2017) 12(2):e0171284. 10.1371/journal.pone.0171284
56.
Volman B . Direct costs and availability of diabetes medicines in low-income and middle-income countries. Amsterdam: WHO Health Action International (2008).
57.
Armstrong-Hough M Kishore SP Byakika S Mutungi G Nunez-Smith M Schwartz JI . Disparities in availability of essential medicines to treat non-communicable diseases in Uganda: A Poisson analysis using the service availability and readiness assessment. PLOS ONE (2018) 13(2):e0192332. 10.1371/journal.pone.0192332
58.
Babar ZUD Ibrahim MIM Singh H Bukahri NI Creese A . Evaluating drug prices, availability, affordability, and price components: Implications for access to drugs in Malaysia. In: KHarvey, editor, 4 (2007). p. e82.PLOS Med3
59.
Deeb L Tan M Alberti KGMM . Insulin availability among international diabetes federation member associations. Report of the task force on insulin distribution.Diabetes Care (1994) 17(3):220–3. 10.2337/diacare.17.3.220
60.
Syed N Rockers PC Vian T Onyango M Laing RO Wirtz VJ . Access to antihypertensive medicines at the household level: A study from 8 counties of Kenya. Glob Heart (2018) 13(4):247–53.e5. e5. 10.1016/j.gheart.2018.08.001
61.
Baxter LM Eldin MS Al Mohammed A Saim M Checchi F . Access to care for non-communicable diseases in mosul, Iraq between 2014 and 2017: A rapid qualitative study. Confl Health (2018) 12(1):48. 10.1186/s13031-018-0183-8
62.
Higuchi M . Access to diabetes care and medicines in the Philippines. Asia Pac J Public Health (2010) 22(1):96S–102S. 10.1177/1010539510373005
63.
Robertson J Macé C Forte G de Joncheere K Beran D . Medicines availability for non-communicable diseases: The case for standardized monitoring. Glob Health (2015) 11(1):18–6. 10.1186/s12992-015-0105-0
64.
Castro B Ing L Park Y Abrams J Ryan M . Addressing noncommunicable disease in Dominican republic: Barriers to hypertension and diabetes care. Ann Glob Health (2018) 84(4):625–9. 10.9204/aogh.2370
65.
Ministry of Health and Family Welfare G of I. Financing and delivery of health care services in India (2005).
66.
Batangan D Echavez C Santiago AA de la Cruz A Santos E The Prices People Have to Pay for Medicines in Philippines, 1–62 (2004).
67.
Ong SE Koh JJK Toh SAES Chia KS Balabanova D McKee M et al Assessing the influence of health systems on type 2 diabetes mellitus awareness, treatment, adherence, and control: A systematic review. PLOS ONE (2018) 13(3):e0195086. 10.1371/journal.pone.0195086
68.
Ide N LoGerfo JP Karmacharya B . Barriers and facilitators of diabetes services in Nepal: A qualitative evaluation. Health Policy Plan (2018) 33(4):474–82. 10.1093/heapol/czy011
69.
Emmerick ICM Luiza VL Camacho LAB Vialle-Valentin C Ross-Degnan D . Barriers in household access to medicines for chronic conditions in three Latin American countries. Int J Equity Health (2015) 14(1):115–4. 10.1186/s12939-015-0254-z
70.
Mendis S Abegunde D Oladapo O Celletti F Nordet P . Barriers to management of cardiovascular risk in a low-resource setting using hypertension as an entry point. J Hypertens (Los Angel) (2004) 22(1):59–64. 10.1097/00004872-200401000-00013
71.
World Health Organization - Europe. Access to new medicines in europe: Technical review of policy initiatives and opportunities for collaboration and research (2015).
72.
PAHO/WHOCaribbean Community Secretariat. Report of the caribbean commission on health and development. Kingston, Jamaica: Ian Randel Publishers (2006). p. 123.
73.
Pan American Health Organization Health in the Americas, II. Scientific and Technical Publication (2007). p. 1–756.
74.
Chan WB Chen JF Goh SY Vu TTH Isip-Tan IT Mudjanarko SW et al Challenges and unmet needs in basal insulin therapy: Lessons from the asian experience. Diabetes Metab Syndr Obes (2017) 10:521–32. 10.2147/DMSO.S143046
75.
Chang H Hawley NL Kalyesubula R Siddharthan T Checkley W Knauf F et al Challenges to hypertension and diabetes management in rural Uganda: A qualitative study with patients, village health team members, and health care professionals. Int J Equity Health (2019) 18(1):38. 10.1186/s12939-019-0934-1
76.
Nnko S Bukenya D Kavishe BB Biraro S Peck R Kapiga S et al Chronic diseases in north-west Tanzania and southern Uganda. Public perceptions of terminologies, aetiologies, symptoms and preferred management. PLOS ONE (2015) 10(11):e0142194. 10.1371/journal.pone.0142194
77.
Cardenas MK Miranda JJ Beran D . Delivery of type 2 diabetes care in low- and middle-income countries: Lessons from Lima, Peru. Diabet Med (2016) 33(6):752–60. 10.1111/dme.13099
78.
Chary A Greiner M Bowers C Rohloff P . Determining adult type 2 diabetes-related health care needs in an indigenous population from rural Guatemala: A mixed-methods preliminary study. BMC Health Serv Res (2012) 12(1):476. 10.1186/1472-6963-12-476
79.
Adams OP Carter AO . Diabetes and hypertension guidelines and the primary health care practitioner in Barbados: Knowledge, attitudes, practices and barriers-a focus group study. BMC Fam Pract (2010) 11:96. 10.1186/1471-2296-11-96
80.
Tripathy JP Sagili KD Kathirvel S Trivedi A Nagaraja SB Bera OP et al Diabetes care in public health facilities in India: A situational analysis using a mixed methods approach. Diabetes Metab Syndr Obes (2019) 12:1189–99. 10.2147/DMSO.S192336
81.
Davachi S Ferrari I . Homelessness and diabetes: Reducing disparities in diabetes care through innovations and partnerships. Can J Diabetes (2012) 36(2):75–82. 10.1016/j.jcjd.2012.04.015
82.
Bovet P Gervasoni JP Mkamba M Balampama M Lengeler C Paccaud F . Low utilization of health care services following screening for hypertension in dar es salaam (Tanzania): A prospective population-based study. BMC Public Health (2008) 8(1):407. 10.1186/1471-2458-8-407
83.
Thorpe CT Bryson CL Maciejewski ML Bosworth HB . Medication acquisition and self-reported adherence in veterans with hypertension. Med Care (2009) 47(4):474–81. 10.1097/mlr.0b013e31818e7d4d
84.
Stewart DW Depue J Rosen RK Bereolos N Goldstein MG Tuitele J et al Medication-taking beliefs and diabetes in American Samoa: A qualitative inquiry. Transl Behav Med (2013) 3(1):30–8. 10.1007/s13142-012-0114-y
85.
Nieblas-Bedolla E Bream KDW Rollins A Barg FK . Ongoing challenges in access to diabetes care among the indigenous population: Perspectives of individuals living in rural Guatemala. Int J Equity Health (2019) 18(1):180. 10.1186/s12939-019-1086-z
86.
Legido-Quigley H Naheed A de Silva HA Jehan I Haldane V Cobb B et al Patients’ experiences on accessing health care services for management of hypertension in rural Bangladesh, Pakistan and Sri Lanka: A qualitative study. PLOS ONE (2019) 14(1):e0211100. 10.1371/journal.pone.0211100
87.
Legido-Quigley H Camacho Lopez PA Balabanova D Perel P Lopez-Jaramillo P Nieuwlaat R et al Patients’ knowledge, attitudes, behaviour and health care experiences on the prevention, detection, management and control of hypertension in Colombia: A qualitative study. PLOS ONE (2015) 10(4):e0122112. 10.1371/journal.pone.0122112
88.
Onyango MA Vian T Hirsch I Salvi DD Laing R Rockers PC et al Perceptions of Kenyan adults on access to medicines for non-communicable diseases: A qualitative study. PLOS ONE (2018) 13(8):e0201917. 10.1371/journal.pone.0201917
89.
Ford CD Kim MJ Dancy BL . Perceptions of hypertension and contributing personal and environmental factors among rural Southern African American women. Ethn Dis (2009) 19(4):407–13.
90.
Peck R Mghamba J Vanobberghen F Kavishe B Rugarabamu V Smeeth L et al Preparedness of Tanzanian health facilities for outpatient primary care of hypertension and diabetes: A cross-sectional survey. Lancet Glob Health (2014) 2(5):E285–92. 10.1016/S2214-109X(14)70033-6
91.
Alberti H Boudriga N Nabli M . Primary care management of diabetes in a low/middle income country: A multi-method, qualitative study of barriers and facilitators to care. BMC Fam Pract (2007) 8(1):63. 10.1186/1471-2296-8-63
92.
Gupta S Dhamija JP Mohan I Gupta R . Qualitative study of barriers to adherence to antihypertensive medication among rural women in India. Int J Hypertens (2019) 2019:5749648–7. 10.1155/2019/5749648
93.
Birabwa C Bwambale MF Waiswa P Mayega RW . Quality and barriers of outpatient diabetes care in rural health facilities in Uganda – A mixed methods study. BMC Health Serv Res (2019) 19(1):706. 10.1186/s12913-019-4535-x
94.
Emmerick ICM Campos MR Luiza VL Chaves LA Bertoldi AD Ross-Degnan D . Retrospective interrupted time series examining hypertension and diabetes medicines usage following changes in patient cost sharing in the ‘Farmácia Popular’ programme in Brazil. BMJ Open (2017) 7(11):e017308. 10.1136/bmjopen-2017-017308
95.
Gaziano TA Pagidipati N . Scaling up chronic disease prevention interventions in lower- and middle-income countries. Annu Rev Public Health (2013) 34(1):317–35. 10.1146/annurev-publhealth-031912-114402
96.
Kratzer J . Structural barriers to coping with type 1 diabetes mellitus in Ghana: Experiences of diabetic youth and their families. Ghana Med J (2012) 46(1):39–45.
97.
Beran D . The impact of health systems on diabetes care in low and lower middle income countries. Curr Diab Rep (2015) 15(4):20. 10.1007/s11892-015-0591-8
98.
Shiyanbola OO Brown CM Ward EC . I did not want to take that medicine”: African-Americans’ reasons for diabetes medication nonadherence and perceived solutions for enhancing adherence. Patient Prefer Adherence (2018) 12:409–21. 10.2147/PPA.S152146
99.
World Health Organization. Health systems respond to non-communicable diseases: Time for ambition. In: MJakabJFarringtonLBorgenmansFMantingh, editors. WHO regional office for europe. Geneva, Switzerland: World Health Organization (2018). p. 1–288.
100.
Sibomana JP McNamara RL Walker TD . Patient, clinician and logistic barriers to blood pressure control among adult hypertensives in rural district hospitals in Rwanda: A cross-sectional study. BMC Cardiovasc Disord (2019) 19(1):231. 10.1186/s12872-019-1203-3
101.
Borzecki AM Oliveria SA Berlowitz DR . Barriers to hypertension control. Am Heart J (2005) 149(5):785–94. 10.1016/j.ahj.2005.01.047
102.
Lee YK Lee PY Ng CJ . A qualitative study on healthcare professionals perceived barriers to insulin initiation in a multi-ethnic population. BMC Fam Pract (2012) 13:28. 10.1186/1471-2296-13-28
103.
Peyrot M Rubin RR Khunti K . Addressing barriers to initiation of insulin in patients with type 2 diabetes. Prim Care Diabetes (2010) 4:S11–8. 10.1016/S1751-9918(10)60004-6
104.
Ross SA Tildesley HD Ashkenas J . Barriers to effective insulin treatment: The persistence of poor glycemic control in type 2 diabetes. Curr Med Res Opin (2011) 27(3):13–20. 10.1185/03007995.2011.621416
105.
Martirosyan L Markhorst J Denig P Haaijer-Ruskamp FM Braspenning J . A pilot qualitative study to explore stakeholder opinions regarding prescribing quality indicators. BMC Health Serv Res (2012) 12:191. 10.1186/1472-6963-12-191
106.
Oliveria SA Menditto LA Yood MU Koo YH Wells KE McCarthy BD . Barriers to the initiation of, and persistence with, insulin therapy. Curr Med Res Opin (2007) 23(12):3105–12. 10.1185/030079907X242638
107.
Cetorelli V Burnham G Shabila N . Prevalence of non-communicable diseases and access to health care and medications among Yazidis and other minority groups displaced by ISIS into the Kurdistan Region of Iraq. Confl Health (2017) 11(1):4. 10.1186/s13031-017-0106-0
108.
Edelman S Pettus J . Challenges associated with insulin therapy in type 2 diabetes mellitus. Am J Med (2014) 127(10):S11–6. 10.1016/j.amjmed.2014.07.003
109.
Alshamsan R Lee JT Rana S Areabi H Millett C . Comparative health system performance in six middle-income countries: Cross-sectional analysis using World health organization study of global ageing and health. J R Soc Med (2017) 110(9):365–75. 10.1177/0141076817724599
110.
Shah VO Ghahate DM Bobelu J Sandy P Newman S Helitzer DL et al Identifying barriers to healthcare to reduce health disparity in Zuni Indians using focus group conducted by community health workers. Clin Transl Sci (2014) 7(1):6–11. 10.1111/cts.12127
111.
Gonzalvo JD . Introduction to basal insulin therapy: Clinical management of diabetes. Am J Manag Care (2018) 24(6):S87–92.
112.
Beran D Yudkin JS . Looking beyond the issue of access to insulin: What is needed for proper diabetes care in resource poor settings. Diabetes Res Clin Pract (2010) 88(3):217–21. 10.1016/j.diabres.2010.03.029
113.
Wang YB Kong DG Ma LL Wang LX . Patient related factors for optimal blood pressure control in patients with hypertension. Afr Health Sci (2013) 13(3):579–83. 10.4314/ahs.v13i3.8
114.
Goldstein HH . Pen devices to improve patient Adherence with insulin therapy in type 2 diabetes. Postgrad Med (2008) 120(3):172–9. 10.3810/pgm.2008.09.1917
115.
Saver BG Doescher MP Jackson JE Fishman P . Seniors with chronic health conditions and prescription drugs: Benefits, wealth, and health. Value Health (2004) 7(2):133–43. 10.1111/j.1524-4733.2004.72325.x
116.
Mentock SM Ng VY Narayana R Ullal H Kumari S Badiger S et al Treatment-seeking behavior and obstacles to treatment compliance in diabetic patients in Mangaluru, India. Diabetes Metab Syndr (2017) 11:S617–22. 10.1016/j.dsx.2017.04.014
117.
Young JH Ng D Ibe C Weeks K Brotman DJ Dy SM et al Access to care, treatment ambivalence, medication nonadherence, and long-term mortality among severely hypertensive african Americans: A prospective cohort study. J Clin Hypertens (2015) 17(8):614–21. 10.1111/jch.12562
118.
Roby DH Kominski GF Pourat N . Assessing the barriers to engaging challenging populations in disease management programs: The medicaid experience. Dis Management Health Outcomes (2008) 16(6):421–8. 10.2165/0115677-200816060-00007
119.
Fang J Wang G Ayala C Lucido SJ Loustalot F . Healthcare access among young adults: Impact of the affordable care act on young adults with hypertension. Am J Prev Med (2017) 53(6):S213–9. 10.1016/j.amepre.2017.07.013
120.
World Health Organization. March, WHO policy perspectives on medicines (2004).Equitable access to essential medicines: A framework for collective action
121.
Bai G Bennet C Wang J Anderson GF . Access to antihypertensive drugs in China. Circulation (2018) 138(17):1777–9. 10.1161/CIRCULATIONAHA.118.033360
122.
Ministry of Health and Family Welfare - Government of India. Report of the national commission on macroeconomics and health (2005).
123.
Pan American Health Organization. Advancing the sustainable health agenda for the americas 2018-2030 (2019).
124.
Pan American Health Organization. 55th Directing Council. 68th session of the regional committee of WHO for the americas (2016). p. 1–131.
125.
Mackey TK Liang BA . Patent and exclusivity status of essential medicines for non-communicable disease. PLOS ONE (2012) 7(11):e51022. 10.1371/journal.pone.0051022
126.
Beran D Yudkin JS de Courten M . Access to care for patients with insulin-requiring diabetes in developing countries: Case studies of Mozambique and Zambia.Diabetes Care (2005) 28(9):2136–40. 10.2337/diacare.28.9.2136
127.
Lee YK Ng CJ Lee PY Khoo EM Abdullah KL Low WY et al What are the barriers faced by patients using insulin? A qualitative study of Malaysian health care professionals’ views. Patient Prefer Adherence (2013) 7:103–9. 10.2147/PPA.S36791
128.
Sengupta A Joseph RK Modi S Syam N . Economic constraints to access to essential medicines in India (2008).
129.
Coca A López-Jaramillo P Thomopoulos C Zanchetti A Latin American Society of Hypertension LASH. Best antihypertensive strategies to improve blood pressure control in Latin America: Position of the Latin American society of hypertension.J Hypertens (2018) 36(2):208–20. 10.1097/HJH.0000000000001593
130.
Pan American Health Organization. 57th directing council. 71st Session of the Regional Committee of WHO for the Americas. Washington, DC, 30 September - 4 October 2019, 2019. p. 1–139.
131.
Halperin IJ Mukerji G Maione M Segal P Wolfs M Goguen J et al Adult patient perspectives on care for type 1 and type 2 diabetes across the Institute of medicine’s 6 domains of quality. Can J Diabetes (2018) 42(1):36–43. 10.1016/j.jcjd.2017.03.005
132.
Krall J Gabbay R Zickmund S Hamm ME Williams KR Siminerio L . Current perspectives on psychological insulin resistance: Primary care provider and patient views. Diabetes Technol Ther (2015) 17(4):268–74. 10.1089/dia.2014.0268
133.
Chawla R Makkar BM Aggarwal S Bajaj S Das AK Ghosh S et al RSSDI consensus recommendations on insulin therapy in the management of diabetes. Int J Diabetes Dev Ctries (2019) 39(S2):43–92. 10.1007/s13410-019-00783-6
134.
Schwalm JDR McCready T Lamelas P Musa H Lopez-Jaramillo P Yusoff K et al Rationale and design of a cluster randomized trial of a multifaceted intervention in people with hypertension: The Heart Outcomes Prevention and Evaluation 4 (HOPE-4) Study. Am Heart J (2018) 203:57–66. 10.1016/j.ahj.2018.06.004
135.
Werfalli M Murphy K Kalula S Levitt N . Current policies and practices for the provision of diabetes care and self-management support programmes for older South Africans. Afr J Prim Health Care Fam Med (2019) 11(1):1–12. 10.4102/phcfm.v11i1.2053
136.
Donihi AC . Practical recommendations for transitioning patients with type 2 diabetes from hospital to home. Curr Diab Rep (2017) 17(7):52. 10.1007/s11892-017-0876-1
137.
World Health Organization. Final report. WHO GCM/NCD working group on the inclusion of NCDs in other programmatic areas (working group 3.1, 2016-2017). Geneva, Switzerland: World Health Organization (2018).
138.
Seiter A . Washington, DC: World Bank (2010).A practical approach to pharmaceutical policy
139.
World Health Organization. Primary health care on the road to universal health coverage: 2019 global monitoring report. Geneva, Switzerland: World Health Organization (2019).
140.
Christiani Y Dhippayom T Chaiyakunapruk N . Assessing evidence of inequalities in access to medication for diabetic populations in low- and middle-income countries: A systematic review. Glob Health Action (2016) 9(1):32505. 10.3402/gha.v9.32505
141.
AlMaatouq MA Al-Arouj M Amod A Assaad-Khalil SH Assaad SN Azar ST et al Barriers to the delivery of optimal antidiabetic therapy in the Middle East and Africa. Int J Clin Pract (2014) 68(4):503–11. 10.1111/ijcp.12342
142.
Nolte E Knai C McKee M . Managing chronic conditions. Experience in eight countries. Copenhagen, Denmark: Observatories Studies Series N˙15 (2008). p. 202.
143.
Murphy GK McAlister FA Weir DL Tjosvold L Eurich DT . Cardiovascular medication utilization and adherence among adults living in rural and urban areas: A systematic review and meta-analysis. BMC Public Health (2014) 14:544. 10.1186/1471-2458-14-544
144.
Rockers PC Laing RO Wirtz VJ . Equity in access to non-communicable disease medicines: A cross-sectional study in Kenya. BMJ Glob Health (2018) 3(3):e000828. 10.1136/bmjgh-2018-000828
145.
Crosson JC Heisler M Subramanian U Swain B Davis GJ Lasser N et al Physicians’ perceptions of barriers to cardiovascular disease risk factor control among patients with diabetes: Results from the translating research into action for diabetes (TRIAD) study. J Am Board Fam Med (2010) 23(2):171–8. 10.3122/jabfm.2010.02.090125
146.
Syed ST Gerber BS Sharp LK . Traveling towards disease: Transportation barriers to health care access. J Community Health (2013) 38(5):976–93. 10.1007/s10900-013-9681-1
147.
de Heer HD Salinas J Lapeyrouse LM Heyman J Morera OF Balcazar HG . Binational utilization and barriers to care among Mexican American border residents with diabetes. Pan Am J Public Health (2013) 34(3):147–54.
148.
Anderson G Rodriguez M . Multiple sclerosis, seizures, and antiepileptics: Role of IL-18, ido, and melatonin. Eur J Neurol (2011) 18(5):680–5. 10.1111/j.1468-1331.2010.03257.x
149.
Pan American Health Organization. Quinquennial report 2013 - 2017 of the director of the. Washington, DC: Pan American Sanitary Bureau (2017).
150.
Campos C . Addressing cultural barriers to the successful use of insulin in hispanics with type 2 diabetes. South Med J (2007) 100(8):812–20. 10.1097/SMJ.0b013e3180f609c4
151.
Mondesir FL Levitan EB Malla G Mukerji R Carson AP Safford MM et al Patient perspectives on factors influencing medication adherence among people with coronary heart disease (CHD) and CHD risk factors. Patient Prefer Adherence (2019) 13:2017–27. 10.2147/PPA.S222176
152.
Schmittdiel JA Marshall CJ Wiley D Chau CV Trinacty CM Wharam JF et al Opportunities to encourage mail order pharmacy delivery service use for diabetes prescriptions: A qualitative study. BMC Health Serv Res (2019) 19(1):422. 10.1186/s12913-019-4250-7
153.
Iwelunmor J Plange-Rhule J Airhihenbuwa CO Ezepue C Ogedegbe O . A narrative synthesis of the health systems factors influencing optimal hypertension control in sub-saharan Africa. PLOS ONE (2015) 10(7):e0130193. 10.1371/journal.pone.0130193
154.
Schafheutle EI Hassell K Noyce PR Weiss MC . Access to medicines: Cost as an influence on the views and behaviour of patients.Health Soc Care Community (2002) 10(3):187–95. 10.1046/j.1365-2524.2002.00356.x
155.
Yarzebski J Bujor CF Goldberg RJ Spencer F Lessard D Gore JM . A community-wide survey of physician practices and attitudes toward cholesterol management in patients with recent acute myocardial infarction. Arch Intern Med (2002) 162(7):797–804. 10.1001/archinte.162.7.797
156.
Aikens JE Piette JD . Diabetic patients’ medication underuse, illness outcomes, and beliefs about antihyperglycemic and antihypertensive treatments. Diabetes Care (2009) 32(1):19–24. 10.2337/dc08-1533
157.
World Health Organization. Measuring medicine prices, availability, affordability and price components. WHO Technical Report Series. 2nd ed.Geneva, Switzerland: World Health Organization (2008).
158.
Venkatesh S Weatherspoon LJ Kaplowitz SA Song WO . Acculturation and glycemic control of asian Indian adults with type 2 diabetes. J Community Health (2013) 38(1):78–85. 10.1007/s10900-012-9584-6
159.
Okemah J Peng J Quiñones M . Addressing clinical inertia in type 2 diabetes mellitus: A review. Adv Ther (2018) 35(11):1735–45. 10.1007/s12325-018-0819-5
160.
Magwire ML . Addressing barriers to insulin therapy: The role of insulin pens. Am J Ther (2011) 18(5):392–402. 10.1097/MJT.0b013e3181ef4dde
161.
Ferrario A Chitan E Seicas R Sautenkova N Bezverhni Z Kluge H et al Progress in increasing affordability of medicines for non-communicable diseases since the introduction of mandatory health insurance in the Republic of Moldova. Health Policy Plan (2016) 31(6):793–800. 10.1093/heapol/czv136
162.
Higuchi M . Access to diabetes care and medicines in the Philippines. Asia Pac J Public Health (2010) 22(3):96S–102S. 10.1177/1010539510373005
163.
Akunne OO Adedapo ADA . Antihypertensive prescription among black patients without compelling indications: Prescription, effectiveness, quality and cost of medication. BMC Health Serv Res (2019) 19(1):373. 10.1186/s12913-019-4202-2
164.
World Health Organization. In: EBlasASivasankara Kurup, editors. Equity, social determinants and public health programmes. Geneva, Switzerland: World Health Organization (2010). p. 1–291.
165.
Maciejko J Jamoua R Premchand A . Assessment and management of patients with hyperlipidemia referred for initiation of PCSK9 inhibitor therapy: A lipid clinic experience. Am J Cardiovasc Drugs (2019) 19:553–9. 10.1007/s40256-019-00352-6
166.
Cohen JD Cziraky MJ Jacobson TA Maki KC Karalis DG . Barriers to PCSK9 inhibitor prescriptions for patients with high cardiovascular risk: Results of a healthcare provider survey conducted by the National Lipid Association. J Clin Lipidol (2017) 11(4):891–900. 10.1016/j.jacl.2017.04.120
167.
McBrien KA Naugler C Ivers N Weaver RG Campbell D Desveaux L et al Barriers to care in patients with diabetes and poor glycemic control-A cross-sectional survey. PLOS ONE (2017) 12(5):e0176135. 10.1371/journal.pone.0176135
168.
Pan American Health Organization. Annual report of the director 2019. Advancing the sustainable health agenda for the americas 2018-2030. Washington, DC: Pan American Health Organization (2019). p. 1–146.
169.
Sadarangani TR Trinh-Shevrin C Chyun D Yu G Kovner C . Cardiovascular risk in middle-aged and older immigrants: Exploring residency period and health insurance coverage. Physiol Behav (2011) 176(10):139–48.
170.
Mohan V Shah S Joshi S Seshiah V Sahay B Banerjee S et al Current status of management, control, complications and psychosocial aspects of patients with diabetes in India: Results from the DiabCare India 2011 Study. Indian J Endocrinol Metab (2014) 18(3):370–8. 10.4103/2230-8210.129715
171.
Shulman NB Martinez B Brogan D Carr AA Miles CG . Financial cost as an obstacle to hypertension therapy. Am J Public Health (1986) 76(9):1105–8. 10.2105/ajph.76.9.1105
172.
Herman D Afulani P Coleman-Jensen A Harrison GG . Food insecurity and cost-related medication underuse among nonelderly adults in a nationally representative sample. Am J Public Health (2015) 105(10):e48–59. 10.2105/AJPH.2015.302712
173.
Billimek J Sorkin DH . Food insecurity, processes of care, and self‐reported medication underuse in patients with type 2 diabetes: Results from the California health interview survey. Health Serv Res (2012) 47(6):2159–68. 10.1111/j.1475-6773.2012.01463.x
174.
Zarogoulidis P Papanas N Kouliatsis G Spyratos D Zarogoulidis K Maltezos E . Inhaled insulin: Too soon to be forgotten?J Aerosol Med Pulm Drug Deliv (2011) 24(5):213–23. 10.1089/jamp.2011.0876
175.
Leichter S . Is the use of insulin analogues cost-effective?Adv Ther (2008) 25(4):285–99. 10.1007/s12325-008-0043-9
176.
Ward W Armbrecht ES Lavin MA . Medication possession and glycemic control among uninsured type 2 diabetics. J Nurse Pract (2012) 8(7):528–33. 10.1016/j.nurpra.2012.02.001
177.
Williams A Manias E Cross W Crawford K . Motivational interviewing to explore culturally and linguistically diverse people’s comorbidity medication self-efficacy. J Clin Nurs (2015) 24(9–10):1269–79. 10.1111/jocn.12700
178.
Schafheutle EI . Patients’ views on the UK policy of prescription charges-Insights from qualitative interviews. Res Soc Adm Pharm (2008) 4(4):343–54. 10.1016/j.sapharm.2008.02.001
179.
Schwartz KL Dailey R Bartoces M Binienda J Archer C Neale AV . Predictors, barriers, and facilitators of lipid-lowering medication use among African Americans in a primary care clinic. J Natl Med Assoc (2009) 101(9):944–52. 10.1016/s0027-9684(15)31043-9
180.
Valenzuela JM Seid M Waitzfelder B Andrea M Beavers DP Dabelea DM et al Prevalence of and disparities in barriers to care experienced by youth with type 1 diabetes. J Pediatr (2014) 164(6):1369–75.e1. 10.1016/j.jpeds.2014.01.035
181.
Tseng CW Tierney EF Dudley RA Waitzfelder B Ackermann RT Karter AJ et al Race/ethnicity and economic differences in cost-related medication underuse among insured adults with diabetes: The translating research into action for diabetes study. Diabetes Care (2008) 31:261–6. 10.2337/dc07-1341
182.
Vanderlee L Ahmed S Ferdous F Farzana FD Das SK Ahmed T et al Self-care practices and barriers to compliance among patients with diabetes in a community in rural Bangladesh. Int J Diabetes Dev Ctries (2016) 36(3):320–6. 10.1007/s13410-015-0460-7
183.
Spain CV Wright JJ Hahn RM Wivel A Martin AA . Self-reported barriers to adherence and persistence to treatment with injectable medications for type 2 diabetes. Clin Ther (2016) 38(7):1653–64.e1. 10.1016/j.clinthera.2016.05.009
184.
Komaric N Bedford S van Driel ML . Two sides of the coin: Patient and provider perceptions of health care delivery to patients from culturally and linguistically diverse backgrounds. BMC Health Serv Res (2012) 12(1):322. 10.1186/1472-6963-12-322
185.
McEwen LN Casagrande SS Kuo S Herman WH . Why are diabetes medications so expensive and what can Be done to control their cost?Curr Diab Rep (2017) 17(9):71. 10.1007/s11892-017-0893-0
186.
Tyson DM Arriola NB Medina-Ramirez P Dao LU Smith CAS Livingston T . You have to control it however you can”: Type 2 diabetes management in a hispanic farmworker community in rural Florida. Hum Organ (2019) 78(3):205–17. 10.17730/0018-7259.78.3.205
187.
World Bank. Type-2 Diabetes care in Ukraine: Breakpoints and implications for action. Washington, DC: World Bank (2018).
188.
Gerber BS Cano AI Caceres ML Smith DE Wilken LA Michaud JB et al A pharmacist and health promoter team to improve medication adherence among latinos with diabetes. Ann Pharmacother (2010) 44(1):70–9. 10.1345/aph.1m389
189.
Piette JD Heisler M Wagner TH . Problems paying out-of-pocket medication costs among older adults with diabetes. Diabetes Care (2004) 27(2):384–91. 10.2337/diacare.27.2.384
190.
Garnero TL Davis NJ Perez-Nieves M Hadjiyianni I Cao D Ivanova JI et al Insulin non-persistence among people with type 2 diabetes: How to get your patients to stay on insulin therapy. Postgrad Med (2018) 130(4):394–401. 10.1080/00325481.2018.1457396
191.
Coleman MT Lott JA Sharma S . Use of continuous quality improvement to identify barriers in the management of hypertension. Am J Med Qual (2000) 15(2):72–7. 10.1177/106286060001500206
192.
Ohene Buabeng K Matowe L Plange-Rhule J . Unaffordable drug prices: The major cause of non-compliance with hypertension medication in Ghana. J Pharm Pharm Sci (2004) 7(3):350–2.
193.
Dalal MR Grabner M Bonine N Stephenson JJ DiGenio A Bieszk N . Are patients on basal insulin attaining glycemic targets? Characteristics and goal achievement of patients with type 2 diabetes mellitus treated with basal insulin and physician-perceived barriers to achieving glycemic targets. Diabetes Res Clin Pract (2016) 121:17–26. 10.1016/j.diabres.2016.08.004
194.
Campbell DJT Tonelli M Hemmelgarn B Mitchell C Tsuyuki R Ivers N et al Assessing outcomes of enhanced chronic disease care through patient education and a value-based formulary study (ACCESS)—Study protocol for a 2×2 factorial randomized trial. Implementation Sci (2015) 11(1):131. 10.1186/s13012-016-0491-6
195.
Lee S Jiang L Dowdy D Hong A Ory M . Attitudes, beliefs, and cost-related medication nonadherence among adults aged 65 or older with chronic diseases. Prev Chronic Dis (2018) 15(E148):180190–10. 10.5888/pcd15.180190
196.
Joo JY Lee H . Barriers to and facilitators of diabetes self-management with elderly Korean-American immigrants. Int Nurs Rev (2016) 63(2):277–84. 10.1111/inr.12260
197.
Lyles CR Seligman HK Parker MM Moffet HH Adler N Schillinger D et al Financial strain and medication adherence among diabetes patients in an integrated health care delivery system: The diabetes study of northern California (DISTANCE). Health Serv Res (2016) 51(2):610–24. 10.1111/1475-6773.12346
198.
Campbell DJT Manns BJ Weaver RG Hemmelgarn BR King-Shier KM Sanmartin C . Financial barriers and adverse clinical outcomes among patients with cardiovascular-related chronic diseases: A cohort study. BMC Med (2017) 15(1):33. 10.1186/s12916-017-0788-6
199.
Mullins CD Blatt L Gbarayor CM Yang HWK Baquet C . Health disparities: A barrier to high-quality care. Bone (2012) 23(1):1–7.
200.
Cersosimo E Musi N . Improving treatment in hispanic/latino patients. Am J Med (2011) 124(10):S16–21. 10.1016/j.amjmed.2011.07.019
201.
Mahoney JJ . Reducing patient drug acquisition costs can lower diabetes health claims. Am J Manag Care (2005) 11(5):S170–6.
202.
Elder NC Tubb MR . Diabetes in homeless persons: Barriers and enablers to health as perceived by patients, medical, and social service providers. Soc Work Public Health (2014) 29(3):220–31. 10.1080/19371918.2013.776391
203.
Guedes MVC Araujo TLde Lopes MVde O Silva Lde Fda Freitas MCde Almeida PCde . Barreiras ao tratamento da hipertensão arterial. Rev Bras Enferm (2011) 64(6):1038–42. 10.1590/s0034-71672011000600008
204.
Gebrezgi MT Trepka MJ Kidane EA . Barriers to and facilitators of hypertension management in asmara, Eritrea: Patients’ perspectives. J Health Popul Nutr (2017) 36(1):11. 10.1186/s41043-017-0090-4
205.
Campbell DJT Manns BJ Leblanc P Hemmelgarn BR Sanmartin C King-Shier K . Finding resiliency in the face of financial barriers: Development of a conceptual framework for people with cardiovascular-related chronic disease.Medicine (2016) 95(49):e5561. 10.1097/MD.0000000000005561
206.
Claydon-Platt K Manias E Dunning T . The barriers and facilitators people with diabetes from a nonEnglish speaking background experience when managing their medications: A qualitative study. J Clin Nurs (2014) 23(15–16):2234–46. 10.1111/jocn.12501
207.
Blackstone S Iwelunmor J Plange-Rhule J Gyamfi J kofi QN Ntim M et al ‘I believe high blood pressure can kill me:’ using the PEN-3 Cultural Model to understand patients’ perceptions of an intervention to control hypertension in Ghana. Ethn Health (2019) 24(3):257–70. 10.1080/13557858.2017.1346178
208.
Paniz VMV Fassa AG Facchini LA Bertoldi AD Piccini RX Tomasi E et al Access to continuous use medication among adults and the elderly in South and Northeast Brazil. Cad Saude Publica (2008) 24(2):267–80. 10.1590/s0102-311x2008000200005
209.
Vialle-Valentin CE Serumaga B Wagner AK Ross-Degnan D . Evidence on access to medicines for chronic diseases from household surveys in five low- and middle-income countries. Health Policy Plan (2015) 30(8):1044–52. 10.1093/heapol/czu107
210.
Bernard DM Johansson P Fang Z . Out-of-pocket healthcare expenditure burdens among nonelderly adults with hypertension. Am J Manag Care (2014) 20(5):406–13.
211.
Rice T Lavarreda SA Ponce NA Brown ER . The impact of private and public health insurance on medication use for adults with chronic diseases. Med Care Res Rev (2005) 62(2):231–49. 10.1177/1077558704273806
212.
Vawter L Tong X Gemilyan M Yoon PW . Barriers to antihypertensive medication adherence among adults - United States, 2005. J Clin Hypertens (2008) 10(12):922–9. 10.1111/j.1751-7176.2008.00049.x
213.
Fang J Yang Q Ayala C Loustalot F . Disparities in access to care among US adults with self-reported hypertension. Am J Hypertens (2014) 27(11):1377–86. 10.1093/ajh/hpu061
214.
Kratzer J . Structural barriers to coping with type 1 diabetes mellitus in Ghana: Experiences of diabetic youth and their families. Ghana Med J (2012) 46(2):39–45.
215.
Baum SJ Toth PP Underberg JA Jellinger P Ross J Wilemon K . PCSK9 inhibitor access barriers—Issues and recommendations: Improving the access process for patients, clinicians and payers. Clin Cardiol (2017) 40(4):243–54. 10.1002/clc.22713
216.
Fritzen JS Motter FR Paniz VMV . Regular access and adherence to medications of the specialized component of pharmaceutical services. Rev Saude Publica (2017) 51:109. 10.11606/S1518-8787.2017051006932
217.
Perry L James S Gallagher R Dunbabin J Steinbeck K Lowe J . Supporting patients with type 1 diabetes using continuous subcutaneous insulin infusion therapy: Difficulties, disconnections, and disarray. J Eval Clin Pract (2017) 23(4):719–24. 10.1111/jep.12703
218.
Grant RW Lutfey KE Gerstenberger E Link CL Marceau LD McKinlay JB . The decision to intensify therapy in patients with type 2 diabetes: Results from an experiment using a clinical case vignette. J Am Board Fam Med (2009) 22(5):513–20. 10.3122/jabfm.2009.05.080232
219.
Karter AJ Stevens MR Herman WH Ettner S Marrero DG Safford MM et al Out-of-pocket costs and diabetes preventive services: The translating research into action for diabetes (TRIAD) study. Diabetes Care (2003) 26(8):2294–9. 10.2337/diacare.26.8.2294
220.
Ryan JG Fedders M Jennings T Vittoria I Yanes M . Clinical outcomes and incremental costs from a medication adherence pilot intervention targeting low-income patients with diabetes at risk of cost-related medication nonadherence. Clin Ther (2014) 36(12):1991–2002. 10.1016/j.clinthera.2014.09.001
221.
Liu YM Kao Yang YH Hsieh CR . The determinants of the adoption of pharmaceutical innovation: Evidence from Taiwan. Soc Sci Med (2011) 72(6):919–27. 10.1016/j.socscimed.2010.12.027
222.
Araujo JLO Pereira MD de Cássia Bergamaschi C de Sá Del Fiol F Lopes LC de Toledo MI et al Access to medicines for diabetes treatment in Brazil: Evaluation of “health has no price” program. Diabetol Metab Syndr (2016) 8(1):35. 10.1186/s13098-016-0150-8
223.
Shah BR Booth GL Lipscombe LL Feig DS Bhattacharyya OK Bierman AS . Near equality in quality for medication utilization among older adults with diabetes with universal medication insurance in Ontario, Canada. J Eval Clin Pract (2014) 20(2):176–83. 10.1111/jep.12104
224.
Tjia J Js S . Will the Medicare prescription drug benefit eliminate cost barriers for older adults with diabetes mellitus?J Am Geriatr Soc (2006) 54(4):606–12. 10.1111/j.1532-5415.2006.00663.x
225.
Johnson HM Warner RC LaMantia JN Bowers BJ . I have to live like I’m old.” young adults’ perspectives on managing hypertension: A multi-center qualitative study. BMC Fam Pract (2016) 17(1):31. 10.1186/s12875-016-0428-9
226.
Wollum A Gabert R McNellan CR Daly JM Reddy P Bhatt P et al Identifying gaps in the continuum of care for cardiovascular disease and diabetes in two communities in South Africa: Baseline findings from the HealthRise project. PLOS ONE (2018) 13(3):e0192603. 10.1371/journal.pone.0192603
227.
Magadzire BP Mathole T Ward K . Reasons for missed appointments linked to a public-sector intervention targeting patients with stable chronic conditions in South Africa: Results from in-depth interviews and a retrospective review of medical records. BMC Fam Pract (2017) 18:82. 10.1186/s12875-017-0655-8
228.
Suraci C Mulas F Rossi MC Gentile S Giorda CB . Management of newly diagnosed patients with type 2 diabetes: What are the attitudes of physicians? A SUBITO!AMD survey on the early diabetes treatment in Italy. Acta Diabetol (2012) 49(6):429–33. 10.1007/s00592-012-0374-5
229.
Albanese NP Pignato AM Monte SV . Provider perception of pharmacy services in the patient-centered medical home. J Pharm Pract (2017) 30(6):612–20. 10.1177/0897190016679759
230.
Davis SN . The role of inhaled insulin in the treatment of type 2 diabetes. J Diabetes Complications (2008) 22(6):420–9. 10.1016/j.jdiacomp.2007.05.001
231.
Korytkowski M . When oral agents fail: Practical barriers to starting insulin. Int J Obes Relat Metab Disord (2002) 26(S3):S18–24. 10.1038/sj.ijo.0802173
232.
Scott A O’Cathain A Goyder E . Socioeconomic disparities in access to intensive insulin regimens for adults with type 1 diabetes: A qualitative study of patient and healthcare professional perspectives. Int J Equity Health (2019) 18(150). 10.1186/s12939-019-1061-8
233.
Mendenhall E Norris SA . Diabetes care among urban women in soweto, South Africa: A qualitative study. BMC Public Health (2015) 15(1):1300–7. 10.1186/s12889-015-2615-3
234.
Szafran O Kennett SL Bell NR Torti JMI . Interprofessional collaboration in diabetes care: Perceptions of family physicians practicing in or not in a primary health care team. BMC Fam Pract (2019) 20:44. 10.1186/s12875-019-0932-9
235.
Larkin ME . Overcoming psychological barriers to insulin use. US Endocrinol (2008) 4(2):46–8. 10.17925/use.2008.04.2.46
236.
Larkin ME Capasso VA Chen CL Mahoney EK Hazard B Cagliero E et al Measuring psychological insulin resistance: Barriers to insulin use. Diabetes Educ (2008) 34(3):511–7. 10.1177/0145721708317869
237.
Brunton S . Initiating insulin therapy in type 2 diabetes: Benefits of insulin analogs and insulin pens. Diabetes Technol Ther (2008) 10(4):247–56. 10.1089/dia.2008.0287
238.
Meece J . Dispelling myths and removing barriers about insulin in type 2 diabetes. Diabetes Educ (2006) 32(1):9S–18S. 10.1177/0145721705285638
239.
Cuddihy RM Borgman SK . Considerations for diabetes. Am J Ther (2013) 20(6):694–702. 10.1097/mjt.0b013e318217a5e3
240.
Stephens P Ross-Degnan D Wagner AK . Does access to medicines differ by gender? Evidence from 15 low and middle income countries. Health Policy (2013) 110(1):60–6. 10.1016/j.healthpol.2013.01.016
241.
Adams AS Madden JM Zhang F Soumerai SB Gilden D Griggs J et al Changes in use of lipid-lowering medications among black and white dual enrollees with diabetes transitioning from medicaid to Medicare Part D drug coverage. Med Care (2014) 52(8):695–703. 10.1097/MLR.0000000000000159
242.
Centers for Disease Control and Prevention. Surveillance of health status in minority communities - racial and ethnic approaches to community health across the U.S. (REACH U.S.) risk factor survey, United States, 2009. MMWR Surveill Summ (2011) 60(6):1–44.
243.
Petrak F Herpertz S Stridde E Pfutzner A . Psychological insulin resistance in type 2 diabetes patients regarding oral antidiabetes treatment, subcutaneous insulin injections, or inhaled insulin. Diabetes Technol Ther (2013) 15(8):703–11. 10.1089/dia.2012.0257
244.
Pour MRS Sadeghiyeh T Hadavi M Besharati M Bidaki R . The barriers against initiating insulin therapy among patients with diabetes living in Yazd, Iran. Diabetes Metab Syndr Obes (2019) 12:1349–54. 10.2147/DMSO.S200867
245.
Drab S . Translating clinical guidelines into clinical practice: Role of the pharmacist in type 2 diabetes management. J Am Pharm Assoc (2009) 49(6):e152–62. 10.1331/JAPhA.2009.08181
Appendix: Search Strategy
Database: PubMed
Date: 27 January 2020
Key words: pharmaceutical preparations OR drugs OR medicines OR medication
AND
access barriers OR access facilitators OR availability barriers OR availability facilitators OR accessibility barriers OR accessibility facilitators OR accommodation barriers OR accommodation facilitators OR affordability barriers OR affordability facilitators OR cost barriers OR acceptability barriers OR acceptability facilitators
AND
diabetes OR diabetes mellitus OR hypertension OR arterial hypertension OR dyslipidemias OR
hypercholesterolemia OR metabolic syndrome
Filters: humans and languages (English, French, Portuguese, Spanish)
Strategy:
(("pharmaceutical preparations"[MeSH Terms] OR ("pharmaceutical"[All Fields] AND "preparations"[All Fields]) OR "pharmaceutical preparations"[All Fields]) OR ("pharmaceutical preparations"[MeSH Terms] OR ("pharmaceutical"[All Fields] AND "preparations"[All Fields]) OR "pharmaceutical preparations"[All Fields] OR "drugs"[All Fields]) OR "medicines"[All Fields] OR ("pharmaceutical preparations"[MeSH Terms] OR ("pharmaceutical"[All Fields] AND "preparations"[All Fields]) OR "pharmaceutical preparations"[All Fields] OR "medication"[All Fields])) AND ((access[All Fields] AND barriers[All Fields]) OR (access[All Fields] AND facilitators[All Fields]) OR (availability[All Fields] AND barriers[All Fields]) OR (availability[All Fields] AND facilitators[All Fields]) OR (accessibility[All Fields] AND barriers[All Fields]) OR (accessibility[All Fields] AND facilitators[All Fields]) OR "accommodation"[All Fields] AND barriers[All Fields]) OR "accommodation"[All Fields] AND facilitators[All Fields] OR "affordability"[All Fields] AND barriers[All Fields] OR ("costs"[All Fields] AND barriers[All Fields]) OR ("affordability"[All Fields] AND facilitators[All Fields]) OR ("costs"[All Fields] AND barriers[All Fields]) OR (acceptability[All Fields] AND barriers[All Fields]) OR (acceptability[All Fields] AND facilitators[All Fields]) AND ("diabetes mellitus"[MeSH Terms] OR ("diabetes"[All Fields] AND "mellitus"[All Fields]) OR "diabetes mellitus"[All Fields] OR "diabetes"[All Fields] OR ("diabetes mellitus"[MeSH Terms] OR ("diabetes"[All Fields] AND "mellitus"[All Fields]) OR "diabetes mellitus"[All Fields]) OR ("hypertension"[MeSH Terms] OR "hypertension"[All Fields]) OR ("hypertension"[MeSH Terms] OR "hypertension"[All Fields] OR ("arterial"[All Fields] AND "hypertension"[All Fields]) OR "arterial hypertension"[All Fields]) OR ("dyslipidemias"[MeSH Terms] OR "dyslipidemias"[All Fields]) OR ("hypercholesterolaemia"[All Fields] OR "hypercholesterolemia"[MeSH Terms] OR "hypercholesterolemia"[All Fields]) OR ("metabolic syndrome"[MeSH Terms] OR ("metabolic"[All Fields] AND "syndrome"[All Fields]) OR "metabolic syndrome"[All Fields])) AND ("humans"[MeSH Terms] AND (English[lang] OR French[lang] OR Portuguese[lang] OR Spanish[lang]))
The strategy created for PubMed was modified to suit the requirements of the other databases. MeSH terms were only used in the databases and indexes that permit such use.
Summary
Keywords
access, diabetes, barriers, facilitators, non-communicable chronic diseases (NCDs), hypertension (HTN), dyslipidemia, medicines
Citation
Castillo-Laborde C, Hirmas-Adauy M, Matute I, Jasmen A, Urrejola O, Molina X, Awad C, Frey-Moreno C, Pumarino-Lira S, Descalzi-Rojas F, Ruiz TJ and Plass B (2022) Barriers and Facilitators in Access to Diabetes, Hypertension, and Dyslipidemia Medicines: A Scoping Review. Public Health Rev 43:1604796. doi: 10.3389/phrs.2022.1604796
Received
25 January 2022
Accepted
27 July 2022
Published
02 September 2022
Volume
43 - 2022
Edited by
Samantha Morais, McGill University, Canada
Reviewed by
Joao Araujo, São Paulo State University, Brazil
Neusa Jessen, Maputo Central Hospital, Mozambique
Updates
Copyright
© 2022 Castillo-Laborde, Hirmas-Adauy, Matute, Jasmen, Urrejola, Molina, Awad, Frey-Moreno, Pumarino-Lira, Descalzi-Rojas, Ruiz and Plass.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms. PHR is edited by the Swiss School of Public Health (SSPH+) in a partnership with the Association of Schools of Public Health of the European Region (ASPHER)+
*Correspondence: Carla Castillo-Laborde, carlacastillo@udd.cl
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.