- 1Division of Cancer Control and Policy, National Cancer Control Institute, National Cancer Center, Goyang, Republic of Korea
- 2HIRA Research Institute, Health Insurance Review & Assessment Service (HIRA), Wonju, Republic of Korea
- 3Gangwon Public Health Policy Institute, Chuncheon, Republic of Korea
- 4Division of Health Administration, College of Software and Digital Healthcare Convergence, Yonsei University, Wonju, Republic of Korea
Objective: This study aims to explore regional health disparities in hypertension-related hospitalizations and confirm this difference according to the states of continuity of care (COC).
Methods: We used the National Health Insurance Service National Sample Cohort data from 2002 to 2019. The dependent variable, hypertension-related hospitalization, included hospitalization for hypertensive diseases (I10–I13, I15), ischemic heart disease (I20–I25), and cerebrovascular disease (I60–I69). Nested case-control matching was performed according to age, sex, and income level. We compared hypertension-related hospitalization fractions in urban and rural areas by classifying them according to the state of COC and analyzed them using conditional logistic regression suitable for matched data.
Results: The odds of hypertension-related hospitalization of hypertensive patients were higher in the rural areas than in the urban areas; however, as the COC increased, the difference decreased. There was no change in the results according to the COC observation period.
Conclusion: To reduce regional health disparities, both the promotion of COC and the improvement of the quality of primary care must be achieved.
Introduction
Access to medical care is high in South Korea compared to that in other countries. Many infrastructures are concentrated in the metropolitan areas due to the high population density [1]; therefore, medical infrastructure is also concentrated in the metropolitan area. The environment within a given community has emerged as a factor affecting the health of residents; furthermore, regional health disparities due to unbalanced allocation of medical resources are increasing [2, 3] (See Supplementary Table S1).
Globally, populations are aging rapidly, resulting in changes in the spectrum of diseases and an increase in the number of people with multiple chronic diseases [4]. In particular, South Korea is the most rapidly aging country in the world [5], and health problems are more severe in rural areas than in cities, as most older people in South Korea live in rural areas. Hypertension and diabetes are typical chronic diseases, among which hypertension, in particular, is the most significant risk factor for cardiocerebrovascular disease, requiring continuous management [6, 7]. The prevalence of hypertension among adults aged 30 years and above in South Korea was approximately 30% as of 2020, and there are disparities in the incidence rate of hypertension by age, income, and region of residence [8]. The age-standardized hypertension prevalence rate by region is 18.6% in Seoul, but Gangwon-do has the highest prevalence rate at 22.0%, which is a big difference. In addition, compared by area of residence, the number of age-standardized hospitalized hypertension patients per 1,000 population was 19.9 in Seoul. Jeollanam-do province had the highest number of age-standardized hospitalized hypertension patients and had 32.8, 50% more than Seoul (Supplementary Table S2).
In particular, some aspects of cardiocerebrovascular disease can cause emergencies that must be treated within the golden hour; hence, the local medical infrastructure plays an important role in this regard [9]. However, South Korea has an unbalanced medical infrastructure, resulting in a lack of response to medical demands within specific timelines. Looking at the average distance to the clinic by region, Seoul was 0.97 km, while Gangwon-do, which was the farthest, averaged 11.05 km, a huge difference (Supplementary Table S1). Such medical infrastructure is creating regional health disparities. However, hypertension, which is the most common risk factor for cardiocerebrovascular disease, is a typical ambulatory care sensitivity condition (ACSC), and the occurrence and exacerbation of complications can be prevented if it is managed continuously before it worsens [10]. The prognosis of the disease may vary depending on the consistency and adequacy of care provided at primary healthcare facilities in the community. Therefore, there is a need to develop a system that can effectively manage hypertension in rural areas.
The World Health Organization (WHO) places great importance on the management of chronic diseases that are closely related to human aging. Therefore, the WHO has indicated the need to maintain continuity of care (COC) in primary healthcare facilities to effectively manage chronic diseases [11]. The COC is one of the critical elements of primary care and represents a terminating and lasting relationship between healthcare providers and patients [12]. Previous studies have found that improving COC in local primary care settings to manage chronic diseases can effectively reduce avoidable hospitalizations and deaths [11, 13], there were also differences in COC depending on the regional scale [14]. Hence, COC is the most important factor in primary care, and improving this indicator will not only improve the health of the people but also help reduce regional health disparities. However, there is a paucity of research on the state of COC and regional health disparities. This study aims to explore regional health disparities in hypertension-related hospitalizations and confirm this difference according to the states of COC. Thus, we present data that has the potential to provide an effective basis for future policies aiming to resolve regional health disparities.
Methods
Data
Data were collected from the National Health Insurance Service National Sample Cohort (NHIS-NSC). South Korea introduced NHIS in 1977 to achieve universal medical coverage. The number of eligible people was gradually expanded, and in 1989 all citizens were covered [15]. NHIS covered 97% all citizens who reside in South Korea except medical aid beneficiaries, and healthcare beneficiaries for veterans [16]. The NHIS-NSC stores medical claims data of the entire Korean population. After stratifying the cohort into 1,476 strata by sex, age, type of insurance, and region, we randomly selected the target population and collected data equivalent to approximately 2% of the total population [17].
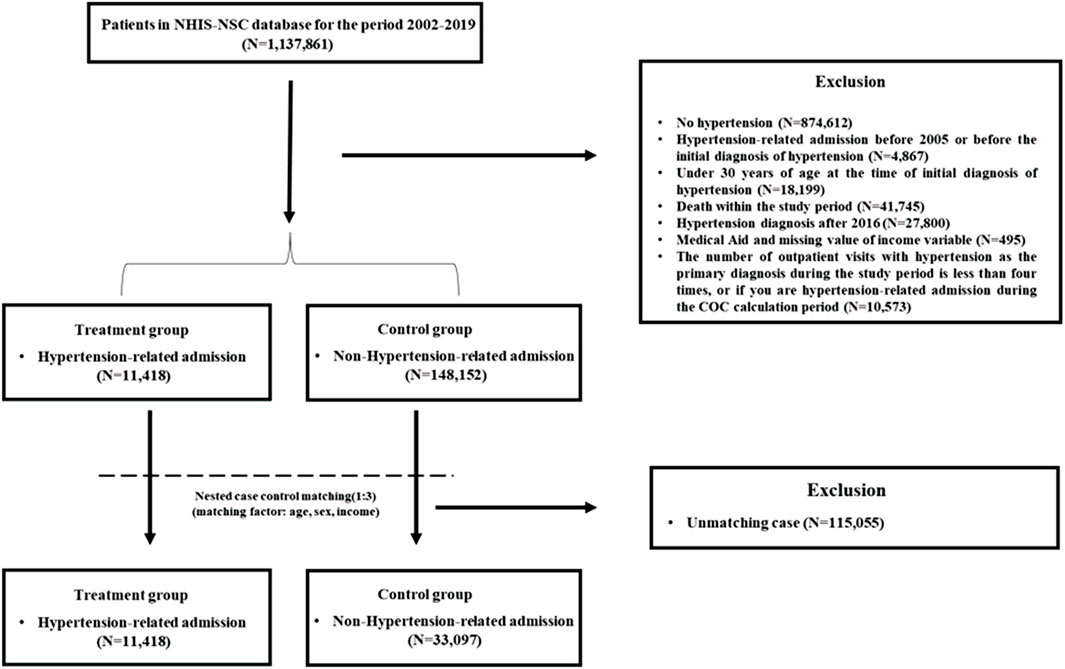
We collected data from 2002 to 2019. Of the 1,137,861 people, the study excluded those with no diagnosis of essential hypertension (I10). In addition, the patients who were admitted according to principal diagnosis for hypertension-related diseases (I10-I13, I15, I20-I25, I60-I69) according to the International Classification of Diseases (ICD-10) before 2005 or before the initial diagnosis of hypertension. Patients aged under 30 years, and those receiving medical aid were excluded from the study. In addition, we excluded hypertension patients who died to reduce possible competing risk from death and to reduce the bias of study results due to underlying health severity. The patients diagnosed with hypertension after 2016 were excluded from the analysis because the COC could not be observed for up to 3 years after 2016. In addition, the patients who visited the outpatient clinic fewer than four times during the analysis period and those who were admitted for hypertension-related diseases during the COC calculation period were excluded from the study. Thereafter, nested case-control (NCC) matching was performed with patients who had been admitted for hypertension-related disease as the treatment group and those who had never been admitted for hypertension-related disease as the control group. A total of 44,519 participants were included in the final analysis, excluding those who were dropped from the matching (Figure 1).
All statistical analyses were performed using the SAS statistical software (version 9.4; Cary, NC, United States). The need for ethical approval was waived by the Institutional Review Board of Yonsei University (1041849-202107-SB-107-01) because this study used only secondary data, and all personal information was anonymized and encrypted.
Study Variables
Dependent Variable
Hypertension is a major risk factor for ischemic heart disease and cerebrovascular disease [18–20]. Therefore, our study defined the dependent variable “hypertension-related hospitalization” as hospitalization for hypertensive disease (I10-I13, I15), ischemic heart disease (I20-I25), or cerebrovascular disease (I60-I69). The principal diagnoses of hypertensive disease, ischemic heart disease, and cerebrovascular disease were confirmed according to the ICD-10 codes. At least one event of hypertension-related hospitalization from 2005 to 2019 was divided “Yes” or “No.”
Independent Variables
Based on the area of residence of study participants, the capital area (Seoul, Gionggi-do) and six metropolitan cities (Incheon-si, Daejeon-si, Gwangju-si, Daegu-si, Ulsan-si, Busan-si) were divided into urban. All other regions were divided into rural. South Korea is divided into -do, -si, -gun, and -gu according to the size of the administrative district. However, in the case of metropolitan cities, despite being in -si units, they allow for their own administrative district status given the city’s size and infrastructure. In South Korea, many infrastructures such as medical care, transportation, and facilities are concentrated in the capital area and the metropolitan city. In this study, we classified cities and rural areas in consideration of these administrative scales and infrastructures.
Control Variables
Control variables included the sociodemographic factors of age, sex, and income, as well as health-related factors of disability severity, CCI score (Charlson comorbidity index), and COC. Age was divided into units of 5 years from 30 to 64 years, with the addition of ≥65 years as a separate group, resulting in eight age groups. Income was divided according to quintiles: individual NHI premiums of 20% or less (quintile 1), 40% or less (quintile 2), 60% or less (quintile 3), 80% or less (quintile 4), 100% or less (quintile 5). Disabilities were categorized into grades 1–6, with grades 1–2 being severe, and grades 3–6 being mild disability [21]. The CCI was used as a representative index for adjusting for comorbidities. A weight of 0–6 was assigned to each disease according to Quan’s criteria, and the scores were divided into 0, 1, 2, 3, and above [22]. The COC is considered a reliable measure because it is used in the absence of routine visits by healthcare providers and is less sensitive to the number of visits by healthcare providers [23]. The COC indicator has the advantage of considering the number of healthcare providers and the number of visits together [12]. The COC has a value between 0 and 1, and the closer it is to 1, the better the COC [23]. Examples of COC scores by outpatient visits are present in Supplementary Figure S1. In this study, COC was calculated separately for 1, 2, and 3 years before the hypertension-related hospitalization. The COC was divided into the good COC group (COC = 1) and the poor COC group (COC < 1). The index was calculated using outpatient visits for essential hypertension (I10) using the following formula:
where N is the total number of outpatient visits, M is the number of healthcare providers, and nj is the number of visits to the jth healthcare provider [23].
Statistical Analysis
The NCC study refers to a method in which an event occurring case is categorized into a treatment group, and participants with similar characteristics are extracted into control groups when the event occurs [24]. In this study, participants who experienced hypertension-related hospitalization were regarded as the treatment group, and a control group with similar characteristics was selected according to age, sex, and income, and 1:3 matching was performed.
Analysis was performed using the conditional logistic regression method, which is suitable for matched data [25]. Analysis was performed according to the COC observation period (1, 2, 3 years) with participants whose principal diagnoses were based on the ICD-10 codes for essential hypertension between 2002 and 2016. A stratified analysis of COC was performed to identify regional health disparities according to the states of COC. Using the COC criterion of 1, stratification analysis proceeded separately for the good COC group and the poor COC group. In addition, sensitivity analysis was performed by changing the COC criterion to 0.75.
Results
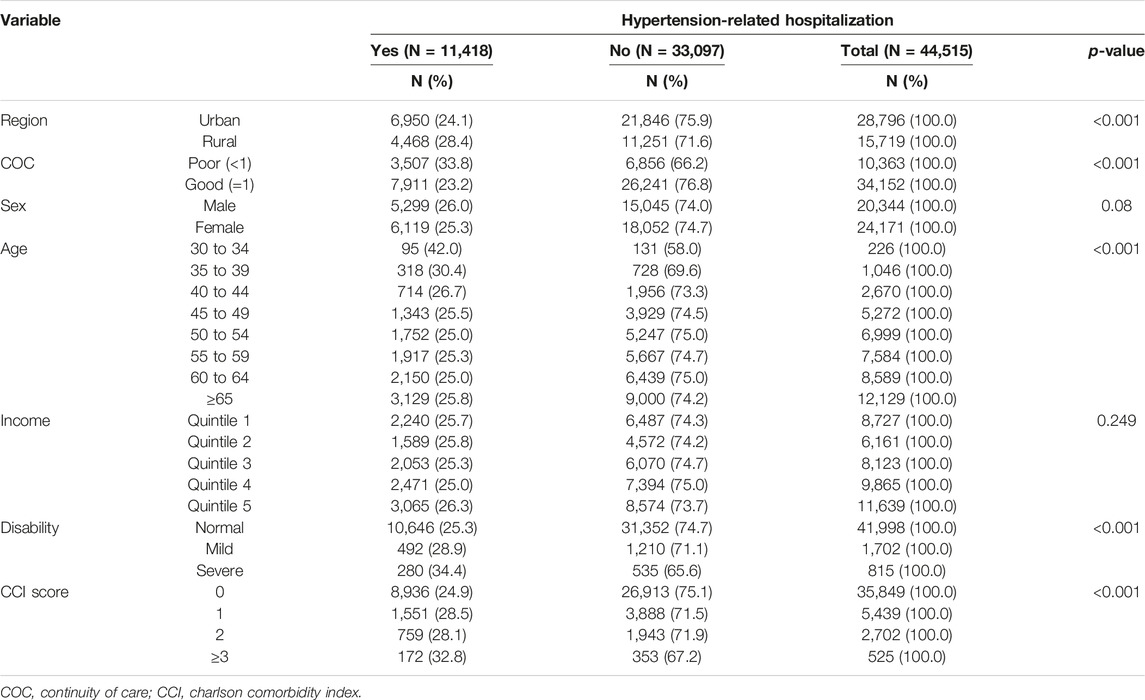
The hypertension-related hospitalization fractions for the patients living in urban and rural areas were 24.1% and 28.4%, respectively. The fraction of hypertension-related hospitalizations was high in rural areas. The fraction of hypertension-related hospitalizations of patients with poor COC was 33.8%. Sex and income were used as matching variables, so there was no significant difference with regard to these variables. In the case of age, there was a difference in the hypertension-related hospitalizations fractions between the 30–34 and 35–39 groups. Furthermore, the more severe the disability and the higher the CCI score, the higher the hypertension-related hospitalizations fraction (Table 1).
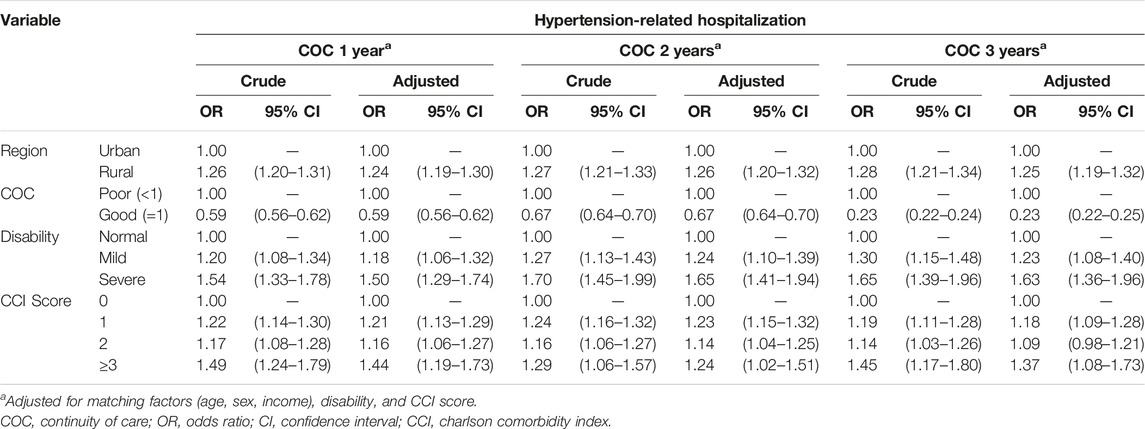
All study participants were divided into COC observation periods of 1, 2, and 3 years, and conditional logistic regression was performed (Table 2); rural areas were found to have higher ORs of hypertension-related hospitalization at 1.24 (95% CI, 1.20–1.31), 1.26 (95% CI, 1.20–1.32), and 1.25 (95% CI, 1.19–1.32), respectively, and poor COC was related to lower ORs than good COC for hypertension-related hospitalization of 0.59 (95% CI, 0.56–0.62), 0.67 (95% CI, 0.64–0.70), 0.23 (95% CI, 0.22–0.25), respectively.
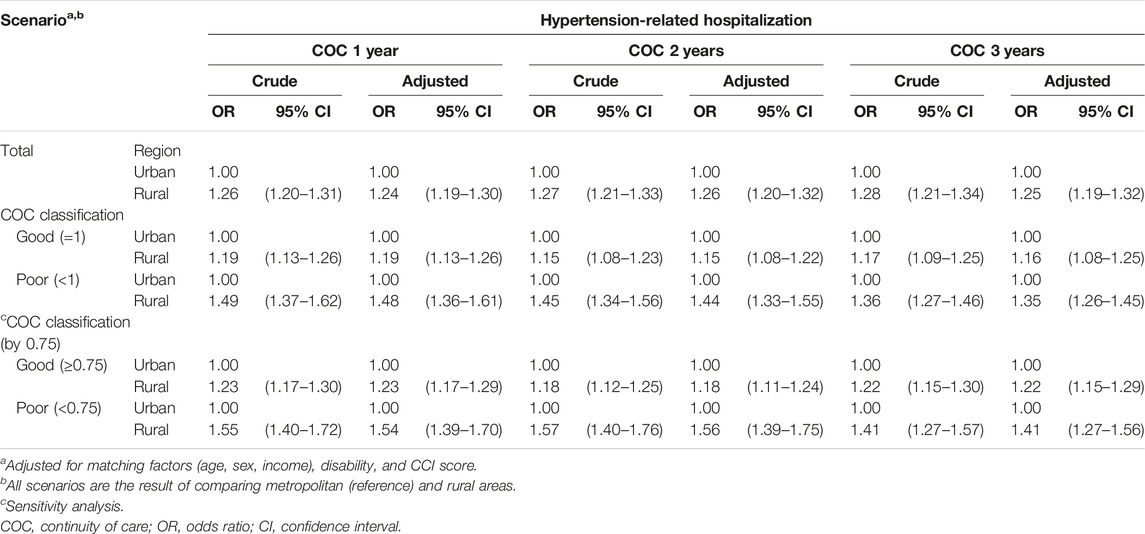
The results in Table 2 confirm that the odds of hypertension-related hospitalization differed according to the COC. Hence, a stratified analysis was performed by dividing the participants into good COC (COC = 1) and poor COC groups (COC < 1) (Table 3). In the good COC group, rural residence was associated with higher ORs of hypertension-related hospitalization at 1.19 (95% CI, 1.13–1.26), 1.15 (95% CI, 1.08–1.22), and 1.16 (95% CI, 1.08–1.25) than urban residence in the COC observation periods of 1, 2, and 3 years, respectively, and in the poor COC group, rural residence was associated with higher ORs at 1.48 (95% CI, 1.36–1.61), 1.44 (95% CI, 1.33–1.55), and 1.35 (95% CI, 1.26–1.45), respectively.
Sensitivity analysis was performed by changing the COC criterion to 0.75 (Table 3). In the good COC group (COC ≥ 0.75), rural residence was associated with higher ORs of hypertension-related hospitalization at 1.23 (95% CI, 1.17–1.29), 1.18 (95% CI, 1.11–1.24), and 1.22 (95% CI, 1.15–1.29) than urban residence in the COC observation periods of 1, 2, and 3 years, respectively, and in the poor COC group (COC < 0.75), rural residence was associated with higher ORs at 1.54 (95% CI, 1.39–1.70), 1.56 (95% CI, 1.39–1.75), and 1.41 (95% CI, 1.27–1.56), respectively, than urban residence. The results of the analysis confirmed that the odds of hypertension-related hospitalization were higher among participants living in rural areas than among those living in urban areas. In addition, there was a difference in the odds of hypertension-related hospitalization between urban and rural areas due to COC.
Discussion
Principal Results
We investigated the factors related to the occurrence of hypertension-related hospitalizations of hypertensive patients, focusing on regional health disparities, using nationally representative medical service claims data. In addition, we confirmed the health disparity in regions according to the maintenance of the continuity of outpatient medical care. Our analysis using NCC matching and conditional logistic regression revealed that the odds of hypertension-related hospitalization were significantly higher in rural areas than in metropolitan areas. This trend was consistent, regardless of the state or calculation period of COC.
Interpretation
Hypertension is one of the most common chronic diseases, and hypertension-related hospitalization can be prevented. Avoidable or preventable hospitalization refers to hospitalization that occurs because adequate primary care is not provided [26], and it has been used as an indicator to identify health inequality in several studies [27–29]. Although hypertension is a primary underlying cardiovascular disease, aggravation of the disease can be prevented through ongoing management [10].
When people achieve a certain level of health through the national medical system and policies, the government’s next task is to solve health inequalities. For example, a statistically significant relationship between racial and ethnic characteristics and preventable hospitalization has been observed in the United States [30]. One of the most prominent issues in South Korea is health inequality between urban and rural regions [31]. According to a study by the Korea Centers for Disease Control and Prevention (KCDC), the regional disparity in the treatment rates of hypertension and diabetes patients has been increasing over the past 3 years [19–21] [32]. There was a statistically significant relationship between residential area and the occurrence of hypertension-related hospitalization, even when other conditions were sufficiently controlled. This result is similar to that of other studies [33, 34] that compared preventable hospitalization in rural and urban areas. The disparity may be the result of physical access to medical facilities, socioeconomic development of a given region, and differences in demographic structure [35, 36].
In addition, this study confirms the results of many previous studies [37–40], wherein a high COC for chronic diseases was strongly associated with a decrease in avoidable hospitalization. Those with a COC value of 1 had lower odds of hypertension-related hospitalization than those with a COC value <1. This trend was maximized when the COC calculation period was 3 years. The occurrence of avoidable hospitalization entails social and economic losses. In a study conducted in Portugal, the average estimated cost per avoidable hospitalization was €2,515 [41].
The Korean government implemented the primary healthcare chronic disease management pilot project in January 2019 after implementing the community-based hypertension and diabetes registry program, a chronic disease management program at the clinical level, a community-based primary care project, and a pilot project for reimbursing chronic disease care [42]. The primary healthcare chronic disease management pilot project aimed to ensure continuous management of patients with high blood pressure and diabetes who visited neighborhood clinics and is in the process of converting to a main project. Several studies have shown that primary care-centered chronic disease management is cost-effective and improves COC and medication adherence [43–46]. To improve COC, it is important to introduce policies at the national level and make steady efforts to manage health at the individual level.
On the other hand, subgroup analysis revealed the possibility of a high COC reducing the health disparity between the regions. We found that the difference in interregional hypertension-related hospitalization was significant even in the group with a high COC. However, the OR of the residential area variable tended to be lower in the group with COC values closer to 1. This trend implies that a high COC may reduce regional disparities. These results are meaningful because they can be used as evidence for asserting the importance of improving the COC.
Limitations
This study had several limitations. First, the matching rate may have been low because of the misclassification of codes in the claim data. However, since we confirmed the hospitalization for hypertension and cardiovascular disease, and as cardiovascular disease trends are being monitored by the National Health Insurance (NHI) and Health Insurance Review & Assessment Service (HIRA), we believe that the code mismatch rate in our study is low [47]. Second, individual health behaviors and regional medical resources could not be considered as variables due to data limitations. Some studies have reported differences in health behaviors between regions, such as drinking, smoking, and regular walking [48, 49], and differences in medical resource allocation that can eventually lead to health disparities [50, 51]. These findings suggest the need for detailed research in the future. Third, through the results of this study, it was confirmed that regional health disparities occur due to differences in the quality of primary care, but other causes could not be determined. Regional health disparities are affected by underlying factors such as differences in healthcare infrastructure, aging populations, and the environment. Therefore, future studies are needed to confirm the impact in addition to primary care. Fourth, hospitalization for other diseases in hypertensive patients may affect hypertension-related hospitalizations, but this study did not consider these effects. However, we tried to control for this effect by adjusting for the health-related variable (disability, and CCI).
Conclusion
The odds of hypertension-related hospitalizations were significantly higher in rural residents than in urban residents, regardless of the state of COC and observation period. These results can be viewed as evidence of regional health disparities. Although it was confirmed that regional health disparities were somewhat resolved through the enhancement of COC, regional health disparities still existed due to differences in the quality of primary care. Therefore, to reduce regional health disparities, both the promotion of COC and the improvement of the quality of primary care must be achieved.
Ethics Statement
The studies involving human participants were reviewed and approved by the Institutional Review Board of Yonsei University (1041849-202107-SB-107-01). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
Conceptualization: W-RL, JK, JYJ, MSK, and K-BY. Methodology: W-RL, JK, and K-BY. Formal analysis: W-RL and K-BY. Writing—original draft: W-RL, JK, JYJ, MSK, and K-BY. Writing—review and editing: W-RL and K-BY.
Funding
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No. 2022R1F1A1074383).
Conflict of Interest
The authors declare that they do not have any conflicts of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/ijph.2023.1605495/full#supplementary-material
References
1.Statistics Korea. Population and Population Density by Region (2021). Available from: https://www.index.go.kr/potal/main/EachDtlPageDetail.do?idx_cd=1007 (Accessed July 22, 2021).
2. Rice, N, and Smith, PC. Ethics and Geographical Equity in Health Care. J Med Ethics (2001) 27(4):256–61. doi:10.1136/jme.27.4.256
3.Challenges and Successes in Reducing Health Disparities: Workshop Summary. Washington, D.C.: National Academies Press; (2008).
4. Tinetti, ME, Fried, TR, and Boyd, CM. Designing Health Care for the Most Common Chronic Condition-Mmultimorbidity. Jama (2012) 307(23):2493–4. doi:10.1001/jama.2012.5265
5. Jang, IY, Lee, HY, and Lee, E, 50th Anniversary Committee of Korean Geriatrics Society. Geriatrics Fact Sheet in Korea 2018 from National Statistics. Ann Geriatr Med Res (2019) 23(2):50–3. doi:10.4235/agmr.19.0013
6. Ezzati, M, Lopez, AD, Rodgers, A, Vander Hoorn, S, and Murray, CJ, Comparative Risk Assessment Collaborating Group. Selected Major Risk Factors and Global and Regional burden of Disease. Lancet (2002) 360:1347–60. doi:10.1016/S0140-6736(02)11403-6
7. Yusuf, S, Hawken, S, Ôunpuu, S, Dans, T, Avezum, A, Lanas, F, et al. Effect of Potentially Modifiable Risk Factors Associated with Myocardial Infarction in 52 Countries (The INTERHEART Study): Case-Control Study. The lancet (2004) 364(9438):937–52. doi:10.1016/S0140-6736(04)17018-9
8.The Korean Society of Hypertension (2021). Korea Hypertension Fact Sheet 2021. Available from: http://www.koreanhypertension.org/reference/guide?mode=read&idno=4581 (Accessed December 13, 2021).
9. Boersma, E, Maas, AC, Deckers, JW, and Simoons, ML. Early Thrombolytic Treatment in Acute Myocardial Infarction: Reappraisal of the golden Hour. The Lancet (1996) 348(9030):771–5. doi:10.1016/S0140-6736(96)02514-7
10. Weinick, RM, Billings, J, and Thorpe, JM. Ambulatory Care Sensitive Emergency Department Visits: a National Perspective. Acad Emerg Med (2003) 10(5):525–526. doi:10.1197/aemj.10.5.525-b
11.Continuity and coordination of cere: a practice brief to support implementation of the World Health Organization. Framework on Integrated People-Centred Health Services. World Health Organization (WHO) (2018). Available at: https://apps.who.int/iris/handle/10665/274628?show=full (Accessed December 13, 2021).
12. Lee, W-R, Yoo, K-B, Jeong, J, and Koo, JH. Chronic Disease Management for People with Hypertension. Int J Public Health (2022) 67:1604452. doi:10.3389/ijph.2022.1604452
13. Longman, JM, Passey, ME, Ewald, DP, Rix, E, and Morgan, GG. Hospitalizations for Chronic Ambulatory Care Sensitive Conditions-A Useful Measure of Potentially Preventable Hospitalization? BMC Health Serv Res (2015) 15(1):472–4. doi:10.1186/s12913-015-1137-0
14. Cho, S, Shin, JY, Kim, HJ, Eun, SJ, Kang, S, Jang, WM, et al. Chasms in Achievement of Recommended Diabetes Care Among Geographic Regions in Korea. J Korean Med Sci (2019) 34(31):e190. doi:10.3346/jkms.2019.34.e190
15. Kwon, S. Thirty Years of National Health Insurance in South Korea: Lessons for Achieving Universal Health Care Coverage. Health Pol Plann (2009) 24(1):63–71. doi:10.1093/heapol/czn037
16.Population coverage (2021). National Health Insurance Services (NHIS). Available online: https://www.nhis.or.kr/english/wbheaa02400m01.do (Accessed January 7, 2023).
17. Lee, J, Lee, JS, Park, SH, Shin, SA, and Kim, K. Cohort Profile: The National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int J Epidemiol (2017) 46(2):e15. doi:10.1093/ije/dyv319
18. Špinar, J. Hypertension and Ischemic Heart Disease. Cor et Vasa (2012) 54(6):e433–8. doi:10.1016/j.crvasa.2012.11.002
19. Daly, B, Toulis, KA, Thomas, N, Gokhale, K, Martin, J, Webber, J, et al. Increased Risk of Ischemic Heart Disease, Hypertension, and Type 2 Diabetes in Women with Previous Gestational Diabetes Mellitus, a Target Group in General Practice for Preventive Interventions: a Population-Based Cohort Study. PLoS Med (2018) 15(1):e1002488. doi:10.1371/journal.pmed.1002488
20. Pistoia, F, Sacco, S, Degan, D, Tiseo, C, Ornello, R, and Carolei, A. Hypertension and Stroke: Epidemiological Aspects and Clinical Evaluation. High Blood Press Cardiovasc Prev (2016) 23(1):9–18. doi:10.1007/s40292-015-0115-2
21. Jeon, B, Noguchi, H, Kwon, S, Ito, T, and Tamiya, N. Disability, Poverty, and Role of the Basic Livelihood Security System on Health Services Utilization Among the Elderly in South Korea. Soc Sci Med (2017) 178:175–83. doi:10.1016/j.socscimed.2017.02.013
22. Quan, H, Li, B, Couris, CM, Fushimi, K, Graham, P, Hider, P, et al. Updating and Validating the Charlson Comorbidity index and Score for Risk Adjustment in Hospital Discharge Abstracts Using Data from 6 Countries. Am J Epidemiol (2011) 173(6):676–82. doi:10.1093/aje/kwq433
23. Lin, IP, and Wu, SC. Effects of Long-Term High Continuity of Care on Avoidable Hospitalizations of Chronic Obstructive Pulmonary Disease Patients. Health Policy (2017) 121(9):1001–7. doi:10.1016/j.healthpol.2017.06.010
25. Koletsi, D, and Pandis, N. Conditional Logistic Regression. Am J Orthod Dentofacial Orthop (2017) 151(6):1191–2. doi:10.1016/j.ajodo.2017.04.009
26. Chen, IH, and Chi, MJ. Effects of Self-Care Behaviors on Medical Utilization of the Elderly with Chronic Diseases - A Representative Sample Study. Arch Gerontol Geriatr (2015) 60(3):478–85. doi:10.1016/j.archger.2015.01.014
27. Löfqvist, T, Burström, B, Walander, A, and Ljung, R. Inequalities in Avoidable Hospitalisation by Area Income and the Role of Individual Characteristics: a Population-Based Register Study in Stockholm County, Sweden. BMJ Qual Saf (2014) 23(3):206–14. doi:10.1136/bmjqs-2012-001715
28. Mercier, G, Georgescu, V, and Bousquet, J. Geographic Variation in Potentially Avoidable Hospitalizations in France. Health Aff (Millwood) (2015) 34(5):836–43. doi:10.1377/hlthaff.2014.1065
29. Wenner, J, Biddle, L, Gottlieb, N, and Bozorgmehr, K. Inequalities in Access to Healthcare by Local Policy Model Among Newly Arrived Refugees: Evidence from Population-Based Studies in Two German States. Int J Equity Health (2022) 21(1):11. doi:10.1186/s12939-021-01607-y
30. Doshi, RP, Aseltine, RH, Sabina, AB, and Graham, GN. Racial and Ethnic Disparities in Preventable Hospitalizations for Chronic Disease: Prevalence and Risk Factors. J Racial Ethn Health Disparities (2017) 4(6):1100–6. doi:10.1007/s40615-016-0315-z
31. Kim, JH. An Exploratory Study of Health Inequality Discourse Using Korean Newspaper Articles: A Topic Modeling Approach. J Prev Med Public Health (2019) 52(6):384–92. doi:10.3961/jpmph.19.221
32. Jeong, E. 2021 Regional Health Statistics at a Glance - Summary (2022). Available from: https://chs.kdca.go.kr/chs/stats/statsMain.do (Accessed July 22, 2022).
33. Nayar, P, Nguyen, AT, Apenteng, B, and Yu, F. Preventable Hospitalizations: Does Rurality or Non-physician Clinician Supply Matter? J Community Health (2012) 37(2):487–94. doi:10.1007/s10900-011-9468-1
34. Thorpe, JM, Van Houtven, CH, Sleath, BL, and Thorpe, CT. Rural-urban Differences in Preventable Hospitalizations Among Community-Dwelling Veterans with Dementia. J Rural Health (2010) 26(2):146–55. doi:10.1111/j.1748-0361.2010.00276.x
35. Uzzoli, A, Bán, A, Beke, S, Pál, V, and Vitrai, J. Health Inequality and its Regional Disparities in Hungary: A Case Study on the Role of Access to Health Care. Curr Polit Econ Russia, East Cent Europe (2020) 35(1):1–48.
36. Olsen, M, Norheim, OF, and Memirie, ST. Reducing Regional Health Inequality: a Sub-national Distributional Cost-Effectiveness Analysis of Community-Based Treatment of Childhood Pneumonia in Ethiopia. Int J Equity Health (2021) 20(1):9. doi:10.1186/s12939-020-01328-8
37. Busby, J, Purdy, S, and Hollingworth, W. How Do Population, General Practice and Hospital Factors Influence Ambulatory Care Sensitive Admissions: a Cross Sectional Study. BMC Fam Pract (2017) 18(1):67. doi:10.1186/s12875-017-0638-9
38. Kao, Y-H, Lin, W-T, Chen, W-H, Wu, S-C, and Tseng, T-S. Continuity of Outpatient Care and Avoidable Hospitalization: a Systematic Review. Am J Manag Care (2019) 25(4):e126–e134.
39. Cheng, SH, Chen, CC, and Hou, YF. A Longitudinal Examination of Continuity of Care and Avoidable Hospitalization: Evidence from a Universal Coverage Health Care System. Arch Intern Med (2010) 170(18):1671–7. doi:10.1001/archinternmed.2010.340
40. Cho, KH, Nam, CM, Choi, Y, Choi, JW, Lee, SH, and Park, EC. Impact of Continuity of Care on Preventable Hospitalization of Patients with Type 2 Diabetes: a Nationwide Korean Cohort Study, 2002-10. Int J Qual Health Care (2016) 28(4):478–85. doi:10.1093/intqhc/mzw050
41. Rocha, JVM, Marques, AP, Moita, B, and Santana, R. Direct and Lost Productivity Costs Associated with Avoidable Hospital Hospitalizations. BMC Health Serv Res (2020) 20(1):1–9.
42. Kim, S. Effect of Primary Care-Level Chronic Disease Management Policy on Self-Management of Patients with Hypertension and Diabetes in Korea. Prim Care Diabetes (2022) 16:677–83. doi:10.1016/j.pcd.2022.08.003
43. Lee, WR, Yoo, KB, Jeong, J, and Koo, JH. Chronic Disease Management for People with Hypertension. Int J Public Health (2022) 67:1604452. doi:10.3389/ijph.2022.1604452
44. Kim, W, Lee, SA, and Chun, SY. A Cost-Effectiveness Analysis of the Chronic Disease Management Program in Patients with Hypertension in Korea. Int J Qual Health Care (2021) 33(2):mzab073. doi:10.1093/intqhc/mzab073
45. Lee, EW, Kim, HS, Yoo, BN, Lee, EJ, and Hyun Park, J. Effect of a Primary Care-Based Chronic Disease Management Program for Hypertension Patients in South Korea. Iran J Public Health (2022) 51(3):624–33. doi:10.18502/ijph.v51i3.8939
46. Kim, JA, Kim, ES, and Lee, EK. Evaluation of the Chronic Disease Management Program for Appropriateness of Medication Adherence and Persistence in Hypertension and Type-2 Diabetes Patients in Korea. Medicine (Baltimore) (2017) 96(14):e6577. doi:10.1097/md.0000000000006577
47. Kim, J, Shin, SJ, and Kang, HT. The Association between Triglyceride-Glucose index, Cardio-Cerebrovascular Diseases, and Death in Korean Adults: A Retrospective Study Based on the NHIS-HEALS Cohort. PloS One (2021) 16(11):e0259212. doi:10.1371/journal.pone.0259212
48. Lee, GY, and Um, YJ. Factors Affecting Obesity in Urban and Rural Adolescents: Demographic, Socioeconomic Characteristics, Health Behavior and Health Education. Int J Environ Res Public Health (2021) 18(5):2405. doi:10.3390/ijerph18052405
49. Seo, AR, and Park, KS. Residential Characteristics as Factors Related to Healthy Behavior Practices-Decision Tree Model Analysis Using a Community Health Survey from Korea. Int J Environ Res Public Health (2022) 19(12):7390. doi:10.3390/ijerph19127390
50. Chang, I, and Kim, BH. Regional Disparity of Medical Resources and its Effect on Age-Standardized Mortality Rates in Korea. Ann Reg Sci (2019) 62(2):305–25. doi:10.1007/s00168-019-00897-z
Keywords: hypertension, hypertension-related hospitalization, continuity of care, regional health disparity, nested case-control study, NHIS-NSC
Citation: Lee W-R, Koo JH, Jeong JY, Kim MS and Yoo K-B (2023) Regional Health Disparities in Hypertension-Related Hospitalization of Hypertensive Patients: A Nationwide Population-Based Nested Case-Control Study. Int J Public Health 68:1605495. doi: 10.3389/ijph.2023.1605495
Received: 16 October 2022; Accepted: 12 January 2023;
Published: 24 January 2023.
Edited by:
Nino Kuenzli, Swiss Tropical and Public Health Institute (Swiss TPH), SwitzerlandCopyright © 2023 Lee, Koo, Jeong, Kim and Yoo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ki-Bong Yoo, eWtib25nQHlvbnNlaS5hYy5rcg==
This Original Article is part of the IJPH Special Issue “Health in all Sustainable Development Goals.”
 Woo-Ri Lee
Woo-Ri Lee