- Department of Pharmacy Practice, ISF College of Pharmacy, Moga, India
Objective: The study aimed to investigate the pharmacist interventions in minimizing drug-related problems in diabetes with co-existing hypertension.
Methods: Prospective observational study.
Results: Overall, a total of 628 interventions were recommended for 1,914 patients during the 5-year period of study. Among all the interventions, the majority were suggested regarding “substituting the drug” (39%), change in frequency of administration (25%), and addition of drug (14%). Patient compliance status was found significant (p = 0.29 ± 0.07).
Conclusion: Clinical pharmacists have a crucial role in minimizing drug related problems. Particularly, there should be a greater emphasis on patient counselling and patient follow-up.
Introduction
Patient safety is the priority of all healthcare workers. However, the treatment and management of co-morbid conditions has proven to be challenging even to the healthcare professionals. This is because the available clinical guidelines are mainly based on the assumption that patients suffer from a single disease (1). Diabetes co-existing with hypertension (HTN) is a very common occurrence especially in type 2 DM (Diabetes Mellitus) patients. According to The Global Burden of Disease study HTN and DM have been identified to be the leading cause of untimely deaths and disability globally (2).
It is globally estimated that the prevalence of type 2 diabetes mellitus (T2DM) will be 366 million by 2030 whereas that of hypertension will be 1.56 billion adults by 2025 (3, 4). The prevalence of hypertension in diabetic patients is almost double that of non-diabetic and the patients with hypertension as a comorbidity are at a higher risk of mortality and cardiovascular disease development (5, 6). A study by Geldsetzer et al (7) which involved 1.3 million adults in India revealed that this comorbid condition was more prevalent in the middle and old age. Having a team approach (i.e., physicians, nurses, clinical pharmacists, dieticians, etc.) in the therapy of DM with HTN patients has shown to be effective (8). Managing the blood pressure levels in diabetic patients, adherence to both pharmacological and non-pharmacological treatments such as exercising, etc., and use of proper medication with minimum adverse effects are some of the methods that can be used to reduce the risk of developing hypertension in diabetic patients.
Clinical pharmacists are specially trained personnel on pharmacotherapy and their major role in healthcare setting is to ensure safe, effective, and judicious use of medications in the patients (9). They identify drug related problems (DRPs) which are recurrent in hospitals particularly during prescribing, dispensing, administration and adherence of the drugs (10). A drug related problem is a negative outcome of a medication administered to a patient and fortunately, they are mainly preventable. Clinical pharmacists have been encouraged to use the SOAP (Subjective, objective, assessment, plan) or FARM (Findings, assessment of findings, resolution of the problems and monitoring) progress note in order to easily identify and report DRPs (11, 12). Common outcomes of DRPs in DM with HTN patients include: decreased quality of life, longer hospital stays, and increased costs (13).
The inclusion of clinical pharmacists in the healthcare team helps address the challenges related to DRPs as they offer valuable interventions on case-by-case basis. A randomized clinical trial study showed that the addition of clinical pharmacist to the healthcare team resulted in decreased mortality and healthcare costs. The pharmacist interventions were on the drug selection, dosages and monitoring needs during the study (14). Additionally, patient counselling and follow-up is another common pharmacist intervention. Clinical pharmacists have therefore become an integral part of quality healthcare delivery systems even as more emphasis is being laid on team care-based model (15, 16).
The absence of long-term published describing the clinical pharmacists’ interventions in India was the rationale for conducting this study. Therefore, the main objective of this study was to investigate the pharmacist interventions in minimizing drug-related problems in diabetes with co-existing hypertension in the medicine departments of three hospitals in Punjab, India.
Methods
Setting
In this observational study, all the patients referred to the medicine department of the three different hospitals of Moga, city located in Punjab state of India (17, 18) were enrolled in the study.
Study Design and Patient Selection
For this multi-centre prospective study, patients were included from November 2015 to December 2020. In the present study, all the interventions of clinical pharmacists made over 5 years were included. The present study is part of a completed research entitled “drug utilization study of diabetes and hypertension at tertiary care hospital.” The population size of the Moga city was found N = 2.98 lakhs (17). The sample size is calculated with the ‘Epi Info’ software (19, 20). A total of 2,622 patients suffering from diabetes mellitus (D.M.) and hypertension (HTN) were screened during the study period. Out of the 2,622 patients, 1,914 patients were enrolled in the statistical analysis. A total of 708 patients were excluded while analysing data because of missing value; some patients were lost during the follow-up. Patients diagnosed with diabetes mellitus and hypertension with or without complications admitted to (IPD) in-patient department of the hospital were assessed. The study’s inclusion criteria include patients visiting the hospital for follow-up, both genders with age >18 years, diabetes with co-existing hypertension patients and those that were willing to participate. Institutional Ethics Committee (IEC-ISFCP, Moga) ISF College of Pharmacy, Moga, Punjab approved the study (Ref. No. ECR/296/Indt/PB/2017/ISFCP/136). The confidence interval of the study was chosen as 97% (21). All statistical tests were carried out at the two-sided 3% significance level by statistical analysis software SPSS ver. 25.
Data collection
Figure 1 gives a simple flow of how data was collected in our study. A pre-validated data collection form which includes a questionnaire containing 105 variables was used to collect data after obtaining consent from the patient. The variables include: Age, gender, type of ADRs, type of drug interactions, type of drug related problem, type of pharmacist intervention, cost, length of hospital stay. All study costs were recorded in INR, and pharmacoeconomic variables were converted to USD (INR: 73.36 = 1 USD).
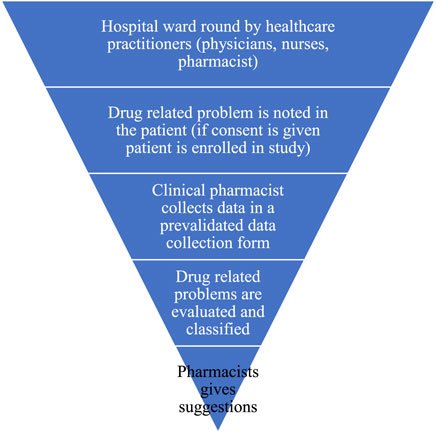
FIGURE 1. Description of the data collection procedure (Drug utilization study of diabetes and hypertension at tertiary care hospitals, India, five years study, 2020).
The mean age of the patients suffering from diabetes mellitus (type-I and type-II) with co-existing hypertension (µ) and standard deviation (S.D.) was found to be (M = 53.85, SD = 11.54) years. The normality test was performed, which was found normally distributed Kolmogorov-Smirnov and Shapiro-Wilk (p = 0.36 and 0.223), respectively (22–24).
Ethics Approval
The present study was approved by IEC of ISF College of Pharmacy, Moga, Punjab (Ref. No. ECR/296/Indt/PB/2017/ISFCP/136).
Results
Out of 1,914 patients, 914 were male (47.8%) and the females were 1,000 (53.65%).
During the study, 63 different types of ADRs were detected by the clinical pharmacist in 628 (32.8%) of the patients. The majority of the patients were suffering from adverse drug reactions like hypotension (3.3%), hypoglycaemia (3.2%), mild itching or rash (1.5%), swelling in their feet or ankles, severe drowsiness (1.4%) followed by skin rashes (1.0%). In 1,914 patients, 42 different kinds of drug interactions were observed in 1,612 cases. The majority of the drug interactions were seen between Insulin + Emeril 226 (11.8%) followed by 111 (5.8%) Emeril + PCM + Diclofenac. The drug-related problems include inappropriate drug form (6.1%), inappropriate drug (4.6%), no clear indication for drug use (4.6%), contraindication for the drug (4.1%), no drug prescribed but clear indication (3.8%), and duplication of a therapeutic group or active ingredient (1.5%).
Additionally, change in frequency of administration was found to be 153 (8.0%), addition of drug 89 (4.6%), change in the duration of therapy 50 (2.6%) and change in drug dose 33 (1.7%). Pharmaceutical aid was included in 22 (1.1%) of the cases.
Tables 1, 2 below demonstrates the characteristics of the drug prescriptions and types of drug related problems noted and their statistics (Tables 3, 4).
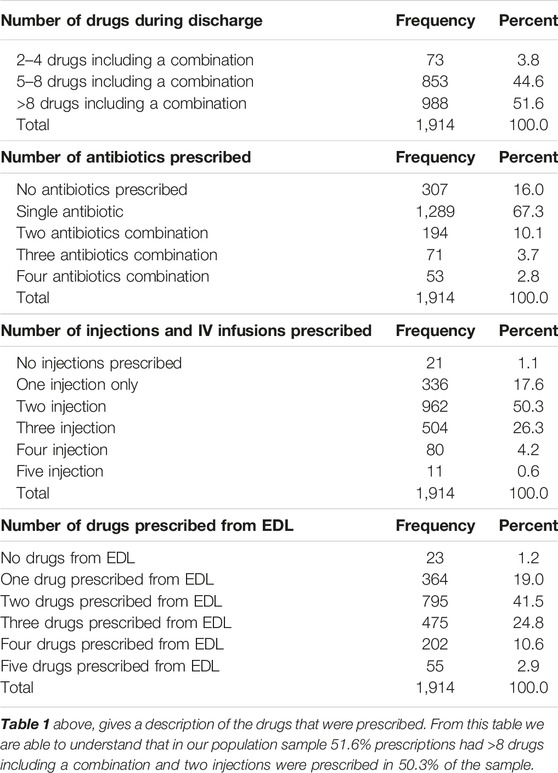
TABLE 1. Characteristics of the drug prescriptions (Drug utilization study of diabetes and hypertension at tertiary care hospitals, India, five years study, 2020).
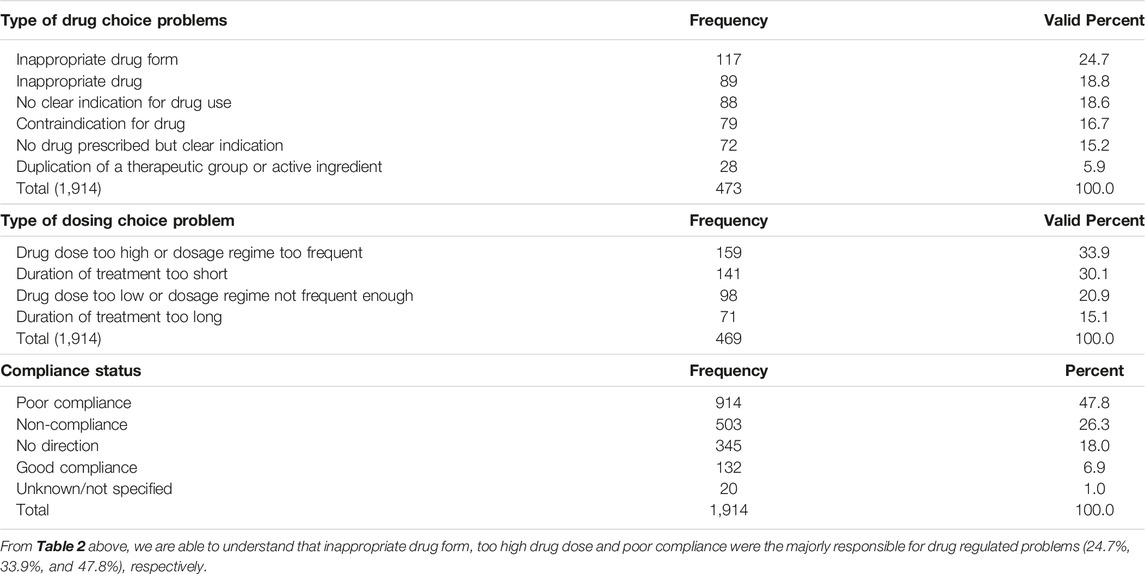
TABLE 2. Types of drug related problems noted (Drug utilization study of diabetes and hypertension at tertiary care hospitals, India, five years study, 2020).
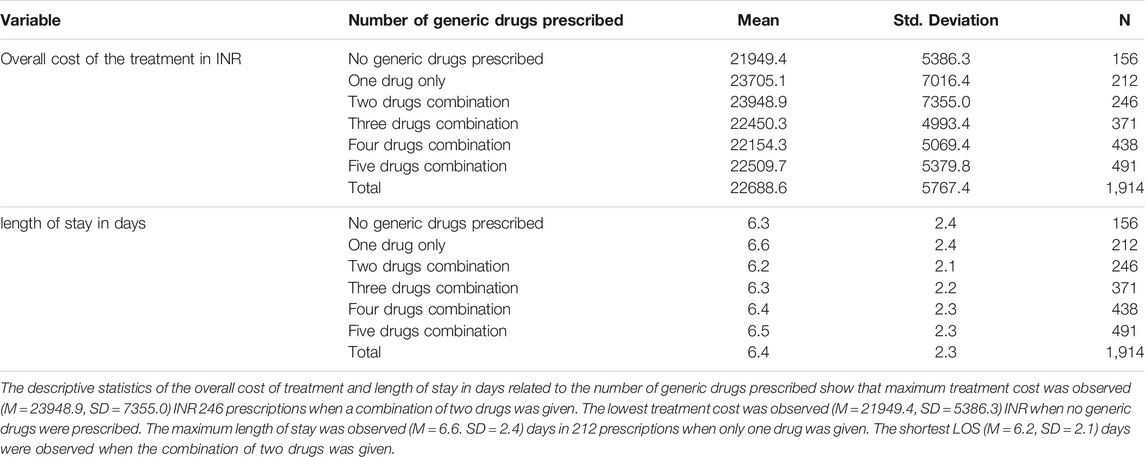
TABLE 3. Descriptive statistics: Overall cost of the treatment and length of stay in days (Drug utilization study of diabetes and hypertension at tertiary care hospitals, India, five years study, 2020).
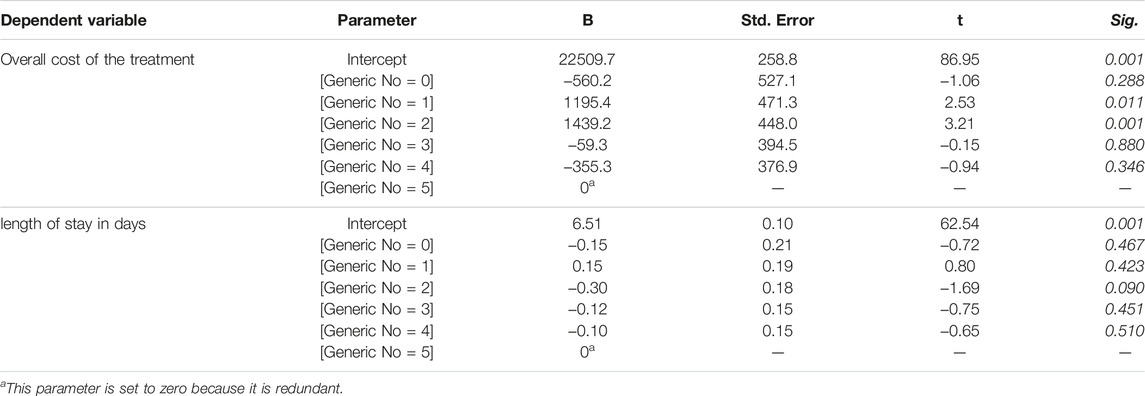
TABLE 4. Parameter estimates: DV- Number of generic drugs prescribed (Drug utilization study of diabetes and hypertension at tertiary care hospitals, India, five years study, 2020).
The mean number of generic drugs prescribed was found to be 3.15 whereas the maximum drugs was found to be five. The mean number of antibiotics prescribed was found to be 1.10 whereas the maximum number of antibiotics prescribed was found to be four. On evaluation of number of injections prescribed it was observed that the mean number of injections prescribed was found 2.17 whereas the maximum number of injections prescribed was found to be five in a day. The mean number of drugs prescribed from essential drug list (EDL) 2.33 whereas the maximum number of drugs prescribed from essential drug list was found five.
Statistics of the Drugs Prescribed During Study
Supplementary File S1 demonstrates how the number of generic drugs prescribed showed that maximum times five drugs were prescribed in 491 patients followed by four drugs in 438 patients.
Brief Summary of the Statistical Analysis We Conducted
Multivariate test was applied to compare no. of generic drugs prescribed with overall cost of treatment and length of stay.
Levene’s test of equality of error was found significant as p-value was >0.03 which assumes equality has been maintained between the samples.
The table test of between. subject effects shows that both the independent variable, length of stay and overall cost of treatment was found significant as p-value was found to be p = 0.001 and p = 0.030, respectively.
Cost is affecting more as compared to length of stay as p-value was found to be 0.001 and 0.030, respectively.
Overall cost: F (5, 1913) 5.2, p = 0.001, Length of stay: F (5, 1913) 1.0, p = 0.030.
The parameter estimates describe changes occurs in overall cost of treatment and length of stay.
The data reveals that the cost of treatment increased by β = 1439.2 for the patient prescribed 2 generic drugs as compared to above 5 drugs and p-value was found 0.001 and 0.011, respectively.
Supplementary File S2 has been provided which reveals that the number of genetic drugs prescribed as dependent variable shows significant results for overall cost of treatment F (5, 1908) = 5.2, p = 0.001 and length of stay in days F (5, 1908) = 1, p = 0.030.
The parameter estimates table for a dependent variable number of generic drugs prescribed shows that [Generic No = 5] as standard for overall cost of the treatment and length of stay (L.O.S) in days. The data revealed that the overall cost of treatment could be lower by β = −355.3 INR if four generic drugs were prescribed instead of five, followed by an increase in overall treatment cost were observed for two generic drugs by β = 1439.2 INR. It was also found that length of stay in days is not affected as much. In most of the groups the LOS was lowered by −0.10 to −0.30 days as shown in Table 4.
Supplementary File S3 has been provided which gives a summary of the drug related problems seen in our study (Punjab, India. 2020).
Discussion
Embracing clinical pharmacy in treatment of patients has shown to be effective particularly in minimizing the economic burden and development of adverse drug reactions. Pharmacist interventions within a multi-disciplinary team have proven to be vital especially in conducting drug reviews. Drug review is a major component of pharmacy practice and it involves assessment of the medications given to patients and their possible outcomes (intended or unintended) (25, 26).
Inappropriate drug form and dose being too high were the main drug related problems discovered in our study. Another study by Rasool et al (27) showed a similar outcome with inappropriate drug from being responsible for 39.75% of the medication errors seen.
A trial conducted by Sosale et al showed that 46% of patients diagnosed with type 2 diabetes mellitus are under the age of 40 (mean age was 34.7 ± 4.2 years) whereas the mean age of our study population was 54 years (28). The reason for this discordance in the age may be due to the different aims of the studies. Their study was tailored towards determining the onset of T2DM in young patients whereas our study had no specific target age group. Drug interactions were seen in 84.2% of our patients which was a little higher than the 70% which was seen in a study conducted by Sankar et al (29). Interestingly, their study only involved 50 patients which may not be able to give a proper representation of the larger population and hence this small difference. A study by Zazuli et al showed that inappropriate drug selection and inappropriate dosage selection contributed 25.3% and 4.4%, respectively occurrence of drug related problems. In our study, inappropriate drug form and inappropriate drug given contributed 6.11% and 4.65%, respectively in the 1,914 cases. Additionally, substituting the drug was the main intervention given by clinical pharmacists as seen in Figure 2. In their study, drug choice problem and dosing choice problem contributed 88.2% towards drug related problems (DRPs) whereas it only contributed 49.2% in our study. This was due to the fact their study was a prospective study for 3 months. In our study, it was revealed that patient compliance status was the most significant factor influencing the DRPs (30).
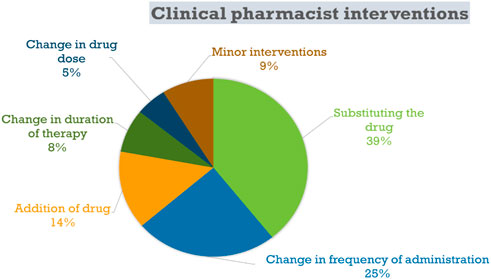
FIGURE 2. Summary of the clinical pharmacist interventions seen in our study (Drug utilization study of diabetes and hypertension at tertiary care hospitals, India, five years study, 2020).
Our study revealed that pharmacists play a major role especially in patient follow-up and that patient compliance is very critical in ensuring desired therapeutic outcome. Also, as seen from other studies proper counselling, patient education and creating public health awareness improves the patients’ compliance (31). Some studies have shown a very good compliance rate of DM with HTN patients such as one conducted by Rao et al where 83.6% of the diabetics were compliant to their medications (32). Poor compliance and non-compliance were discovered to be the most prevalent medication related problem in our patients as they contributed 47.3% and 26.3%, respectively. A recent study has called on the National Programme for Control of Cancer, Diabetes, Cardiovascular Diseases, and Stroke (NPCDCS) in India to conduct more health awareness programmes especially in Punjab where there is a high rate of NCDs (Non-Communicable Diseases) (33). Multidisciplinary collaboration among the healthcare workers such as nurses, pharmacists and physicians has also proven to be a better means of achieving better patient care (34). This study is the first of its kind in North India because the sample size used in this study can be used to give an insight into the factors that are responsible for drug related problems in DM with HTN patients. This study was a 5-year study hence the results have a better representation generally of the kind of interventions involving pharmacists within our region. Furthermore, our study reveals the need for a more collaborative approach in medication treatment with the clinical pharmacist expected to play a great role in patient education as well as counselling.
Limitation of Our Study
The study was limited to 3 hospitals only. In North India, many hospitals exist and similar study needs to be conducted for a better overview.
Impact of Findings on Practice
• Clinical pharmacists are an asset to the healthcare team and patients.
• Most of the drug related problems can be averted through proper patient counselling.
• Patient compliance should not be overlooked.
Conclusion
Our study concludes that pharmacist’s intervention is critical in the improvement of health outcomes in DM with HTN patients. Moreover, our study revealed that patient compliance was found as the greatest contributor to drug related problems.
Ethics Statement
The studies involving human participants were reviewed and approved by IEC of ISF College of Pharmacy, Moga, Punjab (Ref. No. ECR/296/Indt/PB/2017/ISFCP/136). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
IO: Major contributor in writing, drafting and editing of the manuscript. MV: Data curation, original draft preparation. MA: Visualization, investigation. AS: Supervision, data collection, editing the manuscript and data analysis.
Conflict of Interest
The authors declare that they do not have any conflicts of interest.
Acknowledgments
We acknowledge the availability of an online pre-print via the link https://assets.researchsquare.com/files/rs-112180/v1/246361af-4f48-4b36-ba84 1a75faa2273a.pdf?c=1631862401 which is similar to the study we conducted however the objectives were different in both studies. We thank the patients for sharing their details and thanks to ISF College of Pharmacy, Moga, Punjab, and SD Thappar, Moga, Garg Hospital, Moga Medicity Punjab Hospital staff for the continuous support provided.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/ijph.2023.1605808/full#supplementary-material
Abbreviations
DBP, diastolic blood pressure; DM, Diabetes mellitus; DRPs, drug related problems; FBS, fasting blood sugar; HTN, hypertension; INR, Indian rupees; RBS, random blood sugar; SBP, systolic blood pressure; USD, United States dollar.
References
1. Whitty, CJ, MacEwen, C, Goddard, A, Alderson, D, Marshall, M, Calderwood, C, et al. Rising to the challenge of Multimorbidity. BMJ (2020) 368. doi:10.1136/bmj.l6964
2.Institute for Health Metrics and Evaluation. Findings from the Global Burden of Disease Study 2017. Seattle: IHME (2018). Availableat: http://www.healthdata.org/sites/default/files/files/policy_report/2019/GBD_2017_Booklet_Issuu_2.pdf (Accessed March 20, 2023).
3. Sarah, W, Roglic, G, Green, A, Sicree, R, and King, H. Global Prevalence of Diabetes: Estimates for the Year 2000 and Projections for 2030. Diabetes Care (2004) 27(5):1047–53. doi:10.2337/diacare.27.5.1047
4. Kearney, PM, Whelton, M, Reynolds, K, Muntner, P, Whelton, PK, and He, J. Global burden of Hypertension: Analysis of Worldwide Data. Lancet (2005) 365(9455):217–23. doi:10.1016/S0140-6736(05)17741-1
5. Paul, B, Sapra, B, Maheshwari, S, and Goyal, R. Role of Losartan Therapy in the Management of Diabetic Hypertension. J Assoc Physicians India (2000) 48(5):514–8.
6. Abdissa, D, and Kene, K. Prevalence and Determinants of Hypertension Among Diabetic Patients in Jimma university Medical center, Southwest Ethiopia, 2019. Diabet Metab Syndr Obes (2020) 13:2317–25. doi:10.2147/DMSO.S255695
7. Geldsetzer, P, Manne-Goehler, J, Theilmann, M, Davies, JI, Awasthi, A, Vollmer, S, et al. Diabetes and Hypertension in India: A Nationally Representative Study of 1.3 Million Adults. JAMA Intern Med (2018) 178(3):363–72. doi:10.1001/jamainternmed.2017.8094
8. Schiff, GD, Klass, D, Peterson, J, Shah, G, and Bates, DW. Linking Laboratory and Pharmacy: Opportunities for Reducing Errors and Improving Care. Arch Intern Med (2003) 163:893–900. doi:10.1001/archinte.163.8.893
9.American College of Clinical Pharmacy. The Definition of Clinical Pharmacy. Pharmacotherapy (2008) 28:816–7.
10. Touchette, DR, Doloresco, F, Suda, KJ, Perez, A, Turner, S, Jalundhwala, Y, et al. Economic Evaluations of Clinical Pharmacy Services: 2006-2010. Pharmacother J Hum Pharmacol Drug Ther (2014) 34:771–93. doi:10.1002/phar.1414
11. Sapkota, B, Shrestha, R, and Giri, S. Community Pharmacy-Based SOAP Notes Documentation. Medicine (Baltimore) (2022) 101(30):e29495. doi:10.1097/MD.0000000000029495
12. Allameh, Z, Mehrpooya, M, Baniasadi, S, and Fahimi, F. Clinical Pharmacy Services in an Iranian Teaching Hospital: Type, Severity, Resolution, and Accuracy. J Res Pharm Pract (2013) 2(1):10–7. doi:10.4103/2279-042X.114083
13. Ayele, Y, Melaku, K, Dechasa, M, Ayalew, MB, and Horsa, BA. Assessment of Drug Related Problems Among Type 2 Diabetes Mellitus Patients with Hypertension in Hiwot Fana Specialized University Hospital, Harar, Eastern Ethiopia. BMC Res Notes (2018) 11(1):728. doi:10.1186/s13104-018-3838-z
14. Gillespie, U, Alassaad, A, Henrohn, D, Garmo, H, Hammarlund-Udenaes, M, Toss, H, et al. A Comprehensive Pharmacist Intervention to Reduce Morbidity in Patients 80 Years or Older: a Randomized Controlled Trial. Arch Intern Med (2009) 169(9):894–900. doi:10.1001/archinternmed.2009.71
15. Kripalani, S, Roumie, CL, Dalal, AK, Cawthon, C, Businger, A, Eden, SK, et al. Effect of a Pharmacist Intervention on Clinically Important Medication Errors after Hospital Discharge: a Randomized Trial. Ann Intern Med (2012) 157(1):1–10. doi:10.7326/0003-4819-157-1-201207030-00003
16. Sebaaly, J, Parsons, LB, Pilch, NA, Bullington, W, Hayes, GL, and Easterling, H. Clinical and Financial Impact of Pharmacist Involvement in Discharge Medication Reconciliation at an Academic Medical Center: A Prospective Pilot Study. Hosp Pharm (2015) 50(6):505–13. doi:10.1310/hpj5006-505
17.P. Directorate of Census Operations. Directorate of Census Operations. In: District Census Handbook. Chandigarh: Moga (2011).
18. Sharma, ML. Punjab-at-a-glance (District wise) 2011," (2012) Availableat: http://www.pbplanning.gov.in/pdf/PunjabGlance2011CompleteVD Graphs.pdf. (Accessed August 24, 2015).
19.CDC. Epi Info 7 - User Guide,” (2016). Availableat: http://www.cdc.gov/epiinfo/pdfs/UserGuide/EI7Full.pdf (Accessed August 24, 2015).
20. Clark, V. Sample Size Determination. Plast Reconstr Surg (1991) 87(3):569–73. doi:10.1097/00006534-199103000-00030
21. Sharma, A, Neha, J, and Ashish, B. Socio-Demographic Characteristics and Drug Related Problems of Patients Presenting to the Emergency Department: General Linear Model and Factorial Analysis. J Pharm Care Heal Syst (2018) 05–03. doi:10.4172/2376-0419.1000198
22. Kafadar, K. Testing for Normality. J Am Stat Assoc (2003) 98(463):765. doi:10.1198/jasa.2003.s285
23. Ghasemi, A, and Zahediasl, S. Normality Tests for Statistical Analysis: A Guide for Non-statisticians. Int J Endocrinol Metab (2012) 10(2):486–9. doi:10.5812/ijem.3505
24. Altman, DG, Gore, SM, Gardner, MJ, and Pocock, SM. Statistical Guidelines for Contributors to Medical Journals. BMJ (1983) 1(2):1489–93. doi:10.1136/bmj.286.6376.1489
25. Dalton, K, and Byrne, S. Role of the Pharmacist in Reducing Healthcare Costs: Current Insights. Integr Pharm Res Pract (2017) 6:37–46. doi:10.2147/IPRP.S108047
26. Jacobi, J. Clinical Pharmacists: Practitioners Who Are Essential Members of Your Clinical Care Team. Rev Médica Clínica Las Condes (2016) 27:571–7. doi:10.1016/j.rmclc.2016.09.002
27. Rasool, MF, Rehman, A, Imran, I, Abbas, S, Shah, S, Abbas, G, et al. Risk Factors Associated with Medication Errors Among Patients Suffering from Chronic Disorders. Front Public Health (2020) 8:531038. doi:10.3389/fpubh.2020.531038
28. Sosale, B, Sosale, AR, Mohan, AR, Kumar, PM, Saboo, B, and Kandula, S. Cardiovascular Risk Factors, Micro and Macrovascular Complications at Diagnosis in Patients with Young Onset Type 2 Diabetes in India: CINDI 2. Indian J Endocrinol Metab (2016) 20(1):114–8. doi:10.4103/2230-8210.172277
29. Sankar, V, Saaed, Y, Joseph, RM, Azizi, H, and Thomas, PM. Serious Drug-Drug Interactions in the Prescriptions of Diabetic Patients. Med Sci (Basel) (2015) 3(4):93–103. doi:10.3390/medsci3040093
30. Zazuli, Z, Rohaya, A, and Ketut Adnyana, I. Drug-Related Problems in Type 2 Diabetic Patients with Hypertension: A Prospective Study. J Basic Clin Pharm (2017) 8(4).
31. Kjeldsen, LJ, Bjerrum, L, Dam, P, Larsen, BO, Rossing, C, Søndergaard, B, et al. Safe and Effective Use of Medicines for Patients with Type 2 Diabetes - A Randomized Controlled Trial of Two Interventions Delivered by Local Pharmacies. Res Soc Adm Pharm (2015) 11(1):47–62. doi:10.1016/j.sapharm.2014.03.003
32. Rao, CR, Kamath, VG, Shetty, A, and Kamath, A. Treatment Compliance Among Patients with Hypertension and Type 2 Diabetes Mellitus in a Coastal Population of Southern India. Int J Prev Med (2014) 5(8):992–8.
33. Thakur, JS, and Nangia, R. Prevalence, Awareness, Treatment, and Control of Hypertension and Diabetes: Results from Two State-wide STEPS Survey in Punjab and Haryana, India. Front Public Health (2022) 10:768471. doi:10.3389/fpubh.2022.768471
Keywords: diabetes, hypertension, adverse drug reactions, length of stay, drug interactions
Citation: Osoro I, Amir M, Vohra M and Sharma A (2023) Pharmacist Interventions in Minimizing Drug Related Problems in Diabetes With Co-Existing Hypertension: A Five-Year Overview and Ground Report From India. Int J Public Health 68:1605808. doi: 10.3389/ijph.2023.1605808
Received: 24 January 2023; Accepted: 23 March 2023;
Published: 03 April 2023.
Edited by:
Bernd Rechel, European Observatory on Health Systems and Policies, BelgiumReviewed by:
Jihene Sahli, University of Sousse, TunisiaCopyright © 2023 Osoro, Amir, Vohra and Sharma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Amit Sharma, Y2hvaWNlLmFtaXRAZ21haWwuY29t
This Original Article is part of the IJPH Special Issue “Public Health and Primary Care, is 1+1=1?”
 Ian Osoro
Ian Osoro Mohammed Amir
Mohammed Amir Manisha Vohra
Manisha Vohra Amit Sharma
Amit Sharma