- 1Scientific Research Division, Eye & ENT Hospital, Shanghai, China
- 2Otolaryngology Research Institute, Eye & ENT Hospital, Shanghai, China
- 3NHC Key Laboratory of Hearing Medicine, Fudan University, Shanghai, China
- 4Department of Otolaryngology Head and Neck Surgery, The Second Affiliated, Hospital of Anhui Medical University, Hefei, China
- 5Clinical Research Unit of Eye & ENT Hospital, Fudan University, Shanghai, China
- 6No. 2 High School of East China Normal University, Shanghai, China
- 7School of Public Health, Fudan University, Shanghai, China
- 8Medical Dean’s Reception Office, Fudan University, Shanghai, China
- 9State Key Laboratory of Medical Neurobiology, Fudan University, Shanghai, China
Objective: This study aimed to investigate the clinical characteristics and outcomes of ear-nose-throat (ENT) symptoms in SARS-CoV-2 Omicron infected patients resulting from local transmission.
Methods: A convenience sampling network survey was conducted among individuals infected with SARS-CoV-2 to examine the characteristics and progression of ENT symptoms associated with local transmission. The survey comprised 52 questions, and univariable and multivariable logistic regression analyses were employed to assess the rate, severity, and outcome of ENT symptoms across different genders and age groups.
Results: Among the 1,366 individuals included in the investigation, a peak in new infections occurred on 20th December, and the majority (78.4%) were female. The most common symptoms reported were coughing (90.6%), nasal congestion (77.2%), and runny nose (74.3%). Otologic symptoms were predominantly represented by tinnitus (29.7%).
Conclusion: The rate of specific symptoms showed a significant correlation with age and gender. It is crucial to provide timely medical intervention, especially for female patients. This study offers a comprehensive understanding of the symptom spectrum in individuals infected with the virus, providing valuable insights for the development of targeted symptom management strategies.
Introduction
The COVID-19 pandemic is a global outbreak of coronavirus, an infectious disease caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus. As of 12 April 2023, the global impact of COVID-19 has been immense, with over 762 million confirmed cases and nearly 6.9 million deaths [1]. In China, after 3 years of implementing the “dynamic zero” policy, the country’s COVID-19 prevention and control measures have been gradually adjusted. The State Council Joint Prevention and Control Mechanism released the “Notice on Further Optimizing the Scientific and Accurate Prevention and Control of COVID-19” on 11 November 2022, prompting corresponding actions by the Shanghai Municipal Health Commission. Measures such as scaling back large-scale nucleic acid testing (NAT), modifying home isolation strategies, and suspending close contact tracing were promptly implemented. Surveillance data from 25 January 2023, revealed a widespread transmission of SARS-CoV-2 Omicron nationwide, with two sub-variants (BA.5.2 and BF.7) of the Omicron BA.5 variant dominating the current epidemic [2].
Previous studies have indicated that the Omicron BA.5 variant exhibits increased transmissibility and immune evasion capabilities, potentially impacting the host’s immune response and vaccine effectiveness when compared to other variants [3]. However, this variant primarily affects the upper respiratory tract, and the risk of developing pneumonia or severe illness may be lower compared to influenza. Common symptoms of COVID-19 include fever, cough, and fatigue [4], while sore throat and loss of smell are frequently observed in the ear, nose, and throat (ENT) manifestations of the disease [5]. Although fewer cases of hearing loss, tinnitus, vertigo, and related symptoms have been reported in confirmed COVID-19 patients [6, 7], research suggests that these conditions could be potential long-term consequences of the infection, leading to reduced quality of life and negative impacts on communication and daily activities [8–10]. Studies have identified angiotensin-converting enzyme 2 (ACE-2) receptors, which the SARS-CoV-2 virus attaches to, in various regions of the middle and inner ear, including middle ear tissues, the eustachian tube, hair cells in Corti’s organ, vascular striae, and spiral ganglion cells in mouse tissues [11]. Additionally, SARS-CoV-2 viral particles have been detected in the mastoid and middle ear of deceased individuals infected with the virus [12]. Although some individuals infected with COVID-19 do not experience hearing loss, studies have suggested that the infection may have detrimental effects on the outer hair cells in the cochlea [13, 14].
Taste and smell disturbances are common early symptoms of coronavirus infections and often present as initial or solitary symptoms [15–17]. Given the widespread and rapid spread of SARS-CoV-2 infection, it is crucial to comprehensively understand its range of clinical manifestations. However, specific guidelines for managing patients with persistent taste and smell disorders, vertigo, hearing loss, or tinnitus are currently lacking. The treatment of otolaryngological consequences resulting from COVID-19 will continue to be an important issue in the coming years. Further investigation into these symptoms can provide valuable insights for both short-term and long-term management of similar patients.
To elucidate the clinical features and progression of infection, establish a foundation for improving the symptom spectrum of Omicron variant-infected patients, and offer guidance for targeted improvement strategies, we conducted a network survey of individuals infected with SARS-CoV-2 Omicron using convenience sampling.
Methods
Study Population
The study enrolled individuals who had been confirmed as infected with SARS-CoV-2 Omicron through nucleic acid amplification testing or rapid antigen testing between 1 December 2022 and 31 January 2023.
To ensure the reliability of the data, certain exclusion criteria were applied. Individuals who were unable to provide truthful information, those who omitted important details or exhibited clear logical errors regarding their gender, age, height, weight, or infection date, and those who submitted duplicate information were excluded from the study. The questionnaire survey was conducted nationwide from 19 January 2023, to 11 February 2023. Ethical considerations were strictly followed, in accordance with the Measures for the Ethical Review of Biomedical Research Involving Humans of the National Health Commission of the People’s Republic of China. The research protocol received ethical approval from the Eye and ENT Hospital Ethics Panel at Fudan University (Approval No. 2022127) for international data collection.
Primary Outcomes
ENT Symptoms
This study aimed to assess the prevalence of various symptoms including hearing loss, tinnitus, stuffiness, earache, vertigo, nasal obstruction, rhinorrhea, sense of smell, cough, sore throat, and reduced sense of taste. Participants were requested to rate the impact of each symptom on their daily life using a scale from 0 (no impact) to 10 (extreme impact) to determine the severity of each symptom. Additionally, participants were asked to report the outcome of each symptom, categorizing it as untreated and self-healed, completely improved after treatment, partially improved after treatment, or residual symptoms. Furthermore, the study examined the medical treatment sought for ENT-related symptoms to evaluate the medical demand associated with the occurrence of these symptoms.
Medical History
The study also examined pre-existing medical conditions related to the ear, nose, and throat (ENT) including tinnitus, otitis media, rhinitis, and pharyngitis, prior to the onset of the new coronavirus infection.
Content and Methods of the Study
The questionnaire was collaboratively developed by two experienced doctors specializing in otolaryngology and public health. It consisted of eight sections, namely: informed consent, basic patient information, date of SARS-CoV-2 infection, ENT symptoms and outcomes, sleep quality, mental health status post-infection, pre-existing ENT medical history, and underlying medical conditions. In total, the questionnaire comprised 52 questions, utilizing formats such as single-choice, multiple-choice, and self-filling. For more detailed content of the questionnaire, please refer to the following link: [18] (Supplementary Material S1).
This study employed a cross-sectional research design and utilized convenience sampling to recruit participants. Data collection was carried out through self-administration of electronic questionnaires. We also made efforts to distribute the survey through various online platforms such as Weibo and WeChat. Within the questionnaire, all self-evaluated items concerning the impact of symptoms on daily life were rated on a scale of 0–10, with higher scores indicating a greater severity of impact.
Statistical Analysis
The statistical analysis and data visualization were performed using R software version 4.2.2. Metric data that followed a normal distribution were presented as
Results
Basic Information
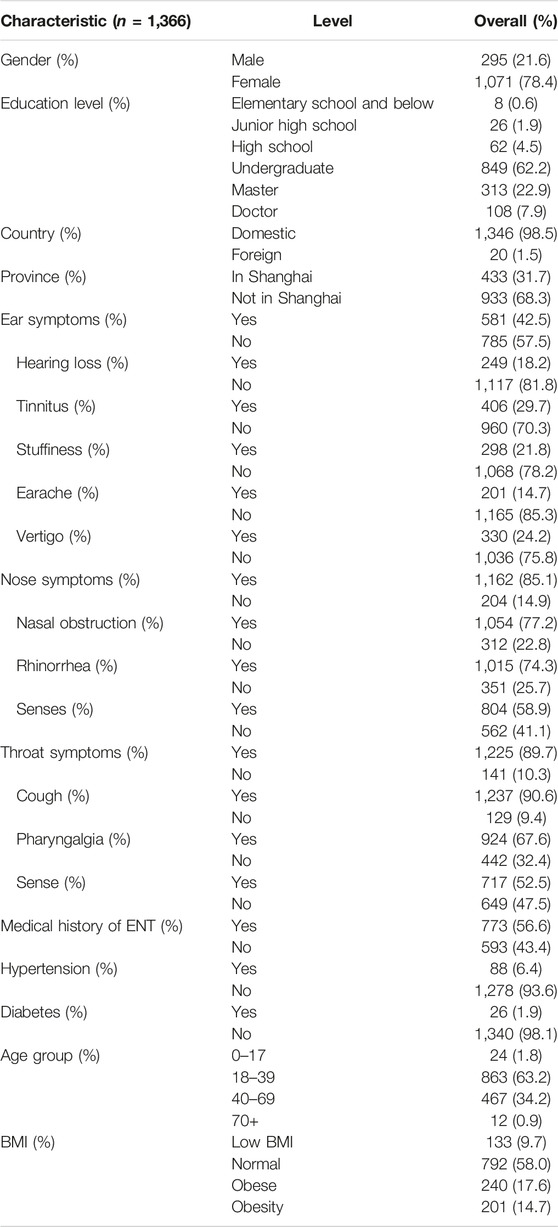
A total of 1,366 individuals participated in the questionnaire, out of which 433 (31.7%) resided in Shanghai, and 20 (1.5%) were located outside mainland China. The remaining participants were distributed across various provinces in China. Figure 1A illustrates the trend of newly infected cases investigated, demonstrating a rapid increase since December 1st, with a peak of 109 infections on 20th December. Subsequently, the number fluctuated and declined, with minimal newly identified cases reported after 15th January. It is worth noting that considering the presence of the incubation period and testing delays, the trend of newly infected individuals obtained from the investigation aligns with the changes in the nucleic acid detection rate reported by the CDC. This suggests a relatively high reliability of the investigation [2].
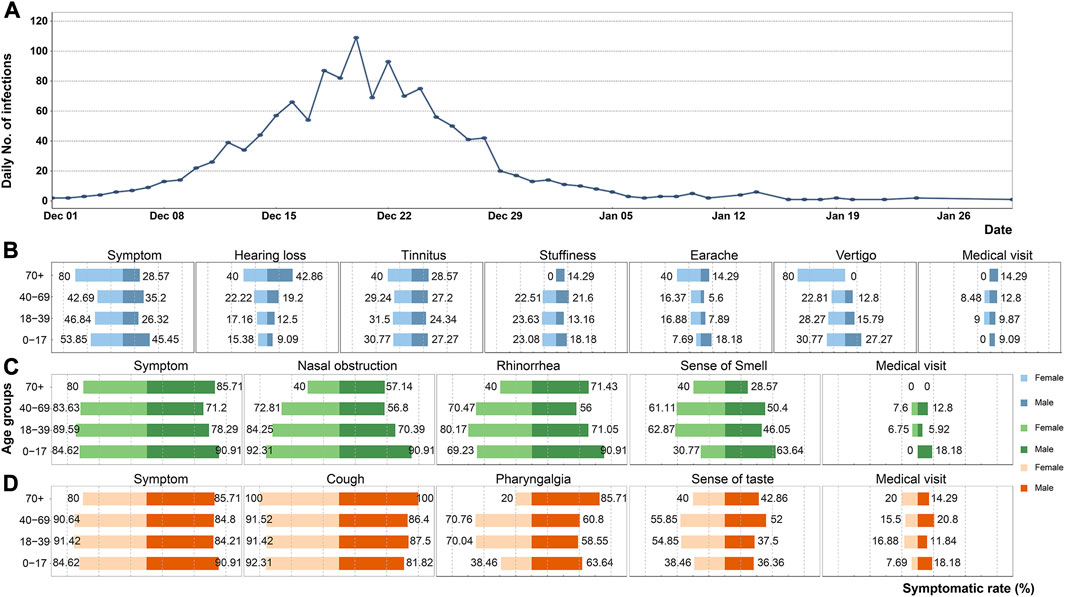
FIGURE 1. Statistical graphs of related results in the survey (China, 2023). (A) Temporal changes of the investigated daily number of infections. (B) Symptomatic rate of otologic symptoms stratified by age and gender. (C) Symptomatic rate of nasal symptoms stratified by age and gender. (D) Symptomatic rate of throat symptoms stratified by age and gender.
Among the 1,366 infected individuals, 1,071 (78.4%) were female. Common symptoms related to the nose and throat were observed, as the Omicron infection primarily affects the upper respiratory tract. Specifically, 1,054 (77.2%) individuals experienced some degree of nasal obstruction, and 1,015 (74.3%) reported rhinorrhea. In terms of otologic symptoms, tinnitus (29.7%) and vertigo (24.2%) were the most prevalent. It is worth noting that a minority of patients had a history of hypertension or diabetes, while 773 (56.6%) individuals had a history of ENT disease. Additional demographic data and the rates of symptomatic manifestations are provided in Table 1.
Symptomatic Rate and Outcome of Otologic Symptoms
In terms of otologic symptoms, we observed a higher rate of symptoms among female individuals. This higher rate was particularly notable for symptoms such as stuffiness, earache, and vertigo. Additionally, females appeared to be at a greater risk in terms of the impact of otologic symptoms on their daily lives and the progression of symptoms.
When considering age groups, the rate of hearing loss symptoms increased with age, as shown in Table 2. The rate of tinnitus symptoms, on the other hand, was similar across all age groups, as depicted in Figure 1B. Earache and vertigo were more commonly observed in individuals over the age of 70. Among females in this age group, four individuals (80.0%) reported experiencing vertigo, whereas no males over 70 reported vertigo symptoms, as shown in Figure 1B.
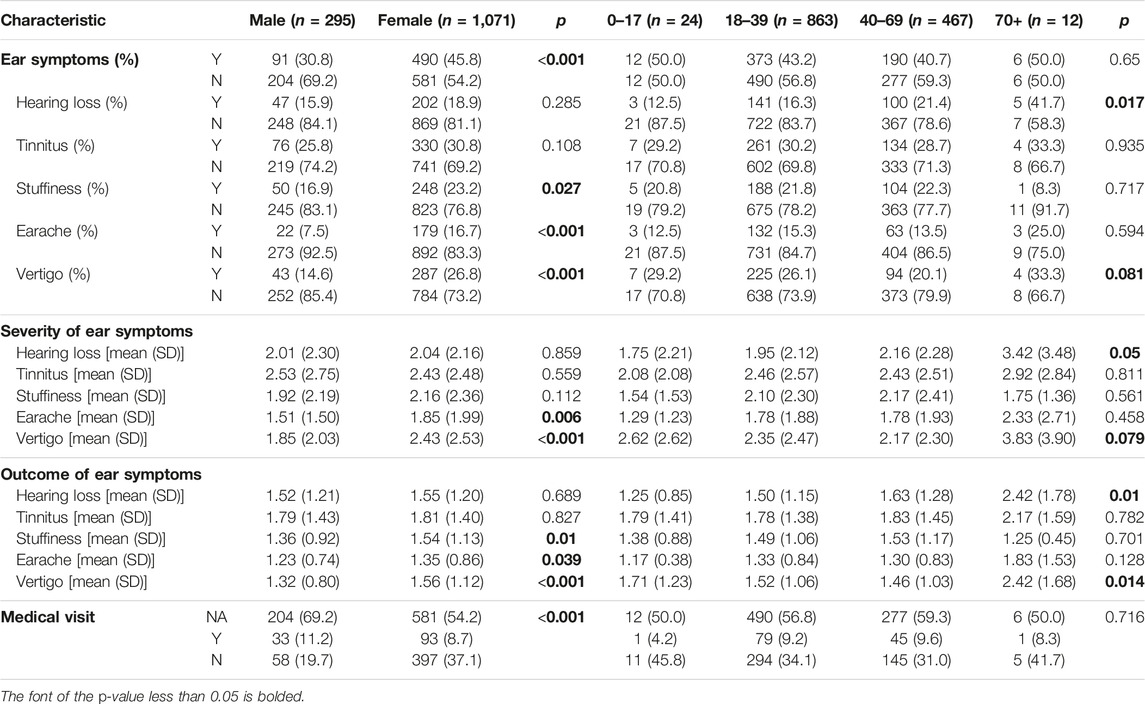
TABLE 2. The symptomatic rate, severity and outcome of otologic symptoms among different genders and age groups (China, 2023).
Apart from the symptomatic rate, similar patterns were observed in terms of the impact on daily life and symptom progression. Overall, the impact of otologic symptoms on patients’ lives was relatively minor, but tinnitus had a more common and severe impact compared to other symptoms, as indicated in Table 2. Furthermore, earache and vertigo had a greater impact on females. A few patients sought medical attention after experiencing otologic symptoms related to COVID-19. In most cases, these symptoms improved or partially improved after treatment, while tinnitus and hearing loss were common residual symptoms, as depicted in Figures 2A, B.
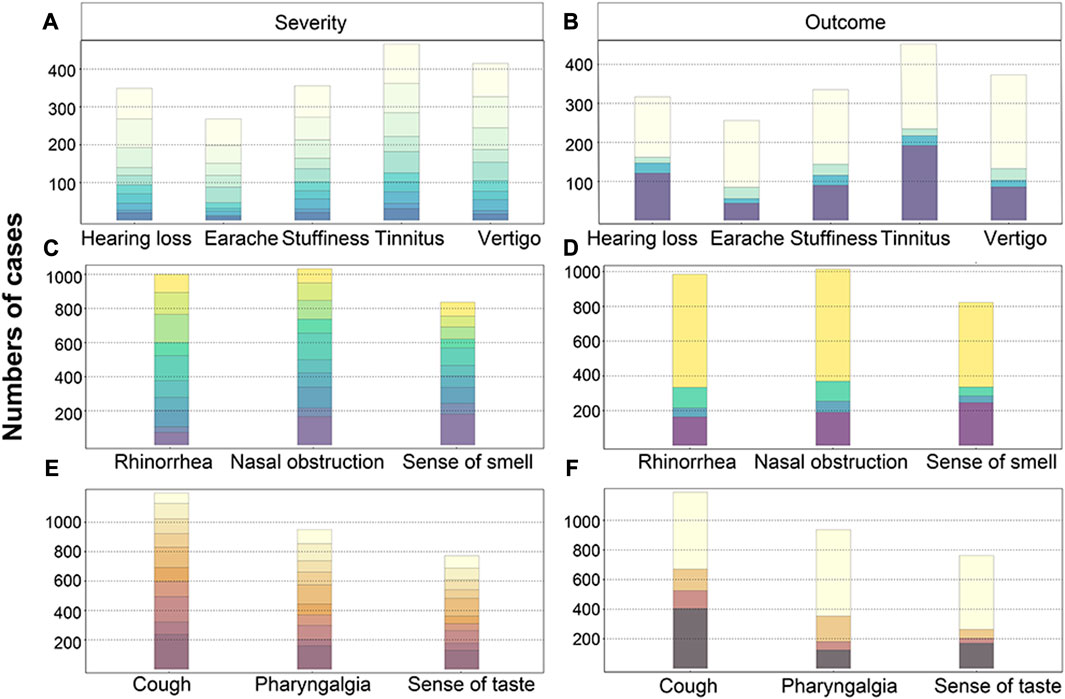
FIGURE 2. Distribution of severity (A,C,E) and outcomes (B,D,F) of otolaryngological symptoms . The number of cases with varying scores of severities for ENT symptoms, including the otologic (A), nasal (C), and throat (E) symptoms. The number of cases with differing outcomes for otologic (B), nasal (D), and throat (F) symptoms. Note: The scores are represented by different colors, ranging from 1 to 10. Lighter shades indicate lower scores, while darker shades indicate higher scores. The vertical axis represents the number of cases (China, 2023).
The impact of BMI on otologic symptoms was found to be insignificant, with only a higher rate of ear pain observed in underweight individuals, as shown in Supplementary Table S1.
Symptomatic Rate and Outcome of Nasal Symptoms
Nasal obstruction, rhinorrhea, and loss of smell had a significant impact on the daily lives of patients, as indicated in Table 3. Nearly half of the patients rated the impact of nasal symptoms as moderate to severe, with scores ranging from 4 to 10, as shown in Figure 2C. The symptomatic rate of rhinologic symptoms was generally higher among female cases, and these symptoms had a more severe impact and progression. Nasal obstruction, rhinorrhea, and other nasal symptoms were observed across all age groups, with a higher symptomatic rate among younger individuals. In fact, the symptomatic rate of nasal obstruction in children exceeded 90%, as depicted in Figure 1C. However, the impact and progression of symptoms were less severe compared to the middle-aged group.
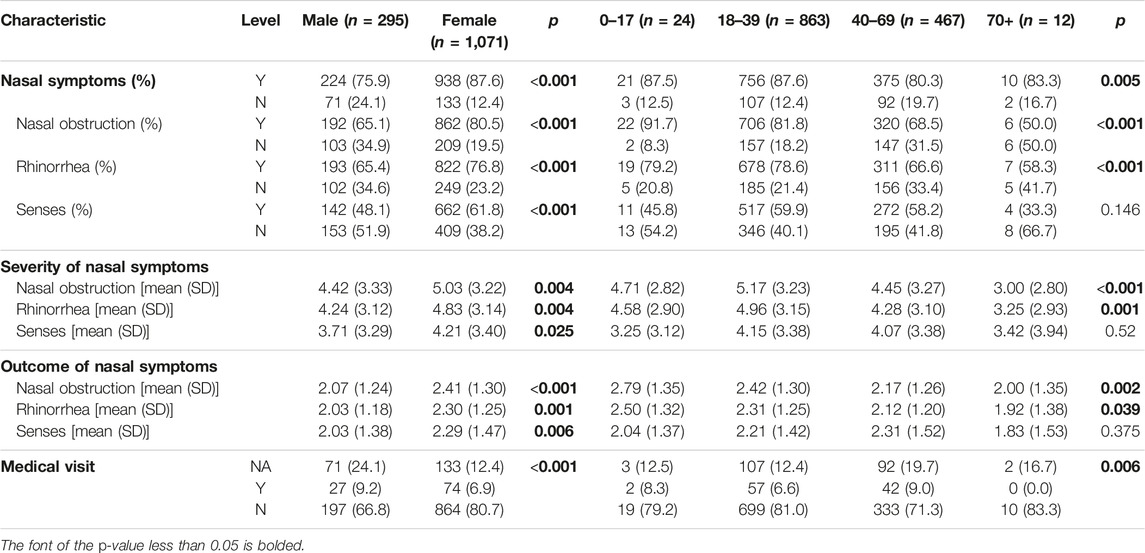
TABLE 3. The symptomatic rate, severity and outcome of nasal symptoms among different genders and age groups (China, 2023).
Few patients sought treatment specifically for rhinologic symptoms. The results indicated a low short-term spontaneous recovery rate for the loss of sense of smell, but few patients reported residual symptoms, as shown in Figures 2C, D. The impact of BMI on rhinologic symptoms was found to be insignificant, as demonstrated in Supplementary Table S2. However, there was a trend of more severe progression of nasal obstruction in underweight individuals.
Symptomatic Rate and Outcome of Throat Symptoms
Throat symptoms were highly prevalent among individuals infected with SARS-CoV-2, with rates exceeding 80%. Similar to ear and nose symptoms, female individuals exhibited higher rates of symptomatic presentations, while no clear association was observed between age (Table 4) or BMI (Supplementary Table S3) and symptomatic rates.
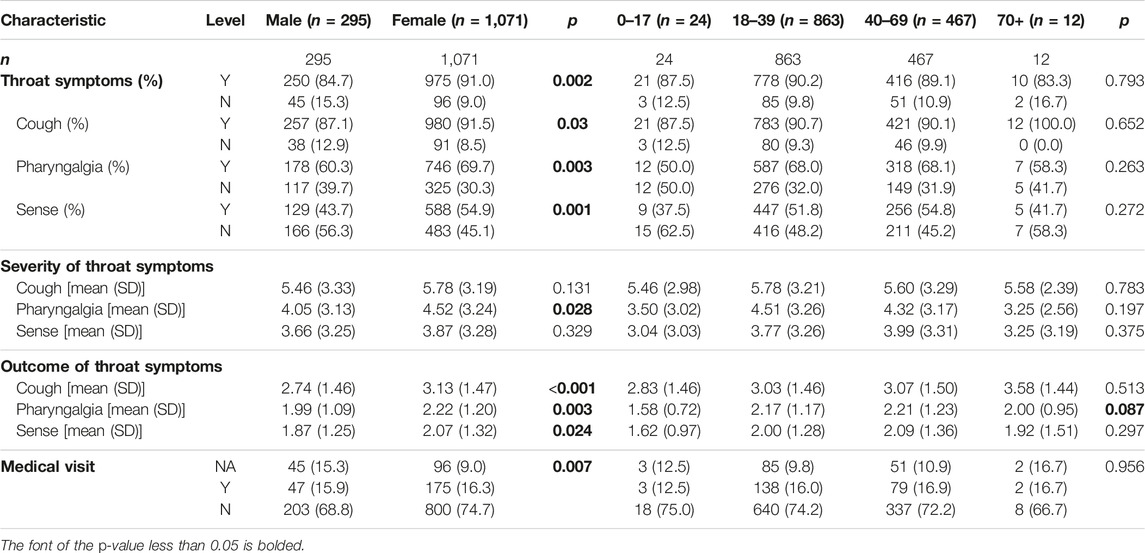
TABLE 4. The symptomatic rate, severity and outcome of throat symptoms among different genders and age groups (China, 2023).
Among the throat symptoms, cough was the most common, with a symptomatic rate of up to 100% in elderly patients, as shown in Figure 1D. Nearly 600 patients rated the impact of cough as severe, with scores ranging from 7 to 10. Furthermore, over 400 patients reported cough as a post-acute sequela of COVID-19 (Figures 2E, F). Additionally, females experienced more severe throat pain and poorer outcomes for all throat symptoms compared to males, as indicated in Table 4. Throat symptoms also exhibited higher rates of medical visits compared to ear or nose symptoms, as depicted in Figure 1.
Discussion
SARS-CoV-2 Omicron infection typically presents with mild or subclinical features, primarily manifesting as symptoms like dry cough, fever, and diarrhea. However, as the pandemic has progressed, neurological manifestations have also been observed in some individuals. The range of clinical presentations associated with SARS-CoV-2 infection is expanding, with reported cases of Guillain-Barre syndrome as a separate entity [19–21]. While research on COVID-19 symptoms has primarily focused on the respiratory system, such as pulmonary symptoms [22], here is relatively limited research on ENT (ear, nose, and throat) aspects. Some studies have reported on hearing and vestibular function [7], including hearing loss [13, 23, 24], tinnitus [25, 26], and vertigo [26, 27]. In comparison to other COVID-19 symptom studies, our research specifically focused on comparing ear, nasal, and throat aspects and utilized a large and representative sample size through cross-sectional survey methods.
Our findings indicate that the symptomatic rate of nasal and throat symptoms is significantly higher than that of ear symptoms. There is a notable correlation between age and the symptomatic rate of certain symptoms. Older adults are less likely to experience nasal obstruction, rhinorrhea, loss of sense of smell, pharyngalgia, and loss of sense of taste. These findings are supported by previous studies [27, 28], that suggest younger individuals are more prone to experiencing ENT symptoms. For instance, a study by Lechien et al. involving 1420 patients found differences in the symptomatic rate of COVID-19 symptoms based on gender and age, with younger individuals more frequently experiencing nasal congestion, rhinorrhea, and pharyngalgia [29]. Another study by Vaira et al. [30] discovered that loss of sense of smell and/or taste commonly occur in the early stages of the disease and gradually disappear, indicating potential viral interference or local inflammation of taste and olfactory receptors rather than permanent neuronal damage or invasion of the central nervous system [30]. Further research is needed to explore the specific mechanisms underlying taste and olfactory disturbances caused by SARS-CoV-2.
Previous reports suggest that older adults tend to have more severe clinical symptoms and outcomes after SARS-CoV-2 Omicron infection [31]. Our research aligns with this understanding, indicating that comorbidities in older individuals may contribute to the increased severity. By comparing and analyzing survey results with existing research [6, 28, 32–37], we have provided new insights and discoveries regarding the symptomatic rate and outcomes of otolaryngological symptoms. We particularly emphasized the importance of addressing tinnitus and hearing loss as symptoms requiring attention and resolution. Additionally, we highlighted the need for greater attention and treatment of otolaryngological symptoms in females, given their higher symptomatic rates and more severe clinical manifestations. Considering the high symptomatic rate of ENT symptoms and their significant impact on quality of life, along with the potential for long-lasting residual effects, it is crucial to prioritize the recognition and management of ENT symptoms associated with SARS-CoV-2 infection.
It’s important to acknowledge the limitations of our study, which utilized cross-sectional internet-based surveys. These surveys are subject to limitations such as sampling biases, as they primarily reach internet audiences, who are typically younger and more educated. Older adults may be less likely to participate in online questionnaires, while women tend to have higher participation rates in online surveys. As our survey specifically targeted SARS-CoV-2 Omicron infected individuals with ENT symptoms, there may be sample biases. Additionally, reports from infected individuals can be influenced by subjective factors, leading to reporting biases. Furthermore, cross-sectional surveys conducted online can only establish correlations between variables and cannot determine causal relationships, resulting in lower levels of evidence.
Given the potential for tinnitus and hearing loss to persist as long-term residual symptoms, healthcare professionals should be vigilant in informing COVID-19 patients about these potential complications to enable early detection and intervention. Moreover, due to the higher symptomatic rate and more severe clinical manifestations of ENT symptoms in female patients, enhanced symptom monitoring and optimized treatment plans are necessary. Lastly, although the elderly population may exhibit a lower symptomatic rate of ENT symptoms, they experience a greater impact on their quality of life and poorer outcomes. Therefore, tailored symptom management strategies for this age group are crucial.
Conclusion
Our investigation reveals an outbreak of COVID-19 infections in December 2022. We found that otologic symptoms have a relatively minor impact on patients’ lives. However, tinnitus and hearing loss are the most commonly reported residual symptoms. Rhinological symptoms have a relatively high symptomatic rate, but they typically do not persist as residual symptoms. On the other hand, laryngeal symptoms have the highest symptomatic rate and exert the greatest impact on patients’ quality of life. Furthermore, our study highlights that female patients are more vulnerable to these effects. These findings serve as a foundation for enhancing our understanding of the symptom spectrum in patients infected with the Omicron variant and provide valuable insights for targeted symptom management strategies.
Data Availability Statement
The datasets generated during or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Statement
The studies involving humans were approved by the Eye and ENT Hospital ethics panel at Fudan University (No. 2022127). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author Contributions
SS, YXL, XH contributed to conception and design of the study. PL organized the database. DW and NW performed the statistical analysis. HY contributed to literature search. YXL wrote the first draft of the manuscript. XH wrote sections of the manuscript. YL, HL and SS contributed to study concept and design, administrative support, data interpretation, and article revision. All authors contributed to manuscript revision, read, and approved the submitted version.
Funding
This work was supported by the National Natural Science Foundation of China (Nos. 81970879, 82371146, 82192862, and 82192860), the Shanghai Science and Technology Committee (STCSM) Science and Technology Innovation Program (20MC1920200) and Research Projects of Shanghai Municipal Health Committee (2020YJZX0110 and 2022XD059).
Conflict of Interest
The authors declare that they do not have any conflicts of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/ijph.2023.1606403/full#supplementary-material
References
1. WHO Coronavirus (COVID-19) Dashboard. WHO Coronavirus (COVID-19) Dashboard With Vaccination Data (2023). Available From: https://covid19.who.int/ (Accessed May 11, 2023).
2. Chinese Center for Disease Control and Prevention. The Situation of the COVID-19 Infection in China (2023). Available From: https://m.chinacdc.cn/jkzt/crb/yl/hrb_11806/jszl_13142/202301/t20230125_263519.html (Accessed May 12, 2023).
3. Cao, Y, Yisimayi, A, Jian, F, Song, W, Xiao, T, Wang, L, et al. BA.2.12.1, BA.4 and BA.5 Escape Antibodies Elicited by Omicron Infection. Nature (2022) 608:593–602. doi:10.1038/s41586-022-04980-y
4. Grant, MC, Geoghegan, L, Arbyn, M, Mohammed, Z, McGuinness, L, Clarke, EL, et al. The Prevalence of Symptoms in 24,410 Adults Infected by the Novel Coronavirus (SARS-CoV-2; COVID-19): A Systematic Review and Meta-Analysis of 148 Studies From 9 Countries. PLoS One (2020) 15:e0234765. doi:10.1371/journal.pone.0234765
5. El-Anwar, MW, Elzayat, S, and Fouad, YA. ENT Manifestation in COVID-19 Patients. Auris Nasus Larynx (2020) 47:559–64. doi:10.1016/j.anl.2020.06.003
6. Maharaj, S, Bello Alvarez, M, Mungul, S, and Hari, K. Otologic Dysfunction in Patients With COVID-19: A Systematic Review. Laryngoscope Investig Otolaryngol (2020) 5:1192–6. doi:10.1002/lio2.498
7. Almufarrij, I, and Munro, KJ. One Year on: An Updated Systematic Review of SARS-CoV-2, COVID-19 and Audio-Vestibular Symptoms. Int J Audiol (2021) 60:935–45. doi:10.1080/14992027.2021.1896793
8. Al-Ani, RM. Ear, Nose, and Throat Manifestations of COVID-19 and Its Vaccines. World J Clin Cases (2022) 10:8808–15. doi:10.12998/wjcc.v10.i25.8808
9. Haider, HF, and Szczepek, AJ. Editorial: Neurotological Consequences of Long COVID. Front Neurol (2022) 13:1087896. doi:10.3389/fneur.2022.1087896
10. Zięba, N, Lisowska, G, Dadok, A, Kaczmarek, J, Stryjewska-Makuch, G, and Misiołek, M. Frequency and Severity of Ear-Nose-Throat (ENT) Symptoms During COVID-19 Infection. Medicina (Kaunas) (2022) 58:623. doi:10.3390/medicina58050623
11. Uranaka, T, Kashio, A, Ueha, R, Sato, T, Bing, H, Ying, G, et al. Expression of ACE2, TMPRSS2, and Furin in Mouse Ear Tissue, and the Implications for SARS-CoV-2 Infection. Laryngoscope (2021) 131:E2013–7. doi:10.1002/lary.29324
12. Frazier, KM, Hooper, JE, Mostafa, HH, and Stewart, CM. SARS-CoV-2 Virus Isolated From the Mastoid and Middle Ear: Implications for COVID-19 Precautions During Ear Surgery. JAMA Otolaryngol Head Neck Surg (2020) 146:964–6. doi:10.1001/jamaoto.2020.1922
13. Mustafa, MWM. Audiological Profile of Asymptomatic Covid-19 PCR-Positive Cases. Am J Otolaryngol (2020) 41:102483. doi:10.1016/j.amjoto.2020.102483
14. Chirakkal, P, Al Hail, AN, Zada, N, and Vijayakumar, DS. COVID-19 and Tinnitus. Ear Nose Throat J (2021) 100:160S–162S. doi:10.1177/0145561320974849
15. Costa, KVTD, Carnaúba, ATL, Rocha, KW, Andrade, KCLD, Ferreira, SMS, and Menezes, PDL. Olfactory and Taste Disorders in COVID-19: A Systematic Review. Braz J Otorhinolaryngol (2020) 86:781–92. doi:10.1016/j.bjorl.2020.05.008
16. Özçelik Korkmaz, M, Eğilmez, OK, Özçelik, MA, and Güven, M. Otolaryngological Manifestations of Hospitalised Patients With Confirmed COVID-19 Infection. Eur Arch Otorhinolaryngol (2021) 278:1675–85. doi:10.1007/s00405-020-06396-8
17. Vaira, LA, Lechien, JR, Salzano, G, Salzano, FA, Maglitto, F, Saussez, S, et al. Gustatory Dysfunction: A Highly Specific and Smell-Independent Symptom of COVID-19. Indian J Otolaryngol Head Neck Surg (2022) 74:2755–7. doi:10.1007/s12070-020-02182-4
18. EYE and ENT Hospital. Survey on Ear, Nose, and Throat Symptoms After COVID-19 Infection (2023). Available From: https://www.wjx.cn/vm/exOmDok.aspx (Accessed January 29, 2023).
19. Whittaker, A, Anson, M, and Harky, A. Neurological Manifestations of COVID-19: A Systematic Review and Current Update. Acta Neurol Scand (2020) 142:14–22. doi:10.1111/ane.13266
20. Ellul, MA, Benjamin, L, Singh, B, Lant, S, Michael, BD, Easton, A, et al. Neurological Associations of COVID-19. Lancet Neurol (2020) 19:767–83. doi:10.1016/S1474-4422(20)30221-0
21. Mao, L, Jin, H, Wang, M, Hu, Y, Chen, S, He, Q, et al. Neurologic Manifestations of Hospitalized Patients With Coronavirus Disease 2019 in Wuhan, China. JAMA Neurol (2020) 77:683–90. doi:10.1001/jamaneurol.2020.1127
22. Anka, AU, Tahir, MI, Abubakar, SD, Alsabbagh, M, Zian, Z, Hamedifar, H, et al. Coronavirus Disease 2019 (COVID-19): An Overview of the Immunopathology, Serological Diagnosis and Management. Scand J Immunol (2021) 93:e12998. doi:10.1111/sji.12998
23. Karimi-Galougahi, M, Naeini, AS, Raad, N, Mikaniki, N, and Ghorbani, J. Vertigo and Hearing Loss During the COVID-19 Pandemic - Is There an Association? Acta Otorhinolaryngol Ital (2020) 40:463–5. doi:10.14639/0392-100X-N0820
24. Munro, KJ, Uus, K, Almufarrij, I, Chaudhuri, N, and Yioe, V. Persistent Self-Reported Changes in Hearing and Tinnitus in Post-Hospitalisation COVID-19 Cases. Int J Audiol (2020) 59:889–90. doi:10.1080/14992027.2020.1798519
25. Beukes, EW, Baguley, DM, Jacquemin, L, Lourenco, MPCG, Allen, PM, Onozuka, J, et al. Changes in Tinnitus Experiences During the COVID-19 Pandemic. Front Public Health (2020) 8:592878. doi:10.3389/fpubh.2020.592878
26. Viola, P, Ralli, M, Pisani, D, Malanga, D, Sculco, D, Messina, L, et al. Tinnitus and Equilibrium Disorders in COVID-19 Patients: Preliminary Results. Eur Arch Otorhinolaryngol (2021) 278:3725–30. doi:10.1007/s00405-020-06440-7
27. Lechien, JR, Chiesa-Estomba, CM, Place, S, Van Laethem, Y, Cabaraux, P, Mat, Q, et al. Clinical and Epidemiological Characteristics of 1420 European Patients With Mild-to-Moderate Coronavirus Disease 2019. J Intern Med (2020) 288:335–44. doi:10.1111/joim.13089
28. Wu, L, Peng, H, He, Y, Pu, L, and Zhong, S. An Online Survey on Clinical Characteristics of Otologic Symptoms Linked to COVID-19 Infection. Front Public Health (2023) 11:1184262. doi:10.3389/fpubh.2023.1184262
29. Li, Y-C, Bai, W-Z, and Hashikawa, T. The Neuroinvasive Potential of SARS-CoV2 May Play a Role in the Respiratory Failure of COVID-19 Patients. J Med Virol (2020) 92:552–5. doi:10.1002/jmv.25728
30. Vaira, LA, Hopkins, C, Petrocelli, M, Lechien, JR, Chiesa-Estomba, CM, Salzano, G, et al. Smell and Taste Recovery in Coronavirus Disease 2019 Patients: A 60-Day Objective and Prospective Study. J Laryngol Otol (2020) 134:703–9. doi:10.1017/S0022215120001826
31. Almishaal, AA, and Alrushaidan, AA. Short- and Long-Term Self-Reported Audiovestibular Symptoms of SARS-Cov-2 Infection in Hospitalized and Nonhospitalized Patients. Audiol Neurootol (2022) 27:297–311. doi:10.1159/000521963
32. Mastrangelo, A, Bonato, M, and Cinque, P. Smell and Taste Disorders in COVID-19: From Pathogenesis to Clinical Features and Outcomes. Neurosci Lett (2021) 748:135694. doi:10.1016/j.neulet.2021.135694
33. Ong, KMC, and Cruz, TLG. Otologic and Vestibular Symptoms in COVID-19: A Scoping Review. World J Otorhinolaryngol Head Neck Surg (2022) 8:287–96. doi:10.1002/wjo2.57
34. Jafari, Z, Kolb, BE, and Mohajerani, MH. Hearing Loss, Tinnitus, and Dizziness in COVID-19: A Systematic Review and Meta-Analysis. Can J Neurol Sci (2022) 49:184–95. doi:10.1017/cjn.2021.63
35. Leong, S, Teh, BM, and Kim, AH. Characterization of Otologic Symptoms Appearing After COVID-19 Vaccination. Am J Otolaryngol (2023) 44:103725. doi:10.1016/j.amjoto.2022.103725
36. Yong, SJ. Long COVID or Post-COVID-19 Syndrome: Putative Pathophysiology, Risk Factors, and Treatments. Infect Dis (Lond) (2021) 53:737–54. doi:10.1080/23744235.2021.1924397
Keywords: COVID-19, ENT, network survey, cross-sectional study, symptomatic rate
Citation: Liu Y, Huang X, Li P, Wang D, Yin H, Wang N, Luo Y, Li H and Sun S (2023) Clinical Profile and Outcome Analysis of Ear-Nose-Throat Symptoms in SARS-CoV-2 Omicron Subvariant Infections. Int J Public Health 68:1606403. doi: 10.3389/ijph.2023.1606403
Received: 17 July 2023; Accepted: 11 September 2023;
Published: 10 October 2023.
Edited by:
Jean Tenena Coulibaly, Félix Houphouët-Boigny University, Côte d'IvoireReviewed by:
Ugochukwu Anthony Eze, National Postgraduate Medical College of Nigeria, NigeriaAnmar Al-Taie, Istinye University, Türkiye
Copyright © 2023 Liu, Huang, Li, Wang, Yin, Wang, Luo, Li and Sun. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yan Luo, bmFuY3lseTIzQDEyNi5jb20=; Huawei Li, aHdsaUBzaG11LmVkdS5jbg==; Shan Sun, c2hhbnN1bkBmdWRhbi5lZHUuY24=
This Original Article is part of the IJPH Special Issue “Neglected Tropical Diseases During the COVID-19 Pandemic”
†These authors have contributed equally to this work
 Yixuan Liu1,2,3†
Yixuan Liu1,2,3† Shan Sun
Shan Sun