Abstract
Objectives: To study the epidemiological characteristics and influencing factors of myopia to provide a scientific basis for the prevention and control of myopia.
Methods: 7,597 students studying in grades 1–3 were followed up. Eye examinations and questionnaire surveys were conducted annually from 2019 to 2021. The influencing factors of myopia were analyzed by logistic regression model.
Results: The prevalence of myopia among students in grades 1–3 in 2019 was 23.4%, which increased to 41.9% and 51.9% after the 1-and 2-year follow-up, respectively. The incidence of myopia and change in the spherical equivalent refraction (SER) were higher in 2020 than in 2021. The 2-year cumulative incidences of myopia were 2.5%, 10.1%, 15.5%, 36.3%, and 54.1% in students with a baseline SER >+1.50D, +1.00D to +1.50D, +0.50D to +1.00D, 0.00D to +0.50D, and -0.50D to 0.00D, respectively. Outdoor activities, sex, age, baseline SER, parental myopia, sleep time, and digital device exposure were associated with myopia.
Conclusion: The prevalence of myopia demonstrated a rapid increase; thus, healthy habits and outdoor activities should be promoted for the prevention and control of myopia.
Introduction
Myopia is a global public health problem (1). The prevalence of myopia among school-age children is increasing, especially in East and Southeast Asia (2). Holden (3) predicted 4.758 billion individuals to have myopia in the world by 2050, accounting for approximately 49.8% of the total population. Studies reported the prevalence of myopia among students in grade 1 in primary and junior middle schools in China to be 3.9% and 67.3%, respectively (4). With the increasing prevalence of myopia, uncorrected refractive error has become an important cause of visual impairment (5). By 2050, approximately 100 million Chinese people may suffer irreversible vision loss and become blind owing to the high prevalence of myopia in China (2). Myopia, especially high myopia, can cause many complications that harm visual health and even result in blindness (6). High myopia-related retinopathy is the leading cause of irreversible blindness in adults in some areas of China (7). Moreover, vision loss is a huge economic burden for individuals worldwide (8), and the global economic cost of visual impairment attributed to uncorrected myopia is $244 billion annually (9).
The causes of myopia are complex. A twin study demonstrated myopia to be highly heritable, thereby suggesting a genetic predisposition (10). Compared to children whose parents have normal vision, children whose parents are myopic possess a significantly increased risk of myopia (11). A major change has not been observed in Genetics and patterns of inheritance in recent years. However, the prevalence of myopia worldwide is still increasing significantly, indicating the role of environmental factors in the development of myopia (12). Environmental factors such as outdoor activities (13), educational level (14), electronic devices (15), sleep time (16), and reading and writing posture (17) are associated with myopia.
Myopia, which is the most common visual impairment among children and adolescents (18), bears serious health risks and financial burden. Owing to the lack of effective treatment methods, understanding the epidemic characteristics, occurrence, development, and influencing factors of myopia is critical to explore and implement effective preventive and control measures. Currently, many cross-sectional studies exist on the prevalence of myopia among school students (19–21), however, few longitudinal studies have examined myopia progression among school students in China. Longitudinal studies on the progression of myopia were carried out in Chongqing, Southwest China, in 2006 (22); Guangzhou, Southern China, in 2010 (23); and Anyang, Central China in 2012 (24). These studies explored the principle of changes in the students’ refraction status but did not investigate and analyze the influencing factors. In addition, these studies were conducted 10 years ago; hence, and it is possible that the principles of myopia progression in the students may have changed. Cohort studies on the progression of myopia have also been conducted in other countries, such as Australia (25) and Northern Ireland (26). However, these studies lacked annual follow-up monitoring data, and the follow-up samples were small.
Currently, there is a lack of recent large-scale longitudinal studies among school students in South China. A longitudinal study can reveal the principles of disease occurrence and development and explore the cause of the disease. In 2019, we conducted the Shenzhen Child and Adolescent Eye Study (21). Based on that study, we conducted a longitudinal study to explore the epidemiological characteristics of myopia among school-aged children and explore the factors influencing myopia. We aimed to provide a theoretical basis for the prevention and control of myopia in this study.
Methods
Ethics Statements
This study was approved by the Ethics Committee of Shenzhen Eye Hospital. The students and their parents or guardians were informed of the objectives and examination procedures of this study, and written informed consent was obtained from the parents or guardians.
Study Design and Population
Shenzhen is located in Southern China and consists of 10 administrative districts. This study was conducted using cluster sampling. One primary school was randomly selected from each administrative district in Shenzhen by a random number, and all the students in grades 1–3 of the selected schools participated in this study. The sample size was calculated using the G*Power software (version 3.1.9.7), which can compute effect sizes (27). According to the G*Power software, the sample size of the students should be 7,220. Considering the possibility of loss to follow-up in the follow-up study, 9,153 students were included in this study for follow-up.
The inclusion criteria were as follows: 1) Students whose parents or guardians agreed to participate in this study, 2) Students who were in grades 1–3 in 2019, and 3) Students who completed all the items in the three inspections from 2019 to 2021. The exclusion criteria were as follows: 1) Students who were unable to undergo the visual acuity test, refraction test, and questionnaire survey, 2) Students with eye disease, and 3) Students who wore orthokeratology lenses. In total, 9,153 students in Shenzhen were enrolled in the study. 8,241 students completed the 1-year follow-up, and 7,597 students completed the 2-year follow-up. The reasons for loss to follow-up were transfer to another school, requesting leave and opting not to undergo the tests. After the 2-year follow-up, 591, 92, and 873 students in grades 1, 2, and 3 were lost to follow-up, respectively. Further analysis revealed that there was no difference in the sex and baseline spherical equivalent refraction (SER) between the lost to follow-up population and the follow-up population. A total of 2,409 students from grade 1 (1,299 boys and 1,110 girls), 2,713 students from grade 2 (1,464 boys and 1,249 girls), and 2,475 students from grade 3 (1,360 boys and 1,115 girls) were followed up from September 2019 to September 2021. Visual acuity and refraction tests were conducted by trained doctors and nurses in September 2019, September 2020, and September 2021 in this study. The questionnaire survey was conducted by trained doctors in September 2021 in this study.
Visual Acuity Test
The visual acuity test was performed in accordance with the specifications for screening for refractive error among school students (28). Visual acuity tests were performed by optometrists using an electronic visual acuity chart (Eye Vision 1603-01) in a bright classroom. Eye mask plates were used to cover the contralateral eye during the examination, and the right eye was examined first before the left eye. In order to ensure the accuracy of the examination, the students were required to sit in their seats and look straight ahead to correct their behavior of leaning forward and squinting at any time. Visual acuity lower than 5.0 in either eye was considered abnormal visual acuity, and visual acuity ≥5.0 in both eyes was considered normal visual acuity.
Refraction Test
The refraction test was conducted in accordance with the specifications for the screening for refractive error among school students (28). Non-cycloplegic refraction tests were performed by optometrists using an autorefractor (NIDEK AR-1). The refractive test was automatically repeated three times for every student, and the average values of SER of the participants were obtained.
Questionnaire Survey
The questionnaire was compiled by numerous experts according to domestic and foreign questionnaires concerning myopia. The questionnaire was completed by the students’ parents or guardians. The questionnaire collected the students’ general information and habits associated with eye health, including but not limited to age, sex, time of birth, parental myopia, education, time spent performing outdoor activities, digital device exposure, sleep time, family average monthly income, and living space.
Definition of Myopia
Myopia was defined as SER <−0.50 diopter (D) tested by non-cycloplegic refraction and uncorrected visual acuity <5.0 (28). According to SER, subjects with myopia were divided into three groups in this study: mild myopia (−0.50 D ∼ −3.00 D), moderate myopia (−3.00 D ∼ −6.00D) and high myopia (≤−6.00D).
Statistical Analyses
SER follows a normal distribution according to the Kolmogorov–Smirnov test; SER is expressed as the mean and standard deviation. Independent samples t-tests were performed to compare the means between groups, and repeated measures analysis of variance was used to estimate the effect size. Qualitative data are presented as frequency and percentage, and Chi-square tests were performed to compare the percentages between the groups. Pearson’s correlation analysis revealed that the SERs of the left and right eyes were correlated (r = 0.80, p < 0.001), and the SERs of the right eyes were used to evaluate the epidemiological characteristics of myopia in this study. The incidence of myopia in this study was calculated as the number of new myopia cases during the follow-up period divided by the number of students who were not myopic at the beginning of the follow-up, and the prevalence of myopia was defined as the number of students with myopia divided by the number of students during the observation period. Logistic regression was conducted to analyze the factors of the incidence of myopia, and odds ratios (ORs) and 95% confidence intervals (95% CIs) were provided. Logistic regression models were used to analyze the influencing factors of myopia. We first conducted a simple model analysis, and subsequently conducted multiple model analyses with statistically significant variables. Collinearity analysis was performed on all the independent variables before the multiple logistic regression analysis, and independent variables with a variance inflation factor less than 10 were included in the model. We controlled for the effect of other confounders to assess the effect of one factor on the prevalence of myopia. Statistical analyses and data visualization were performed by R software (version 4.1.0), and statistical significance was set at p < 0.05.
Results
The prevalence of myopia in 2019, 2020, and 2021 was 23.4%, 41.9%, and 51.9%, respectively (χ2= 1257.34, p < 0.001). The baseline prevalence of myopia among students in grades 1, 2, and 3 was 13.7%, 21.9%, and 34.5%, respectively, in 2019% and 38.2%, 51.9%, and 62.2%, respectively, after the 2-year follow-up. The baseline prevalence of myopia among boys in grades 1, 2, and 3 was 13.7%, 20.7%, and 33.7% in 2019, respectively, and 35.0%, 47.3%, and 57.9%, respectively, after the 2-year follow-up. The baseline prevalence of myopia among girls in grades 1, 2, and 3 was 13.7%, 23.4%, and 35.5%, respectively, in 2019% and 42.1%, 57.1%, and 67.5%, respectively, after the 2-year follow-up (Table 1; Figure 1). The prevalence of myopia among boys and girls increased gradually over time (p < 0.001).
TABLE 1
| Incidence (%) | χ 2 | P | Prevalence (%) | χ 2 | P | ||||
|---|---|---|---|---|---|---|---|---|---|
| 1-year follow-up (2020) | 2-year follow-up (2021) | Baseline (2019) | 1-year follow-up (2020) | 2-year follow-up (2021) | |||||
| Grade 1 | |||||||||
| All (n = 2,409) | 22.5 | 20.6 | 1.87 | 0.17 | 13.7 | 28.1 | 38.2 | 373.30 | <0.001 |
| Boys (n = 1,299) | 20.7 | 16.2 | 6.60 | 0.01 | 13.7 | 26.8 | 35.0 | 52.67 | <0.001 |
| Girls (n = 1,110) | 24.5 | 26.0 | 0.47 | 0.49 | 13.7 | 29.7 | 42.1 | 231.67 | <0.001 |
| Grade 2 | |||||||||
| All (n = 2,713) | 31.5 | 23.8 | 25.40 | <0.001 | 21.9 | 42.7 | 51.9 | 539.60 | <0.001 |
| Boys (n = 1,464) | 28.8 | 19.7 | 21.14 | <0.001 | 20.7 | 40.2 | 47.3 | 251.45 | <0.001 |
| Girls (n = 1,249) | 34.9 | 29.2 | 5.55 | 0.02 | 23.4 | 45.6 | 57.1 | 301.20 | <0.001 |
| Grade 3 | |||||||||
| All (n = 2,475) | 35.9 | 24.4 | 39.24 | <0.001 | 34.5 | 48.2 | 62.2 | 384.63 | <0.001 |
| Boys (n = 1,360) | 30.8 | 21.0 | 18.16 | <0.001 | 33.7 | 50.6 | 57.9 | 170.42 | <0.001 |
| Girls (n = 1,115) | 42.3 | 29.4 | 18.62 | <0.001 | 35.5 | 58.9 | 67.5 | 249.37 | <0.001 |
| Grades 1–3 | 29.5 | 22.7 | 52.43 | <0.001 | 23.4 | 41.9 | 51.9 | 1257.34 | <0.001 |
| Boys (n = 4,123) | 26.5 | 19.4 | 40.73 | <0.001 | 22.8 | 39.4 | 46.9 | 554.30 | <0.001 |
| Girls (n = 3,474) | 33.1 | 31.5 | 1.37 | 0.24 | 24.2 | 44.8 | 55.6 | 730.75 | <0.001 |
Incidence and prevalence of myopia among students in grades 1–3 (Shenzhen, China. 2019–2021).
FIGURE 1
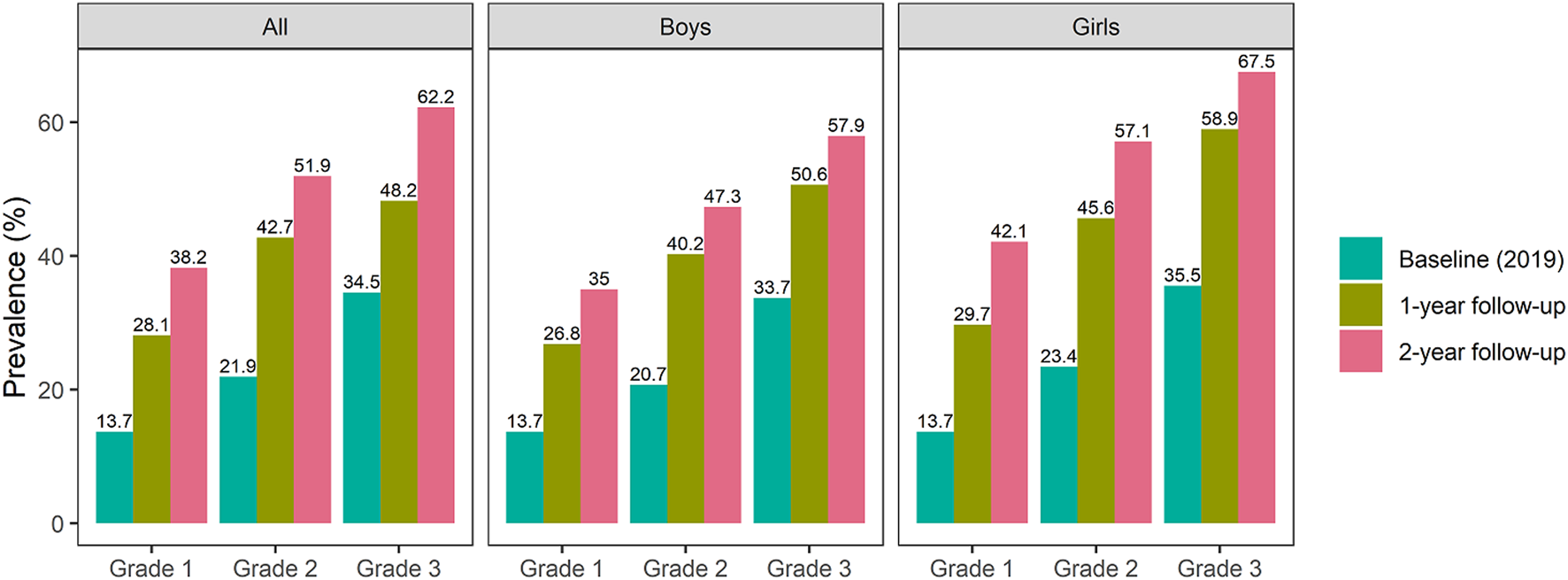
Prevalence of myopia among primary school students in grades 1–3 according to sex (Shenzhen, China. 2019–2021).
For grade 1 students, the prevalence of mild, moderate, and high myopia was 13.0%, 0.6%, and 0.2% at baseline, respectively, and it increased to 33.4%, 4.6%, and 0.2% after the 2-year follow-up, respectively. For grade 2 students, the prevalence of mild, moderate, and high myopia was 20.1%, 1.8%, and 0.1% at baseline, and it increased to 41.6%, 9.5%, and 0.8% after the 2-year follow-up, respectively. For grade 3 students, the prevalence of mild, moderate, and high myopia was 29.8%, 4.4%, and 0.3% at baseline, and increased to 45.7%, 15.3%, and 1.2% after the 2-year follow-up, respectively. The prevalence of mild, moderate and high myopia among students from grades 1–3 increased with the increase in grade (Supplementary Figure S1).
The incidences of myopia among the students in this study were 29.5% and 22.7% during 1- and 2-year follow-up, respectively; the incidence was higher in the former year than in the latter year (χ2= 52.43, p < 0.001). The incidences of myopia were 22.5%, 31.5%, and 35.9% in 2020 for grades 1, 2, and 3 students, respectively, and 20.6%, 23.8%, and 24.4% in 2021, respectively (Table 1). The SERs of the right eye among primary school students in 2019, 2020, and 2021 were −0.40 D, −0.87 D, and −1.12 D, respectively. The SERs of the right eye among grades 1, 2, and 3 were −0.15 D, −0.36 D, and −0.70 D in 2019, respectively, which decreased to −0.76 D, −1.12 D, and −1.49 D, respectively, in 2021. The 2-year progression of the SER was 0.61D, 0.76D, and 0.79D for grade 1, grade 2 and grade 3, respectively. The change in the SER among students in 2020 was significantly higher than that in 2021 (Table 2).
TABLE 2
| SER | F* | P | Change of the SER | t | P | ||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline (2019) | 1-year follow-up (2020) | 2-year follow-up (2021) | 1-year follow-up (2020) | 2-year follow-up (2021) | |||||
| Grade 1 | |||||||||
| All (n = 2,409) | −0.15 (1.02) | −0.51 (1.13) | −0.76 (1.29) | 591.41 | <0.001 | −0.35 (1.07) | −0.25 (0.90) | −3.56 | <0.001 |
| Boys (n = 1,299) | −0.17 (1.11) | −0.46 (1.19) | −0.71 (1.35) | 5.14 | <0.001 | −0.29 (1.09) | −0.25 (0.86) | −0.91 | 0.04 |
| Girls (n = 1,110) | −0.13 (0.90) | −0.56 (1.06) | −0.82 (1.21) | 7.81 | <0.001 | −0.43 (1.04) | −0.25 (0.95) | −4.24 | <0.001 |
| Grade 2 | |||||||||
| All (n = 2,713) | −0.36 (1.05) | −0.88 (1.34) | −1.12 (1.50) | 735.81 | <0.001 | −0.52 (1.03) | −0.24 (0.87) | −10.76 | <0.001 |
| Boys (n = 1,464) | −0.32 (1.05) | −0.83 (1.34) | −1.05 (1.52) | 105.33 | <0.001 | −0.51 (0.96) | −0.22 (0.83) | −8.96 | <0.001 |
| Girls (n = 1,249) | −0.41 (1.05) | −0.93 (1.34) | −1.20 (1.48) | 94.91 | <0.001 | −0.52 (1.10) | −0.26 (0.91) | −6.31 | <0.001 |
| Grade 3 | |||||||||
| All (n = 2,475) | −0.70 (1.31) | −1.20 (1.52) | −1.49 (1.70) | 840.74 | <0.001 | −0.52 (1.02) | −0.27 (0.79) | −9.81 | <0.001 |
| Boys (n = 1,360) | −0.66 (1.33) | −1.15 (1.54) | −1.41 (1.74) | 116.43 | <0.001 | −0.50 (1.03) | −0.25 (0.72) | −7.66 | <0.001 |
| Girls (n = 1,115) | −0.74 (1.28) | −1.27 (1.49) | −1.59 (1.65) | 102.18 | <0.001 | −0.55 (1.08) | −0.30 (0.87) | −6.25 | <0.001 |
| Grades 1–3 | |||||||||
| All (n = 7,597) | −0.40 (1.15) | −0.87 (1.38) | −1.12 (1.54) | 271.93 | <0.001 | −0.47 (1.04) | −0.25 (0.85) | −14.28 | <0.001 |
| Boys (n = 4,123) | −0.38 (1.18) | −0.82 (1.40) | −1.06 (1.57) | 130.37 | <0.001 | −0.44 (1.02) | −0.24 (0.81) | −9.86 | <0.001 |
| Girls (n = 3,474) | −0.43 (1.12) | −0.93 (1.35) | −1.20 (1.49) | 114.80 | <0.001 | −0.50 (1.08) | −0.27 (0.91) | −9.60 | <0.001 |
Change of the SER (D) in students from grades 1–3 (Shenzhen, China. 2019–2021).
Data are presented as mean (standard deviation). SER, spherical equivalent refraction. *, repeated measures analysis of variance.
The 2-year cumulative incidences of myopia among primary school students with a baseline SER of 0.00 D to −0.50 D, +0.50 D to 0.00 D, +1.00 D to +0.50 D, +1.50 D to +1.00 D, and > +1.50 D were 54.1%, 36.3%, 15.5%, 10.1%, and 2.5% after the 2-year follow-up, respectively. The incidence of myopia decreased significantly after the 2-year follow-up with an increase in the baseline SER (χ2= 420.40, p < 0.001) (Table 3).
TABLE 3
| Baseline SER (D) | All | Boys | Girls | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Incidence, % | χ 2 * | P | n | Incidence, % | χ 2 * | P | n | Incidence, % | χ 2 * | P | |
| −0.5 < SER ≤0 | 2,060 | 54.1 | 420.40 | <0.001 | 1,112 | 49.2 | 229.21 | <0.001 | 948 | 59.7 | 190.20 | <0.001 |
| 0 < SER ≤0.5 | 1,949 | 36.3 | 1,102 | 31.6 | 847 | 42.4 | ||||||
| 0.5 < SER ≤1 | 607 | 15.5 | 343 | 11.7 | 264 | 20.5 | ||||||
| 1 < SER ≤1.5 | 109 | 10.1 | 60 | 10.0 | 49 | 10.2 | ||||||
| SER >1.5 | 80 | 2.5 | 49 | 0.0 | 31 | 6.5 | ||||||
2-year cumulative incidence of myopia among primary school students according to the baseline SER (Shenzhen, China. 2019–2021).
SER, spherical equivalent refraction; D, diopters; *, Chi square test for trend.
The demographic characteristics of participants in this study is shown in Table 4. The prevalence of myopia was higher among girls than boys (χ2= 30.56, p < 0.001). The prevalence of myopia among students with myopic parents (χ2= 72.60, p < 0.001), digital device exposure for >1 h per day (χ2= 64.22, p < 0.001), <9 h of sleep per day (χ2= 264.52, p < 0.001), who spent less time performing outdoor activities per day (t = 8.14, p < 0.001), with a lower baseline SER (t = 19.48, p < 0.001), older age (t = −12.10, p < 0.001), and higher parental education (χ2= 4.71, p < 0.001) was higher than that of students without myopic parents, digital device exposure for <1 h per day, >9 h of sleep per day, who spent more time performing outdoor activities per day, had a higher baseline SER, younger age, and lower parental education, respectively.
TABLE 4
| Characteristic | No myopia (n = 3,654) | Myopia (n = 3,943) | Statistical value | P |
|---|---|---|---|---|
| Sex, n (%) | ||||
| Boy | 2,103 (51.0) | 2,020 (49.0) | χ 2 = 30.56 | <0.001 |
| Girl | 1,551 (44.6) | 1,923 (55.4) | ||
| Age, mean (SD), years | 9.21 (2.18) | 11.41 (1.94) | t = −12.10 | <0.001 |
| Parental myopia, n (%) | ||||
| 0 parent | 2,420 (51.4) | 2,288 (48.6) | χ 2 = 72.60 | <0.001 |
| 1 parent | 843 (45.8) | 999 (54.2) | ||
| 2 parents | 391 (37.3) | 656 (62.7) | ||
| Time of birth, n (%) | ||||
| Premature infant | 254 (45.8) | 300 (54.2) | χ 2 = 1.21 | 0.27 |
| Normal term infant | 3,400 (48.3) | 3,643 (51.7) | ||
| Parental education, n (%) | ||||
| High school and below | 1,101 (50.0) | 1,099 (50.0) | χ 2 = 4.71 | 0.03 |
| Junior college and above | 2,553 (47.3) | 2,844 (52.7) | ||
| Average monthly income, yuan, n (%) | ||||
| <10,000 | 1,862 (49.3) | 1,917 (50.7) | χ 2 = 3.69 | 0.16 |
| 10,000–49,999 | 1,470 (47.1) | 1,651 (52.9) | ||
| ≥50,000 | 332 (47.0) | 375 (53.0) | ||
| Average living space, square meters, n (%) | ||||
| <20 | 1,295 (48.9) | 1,354 (51.1) | χ 2 = 3.08 | 0.38 |
| 20–29 | 1,004 (46.4) | 1,160 (53.6) | ||
| 30–39 | 704 (47.5) | 779 (52.5) | ||
| ≥40 | 626 (48.1) | 675 (51.9) | ||
| Sleep time per day, hours (%) | ||||
| <8 | 763 (34.8) | 1,432 (65.2) | χ 2 = 264.52 | <0.001 |
| 8–9 | 2,190 (51.3) | 2,078 (48.7) | ||
| >9 | 711 (62.2) | 433 (37.8) | ||
| Digital device exposure per day, hours (%) | ||||
| <0.5 | 1,444 (53.7) | 1,243 (46.3) | χ 2 = 64.22 | <0.001 |
| 0.5–1 | 1,325 (47.1) | 1,490 (52.9) | ||
| >1 | 885 (42.2) | 1,210 (57.8) | ||
| Time spent performing outdoor activities per day, mean (SD), hours | 2.68 (1.47) | 1.14 (1.01) | t = 8.14 | <0.001 |
| Baseline SER of the right eye, mean (SD), D | −0.08 (0.81) | −2.45 (1.75) | t = 19.48 | <0.001 |
Characteristics of students in the present study in 2021 (Shenzhen, China. 2019–2021).
SD, standard deviation; SER, spherical equivalent refraction; D, diopters.
A multiple logistic regression model was constructed to analyze the influencing factors of myopia. According to the OR and 95% CI, students with myopia were girl (OR = 1.77, 95% CI: 1.21–2.24), older (OR = 1.35, 95% CI: 1.18–1.54), had a lower baseline SER (OR = 0.12, 95% CI: 0.01–0.23), had one parent with myopia (OR = 1.47, 95% CI: 1.23–1.71), had two parents with myopia (OR = 1.51, 95% CI: 1.20–1.82), slept >9 h per day (OR = 0.45, 95% CI: 0.26–0.64), slept 8–9 h per day (OR = 0.51, 95% CI: 0.34–0.68), spent less time performing outdoor activities (OR = 0.84, 95% CI: 0.73–0.96), spent >1 h per day using a digital device (OR = 1.39, 95% CI: 1.03–1.75), and spent 0.5–1 h per day using a digital device (OR = 1.34, 95% CI: 1.01–1.66) (Figure 2). For each 1 year increase in age, the risk of myopia in older students was 1.35 times that of younger students. For each 1D increase in baseline SER, the risk of myopia in students with higher baseline SER was 0.12 times that of those with lower baseline SER. For each 1 h increase in time spent in outdoor activities per day, the risk of myopia among those who spent more time in outdoor activities was 0.84 times that of those who spent less time in outdoor activities.
FIGURE 2
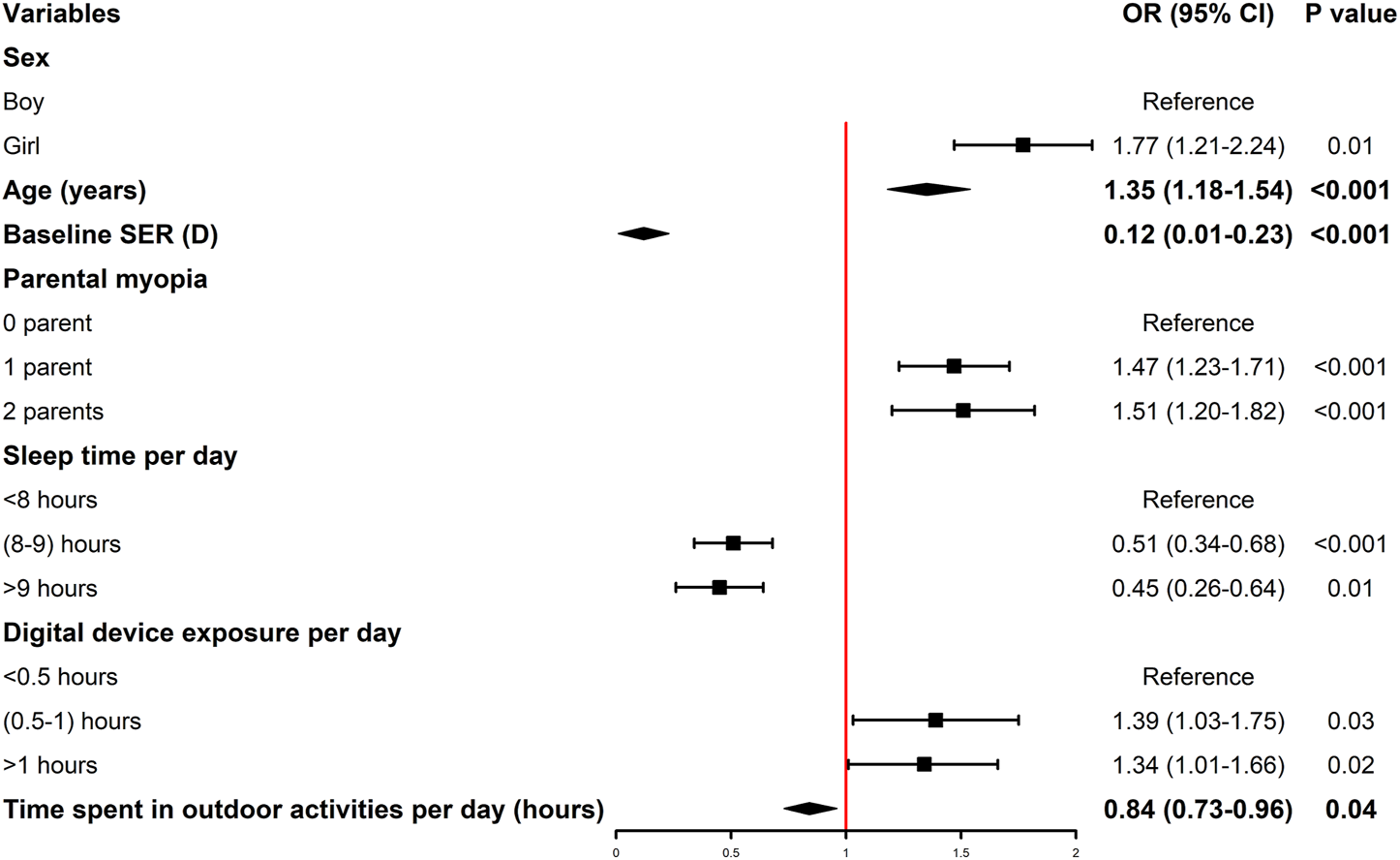
ORs and 95% CIs of myopia according to the influencing factors (Shenzhen, China. 2019–2021). OR, odds ratio; CI, confidence interval; SER, spherical equivalent refraction; D, diopters. *, The OR values of quantitative variables are represented by diamond legend, while those of qualitative variables are represented by square legend. The 95% CI of the OR of the quantitative variable is represented by the leftmost and rightmost ends of the diamond.
Discussion
We investigated the prevalence and incidence of myopia and change in SER among students in grades 1–3 from 2019 to 2021 and explored the influencing factors of myopia in this study. Myopia developed early in primary school students in Shenzhen, and the incidence of myopia was high, especially during the coronavirus disease 2019 (COVID-19) pandemic. The prevalence of myopia among students increased annually, and the incidence of myopia was higher in 2020 than in 2021. Sex, age, parental myopia, digital device exposure per day, baseline SER, sleep time per day, and time spent performing outdoor activities per day were the potential factors influencing myopia.
Many studies have demonstrated myopia to be related to sex of the individual (29, 30). In the present study, the prevalence of myopia among girls was higher than that among boys. Therefore, girls were not only more prone to myopia compared to boys but also a worse degree of myopia. The Anyang cohort study found that the incidence of myopia among boys in primary school was lower than that among girls (24). Moreover, the prevalence of myopia among boys in Poland was lower than that among girls (31). Eighteen-year-old Caucasian and East Asian girls were twice as likely to be myopic compared with 18-year-old boys; however, there was no significant difference between different sexes among Latinos, South Asians, and Hispanics (32). Myopia is also related to factors other than sex. This could be owing to the following reasons: First, girls tend to undergo puberty earlier compared to boys, and their axis grows faster, which can result in an increase in the prevalence of myopia. Second, girls prefer low-level physical activities, such as reading and writing, resulting in more near work and a lack of outdoor activities, which leads to an increase in the prevalence of myopia (33). At present, the relationship between myopia and sex among different populations is inconsistent. Further studies are warranted owing to the complex etiology of myopia.
The incidence of myopia and change in SER among primary school students in Shenzhen increased with the increase of grade level, which is consistent with the findings of another study (34). In the present study, both the incidence of myopia and the change in SER in 2020 were much higher than that in 2021. However, in the present study, the higher incidence in 2020 than in 2021 was not similar among girls in grade 1, possibly because they had higher hyperopia reserves than boys (−0.13 D vs. −0.17 D). Although the incidence of myopia and change in SER can be obtained directly from longitudinal examination in the same population, the effects of physiological refractive development on the change in the incidence and SER between the two time points should be considered. The annual incidence of myopia in primary school students has been shown to increase with age (24). Moreover, the annual change in SER in primary school students first increased and then decreased with the increase of age, and the annual change in SER reached the maximum in grade 3 and 4 students (−0.59 D) (24). The COVID-19 broke out in China in December 2019. To stop the spread of the COVID-19, all the students in China received online education at home and did not receive education in person at school until May 2020 (21). The annual change in the SER among primary school students from grades 1 to 3 during the COVID-19 pandemic (in 2019–2020) in this study was smaller than that in primary school students from grades 1 to 3 in Shanghai in 2010–2015 (33). The prevalence of myopia among students increased and the progression of myopia accelerated during the COVID-19 pandemic (21, 34, 35). To prevent and control the COVID-19 pandemic in 2020, students attended classes at home, which led to a decrease in the children’s physical activities and an increase in the use of electronic devices (36). Therefore, the lifestyle changes attributed to the COVID-19 pandemic may have resulted in a higher incidence and larger SER changes in the 1-year follow-up compared to the 2-year follow-up. The annual incidence of myopia among students in primary school in this study was higher than that in Australia (<2.2%) (25), Singapore (14.2%) (37), Anyang (20.0%–30.0%) (38), and Chongqing (10.6%) (22), but was close to that in Guangzhou (20.0%–30.0%) (23). Myopia screening by non-cycloplegic refraction was conducted in this study, which was consistent with that in Guangzhou (23) and but not with that in Australia (25), Singapore (37), Anyang (38), and Chongqing (22). However, myopia screening by non-cycloplegic refraction cannot identify pseudomyopia, which may result in the overestimation of the prevalence of myopia (38).
Eyes are in a hyperopic state (+2.50 to +3.00 D) at birth. With the growth and development of the eye, the eye tends to become slightly hyperopic or emmetropic, i.e., emmetropization (39). The refractive D of hyperopia is called the hyperopia reserve (38). In the present study, with the increase in the hyperopia reserve, the cumulative incidence of myopia in primary school students decreased during the 2-year follow-up period. The 2-year cumulative incidence of myopia among students with an SER of −0.50 D to 0.00 D can be as high as 57.6%, and <20% with an SER > +1.00 D. Previous studies have suggested that an increase in the early intervention efforts for primary school students whose hyperopia reserve is < +1.00 D could prevent rapid consumption of the hyperopia reserve.
The risk of myopia is associated with parental myopia according to previous studies (40, 41). Moreover, we found parental myopia have a great influence on myopia in children. Studies have identified more than 150 single-nucleotide polymorphisms associated with myopia (42). Consistent with previous studies (40), students who spent more time performing outdoor activities were less likely to become myopic. Previous studies have demonstrated that exposure to high-intensity sunlight can slow axial growth (43, 44), and may stimulate dopamine synthesis and release (45). Digital devices, such as computers and smartphone, have become exceeding popular in recent years, and one-third of the children aged 1–6 use mobile phones for 1–2 h per day (46). The prevalence of myopia increases with the popularity of digital devices (47), and exposure to digital devices can increase the risk of myopia (48). Consistent with previous studies (47, 48), students who spent more time using electronic devices were more likely to become myopic. Previous studies have confirmed that the SER increases by 0.10 D with a 1 h/day increase in sleep, and students who slept for more than 9 h/day had a 40% lower risk of developing myopia than those who slept for less than 5 h/day (16). Overall, the lack of sleep could be an important risk factor of myopia (49). In accordance with previous studies, we found that students who spent more time sleeping were less likely to become myopic. Furthermore, previous studies have shown that a higher risk of myopia was associated with higher family income (50, 51), and children living in areas with a higher population density have a higher risk of myopia (52–54). Moreover, the incidence of myopia in premature infants was as high as 75.5% (55). Contrary to previous studies, the prevalence of myopia was not associated with family income, living space, and time of birth in this study.t
The strengths of our study are as follows. The participants in this study were primary school students in grades 1–3, which reflect the epidemiological characteristics among children and adolescents in the early education stage. Thus, we were able to explore the development of refraction and myopia early, and provide a scientific basis for the prevention and control of myopia. However, this study has some limitations. First, myopia screening was performed by non-cycloplegic refraction, which cannot identify pseudomyopia and may overestimate the prevalence of myopia. The accuracy of cycloplegic refraction is high and widely used in clinical diagnosis. We should use cycloplegia to paralyze the ciliary muscle of the eye to obtain an accurate refractive status. Since cycloplegia could cause side effects (56), paralyzing the ciliary muscle in all the participants for myopia screening in large populations is challenging. Therefore, many studies use non-cycloplegic refraction to conduct myopia screening. Studies have confirmed the sensitivity and specificity of myopia screening in children aged 6–12 years (85.06% and 89.74%, respectively) who underwent a combination of distant uncorrected visual acuity and non-cycloplegic auto-refraction (57). Second, all the risk factor data in the present study were obtained from a questionnaire, which was subjective. Considering the retrospective design of the investigation, the results are particularly susceptible to recall bias. Past behavior or exposure history relies on the participant’s recollection, but certain details could be challenging to recall accurately. Third, some studies found that biometric indicators, such as the axial length (58) and corneal curvature (59), are associated with refraction status, and biometric indicators were not collected in this study. Fourth, the follow-up duration was short (2 years); thus, we may have not comprehensively analyzed the epidemiological characteristics of myopia.
Conclusion
In conclusion, we found that the prevalence of myopia among primary school students increased annually. The incidence of myopia and the progression of SER in 2020 were higher than that in 2021. The 2-year progression of the SER was 0.61D, 0.76D, and 0.79D for grades 1, 2, and 3, respectively. The prevalence of myopia among girls were higher than that among boys. In accordance with the Implementation Plan for Comprehensive Prevention and Control of Myopia in Children and Adolescents in China (60), the prevalence of myopia among primary school students is anticipated to be regulated to within 38% by 2030. Thus, interventions for myopia in primary school students should be strengthened, especially in the lower grades. Establishing good habits concerning eye use, encouraging outdoor activities, maintaining adequate sleep, and monitoring hyperopia reserve among primary school students are crucial for the prevention of myopia.
Statements
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of Shenzhen Eye Hospital. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author contributions
JM, DZ, JF, ML, MJ, XS, JW, and SZ: conceptualization and methodology. DZ, JF, MJ, XS, and JW: data curation. JM, DZ, JF, and SZ: formal analysis. SZ: supervision. JM: visualization and writing (original draft). DZ, JF, and SZ: writing (review and editing). All authors have approved the final version of the manuscript.
Funding
This work was supported by Sanming Project of Medicine in Shenzhen (No. SZSM202011015).
Acknowledgments
The authors would like to thank Prof. Mingguang He for helping with the reviewing of the article.
Conflict of interest
The authors declare that they do not have any conflicts of interest.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/ijph.2023.1605424/full#supplementary-material
References
1.
Wu PC Huang HM Yu HJ Fang PC Chen CT . Epidemiology of Myopia. Asia Pac J Ophthalmol (Phila) (2016) 5(6):386–93. 10.1097/APO.0000000000000236
2.
Spillmann L . Stopping the Rise of Myopia in Asia. Graefes Arch Clin Exp Ophthalmol (2020) 258(5):943–59. 10.1007/s00417-019-04555-0
3.
Holden BA Fricke TR Wilson DA Jong M Naidoo KS Sankaridurg P et al Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology (2016) 123(5):1036–42. 10.1016/j.ophtha.2016.01.006
4.
Li SM Liu LR Li SY Ji YZ Fu J Wang Y et al Design, Methodology and Baseline Data of a School-Based Cohort Study in central China: the Anyang Childhood Eye Study. Ophthalmic Epidemiol (2013) 20(6):348–59. 10.3109/09286586.2013.842596
5.
Xu T Wang B Liu H Wang H Yin P Dong W et al Prevalence and Causes of Vision Loss in China from 1990 to 2019: Findings from the Global burden of Disease Study 2019. Lancet Public Health (2020) 5(12):e682–e691. 10.1016/S2468-2667(20)30254-1
6.
Wong TY Ferreira A Hughes R Carter G Paul MP . Epidemiology and Disease burden of Pathologic Myopia and Myopic Choroidal Neovascularization: an Evidence-Based Systematic Review. Am J Ophthalmol (2014) 157(1):9–25.e12. 10.1016/j.ajo.2013.08.010
7.
Liang YB Friedman DS Wong TY Wang JJ Zhan SY Sun LP et al Prevalence and Causes of Low Vision and Blindness in a Rural Chinese Adult Population: the Handan Eye Study. Ophthalmology (2008) 115(11):1965–72. 10.1016/j.ophtha.2008.05.030
8.
Eckert KA Carter MJ Lansingh VC Wilson DA Furtado JM Frick KD et al A Simple Method for Estimating the Economic Cost of Productivity Loss Due to Blindness and Moderate to Severe Visual Impairment. Ophthalmic Epidemiol (2015) 22(5):349–55. 10.3109/09286586.2015.1066394
9.
Frick KD Joy SM Wilson DA Naidoo KS Holden BA . The Global burden of Potential Productivity Loss from Uncorrected Presbyopia. Ophthalmology (2015) 122(8):1706–10. 10.1016/j.ophtha.2015.04.014
10.
Chen Y Han X Guo X Li Y Lee J He M . Contribution of Genome-wide Significant Single Nucleotide Polymorphisms in Myopia Prediction: Findings from a 10-year Cohort of Chinese Twin Children. Ophthalmology (2019) 126(12):1607–14. 10.1016/j.ophtha.2019.06.026
11.
Morgn IG Ohno-Matsui K Saw SM . Myopia. Lancet (2012) 379(9827):1739–48. 10.1016/S0140-6736(12)60272-4
12.
French AN Morgan IG Rose KA . Risk Factors for Incident Myopia in Australian Schoolchildren: the Sydney Adolescent Vascular and Eye Study. Ophthalmology (2013) 120(10):2100–8. 10.1016/j.ophtha.2013.02.035
13.
He M Xiang F Zeng Y Mai J Chen Q Zhang J et al Effect of Time Spent Outdoors at School on the Development of Myopia Among Children in China A Randomized Clinical Trial. JAMA (2015) 314(11):1142–8. 10.1001/jama.2015.10803
14.
Yang L Vass C Smith L Alfred J Thomas W . Thirty-five-year Trend in the Prevalence of Refractive Error in Austrian Conscripts Based on 1.5 Million Participants. Br J Ophthalmol (2020) 104(10):1338–44. 10.1136/bjophthalmol-2019-315024
15.
Hansen MH Laigaard PP Olsen EM Skovgaard AM Larsen M Kessel L et al Low Physical Activity and Higher Use of Screen Devices Are Associated with Myopia at the Age of 16-17 Years in the CCC2000 Eye Study. Acta Ophthalmol (2020) 98(3):315–21. 10.1111/aos.14242
16.
Jee D Morgan IG Kim EC . Inverse Relationship between Sleep Duration and Myopia. Acta Ophthalmol (2016) 94(3):e204–10. 10.1111/aos.12776
17.
Wen L Cao Y Cheng Q Li X Pan L Li L et al Objectively Measured Near Work, Outdoor Exposure and Myopia in Children. Br J Ophthalmol (2020) 104:1542–7. 10.1136/bjophthalmol-2019-315258
18.
Saw SM Katz J Schein OD Chew SJ Chan TK . Epidemiology of Myopia. Epidemiol Rev (1996) 18(2):175–87. 10.1093/oxfordjournals.epirev.a017924
19.
Guo L Yang J Mai J Du X Guo Y Li P et al Prevalence and Associated Factors of Myopia Among Primary and Middle School-Aged Students: a School-Based Study in Guangzhou. Eye (Lond) (2016) 30:796–804. 10.1038/eye.2016.39
20.
Li Z Xu K Wu S Lv J Jin D Song Z et al Population-based Survey of Refractive Error Among School-Aged Children in Rural Northern China: the Heilongjiang Eye Study. Clin Exp Ophthalmol (2014) 42:379–84. 10.1111/ceo.12198
21.
Mu J Zhong H Liu M Jing M Shuai X Chen Y et al Trends in Myopia Development Among Primary and Secondary School Students during the COVID-19 Pandemic: A Large-Scale Cross-Sectional Study. Front Public Health (2022) 10:859285. 10.3389/fpubh.2022.859285
22.
Zhou WJ Zhang YY Li H Wu YF Xu J Lv S et al Five-year Progression of Refractive Errors and Incidence of Myopia in School-Aged Children in Western China. J Epidemiol (2016) 26:386–95. 10.2188/jea.JE20140258
23.
Wang SK Guo Y Liao C Chen Y Su G Zhang G et al Incidence of and Factors Associated with Myopia and High Myopia in Chinese Children, Based on Refraction without Cycloplegia. JAMA Ophthalmol (2018) 136:1017–24. 10.1001/jamaophthalmol.2018.2658
24.
Li SM Wei S Atchison DA Kang MT Liu L Li H et al Annual Incidences and Progressions of Myopia and High Myopia in Chinese Schoolchildren Based on a 5-year Cohort Study. Invest Ophthalmol Vis Sci (2022) 63(1):8. 10.1167/iovs.63.1.8
25.
French AN Morgan IG Burlutsky G Mitchell P Rose KA . Prevalence and 5 to 6 Year Incidence and Progression of Myopia and Hyperopia in Australian Schoolchildren. Ophthalmology (2013) 120:1482–91. 10.1016/j.ophtha.2012.12.018
26.
McCullough SJ O'Donoghue L Saunders KJ . Six Year Refractive Change Among white Children and Young Adults: Evidence for Significant Increase in Myopia Among white UK Children. PLoS One (2016) 11:e0146332. 10.1371/journal.pone.0146332
27.
Faul F Erdfelder E Lang AG Buchner AG . G*Power 3: a Flexible Statistical Power Analysis Program for the Social, Behavioral, and Biomedical Sciences. Behav Res Methods (2007) 39(2):175–91. 10.3758/bf03193146
28.
National Health Commission of the People's Republic of China. Specification for Screening of Refractive Error in Primary and Secondary School Students. (WS/T 663-2020). Beijing: National Health Commission of the People's Republic of China (2020).
29.
Shapira Y Mimouni M Machluf Y Chaiter Y Mezer E . The Increasing burden of Myopia in israel Among Young Adults over a Generation: Analysis of Predisposing Factors. Ophthalmology (2019) 126(12):1617–26. 10.1016/j.ophtha.2019.06.025
30.
Zhang Y Qiu K Zhang Q . Ametropia Prevalence of Primary School Students in Chinese Multi-Ethnic Regions. Strabismus (2020) 28(1):13–6. 10.1080/09273972.2019.1665691
31.
Czepita M Czepita D Safranow K . Role of Gender in the Prevalence of Myopia Among Polish Schoolchildren. J Ophthalmol (2019) 2019:9748576. 10.1155/2019/9748576
32.
Rudnicka AR Kapetanakis VV Wathern AK Logan NS Gilmartin B Whincup PH et al Global Variations and Time Trends in the Prevalence of Childhood Myopia, a Systematic Review and Quantitative Meta-Analysis: Implications for Aetiology and Early Prevention. Br J Ophthalmol (2016) 100(7):882–90. 10.1136/bjophthalmol-2015-307724
33.
Ma Y Zou H Lin S Xu X Zhao R Lu L et al Cohort Study with 4-year Follow-Up of Myopia and Refractive Parameters in Primary Schoolchildren in Baoshan District, Shanghai. Clin Exp Ophthalmol (2018) 46:861–72. 10.1111/ceo.13195
34.
Wang J Li Y Musch DC Wei N Qi X Ding G et al Progression of Myopia in School-Aged Children after COVID-19 home Confinement. JAMA Ophthalmol (2021) 14:293–300. 10.1001/jamaophthalmol.2020.6239
35.
Wang W Zhu L Zheng S Ji Y Xiang Y Lv B et al Survey on the Progression of Myopia in Children and Adolescents in Chongqing during COVID-19 Pandemic. Front Public Health (2021) 9:646770. 10.3389/fpubh.2021.646770
36.
Wang G Zhang Y Zhao J Zhang J Jiang F . Mitigate the Effects of home Confinement on Children during the COVID-19 Outbreak. Lancet (2020) 395(10228):945–7. 10.1016/S0140-6736(20)30547-X
37.
Saw SM Tong L Chua WH Chia KS Koh D Tan DTH et al Incidence and Progression of Myopia in Singaporean School Children. Invest Ophthalmol Vis Sci (2005) 46:51–7. 10.1167/iovs.04-0565
38.
Wei SF Li SM Liu L Li H Kang MT Sun YY et al Sleep Duration, Bedtime, and Myopia Progression in a 4-year Follow-Up of Chinese Children: the Anyang Childhood Eye Study. Invest Ophthalmol Vis Sci (2020) 61(3):37. 10.1167/iovs.61.3.37
39.
Medina A . The Cause of Myopia Development and Progression: Theory, Evidence, and Treatment. Surv Ophthalmol (2021) S0039-6257(21):488–509. 10.1016/j.survophthal.2021.06.005
40.
Jones LA Sinnott LT Mutti DO Mitchell GL Moeschberger ML Zadnik K . Parental History of Myopia, Sports and Outdoor Activities, and Future Myopia. Invest Ophthalmol Vis Sci (2007) 48(8):3524–32. 10.1167/iovs.06-1118
41.
Jones-Jordan LA Sinnott LT Manny RE Cotter SA Kleinstein RN Mutti DO et al Early Childhood Refractive Error and Parental History of Myopia as Predictors of Myopia. Invest Ophthalmol Vis Sci (2010) 51(1):115–21. 10.1167/iovs.08-3210
42.
Morgan IG Rose KA . Myopia: Is the Nature-Nurture Debate Finally over?Clin Exp Optom (2019) 102(1):3–17. 10.1111/cxo.12845
43.
Ulaganathan S Read SA Collins MJ Vincent SJ . Influence of Seasons upon Personal Light Exposure and Longitudinal Axial Length Changes in Young Adults. Acta Ophthalmol (2019) 97(2):e256–e265. 10.1111/aos.13904
44.
Hagen LA Gjelle J Arnegard S Pedersen HR Gilson SJ Baraas RC . Prevalence and Possible Factors of Myopia in Norwegian Adolescents. Sci Rep (2018) 8(1):13479. 10.1038/s41598-018-31790-y
45.
Chakraborty R Ostrin LA Nickla DL Iuvone PM Pardue MT Stone RA . Circadian Rhythms, Refractive Development, and Myopia. Ophthalmic Physiol Opt (2018) 38(3):217–45. 10.1111/opo.12453
46.
Cho KS Lee JM . Influence of Smartphone Addiction Proneness of Young Children on Problematic Behaviors and Emotional Intelligence: Mediating Self-Assessment Effects of Parents Using Smartphones. Comput Hum Behav (2017) 66:303–11. 10.1016/j.chb.2016.09.063
47.
Foreman J Salim AT Praveen A Fonseka D Ting DSW Guang HM et al Association between Digital Smart Device Use and Myopia: a Systematic Review and Meta-Analysis. Lancet Digit Health (2021) 3(12):e806–e818. 10.1016/S2589-7500(21)00135-7
48.
Rose KA French AN Morgan IG . Environmental Factors and Myopia: Paradoxes and Prospects for Prevention. Asia-pacific J Ophthalmol (2016) 5:403–10. 10.1097/APO.0000000000000233
49.
Hua WJ Jin JX Wu XY Yang JW Jiang X Gao GP et al Elevated Light Levels in Schools Have a Protective Effect on Myopia. Ophthalmic Physiol Opt (2015) 35(3):252–62. 10.1111/opo.12207
50.
Lim HT Yoon JS Hwang SS Lee SY . Prevalence and Associated Sociodemographic Factors of Myopia in Korean Children: the 2005 Third Korea National Health and Nutrition Examination Survey (KNHANES III). Jpn J Ophthalmol (2012) 56(1):76–81. 10.1007/s10384-011-0090-7
51.
Wu LJ You QS Duan JL Luo YX Liu LJ Li X et al Prevalence and Associated Factors of Myopia in High-School Students in Beijing. PLoS One (2015) 10(3):e0120764–42. 10.1371/journal.pone.0120764
52.
He M Zheng Y Xiang F . Prevalence of Myopia in Urban and Rural Children in mainland China. Optom Vis Sci (2009) 86:40–4. 10.1097/OPX.0b013e3181940719
53.
Uzma N Kumar BS Khaja Mohinuddin Salar BM Zafar MA Reddy VD . A Comparative Clinical Survey of the Prevalence of Refractive Errors and Eye Diseases in Urban and Rural School Children. Can J Ophthalmol (2009) 44:328–33. 10.3129/i09-030
54.
Ip JM Rose KA Morgan IG Burlutsky G Mitchell P . Myopia and the Urban Environment: Findings in a Sample of 12-Year-Old Australian School Children. Invest Ophthalmol Vis Sci (2008) 49:3858–63. 10.1167/iovs.07-1451
55.
Kim JY Kwak SI Yu YS . Myopia in Premature Infants at the Age of 6 Months. Korean J Ophthalmol (1992) 6(1):44–9. 10.3341/kjo.1992.6.1.44
56.
Bagheri A Givrad S Yazdani S Reza Mohebbi M . Optimal Dosage of Cyclopentolate 1% for Complete Cycloplegia: a Randomized Clinical Trial. Eur J Ophthalmol (2007) 17(3):294–300. 10.1177/112067210701700303
57.
Lin S Ma Y He X Zhu J Zou H . Using Decision Curve Analysis to Evaluate Common Strategies for Myopia Screening in School Aged Children. Ophthalmic Epidemiol (2019) 26(4):286–94. 10.1080/09286586.2019.1616774
58.
Fan DS Cheung EY Lai RY Kwok AKH Lam DSC . Myopia Progression Among Preschool Chinese Children in Hong Kong. Ann Acad Med Singap (2004) 33(1):39–43.
59.
Jong M Sankaridurg P Naduvilath T Li W He M . The Relationship between Progression in Axial Length/Corneal Radius of Curvature Ratio and Spherical Equivalent Refractive Error in Myopia. Optom Vis Sci (2018) 95(10):921–9. 10.1097/OPX.0000000000001281
60.
Xiong X Zhou L Zeng C Wang J Ye M Meng Y et al A longitudinal study on the progression and influencing factors of myopia in primary school students from grade one to grade three in Hubei Province. Chin J Ophthalmol (2021) 57(10):749–756. 10.3760/cma.j.cn112142-20201106-00740
Summary
Keywords
prevalence, longitudinal study, myopia, schoolchildren, influencing factor
Citation
Mu J, Zeng D, Fan J, Liu M, Jiang M, Shuai X, Wang J and Zhang S (2023) Epidemiological Characteristics and Influencing Factors of Myopia Among Primary School Students in Southern China: A Longitudinal Study. Int J Public Health 68:1605424. doi: 10.3389/ijph.2023.1605424
Received
21 September 2022
Accepted
06 February 2023
Published
14 February 2023
Volume
68 - 2023
Edited by
Seyma Karaketir, Istanbul University, Türkiye
Reviewed by
Chia Hui Tan, China Medical University, Taiwan
Updates
Copyright
© 2023 Mu, Zeng, Fan, Liu, Jiang, Shuai, Wang and Zhang.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shaochong Zhang, 30302m@163.com
†These authors have contributed equally to this work
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.