- 1Department of Preventive Medicine, College of Medicine, The Catholic University of Korea, Seoul, Republic of Korea
- 2Department of Humanities and Social Medicine, College of Medicine and Catholic Institute for Healthcare Management, The Catholic University of Korea, Seoul, Republic of Korea
Objectives: The aim of this study was to examine the association between changes in oral health related quality of life (OHRQoL) and depressive symptoms in the elderly South Koreans.
Methods: We used the 2018 and 2020 Korean Longitudinal Study of Ageing data. Our study population was a total of 3,604 participants aged over 65 in 2018. The independent variable of interest was the changes in the Geriatric Oral Health Assessment Index as OHRQoL between 2018 and 2020. The dependent variable was depressive symptoms in 2020. Multivariable logistic regression analyzed the associations between changes in OHRQoL and depressive symptoms.
Results: Participants with improvement in OHRQoL over 2-year period were likely to have fewer depressive symptoms in 2020. Especially, changes in the oral pain and discomfort dimension score was associated with depressive symptoms. A decline in oral physical function, such as difficulty in chewing and speaking, was also associated with depressive symptoms.
Conclusion: Negative change in OHRQoL is a risk factor for depression in elderly. This results suggest the importance of maintaining good oral health in later life, as a protective factor against depression.
Introduction
According to the Organization for Economic Co-operation and Development (OECD) demography statistics, the average annual increase of South Korea’s elderly population was 3.3% from 1970 to 2018, which is the fastest among all OECD countries (1). In 2020, 15.7% of the Korean population was aged ≥65 years; this is expected to increase to 20.3% in 2025 and 43.9% in 2060 (2). As the aging population increases rapidly, the importance of oral health of the elderly is increasing. Oral health is an essential factor for maintaining health, wellbeing, and quality of life (3). The World Health Organization defines oral health as “a state of being free from mouth and facial pain, oral and throat cancer, oral infection and sores, periodontal (gum) disease, tooth decay, tooth loss, and other diseases and disorders that limit an individual’s capacity in biting, chewing, smiling, speaking, and psychosocial wellbeing” (4).
Previous studies have suggested an association between tooth loss and the incidence of depressive symptoms among older adults (5, 6). Depression is associated with untreated tooth decay, loss of natural teeth, and frequency of dental visits (7, 8). Some studies reported that reductions in subjective mastication and pronunciation ability, and oral dryness are risk factors for depression (9, 10). The deterioration of oral function and orofacial appearance related to social activities; speaking, smiling, and eating, significantly mediated the relationship between tooth loss and the incidence of depressive symptoms (6).
Oral health can be defined and measured both objectively and subjectively. Along with the number of remaining teeth and chewing ability, oral health-related quality of life (OHRQoL) has received considerable attention as a subjective marker of oral health. OHRQoL considers not only chewing ability, but also more information about several other important oral health parameters. Patient-centered care is becoming increasingly important. OHRQoL is a representative measure of subjective oral health that was developed to analyze the effects of self-perceived oral health on daily activities and wellbeing (11, 12).
Many studies have demonstrated that a lower OHRQoL is associated with a higher likelihood of depressive symptoms (5, 13–16). Longitudinal studies reported that worsening showed worsening in OHRQoL is associated with depressive symptoms at follow-up (5, 14). Similarly, cross-sectional studies conducted in Korea showed association between lower OHRQoL and higher depression in elderly populations (17). However, those studies included small study population or used cross-sectional study design. Therefore, this study aims to clarify the association between changes in OHRQoL and depressive symptoms in an elderly South Korean population using representative data and longitudinal analysis.
Methods
Data
We used 2018 and 2020 data from the Korean Longitudinal Study of Ageing (KLoSA), which provides in-depth interview data from Koreans aged ≥45 years living in households selected by multistage stratified probability sampling. The respondents were considered representative of the Korean adult population. Trained interviewers collected the data using a computer-aided interview system (18).
In total, 3,860 patients aged ≥65 years in 2018 participated in both the 2018 and 2020 surveys. Participants with missing data (n = 36) were excluded from the analysis. The questionnaires from proxy respondents (n = 208) were also excluded because their data on depressive symptoms and other indicators of psychological wellbeing were considered potentially unreliable (19). Ultimately, 3,615 elderly Koreans were included in our study. (Figure 1). This study was approved by the Institutional Review Board of The Catholic University of Korea (MC22ZISI0042).
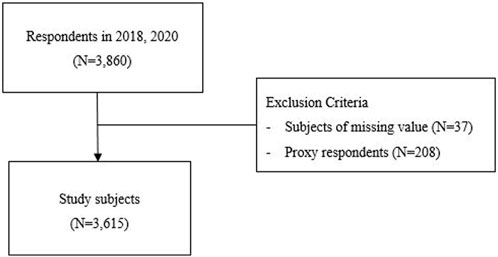
FIGURE 1. Selection of study subjects (Korean longitudinal study of ageing, South Korea, 2018–2020).
Variables
The independent variable was the changes in OHRQoL assessed using the Geriatric Oral Health Assessment Index (GOHAI) between 2018 and 2020. GOHAI is self-reported questionnaire designed to assess oral health problems affecting quality of life, especially for use in the elderly population (20). The GOHAI includes 12 questions related to oral health and the frequency of oral health problems. The problems are rated using a 6-point Likert scale (0, always; 1, very often; 2, often; 3, sometimes; 4, seldom; 5, never). The GOHAI is calculated by summing the scores of the 12 items; total scores thus range from 0 to 60. Higher scores indicate higher OHRQoL.
The GOHAI encompasses three dimensions: physical function dimension (limitation with certain food types, difficulty with biting/chewing, uncomfortable to swallow, prevented from speaking), psychosocial dimension (limited contact with other people, unhappy with appearance of gums and teeth, worried about teeth or gums, nervous/self-conscious about teeth or gums, uncomfortable eating in front of others), and pain and discomfort dimension (discomfort when eating, use of medications to relieve gum pain, teeth sensitive to hot/cold). We used a validated Korean translation of the GOHAI (21). The Cronbach’s alpha of the GOHAI was 0.830 in this study.
Dependent variable was the presence of depressive symptoms in 2020, as assessed by the Center of Epidemiologic Studies Depression Scale, 10-item version (CES-D10) (22). Total scores range from 0 to 10, and the cutoff CES-D10 score for the depressive symptoms is 4 (23). The Cronbach’s alpha for the CES-D10 was 0.853 in this study.
Covariates were included based on the results of previous population-based studies of depressive symptoms, including age (65–69, 70–74, 75–79, or ≥80 years), sex (male or female), educational level (elementary school or less, middle school, high school, or college or over), spouse (yes or no), number of family members (1, 2, or ≥3), health insurance type (National Health Insurance or medical aid), household income quartile (Q1–4), self-rated health (SRH) (good, fair, or poor), chronic diseases (0, 1–2, or ≥3), and activity of daily living (ADL) (0, 1 or over). Oral health was assessed according to changes in the numbers of dental implants and remaining teeth.
Statistical Analysis
Sampling weights were applied to estimate the representative population. Categorical and continuous data are expressed as weighted percentages and means, respectively. The chi-square test and t-test were conducted to examine the distribution and differences in sociodemographic characteristics, health-related characteristics according to depressive status, and changes in GOHAI total, dimension, and item scores. Multivariable logistic regression analysis was performed to analyze the associations between changes in OHRQoL and depressive symptoms, adjusted by 2018 baseline characteristics (GOHAI, socioeconomic characteristics, and health-related characteristics) and changes in oral health (numbers of dental implants and using denture).
To prevent multicollinearity, separate multivariate logistic regression models were constructed to evaluate the total GOHAI scores and GOHAI subdimension scores. Statistical significance was set at α = 0.05. Data were analyzed using SAS ver. 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
General Characteristics
Table 1 shows the distribution of the 2018 baseline general characteristics of the study subjects. Female was 57.1%, and the greatest proportion in educational level was elementary school or less 47.4%. Regarding living arrangements, 69.3% of the participants lived with their spouse and 56.2% lived with at least two family members. With respect to SRH, only 22.0% of the subjects self-rated their health status as “Good”. 21.2% did not have a chronic disease and 2.2% had ADL limitations.
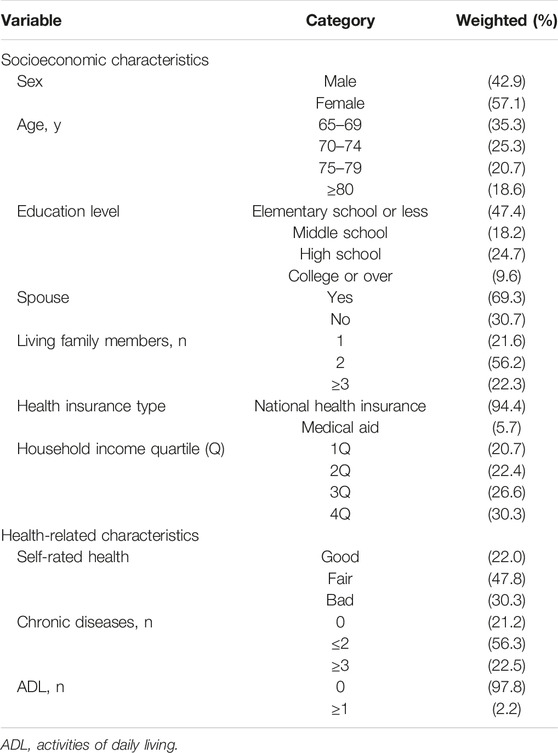
TABLE 1. Baseline general characteristics of the study subjects in 2018 (Korean longitudinal study of ageing, South Korea, 2018–2020).
Changes in OHRQoL and Oral Health
The GOHAI score was 37.5 ± 0.15 in 2018 and 38.3 ± 0.14 in 2020. OHRQoL was slightly higher in 2020 than 2018. Regarding the dimensions of the GOHAI, the physical function dimension and oral pain and discomfort dimension scores increased more than the psychosocial dimension score between 2018 and 2020. Issues related to chewing, speech, and oral pain and discomfort improved positively. The GOHAI items showing the greatest score increases were “Able to swallow comfortably” (physical function dimension), and “Able to eat without discomfort” and “Used medication to relieve pain” (pain and discomfort dimension).
We also analyzed oral health according to the number of remaining teeth and dental implants. The number of remaining teeth was 19.6 ± 0.17 in 2018 and 17.3 ± 0.19 in 2020, and the number of implants was 1.3 ± 0.06 in 2018 and 3.8 ± 0.13 in 2020. The number of remaining teeth decreased approximately by 2.3, while the number of dental implants increased approximately by 2.5. Using denture was 30.4% in 2018 and it decreased to 28.8% in 2020 (Table 2).
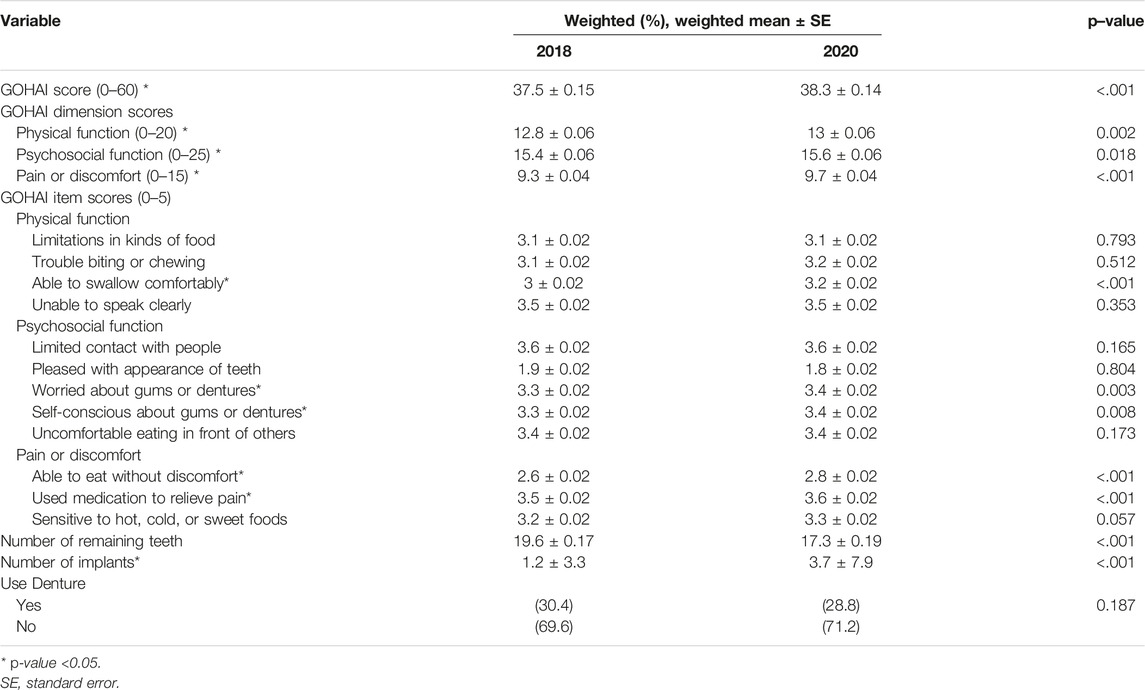
TABLE 2. Changes in oral health-related quality of life and oral health (Korean longitudinal study of ageing, South Korea, 2018–2020).
Baseline Characteristics by 2020 Depressive Symptoms
Table 3 shows 2018 baseline characteristics by 2020 depressive symptoms. In total, 11.8% of the subjects had depressive symptoms. Female, aged ≥80 years, a lower educational level (elementary or less), a lower income level (Q1), and poor health status (poor SRH or chronic diseases) showed more proportion in depressive symptoms group. Especially the subjects with depression had poor oral health compared with those without depressive symptoms. The mean GOHAI score was 5.5 points lower in the depression group than in the group without depressive symptoms (32.6 ± 0.39 vs. 38.1 ± 0.15), indicating that the depressed patients had a lower OHRQoL. Furthermore, the mean number of teeth was 2.7 lower in the depression group than in the group without depressive symptoms (17.3 ± 0.53 vs. 20 ± 0.18), as was the mean number of implants (1.1 ± 0.14 vs. 1.4 ± 0.06). Finally, the proportion of patients with dentures was 7.1% higher in the depressive symptoms group than in the group without depressive symptoms (36.7% vs. 29.6%).
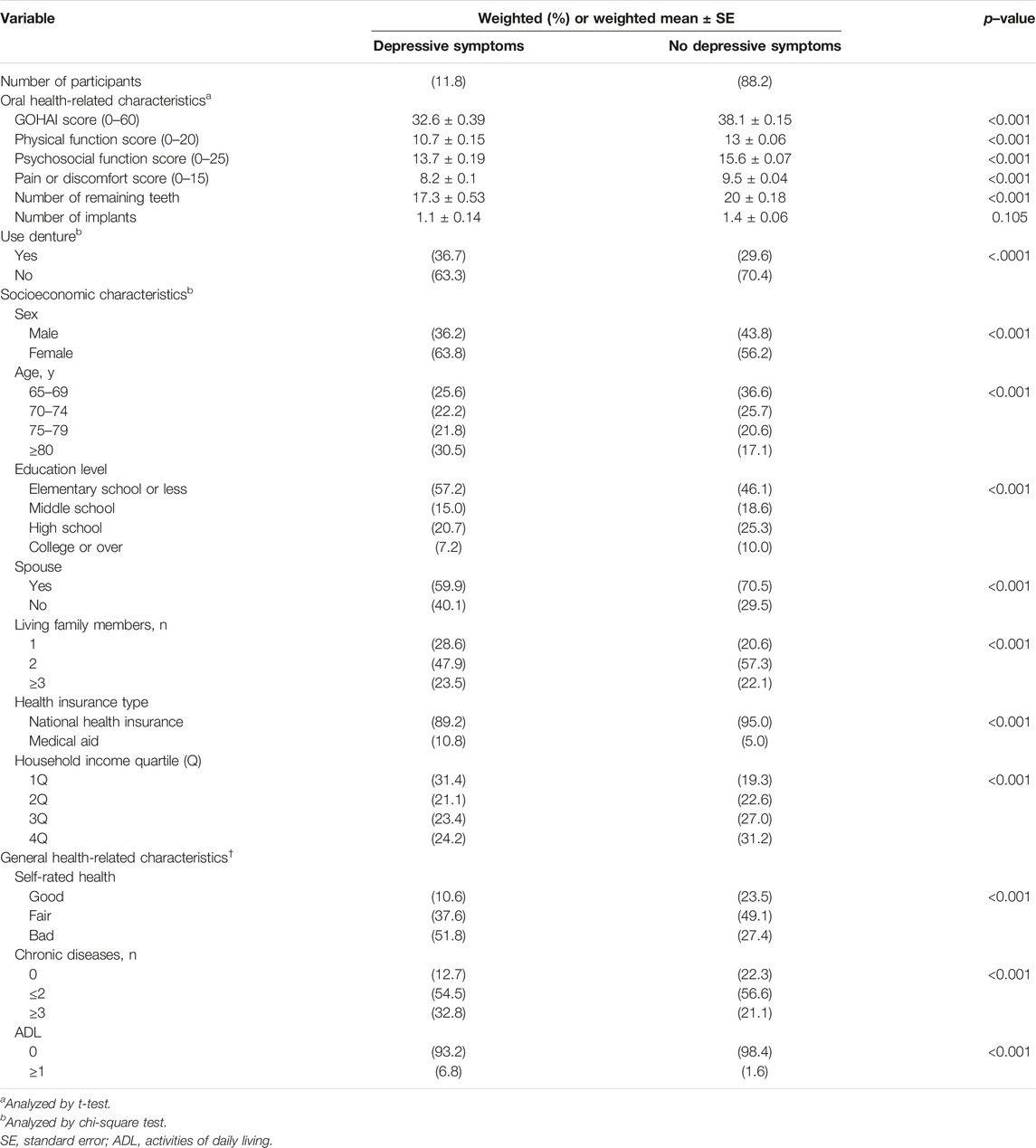
TABLE 3. Baseline characteristics according to depressive symptoms in 2020 (Korean longitudinal study of ageing, South Korea, 2018–2020).
Association Between Changes in OHRQoL and Depressive Symptoms
Compared with unadjusted odds ratio in model 1, the likelihood of depressive symptoms was significantly associated with changes in OHRQoL (OR: 0.92, 95% CI: 0.92–0.92) after adjustment for 2018 baseline characteristics and changes in oral health. It indicates increase in GOHAI score was associated with lower risk of depressive symptoms at follow-up.
In model 2, changes in the oral pain and discomfort dimension score (OR: 0.86, 95% CI: 0.79–0.93) had the strongest association with depressive symptoms; changes in physical function score (OR: 0.90, 95% CI: 0.85–0.95) was also significantly associated with depressive symptoms. It indicates increase on the oral pain and discomfort and physical function GOHAI subdimensions were inversely associated with the likelihood of depressive symptoms at follow-up. However, there were no associations between the changes in psychosocial subdimension scores and depressive symptoms at follow-up. Thus, improved oral pain and discomfort and physical function were associated with fewer depressive symptoms in our elderly Korean population (Table 4).
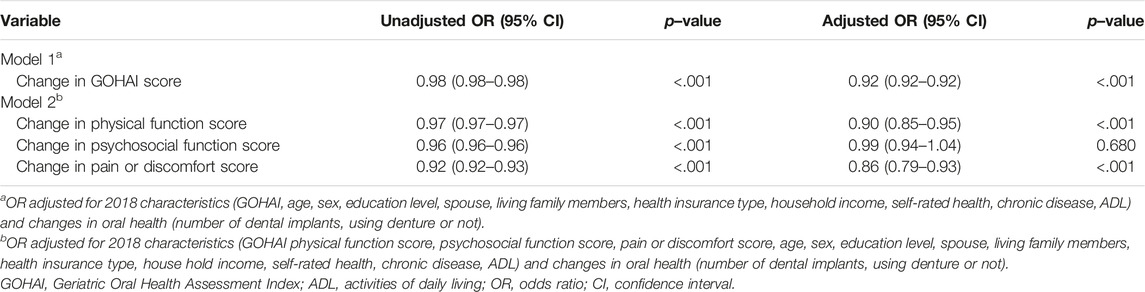
TABLE 4. Association between changes in oral health-related quality of life and depressive symptoms (Korean longitudinal study of ageing, South Korea, 2018–2020).
Discussion
This study analyzed the association between changes in OHRQoL, as assessed by the GOHAI, and depressive symptoms in elderly (aged ≥65 years) South Koreans. Participants with improved OHRQoL over 2-year period were likely to have fewer depressive symptoms in 2020, especially when oral pain and discomfort dimension changed positively, the likelihood of depressive symptoms decreased the most. Our results are similar to those of previous studies. A longitudinal study conducted in the UK reported that deterioration in oral health and OHRQoL in an elderly cohort had a negative effect on depressive symptoms over a 4-year period (5). A Japanese study showed a low baseline OHRQoL increased the probability of depressive symptoms after 4 years (14). Also, a cross-sectional study reported that lower OHRQoL was associated with more severe depression in the elderly (15, 16). Caution is required when making comparisons with cross-sectional studies.
In this study, the prevalence of depressive symptoms was 11.8% in 2020, similar to the rates in other studies of the elderly (i.e., 9.1–9.3% (24) and 11.0% (14)). The GOHAI was 37.0 and 37.8 in 2018 and 2020 in our study, compared with 45.8 in a Mexican study, and 53.6 (15) and 50.8 (25) in Japanese studies. Differences in GOHAI among countries can be explained by differences in self-rated oral health status. In one study, South Koreans had poorer self-rated oral health compared with a US population, even though the oral health (i.e., the number of teeth; decayed, missing, filled teeth index; decayed teeth index; filled teeth index; and missing teeth index) considered better (26).
Differences between countries are more pronounced for the dimension of the GOHAI. A study in Japan, oral dryness and pain were associated with depression (13). A previous study in South Korea reported similar results; specifically, there was association between oral pain and physical dimension of the OHRQoL and depression (27). According to an Asian study of the elderly, oral pain and discomfort appears to be the most relevant dimension with respect to depression in elderly Asian populations (28).
A decline in oral physical function, such as difficulty in chewing and speaking, is also associated with depression (9). Difficulty chewing tough foods may have an impact on daily enjoyment and life in older adults. Eating with relatives and friends also involves communication. Decreased oral function can impair social contact in older adults (29).
Common causes of oral pain and discomfort in the elderly include dental caries (30), periodontal disease (31), and oral dryness (32), while problems with oral physical function arise due to unsuitable dentures, lost teeth, and oral dryness (32–34). To solve those problems, the Korean government has implemented insurance policies covering two implants, one partial or full denture treatment, and the costs of maintaining dentures (through the National Health Insurance plan for the elderly, i.e., those aged ≥65 years) (35). These healthcare policies have improved dental care for the Korean elderly (36) and could help reduce oral health-related depression in this age group. Therefore, clinicians managing elderly patients with depression should focus on oral health. The government should also consider oral health and depression together when developing mental health-promoting strategies for the elderly. This study provides basic data that could inform policies aimed at the prevention and management of depression in the elderly.
Strengths and Limitations
This study had several limitations. First, we only analyzed changes in OHRQoL over a 2-year period; research considering longer periods is needed to confirm a causal relationship between oral health and depressive symptoms. Nevertheless, this study provides useful information for future long-term longitudinal studies. Second, the KLoSA data is secondary, and various oral health parameters potentially important to depression, such as gingival bleeding, oral dryness, and dissatisfaction with dentures, were not considered. Despite its limitations, this study showed an association between changes in OHRQoL and depressive symptoms based on an analysis of KLoSA data representative of the Korean elderly population.
Conclusion
This study showed that decrease in Oral health-related quality of life was a risk factor for depression in elderly. Oral health is a dynamic phenomenon influenced by many factors that change over time, and can generate positive, as well as negative emotions. This results have important implications for gerontologists and practitioners. The importance of maintaining good oral health in later life, as a protective factor against depression.
Ethics Statement
The KLoSA was approved by National Statistical Office (No. 336002) and was conducted after acquiring verbal consent from the study participants. This studies approved to use data by Institutional Review Board, The Catholic University of Korea.
Author Contributions
KP: Conceptualization; Data curation; Formal analysis; Visualization; Writing-original draft; Writing-review and editing. YK: Methodology; Validation; Writing-review and editing. SK: Methodology; Validation; Writing-review and editing. HL: Conceptualization; Methodology; Validation; Writing-review and editing. All authors read and approved the final manuscript.
Funding
This research was supported by a fund from the Catholic Medical Center Research Foundation made in the program year of 2022 (Grant number: 5-2022-B0001-00207).
Conflict of Interest
The authors declare that they do not have any conflicts of interest.
Abbreviations
CES-D10, Center of Epidemiologic Studies Depression Scale, 10-item version; CI, Confidence Interval; GOHAI, Geriatric Oral Health Assessment Index; KLoSA, Korean Longitudinal Study of Ageing; OECD, Organization for Economic Co-operation and Development; OHRQoL, Oral Health Related Quality of Life; OR, Odds Ratio; SRH, Self Rated Health; VIF, Variance Inflation Factor.
References
1. De La Maisonneuve, C, and Oliveira Martins, J. Public Spending on Health and Long-term Care: A new set of projections. OECD Economic Policy Papers No. 6. Paris: OECD (2013). doi:10.1787/2226583X
2.Statistics Korea. Statistics on the Aged (2020). Available from: https://kostat.go.kr/board.es?mid=a20111030000&bid=11759&tag=&act=view&list_no=388599&ref_bid=&keyField=&keyWord=&nPage=1 (Accessed May 21, 2020).
3. Petersen, PE. The World Oral Health Report 2003: Continuous Improvement of Oral Health in the 21st century--the Approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiol (2003) 31:3–23. doi:10.1046/j.2003.com122.x
4.World Health Organization. Oral health. Availlable from: https://www.afro.who.int/health-topics/oral-health (Accessed May 19, 2022).
5. Rouxel, P, Tsakos, G, Chandola, T, and Watt, RG. Oral Health-A Neglected Aspect of Subjective Well-Being in Later Life. J Gerontol B Psychol Sci Soc Sci (2018) 73(3):382–6. doi:10.1093/geronb/gbw024
6. Kusama, T, Kiuchi, S, Umehara, N, Kondo, K, Osaka, K, and Aida, J. The Deterioration of Oral Function and Orofacial Appearance Mediated the Relationship between Tooth Loss and Depression Among Community-Dwelling Older Adults: a JAGES Cohort Study Using Causal Mediation Analysis. J affective Disord (2021) 286:174–9. doi:10.1016/j.jad.2021.02.071
7. Wright, FAC, Takehara, S, Stanaway, FF, Naganathan, V, Blyth, FM, Hirani, V, et al. Associations between Oral Health and Depressive Symptoms: Findings from the Concord Health and Ageing in Men Project. Australas J ageing (2020) 39(3):e306–e314. doi:10.1111/ajag.12763
8. Goto, M, Ishii, T, and Sakakibara, Y. Preliminary Study of Mastication as an Indicator of Adult Dental Health. J Dental Health (1985) 35(5):815–6. doi:10.5834/jdh.35.815
9. Park, MS, Hwang, K-G, and Choi, BY. Correlation between Depressive Symptoms and Subjective Mastication Ability and Ability to Pronunciation Among Korean Elderly. Epidemiol Health (2016) 38:e2016035. doi:10.4178/epih.e2016035
10. Skośkiewicz-Malinowska, K, Malicka, B, Ziętek, M, and Kaczmarek, U. Oral Health Condition and Occurrence of Depression in the Elderly. Medicine (Baltimore) (2018) 97(41):e12490. doi:10.1097/MD.0000000000012490
11. Kressin, N. Associations Among Different Assessments of Oral Health Outcomes. J dental Educ (1996) 60(6):501–7. doi:10.1002/j.0022-0337.1996.60.6.tb03057.x
12. Kressin, NR, III, AS, Atchison, KA, Kazis, L, and Jones, JA. Is depressive symptomatology associated with worse oral functioning and well-being among older adults? J Public Health Dent (2002) 62(1):5–12. doi:10.1111/j.1752-7325.2002.tb03414.x
13. Takiguchi, T, Yoshihara, A, Takano, N, and Miyazaki, H. Oral Health and Depression in Older Japanese People. Gerodontology (2016) 33(4):439–46. doi:10.1111/ger.12177
14. Ohi, T, Murakami, T, Komiyama, T, Miyoshi, Y, Endo, K, Hiratsuka, T, et al. Oral Health-Related Quality of Life Is Associated with the Prevalence and Development of Depressive Symptoms in Older Japanese Individuals: The Ohasama Study. Gerodontology (2022) 39(2):204–12. doi:10.1111/ger.12557
15. Hayashi, K, Izumi, M, Mastuda, Y, Isobe, A, and Akifusa, S. Relationship between Anxiety/depression and Oral Health-Related Quality of Life in Inpatients of Convalescent Hospitals. Odontology (2019) 107(2):254–60. doi:10.1007/s10266-018-0394-x
16. Hassel, AJ, Danner, D, Schmitt, M, Nitschke, I, Rammelsberg, P, and Wahl, H-W. Oral Health-Related Quality of Life Is Linked with Subjective Well-Being and Depression in Early Old Age. Clin Oral Investig (2011) 15(5):691–7. doi:10.1007/s00784-010-0437-3
17. Kim, SY, and Kim, JH. The Relationship between Old-Age Oral Health and Depression Levels. Health Soc Welfare Rev (2021) 41(4):62–71. doi:10.15709/HSWR.2021.41.4.62
18.Employment Survey. Population Aging Panel Survey (KLoSA, KLoEE) (2015). Available from: https://survey.keis.or.kr/klosa/klosa04.jsp (Accessed May 19, 2022).
19. Yang, Y, and George, LK. Functional Disability, Disability Transitions, and Depressive Symptoms in Late Life. J Aging Health (2005) 17(3):263–92. doi:10.1177/0898264305276295
20. Atchison, KA, and Dolan, TA. Development of the Geriatric Oral Health Assessment index. J dental Educ (1990) 54(11):680–7. doi:10.1002/j.0022-0337.1990.54.11.tb02481.x
21. Shin, S-J, and Jung, S-H. A Korean Version of the Geriatric Oral Health Assessment index (GOHAI) in Elderly Populations: Validity and Reliability. J Korean Acad Oral Health (2011) 35(2):187–95. https://www.jkaoh.org/journal/view.html?uid=98&vmd=Full
22. Kohout, FJ, Berkman, LF, Evans, DA, and Cornoni-Huntley, J. Two Shorter Forms of the CES-D (Center for Epidemiological Studies Depression) Depression Symptoms index. J Aging Health (1993) 5(2):179–93. doi:10.1177/089826439300500202
23. Irwin, M, Artin, KH, and Oxman, MN. Screening for Depression in the Older Adult: Criterion Validity of the 10-item Center for Epidemiological Studies Depression Scale (CES-D). Arch Intern Med (1999) 159(15):1701–4. doi:10.1001/archinte.159.15.1701
24. Sjöberg, L, Karlsson, B, Atti, AR, Skoog, I, Fratiglioni, L, and Wang, HX. Prevalence of Depression: Comparisons of Different Depression Definitions in Population-Based Samples of Older Adults. J Affect Disord (2017) 221:123–31. doi:10.1016/j.jad.2017.06.011
25. Noguchi, S, Makino, M, Haresaku, S, Shimada, K, and Naito, T. Insomnia and Depression Impair Oral Health-Related Quality of Life in the Old-Old. Geriatr Gerontol Int (2017) 17(6):893–7. doi:10.1111/ggi.12816
26. Choi, J-A, Mun, S-J, Chung, W-G, and Han, S-Y. Differences in Determinants Influencing Self-Rated Oral Health in Korean and American Adults. Int J Environ Res Public Health (2022) 19(6):3618. doi:10.3390/ijerph19063618
27. Choi, SH, Kim, JS, Cha, JY, Lee, KJ, Yu, HS, and Hwang, CJ. Subjective Food Intake Ability Related to Oral Health-Related Quality of Life and Psychological Health. J Oral Rehabil (2016) 43(9):670–7. doi:10.1111/joor.12412
28. Wan, KY, McMillan, AS, and Wong, MC. Orofacial Pain Symptoms and Associated Disability and Psychosocial Impact in Community-Dwelling and Institutionalized Elderly in Hong Kong. Community Dent Health (2012) 29(1):110–6. doi:10.1922/CDH_2578McMillan07
29. Mikami, Y, Watanabe, Y, Motokawa, K, Shirobe, M, Motohashi, Y, Edahiro, A, et al. Association between Decrease in Frequency of Going Out and Oral Function in Older Adults Living in Major Urban Areas. Geriatr Gerontol Int (2019) 19(8):792–7. doi:10.1111/ggi.13715
30. Masood, M, Newton, T, Bakri, NN, Khalid, T, and Masood, Y. The Relationship between Oral Health and Oral Health Related Quality of Life Among Elderly People in United Kingdom. J Dentistry (2017) 56:78–83. doi:10.1016/j.jdent.2016.11.002
31. Santucci, D, and Attard, N. The Oral Health-Related Quality of Life in State Institutionalized Older Adults in Malta. Int J Prosthodont (2015) 28(4):402–11. doi:10.11607/ijp.4185
32. Castrejón-Pérez, RC, Borges-Yáñez, SA, Irigoyen-Camacho, ME, and Cruz-Hervert, LP. Negative Impact of Oral Health Conditions on Oral Health Related Quality of Life of Community Dwelling Elders in Mexico City, a Population Based Study. Geriatr Gerontol Int (2017) 17(5):744–52. doi:10.1111/ggi.12780
33. Enoki, K, Ikebe, K, Matsuda, KI, Yoshida, M, Maeda, Y, and Thomson, WM. Determinants of Change in Oral Health-Related Quality of Life over 7 Years Among Older Japanese. J Oral Rehabil (2013) 40(4):252–7. doi:10.1111/joor.12031
34. Kunrath, I, and Silva, AER. Oral Health and Depressive Symptoms Among Older Adults: Longitudinal Study. Aging Ment Health (2021) 25(12):2265–71. doi:10.1080/13607863.2020.1855104
35.Welfare MoHa. Elderly Implant Care expanded aged over 65 (2016). Available from: https://www.mohw.go.kr/react/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&page=1&CONT_SEQ=330878&SEARCHKEY=TITLE&SEARCHVALUE=%EC%9E%84%ED%94%8C%EB%9E%80%ED%8A%B8 (Accessed June 20, 2022).
Keywords: depressive symptoms, aged, oral health related quality of life, geriatric oral health assessment index, Korean longitudinal study of ageing
Citation: Park KE, Lee H, Kwon YD and Kim S (2023) Association Between Changes in Oral Health-Related Quality of Life and Depressive Symptoms in the Korean Elderly Population. Int J Public Health 68:1605403. doi: 10.3389/ijph.2023.1605403
Received: 16 September 2022; Accepted: 13 March 2023;
Published: 28 March 2023.
Edited by:
Nino Kuenzli, Swiss School of Public Health (SSPH+), SwitzerlandCopyright © 2023 Park, Lee, Kwon and Kim. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hooyeon Lee, aHlsZWVAY2F0aG9saWMuYWMua3I=
This Original Article is part of the IJPH Special Issue “Health in All Sustainable Development Goals.”
 Kyoung Eun Park
Kyoung Eun Park Hooyeon Lee1*
Hooyeon Lee1* Young Dae Kwon
Young Dae Kwon