- 1Department of Midwifery, College of Health Sciences, Woldia University, Woldia, Ethiopia
- 2Department of Medical Laboratory Science, College of Health Sciences, Woldia University, Woldia, Ethiopia
- 3Department of Pediatrics and Child Health Nursing, School of Nursings, College of Medicine and Health Science, Woldia University, Woldia, Ethiopia
Objectives: We conducted this review to identify factors associated with birth preparedness and complication readiness (BPCR) among pregnant women in Ethiopia. BPCR is a comprehensive approach that helps address delays in seeking care for obstetric problems.
Methods: PRISMA was followed and different databases were used to find studies. Adjusted Odds Ratio (AOR) with a 95% Confidence Interval was used to identify factors. The I2 statistic, funnel plot, and Egger test were used to assess the heterogeneity of studies and publication bias.
Results: Knowledge of BPCR, danger signs during pregnancy, labor, and postpartum (AOR = 1.99, 95% CI: 1.51, 2.64, AOR = 1.55; 95% CI: 1.35, 1.80; AOR = 1.45; 95% CI: 1.27, 1.63, and AOR = 1.4; 95% CI: 1.21, 1.63), respectively, residency (AOR = 1.49; 95% CI: 1.32, 1.68), antenatal care visit (AOR = 1.59; 95% CI: 1.43, 1.78), history of stillbirth (AOR = 1.58; 95% CI: 1.36, 1.86), and educational status (AOR = 1.62: 95% CI: 1.45, 1.78) were significantly associated with BPCR practice.
Conclusion: This study identified some modifiable factors in the practice of BPCR. Integrating counseling and expanding ANC services in health facilities may improve BPCR practice.
Introduction
Pregnant women are vulnerable to problems that emerge during pregnancy and childbirth and can end in death at any time, anywhere in the world. Worldwide, 800 women die every day; 95% of these deaths take place in low- and middle-income nations; Sub-Saharan Africa and Southern Asia account for approximately 87% of the expected total number of global maternal deaths, and Sub-Saharan Africa alone accounts for approximately 70% of these deaths [1, 2]. By implementing comprehensive maternal health services, the majority of these deaths can be avoided [3].
Pregnancy, childbirth, postpartum period, and neonatal care are all included in birth preparedness and complication readiness, or BPCR, which is the state of being ready for delivery and any obstetric emergency [4, 5]. The Johns Hopkins Program for International Education in Gynecology and Obstetrics (JHIEGO) maternal and neonatal health program describes BPCR as focusing on three delays: delays in making the decision to seek care for an obstetric complication, delays in going to a medical facility after making the decision, and delays in receiving care at the facility [6]. Its components include identifying a place to give birth, identifying a skilled birth attendant, saving money for birth-related and emergency expenses, identifying a support person during pregnancy, labor, and postpartum periods, identifying means of transport in case of an obstetric emergency, preparing equipment needed for delivery and identifying a potential blood donor in case of an emergency [7, 8].
The UN Sustainable Development Goals (SDGs) of reducing maternal mortality to less than 70 per 100,000 live births, neonatal mortality to at least 12 per 1,000 live births, and under-five mortality to at least as low as 25 per 1,000 live births can be greatly supported and achieved by implementing BPCR, especially in developed nations [7, 9, 10]. Ethiopia as a member country has adopted these goals and has been giving great attention and efforts to achieve the target by 2030. In Ethiopia maternal, neonatal, and under-five mortality rates have decreased, although they are still high and far from the target of the SDGs [10]. Still, 1 in 267 women dies from pregnancy-related complications, 1 in 20 children dies before reaching the age of 5, 1 in 28 infants dies before reaching 1 year of age, and 1 in 38 newborns dies within their first 4 weeks of life which is still too high [11, 12].
Research findings revealed that BPCR therapies contributed to a decreased incidence of adverse outcomes for both mothers and neonates. Specifically, women who practice BPCR had lower rates of low birth weight neonates (4.3% vs. 14.8%), admission to a neonatal intensive care unit (14.8% vs. 32.2%), and postpartum anemia (35.7% vs. 58.3%) [4, 13, 14]. Other study results indicated that BPCR interventions contributed to a 28% reduction in the risk of maternal mortality and an 18% reduction in the risk of neonatal mortality [4].
Birth preparedness and complication readiness is a comprehensive method for increasing the timely utilization of skilled maternal and neonatal care [2, 7]. Although there is clear evidence that birth preparedness and complication readiness can improve maternal and neonatal health outcomes, national data on factors associated with BPCR practices BPCR are scarce, and regional variations exist [9, 15–36]. In Ethiopia, one study has been conducted at the national level on the practice of birth preparedness and complication readiness plans [37], but comprehensive studies on the predictors of BPCR practices at the national level are lacking, except for small-scale studies. Therefore, this systematic review and meta-analysis aimed to identify predictors of birth preparedness and complication readiness practices among pregnant mothers in Ethiopia.
Methods
Development of the Review Methodology
The Preferred Reporting Elements for Systematic Reviews and Meta-Analyses Protocols (PRISMA-P) 2020 statement was used to develop the methodology of the review, and all items of the PRISMA-P checklist were covered (Supplementary Figure 1). The PRISMA flow charts showing the study selection process from the first identified records to the included studies, were noted in the results. The International Prospective Register of Systematic Reviews (PROSPERO) delivered registration number CRD42023442256 for this systematic review and meta-analysis.
Search Date
The initial searches for this systematic review were started on 01/07/2023, and the protocol was registered on 15/07/2023. This systematic review and meta-analysis includes all studies published in Ethiopia until 24/10/2023.
Search Strategy
The first author (AA) conducted the literature search. Only research that was published in English was included in the search. We used various combinations of keywords to search in the databases and to find articles for the review, major medical electronic databases including MEDLINE, PubMed, Google Scholar, CINAHL, EMBASE, Scopus, and African Journals Online were used. The search strings or terms stemmed from the following keywords: birth preparedness, complication readiness, knowledge of danger signs, associated factors, and Ethiopia. A sample of the PubMed search strategy (“factors$ or determinants) and (“birth preparedness”) and (complication readiness$ or “knowledge of danger signs”) (pregnant$ or “prenatal”).
Eligibility Criteria
We considered studies that examined the prevalence and associated factors of BPCR. Regardless of the time of data collection or year of publication, we included studies that had been conducted in both community and facility settings, with the primary outcome variable being characterized as “practice of BPCR and its associated factors among pregnant women” in the analysis. Case series, case reports, reviews, and studies that did not record the outcome variable were not included. Research that primarily provided qualitative insights into the use of BPCR was also excluded. Only quantitative data from studies that reported both qualitative and quantitative findings were taken into consideration.
Study Selection Procedure
Screening
Initial studies were identified using search terms and filters in databases and other relevant sources. Duplicate studies were removed from the identified studies after exporting them to EndNote, a citation management tool. According to the inclusion criteria, the studies were independently screened by four authors (MA, CM, GK, and ES) using the data from the titles and abstracts. The titles and abstracts of the studies were categorized as included, excluded, or undetermined based on this screening process. For a more thorough eligibility evaluation, we then obtained the full text of each included and inconclusive study (Figure 1).
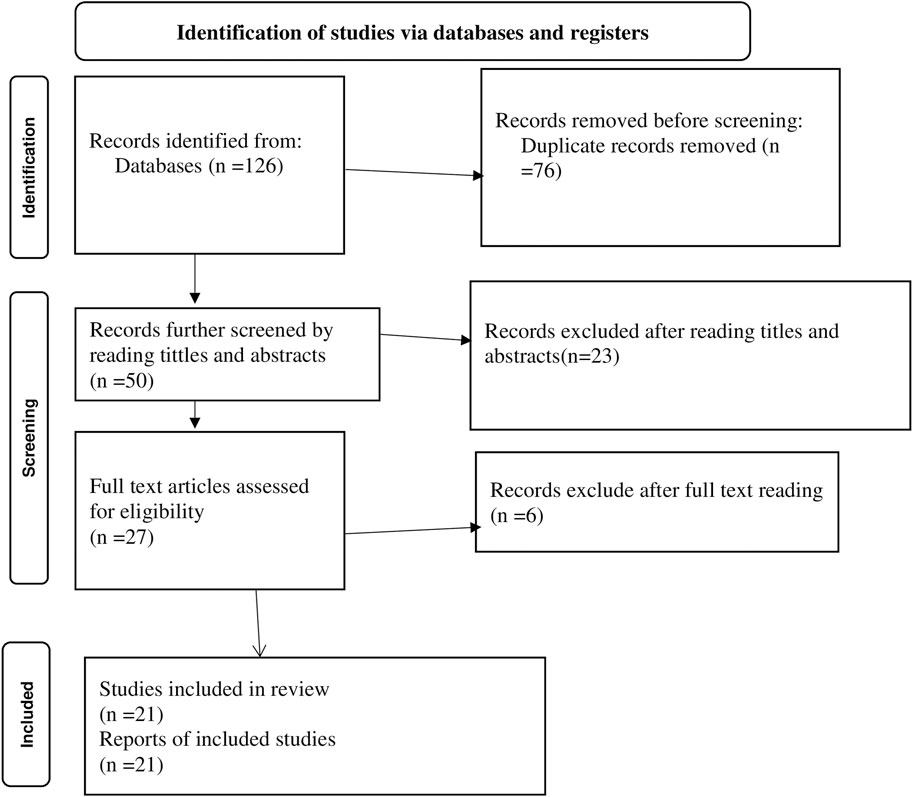
Figure 1. PRISMA flow chart showing the included searches for systematic review and meta-analysis on predictors of birth preparedness and complication readiness practice among pregnant women in Ethiopia, 2023.
Quality Assessment
Two authors (AA and MA) evaluated the methodological quality, risk of bias, and validity of the included articles by using the Joanna Briggs Institute (JBI) checklist designed for analytical cross-sectional studies. There are eight questions on the checklist (1. Are the criteria for inclusion in the sample clearly defined? 2. Were the study subjects and the setting described in detail? 3. Was the exposure measured validly and reliably? 4. Were objective, standardized criteria used for the measurement of the condition? 5. Were confounding factors identified? 6. Were strategies for dealing with confounding factors stated? 7. Were outcomes measured validly and reliably? and 8. Was an appropriate statistical analysis used?), categorized into “Yes,” “No,” “Unclear” and “Not applicable.” Scores of 50% and above on the quality assessment indicators were considered low risk [38]. Any disagreement over the assessment of the risk of bias and research quality between the two authors was managed by involving the third and fourth authors (ES and GK).
Outcome Measurements
The out comes of this review was identification of factors affecting birth preparedness and complication readiness practices among pregnant women in Ethiopia which were measured by identifying the place of delivery, saving money for delivery, identifying a mode of transportation to the place of delivery or in case of emergency, identifying a potential blood donor, identifying a skilled birth provider, and identifying a support person or decision maker. Factors that could be involved in BPCR practices were measured as higher levels of maternal educational status (yes/no), maternal residence (urban/rural), government employee (yes/no), knowledge of BPCR (yes/no), knowing danger signs during pregnancy (yes/no), knowing danger signs during labor and delivery (yes/no, knowing danger signs during the post-natal period (yes/no), having antenatal care follow-up during pregnancy (yes/no) and history of stillbirth (yes/no).
Data Extraction Process
The data were meticulously abstracted by two authors (AA and CM) using a data extraction template. To represent all the included research, a list of items relevant to the study characteristics is presented in the summary table. Names of the authors, study year, design, setting, sample size, demographics, and study-specific predictive factors were all included in the detailed list of items. Throughout the data extraction procedure for the exposure variables, we separated the individual classifications displayed for each variable into two categories: exposed and non-exposed to the outcome. For the variables, the non-exposed group served as the reference. For example, the exposed category for place of residence was rural, whereas the non-exposed group was urban. We then prepared them for quantitative synthesis using the matching combined numerical values. After face-to-face discussions, disagreements between the two authors were resolved and an agreement was reached.
Data Synthesis and Statistical Analysis
A summary table was used to present the main findings of the included articles. Additionally, Stata 17 was used for analysis. We used 95% confidence intervals (CIs) for adjusted odds ratios (AORs) to compute summary statistics (pooled effect sizes). The results of the meta-analysis were graphically shown using forest plots. The I2 statistic was used to evaluate statistical heterogeneity and the degree of heterogeneity between the studies; if a value was ≥50%, significant heterogeneity was considered and we performed sub-group analysis based on study region, study design, and year of publication. Egger’s test was used to test the publication bias by considering a P-value: a P-value of <0.05 meant that there was potential publication bias or small-study effects, and a P-value ≥ 0.05 suggested the absence of strong publication bias or small-study effects [39].
Results
Description of the Studies
A search of primary electronic health and medical databases along with other relevant sources identified 126 studies. Based on their title and abstract, 50 of the identified studies were kept for further eligibility screening, while the remaining 76 were excluded as duplicates. After reviewing the titles and abstracts of 23 records, it was determined that 9 studies did not meet the inclusion criteria and 14 studies were conducted in a location or environment unrelated to the research question. Six of the 27 papers that remained were eliminated after their full texts were reviewed because, as indicated by their titles, abstracts, and texts, their content did not relate to the topic of our evaluation. After thorough evaluation, the remaining 21 studies were included in this review (Figure 1). Seven institutional-based and fourteen community-based cross-sectional studies with a total sample size of 13,877 were included in this review. Of the included studies nine were from the SNNP region, four were from the Amhara region, five were from the Oromia region, two were from the Harare region, and one was from the Afar region (Table 1).
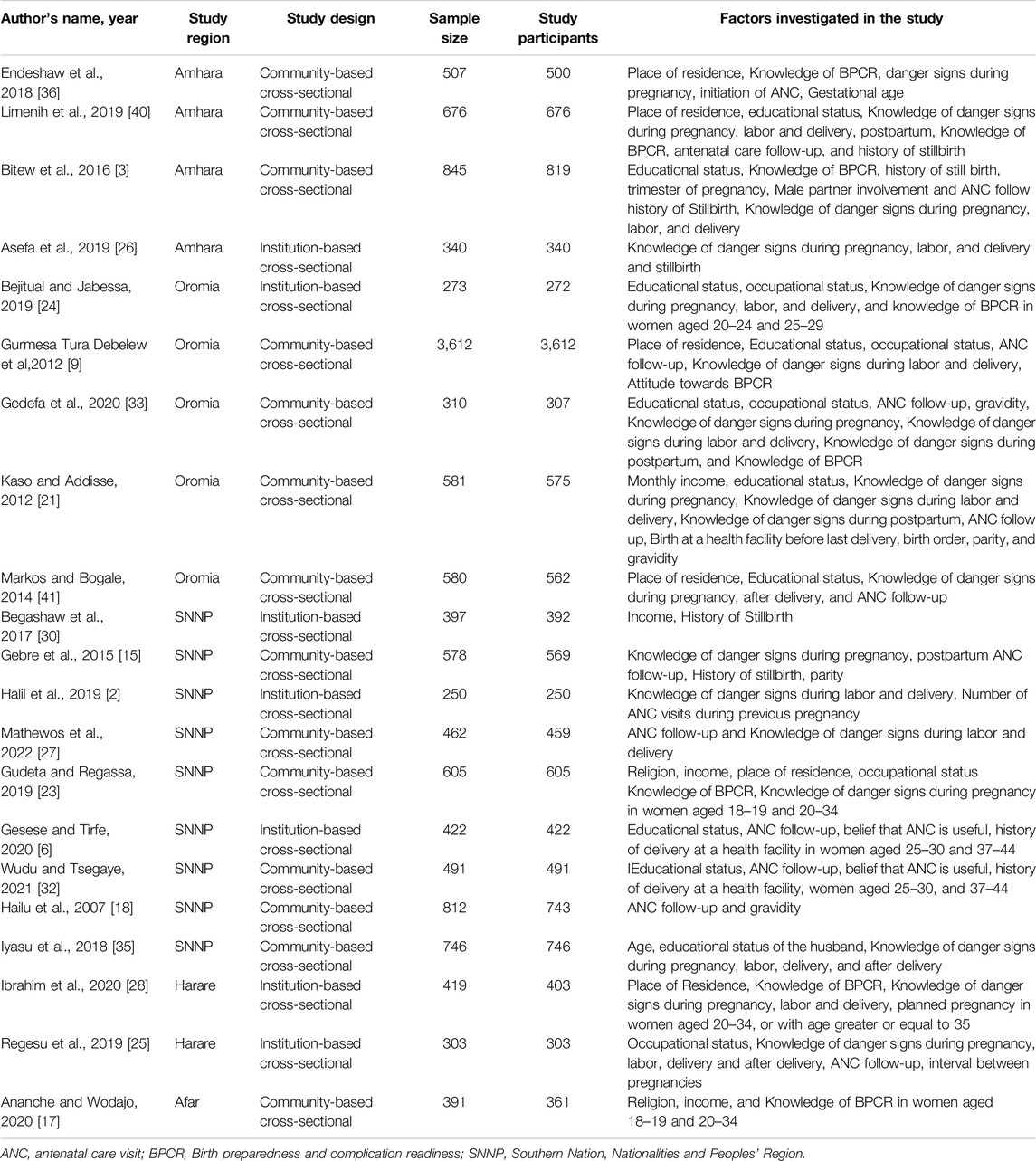
Table 1. Description of the included studies to identify predictors of birth preparedness and complication readiness practice among pregnant women in Ethiopia, 2023.
Factors Associated With BPCR Practices
The current review reveals various factors associated with BPCR practices in Ethiopia. Significantly associated factors include maternal knowledge of BPCR, maternal knowledge of pregnancy danger signs, maternal knowledge of labor and delivery danger signs, maternal knowledge of postpartum danger signs, place of residence, ANC follow-up, history of stillbirth, and maternal education.
Place of Residence
Factor analysis of the included studies revealed a significant positive association between BPCR practices and place of residence. Women who lived in urban areas had a 1.49-fold higher chance of practicing BPCR than their counterparts (AOR = 1.49; 95% CI: 1.32, 1.68). This included the heterogeneity of the study (I2 = 22.58%, p < 0.0001) (Figure 2), and the Egger test revealed publication bias with a p-value of 0.0223. For this, we conducted a nonparametric trim-and-fill analysis of publication bias and this showed no imputed study and we report with the original finding.
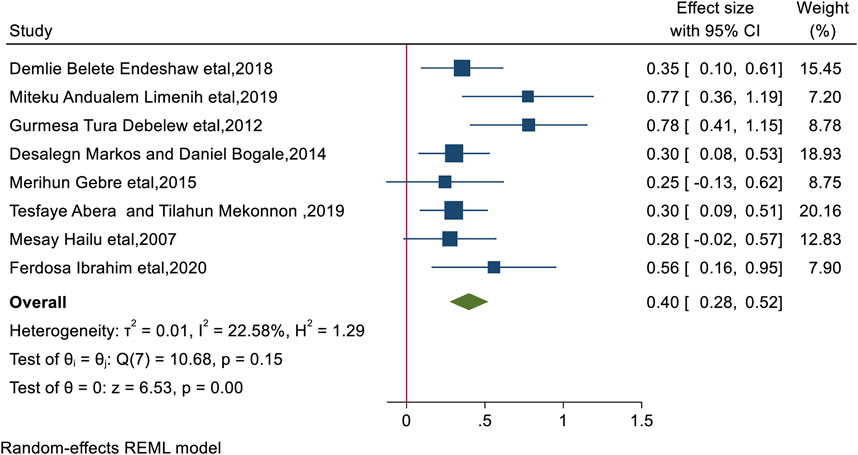
Figure 2. The overall pooled odds ratio of the association between residency and practice of birth preparedness and complication among pregnant women in Ethiopia, 2023.
Maternal Education
According to this study, maternal education was found to be associated positively with BPCR use, with women who completed secondary education or higher adopting BPCR practices 1.62 times more than their counterparts (AOR = 1.62: 95% CI: 1.45, 1.78). Significant heterogeneity was not detected in included study (I2 = 1.41%, p < 0.0001), and the Egger test revealed no publication bias with a p-value of 0.27 (Figure 3).
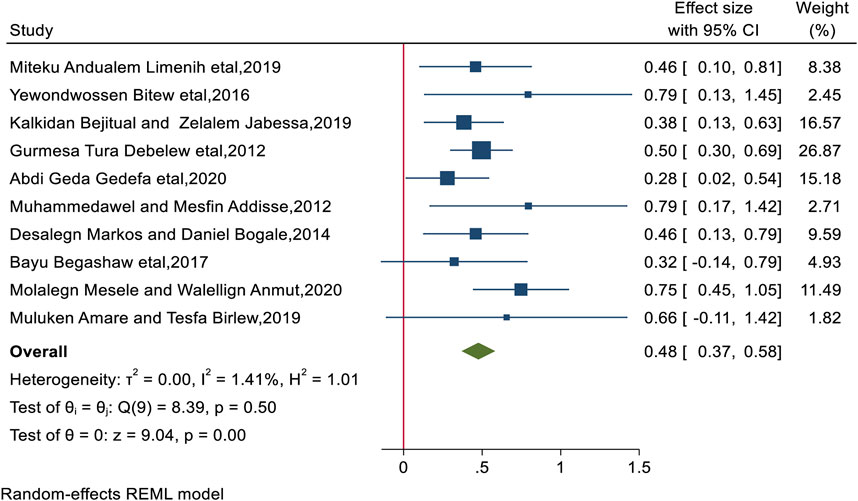
Figure 3. The overall pooled odds ratio of the association between the mother’s educational status and practice of birth preparedness and complication readiness among pregnant women in Ethiopia, 2023.
Maternal Knowledge of BPCR
BPCR practices were found to be significantly positively correlated with maternal knowledge of BPCR. This review showed that women who knew about BPCR were nearly twice as likely to practice BPCR as women who did not (AOR = 1.99, 95% CI: 1.51, 2.64). There was significant heterogeneity (I2 = 82.78%, p < 0.0001). The Egger test yields a p-value of 0.969, indicating no publication bias (Figure 4).
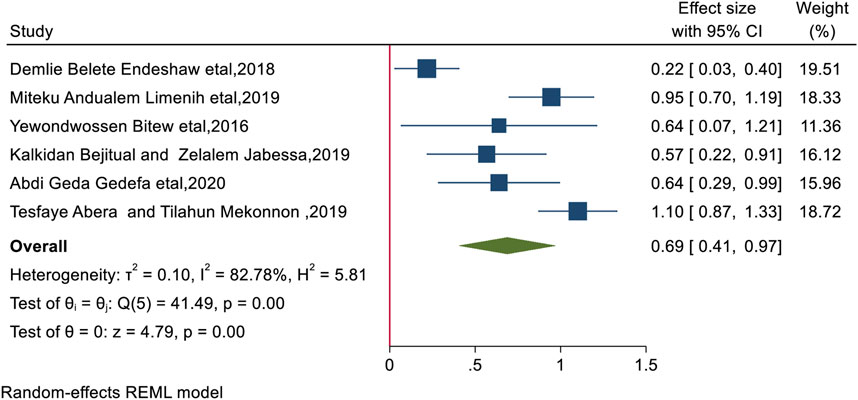
Figure 4. The overall pooled odds ratio of the association between knowledge of birth preparedness and complication readiness and practice of birth preparedness and complication readiness among pregnant women in Ethiopia, 2023.
Antenatal Care Visit
The conclusions of the review showed that women who received ANC visits had a much higher likelihood of practicing BPCR than their counterparts (AOR = 1.59; 95% CI: 1.43, 1.78), women who received ANC visits were 1.59 times more likely to practice BPCR than their counterparts. The included studies had no significant heterogeneity (I2 = 36.46%, p < 0.0001), while the Egger test revealed publication bias with a significant p-value of 0.0018, for which we performed a nonparametric trim-and-fill analysis of publication bias, indicating no imputed study (Figure 5).
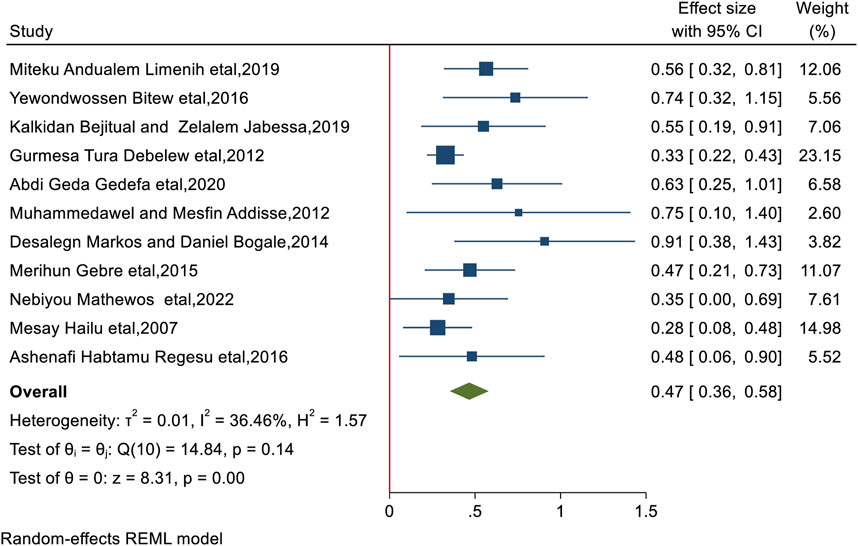
Figure 5. The overall pooled odds ratio of the association between antenatal care follow-up and practice of birth preparedness and complication readiness among pregnant women in Ethiopia, 2023.
History of Stillbirth
According to this review, women who had previously experienced a stillbirth had a higher likelihood of using BPCR than other women (AOR = 1.58; 95% CI: 1.36, 1.86). Women having a history of stillbirths were 1.58 times more likely to practice BPCR. The heterogeneity of this included study was low (I2 = 8.35%, p < 0.0001) and there is no publication bias using the Egger test with a nonsignificant p-value of 0.37 (Supplementary Figure 2).
Knowledge of Danger Signs During Pregnancy
The overall odds ratio (AOR = 1.55; 95% CI: 1.35, 1.80) indicated that women who knew the danger signs during pregnancy were 1.55 times more likely to practice BPCR than women who did not know the signs during pregnancy. The heterogeneity of the study was high (I2 = 82.78%, p < 0.0001) and the Egger test yielded a p-value of 0.46 indicating no publication bias (Supplementary Figure 3).
Knowledge of Danger Signs During Labor and Delivery
The findings of the review showed a significant positive association between women’s knowledge of danger signs during labor and delivery and their likelihood of practicing BPCR (AOR = 1.45; 95% CI: 1.27, 1.63), with women who were aware of the warning signs during labor and delivery being 1.45 times more likely to use BPCR than those who were not. The Egger test yielded a p-value of 0.54, with no indication of publication bias, and heterogeneity was found in the included studies (I2 = 69.26%, p < 0.0001) (Supplementary Figure 4).
Knowledge of Postpartum Danger Signs
Our analysis revealed a significant positive association between women’s knowledge of postpartum danger signs and BPCR practice (AOR = 1.4; 95% CI: 1.21, 1.63), with women who were aware of postpartum danger signs being 1.4 times more likely to practice BPCR than women who were not aware. This accounted for the heterogeneity of the study (I2 = 76.87%, p < 0.0001), and the Egger test revealed no publication bias with a p-value of 0.46 (Supplementary Figure 5).
Parity, Partner Involvement
Our systematic review showed no significant association between parity, partner involvement, and BPCR practice (OR = 0.59; 95% CI: −0.16, 1.34) and (OR = 0.65; 95% CI: −0.18, 1.47), respectively.
Subgroup Analysis
When the I2 was greater than 50% it indicated high heterogeneity, we performed a subgroup analysis to identify the sources of heterogeneity (differences) in the study results. In this review, we performed a subgroup analysis by considering the study region (Amhara, SNNP, Oromia, Harare) and study design (community-based vs. institutional). Following the sub-group analysis, the study with the highest I2 showed the source of heterogeneity (Supplementary Figure 6).
Publication Bias
In this systematic review and meta-analysis, we assessed the publication bias by performing the Egger test and funnel plot (Supplementary Figure 7) and we considered no publication bias to exist if the value of the Egger test was non-significant or if the value of P was ≥0.05. In this review of factor analysis, the value of the Eggers test was found to be significant and the funnel plot was asymmetrically distributed on the factors of place of residence and ANC visit. For this we conducted a trim-and-fill analysis, which indicated zero imputed studies. Consequently, we report only the observed findings for the final results.
Discussion
This systematic review and meta-analysis aimed to identify the predictors of birth preparedness and complication readiness plans among Ethiopian women. Twenty-one studies were included in this meta-analysis. Maternal knowledge of BPCR plans, danger signs during pregnancy, labor, and postpartum, maternal education, maternal, place of residence, history of stillbirth, and ANC visits were significantly associated with BPCR practice in Ethiopia. Parity and paternal involvement in the BPCR showed no significant association with BPCR practices.
This systematic review and meta-analysis revealed that educational status and residence were significantly associated with BPCR practice. Urban women were more likely to practice BPCR than rural women; this is supported by a study conducted in Northern Ghana [42]. Urban women’s higher media exposure, practical access to healthcare facilities, and strong understanding of health issues may explain this. Women who have secondary and above education were also more likely to practice BPCR which is supported by other studies conducted in different countries [5, 42–52]. Women who have received education are more likely to seek medical attention, and it also helps them become confident and effective decision-makers, improving their readiness for childbirth and complications. Living in urban areas and receiving an education broadens awareness of obstetric difficulties and gives one access to BP/CR health information, allowing them to practice being ready for birth and for complications. Despite the above evidence, a study conducted in rural areas of Indian mothers revealed that the educational status of the mothers is not associated with BPCR practices [53]. This might be explained by a difference in sample size and variation in the study area.
The findings of this systematic review and meta-analysis revealed that women who knew about birth preparedness and complication readiness plans were significantly associated with BPCR practices, which is supported by a study conducted in Nepal, and India [43, 54]. This may be explained by the fact that women are more likely to engage in active planning and take preventative actions to ensure the health of both the mother and the newborn when they know what to expect during pregnancy and how to prepare for any issues and may practice BPCR.
This systematic review and meta-analysis showed that women who had antenatal care follow-up and a history of stillbirth during pregnancy were other predictors of birth preparedness and complication readiness practice, which is supported by studies conducted in Nepal, Kenya, Tanzania, and the Pakistani province of Sindh [43, 46, 55]. This may be explained by the fact that antenatal care visits provide mothers with essential knowledge regarding the significance of getting ready for childbirth, recognizing warning signs of problems, and knowing what to do in an emergency during these visits, and healthcare providers may look at the mother’s and the baby’s health and address any issues.
Antenatal care follow-up minimizes the risks associated with birthing and increases the use of BPCR by empowering pregnant moms by offering more knowledge and preparation. A history of stillbirth has been associated with the practice of BPCR. This could be explained by the fact that women who have had stillbirths tend to be more aware and optimistic during their subsequent pregnancies. This sensitive awareness usually motivates more careful participation in behaviors related to complication readiness and birth preparedness. They might be more likely to adhere to antenatal care plans, carefully examine and comply with medical advice, and take necessary precautions to avert any difficulties. As a result, a history of stillbirth can serve as a predictor for better antenatal care in the future, preventing recurrence.
This systematic review and meta-analysis showed that the odds of practicing BPCR were higher among women with knowledge of the danger signs during pregnancy. This is supported by studies conducted in Kenya and Tanzania [46], in the Kassena-Nankana district of Ghana [44], in resource-limited settings in rural northern Ghana [45], India [56], in the Thatta district, Sindh, Pakistan [55], in the urban slums of Shivamogga City, India [47], Nepal [43], and rural areas in Bangladesh [57] which could be explained by the fact that being aware of the danger signs associated with pregnancy can help women feel more prepared for giving birth, improve their behavior when seeking medical attention, and make better decisions regarding their health. It can also help identify potentially life-threatening complications early on and reduce unnecessary delays in seeking medical attention. This systematic review and meta-analysis also showed that the odds of practicing BPCR were higher among women who knew danger signs during labor and after giving birth. This finding is supported by studies conducted in Nepal, Kenya, Tanzania, Sindh, India, and Bangladesh [43, 46, 55–57]. It could be explained by the fact that women who are knowledgeable about childbirth, postpartum difficulties, labor, and delivery would be more worried about their safety and survival. Furthermore, women may be ready to avert the worst before it happens if they have greater awareness about delivery and postpartum risk signs. It also aids in their efforts to safeguard their safety and wellbeing, as well as the health of their child. This ultimately results in the need for medical guidance and support from healthcare professionals. This suggests that improved knowledge of labor and postpartum warning indicators will significantly improve BPCR practices.
Strengths and Limitations of the Study
The inclusion of both community- and institutional-level studies is one of the strengths of this study. This review employs a systematic review and meta-analysis approach to estimate national predictors of BPCR practice in Ethiopia for the first time; healthcare policymakers, researchers, and practitioners may find important information from this work. Because there was insufficient research in certain regions, the results might not apply to the entire country. Only cross-sectional research was included in our analysis because no studies employing alternative methodologies were found. As a result, we suggest more studies to address these gaps.
Conclusion
In this systematic review and meta-analysis, place of residence, maternal education, maternal knowledge of BPCR, antenatal care visit, history of stillbirth, knowledge of danger signs during pregnancy, knowledge of danger signs during labor and delivery, and knowledge of danger signs after delivery were the main identified factors affecting BPCR practices. Some of the variables were related to a lack of knowledge about maternal complications and were modifiable factors related to BPCR practices. Improving ANC services, improving women’s education, and integrating counseling into health facilities may lead to better BPCR practices. The findings of this study may help the policymaker design a policy to overcome the problems and increase overall maternal and neonatal health outcomes. Also, the findings of this review may be used as a baseline for future researchers who are interested in this field.
Author Contributions
All authors contributed to the study protocol and AA wrote the design of the work, drafted the work, and substantively revised it. MA, ES, GK, CM, and AB revised subsequent drafts of the protocol and approved the result with some revisions. All authors contributed to the article and approved the submitted version.
Funding
The authors declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of Interest
The authors declare that they do not have any conflicts of interest.
Acknowledgments
We acknowledge Woldia University for giving us internet service and we would like to thank all the authors of the primary studies that we included in this systematic review and meta-analysis.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/ijph.2024.1607296/full#supplementary-material
References
1. World Health Organization. Maternal Mortality. Available from: https://www.who.int/news-room/fact-sheets/detail/maternal-mortality (Accessed March 22, 2024).
2. Halil, HM, Abdo, RA, Kebede, BA, and Godana, GA. Birth Preparedness and Complication Readiness Among Antenatal Care Attendants at Butajira General Hospital, Southern Ethiopia. J Preg Child Health (2019) 6(4):417.
3. Bitew, Y, Awoke, W, and Chekol, S. Birth Preparedness and Complication Readiness Practice and Associated Factors Among Pregnant Women, Northwest Ethiopia. Int Sch Res Notices (2016) 2016:8. doi:10.1155/2016/8727365
4. Soubeiga, D, Gauvin, L, Hatem, MA, and Johri, M. Birth Preparedness and Complication Readiness (BPCR) Interventions to Reduce Maternal and Neonatal Mortality in Developing Countries: Systematic Review and Meta-Analysis. BMC Pregnancy Childbirth (2014) 14:129–11. doi:10.1186/1471-2393-14-129
5. Chandrakar, T, Verma, N, Gupta, SA, and Dhurandhar, D. Evaluation of Birth Preparedness and Complication Readiness Index Among Women of Central India: A Community - Based Survey of Slums. J Med Evid (2022) 3:134. doi:10.4103/jme.jme_59_22
6. Gesese, MM, and Tirfe, WA. Birth Preparedness and Complication Readiness Practice and Associated Factors Among Women Attending Antenatal Care Follow Up in Yirgalem General Hospital, Sidama Zone, Southern Ethiopia, 2019. Research Square (2020). doi:10.21203/rs.3.rs-55574/v1
7. Tafa, A, Hailu, D, Ebrahim, J, Gebrie, M, and Wakgari, N. Birth Preparedness and Complication Readiness Plan Among Antenatal Care Attendants in Kofale District, South East Ethiopia: A Cross Sectional Survey. Divers Equality Health Care (2018) 15:23–9. doi:10.21767/2049-5471.1000152
8. Maternal and Neonatal Health (MNH) Program. Birth Preparedness and Complication Readiness. (2004). Baltimore, MD: JHPIEGO. 21231–3492.
9. United Nations Ethiopia. Sustainable Development Goal 3 Good Health and Wellbeing (2014) 8688:1–14. Available from: https://ethiopia.un.org/en/sdgs/3 (Accessed March 26, 2024).
10. Ayele, AA, Tefera, YG, and East, L. Ethiopia’s Commitment Towards Achieving Sustainable Development Goal on Reduction of Maternal Mortality: There Is a Long Way to Go. Womens Health (Lond) (2021) 17:17455065211067073. doi:10.1177/17455065211067073
11. Department of Economic and Social Affairs Population Division. Ethiopia Infant Mortality Rate 1950–2023 H Macrotrends (2023). Available from: https://population.un.org/wpp/net/countries/ETH/ethiopia/infan (Accessed March 30, 2024).
12. Survival and Health Expanding Access and Improving Health Care Quality and Standards in Ethiopia, Available from: https://www.unicef.org/ethiopia/survival-and-health (Accessed March 30, 2024).
13. Article, O, Umeh, U, Ugwu, E, Imediegwu, O, Oguejiofor, N, Grema, B, et al. Effects of Birth Preparedness and Complication Readiness on Pregnancy Outcome in Nigeria. Niger J Med (2022) 31:182. doi:10.4103/njm.njm_196_21
14. Shah, N, and Rohra, DK. Home Deliveries: Reasons and Adverse Outcomes in Women Presenting to a Tertiary Care Hospital. J Pak Med Assoc (2010). 60(7):555–8.
15. Gebre, M, Gebremariam, A, and Abebe, TA. Birth Preparedness and Complication Readiness Among Pregnant Women in Duguna Fango District, Wolayta Zone, Ethiopia. PLoS One (2015) 10:e0137570. doi:10.1371/journal.pone.0137570
16. Chala, H, Asseged, S, Woldeyohannes, D, and Tekalegn, Y. Factors Associated With Birth Preparedness and Complication Readiness Among Antenatal Clinic Attendants in Selected Public Hospitals in Addis Ababa, Ethiopia: Institution Based Cross Sectional Study. J Public Health Epidemiol (2018) 10:287–94. doi:10.5897/JPHE2018.1024
17. Ananche, TA, and Wodajo, LT. Birth Preparedness Complication Readiness and Determinants Among Pregnant Women: A Community-Based Survey From Ethiopia. BMC Pregnancy Childbirth (2020) 20:631. doi:10.1186/s12884-020-03297-w
18. Hailu, M, Gebremariam, A, Alemseged, F, and Deribe, K. Birth Preparedness and Complication Readiness Among Pregnant Women in Southern Ethiopia. PLoS One (2011) 6(6):e21432. doi:10.1371/journal.pone.0021432
19. Debelie, TZ, Abdo, AA, Temesgen, K, Limenih, A, Asaye, MM, et al. Birth Preparedness and Complication Readiness Practice and Associated Factors Among Pregnant Women in Northwest Ethiopia: 2018. PLoS One (2021) 16(4):e0249083. doi:10.1371/journal.pone.0249083
20. Dessu, S, Gomba, ZD, and Bojola, F. Assessment of Birth Preparedness and Complication Readiness and Associated Factors Among ANC Attendant Pregnant Mothers in Arba Minch Town Governmental Institutions, Arba Minch, Southern Ethiopia. Int J Sex Reprod Health Care (2019) 2(1):1–5. doi:10.17352/ijsrhc.000003
21. Kaso, M, and Addisse, M. Birth Preparedness and Complication Readiness in Robe Woreda, Arsi Zone, Oromia Region, Central Ethiopia: A Cross-Sectional Study. Reprod Health (2014) 11:55–12. doi:10.1186/1742-4755-11-55
22. Ayalew, AF, Gelaw, AY, and Banite, GM. Level of Birth Preparedness for Complication Readiness Plan and Associated Factors Among Women Who Gave Live Birth in Bahir Dar, Amhara Regional State, Ethiopia, 2018. Research Square (2019). doi:10.21203/rs.2.11592/v1
23. Gudeta, TA, and Regassa, TM. Factors Associated With Birth Preparedness and Complication Readiness Among Pregnant Women in Bench Maji Zone, Southwest Ethiopia: A Community-Based Cross-Sectional Study. Ethiop J Health Sci (2019):567–76. doi:10.4314/ejhs.v29i5.6
24. Bejitual, K, and Jabessa, Z. Birth Preparation and Complication Readiness Among Antenatal Care Attendants in Bule Hora Governmental Health Facilities in Oromia Region, Ethiopia, in 2019. J Midwifery Reprod Health. (2021) 9(2):2669–78. doi:10.22038/jmrh.2020.42288.1483
25. Regesu, AH, Oda, AT, Adem, MK, and Wako, MK. Birth Preparedness and Complication Readiness and Associated Factors Among Mothers Attending Antenatal Care at Chiro District Health Centers, West Hararge, Ethiopia. Int J Health Sci Res (2019) 9:187–95.
26. Asefa, A, Getachew, B, Belete, AM, and Molla, D. Knowledge and Practice on Birth Preparedness Complication Readiness Among Pregnant Women Visiting Debreberhan Town Governmental Health Institutions, North-East Ethiopia. J Womens Health (2022) 11:587. doi:10.35248/2167-0420.22.11.587
27. Mathewos, N, Shaka, MF, and Tesfaye, SH. Assessment of Birth Preparedness and Complication Readiness and Associated Factors Among Reproductive Age Women in Wonago District, Gedeo Zone, Southern Ethiopia. East Afr. J. Public Health Biomed. Sci. (2022) 1:1–20. doi:10.21203/rs.3.rs-2343263/v1
28. Ibrahim, F, Dessie, Y, Assefa, N, and Tiruye, G. Birth Preparedness and Complication Readiness Among Pregnant Women Attending Antenatal Care Clinics in Public Health Facilities, Harari Region, Eastern Ethiopia. East Afr J Health Biomed Sci (2020) 4:15–26.
29. Affipunguh, PK, and Laar, AS. Assessment of Knowledge and Practice Towards Birth Preparedness and Complication Readiness Among Women in Northern Ghana: A Cross-Sectional Study. Int J Sci Rep (2016) 5(10):4293–301. doi:10.18203/issn.2454-2156.IntJSciRep20161878
30. Begashaw, B, Tesfaye, Y, Zelalem, E, Ubong, U, and Kumalo, A. Assessment of Birth Preparedness and Complication Readiness Among Pregnant Mothers Attending Ante Natal Care Service in Mizan-Tepi University Teaching Hospital, South West Ethiopia. Clinics Mother Child Health (2017) 14:257. doi:10.4172/2090-7214.1000257
31. Mekonnen, O, Belete, ZA, Adugnaw, E, and Neges, K. Assessment of Knowledge, Attitude and Practices on Birth Preparedness and Complication Readiness Among Pregnant Women Attending Antenatal Follow Up at Mizan-Tepi University Teaching Hospital, Southwest Ethiopia. Research Square (2022) 1. doi:10.21203/rs.3.rs-1699626/v1
32. Wudu, MA, and Tsegaye, TB. Birth Preparedness and Complication Readiness and Associated Factors Among Recently Delivered Mothers in Mizan-Aman Town, Southwest Ethiopia, 2019. Int J Womens Health (2021) 13:177–87. doi:10.2147/IJWH.S279201
33. Gedefa, AG, Bekele, AA, Kitila, KM, and Eba, LB. Barriers to Birth Preparedness and Complication Readiness Among Pregnant Women in Rural Ethiopia: Using a Mixed Study Design, 2020. BMJ (2023) 13(4):e069565. doi:10.1136/bmjopen-2022-069565
34. Abebaw, N, Abdu, M, Biza, N, and Assalfew, B. Assessments of Birth Preparedness and Complication Readiness Among Women of Childbirth in Samara Logia Town, Afar, North East Ethiopia. Am J Lab Med (2020) 5(4):95–101. doi:10.11648/j.ajlm.20200504.13
35. Iyasu, A, Hordofa, MA, Zeleke, H, and Leshargie, CT. Level and Factors Associated With Birth Preparedness and Complication Readiness Among Semi - Pastoral Pregnant Women in Southern Ethiopia, 2016. BMC Res Notes (2018) 11(1):442. doi:10.1186/s13104-018-3539-7
36. Endeshaw, DB, Gezie, LD, and Yeshita, HY. Birth Preparedness and Complication Readiness Among Pregnant Women in Tehulederie District, Northeast Ethiopia: A Community-Based Cross-Sectional Study. BMC Nurs (2018) 17:10–9. doi:10.1186/s12912-018-0278-y
37. Berhe, AK, Muche, AA, Fekadu, GA, and Kassa, GM. Birth Preparedness and Complication Readiness Among Pregnant Women in Ethiopia: A Systematic Review and Meta-Analysis. Reprod Health (2018) 15:182–10. doi:10.1186/s12978-018-0624-2
38. Lake, EA, Demissie, BW, Gebeyehu, NA, Azeze, GA, Gelaw, KA, Fite, RO, et al. Knowledge and Practice of Mothers Towards Sunshine Exposure of Their Children in Ethiopia: A Systematic Review and Meta - Analysis. BMC Pediatr (2022) 22:213–1. doi:10.1186/s12887-022-03281-7
39. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ (2021) 372:n71. doi:10.1136/bmj.n71
40. Limenih, MA, Belay, HG, and Tassew, HA. Birth Preparedness, Readiness Planning and Associated Factors Among Mothers in Farta District, Ethiopia: A Cross-Sectional Study. BMC Pregnancy Childbirth (2019) 19(1):171–10. doi:10.1186/s12884-019-2325-4
41. Markos, D, and Bogale, D. Birth Preparedness and Complication Readiness Among Women of Child Bearing Age Ggroup in Goba Woreda, Oromia Region, Ethiopia. BMC Pregnancy Childbirth (2014) 14(1):282.
42. Affipunguh, PK, and Laar, AS. Assessment of Knowledge and Practice Towards Birth Preparedness and Complication Readiness Among Women in Northern Ghana: A Cross-Sectional Study. Int J Sci Rep (2016) 2(6):121–9. doi:10.18203/issn.2454-2156.intjscirep20161878
43. Silwal, K, Poudyal, JK, Shah, R, Parajuli, S, Basaula, Y, Munikar, S, et al. Factors Influencing Birth Preparedness in Rapti Municipality of Chitwan, Nepal. Int J Pediatr (2020) 2020:7402163. doi:10.1155/2020/7402163
44. Saaka, M, and Alhassan, L. Prevalence and Predictors of Birth Preparedness and Complication Readiness in the Kassena - Nankana District of Ghana: An Analytical Cross- Sectional Study. BMJ Open (2021) 11(3):e042906. doi:10.1136/bmjopen-2020-042906
45. Bapula, A, Newton, SK, Dormechele, W, Rahinatu, BB, Otupiri, E, and Rahinatu, BB. Birth Preparedness and Complication Readiness Among Pregnant Women in Resource-Limited Setting in Rural Northern Ghana. PAMJ-One Health (2021) 6:9. doi:10.11604/pamj-oh.2021.6.9.26900
46. Orwa, J, Gatimu, SM, Mantel, M, Luchters, S, Mugerwa, MA, Brownie, S, et al. Birth Preparedness and Complication Readiness Among Women of Reproductive Age in Kenya and Tanzania: A Community-Based Cross-Sectional Survey (2020) 20:636. doi:10.1186/s12884-020-03329-5
47. City, S, Patil, AA, Koppad, R, Nagendra, K, and Sv, C. Level of Birth Preparedness and Complication Readiness Among Pregnant Women Residing in Urban Slums of Shivamogga City, India. Natl J Community Med (2022) 13:146–50. doi:10.55489/njcm.1332022390
48. Sharma, N, Kumar, N, Singh, S, Malik, JS, and Jangra, A. Status and Determinants of Birth Preparedness and Complication Readiness in a Rural Block of Haryana. J Fam Med Prim Care (2019) 8:482–6. doi:10.4103/jfmpc.jfmpc_372_18
49. Wanjohi, JM, Wanyoro, AK, and Makunyi, EG. Predictors of Birth Preparedness Among Women in Laikipia County, Kenya. Int J Community Med Public Health (2022). doi:10.18203/2394-6040.ijcmph20221511
50. Tobin, E, Enebeli, N, and Ofili, A. Assessment of birth preparedness and complication readiness among pregnant women attending Primary Health Care Centres in Edo State, Nigeria. Ann. Niger. Med. (2014) 8:76. doi:10.4103/0331-3131.153358
51. Agarwal, S, Sethi, V, Srivastava, K, Jha, PK, and Baqui, AH. Birth Preparedness and Complication Readiness Among Slum Women in Indore City, India. J Health Popul Nutr (2010) 28(4):383–91. doi:10.3329/jhpn.v28i4.6045
52. Kasmai, KE, Akpa, OM, and Olayemi, O. Birth Preparedness and Complication Readiness Among Pokot Nomadic Pastoralists’ Pregnant Women in East Pokot District, Midwest-Kenya. Am J Biomed Life Sci (2018). 6:17–23. doi:10.11648/j.ajbls.20180601.13
53. Saha, R, Sarkar, AP, Saha, I, Misra, R, Dasgupta, S, and Chatterjee, S. The Status of Birth Preparedness and Complication Readiness Among Rural Indian Mothers. Int J Public Health Res (2014) 4(2):510–8.
54. Kar, M, Karmee, N, and Satapathy, DM. Birth Preparedness and Complication Readiness Among Pregnant and Recently Delivered Women in Villages of a Block of Ganjam, Odisha, India: A Community Based Cross-Sectional Study. Int J Reprod Contracept Obstet Gynecol (2019) 8(5):2003–10. doi:10.18203/2320-1770.ijrcog20191958
55. Noor, R, Shahid, F, Zafar, M, Hydrie, I, Imran, M, Hassan, S, et al. Factors Influencing Birth Preparedness and Complication Readiness Among Childbearing Age Women in Thatta District, Sindh. PLoS One (2022) 17:e0275243–13. doi:10.1371/journal.pone.0275243
56. Akshaya, KM, and Shivalli, S. Birth Preparedness and Complication Readiness Among the Women Beneficiaries of Selected Rural Primary Health Centers of Dakshina Kannada District, Karnataka, India. PLoS One (2017) 12:e0183739–15. doi:10.1371/journal.pone.0183739
Keywords: birth preparedness, complication readiness, pregnancy, knowledge of danger signs, Ethiopia
Citation: Alamrew A, Ayele M, Shitie Lake E, Mulugeta C, Kumie G and Birara Zemariam A (2024) Predictors of Birth Preparedness and Complication Readiness Practices Among Pregnant Women in Ethiopia, a Systematic Review and Meta-Analysis. Int J Public Health 69:1607296. doi: 10.3389/ijph.2024.1607296
Received: 19 March 2024; Accepted: 14 August 2024;
Published: 02 September 2024.
Edited by:
Sonja Merten, Swiss Tropical and Public Health Institute, SwitzerlandCopyright © 2024 Alamrew, Ayele, Shitie Lake, Mulugeta, Kumie and Birara Zemariam. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Abebaw Alamrew, YWJlYmF3YWxhbXJldzA0QGdtYWlsLmNvbQ==
 Abebaw Alamrew
Abebaw Alamrew