Abstract
Objectives: Efforts to contain the COVID-19 pandemic should take into account worsening health inequities. While many public health experts have commented on inequities, no analysis has yet synthesized recommendations into a guideline for practitioners. The objective of this rapid review was to identify the areas of greatest concern and synthesize recommendations.
Methods: We conducted a rapid systematic review (PROSPERO: CRD42020178131). We searched Ovid MEDLINE, Embase, PsycINFO, CINAHL and Cochrane Central Register of Controlled Trials databases from December 1, 2019 to April 27, 2020. We included English language peer-reviewed commentaries, editorials, and opinion pieces that addressed the social determinants of health in the context of COVID-19.
Results: 338 articles met our criteria. Authors represented 81 countries. Income, housing, mental health, age and occupation were the most discussed social determinants of health. We categorized recommendations into primordial, primary, secondary and tertiary prevention that spoke to the social determinants of COVID-19 and equity.
Conclusion: These recommendations can assist efforts to contain COVID-19 and reduce health inequities during the pandemic. Using these recommendations, public health practitioners could support a more equitable pandemic response.
Systematic Review Registration: PROSPERO, CRD42020178131.
Introduction
SARS-CoV-2 emerged as a novel pathogen in late 2019 and quickly became a leading cause of morbidity and mortality worldwide [1]. In over 1 year, the COVID-19 pandemic spread globally and resulted in over 150 million confirmed cases and over 3 million deaths [2]. Efforts to contain the virus have caused economic recessions [3], halted global travel and trade, and required the mass closure of places of employment and education [4]. Initially called a “great equalizer” [5], experts in public health quickly recognized that the COVID-19 pandemic and its aftermath disproportionately impacts individuals and communities that had previously been made vulnerable by the social determinants of health (SDoH).
Reports emerged in March 2020 that COVID-19 outcomes were associated with key SDoH. Data from Canada, the United States, and the United Kingdom indicated higher rates of COVID-19 infections, hospital admissions, and mortality in low-income areas with high household density [6]. Racialized communities in these countries were particularly impacted [7], likely due to systemic racism that affects occupation and work, socioeconomic status, access to health care, and housing. The risk of COVID-19 varied by neighbourhood [7], housing status (e.g., homeless shelters, prisons) [8, 9], type of work (e.g., essential services, retail) [10], and income [7].
Numerous experts have provided recommendations on how public health officials and policymakers should consider the SDoH of COVID-19. The objective of this rapid review is to identify the areas of greatest concern and synthesize recommendations to support a more equitable pandemic response.
Methods
We conducted a rapid review following Cochrane Rapid Review Methods Group [11] and PRISMA guidelines [12]. This review is registered with PROSPERO (CRD42020178131).
Search Strategy and Selection Criteria
We searched Ovid MEDLINE, Embase, PsycINFO, CINAHL and Cochrane Central Register of Controlled Trials bibliographic databases from December 1, 2019 to April 1, 2020, updating the search on April 16, 2020 and on April 27, 2020 (Supplementary Appendix S1). We included English language commentaries, editorials, analyses and opinion pieces from peer-reviewed journals that discussed COVID-19 in relation to equity, the social determinants of health, and/or vulnerable populations. Using the WHO Commission on the Social Determinants of Health framework [13] we included articles that discussed the following SDoH: age, disability, education, food security, gender, governance, housing, immigration status, income, mental health, occupation, race and ethnicity, rural/urban geography, sexual orientation, and social isolation or social capital. We excluded quantitative original research (separately analysed in PLOS ONE [14]), qualitative original research, reviews, and mixed-methods studies.
Publication Selection
Titles, abstracts, and full-text (where necessary) were screened against our inclusion and exclusion criteria using DistillerSR citation management software (Evidence Partners, Ottawa, Canada). Following rapid systematic review methods, 80% of retrieved records were single screened by one team of three independent reviewers, and 20% were double screened by a second team of five independent reviewers. The second team verified exclusion decisions for single-reviewed records. A third team resolved conflicts for double-reviewed records by deliberation. Following this initial review, two authors conducted a secondary full text review of all included articles.
Data Extraction, Quality Appraisal, and Synthesis
After finalizing the included articles, the study team independently reviewed 20 randomly selected articles to create a data extraction table and initial coding framework. Through meetings, this coding framework was refined to support our narrative analysis and synthesis. We organized recommendations by SDoH, and into primordial, primary, secondary, and tertiary prevention [15]. Primordial prevention focuses on factors that reduce foundational risk factors (e.g., psychosocial, environmental), primary prevention prevents onset of disease by altering behaviours and exposures, secondary prevention focuses on detecting and treating early stages of disease, and tertiary prevention focuses on mitigating the impact of disease on those infected [15–17]. We also analyzed the country of origin of authors, article type, and type of evidence used. Three authors individually completed data extraction, coding, and quality assessment (Supplementary Appendix S2). We used the Joanna Briggs Institute Critical Appraisal Tool for text and opinion studies for quality appraisal [18]. Due to the heterogenous nature of the articles, a metanalysis could not be completed, so the studies were synthesized using a narrative approach.
Results
A total of 7,376 citations were screened (Figure 1), of which 338 articles met our inclusion criteria (Supplementary Appendix S3). The authors represent 81 countries from Africa, Asia, Australia, Europe, North America, and South America. The majority of the articles analyzed were of good quality using the Joanna Briggs Institute Critical Appraisal Tool. In 327 (96.7%) of the articles, the source of the opinions was easily identifiable. In 292 (86.4%) articles, the identified source of the opinion had standing in the relevant field of expertise. In 313 (92.6%) articles, the best interests of the population being discussed was the central focus. In 314 (92.9%) articles, the opinions discussed were presented logically, and seemed to be the result of analytical thought. In 269 (79.6%) articles, relevant literature in the field was referred to. In 182 (53.8%) articles, inconsistencies with the literature were identified and logically defended.
FIGURE 1
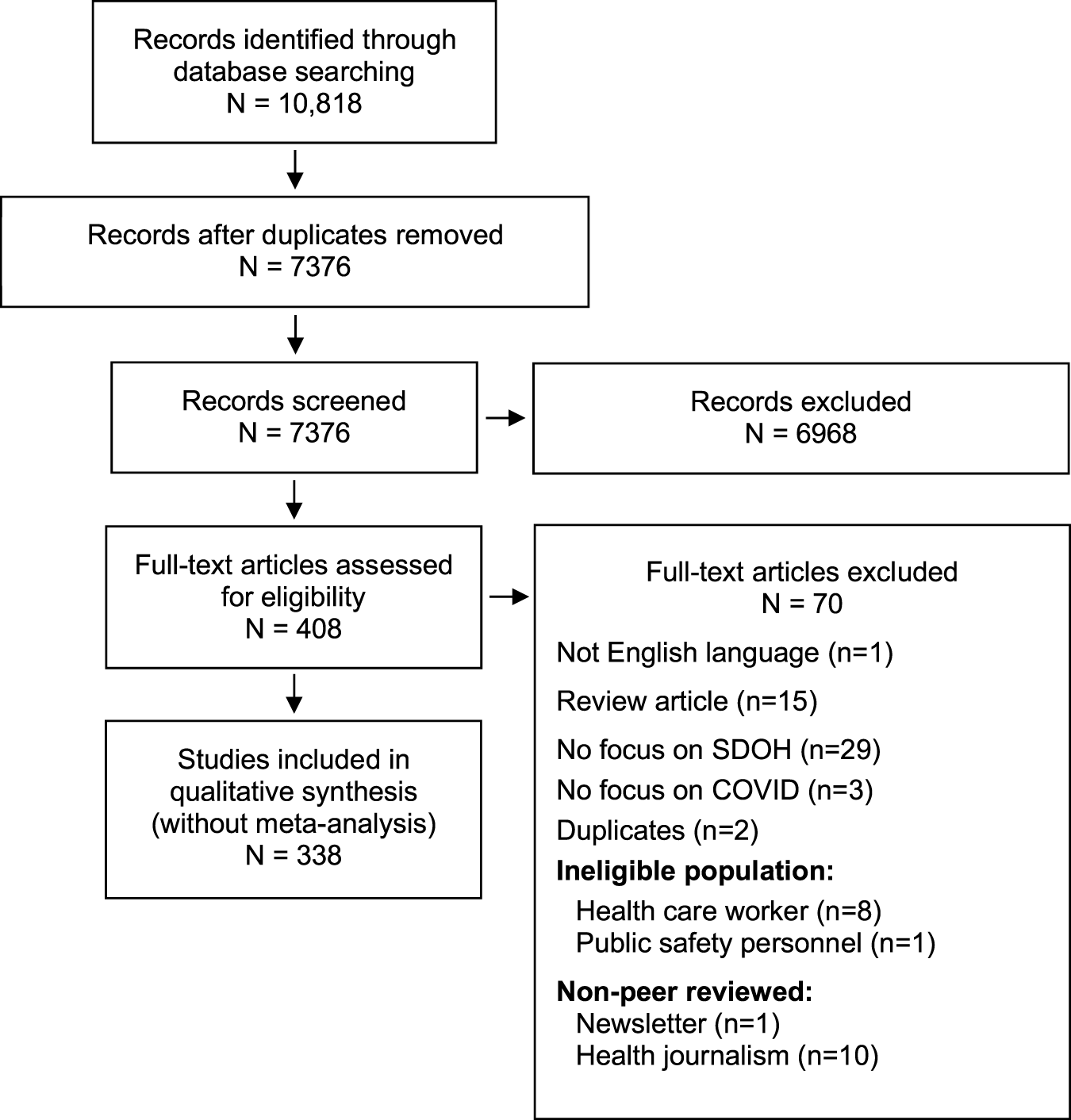
PRISMA flow diagram (Systematic Review, Global, 2019-2020).
Recommendations addressed all levels of prevention (Table 1) and addressed many social determinants of health. Income, housing, mental health, age and occupation were most discussed in connection to COVID-19 (Figure 2). More specifically, 170 articles spoke about income (including bigger picture discussions of GDP as well as individual income and health insurance). 86 articles spoke about housing, including those experiencing homeless, long-term care residents, and incarcerated individuals. 84 articles discussed the effects having a mental health condition, 83 articles spoke to age (including specific vulnerable populations such as the elderly and children), and 77 articles discussed the interplay between occupation and COVID-19. Other social determinants of health discussed included race and ethnicity, governance, social isolation, gender, immigration, food security, disability, education, geography, and sexual orientation.
TABLE 1
| Level of Public Health Prevention | Definition |
|---|---|
| Primordial prevention | Addressing the foundational risk factors for COVID-19 |
| Primordial prevention: policy | Changing or creating legislation, rules or regulations to protect vulnerable populations |
| Primordial prevention: research | Increasing knowledge surrounding the social determinants of health and COVID-19 |
| Primordial prevention: advocacy | Calls for mobilization of people in power to protect vulnerable populations |
| Primary prevention | Preventing infection of COVID-19 through reducing exposure |
| Primary prevention: telehealth | Delivering healthcare through a virtual communication platform |
| Primary prevention: communication and education | Improving communication and public education surrounding COVID-19 |
| Primary prevention: quarantine | Preventing the spread of COVID-19 through physical separation |
| Primary prevention: protective measures | Preventing the spread of infection through personal protective equipment and infection control practices |
| Primary prevention: unintended consequences of the pandemic/containment | Mitigating negative effects of the COVID-19 pandemic and of enforced containment strategies unrelated to direct COVID-19 infection |
| Secondary prevention | Detecting and containing COVID-19 in those who are infected |
| Secondary prevention: COVID-19 testing | Detecting COVID-19 infection |
| Secondary prevention: contact tracing | Identifying individuals with potential exposure to COVID-19 cases |
| Secondary prevention: isolation of COVID-19 cases | Preventing the spread of COVID-19 from those who are infected |
| Tertiary prevention | Mitigating the complications of COVID-19 on those who are infected |
| Tertiary prevention: supports for COVID-19 patients and contacts | Supporting individuals who are infected or who have had exposure to someone who was infected with COVID-19 |
Definitions of public health prevention activities by level.
FIGURE 2
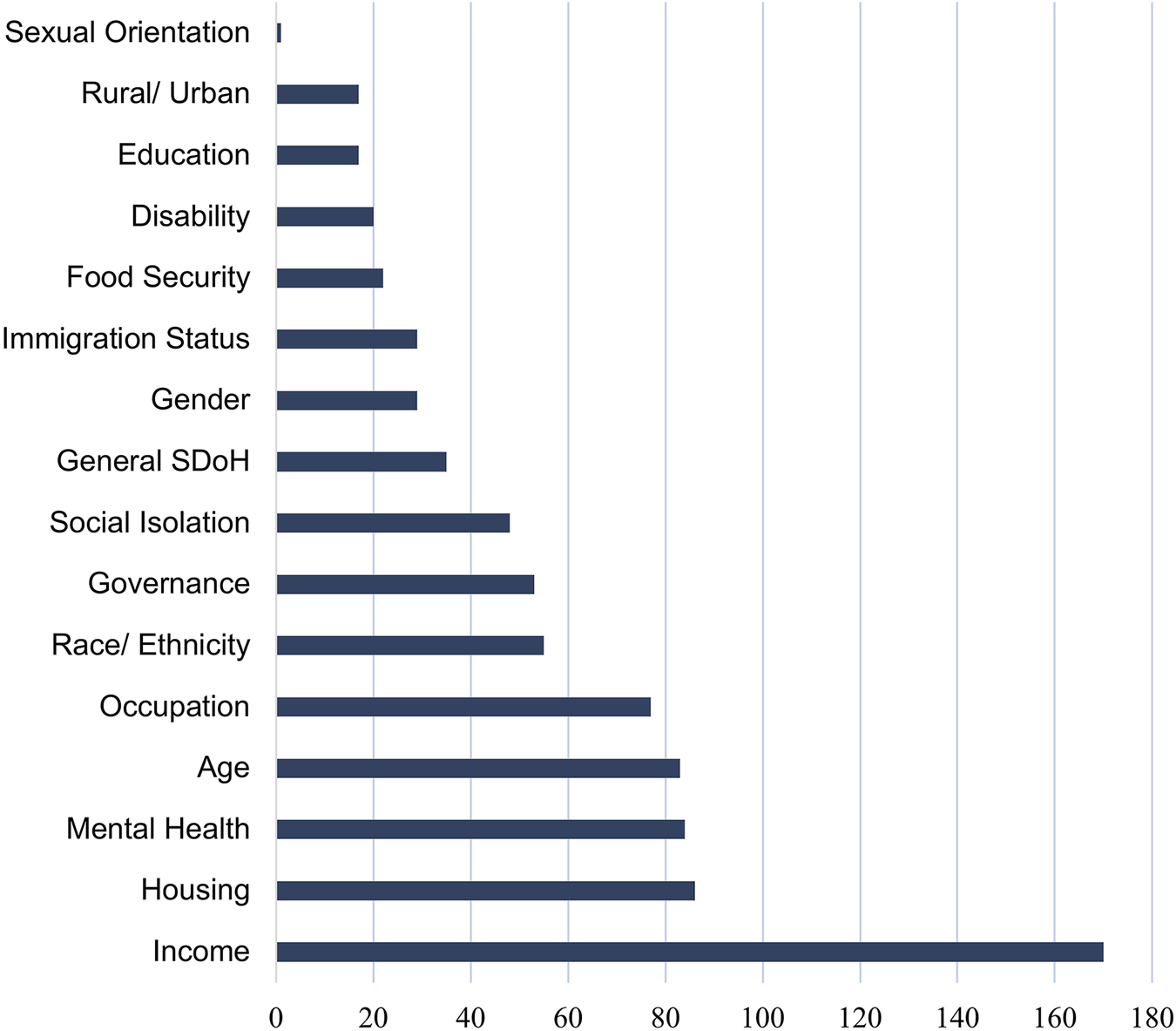
Graph of articles according to social determinant of health discussed (Systematic Review, Global, 2019-2020).
Primordial Prevention
Thirty-seven articles made general recommendations about primordial prevention to address the SDoH of COVID-19. Articles advocated for international cooperation, noting that providing support to low- and middle-income countries (LMIC) will strengthen the global COVID-19 response [19]. Authors recommended addressing longstanding systematic inequalities in income, housing and employment, to minimize social disparities and protect the most vulnerable [20]. Specific calls focused on supporting persons living with HIV [21], immigrants [22], elderly populations [22], homeless populations [22], and those with mental illness [22]. Some articles highlighted the need to include individuals from marginalized populations in the decision making processes [23], so that “their needs and barriers are understood and incorporated into a comprehensive response that works for everyone” [23].
Fifty-two articles proposed specific policy changes to address the SDoH of COVID-19. Many of these articles called for increased funding, for example, to improve health systems [23–25], to increase pandemic preparedness in prisons [26], and to increase access to opioid use disorder treatment programs [27]. Economic support policies for low-income individuals were important given the impact of containment strategies [28], but new policies must be equitable [29]. For example, one article recommended granting “temporary citizenship rights to every person in the country” [30]. Policies must not further disadvantage already marginalized persons [31]. Lau et al. advocated that “restrictions on freedom of movement must not be applied in a discriminatory way to displaced populations” [32]. Fourteen articles suggested new policies or policy changes that would directly assist marginalized populations [33]. These included reexamining judicial policies, like cash bail or pre-trial incarceration, to decrease the prison population [34], protecting the health of migrant workers [35], reducing enforcement of immigration policies that lead to detention [36], allowing homeless individuals to stay in hotel rooms [37], relaxing restrictions on controlled substances prescriptions for individuals with opioid use disorders [27], and increasing elder abuse penalties [38].
Fifty articles recommended COVID-19 research on the SDoH. Some articles advocated for COVID-19 data to be disaggregated by sex/gender [39], race/ethnicity [40], age [41], location [42], and socioeconomic status [43]. Authors called for research into the psychological effects of the pandemic and of containment strategies in general [44], and specific to elderly populations [45], pediatric populations [45], and illicit drug users [46]. Studies discussed the need for developing rapid point-of-care tests for LMIC that may have limited capacity for laboratory testing [47]. Ten articles highlighted the need for research into the impacts of COVID-19 and barriers to care for specific populations, including people who use drugs [48], victims of interpersonal violence [49], elderly populations [50], persons living with HIV [51], those accessing reproductive care [52], and individuals with dementia [53].
Fifteen articles called for health providers and organizations to engage in advocacy. Recommendations were directed at healthcare professionals to use their professional voices to advocate for disadvantaged groups [54–56]. Other articles called for advocacy from international health organizations [57] or governments [58]. Areas for advocacy included continued access to abortion care [59] and mental health treatment [60], increased social supports [61], increased child well-being [62], and increased supports for individuals with substance use disorders [63], who are homeless [55], or who are incarcerated [55].
Primary Prevention
Many articles focused on improving primary prevention for at-risk populations in order to combat COVID-19. Some recommended that LMIC focus on primary prevention strategies to avoid overburdening healthcare systems with limited capacity [64]. Yamey et al. call for a global resource allocation system “with national allocations determined through a fair and objective process” based on need [65].
Fifty articles suggested using telehealth to reduce COVID-19 exposure. Seven articles focused on extending the scope of, and reducing barriers to, telehealth, such as reducing the restrictions on reimbursement of telehealth services [66], allowing services to cross US State lines [67], and lifting restrictions on prescribing controlled substances [68]. Studies recommended making telehealth services more accessible, including to those without access to adequate technology or internet services [69], those with low technological literacy [70], and individuals with disabilities [71]. Recommendations included making internet access free for the duration of the pandemic [72], providing computers to low income families [67], or delivering services by phone [73]. Seventeen articles recommended telehealth services for mental health care in order to combat the impacts of the pandemic [74], as well as to provide continued care for those with existing mental health conditions [75]. Telehealth may also be used for populations who face barriers accessing care, such as individuals in rural communities [76], requiring stroke care [77], with dementia [78], with chronic health conditions or chronic pain [71], who are homeless [75], who are pregnant [79], with substance use disorders [46], with HIV [46], and those seeking contraceptive or abortion services [23].
Improving communication and education surrounding COVID-19 was discussed in 81 articles. Many articles highlighted specific populations with greater communication and education needs regarding COVID-19 prevention, including homeless populations [80], individuals with substance use disorders [48], residents of LTCs [81], elderly populations [38], and displaced populations [32]. This would require using a variety of media in order to reach a broad audience [82], including social media [83]. Authors focused on the need to ensure that “all public health messaging, technologies, and communications are accessible to all” [84]. This includes providing information in multiple languages [85], including sign languages [85]; in appropriate forms for varying literacy levels [86]; and in ways that are culturally appropriate [87]. Other accessibility recommendations included transparent masks to support those who rely on lip reading [84] and real-time captioning [84]. Articles advocated for increasing communication about the negative consequences of the COVID-19 pandemic not directly related to SARS-CoV-2 infection [88], such as reducing stigma and anti-Asian racism [89], increasing awareness of higher rates of intimate partner violence [90], and mitigating negative impacts on mental health [91].
Thirty-two articles focused on equitable quarantine practices. Six recommended improving quarantine facilities for individuals in unstable or group living situations [37], including reducing crowding in prisons [8], schools [92], and immigrant detention centres [93]. Ivers and Walton state: “we need radical social investments to support the most impoverished, and we must decongest prisons and release detained asylum seekers to prevent unnecessary deaths” [42]. Quarantining homeless populations was discussed, with calls for additional space for proper distancing [94], or for homeless individuals to use empty hotel rooms during quarantine [37]. Authors discussed measures that would allow individuals to stay home to reduce risk of infection [50], including increasing home care for elderly patients [70], remote treatment for individuals with opioid use disorders [95], and mailed prescriptions [96].
Thirty-four articles recommended improving protective measures for at-risk individuals. Some discussed the need for increased personal protective equipment (PPE) for specific groups, including workers with occupational exposure [97], in jails [34], in schools [92], for caregivers of home-care patients [98], in group living facilities [71], in LMIC [99], and in opioid treatment facilities [100]. Some recommended PPE be provided to individuals in high-risk populations, such as elderly [101] and those with disabilities [102], along with increased training on proper use specifically in the context of LTCs [54].
Eighty-two articles included suggestions about the unintended consequences of containment strategies. Articles discussed the consequences of school closures, with recommendations including providing meals to families who normally rely on school-provided meals [103], providing technology to low-income families so children can participate in online learning [92], providing resources for parents now providing full time childcare [92], and providing mental health resources to students who would normally access support at school [45]. Authors aimed to mitigate the increased risk of intimate partner violence and child abuse that accompanies containment strategies, including increased funding and advertising of domestic violence resources [104] and improved monitoring of children and women for signs of violence at home [62]. Some discussed the need to address stigma and discrimination associated with COVID-19 [105], specifically on the basis of race [106] and age [107].
Social isolation is an unintended consequence of containment. Many articles advocated for mental health supports to combat the psychological impacts of containment strategies, including for those with pre-existing mental health conditions [108], pediatric populations [109], healthcare workers [108], individuals with high-exposure occupations [110], and individuals with dementia [111]. Some recommended mitigating isolation through virtual and safe social contact for isolated elderly individuals [112], pediatric populations [113], those with mental health conditions [114], persons with HIV [115], and individuals in rural communities [116].
Secondary Prevention
Many articles discussed secondary prevention strategies for marginalized populations. Walenski and Del Rio argued that while testing, isolation and contact tracing in underserviced populations is important, it is crucial that this does not exacerbate the marginalization of these communities [20]. Similarly, Quaresima, Naldini and Cirillo suggested secondary prevention strategies should be community-based to ensure that they are understood and respect “local customs and cultural beliefs” [117].
Thirty-four articles advocated for improving COVID-19 testing for marginalized populations. Some commented on the need for fast and accessible testing in resource limited settings in order to control the spread of the virus [118]. Others called for free COVID-19 testing, regardless of citizenship status [20]. Eight articles advocated for increased testing accessibility within specific populations, such as individuals who are homeless [119], in LTCs [120], in immigrant detention facilities [121], in correctional facilities [34], and refugees [32]. Two authors called for wealthier countries to donate testing kits or funds to help control the spread of COVID-19 [122].
Fourteen articles discussed the isolation of COVID-19 cases in marginalized populations. Certain authors recommended providing facilities for isolation in group living settings, such as LTCs [123], immigration detention centres [121], and prisons [8]. Wurcel et al. stated that “there should be dedicated spaces within jails for isolation of persons with confirmed or suspected COVID-19 who are not ill enough to warrant hospital transfer” [34]. Two articles called for improved isolation facilities within hospitals [124]. Zhu et al. discussed protecting healthcare workers [124], and Gupta et al. focused on specialized isolation facilities for psychiatric inpatients [125]. Authors argued that unique support is needed for the isolation of COVID-19 cases in specific populations, including Indigenous peoples [126], homeless populations [127], and individuals with dementia [128].
Tertiary Prevention
For tertiary prevention, authors recommended creating systems and guidelines to improve care for cases of COVID-19 among vulnerable populations. This includes creating standardized guidelines for assessing and prioritizing patients in resource-limited settings in order to remove biases, such as ageism, from decision-making processes [107], as well as mitigating “additional emotional distress when allocating resources and denying care to patients” [99] on healthcare workers.
Twenty-one articles discussed tertiary prevention recommendations related to increased supports for COVID-19 patients among vulnerable populations. General calls for equitable access to treatment included a recommendation for Medicare for all Americans [97], for Medicaid co-payments to be waived for all Americans [127], for any COVID-19 therapeutics to be made available to all [42], and for any barriers to care to be addressed [129]. Recommendations for disadvantaged groups called for accessible care for international migrant workers [35], the uninsured [85], residents and staff of LTCs [85], incarcerated individuals [85], refugees or ICE detention centers [85], individuals in homeless shelters [85], rural populations [130], individuals who use drugs [48], and displaced populations [32]. Five articles recommended tailoring care to address both COVID-19 and existing comorbidities, including psychiatric illness [54], obesity [131], opioid use disorder [100], spinal cord injury [132], and malnourishment [133]. Articles recommended improving the quality of COVID-19 care for elderly patients through increasing community-based care [134], increasing the scope of care of clinicians in LTCs [135], and allowing visitors for elderly patients nearing death in hospital [136].
Discussion
We identified 338 commentaries, editorials, and opinion pieces in peer-reviewed publications that offered recommendations on addressing equity and SDoH during the COVID-19 pandemic. Recommendations for primordial prevention focused on improved policy, focused research, and targeted advocacy initiatives. Primary prevention includes accessible telehealth and communication strategies, and equitable quarantine and protective measures. Secondary prevention includes increased testing and more comprehensive isolation practices. Tertiary prevention recommendations advocated for increased supports for marginalized COVID-19 patients. Most articles focused on primordial and primary prevention of COVID-19. Recommendations were consistent, and the SDoH of COVID-19 are a global concern. Almost all SDoH were discussed, with income, housing, mental health, and age most commonly referenced.
Our findings fit with calls to address inequities related to COVID-19 [137, 138]. The US Centers for Disease Control created a health equity strategy for COVID-19, recognizing that the “health impact of COVID-19 has exposed long-standing inequities” [139]. The Pan-American Health Organization, American Medical Association, and Canadian National Collaborating Centre for Determinants of Health have also released responses, considerations, and resources to help inform and build equity-based COVID-19 policy and research [140–142].
Our review had limitations. The body of literature on COVID-19 continues to expand rapidly and our review shows only early articles on this subject. We only reviewed papers published in English. We used a public health prevention framework to organize the article recommendations; there are many other ways these articles could have been coded and analyzed. We attempted to minimize these biases by having multiple reviewers in article selection and extraction stages, as well as by using an established critical appraisal tool. There are further limitations in our methodology of choosing a rapid systemic review, and future work should consider not only a research update but a scoping review to fully analyze this subject.
This is the first synthesis of recommendations on addressing SDoH of COVID-19 and can inform public health strategies and policies. Vulnerable populations should be involved in decision-making processes to create relevant and just policy. Strategies should be adapted for local populations, contexts, and geographies. We know now that COVID-19 is disproportionately impacting individuals according to race, income, occupation, and housing status [7, 143–145]. These impacts can widen inequities in the future. With a third wave already here, the expert recommendations discussed in this rapid review need to move from discussion to implementation in order to lessen the inequitable global impact of COVID-19.
Statements
Author contributions
AP, CB, and TU conceptualized the study. AC-N, CB, and TU were involved in screening citations. Discrepancies were discussed with AP. AC-N, CB, and KW carried out data extraction and quality assessment. CB and KW developed the first draft, and all authors provided edits.
Funding
This project was supported in part by an Early Researcher Award from the Government of Ontario, held by AP, and a University of Toronto COVID-19 Student Engagement Award, which supported TU and CB. TU was also supported by a Canada Graduate Scholarship from the Canadian Institutes for Health Research. AC-N was supported by the Canadian Institutes for Health Research. KW was supported from the Innovation Funds from the Academic Health Science Centre Alternative Funding Plan. AP is supported as a Clinician-Scientist by the Department of Family and Community Medicine, Faculty of Medicine, University of Toronto, the Department of Family and Community Medicine, St. Michael’s Hospital, and the Li Ka Shing Knowledge Institute, St. Michael’s Hospital, by a fellowship from the Physicians’ Services Incorporated Foundation and as the Associate Director for Clinical Research at the University of Toronto Practice-Based Research Network (UTOPIAN). Funding for publication has been made possible through the Department of Family and Community Medicine, University of Toronto and the Department of Family and Community Medicine, St. Michael’s Hospital. The study sponsors had no role in study design; collection, analysis, and interpretation of data; writing the report; and the decision to submit the report for publication.
Acknowledgments
We thank the following individuals who assisted with reviewing citations for inclusion in this systematic review: Anne Marie Tynan, Rose Wang, Ayu Hapsari, Melissa Perri, Khysa Bishop, Shailesh Advani and Nada Dali. We would like to thank Robert Smith for his input throughout this study, and Carolyn Ziegler for her help with searching the literature.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/phrs.2021.1604031/full#supplementary-material
References
1.
Keating D Esteban C . Covid-19 Is Rapidly Becoming America’s Leading Cause of Death. Washington, DC: Washington Post [Internet] (2020). Available from: https://www.washingtonpost.com/outlook/2020/04/16/coronavirus-leading-cause-death/?arc404=true (Accessed June 12, 2020)
2.
World Health Organization. WHO Coronovirus Disease (COVID-19) Dashboard (2020).
3.
Montenovo L Jiang X Rojas FL Schmutte IM Simon KI Weinberg BA et al Determinants of Disparities in COVID-19 Job Losses. Cambridge, MA: NBER Work Pap (2020). p. 1689–99.
4.
Douglas M Katikireddi SV Taulbut M McKee M McCartney G . Mitigating the Wider Health Effects of Covid-19 Pandemic Response. BMJ [Internet] (2020). Available from: http://www.bmj.com/content/369/bmj.m1557.abstract. (Accessed June 12, 2020) 369m1557
5.
Jones BL Jones JS . Gov. Cuomo Is Wrong, Covid-19 Is Anything but an Equalizer. Washington Post [Internet] (2020). Available from: https://www.washingtonpost.com/outlook/2020/04/05/gov-cuomo-is-wrong-covid-19-is-anything-an-equalizer/ (Accessed June 12, 2020).
6.
Chen JT Krieger N . Revealing the Unequal burden of COVID-19 by Income, Race/ethnicity, and Household Crowding: US County vs. ZIP Code Analyses. J Public Health Manag Pract (2021) 27 Suppl 1. COVID-19 and Public Health: Looking Back, Moving Forward:S43–S56. 10.1097/PHH.0000000000001263
7.
Azar KMJ Shen Z Romanelli RJ Lockhart SH Smits K Robinson S et al Disparities in Outcomes Among COVID-19 Patients in A Large Health Care System in California. Health Aff (Millwood) (2020) 39:1253–62. 10.1377/hlthaff.2020.00598
8.
Akiyama M Spaulding A Rich J . Flattening the Curve for Incarcerated Populations - Covid-19 in Jails and Prisons. N Engl J Med (2020). 10.1056/nejmp2005687
9.
Tobolowsky FA Gonzales E Self JL Rao CY Keating R Marx GE et al COVID-19 Outbreak Among Three Affiliated Homeless Service Sites - King County, Washington, 2020. MMWR Morb Mortal Wkly Rep (2020) 69:523–6. 10.15585/mmwr.mm6917e2
10.
Gamio L . The Workers Who Face the Greatest Coronavirus Risk. New York Times (2020).
11.
Garritty C Gartlehner G Kamel C King V Nussbaumer-Streit B Stevens A et al Interim Guidance from the Cochrane Rapid Reviews Methods Group (2020). Available at: https://methods.cochrane.org/rapidreviews/sites/methods.cochrane.org.rapidreviews/files/public/uploads/cochrane_rr_-_guidance-23mar2020-final.pdf
12.
Moher D Liberati A Tetzlaff J Altman DG . Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA Statement. Bmj (2009) 339:b2535. Available from: http://www.bmj.com/cgi/doi/10.1136/bmj.b2535 (Accessed June 12, 2020). 10.1136/bmj.b2535
13.
World Health Organization. Commission on Social Determinants of Health. Geneva (2008).
14.
Upshaw TL Brown C Smith R Perri M Ziegler C Pinto AD et al Social Determinants of COVID-19 Incidence and Outcomes: A Rapid Review. PLoS ONE (2021) 16:e0248336. PLoS One [Internet]. 10.1371/journal.pone.0248336
15.
The Association of Faculties of Medicine of Canada. In: DonovanD, editor. AFMC Primer on Population Health [Internet]. Ottawa, ON, Canada: Association of Faculties of Medicine of Canada. Available from: https://ubccpd.ca/sites/ubccpd.ca/files/AFMC Primer on Population Health 2014-12-23 ((2).pdf (Accessed June 12, 2020).
16.
The Centre for Disease Control and Prevention. Prevention. Picture of America [Internet] (2017). Available from: https://www.cdc.gov/pictureofamerica/pdfs/picture_of_america_prevention.pdf (Accessed June 12, 2020).
17.
Pandve H . Quaternary Prevention: Need of the Hour. Medknow Publications & Media Pvt Ltd. J Fam Med Prim Care (2014) 3:309–10. Available from:. 10.4103/2249-4863.148090https://pubmed.ncbi.nlm.nih.gov/25657934 (Accessed June 12, 2020).
18.
Joanna Briggs Institute. Checklist for Text and Opinion (2017). Available from: http://joannabriggs.org/assets/docs/critical-appraisal-tools/JBI_Critical_Appraisal-Checklist_for_Text_and_Opinion2017.pdf (Accessed June 12, 2020), 5
19.
Buss PM Tobar S . COVID-19 and Opportunities for International Cooperation in Health. Cad Saude Publica Fundacao Oswaldo Cruz (2020) 36:e00066920. 10.1590/0102-311x00066920
20.
Walensky RP Del Rio C . From Mitigation to Containment of the COVID-19 Pandemic. Jama (2020) 323:1889–90. 10.1001/jama.2020.6572
21.
Shiau S Krause KD Valera P Swaminathan S Halkitis PN . The Burden of COVID-19 in People Living with HIV: A Syndemic Perspective. In: AIDS Behav, 1–6. Springer (2020).
22.
Galea S Merchant RM Lurie N . The Mental Health Consequences of COVID-19 and Physical Distancing. JAMA Intern Med (2020) 180:817–8. 10.1001/jamainternmed.2020.1562
23.
John N Casey SE Carino G McGovern T . Lessons Never Learned: Crisis and Gender‐based Violence. Developing World Bioeth (2020) 20:65–8. Blackwell Publishing Ltd. 10.1111/dewb.12261
24.
Nkengasong JN Mankoula W . Looming Threat of COVID-19 Infection in Africa: Act Collectively, and Fast. The Lancet (2020) 395:841–2. 10.1016/s0140-6736(20)30464-5
25.
Paintsil E . COVID-19 Threatens Health Systems in Sub-saharan Africa: The Eye of the Crocodile. J Clin Invest Am Soc Clin Invest (2020) 130:2741–4. 10.1172/jci138493
26.
Yang H Thompson JR . Fighting Covid-19 Outbreaks in Prisons. Bmj (2020) 369:m1362. 10.1136/bmj.m1362
27.
Becker WC Fiellin DA . When Epidemics Collide: Coronavirus Disease 2019 (COVID-19) and the Opioid Crisis. Ann Intern Med (2020) 173:59–60. 10.7326/m20-1210
28.
Azim D Kumar S Nasim S Arif TB Nanjiani D . COVID-19 as a Psychological Contagion: A New Pandora’s Box to Close? Infect Control Hosp Epidemiol. Cambridge University Press (2020). p. 1–2.
29.
Smith JA Judd J . COVID‐19: Vulnerability and the Power of Privilege in a Pandemic. Health Promot J Austral (2020) 31:158–60. 10.1002/hpja.333
30.
Bhopal RS . COVID-19: Immense Necessity and Challenges in Meeting the Needs of Minorities, Especially Asylum Seekers and Undocumented Migrants. Public Health (2020) 182:161–2. 10.1016/j.puhe.2020.04.010
31.
Agoramoorthy G . Infect Control Hosp Epidemiol. Cambridge University Press (2020). 10.1017/ice.2020.140India Fights Hard to Neutralize the Spread of Covid-19
32.
Lau LS Samari G Moresky RT Casey SE Kachur SP Roberts LF et al COVID-19 in Humanitarian Settings and Lessons Learned from Past Epidemics. Nat Med (2020) 26:647–8. 10.1038/s41591-020-0851-2
33.
Carta MG Romano F Orrù G . The True Challenges of the Covid-19 Epidemics: The Need for Essential Levels of Care for All. Open Respir Med J (2020) 14:8–9. 10.2174/1874306402014010008
34.
Wurcel AG Dauria E Zaller N Nijhawan A Beckwith C Nowotny K et al Spotlight on Jails: COVID-19 Mitigation Policies Needed Now. Clin Infect Dis [Internet] (2020). Available from: https://academic.oup.com/cid/advance-article-abstract/doi/10.1093/cid/ciaa346/5812998.
35.
Liem A Wang C Wariyanti Y Latkin CA Hall BJ . The Neglected Health of International Migrant Workers in the COVID-19 Epidemic. The Lancet Psychiatry (2020) 7:e20. 10.1016/s2215-0366(20)30076-6
36.
Lopez MM Holmes SM . Raids on Immigrant Communities during the Pandemic Threaten the Country's Public Health. Am J Public Health (2020) 110:958–9. 10.2105/ajph.2020.305704
37.
Patrick K Stanbrook MB Laupacis A . Social Distancing to Combat COVID-19: We Are All on the Front Line. CMAJ (2020) 192:E516. cmaj.200606. 10.1503/cmaj.200606
38.
Han SD Mosqueda L . Elder Abuse in the COVID ‐19 Era. J Am Geriatr Soc (2020) 68:1386–7. 10.1111/jgs.16496
39.
Wenham C Smith J Morgan R . COVID-19: the Gendered Impacts of the Outbreak. The Lancet (2020) 395:846–8. 10.1016/s0140-6736(20)30526-2
40.
Zavaleta C . COVID-19: Review Indigenous Peoples' Data. Nature (2020) 580:185. 10.1038/d41586-020-01032-1
41.
The Lancet . The Gendered Dimensions of COVID-19. The Lancet (2020) 395:1168. 10.1016/s0140-6736(20)30823-0
42.
Ivers LC Walton DA . COVID-19: Global Health Equity in Pandemic Response. Am J Trop Med Hyg Am Soc Trop Med Hyg (2020) 102:1149–50. 10.4269/ajtmh.20-0260
43.
Hargreaves J Davey C Hargreaves J Davey C Auerbach J Blanchard J et al Three Lessons for the COVID-19 Response from Pandemic HIV. The Lancet HIV (2020) 7:e309–e311. 10.1016/s2352-3018(20)30110-7
44.
DePierro J Lowe S Katz C . Lessons Learned from 9/11: Mental Health Perspectives on the COVID-19 Pandemic. Psychiatry Res. Elsevier Ireland Ltd (2020). p. 288. 10.1016/j.psychres.2020.113024
45.
Holmes EA O'Connor RC Perry VH Tracey I Wessely S Arseneault L et al The Lancet Psychiatry, 7. Elsevier (2020). p. 547–60. 10.1016/s2215-0366(20)30168-1Multidisciplinary Research Priorities for the COVID-19 Pandemic: a Call for Action for Mental Health ScienceThe Lancet Psychiatry
46.
Carrico AW Horvath KJ Grov C Moskowitz JT Pahwa S Pallikkuth S et al Double Jeopardy: Methamphetamine Use and HIV as Risk Factors for COVID-19. AIDS Behav. Springer (2020). p. 1–4.
47.
van der Werf S Peltekian C . Facing Challenges with the Novel Coronavirus SARS-CoV-2 Outbreak. Virologie (Montrouge) (2020) 24:e12–15. 10.1684/vir.2020.0826
48.
Jenkins WD Bolinski R Bresett J Van Ham B Fletcher S Walters S et al COVID-19 During the Opioid Epidemic - Exacerbation of Stigma and Vulnerabilities. J Rural Heal (2021) 37 (1):172–4. 10.1111/jrh.12442
49.
Mukhtar S . Preparedness and Proactive Infection Control Measures of Pakistan during COVID-19 Pandemic Outbreak. Res Soc Adm Pharm (2020) S1551-7411:30373–9. 10.1016/j.sapharm.2020.04.011
50.
Nicol GE Piccirillo JF Mulsant BH Lenze EJ . Action at a Distance: Geriatric Research during a Pandemic. J Am Geriatr Soc (2020) 68:922–5. 10.1111/jgs.16443
51.
Drain PK Garrett N . SARS-CoV-2 Pandemic Expanding in Sub-saharan Africa: Considerations for COVID-19 in People Living with HIV. EClinicalMedicine (2020) 22:100342. 10.1016/j.eclinm.2020.100342
52.
Ahonsi B . A Research Agenda on the Sexual and Reproductive Health Dimensions of the COVID-19 Pandemic in Africa. Afr J Reprod Health (2020) 24:22–5. 10.29063/ajrh2020/v24i1.3
53.
Alzheimer’s Disease Research Enterprise in the Era of COVID-19/SARS-CoV-2. Alzheimer’s Dement, 16. John Wiley & Sons (2020). p. 587–8.
54.
Shalev D Shapiro PA . Epidemic Psychiatry: The Opportunities and Challenges of COVID-19. Gen Hosp Psychiatry (2020) 64:68–71. 10.1016/j.genhosppsych.2020.03.009
55.
Walter-McCabe HA . Coronavirus Pandemic Calls for an Immediate Social Work Response. Soc Work Public Health (2020) 35:69–72. 10.1080/19371918.2020.1751533
56.
Patel L Elliott A Storlie E Kethireddy R Goodman K Dickey W . Ethical and Legal Challenges during the COVID-19 Pandemic – Are We Thinking about Rural Hospitals?J Rural Heal (2021) 37 (1):175–8. 10.1111/jrh.12447
57.
Salazar Mather TP Gallo Marin B Medina Perez G Christophers B Paiva ML Oliva R et al Love in the Time of COVID-19: Negligence in the Nicaraguan Response. Lancet Glob Health (2020) 8:e773. 10.1016/s2214-109x(20)30131-5
58.
Vessey JA Betz CL . Everything Old Is New Again: COVID-19 and Public Health. J Pediatr Nurs W.B Saunders (2020) 52:A7–A8. 10.1016/j.pedn.2020.03.014
59.
Bayefsky MJ Bartz D Watson KL . Abortion during the CoviD-19 Pandemic - Ensuring Access to an Essential Health Service. N Engl J Med (2020) 382:e47. 10.1056/nejmp2008006
60.
Fiorillo A Gorwood P . The Consequences of the COVID-19 Pandemic on Mental Health and Implications for Clinical Practice. Eur Psychiatr (2020) 63:e32. 10.1192/j.eurpsy.2020.35
61.
Jung SJ Jun JY . Mental Health and Psychological Intervention amid COVID-19 Outbreak: Perspectives from South Korea. Yonsei Med J (2020) 61:271–2. 10.3349/ymj.2020.61.4.271
62.
Humphreys KL Myint MT Zeanah CH . Increased Risk for Family Violence during the COVID-19 Pandemic. Pediatrics. American Academy of Pediatrics (AAP (2020). p. e20200982.
63.
Volkow ND . Collision of the COVID-19 and Addiction Epidemics. Ann Intern Med (2020) 173:61–2. 10.7326/m20-1212
64.
Monjur MR Hassan MZ . Infect Control Hosp Epidemiol. Cambridge University Press (2020). p. 1.Early Phases of COVID-19 Management in a Low-Income Country: Case of Bangladesh
65.
Yamey G Schäferhoff M Hatchett R Pate M Zhao F McDade KK . Ensuring Global Access to COVID-19 Vaccines. The Lancet (2020) 395:1405–6. 10.1016/s0140-6736(20)30763-7
66.
Sodhi M . Telehealth Policies Impacting Federally Qualified Health Centers in Face of COVID-19. J Rural Heal (2021) 37 (1):158–60. 10.1111/jrh.12445
67.
Goldschmidt K . The COVID-19 Pandemic: Technology Use to Support the Wellbeing of Children. J Pediatr Nurs (2020) 53:88–90. 10.1016/j.pedn.2020.04.013
68.
Whaibeh E Mahmoud H Naal H . Telemental Health in the Context of a Pandemic: the COVID-19 Experience. Curr Treat Options Psych (2020) 7:198–202. 10.1007/s40501-020-00210-2
69.
Calton B Abedini N Fratkin M . Telemedicine in the Time of Coronavirus. J Pain Symptom Manage (2020) 60:e12–e14. 10.1016/j.jpainsymman.2020.03.019
70.
Steinman MA Perry L Perissinotto CM . Meeting the Care Needs of Older Adults Isolated at Home during the COVID-19 Pandemic. JAMA Intern Med (2020) 180:819–20. 10.1001/jamainternmed.2020.1661
71.
Duong MT Karlawish J . Caregiving at a Physical Distance: Initial Thoughts for COVID ‐19 and beyond. J Am Geriatr Soc (2020) 68:1170–2. 10.1111/jgs.16495
72.
Yip PSF Chau PH Physical Distancing and Emotional Closeness amidst COVID-19. Crisis (2020) 41 (3). 153–5. 10.1027/0227-5910/a000710
73.
Mahmood S Hasan K Colder Carras M Labrique A . Global Preparedness against COVID-19: We Must Leverage the Power of Digital Health. JMIR Public Health Surveill (2020) 6:e18980. 10.2196/18980
74.
Khoury R Karam G . In: Impact of COVID-19 on Mental Healthcare of Older Adults: Insights from Lebanon (Middle East). Cambridge University Press (2020). p. 1–4.Int Psychogeriatrics
75.
Kar SK Arafat SMY Marthoenis M Kabir R . Homeless Mentally Ill People and COVID-19 Pandemic: The Two-Way Sword for LMICs. Asian J Psychiatr. Elsevier B.V. (2020). p. 51.
76.
Sood A Pollard C Suer KL Vlahovich K Walker J . Caring for Miners During the Coronavirus Disease-2019 (COVID-19) Pandemic. J Rural Health (2021) 37 (1). 165–8. 10.1111/jrh.12444
77.
Markus HS Brainin M . COVID-19 and Stroke-A Global World Stroke Organization Perspective. Int J Stroke (2020) 15:361–4. 10.1177/1747493020923472
78.
Flint AJ Bingham KS Iaboni A . Effect of COVID-19 on the Mental Health Care of Older People in Canada. Int Psychogeriatrics. Cambridge University Press (2020).
79.
Rashidi Fakari F Simbar M . Coronavirus Pandemic and Worries during Pregnancy; a Letter to Editor. Arch Acad Emerg Med [Internet] (2020) 8:e21. Available from: http://journals.sbmu.ac.ir/aaem (Accessed June 12, 2020)
80.
Neto MLR de Souza RI Quezado RMM Mendonça ECS de Araújo TI Luz DCRP et al When Basic Supplies Are Missing, what to Do? Specific Demands of the Local Street Population in Times of Coronavirus - a Concern of Social Psychiatry. Psychiatry Res (2020) 288:112939. 10.1016/j.psychres.2020.112939
81.
Lai C-C Wang J-H Ko W-C Yen M-Y Lu M-C Lee C-M et al COVID-19 in Long-Term Care Facilities: An Upcoming Threat that Cannot Be Ignored. J Microbiol Immunol Infect (2020) 53:444–6. 10.1016/j.jmii.2020.04.008
82.
Louis-Jean J Cenat K Sanon D Stvil R . Coronavirus (COVID-19) in Haiti: A Call for Action. J Community Health (2020) 45:437–9. 10.1007/s10900-020-00825-9
83.
Merchant RM Lurie N . Social Media and Emergency Preparedness in Response to Novel Coronavirus. Jama (2020) 323:2011–2. 10.1001/jama.2020.4469
84.
Pineda VS Corburn J . Disability, Urban Health Equity, and the Coronavirus Pandemic: Promoting Cities for All. J Urban Health (2020) 97:336–41. 10.1007/s11524-020-00437-7
85.
Berger ZD Evans NG Phelan AL Silverman RD . Covid-19: Control Measures Must Be Equitable and Inclusive. Bmj (2020) 368:m1141. 10.1136/bmj.m1141
86.
Hargreaves S Kumar BN McKee M Jones L Veizis A . Europe's Migrant Containment Policies Threaten the Response to Covid-19. Bmj (2020) 368:m1213. 10.1136/bmj.m1213
87.
Sharma S Lawrence C Giovinazzo F . Transplant Programs during COVID‐19: Unintended Consequences for Health Inequality. Am J Transpl (2020) 20:1954–5. 10.1111/ajt.15931
88.
Tandon PN . COVID-19: Impact on Health of People & Wealth of Nations. Indian J Med Res (2020) 151:121–3. 10.4103/ijmr.IJMR_664_20
89.
Malta M Rimoin AW Strathdee SA . The Coronavirus 2019-nCoV Epidemic: Is Hindsight 20/20?. EClinicalMedicine (2020) 20:100289. 10.1016/j.eclinm.2020.100289
90.
van Gelder N Peterman A Potts A O'Donnell M Thompson K Shah N et al COVID-19: Reducing the Risk of Infection Might Increase the Risk of Intimate Partner Violence. EClinicalMedicine (2020) 21:100348. 10.1016/j.eclinm.2020.100348
91.
Druss BG . JAMA Psychiatry. American Medical Association (2020). 10.1001/jamapsychiatry.2020.0894Addressing the COVID-19 Pandemic in Populations with Serious Mental Illness
92.
Armitage R Nellums LB . Considering Inequalities in the School Closure Response to COVID-19. Lancet Glob Health (2020) 8:e644. 10.1016/s2214-109x(20)30116-9
93.
Page KR Venkataramani M Beyrer C Polk S . Undocumented U.S. Immigrants and Covid-19. N Engl J Med (2020) 382:e62. 10.1056/nejmp2005953
94.
Tsai J Wilson M . COVID-19: a Potential Public Health Problem for Homeless Populations. The Lancet Public Health(s) (2020) 5:e186–e187. Published by Elsevier Ltd. This is an Open Access article under the CC BY 4.0 license. 10.1016/s2468-2667(20)30053-0
95.
Alexander GC Stoller KB Haffajee RL Saloner B . An Epidemic in the Midst of a Pandemic: Opioid Use Disorder and COVID-19. Ann Intern Med (2020) 173:57–8. 10.7326/M20-1141
96.
Hedima EW Adeyemi MS Ikunaiye NY Community Pharmacists: On the Frontline of Health Service against COVID-19 in LMICs, S1551-7411. Res Soc Adm Pharm. Elsevier Inc. (2020). p. 30385.
97.
Castillo B . Virulent Greed. Natl Nurse, 9. Silver Spring, MD: Silver Spring (2020).
98.
Tseng TG Wu HL Ku HC Tai CJ . The Impact of the COVID-19 Pandemic on Disabled and Hospice Home Care Patients. J Gerontol A Biol Sci Med Sci NLM (Medline) (2020) 75(9):e128–e129. 10.1093/gerona/glaa081
99.
Ademuyiwa AO Bekele A Berhea AB Borgstein E Capo-Chichi N Derbew M et al COVID-19 Preparedness within the Surgical, Obstetric, and Anesthetic Ecosystem in Sub-saharan Africa. Ann Surg NLM (Medline) (2020) 272:e9–e13. 10.1097/sla.0000000000003964
100.
Sun Y Bao Y Kosten T Strang J Shi J Lu L . Editorial: Challenges to Opioid Use Disorders during COVID‐19. Am J Addict (2020) 29:174–5. 10.1111/ajad.13031
101.
Feng S Shen C Xia N Song W Fan M Cowling BJ . Rational Use of Face Masks in the COVID-19 Pandemic. Lancet Respir Med (2020) 8:434–6. 10.1016/s2213-2600(20)30134-x
102.
Armitage R Nellums LB . The COVID-19 Response Must Be Disability Inclusive. The Lancet Public Health (2020) 5:e257. 10.1016/s2468-2667(20)30076-1
103.
Cowling BJ Aiello AE . Public Health Measures to Slow Community Spread of Coronavirus Disease 2019. J Infect Dis NLM (Medline) (2020) 221:1749–51. 10.1093/infdis/jiaa123
104.
Bradbury-Jones C Isham L . The Pandemic Paradox: The Consequences of COVID-19 on Domestic Violence. J Clin Nurs (2020) 29:2047–9. 10.1111/jocn.15296
105.
Usher K Durkin J Bhullar N . The COVID‐19 Pandemic and Mental Health Impacts. Int J Ment Health Nurs (2020) 29:315–8. 10.1111/inm.12726
106.
Al-Quteimat OM Amer Mustafa A . Amer AM. SARS-CoV-2 Outbreak: How Can Pharmacists Help?. Res Soc Adm Pharm Elsevier Inc (2020) 17(2):480–2. 10.1016/j.sapharm.2020.03.018
107.
Ayalon L Chasteen A Diehl M Levy B Neupert SD Rothermund K et al Aging in Times of the COVID-19 Pandemic: Avoiding Ageism and Fostering Intergenerational Solidarity. J Gerontol B Psychol Sci Soc Sci NLM (Medline) (2020) 76(2):e49–e52. 10.1093/geronb/gbaa051
108.
Cullen W Gulati G Kelly BD . Mental Health in the COVID-19 Pandemic. QJM [Internet] (2020) 113:311–2. Available from: https://academic.oup.com/qjmed/article-abstract/doi/10.1093/qjmed/hcaa110/5813733 (Accessed June 12, 2020). 10.1093/qjmed/hcaa110
109.
Liu JJ Bao Y Huang X Shi J Lu L . Mental Health Considerations for Children Quarantined Because of COVID-19. Lancet Child Adolesc Health (2020) 4:347–9. 10.1016/s2352-4642(20)30096-1
110.
Koh D , Occupational Risks for COVID-19 Infection, Occup Med (Chic Ill), 70. Oxford University Press (2020). p. 3–5. 10.1093/occmed/kqaa036
111.
Wang H Li T Barbarino P Gauthier S Brodaty H Molinuevo JL et al Dementia Care during COVID-19. The Lancet (2020) 395:1190–1. 10.1016/s0140-6736(20)30755-8
112.
Gostin LO Hodge JG Wiley LF . Presidential Powers and Response to COVID-19. Jama (2020) 323:1547–8. 10.1001/jama.2020.4335
113.
Nicol GE Karp JF Reiersen AM Zorumski CF Lenze EJ . "What Were You before the War?" Repurposing Psychiatry during the COVID-19 Pandemic. J Clin Psychiatry (2020) 81:81. 10.4088/JCP.20com13373
114.
Kavoor AR , 51. Elsevier B.V. (2020). p. 102051. 10.1016/j.ajp.2020.102051COVID-19 in People with Mental Illness: Challenges and VulnerabilitiesAsian J Psychiatry
115.
Marziali ME Card KG McLinden T Wang L Trigg J Hogg RS . Physical Distancing in COVID-19 May Exacerbate Experiences of Social Isolation Among People Living with HIV. AIDS Behav. Springer (2020). p. 1–3.
116.
Monteith LL Holliday R Brown TL Brenner LA Mohatt NV . Preventing Suicide in Rural Communities during the COVID-19 Pandemic. J Rural Heal (2021) 37 (1):179–84. 10.1111/jrh.12448
117.
Quaresima V Naldini MM Cirillo DM . The Prospects for the SARS-CoV-2 Pandemic in Africa. EMBO Mol Med (2020) 12:e12488. 10.15252/emmm.202012488
118.
Ghebreyesus TA Swaminathan S . Scientists Are Sprinting to Outpace the Novel Coronavirus. The Lancet (2020) 395:762–4. Available from: https://www.who.int/dg/speeches/detail/who (Accessed June 12, 2020). 10.1016/s0140-6736(20)30420-7
119.
Tsai J Wilson M . COVID-19: a Potential Public Health Problem for Homeless Populations. The Author(s). Published by Elsevier Ltd. This is an Open Access article under the CC BY 4.0 license. Lancet Public Heal [Internet] (2020) 5:e186–7. 10.1016/S2468-2667(20)30053-0
120.
Gardner W States D Bagley N . The Coronavirus and the Risks to the Elderly in Long-Term Care. J Aging Soc Pol (2020) 32:310–5. 10.1080/08959420.2020.1750543
121.
Meyer JP Franco-Paredes C Parmar P Yasin F Gartland M . COVID-19 and the Coming Epidemic in US Immigration Detention Centres. Lancet Infect Dis (2020) 20:646–8. 10.1016/s1473-3099(20)30295-4
122.
Mohamed K Rodríguez-Román E Rahmani F Zhang H Ivanovska M Makka SA et al Borderless Collaboration Is Needed for COVID-19; A Disease that Knows No Borders. Infect Control Hosp Epidemiol (2020) 1–2. 10.1017/ice.2020.162
123.
Gaur S Dumyati G Nace DA Jump RLP . Unprecedented Solutions for Extraordinary Times: Helping Long-Term Care Settings deal with the COVID-19 Pandemic. Infect Control Hosp Epidemiol (2020) 41:729–30. 10.1017/ice.2020.98
124.
Zhu Y Chen L Ji H Xi M Fang Y Li Y . The Risk and Prevention of Novel Coronavirus Pneumonia Infections Among Inpatients in Psychiatric Hospitals. Neurosci Bull (2020) 36:299–302. 10.1007/s12264-020-00476-9
125.
Gupta N Singhai M Garg S Shah D Sood V Singh SK . The Missing Pieces in the Jigsaw and Need for Cohesive Research amidst Coronavirus Infectious Disease 2019 Global Response. Med J Armed Forces India (2020) 76:132–5. 10.1016/j.mjafi.2020.04.001
126.
Ferrante L Fearnside PM . Protect Indigenous Peoples from COVID-19. Science (2020) 368:251. 10.1126/science.abc0073
127.
Bachireddy C Chen C Dar M . Securing the Safety Net and Protecting Public Health during a Pandemic. Jama (2020) 323:2009–10. 10.1001/jama.2020.4272
128.
Zimmerman S Sloane PD Katz PR Kunze M O'Neil K Resnick B . The Need to Include Assisted Living in Responding to the COVID-19 Pandemic. J Am Med Directors Assoc (2020) 21:572–5. 10.1016/j.jamda.2020.03.024
129.
Parmet WE Sinha MS . Covid-19 - the Law and Limits of Quarantine. N Engl J Med (2020) 382:e28–3. 10.1056/NEJMp2004211
130.
Agyeman AA Laar A Ofori-Asenso R . Will COVID-19 Be a Litmus Test for post-Ebola Sub-saharan Africa? J Med Virol. John Wiley & Sons (2020). p. 1–3.
131.
Dietz W Santos‐Burgoa C . Obesity and its Implications for COVID‐19 Mortality. Obesity (2020) 28:1005. 10.1002/oby.22818
132.
Palipana D . COVID-19 and Spinal Cord Injuries: The Viewpoint from an Emergency Department Resident with Quadriplegia. Emerg Med Australas (2020) 32 (4):692–3. 10.1111/1742-6723.13525
133.
Barazzoni R Bischoff SC Breda J Wickramasinghe K Krznaric Z Nitzan D et al ESPEN Expert Statements and Practical Guidance for Nutritional Management of Individuals with SARS-CoV-2 Infection. Clin Nutr (2020) 39:1631–8. 10.1016/j.clnu.2020.03.022
134.
Mazumder H Hossain MM Das A . Geriatric Care during Public Health Emergencies: Lessons Learned from Novel Corona Virus Disease (COVID-19) Pandemic. J Gerontological Soc Work (2020) 63:257–8. 10.1080/01634372.2020.1746723
135.
Young HM Fick DM . Public Health and Ethics Intersect at New Levels with Gerontological Nursing in COVID-19 Pandemic. J Gerontol Nurs (2020) 46:4–7. Available from:. 10.3928/00989134-20200403-01https://bit.ly/3dLeIpA (Accessed June 12, 2020).
136.
O’Neill D . Protecting Our Longevity Dividend during Covid-19. Ir Med J (2020) 113:50.
137.
Wang Z Tang K . Combating COVID-19: Health Equity Matters. Nat Med (2020) 26:458. 10.1038/s41591-020-0823-6
138.
Berkowitz SA Cené CW Chatterjee A . Covid-19 and Health Equity - Time to Think Big. N Engl J Med (2020) 383:e76. 10.1056/NEJMp2021209
139.
The Centre for Disease Control and Prevention. CDC COVID-19 Response Health Equity Strategy: Accelerating Progress towards Reducing COVID-19 Disparities and Achieving Health Equity [Internet] (2020). Available from: https://www.cdc.gov/coronavirus/2019-ncov/downloads/community/CDC-Strategy.pdf (Accessed June 12, 2020)
140.
Pan American Health Organization. Promoting Health Equity, Gender and Ethnic equality, and Human Rights in COVID-19 Responses: Key Considerations [Internet] (2020). Available from: https://iris.paho.org/handle/10665.2/52058 (Accessed June 12, 2020)
141.
American Medical Association. COVID-19 Health Equity Resources [Internet]. 2020 [cited 2020 Aug 15]. Available from: https://www.ama-assn.org/delivering-care/health-equity/covid-19-health-equity-resources (Accessed June 12, 2020)
142.
National Collaborating Centre for Determinants of Health. Equity-informed Responses to COVID-19 (2020).
143.
Lusignan Sde Dorward J Correa A Jones N Akinyemi O Amirthalingam G et al Risk Factors for SARS-CoV-2 Among Patients in the Oxford Royal College of General Practitioners Research and Surveillance Centre Primary Care Network: a Cross-Sectional Study. Lancet Infect Dis (2020). 10.1016/s1473-3099(20)30371-6
144.
Hastie CE Mackay DF Ho F Celis-Morales CA Katikireddi SV Niedzwiedz CL et al Vitamin D Concentrations and COVID-19 Infection in UK Biobank. Diabetes Metab Syndr Clin Res Rev (2020) 14:561–5. 10.1016/j.dsx.2020.04.050
145.
Mosites E Parker EM Clarke KEN Gaeta JM Baggett TP Imbert E et al Assessment of SARS-CoV-2 Infection Prevalence in Homeless Shelters - Four U.S. Cities, March 27-April 15, 2020, 69. Atlanta, GA: MMWR Morb Mortal Wkly Rep (2020). 10.15585/mmwr.mm6917e1
Summary
Keywords
public health, social determinants of health, SARS-CoV-2, health equity, COVID-19, prevention
Citation
Brown C, Wilkins K, Craig-Neil A, Upshaw T and Pinto AD (2022) Reducing Inequities During the COVID-19 Pandemic: A Rapid Review and Synthesis of Public Health Recommendations. Public Health Rev 42:1604031. doi: 10.3389/phrs.2021.1604031
Received
11 February 2021
Accepted
04 November 2021
Published
17 January 2022
Volume
42 - 2021
Edited by
Kasia Czabanowska, Maastricht University, Netherlands
Reviewed by
Susanne Unverzagt, Martin Luther University of Halle-Wittenberg, Germany
Updates
Copyright
© 2022 Brown, Wilkins, Craig-Neil, Upshaw and Pinto.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms. PHR is edited by the Swiss School of Public Health (SSPH+) in a partnership with the Association of Schools of Public Health of the European Region (ASPHER)+
*Correspondence: Andrew David Pinto, andrew.pinto@utoronto.ca
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.