- 1National Center for Chronic and Non-Communicable Diseases Control and Prevention, Chinese Center for Disease Control and Prevention, Beijing, China
- 2Department of Epidemiology and Biostatistics, School of Public Health, Anhui Medical University, Hefei, China
- 3School of Medicine and Dentistry, Griffith Health, Griffith University, Birtinya, QLD, Australia
- 4Affiliated Hospital of Chengde Medical University, Chengde, China
- 5School of Public Health and Social Work, Faculty of Health, Queensland University of Technology, Brisbane, QLD, Australia
Objectives: To identify the long-term spatiotemporal trend of ozone-related chronic obstructive pulmonary disease (COPD) burden by sex and country and to explore potential drivers.
Methods: We retrieved data of ozone-related COPD death and disability adjusted life year (DALY) from the Global Burden of Disease 2019. We used a linear regression of natural logarithms of age-standardized rates (ASRs) with calendar year to examine the trends in ASRs and a panel regression to identify country-level factors associated with the trends.
Results: Global ozone-attributable COPD deaths increased from 117,114 to 208,342 among men and from 90,265 to 156,880 among women between 1990 and 2019. Although ASRs of ozone-related COPD death and DALY declined globally, they increased in low and low-middle Socio-demographic Index (SDI) regions, with faster rise in women. Elevated average maximum temperature was associated with higher ozone-attributable COPD burden, while more green space was associated with lower burden.
Conclusion: More efforts are needed in low and low-middle SDI regions, particularly for women, to diminish inter-country inequality in ozone-attributable COPD. Global warming may exacerbate the burden. Expanding green space may mitigate the burden.
Introduction
Chronic obstructive pulmonary disease (COPD) led to over three million deaths and 74 million disability-adjusted life years (DALYs) lost in 2019 worldwide, which was the third and fourth most common cause of death or disability, respectively [1]. Population growth and population ageing may further exacerbate the heavy burden of COPD.
Although smoking, occupational exposures and indoor air pollution are identified as major contributors to COPD, ambient air pollution, particularly ozone [2–4], has been increasingly reported to play an important role in the progression of COPD [2, 5–10]. Ozone is a type of gaseous pollutant formed by atmospheric chemical reactions of nitrogen oxides and volatile organic compound precursor under the conditions of high temperature and strong solar radiation. It is therefore the air pollutant that is most sensitive to meteorological factors [11]. Urbanization, industrialization, and together with global warming in the coming decades may aggravate the health impacts of ozone pollution [12]. Despite global efforts to control emissions of ozone precursors, the concentration of ozone remains high, particularly in East Asia where its concentration presents a significant upward trend [13, 14]. In some countries such as China, the concentration of ambient particulate matter has dropped with the stringent control measures, but the ambient ozone pollution remains serious [15–17]. Moreover, unlike particulate matter, which can reduce atmospheric visibility, ozone pollution is more difficult to detect and protect against.
As a strong oxidant, ozone exposure leads to COPD progression through lung inflammation and alveolar epithelial damage [18–20]. A meta-analysis on the relationship between air pollution and COPD showed that pooled relative risk associated with ozone was higher than other air pollutants, and the estimations on ozone-COPD relationship had the highest level of heterogeneity [21]. Disparities in climate, environment, demographic characteristics, and socioeconomic level in different studies may partly explain the heterogeneity of the results. Revealing the spatial and temporal variations of ozone-associated COPD at the national level, and identifying nation-specific factors that modify the effect of ozone exposure will help understand the drivers behind the variations and facilitate interventions for COPD.
However, the existing studies on ozone-related COPD burden have been either carried out in a certain country or region [22, 23], have failed to compare the sex disparity in different countries and regions [24], or have not examined the modification effect of various country-specific characteristics [24–26]. The global burden of disease study (GBD) 2019 uses a unified method to estimate ozone-related COPD burden by sex at the levels of country and region, which allows us to compare the trend in the burden by sex across countries and regions, and to evaluate influencing factors at the level of country by further incorporating socioenvironmental factors [1, 27].
This study aimed to use data from the GBD 2019 to investigate the spatiotemporal trends in COPD mortality and DALY associated with ozone by sex at the regional and national levels. We also aimed to assess whether country-level environment, demographic characteristics, and socioeconomic variables have modified the observed trends.
Methods
Data of Ozone-Related COPD Burden
We collected the annual numbers, age-standardized rates (ASRs), and the proportions (accounting for the total burden from COPD) of death and DALY of ozone-attributable COPD by country, region, and sex for the period 1990–2019 from the GBD study results [28]. The GBD 2019 covered 21 regions and 204 countries. Countries were categorized into five groups (high, low, middle, high-middle, and low-middle) according to the Socio-demographic Index (SDI). The SDI was a synthetic metrics that reflected the degree of development associated with health conditions. A higher value in SDI meant a higher level of development [1].
The full details of the GBD methodology had been reported elsewhere [1, 24, 26]. In terms of mortality, data used for estimation included vital registration and surveillance from the cause of death database. COPD deaths were coded as J41-J44, J47 by the International Classification of Diseases, 10th version (ICD-10) and 491–492, 496 by the ICD-9. The standard Cause of Death Ensemble model approach was applied to develop mixed effects or spatiotemporal regression models for COPD mortality estimation [5, 24].
In terms of non-fatal health loss, the estimation was based on the data from representative surveys, prevalence studies, and medical claims. COPD was defined by expiratory volume in one second/forced vital capacity (FEV1/FVC) <70% (post-bronchodilator) as per the recommendation of the 2022 Global Initiative for Chronic Obstructive Lung Disease (GOLD) [10]. Data using alternative case-definitions of COPD prevalence (i.e., FEV1/FVC<0.7 pre-bronchodilator) were crosswalked to this definition. The severity of COPD was classified as mild, moderate, and severe according to the GOLD criteria. A DisMod-MR 2.1 model was employed to estimate COPD prevalence and the proportions of three GOLD severity groups. These proportions were mapped into the three COPD health states for which disability weights (DWs) were available using the Medical Expenditure Panel Survey data from the United States. The prevalence of each COPD health state was multiplied by its DW and was then adjusted for comorbidity to obtain the years lived with disability (YLD) [5, 25].
Years of life lost (YLLs) were calculated by multiplying the number of deaths at a given age by the standard life expectancy at the corresponding age. DALYs were the sum of YLDs and YLLs [5, 25].
A comparative risk assessment method was used by the GBD 2019 to quantify the burden of disease related to ozone pollution. Population-attributable fraction (PAF) was calculated through exposure data of ambient ozone, relative risk for COPD, and a theoretical minimum risk exposure level (TMREL) for ozone. A chemical transport model based on satellite data was used to estimate ozone exposure. Relative risk was pooled from meta-analysis of cohort studies. The TMREL for ozone was set to a uniform distribution between the lowest and fifth percentile measured by the Cancer Prevention Study-II of American Cancer Society [5, 25]. Ethical approval was not required because we used pre-existing and de-identified data in this study and we did not have any contact with the subjects.
Data of Potential Country-Level Modifiers
The following country- and year-specific factors that might modify ozone-related COPD were included in the present study according to previous studies [29–33]. Age-standardized prevalence of smoking tobacco use by sex was derived from the GBD 2019 [34]. Demographic and socioeconomic factors including average years of schooling (average number of years people aged 25 years or older participated in formal education), population density, proportion of population aged 65 years or older, proportion of urban population, and gross domestic product (GDP) per capita were collected from the Our World in Data [35]. Data in this platform have been widely used in previous studies [36, 37]. We also included environmental factors including average temperature, average maximum temperature, average minimum temperature, rainfall, and Normalized Derived Vegetation Index (NDVI) (the values ranged from 0 to 1 with greater value presenting a higher vegetation coverage). Daily temperature and rainfall were collected from the National Oceanic and Atmospheric Administration of the United States [38]. In consistent with other epidemiological studies [39], we calculated average annual temperature, average annual maximum temperature, and average annual minimum temperature during summer months for each country (June to August for northern hemisphere and December to February for southern hemisphere). We collected NDVI from the National Aeronautics and Space Administration [40] and calculated the annual average.
Statistical Analysis
We conducted three-step analyses. Step 1: we presented the numbers, ASRs, and proportions of COPD death and DALY attributable to ozone by sex, country, and region with 95% uncertainty intervals (UI). We used maps to show their spatial distributions. Step 2: we fitted the natural logarithm of ASR of ozone-related COPD death and DALY to the calendar year by linear regression with the equation
where
We performed all analyses with R (version 4.1.0, package of plm). A p-value < 0.05 was viewed as statistically significant.
Results
COPD Deaths and DALYs Associated With Ozone by Region
Percentage of COPD Deaths and DALYs Associated With Ozone
Ozone pollution contributed to 11.07% and 11.20% of all deaths from COPD among men and women worldwide in 2019, respectively. Across regions with different SDIs, the proportion attributable to ozone pollution increased among both men and women from 1990 to 2019, with the exception of high-SDI region. Among 21 GBD regions, the decrease in the proportion only occurred in seven regions [Central Asia, Eastern Europe, Central Europe, Oceania, High-income North America, Caribbean, and Central Latin America (Figure 1)].
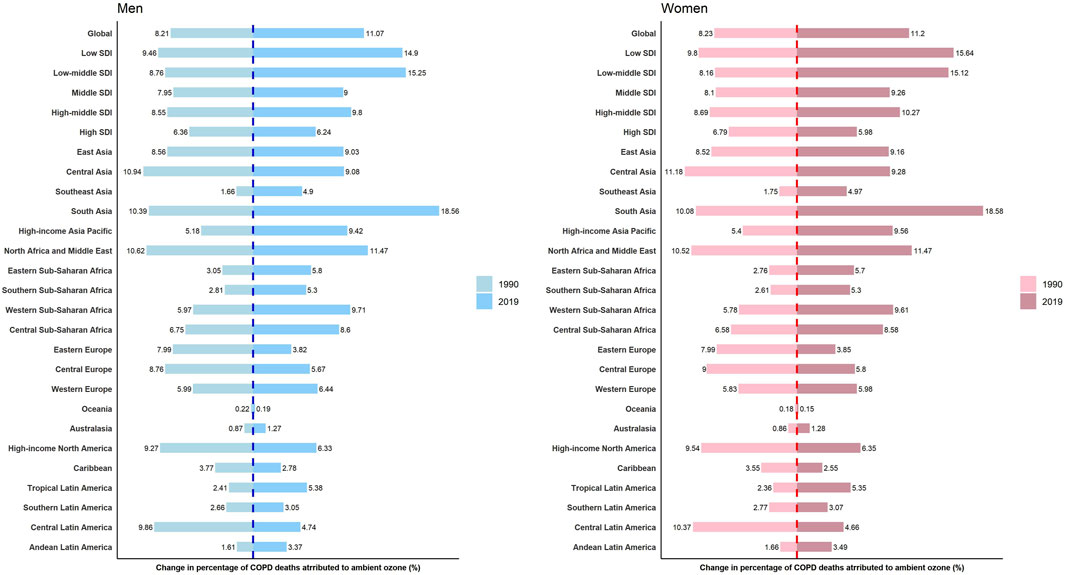
Figure 1. The proportions of chronic obstructive pulmonary disease deaths attributable to ozone among total chronic obstructive pulmonary disease deaths by sex and region (Global, 1990 and 2019).
Contribution of ozone pollution to DALYs from COPD was on the rise globally in both men and women during the study period. In addition to the GBD regions where the percentage of ozone-related COPD deaths decreased, a decline in the percentage of ozone-related COPD DALYs occurred in East Asia, North Africa and Middle East, and Western Europe as well (Supplementary Figure S1).
Number and ASR of COPD Death Associated With Ozone
The global number of ozone-related COPD deaths increased from 117,114 (95% UI, 51,903 to 187,913) to 208,342 (95% UI, 96,725 to 327,371) among men during the study period. The age-standardized mortality rate (ASMR) of ozone-attributable COPD among men decreased globally, from 8.05 (95% UI, 3.58–12.86) to 6.20 (95% UI, 2.88–9.68) per 100,000 person-years, with an APC of −1.07% (95% CI, −1.34% to −0.80%). However, the ASMR increased in the regions with low [APC 0.74% (95% CI, 0.55, 0.94)] and low-middle SDI [APC 0.61% (95% CI, 0.45, 0.77)]. Among 21 GBD regions, the ASMR among men increased in six regions (Table 1A).
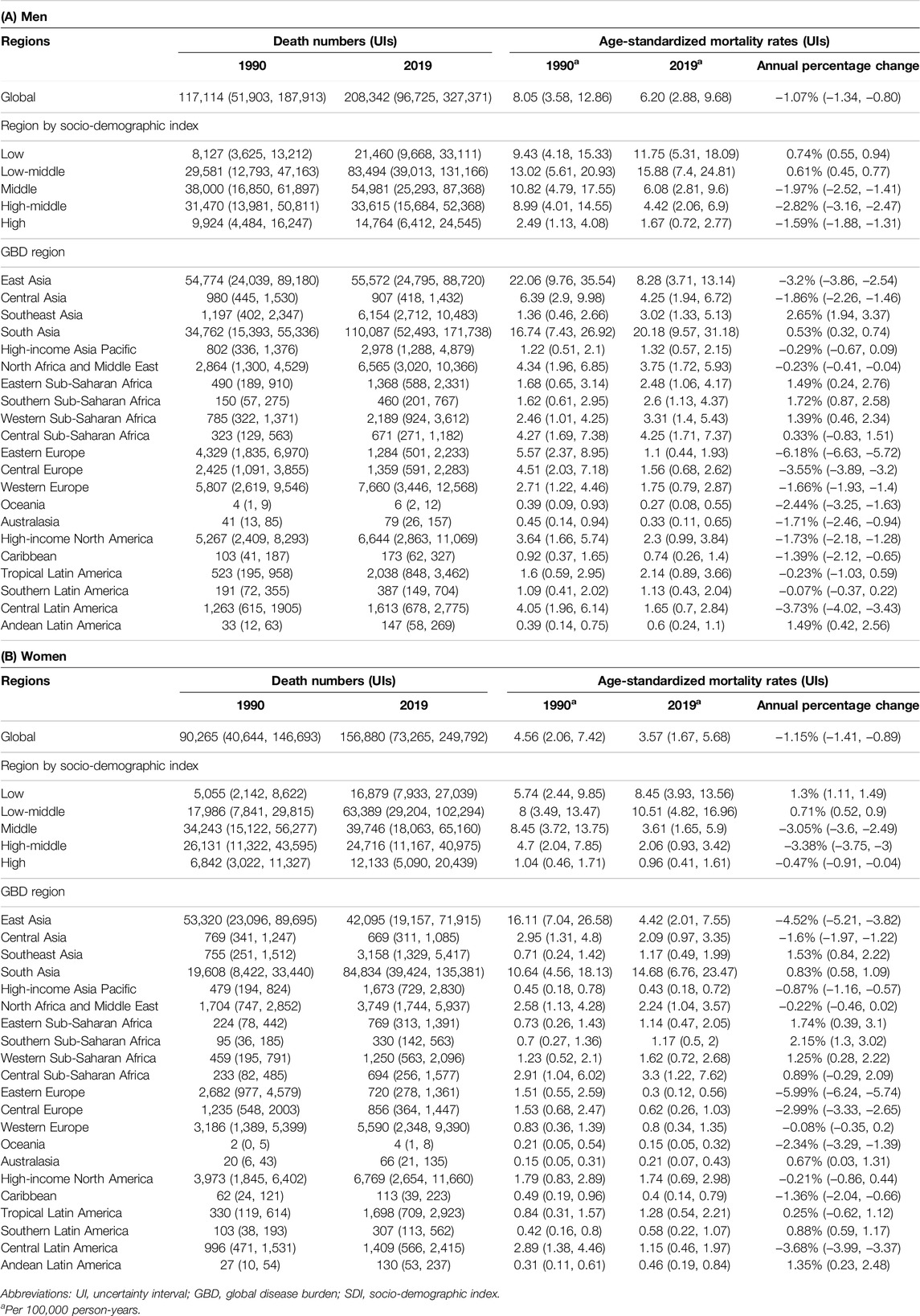
Table 1. Death numbers and age-standardized mortality rates of chronic obstructive pulmonary disease attributable to ozone by sex and region (Global, 1990 and 2019).
The number of ozone-related COPD deaths in women was constantly lower than that in men across regions with different SDIs. The death number among women increased from 90,265 (95% UI, 40,644 to 146,693) to 156,880 (95% UI, 73,265 to 249,792) globally from 1990 to 2019. The ASMR of ozone-attributable COPD in women also decreased globally, from 4.56 (95% UI, 2.06–7.42) to 3.57 (95% UI, 1.67–5.68) per 100,000 person-years, with an APC of −1.15% (95% CI, −1.41% to −0.89%). Women in the regions with low [APC 1.30% (95% CI, 1.11, 1.49)] and low-middle SDI [APC 0.71% (95% CI, 0.52, 0.90)] also experienced an increased ASMR, with the APC higher than men in corresponding regions. Among 21 GBD regions, the ASMR among women increased in eight regions [Table 1B].
Number and ASR of COPD DALY Associated With Ozone
Global numbers of ozone-attributable COPD DALYs increased among both men and women from 1990 to 2019, whereas the age-standardized DALY rates (ASDRs) decreased significantly among both sexes. Nevertheless, the ASDR still increased in the regions with low and low-middle SDI. Among 21 GBD regions, the increments in ASDR in men and women were observed in four and five regions, respectively (Supplementary Table S1).
COPD Deaths and DALYs Associated With Ozone by Country
Percentage of COPD Deaths and DALYs Associated With Ozone
The percentages of ozone-attributable COPD deaths increased in both men and women in 118 countries of 204 countries (57.8%, n = 118/204). The highest increase occurred in Bangladesh, Maldives, and India (Figure 2; Supplementary Table S2). The percentages of ozone-attributable COPD DALYs in men and women increased in 109 (53.4%, n = 109/204) and 107 countries (52.5%, n = 107/204) out of 204 countries, respectively. The highest increase occurred in India, Bangladesh, and Nepal among men, and in India, Maldives, and Bangladesh among women (Supplementary Figure S2; Supplementary Table S3).
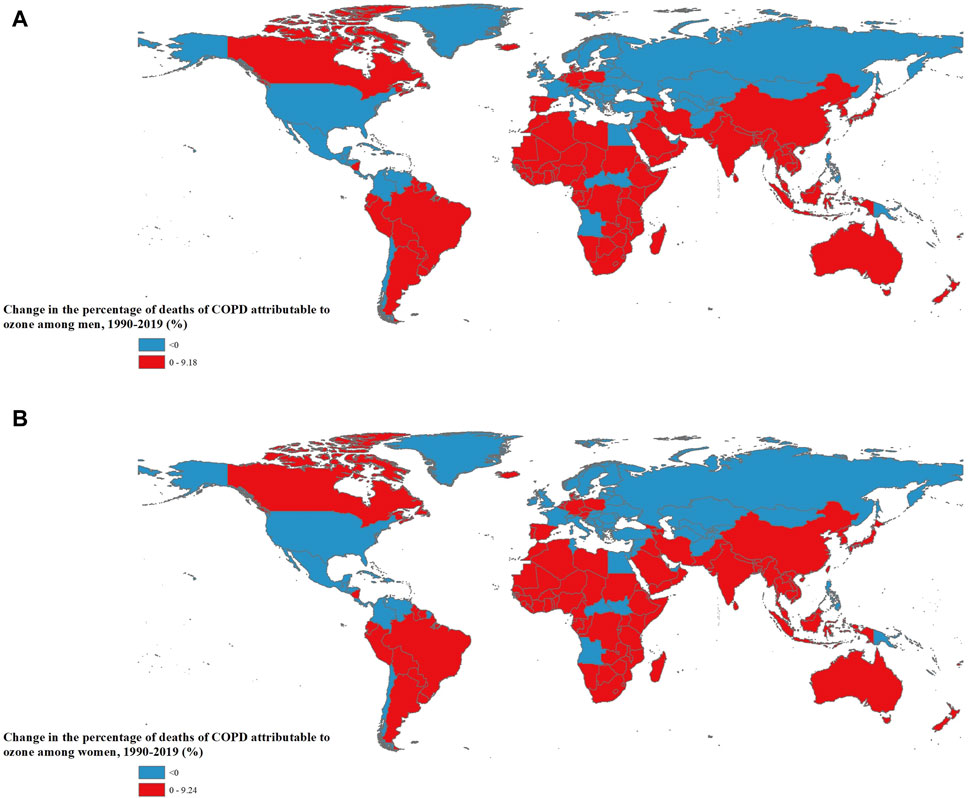
Figure 2. The change in the proportions of chronic obstructive pulmonary disease deaths attributable to ozone among total chronic obstructive pulmonary disease deaths by sex and country [(A): Men; (B): Women] (Global, 1990 to 2019).
Number and ASR of COPD Death Associated With Ozone
Among 204 countries and territories, Nepal, India, and Pakistan had the highest ASMR of ozone-attributable COPD in men in 2019, and Nepal, India, and Bhutan had the highest value in women (Figure 3; Supplementary Table S2). The number of COPD-related deaths in men was the highest in India, China, and Pakistan in 2019, while the number in women was the highest in India, China, and United States (Supplementary Table S2).
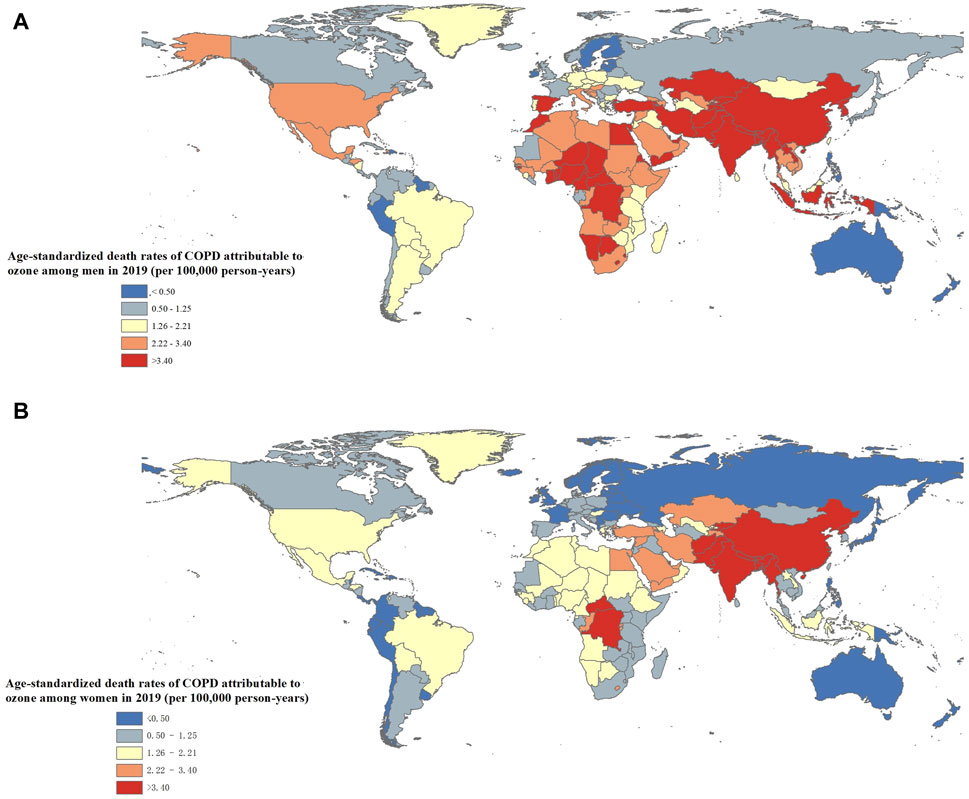
Figure 3. The age-standardized death rates of chronic obstructive pulmonary disease attributable to ozone by sex and country [(A): Men; (B): Women] (Global, 2019).
Among 204 countries, the ASMR of ozone-attributable COPD in men significantly increased in 59 countries out of 204 countries (28.9%, n = 59/204), with Madagascar, Mozambique, and Kenya having the highest annual growth. The ASMR in women significantly increased in 71 countries (34.8%, n = 71/204), with Madagascar, Seychelles, and Kenya having the highest annual growth (Figure 4; Supplementary Table S2).
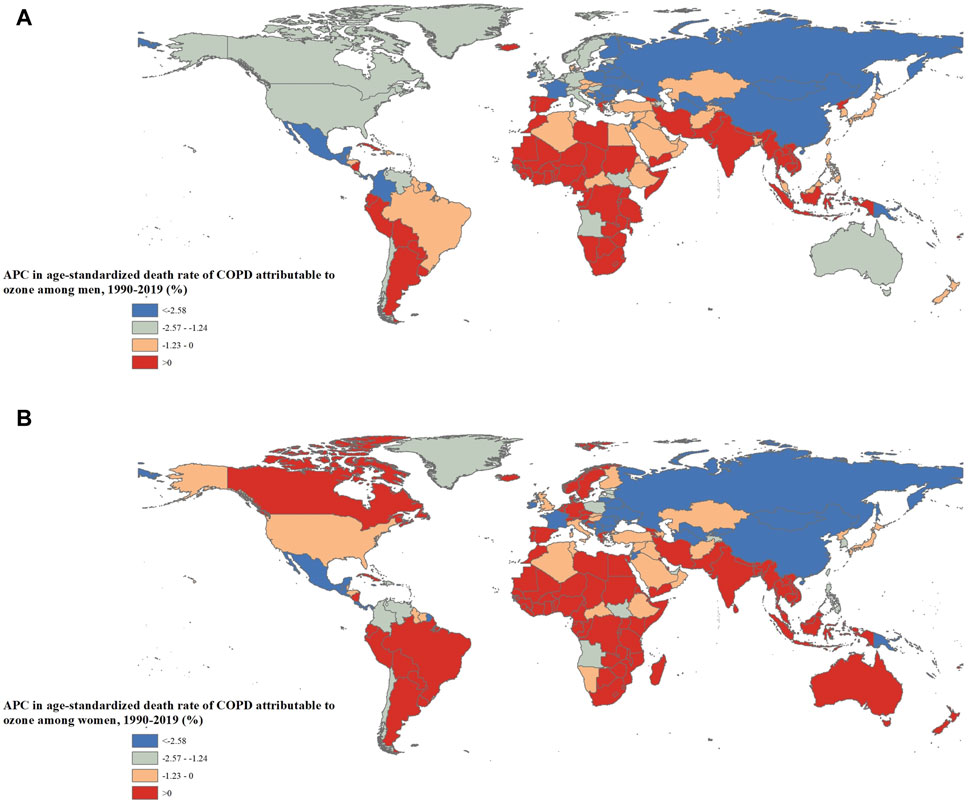
Figure 4. Annual percentage change in the age-standardized death rates of chronic obstructive pulmonary disease attributable to ozone by sex and country [(A): Men; (B): Women] (Global, 1990 to 2019).
Number and ASR of COPD DALY Associated With Ozone
The DALY numbers and ASDRs of ozone-attributable COPD by sex and country are shown in Supplementary Table S3. The distribution (Supplementary Figure S3) and trend of (Supplementary Figure S4) ozone-attributable COPD DALY were similar to the death.
Country-Level Factors Associated With Ozone-Related COPD
The patterns of the significant associations between country-level factors and ozone-attributable COPD burden were similar in terms of death and DALY in both men and women (Table 2; Supplementary Table S4). Smoking prevalence was positively associated with the rate of the burden. With regards to demographic factors, average years of schooling was negatively associated with the burden. A higher population density and a higher percentage of population aged ≥65 years old were associated with a higher ozone-related COPD burden. In terms of socioeconomic factors, countries with a higher percentage of urban population were more likely to have a lighter ozone-attributable COPD burden. Among meteorological factors, average maximum and minimum temperature and rainfall were positively associated with ozone-related COPD burden. In contrast, NVDI was associated with significantly decreased ozone-attributable COPD deaths and DALYs in both men and women.
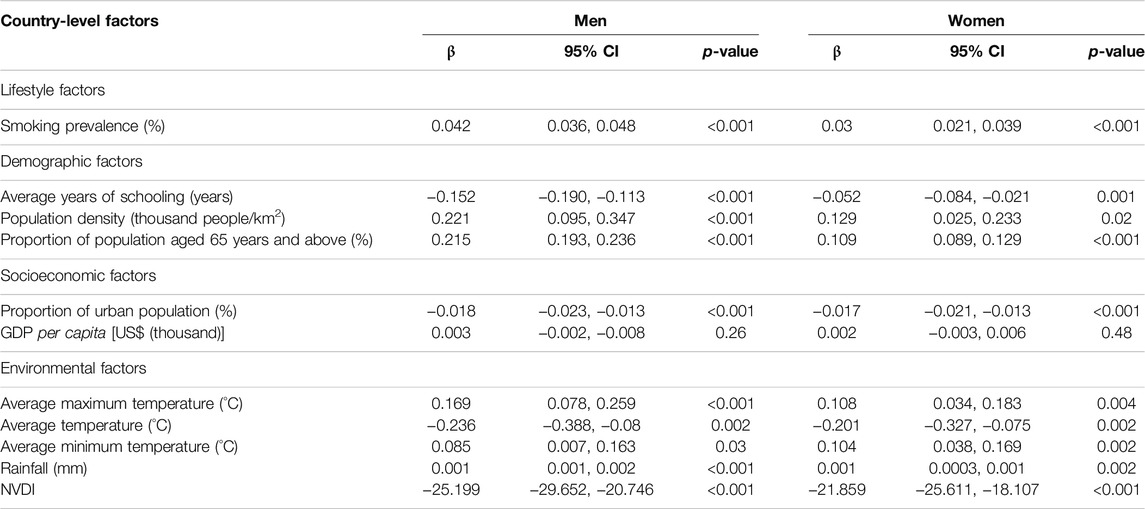
Table 2. Association between country-level factors and mortality rate of chronic obstructive pulmonary disease attributable to ozone pollution (Global, 1990 to 2019).
Discussion
Ozone is a worldwide threat to COPD, but there is limited evidence detailing how ozone-related COPD burden changed spatially and temporally by sex at the national level and what the underlying drivers were. In this study, we reported that the trends in the ASRs of ozone-attributable COPD death and DALY showed a great spatial variation, with low and low-middle SDI regions having a significant increasing trend. It’s worth noting that such increasing trend was more marked among women than men. More importantly, we found that such variation could be related to a variety of country-level environmental and socioeconomic characteristics, suggesting that tailored strategies taking into account these characteristics are crucial for ozone-attributable COPD prevention and control.
The GBD study 2015 reported that 254,000 deaths from COPD were associated with exposure to ozone worldwide in 2015, representing 8.0% of total COPD deaths [45]. Our study found that more than 364,000 COPD deaths (over 208,000 for men and 156,000 for women) were associated with exposure to ozone in 2019, accounting for around 11.0% of total COPD deaths. This raise may be due to the increases in both levels of ozone and COPD mortality and the updated estimation method. Although some studies have initially described ozone-related COPD burden based on the GBD 2019 [24–26], our study further detailed the spatial and temporal trends in the number, percentage, and ASR of ozone-related COPD death and DALY by sex in each country, and for the first time assessed the modifying effects of a variety of country-level environmental and socioeconomic factors on such trends [24].
Our study found that although the ASRs of ozone-attributable COPD death and DALY declined worldwide, the ASRs in regions of low SDI and low-middle SDI were still on the rise. Nepal, India, Pakistan, and Bhutan in particular showed the highest ASMR attributable to ozone pollution. With rapid economic development, these regions are experiencing the most severe ambient air pollution in the world [46]. Relatively low socioeconomic level may be another reason for the higher ASMR in these regions because poverty has been reported to be associated with airflow obstruction [47, 48]. Moreover, the relatively poor treatment and health service may further aggravate the mortality burden from COPD in less developed countries as health resources have been mainly allocated to infectious diseases rather than non-communicable diseases such as COPD. In this study, we also found that country-level socioeconomic indicator, i.e., proportion of urban population, was negatively associated with the mortality rate of COPD through panel analysis, which is able to reflect, to some extent, the negative relationship between socioeconomic level and COPD mortality. These findings revealed a huge inequity in the ozone-attributable COPD burden among countries with different SDI levels. Due to limited resources, countries with low and low-middle SDI were facing the dilemma of economic development and air pollution control. More international efforts are needed to decrease ozone pollution exposure and related health disparities.
We found that the absolute numbers and ASRs of COPD burden were higher among men than women, which is consistent with previous studies [5]. However, it is worth noting that the increase in ASMR among women (34.8% of all countries) was observed in more countries compared to men (28.9% of all countries) from 1990 to 2019. The ASMR in low and low-middle SDI regions increased more rapidly among women than men (higher absolute values of APC in women than men), and the ASMR in high SDI region decreased more slowly among women than men (lower absolute value of APC in women than men). This may indicate that women are more susceptible to the process of air quality deterioration. Physiological differences in hormone, lung volume, deposition, and reactivity may partly explain the disparity in susceptibility between men and women [49, 50]. Another possible examination is the disparity in the trend of smoking prevalence between men and women. It has been reported that smoking among men decreased more dramatically than that among women in high-income countries from 2007 to 2019 [51]. Smoking and ozone exposure may have joint effect on COPD mortality. Our finding suggests that more attention should be paid to women in preventing the influence of ozone on respiratory system. More refined data collection and analysis is needed to discern the reasons for the disparity in response to ozone between men and women.
We further evaluated potential modifiers on ozone-related COPD death and DALY at the national level using panel analyses. Countries with a higher smoking prevalence were found to have higher rates of COPD mortality and DALY, suggesting that smoking may have synergistic effect with air pollution [52]. With the implementation of multiple tobacco control initiatives such as the World Health Organization Framework Convention on Tobacco Control (WHO FCTC) and the MPOWER measures, smoking prevalence had decreased worldwide during the last three decades, but the absolute number of smokers continued to increase [51, 53]. Moreover, a wide implementation gap for tobacco control policies still existed among countries and only two countries (Brazil and Turkey) have fully applied all MPOWER measures [46, 53]. Strong and extensive implementation of evidence-based interventions is needed to speed up reduction in health influence of smoking.
Our results show population density and percentage of population aged ≥65 years old were positively related with ozone-attributable COPD mortality and DALY rates, which indicates that COPD burden will continue to elevate with global population growth and population ageing. Average years of schooling and proportion of urban population that reflect the socioeconomic levels were found to be negatively associated with the rates of ozone-attributable COPD mortality and DALY. The possible explanation is that countries with higher socioeconomic levels tend to implement better early warning and protective measures against air pollution and be able to afford better healthcare services [32].
Our study found that countries with higher average maximum and minimum temperatures were likely to have higher ozone-attributable COPD mortality and DALY rates. Previous studies also discovered that temperature synergistically modified the ozone-mortality [54]. Our study provides the evidence of this synergistic effect through analysis across multiple countries worldwide. The ozone-attributable COPD burden is predicted to surge further as climate change becomes more fiercer and heat waves become more frequent. The coordinated efforts in early warning and protection against climate change and ozone pollution are needed to reduce the synergistic effect.
It is noticeable that our study found increased greenness could attenuate the susceptibility of COPD death and DALY related to ozone pollution. Most previous studies on green space and respiratory diseases focused on its direct protective effect [55–58]. Only two studies revealed a favorable modification effect of greenness on the association between ozone pollution and respiratory diseases [59, 60]. The underlying reasons for the modification effect may include the differences in health behaviors and stress reduction in regions of different greenness. For example, people live in a greener space may be more likely to take protection measures against ozone pollution and lead a healthier lifestyle (i.e., less likely to smoke), and may be more likely to be able to recover from psychological stress [61, 62]. This finding suggests the importance of enlarging green space in improving resiliency from the health influence of ozone pollution. It also indicates that future studies on the health effect of air pollution should take the modification effect of greenness into account.
Our study has several novel findings with public health significance. First, the marked disparity in the trend of ASR of ozone-attributable COPD death and DALY across regions with different SDI underscores the urgency to allocate more resources in regions with low or low-middle SDI to mitigate health inequality. Second, the discrepancy in the trend of ASR of ozone-attributable COPD death and DALY between men and women indicates that women may be more vulnerable to the deterioration of air quality and should receive more attention. Third, our panel analyses identified that smoking and high temperature may aggravate ozone-related COPD burden, whereas greenspace may alleviate the burden, providing an essential basis for identifying susceptible countries and formulating policy to mitigate the health effect of ozone pollution.
Our study has several limitations. First, in addition to COPD, other respiratory diseases such as asthma may also be associated with ozone pollution. Further studies are needed to assess the asthma burden attributable to ozone. Second, some potential modifiers (e.g., solar radiation, occupational exposures and indoor air pollution), were not included in panel analysis because of the lack of long-term continuous data at the national level. Third, as an ecological study, our estimates at the country-level could not fully rule out the potential for bias. Further studies about the modification of socioenvironmental factors on ozone-attributable COPD at the individual level are warranted. Fourth, there are a few ineluctable limitations in the GBD study. For instance, some countries lack relevant data or have data with low quality. To compensate for this, the GBD study used data processing and modelling methods to constantly improve the estimation [1].
Conclusion
The ASR of ozone-attributable COPD death was increasing in regions with low or low-middle SDI, urging that more resources need to be invested in these regions to diminish ozone-related health inequalities between countries. Such increase was faster in women than man, which indicates women need more attention to reduce the respiratory effect of ozone. Increasing ambient temperature was associated with a higher burden of ozone-related COPD, and more green space may help alleviate the burden. These findings provide crucial basis for reducing the ozone-related COPD burden through urban design and coordinated control of ozone pollution and climate change.
Data Availability Statement
The data that support the findings of this study are openly available at the following URL/DOI: https://vizhub.healthdata.org/gbd-results/.
Author Contributions
NW: Conceptualization, data curation, formal analysis, funding acquisition, methodology, visualization, writing–original draft. JC: Data curation, writing–review and editing. ZX: Writing–review and editing. SW: Writing–review and editing. QW: Data curation. XF: Project administration. WH: Conceptualization, writing–review and editing. BW: Supervision, writing–review and editing. All authors contributed to the article and approved the submitted version.
Funding
The authors declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Youth Science Foundation of Chinese Center for Diseases Control and Prevention (grant number: 2022A201). The funders had no role in the study design, data collection, and analysis, decision to publish or preparation of the manuscript.
Conflict of Interest
The authors declare that they do not have any conflicts of interest.
Acknowledgments
We highly appreciate the work by the GBD 2019 collaborators.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/ijph.2024.1606062/full#supplementary-material
References
1. GBD Diseases Injuries Collaborators. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet (2020) 396(10258):1204–22. doi:10.1016/S0140-6736(20)30925-9
2. Hansel, NN, McCormack, MC, and Kim, V. The Effects of Air Pollution and Temperature on COPD. COPD (2016) 13(3):372–9. doi:10.3109/15412555.2015.1089846
3. Huangfu, P, and Atkinson, R. Long-term Exposure to NO2 and O3 and All-Cause and Respiratory Mortality: A Systematic Review and Meta-Analysis. Environ Int (2020) 144:105998. doi:10.1016/j.envint.2020.105998
4. Gao, H, Wang, K, W, WA, Zhao, W, and Xia, ZL. A Systematic Review and Meta-Analysis of Short-Term Ambient Ozone Exposure and COPD Hospitalizations. Int J Environ Res Public Health (2020) 17(6):2130. doi:10.3390/ijerph17062130
5. GBD Chronic Respiratory Disease Collaborators. Prevalence and Attributable Health burden of Chronic Respiratory Diseases, 1990-2017: A Systematic Analysis for the Global Burden of Disease Study 2017. Lancet Respir Med (2020) 8(6):585–96. doi:10.1016/S2213-2600(20)30105-3
6. Li, X, Cao, X, Guo, M, Xie, M, and Liu, X. Trends and Risk Factors of Mortality and Disability Adjusted Life Years for Chronic Respiratory Diseases From 1990 to 2017: Systematic Analysis for the Global Burden of Disease Study 2017. BMJ (Clinical research ed) (2020) 368:m234. doi:10.1136/bmj.m234
7. Liu, S, Lim, YH, Pedersen, M, Jorgensen, JT, Amini, H, Cole-Hunter, T, et al. Long-Term Air Pollution and Road Traffic Noise Exposure and COPD: The Danish Nurse Cohort. Eur Respir J (2021) 58(6):2004594. doi:10.1183/13993003.04594-2020
8. Shin, S, Bai, L, Burnett, RT, Kwong, JC, Hystad, P, van Donkelaar, A, et al. Air Pollution as a Risk Factor for Incident Chronic Obstructive Pulmonary Disease and Asthma. A 15-Year Population-Based Cohort Study. Am J Respir Crit Care Med (2021) 203(9):1138–48. doi:10.1164/rccm.201909-1744OC
9. Wang, C, Xu, J, Yang, L, Xu, Y, Zhang, X, Bai, C, et al. Prevalence and Risk Factors of Chronic Obstructive Pulmonary Disease in China (The China Pulmonary Health [CPH] Study): A National Cross-Sectional Study. Lancet (2018) 391(10131):1706–17. doi:10.1016/S0140-6736(18)30841-9
10. Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis Management, and Prevention of Chronic Obstructive Pulmonary Disease (2022). Available at: https://goldcopd.org/wp-content/uploads/2021/12/GOLD-REPORT-2022-v1.1-22Nov2021_WMV.pdf (Accessed May 16, 2022).
11. Atkinson, RW, Butland, BK, Dimitroulopoulou, C, Heal, MR, Stedman, JR, Carslaw, N, et al. Long-term Exposure to Ambient Ozone and Mortality: A Quantitative Systematic Review and Meta-Analysis of Evidence From Cohort Studies. BMJ Open (2016) 6(2):e009493. doi:10.1136/bmjopen-2015-009493
12. Romanello, M, McGushin, A, Di Napoli, C, Drummond, P, Hughes, N, Jamart, L, et al. The 2021 Report of the Lancet Countdown on Health and Climate Change: Code Red for a Healthy Future. Lancet (2021) 398(10311):1619–62. doi:10.1016/S0140-6736(21)01787-6
13. Bakola, M, Hernandez Carballo, I, Jelastopulu, E, and Stuckler, D. The Impact of COVID-19 Lockdown on Air Pollution in Europe and North America: A Systematic Review. Eur J Public Health (2022) 32(6):962–8. doi:10.1093/eurpub/ckac118
14. Wang, T, Xue, L, Brimblecombe, P, Lam, YF, Li, L, and Zhang, L. Ozone Pollution in China: A Review of Concentrations, Meteorological Influences, Chemical Precursors, and Effects. Sci total Environ (2017) 575:1582–96. doi:10.1016/j.scitotenv.2016.10.081
15. Huang, J, Pan, X, Guo, X, and Li, G. Health Impact of China's Air Pollution Prevention and Control Action Plan: An Analysis of National Air Quality Monitoring and Mortality Data. Lancet Planet Health (2018) 2(7):e313–e23. doi:10.1016/S2542-5196(18)30141-4
16. Yin, P, Brauer, M, Cohen, AJ, Wang, H, Li, J, Burnett, RT, et al. The Effect of Air Pollution on Deaths, Disease Burden, and Life Expectancy across China and its Provinces, 1990-2017: An Analysis for the Global Burden of Disease Study 2017. Lancet Planet Health (2020) 4(9):e386–e98. doi:10.1016/S2542-5196(20)30161-3
17. Cai, W, Zhang, C, Suen, HP, Ai, S, Bai, Y, Bao, J, et al. The 2020 China Report of the Lancet Countdown on Health and Climate Change. Lancet Public Health (2021) 6(1):e64–e81. doi:10.1016/S2468-2667(20)30256-5
18. Corradi, M, Alinovi, R, Goldoni, M, Vettori, M, Folesani, G, Mozzoni, P, et al. Biomarkers of Oxidative Stress After Controlled Human Exposure to Ozone. Toxicol Lett (2002) 134(1-3):219–25. doi:10.1016/s0378-4274(02)00169-8
19. Thurston, GD, Balmes, JR, Garcia, E, Gilliland, FD, Rice, MB, Schikowski, T, et al. Outdoor Air Pollution and New-Onset Airway Disease. An Official American Thoracic Society Workshop Report. Ann Am Thorac Soc (2020) 17(4):387–98. doi:10.1513/AnnalsATS.202001-046ST
20. Srebot, V, Gianicolo, EA, Rainaldi, G, Trivella, MG, and Sicari, R. Ozone and Cardiovascular Injury. Cardiovasc Ultrasound (2009) 7:30. doi:10.1186/1476-7120-7-30
21. Li, J, Sun, S, Tang, R, Qiu, H, Huang, Q, Mason, TG, et al. Major Air Pollutants and Risk of COPD Exacerbations: A Systematic Review and Meta-Analysis. Int J Chron Obstruct Pulmon Dis (2016) 11:3079–91. doi:10.2147/copd.s122282
22. Huang, J, Li, G, Xu, G, Qian, X, Zhao, Y, Pan, X, et al. The Burden of Ozone Pollution on Years of Life Lost from Chronic Obstructive Pulmonary Disease in a City of Yangtze River Delta, China. Environ Pollut (2018) 242(Pt B):1266–73. doi:10.1016/j.envpol.2018.08.021
23. Qiu, H, Tan, K, Long, F, Wang, L, Yu, H, Deng, R, et al. The Burden of COPD Morbidity Attributable to the Interaction Between Ambient Air Pollution and Temperature in Chengdu, China. Int J Environ Res Public Health (2018) 15(3):492. doi:10.3390/ijerph15030492
24. Wang, Y, Wang, K, Cheng, W, and Zhang, Y. Global burden of Chronic Obstructive Pulmonary Disease Attributable to Ambient Ozone in 204 Countries and Territories During 1990-2019. Environ Sci Pollut Res Int (2022) 29(6):9293–305. doi:10.1007/s11356-021-16233-y
25. Safiri, S, Carson-Chahhoud, K, Noori, M, Nejadghaderi, SA, Sullman, MJM, Ahmadian Heris, J, et al. Burden of Chronic Obstructive Pulmonary Disease and its Attributable Risk Factors in 204 Countries and Territories, 1990-2019: Results From the Global Burden of Disease Study 2019. BMJ (Clinical research ed) (2022) 378:e069679. doi:10.1136/bmj-2021-069679
26. Zou, J, Sun, T, Song, X, Liu, YM, Lei, F, Chen, MM, et al. Distributions and Trends of the Global Burden of COPD Attributable to Risk Factors by SDI, Age, and Sex From 1990 to 2019: A Systematic Analysis of GBD 2019 Data. Respir Res (2022) 23(1):90. doi:10.1186/s12931-022-02011-y
27. GBD Risk Factors Collaborators. Global burden of 87 Risk Factors in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet (2020) 396(10258):1223–49. doi:10.1016/S0140-6736(20)30752-2
28. Institute for Health Metrics and Evaluation. GBD Results (2019). Available from: https://vizhub.healthdata.org/gbd-results/ (Accessed June 15, 2022).
29. Paulin, LM, Gassett, AJ, Alexis, NE, Kirwa, K, Kanner, RE, Peters, S, et al. Association of Long-Term Ambient Ozone Exposure With Respiratory Morbidity in Smokers. JAMA Intern Med (2020) 180(1):106–15. doi:10.1001/jamainternmed.2019.5498
30. Gaffney, AW, Himmelstein, DU, Christiani, DC, and Woolhandler, S. Socioeconomic Inequality in Respiratory Health in the US From 1959 to 2018. JAMA Intern Med (2021) 181(7):968–76. doi:10.1001/jamainternmed.2021.2441
31. Fischer, P, Hoek, G, Brunekreef, B, Verhoeff, A, and van Wijnen, J. Air Pollution and Mortality in The Netherlands: Are the Elderly More at Risk? Eur Respir J Suppl (2003) 40:34s–8s. doi:10.1183/09031936.03.00402503
32. Nordeide Kuiper, I, Svanes, C, Markevych, I, Accordini, S, Bertelsen, RJ, Braback, L, et al. Lifelong Exposure to Air Pollution and Greenness in Relation to Asthma, Rhinitis and Lung Function in Adulthood. Environ Int (2021) 146:106219. doi:10.1016/j.envint.2020.106219
33. Analitis, A, De' Donato, F, Scortichini, M, Lanki, T, Basagana, X, Ballester, F, et al. Synergistic Effects of Ambient Temperature and Air Pollution on Health in Europe: Results From the PHASE Project. Int J Environ Res Public Health (2018) 15(9):1856. doi:10.3390/ijerph15091856
34. Institute for Health Metrics and Evaluation. Global Burden of Disease Study 2019 (GBD 2019) Data Resources (2019). Available from: https://ghdx.healthdata.org/gbd-2019 (Accessed June 15, 2022).
35. Global Change Data Lab. Our World in Data (2021). Available from: https://ourworldindata.org/charts (Accessed June 15, 2022).
36. Wyckoff, MH, Wyllie, J, Aziz, K, de Almeida, MF, Fabres, JW, Fawke, J, et al. Neonatal Life Support 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Resuscitation (2020) 156:A156–A187. doi:10.1016/j.resuscitation.2020.09.015
37. Mathieu, E, Ritchie, H, Ortiz-Ospina, E, Roser, M, Hasell, J, Appel, C, et al. A Global Database of COVID-19 Vaccinations. Nat Hum Behav (2021) 5(7):947–53. doi:10.1038/s41562-021-01122-8
38. National Oceanic and Atmospheric Administation. Assessing the Global Climate in June 2024 (2021). Available from: https://www.noaa.gov/ (Accessed June 15, 2022).
39. Song, J, Pan, R, Yi, W, Wei, Q, Qin, W, Song, S, et al. Ambient High Temperature Exposure and Global Disease Burden During 1990-2019: An Analysis of the Global Burden of Disease Study 2019. Sci total Environ (2021) 787:147540. doi:10.1016/j.scitotenv.2021.147540
40. National Aeronautics and Space Administration. Moderate Resolution Imaging Spectroradiometer (2022). Available from: https://modis.gsfc.nasa.gov/ (Accessed June 15, 2022).
41. Wang, N, Mengersen, K, Tong, S, Kimlin, M, Zhou, M, and Hu, W. Global, Regional, and National Burden of Lung Cancer and its Attributable Risk Factors, 1990 to 2017. Cancer (2020) 126(18):4220–34. doi:10.1002/cncr.33078
42. Breto, C, Ionides, EL, and King, AA. Panel Data Analysis via Mechanistic Models. J Am Stat Assoc (2019) 115(531):1178–88. doi:10.1080/01621459.2019.1604367
43. Bollen, KA, and Brand, JE. A General Panel Model With Random and Fixed Effects: A Structural Equations Approach. Soc Forces (2010) 89(1):1–34. doi:10.1353/sof.2010.0072
44. Campelo Barroso Carneiro, VC, Ribeiro de Oliveira, PT, Rassy Carneiro, S, Cardoso Maciel, M, and da Silva Pedroso, J. Evidence of the Effect of Primary Care Expansion on Hospitalizations: Panel Analysis of 143 Municipalities in the Brazilian Amazon. PLoS One (2021) 16(4):e0248823. doi:10.1371/journal.pone.0248823
45. Cohen, AJ, Brauer, M, Burnett, R, Anderson, HR, Frostad, J, Estep, K, et al. Estimates and 25-Year Trends of the Global Burden of Disease Attributable to Ambient Air Pollution: An Analysis of Data From the Global Burden of Diseases Study 2015. Lancet (2017) 389(10082):1907–18. doi:10.1016/S0140-6736(17)30505-6
46. Abdul Jabbar, S, Tul Qadar, L, Ghafoor, S, Rasheed, L, Sarfraz, Z, Sarfraz, A, et al. Air Quality, Pollution and Sustainability Trends in South Asia: A Population-Based Study. Int J Environ Res Public Health (2022) 19(12):7534. doi:10.3390/ijerph19127534
47. Townend, J, Minelli, C, Mortimer, K, Obaseki, DO, Al Ghobain, M, Cherkaski, H, et al. The Association Between Chronic Airflow Obstruction and Poverty in 12 Sites of the Multinational BOLD Study. Eur Respir J (2017) 49(6):1601880. doi:10.1183/13993003.01880-2016
48. Gershon, AS, Warner, L, Cascagnette, P, Victor, JC, and To, T. Lifetime Risk of Developing Chronic Obstructive Pulmonary Disease: A Longitudinal Population Study. Lancet (2011) 378(9795):991–6. doi:10.1016/S0140-6736(11)60990-2
49. Shin, HH, Gogna, P, Maquiling, A, Parajuli, RP, Haque, L, and Burr, B. Comparison of Hospitalization and Mortality Associated With Short-Term Exposure to Ambient Ozone and PM2.5 in Canada. Chemosphere (2021) 265:128683. doi:10.1016/j.chemosphere.2020.128683
50. Clougherty, JE. A Growing Role for Gender Analysis in Air Pollution Epidemiology. Cien Saude Colet (2011) 16(4):2221–38. doi:10.1590/s1413-81232011000400021
51. World Health Organization. WHO Report on the Global Tobacco Epidemic 2021: Addressing New and Emerging Products (2021). Available from: https://www.who.int/publications/i/item/9789240032095 (Accessed July 27, 2021).
52. Xing, DF, Xu, CD, Liao, XY, Xing, TY, Cheng, SP, Hu, MG, et al. Spatial Association Between Outdoor Air Pollution and Lung Cancer Incidence in China. BMC Public Health (2019) 19(1):1377. doi:10.1186/s12889-019-7740-y
53. GBD Tobacco Collaborators. Spatial, Temporal, and Demographic Patterns in Prevalence of Smoking Tobacco Use and Attributable Disease Burden in 204 Countries and Territories, 1990-2019: A Systematic Analysis From the Global Burden of Disease Study 2019. Lancet (2021) 397(10292):2337–60. doi:10.1016/S0140-6736(21)01169-7
54. Ren, C, Williams, GM, Mengersen, K, Morawska, L, and Tong, S. Does Temperature Modify Short-Term Effects of Ozone on Total Mortality in 60 Large Eastern US Communities? An Assessment Using the NMMAPS Data. Environ Int (2008) 34(4):451–8. doi:10.1016/j.envint.2007.10.001
55. Crouse, DL, Pinault, L, Balram, A, Hystad, P, Peters, PA, Chen, H, et al. Urban Greenness and Mortality in Canada's Largest Cities: A National Cohort Study. Lancet Planet Health (2017) 1(7):e289–e97. doi:10.1016/S2542-5196(17)30118-3
56. Bereziartua, A, Chen, J, de Hoogh, K, Rodopoulou, S, Andersen, ZJ, Bellander, T, et al. Exposure to Surrounding Greenness and Natural-Cause and Cause-Specific Mortality in the ELAPSE Pooled Cohort. Environ Int (2022) 166:107341. doi:10.1016/j.envint.2022.107341
57. Stas, M, Aerts, R, Hendrickx, M, Delcloo, A, Dendoncker, N, Dujardin, S, et al. Exposure to Green Space and Pollen Allergy Symptom Severity: A Case-Crossover Study in Belgium. Sci total Environ (2021) 781:146682. doi:10.1016/j.scitotenv.2021.146682
58. Heo, S, and Bell, ML. The Influence of Green Space on the Short-Term Effects of Particulate Matter on Hospitalization in the U.S. For 2000-2013. Environ Res (2019) 174:61–8. doi:10.1016/j.envres.2019.04.019
59. Sun, S, Sarkar, C, Kumari, S, James, P, Cao, W, Lee, RS, et al. Air Pollution Associated Respiratory Mortality Risk Alleviated by Residential Greenness in the Chinese Elderly Health Service Cohort. Environ Res (2020) 183:109139. doi:10.1016/j.envres.2020.109139
60. Kasdagli, MI, Katsouyanni, K, de Hoogh, K, Lagiou, P, and Samoli, E. Associations of Air Pollution and Greenness With Mortality in Greece: An Ecological Study. Environ Res (2021) 196:110348. doi:10.1016/j.envres.2020.110348
61. Markevych, I, Schoierer, J, Hartig, T, Chudnovsky, A, Hystad, P, Dzhambov, AM, et al. Exploring Pathways Linking Greenspace to Health: Theoretical and Methodological Guidance. Environ Res (2017) 158:301–17. doi:10.1016/j.envres.2017.06.028
Keywords: chronic obstructive pulmonary disease, ozone, GBD, global warming, green space
Citation: Wang N, Cheng J, Xu Z, Wang S, Wang Q, Feng X, Hu W and Wang B (2024) Potential Drivers for the Spatiotemporal Patterns of the Global Burden of Chronic Obstructive Pulmonary Disease Attributable to Ambient Ozone, 1990–2019. Int J Public Health 69:1606062. doi: 10.3389/ijph.2024.1606062
Received: 04 April 2023; Accepted: 09 July 2024;
Published: 23 July 2024.
Edited by:
Kiros Berhane, Columbia University, United StatesReviewed by:
Mulubirhan Assefa Alemayohu, University of Pavia, ItalyCaroline Barakat, Ontario Tech University, Canada
Copyright © 2024 Wang, Cheng, Xu, Wang, Wang, Feng, Hu and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Baohua Wang, d2FuZ2Jhb2h1YUBuY25jZC5jaGluYWNkYy5jbg==
 Ning Wang
Ning Wang Jian Cheng2
Jian Cheng2