- 1Business School, Dongguan City University, Dongguan, China
- 2Taizhou Hospital of Zhejiang Province Affiliated to Wenzhou Medical University, Taizhou, China
- 3Business College, Taizhou University, Taizhou, Zhejiang, China
- 4Institute of Public Health and Emergency Management, Taizhou University, Taizhou, Zhejiang, China
- 5Key Laboratory of Evidence-Based Radiology of Taizhou, Linhai, Zhejiang, China
- 6Department of Orthopaedics, Taizhou Hospital of Zhejiang Province Affiliated to Wenzhou Medical University, Taizhou, China
Objectives: To develop an evaluation model for, and identify key factors contributing to, burnout in orthopedic surgeons, providing a reference for the management of burnout among orthopedic surgeons in hospitals.
Methods: We developed an analytic hierarchy process (AHP) model with 3 dimensions and 10 sub-criteria based on an extensive literature review and expert assessment. We used expert and purposive sampling and 17 orthopedic surgeons were selected as research subjects. The AHP process was then used to obtain the weights and to prioritize the dimensions and criteria for burnout in orthopedic surgeons.
Results: The dimension of C1 (personal/family) was the key factor affecting burnout in orthopedic surgeons, and in the sub-criteria, the top four sub-criteria were C11 (little time for family), C31 (anxiety about clinical competence), C12 (work-family conflict), and C22 (heavy work load).
Conclusion: This model was effective in analyzing the key factors contributing to job burnout risk, and the results can inform improved management of the levels of burnout affecting orthopedic surgeons in hospitals.
Introduction
Burnout is an important concept in occupational stress and mental health research and was first proposed by Freudenberg in 1974 (1). Since then, research on job burnout has received increasing attention, and burnout in different occupations has become a research hotspot in the field of occupational stress, including physician burnout (2), faculty burnout (3), and nurse burnout (4). Job burnout is defined as a comprehensive reaction marked by extreme physical and mental exhaustion caused by occupational stress, and it is characterized by two features: one key aspect is the negative, cynical attitude and feelings toward clients, and the other is an increase in emotional exhaustion (5).
Physician burnout has become one of the core topics in occupational stress research in the medical field (6–8). This research has identified physician burnout as a public health problem (9), especially in the context of the current COVID-19 pandemic (10, 11). Physicians and nurses typically help others and are generally under heavy work pressure, and some of them even suffer from depression as a result (12, 13). Therefore, discussing job burnout among physicians is of great practical significance.
Studies have shown that during the current pandemic, the occupational stress of physicians has increased significantly (14). Stress is a state of increased tension as a protective reaction to various adverse factors. At the same time, emotions are a mental process that reflects the attitude towards these factors. Burnout caused by negative emotions, such as anxiety, anger, depression and sadness, affects the physical and mental health of physicians (15, 16) and can decrease their career (9, 16) and life satisfaction (13, 17) among other factors. This can have significant adverse effects on the medical system; for example, burnout has been shown to lead to medical malpractice (18, 19) and to reduce the quality of medical treatment patients receive (20, 21).
Orthopedic surgery is a challenging profession that often involves a heavy workload, generally long working hours, and requires a wide range of medical knowledge and specialist surgical skills (22, 23). Research has shown that half of orthopedic surgeons report experiencing burnout (24, 25). Overall, orthopedic surgeons had the second highest burnout rate (trauma surgeons ranked first) (26). However, there were discrepancies between burnout level for orthopedic surgeons and physicians in other medical specialties (15). Based on this review of the relevant literature, this study aimed to identify the main factors affecting burnout in orthopedic surgeons and to build a hierarchy model. To achieve this, we designed and conducted a questionnaire survey and elicited responses from 17 orthopedic surgeons. The questionnaire results were summarized and discussed using the analytic hierarchy process (AHP) to obtain the weight order of each criterion in pairwise comparisons (27). Subsequent to this, hospital decision-makers can further focus on the primary factors contributing to orthopedic physicians’ burnout, and implement corresponding policy measures to improve their working conditions and enhance the hospital’s management level.
Methods
Study Design and Modeling Process
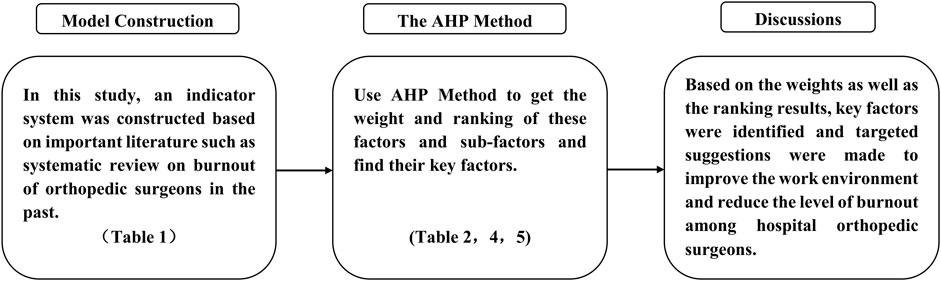
This study constructs an indicator system by reviewing past systematic reviews and other important literature on occupational burnout among orthopedic surgeons. We then obtain the weights and rankings of these factors and sub-factors through a survey of 17 orthopedic physicians using the AHP method, identifying the critical factors. Please see Figure 1 for the flowchart.
The Model of Burnout Factors for Orthopedic Surgeons
This study builds on multiple previous studies to identify key factors that influence orthopedic surgeon burnout. Existing research has used a variety of methods to explore this topic such as systematic reviews, content analyses, meta-analyses, and case studies. For example, the Maslach Burnout Inventory is a widely used measure and is considered the gold standard for burnout assessment. It is a scoring system validated across multiple occupations and fields of study and includes three components: burnout, depersonalization, and personal achievement (28).
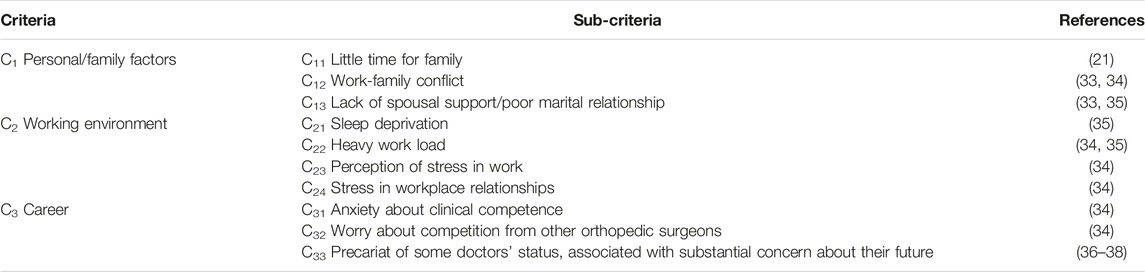
Sibeoni and Bellon-Champel (29) analyzed the factors related to physician burnout through a systematic review and meta-synthesis method, and divided these factors into two themes: the stress factor and protective factor. The stress factor theme initially considered organizational factors, then relationship factors, and finally personal factors. Travers (30) concluded in a review article that there were six relevant factors affecting burnout in orthopedic surgeons but highlighted the two most significant factors as the intensity and complexity of the work and its significant emotional requirements. Hui and Leung (31) analyzed the positive and negative factors of occupational burnout among orthopedic surgeons using a systematic review method that focused on four factors: personal, family, work environment, and occupation. Verret et al. (32) used a simple linear regression model to summarize burnout factors in orthopedic surgeons at different career stages. Through an open-comment analysis, they identified five major problematic categories in work life: workload, resources, interaction, environment, and self-care. Based on the above key articles, this study constructed a model of burnout factors for orthopedic surgeons, and its related factors and sub-factors are shown in Table 1.
The Analytic Hierarchy Process Method
The AHP is a subjective evaluation method proposed by Saaty, an American operational research scientist, in the early 1970s (39). This is a multi-attribute evaluation method used under certain conditions. The AHP is a systematic, simple, flexible, and effective decision-making method that systematizes complex problems using a hierarchical structure. This method decomposes the elements related to decision-making into multiple levels, such as objectives, criteria, and schemes and conducts qualitative and quantitative analysis on this basis (27). The AHP has the advantage of simplifying complex problems and calculations. It is widely used in many fields such as personnel quality evaluation (40), multi-scheme comparison (41), scientific and technological achievement evaluation (42), and work effectiveness evaluation (43). The AHP mainly includes four steps (27): the first step is the construction of the hierarchical structure model; the second step is the construction of the judgment matrix; the third step is testing the hierarchical single ordering and its consistency (this determines the weight of indicators); and the fourth step is the hierarchical total ordering and its consistency test.
Step 1. Obtain the paired comparison matrix from each expert.
Each expert applied a 9-point Likert scale (from equally important to absolutely important) to assess the degree of relative importance between criteria, as shown in Eq. 1.
where
Step 2. Calculate the relative weight between criteria.
The approximate weight of each criterion is obtained by the maximum eigenvalue of the eigenvector, which is given by Eq. 2.
Step 3. obtain the consistency of pairwise matrix.
Because the decision maker’s judgment matrix is irrational, we can use Eqs 3, 4 to calculate the deviation degree of judgment inconsistency, which is called the consistency index (CI) and consistency ratio (CR).
where
If the C.R.
Data Collection
The study was conducted between 18 March and 20 April 2022, and each questionnaire took 20–30 min. The participants in the study were all orthopedic surgeons with higher education, extensive clinical experience, and good professional knowledge. With 17 participants, all from the Department of Orthopedics of Taizhou Hospital of Zhejiang Province, this study met the requirements of the AHP analysis method.
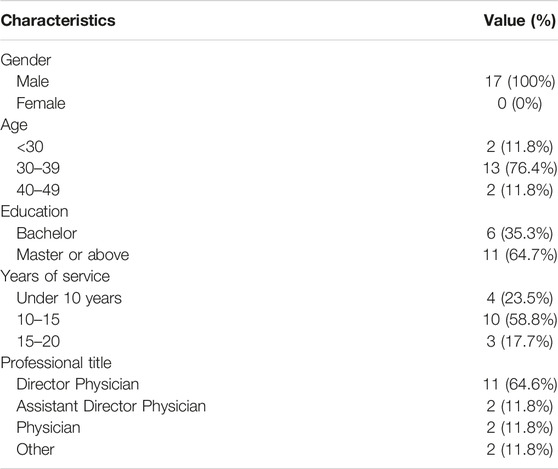
All participants were male; 13 participants were between the ages of 30 and 39, accounting for 76.4%; 2 participants were under the age of 30 and 2 over the age of 40, each category accounting for 11.8%. The participants were highly educated: all of them had a bachelor’s degree, while 64.7% had a master’s degree or above. Only four participants had less than 10 years of work experience, and 76.5% had more than 10 years of work experience. From the job title perspective, 64.7% of the participants had director physician titles and, of the remaining 35.3%, two participants were assistant director physicians and two were physicians. Specific descriptive information is shown in Table 3.
Results
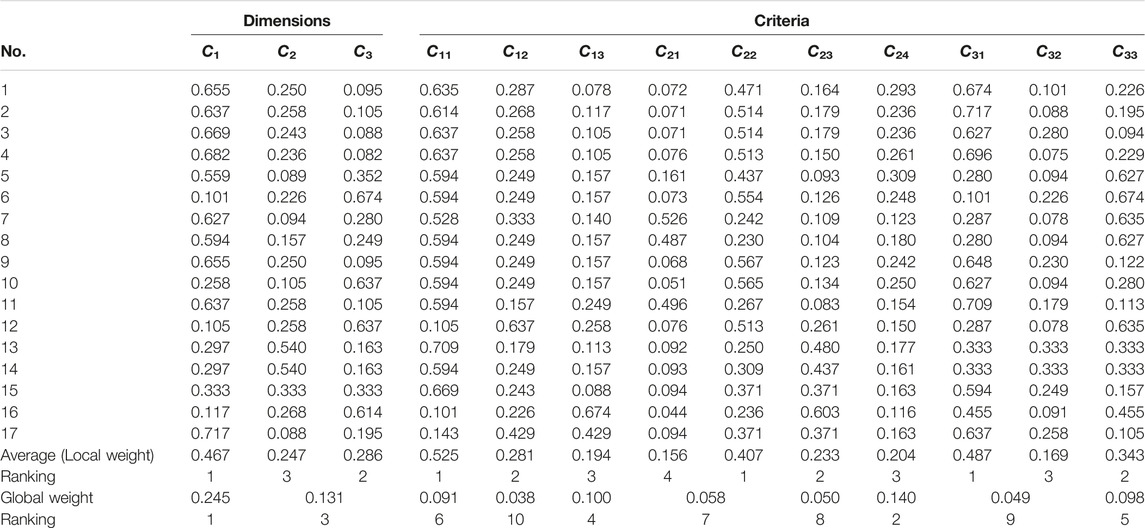
In our study, we took the first orthopedic surgeon as an example for calculation and filled in the original paired matrix according to the AHP method. The CI and CR values of the original paired matrix of the criteria and sub-criteria were all less than 0.1, their consistency passed the test, and the results are shown in Table 4.
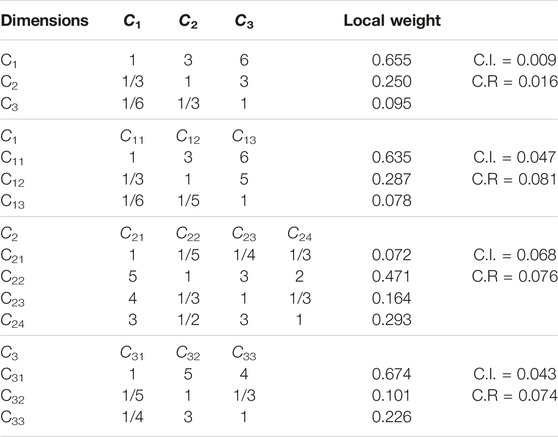
TABLE 4. Paired comparison matrix and local weight results for the first orthopedic surgeon (China, 2023).
Table 5 shows the weight of the results of 17 orthopedic surgeons, and the CR and CI values are both less than 0.1, indicating that the constructed matrix has passed the consistency test, and the results include weight ordering of criteria and sub-criteria, and the results are analyzed as follows: From the perspective of local weights, the criteria weight is ranked C1 (personal/family factors)
The global weight of each sub-criterion is calculated by multiplying its local weight with the corresponding criteria’s local weight along the AHP hierarchy. In terms of the global weight of each sub-criteria, the top four sub-criteria are C11 (little time for family), C31 (anxiety about clinical competence), C12 (work-family conflict) and C22 (heavy work load).
Discussion
Clinical Research Implications
Based on the weight results in the previous section, from the perspective of local weight, the weight value of personal and family factors is 0.467, which is close to 0.5, indicating that personal and family factors are the key factors causing burnout of orthopedic surgeons and have a high degree of influence (44). From the perspective of global weight, the top four sub-criteria are C11, C31, C12, and C22, these factors are little time for family, anxiety about clinical competence, work-family conflict, and heavy work load.
Among the criteria of personal and family, the sub-criteria influencing burnout of orthopedic surgeons were little time for family and work-family conflict, with weights of 0.245 and 0.140. Orthopedic surgeons believe that the workday is too long, there is no time for their personal lives, and they struggle to balance their personal and work lives (45–47). According to Agana research, working hours are the most important factor affecting orthopedic surgeons’ satisfaction, accounting for 62% of the overall job satisfaction (48). Studies suggest that work-family conflict can seriously affect the burnout level of orthopedic surgeons (35), and that frequent conflict leads to poor marital relationships, which further increases the burnout level (34).
The local weight of career and working environment is 0.247 and 0.286. The global weight of the sub-criteria of anxiety about clinical competence in the career criteria, ranks the second. Meanwhile, it can be seen that the local weight value of anxiety about clinical competence is also high, which is 0.487, the highest value of all local weights. It can also be concluded that anxiety about clinical competence has a significant impact on orthopedic surgeon burnout (46).
In the dimension of the working environment, the key sub-criterion is work overload, which has a global weight of 0.1. Work overload is a major source of exhaustion and, in turn, is at the root of burnout. Work overload represents the basic individual stress component of burnout (49), and has high impact on burnout among orthopedic surgeons (50). Continuously increasing responsibilities and extremely high workload were commonly reported problems (32, 36), especially at this stage of the COVID-19 pandemic, the additional workload has led to higher levels of burnout among orthopedic surgeons (51). Workloads also include administrative workloads, such as excessive paperwork, electronic medical records (52), and conference report (53), which also affects their burnout levels.
Clinical Practice Implications
The general burnout rate among physicians is approximately 40% (44, 54) and the burnout rate of orthopedic surgeons is nearly 55% higher than this general level (55). Furthermore, a study has shown that the burnout rate among Chinese orthopedic surgeons is as high as 85% (24). High burnout rates indicate that these orthopedic physicians face various stressors, which may even cause them to lose their temper at work or develop various health risks, such as heart disease and stroke (24, 56). These issues can severely affect the quality of medical care and potentially lead to an increase in medical errors (19, 57).
According to this study, personal and family factors were key factors in contributing to burnout among orthopedic surgeons. This indicates that, in line with previous findings, reducing working hours to allow orthopedic surgeons to spend time with their families would be an effective way to reduce burnout levels (57, 58), increase happiness at work, and avoid family conflict (48).
Among the factors in the working environment, workload is positively correlated with working time. Therefore, in addition to reducing working hours, it is necessary to improve the efficiency of orthopedic surgeons, especially by reducing administrative workload, reducing the number and length of mandatory meetings, and avoiding bureaucracy (53). To achieve this, system and process transformation are needed, such as upgrading work structure and processes with new technology and simplifying the internal electronic resume platform in hospitals (17).
Limitations
Our study presents several limitations. First, the investigation builds upon previous research to establish an assessment model for factors contributing to orthopedic physicians’ burnout. These prior studies employed diverse methodologies and, to some extent, were subjective. Second, while our model incorporated key factors identified in previous research, not all factors were compared pairwise due to methodological constraints. Third, past studies were based on correlation, regression, and structural equation models, whereas our results stem from an AHP method, implying that comparisons with many earlier findings may be challenging. Fourth, the participants comprises orthopedic physicians from a specific hospital, suggesting that the results may not be generalizable to other medical professionals in different hospitals. Lastly, due to limitations in the research methodology and participants, factors such as model construction, gender differences among participants, and others were not fully addressed, providing potential avenues for future research.
Conclusion
In this study, 17 orthopedic surgeons were selected as research subjects to construct an evaluation model of occupational burnout factors. The AHP method was used to obtain weighted results for the factors affecting burnout in orthopedic surgeons, key factors were identified, and improvement strategies were discussed. The results showed that the personal family factor was the key factor affecting burnout in orthopedic surgeons, and in the sub-criteria, the key factors were little time for family, anxiety about clinical competence, work-family conflict, and heavy workload. This research model enriches our understanding of burnout among orthopedic surgeons, and the research results have a certain reference value for informing efforts to reduce burnout rates among orthopedic surgeons.
Ethics Statement
The studies involving human participants were reviewed and approved by the Institutional Review Board (IRB) in Taizhou Hospital of Zhejiang Province Affiliated to Wenzhou Medical University, Taizhou, China (ID: K20220238). All procedures were performed in accordance with the guidelines of our institutional ethics committee and adhered to the tenets of the Declaration of Helsinki. All participants’ information was anonymous. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
SW, YJ, and LL participated in the study and drafted the manuscript. YJ and ZZ were involved in the study design and data collection. RL and Y-CC compiled the data and calculated the AHP weighting results. SW, LL, Y-CC, and ZZ participated in the analysis and discussion of the AHP weighting results. Y-CC and ZZ conceived the design of this study and participated in the coordination and communication of the entire study. All authors read and approved the final manuscript.
Conflict of Interest
The authors declare that they do not have any conflicts of interest.
References
1. Vega, NV, Sanabria, A, Domínguez, LC, Osorio, C, and Bejarano, M. Síndrome de desgaste profesional. Revista Colombiana de Cirugía (2009) 24(3):138–46.
2. Rotenstein, LS, Torre, M, Ramos, MA, Rosales, RC, Guille, C, Sen, S, et al. Prevalence of Burnout Among Physicians A Systematic Review. Jama-Journal Am Med Assoc (2018) 320(11):1131–50. doi:10.1001/jama.2018.12777
3. Herman, KC, Hickmon-Rosa, J, and Reinke, WM. Empirically Derived Profiles of Teacher Stress, Burnout, Self-Efficacy, and Coping and Associated Student Outcomes. J Positive Behav Interventions (2018) 20(2):90–100. doi:10.1177/1098300717732066
4. Jun, J, Ojemeni, MM, Kalamani, R, Tong, J, and Crecelius, ML. Relationship between Nurse Burnout, Patient and Organizational Outcomes: Systematic Review. Int J Nurs Stud (2021) 119:103933. doi:10.1016/j.ijnurstu.2021.103933
5. Maslach, C, and Jackson, SE. The Measurement of Experienced Burnout. J organizational Behav (1981) 2(2):99–113. doi:10.1002/job.4030020205
6. Clough, BA, Ireland, MJ, Leane, S, and March, S. Stressors and Protective Factors Among Regional and Metropolitan Australian Medical Doctors: A Mixed Methods Investigation. J Clin Psychol (2020) 76(7):1362–89. doi:10.1002/jclp.22940
7. Olson, K, Marchalik, D, Farley, H, Dean, SM, Lawrence, EC, Hamidi, MS, et al. Organizational Strategies to Reduce Physician Burnout and Improve Professional Fulfillment. Curr Probl Pediatr Adolesc Health Care (2019) 49(12):100664. doi:10.1016/j.cppeds.2019.100664
8. Dewa, CS, Loong, D, Bonato, S, Thanh, NX, and Jacobs, P. How Does Burnout Affect Physician Productivity? A Systematic Literature Review. BMC Health Serv Res (2014) 14(1):325–10. doi:10.1186/1472-6963-14-325
9. West, CP, Shanafelt, TD, and Kolars, JC. Quality of Life, Burnout, Educational Debt, and Medical Knowledge Among Internal Medicine Residents. Jama (2011) 306(9):952–60. doi:10.1001/jama.2011.1247
10. Lazarides, AL, Belay, ES, Anastasio, AT, Cook, CE, and Anakwenze, OA. Physician Burnout and Professional Satisfaction in Orthopedic Surgeons during the COVID-19 Pandemic. Work (2021) 69(1):15–22. doi:10.3233/WOR-205288
11. Tan, BY, Kanneganti, A, Lim, LJH, Tan, M, Chua, YX, Tan, L, et al. Burnout and Associated Factors Among Health Care Workers in Singapore during the COVID-19 Pandemic. J Am Med Directors Assoc (2020) 21(12):1751–8. doi:10.1016/j.jamda.2020.09.035
12. Kerlin, MP, McPeake, J, and Mikkelsen, ME. Burnout and Joy in the Profession of Critical Care Medicine. Crit Care (2020) 24(1):98. doi:10.1186/s13054-020-2784-z
13. Ariely, D, and Lanier, WL. Disturbing Trends in Physician Burnout and Satisfaction with Work-Life Balance: Dealing with Malady Among the Nation's Healers. In: Mayo Clinic Proceedings. Amsterdam, Netherlands: Elsevier (2015).
14. Gazelle, G, Liebschutz, JM, and Riess, H. Physician Burnout: Coaching a Way Out. J Gen Intern Med (2015) 30(4):508–13. doi:10.1007/s11606-014-3144-y
15. Zhang, Q, Mu, MC, He, Y, Cai, ZL, and Li, ZC. Burnout in Emergency Medicine Physicians: a Meta-Analysis and Systematic Review. Medicine (2020) 99(32):e21462. doi:10.1097/MD.0000000000021462
16. Busis, NA, Shanafelt, TD, Keran, CM, Levin, KH, Schwarz, HB, Molano, JR, et al. Burnout, Career Satisfaction, and Well-Being Among US Neurologists in 2016. Neurology (2017) 88(8):797–808. doi:10.1212/WNL.0000000000003640
17. Shanafelt, T, Goh, J, and Sinsky, C. The Business Case for Investing in Physician Well-Being. JAMA Intern Med (2017) 177(12):1826–32. doi:10.1001/jamainternmed.2017.4340
18. Fahrenkopf, AM, Sectish, TC, Barger, LK, Sharek, PJ, Lewin, D, Chiang, VW, et al. Rates of Medication Errors Among Depressed and Burnt Out Residents: Prospective Cohort Study. Bmj (2008) 336(7642):488–91. doi:10.1136/bmj.39469.763218.BE
19. Kwah, J, Weintraub, J, Fallar, R, and Ripp, J. The Effect of Burnout on Medical Errors and Professionalism in First-Year Internal Medicine Residents. J graduate Med Educ (2016) 8(4):597–600. doi:10.4300/JGME-D-15-00457.1
20. Shanafelt, TD, Bradley, KA, Wipf, JE, and Back, AL. Burnout and Self-Reported Patient Care in an Internal Medicine Residency Program. Ann Intern Med (2002) 136(5):358–67. doi:10.7326/0003-4819-136-5-200203050-00008
21. Daniels, AH, DePasse, JM, and Kamal, RN. Orthopaedic Surgeon Burnout: Diagnosis, Treatment, and Prevention. J Am Acad Orthopaedic Surgeons (2016) 24(4):213–9. doi:10.5435/JAAOS-D-15-00148
22. Marsh, JL. Avoiding Burnout in an Orthopaedic Trauma Practice. J orthopaedic Trauma (2012) 26:S34–6. doi:10.1097/BOT.0b013e3182641fee
23. Pellegrini, VD. A Perspective on the Effect of the 80-hour Work Week: Has it Changed the Graduating Orthopaedic Resident? JAAOS-Journal Am Acad Orthopaedic Surgeons (2017) 25(6):416–20. doi:10.5435/JAAOS-D-17-00240
24. Zheng, H, Shao, H, and Zhou, Y. Burnout Among Chinese Adult Reconstructive Surgeons: Incidence, Risk Factors, and Relationship with Intraoperative Irritability. The J arthroplasty (2018) 33(4):1253–7. doi:10.1016/j.arth.2017.10.049
25. Balch, CM, Shanafelt, TD, Sloan, JA, Satele, DV, and Freischlag, JA. Distress and Career Satisfaction Among 14 Surgical Specialties, Comparing Academic and Private Practice Settings. Ann Surg (2011) 254(4):558–68. doi:10.1097/SLA.0b013e318230097e
26. Wang, J, Hu, B, Peng, Z, Song, H, Cai, S, Rao, X, et al. Prevalence of Burnout Among Intensivists in mainland China: a Nationwide Cross-Sectional Survey. Crit Care (2021) 25(1):8. doi:10.1186/s13054-020-03439-8
27. Saaty, TL. Decision Making with the Analytic Hierarchy Process. Int J Serv Sci (2008) 1(1):83–98. doi:10.1504/ijssci.2008.017590
28. Maslach, C, Jackson, SE, and Leiter, MP. Maslach Burnout Inventory. Lanham Maryland: Scarecrow Education (1997).
29. Sibeoni, J, Bellon-Champel, L, Mousty, A, Manolios, E, Verneuil, L, and Revah-Levy, A. Physicians’ Perspectives about Burnout: a Systematic Review and Metasynthesis. J Gen Intern Med (2019) 34(8):1578–90. doi:10.1007/s11606-019-05062-y
30. Travers, V. Burnout in Orthopedic Surgeons. Orthopaedics Traumatol Surg Res (2020) 106(1):S7–S12. doi:10.1016/j.otsr.2019.04.029
31. Hui, RWH, Leung, KC, Hwang, AC, Ge, S., Lai, GGW, Leung, AN, et al. Burnout in Orthopaedic Surgeons: A Systematic Review. J Clin Orthop Trauma (2019) 10:S47–S52. doi:10.1016/j.jcot.2019.01.028
32. Verret, CI, Nguyen, J, Albert, TJ, and Fufa, DT. How Do Areas of Work Life Drive Burnout in Orthopaedic Attending Surgeons, Fellows, and Residents? Clin Orthop Relat Res (2021) 479(2):251–62. doi:10.1097/CORR.0000000000001457
33. Sedel, L. Letter to the Editor: Recognizing and Preventing Burnout Among Orthopaedic Leaders. Clin Orthopaedics Relat Res (2009) 467(4):1111. doi:10.1007/s11999-009-0704-2
34. Sargent, MC, Sotile, W, Sotile, MO, Rubash, H, and Barrack, RL. Stress and Coping Among Orthopaedic Surgery Residents and Faculty. J Bone Jt Surgery-American Volume (2004) 86A(7):1579–86. doi:10.2106/00004623-200407000-00032
35. Saleh, KJ, Quick, JC, Conaway, M, Sime, WE, Martin, W, Hurwitz, S, et al. The Prevalence and Severity of Burnout Among Academic Orthopaedic Departmental Leaders. J Bone Jt Surgery-American Volume (2007) 89A(4):896–903. doi:10.2106/JBJS.F.00987
36. Çiçeklioğlu, M, Öcek, ZA, Turk, M, and Taner, Ş. The Influence of a Market-Oriented Primary Care Reform on Family Physicians' Working Conditions: A Qualitative Study in Turkey. Eur J Gen Pract (2015) 21(2):97–102. doi:10.3109/13814788.2014.966075
37. Mcgowan, Y, Humphries, N, Burke, H, Conry, M, and Morgan, K. Through Doctors' Eyes: A Qualitative Study of Hospital Doctor Perspectives on Their Working Conditions. Br J Health Psychol (2013) 18(4):874–91. doi:10.1111/bjhp.12037
38. Turk, M, Davas, A, Tanik, FA, and Montgomery, AJ. Organizational Stressors, Work-Family Interface and the Role of Gender in the Hospital: Experiences from Turkey. Br J Health Psychol (2014) 19(2):442–58. doi:10.1111/bjhp.12041
39. Saaty, RW. The Analytic Hierarchy Process—What it Is and How it Is Used. Math Model (1987) 9(3-5):161–76. doi:10.1016/0270-0255(87)90473-8
40. Taylor, FA, Ketcham, AF, and Hoffman, D. Personnel Evaluation with AHP. Holden, MA: Management Decision (1998).
41. Wei, C-C, Chien, C-F, and Wang, M-JJ. An AHP-Based Approach to ERP System Selection. Int J Prod Econ (2005) 96(1):47–62. doi:10.1016/j.ijpe.2004.03.004
42. Cheng, C-H, Yang, K-L, and Hwang, C-L. Evaluating Attack Helicopters by AHP Based on Linguistic Variable Weight. Eur J Oper Res (1999) 116(2):423–35. doi:10.1016/s0377-2217(98)00156-8
43. Dağdeviren, M, and Yüksel, İ. Developing a Fuzzy Analytic Hierarchy Process (AHP) Model for Behavior-Based Safety Management. Inf Sci (2008) 178(6):1717–33. doi:10.1016/j.ins.2007.10.016
44. Sargent, MC, Sotile, W, Sotile, MO, Rubash, H, and Barrack, RL. Quality of Life during Orthopaedic Training and Academic Practice: Part 1: Orthopaedic Surgery Residents and Faculty. JBJS (2009) 91(10):2395–405. doi:10.2106/JBJS.H.00665
45. Miyasaki, JM, Rheaume, C, Gulya, L, Ellenstein, A, Schwarz, HB, Vidic, TR, et al. Qualitative Study of Burnout, Career Satisfaction, and Well-Being Among US Neurologists in 2016. Neurology (2017) 89(16):1730–8. doi:10.1212/WNL.0000000000004526
46. Orri, M, Revah-Lévy, A, and Farges, O. Surgeons’ Emotional Experience of Their Everyday Practice-A Qualitative Study. PLoS One (2015) 10(11):e0143763. doi:10.1371/journal.pone.0143763
47. Kjeldmand, D, and Holmström, I. Balint Groups as a Means to Increase Job Satisfaction and Prevent Burnout Among General Practitioners. Ann Fam Med (2008) 6(2):138–45. doi:10.1370/afm.813
48. Agana, DF, Porter, M, Hatch, R, Rubin, D, and Carek, P. Job Satisfaction Among Academic Family Physicians. Fam Med (2017) 49(8):622–5.
49. Portoghese, I, Galletta, M, Coppola, RC, Finco, G, and Campagna, M. Burnout and Workload Among Health Care Workers: the Moderating Role of Job Control. Saf Health work (2014) 5(3):152–7. doi:10.1016/j.shaw.2014.05.004
50. Rossi, AM, Perrewe, PL, and Sauter, SL. Stress and Quality of Working Life: Current Perspectives in Occupational Health. Charlotte, NC: Information Age Publishing, Inc. (2006).
51. Mavrogenis, AF, and Scarlat, MM. Stress, Anxiety, and Burnout of Orthopaedic Surgeons in COVID-19 Pandemic. Berlin, Germany: Springer (2022). p. 1–5.
52. Somerson, JS, Patton, A, Ahmed, AA, Ramey, S, and Holliday, EB. Burnout Among United States Orthopaedic Surgery Residents. J Surg Educ (2020) 77(4):961–8. doi:10.1016/j.jsurg.2020.02.019
53. Shanafelt, TD, Balch, CM, Bechamps, GJ, Russell, T, Dyrbye, L, Satele, D, et al. Burnout and Career Satisfaction Among American Surgeons. Ann Surg (2009) 250(3):463–71. doi:10.1097/SLA.0b013e3181ac4dfd
54. Faivre, G, Kielwasser, H, Bourgeois, M, Panouilleres, M, Loisel, F, and Obert, L. Burnout Syndrome in Orthopaedic and Trauma Surgery Residents in France: a Nationwide Survey. Orthopaedics Traumatol Surg Res (2018) 104(8):1291–5. doi:10.1016/j.otsr.2018.08.016
55. Shanafelt, TD, Hasan, O, Dyrbye, LN, Sinsky, C, Satele, D, Sloan, J, et al. Changes in Burnout and Satisfaction with Work-Life Balance in Physicians and the General US Working Population between 2011 and 2014. In: Mayo Clinic Proceedings. Amsterdam, Netherlands: Elsevier (2015).
56. Saleh, KJ, Quick, JC, Sime, WE, Novicoff, WM, and Einhorn, TA. Recognizing and Preventing Burnout Among Orthopaedic Leaders. Clin orthopaedics Relat Res (2009) 467(2):558–65. doi:10.1007/s11999-008-0622-8
57. West, CP, Dyrbye, LN, Erwin, PJ, and Shanafelt, TD. Interventions to Prevent and Reduce Physician Burnout: a Systematic Review and Meta-Analysis. The Lancet (2016) 388(10057):2272–81. doi:10.1016/S0140-6736(16)31279-X
Keywords: burnout, multiple criteria decision-making (MCDM), orthopedic surgeons, analytic hierarchy process (AHP), key factors
Citation: Wang S, Li L, Jin Y, Liao R, Chuang Y-C and Zhu Z (2023) Identifying Key Factors for Burnout Among Orthopedic Surgeons Using the Analytic Hierarchy Process Method. Int J Public Health 68:1605719. doi: 10.3389/ijph.2023.1605719
Received: 25 December 2022; Accepted: 11 April 2023;
Published: 03 May 2023.
Edited by:
L. Suzanne Suggs, University of Italian Switzerland, SwitzerlandReviewed by:
Serhii Tukaiev, Università della Svizzera Italiana, SwitzerlandJuan Gómez-Salgado, University of Huelva, Spain
Copyright © 2023 Wang, Li, Jin, Liao, Chuang and Zhu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yen-Ching Chuang, eWVuY2hpbmcuY2h1YW5nQGdtYWlsLmNvbQ==; Zhong Zhu, emh1ekBlbnplbWVkLmNvbQ==
†These authors have contributed equally to this work and share first authorship
This Original Article is part of the IJPH Special Issue “Health in All Sustainable Development Goals”
 Shiqian Wang
Shiqian Wang Lin Li1†
Lin Li1† Yen-Ching Chuang
Yen-Ching Chuang