- 1Development Research Group, Department of Politics and Public Administration, University of Konstanz, Konstanz, Germany
- 2Leibniz Institute of Vegetable and Ornamental Crops, Großbeeren, Germany
- 3ISDC—International Security and Development Center, Berlin, Germany
- 4Albrecht Daniel Thaer Institute for Agricultural and Horticultural Sciences, Faculty of Life Sciences, Humboldt University of Berlin, Berlin, Germany
Objective: Providing country-level estimates for prevalence rates of Generalized Anxiety Disorder (GAD), COVID-19 exposure and food insecurity (FI) and assessing the role of persistent threats to survival—exemplified by exposure to COVID-19 and FI—for the mental health crisis in Africa.
Methods: Original phone-based survey data from Mozambique, Sierra Leone, Tanzania and Uganda (12 consecutive cross-sections in 2021; n = 23,943) were analyzed to estimate prevalence rates of GAD. Logistic regression models and mediation analysis using structural equation models identify risk and protective factors.
Results: The overall prevalence of GAD in 2021 was 23.3%; 40.2% in Mozambique, 17.0% in Sierra Leone, 18.0% in Tanzania, and 19.1% in Uganda. Both COVID-19 exposure (ORadj. 1.4; CI 1.3–1.6) and FI (ORadj 3.2; CI 2.7–3.8) are independent and significant predictors of GAD. Thus, the impact of FI on GAD was considerably stronger than that of COVID-19 exposure.
Conclusion: Persistent threats to survival play a substantial role for mental health, specifically GAD. High anxiety prevalence in the population requires programs to reduce violence and enhance social support. Even during a pandemic, addressing FI as a key driver of GAD should be prioritized by policymakers.
Introduction
Mental and behavioral illnesses account for 4.9% of disability-adjusted life-years (DALYs); specifically, Generalized Anxiety Disorder (GAD) is amongst the top ten causes of years lived with disability (YLD) [1]. Introduced in the Diagnostic and Statistical Manual (DSM) Version III, GAD is characterized by excessive, uncontrollable worry with a minimum duration of 6 months [2]. Comorbidity is most frequent with depression [3]. Evidence-based treatments such as cognitive behavior therapy and SSRI/SNRI agents are successful in about 50% of cases [3].
Globally, prevalence rates of GAD are estimated at about 0.1%–3.0% (30 days prevalence) in the general population [4]. Multinational studies and a meta-analysis indicate lower GAD rates in low- and middle-income countries [4]. For this study, we conducted a rapid systematic review following PICOS [5] to obtain insights on GAD prevalence rates in the general population in Africa. Presented in Table 1, we found nine studies revealing rates from 0% to 49.6% (see Supplementary Material SI). A part of the variance is due to different assessment methodologies and diagnostic criteria, however recent studies relied predominantly on the GAD-7 of the Patient Health Screening [16]; within these studies the prevalence rates still range from 5.6% in Libya to 49.6% in Nigeria, notably with differences in cut-off levels. Many Africans who suffer from mental illness do not have access to treatment. Treatment gap estimates based on the mere availability of a psychiatrist/clinical psychologist range between 75% and 99% [17, 18].
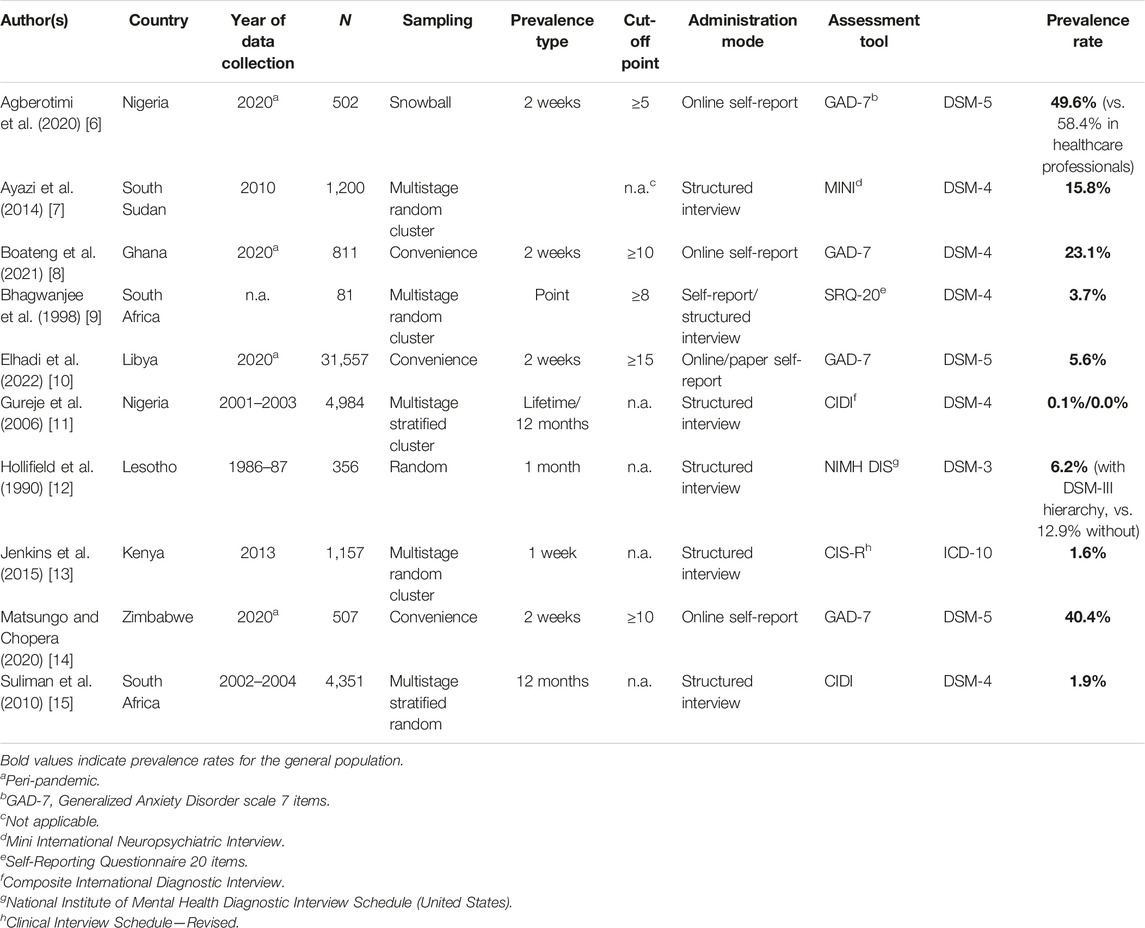
TABLE 1. Studies on prevalence rates of generalized anxiety disorder in the adult general population, country level. (selected studies - Africa, published between 1980 and 2023).
In addition to the suffering of affected individuals and their families, costs to society and economic development are enormous as mental illness may render individuals dysfunctional across different life domains. Neuroeconomic experiments further indicate the impact of anxiety and GAD specifically on individual decision making and thus highlights its relevance for collective dynamics and processes when incidence surges [19].
Alongside with genetic predisposition [20], female sex, and parental model learning [21], adverse life events and health issues increasing the vulnerability of a person have shown to increase the risk of GAD [22]. Based on results of a 12 years prospective study, Zhang et al. highlighted that both recent and distal adverse life events independently contributed to GAD [23]. The cumulative impact of immediate threats to survival—classified as traumatic events—with posttraumatic stress disorder is well established [24]. Like traumatic events, persistent threats to survival may accumulate and impact mood and cognition and compromise mental health via an increase of general anxiety levels. In this study, we estimate prevalence rates for GAD and investigate the interplay of concurring persistent threats in Sub-Saharan Africa (SSA).
Recently, the mental health crisis in SSA, marked by a surge in the prevalence of mental illness and large treatment gaps, has coincided both with the risk of contracting SARS-CoV-2 [25] and increased levels of food insecurity (FI) [26, 27]. Both the threat of infection and insufficient food insecurity present persistent stressors relevant to survival. Figure 1A provides information about COVID-19 and FI in SSA.
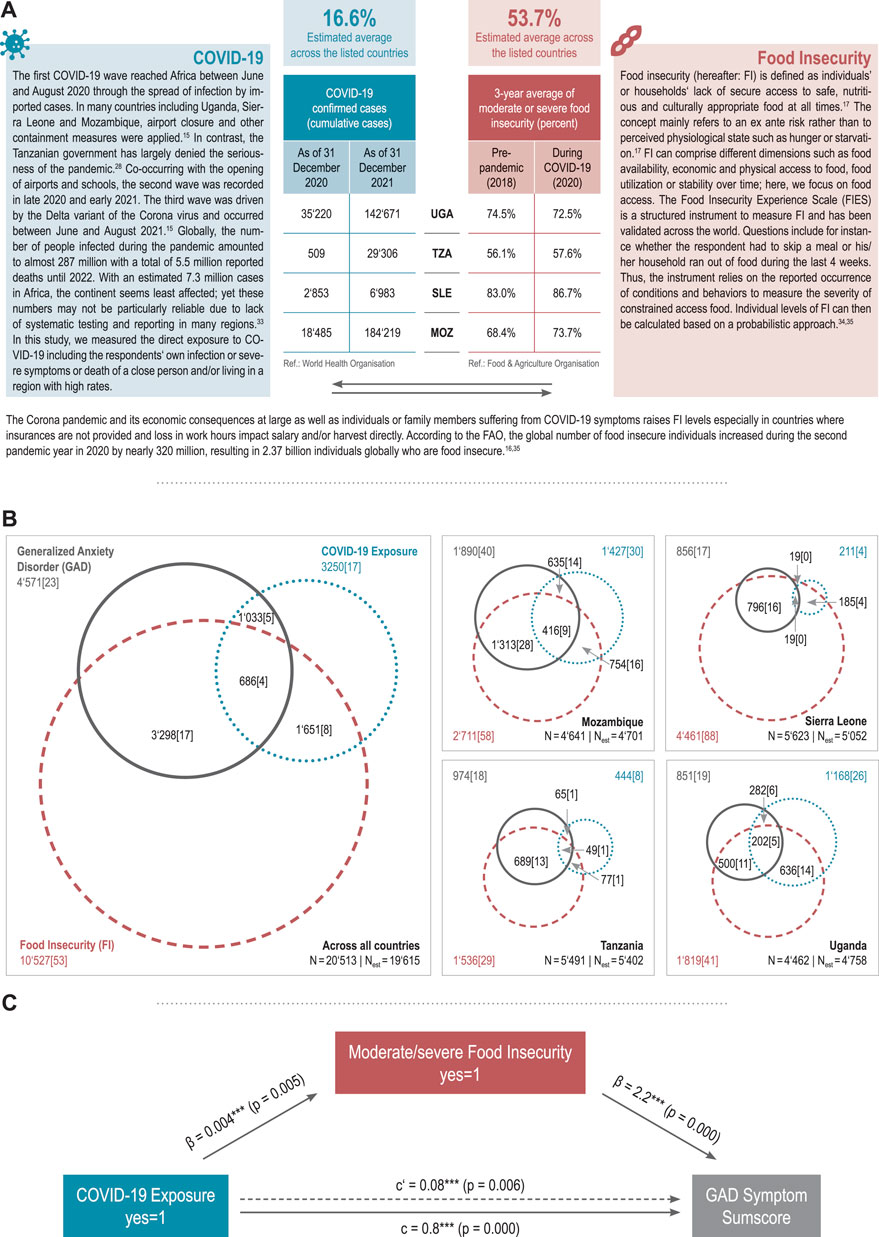
FIGURE 1. Panel (A): Fact sheet COVID-19 and food insecurity (Life with Corona—Africa, Mozambique, Sierra Leone, Tanzania, Uganda, 2021). Panel (B): Overlap between generalized anxiety disorder, COVID-19 and food insecurity, Venn diagrams (Life with Corona—Africa, Mozambique, Sierra Leone, Tanzania, Uganda, 2021) Panel (C): Determinants of generalized anxiety disorder, mediation model (Life with Corona—Africa, Mozambique, Sierra Leone, Tanzania, Uganda, 2021).
COVID-19–Anxiety
Globally, the COVID-19 pandemic has caused a surge in anxiety [8, 28]. With a survey covering 58 countries and over 100,000 respondents in March and April 2020, Paudel et al. demonstrated the link between the number of reported COVID-19 cases and anxiety levels [29]. Moreover, containment policies including self-isolation or social distancing orders were shown to be associated with increased anxiety and emotional instability for those who stayed at home [29]. A meta-analysis covering 204 countries pointed to a particularly strong psychological burden of the pandemic for women and younger populations [30]. Studies from the SSA region also indicate a heightened incidence of anxiety during the COVID-19 pandemic [8, 28].
FI–Anxiety
A recent systematic review of the relationship between FI and mental health in Africa revealed a dose-response relationship [31]. Emerging evidence on the underlying mechanisms suggests that FI directly deteriorates mental health by depriving from fulfillment of a basic need and by creating uncertainty over the ability to meet these needs in the future [32] other mechanisms such as nutrient deficiencies affecting brain function or one’s perceived relative economic status manifested in FI were shown to be of secondary importance [31–33]. The inherent link between FI and mental health is also supported by the study of Jones and colleagues who found a robust association regardless of culture or a countries’ wealth [34].
Our study provides new evidence on the prevalence and associated factors of GAD in the African context. To this end, we draw on novel phone-based survey data providing estimates of prevalence rates of GAD according to the DSM-5 alongside with direct COVID-19 exposure and FI in the general adult population in four African low- and middle-income countries–Mozambique, Sierra Leone, Tanzania and Uganda. We then analyze whether the pandemic adversely affected mental health directly and indirectly by testing whether FI is a mediator of the relation between COVID-19 exposure and GAD.
Methods
Study Design and Setting
As part of the Life with Corona (LwC) project [35], the LwC-Africa study collected phone survey data from adults (>17 years) in Mozambique, Sierra Leone, Tanzania and Uganda throughout the year 2021 [36]. During the COVID-19 pandemic, conducting face-to-face interviews could have posed a risk to both the interviewer and the respondent. Moreover, utilizing online surveys in low- and middle-income countries would have introduced a potential bias by selectively including individuals with internet access. To mitigate these challenges, telephone interviews were employed, as a substantial portion of the population possesses a cell phone, offering a more inclusive and accessible mode of data collection. The countries were selected for their variance regarding geography, demographics, and response to the COVID-19 pandemic (e.g., [25, 37]).
Procedure
The survey was implemented in 12 rounds of data collection from January to December 2021 by a non-governmental organization (BRAC International in Sierra Leone, Tanzania and Uganda) and a local company (Intercampus in Mozambique) using large in-house databases of mobile phone contacts from active and previous research; in each round, participants were randomly selected, but the composition of the population in each country in terms of gender, age, location (urban/rural) was accounted for aiming at 500 new randomly selected participants per month and country. Our sample size was informed by and consistent with the literature [36]. Before the interview, informed oral consent was obtained from all individual participants included in the study by reading out the consent statement at the start of the interviews. The statement contains information regarding the purpose of the interview and the confidentiality of their personal information. The statement also contains information regarding the respondent’s rights to refuse to respond to any individual question or the entire interview. The calls to the respondents were made during the day from the call centers of the survey companies. Usually, two to three calls were made to secure an interview. When repeated attempts to reach a selected respondent were not successful, a replacement satisfying the stratification criteria was used. In line with similar studies [38], the response rate was about 50% whereby the main reasons for non-response were inactive phone contacts and non-response to the phone calls. The average interview duration was 16.5 min. The study was approved by the ethical commission of UNU-WIDER.
Participants
A total of N = 23,943 participants were interviewed (nMozambique = 6000; nSierra Leone = 6217; nTanzania = 6033; nUganda = 6033). To obtain a representative sample and more precise estimation of prevalence rates per country, we applied post-stratification weights for age, gender and location [39]. Resulting sociodemographic estimates and country comparisons are presented in Table 2.
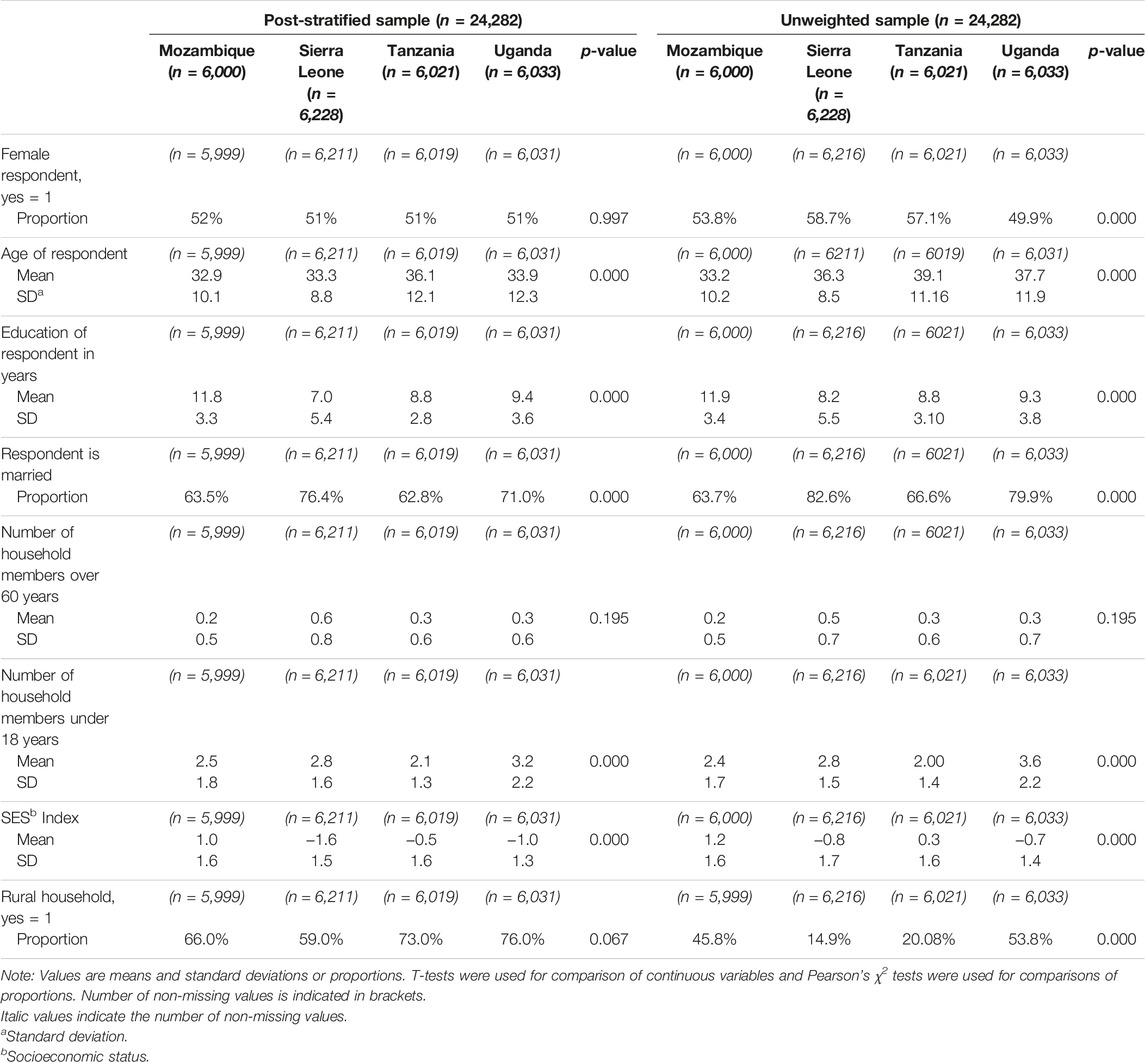
TABLE 2. Socio-demographic characteristics by country (Life with Corona—Africa, Mozambique, Sierra Leone, Tanzania, Uganda, 2021).
Measures
Computer-assisted telephone interviews were conducted by trained enumerators; the 4 days training included relevant concepts, mock interviews, administration of the computer-assisted telephone interviews (CATI) protocol, piloting of the survey, and debriefing sessions. The original English version of the questionnaire was translated into Luganda, Runyankole, Acholi, Lusoga, Kiswahili, Krio/Creole and Portuguese. Validity of the translations for use in the respective countries was ensured based on repeated mock interviews among the enumerators, fluent speakers of the local languages, during the training as well as the pre-survey piloting of the questionnaire.
GAD according to DSM-5 was measured with the 7-item Generalized Anxiety Disorder scale (GAD-7) [16]. Each item (e.g., Feeling nervous, anxious, or on edge; Not being able to stop or control worrying; Worrying too much about different things) was rated on a scale from 0 (not at all) to 3 (nearly every day) according to the presence of symptoms during the last 2 weeks. A sumscore ranging 0–21 was used to indicate symptom severity. Following a systematic review/meta-analysis conducted by Plummer and colleagues, who presented a sensitivity of 0.83 and specificity 0.84 [40] we used a cut-off value of 8 to estimate the diagnosis of GAD. We present prevalence rates at alternative thresholds in the Supplementary Table S7. Although validation studies are not available for the specific countries included in our study, the GAD-7 is a standardized instrument validated for various (African) countries [41]. Recognizing the importance of context-specific validation, we strongly advocate for further validation studies in African countries to enhance the reliability and applicability of mental health assessment tools in diverse cultural settings.
COVID-19 exposure was measured with four dichotomous (yes [1]/no [0]) questions asking whether the respondent was infected by the Coronavirus, met anyone who acutely suffered from COVID-19 symptoms, felt to live in an area with high incidence or knew someone who died from the consequences of Coronavirus infection. We had to rely on subjective self-assessment of perceived exposure as there has been a wide gap in testing in most African countries [42]. Similar to other sensitive topics in surveys, data quality regarding questions about COVID-19 exposure may be constrained by survey biases such as reporting bias due to social desirability, fear of stigma and discrimination. For the prevalence rates, we analyzed calculated a score summing up all yes [1] answers; COVID-19 exposure was counted as positive when at least the answer to one of the four questions was yes.
FI was measured using the Food Insecurity Experience Scale (FIES) [43]; a globally used and validated measure. The eight questions focus on experiences and behaviors related to difficulties in accessing food (e.g., worrying about food scarcity, eating less nutritious food, skipping meals or running out of food) in a 4 weeks recall period and can be answered with yes [1]/no [0]. Using a probabilistic approach, the respondents’ status with regard to a policy relevant level of FI (moderate-or-severe FI) was determined as suggested by FAO [43, 44].
Furthermore, we collected information about sociodemographic characteristics (gender, age, years of education, and marital status), living in a rural/urban area, household composition and wealth indicating the socio-economic status of the respondent (hereafter: SES index); the latter was calculated via Principal Component Analysis to reduce the dimensionality of numerous variables (see Supplementary Material SⅡ). This approach captures household living standards and therefore avoids common measurement biases related to income or expenditure measures [45]; higher SES index indicates more assets, better infrastructure, and housing.
Statistical Analysis
To estimate prevalence rates of GAD diagnosis and exposure to COVID-19 FI, we use frequencies and percentages on our sample with post-stratification weights applied for age, gender and location (urban/rural). Respondents were excluded when information in any main variable was missing (missing values: nGAD-7 = 1; nCOVID-19 = 3,576; nFI = 230). To examine the association of the pandemic and FI and the risk of developing GAD, we conducted logistic regression analyses. Furthermore, we performed a mediation analysis using structural equation modeling [46] hypothesizing that FI mediates the association of COVID-19 and GAD. To allow for full convergence of the mediation model, we omit country-fixed effects and only include region and survey round dummies. The reliability of mediation analysis relies on certain vital assumptions, including the lack of multicollinearity, minimal measurement errors (especially in the mediator), control of omitted variable bias by incorporating relevant confounders, and linearity. We have found that these necessary assumptions are met, thus confirming the validity of the use of mediation analysis in our study. The statistical analyses were performed in Stata version 17.
Results
In our post-stratified sample of 20,513 individuals, a total of 23.3% were above the GAD-7-threshold indicating a diagnosis of GAD. By country, 40.2% in Mozambique, 17.0% in Sierra Leone, 18.0% in Tanzania and 19.1% in Uganda suffered from GAD. COVID-19 exposure is highest in Mozambique and Uganda with 30.4% and 26.2%; the proportion of subjects reporting any exposure to COVID-19 is comparably low in Tanzania (8.2%) and Sierra Leone (4.2%). Overall, the estimated prevalence of FI was 53.7%. The estimated prevalence rate of FI is highest in Sierra Leone (88.3%), followed by Mozambique (57.7%), Uganda (40.8%), and Tanzania (28.4%). Venn diagrams (Figure 1B) show a substantial overlap of GAD with both COVID-19 exposure and FI. Supplementary Table S2 presents variation in prevalence rates over time.
Logistic regression models (Table 3) show that both COVID-19 exposure and FI present as significant risk factors of GAD. Being exposed to COVID-19 is associated with 1.7 (CI 1.4–2.0; p = 0.000) higher odds of GAD, while being moderate/severe FI is associated with 2.9 higher odds of GAD compared to food secure individuals (CI 2.4–3.4; p = 0.000). The adjusted model accounts for respondents’ characteristics, region, country and survey round. The effect of FI on GAD (adj. OR 3.1; CI 2.6–3.7; p = 0.000) is more than twice as large as COVID-19 exposure (adj. OR 1.4; CI 1.3–1.6; p = 0.000). While each additional young household member (OR 1.1; CI 1.1–1.1; p = 0.000) is significantly associated with higher odds of GAD, higher SES presents as protective factor (OR 0.8; CI 0.8–0.9; p = 0.000).
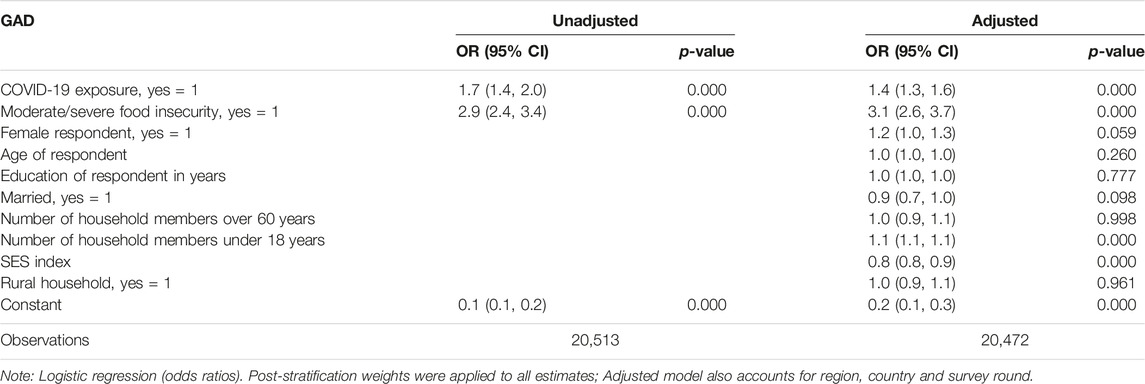
TABLE 3. Logistic regression of the determinants of generalized anxiety disorder (Life with Corona—Africa, Mozambique, Sierra Leone, Tanzania, Uganda, 2021).
The mediation model (Table 4 and Figure 1C) shows a significant total effect of COVID-19 exposure on GAD (β = 0.08, p = 0.000). It also confirms a significant association between COVID-19 exposure and FI (β = 0.04, p = 0.005) and a significant association between FI and the GAD symptom sum score (β = 2.2, p = 0.000). Moreover, a significant direct effect of COVID-19 exposure on the GAD symptom sum score (direct effect: β = 0.8, p = 0.000) is detected. The mediation model shows a significant indirect (partly mediated) effect of COVID-19 on GAD trough FI (indirect effect: β = 0.1, p = 0.005). About 9.4% of the effect of COVID-19 on GAD is mediated by FI and the mediated effect is about 0.1 times as large as the direct effect.
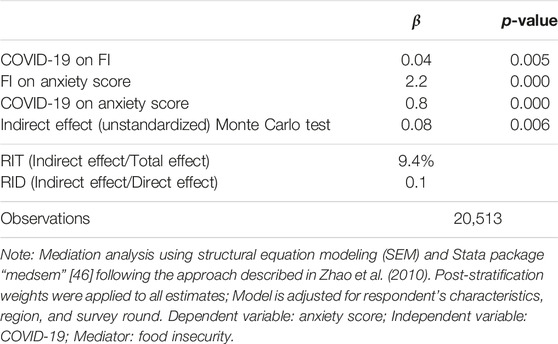
TABLE 4. Mediation analysis of the determinants of generalized anxiety disorder (Life with Corona—Africa, Mozambique, Sierra Leone, Tanzania, Uganda, 2021).
Discussion
This study finds an overall estimated prevalence of 23.3% for GAD in Mozambique, Sierra Leone, Tanzania and Uganda; 8.4% were directly exposed to COVID-19% and 16.4% presented with moderate-to-high levels of FI. 16.8% of individuals with GAD are food insecure and 8.4% have been exposed to COVID-19; 3.5% of the participants were exposed to both persistent stressors. Accordingly, logistic regression shows that exposure to COVID-19 and in particular FI is associated with a risk of developing GAD. A higher number of dependents under 18 years and lower SES also presented as risk factors for GAD whereas gender and other sociodemographic variables did not reach significance. The mediation analysis reveals that FI as a preexisting persistent threat to survival works as an additional vehicle transforming the stress induced by the pandemic into GAD.
Estimated peri-pandemic GAD prevalence rates –40.2% in Mozambique, 17.0% in Sierra Leone, 18.0% in Tanzania and 19.1% in Uganda– assessed with the GAD-7 at a cut-off point ≥8 following Plummer and colleagues [40] reflect a variance of comparable previous studies: In Ghana, Boateng et al. found 23.1% [8] and in Zimbabwe Matsungo et al. found 40.4% [14]; both with a cut-off point at GAD-7 ≥ 10. In Nigeria, Agberotimi and colleagues found 49.6% (GAD-7 ≥ 5) [6]. In a large study of more than 30 k participants and a strict cut-off score GAD-7 ≥ 15, Elhadi and colleagues found 5.6% in Libya [10]. For comparison, Jia et al. conducted a study in United Kingdom and found a prevalence rate of 23.6% (cut off ≥ 8) [47] and Solomou and colleagues found a rate of 23.1% (GAD-7 ≥ 10) in Cyprus [48]. Prevalence rates for our data with the various cut-off scores for each country are presented in the Supplementary Table S7. All studies that assessed GAD during the pandemic applied the GAD-7 online as self-report instrument and were conducted in 2020. For a better understanding of the prevalence rates of GAD in Africa, more rigorous epidemiological and longitudinal research is needed, including validation studies with expert clinical diagnostic interviews. Moreover, whether COVID-19 related GAD cases are in remission as the pandemic declines warrants further research.
Notably, GAD prevalence rates of this study mirror the patterns of confirmed COVID-19 cases as reported by the WHO: The proportion of respondents reporting COVID-19 exposure is comparably low in Tanzania (8.2%) and Sierra Leone (4.2%) versus Uganda (26.2%) and Mozambique (30.4%). Moreover, our estimated rates of FI reflect those reported by FAO and the relative status of countries: The FI rate is highest in Sierra Leone (88.3%), followed by Mozambique (57.7%), Uganda (40.8%), and Tanzania (28.4%). However, except for Mozambique, our FI rates are significantly lower than those of the FAO as discussed in the limitations below.
Primarily and in line with prospective studies [23], we found that both–COVID-19 and FI–independently presented significant risk factors for GAD. Statistical significance is determined using a threshold of p < 0.05. Moreover, the direct effect of moderate/severe FI –the preceding persistent threat– is substantively stronger than the direct exposure to COVID-19: ORCov-19 = 1.7 vs. ORFI = 2.9; while the GAD risk doubles in face of COVID-19 exposure, it triples with a moderate/severe level of FI. Whether this is due to its potentially preceding character, or the severity of threat warrants further exploration. Importantly however, our results suggest that moderate/severe FI further emerges as a mediator for the relation of COVID-19 and GAD explaining 9.4% of the total effect of COVID-19 on GAD. Unsurprisingly, the number of dependents (<17 years) presented as a risk factor and higher SES protected from GAD. Interestingly, we did not find an increased risk for women –a risk factor for GAD in many other studies [49]. This may indicate that gender disparity decreases as persistent threats to survival increase; further analyses are however required to understand this aspect.
Limitations
Acknowledging the limitations inherent in our study, we stress that our analysis can only estimate associations and not infer causal effects due to the cross-sectional nature of the observational data. Moreover, FI prevalence might be underestimated due to the sampling strategy via mobile phones. For the 2019–2021 timeframe, an estimated 79% of the adult population (<17 years) in Uganda own a cell phone, 75% in Tanzania; 76% in Sierra Leone; and 62% in Mozambique [50]; individuals without a mobile phone potentially show higher FI values. Consequently, GAD prevalence rates might also be higher. However, since we control for household composition and wealth, we guard against possible bias in our analyses. Another limitation is that self-administered instruments such as the GAD-7 may not allow for differential diagnosis, but rather provide complementary information. Nevertheless, sensitivity and specificity tests in validation studies show that GAD-7 has acceptable properties for identifying GAD compared to the established gold standard clinical diagnosis [40].
Conclusion
Our analysis suggests two main insights: Firstly, we learn from our data that about 2–4 in ten individuals –a considerable proportion– in Mozambique, Sierra Leone, Tanzania and Uganda presented with excessive and uncontrollable worries during the COVID-19 pandemic. Secondly, persistent stressors such as COVID-19 and moderate/severe FI but particularly FI contribute significantly to the risk of GAD. What does this tell us about the African experience of the pandemic, its legacy for development and avenues for policy action?
Anxiety induces the action disposition of avoidance or defense. While fueling anxiety may carry the advantage of stronger compliance to contagion containment measures, e.g., [48, 51], it may also cause higher GAD rates (amongst other consequences): For instance, a meta-analysis with 72,585 participants [52] revealed that participants with GAD presented with a higher incidence of lifetime perpetration of intimate partner violence. Assessing the transgenerational impact of GAD, Woodruff et al. found mothers with high anxiety levels less engaged with their children [53] and Moore et al. found less warmth, and higher levels of control and criticism [54]. Other transgenerational studies consistently indicate high GAD incidence rates in the offspring. Moreover, experimental laboratory studies show that patients with GAD are more likely to accept and react less strongly to unfair decision [55]. Thus, community-level social corrective reactions may decline while actual and subjective safety and stability in the families may decrease. Higher levels of day-to-day violence in communities and families should be considered as immediate consequence alongside with additional waves of migration. This indicates priority areas for peri- and post-pandemic development programs which include the reduction of violence at the family and community level, as well as an increase in social support.
Moreover, our findings underscore the detrimental effects of concurring persistent stressors on GAD risk. In contrast to other risk factors for anxiety disorders highlighted in previous research, such as immediate threats to survival (psychological trauma), genetic predisposition, and/or health status, we broaden the focus to include persistent threats to survival. In this context, the array of possible policy responses expands: Ensuring that all people can meet their basic needs would not only address these long-term stressors but would also have an important multiplier function. Thus, our findings have immediate policy implications for supporting food programs, as food security is a fundamental determinant of resilience and particularly important when other threats to human life arise. Moreover, addressing food insecurity lends itself more readily to population-wide interventions [56]. Thus, even during global health crises such as the COVID-19 pandemic, addressing FI as a key driver of GAD should be a top priority for policymakers.
Ethics Statement
The studies involving humans were approved by the ethical commission of UNU-WIDER. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin because data was collected using a mobile phone survey. Before the interview, informed oral consent was obtained from all individual participants included in the study by reading out the consent statement at the start of the interviews. The statement contains information regarding the purpose of the interview and the confidentiality of their personal information. The statement also contains information regarding the respondent’s rights to refuse to respond to any individual question or the entire interview.
Author Contributions
JB: Conceptualization, formal analysis, methodology, visualization, writing–original draft, writing–review and editing. AK: Conceptualization, writing–original draft, writing–review and editing. LA: Conceptualization, writing–original draft, writing–review and editing. MR: Formal analysis, funding acquisition, methodology, writing–review and editing. AH: Funding acquisition, supervision, writing–review and editing. WS: Conceptualization, methodology, funding acquisition, supervision, writing–review and editing. TB: Conceptualization, methodology, funding acquisition, supervision, writing–review and editing. All authors contributed to the article and approved the submitted version.
Funding
The project on which this paper is based was funded by the Federal Ministry of Education and Research (BMBF) under the funding code 01KI20533A and 01KI20533B as well as by the Alexander von Humboldt Foundation.
Conflict of Interest
The authors declare that they do not have any conflicts of interest.
Acknowledgments
For excellent research assistance, we thank Dorothea von Kalnein and Taiwo Oludare Abioye. We thank James Ward Khakshi (BRAC, Uganda) and Andreas Kokott (Intercampus, Mozambique) for their excellent coordination of the phone survey data collection in Sierra Leone, Tanzania and Uganda as well as Mozambique, respectively. The responsibility for the content of this publication lies with the authors.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/ijph.2023.1606369/full#supplementary-material
References
1. GBD 2019 Mental Disorders Collaborators. Global, Regional, and National Burden of 12 Mental Disorders in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry (2022) 9(2):137–50. doi:10.1016/S2215-0366(21)00395-3
2. American Psychiatric Associaton (APA). Diagnostic and Statistical Manual of Mental Disorders: DSM-5™. 5th ed. Washington, DC: American Psychiatric Publishing, Inc (2013).
3. Stein, MB, and Sareen, J. Clinical Practice. Generalized Anxiety Disorder. New Engl J Med (Nejm) (2015) 373(21):2059–68. doi:10.1056/NEJMcp1502514
4. Ruscio, AM, Hallion, LS, Lim, CCW, Aguilar-Gaxiola, S, Al-Hamzawi, A, Alonso, J, et al. Cross-Sectional Comparison of the Epidemiology of DSM-5 Generalized Anxiety Disorder Across the Globe. JAMA Psychiatry (2017) 74(5):465–75. doi:10.1001/jamapsychiatry.2017.0056
5. Methley, AM, Campbell, S, Chew-Graham, C, McNally, R, and Cheraghi-Sohi, S. PICO, PICOS and SPIDER: A Comparison Study of Specificity and Sensitivity in Three Search Tools for Qualitative Systematic Reviews. BMC Health Serv Res (2014) 14(1):579–10. doi:10.1186/s12913-014-0579-0
6. Agberotimi, SF, Akinsola, OS, Oguntayo, R, and Olaseni, AO. Interactions Between Socioeconomic Status and Mental Health Outcomes in the Nigerian Context Amid COVID-19 Pandemic: A Comparative Study. Front Psychol (2020) 11:559819. doi:10.3389/fpsyg.2020.559819
7. Ayazi, T, Lien, L, Eide, A, Swartz, L, and Hauff, E. Association Between Exposure to Traumatic Events and Anxiety Disorders in a Post-Conflict Setting: A Cross-Sectional Community Study in South Sudan. BMC Psychiatry (2014) 146. doi:10.1186/1471-244X-14-6
8. Boateng, GO, Doku, DT, Enyan, NIE, Owusu, SA, Aboh, IK, Kodom, RV, et al. Prevalence and Changes in Boredom, Anxiety and Well-Being Among Ghanaians During the COVID-19 Pandemic: A Population-Based Study. BMC Public Health (2021) 21:985. doi:10.1186/s12889-021-10998-0
9. Bhagwanjee, A, Parekh, A, Paruk, Z, Petersen, I, and Subedar, H Prevalence of Minor Psychiatric Disorders in an Adult African Rural Community in South Africa. Psychol Med (1998) 28 (5):1137–1147. doi:10.1017/s0033291798006965
10. Elhadi, M, Msherghi, A, Khaled, A, Alsoufi, A, Alhadi, A, Kareem, A, et al. Impact of Lockdown Due to the COVID-19 Pandemic on Mental Health Among the Libyan Population. PLoS ONE (2022) 17(4):e0267426. doi:10.1371/journal.pone.0267426
11. Gureje, O, Lasebikan, VO, Kola, L, and Makanjuola, VA Lifetime and 12-Month Prevalence of Mental Disorders in the Nigerian Survey of Mental Health and Well-Being. Br J Psychiatry (2006):188465–188471. doi:10.1192/bjp.188.5.465
12. Hollifield, M, Katon, W, Spain, D, and Pule, L Anxiety and Depression in a Village in Lesotho, Africa: A Comparison With the United States. Br J Psychiatry (1990):156343–156350. doi:10.1192/bjp.156.3.343
13. Jenkins, R, Othieno, C, Ongeri, L, Sifuna, P, Ongecha, M, Kingora, J, et al. Common Mental Disorder in Nyanza Province, Kenya in 2013 and its Associated Risk Factorsan Assessment of Change Since 2004, Using a Repeat Household Survey in a Demographic Surveillance Site. BMC Psychiatry (2015):15309. doi:10.1186/s12888-015-0693-5
14. Matsungo, TM, and Chopera, P. Effect of the COVID-19-Induced Lockdown on Nutrition, Health and Lifestyle Patterns Among Adults in Zimbabwe. BMJ Nutr Prev Health (2020) 3:205–12. doi:10.1136/bmjnph-2020-000124
15. Suliman, S, Stein, DJ, Myer, L, Williams, DR, and Seedat, S Disability and Treatment of Psychiatric and Physical Disorders in South Africa. J Nerv Ment Dis (2010) 198(1):8–15. doi:10.1097/NMD.0b013e3181c81708
16. Spitzer, RL, Kroenke, K, Williams, JBW, and Löwe, B. A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD-7. Arch Intern Med (2006) 166(10):1092–7. doi:10.1001/archinte.166.10.1092
17. Williams, DR, Herman, A, Stein, DJ, Heeringa, SG, Jackson, PB, Moomal, H, et al. Twelve-Month Mental Disorders in South Africa: Prevalence, Service Use and Demographic Correlates in the Population-Based South African Stress and Health Study. Psychol Med (2008) 38(2):211–20. doi:10.1017/S0033291707001420
18. Wondimagegnehu, A, Funk, M, and Gakurah, T. WHO Profile on Mental Health in Development (WHO proMIND). Sierra Leone. Geneva: WHO (2012).
19. Paulus, MP, and Yu, AJ. Emotion and Decision-Making: Affect-Driven Belief Systems in Anxiety and Depression. Trends Cogn Sci (2012) 16(9):476–83. doi:10.1016/j.tics.2012.07.009
20. Hettema, JM, Neale, MC, and Kendler, KS. A Review and Meta-Analysis of the Genetic Epidemiology of Anxiety Disorders. Am J Psychiatry (2001) 158(10):1568–78. doi:10.1176/appi.ajp.158.10.1568
21. Aktar, E, Nikolić, M, and Bögels, SM. Environmental Transmission of Generalized Anxiety Disorder From Parents to Children: Worries, Experiential Avoidance, and Intolerance of Uncertainty. Dialogues Clin Neurosci (2017) 19(2):137–47. doi:10.31887/DCNS.2017.19.2/eaktar
22. Moreno-Peral, P, Conejo-Cerón, S, Motrico, E, Rodríguez-Morejón, A, Fernández, A, García-Campayo, J, et al. Risk Factors for the Onset of Panic and Generalised Anxiety Disorders in the General Adult Population: A Systematic Review of Cohort Studies. J Affect Disord (2014) 168:337–48. doi:10.1016/j.jad.2014.06.021
23. Zhang, X, Norton, J, Carrière, I, Ritchie, K, Chaudieu, I, and Ancelin, ML. Risk Factors for Late-Onset Generalized Anxiety Disorder: Results From a 12-Year Prospective Cohort (The ESPRIT Study). Transl Psychiatry (2015) 5(3):e536. doi:10.1038/tp.2015.31
24. Wilker, S, Pfeiffer, A, Kolassa, S, Koslowski, D, Elbert, T, and Kolassa, IT. How to Quantify Exposure to Traumatic Stress? Reliability and Predictive Validity of Measures for Cumulative Trauma Exposure in a Post-Conflict Population. Eur J Psychotraumatol (2015) 6:28306. doi:10.3402/ejpt.v6.28306
25. World Health Organization Regional Office for Africa. Six in Seven COVID-19 Infections Go Undetected in Africa (2021). Available at: https://www.afro.who.int/news/six-seven-covid-19-infections-go-undetected-africa (Accessed November 01, 2022).
26. Food and Agriculture Organization of the United Nations (FAO). An Introduction to the Basic Concepts of Food Security. FAO (2008).
27. Food and Agriculture Organization of the United Nations (FAO). International Fund for Agricultural Development (IFAD), United Nations Children’s Fund (UNICEF) the State of Food Security and Nutrition in the World 2021: Transforming Food Systems for Food Security, Improved Nutrition Transforming Food Systems and Affordable Healthy Diets for All. Rome: FAO, IFAD, UNICEF, WFP and WHO (2021).
28. Bello, UM, Cheong, AMY, Kannan, P, Salihu, D, Miller, T, Pun, JW, et al. Prevalence of Anxiety and Depression Among the General Population in Africa During the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. Front Public Health (2022) 10:814981. doi:10.3389/fpubh.2022.814981
29. Paudel, J. Home Alone: Implications of COVID-19 for Mental Health. Soc Sci Med (2021) 285:114259. doi:10.1016/j.socscimed.2021.114259
30. COVID-19 Mental Disorders Collaborators Global Prevalence and Burden of Depressive and Anxiety Disorders in 204 Countries and Territories in 2020 Due to the COVID-19 Pandemic. The Lancet (2021) 398(10312):1700–12. doi:10.1016/S0140-6736(21)02143-7
31. Trudell, JP, Burnet, ML, Ziegler, BR, and Luginaah, I. The Impact of Food Insecurity on Mental Health in Africa: A Systematic Review. Soc Sci Med (2021) 278:113953. doi:10.1016/j.socscimed.2021.113953
32. Weaver, LJ, Owens, C, Tessema, F, Kebede, A, and Hadley, C. Unpacking the "Black Box" of Global Food Insecurity and Mental Health. Soc Sci Med (2021) 282:114042. doi:10.1016/j.socscimed.2021.114042
33. Elgar, FJ, Pickett, W, Pförtner, TK, Gariépy, G, Gordon, D, Georgiades, K, et al. Relative Food Insecurity, Mental Health and Wellbeing in 160 Countries. Soc Sci Med (2021) 268:113556. doi:10.1016/j.socscimed.2020.113556
34. Jones, AD. Food Insecurity and Mental Health Status: A Global Analysis of 149 Countries. Am J Prev Med (2017) 53(2):264–73. doi:10.1016/j.amepre.2017.04.008
35. Stojetz, W, Ferguson, NTN, Baliki, G, Díaz, O, Elfes, J, Esenaliev, D, et al. The Life With Corona Survey. Soc Sci Med (2022) 306:115109. doi:10.1016/j.socscimed.2022.115109
36. Brück, T, and Regassa, MD. Usefulness and Misrepresentation of Phone Surveys on COVID-19 and Food Security in Africa. Food Sec (2023) 15(2):423–53. doi:10.1007/s12571-022-01330-8
37. Buguzi, S. Covid-19: Counting the Cost of Denial in Tanzania. BMJ (2021) 373:n1052. doi:10.1136/bmj.n1052
38. Innovations for Poverty Action (IPA). Remote Surveying in a Pandemic: Research Synthesis. IPA (2020).
39. Valliant, R, and Dever, JA. Survey Weights: A Step-by-Step Guide to Calculation. College Station Texas: Stata Press A Stata Press Publication StataCorp LLC (2018).
40. Plummer, F, Manea, L, Trepel, D, and McMillan, D. Screening for Anxiety Disorders With the GAD-7 and GAD-2: A Systematic Review and Diagnostic Metaanalysis. Gen Hosp Psychiatry (2016) 39:24–31. doi:10.1016/j.genhosppsych.2015.11.005
41. Mughal, AY, Devadas, J, Ardman, E, Levis, B, Go, VF, and Gaynes, BN. A Systematic Review of Validated Screening Tools for Anxiety Disorders and PTSD in Low to Middle Income Countries. BMC Psychiatry (2020) 20(1):338. doi:10.1186/s12888-020-02753-3
42. Adepoju, P. Closing Africa's Wide COVID-19 Testing and Vaccination Gaps. The Lancet Microbe (2021) 2(11):e573. doi:10.1016/S2666-5247(21)00284-6
43. Food and Agriculture Organization of the United Nations (FAO). Methods for Estimating Comparable Prevalence Rates of Food Insecurity Experienced by Adults Throughout the World. Rome: FAO (2016).
44. Cafiero, C, Viviani, S, and Nord, M. Food Security Measurement in a Global Context: The Food Insecurity Experience Scale. Measurement (2018) 116:146–52. doi:10.1016/j.measurement.2017.10.065
45. Vyas, S, and Kumaranayake, L. Constructing Socio-Economic Status Indices: How to Use Principal Components Analysis. Health Policy Plan (2006) 21:459–68. doi:10.1093/heapol/czl029
46. Mehmetoglu, M. Medsem: A Stata Package for Statistical Mediation Analysis. IJCEE (2018) 8(1):63. doi:10.1504/ijcee.2018.10007883
47. Jia, R, Ayling, K, Chalder, T, Massey, A, Gasteiger, N, Broadbent, E, et al. The Prevalence, Incidence, Prognosis and Risk Factors for Symptoms of Depression and Anxiety in a UK Cohort During the COVID-19 Pandemic. BJPsych Open (2022) 8(2):e64–9. doi:10.1192/bjo.2022.34
48. Solomou, I, and Constantinidou, F. Prevalence and Predictors of Anxiety and Depression Symptoms During the COVID-19 Pandemic and Compliance With Precautionary Measures: Age and Sex Matter. Int J Environ Res Public Health (2020) 17(14):4924. doi:10.3390/ijerph17144924
49. Jalnapurkar, I, Allen, M, and Pigott, T. Sex Differences in Anxiety Disorders: A Review. J Psychiatry Depress Anxiety (2018) 4(1):1–9. doi:10.24966/pda-0150/100011
50. Afrobarometer. Afrobarometer Data (2022). [Data set], [Mozambique, Sierra Leone, Tanzania, Uganda], [Round 8], [Years 2019/2021] Available at: http://www.afrobarometer.org (Accessed February 13, 2023).
51. Copping, LT. Anxiety and Covid-19 Compliance Behaviors in the UK: The Moderating Role of Conspiratorial Thinking. Pers Individ Dif (2022) 192:111604. doi:10.1016/j.paid.2022.111604
52. Oram, S, Trevillion, K, Khalifeh, H, Feder, G, and Howard, LM. Systematic Review and Meta-Analysis of Psychiatric Disorder and the Perpetration of Partner Violence. Epidemiol Psychiatr Sci (2014) 23(4):361–76. doi:10.1017/S2045796013000450
53. Woodruff-Borden, J, Morrow, C, Bourland, S, and Cambron, S. The Behavior of Anxious Parents: Examining Mechanisms of Transmission of Anxiety From Parent to Child. J Clin Child Adolesc Psychol (2002) 31(3):364–74. doi:10.1207/S15374424JCCP3103_08
54. Moore, PS, Whaley, SE, and Sigman, M. Interactions Between Mothers and Children: Impacts of Maternal and Child Anxiety. J Abnorm Psychol (2004) 113(3):471–6. doi:10.1037/0021-843X.113.3.471
55. Robson, SE, Repetto, L, Gountouna, VE, and Nicodemus, KK. A Review of Neuroeconomic Gameplay in Psychiatric Disorders. Mol Psychiatry (2020) 25(1):67–81. doi:10.1038/s41380-019-0405-5
Keywords: generalized anxiety disorder, mental health, COVID-19, food insecurity, Africa
Citation: Beck J, Koebach A, Abreu L, Regassa MD, Hoeffler A, Stojetz W and Brück T (2024) COVID-19 Pandemic and Food Insecurity Fuel the Mental Health Crisis in Africa. Int J Public Health 68:1606369. doi: 10.3389/ijph.2023.1606369
Received: 03 July 2023; Accepted: 18 December 2023;
Published: 12 January 2024.
Edited by:
Daryna Pavlova, Ukrainian Institute for Social Research After Olexander Yaremenko, UkraineReviewed by:
Rahim Badrfam, Alborz University of Medical Sciences, IranEtheldreda Nakimuli-Mpungu, Makerere University College of Health Sciences, Uganda
One reviewer who chose to remain anonymous
Copyright © 2024 Beck, Koebach, Abreu, Regassa, Hoeffler, Stojetz and Brück. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jule Beck, anVsZS5iZWNrQHVuaS1rb25zdGFuei5kZQ==
 Jule Beck
Jule Beck Anke Koebach
Anke Koebach Liliana Abreu
Liliana Abreu Mekdim Dereje Regassa
Mekdim Dereje Regassa Anke Hoeffler
Anke Hoeffler Wolfgang Stojetz3
Wolfgang Stojetz3 Tilman Brück
Tilman Brück