- 1Unisanté, University Center for Primary Care and Public Health, Department of Epidemiology and Health Systems, University of Lausanne, Lausanne, Switzerland
- 2La Source School of Nursing, HES–SO University of Applied Sciences and Arts Western Switzerland, Lausanne, Switzerland
- 3Lausanne University Hospital, Lausanne, Switzerland
Objectives: The Swiss Cohort of Healthcare Professionals and Informal Caregivers (SCOHPICA) was created to study the career trajectories, retention intentions, and wellbeing of healthcare professionals (HCPs), addressing challenges such as staff turnover, low job satisfaction and burnout.
Methods: SCOHPICA is a prospective open cohort. An electronic questionnaire was used to collect data from HCPs across multiple healthcare settings in Switzerland, encompassing the intention to stay in the profession, wellbeing, and various organizational, psychosocial, occupational and sociodemographic determinants.
Results: The first (2022) baseline sample included 1707 HCPs from over 20 professions. Notably, 13% did not intend to stay in their profession, with intermediate caregivers (24%), registered nurses (17%) and pharmacists (17%) reporting the highest rates. Pharmacists scored lowest in wellbeing. Across determinants, pharmacists, physicians, and registered nurses reported worse scores for workload and work-life balance. Nursing professions had lower scores in various determinants, including influence at work, staffing and resource adequacy, and possibilities for development.
Conclusion: SCOHPICA will provide critical insights on HCPs’ work conditions and experiences, supporting health workforce monitoring and management, and informing policy-making to ensure high-quality healthcare delivery.
Introduction
Health workforce issues are high in the agenda of European policymakers, due to the multiple challenges affecting the wellbeing of health professionals’ and the functioning of health systems [1, 2]. These challenges are partly driven by labor market failures, health emergencies, underinvestment in the sector, health and demographic trends, as well as the rise of noncommunicable diseases [3]. The COVID-19 pandemic has intensified the issues, leading to increased demand for health services, higher levels of stress and burnout among health workers, including higher risks to their health and safety due to inadequate working conditions [4, 5].
Healthcare professionals (HCPs) are pivotal to health systems. Ensuring a sufficient number of professionals, equitable distribution and providing adequate training and working conditions are essential for delivering accessible and high-quality care [6]. The World Health Organization (WHO) has outlined objectives for 2030 to enhance performance and investment in the health workforce, strengthen health institution capacities, and improve data collection on HCPs [2]. The Working for Health 2022–2030 Action Plan [1] addresses these objectives, emphasizing the urgent need for investment in health workers’ education, skills, employment, and protection, as put forward by the Seventy-fourth World Health Assembly Resolution [7].
Across Europe, the challenges confronting the health workforce have been acute, with the WHO reporting staff shortages driven by insufficient recruitment and retention of HCPs, unattractive working conditions, limited opportunities for ongoing professional development, and poor mental health among health workers [6]. In Switzerland, working conditions for HCPs have deteriorated, exacerbated by the COVID-19 pandemic [8–10]. Career departures are a significant concern, with approximately 12% of physicians and 16%–19% of nurses and intermediate caregivers leaving their professions [11]. Projections suggest that by 2029, there will be a need for 70,000 nurses to both replace the existing workforce and meet population healthcare needs [12]. However, coverage rates are predicted to fall below 80%, indicating a substantial workforce deficit [12]. Forecasts also predict shortages in various medical specialties, necessitating reliance on foreign workforce [13]. Addressing these challenges requires comprehensive data to inform strategic actions aimed at safeguarding the health workforce, ensuring the resilience of health systems, and promoting population health.
Health workforce research has shown that organizational (e.g., workload, work environment, recognition, leadership), psychosocial (e.g., cohesion and social support), psychological (e.g., stress, resilience) and sociodemographic (e.g., age, gender) determinants may affect HCPs’ wellbeing and intention to stay in the job/profession [14–18]. In Switzerland, studies have also investigated job stress, job satisfaction, burnout, and intention to stay in/leave the job/profession among HCPs [19–31]. However, Swiss and international studies have mostly focused on physicians or nurses, often within a limited scope of settings (mainly hospitals), leaving other healthcare professions understudied [6, 32]. As a recent review has stressed [18], only a few studies have addressed issues of wellbeing and retention intentions among allied health workforce. Additionally, most studies have used cross-sectional designs, which do not capture the longitudinal experience of HCPs. In sum, nationwide and longitudinal research spanning multiple healthcare sectors and professions has been limited. Such research is essential to grasp the determinants influencing HCPs’ career trajectories, wellbeing, and intentions to stay in their profession. As the WHO stressed, such paucity of data and research may hamper the adequate planning, monitoring, coordination and management of the health workforce [6].
This paper presents findings on the wellbeing, intention to stay in the profession, and the determinants of these outcomes, among HCPs in Switzerland. It is part of the Swiss Cohort of Healthcare Professionals and Informal Caregivers (SCOHPICA) project, which aims to gather comprehensive nationwide and longitudinal data on the professional trajectories, experiences and conditions of HCPs and informal caregivers (ICs). While the SCOHPICA project encompasses both HCPs and informal caregivers (ICs) in its longitudinal study, this paper concentrates on HCPs, using data from SCOHPICA’s first baseline survey.
Methods
Study Design, Population, and Data
This study draws on an analysis of the first 2022 baseline survey from the HCPs’ cohort of SCOHPICA. SCOHPICA is a national prospective open cohort study that collects data from all types of HCPs (e.g., general practitioners, specialist physicians, medical assistants, nurses, nurse aides, paramedics, psychologists, physiotherapists, dieticians, pharmacists, etc.) who work in direct contact with patients across different healthcare settings (e.g., hospitals, private practices, clinics, nursing homes, community services, etc.) in Switzerland, regardless of their employment status (i.e., whether self-employed or salaried). Students, retired HCPs, and those who were not working at the time of the baseline survey are not eligible to participate. The questionnaire was developed in the Swiss national languages, thereby individuals who cannot read French, German or Italian were not included in the study. SCOPICA’s study protocol details the specifics of the study design, recruitment process, ethical considerations and planned analyses [33].
SCOHPICA’s first baseline survey was conducted from 1 October 2022 to 31 January 2023. While the survey aimed to reach at least 1,500 HCPs for adequate measurement precision, it obtained responses from 1853 HCPs. Data collection was carried out through a self-administered electronic questionnaire, which was made available to HCPs on SCOHPICA website [34]. This questionnaire, comprising approximately 140 questions, was designed to be completed in around 30 min. Participants provided their informed consent before starting the questionnaire.
Intention to Stay in the Profession and Wellbeing of Healthcare Professionals
Two main outcome variables of the SCOHPICA study were considered. The first variable was the HCPs’ intention to stay in their profession, assessed through the question, “If your working conditions/environment were to remain the same over the next few months, would you stay in your current profession?” Responses were measured on a 5-point scale, ranging from “No, not at all” to “Yes, absolutely.” The second variable was the wellbeing of HCPs, which was evaluated using the Flourish Index [35]. This index consists of 10 items, each rated on a 10-point scale spanning from 1 indicating a low wellbeing to 10 a high wellbeing. The index’s score range also spans from 1 (low wellbeing) to 10 (high wellbeing).
Determinants of the Intention to Stay in the Profession and Wellbeing
SCOHPICA’s baseline questionnaire was designed to gather data on a range of determinants that may influence HCPs' wellbeing and intention to stay in the profession. The selection of these determinants was informed by preliminary literature reviews [17, 18], and consultations with SCOHPICA’s expert panel. Details on the instruments used for measuring these determinants can be found in SCOHPICA’s protocol [33].
In this paper, we focus on the determinants that showed acceptable internal consistency, as evaluated using Cronbach’s alpha. These determinants are detailed, along with the number of items and scales used, primarily using Likert scales, as follows:
- Workload: 5 items; 5-point scale from “Less than once a month/Never” to “Several times a day,” score range of 1–5.
- Control over Working Time: 4 items; 5-point scale from “Never/Hardly ever” to “Very often/Always,” score range of 0–100.
- Staffing and Resource Adequacy: 5 items; 4-point scale from “Strongly disagree” to “Strongly agree,” score range of 1–4.
- Possibilities for Development: 3 items; 5-point scale from “To a very large extent” to “To a very small extent,” score range of 0–100.
- Work-life Balance: 5 items; 4-point scale from “Yes, absolutely” to “No, not at all,” score range of 0–100.
- Leadership: 7 items; 5-point scale from “Never/Hardly ever” to “Very often/Always,” score range of 1–5.
- Influence at Work: 6 items; 5-point scale from “Never/Hardly ever” to “Very often/Always,” score range of 0–100.
- Sense of Community at Work: 3 items; 5-point scale from “Never/Hardly ever” to “Very often/Always”, score range of 0–100.
- Interprofessional Collaboration: 14 items; 5-point scale from “Strongly disagree” to “Strongly agree,” score range of 1–5.
- Recognition at Work: 12 items; 5-point scale from “Strongly disagree” to “Strongly agree,” score range of 1–5.
- Preparedness to Work Reality: 2 items were analyzed separately, 1) “Do you feel that, overall, your training has prepared you well for your professional activity?” 2) “In my work, I use the full extent of my practice,” 5-point scale from “Strongly disagree” to “Strongly agree,” score range of 1–5.
- Meaning of Work: 2 items; 5-point scale from “To a very large extent” to “To a very small extent”, score range of 0–100.
- Intolerance to Uncertainty: 6 items; 5-point scale from “Not at all my characteristic” to “Entirely my characteristic,” score range of 1–5.
- Burnout: 1 item; 5-point scale from “I do not have burnout symptoms” to “I feel completely burned out,” score range of 1–5.
- Self-rated Health: 1 item; 5-point scale from “Excellent” to “Poor,” score range of 1–5.
- Job Satisfaction: 1 item; 4-point scale from “Very unsatisfied” to “Very satisfied,” score range of 0–100.
All determinants reflect a positive experience or condition with higher scores, except for workload, burnout, and self-rated health, where higher scores indicate a negative experience or condition.
Socioprofessional and Sociodemographic Variables
The baseline questionnaire gathered data on aspects related to HCPs’ work and occupation:
- Current profession: paramedic, physician, medical assistant, pharmacist, midwife, registered nurse, physiotherapist, etc.
- Occupational context: public hospital, private hospital, solo/two-physician practice, group practice, home care, nursing home, pharmacy, etc.
- Occupational sector: somatic care, home care, mental health, rehabilitation, long-term care, other.
- Country of training: open-ended answer.
- Numbers of years in the profession: number of years.
- Employment rate: from 0% to 100%.
- Hours worked per week: number of hours.
- Managerial responsibilities: yes, no.
- Monthly individual income (in CHF): below 2000, 2001–4,000, 4,001–6,000, 6,001–8,000, 8,001–10000, more than 10,000.
Sociodemographic data was also collected:
- Gender: man, woman, other, do not wish to answer.
- Age: <35 years, 35–44 years, 45–54 years, ≥55 years.
- Nationality: Swiss, Swiss and other nationality, foreign national.
- Marital/partnership status: single, cohabiting partner/registered partnership/married, separated/dissolved partnership/divorced, widowed.
- Children: yes, no.
- Informal caregiving: yes currently, yes in the past, no.
- Language: German, French, Italian.
Statistical Analyses
We conducted descriptive analyses to summarize the characteristics of each variable in our study. We calculated the median and interquartile range (IQR) for the score of each determinant, both for the overall sample and for specific professional groups which had more than 50 participants. When the median score of a professional group differed from the other professions, we used a non-parametric equality-of-medians test to assess the difference in median scores. This test offers the advantage of not requiring the data to be normally distributed and is less sensitive to outliers compared to a t-test. In our analysis, p-values of 0.05 and smaller were reported. However, we only considered p-values of 0.01 or lower as statistically significant, to account for multiple testing and adopt a more conservative approach. This adjustment was made to ensure greater rigor and reliability in our findings.
For handling occasional missing data, we applied listwise deletion, which involved excluding the cases with missing responses from the analyses. For cases with missing responses in determinant items, we calculated the score using the mean of the items to which participants did respond. This was only applied if participants had answered more than 50% of the items within a determinant and at least two items within a determinant.
All statistical analyses were carried out using StataBE 18.
Results
Description of the Sample
The 2022 SCOHPICA baseline survey comprised 1707 HCPs, following data cleaning that excluded ineligible cases and those with partial answers. Sociodemographic characteristics of the survey participants are presented in Table 1. Women accounted for 78.1% of the participants. In terms of age distribution, 30.8% were under 35 years old, 48.9% were between 35 and 54 years old, and 20.4% were 55 years or older. Swiss nationals made up 82.2%, while foreign nationals constituted 17.8%. Regarding marital status, 56.1% of the respondents were married or cohabiting, 33.1% were single, and 10.1% were separated or divorced. 53.7% of the participants had children. Concerning informal caregiving, 23% were current caregivers, and 12.1% had been caregivers in the past. Most participants completed the questionnaire in French (50.5%) or German (43%), with a smaller proportion in Italian (6.5%).
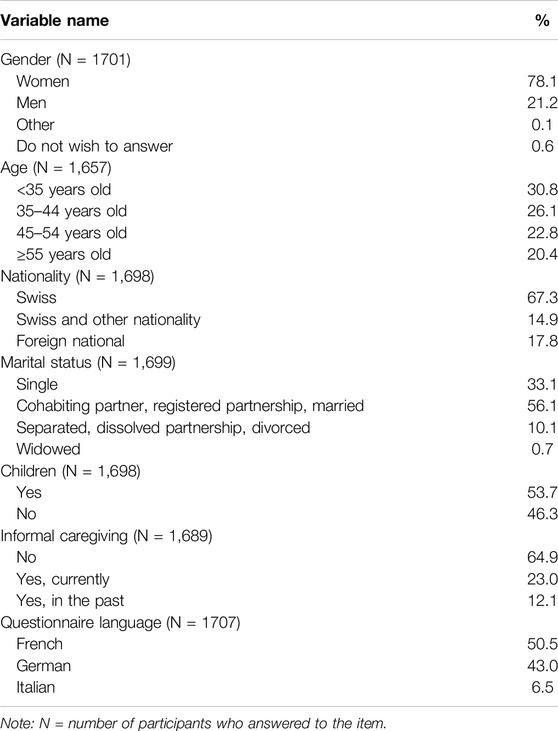
Table 1. Sociodemographic characteristics of 1707 healthcare professionals, Swiss Cohort of Healthcare Professionals and Informal Caregivers baseline data 2022. (Switzerland, 2024).
Socioprofessional characteristics of HCPs are presented in Table 2. HCPs from over 20 different professions responded to the survey, with ten professional categories having 50 or more participants, which included registered nurses as the largest group (32.4%), followed by physicians (12.4%), physiotherapists (9.1%), occupational therapists (5.3%), medical assistants (4.4%), pharmacists (4.2%), advanced practice nurses and paramedics (each at 3.6%), and dietitians and intermediate caregivers (3.4% and 3.2%, respectively).
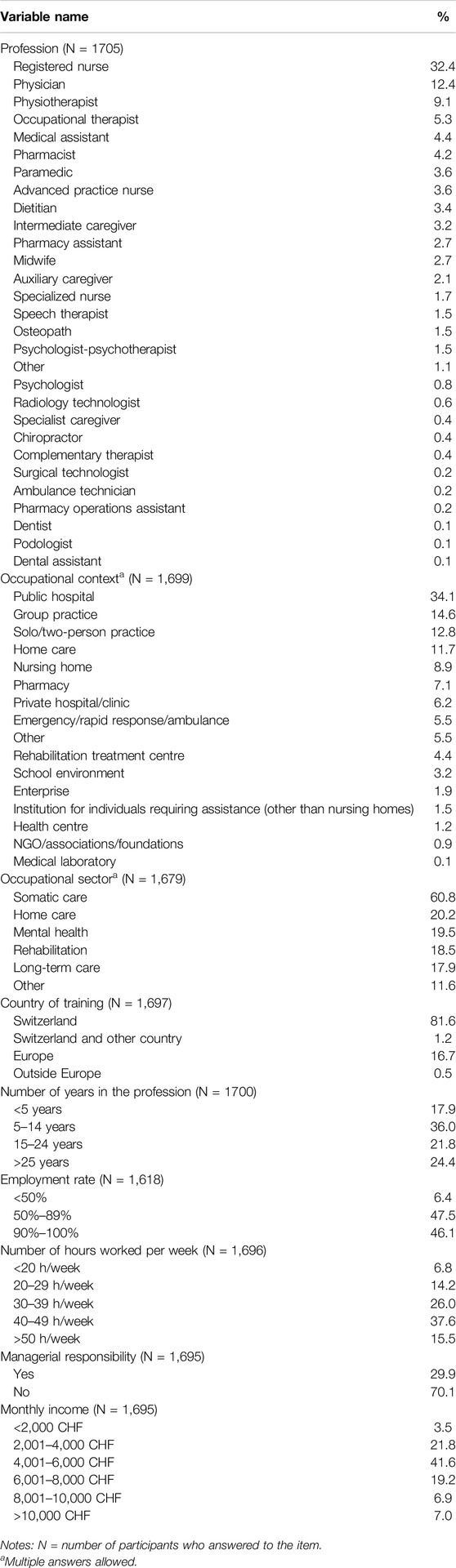
Table 2. Socioprofessional characteristics of 1707 healthcare professionals, Swiss Cohort of Healthcare Professionals and Informal Caregivers baseline data 2022 (Switzerland, 2024).
Regarding the occupational context, 34.1% of the participants worked in public hospitals, followed by 14.6% in group practices and 12.8% in solo or two-person practices. The majority of respondents were involved in somatic care (60.8%), followed by home care (20.2%), mental health (19.5%), rehabilitation (18.5%), and long-term care (17.9%). Most HCPs received their training in Switzerland (82.8%), with a smaller proportion trained in Europe (16.7%). In terms of experience, 36% had 5–14 years of experience, 21.8% had 15–24 years, and 24.4% had over 25 years. Work hours varied, with 37.6% working 40–49 h per week, 26% working 30–39 h, and 15.5% working more than 50 h. Managerial responsibility was held by 29.9% of the participants, and the largest group (41.6%) earned 4,001–6,000 CHF per month.
Intention to Stay in the Profession and Wellbeing of Healthcare Professionals
Figure 1 illustrates HCPs’ intention to stay in their profession. Overall, 13.2% of HCPs did not intend to stay in their profession when combining the responses of “no, not at all” and “no, not really.” This rate was highest among intermediate caregivers (23%), registered nurses (18%), pharmacists (17%), paramedics (13%) and medical assistants (13%). Regarding wellbeing, as measured by the Flourish Index, the overall score was 7.8 (Table 3). Pharmacists reported the lowest wellbeing median score at 7.5, followed by occupational therapists (7.6), registered nurses (7.7) and physicians (7.7), although their scores were not significantly lower than the other professions. Figure 2 depicts HCPs’ wellbeing scores by profession.
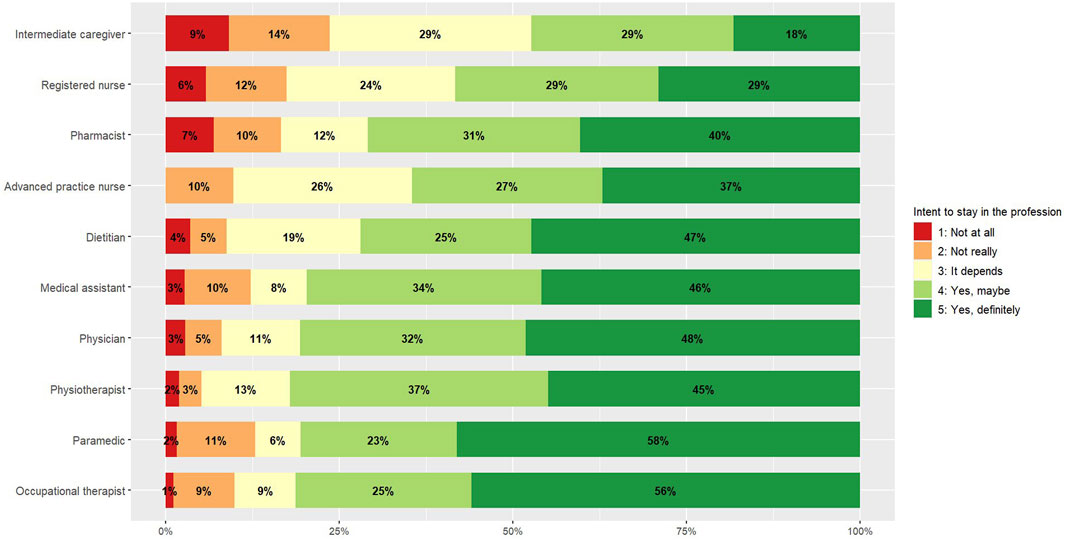
Figure 1. Intention to stay in the profession, by profession (Switzerland, 2024). Note: Results are presented only for professional categories with ≥50 participants.
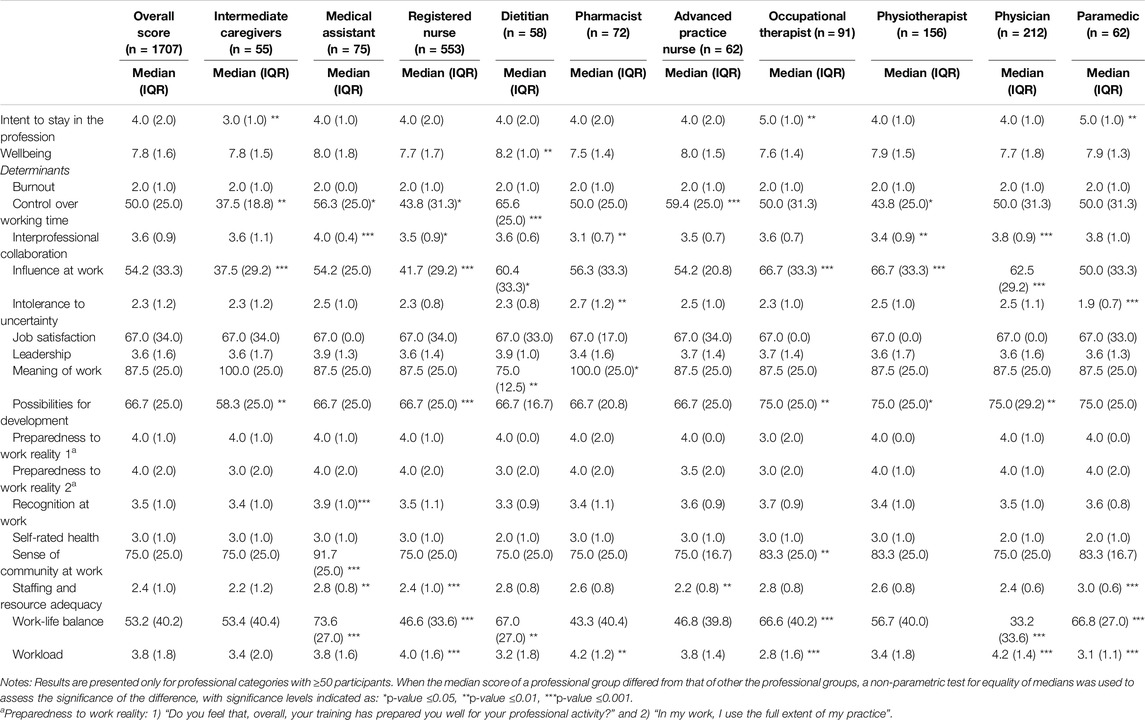
Table 3. Healthcare professionals' wellbeing, intention to stay in the profession and determinants, by profession, median and interquartile range (IQR) (Switzerland, 2024).
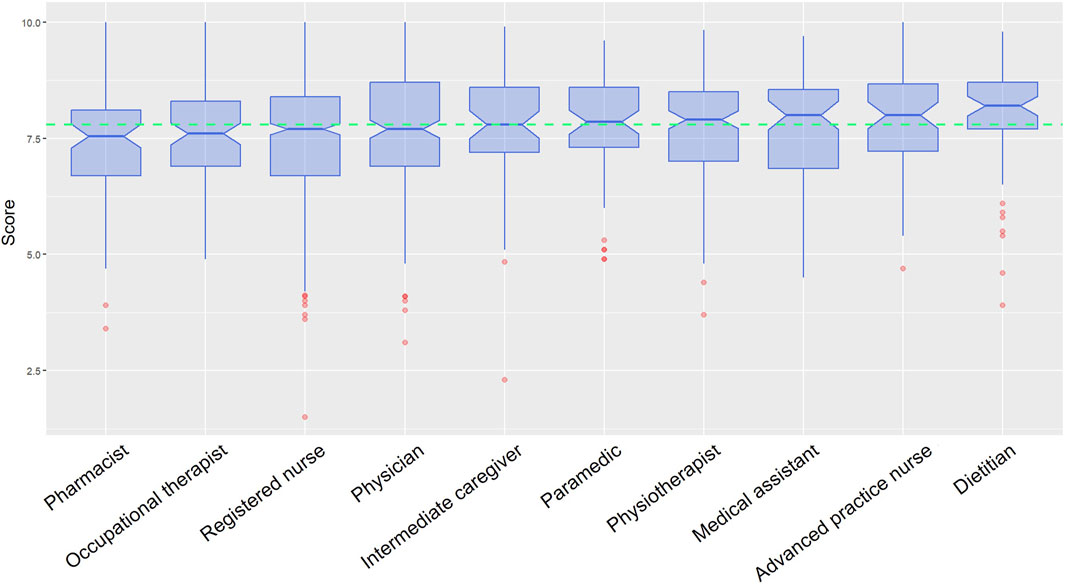
Figure 2. Wellbeing (Flourish index), by profession (Switzerland, 2024). Note: Results are presented only for professional categories with ≥50 participants.
Determinants of the Intention to Stay in the Profession and Wellbeing
Table 3 presents the results of the determinants of HCPs’ intention to stay in the profession and wellbeing. The median score for workload was 3.8, with registered nurses, pharmacists, and physicians experiencing significantly higher workloads than the median of other professions. Compared to other professional groups, registered nurses reported significantly lower scores in staffing and resource adequacy, possibilities for development, work-life balance and influence at work. Physicians also had a significantly lower work-life balance score. Physiotherapists and pharmacists reported lower scores in interprofessional collaboration. Advanced practice nurses scored lower in staffing and resource adequacy, paramedics in intolerance to uncertainty, dietitians in meaning of work, and intermediate caregivers in control over working time, possibilities for development and influence at work. Medical assistants and occupational therapists, in contrast, did not exhibit lower scores in any determinant compared to other professional groups. Finally, no significant differences were observed between professional groups in terms of leadership, job satisfaction and self-rated health scores.
Discussion
This paper presented findings on the wellbeing and intention to stay in the profession of HCPs, along with the determinants of these outcomes, based on data from 1707 HCPs in SCOHPICA’s first baseline survey (2022). Notably, the data collection spanned over 20 healthcare professions across various healthcare settings throughout Switzerland. The results indicated that a concerning proportion of HCPs (13%) did not intend to stay in their profession should their current working conditions persist. This figure was highest among intermediate caregivers (23%), registered nurses (18%) and pharmacists (17%). Furthermore, the results highlighted divergences between professions across different factors. Registered nurses, physicians, and pharmacists reported the highest workload levels and lower work-life balance scores. Nursing professions (registered nurses, advanced practice nurses and intermediate caregivers) faced common challenges related to staffing and resource adequacy, influence at work, opportunities for development and control over working time.
The high turnover intentions observed in our study among intermediate caregivers and registered nurses align with findings from a Swiss study, which reported an 18.5% intention to leave the profession among caregivers and nurses [27]. Similarly, another study spanning four European countries found that 13.6% of nurses expressed the intention to leave their profession [36]. However, accurately comparing the prevalence of turnover intentions across different studies is challenging due to variations in definitions and measurements. Some studies may focus on intentions to stay in or leave the job, while others focus on staying in/leaving the profession. The timeframe used to assess these intentions also varies, with some studies evaluating turnover intentions prospectively over the next several years and others retrospectively, considering intentions within the past year. Some studies do not specify any timeframe at all. In our study, we focused on the intention to stay in the profession, considering the near future (i.e., “the next few months”) as the timeframe, as in the studies by Maniscalco and colleagues [36] and Hammig [27]. Surveying healthcare professionals (HCPs) who have already left the profession would ideally provide better insights into their turnover intentions. However, recruiting these individuals presents significant challenges and feasibility issues.
This study identified several determinants that disproportionately affected certain professions. Previous research has stressed the significant association of these determinants with intentions to leave those professions. For instance, we observed that physicians experienced workload and work-life balance issues, and pharmacists grappled with workload and lower wellbeing, while previous studies highlighted these determinants as significant drivers of turnover intentions among physicians and pharmacists [18, 24, 27, 29, 37, 38]. Additionally, nursing professions faced challenges related to workload, work-life balance, staffing and resource adequacy, influence at work, opportunities for development and control over working time, all of which were shown to contribute to nurses leaving their profession in past research [20, 23, 27, 29]. Notably, our results revealed that both intermediate caregivers and registered nurses (the two professions with the lowest intention to stay in the profession) had the lowest scores in control over working time, influence at work and possibilities for development, compared to other professions, characterizing these two professions.
Practical implications of our results involve the need for targeted interventions to improve working conditions, reduce turnover intentions, and enhance wellbeing among HCPs, which are relevant both in the Swiss context and internationally. Importantly, our study highlights the necessity of adopting a comparative perspective that considers multiple healthcare professions and their unique challenges. Acknowledging the differences and commonalities between professions will enable the development of appropriate strategies. Hence, future research, policymakers and healthcare managers should identify and prioritize the key factors influencing turnover intentions across different professions. Additionally, monitoring the impact of these interventions on HCP’s turnover intentions and wellbeing in future research will help inform and refine retention strategies.
Specific recommendations include enhancing working conditions by implementing measures to manage and reduce workload, particularly for physicians, pharmacists, and nurses. This involves promoting initiatives that support work-life balance and provide access to staff support services and resources. Increasing HCPs’ control over their schedules is essential, allowing for more autonomy and flexibility to accommodate personal needs and reduce burnout. Professional development and career growth should be fostered by developing clear career paths and providing opportunities for continuing education and mentoring programs. Retention strategies should be developed for professions with high turnover intentions, such as intermediate caregivers and registered nurses. These strategies should aim at increasing empowerment in the workplace and may include recognition and reward systems, flexible scheduling, enhanced autonomy, and clear pathways for career progression. Additionally, conducting regular constructive feedback sessions can allow for adjustments in working conditions, reduce turnover, and provide insights to inform retention strategies.
Interestingly, our study found that 18% of HCPs were foreign nationals, with an equal percentage having received their training abroad. This underscores the reliance on international healthcare workers and their importance to the Swiss healthcare system, as pointed out in previous reports [12, 13]. Health workforce migration is an international challenge affecting many countries, as highlighted in a recent WHO report [6], and is strongly related to the issue of health workforce shortages. Given the crucial role of these migration movements, our future research will examine these issues in greater detail, exploring their relationship to HCPs’ intentions to stay in the profession and their wellbeing.
This is the first study providing insights into HCPs’ intention to stay in their professions, their wellbeing, and the determinants thereof, across multiple healthcare professions and settings throughout an entire country. Previous research lacked this breadth of coverage, hindering comparisons of diverse experiences and conditions among HCPs. Such comprehensive information is highly valuable for healthcare stakeholders, especially given the lack of accurate and thorough data on HCPs, and the highlighted workforce shortages within the Swiss healthcare system [12, 13]. Hence, SCOHPICA has the potential to play a crucial role in monitoring the conditions of healthcare workers, thereby supporting the design of management and policy interventions aimed at improving working conditions and retaining HCPs. This aligns with international recommendations to enhance data collection on the health workforce, not only to address pressing challenges such as staff shortages but also to effectively plan, manage, coordinate and inform decisions concerning the health workforce [1, 2, 6].
This study is part of the broader SCOHPICA project framework, which employs a cohort design that will be complemented by life history calendars. Subsequent investigations within this project will delve into the professional trajectories of HCPs using longitudinal analysis, as well as optimal matching and clustering techniques to create typologies of professional trajectories. A longitudinal perspective will be important for understanding the transition from intention to the actual decision to stay in/leave the profession. Additionally, future analyses will apply advanced statistical methodologies, including structural equation modeling, to elucidate the intricate relationships and mediating pathways among the determinants affecting HCPs’ professional trajectories, retention intentions, and wellbeing.
It is important to acknowledge the limitations of this study. Firstly, due to the impracticality of drawing representative samples of all HCPs and obtaining their contact emails in Switzerland, the study employed non-probability sampling. Secondly, certain professional categories may have been underrepresented, particularly those that are more challenging to recruit, and smaller sample sizes might have influenced the ability to detect statistically significant differences. However, we anticipate increased participation from a diverse range of professions in future data collection waves. In fact, as an open cohort, SCOHPICA will recruit new participants annually, thereby increasing the cohort size, enhancing statistical power and representativeness, and enabling subgroup and stratified analyses. For upcoming survey waves, the SCOHPICA team will continue to collaborate closely with professional associations of HCPs at both national and regional levels, and with employers of HCPs (e.g., hospitals, home care, etc.). This should promote participation in the survey, particularly among professions that were underrepresented in the first survey wave. To reach HCPs, we employ targeted communication and recruitment strategies. For example, we provide communication packages to associations, enabling them to share the SCOHPICA questionnaire link with their members via emails, newsletters, and websites. Thirdly, there is a risk of selection bias if individuals who choose not to respond to the survey differ significantly in their characteristics from those who do participate. Without data on non-respondents, we are not able to assess the extent of this bias. Lastly, this study relies on self-reported data, which can be subject to recall and social desirability biases, leading to potential measurement bias. To mitigate these biases, the SCOHPICA questionnaire incorporated validated questions and underwent pre-testing to ensure its reliability and accuracy.
To conclude, the comprehensive scope of SCOHPICA’s study fills a significant gap in existing research, covering all healthcare professions across different sectors and providing critical insights into the health workforce. With the scarcity of data on HCPs and the pressing need for improved workforce planning, SCOHPICA’s findings will be crucial for addressing challenges such as attrition, staff shortages, inadequate working conditions, increased workloads, and burnout in the healthcare workforce. By supporting the monitoring, planning, and management of Switzerland’s health workforce, SCOHPICA will play a key role in addressing health system challenges, informing future policies, implementing targeted interventions, and promoting the delivery of high-quality care.
Ethics Statement
The studies involving humans were approved by the Cantonal Research Ethics Committee Vaud (CER-VD), Switzerland (project ID: 2022-01410). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author Contributions
Conceptualization: VJ, JJ, EZ, LR, TC, AO, IG, and IP-B; funding acquisition: IP-B; methodology: VJ, JJ, EZ, LR, TC, AB, IG, and IP-B; project administration: IP-B; supervision: IP-B, AB, and IG; writing–original draft: VJ; writing–review and editing: VJ, JJ, EZ, LR, TC, AB, IG, and IP-B. All authors contributed to the article and approved the submitted version.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. The project has been funded by different sources. It has received starting grants from the Swiss Academies of Arts and Sciences, the Swiss Federal Office of Public Health, the Swiss Health Observatory and the Fondation pour l’Université de Lausanne. There is no involvement nor influence of these funders on any stage of the present study, including its protocol, design, data collection and analyses, and results publications and dissemination.
Conflict of Interest
The authors declare that they do not have any conflicts of interest.
Acknowledgments
The conceptualization and launch of this project would not have been possible without the support of partners from different institutions, administrative and communication staff, part-time assistants and interns from Unisanté, the Institut et Haute Ecole de la Santé La Source and the Lausanne University Hospital, scientific experts and SCOHPICA’s advisory panel including Aide et soins à domicile Suisse, ARTISET, Association suisse des infirmières et infirmiers, Competence Network Health Workforce, la Conférence des directrices et directeurs cantonaux de la santé, Médecins de famille et de l’enfance Suisse, pharmaSuisse, Swiss Federal Office of Public Health, Swiss Health Observatory, the Swiss Medical Association, Swiss Nurse Leaders, Unisanté and University of Lausanne. We also would like to thank all individuals and the professional, state and umbrella associations of HCPs at national and cantonal level who supported SCOHPICA’s first 2022 recruitment phase of HCPs). Last but not least, we would like to thank all the participants for contributing their time and participating in this study.
References
1. World Health Organization. Working for Health 2022–2030 Action Plan: Education and Employment. Geneva: World Health Organization (2022).
2. World Health Organization. Global Strategy on Human Resources for Health: Workforce 2030. Geneva: World Health Organization (2016).
3. World Health Organization. Working for Health and Growth: Investing in the Health Workforce. Report of the High-Level Commission on Health Employment and Economic Growth. Geneva: WHO (2016).
4. World Health Organization. Health Workforce Policy and Management in the Context of the COVID-19 Pandemic Response. Geneva: WHO (2020). Contract No.: WHO/2019-nCoV/health_workforce/2020.1.
5. Vanhaecht, K, Seys, D, Bruyneel, L, Cox, B, Kaesemans, G, Cloet, M, et al. COVID-19 Is Having a Destructive Impact on Health-Care Workers' Mental Well-Being. Int J Qual Health Care (2021) 33(1):mzaa158. doi:10.1093/intqhc/mzaa158
6. World Health Organization. Health and Care Workforce in Europe: Time to Act. Geneva: World Health Organization Regional Office for Europe (2022).
7. World Health Organization. Resolution WHA74.14: Protecting, Safeguarding and Investing in the Health and Care Workforce (2021).
8. Weilenmann, S, Ernst, J, Petry, H, Pfaltz, MC, Sazpinar, O, Gehrke, S, et al. Health Care Workers' Mental Health During the First Weeks of the SARS-CoV-2 Pandemic in Switzerland-A Cross-Sectional Study. Front Psychiatry (2021) 12:594340. doi:10.3389/fpsyt.2021.594340
9. Stierli, R, Rozsnyai, Z, Felber, R, Jörg, R, Kraft, E, Exadaktylos, AK, et al. Primary Care Physician Workforce 2020 to 2025-A Cross-Sectional Study for the Canton of Bern. Swiss Med Wkly (2021) 151:w30024. doi:10.4414/SMW.2021.w30024
10. Competence Network Health Workforce. Synthesis CNHW. Bern: Competence Network Health Workforce (2021).
11. Lobsiger, M, and Liechti, D. Personnel de santé en Suisse: Sorties de la profession et effectif. Une analyse sur la base de relevé structurels de 2016 à 2018. Obsant Rapport 01/2021. Neuchâtel: Observatoire de la santé (2021).
12. Merçay, C, Grünig, A, and Dolder, P. Personnel de santé en Suisse – Rapport national 2021: Effectifs, besoins, offre et mesures pour assurer la relève. Report No.: Obsan Rapport 03/2021. Neuchâtel: L’Observatoire suisse de la santé Obsan (2021).
13. Burla, L, Widmer, M, and Zeltner, C. Projections des besoins et des effectifs de médecins spécialistes en Suisse; Partie 1: Total des domaines de spécialité, médecine de premier recours, pédiatrie, psychiatrie et psychothérapie et orthopédie; Rapport final de l’Obsan et du comité «Coordination de la formation postgrade des médecins» sur mandat du dialogue «Politique nationale suisse de la santé». Neuchâtel: L’Observatoire suisse de la santé Obsan (2022).
14. Adriaenssens, J, De Gucht, V, and Maes, S. Determinants and Prevalence of Burnout in Emergency Nurses: A Systematic Review of 25 Years of Research. Int J Nurs Stud (2015) 52(2):649–61. doi:10.1016/j.ijnurstu.2014.11.004
15. Van der Heijden, B, Brown Mahoney, C, and Xu, Y. Impact of Job Demands and Resources on Nurses' Burnout and Occupational Turnover Intention Towards an Age-Moderated Mediation Model for the Nursing Profession. Int J Environ Res Public Health (2019) 16(11):2011. doi:10.3390/ijerph16112011
16. Nancarrow, S, and Bradbury, J. Pit SW, Ariss S. Intention to Stay and Intention to Leave: Are They Two Sides of the Same Coin? A Cross-Sectional Structural Equation Modelling Study Among Health and Social Care Workers. J Occup Health (2014) 56(4):292–300. doi:10.1539/joh.14-0027-oa
17. Courvoisier, N, Gilles, I, Keserue Pittet, O, and Peytremann Bridevaux, I. Déterminants de l’intention de rester dans leur profession ou à leur poste de professionnel·le·s des soins: revue de littérature. Lausanne, Unisanté – Centre universitaire de médecine générale et santé publique. Lausanne: Raisons de santé (2023). p. 340.
18. Roth, L, Le Saux, C, Gilles, I, and Peytremann-Bridevaux, I. Factors Associated With Intent to Leave the Profession for the Allied Health Workforce: A Rapid Review. Med Care Res Rev (2024) 81(1):3–18. doi:10.1177/10775587231204105
19. Aeschbacher, R, and Addor, V. Competitive Employer Positioning Through Career Path Analysis: The Case of the Swiss Nursing Sector. Hum Resour Health (2021) 19(1):47. doi:10.1186/s12960-021-00586-z
20. Addor, V, Jeannin, A, Schwendimann, R, and Roulet Jeanneret, F. Career Paths of 1988 and 1998 Nurse Graduates in Switzerland: Nurses at Work Pilot Study. J Nurs Manag (2017) 25(4):318–25. doi:10.1111/jonm.12469
21. Addor, V, Schwendimann, R, Gauthier, J-A, Wernli, B, Jackel, D, and Paignon, A. L'étude Nurses at Work: Parcours professionnels des infirmières/infirmiers au cours des 40 dernières années en Suisse. Report No.: OBSAN BULLETIN 8/2016. Neuchâtel: OBSAN (2016).
22. Gaudenz, C, De Geest, S, Schwendimann, R, and Zuniga, F. Factors Associated With Care Workers' Intention to Leave Employment in Nursing Homes: A Secondary Data Analysis of the Swiss Nursing Homes Human Resources Project. J Appl Gerontol (2019) 38(11):1537–63. doi:10.1177/0733464817721111
23. Gilles, I, Burnand, B, and Peytremann-Bridevaux, I. Factors Associated With Healthcare Professionals Intent to Stay in Hospital: A Comparison Across Five Occupational Categories. Int J Qual Health C (2014) 26(2):158–66. doi:10.1093/intqhc/mzu006
24. Gilles, I, Mayer, M, Courvoisier, N, and Peytremann-Bridevaux, I. Joint Analyses of Open Comments and Quantitative Data: Added Value in a Job Satisfaction Survey of Hospital Professionals. PLoS ONE (2017) 12(3):e0173950. doi:10.1371/journal.pone.0173950
25. Golz, C, Peter, KA, Zwakhalen, SMG, and Hahn, S. Technostress Among Health Professionals - A Multilevel Model and Group Comparisons Between Settings and Professions. Inform Health Soc Care (2021) 46(2):136–47. doi:10.1080/17538157.2021.1872579
26. Grylka-Baeschlin, S, Aeberli, R, Guenthard-Uhl, B, Meier-Kaeppeli, B, Leu-Tenegger, V, Volken, T, et al. Job Satisfaction of Midwives Working in a Labor Ward: A Repeat Measure Mixed-Methods Study. Eur J Midwifery (2022) 6:8. doi:10.18332/ejm/145494
27. Hammig, O. Explaining Burnout and the Intention to Leave the Profession Among Health Professionals - a Cross-Sectional Study in a Hospital Setting in Switzerland. BMC Health Serv Res (2018) 18(1):785. doi:10.1186/s12913-018-3556-1
28. Moeckli, B, Burgermeister, LC, Siegrist, M, Clavien, PA, and Kaser, SA. Evolution of the Surgical Residency System in Switzerland: An In-Depth Analysis Over 15 Years. World J Surg (2020) 44(9):2850–6. doi:10.1007/s00268-020-05552-9
29. Peter, KA, Hahn, S, Schols, J, and Halfens, RJG. Work-Related Stress Among Health Professionals in Swiss Acute Care and Rehabilitation Hospitals-A Cross-Sectional Study. J Clin Nurs (2020) 29(15-16):3064–81. doi:10.1111/jocn.15340
30. Peter, KA, Meier-Kaeppeli, B, Pehlke-Milde, J, and Grylka-Baeschlin, S. Work-Related Stress and Intention to Leave Among Midwives Working in Swiss Maternity Hospitals - a Cross-Sectional Study. BMC Health Serv Res (2021) 21(1):671. doi:10.1186/s12913-021-06706-8
31. Schwendimann, R, Dhaini, S, Ausserhofer, D, Engberg, S, and Zuniga, F. Factors Associated With High Job Satisfaction Among Care Workers in Swiss Nursing Homes - a Cross Sectional Survey Study. BMC Nurs (2016) 15:37. doi:10.1186/s12912-016-0160-8
32. Kuhlmann, E, Batenburg, R, Wismar, M, Dussault, G, Maier, CB, Glinos, IA, et al. A Call for Action to Establish a Research Agenda for Building a Future Health Workforce in Europe. Health Res Pol Syst (2018) 16(1):52. doi:10.1186/s12961-018-0333-x
33. Peytremann-Bridevaux, I, Jolidon, V, Gilles, I, Jubin, J, Zuercher, E, Roth, L, et al. Protocol for the Swiss COhort of Healthcare Professionals and Informal CAregivers (SCOHPICA): Professional Trajectories, Intention to Stay in or Leave the Job and Well-Being of Healthcare Professionals. PLoS ONE (2024). Under revision.
34. SCOHPICA (2024). Website of the Swiss Cohort of Healthcare Professionals and Informal Caregivers. Available at: https://scohpica.ch/.
35. Węziak-Białowolska, D, McNeely, E, and VanderWeele, T. Flourish Index and Secure Flourish Index – Development and Validation (2017).
36. Maniscalco, L, Enea, M, de Vries, N, Mazzucco, W, Boone, A, Lavreysen, O, et al. Intention to Leave, Depersonalisation and Job Satisfaction in Physicians and Nurses: A Cross-Sectional Study in Europe. Sci Rep-uk (2024) 14(1):2312. doi:10.1038/s41598-024-52887-7
37. Thin, SM, Nakpun, T, Nitadpakorn, S, Sorofman, BA, and Kittisopee, T. What Drives Pharmacists' Turnover Intention: A Systematic Review. Pharm Pract-granada (2021) 19(4):2559. doi:10.18549/PharmPract.2021.4.2559
Keywords: healthcare professionals, well-being, retention intentions, professional trajectories, cohort study
Citation: Jolidon V, Jubin J, Zuercher E, Roth L, Carron T, Oulevey Bachmann A, Gilles I and Peytremann-Bridevaux I (2024) Health Workforce Challenges: Key Findings From the Swiss Cohort of Healthcare Professionals and Informal Caregivers (SCOHPICA). Int J Public Health 69:1607419. doi: 10.3389/ijph.2024.1607419
Received: 23 April 2024; Accepted: 16 July 2024;
Published: 26 July 2024.
Edited by:
Bojana Knezevic, University Hospital Centre Zagreb, CroatiaReviewed by:
Jose Mira, Miguel Hernández University of Elche, SpainTwo reviewers who chose to remain anonymous
Copyright © 2024 Jolidon, Jubin, Zuercher, Roth, Carron, Oulevey Bachmann, Gilles and Peytremann-Bridevaux. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Isabelle Peytremann-Bridevaux, aXNhYmVsbGUucGV5dHJlbWFubi1icmlkZXZhdXhAdW5pc2FudGUuY2g=
 Vladimir Jolidon
Vladimir Jolidon Jonathan Jubin1,2
Jonathan Jubin1,2 Isabelle Peytremann-Bridevaux
Isabelle Peytremann-Bridevaux