Abstract
Objective: High blood pressure is the leading risk factor for cardiovascular disease. The hypertension care cascade (HCC) is increasingly being used to evaluate the effectiveness of interventions. This systematic review aims to examine HCC in low-income settings.
Methods: The search strategy included articles published between January 2010 and April 2023. We excluded studies with incomplete HCC, on fragile patients or aged <18 years, reviews. We used the MOOSE guideline. Five researchers retrieved data on the survey year, country, population, HCC and diagnostic methods for hypertension. We used JBI Critical Appraisal Tools for quality assessment.
Results: Ninety-five articles were analyzed. Average hypertension prevalence was 33% (95% CI: 31%–34%), lower in LICs than in LMICs (25% vs. 34%). The overall mean awareness of hypertension was 48% (95% CI: 45%–51%), its treatment was 35% (95% IC: 32%–38%) and its control 16% (95% CI: 14%–18%). In almost all steps, percentages were lower in LICs and in Sub-Saharan Africa.
Conclusion: Trends in HCC vary between countries, with poorer performance in LICs. This review highlights the need for interventions tailored to low-income settings in order to improve hypertension care.
Introduction
Cardiovascular diseases (CVDs) are the main cause of illness, death, and disability worldwide. They were responsible for approximately 393 million (95% UI 368–417) disability adjusted life years (DALYs) in 2019 and were the leading cause of disease burden, accounting for 18.6 million (17.1–19.7) deaths. Raised blood pressure is the preeminent risk factor for CVDs, contributing to 235 million (95% IU 211–261) DALYs and 10.8 million (9.51–12.1) deaths. Overall, 8.5 million people died due to hypertension, 88% in Low (LIC) and Lower Middle-Income Countries (LMICs) [1, 2]. In LICs and LMICs, increases in the four main socio-economic related behavioral risk factors for hypertension, namely physical inactivity, unhealthy diet, tobacco use, and alcohol consumption, are strongly linked to the soaring hypertension epidemic [3–5]. While hypertension can be effectively managed at the primary care level through a combination of lifestyle changes, counselling, and pharmaceutical interventions, it is evident that many health systems in low income settings are ill-equipped to handle this condition [6–11]. According to the Lancet Commission on Hypertension and the World Heart Federation, controlled hypertension in affected patients are key indicators for health systems, and leads to reduced associated disability and premature mortality, in addition to avoiding substantial productivity losses [12, 13]. However, effective hypertension management relies on raising awareness about the condition and ensuring active engagement in appropriate treatment. The cascade of care, which encompass the journey from diagnosis to control, serves as a valuable framework to evaluating health systems, particularly in the context of chronic diseases [14, 15].
From 2000 to 2010, the rates of hypertension diagnosis, awareness, treatment, and control improved by ≥10% in High Income Countries. By contrast, in LICs and LMICs, improvements were narrow for awareness (32.3%–37.9%), treatment (24.9%–29.0%), and control (8.4%–7.7%) [16]. Hence, a deep dive into hypertension cascade of care is pivotal to define a standard for monitoring and planning public health strategies to manage hypertension control [17]. Despite extensive current evidence providing pooled analysis about hypertension care cascades across different continents, none appear to spotlight LICs and LMICs [1, 18]. Compared to both High and Upper-Middle Income countries, LICs and LMICs had higher age standardized mortality rates from high blood pressure and related cardiovascular diseases [16].
To effectively combat the mortality and morbidity associated with hypertension, it is imperative to deepen our understanding of disparities within the hypertension care continuum. This knowledge forms a crucial foundation for enhancing both national and international initiatives aimed at addressing uncontrolled hypertension. Quality improvement methodologies such as Plan-Do-Study-Act cycles, cascade analysis, process mapping, root cause analysis offer valuable tools for advancing our efforts in this critical endeavor [19].
Therefore, the objective of this study is to analyze disparities in hypertension prevalence, awareness, treatment, and control across various factors such as income level, geographical area, survey year, and population size.
Methods
Search Strategy and Inclusion Criteria
The review process was developed in accordance with Meta-analysis Of Observational Studies in Epidemiology (MOOSE) Guidelines [20]. It comprised searches from four electronic databases—PubMed, Embase, Scopus, and CHINAL Complete. The research protocol was uploaded on PROSPERO (ID CRD42022339717). The collected studies were published between January 2010 and April 2023, concerning hypertension care cascade in LICs and LMICs according to the World Bank classification by income level [21] (Supplementary Material S1). A selected combination of key words and MeSH terms coupled to hypertension care cascade were applied. We collected studies that included all of the following to inform the full hypertension care cascade: prevalence, awareness, treatment, and control for hypertension (Supplementary Material S2). The process of study selection comprised two-phases. First, search results were imported into Rayyan (https://www.rayyan.ai/) to manage citations. Second, two researchers conducted a title-abstract screening taking into consideration prevalence, awareness, treatment, and control of hypertension. A third reviewer solved conflicts. Studies not reporting a full care cascade for hypertension or with inconsistent data for prevalence and/or awareness and/or treatment and/or control of hypertension were excluded. Articles in English, French, Spanish, and Italian were included. Multiple years within the same studies on the same country were included if presenting clear data by year. Reviews, meta-analyses, comments, editorials, studies focusing on patients’ subgroups (e.g., chronic kidney disease, chronic cardiovascular disease), study settings that could embed selection bias (e.g., universities, hospitals), patients affected by specific diseases other than hypertension, or undergoing medical treatments for those conditions, or paediatric population (<18 years) were excluded.
Data Extraction
Five independent researchers conducted data extraction that included: the title, author/s, publication year, journal, survey year, country of study, country-income classification, sample size, study population, age range, diagnostic methods for hypertension, and information regarding the prevalence, awareness, treatment, and control of hypertension. Data about risk factors (e.g., smoking), BMI, diabetes, sex, age mean, or median were also retrieved when present. When absolute numbers were not available for care cascade steps, we retrieved them from unweighted frequency rates. Authors were contacted in case of discordant or not clearly reported data.
Quality Assessment
A cross-sectional assessment of the risk of bias was conducted using the Joanna Briggs Institute (JBI) Critical Appraisal Tools. Discrepancies were resolved through a two-round assessment process [22]. The specific criteria of JBI checklists can be found in the Supplementary Material (JBI Checklist).
Definition of Hypertension, Awareness, Treatment, and Control
The available studies use different definitions and different denominators to present their results, thus requiring a standardized way to present our results. Most of the studies employed a definition of hypertension as a systolic blood pressure (SBP) greater than or equal to 140 mmHg and/or a diastolic blood pressure (DBP) greater than or equal to 90 mmHg, or self-reported use of antihypertensive medication.
Awareness was measured as self-reported prior diagnosis of hypertension and expressed as the proportion of individuals with hypertension who were aware of their condition. Treatment was defined as the use of medication to manage hypertension at the time of the study and was reported either among all individuals with hypertension or among those who were aware of their condition. Control was defined as an SBP less than 140 mmHg and a DBP less than 90 mmHg, and was reported among all individuals with hypertension, those who were aware of their condition, or those receiving treatment for hypertension.
Data Analysis
The analysis of the cascade of care is based on cross-sectional studies and longitudinal studies with a cross-sectional data analysis. We considered four stages of the hypertension continuum of care which correspond to prevalence, awareness, treatment, and control. This approach focuses on identifying the losses that occur when patients move from one stage to another. In addition to loss between stages, we analyzed each stage of awareness, treatment, and control as a proportion of the population with hypertension. We used the metaprop package (STATA17) applying the Freeman Tukey transformation [23] and exact method for confidence intervals. We used a random effect model to consider differences across countries. Subgroups analysis considered Gross National Income (GNI), geographical area and time period before-after 2015 [24]. The I2 statistic was used to evaluate differences between subgroups. To test the results robustness, we conducted sensitivity analysis not considering May Measurement Month (MMM) studies as subjects are volunteers, or studies reporting only cascade step percentages or excluding studies with a high risk of bias (JBI score <5). We also performed sensitivity analysis excluding studies conducted in India, due to high number of publications, and excluding studies with an ill-defined survey date or a follow-up longer than 2 years. Since predictor variables (i.e., smoke habits, diabetes, BMI age) were not available for all the studies, we did not run any meta-regression.
Publication Bias
We used doiplot for publication bias, considering prevalence of hypertension as effect size [25], the LFK index to test statistical significance, and JBI qualitative evaluation to identify risk of bias [26]. We considered a JBI score <5 as high risk of bias, 5–6 as moderate and 7–9 as low.
Results
Through the search strings (Supplementary Material S2) 3,889 articles were retrieved. After references imported in Zotero and Rayyan, 1,043 articles were removed as duplicates. Following title and abstract analysis, 2,630 papers were excluded, failing to meet the inclusion criteria. 216 were eligible for full text analysis and 95 were eventually included for data extraction (Supplementary Figure S1). [27–121] Three studies had data about more than one population.
Eventually, 100 cascades of care were analysed (Supplementary Material S3). 16 studies were conducted in East Asia & Pacific, 36 in Sub-Saharan Africa, 31 in South Asia, 13 studies in Middle East & North Africa, 3 studies in Latin America & Caribbean and 1 in Europe & Central Asia. Among the included articles, 31 were MMMs. After the JBI quality assessment, 40 studies (including all the MMMs) were at high risk of bias, 20 at moderate, and 40 at low risk (Supplementary Material S4). Data on age, BMI, gender, diabetes, and smoking habits were not available for all articles (Supplementary Material S5).
Hypertension Prevalence
The overall prevalence of hypertension was 33% (95%CI: 31%–34%) (Figure 1). Six studies found a prevalence higher than 50% (Pakistan [101] and Ghana [48], 59%; Gaza and Cameroon [120], 57%; Philippines [103], 53%; India [66, 72], 72% and 52%). In three studies, hypertension prevalence was lower than 10% (Kyrgyzstan [84], 9%; Burkina Faso [35] and India [73], 8%). The doiplot graph suggested no publication bias (Supplementary Figure S2). The subgroup analysis for geographical area (Supplementary Figure S3) showed slight difference between geographical areas. Hypertension prevalence was lower in LICs than LMCIs (25% vs. 34%; p <0.001) as shown in (Figure 1). No significant differences in study results were observed when comparing data from studies conducted before and after 2015, as indicated in (Supplementary Figure S5). Furthermore, excluding studies with an ill-defined or excessively long survey date did not yield any discernible differences, as shown in (Supplementary Figure S4). Additionally, four studies reported hypertension data as percentage, an conducting a sensitivity analysis that excluded these articles resealed no significant variations, as depicted in (Supplementary Figures S6, S7).
FIGURE 1
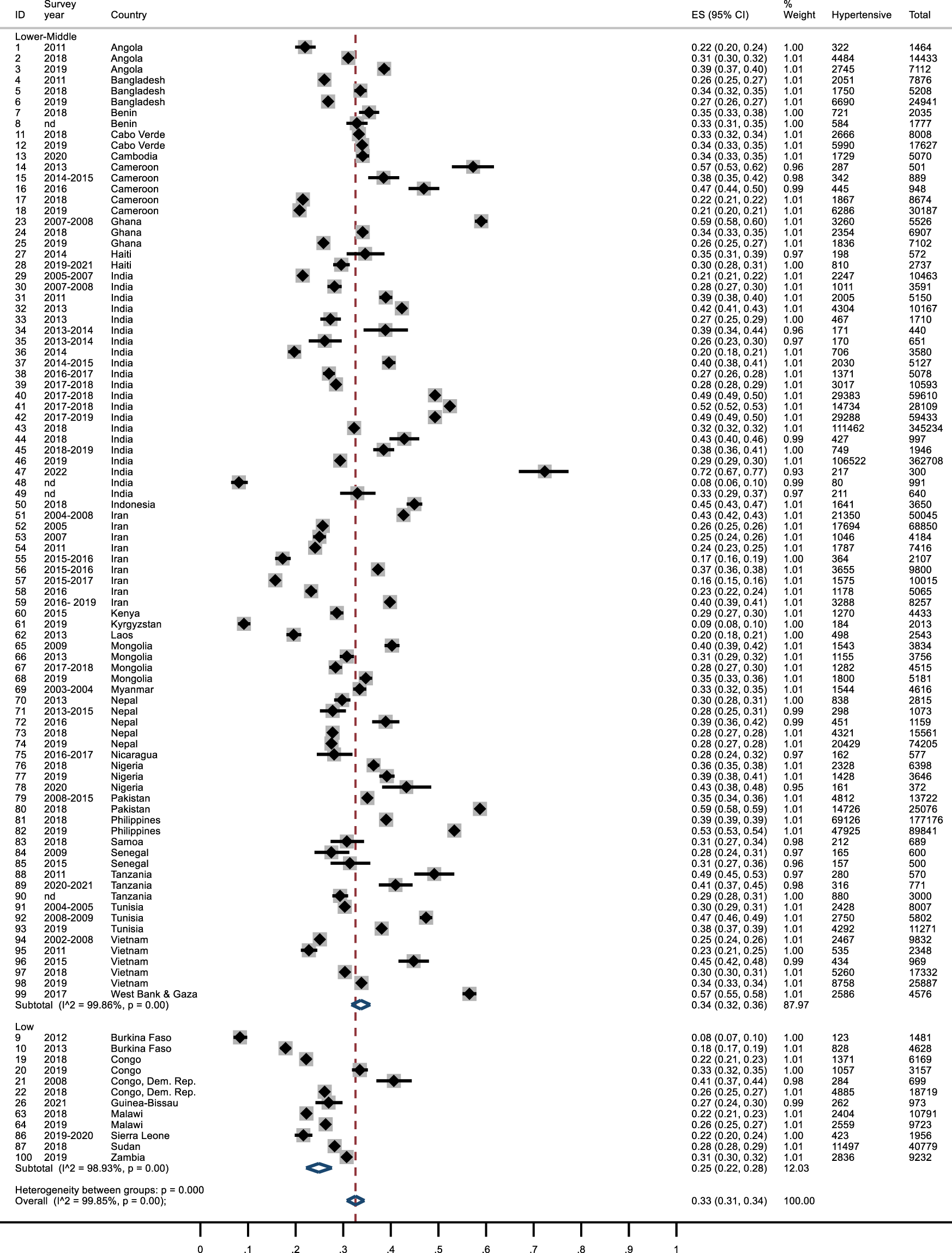
Forest plot of hypertension prevalence by country income. The effect size (ES) ranges from 0 to 1. The survey year refers to the year when the survey was conducted. The correspondence between the identification number (ID) and the reference is reported in Supplementary Table S3. Lower Income countries and Lower-Middle Income Countries, January 2010 and April 2023.
After excluding MMMs or studies with a high JBI risk of bias, the overall prevalence was similar to the comprehensive analysis, while confidence intervals were slightly wider, and the risk of publication bias seemed to increase (Supplementary Figures S8–S11). Percentage did not change after removing the studies conducted in India (Supplementary Figures S12, S13).
Awareness
The overall mean awareness among hypertensive subjects was 48% (95% CI: 0.45–0.51). In seven studies it was less than 20% (Burkina-Faso [36], Cameroon [41], Ghana [49], India [73], Malawi [86, 87] and Samoa [104]), while in four surveys is was higher than 75% (Bangladesh [32], India [69], Iran [80] and Pakistan [101]). Awareness was lower in LICs (0.31; 95% CI: 0.23–0.39) compared to MICs (0.50; 95% CI: 0.48–0.53) Figure 2. In Sub-Saharan Africa, 39% of subjects were aware of hypertension, less than in Middle East and North Africa (0.54; 95% CI: 0.45–0.64). In East Asia & Pacific and South Asia, awareness was around 50% (0.54; 95% CI: 0.49–0.59), whereas in Latin America & Caribbean was higher (0.65; 95% CI: 0.50–0.78) (Supplementary Figure S14). After 2015, awareness of hypertension appeared to have increased (Supplementary Figure S16). After excluding publications with data about awareness reported as percentage, MMMs, studies with JBI score<5 or reports from India, the values relating to the awareness of hypertension did not change significantly (Supplementary Figures S15, S17–S20).
FIGURE 2
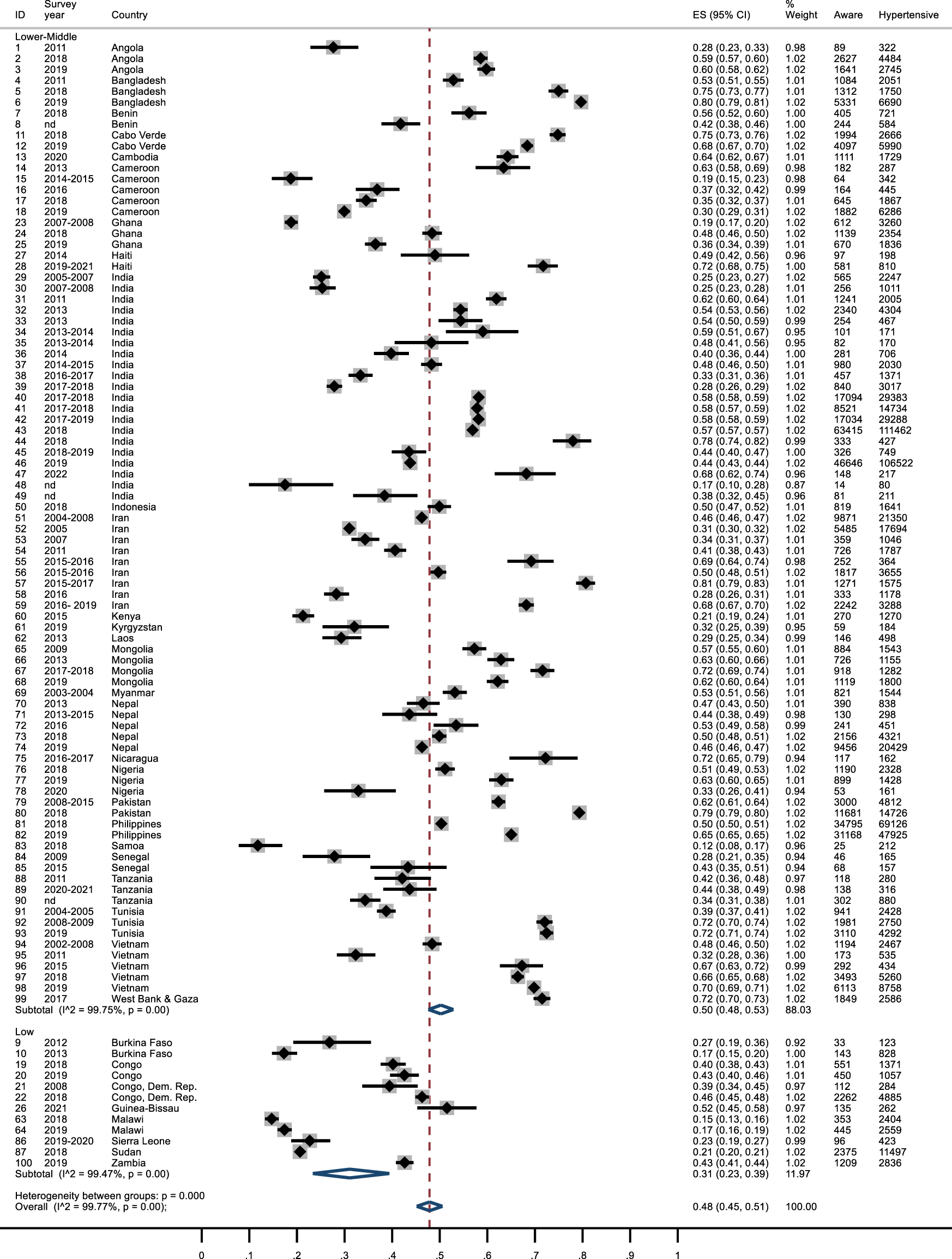
Awareness of hypertension forest plot by country income. Lower Income countries and Lower-Middle Income Countries, January 2010 and April 2023.
Treatment
Overall, 35% of hypertensive subjects were in treatment (95% IC: 0.32–0.38). Estimates ranged from 3% in Angola [27] to over 70% in Bangladesh [32], Iran [80]and Pakistan [101], although about half of the studies found a percentage of treated subjects between 20% and 50%. Treatment of hypertension was higher in LMICs (0.36; 95% CI: 0.33–0.39) than in LICs (0.22; 95% CI: 0.17–0.27) (Figure 3). There were differences across geographical areas: in Sub-Saharan Africa treatment rates were lower compared to Middle East & North Africa (26% vs. 44%). In Asia results were similar (South Asia 0.39; 95% CI: 0.35–0.43; East Asia & Pacific 0.37; 95% CI: 0.31–0.43). In Latin America almost half of hypertensive patients were treated (Supplementary Figure S21).
FIGURE 3
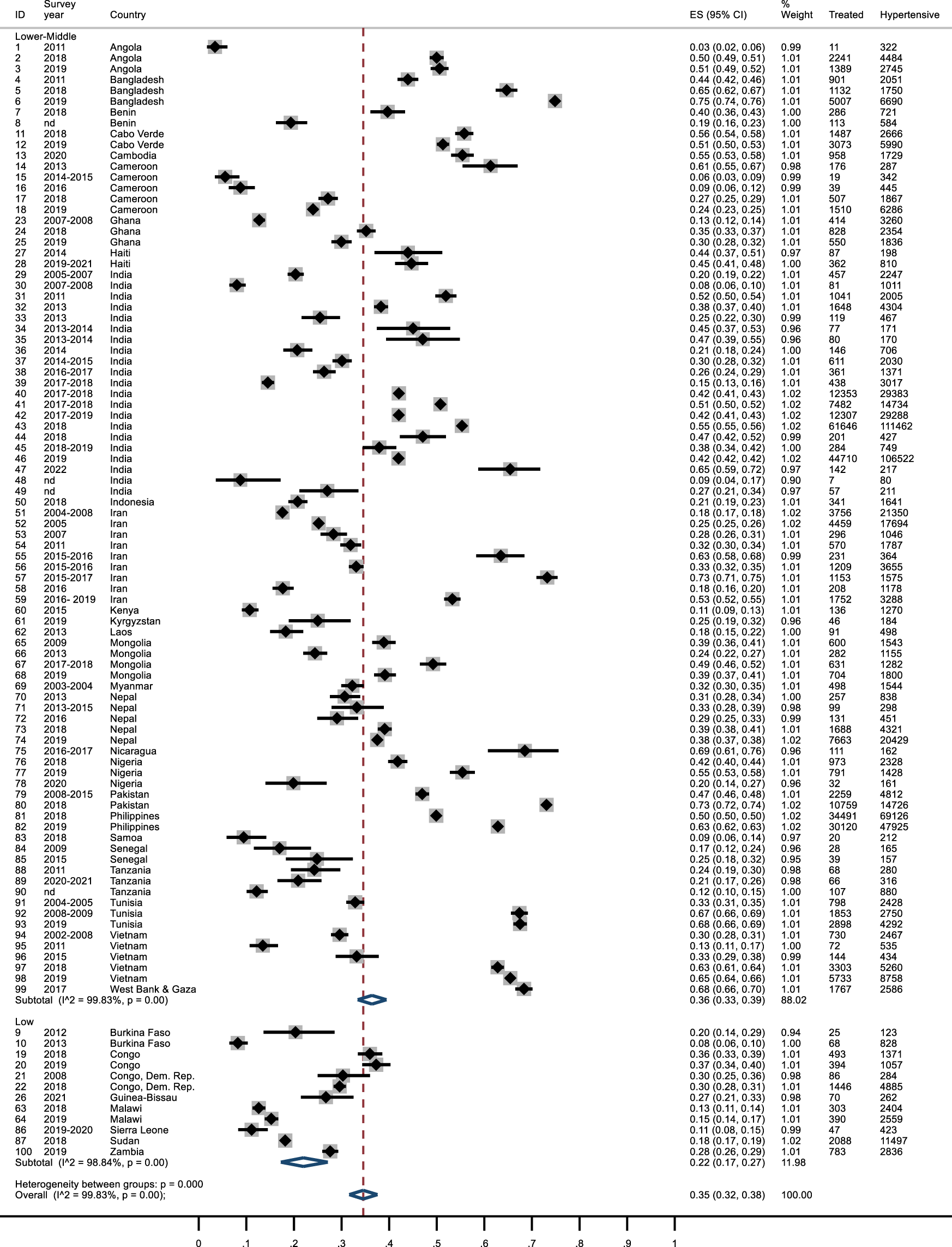
Forest plot: treatment of hypertension by income. Lower Income countries and Lower-Middle Income Countries, January 2010 and April 2023.
Treatment of hypertension seemed to have increased after 2015 (Supplementary Figure S23). The overall percentage of treated subjects among those aware of having hypertension was 74% (95% CI: 0.70–0.78), with no difference between LICs and LMICs (Supplementary Figure S24) and some differences across geographical areas (Supplementary Figure S25). After removing 13 studies with treated subjects reported as a percentage, results were similar (Supplementary Figure S26). After excluding the MMMs studies, the overall percentage decreased from 35% to 31% (Supplementary Figure S27). Similar results emerged after excluding studies with a JBI score <5 (Supplementary Figure S28). Percentages did not change after removing results from India (Supplementary Figure S29).
Control
Overall, 16% of hypertensive subjects had their hypertension controlled (95% CI: 0.14–0.18). Three studies reported a control of hypertension <2% (Angola [27], Cameroon [41] and Ghana [49]), whereas two studies in Bangladesh [31, 32], one in India [68] and two in Iran [78, 80] found >40% of controlled hypertensive subjects. In LICs the percentage of controlled hypertension was lower than LMICs (11% vs. 17%) (Figure 4). Studies conducted in Sub-Saharan Africa showed a percentage below the global mean (0.11; 95% CI: 0.09–0.13), while the other geographical areas had higher values (Supplementary Figure S30). After excluding MMMs studies or those with a JBI score <5, the percentage of controlled hypertension reduced to 14% (Supplementary Figures S32, S33). Control of hypertension was higher in more recent studies (Supplementary Figure S34). Results did not change after removing studies from India or those with data reported as percentages or studies with ill-defined survey date (Supplementary Figures S31, S35, S36). Subjects with controlled hypertension, among those being treated, were about 47% (95% CI: 0.45–0.50), without significant differences between LICs and LMICs (Supplementary Figure S37). Four studies reported a score <20% (Cameroon [41] 16%; Ghana [49] 12%; India [60, 61] 19%), while in 3 studies >80% of treated subjects were controlled (India [62, 64] 84% and 87%; Laos [85] 91%). Sub-Saharan Africa showed a percentage of treated subjects below the global mean (42%) (Supplementary Figure S38).
FIGURE 4
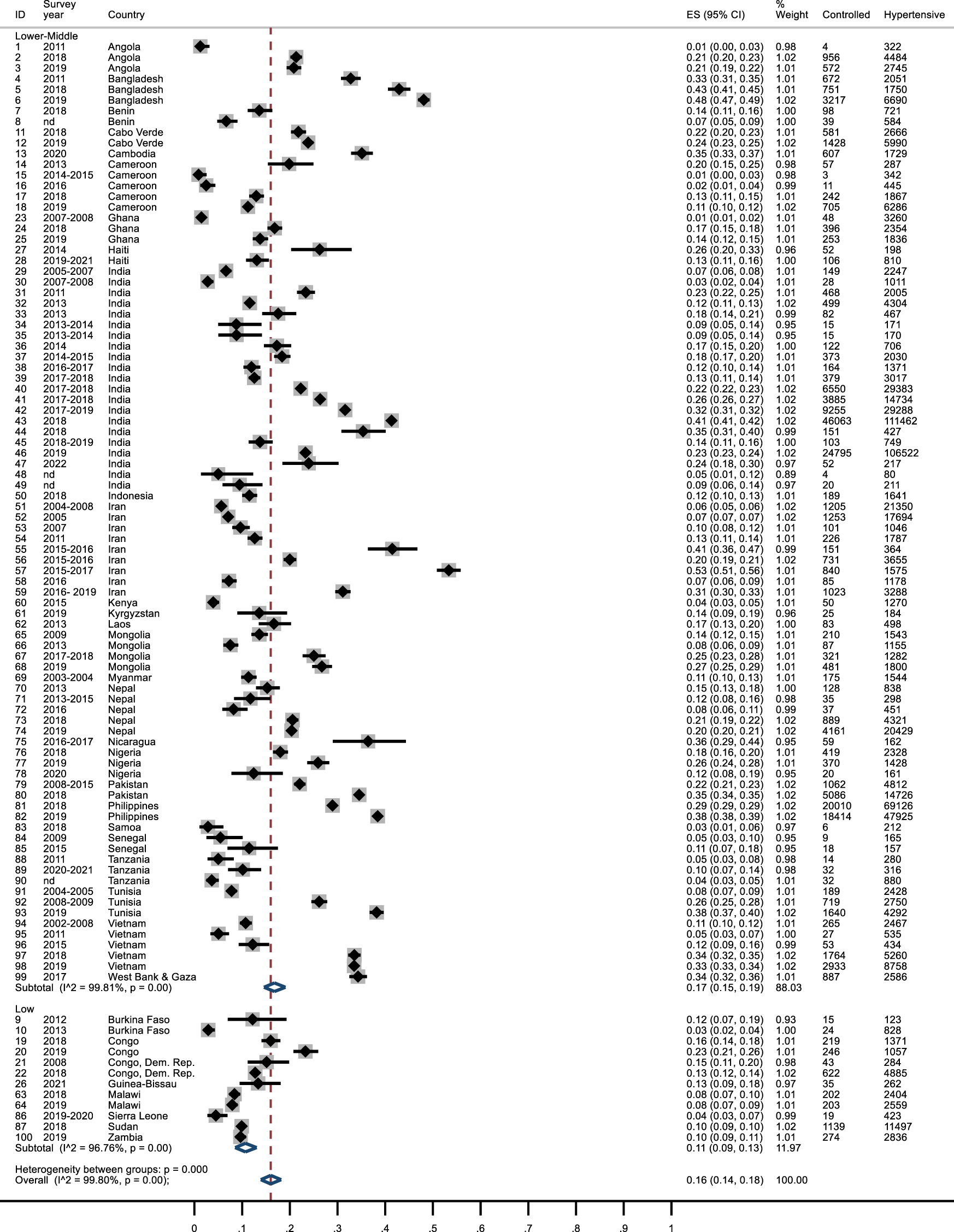
Forest plot: control of hypertension by income. Lower Income countries and Lower Middle-Income Countries, January 2010 and April 2023.
Discussion
To our knowledge, this study represents the first comprehensive examination of the complete hypertension cascade of care specifically focused on LICs and LMICs. The findings offer valuable insights into the global challenge of hypertension in resource-constrained settings, revealing significant variations across countries and geographical regions. We collected data from 35 countries, representing a total population of 1.5 billion individuals.
Our study highlights the overall unpreparedness of the examined health systems, with only a small percentage of individuals with hypertension being aware of their condition and receiving treatment, and an even lower percentage achieving control over their hypertension. Although positive results in hypertension control rates were observed during the 80s and 90s, it has since plateaued, raising concerns about a potential decline in progress [122].
These findings underscore the pressing need for enhanced hypertension care and management, particularly in low-income settings. Supporting the idea that LICs and LMICs should be considered separately, our analysis revealed that LMICs outperformed LICs in all stages of the cascade of care. This is consistent with previous research, emphasizing that hypertension poses a growing challenge regardless of the income level [1]. Significant gaps exist among countries and especially across geographical areas, [1, 104]. East Asia and the Pacific region exhibited the highest prevalence rates at 32%, whereas South Asia had the lowest rates at 24%. Conversely, Latin America and the Caribbean demonstrated better performance in terms of awareness, treatment, and control, while Sub-Saharan African countries showed lower scores. Our sensitivity analysis confirmed that the limited data from Latin America and the Caribbean did not unduly influence our overall results. Social determinants of health play a crucial role in noncommunicable diseases [123]. Addressing the hypertension epidemic requires a multidisciplinary and multilateral approach to prevent further widening of health gaps, particularly in more fragile countries [124]. Lower levels of education and/or income are risk factors associated with higher dropout rates from the care pathway [125]. Moreover, inadequate patients’ preparedness may impede understanding of health information and limit patients’ engagement. Out of pocket payments and opportunity costs remain a significant barriers to accessing care [126], exacerbated by staff shortage. Removing or lowering user fees and investments in mid-level providers in hypertension management in low-income settings are both important policies to improve access to care [127, 128].
Prioritizing health policies that specifically target hypertension care in vulnerable populations can effectively reduce disparities in healthcare access and mitigate the risk of catastrophic health expenditures [129]. Moreover, the implementation of a quality improvement collaborative approach to promote the adoption of hypertension (HTN) care cascade and its integration with communicable disease programs, notably HIV, has demonstrated noteworthy effectiveness in the short term while also presenting favorable long-term prospects, as underscored in the study by Basenero et al. [19].
However, it is important to note that, even when health systems are optimally organized, simply ensuring access may not be sufficient to improve population health [130]. Quality standards, such as ensuring the right patient receives care in the right place and at the right time [131] are essential components that must be incorporated to achieve significant improvements in overall population health outcomes.
In contrast to the recent study conducted by the NCD Risk Factor Collaboration (NCD-RisC) [1], our review focused exclusively on peer-reviewed publications available in prominent scientific databases, with the deliberate exclusion of studies from grey literature. Despite the presence of numerous grey literature publications (i.e. World Bank reports), we decided to exclude it. Several compelling reasons informed this choice. First of all, it should be note that the WHO reports are themselves based on the MMM studies, which were the included in our investigation. Furthermore, our rigorous analysis and inclusion criteria demanded a stringent assessment of cluster definitions within the studies considered dictated by the cascade of care model. This involved the comprehensive consideration of all stages of the care cascade and the examination of general populations rather than specific clusters (i.e. HIV, CKD, etc.). In order to ensure the robustness of our findings, sensitivity analyses were conducted to confirm that the exclusion of specific items did not significantly impact the final results [132].
Additionally, we observed a growing trend of policies aimed at reducing the burden of cardiovascular diseases, leading to an increase in national and sub-national surveys as well as the development of technical packages [74]. This trend, however, results in multiple publications for the same country, which, for the purpose of our study, appeared inconsistent and-or redundant. Even hypertension prevalence-based studies and large courts surveillance programs that did not fit our inclusion criteria are pivotal to implement public health policies and scarce healthcare resources’ management [133, 134].
A distinctive advantage of this review lies in its comprehensive examination of the entire care cascade, coupled with the differentiation between, LICs and LMICs as distinct entities. This approach not only facilitates the assessment of disease control but also enables the identification of critical steps within the cascade where a significant proportion of individuals may be lost, thus offering valuable insights to inform the development of interventions and future policy initiatives [110].
Furthermore, the identification of dropout rates at each stage of the cascade has the potential to highlight the need to expand the scope of comprehensive, multidimensional interventions, particularly at the primary care level, with the aim of improving overall health outcomes.
One of the limitations we encountered pertains to the diverse methods employed for blood pressure measurement in certain studies, although it’s worth highlighting that, in the majority of cases, the WHO guidelines were adhered to. However, it is crucial to emphasize that all the studies we included into our analysis uniformly embraced the internationally recognized parameter of a fixed threshold for diagnosing hypertension, specifically set at 140–90 mmHg [135].
A validated automated sphygmomanometer was used in all studies, but digital (OMRON) sphygmomanometers were not systematically applied. Additionally, paper-based questionnaires may have introduced bias in data recording. These disparities may have affected some of the outcomes observed across countries and regions. However, key features in the questionnaires regarding individuals’ history of hypertension diagnosis and hypertensive of medication use were comparable. As already stated, we considered pregnant women and patients affected by other chronic conditions (i.e., kidney or infectious disease) as potential bias for the results, so we excluded studies focusing on these populations from our analysis.
Although we did not conduct a temporal analysis due to insufficient data, it is worth noting that since 2015, some countries have shown signs of improvement in terms of awareness, treatment, and control of hypertension. These positive changes may be attributed to local advocacy efforts and awareness campaigns, highlighting the potential for enhanced hypertension care even in resource-constrained settings [43, 44].
The hypertension cascade of care steps analyzed in this study did not include information about gender and other variables due to limited reporting. We were only able to provide an average representation of the female population, which comprised approximately 50% of the total participants interviewed across the studies. However, it’s worth noting that in some studies, this percentage ranged from as low as 25% to as high as 70%.
In less than half of the studies included in our analysis, we could readily extract specific data on individuals with diabetes, smokers, or those who were overweight. Notably, when it came to overweight, many studies primarily reported data only for obese subjects (BMI≥30). Moreover, there was uneven representation of countries, and methodological differences could led to heterogeneous results. To address these limitations, subgroup analyses were performed. Additionally, the JBI quality scores for some studies were found to be low.
MMM studies constitute a significant component of the meta-analysis basket of publications. Despite the limitations associated with recruiting voluntary participants, which may result in non-representative sampling, these surveys offer valuable insights for understanding global trends more accurately. Incorporating MMM studies in the analysis allows for a more comprehensive examination and enables stakeholders to better understand changes in care cascades over time.
Lastly, it is important to highlight that while the current care cascade framework includes outcome quality measures, it regrettably lacks any specific mentions pertaining to the quality of health services. The omission of quality-based indicators is notable because it restricts the comprehensive analysis of health system intervention performance. The inclusion of quality-based measures in the evaluation framework is essential to gain a more holistic understanding of the effectiveness of interventions. It allows for a nuanced assessment of not only outcomes, but also the processes and structures that underpin the delivery of healthcare. By overlooking the quality of health services, we risk an incomplete assessment of health interventions, hindering our ability to make informed decisions and improve health systems [132].
Conclusion
This study further substantiates the escalating issue of hypertension in LICs and the consistent disparities observed when compared to LMICs. It is imperative to enhance awareness regarding the prevalence, treatment, and control of hypertension among the population, particularly in LICs, to facilitate adequate investment in the management of this disease. This cross-country comparison study, focusing on hypertension care cascades, underscores the critical importance of conducting comprehensive and rigorous assessments of the entire spectrum of hypertension care. Employing standardized methods ensures the consistency and comparability of results across diverse settings.
Additionally, it is imperative to expand data collection efforts beyond the traditional clinical metrics. Gathering comprehensive information on aspects such as care delivery processes, health education initiatives, and patient attendance patterns can offer invaluable insights.
Furthermore, it is imperative to expand data collection efforts beyond the traditional clinical metrics. Gathering comprehensive information on aspects such as care delivery processes, health education initiatives, and patient attendance patterns can offer invaluable insights. These insights not only aid in shaping health policy planning but also provide a holistic perspective on the multifaceted nature of hypertension management.
As we advance in our understanding of hypertension care cascades, it is essential that future research places a strong emphasis on the incorporation of quality-adjusted service metrics. These metrics serve as vital tools in driving the development of successful hypertension management systems. They enable us to assess not only the quantity but also the quality of healthcare services, ultimately leading to more effective and patient-centered care.
Statements
Author contributions
The authors confirm contribution to the paper as follows: study conception and design: FT; data collection: FF, DL; analysis and interpretation of results: FF, DL, BO; draft manuscript preparation: FF, DL, FT. All authors reviewed the results and approved the final version of the manuscript.
Funding
This study was supported by the grant number 183760 by Swiss Programme for Research on Global Issues for Development (r4d programme) a joint funding initiative by the Swiss Agency for Development and Cooperation (SDC) and the Swiss National Science Foundation (SNSF). https://p3.snf.ch/project-183760, https://www.snf.ch/en, https://www.eda.admin.ch/sdc. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Acknowledgments
We thank Brady Hooley, Sierra Ottilie-Kovelman, and Anna Verjas for their assistance in data extraction and full text screening of the articles.
Conflict of interest
The authors declare that they do not have any conflicts of interest.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/ijph.2023.1606428/full#supplementary-material
Supplementary Data sheet 1JBI Checklist
Supplementary Data Sheet 2Supplementary Material S1
Supplementary Data sheet 3Supplementary Material S2
Supplementary Data sheet 4Supplementary Material S3
Supplementary Data sheet 5Supplementary Material S4
Supplementary Data sheet 6Supplementary Material S5
Supplementary Data sheet 7Supplementary Figures (S1-S38)
References
1.
NCD Risk Factor Collaboration (NCD-RisC). Worldwide Trends in Hypertension Prevalence and Progress in Treatment and Control From 1990 to 2019: A Pooled Analysis of 1201 Population-Representative Studies With 104 Million Participants. Lancet Lond Engl (2021) 398:957–80. 10.1016/S0140-6736(21)01330-1
2.
Zhou B Perel P Mensah GA Ezzati M . Global Epidemiology, Health Burden and Effective Interventions for Elevated Blood Pressure and Hypertension. Nat Rev Cardiol (2021) 18:785–802. 10.1038/s41569-021-00559-8
3.
Bentham J Singh GM Danaei G Green R Lin JK Stevens GA et al Multi-Dimensional Characterisation of Global Food Supply From 1961-2013. Nat Food (2020) 1:70–5. 10.1038/s43016-019-0012-2
4.
Griswold MG Fullman N Hawley C Arian N Zimsen SRM Tymeson HD et al Alcohol Use and Burden for 195 Countries and Territories, 1990–2016: A Systematic Analysis for the Global Burden of Disease Study 2016. The Lancet (2018) 392:1015–35. 10.1016/S0140-6736(18)31310-2
5.
Bilano V Gilmour S Moffiet T d’Espaignet ET Stevens GA Commar A et al Global Trends and Projections for Tobacco Use, 1990-2025: An Analysis of Smoking Indicators From the WHO Comprehensive Information Systems for Tobacco Control. Lancet Lond Engl (2015) 385:966–76. 10.1016/S0140-6736(15)60264-1
6.
Ettehad D Emdin CA Kiran A Anderson SG Callender T Emberson J et al Blood Pressure Lowering for Prevention of Cardiovascular Disease and Death: A Systematic Review and Meta-Analysis. Lancet Lond Engl (2016) 387:957–67. 10.1016/S0140-6736(15)01225-8
7.
Valenzuela PL Carrera-Bastos P Gálvez BG Ruiz-Hurtado G Ordovas JM Ruilope LM et al Lifestyle Interventions for the Prevention and Treatment of Hypertension. Nat Rev Cardiol (2021) 18:251–75. 10.1038/s41569-020-00437-9
8.
Carey RM Muntner P Bosworth HB Whelton PK . Prevention and Control of Hypertension: JACC Health Promotion Series. J Am Coll Cardiol (2018) 72:1278–93. 10.1016/j.jacc.2018.07.008
9.
Appel LJ . Lifestyle Modification as a Means to Prevent and Treat High Blood Pressure. J Am Soc Nephrol JASN (2003) 14:S99–102. 10.1097/01.asn.0000070141.69483.5a
10.
Albelbeisi AH Albelbeisi A El Bilbeisi AH Taleb M Takian A Akbari-Sari A . Public Sector Capacity to Prevent and Control of Noncommunicable Diseases in Twelve Low- and Middle-Income Countries Based on WHO-PEN Standards: A Systematic Review. Health Serv Insights (2021) 14:1178632920986233. 10.1177/1178632920986233
11.
World Health Organization. Assessing National Capacity for the Prevention and Control of Noncommunicable Diseases: Report of the 2019 Global Survey. Geneva: World Health Organization (2020).
12.
Adler AJ Prabhakaran D Bovet P Kazi DS Mancia G Mungal-Singh V et al Reducing Cardiovascular Mortality Through Prevention and Management of Raised Blood Pressure: A World Heart Federation Roadmap. Glob Heart (2015) 10:111–22. 10.1016/j.gheart.2015.04.006
13.
Olsen MH Angell SY Asma S Boutouyrie P Burger D Chirinos JA et al A Call to Action and a Lifecourse Strategy to Address the Global Burden of Raised Blood Pressure on Current and Future Generations: The Lancet Commission on Hypertension. Lancet Lond Engl (2016) 388:2665–712. 10.1016/S0140-6736(16)31134-5
14.
Beaglehole R Epping-Jordan J Patel V Chopra M Ebrahim S Kidd M et al Improving the Prevention and Management of Chronic Disease in Low-Income and Middle-Income Countries: A Priority for Primary Health Care. The Lancet (2008) 372:940–9. 10.1016/S0140-6736(08)61404-X
15.
Berry KM Parker WA McHiza ZJ Sewpaul R Labadarios D Rosen S et al Quantifying Unmet Need for Hypertension Care in South Africa Through a Care Cascade: Evidence From the SANHANES, 2011-2012. BMJ Glob Health (2017) 2:e000348. 10.1136/bmjgh-2017-000348
16.
Mills KT Bundy JD Kelly TN Reed JE Kearney PM Reynolds K et al Global Disparities of Hypertension Prevalence and Control: A Systematic Analysis of Population-Based Studies From 90 Countries. Circulation (2016) 134:441–50. 10.1161/CIRCULATIONAHA.115.018912
17.
Schmidt B-M Durao S Toews I Bavuma CM Hohlfeld A Nury E et al Screening Strategies for Hypertension. Cochrane Database Syst Rev (2020) 2020:CD013212. 10.1002/14651858.CD013212.pub2
18.
Beaney T Schutte AE Tomaszewski M Ariti C Burrell LM Castillo RR et al May Measurement Month 2017: An Analysis of Blood Pressure Screening Results Worldwide. Lancet Glob Health (2018) 6:e736–43. 10.1016/S2214-109X(18)30259-6
19.
Basenero A Neidel J Ikeda DJ Ashivudhi H Mpariwa S Kamangu JWN et al Integrating Hypertension and HIV Care in Namibia: A Quality Improvement Collaborative Approach. PLOS ONE (2022) 17:e0272727. 10.1371/journal.pone.0272727
20.
Stroup DF Berlin JA Morton SC Olkin I Williamson GD Rennie D et al Meta-Analysis of Observational Studies in Epidemiology: A Proposal for Reporting. Meta-Analysis of Observational Studies in Epidemiology (MOOSE) Group. JAMA (2000) 283:2008–12. 10.1001/jama.283.15.2008
21.
World Bank Country and Lending Groups. World Bank Data Help Desk (2022). Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups (Accessed March 24, 2022).
22.
Munn Z Moola S Riitano D Lisy K . The Development of a Critical Appraisal Tool for Use in Systematic Reviews Addressing Questions of Prevalence. Int J Health Pol Manag (2014) 3:123–8. 10.15171/ijhpm.2014.71
23.
Nyaga VN Arbyn M Aerts M . Metaprop: A Stata Command to Perform Meta-Analysis of Binomial Data. Arch Public Health (2014) 72:39. 10.1186/2049-3258-72-39
24.
Forouzanfar MH Liu P Roth GA Ng M Biryukov S Marczak L et al Global Burden of Hypertension and Systolic Blood Pressure of at Least 110 to 115 Mm Hg, 1990-2015. JAMA (2017) 317:165–82. 10.1001/jama.2016.19043
25.
Hunter JP Saratzis A Sutton AJ Boucher RH Sayers RD Bown MJ . In Meta-Analyses of Proportion Studies, Funnel Plots Were Found to Be an Inaccurate Method of Assessing Publication Bias. J Clin Epidemiol (2014) 67:897–903. 10.1016/j.jclinepi.2014.03.003
26.
Barker TH Migliavaca CB Stein C Colpani V Falavigna M Aromataris E et al Conducting Proportional Meta-Analysis in Different Types of Systematic Reviews: A Guide for Synthesisers of Evidence. BMC Med Res Methodol (2021) 21:189. 10.1186/s12874-021-01381-z
27.
Pires JE Sebastião YV Langa AJ Nery SV . Hypertension in Northern Angola: Prevalence, Associated Factors, Awareness, Treatment and Control. BMC Public Health (2013) 13:90. 10.1186/1471-2458-13-90
28.
Victória Pereira S Neto M Feijão A Oliveira P Brandão M Soito E et al May Measurement Month 2018: An Analysis of Blood Pressure Screening Results From Angola. Eur Heart J Suppl (2020) 22:H8–10. 10.1093/eurheartj/suaa015
29.
Victória Pereira S Neto M Feijão A Lutucuta E Mbala C Muela H et al May Measurement Month 2019: An Analysis of Blood Pressure Screening Results From Angola. Eur Heart J Suppl (2021) 23:B9–11. 10.1093/eurheartj/suab038
30.
Rahman MDM Gilmour S Akter S Abe SK Saito E Shibuya K . Prevalence and Control of Hypertension in Bangladesh: A Multilevel Analysis of a Nationwide Population-Based Survey. J Hypertens (2015) 33:465–72. 10.1097/HJH.0000000000000421
31.
Malik FTN Al Mamun MA Ishraquzzaman M Kalimuddin M Shahriar Huq T Rahman MS et al May Measurement Month 2018: An Analysis of Blood Pressure Screening Results From Bangladesh. Eur Heart J Suppl (2020) 22:H20–2. 10.1093/eurheartj/suaa086
32.
Malik FTN Al Mamun MA Choudhury SR Ishraquzzaman M Kalimuddin M Huq TS et al May Measurement Month 2019: An Analysis of Blood Pressure Screening Results From Bangladesh. Eur Heart J Suppl (2021) 23:B21–3. 10.1093/eurheartj/suab017
33.
Houehanou C Sonou A Adjagba P Dohou H Hounkponou M Kpolédji G et al May Measurement Month 2018: An Analysis of Blood Pressure Screening Results From Benin. Eur Heart J Suppl (2022) 24:F9–11. 10.1093/eurheartjsupp/suac039
34.
Desormais I Amidou SA Houehanou YC Houinato SD Gbagouidi GN Preux PM et al The Prevalence, Awareness, Management and Control of Hypertension in Men and Women in Benin, West Africa: The TAHES Study. BMC Cardiovasc Disord (2019) 19:303. 10.1186/s12872-019-01273-7
35.
Doulougou B Kouanda S Ouédraogo GH Meda BI Bado A Zunzunegui MV . Awareness, Treatment, Control of Hypertension and Utilization of Health Care Services Following Screening in the North-Central Region of Burkina Faso. Pan Afr Med J (2014) 19:259. 10.11604/pamj.2014.19.259.4707
36.
Cissé K Kouanda S Coppieters’t Wallant Y Kirakoya-Samadoulougou F . Awareness, Treatment, and Control of Hypertension Among the Adult Population in Burkina Faso: Evidence From a Nationwide Population-Based Survey. Int J Hypertens (2021) 2021:5547661–9. 10.1155/2021/5547661
37.
Azevedo V Dias L Soares I Garcia G Xia X Ster AC et al May Measurement Month 2018: An Analyses of Blood Pressure Screening Results From Cabo Verde. Eur Heart J Suppl (2020) 22:H30–2. 10.1093/eurheartj/suaa020
38.
Azevedo V Dias L Garcia G Soares I Silva M Delgado I et al May Measurement Month 2019: An Analysis of Blood Pressure Screening Results From Cape Verde. Eur Heart J Suppl (2021) 23:B37–9. 10.1093/eurheartj/suab053
39.
Chham S Buffel V Van Olmen J Chhim S Ir P Wouters E . The cascade of Hypertension Care in Cambodia: Evidence From a Cross-Sectional Population-Based Survey. BMC Health Serv Res (2022) 22:838. 10.1186/s12913-022-08232-7
40.
Tianyi FL Agbor VN Njamnshi AK . Prevalence, Awareness, Treatment, and Control of Hypertension in Cameroonians Aged 50 Years and Older: A Community-Based Study. Health Sci Rep (2018) 1:e44. 10.1002/hsr2.44
41.
Lemogoum D Van de Borne P Lele CEB Damasceno A Ngatchou W Amta P et al Prevalence, Awareness, Treatment, and Control of Hypertension Among Rural and Urban Dwellers of the Far North Region of Cameroon. J Hypertens (2018) 36:159–68. 10.1097/HJH.0000000000001513
42.
Mbouemboue OP Ngoufack TJO . High Blood Pressure Prevalence, Awareness, Control, and Associated Factors in a Low-Resource African Setting. Front Cardiovasc Med (2019) 6:119. 10.3389/fcvm.2019.00119
43.
Dzudie A Njume E Boombhi J Awungia A Ndom MS Ebasone PV et al May Measurement Month 2018: Blood Pressure Screening Results in Cameroon. Eur Heart J Suppl (2020) 22:H33–6. 10.1093/eurheartj/suaa019
44.
Dzudie A Njume E Mfekeu LK Djomou A Ba H Ndom MS et al May Measurement Month 2019: An Analysis of Blood Pressure Screening Results From Cameroon. Eur Heart J Suppl (2021) 23:B33–6. 10.1093/eurheartj/suab056
45.
Ellenga Mbolla BF Kouala Landa CM Bakekolo PR Makani Bassakouahou JK Bouithy SN Eyeni-Sinomono T et al May Measurement Month 2018: An Analysis of Blood Pressure Screening Results From Republic of the Congo. Eur Heart J Suppl (2020) 22:H47–9. 10.1093/eurheartj/suaa026
46.
Ellenga-Mbolla B Makani-Bassakouahou J Landa CK Monabeka M-G Ossou-Nguiet P-M Ngamami SM et al May Measurement Month 2019: An Analysis of Blood Pressure Screening Results From Republic of the Congo. Eur Heart J Suppl (2021) 23:B49–51. 10.1093/eurheartj/suab028
47.
Katchunga PB M’Buyamba-Kayamba JR Masumbuko BE Lemogoum D Kashongwe ZM Degaute JP et al Hypertension in the Adult Congolese Population of Southern Kivu: Results of the Vitaraa Study. Presse Médicale (2011) 40:e315–23. 10.1016/j.lpm.2010.10.036
48.
Buila NB Ngoyi GN Bayauli PM Katamba FK Lubenga YN Kazadi SM et al Analysis of Blood Pressure and Selected Cardiovascular Risk Factors in the Democratic Republic of the Congo: The May Measurement Month 2018 Results. Eur Heart J Suppl (2020) 22:H50–2. 10.1093/eurheartj/suaa027
49.
Sanuade OA Awuah RB Kushitor M . Hypertension Awareness, Treatment and Control in Ghana: A Cross-Sectional Study. Ethn Health (2020) 25:702–16. 10.1080/13557858.2018.1439898
50.
Twumasi-Ankrah B Myers-Hansen GA Adu-Boakye Y Tannor EK Nyarko OO Boakye E et al May Measurement Month 2018: An Analysis of Blood Pressure Screening Results From Ghana. Eur Heart J Suppl (2020) 22:H59–61. 10.1093/eurheartj/suaa029
51.
Twumasi-Ankrah B Poulter NR Tannor EK Adu-Boakye Y Nyarko OO Opoku G et al May Measurement Month 2019: An Analysis of Blood Pressure Screening Results From Ghana-Sub-Saharan Africa. Eur Heart J Suppl (2021) 23:B62–5. 10.1093/eurheartj/suab023
52.
Turé R Damasceno A Djicó M Lunet N . Prevalence, Awareness, Treatment, and Control of Hypertension in Bissau, Western Africa. J Clin Hypertens (2022) 24:358–61. 10.1111/jch.14443
53.
Polsinelli VB Satchidanand N Singh R Holmes D Izzo JL . Hypertension and Aging in Rural Haiti: Results From a Preliminary Survey. J Hum Hypertens (2017) 31:138–44. 10.1038/jhh.2016.52
54.
Metz M Pierre JL Yan LD Rouzier V St-Preux S Exantus S et al Hypertension Continuum of Care: Blood Pressure Screening, Diagnosis, Treatment, and Control in a Population-Based Cohort in Haiti. J Clin Hypertens (2022) 24:246–54. 10.1111/jch.14399
55.
Kaur P Rao SR Radhakrishnan E Rajasekar D Gupte MD . Prevalence, Awareness, Treatment, Control and Risk Factors for Hypertension in a Rural Population in South India. Int J Public Health (2012) 57:87–94. 10.1007/s00038-011-0303-3
56.
Yip W Wong TY Jonas JB Zheng Y Lamoureux EL Nangia V et al Prevalence, Awareness, and Control of Hypertension Among Asian Indians Living in Urban Singapore and Rural India. J Hypertens (2013) 31:1539–46. 10.1097/HJH.0b013e328361d52b
57.
Geevar Z Krishnan MN Venugopal K Sanjay G Harikrishnan S Mohanan PP et al Prevalence, Awareness, Treatment, and Control of Hypertension in Young Adults (20–39 Years) in Kerala, South India. Front Cardiovasc Med (2022) 9:765442. 10.3389/fcvm.2022.765442
58.
Banerjee S Mukherjee TK Basu S . Prevalence, Awareness, and Control of Hypertension in the Slums of Kolkata. Indian Heart J (2016) 68:286–94. 10.1016/j.ihj.2015.09.029
59.
Cao Y Sathish T Haregu T Wen Y Mello GT Kapoor N et al Factors Associated With Hypertension Awareness, Treatment, and Control Among Adults in Kerala, India. Front Public Health (2021) 9:753070. 10.3389/fpubh.2021.753070
60.
Janki B Mohan Singh RC Sadhana A . Prevalence, Awareness, Treatment and Control of Hypertension Among the Elderly Residing in Rural Area of Haldwani Block, in Nainital District of Uttarakhand. J Cardiovasc Dis Res (2016) 7:112–5. 10.5530/jcdr.2016.3.3
61.
Karmakar N Nag K Saha I Parthasarathi R Patra M Sinha R . Awareness, Treatment, and Control of Hypertension Among Adult Population in a Rural Community of Singur Block, Hooghly District, West Bengal. J Educ Health Promot (2018) 7:134. 10.4103/jehp.jehp_164_18
62.
Negi PC Chauhan R Rana V Vidyasagar V Lal K . Epidemiological Study of Non-Communicable Diseases (NCD) Risk Factors in Tribal District of Kinnaur, HP: A Cross-Sectional Study. Indian Heart J (2016) 68:655–62. 10.1016/j.ihj.2016.03.002
63.
Thakur JS Nangia R . Prevalence, Awareness, Treatment, and Control of Hypertension and Diabetes: Results From Two State-Wide STEPS Survey in Punjab and Haryana, India. Front Public Health (2022) 10:768471. 10.3389/fpubh.2022.768471
64.
Amarchand R Kulothungan V Krishnan A Mathur P . Hypertension Treatment Cascade in India: Results From National Noncommunicable Disease Monitoring Survey. J Hum Hypertens (2022) 37:394–404. 10.1038/s41371-022-00692-y
65.
Boro B Banerjee S . Decomposing the Rural–Urban Gap in the Prevalence of Undiagnosed, Untreated and Under-Treated Hypertension Among Older Adults in India. BMC Public Health (2022) 22:1310. 10.1186/s12889-022-13664-1
66.
Kothavale A Puri P Sangani PG . Quantifying Population Level Hypertension Care Cascades in India: A Cross-Sectional Analysis of Risk Factors and Disease Linkages. BMC Geriatr (2022) 22:98. 10.1186/s12877-022-02760-x
67.
Lee J Wilkens J Meijer E Sekher TV Bloom DE Hu P . Hypertension Awareness, Treatment, and Control and Their Association With Healthcare Access in the Middle-Aged and Older Indian Population: A Nationwide Cohort Study. PLOS Med (2022) 19:e1003855. 10.1371/journal.pmed.1003855
68.
Maheshwari A Verma N Bhardwaj S Jose AP Bhalla S More A et al May Measurement Month 2018: An Analysis of Blood Pressure Screening Campaign Results in India. Eur Heart J Suppl (2020) 22:H62–5. 10.1093/eurheartj/suaa030
69.
Saju MD Allagh KP Scaria L Joseph S Thiyagarajan JA . Prevalence, Awareness, Treatment, and Control of Hypertension and Its Associated Risk Factors: Results From Baseline Survey of SWADES Family Cohort Study. Int J Hypertens (2020) 2020:4964835–7. 10.1155/2020/4964835
70.
Saxena V Kalyani V Kodi SM Dhar M Verma A Senkadhirdasan, et al Control of Blood Pressure in District Dehradun, India: Is Rule of Halves Still Valid? Indian J Public Health Res Dev (2021). 10.37506/ijphrd.v12i3.16122
71.
Patil M Jose AP More A Maheshwari A Verma N Shah R et al May Measurement Month 2019: An Analysis of Blood Pressure Screening Results From India. Eur Heart J Suppl (2021) 23:B73–6. 10.1093/eurheartj/suab047
72.
Maniyara K Kodali PB Thankappan KR . Prevalence, Awareness, Treatment, Control and Correlates of Prevalence and Control of Hypertension Among Older Adults in Kerala: A Mixed Methods Study. Indian Heart J (2023) 75:185–9. 10.1016/j.ihj.2023.03.004
73.
Prashanth HL Chandrashekar S Madhusudhana M . Hypertension in Young Adults - an Urban and Rural Comparative Study. Indian J Public Health Res Dev (2013) 4:168. 10.5958/j.0976-5506.4.4.166
74.
Singh S Shankar R Singh GP . Prevalence and Associated Risk Factors of Hypertension: A Cross-Sectional Study in Urban Varanasi. Int J Hypertens (2017) 2017:5491838–10. 10.1155/2017/5491838
75.
Geldsetzer P Tan MM Dewi F Quyen B Juvekar S Hanifi S et al Hypertension Care in Demographic Surveillance Sites: A Cross-Sectional Study in Bangladesh, India, Indonesia, Malaysia, Viet Nam. Bull World Health Organ (2022) 100:601–9. 10.2471/BLT.22.287807
76.
Malekzadeh MM Etemadi A Kamangar F Khademi H Golozar A Islami F et al Prevalence, Awareness and Risk Factors of Hypertension in a Large Cohort of Iranian Adult Population. J Hypertens (2013) 31:1364–71. 10.1097/HJH.0b013e3283613053
77.
Esteghamati A Etemad K Koohpayehzadeh J Abbasi M Meysamie A Khajeh E et al Awareness, Treatment and Control of Pre-Hypertension and Hypertension Among Adults in Iran. Arch Iran Med (2016) 19:456–64. 10.1186/s12889-020-08831-1
78.
Eghbali M Khosravi A Feizi A Mansouri A Mahaki B Sarrafzadegan N . Prevalence, Awareness, Treatment, Control, and Risk Factors of Hypertension Among Adults: A Cross-Sectional Study in Iran. Epidemiol Health (2018) 40:e2018020. 10.4178/epih.e2018020
79.
Mirzaei M Mirzaei M Bagheri B Dehghani A . Awareness, Treatment, and Control of Hypertension and Related Factors in Adult Iranian Population. BMC Public Health (2020) 20:667. 10.1186/s12889-020-08831-1
80.
Rajati F Hamzeh B Pasdar Y Safari R Moradinazar M Shakiba E et al Prevalence, Awareness, Treatment, and Control of Hypertension and Their Determinants: Results From the First Cohort of Non-Communicable Diseases in a Kurdish Settlement. Sci Rep (2019) 9:12409. 10.1038/s41598-019-48232-y
81.
Nikparvar M Farshidi H Madani A Rad RE Azad M Eftekhaari TE et al Prevalence, Awareness, Treatment, and Control of Hypertension in Hormozgan Province, Iran. Int Cardiovasc Res J (2019) 13:1.
82.
Oraii A Shafiee A Jalali A Alaeddini F Saadat S Sadeghian S et al Prevalence, Awareness, Treatment, and Control of Hypertension Among Adult Residents of Tehran: The Tehran Cohort Study. Glob Heart (2022) 17:31. 10.5334/gh.1120
83.
Mohamed SF Mutua MK Wamai R Wekesah F Haregu T Juma P et al Prevalence, Awareness, Treatment and Control of Hypertension and Their Determinants: Results From a National Survey in Kenya. BMC Public Health (2018) 18:1219. 10.1186/s12889-018-6052-y
84.
Mirrakhimov E Zakirov U Abilova S Asanbaev A Bektasheva E Asanaliev N et al May Measurement Month 2019: Analysis of Blood Pressure Screening in Bishkek, Kyrgyzstan. Eur Heart J Suppl (2022) 24:F19–21. 10.1093/eurheartjsupp/suac042
85.
Pengpid S Vonglokham M Kounnavong S Sychareun V Peltzer K . The Prevalence, Awareness, Treatment, and Control of Hypertension Among Adults: The First Cross-Sectional National Population-Based Survey in Laos. Vasc Health Risk Manag (2019) 15:27–33. 10.2147/VHRM.S199178
86.
Ndhlovu HLL Masiye JK Chirwa ML Nyirenda NM Dhlamini TD Beaney T et al May Measurement Month 2018: An Analysis of Blood Pressure Screening Results From Malawi. Eur Heart J Suppl (2020) 22:H80–2. 10.1093/eurheartj/suaa034
87.
Ndhlovu HLL Chirwa ML Mbeba MK Nyirenda NM Mbulaje LD Beaney T et al May Measurement Month 2019: An Analysis of Blood Pressure Screening Results From Malawi. Eur Heart J Suppl (2021) 23:B95–7. 10.1093/eurheartj/suab041
88.
Pengpid S Peltzer K . National Trends in Prevalence, Awareness, Treatment, and Control of Hypertension Among Adults in Mongolia From 4 Cross-Sectional Surveys in 2005, 2009, 2013, and 2019. Medicine (Baltimore) (2022) 101:e30140. 10.1097/MD.0000000000030140
89.
Potts H Baatarsuren U Myanganbayar M Purevdorj B Lkhagvadorj B Ganbat N et al Hypertension Prevalence and Control in Ulaanbaatar, Mongolia. J Clin Hypertens (2020) 22:103–10. 10.1111/jch.13784
90.
Zaw KK Latt TS Aung PP Thwin TG Myint TK . Prevalence of Hypertension and Its Associated Factors in the Adult Population in Yangon Division, Myanmar. Asia Pac J Public Health (2011) 23:496–506. 10.1177/1010539509349147
91.
Neupane D Shrestha A Mishra SR Bloch J Christensen B McLachlan CS et al Awareness, Prevalence, Treatment, and Control of Hypertension in Western Nepal. Am J Hypertens (2017) 30:907–13. 10.1093/ajh/hpx074
92.
Karmacharya BM Koju RP LoGerfo JP Chan KCG Mokdad AH Shrestha A et al Awareness, Treatment and Control of Hypertension in Nepal: Findings From the Dhulikhel Heart Study. Heart Asia (2017) 9:1–8. 10.1136/heartasia-2016-010766
93.
Khanal MK Dhungana RR Bhandari P Gurung Y Paudel KN . Prevalence, Associated Factors, Awareness, Treatment, and Control of Hypertension: Findings From a Cross Sectional Study Conducted as a Part of a Community Based Intervention Trial in Surkhet, Mid-Western Region of Nepal. PLOS ONE (2017) 12:e0185806. 10.1371/journal.pone.0185806
94.
Adhikari TB Bhattarai H Ranabhat K Khanal P Mishra SR Koirala S et al May Measurement Month 2018: An Analysis of Blood Pressure Screening Results From Nepal. Eur Heart J Suppl (2020) 22:H92–5. 10.1093/eurheartj/suaa037
95.
Bhattarai H McLachlan CS Khanal P Adhikari TB Ranabhat K Koirala S et al May Measurement Month 2019: An Analysis of Blood Pressure Screening Results From Nepal. Eur Heart J Suppl (2021) 23:B110–3. 10.1093/eurheartj/suab042
96.
Valladares MJ Rodríguez Sándigo NA Rizo Rivera GO Rodríguez Jarquín MA Rivera Castillo RM López Bonilla IM . Prevalence, Awareness, Treatment, and Control of Hypertension in a Small Northern Town in Nicaragua: The Elieth-HIFARI Study. Health Sci Rep (2019) 2:e120. 10.1002/hsr2.120
97.
Wahab KW Kolo PM Sani MU Okubadejo NU Peter JO Aigbe F et al May Measurement Month 2018: An Analysis of Blood Pressure Screening Results From Nigeria. Eur Heart J Suppl (2020) 22:H96–9. 10.1093/eurheartj/suaa038
98.
Wahab KW Kolo PM Odili A Iwuozo E Ifebunandu N Ademiluyi B et al May Measurement Month 2019: An Analysis of Blood Pressure Screening Results From Nigeria. Eur Heart J Suppl (2021) 23:B114–6. 10.1093/eurheartj/suab059
99.
Obagha CE Danladi B Kamateeka M Chori BS Ogbonnaya U Maduka D et al Unmet Needs of Hypertension Care in Nigeria: Results of the Community Action Against Non-Communicable Diseases (COMAAND) Project Preintervention Survey. Blood Press Monit (2022) 27:27–32. 10.1097/MBP.0000000000000561
100.
Shafi ST Shafi T . A Survey of Hypertension Prevalence, Awareness, Treatment, and Control in Health Screening Camps of Rural Central Punjab, Pakistan. J Epidemiol Glob Health (2017) 7:135–40. 10.1016/j.jegh.2017.01.001
101.
Memon FS Wang W Beaney T Bai K Poulter NR Ishaq M . May Measurement Month 2018: An Analysis of Blood Pressure Screening Results From Pakistan. Eur Heart J Suppl (2022) 24:F31–3. 10.1093/eurheartjsupp/suac034
102.
Castillo RR Mercado-Asis LB Atilano AA David-Ona DI Diaz AF Granada CN et al May Measurement Month 2018: An Analysis of Blood Pressure Screening in the Philippines. Eur Heart J Suppl (2020) 22:H104–7. 10.1093/eurheartj/suaa040
103.
Diaz ABF David-Ona DI Mercado-Asis LB Atilano AA Vilela GC Bonzon DD et al May Measurement Month 2019: An Analysis of Blood Pressure Screening Results in the Philippines. Eur Heart J Suppl (2021) 23:B120–3. 10.1093/eurheartj/suab061
104.
LaMonica LC McGarvey ST Rivara AC Sweetman CA Naseri T Reupena MS et al Cascades of Diabetes and Hypertension Care in Samoa: Identifying Gaps in the Diagnosis, Treatment, and Control Continuum – A Cross-Sectional Study. Lancet Reg Health - West Pac (2022) 18:100313. 10.1016/j.lanwpc.2021.100313
105.
Duboz P Boëtsch G Gueye L Macia E . Hypertension Prevalence, Awareness, Treatment and Control in Dakar (Senegal). J Hum Hypertens (2014) 28:489–93. 10.1038/jhh.2013.142
106.
Duboz P Boëtsch G Gueye L Macia E . Hypertension in the Ferlo (Northern Senegal): Prevalence, Awareness, Treatment and Control. Pan Afr Med J (2016) 25:177. 10.11604/pamj.2016.25.177.10105
107.
Geraedts TJM Boateng D Lindenbergh KC Delft D Mathéron HM Mönnink GLE et al Evaluating the Cascade of Care for Hypertension in Sierra Leone. Trop Med Int Health (2021) 26:1470–80. 10.1111/tmi.13664
108.
Beheiry HM Abdalla AA Fahal NA Mohamed MI Ibrahim DA Medani SA et al May Measurement Month 2018: An Analysis of Blood Pressure Screening Results From Sudan. Eur Heart J Suppl (2020) 22:H122–4. 10.1093/eurheartj/suaa045
109.
Muhamedhussein MS Nagri ZI Manji KP . Prevalence, Risk Factors, Awareness, and Treatment and Control of Hypertension in Mafia Island, Tanzania. Int J Hypertens (2016) 2016:1281384–5. 10.1155/2016/1281384
110.
Osetinsky B Mhalu G Mtenga S Tediosi F . Care Cascades for Hypertension and Diabetes: Cross-Sectional Evaluation of Rural Districts in Tanzania. Plos Med (2022) 19:e1004140–17. 10.1371/journal.pmed.1004140
111.
Muhihi AJ Anaeli A Mpembeni RNM Sunguya BF Leyna G Kakoko D et al Prevalence, Awareness, Treatment, and Control of Hypertension Among Young and Middle-Aged Adults: Results From a Community-Based Survey in Rural Tanzania. Int J Hypertens (2020) 2020:9032476–13. 10.1155/2020/9032476
112.
Ben Romdhane H Ben Ali S Skhiri H Traissac P Bougatef S Maire B et al Hypertension Among Tunisian Adults: Results of the TAHINA Project. Hypertens Res (2012) 35:341–7. 10.1038/hr.2011.198
113.
Boujnah R Nazek L Maalej M Achhab YE Nejjari C . Hypertension in Tunisian Adults Attending Primary Care Physicians (ETHNA-Tunisia). Indian Heart J (2018) 70:544–7. 10.1016/j.ihj.2017.11.005
114.
Haj Amor S Beaney T Saidi O Clarke J Poulter NR Ben Alaya N et al May Measurement Month 2019: An Analysis of Blood Pressure Screening Results From Tunisia. Eur Heart J Suppl (2021) 23:B144–6. 10.1093/eurheartj/suab032
115.
Son PT Quang NN Viet NL Khai PG Wall S Weinehall L et al Prevalence, Awareness, Treatment and Control of Hypertension in Vietnam—Results From a National Survey. J Hum Hypertens (2012) 26:268–80. 10.1038/jhh.2011.18
116.
Ha DA Goldberg RJ Allison JJ Chu TH Nguyen HL . Prevalence, Awareness, Treatment, and Control of High Blood Pressure: A Population-Based Survey in Thai Nguyen, Vietnam. PLoS ONE (2013) 8:e66792. 10.1371/journal.pone.0066792
117.
Hien HA Tam NM Tam V Derese A Devroey D . Prevalence, Awareness, Treatment, and Control of Hypertension and Its Risk Factors in (Central) Vietnam. Int J Hypertens (2018) 2018:6326984–12. 10.1155/2018/6326984
118.
Van Minh H Lan Viet N Sinh CT Hung PN Ngoc NTM Van Hung N et al May Measurement Month 2018: An Analysis of Blood Pressure Screening Results From Vietnam. Eur Heart J Suppl (2020) 22:H139–41. 10.1093/eurheartj/suaa049
119.
Minh HV Poulter NR Viet NL Sinh CT Hung PN Ngoc NTM et al Blood Pressure Screening Results From May Measurement Month 2019 in Vietnam. Eur Heart J Suppl (2021) 23:B154–7. 10.1093/eurheartj/suab035
120.
Abu Hamad BA Jamaluddine Z Safadi G Ragi ME Ahmad RES Vamos EP et al The Hypertension Cascade of Care in the Midst of Conflict: The Case of the Gaza Strip. J Hum Hypertens (2022) 37:957–68. 10.1038/s41371-022-00783-w
121.
Goma F Syatalimi C Tembo P Mukupa M Chikopela T Kaluba L et al May Measurement Month 2019: An Analysis of Blood Pressure Screening Results From Zambia. Eur Heart J Suppl (2021) 23:B158–60. 10.1093/eurheartj/suab043
122.
Zhou B Danaei G Stevens GA Bixby H Taddei C Carrillo-Larco RM et al Long-Term and Recent Trends in Hypertension Awareness, Treatment, and Control in 12 High-Income Countries: An Analysis of 123 Nationally Representative Surveys. The Lancet (2019) 394:639–51. 10.1016/S0140-6736(19)31145-6
123.
Marmot M Bell R . Social Determinants and Non-Communicable Diseases: Time for Integrated Action. BMJ (2019) 364:l251. 10.1136/bmj.l251
124.
World Health Organization. World Health Statistics 2018: Monitoring Health for the SDGs, Sustainable Development Goals. Geneva, Switzerland: World Health Organization (2018).
125.
Geldsetzer P Manne-Goehler J Marcus ME Ebert C Zhumadilov Z Wesseh CS et al The State of Hypertension Care in 44 the State of Hypertension Care in 44 Low-Income and Middle-Income Countries: A Cross-Sectional Study of Nationally Representative Individual-Level Data From 1·1 Million Adults. The Lancet (2019) 394:652–62. 10.1016/S0140-6736(19)30955-9
126.
Chimbindi N Bor J Newell ML Tanser F Baltusen R Hontelez J et al Time and Money: The True Costs of Health Care Utilization for Patients Receiving "Free" HIV/Tuberculosis Care and Treatment in Rural KwaZulu-Natal. J Acquir Immune Defic Syndr (2015) 70:e52–60. 10.1097/QAI.0000000000000728
127.
Kohli-Lynch CN Erzse A Rayner BL Hofman KJ . Hypertension in the South African Public Healthcare System: A Cost-of-Illness and Burden of Disease Study. BMJ Open (2022) 12:e055621. 10.1136/bmjopen-2021-055621
128.
Mills KT Stefanescu A He J . The Global Epidemiology of Hypertension. Nat Rev Nephrol (2020) 16:223–37. 10.1038/s41581-019-0244-2
129.
Kostova D Spencer G Moran AE Cobb LK Husain MJ Datta BK et al The Cost-Effectiveness of Hypertension Management in Low-Income and the Cost-Effectiveness of Hypertension Management in Low-Income and Middle-Income Countries: A review. BMJ Glob Health (2020) 5:e002213. 10.1136/bmjgh-2019-002213
130.
Leslie HH Malata A Ndiaye Y Kruk ME . Effective Coverage of Primary Care Services in Eight High-Mortality Countries. BMJ Glob Health (2017) 2:e000424. 10.1136/bmjgh-2017-000424
131.
Nowak NA Rimmasch H Kirby A Kellogg C . Right Care, Right Time, Right Place, Every Time. Healthc Financ Manag J Healthc Financ Manag Assoc (2012) 66:82–8.
132.
Peters MA Noonan CM Rao KD Edward A Alonge OO . Evidence for an Expanded Hypertension Care Cascade in Low- and Middle-Income Countries: A Scoping Review. BMC Health Serv Res (2022) 22:827. 10.1186/s12913-022-08190-0
133.
Khoiry QA Alfian SD Abdulah R . Modifiable and Non-Modifiable Factors Associated With Low Awareness of Hypertension Treatment in Indonesia: A Cross-Sectional Population-Based National Survey. Glob Heart (2022) 17:56. 10.5334/gh.1143
134.
Mashuri YA Ng N Santosa A . Socioeconomic Disparities in the Burden of Hypertension Among Indonesian Adults - a Multilevel Analysis. Glob Health Action (2022) 15:2129131. 10.1080/16549716.2022.2129131
135.
Falaschetti E Mindell J Knott C Poulter N . Hypertension Management in England: A Serial Cross-Sectional Study From 1994 to 2011. Lancet Lond Engl (2014) 383:1912–9. 10.1016/S0140-6736(14)60688-7
Summary
Keywords
hypertension (HTN), care cascade, low income country (LIC), lower-middle income country (LMIC), prevalence
Citation
Lamloum D, Fassio F, Osetinsky B and Tediosi F (2023) Care Cascades for Hypertension in Low-Income Settings: A Systematic Review and Meta-Analysis. Int J Public Health 68:1606428. doi: 10.3389/ijph.2023.1606428
Received
21 July 2023
Accepted
28 September 2023
Published
12 October 2023
Volume
68 - 2023
Edited by
Rajesh Kumar Rai, Society for Health and Demographic Surveillance, India
Reviewed by
Biju Soman, Sree Chitra Tirunal Institute for Medical Sciences and Technology (SCTIMST), India
Updates
Copyright
© 2023 Lamloum, Fassio, Osetinsky and Tediosi.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Demetrio Lamloum, demetrio.lamloum@master.sdabocconi.it; Federico Fassio, federico.fassio01@universitadipavia.it
†These authors have contributed equally to this work
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.