- 1Department of Public Health, Madda Walabu University Goba Referral Hospital, Bale-Goba, Ethiopia
- 2Department of Human Anatomy, Madda Walabu University Goba Referral Hospital, Bale-Goba, Ethiopia
- 3Research Centre for Public Health, Equity and Human Flourishing, Torrens University Australia, Adelaide Campus, Adelaide, SA, Australia
- 4College of Nursing, University of Saskatchewan, Saskatoon, SK, Canada
- 5School of Public Health, College of Health Science, Addis Ababa University, Addis Ababa, Ethiopia
- 6School of Medicine, Madda Walabu University Goba Referral Hospital, Bale-Goba, Ethiopia
- 7Department of Midwifery, Madda Walabu University Goba Referral Hospital, Bale-Goba, Ethiopia
- 8School of Health Sciences, Western Sydney University, Penrith, NSW, Australia
Objectives: This systematic review and meta-analysis aimed to: i) determine the pooled prevalence of acute diarrhea; and ii) synthesize and summarize current evidence on factors of acute diarrheal illnesses among under-five children in Ethiopia.
Methods: A comprehensive systematic search was conducted in PubMed, SCOPUS, HINARI, Science Direct, Google Scholar, Global Index Medicus, Directory of Open Access Journals (DOAJ), and the Cochrane Library. This systematic review and meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline. The methodological quality of each included article was assessed using the Joanna Briggs Institute (JBI) quality assessment tool for cross-sectional and case-control studies. A random-effect meta-analysis model was used to estimate the pooled prevalence of diarrheal illnesses. Heterogeneity and publication bias were assessed using I2 test statistics and Egger’s test, respectively. The statistical analysis was done using STATA™ software version 14.
Results: Fifty-three studies covering over 27,458 under-five children who met the inclusion criteria were included. The pooled prevalence of diarrhea among under-five children in Ethiopia was found to be 20.8% (95% CI: 18.69–22.84, n = 44, I2 = 94.9%, p < 0.001). Our analysis revealed a higher prevalence of childhood diarrhea in age groups of 12–23 months 25.42% (95%CI: 21.50–29.35, I2 = 89.4%, p < 0.001). In general, the evidence suggests that diarrheal risk factors could include: i) child level determinants (child’s age 0–23 months, not being vaccinated against rotavirus, lack of exclusive breastfeeding, and being an under-nourished child); ii) parental level determinants {mothers poor handwashing practices [pooled odds ratio (OR) = 3.05; 95% CI:2.08–4.54] and a history of maternal recent diarrhea (pooled OR = 3.19, 95%CI: 1.94–5.25)}; and iii) Water, Sanitation and Hygiene (WASH) determinants [lack of toilet facility (pooled OR = 1.56, 95%CI: 1.05–2.33)], lack handwashing facility (pooled OR = 4.16, 95%CI: 2.49–6.95) and not treating drinking water (pooled OR = 2.28, 95% CI: 1.50–3.46).
Conclusion: In Ethiopia, the prevalence of diarrhea among children under the age of five remains high and is still a public health problem. The contributing factors to acute diarrheal illnesses were child, parental, and WASH factors. A continued focus on improving access to WASH facilities, along with enhancing maternal hygiene behavior will accelerate reductions in diarrheal disease burden in Ethiopia.
Introduction
Childhood diarrheal disease remains to be the existential threat to global public health scourge. According to the Global Burden of Disease Study 2019, diarrhea disease was listed among the top three most common problems causing a significant health burden in children [1]. Evidence indicates that deaths from diarrheal disease among children under 5 are most prevalent in South Asia and sub-Saharan Africa, where access to healthcare, safe water, and sanitation remains limited [2, 3]. In Ethiopia, although there has been a reduction in the prevalence of diarrheal disease from 24% in 2000 to 12% in 2016, progress has not been sufficiently rapid to fully tackle this significant public health issue [4, 5].
Previous studies conducted in Ethiopia have identified many factors that are associated with childhood diarrhea. These factors include: child’s age [6–10], place of residency [11–13], lack of exclusive breastfeeding [14–17], unvaccinated against rotavirus [7, 14, 18–22], undernutrition [23–25], limited maternal education [11, 23, 24, 26], inadequate knowledge about diarrheal disease [8, 27], poor handwashing practices [15, 24, 28, 29], low wealth status [14, 26, 27, 30, 31], unimproved sources of drinking water [6, 9, 12, 13, 19, 32], and unimproved toilet facilities [7, 19, 20, 32–36].
Despite the fact that diarrhea is largely preventable, it remains a public health problem in Ethiopia, and its burden is still a serious concern. Estimates of the burden of diarrheal disease and its associated factors in Ethiopia at the national level are not well known, masking the current status, a prohibitive factor to tracking progress and reducing morbidity. While it is known this to be an ongoing and significant public health issue needing current evidence, the most review evidence have been over 5 years old [37], which may not reflect the present situation. Additionally, preliminary studies that have recently been conducted throughout the country have reported inconsistent findings [7, 12, 13, 26, 31, 33, 34, 38–44], making it necessary to update the existing review in order to estimate the current nationwide and regional pooled prevalence of diarrheal diseases and associated factors. Therefore, this systematic review and meta-analysis provide updated results of pooled estimates of childhood diarrhea morbidity and summarized its associated factors in Ethiopia. The findings affirm the current status of diarrheal diseases and set a benchmark for tracking the progress toward achieving the Sustainable Development Goals (SDG).
Methods
Protocol Registry
The protocol for this review was registered in the International Prospective Register of Systematic Reviews (PROSPERO), the University of York Centre for Reviews and Dissemination (record ID: CRD42022354416).
Search Strategy and Information Sources
This is an update of the systematic review and meta-analysis, which was conducted using the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines 2020 [45] (Supplementary Material S1).
Eligibility Criteria
Population: children under the age of 5 years (under-fives).
The outcome of interest: prevalence of acute diarrheal illness. Studies that reported diarrhea above 2 weeks were excluded.
Study design: Observational studies (cohort, case-control, and cross-sectional studies) that assessed the prevalence and associated factors of under-five diarrheal disease were included in the study. Any observational studies that did not report either the prevalence or associated factors of acute diarrhea by controlling possible confounders were excluded from the study. Additionally, interventional studies (randomized controlled trials (RCTs), cluster randomized controlled trials (cRCTs) and quasi-experimental (QE) trials), systematic reviews, commentaries, letters to editors, qualitative studies, case studies, books, reports, conference abstracts, non-primary studies, and analysis of policy briefs were excluded.
Study setting: Only studies conducted in Ethiopia.
Publication status: Both published and unpublished studies were considered.
Language: Articles published in the English language were considered.
Publication year: All articles published since 2017 were considered.
Operational Definition
Acute diarrhea: is defined as the passage of three or more loose or liquid stools per day or an increase in stool frequency or liquidity that is considered abnormal during the 2 weeks as reported by the mothers or caregivers [46].
Information Sources
A comprehensive review of English language literature using list of relevant Medical Subject Heading Terms (MeSH) words and sub-headings of keywords was generated and used to search articles from major databases including PubMed, SCOPUS, HINARY, Science Direct, Google Scholar, Global Index Medicus, Directory of Open Access Journals (DOAJ), and the Cochrane Library. Each database’s or search engine’s retrieved articles were added to an EndNote library. Additionally, articles from the retrieved bibliographies that met the inclusion criteria were added to be reviewed. We also used Google Scholar and Google to track citations.
Searching Strategy
The following combination of keywords and other MeSH words was used in the search: diarrhea [MeSH Terms], Diarrhea [Text Word], Diarrhoea [All Filed], Prevalence [Text Word], Factor*, determinant*, child [MeSH Terms], infant [MeSH Terms], under-five children, and Ethiopia. The search terms were used separately and in combination using Boolean operators like “OR” or “AND.” A detail searching strategy was provide in the Supplementary Material S2. The electronic database search was supplemented with gray literature searches via Google Scholar and Google searches. A secondary search method known as “footnote chasing” was also used to identify further and relevant articles. Reference lists of included studies were manually searched for additional relevant articles. Moreover, preprint articles from the MedRxiv, BioRxiv, and Research square databases were also accessed to ensure wider coverage. The related systematic review and meta-analysis published in 2017, in which the subjects from the included studies were mostly enrolled before 2017. In this review, all papers published from first of November 2017 to June 30th, 2022, were considered. All papers published until the June 30th, 2022 were considered. An initial search was conducted on June 1st, 2022 and later repeated on June 30th, 2022 to identify articles.
Study Selection Process
In accordance with predetermined inclusion and exclusion criteria, two investigators (BS and DA) independently screened and identified relevant articles by title, abstract, and full text. The screened articles were compiled by the two authors (BS and DA), and any disagreements between them were settled through discussion. Duplicate articles were then removed from the review after all the searched articles were exported into the EndNote™ version X8 software. After reading the complete texts of the remaining articles, we retained studies that met the inclusion criteria. Based on the eligibility requirements, BS and DA independently reviewed the full text of the articles based on the study eligibility criteria.
Data Extraction
Microsoft™ Excel was used to extract the data. The primary author, publication year, study design, study area, sample size, prevalence of diarrhea, number of children, age of children, sampling techniques, and factors associated with diarrhea were included in the summary of the studies that were included in the review.
Risk of Bias Assessment of the Studies
The quality of the included studies was evaluated using the Joanna Briggs Institute (JBI) method for quality evaluation. We used the JBI checklist for case-control studies and observational studies were used [47]. Two reviewers independently evaluated the included studies’ quality (BS and DA). There are eight and ten parameters in the evaluation tools for cross-sectional and case-control studies, respectively. When the information provided was insufficient to make a decision, we decided to assess a 1 rating for the specific item (a failure to satisfy a specific item or unclear/not applicable). Bias risks were divided into three categories: low (0–2), moderate (3 or 4), and high (total score of 5 or higher). Disagreements are usually remedied through discussion until consensus is reached. However, for the current study, there was no disagreement in selecting the potential research (Supplementary Material S3).
Synthesis of Results
The prevalence of diarrhea and/or associated factors were used in reporting the findings of each study. Where available, 95% CI for reported diarrhea was obtained from the eligible studies. Based on published studies, 95% CI were calculated using available data where the full text of the eligible studies did not report diarrheal estimates. Narrative methods including text and table were used as a tool for associated factors data presentation. The heterogeneity among included studies was assessed by I2 statistics and the Cochran Q-test. The included studies exhibited significant high heterogeneity (I2 = 94.9%, p < 0.001), which led us to compute a random effect meta-analysis model to estimate the pooled prevalence of diarrhea. The pooled prevalence of diarrhea and their corresponding 95% CI were presented using a forest plot. Subgroup analyses were performed to investigate the observed heterogeneity, based on the sub-regions of Ethiopia. Further statistical analyses, such as univariate meta-regression, was also performed to identify possible sources of heterogeneity.
We used a qualitative approach to summarize the factors associated with diarrhea and synthesize the relevant information based on the objectives of the study. We did not perform a meta-analysis for all identified factors due to the considerable heterogeneity of the included studies. We have discussed identified associated factors and estimates descriptively. For some variables, however, the adjusted odds ratios (AOR) were pooled using the generic inverse variance method, which involved converting the adjusted odds ratio to a logarithmic scale and then calculating standard error based on the 95% confidence intervals [48]. The Cochran Q-test and Haggin I2 statistics were used to assess the presence and degree of heterogeneity among included studies [49].
Publication Bias
In this meta-analysis, the presence of publication bias was evaluated using funnel plots and Egger’s weighted regression test at a significance level of less than 0.05.
Sensitivity Analysis
To identify the source of heterogeneity, a leave-one-out analysis was employed. Sensitivity analysis using a random-effects model was performed to assess the influence of a single study on the overall pooled prevalence estimate.
Results
Study Selection
Overall, the searches identified 707 articles (i.e., identification of studies via databases and registers). Of the initial articles, 444 articles were excluded due to duplication. We screened the titles and abstracts of 263 articles and obtained 91 full text articles, of which 53 studies met the inclusion criteria and were included in the final systematic review and meta-analysis. Of the included 53 studies, 44 studies were eligible for meta-analysis (Figure 1).
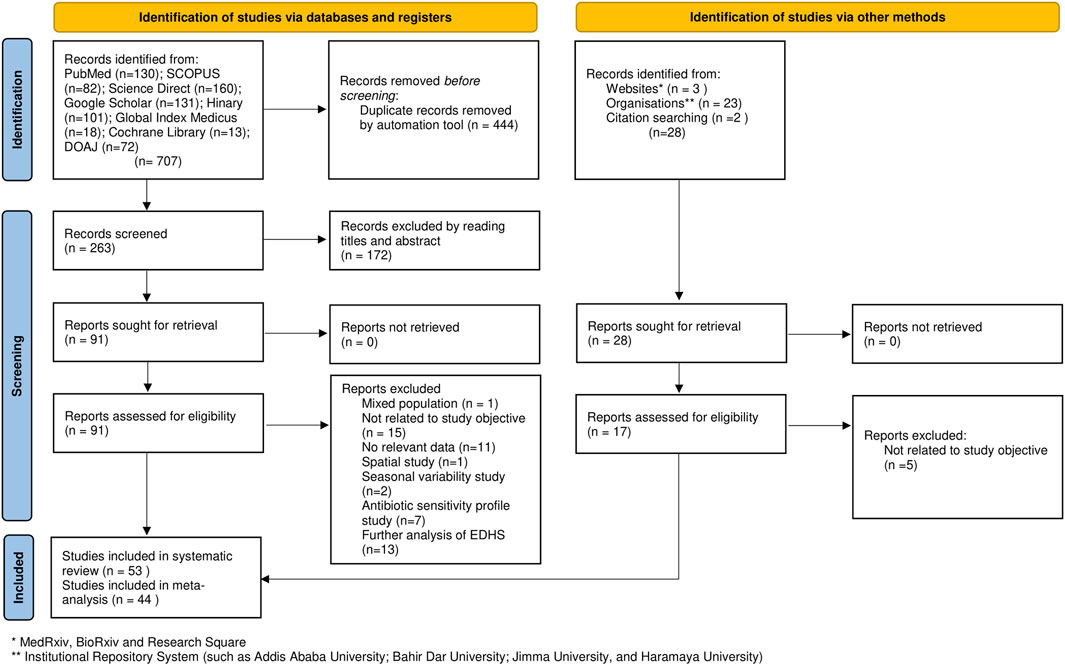
Figure 1. Flow chart of study selection for systematic review and meta-analysis of prevalence of acute diarrhea and associated factors among under-five children in Ethiopia, (Ethiopia, 2017–2022).
Characteristics of Included Studies
The descriptive summary of included cross-sectional and case-control studies were presented in Table 1. Of the included 53 studies, 9 were case-control studies, 12 comparative cross-sectional studies, and 32 cross-sectional studies by design. A total of 27,458 under-five children were included as participants in the current systematic review and meta-analysis. In the current review, the sample size varied from small (n = 191) [61] to large (n = 2,030) [6]. In this review, the lowest prevalence of diarrhea (9.4%) was found in a study conducted in Bahir Dar, northwest Ethiopia Amhara region [14], while the highest prevalence (36.5%) of diarrhea was reported in a study conducted at west Guji zone, Oromia region [62].
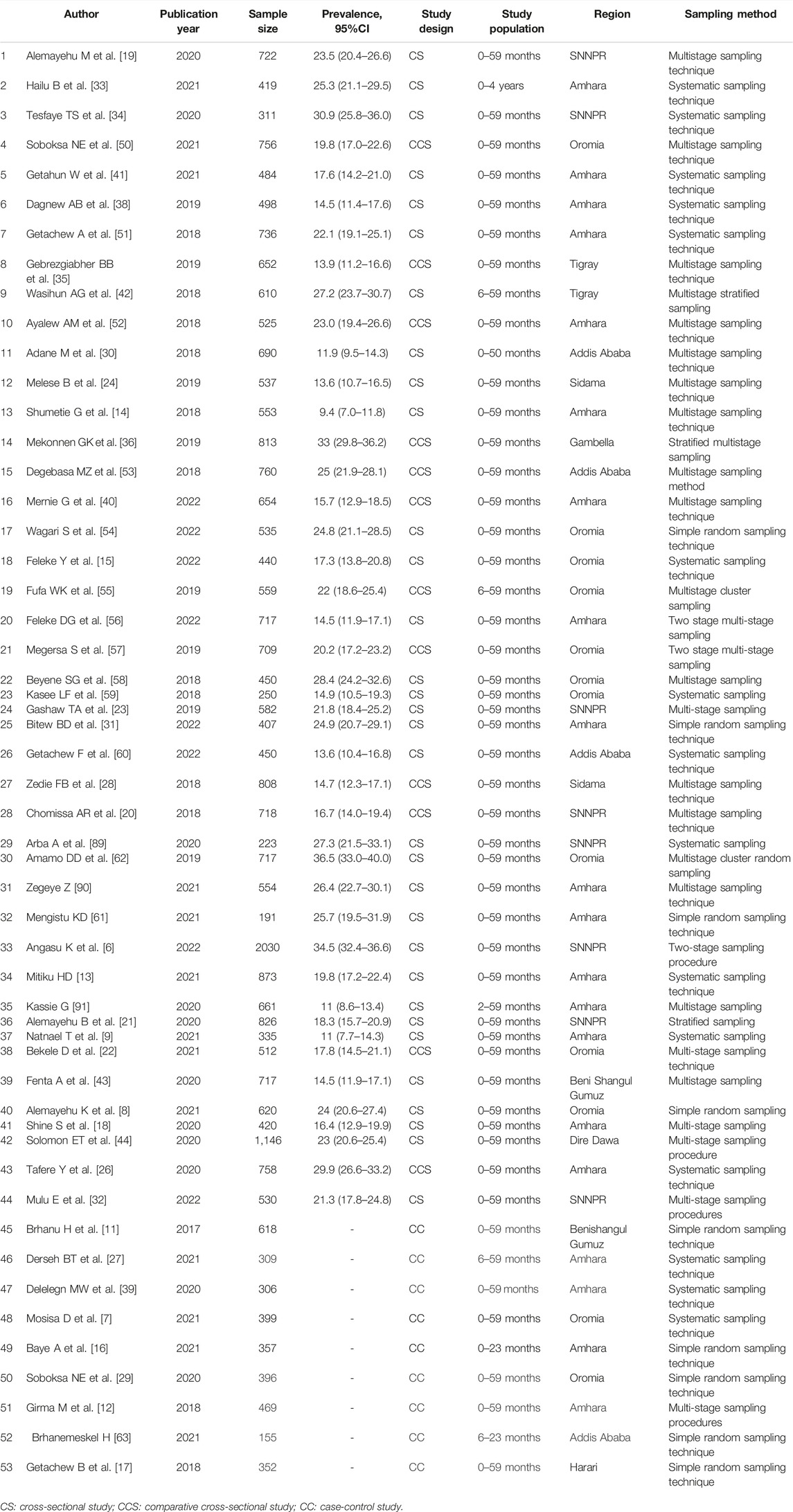
Table 1. Descriptive summary of studies included in this systematic review and meta-analysis of the prevalence and risk factors of diarrhea among under-five children in Ethiopia (Ethiopia, 2017–2022).
Meta-Analysis
The meta-analysis included only studies with a cross-sectional design. The overall pooled prevalence of diarrhea among under-five children in Ethiopia was found to be 20.8% (95% CI: 18.69–22.84, I2 = 94.9%, p < 0.001) (Figure 2).
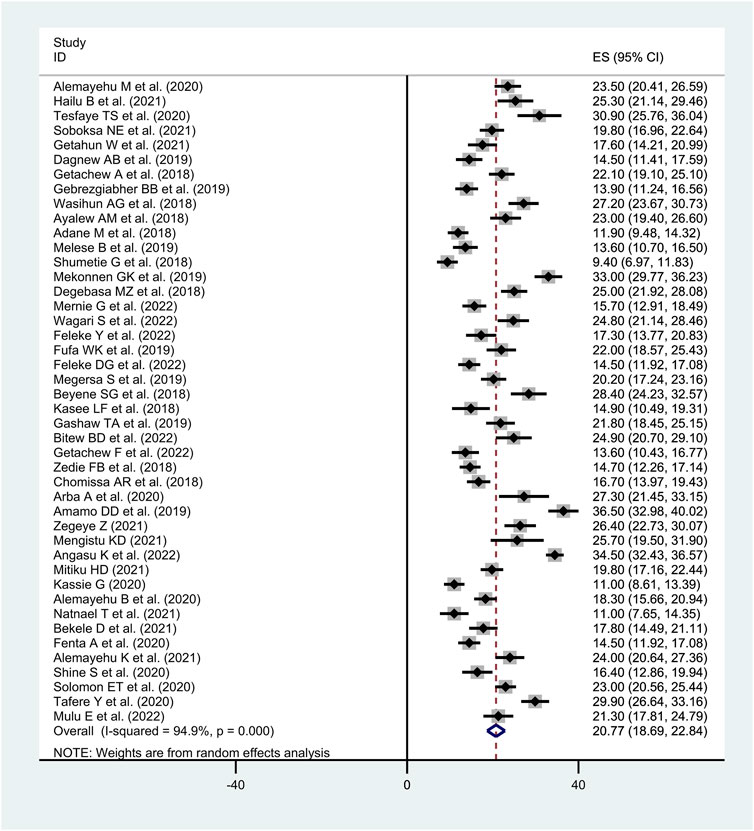
Figure 2. Forest plot of the pooled prevalence of diarrhea among under-five children in Ethiopia, (Ethiopia, 2017–2022).
We performed subgroup analysis based the studies’ geographical settings (i.e., region of the country). Accordingly, the highest proportion of acute diarrhea was observed in Gambella region with a prevalence of 33.0% (95% CI: 29.76–36.23) followed by SNNPR region with a prevalence of 24.2% (95% CI: 18.94–29.47), Dire Dawa city administration 23.0% (95% CI: 20.56–25.44), Oromia 22.6% (95% CI: 18.85–26.28), Amhara region 19.1% (95% CI: 15.95–22.14) and the lowest proportion was reported from Sidama region at 14.2% (95% CI: 12.37–16.11) (Table 2).
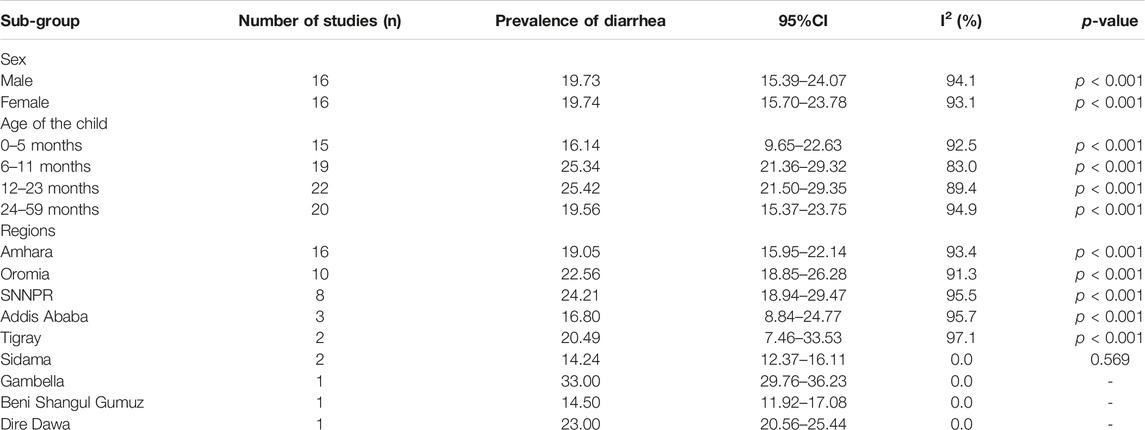
Table 2. Subgroup analysis of acute diarrhea among under-five children in Ethiopia (Ethiopia, 2017–2022).
We conducted a stratification analysis on prevalence, considering age groups and gender. Our findings revealed that the prevalence of diarrhea among male under-five children in Ethiopia was 19.73% (95% CI: 15.39–24.07, I2 = 94.1%, p < 0.001), a rate comparable to that of female children. Additionally, our analysis revealed that the prevalence of childhood diarrhea varied across different age groups:0–5 months was 16.14% (95%CI: 9.65–22.63, I2 = 92.5%, p < 0.001), 6–11 months 25.34% (95%CI: 21.36–29.32, I2 = 83.0%, p < 0.001), 12–23 months 25.42% (95%CI: 21.50–29.35, I2 = 89.4%, p < 0.001), and 24–59 months 19.56% (95%CI: 15.37–23.75, I2 = 94.9%, p < 0.001) (Table 2 and Supplementary Material S4A–D).
Publication Bias
In this meta-analysis, possible publication bias was visualized through funnel plots and using Egger’s weighted regression test. Asymmetrical large, inverted funnel resembled the absence of publication biases (Figure 3). The Egger’s tests were also not statistically significant for the estimated prevalence of diarrhea in Ethiopia, with a p-value of 0.06.
Figure 3. Funnel plot showing publication bias of prevalence of diarrhea among under-five children in Ethiopia, (Ethiopia, 2017–2022).
Sensitivity Analyses
To detect the influence of one study on the overall meta-analysis estimate, sensitivity analysis was conducted using a random-effects model. There was no evidence for the influence of a single study on the overall pooled result of diarrheal morbidity in Ethiopia (Supplementary Material S5).
Meta-Regression
We conducted a univariate meta-regression analysis by considering publication year, sample size, and quality score as covariates to identify the possible sources of heterogeneity across primary studies, but none of these variables was found to be a statistically significant source of heterogeneity. The results of meta-regression analysis also showed no significant relationship between prevalence of diarrheal disease and sampled size (p = 0.084) and publication year (p = 0.729).
Meta-Analysis of Selected Associated Factors and Evidence From the Reviewed Studies
Table 3 demonstrates the summary of the studies included in this review. The factors associated with acute diarrheal disease have been divided into categories of child, parental, and WASH and environmental factors.
Table 3. Summary of risk factors and there strength of association of acute diarrhea among under-five children in Ethiopia, (Ethiopia, 2017–2022).
Child Related Factors
The most consistent factors associated with diarrhea, as shown in Table 3 were the child’s age, feeding status, nutritional status, and vaccination status for rotavirus.
Several studies consistently reported the highest prevalence of diarrhea among children occurred between one and 12 months of age [7, 8, 11, 15, 18, 31, 36, 54, 62]. Studies also found that bottled-fed children [11, 32, 63], not breastfeeding [38, 51], lack of exclusive breastfeeding [14–17], and starting complementary feeding before 6 months [61, 62] were the commonly identified associated factors with childhood diarrheal disease. Moreover, not being vaccinated against rotavirus [7, 14, 18–22], playing with soil and a habit of eating soil [33], being underweight [23, 24], and not receiving Vitamin A supplementation [22, 62] were factors associated with higher risk of diarrheal disease. Three studies found an increased risk of diarrheal disease among children living in households with two and above under-fives [50, 53, 62] (Table 3).
Supplementary Material S4A–F presents the pooled odds ratios of the association between child age, the child’s sex, and childhood diarrhea in Ethiopia. As depicted in Supplementary Material S6A, there is no statistically significant difference in the odds of experiencing childhood diarrheal disease between male and female children under the age of five (pooled OR = 0.61; 95% CI: 0.35–1.07, I2 = 88.0%, p < 0.001).
The likelihood of childhood diarrhea was 1.79 times higher among children aged 0–5 months (pooled OR = 1.79, 95% CI: 1.05–3.05, I2 = 60.8%, p = 0.006), 2.40 times higher among children aged 6–11 months (pooled OR = 2.40, 95% CI: 1.77–3.25, I2 = 38.3%, p = 0.071), and 1.65 times higher among children aged 12–23 months (pooled OR = 1.65, 95% CI: 1.07–2.54, I2 = 73.1%, p < 0.001) compared with children aged 48–59 months (Supplementary Material S6B–D).
However, there is no statistically significant association observed between diarrhea occurrence among children aged 24–35 months (pooled OR = 1.16, 95% CI: 0.89–1.51, I2 = 27.5%, p = 0.168) and 36–47 months (pooled OR = 1.15, 95% CI: 0.73–1.80, I2 = 62.1%, p = 0.015) when compared with those aged 48–59 months (Supplementary Material S6E, F).
Parental and Household Factors
Across the studies, the lack of maternal education [6, 11, 23, 24, 26, 62], poor maternal knowledge about diarrheal disease and its prevention measures [8, 27], and mothers poor handwashing practices (i.e., not washing their hands at the critical times, such as after visiting toilet, after touching children’s feces) [7, 12, 13, 26, 31, 33, 34, 38–44] were identified associated factors with acute diarrheal disease (Table 3).
This meta-analysis’s findings showed that there was association between mothers not washing their hands after using the toilet with children having diarrhea (pooled OR = 3.05; 95% CI:2.08–4.54, I2 = 75.3%, p < 0.001, n = 15) (Supplementary Material S7A). Four studies [6, 15, 30, 54] used different reference categories, and we pooled the confounder adjusted odds ratios separately. Similarly, the odds of childhood diarrhea was lower by 51% among children whose mothers washed their hands at the critical time (pooled OR = 0.49, 95% CI: 0.31–0.70, I2 = 48.6%, p = 0.120, n = 4).
Mothers’ history of diarrheal episodes in the previous 2 weeks before the study was also identified as a risk factor for childhood diarrheal disease [7, 11, 17, 19, 20, 26, 27, 35, 39, 60, 64]. The overall result of the meta-analysis revealed that children whose mothers had a history of diarrhea in the previous 2 weeks were three times more likely to develop diarrhea than children without a history of maternal diarrhea in the previous 2 weeks (pooled OR = 3.19, 95%CI: 1.94–5.25, n = 13). We used a random effect meta-analysis model to estimate pooled OR because the included studies had high heterogeneity (I2 = 79.4%, p-value = 0.006) (Supplementary Material S7B). Since two studies [28, 54] used different reference categories, we pooled the odds ratios separately. Likewise, the odds of diarrhea was reduced in children whose mothers had not recently experienced any diarrheal episode (pooled OR = 0.49, 95% CI: 0.35–0.68, I2 = 0.0%, p = 0.901, n = 2).
Water, Sanitation and Hygiene (WASH) Factors
As shown in Table 3, the most consistent WASH related factors associated with diarrheal disease in Ethiopia were i) the lack of toilet facility or use of unimproved toilet facility [7, 19, 20, 32–36], ii) the poor latrine hygienic condition [9, 16, 17, 19, 26, 43, 56], iii) unsafe child stool disposal [11, 12,19, 20, 26, 27, 39–41], iv) poor domestic solid waste disposal [7, 8,14, 19, 40, 42, 56, 62], v) not treating drinking water [11, 27, 28, 39, 50], vi) collecting water from unimproved drinking sources [6, 9, 12, 13, 19, 21, 32, 40, 42], and vii) lacked handwashing facilities near the toilet facilities [12, 38, 56, 60].
The pooled result of this meta-analysis indicated that children from households that lacked handwashing facilities near the toilet were 4.16 times more likely to have diarrheal morbidity as compared to their counterparts (pooled OR = 4.16, 95%CI: 2.49–6.95, I2 = 71.1%, p = 0.001, n = 9) (Supplementary Material S7C). Children living in households without latrine facilities were found to be 1.56 times more likely to develop diarrhea than children living in households with latrine facilities (pooled OR = 1.56, 95%CI: 1.05–2.33, I2 = 71.1%, p = 0.001, n = 9) (Supplementary Material S7D).
The meta-analysis results of ten studies that reported confounder adjusted association between household water treatment and childhood diarrhea. The overall result showed that, children from households that did not use treated drinking water at home were two times higher odds of having diarrheal disease compared to children living in households that used home treated drinking water (pooled OR = 2.28, 95% CI: 1.50–3.46, I2 = 64.5%, p = 0.003, n = 10) (Supplementary Material S7E).
Discussion
Childhood diarrheal disease can cause significant morbidity and remain a significant public health issue across the world. This systematic review and meta-analysis aimed to estimate the pooled prevalence of diarrhea disease and summarize the potential associated factors among under-fives in Ethiopia. The pooled prevalence showed that one in every five children under the age of 5 years in Ethiopia experienced diarrheal disease. Overall, early childhood, poor child nutrition status, use of unimproved sanitation, lack of hand washing facilities, maternal diarrhea illness in previous 2 week, inadequate maternal hygiene knowledge and behavior, and improper domestic solid waste disposal were important factors associated with diarrheal disease.
The meta-analysis findings from the included 44 studies indicated that 20.8% of children under five in Ethiopia experienced diarrheal diseases. The results are comparable with the 2016 Ugandan Demographic and Health Survey (DHS) that reported the prevalence of diarrhea among children <5 years in Uganda to be 20% [65]. Our finding was in line with the prior pooled prevalence estimates of diarrhea 22% [37]. Although the results showed a relatively lower prevalence, this figure seemed to imply that the prevalence of diarrheal disease has not dropped significantly. As such, it would be reasonable to argue that diarrheal disease was still a significant public health concern of high magnitude in Ethiopia. On the other hand, our finding showed that the diarrheal disease prevalence was higher than the overall prevalence of diarrheal disease among under-fives in sub-Saharan Africa 15.3% [66] and the East Africa pooled estimate 14.28% [67]. The observed higher prevalence of diarrheal disease in this review compared to the East Africa regional estimate could be due to the differences in methodological approaches. The DHS sampling, design, and setting were very different from the type of analysis that was used in the current study. The results of DHS reports are based on primary data collection, whereas we reviewed and used prevalence measurements from previously conducted primary studies from different areas, populations, and seasons.
The top three regions with the highest prevalence of diarrhea were observed in the Gambella region, 33.0%, SNNPR region 24.21%, and Dire Dawa city administration 23.0%, according to the subgroup analysis of this study. The Sidama region had the lowest proportion of diarrheal disease, at 14.24%. Regional estimates could differ due to differences in basic sanitation, household behavioral characteristics, and access to healthcare facilities. The high prevalence of diarrheal disease in the Gambella region could also be due to the inclusion of a single comparative cross-sectional study in sub-group meta-analysis, which was limited to a single area and did not represent the entire region. Corresponding to the Ethiopia DHS 2016 report, the Gambela region had the highest diarrheal morbidity in Ethiopia (14.5%), followed by the SNNP region (13.9%) [4].
The findings of our review suggest that there is no significant difference in the prevalence of childhood diarrheal disease between male and female children under the age of five. This observation aligns with previous studies that have also failed to identify gender as a significant risk factor for diarrheal illness [68]. Our study adds to the body of evidence indicating that diarrheal disease does not exhibit a gender-specific pattern among young Ethiopian children. Our review also highlights a notably high prevalence of diarrheal disease among children aged 12–23 months. Several factors may contribute to the heightened susceptibility in this age group, including increased mobility and exploratory behavior, which lead to greater exposure to contaminated environments [69].
The current study found lack of exclusive breastfeeding to be associated with a higher likelihood of diarrheal disease in children [14–17]. Evidence showed that breastfeeding is an ideal food for infants and young children and it prevents nearly half of all diarrheal episodes and 72% of diarrheal-related hospitalizations [70, 71]. Breast milk is safe, clean, and contains antibodies which help to protect children against many common childhood illnesses [72]. A meta-analyses of eighteen studies showed that not breastfeeding resulted in an excess risk of diarrheal mortality in comparison to exclusive breastfeeding among infants 0–5 months of age and to any breastfeeding among children aged 6–23 months [70]. This study identified significant association between being underweight [26, 27] and wasting [14] and childhood diarrhea. The relationship between child undernutrition and diarrheal illnesses was clearly shown [73] as diarrheal disease and malnutrition being bidirectionally related, meaning that: diarrhea causes malnutrition, and malnutrition worsens the course of diarrheal disease [74].
Across the studies, lack of maternal education was consistently associated with higher odds of childhood diarrheal [6, 11, 23, 24, 26, 62], which is consistent with research conducted in Nigeria [75]. The educational attainment of mothers influences hygienic practices, child feeding, weaning, and sanitation practices, all of which are crucial factors against the onset of childhood diarrheal disease. Primary studies identified mothers’ poor handwashing practices [7, 12, 13, 26, 31, 33, 34, 38–44] and mothers’ history of diarrheal episodes in the previous 2 weeks [7, 11, 17, 19, 20, 26, 27, 35, 39, 60, 64] as potential factor associated with childhood diarrhea. The result of this meta-analysis revealed that, the odds of childhood diarrhea was three times higher among children whose mothers did not practice hand washing at critical times. Likewise, the odds of childhood diarrhea among children whose mother had a history of diarrhea in the previous 2 weeks was three times higher than their counterparts. The importance of proper handwashing at critical times with appropriate handwashing agents has long been established in the reduction of diarrheal disease with handwashing with soap reducing the burden significantly [76–78]. For instance, a recent systematic review, handwashing promotion in communities prevents one-quarter of diarrhea episodes in Low and Middle-Income Countries (LMICs) [79]. The pooled result of this meta-analysis indicated that children from households that lacked handwashing facilities near the toilet were four times more likely to have diarrheal morbidity as compared to their counterparts. This finding supports previous studies which have identified lack of a handwashing station as predictors of diarrheal disease [12, 38, 56, 60]. This finding was not surprising as several studies explore strong link between handwashing and childhood diarrhea [80]. A systematic review of the literature by Shah et al. also reported handwashing are effective strategy for preventing all causes of diarrheal disease [81].
Children living in households that used untreated drinking water and those collecting water from unimproved drinking water sources were at a higher risk of diarrheal disease. Several studies provided evidence that improving access to safe drinking water reduces the risk of diarrheal disease in children [25, 82]. In our meta-analysis, the odds of developing childhood diarrhea in households that did not use treated drinking water at home were two fold higher compared to children used home treated drinking water, and that improved water quality was generally is an effective strategy in preventing diarrheal disease [83]. Although evidence exists that improved sanitation is one of the key factors in the reduction of diarrheal diseases [52, 84], however, to establish the effect of improved latrines on diarrheal disease prevention in the absence of universal or at least adequate latrine coverage in a given community is controversial and difficult as indicated in the recent cluster-randomized controlled trial on sanitation interventions reporting that improved latrines had no protective effect against childhood diarrheal prevalence [85, 86]. However, other systematic review and meta-analysis have shown that both improved neighborhood sanitation conditions and household sanitation are associated with reduced diarrheal illness [87].
Limitations
First, in the majority of the included studies diarrheal disease was based on self-reported screening and was not further clinically confirmed. Second, our study could lack representativeness at a country level as we did not find a study from some regions of Ethiopia. Third, there was high heterogeneity between included studies, as indicated by the I2 statistic. Fourth, we were unable to pool all the adjusted odds ratio as a number of the included studies showed significant heterogeneity and used different reference category. As a result, this work only summarizes the findings as described in the study protocol. Fifth, because the studies in this review were all observational in design, it is possible that other confounding variables could influence the identified associated factors. Sixth, the majority of included articles were observational studies (i.e., cross-sectional studies), so causality cannot be inferred. Last but not least, because our search was restricted to publicly accessible databases, we were unable to include databases like EMBASE.
Conclusion
Our study indicated that approximately one in five under-five children in Ethiopia experienced diarrheal disease during the 2 weeks, and there were regional variations in diarrheal prevalence among under-five children. The key contributing factors to childhood diarrheal were related to child, parental, and WASH factors (such as poor handwashing practices, use of untreated drinking, household that lacked handwashing facility near the toilet facility, and lack of toilet facility). To address diarrheal disease and achieve the Sustainable Development Goals and the 2030 agenda [88], Ethiopia must strive to strengthen current strategies and consider the identified factors. To reduce diarrheal disease among children under the age of five, priority should be given to strengthening interventions that focus on improving household WASH facilities and raising awareness about the importance of handwashing, proper sanitation, and hygiene practices.
Author Contributions
BS: Conceptualization, Formal analysis, Investigation, Methodology, Writing–original draft. DA: Investigation, Methodology; Writing–review and editing. LM, PP, AK, YT, FD, DZ, TM, and DG: Visualization, Validation, Writing–review and editing. KA: Supervision, Visualization, Validation, Writing–review and editing. All authors contributed to the article and approved the submitted version.
Funding
The author(s) declare(s) that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of Interest
The authors declare that they do not have any conflicts of interest.
Acknowledgments
The authors would like to thank Madda Walabu University Goba Referral Hospital Public Health Department staff for providing their unreserved support.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/ijph.2024.1606399/full#supplementary-material
References
1. Vos, T, Lim, SS, Abbafati, C, Abbas, KM, Abbasi, M, Abbasifard, M, et al. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990–2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet (2020) 396(10258):1204–22. doi:10.1016/S0140-6736(20)30925-9
2. Troeger, C, Forouzanfar, M, Rao, PC, Khalil, I, Brown, A, Reiner, RC, et al. Estimates of Global, Regional, and National Morbidity, Mortality, and Aetiologies of Diarrhoeal Diseases: A Systematic Analysis for the Global Burden of Disease Study 2015. Lancet Infect Dis (2017) 17(9):909–48. doi:10.1016/S1473-3099(17)30276-1
3. Ugboko, HU, Nwinyi, OC, Oranusi, SU, and Oyewale, JO. Childhood Diarrhoeal Diseases in Developing Countries. Heliyon (2020) 6(4):e03690. doi:10.1016/j.heliyon.2020.e03690
4. EDHS. Central Statistical Agency (CSA) [Ethiopia] and ICF. 2016. Ethiopia Demographic and Health Survey 2016. Addis Ababa, Ethiopia, and Rockville, Maryland, USA: CSA and ICF (2016).
5. EDHS. Central Statistical Authority [Ethiopia] and ORC Macro. 2001. Ethiopia Demographic and Health Survey 2000. Addis Ababa, Ethiopia and Calverton, Maryland, USA: Central Statistical Authority and ORC Macro (2000).
6. Angasu, K, Dame, KT, and Negash, A. Diarrheal Morbidity and Associated Factors Among Under-Five Children in Southwest Ethiopia: Institution Based Cross-Sectional Study. Durham, NC, United States: Research Square (2022). Available from: https://www.researchsquare.com/article/rs-1210060/v1 (Accessed June 15, 2022).
7. Mosisa, D, Aboma, M, Girma, T, and Shibru, A. Determinants of Diarrheal Diseases Among Under Five Children in Jimma Geneti District, Oromia Region, Ethiopia, 2020: A Case-Control Study. BMC Pediatr (2021) 21(1):532. doi:10.1186/s12887-021-03022-2
8. Alemayehu, K, Oljira, L, Demena, M, Birhanu, A, and Workineh, D. Prevalence and Determinants of Diarrheal Diseases Among Under-Five Children in Horo Guduru Wollega Zone, Oromia Region, Western Ethiopia: A Community-Based Cross-Sectional Study. Can J Infect Dis Med Microbiol (2021) 2021:5547742. doi:10.1155/2021/5547742
9. Natnael, T, Lingerew, M, and Adane, M. Prevalence of Acute Diarrhea and Associated Factors Among Children Under Five in Semi-Urban Areas of Northeastern Ethiopia. BMC Pediatr (2021) 21(1):290. doi:10.1186/s12887-021-02762-5
10. Sahiledengle, B, Kumie, A, Atlaw, D, Tekalegn, Y, Woldeyohannes, D, Zenbaba, D, et al. The Role of Household Flooring on Childhood Diarrhea Among Children 0 to 23 Months of Age in Ethiopia: A Nationally Representative Cross-Sectional Study Using a Multi-Level Mixed Effect Analysis. Environ Health Insights (2021) 15:11786302211064423. doi:10.1177/11786302211064423
11. Brhanu, H, Negese, D, and Gebrehiwot, M. Determinants of Acute Diarrheal Disease Among Under-Five Children in Pawi Hospital, Northwest Ethiopia. Am J Pediatr (2017) 3(6):68. doi:10.11648/j.ajp.20170306.12
12. Girma, M, Gobena, T, Medhin, G, Gasana, J, and Roba, KT. Determinants of Childhood Diarrhea in West Gojjam, Northwest Ethiopia: A Case Control Study. Pan Afr Med J (2018) 30:234. doi:10.11604/pamj.2018.30.234.14109
13. Mitiku, HD. Determinates of Diarrhea Among Under-Five Children in Northwest Ethiopia. IJIER (2021) 9(5):92–103. doi:10.31686/ijier.vol9.iss5.3074
14. Shumetie, G, Gedefaw, M, Kebede, A, and Derso, T. Exclusive Breastfeeding and Rotavirus Vaccination Are Associated With Decreased Diarrheal Morbidity Among Under-Five Children in Bahir Dar, Northwest Ethiopia. Public Health Rev (2018) 39:28. doi:10.1186/s40985-018-0107-6
15. Feleke, Y, Legesse, A, and Abebe, M. Prevalence of Diarrhea, Feeding Practice, and Associated Factors Among Children Under Five Years in Bereh District, Oromia, Ethiopia. Infect Dis Obstet Gynecol (2022) 2022:4139648. doi:10.1155/2022/4139648
16. Baye, A, Adane, M, Sisay, T, and Hailemeskel, HS. Priorities for Intervention to Prevent Diarrhea Among Children Aged 0–23 Months in Northeastern Ethiopia: A Matched Case-Control Study. BMC Pediatr (2021) 21(1):155. doi:10.1186/s12887-021-02592-5
17. Getachew, B, Mengistie, B, Mesfin, F, and Argaw, R. Factors Associated With Acute Diarrhea Among Children Aged 0-59 Months in Harar Town, Eastern Ethiopia. East Afr J Health Biomed Sci (2018) 2(1):26–35.
18. Shine, S, Muhamud, S, Adanew, S, Demelash, A, and Abate, M. Prevalence and Associated Factors of Diarrhea Among Under-Five Children in Debre Berhan Town, Ethiopia 2018: A Cross Sectional Study. BMC Infect Dis (2020) 20(1):174. doi:10.1186/s12879-020-4905-3
19. Alemayehu, M, Alemu, T, and Astatkie, A. Prevalence and Determinants of Diarrhea Among Under-Five Children in Benna Tsemay District, South Omo Zone, Southern Ethiopia: A Community-Based Cross-Sectional Study in Pastoralist and Agropastoralist Context. Adv Public Health (2020) 2020:1–11. doi:10.1155/2020/4237368
20. Abdi Reshid, C. Prevalence and Associated Risk Factors of Diarrhea in Under-Five Children Among Health Extension Model and Non-Model Kebeles in Getta District, Southern Ethiopia: A Community Based Comparative Cross-Sectional Study. Master’s thesis. Jimma, Ethiopia: Jimma University (2018).
21. Alemayehu, B, Ayele, BT, Kloos, H, and Ambelu, A. Individual and Community-Level Risk Factors in Under-Five Children Diarrhea Among Agro-Ecological Zones in Southwestern Ethiopia. Int J Hyg Environ Health (2020) 224:113447. doi:10.1016/j.ijheh.2019.113447
22. Bekele, D, Merdassa, E, Desalegn, M, Mosisa, G, and Turi, E. Determinants of Diarrhea in Under-Five Children Among Health Extension Model and Non-Model Families in Wama Hagelo District, West Ethiopia: Community-Based Comparative Cross-Sectional Study. J Multidiscip Healthc (2021) 14:2803–15. doi:10.2147/JMDH.S324846
23. Gashaw, TA. Prevalence and Determinate Factors of Diarrhea Morbidity Among Under Five Children in Shake Zone, Southwest Ethiopia, a Community Based Cross-Sectional Study. Arch Community Med Public Health (2019) 5(1):008–14. doi:10.17352/2455-5479.000046
24. Melese, B, Paulos, W, Astawesegn, FH, and Gelgelu, TB. Prevalence of Diarrheal Diseases and Associated Factors Among Under-Five Children in Dale District, Sidama Zone, Southern Ethiopia: A Cross-Sectional Study. BMC Public Health (2019) 19(1):1235. doi:10.1186/s12889-019-7579-2
25. Kumie, A. The Effect of Improved Water and Sanitation on Diarrhea: Evidence From Pooled Ethiopia Demographic and Health Surveys – A Multilevel Mixed-Effects Analysis. Ethiop J Health Dev (2020) 34(4).
26. Tafere, Y, Abebe Abate, B, Demelash Enyew, H, and Belete Mekonnen, A. Diarrheal Diseases in Under-Five Children and Associated Factors Among Farta District Rural Community, Amhara Regional State, North Central Ethiopia: A Comparative Cross-Sectional Study. J Environ Public Health (2020) 2020:6027079. doi:10.1155/2020/6027079
27. Derseh, BT, Tafese, NM, Panari, H, Bilchut, AH, and Dadi, AF. Behavioral and Environmental Determinants of Acute Diarrhea Among Under-Five Children From Public Health Facilities of Siyadebirena Wayu District, North Shoa Zone, Amhara Regional State, Ethiopia: Unmatched Case-Control Study. PLOS ONE (2021) 16(11):e0259828. doi:10.1371/journal.pone.0259828
28. Berhe Zedie, F, and Hailu Kassa, D. Socio-Economic, Behavioral and Environmental Factors Associated With Diarrhea Among Under Five Children in Health Development and Non-Health Development Army Member Mothers in Wondogenet, South Ethiopia. Health Educ Care (2018) 3(3):1–8. doi:10.15761/hec.1000144
29. Soboksa, NE, Gari, SR, Hailu, AB, and Alemu, BM. Association Between Microbial Water Quality, Sanitation and Hygiene Practices and Childhood Diarrhea in Kersa and Omo Nada Districts of Jimma Zone, Ethiopia. PLOS ONE (2020) 15(2):e0229303. doi:10.1371/journal.pone.0229303
30. Adane, M, Mengistie, B, Mulat, W, Medhin, G, and Kloos, H. The Most Important Recommended Times of Hand Washing With Soap and Water in Preventing the Occurrence of Acute Diarrhea Among Children Under Five Years of Age in Slums of Addis Ababa, Ethiopia. J Community Health (2018) 43(2):400–5. doi:10.1007/s10900-017-0437-1
31. Bitew, BD, Getachew, A, and Azanaw, J. Diarrhea Prevalence and Associated Factors Among Under-Five Children in the Periphery Area of Azezo Sub-City, Gondar, Northwest Ethiopia: A Community Based Cross-Sectional Study. Durham, NC, United States: Research Square (2021). Available from: https://www.researchsquare.com/article/rs-1129227/v1 (Accessed June 15, 2022).
32. Mulu, E, Nigusie, A, and Endehabtu, BF. Prevalence and Factors Associated With Acute Diarrheal Disease Among Under-Five Children in Southern Ethiopia: Community Based Cross Sectional Study. Durham, NC, United States: Research Square (2020). Available from: https://www.researchsquare.com/article/rs-28183/v1 (Accessed June 15, 2022).
33. Hailu, B, Ji-Guo, W, and Hailu, T. Water, Sanitation, and Hygiene Risk Factors on the Prevalence of Diarrhea Among Under-Five Children in the Rural Community of Dangila District, Northwest Ethiopia. J Trop Med (2021) 2021:2688500. doi:10.1155/2021/2688500
34. Tesfaye, TS, Magarsa, AU, and Zeleke, TM. Moderate to Severe Diarrhea and Associated Factors Among Under-Five Children in Wonago District, South Ethiopia: A Cross-Sectional Study. Pediatr Health Med Ther (2020) 11:437–43. doi:10.2147/PHMT.S266828
35. Gebrezgiabher, BB, Abraha, TH, Tetemke, D, Gidey, G, Asres, N, Tesfamariam, A, et al. Diarrheal Disease in Under-Five Children Among Model and Non-Model Families in Northern Ethiopia, 2017: A Comparative Cross-Sectional Study. BMC Res Notes (2019) 12(1):300. doi:10.1186/s13104-019-4322-0
36. Mekonnen, GK, Alemu, BM, Mulat, W, Sahilu, G, and Kloos, H. Risk Factors for Acute Childhood Diarrhea: A Cross-Sectional Study Comparing Refugee Camps and Host Communities in Gambella Region, Ethiopia. Trav Med Infect Dis (2019) 31:101385. doi:10.1016/j.tmaid.2019.02.003
37. Alebel, A, Tesema, C, Temesgen, B, Gebrie, A, Petrucka, P, and Kibret, GD. Prevalence and Determinants of Diarrhea Among Under-Five Children in Ethiopia: A Systematic Review and Meta-Analysis. PLOS ONE (2018) 13(6):e0199684. doi:10.1371/journal.pone.0199684
38. Dagnew, AB, Tewabe, T, Miskir, Y, Eshetu, T, Kefelegn, W, Zerihun, K, et al. Prevalence of Diarrhea and Associated Factors Among Under-Five Children in Bahir Dar City, Northwest Ethiopia, 2016: A Cross-Sectional Study. BMC Infect Dis (2019) 19(1):417. doi:10.1186/s12879-019-4030-3
39. Delelegn, MW, Endalamaw, A, and Belay, GM. Determinants of Acute Diarrhea Among Children Under-Five in Northeast Ethiopia: Unmatched Case–Control Study. Pediatr Health Med Ther (2020) 11:323–33. doi:10.2147/PHMT.S256309
40. Mernie, G, Kloos, H, and Adane, M. Prevalence of and Factors Associated With Acute Diarrhea Among Children Under Five in Rural Areas in Ethiopia With and Without Implementation of Community-Led Total Sanitation and Hygiene. BMC Pediatr (2022) 22(1):148. doi:10.1186/s12887-022-03202-8
41. Getahun, W, and Adane, M. Prevalence of Acute Diarrhea and Water, Sanitation, and Hygiene (WASH) Associated Factors Among Children Under Five in Woldia Town, Amhara Region, Northeastern Ethiopia. BMC Pediatr (2021) 21(1):227. doi:10.1186/s12887-021-02668-2
42. Wasihun, AG, Dejene, TA, Teferi, M, Marugán, J, Negash, L, Yemane, D, et al. Risk Factors for Diarrhoea and Malnutrition Among Children Under the Age of 5 Years in the Tigray Region of Northern Ethiopia. PLOS ONE (2018) 13(11):e0207743. doi:10.1371/journal.pone.0207743
43. Fenta, A, Alemu, K, and Angaw, DA. Prevalence and Associated Factors of Acute Diarrhea Among Under-Five Children in Kamashi District, Western Ethiopia: Community-Based Study. BMC Pediatr (2020) 20(1):236. doi:10.1186/s12887-020-02138-1
44. Solomon, ET, Gari, SR, Kloos, H, and Mengistie, B. Diarrheal Morbidity and Predisposing Factors Among Children Under 5 Years of Age in Rural East Ethiopia. Trop Med Health (2020) 48:66. doi:10.1186/s41182-020-00253-4
45. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ (2021) 372:n71. doi:10.1136/bmj.n71
46. World Health Organization. Diarrhoeal Disease (2022). Available from: https://www.who.int/news-room/fact-sheets/detail/diarrhoeal-disease (Accessed July 20, 2022).
47. Joanna Briggs Institute (JBI). Critical-appraisal-Tools - Critical Appraisal Tools (2022). Available from: https://jbi.global/critical-appraisal-tools (Accessed November 28, 2022).
48. Reeves, BC, Deeks, JJ, Higgins, JP, Shea, B, Tugwell, P, Wells, GA, et al. Including Non-Randomized Studies on Intervention Effects. Cochrane handbook Syst Rev Interventions (2019) 595–620. doi:10.1002/9781119536604.ch24
49. DerSimonian, R, and Laird, N. Meta-Analysis in Clinical Trials. Control Clin Trials (1986) 7(3):177–88. doi:10.1016/0197-2456(86)90046-2
50. Soboksa, NE, Hailu, AB, Gari, SR, and Alemu, BM. Water Supply, Sanitation and Hygiene Interventions and Childhood Diarrhea in Kersa and Omo Nada Districts of Jimma Zone, Ethiopia: A Comparative Cross-Sectional Study. J Health Popul Nutr (2019) 38(1):45. doi:10.1186/s41043-019-0205-1
51. Getachew, A, Guadu, T, Tadie, A, Gizaw, Z, Gebrehiwot, M, Cherkos, DH, et al. Diarrhea Prevalence and Sociodemographic Factors Among Under-Five Children in Rural Areas of North Gondar Zone, Northwest Ethiopia. Int J Pediatr (2018) 2018:6031594. doi:10.1155/2018/6031594
52. Ayalew, AM, Mekonnen, WT, Abaya, SW, and Mekonnen, ZA. Assessment of Diarrhea and its Associated Factors in Under-Five Children Among Open Defecation and Open Defecation-Free Rural Settings of Dangla District, Northwest Ethiopia. J Environ Public Health (2018) 2018:4271915. doi:10.1155/2018/4271915
53. Degebasa, M, Dawit, Z, and Marama, M. Diarrheal Status and Associated Factors in Under Five Years Old Children in Relation to Implemented and Unimplemented Community-Led Total Sanitation and Hygiene in Yaya Gulele in 2017. Pediatr Health Med Ther (2018) 9:109–21. doi:10.2147/PHMT.S159366
54. Wagari, S, Girma, H, and Geremew, A. Water, Sanitation, and Hygiene Service Ladders and Childhood Diarrhea in Haramaya Demographic and Health Surveillance Site, Eastern Ethiopia. Environ Health Insights (2022) 16:11786302221091416. doi:10.1177/11786302221091416
55. Kebede, FW, Berhe Gebremedhin, G, Gebregergs, GB, and Marama Mokonnon, T. Assessment of Poor Home Management Practice of Diarrhea and Associated Factors Among Caregivers of Under-Five Years Children in Urban and Rural Residents of Doba Woreda, Ethiopia: Comparative Cross-Sectional Study. Int J Pediatr (2019) 2019:8345245. doi:10.1155/2019/8345245
56. Feleke, DG, Chanie, ES, Admasu, FT, Bahir, S, Amare, AT, and Abate, HK. Two-Week Prevalence of Acute Diarrhea and Associated Factors Among Under Five Years’ Children in Simada Woreda, South Gondar Zone, Northwest Ethiopia, 2021: A Multi-Central Community Based Cross-Sectional Study. Pan Afr Med J (2022) 42:12. doi:10.11604/pamj.2022.42.12.32599
57. Megersa, S, Benti, T, and Sahiledengle, B. Prevalence of Diarrhea and its Associated Factors Among Under-Five Children in Open Defecation Free and Non-Open Defecation Free Households in Goba District Southeast Ethiopia: A Comparative Cross-Sectional Study. Clin Mother Child Health (2019) 16(3):324.
58. Beyene, SG, and Melku, AT. Prevalence of Diarrhea and Associated Factors Among Under Five Years Children in Harena Buluk Woreda Oromia Region, South East Ethiopia, 2018. J Public Health Int (2018) 1(2):9–26. doi:10.14302/issn.2641-4538.jphi-18-2470
59. Kasye, DG, Garoma, NH, and Kassa, MA. Assessment of the Prevalence of Diarrheal Disease Under-Five Children Serbo Town, Jimma Zone South West Ethiopia. Clin Mother Child Health (2018) 15(1). doi:10.4172/2090-7214.1000281
60. Getachew, F, Tamene, M, Gesese, A, Gebremariam, S, and Mezgebe, T. Water Handling, Sanitation, and Hygienic Practices and its Association With Under-Five Childhood Diarrhea Among Households of Kirkos Sub City, Addis Ababa, Ethiopia. J Nurs Health C (2022) 7(2):01–7.
61. Mengistu, KD. Prevalence of Diarrhea and Associated Risk Factors Among Under Five Children Visiting Hamusit Health Center, Dera District, South Gondar Zone, Northwest Ethiopia. Master’s thesis. Bahir Dar, Ethiopia: Bahir Dar University (2021).
62. Damene, DA, Melkamu, BS, and Yimer, HD. Prevalence of Acute Diarrhea and Associated Precipitating Factors Among Under-Five Children in West Guji Zone, Oromia Region, Ethiopia, 2018: Community Based Cross Sectional Study. J Infect Dis Immun (2020) 12(1):1–12. doi:10.5897/jidi2019.0186
63. Brhanemeskel, H. Assessment of Undernutrition and the Prevalence of Infections, Allergy and Diarrhea Among Bottle-Feed Infants and its Comparison With Non-Bottle Fed Infants Aged 6-23 Months in Bole Sub-City Health Centers, Addis Ababa, Ethiopia: A Case Control Study. Bahir Dar, Ethiopia. Master’s thesis. Bahir Dar, Ethiopia: Bahir Dar University (2021).
64. Solomon, ET, Robele, S, Kloos, H, and Mengistie, B. Effect of Household Water Treatment With Chlorine on Diarrhea Among Children Under the Age of Five Years in Rural Areas of Dire Dawa, Eastern Ethiopia: A Cluster Randomized Controlled Trial. Infect Dis Poverty (2020) 9(1):64. doi:10.1186/s40249-020-00680-9
65. Uganda Demographic and Health Survey. Uganda Bureau of Statistics Kampala. Uganda Demographic and Health Survey 2016 Key Indicators Report Uganda (2016). Available from: https://dhsprogram.com/pubs/pdf/FR333/FR333.pdf (Accessed July 28, 2022).
66. Demissie, GD, Yeshaw, Y, Aleminew, W, and Akalu, Y. Diarrhea and Associated Factors Among Under Five Children in Sub-Saharan Africa: Evidence From Demographic and Health Surveys of 34 Sub-Saharan Countries. PLOS ONE (2021) 16(9):e0257522. doi:10.1371/journal.pone.0257522
67. Tareke, AA, Enyew, EB, and Takele, BA. Pooled Prevalence and Associated Factors of Diarrhea Among Under-Five Years Children in East Africa: A Multilevel Logistic Regression Analysis. PLOS ONE (2022) 17(4):e0264559. doi:10.1371/journal.pone.0264559
68. Khalil, I, Colombara, DV, Forouzanfar, MH, Troeger, C, Daoud, F, Moradi-Lakeh, M, et al. Burden of Diarrhea in the Eastern Mediterranean Region, 1990–2013: Findings From the Global Burden of Disease Study 2013. Am J Trop Med Hyg (2016) 95(6):1319–29. doi:10.4269/ajtmh.16-0339
69. Koyuncu, A, Dufour, MSK, Watadzaushe, C, Dirawo, J, Mushavi, A, Padian, N, et al. Household Flooring Associated With Reduced Infant Diarrhoeal Illness in Zimbabwe in Households With and Without WASH Interventions. Trop Med Int Health (2020) 25(5):635–43. doi:10.1111/tmi.13385
70. Lamberti, LM, Fischer Walker, CL, Noiman, A, Victora, C, and Black, RE. Breastfeeding and the Risk for Diarrhea Morbidity and Mortality. BMC Public Health (2011) 11(Suppl. 3):S15. doi:10.1186/1471-2458-11-S3-S15
71. Victora, CG, Bahl, R, Barros, AJD, França, GVA, Horton, S, Krasevec, J, et al. Breastfeeding in the 21st Century: Epidemiology, Mechanisms, and Lifelong Effect. Lancet (2016) 387(10017):475–90. doi:10.1016/S0140-6736(15)01024-7
72. World Health Organization. Breastfeeding (2022). Available from: https://www.who.int/health-topics/breastfeeding (Accessed August 2, 2022).
73. Nuzhat, S, Shahunja, KM, Shahid, AS, Khan, SH, Islam, SB, Islam, MR, et al. Diarrhoeal Children With Concurrent Severe Wasting and Stunting Compared to Severe Wasting or Severe Stunting. Trop Med Int Health (2020) 25(8):928–35. doi:10.1111/tmi.13446
74. Nel, E. Diarrhoea and Malnutrition. South Afr J Clin Nutr (2010) 23(Suppl. 1):15–8. doi:10.1080/16070658.2010.11734262
75. Desmennu, AT, Oluwasanu, MM, John-Akinola, YO, Opeyemi, O, and Ayo, AS. Maternal Education and Diarrhea Among Children Aged 0-24 Months in Nigeria. Afr J Reprod Health (2017) 21(3):27–36. doi:10.29063/ajrh2017/v21i3.2
76. Solomon, ET, Gari, SR, Kloos, H, and Alemu, BM. Handwashing Effect on Diarrheal Incidence in Children Under 5 Years Old in Rural Eastern Ethiopia: A Cluster Randomized Controlled Trial. Trop Med Health (2021) 49(26):26. doi:10.1186/s41182-021-00315-1
77. Ejemot, RI, Ehiri, JE, Meremikwu, MM, and Critchley, JA. Cochrane Review: Hand Washing for Preventing Diarrhoea. Evid-based Child Health Cochrane Rev J (2009) 4(2):893–939. doi:10.1002/ebch.373
78. Edward, A, Jung, Y, Chhorvann, C, Ghee, AE, and Chege, J. Association of Mother’s Handwashing Practices and Pediatric Diarrhea: Evidence From a Multi-Country Study on Community Oriented Interventions. J Prev Med Hyg (2019) 60(2):E93–E102. doi:10.15167/2421-4248/jpmh2019.60.2.1088
79. Ejemot-Nwadiaro, RI, Ehiri, JE, Arikpo, D, Meremikwu, MM, and Critchley, JA. Hand Washing Promotion for Preventing Diarrhoea. Cochrane Database Syst Rev (2015) 2015(9):CD004265. doi:10.1002/14651858.CD004265.pub3
80. Hirai, M, Roess, A, Huang, C, and Graham, JP. Exploring the Link Between Handwashing Proxy Measures and Child Diarrhea in 25 Countries in Sub-Saharan Africa: A Cross-Sectional Study. J Water Sanit Hyg Dev (2017) 7(2):312–22. doi:10.2166/washdev.2017.126
81. Shah, D, Choudhury, P, Gupta, P, Mathew, JL, Gera, T, Gogia, S, et al. Promoting Appropriate Management of Diarrhea: A Systematic Review of Literature for Advocacy and Action: UNICEF-PHFI Series on Newborn and Child Health, India. Indian Pediatr (2012) 49(8):627–49. doi:10.1007/s13312-012-0134-1
82. Clasen, TF, Alexander, KT, Sinclair, D, Boisson, S, Peletz, R, Chang, HH, et al. Interventions to Improve Water Quality for Preventing Diarrhoea. Cochrane Database Syst Rev (2015) 2015(10):CD004794. doi:10.1002/14651858.CD004794.pub3
83. Clasen, T, Schmidt, WP, Rabie, T, Roberts, I, and Cairncross, S. Interventions to Improve Water Quality for Preventing Diarrhoea: Systematic Review and Meta-Analysis. BMJ (2007) 334(7597):782. doi:10.1136/bmj.39118.489931.BE
84. Agustina, , Dukabain, OM, Singga, S, Wanti, W, Suluh, DG, and Mado, FG. Home Sanitation Facilities and Prevalence of Diarrhea for Children in Oelnasi Village, Kupang Tengah Sub-District. Gac Sanit (2021) 35(Suppl. 2):S393–S395. doi:10.1016/j.gaceta.2021.10.059
85. Patil, SR, Arnold, BF, Salvatore, AL, Briceno, B, Ganguly, S, Colford, JM, et al. The Effect of India’s Total Sanitation Campaign on Defecation Behaviors and Child Health in Rural Madhya Pradesh: A Cluster Randomized Controlled Trial. Plos Med (2014) 11(8):e1001709. doi:10.1371/journal.pmed.1001709
86. Clasen, T, Boisson, S, Routray, P, Torondel, B, Bell, M, Cumming, O, et al. Effectiveness of a Rural Sanitation Programme on Diarrhoea, Soil-Transmitted Helminth Infection, and Child Malnutrition in Odisha, India: A Cluster-Randomised Trial. Lancet Glob Health (2014) 2(11):e645–53. doi:10.1016/S2214-109X(14)70307-9
87. Jung, YT, Hum, RJ, Lou, W, and Cheng, YL. Effects of Neighbourhood and Household Sanitation Conditions on Diarrhea Morbidity: Systematic Review and Meta-Analysis. PLOS ONE (2017) 12(3):e0173808. doi:10.1371/journal.pone.0173808
88. United Nations. Transforming Our World: The 2030 Agenda for Sustainable Development (2022). Available from: https://sdgs.un.org/2030agenda (Accessed September 29, 2022).
89. Arba, A, Aydiko, E, and Baza, D. Prevalence of Diarrheal Disease Among Under-Five Children in Worabe Town, Southern Ethiopia. Am J Life Sci (2020) 8(4):45. doi:10.11648/j.ajls.20200804.11
90. Zegeye, Z. Prevalence of Childhood Diarrhea Disease and Associated Factors Among Under Five Children in Slum Area of Metropolitan City, Bahir Dar, Gondar and Dessie in Amhara Region, Ethiopia. Master’s thesis. Bahir Dar, Ethiopia: Bahir Dar University (2021).
Keywords: diarrhea, Ethiopia, risk factors, under-five children, WASH
Citation: Sahiledengle B, Atlaw D, Mwanri L, Petrucka P, Kumie A, Tekalegn Y, Desta F, Zenbaba D, Mesfin T, Gomora D and Agho KE (2024) Burden of Childhood Diarrhea and Its Associated Factors in Ethiopia: A Review of Observational Studies. Int J Public Health 69:1606399. doi: 10.3389/ijph.2024.1606399
Received: 15 July 2023; Accepted: 20 May 2024;
Published: 05 June 2024.
Edited by:
Jean Tenena Coulibaly, Félix Houphouët-Boigny University, Côte d’IvoireReviewed by:
Gaoussou Coulibaly, Félix Houphouët-Boigny University, Côte d’IvoireOne reviewer who chose to remain anonymous
Copyright © 2024 Sahiledengle, Atlaw, Mwanri, Petrucka, Kumie, Tekalegn, Desta, Zenbaba, Mesfin, Gomora and Agho. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Biniyam Sahiledengle, YmluaXlhbS5zYWhpbGVkZW5nbGVAZ21haWwuY29t
 Biniyam Sahiledengle
Biniyam Sahiledengle Daniel Atlaw
Daniel Atlaw Lillian Mwanri3
Lillian Mwanri3