- 1Division of Cancer Control and Policy, National Cancer Control Institute, National Cancer Center, Goyang, South Korea
- 2Department of Healthcare Institution Support, National Health Insurance Service, Wonju, South Korea
- 3Department of Family Medicine, College of Medicine, Chung-Ang University, Seoul, South Korea
- 4Department of Nursing Science, Sungshin Women’s University, Seoul, South Korea
- 5Department of Humanities and Social Medicine, College of Medicine and Catholic Institute for Healthcare Management, The Catholic University of Korea, Seoul, South Korea
- 6Division of Health Administration, College of Software and Digital Healthcare Convergence, Yonsei University, Wonju, South Korea
Objective: Social distancing has been confirmed to reduce the incidence of not only the COVID-19, but also the incidence of other diseases. Therefore, this study aimed to investigate the effect of social distancing policies on the incidence of infectious eye diseases by monitoring their nationwide incidence data in all age groups.
Methods: In this study, to analyse the impact of COVID-19 policy on IEDSC, the time periods were divided into two interventions. The first intervention was the first COVID-19 patient report in Korea on 19 January 2020. The second intervention was relaxation of the social distancing policy on 6 May 2020. Segmented regression analysis of the interrupted time series was used to assess COVID-19 policies on the IEDSC.
Results: After the first incidence of a COVID-19 patient, IEDSCs decreased significantly in all age groups, while the relaxation of the social distancing policy increased IEDSCs significantly, mostly in all groups.
Conclusion: In the post-COVID-19 era, we hope that national-level interventions such as reducing air pollution and employing precautionary measures will significantly reduce the financial burden of developing infectious ophthalmic diseases.
Introduction
In December 2019, pneumonia caused by a novel coronavirus was reported in Wuhan, China [1]. After the first case occurred, coronavirus disease 2019 (COVID-19) spread rapidly [2], and on 21 January 2020, the first confirmed case occurred in South Korea [3]. In the early stages of the pandemic, non-pharmaceutical interventions such as mask-wearing, hand hygiene, and social distancing were recommended because of the absence of vaccines and antiviral agents to control COVID-19 [4, 5]. In February 2020, after a super-spreader was validated (31st patient), the number of Korean COVID-19 cases was confirmed, and fatalities increased rapidly [6]. Therefore, the government implemented social distancing by the end of February 2020 to prevent the spread of COVID-19 [4]. Social distancing is a measure to mitigate the epidemic of infectious diseases so as to not exceed the capacity of medical institutions [7]. According to the WHO, “social distancing” is an intervention that maintains a physical distance between people and reduces the number of times people come in close contact to prevent the spread of contagious disease [8]. The measures undertaken include school closures and community isolation [8]. Furthermore, 70% of countries worldwide have implemented these social distancing measures [9]. In South Korea, along with personal-level public hygiene management such as ventilation, sterilization, mask-wearing, and personal hygiene management, social distancing was established by working from home and implementing closures of religious facilities, pubs, and schools [5]. After social distancing, public movement gradually declined [10] and the number of confirmed COVID-19 infections gradually decreased. As a result, the Korean government implemented a relaxed social distancing policy on 6 May 2020 [7]. Relaxed social distancing provides personal-level public health management according to detailed guidelines [11]. Social distancing reduces the incidence of COVID-19 and other diseases [5, 12–16]. Prior studies revealed that the social distancing policy has contributed to reducing paediatric infection by eliminating children’s interactions. These studies demonstrated the important association between non-pharmaceutical interventions and infectious disease transmission [5, 12–14]. Additionally, it has been confirmed that social distancing policies effectively slow the spread of viral respiratory diseases in children [15], and that Enterovirus and all-cause pneumonia decreased during COVID-19 [16].
Viral conjunctivitis is the most common type of infectious conjunctivitis and is caused by adenoviruses, enteroviruses, etc. There are no effective antiviral agents for treating viral conjunctivitis, and treatment for the disease has a supportive role in alleviating the symptoms [17–19]. However, research on infectious eye diseases is important because conjunctivitis may have negative effects on many people, resulting in economic and social burdens. In the United States, six million people are affected annually by conjunctivitis. Over $ 2 billion is spent annually on emergency room visits due to eye diseases, and approximately 28% of emergency room visits are due to conjunctivitis [17, 20]. The burden of illness due to infectious eye disease has gradually increased. Social distancing has reduced the number of patients with other infectious diseases as well as with infectious eye diseases. Therefore, this study aimed to investigate the effect of social distancing policies on the incidence of infectious eye diseases (IED) by monitoring their nationwide incidence data in all age groups.
Methods
Data
Infectious Eye Disease Suspected Case (IEDSC) data were obtained from the Infectious Disease Portal of the Korea Centers for Disease Control and Prevention (KCDC) [21]. The KCDC reports several infectious diseases on its website on a weekly basis. Reported infectious eye diseases include epidemic keratoconjunctivitis and acute haemorrhagic conjunctivitis. Suspected cases were defined as the number of patients with epidemic keratoconjunctivitis and acute haemorrhagic conjunctivitis in 80 sample-monitoring hospitals [21, 22]. These data were categorized by age (0–6 years, 7–19 years, 20 years or older) [21]. The study period started from the 1st week (1st week of January) in 2017 to the 35th week (4th week of August) in 2020.
In this study, to analyse the impact of COVID-19 policy on IEDSC, the time periods were divided into two interventions. The first intervention was a COVID-19 patient report in Korea on 19 January 2020. The second intervention was the relaxation of the social distancing policy on 6 May 2020. The Korean social distancing policy is an infectious disease management strategy that minimizes contact between individuals and groups to reduce the spread of infectious diseases [23]. It began on 22 March 2020 and was relaxed on 6 May 2020 [24].
Variables
The dependent variable in this study was the overall IEDSC (epidemic keratoconjunctivitis and acute haemorrhagic conjunctivitis) and IEDSC data categorized by age (0–6 years old, 7–19 years old, 20 years or older). Log transformation was performed. Month dummy variables were included as covariates to capture the monthly variations.
Statistical Analysis
Segmented regression analysis of the interrupted time series was used to assess COVID-19 policies on the IEDSC. Segmented regression is a quasi-experimental analysis used to evaluate policy interventions [25]. The regression model is as follows:
• Yt: IEDSC per 1,000 outpatient visits
• timet: basic trend (continuous, unit: week)
• time after intervention 1t: the period from week 3 of January 2020; first patient incidence of COVID-19 (continuous, unit: week)
• Intervention 2t: week 1 of May 2020; the relaxing of social distancing policy (0, 1)
• time after intervention 1-2t: the period after intervention 2 (continuous, unit: week)
• month 1–month 11: indicators for monthly seasonality (0, 1)
•
The time variables present a basic trend and provide a continuous weekly value (1–191 weeks). The time variable was the baseline trend variable. The time after intervention 1 was 0 before the first incidence of COVID-19 and increased from 1 after. The time after intervention 2 was 0 before week 1 of May 2020 and increased from 1 after the social distancing policy was relaxed.
Since there are many intervention variables related to time, interpretation of the segmented regression analysis is difficult. Therefore, we calculated the relative reduction and marginal effects of the dependent variables. The relative reduction was estimated by comparing the IEDSC of 2020 with the average IEDSC of 2017–2019. The marginal effects of COVID-19 incidence in the 4th week of August 2020, compared to the 3rd week of January 2020, were calculated using the formula
Results
Figure 1 shows the time trends of outpatients per 1,000 for each age group of the IEDSC. According to the overall trend, the number of patients increased rapidly in summer, exhibiting seasonal characteristics. We observed that this trend decreased in spring and winter. The first incidence of COVID-19 in a patient was on 19 January 2020, showed that the weekly IEDSC rate was below 20. In addition, the relaxation of the social distancing policy showed that the number of weekly IEDSC had gradually increased.

FIGURE 1. Total incidence of infectious eye disease suspected case and subgroup time trends (South Korea, 2017–2020).
An interrupted time-series analysis was performed to check the effect of the two events related to COVID-19 (Table 1). Monthly seasonal effects were significant in all age groups and IEDSC diseases. After the first COVID-19 patient incidence, IEDSCs decreased significantly in all age groups and in all diseases. Relaxing the social distancing policy significantly increased IEDSCs, mostly in all groups.

TABLE 1. Interrupted time series analysis to identify the effect of coronavirus disease 2019 on the incidence of infectious eye disease suspected case (South Korea, 2017–2020).
Figure 2 shows a comparison between the prediction and actual values of our analysis model. The predicted values were accurately estimated (overall R2 = 0.86).

FIGURE 2. Total incidence of infectious eye disease suspected case actual data and adjusted mean data’s time trends (South Korea, 2017–2020).
Regarding the changes in IEDSC rate in 2020 compared to changes in 2017–2019, the estimated average reduction in total IEDSC rate was 62.3% (Figure 3). The IEDSC rate in the age group 0–6 was reduced by 74.7% on average. The average reduction was 62.3%, 53.6%, and 59.7% in the age 7–19, age ≥20, and epidemic keratoconjunctivitis groups, respectively. Acute haemorrhagic conjunctivitis did not decrease significantly, with an average reduction rate of 20.4%.

FIGURE 3. Weekly infectious eye disease suspected case incidence rate for all causes by age group and infection groups (South Korea, 2017–2020).
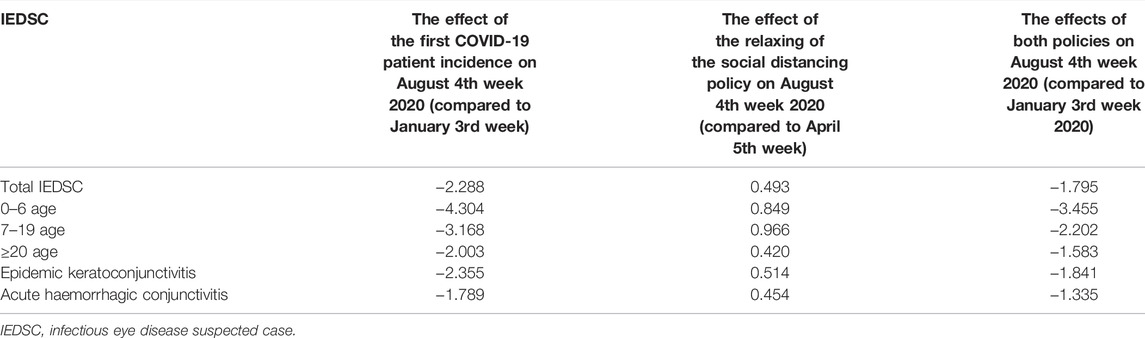
Table 2 presents the marginal effects of the dependent variables. The first COVID-19 patient incidence decreased the IEDSC, and later increased due to the effect caused by the relaxation of the social distancing policy. Considering the effects of these two events, the IEDSC in all groups decreased.
Discussion
Key Findings
The current study used the KCDC’s nationwide infectious disease incidence monitoring data to investigate the impact of the social distancing policy implemented in the COVID-19 fundamental response strategy on IEDSC incidence in all age groups. Although a seasonal epidemic showed an increase in all IEDSCs from spring to summer in 2018–2019, the number of IEDSCs rapidly decreased in spring 2020 after implementing the social distancing policy and slightly increased in summer after the relaxing of the social distancing policy. This finding showed that social distancing effectively reduced the number of IED patients in all age groups.
Interpretation
Most infections of viral conjunctivitis are transmitted by direct contact via contaminated fingers, swimming pool water, or infected patients in hospitals, kindergartens, and schools. Good hand hygiene and isolation from the infected patients are recommended to prevent the spread of acute viral conjunctivitis [17, 18]. The implementation of social distancing policy may prevent people from contacting IED patients or visiting public places such as swimming pools and hospitals; other public health interventions such as hand hygiene combined with social distancing policy may create a synergistic effect to decrease the number of IED patients [4, 17, 18]. Furthermore, postponing the start of kindergarten and school closures from February–March 2020 may also be helpful in preventing transmission of infectious conjunctivitis, especially childhood conjunctivitis [18, 26]. A previous study confirmed that social distancing at schools and daycare centre closures would substantially eliminate contact between children, significantly reducing multiple communicable diseases [10]. The rapid increase in the number of IED patients between 0 and 6 years after ending the social distancing policy, as observed in this study, also supports the relationship between social distancing and childhood conjunctivitis. Therefore, the study findings strengthen the evidence linking the implementation of social distancing policies to a decrease in the risk of acute conjunctivitis.
However, there are concerns regarding the interpretation of the findings in this study. Previous research has reported that an increase in particulate matter exposure, such as PM10 and PM2.5 was associated with an increased risk of acute conjunctivitis in Singapore and China [27, 28]. According to a report on air quality in South Korea, air pollution, especially with PM10 and PM2.5, in February–May 2020 was lower than the air pollution of the same month in 2017–2019; while the air pollution in June 2020 was similar to that of the same month in 2017–2019 [29]. This was observed because social distancing policies may have suppressed social activities and reduced traffic, which led to decreased air pollutant concentrations, especially in urban areas. China has also reduced industrial activities and travel, closed schools, and established numerous quarantine stations to reduce the spread of the illness after the outbreak of COVID-19 [30]. As a result, it was confirmed that the concentration of NO2 (nitrogen dioxide) in fossil fuels in February 2020 was lower than that in February 2019, and air pollution was reduced [31]. The trend of air pollution may also influence the incidence of IED outpatients; therefore, further research should include air pollution as a risk factor. As another concern, a systematic review reported that conjunctivitis can be a symptom of COVID-19 [32]. A thorough differential diagnosis of the virus is necessary for infected conjunctivitis because the possibility of viral infection due to COVID-19 should not be ruled out.
In general, most cases of keratoconjunctivitis and acute haemorrhagic conjunctivitis occur in summer, around July–September [33, 34]. Interestingly, in this study, social distancing showed substantial and consistent efficacy in suppressing the transmission of keratoconjunctivitis compared with that of acute haemorrhagic conjunctivitis. Furthermore, the number of keratoconjunctivitis outpatients rapidly increased compared to that of acute haemorrhagic conjunctivitis outpatients after relaxing the social distancing policy. This difference in the number of keratoconjunctivitis and acute haemorrhagic conjunctivitis outpatients may be because keratoconjunctivitis is majorly caused by adenovirus, while acute haemorrhagic conjunctivitis is majorly caused by enterovirus [17–19]. Previous research has shown that keratoconjunctivitis may be affected by humidity, rainfall, and wind speed rather than by temperature [35]. In 2020, the weather in South Korea showed the longest rainy season with high humidity and torrential downpours from the end of June to mid-August [36]. Therefore, environmental factors should be considered in further research to investigate the patterns of the number of keratoconjunctivitis and acute haemorrhagic conjunctivitis outpatients.
Strengths and Limitations
This study investigated the impact of social distancing policies on the number of IED patients. The study findings provide evidence that appropriate social distancing can prevent the transmission of IED, especially in children and adolescents. This study had some limitations. First, this study included only viral conjunctivitis and did not include other common types of conjunctivitis, such as those of bacterial and allergenic origin. Therefore, the results cannot be generalized to individuals with other types of conjunctivitis. Second, this study did not adjust for the effects of air quality and region (urban versus country) as a risk factor for the number of IED patients, which limits the interpretation of the findings.
Conclusion
In this study, the COVID-19 public health response and social distancing policy were found to have an indirect impact on the development of IED among children and adolescents. As a result, post-COVID-19 period also needs maintenance of personal hygiene measures, such as hand hygiene after coughing. In addition, we hope that national-level interventions such as reducing air pollution, along with the precautionary measures will significantly reduce the financial burden of developing infectious ophthalmic diseases.
Ethics Statement
The studies involving human participants were reviewed and approved by the Yonsei University Wonju Institutional Review Board. Written informed consent from the participants’ legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author Contributions
Methodology: W-RL, L-HK, K-BY, and J-WN; literature review: W-RL, L-HK, G-ML, JC, YK, J-WN, and K-BY; formal analysis: W-RL, L-HK, and K-BY; resources: K-BY; first draft preparation of the manuscript: W-RL, L-HK, G-ML, JC, YK, J-WN, and K-BY; review and editing of the manuscript: W-RL, L-HK, G-ML, JC, YK, J-WN, and K-BY.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Zhu, N, Zhang, D, Wang, W, Li, X, Yang, B, Song, J, et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med (2020) 382:727–33. doi:10.1056/NEJMoa2001017
2. Shen, J, Wu, J, Yang, Y, Wang, P, Luo, T, Guo, Y, et al. The Paradoxical Problem with COVID-19 Ocular Infection: Moderate Clinical Manifestation and Potential Infection Risk. Comput Struct Biotechnol J (2021) 19:1063–71. doi:10.1016/j.csbj.2021.01.039
3.COVID-19 National Emergency Response Center. Epidemiology and Case Management Team, Korea Centers for Disease Control and Prevention. Coronavirus Disease-19: The First 7,755 Cases in the Republic of Korea. Osong Public Health Res Perspect (2020) 11(2):85–90. doi:10.24171/j.phrp.2020.11.3.09
4. Jang, WM, Jang, DH, and Lee, JY. Social Distancing and Transmission-Reducing Practices during the 2019 Coronavirus Disease and 2015 Middle East Respiratory Syndrome Coronavirus Outbreaks in Korea. J Korean Med Sci (2020) 35:e220. doi:10.3346/jkms.2020.35.e220
5. Choe, YJ, and Lee, J-K. The Impact of Social Distancing on the Transmission of Influenza Virus, South Korea. Osong Public Health Res Perspect (2020) 11:91–2. doi:10.24171/j.phrp.2020.11.3.07
6. Shim, E, Tariq, A, Choi, W, Lee, Y, and Chowell, G. Transmission Potential and Severity of COVID-19 in South Korea. Int J Infect Dis (2020) 93:339–44. doi:10.1016/j.ijid.2020.03.031
7. Park, I-N, and Yum, HK. Stepwise Strategy of Social Distancing in Korea. J Korean Med Sci (2020) 35:e264. doi:10.3346/jkms.2020.35.e264
8.Risk communication and community engagement guidance for physical and social distancing. World Health Organization (2020). Available online: https://www.afro.who.int/sites/default/files/Covid-19/Techinical%20documents/Risk%20Communication%20and%20Community%20Engagement%20Guidance%20for%20Physical%20and%20Social%20Distancing.pdf (Accessed September 28, 2022).
9. Castex, G, Dechter, E, and Lorca, M. COVID-19: The Impact of Social Distancing Policies, Cross-Country Analysis. Econ Di Scli Cha (2021) 5(1):135–59. doi:10.1007/s41885-020-00076-x
10.Coronavirus infectious disease-19 Central Disaster and Safety Headquarters Regular Briefing. Korea Centers for Disease Control and Prevention (2020). Available online: http://ncov.mohw.go.kr/tcmBoardView.do?contSeq=353917 (Accessed April 4, 2020).
11.Coronavirus Infectious Disease-19 Central Disaster and Safety Headquarters Press Release. Ministry of Health and Welfare (2020). Available online: http://ncov.mohw.go.kr/upload/140/202005/1588499802355_20200503185642.pdf (Accessed May 3, 2020).
12. Hatoun, J, Correa, ET, Donahue, SMA, and Vernacchio, L. Social Distancing for COVID-19 and Diagnoses of Other Infectious Diseases in Children. Pediatrics (2020) 146:e2020006460. doi:10.1542/peds.2020-006460
13. McBride, DL. Social Distancing for COVID-19 Decreased Infectious Diseases in Children. J Pediatr Nurs (2021) 58:100. doi:10.1016/j.pedn.2021.02.018
14. Todd, IM, Miller, JE, Rowe, SL, Burgner, DP, and Sullivan, SG. Changes in Infection-Related Hospitalizations in Children Following Pandemic Restrictions: an Interrupted Time-Series Analysis of Total Population Data. Int J Epidemiol (2021) 50:1435–43. doi:10.1093/ije/dyab101
15. Kuitunen, I, Artama, M, Mäkelä, L, Backman, K, Heiskanen-Kosma, T, and Renko, M. Effect of Social Distancing Due to the COVID-19 Pandemic on the Incidence of Viral Respiratory Tract Infections in Children in Finland during Early 2020. Pediatr Infect Dis J (2020) 39(12):e423–e427. doi:10.1097/INF.0000000000002845
16. Chiu, NC, Chi, H, Tai, YL, Peng, CC, Tseng, CY, Chen, CC, et al. Impact of Wearing Masks, Hand hygiene, and Social Distancing on Influenza, Enterovirus, and All-Cause Pneumonia during the Coronavirus Pandemic: Retrospective National Epidemiological Surveillance Study. J Med Internet Res (2020) 22(8):e21257. doi:10.2196/21257
17. Azari, AA, and Barney, NP. Conjunctivitis: a Systematic Review of Diagnosis and Treatment. JAMA (2013) 310:1721–30. doi:10.1001/jama.2013.280318
18. Oh, JJ, and Rho, CR. Causes of Epidemic Keratoconjunctivitis and Therapeutic Measures. J Korean Med Assoc (2017) 60:491–6. doi:10.5124/jkma.2017.60.6.491
19. Zhang, L, Zhao, N, Sha, J, Wang, C, Jin, X, Amer, S, et al. Virology and Epidemiology Analyses of Global Adenovirus-Associated Conjunctivitis Outbreaks. Epidemiol Infect (1953–20132016) 144:1661–72. doi:10.1017/S0950268815003246
20. Channa, R, Zafar, SN, Canner, JK, Haring, RS, Schneider, EB, and Friedman, DS. Epidemiology of Eye-Related Emergency Department Visits. JAMA Ophthalmol (2016) 134:312–9. doi:10.1001/jamaophthalmol.2015.5778
21.Infectious Disease Portal. Korea Centers for Disease Control and Prevention (2022). Available online: https://www.kdca.go.kr/npt/biz/npp/iss/eyeDisordersStatisticsMain.do (Accessed September 6, 2020).
22.Infectious Disease Monitoring System. Korea Centers for Disease Control and Prevention (2022). Available online: http://www.cdc.go.kr/contents.es?mid=a20301110300 (Accessed September 6, 2020).
23.Coronavirus Infectious Disease-19 Central Disaster and Safety Headquarters Regular Briefing. Korea Centers for Disease Control and Prevention (2020). Available online: http://ncov.mohw.go.kr/tcmBoardView.do?contSeq=360602 (Accessed November 1, 2020).
24. Kim, S, Ko, Y, Kim, Y-J, and Jung, E. The Impact of Social Distancing and Public Behavior Changes on COVID-19 Transmission Dynamics in the Republic of Korea. PLoS One (2020) 15:e0238684. doi:10.1371/journal.pone.0238684
25. Wagner, AK, Soumerai, SB, Zhang, F, and Ross‐Degnan, D. Segmented Regression Analysis of Interrupted Time Series Studies in Medication Use Research. J Clin Pharm Ther (2002) 27:299–309. doi:10.1046/j.1365-2710.2002.00430.x
26.Coronavirus Infectious Disease-19 Central Accident Management Headquarters Regular Briefing. Korea Centers for Disease Control and Prevention (2020). Available online: http://ncov.mohw.go.kr/tcmBoardView.do?contSeq=353081 (Accessed February 24, 2020).
27. Aik, J, Chua, R, Jamali, N, and Chee, E. The burden of Acute Conjunctivitis Attributable to Ambient Particulate Matter Pollution in Singapore and its Exacerbation during South-East Asian Haze Episodes. Sci Total Environ (2020) 740:140129. doi:10.1016/j.scitotenv.2020.140129
28. Chen, R, Yang, J, Chen, D, Liu, W, Zhang, C, Wang, H, et al. Air Pollution and Hospital Outpatient Visits for Conjunctivitis: a Time-Series Analysis in Tai’an, China. Environ Sci Pollut Res Int (2021) 28:15453–61. doi:10.1007/s11356-020-11762-4
29.Korean Environment Corporation. Annual Air Quality Trends. Incheon: National Institute of Environmental Research (2022). Available online: https://www.airkorea.or.kr/web/detailViewDown?pMENU_NO=125 (Accessed September 6, 2020).
30. Wilder-Smith, A, and Freedman, DO. Isolation, Quarantine, Social Distancing and Community Containment: Pivotal Role for Old-Style Public Health Measures in the Novel Coronavirus (2019-nCoV) Outbreak. J Trav Med (2020) 27:taaa020. doi:10.1093/jtm/taaa020
31. He, L, Zhang, S, Hu, J, Li, Z, Zheng, X, Cao, Y, et al. On-road Emission Measurements of Reactive Nitrogen Compounds from Heavy-Duty Diesel Trucks in China. Environ Pollut (2020) 262:114280. doi:10.1016/j.envpol.2020.114280
32. Jin, Y-P, Trope, GE, El-Defrawy, S, Liu, EY, and Buys, YM. Ophthalmology-focused Publications and Findings on COVID-19: A Systematic Review. Eur J Ophthalmol (2021) 31:1677–87. doi:10.1177/1120672121992949
33. Min-Hye Lee, OP, Park, H-K, Lee, E-G, and Chun, B-C. The Epidemic Characteristics of Epidemic Keratoconjunctivitis and Acute Haemorrhagic Conjunctivitis in Korea during 2004-2007. Korean Public Health Resear (2009) 35:39–51. doi:10.22900/kphr.2009.35.2.005
34. Lee, J, Bilonick, RA, Romanowski, EG, and Kowalski, RP. Seasonal Variation in Human Adenovirus Conjunctivitis: A 30-year Observational Study. Ophthalmic Epidemiol (2018) 25:451–6. doi:10.1080/09286586.2018.1509096
35. Das, AV, and Basu, S. Epidemic Keratoconjunctivitis in India: Trend Analysis and Implications for Viral Outbreaks. Indian J Ophthalmol (2020) 68:732–6. doi:10.4103/ijo.IJO_626_20
36.Policy briefing in Korea: press release. Korea Meteorological Administration (2020). Available online: https://www.korea.kr/news/pressReleaseView.do?newsId=156410037#sitemap-layer (Accessed September 9, 2020).
Keywords: COVID-19, social distancing, interrupted time series, infectious eye disease, segmented regression, nationwide infectious disease incidence monitoring data
Citation: Lee W-R, Kim L-H, Lee G-M, Cheon J, Kwon YD, Noh J-W and Yoo K-B (2022) Effect of COVID-19-Related Interventions on the Incidence of Infectious Eye Diseases: Analysis of Nationwide Infectious Disease Incidence Monitoring Data. Int J Public Health 67:1605211. doi: 10.3389/ijph.2022.1605211
Received: 13 July 2022; Accepted: 11 October 2022;
Published: 20 October 2022.
Edited by:
Nino Kuenzli, Swiss Tropical and Public Health Institute (Swiss TPH), SwitzerlandReviewed by:
Yi-Lin Tsai, Stanford University, United StatesCopyright © 2022 Lee, Kim, Lee, Cheon, Kwon, Noh and Yoo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jin-Won Noh, amlud29uLm5vaEBnbWFpbC5jb20=; Ki-Bong Yoo, eWtib25nQHlvbnNlaS5hYy5rcg==
†These authors have contributed equally to this work
This Original Article is part of the IJPH Special Issue “Health in all Sustainable Development Goals”
 Woo-Ri Lee
Woo-Ri Lee Li-Hyun Kim2†
Li-Hyun Kim2†