- 1Department of Health Care Management, Faculty of Economics and Management, Technical University Berlin, Berlin, Germany
- 2European Observatory on Health Systems and Policies, Brussels, Belgium
- 3European Observatory on Health Systems and Policies, London School of Economics and Political Science, London, United Kingdom
Objectives: Skill-mix changes to step up health promotion and prevention are increasing, but there is limited evidence on their effects.
Methods: Overview of reviews, based on a protocol. The search was carried out in six databases, screening was performed ensuring high interrater reliability. All countries, health professions and lay workers in all settings (except hospitals) were included, quality appraisals performed.
Results: A total of 31 systematic reviews were included. Expanded roles performing outreach (e.g., home visits) had mostly positive effects on access and health outcomes, primarily for hard-to-reach groups. Task-shifting in colorectal or skin cancer screenings (performed by advanced practice nurses) were suggested effective; supporting roles (by community health workers) increased uptake in screenings, but based on limited evidence. Expanded roles of various professions focusing on lifestyle modification showed promising effects in most reviews, including weight, diet, smoking cessation and physical activity. Reviews on cost-effectiveness were based on limited evidence.
Conclusion: Promising skill-mix changes included expanded roles providing lifestyle modifying interventions, task-shifting, and outreach roles for hard-to-reach groups, whereas evidence on costs was limited.
Introduction
The rise in chronic conditions globally (1–3) has increased policy attention on health promotion, reinforced by the 2018 Astana declaration (4, 5). Developing healthy policies and integrating health promotion in primary care have shown some, albeit limited progress (6, 7). Primary care services focus on curative care and less on prevention (8), while health professionals often face high workloads and lack the necessary skills (9). In response, several countries have changed the skill-mix of their workforce, defined as changes to the skills, roles or tasks of individual health professions or teams (10, 11). Examples are new roles (e.g., outreach), task-shifting or multiprofessional collaboration (10–12). In Europe, the health workforce has increasingly diversified (13), in the United States (U.S.), high-performing primary care practices have included new professional roles, outreach and patient coaching (14).
Frequent skill-mix changes have been introduced among nurses and pharmacists. An OECD study highlighted that in many countries, nurses work in expanded roles in prevention (15). The roles of pharmacists increasingly include prevention activities, in particular since the COVID-19 pandemic (16, 17). Other studies covered physician assistants, medical assistants or dental hygienists (18–20). Moreover, community health workers (CHW) are increasingly working in prevention (21–23). Reasons triggering skill-mix changes have been referred to as provider shortages, limited access to services, increasing chronic conditions and the need for tailored services for hard-to-reach populations (11, 24, 25).
Several systematic reviews exist on skill-mix, but often focus only on single professions or on a narrow set of outcomes. This paper takes a larger study on skill-mix as a starting point (24), which consisted of an overview of reviews and country case studies, published as a policy-focused book (25). It found that many European countries have adopted strategies on health promotion and patient-centred care and identified a range of reviews on skill-mix across the life cycle (25). However, the evidence was synthesized at a highly aggregate level, a detailed analysis of individual reviews was not undertaken, it focused on Europe and other high-income countries and the search was conducted in 2018.
The present study therefore aimed to: i) update the identification of systematic reviews on skill-mix in health promotion, primary or secondary prevention; ii) cover all countries; iii) apply a skill-mix typology; iv) synthesise the evidence on outcomes for groups of interventions.
Methods
This overview of systematic reviews (26, 27) expands and updates the evidence of a previous study on skill-mix innovation, effectiveness and implementation (24, 25). The protocol was registered in PROSPERO (Nr. CRD42018090272) (28), published in March 2018, when the search had taken place and screening process had started, but was not finalised. For this study, there were the following deviations from the protocol. First, for this paper, there was no year restriction in the search applied, contrary to the protocol and earlier work which covered the years 2010–2018 only (25). This study provided an update of the search in June 2021. Second, this paper focused on health promotion, primary and secondary prevention; whereas the protocol and previous work covered more areas (e.g., health promotion, prevention, rehabilitation, management of diseases) (24, 25). Third, high, middle- and low-income countries were included, contrary to the protocol and earlier work (25) which focused on Europe and other high-income countries and excluded reviews that only covered low- and middle-income countries. Finally, this study applied skill-mix typologies, which was not performed in earlier work (24, 25), and used three typologies (instead of four as originally specified in the protocol, see section: data synthesis).
Definition
Skill-mix changes were defined as new or changing roles, tasks or skills of health professionals and/or teams (28). Examples include role expansions (e.g., new roles, roles which did not exist previously or were not routinely performed); task-shifting (from higher to lower qualified professions); and team work (multiprofessional collaboration) (10, 24, 29). All health professions were included (e.g., physicians, nurses, midwives, physician assistants, pharmacists, medical assistants) as well as CHWs with no or limited training.
Types of Studies
All systematic reviews with narrative or meta analysis were included with comparison groups on skill-mix changes and outcomes. Excluded were rapid reviews, scoping reviews, integrative reviews, protocols and other studies. Reviews published in languages other than English were excluded.
Population and Setting
All population groups and individuals in ambulatory care, community or other settings, including at home were included. Interventions that focused on the interface between inpatient and ambulatory care were also included. Hospitals were excluded, as was emergency medicine.
Types of Intervention
Interventions covered skill-mix changes providing health promotion (for healthy populations) or prevention activities (preventing the onset of diseases). Examples include prevention for population group (e.g., maternal and child health (MCH), immunization, screenings) or individual at-risk factors (e.g., smoking, weight/obesity) (4, 30). This review covered primary and secondary prevention, but excluded tertiary prevention. The latter is commonly addressed by improvements of treatment and medication regimens or rehabilitation, which was not the focus of this study (4, 30) contrary to earlier work (25).
Comparison
The comparison groups were either standard-of-care, usual care or previous skill-mix configurations as identified in the reviews.
Outcome Measures
Primary outcomes were individual or population-related outcomes (e.g., health- or disease-specific, mortality, patient experience) and health system related outcomes (e.g., access to services, resource use, costs).
Search Method
Electronic Searches
The search strategy was reviewed internally, piloted, and developed with a librarian specialised in conducting systematic searches. It was conducted in January 2018 and updated on 24 June 2021. It was run in Embase first, then adapted to the following databases: Medline in Ovid, Cochrane CENTRAL, Web of Science Core Collection, CINAHL EBSCOhost (Cumulative Index to Nursing and Allied Health Literature), PsychINFO Ovid and Google scholar. Search terms included combined Medical Subject Headings with free text words (Supplementary Material S1). Filters were used depending on the databases to identify systematic reviews. No supplementary primary studies were included. In addition to the electronic search, snowballing was used to identify other reviews by going through the reference lists of relevant reviews.
Data Collection and Analysis
Selection of Reviews
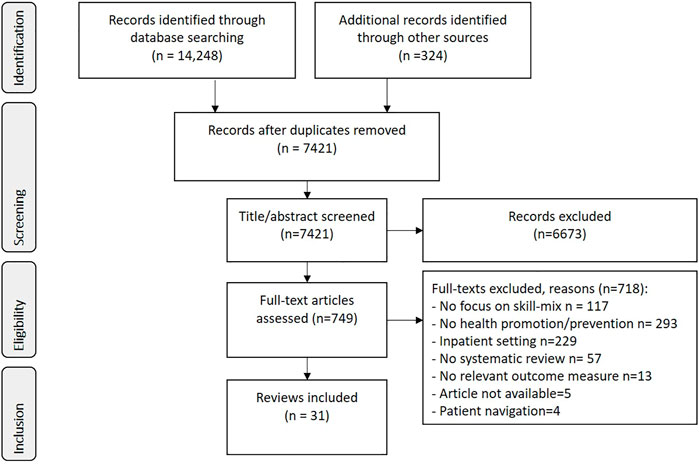
The electronic search produced a total of 14,572 hits from electronic databases and snowballing (see PRISMA Flow Diagram (31), Figure 1). After the removal of duplicates, screening of the titles and abstracts was executed by CM, JW, MK in Rayyan (32). Prior to the screening, the title/abstracts of the first 100 hits and the first 20 full-text articles were screened by the three researchers resulting in high agreement rates (title/abstract: 0.86, full-text: 0.78), using an extended version of Cohen’s kappa coefficient which is suitable for three researchers (33, 34). Of the 749 full-text versions assessed by the researchers, 718 were excluded (see Figure 1).
Data Extraction
An excel data extraction form was used (35), covering country, participants, professions, intervention, comparison group, care settings and outcomes. A piloting phase was performed, during which one researcher double-checked the data extraction of the first five reviews of the other reviewers. Differences were resolved through discussion.
Data Synthesis
Data was narratively synthesized. Meta-analysis was not possible due to the heterogeneity of the interventions and outcomes. Data synthesis was undertaken for the following themes: MCH; screenings; vaccination; lifestyle modification related to Smoking, Nutrition, Physical Activity, Weight reduction/management (SNAPW) (36). Potential overlap in individual studies, e.g., the population, interventions, comparators, and/or outcomes was not examined.
The interventions described in the reviews were categorized into the following three skill-mix typologies: 1) task-shifting, defined as shifting tasks from a higher to a lower qualified professional/worker (or as part of teams) with a higher qualified professional in the comparison group; 2) role expansion, defined as new roles, professions which did not exist previously or were not routinely performed, with various comparison groups (other professions, usual care), 3) other/hybrid/various, defined as all other interventions. In the protocol, it was planned to also use additional typologies on team work and collaboration, but this was not feasible, hence a third category was used instead. Reviews were grouped by typology, cadres (by health professions, lay workers), outcomes and population groups. All skill-mix changes were covered, except for the role of patient navigators, which was covered elsewhere (37).
We followed the Preferred Reporting Items for Overview of Reviews (PRIOR) guideline developed for overview of reviews of healthcare interventions (Supplementary Material S2) (38).
Quality Assessment
Quality appraisals were performed two researchers (LP, CM), after piloting, using the Assessment of Multiple Systematic Reviews (AMSTAR) II checklist (39). Inconsistencies were discussed until agreement was reached. Summary scores for each review and by sub-themes were provided.
Results
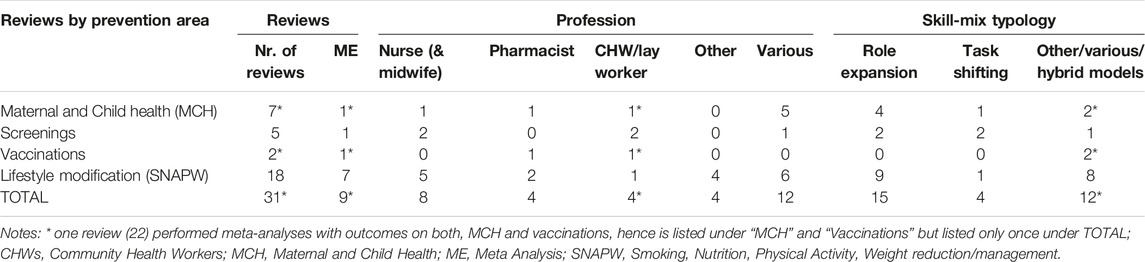
A total of 31 reviews were included. Seven reviews focused on skill-mix changes on MCH, five on screenings, two on vaccinations and 18 on lifestyle modifications (Table 1). One review covered both vaccination and MCH (22). Eight reviews focused on changes to the roles of nurses (and midwives), and four on pharmacists and lay workers/community health workers. In terms of skill-mix typology, 15 reviews analysed role expansions, four task-shifting from higher to lower qualified professions or teams. Among the remaining 12 reviews, either task-shifting and role expansion were both covered, hybrid or multiple models were analysed (e.g., case manager roles and introducing team work), or it was unclear what skill-mix typology was covered.
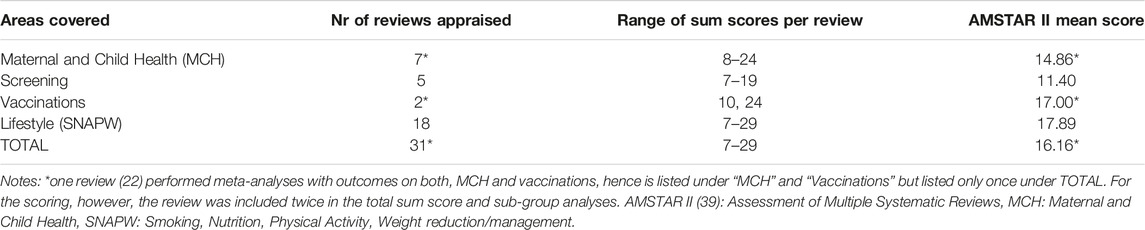
Quality of the Reviews
The quality appraisal ranged from low to high quality (summary scores: 7 to 29 points) (Table 2). The lowest mean score was identified for the reviews on screening, the highest on lifestyle modification. A full list of the AMSTAR II appraisals is available in Supplementary Material S3.
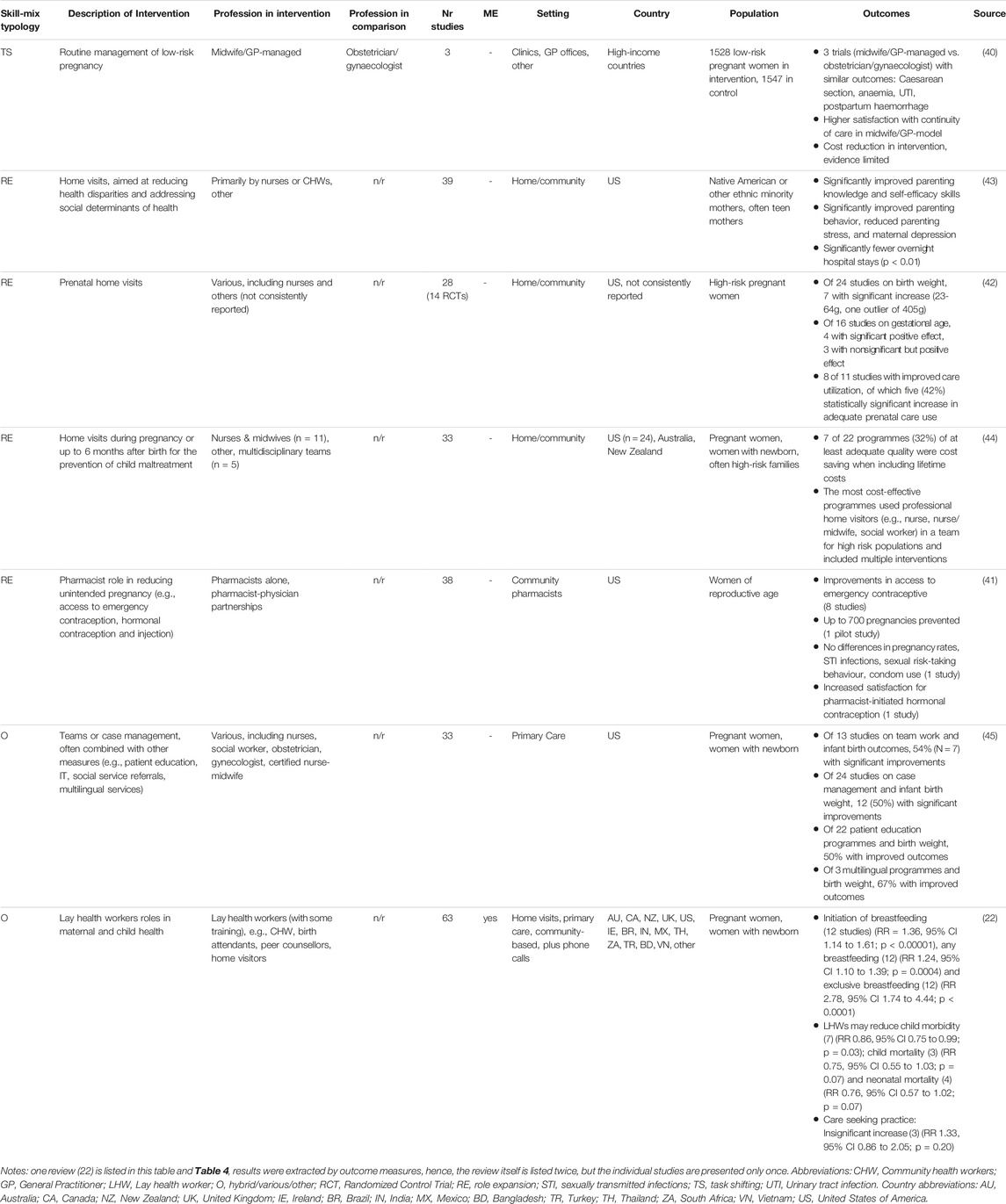
Maternal and Child Health (MCH)
Of the seven reviews (Table 3), one analysed task-shifting, whereby midwives or midwife/GP teams took over routine visits of women with low-risk pregnancy from obstetricians/gynecologists (40). Four reviews focused on role expansions, of which one analysed pharmacists providing emergency contraception (41) and three prenatal and/or postnatal home visits delivered by nurses, CHWs or multiprofessional teams (42–44). The remaining two reviews covered multiple skill-mix typologies, one subsumed task-shifting and role expansion performed by lay workers (22), the other changes to team work and introducing case manager roles (45).
The review on task-shifting (40) showed no differences in the majority of clinical outcomes between the midwife/GP and obstetritian/gynecologists model. There was higher satisfaction with continuity of care and indication of reduced costs in the midwife-GP model. The midwife/GP model had lower rates of pregnancy-induced hypertension and pre-eclampsia as well as preterm delivery and antepartum haemorrhage; however, recognition of fetal malpresentation tended to be higher in the obstetritian/gynecologist group.
In the three reviews analysing pre- or postnatal home visits, most interventions were delivered by nurses, CHWs or teams and covered parenting skills improvements, lactation support, education or substance abuse prevention focusing on ethnic minorities or at-risk groups. Significantly improved outcomes were shown for increased parenting knowledge, reduced stress, maternal depression and fewer hospital stays, if targeted at ethnic minorities or focused on addressing social determinants of health (43). Improved utilization of prenatal care were found (8 of 11 studies), but mixed results on birth weight and gestational age (42). The economic analysis (44) showed large variation in the number of home visits per programme and the educational background of the home visitors. It found variation in the incremental costs of home visits, ranging from USD 1,800 to 30,000 per family, and in the estimated cost-effectiveness per case of maltreatment prevented.
The review analysing pharmacists with expanded roles in providing emergency contraception (e.g., provision of depot reinjection, initiation of oral contraceptives) (41) found improvements for women in accessing emergency contraceptives. There was limited evidence on prevention of pregnancies, increased patient satisfaction and several non-significant outcomes were reported (e.g., pregnancy rates) (ibid.). The two remaining reviews covering multiple skill-mix typologies including teamwork and lay health workers providing MCH services (22, 45), showed statistically improved outcomes on breastfeeding (promoting initiation: 1.36, 95% CI 1.14 to 1.61; p < 0.00001; exclusive breastfeeding: RR 2.78, 95% CI 1.74 to 4.44; p < 0.0001), child morbidity (RR 0.86, 95% CI 0.75 to 0.99; p = 0.0) and mortality (RR 0.75, 95% CI 0.55 to 1.03; p = 0.07), but an insignificant increase in care seeking practice, based on meta analyses (22); whereas the other review found improved infant birth outcomes, such as increased infant weight, particularly among multilingual programmes (45).
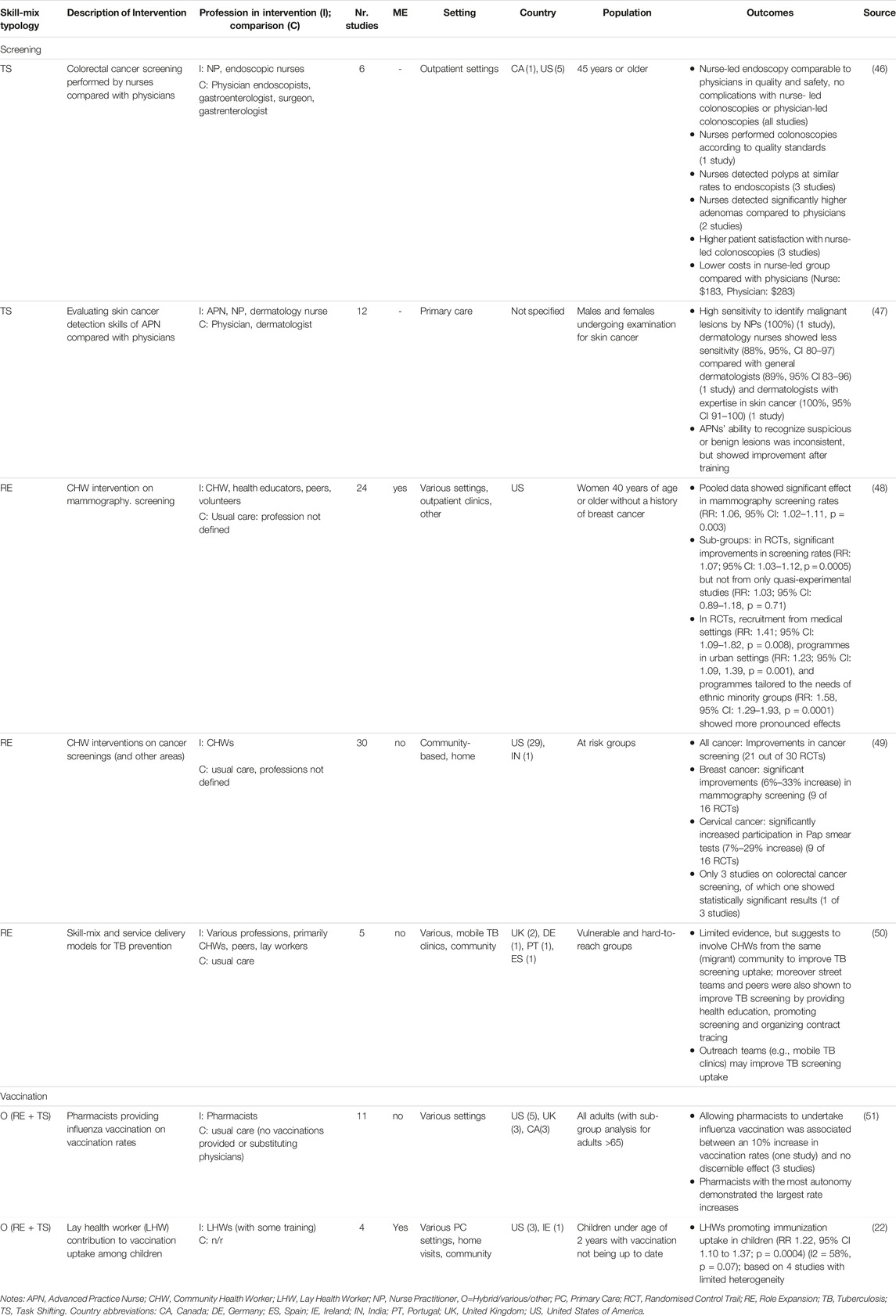
Screenings
Of the five reviews (Table 4) (46–50), two analysed task shifting, whereby nurses performed colorectal cancer and skin cancer screenings (46, 47). Three reviews analysed the roles of CHWs, one on mammography screening uptake (48), one on screenings for several types of cancer (49) and one on TB screening for hard-to-reach populations (50).
Of the reviews on task-shifting from physicians to nurses, there were no differences in the quality of care in colorectal cancer screenings (endoscopies, colonoscopies) provided by Advanced Practice Nurses or other specialized nurses (e.g., endoscopic nurse) compared with physicians (e.g., endoscopists, gastroenterologists) (46), but significantly higher levels of adenomas detected by these nurses compared with physicians. Patient satisfaction was higher in the nurse-led groups. For skin cancer screenings performed by specialized nurses, results were mixed by nurses’ qualification and training (47). Nurse Practitioners if adequately trained were shown to be able to identifiy malignant lesions with equal levels of sensitivity to dermatologists with expertise in skin cancer and higher levels of sensitivity than dermatologists. However, dermatology nurses showed lower sensitivity (ibid.).
A review on CHWs and screenings found statistically higher mammography screening rates when CHWs provided, e.g., outreach, education, home visits, sessions in communities (RR: 1.06, 95% CI: 1.02–1.11, p = 0.003), with sub-group analyses showing more pronounced effects for programmes targeting ethnic minorities, participants recruited from medical settings and in urban areas (48). In a review of various screenings, CHWs performed education, counseling, case management, navigation assistance, facilitated access and social support, which were delivered in collaboration with or supervised by other health professionals (49). The review found significant improvements in screening uptake for mammography (6%–33% increase) and cervical cancer (7%–29% increase in pap smear tests) compared to usual care. The review on tuberculosis prevention (50) focused on hard-to-reach populations, services were performed by various professions, but with a focus on CHWs, especially from the same migrant community, street teams, peers and outreach teams. It showed improved TB screening uptake with health education, promoting screening uptake and organizing contract tracing, yet based on limited evidence (ibid.).
Vaccinations
The two reviews on vaccinations (Table 4) covered task-shifting and role expansion with limited delination of the two concepts (22, 51). The review on community pharmacists (51) found that influenza vaccination rates varied but pharmacists with greater autonomy showed higher vaccination rates. There was some evidence of a small effect of pharmacists substituting for physicians which also impacts on vaccination rates.
The meta-analysis on the role of lay health workers in promoting access to immunization (through home visits, postcards or phone calls, or both) for specifically for children (under age of 2 years) whose immunization schedules were not up to date or who had not received any vaccinations (22) found a statistically significant increase in immunization uptake in children (RR 1.22, 95% CI 1.10 to 1.37; p = 0.0004) compared to usual care.
Skill-Mix and Lifestyle Modification
The 18 systematic reviews were grouped following SNAPW (Table 5). One review addressed skill-mix changes on smoking cessation (52), four reviews evaluated skill-mix and lifestyle change related to healthy nutrition (53–56), two covered physical activity (57, 58), five focused on obesity prevention (59–63) and six covered various interventions (64–69).
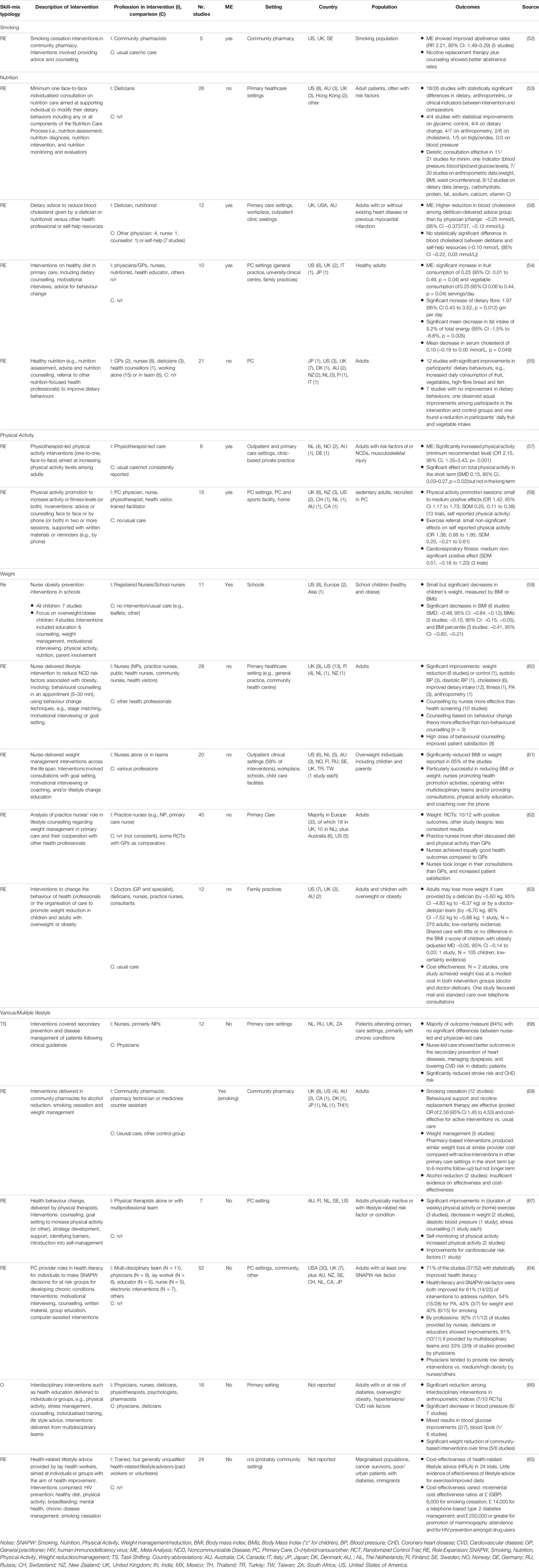
TABLE 5. Skill-mix with focus on SNAPW lifestyle modification (various countries, search performed in 2021).
Smoking
The meta-analysis on community pharmacists providing smoking cessation interventions (either one-to-one counseling or group sessions) to smokers coming to the pharmacy (52) found significantly improved abstinence rates (RR: 2.21, 95% CI: 1.49–3.29) compared to usual or no care.
Nutrition/Diet
Of the four reviews, two analysed the roles of dieticians (53, 56), the others covered multiple professions (54, 55). The two reviews assessing the role of dieticians found that the majority of included studies showed statistically significant improvements favouring the intervention provided by dieticians. In one review, the majority of studies showed significant improvements in dietary, anthropometric or clinical indicators (blood pressure, serum measures, including cholesterol, triglycerides, and sodium; and blood glucose measures), the comparison groups entailed groups which received no intervention, usual care (medical care that did not include nutrition care from any health professional) or minimal care (attendance at a single general nutrition session or provision of a diet sheet) (53). A meta analysis (56) found that dietary advice and related services provided by dieticians significantly lowered blood cholesterol in the short to medium term compared with doctors (−0.25 mmol/L 95% CI: −0.373,737, −0.12 mmol/L). Results were not statistically different between dieticians and self-help resources and there was no evidence that dieticians were better than nurses or other professions, based on the small number of studies included.
The reviews covering interventions targeting diet by multiple professions (e.g., GPs, physicians, nurses, nutritionists) found generally positive outcomes on dietary behaviour (54, 55), of which a meta analysis (54) showed statistically significant increases in fruit (0.25 95% 95% CI: 0.01 to 0.49, p = 0.04) and vegetable consumptions (0.25 95% CI: 0.06 to 0.44, p = 0.01) and dietary fibre among healthy adults, and decreases in total fat intake (5.2% of total energy 95% CI: 1.5%–8.8%, p = 0.005), as well as positive changes in serum cholesterol compared to usual care or no intervention.
Physical Activity
Of the two systematic reviews, one showed that physiotherapist-led one-on-one counselling significantly improved physical activity levels compared to usual care (OR 2.15, 95% CI, 1.35–3.43, p = 0.001) (57). Orrow, Kinmonth (58) found statistically significant small to medium positive effects on adults’ self-reported physical activity levels (OR 1.42, 95% CI 1.17 to 1.73; SDM 0.25, 0.11–0.38), when primary care professionals provided advice or counselling in two or more sessions, whereas referrals found non-significant effects.
Weight Reduction and Obesity Prevention
Of the five reviews (59–63), four covered the roles of nurses (59–62) and one subsumed various professionals (63). Interventions ranged from nurses delivering obesity prevention activities in schools (59), in primary care settings (60–62) and various interventions to promote weight reduction in children and adults with overweight (63).
The reviews on nurse-delivered interventions found statistically improved weight reduction of school children (BMI, SMD: −0.48, 95% CI: −0.84, −0.12) delivered in school settings compared to usual care (e.g., leaflets) or no interventions (59); on adults’ weight, blood pressure, cholesterol, dietary intake (60) and on BMI in 65% of studies compared to interventions provided by other health professionals (61). Positive outcomes were associated with nurses providing individual counselling sessions compared to usual care or health screening (60–62), long-term follow-up assessments compared to GPs (62), health promotion activities, education on physical activity and working within multidisciplinary teams (61).
A review on obesity prevention (63) analysed a wide range of interventions expanding roles or organization of care. The largest effect on adult weight reduction had dietician-delivered interventions (Mean difference (MD): −5.60 kg, 95% CI −4.83 kg to −6.37 kg) or a doctor-dietician shared care team (MD: −6.70 kg, 95% CI −7.52 kg to −5.88 kg), whereas providing education to GP’s, clinical decision tools or increased GP compliance to guidelines led to little or no difference in weight. Two studies investigated costs of which one showed that weight lost was achieved at modest costs in doctor-dietician and doctor-led interventions compared with usual care.
Various Lifestyle-Related Interventions
Of the six reviews (64–69), one analysed task-shifting from physicians to nurses (68), one evaluated extending roles among community pharamacists (69), two evaluated extended roles among various professionals or teams (64, 66), one review covered the roles of physical therapists (67) and one lay workers (65).
In the review on task-shifting from physicians to nurses (68), the interventions were delivered primarily by Nurse Practitioners, following clinical protocols. Nurse-led care was comparable to physician-led care for the majority of outcomes (84%). For the remainder 16%, nurse-led care showed statistically significant improvements, for instance preventing heart diseases or lowering CVD risk among patients with diabetes.
The review on role expansions of community pharamcists (69) covered lifestyle advice on smoking, weight and alcohol consumption; it showed that behavioural support and nicotine replacement therapy interventions were more effective (OR 2.56, 95% CI 1.45–4.53) and cost-effective compared to non-active control, usual care, or other intervention. Pharmacist-delivered weight loss interventions led to similar weight loss as interventions in other primary care settings in the short-term (up to 6 months) with similar provider costs. Longer term effects on weight loss were inconclusive. On interventions targeting reduction of alcohol intake, there was insufficient evidence on effectiveness and cost-effectiveness.
The review on expanded roles of physical therapists in lifestyle advice showed significant improvement in physical activity, weight, blood pressure and cardiovascular risk factors compared to usual care, but based on small numbers of studies (67). Studies with multiple intervention components and several behavioural sessions (instead of one-off exercise prescription or single counselling) were associated with improved outcomes. Yet, many studies analysed short-term effects instead of longer-term outcomes.
A review on primary care professionals providing health literacy interventions (64) reported improvements in 71% of the studies. Interventions varied and included motivational interviewing, counselling, written material, group education, computer-assisted interventions, and multiple interventions. A review on interdisciplinary interventions with behavioural elements on lifestyle changes and effects on SNAPW risk factor outcomes (66) showed mixed results, improvements were identified for weight loss, but not for blood lipids, glucose and blood pressure. Interventions were more effective if provided by collaborations between dieticians, exercise physiologists, psychologists and intensive patient engagement compared to usual care provided by physicians or dieticians only, but required ongoing patient support for long-term effect (66).
The cost-effectiveness analysis on lay workers providing health-related lifestyle-related advice to poor and marginalized groups and cancer survivors, among others, covered various interventions including smoking cessation, diabetes management and HIV prevention among drug users. It found large differences in the cost effectiveness ratios of the interventions (incremental cost ratios estimated at 6,000 GBP for smoking cessation, up to 250,000 GBP or higher for mammography and for HIV prevention) (65).
Discussion
A total of 31 systematic reviews were identified on skill-mix changes focused on health promotion and prevention interventions and outcomes. Seven covered MCH, five screenings and two vaccinations. The majority (N = 18) analysed skill-mix targeting lifestyle modification. There was large variability in the number of reviews available by prevention area and their quality, as demonstrated by the AMSTAR II scores.
New skill-mix roles in MCH were home visitors who often focused interventions on vulnerable or at-risk groups. The results indicated several positive outcomes for mothers or parents, particularly if aimed at women at risk, if provided by health professionals (nurses, social workers) in teams and via bundled interventions. Previous research on patient navigators performing home visits for people with cancer, other chronic conditions, transitional care or on screenings, found improved access, reduced hospital readmissions and improved patient outcomes (37).
Regarding screenings, the included reviews suggested that Advanced Practice Nurses can provide safe and effective screening of a similar quality to physicians for most measures in colorectal cancer and skin cancer, if adequately trained. A Cochrane review on nurses substituting for physicians found similar results in primary care and chronic care, however, it covered all nurses (70), and information on educational background was not always sufficiently available. In our overview of reviews, CHWs were shown to contribute in supportive roles by educating, awareness raising and other interventions and showed improved uptake of cancer screening, particularly among ethnic minorities and hard to reach groups. However, AMSTAR II grading was low for many reviews on screening.
On vaccination, we identified only two reviews. The one on pharmacists suggests that enabling pharmacists to administer vaccines can improve vaccination rates when given greater autonomy. The other review found that lay workers can promote vaccine uptake. No systematic reviews were identified on other professions. In addition, the majority of evidence on screening and vaccinations were from the US, Canada and UK. The experiences of countries during the COVID-19 pandemic (16, 17) allowing non-medical professions to vaccinate, often under pandemic laws, should be evaluated as to the effectiveness, efficiency and scalability in different contexts.
Many of the 18 reviews on lifestyle modification were of high quality, demonstrated by the highest AMSTAR II sum score compared with the other prevention areas. Community pharmacists were suggested to be effective in promoting smoking cessation. Nurse- or dietician-delivered interventions were shown promising to support weight-management. Nurse-delivered interventions were effective when delivered autonomously or within teams, in schools or primary healthcare settings. Interventions led by physiotherapists or other primary care professionals were suggested effective at promoting physical activity. It should be noted, however, that many studies did not analyse long-term effects.
In terms of skill-mix typology, we identified 15 reviews on role expansions, four on task-shifting and 12 “other” (mix of typologies, various, not clearly identifiable). The reasons for the difference in the number of reviews on role expansions vs. task-shifting is unknown. A Cochrane review on task-shifting from physicians to nurses found that little research existed for preventive services and health education (70). The difference may also suggest that skill-mix in health promotion and prevention remains a largely new area, hence reflects role expansion rather than task shifting. This is supported by previous research on providers (71), primary care practices (8, 72) and international skill-mix developments (25). Yet, the 12 reviews in our study identified as “other” suggest that the boundaries of skill-mix changes are not always clear-cut, in line with previous literature (11, 70, 73).
On the task-shifting typology, previous research showed the safety and effectiveness of task-shifting from physicians to nurses or pharmacists, e.g., for patients with chronic conditions (74, 75), and from physicians to nurses for all conditions in primary care (70) or for non-medical prescribing (76–79), if adequately trained.
The majority of reviews in our analysis covered multiple professions. Among the reviews covering single professions, most were on nurses, followed by pharmacists and lay workers. Similar findings were reported for skill-mix and chronic conditions, where the largest number of reviews covered nurses and pharmacists (74). In many countries, nurses’ and pharmacists’ scopes-of-practice has expanded over the last decade (15–17, 80, 81), including prescribing authority for nurses (82), and other clinical tasks (81), which has been reinforced by the COVID-19 pandemic in some countries (17, 83).
The number of systematic reviews in our analysis focusing on costs or cost effectiveness of skill-mix changes was small and showed no coherent results (40, 44, 63, 65, 69). The review on weight reduction showed that weight loss was achieved at modest costs in both intervention groups (doctor-dietician and doctor-led), compared with usual care but based on only one study (63). Two reviews found large variations in the interventions, their intensity, incremental costs and cost effectiveness (44, 65). The professions delivering the interventions varied (44), one review (65) covered lay workers and peers. All reviews were based on small numbers of studies or reported several limitations (40, 44, 63, 65, 69), which is in line with previous research in primary care, for instance for nurses substituting for physicians (70) and various new professional roles (84).
Several of the included reviews covered skill-mix changes taking place in people’s homes, communities or other settings (e.g., schools), suggesting that the primary care settings are diversifying. Skill-mix changes have been identified as one of the levers for re-orienting primary care services from curative care to integrated services (5). Implementation requires changes to the skills and roles of the professions involved, team and organizational changes, as well as changes to policy and financing (85). Education and training has been identified as critical (86, 87). A systematic review found that professional training may lead to a small but significant change in health professionals’ skills and behaviour for up to 12 months, which may subsequently change patients’ health behaviour (88). More research is needed on training contents, uptake in clinical practice and other interventions to achieve long-term effects among individuals and population groups.
Limitations
This overview of reviews faces several limitations. First, we did not search for individual primary studies, nor did we examine overlap across the included systematic reviews. Moreover, the number of included reviews and their quality was highly variable. Second, whereas several reviews covered nurses, followed by pharmacists and CHWs, few covered other professions or multiprofessional teams. Many reviews covered multiple professions, which limit the results to roles or functions, but not by profession. Third, the exact roles and tasks performed were not always sufficiently reported. Moreover, while we used a skill-mix typology according to pre-defined criteria, it was not always possible to delineate between role expansion and task-shifting, which may have led to an overreporting of the category on “other”. Fourth, there were few reviews on costs. Future research should analyse at more detailed levels which professions with which education, skills and roles are most effective and cost-effective for specific prevention roles.
Conclusion
Several promising skill-mix innovations were identified. They include expanded roles on lifestyle change, outreach roles and task-shifting. Yet, the quality of the evidence varied. There was inconclusive evidence on costs. More research is required on the educational requirements for new skill-sets by professions and upatek in practice to enhance links between primary care and population health.
Author Contributions
CM was responsible for the overall design and conduct of the overview of reviews and wrote the first draft manuscript and subsequent versions. CM, JW, and GW conducted the extraction, analysis and interpretation of the data. GW and JW contributed to methodology, revised and reviewed the manuscript. LP was involved in data collection, quality appraisals and reviewed the paper. All authors read, commented upon, and approved the final manuscript.
Funding
This research was financially supported by the UK Health Foundation. The funder had no role in the study design, analysis or write-up of the results. Open Access funding was enabled and organized by the European Observatory on Health Systems and Policies.
Conflict of Interest
The authors declare that they do not have any conflicts of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/ijph.2023.1605448/full#supplementary-material
References
1.GBD 2017 DALYsHALE Collaborators. Global, Regional, and National Disability-Adjusted Life-Years (DALYs) for 359 Diseases and Injuries and Healthy Life Expectancy (HALE) for 195 Countries and Territories, 1990-2017: a Systematic Analysis for the Global Burden of Disease Study 2017. Lancet (2018) 392(10159):1859–922. doi:10.1016/S0140-6736(18)32335-3
2.GBD 2017 SDG Collaborators. Measuring Progress from 1990 to 2017 and Projecting Attainment to 2030 of the Health-Related Sustainable Development Goals for 195 Countries and Territories: a Systematic Analysis for the Global Burden of Disease Study 2017. Lancet (2018) 392(10159):2091–138. doi:10.1016/S0140-6736(18)32281-5
3. Candari, CJ, Cylus, J, and Nolte, E. Assessing the Economic Costs of Unhealthy Diets and Low Physical Activity: An Evidence Review and Proposed Framework. Copenhagen (Denmark): European Observatory on Health Systems and Policies (2017).
4.World Health Organization. Promoting Health: Guide to National Implementation of the Shanghai Declaration. Geneva: World Health Organization (2018).
6. Rechel, B, Jakubowski, E, McKee, M, and Nolte, E. Organization and Financing of Public Health Services in Europe. Copenhagen (Denmark): European Observatory on Health Systems and Policies (2018). World Health Organization 2018 (acting as the host organization for, and secretariat of, the European Observatory on Health Systems and Policies).
7. Rechel, B, Maresso, A, Sagan, A, Hernández-Quevedo, C, Richardson, E, Jakubowski, E, et al. The Role of Public Health Organizations in Addressing Public Health Problems in Europe. The Case of Obesity, Alcohol and Antimicrobial Resistance. Copenhagen (Denmark): European Observatory on Health Systems and Policies (2018). World Health Organization 2018 (acting as the host organization for, and secretariat of, the European Observatory on Health Systems and Policies).
8. Kringos, DS, Boerma, WGW, Hutchinson, A, and Saltman, RB. Building Primary Care in a Changing Europe. Copenhagen (Denmark): European Observatory on Health Systems and Policies (2015). World Health Organization 2015 (acting as the host organization for, and secretariat of, the European Observatory on Health Systems and Policies).
9. Frenk, J, Chen, L, Bhutta, ZA, Cohen, J, Crisp, N, Evans, T, et al. Health Professionals for a new century: Transforming Education to Strengthen Health Systems in an Interdependent World. Lancet (2010) 376(9756):1923–58. doi:10.1016/S0140-6736(10)61854-5
10. Sibbald, B, Shen, J, and McBride, A. Changing the Skill-Mix of the Health Care Workforce. J Health Serv Res Pol (2004) 9:28–38. doi:10.1258/135581904322724112
11. Dubois, C-A, and Singh, D. From Staff-Mix to Skill-Mix and beyond: towards a Systemic Approach to Health Workforce Management. Hum Resour Health (2009) 7:87. doi:10.1186/1478-4491-7-87
12. Bhopal, A, Baker, PA, Meldrum, JL, Chan, JK, and Gopfert, AP. Embed a Public Health Ethos in the Medical Workforce. Lancet (2015) 385(9971):853–4. doi:10.1016/S0140-6736(15)60479-2
13. de Bont, A, van Exel, J, Coretti, S, Okem, ZG, Janssen, M, Hope, KL, et al. Reconfiguring Health Workforce: a Case-Based Comparative Study Explaining the Increasingly Diverse Professional Roles in Europe. BMC Health Serv Res (2016) 16(1):637. doi:10.1186/s12913-016-1898-0
14. Ladden, MD, Bodenheimer, T, Fishman, NW, Flinter, M, Hsu, C, Parchman, M, et al. The Emerging Primary Care Workforce: Preliminary Observations from the Primary Care Team: Learning from Effective Ambulatory Practices Project. Acad Med (2013) 88(12):1830–4. doi:10.1097/ACM.0000000000000027
15. Maier, CB, Aiken, LH, and Busse, R. Nurses in Advanced Roles in Primary Care: Policy Levers for Implementation. Paris: OECD (2017).
16. Agomo, CO. The Role of Community Pharmacists in Public Health: a Scoping Review of the Literature. J Pharm Health Serv Res (2011) 3(1):25–33. doi:10.1111/j.1759-8893.2011.00074.x
17. Merks, P, Jakubowska, M, Drelich, E, Świeczkowski, D, Bogusz, J, Bilmin, K, et al. The Legal Extension of the Role of Pharmacists in Light of the COVID-19 Global Pandemic. Res Soc Administrative Pharm (2021) 17(1):1807–12. doi:10.1016/j.sapharm.2020.05.033
18. van Erp, RMA, van Doorn, AL, van den Brink, GT, Peters, JWB, Laurant, MGH, and van Vught, AJ. Physician Assistants and Nurse Practitioners in Primary Care Plus: A Systematic Review. Int J integrated Care (2021) 21(1):6. doi:10.5334/ijic.5485
19. Hooker, RS, Cawley, JF, and Asprey, DP. Physician Assistants: Policy and Practice. 4th ed. Philadelphia: F.A. Davies Company (2017).
20. Brocklehurst, P, and Macey, R. Skill-mix in Preventive Dental Practice-Wwill it Help Address Need in the Future? BMC oral health. 2015;15:S10, doi:10.1186/1472-6831-15-S1-S10
21. Hartzler, AL, Tuzzio, L, Hsu, C, and Wagner, EH. Roles and Functions of Community Health Workers in Primary Care. Ann Fam Med (2018) 16(3):240–5. doi:10.1370/afm.2208
22. Lewin, S, Munabi-Babigumira, S, Glenton, C, Daniels, K, Bosch-Capblanch, X, van Wyk, BE, et al. Lay Health Workers in Primary and Community Health Care for Maternal and Child Health and the Management of Infectious Diseases. Cochrane Database Syst Rev (2010) 2010(3):Cd004015. doi:10.1002/14651858.CD004015.pub3
23.California Health Workforce Alliance. Taking Innovation to Scale: Community Health Workers, Promotores, and the Triple Aim. A Statewide Assessment of the Roles and Contributions of California’s Community Health Workers. Final Report. December 2013; 2013.
24. Maier, CB, Kroezen, M, Busse, R, and Wismar, M. In: CB Maier, M Kroezen, R Busse, and M Wismar, editors. Skill-mix Innovation, Effectiveness and Implementation. Improving Primary and Chronic Care. Cambridge University Press (2022).
25. van den Broucke, S, Czabanowska, K, Budde, H, Pfirter, L, and Maier, CB. Keeping People Healthy: Skill-Mix Innovations for Improved Disease Prevention and Health Promotion. In: CB Maier, M Kroezen, M Wismar, and R Busse, editors. Skill-mix Innovation, Effectiveness and Implementation: Improving Primary and Chronic Care. European Observatory on Health Systems and Policies. Cambridge: Cambridge University Press (2022). p. 83–116.
26. Higgins, JPT, and Green, SE. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration (2011). updated March 2011.
27. Misfeldt, R, Linder, J, Lait, J, Hepp, S, Armitage, G, Jackson, K, et al. Incentives for Improving Human Resource Outcomes in Health Care: Overview of Reviews. J Health Serv Res Pol (2014) 19(1):52–61. doi:10.1177/1355819613505746
28. Maier, CB, Kroezen, M, Hartl, K, Budde, H, Winkelmann, J, Wismar, M, et al. Overview of Systematic Reviews: Outcomes of Health Workforce Skill-Mix Changes in Primary and Ambulatory Care. PROSPERO (2018) CRD42018090272.
29. Laurant, M, Reeves, D, Hermens, R, Braspenning, J, Grol, R, and Sibbald, B. Substitution of Doctors by Nurses in Primary Care. Cochrane Database Syst Rev (2005) 2:CD001271. doi:10.1002/14651858.CD001271.pub2
31. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The PRISMA 2020 Statement: an Updated Guideline for Reporting Systematic Reviews. Bmj (2021) 372:790–9. doi:10.1016/j.rec.2021.07.010
32. Ouzzani, M, Hammady, H, Fedorowicz, Z, and Elmagarmid, A. Rayyan — a Web and mobile App for Systematic Reviews. Syst Rev (2016) 5:210. doi:10.1186/s13643-016-0384-4
33. Viera, AJ, and Garrett, JM. Understanding Interobserver Agreement: the Kappa Statistic. Fam Med (2005) 37(5):360–3.
34. Banerjee, M, Capozzoli, M, McSweeney, L, and Sinha, D. Beyond Kappa: A Review of Interrater Agreement Measures. Can J Stat (1999) 27(1):3–23. doi:10.2307/3315487
35. Thomson, D, Russell, K, Becker, L, Klassen, T, and Hartling, L. The Evolution of a New Publication Type: Steps and Challenges of Producing Overviews of Reviews. Res Synth Methods (2010) 1(3-4):198–211. doi:10.1002/jrsm.30
36.WHO Regional Office for the Eastern Mediterranean. Health Promotion and Disease Prevention through Population-Based Interventions, Including Action to Address Social Determinants and Health Inequity. WHO (2020). Available from: http://www.emro.who.int/about-who/public-health-functions/health-promotion-disease-prevention.html (Accessed September 29, 2022).
37. Budde, H, Williams, GA, Winkelmann, J, Pfirter, L, and Maier, CB. The Role of Patient Navigators in Ambulatory Care: Overview of Systematic Reviews. BMC Health Serv Res (2021) 21(1):1166. doi:10.1186/s12913-021-07140-6
38. Gates, M, Gates, A, Pieper, D, Fernandes, RM, Tricco, AC, Moher, D, et al. Reporting Guideline for Overviews of Reviews of Healthcare Interventions: Development of the PRIOR Statement. Bmj (2022) 378:e070849. doi:10.1136/bmj-2022-070849
39. Shea, BJ, Reeves, BC, Wells, G, Thuku, M, Hamel, C, Moran, J, et al. AMSTAR 2: a Critical Appraisal Tool for Systematic Reviews that Include Randomised or Non-randomised Studies of Healthcare Interventions, or Both. BMJ (2017) 358:j4008. doi:10.1136/bmj.j4008
40. Khan-Neelofur, D, Gülmezoglu, M, and Villar, J. Who Should Provide Routine Antenatal Care for Low-Risk Women, and How Often? A Systematic Review of Randomised Controlled Trials. WHO Antenatal Care Trial Research Group. Paediatric perinatal Epidemiol (1998) 12:7–26. doi:10.1046/j.1365-3016.12.s2.6.x
41. Farris, KB, Ashwood, D, McIntosh, J, DiPietro, NA, Maderas Nm, L, Landau, SC, et al. Preventing Unintended Pregnancy: Pharmacists’ Roles in Practice and Policy via Partnerships. J Am Pharm Assoc (2010) 50(5):604–12. doi:10.1331/JAPhA.2010.09195
42. Issel, LM, Forrestal, SG, Slaughter, J, Wiencrot, A, and Handler, A. A Review of Prenatal home-visiting Effectiveness for Improving Birth Outcomes. J Obstet Gynecol Neonatal Nurs (2011) 40(2):157–65. doi:10.1111/j.1552-6909.2011.01219.x
43. Abbott, LS, and Elliott, LT. Eliminating Health Disparities through Action on the Social Determinants of Health: A Systematic Review of Home Visiting in the United States, 2005-2015. Public Health Nurs (2017) 34(1):2–30. doi:10.1111/phn.12268
44. Dalziel, K, and Segal, L. Home Visiting Programmes for the Prevention of Child Maltreatment: Cost-Effectiveness of 33 Programmes. Arch Dis Child (2012) 97(9):787–98. doi:10.1136/archdischild-2011-300795
45. Kroll-Desrosiers, AR, Crawford, SL, Moore Simas, TA, Rosen, AK, and Mattocks, KM. Improving Pregnancy Outcomes through Maternity Care Coordination: A Systematic Review. Women’s Health Issues (2016) 26(1):87–99. doi:10.1016/j.whi.2015.10.003
46. Joseph, J, Vaughan, R, and S, H. Effectiveness of Nurse-Performed Endoscopy in Colorectal Cancer Screening: a Systematic Review. GASTROINTEST NURS (2015) 13(4):26–33. doi:10.12968/gasn.2015.13.4.26
47. Loescher, LJ, Harris, JM, and Curiel-Lewrowski, C. A Systematic Review of Advanced Practice Nurses’ Skin Cancer Assessment Barriers, Skin Lesion Recognition Skills, and Skin Cancer Training Activities. J Am Acad Nurse Pract (2011) 23(12):667–73. doi:10.1111/j.1745-7599.2011.00659.x
48. Wells, KJ, Luque, JS, Miladinovic, B, Vargas, N, Asvat, Y, Roetzheim, RG, et al. Do community Health Worker Interventions Improve Rates of Screening Mammography in the United States? A Systematic Review. Cancer Epidemiol Biomarkers Prev (2011) 20(8):1580–98. doi:10.1158/1055-9965.EPI-11-0276
49. Kim, K, Choi, JS, Choi, E, Nieman, CL, Joo, JH, Lin, FR, et al. Effects of Community-Based Health Worker Interventions to Improve Chronic Disease Management and Care Among Vulnerable Populations: A Systematic Review. Am J Public Health (2016) 106(4):e3–e28. doi:10.2105/AJPH.2015.302987
50. Heuvelings, CC, Greve, PF, De Vries, SG, Visser, BJ, Bélard, S, Janssen, S, et al. Effectiveness of Service Models and Organisational Structures Supporting Tuberculosis Identification and Management in Hard-To-Reach Populations in Countries of Low and Medium Tuberculosis Incidence: A Systematic Review. BMJ open (2018) 8(9):e019642. doi:10.1136/bmjopen-2017-019642
51. Spinks, J, Bettington, E, Downes, M, Nissen, L, and Wheeler, A. Does Policy Change to Allow Pharmacist Provision of Influenza Vaccination Increase Population Uptake? A Systematic Review. Aust Health Rev : a Publ Aust Hosp Assoc (2020) 44(4):582–9. doi:10.1071/AH19196
52. Saba, M, Diep, J, Saini, B, and Dhippayom, T. Meta-analysis of the Effectiveness of Smoking Cessation Interventions in Community Pharmacy. J Clin Pharm Ther (2014) 39(3):240–7. doi:10.1111/jcpt.12131
53. Mitchell, LJ, Ball, LE, Ross, LJ, Barnes, KA, and Williams, LT. Effectiveness of Dietetic Consultations in Primary Health Care: A Systematic Review of Randomized Controlled Trials. J Acad Nutr Diet (2017) 117(12):1941–62. doi:10.1016/j.jand.2017.06.364
54. Bhattarai, N, Prevost, AT, Wright, AJ, Charlton, J, Rudisill, C, and Gulliford, MC. Effectiveness of Interventions to Promote Healthy Diet in Primary Care: Systematic Review and Meta-Analysis of Randomised Controlled Trials. BMC Public Health (2013) 13:1203. doi:10.1186/1471-2458-13-1203
55. Ball, L, Leveritt, M, Cass, S, and Chaboyer, W. Effect of Nutrition Care provided by Primary Health Professionals on Adults' Dietary Behaviours: a Systematic Review. Fam Pract (2015) 32(6):605–17. doi:10.1093/fampra/cmv067
56. Thompson, RL, Summerbell, CD, Hooper, L, Higgins, JP, Little, P, Talbot, D, et al. Dietary Advice Given by a Dietitian versus Other Health Professional or Self-Help Resources to Reduce Blood Cholesterol. Cochrane Database Syst Rev (2003) CD001366. doi:10.1002/14651858.CD001366
57. Kunstler, BE, Cook, JL, Freene, N, Finch, CF, Kemp, JL, OʼHalloran, PD, et al. Physiotherapist-Led Physical Activity Interventions Are Efficacious at Increasing Physical Activity Levels: A Systematic Review and Meta-Analysis. Clin J Sport Med : official J Can Acad Sport Med (2018) 28(3):304–15. doi:10.1097/JSM.0000000000000447
58. Orrow, G, Kinmonth, AL, Sanderson, S, and Sutton, S. Effectiveness of Physical Activity Promotion Based in Primary Care: Systematic Review and Meta-Analysis of Randomised Controlled Trials. Bmj (2012) 344:e1389. doi:10.1136/bmj.e1389
59. Schroeder, K, Travers, J, and Smaldone, A. Are School Nurses an Overlooked Resource in Reducing Childhood Obesity? A Systematic Review and Meta-Analysis. J Sch Health (2016) 86(5):309–21. doi:10.1111/josh.12386
60. Sargent, GM, Forrest, LE, and Parker, RM. Nurse Delivered Lifestyle Interventions in Primary Health Care to Treat Chronic Disease Risk Factors Associated with Obesity: a Systematic Review. Obes Rev : Off J Int Assoc Study Obes (2012) 13(12):1148–71. doi:10.1111/j.1467-789X.2012.01029.x
61. Petit Francis, L, Spaulding, E, Turkson-Ocran, RA, and Allen, J. Randomized Trials of Nurse-Delivered Interventions in Weight Management Research: A Systematic Review. West J Nurs Res (2017) 39(8):1120–50. doi:10.1177/0193945916686962
62. van Dillen, SM, and Hiddink, GJ. To what Extent Do Primary Care Practice Nurses Act as Case Managers Lifestyle Counselling Regarding Weight Management? A Systematic Review. BMC Fam Pract (2014) 15:197. doi:10.1186/s12875-014-0197-2
63. Flodgren, G, Gonçalves-Bradley Daniela, C, and Summerbell Carolyn, D. Interventions to Change the Behaviour of Health Professionals and the Organisation of Care to Promote Weight Reduction in Children and Adults with Overweight or Obesity. Cochrane Database Syst Rev (2017) 11(11):CD000984. doi:10.1002/14651858.CD000984.pub3
64. Dennis, S, Williams, A, Taggart, J, Newall, A, Denney-Wilson, E, Zwar, N, et al. Which Providers Can Bridge the Health Literacy gap in Lifestyle Risk Factor Modification Education: a Systematic Review and Narrative Synthesis. BMC Fam(2012) 13:44. doi:10.1186/1471-2296-13-44
65. Pennington, M, Visram, S, Donaldson, C, White, M, Lhussier, M, Deane, K, et al. Cost-effectiveness of Health-Related Lifestyle Advice Delivered by Peer or Lay Advisors: Synthesis of Evidence from a Systematic Review. Cost Eff Resour Alloc (2013) 11(1):30. doi:10.1186/1478-7547-11-30
66. Tapsell, LC, and Neale, EP. The Effect of Interdisciplinary Interventions on Risk Factors for Lifestyle Disease: A Literature Review. Health Educ Behav (2016) 43(3):271–85. doi:10.1177/1090198115601092
67. Frerichs, W, Kaltenbacher, E, van de Leur, JP, and Dean, E. Can Physical Therapists Counsel Patients with Lifestyle-Related Health Conditions Effectively? A Systematic Review and Implications Review. Physiother Theor Pract (2012) 28(8):571–87. doi:10.3109/09593985.2011.654179
68. Martinez-Gonzalez, NA, Tandjung, R, Djalali, S, and Rosemann, T. The Impact of Physician-Nurse Task Shifting in Primary Care on the Course of Disease: a Systematic Review. Hum Resour Health (2015) 13:55. doi:10.1186/s12960-015-0049-8
69. Brown, TJ, Todd, A, O'Malley, C, Moore, HJ, Husband, AK, Bambra, C, et al. Community Pharmacy-Delivered Interventions for Public Health Priorities: a Systematic Review of Interventions for Alcohol Reduction, Smoking Cessation and Weight Management, Including Meta-Analysis for Smoking Cessation. BMJ open (2016) 6(2):e009828. doi:10.1136/bmjopen-2015-009828
70. Laurant, M, van der Biezen, M, Wijers, N, Watananirun, K, Kontopantelis, E, and van Vught, A. Nurses as Substitutes for Doctors in Primary Care. Cochrane Database Syst Rev (2018)(7) CD001271. doi:10.1002/14651858.CD001271.pub3
71. Osborn, R, Moulds, D, Squires, D, Doty, MM, and Anderson, C. International Survey of Older Adults Finds Shortcomings in Access, Coordination, and Patient-Centered Care. Health Aff (Millwood) (2014) 33(12):2247–55. doi:10.1377/hlthaff.2014.0947
72. Kringos, DS, Boerma, WGW, Hutchinson, A, and Saltman, RB. Building Primary Care in a Changing Europe. Case Studies. Copenhagen (Denmark): European Observatory on Health Systems and Policies (2015). World Health Organization 2015 (acting as the host organization for, and secretariat of, the European Observatory on Health Systems and Policies).
73. Delamaire, M-L, and Lafortune, G. Nurses in Advanced Roles: A Description and Evaluation of Experiences in 12 Developed Countries. 54 DELSA/HEA/WD/HWP. In: OECD Health Working Paper, 5 (2010).
74. Winkelmann, J, Williams, GA, Rijken, M, Polin, K, and Maier, CB. Chronic Conditions and Multimorbidity: Skill-Mix Innovations for Enhanced Quality and Coordination of Care. In: CB Maier, M Kroezen, M Wismar, and R Busse, editors. Skill-mix Innovation, Effectiveness and Implementation: Improving Primary and Chronic Care. European Observatory on Health Systems and Policies. Cambridge: Cambridge University Press (2022). p. 152–220.
75. Martínez-González, NA, Rosemann, T, Tandjung, R, and Djalali, S. The Effect of Physician-Nurse Substitution in Primary Care in Chronic Diseases: A Systematic Review. Swiss Med Wkly (2015) 145:w14031. doi:10.4414/smw.2015.14031
76. Kroezen, M, de Veer, A, Francke, A, Groenewegen, P, and van Dijk, L. Changes in Nurses' Views and Practices Concerning Nurse Prescribing between 2006 and 2012: Results from Two National Surveys. J Adv Nurs (2014) 70(11):2550–61. doi:10.1111/jan.12404
77. Kroezen, M, Francke, AL, Groenewegen, PP, and van Dijk, L. Nurse Prescribing of Medicines in Western European and Anglo-Saxon Countries: a Survey on Forces, Conditions and Jurisdictional Control. Int J Nurs Stud (2012) 49(8):1002–12. doi:10.1016/j.ijnurstu.2012.02.002
78. van Ruth, LM, Mistiaen, P, and Francke, AL. Effects of Nurse Prescribing of Medication: a Systematic Review. INTERNET J HEALTHC ADM (2008) 5(2):1–31.
79. Weeks, G, George, J, Maclure, K, and Stewart, D. Non-medical Prescribing versus Medical Prescribing for Acute and Chronic Disease Management in Primary and Secondary Care. Cochrane Database Syst Rev (2016) 11:Cd011227. doi:10.1002/14651858.CD011227.pub2
80. Maier, CB, Barnes, H, Aiken, LH, and Busse, R. Descriptive, Cross-Country Analysis of the Nurse Practitioner Workforce in Six Countries: Size, Growth, Physician Substitution Potential. BMJ open (2016) 6(9):e011901. doi:10.1136/bmjopen-2016-011901
81. Maier, CB, and Aiken, LH. Task Shifting from Physicians to Nurses in Primary Care in 39 Countries: a Cross-Country Comparative Study. Eur J Public Health (2016) 26(6):927–34. doi:10.1093/eurpub/ckw098
82. Maier, CB. Nurse Prescribing of Medicines in 13 European Countries. Hum Resour Health (2019) 17(1):95. doi:10.1186/s12960-019-0429-6
83. O'Reilly-Jacob, M, Perloff, J, Sherafat-Kazemzadeh, R, and Flanagan, J. Nurse Practitioners' Perception of Temporary Full Practice Authority during a COVID-19 Surge: A Qualitative Study. Int J Nurs Stud (2022) 126:104141. doi:10.1016/j.ijnurstu.2021.104141
84. Tsiachristas, A, Wallenburg, I, Bond, CM, Elliot, RF, Busse, R, van Exel, J, et al. Costs and Effects of New Professional Roles: Evidence from a Literature Review. Health Policy (2015) 119(9):1176–87. doi:10.1016/j.healthpol.2015.04.001
85. Maier, CB, Scarpetti, G, Kroezen, M, Akeroyd, MS, Budde, H, Pfirter, L, et al. Implementing Skill-Mix Changes: Lessons for Policy and Practice. In: CB Maier, M Kroezen, M Wismar, and R Busse, editors. Skill-mix Innovation, Effectiveness and Implementation: Improving Primary and Chronic Care. European Observatory on Health Systems and Policies. Cambridge: Cambridge University Press (2022). p. 70–82.
86. Batenburg, R, and Kroezen, M. Education and Planning: Anticipating and Responding to Skill Gaps, Changing Skill Needs and Competencies. In: CB Maier, M Kroezen, M Wismar, and R Busse, editors. Skill-mix Innovation, Effectiveness and Implementation: Improving Primary and Chronic Care. European Observatory on Health Systems and Policies. Cambridge: Cambridge University Press (2022). p. 294–320.
87. Maier, CB, Batenburg, R, Birch, S, Zander, B, Elliott, R, and Busse, R. Health Workforce Planning: Which Countries Include Nurse Practitioners and Physician Assistants and to what Effect? Health Policy (2018) 122(10):1085–92. doi:10.1016/j.healthpol.2018.07.016
88. Hatfield, TG, Withers, TM, and Greaves, CJ. Systematic Review of the Effect of Training Interventions on the Skills of Health Professionals in Promoting Health Behaviour, with Meta-Analysis of Subsequent Effects on Patient Health Behaviours. BMC Health Serv Res (2020) 20(1):593. doi:10.1186/s12913-020-05420-1
Keywords: health promotion, prevention, outcomes, skill-mix, task-shifting, outreach, role expansion
Citation: Maier CB, Winkelmann J, Pfirter L and Williams GA (2023) Skill-Mix Changes Targeting Health Promotion and Prevention Interventions and Effects on Outcomes in all Settings (Except Hospitals): Overview of Reviews. Int J Public Health 68:1605448. doi: 10.3389/ijph.2023.1605448
Received: 01 October 2022; Accepted: 14 April 2023;
Published: 09 May 2023.
Edited by:
Gabriel Gulis, University of Southern Denmark, DenmarkReviewed by:
Bosiljka Djikanovic, University of Belgrade, SerbiaCopyright © 2023 Maier, Winkelmann, Pfirter and Williams. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Claudia Bettina Maier, Yy5tYWllckB0dS1iZXJsaW4uZGU=
This Review is part of the IJPH Special Issue Public Health and Primary Care, is 1 + 1 = 1?
 Claudia Bettina Maier
Claudia Bettina Maier Juliane Winkelmann2
Juliane Winkelmann2