Abstract
Objectives: Although the evidence from numerous longitudinal studies has indicated a remarkable change in cognitive function (CF) and depressive symptoms (DS) over time, the parallel latent growth curve model (LGCM) has seldom been used to simultaneously investigate the relationship between their change trajectories. This study aimed to examine whether a change in DS was associated with CF over time using an LGCM.
Methods: Data were collected from the Chinese Longitudinal Healthy Longevity Survey’s 2011, 2014, and 2018 waves. A parallel LGCM examined the association between CF and DS.
Results: The multivariate conditioned model’s goodness of fit supported the validity of the longitudinal model (Tucker-Lewis index [TLI] = 0.90, comparative fit index [CFI] = 0.96, root mean square error of approximation [RMSEA] = 0.04). The results showed that the CF intercept was positively to the DS slope (β = 0.42, p = 0.004). The CF and DS slopes were significantly linked (β = −0.65, p = 0.002).
Conclusion: The findings expand the knowledge about CF’s effect on DS in older adults.
Introduction
Depressive symptoms (DS) and cognitive function (CF) impairment are globally recognized as the most common mental disorders in older adults [1, 2]. A chronic unhealthy mental state caused by depression or lack of interest in external stimuli causes significant disturbance to older adults’ lives and leads to adverse health outcomes, such as mortality, chronic disease incidence rate, economic burden, functional disability, and decline in quality of life (QOL) [1,3,4]. The prevention and treatment of depressive symptoms are crucial for older adults [5]. Cognitive impairment is often manifested as the impairment of one or more abilities related to perception, attention, memory, and thinking [6]. Over 46 million older adults suffer from cognitive impairment, which imposes a heavy burden on families and society [7,8]. Moreover, the cumulative dementia incidence rate is 14.9% in older adults with mild cognitive impairment aged above 65 years [9]. Exploring the different development trajectories and influencing factors of older adults’ cognitive function and depressive symptoms can guide targeted intervention measures to decelerate the decline of cognitive impairment and reduce depressive symptoms.
Most of the extant studies have used cross-sectional surveys to explore the correlation between depressive symptoms and cognitive impairment, with inconclusive results [10]. Some studies have associated the presence of depressive symptoms with cognitive decline or dementia [11, 12], some have found that the effect of depression on one cognitive ability (i.e., processing speed) has an additional effect on other cognitive abilities that interfere with everyday problem-solving [13,14], and some have found no correlation between these variables [15,16]. These inconsistent results have mostly been reported in studies that have concentrated on a single assessment (mostly at the baseline) of depressive symptoms and cognitive function decline. Considering that depressive symptoms tend to fluctuate over time, these studies have failed to fully capture the continuous impact of cognitive decline on these symptoms, thus limiting the understanding of the condition.
To the best of this study’s knowledge, only a few longitudinal studies have examined the relationship between cognitive function and depressive symptoms, and most have focused on the longitudinal effects of depressive symptoms on cognitive function [17,18]. For example, a longitudinal study with fewer than 400 participants purported an association between cognitive function and depressive symptoms in older adults [19] which limited the results’ universality. One study has suggested that there is no evidence of a relationship between cognitive function and depressive symptoms [20], while another has suggested a negative correlation between the two [21,22]. Moreover, some studies have examined the association between baseline depressive symptoms and incidental cognitive impairment [23–25] rather than a correlation among their trajectories. Others have evaluated cognitive function and depressive symptoms by repeatedly using cross-lag panel analysis, which has more application value in a two-way relationship; however, each result was exposed before the follow-up period, which did not exceed 3 years [19]. Understanding the changing trends of cognitive impairment and depressive symptoms could be improved by performing long-term follow-ups and repeated evaluations to further confirm their relationship. However, the longitudinal effects of cognitive function on depressive symptoms have not been fully investigated.
To further clarify whether cognitive function and other covariates impact depressive symptoms and to provide guidance for depression prevention measures, this study uses a latent growth curve model (LGCM) to analyze large longitudinal sample data for up to 7 years. An LGCM is an advanced analytical method that can create random intercepts and slopes to depict different trajectories over time [26]. It can also allow for the simultaneous estimation of individual and group variation and can be used to model aspects of change, describe a single individual trajectory, and capture individual differences in a trajectory over time [27].
To test whether cognitive function and other covariates are predictive of depressive symptoms development, this study uses an LGCM model based on three waves of the Chinese Longitudinal Healthy Longevity Study (CLHLS) data. The previous cognitive function- and depressive symptoms-related research on older adults has explored the following factors: exercise [28], sex [29], marital status [30], education [31,32], living conditions [33], and chronic diseases [34]. Therefore, this study examines whether these covariates confound the association, and their effect on the cognitive function and depressive symptoms trajectories.
Methods
Study Design and Participants
The study data were from the CLHLS, a large national survey of the Chinese population over the age of 65. Three waves of the CLHLS were used: 2011 (T1), 2014 (T2), and 2018 (T3). The samples were randomly selected from 22 of the 31 Chinese provinces (representing 85% of China’s total population) so as to provide a nationally representative study of older Chinese adults. The study conducted eight rounds of surveys in 1998, 2000, 2002, 2005, 2008, 2011, 2014, and 2018 [35]. During the surveys, face-to-face communication was conducted to collect information on the depressive symptoms and cognitive function of older adults. All investigators were subjected to unified training before starting the investigation to act as investigators when qualified. The CLHLS is an ongoing project, and a variety of mechanisms are in place to ensure the quality of the CLHLS data. Details regarding the sampling design and data quality mechanisms can be found elsewhere [36]. Informed consent was obtained from each respondent during the surveys [37]. After accounting for the dropouts and death of the older adults in the three waves, the samples comprised of 9765 participants in 2011, 7192 participants in 2014, and 15,874 participants in 2018. To merge the longitudinal data from the three waves, this study filtered for missing values, outliers, and the identity code (ID) was the only matching condition. This study gathered the data from the three waves to finally obtain a sample of 2454 participants who had participated in the CLHLS surveys (i.e., in 2011, 2014, and 2018), of which 1262 had provided valid questionnaires (i.e., they had participated in the three surveys and had answered the depressive symptoms and cognitive function scales completely). Missing values were imputed using multiple imputation. The included and excluded participants significantly differed in terms of sex, age, and chronic disease. The excluded participants (i.e., those who did not complete the depressive symptoms and cognitive function scales) were, on average, older (p < 0.001), female (p < 0.001), and had more chronic diseases (p < 0.001). Unsurprisingly, the included participants were younger and healthier when compared to the excluded participants, given the need to fulfill at least three waves of data collection spanning 7 years.
Measures
Depressive Symptoms
The CLHLS uses a five-item scale that assesses depressive symptoms in older adults; this scale has often been used to indicate depressive symptoms [2, 38–40]. Regarding the five items, the first two and last three items indicate positive and negative emotions, respectively. Positive items include “Do you see the bright side of things?” and “Do you feel the same level of happiness now as to when you were young?” Negative items include “Is anxiety a frequent occurrence for you?,” “Is it common for you to feel lonely and isolated?,” and “Is it true that the older you get, the less useful you seem to be?” To ensure measurement consistency, this study inversely assigned the two positive items as negative scores. The item responses were “Always,” “Often,” “Sometimes,” “Seldom,” and “Never,” and the scores ranged from 1–5, with a higher score indicating greater negativity. Therefore, this study calculated that the scores ranged from 5 to 25, with higher scores indicating more severe depressive symptoms. The Cronbach’s α coefficients of the three survey waves (2011, 2014, and 2018) were 0.66, 0.70, and 0.66, respectively, which were above the acceptable value of 0.6 [41]. The principle component analysis generated one factor with eigenvalues of ≥1, thus explaining 44.5% of the total variance [2].
Cognitive Function
Cognitive function was assessed using the Chinese version of the Mini-Mental State Examination (CMMSE). The scale has good reliability and validity in the general population [42]. The sensitivity of the CMMSE is 95.9% and the specificity is 96.4%, which are both above 95% [43]; thus, the CMMSE is sensitive to changes over time in the older adult population. The CMMSE scale contains 24 questions on 5 dimensions: Orientation, language, recall, attention, and calculating ability. One point was allocated for a correct answer and zero points were allocated for incorrect answers, except for one question (“Please name as many kinds of food as possible in 1 min”; one point was given for each food named and seven points were given for those who named seven or more foods). The CMMSE scores ranged from 0 to 30, with higher scores denoting better cognitive function. The Cronbach’s α coefficients of the three survey waves (2011, 2014, and 2018) were 0.72, 0.72, and 0.81, respectively.
Covariates
The covariates included personal physical factors (exercise), demographic factors (sex, marital status, and education), living conditions, and chronic diseases. All variables were measured during the first assessment (T1) and were regarded as covariates of the cognitive function and depressive symptoms intercept and slope factors, thus allowing for the examination of the effects of each covariate while controlling for all others. Males and females were coded as one and zero, respectively. Exercise was coded as one; no exercise was coded as zero. Regarding marital status, those who were divorced, widowed, and never married were coded as zero (i.e., no spouse); living with a spouse was coded as one (i.e., spouse). In the surveys, the question, “How many years did you go to school for?” was a continuous variable. Years of education was selected to reflect the education level of older adults, and was included in the model analysis. Regarding living conditions, those who lived alone or in nursing institutions were coded as zero (i.e., not living with family); living with family was coded as one. Chronic physical disease was regarded as a time-varying covariate and included hypertension, diabetes, heart disease, stroke, bronchitis, tuberculosis, cataracts, glaucoma, cancer, gastric or duodenal ulcer, Parkinson’s disease, bedsore, arthritis, and dementia. Chronic physical diseases were grouped as zero (i.e., no chronic disease), one (i.e., one chronic disease), and two (i.e., more than two chronic diseases).
Data Analysis
This study used SPSS 25.0 and MPlus 8.1 software to build the LGCM. It defined the structure of two latent variables: the baseline level (intercept) and the change rate (slope). The mean intercept reflected the average of the individual baseline levels and the intercept variation reflected their heterogeneity. The synonymous slope mean reflected the overall change rate and the slope variation reflected the individual differences. This study evaluated the linear trajectory as the overall sample and discussed the potential influencing factors to analyze the individual differences between the baseline level of cognitive function, the potential factors of depressive symptoms, and the relationship between them, as well as the change rate over time [44]. This study estimated the linear variation between cognitive function and depressive symptoms to determine the degree of model fit. This study adopted the intercept and slope of cognitive function and depressive symptoms to evaluate the structural correlation between the two variables.
This study presented the participants’ characteristics, including cognitive function scores, depressive symptoms scores, and covariate distributions or scores, as descriptive statistics. The partial missing values of other covariates were interpolated by multiple interpolations [45]. Since the chi-square statistic is sensitive to sample size, this study assessed the model’s goodness of fit using the comparative fit index (CFI >0.90), Tucker-Lewis index (TLI >0.90), and root mean square error of approximation index (RMSEA <0.08) [46].
Results
Participants’ Characteristics
This study included 1,262 participants (661 males, 601 females). Overall, 41.5%, 29.3%, and 29.2% of the participants had never received an education, received an education for 5 years, and received an education for 6 years or more, respectively. Table 1 presents the other sample characteristics.
TABLE 1
| Variables | n | % |
|---|---|---|
| Sex | ||
| Male | 661 | 52.4 |
| Female | 601 | 47.6 |
| Exercise | ||
| Yes | 467 | 37.0 |
| No | 795 | 63.0 |
| Marital status | ||
| Having a spouse | 853 | 67.6 |
| No spouse | 409 | 32.4 |
| Education | ||
| 0 | 524 | 41.5 |
| 1–5 | 370 | 29.3 |
| >5 | 368 | 29.2 |
| living condition | ||
| Living with the family | 1085 | 86.0 |
| Not living with the family | 177 | 14.0 |
Sample characteristics (Chinese Longitudinal Health Longevity Survey, China, 2011–2018).
Change Trend of Depressive Symptoms
The nonlinear curve model of depressive symptoms could not be fitted, so the linear model was chosen. Tables 2, 3 show the change trend of depressive symptoms in the time and unconditional linear models, respectively. The results demonstrate that depressive symptoms increases from the first to the third wave, and the index indicates a good model fit. The intercept (baseline) mean of depressive symptoms is 10.53 (p < 0.001), and its average slope is 0.06 (p < 0.001), indicating that older adults’ depressive symptoms show a linear upward trend first to the third wave. The variations in intercept and slope are 3.89 (p < 0.001) and 0.06 (p = 0.025), respectively, indicating significant individual differences in the baseline of depressive symptoms level and change rate of older adults.
TABLE 2
| Variable | Time 1 | Time 2 | Time 3 | |||
|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | |
| Depressive Symptoms | 10.53 | (3.21) | 10.71 | (3.26) | 10.98 | (3.16) |
| Cognitive function | 27.93 | (2.76) | 27.81 | (2.69) | 27.03 | (3.56) |
Mean and standard deviation by each variable (Chinese Longitudinal Health Longevity Survey, China, 2011–2018).
TABLE 3
| Variable | 2(df) | TLI | CFI | RMSEA | Intercept | Slope | ||
|---|---|---|---|---|---|---|---|---|
| Mean | Variance | Mean | Variance | |||||
| Depressive Symptoms | 0.02(1) | 1.00 | 1.00 | 0.00 | 10.53 | 3.89 | 0.06 | 0.06 |
| Cognitive function | 11.64(1) | 0.91 | 0.97 | 0.09 | 28.05 | 1.965 | −0.13 | 0.03 |
| Multivariate linearity LGM | 64.61(24) | 0.90 | 0.96 | 0.04 | ||||
Results of each variable’s model suitability (Chinese Longitudinal Health Longevity Survey, China, 2011–2018).
Change Trend of Cognitive Function
The nonlinear curve model of cognitive function could not be fitted, so the linear model was chosen. Tables 2, 3 show the change trend of cognitive function in the time and unconditional linear models, respectively. The results indicate that older adults’ cognitive function shows a declining trend during the 7-year observation period, and is more significant in the second and third waves. In the linear unconditional model, only the RMSEA value is slightly higher, and the other fitting indexes are good. The intercept (baseline) mean of cognitive function is 28.05 (p < 0.001). The average slope of cognitive function is −0.13 (p < 0.001), indicating that older adults’ cognitive function shows a linear downward trend during the 7-year observation period. A variation of 1.97 is shown between the intercept and slope, at (p < 0.001) and 0.03 (p > 0.05), respectively, indicating significant individual differences in the baseline cognitive function level and change rate of older adults. but the change in cognition speed is generally consistent.
How do Cognitive Function and Covariates Longitudinally Affect Older Adults’ Depressive Symptoms?
This study used the LGCM to examine whether depressive symptoms changed over time as a result of cognitive function. All covariates were simultaneously entered into the model to allow for an examination of each covariate’s effect while controlling for all other covariates. In Table 3, all indices indicate that the final model fits well. The TLI, CFI, and RMSEA of the acceptable model are 0.90, 0.96, and 0.04, respectively. The final model indicates that the cognitive function intercept affects the depressive symptoms intercept (β = −0.42, p < 0.001) and slope (β = 0.42, p = 0.004). That is, the higher the baseline level of cognitive function, the lower the baseline level of depressive symptoms, and the faster the upward trend of depressive symptoms. There is a significant negative correlation between the cognitive function and depressive symptoms slope (β = −0.65, p = 0.002). Therefore, the faster the cognitive function decline, the faster the upward trend of depressive symptoms.
In Figure 1, the covariates show that sex has a significant impact on the intercept of the cognitive function trajectory (β = −0.15, p = 0.003), indicating that the baseline level of older adult female’s cognitive function is worse than that of older adult males. The depressive symptoms intercept and cognitive function slope are unaffected by sex. There is a positive correlation between education, the cognitive function intercept and slope (β = 0.37, p < 0.001; β = 0.17, p = 0.022), and the depressive symptoms intercept (β = −0.19, p = 0.003). Thus, the higher the education level, the better the cognitive function change rate, and the lower the baseline level of depressive symptoms. The cognitive function change rate is affected by education level. Thus, higher education levels are associated with faster cognitive function decline change rates. There is a positive correlation between exercise and the cognitive function intercept (β = 0.11, p < 0.021), but a negative correlation between exercise and the cognitive function slope (β = −0.17, p = 0.016). This suggests that older adults who exercise regularly have a higher baseline cognitive function level and a slower rate of cognitive function decline. Marital status, chronic diseases and living conditions do not affect the depressive symptoms and cognitive function trajectories.
FIGURE 1
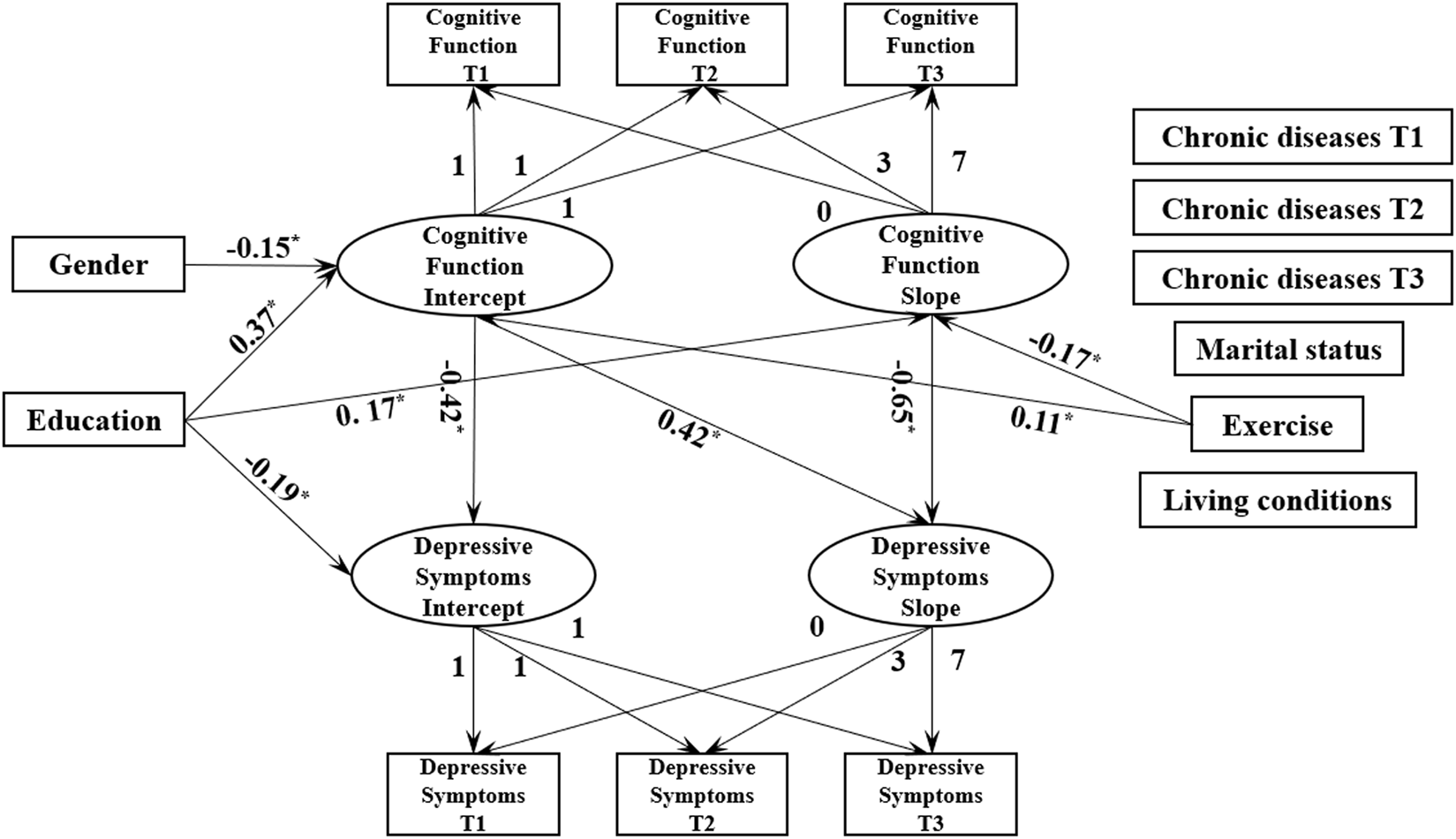
Multivariate linearity Latent Growth Curve Model (Chinese Longitudinal Health Longevity Survey, China, 2011–2018).
Discussion
This study used an LGCM to model aspects of change in the longitudinal trajectories of cognitive function and depressive symptoms, so as to describe individual trajectories and capture individual differences over time. The overall research framework included depressive symptoms, cognitive function, and the covariates to analyze the influencing characteristics of cognitive function and the covariates on depressive symptoms in older adults. Analyzing the relationship between cognitive function, depressive symptoms, and the covariates can remedy the lack of extant literature and provide important evidence. This study shows that older adults’ cognitive function can influence their development of depressive symptoms, to some extent, and the longitudinal results confirm the findings of previous cross-sectional analyses [47].
Longitudinal Trajectories of Depressive Symptoms and Cognitive Function in Older Adults
This study reveals that older adults’ depressive symptoms increase linearly. When older adults enter advanced age, their organ function deteriorates, various chronic diseases follow, and economic burden increases. Hence, the emergence of disease expedites the reduction in older adults’ QOL and their feeling of missing the sense of novelty toward life [48]. The superposition of various problems also triggers an increase in the depression level in older adults. This study’s finding that older adults’ cognitive function decrease linearly is consistent with the previous studies that have suggested that the cognitive function of older adults will dramatically decline after the age of 60 [49]. A major risk factor for cognitive function decline is aging, which could be related to the decrease in brain function caused by advanced age and brain atrophy over time. A previous study has suggested that cognitive decline may be associated with the volume of thalamic atrophy [50]. Older adult patients with cognitive impairment and depressive symptoms should receive clinical attention. While focusing on their cognitive function, sufficient attention should also be paid to older adults’ mental health. Medical workers could provide older adults with health education related to cognitive function and mental health problems. Moreover, community nurses could formulate effective and dynamic assessment strategies to improve older adults’cognitive function and depressive symptoms, and encourage them to participate in cognitive function and psychological tests.
Influential Relationship of Developmental Trajectory Between Older Adults’ Cognitive Function and Depressive Symptoms
This study reveals that the baseline level of cognitive function in older adults can significantly predict the baseline value and change rate of depressive symptoms. The higher the baseline level of cognitive function, the lower the baseline level of depressive symptoms, but the faster the growth of depressive symptoms in the process of its subsequent development. Moreover, the faster the cognitive function decline, the faster the upward trend of depressive symptoms. Researchers have examined the association between cumulative depressive symptoms and cognitive decline in several cohort studies, with inconsistent conclusions. For example, some studies have reported a link between depressive symptoms and cognitive function [47, 51, 52], while others have found no association [20, 53], or an association in sub-groups only [54]. Some cross-sectional studies have shown that older adults’ cognitive function negatively affected their depressive symptoms [54, 55]; moreover, patients with depression have decreased working memory and attention, and the severity is negatively correlated with depressive symptoms. The awareness of cognitive decline may cause depression as a psychological reaction to the loss of cognitive function [56]. Therefore, people with cognitive impairment have a higher incidence of depression, and after their cognitive function is impaired, depression will occur. Normal cognitive function can help them buffer the painful experience caused by depressive symptoms. Therefore, based on the characteristics of older adults in the community, a comprehensive intervention program should be constructed that includes cognitive impairment and depression to promote the development of healthy aging. Moreover, nursing professionals and family caregivers should help older adults to retain a favorable level of cognitive function by cultivating cognitive training, so as to reduce their depressive symptoms level.
Related Factors Influencing the Depressive Symptoms and Cognitive Function Trajectories in Older Adults
Epidemiological studies have suggested that long-term exposure to complex functional and leisure environments or social activities can enhance cognitive function [57]. In traditional Chinese society and culture, males are exposed to such activities or environments for longer periods, which plays an affirmative role in their cognitive function reserve and prevents neurological decline [58].
The current study reveals that the higher the older adults’ education level, the higher their baseline cognitive function, and the lower their baseline depressive symptoms. A previous study has suggested that uneducated older adults are three to four times more likely to develop cognitive impairment than those who have received an education [59]. The current study further supports the idea that a few years of schooling can have a protective influence on cognitive dysfunction, since older adults with more years of education have higher cognitive function.
This study demonstrates that exercise has a positive effect on older adults’ baseline cognitive function, while cognitive function decline is slower in those who exercise. Similar findings have been found in other studies [18,60]. According to a randomized controlled trial of middle-aged and older adults, exercise can have a beneficial effect on specific aspects of cognitive function [18,61]; the current study’s conclusions are consistent with this finding. Hence, exercise may play an important role in promoting older adults’ cognitive function as it can indirectly reduce cognitive function decline and improve cognitive function.
Implications for Practice
This study shows that depression and cognitive impairment are persistent problems among older adults. Nevertheless, only 2.4% of older adults are diagnosed as having depression [62]. Therefore, there is an urgent need to vigorously build a team of mental health nursing personnel and improve the professionalism of nursing services to cope with the increasing demand for mental health services for older adults.
This study suggests that nursing professionals and family caregivers should pay special attention to the psychological conditions of older adults with rapidly declining cognitive function because the increase of depressive symptoms can occur during this critical period. Early detection and intervention of predictive indicators based on cognitive function could be effective in preventing the increase of depression levels, delaying the progress of depression, and reducing its prevalence and related public health burden. Moreover, the community could regularly guide older adults in community exercise activities, so as to sequentially slow down their cognitive decline and maximize the benefits of physical and mental health.
Limitations and Future Perspectives
This study has the following limitations. First, the measurement of depressive symptoms cannot completely represent the clinical diagnosis and assessment of depression. Second, the use of the CMMSE to characterize cognitive function may be associated with ceiling effects and inadequate sensitivity in detecting subtle cognitive impairment. The future studies would benefit from the use of more sensitive scales to identify depressive symptoms and cognitive function. Third, this study excluded people who were older and who had more chronic diseases, so it is necessary to further explore the longitudinal association between depressive symptoms and cognitive function in this group in the future.
Conclusion
This study uses an LGCM to explore whether changes in depressive symptoms over time are associated with cognitive function. The findings may have clinical implications for healthcare providers involved with depressive symptoms prevention or care. Notably, the decline rate of cognitive function in older adults can effectively predict the growth rate of depressive symptoms. Education and exercise can effectively ameliorate older adults’depressive symptoms. The findings can help nursing staff and health managers to address this situation., so as to reinforce the prevention of depressive symptoms in older adults and take targeted measures to reduce their risk of depression by promoting healthy exercise.
Statements
Ethics statement
The CLHLS study was approved by the Biomedical Ethics Committee of Peking University (IRB00001052-13074). The survey respondents gave their informed consent before participation.
Author contributions
LY and ZG contributed conception and design of the study; ZG, XW, CL, and LY organized the database and performed the statistical analysis; ZG wrote the manuscript; LY, CL, XM, JK, MX, and KZ contributed to data interpretation and revising the manuscript.
Funding
This work was supported by the Qingdao Philosophy and Social Science Planning Project (QDSKL2101068).
Acknowledgments
The authors thank the study participants.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/ijph.2022.1605124/full#supplementary-material
Supplementary Table S1Standardised coefficients for covariates in the multivariate linearity latent growth curve model (Chinese Longitudinal Health Longevity Survey, China, 2011–2018).
References
1.
Yadav UN Thapa TB Mistry SK Pokhrel R Harris MF . Socio-demographic Characteristics, Lifestyle Factors, Multi-Morbid Conditions and Depressive Symptoms Among Nepalese Older Adults. BMC Psychiatry (2020) 20(1):261. 10.1186/s12888-020-02680-3
2.
Shen K Zhang B Feng Q . Association between tea Consumption and Depressive Symptom Among Chinese Older Adults. BMC Geriatr (2019) 19:246. 10.1186/s12877-019-1259-z
3.
Meng R Yu C Liu N He M Li L . Association of Depression with All-Cause and Cardiovascular Disease Mortality Among Adults in China. Jama Netw Open (2020) 3(2):e1921043. 10.1001/jamanetworkopen.2019.21043
4.
Maruta M Makizako H Ikeda Y Miyata H Nakamura A Han G et al Associations between Depressive Symptoms and Satisfaction with Meaningful Activities in Community-Dwelling Japanese Older Adults. J Clin Med (2020) 9(3):795. 10.3390/jcm9030795
5.
Jorm AF Patten SB Brugha TS Mojtabai R . Has Increased Provision of Treatment Reduced the Prevalence of Common Mental Disorders? Review of the Evidence from Four Countries. World Psychiatry : official J World Psychiatr Assoc (Wpa) (2017) 16(1):90–9. 10.1002/wps.20388
6.
Quinn TJ Myint PK McCleery J Taylor Rowan M Stewart C . Anticholinergic burden (Prognostic Factor) for Prediction of Dementia or Cognitive Decline in Older Adults with No Known Cognitive Syndrome. Cochrane Database Syst Rev (2020) 2020(2):D13540. 10.1002/14651858.cd013540
7.
Pieper NT Grossi CM Chan W Loke YK Savva GM Haroulis C et al Anticholinergic Drugs and Incident Dementia, Mild Cognitive Impairment and Cognitive Decline: a Meta-Analysis. Age and Ageing (2020) 49(6):939–47. 10.1093/ageing/afaa090
8.
Zhang Y Wang P . Age-Related Increase of Insulin-Degrading Enzyme Is Inversely Correlated with Cognitive Function in APPswe/PS1dE9 Mice. Med Sci monitor : Int Med J Exp Clin Res (2018) 24:2446–55. 10.12659/msm.909596
9.
Petersen RC Lopez O Armstrong MJ Getchius TSD Ganguli M Gloss D et al Practice Guideline Update Summary: Mild Cognitive Impairment: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology (2018) 90(3):126–35. 10.1212/wnl.0000000000004826
10.
Zheng F Zhong B Song X Xie W . Persistent Depressive Symptoms and Cognitive Decline in Older Adults. Br J Psychiatry : J Ment Sci (2018) 213(5):638–44. 10.1192/bjp.2018.155
11.
Röhr S Löbner M Gühne U Heser K Kleineidam L Pentzek M et al Changes in Social Network Size Are Associated with Cognitive Changes in the Oldest-Old. Front Psychiatry (2020) 11:330. 10.3389/fpsyt.2020.00330
12.
Formánek T Csajbók Z Wolfová K Kučera M Tom S Aarsland D et al Trajectories of Depressive Symptoms and Associated Patterns of Cognitive Decline. Scientific Rep (2020) 10(1):20888.
13.
Yen Y Rebok GW Gallo JJ Jones RN Tennstedt SL . Depressive Symptoms Impair Everyday Problem-Solving Ability through Cognitive Abilities in Late Life. Am J Geriatr Psychiatry : official J Am Assoc Geriatr Psychiatry (2011) 19(2):142–50. 10.1097/jgp.0b013e3181e89894
14.
Kiosses DN Alexopoulos GS . IADL Functions, Cognitive Deficits, and Severity of Depression: a Preliminary Study. Am J Geriatr Psychiatry : official J Am Assoc Geriatr Psychiatry (2005) 13(3):244–9. 10.1097/00019442-200503000-00010
15.
LaMonica HM Biddle DJ Naismith SL Hickie IB Maruff P Glozier N . The Relationship between Depression and Cognitive Function in Adults with Cardiovascular Risk: Evidence from a Randomised Attention-Controlled Trial. PLoS One (2018) 13(9):e203343. 10.1371/journal.pone.0203343
16.
Richard E Reitz C Honig LH Schupf N Tang MX Manly JJ et al Late-life Depression, Mild Cognitive Impairment, and Dementia. JAMA Neurol (2013) 70(3):374–82. 10.1001/jamaneurol.2013.603
17.
Ahn S Mathiason MA Yu F . Longitudinal Cognitive Profiles by Anxiety and Depressive Symptoms in American Older Adults with Subjective Cognitive Decline. J Nurs Scholarship (2021) 53(6):698–708. 10.1111/jnu.12692
18.
Choi D Han K Jeon J Jang S Kim SJ Park E . Association between Depressive-Symptom Trajectories and Cognitive Function in the Late Middle-Aged and Older Population: Results of the Korean Longitudinal Study of Ageing. Sci Rep (2019) 9(1):7807. 10.1038/s41598-019-44158-7
19.
Perrino T Mason CA Brown SC Spokane A Szapocznik J . Longitudinal Relationships between Cognitive Functioning and Depressive Symptoms Among Hispanic Older Adults. Journals Gerontology Ser B, Psychol Sci Soc Sci (2008) 63(5):P309–P317. 10.1093/geronb/63.5.p309
20.
Dufouil C Fuhrer R Dartigues JF Alperovitch A . Longitudinal Analysis of the Association between Depressive Symptomatology and Cognitive Deterioration. Am J Epidemiol (1996) 144:634–41. 10.1093/oxfordjournals.aje.a008974
21.
Kambe T Yasuda A Kinoshita S Shigeta M Kinoshita T . Severity of Depressive Symptoms and Volume of Superior Temporal Gyrus in People Who Visit a Memory Clinic Unaccompanied. Demen Geriatr Cogn Disord extra (2018) 8(2):207–13. 10.1159/000489008
22.
Jae H Kim Y Junhyun K Eun-Cheol P . Association between Changes in Depressive State and Cognitive Function. Int J Environ Res Public Health (2019) 16(24):4944. 10.3390/ijerph16244944
23.
Geda YE Roberts RO Mielke MM Knopman DS Christianson TJH Pankratz VS et al Baseline Neuropsychiatric Symptoms and the Risk of Incident Mild Cognitive Impairment: a Population-Based Study. Ajp (2014) 171(5):572–81. 10.1176/appi.ajp.2014.13060821
24.
Pink A Stokin GB Bartley MM Roberts RO Sochor O Machulda MM et al Neuropsychiatric Symptoms, APOE ε4, and the Risk of Incident Dementia: a Population-Based Study. Neurology (2015) 84(9):935–43. 10.1212/wnl.0000000000001307
25.
Saczynski JS Beiser A Seshadri S Auerbach S Wolf PA Au R . Depressive Symptoms and Risk of Dementia. the Framingham Heart Study (2010) 75:35–41. 10.1212/WNL.0b013e3181e62138
26.
Sha T Gao X Chen C Li L He Q Wu X et al Associations of Pre-Pregnancy BMI, Gestational Weight Gain and Maternal Parity with the Trajectory of Weight in Early Childhood: A Prospective Cohort Study. Int J Environ Res Public Health (2019) 16(7):1110. 10.3390/ijerph16071110
27.
Wang P Lin H Yang YC Hsu C Chung K Wu H et al Gender and Age Effects on the Trajectory of Depression in Opioid Users during Methadone Maintenance Treatment. Front Psychiatry (2017) 8:288. 10.3389/fpsyt.2017.00288
28.
Bueno-Antequera J Munguía-Izquierdo D . Exercise and Depressive Disorder. Adv Exp Med Biol (2020) 1228:271–87. 10.1007/978-981-15-1792-1_18
29.
Zeng Y . Chinese Longitudinal Healthy Longevity Survey and Some Research Findings. Geriatr Gerontol Int (2010) 4:S49–S52. 10.1111/j.1447-0594.2004.00147.x
30.
Patsou ED Alexias GT Anagnostopoulos FG Karamouzis MV . Physical Activity and Sociodemographic Variables Related to Global Health, Quality of Life, and Psychological Factors in Breast Cancer Survivors. Psychol Res Behav Manag (2018) 11:371–81. 10.2147/prbm.s170027
31.
Lobo E Gracia-García P Lobo A Saz P De-la-Cámara C . Differences in Trajectories and Predictive Factors of Cognition over Time in a Sample of Cognitively Healthy Adults, in Zaragoza, Spain. Int J Environ Res Public Health (2021) 18(13):7092. 10.3390/ijerph18137092
32.
Nguyen TT Tchetgen Tchetgen EJ Kawachi I Gilman SE Walter S Glymour MM . The Role of Literacy in the Association between Educational Attainment and Depressive Symptoms. SSM - Popul Health (2017) 3:586–93. 10.1016/j.ssmph.2017.07.002
33.
Mohebbi M Agustini B Woods RL McNeil JJ Nelson MR Shah RC et al Prevalence of Depressive Symptoms and its Associated Factors Among Healthy Community-Dwelling Older Adults Living in Australia and the United States. Int J Geriatr Psychiatry (2019) 34(8):1208–16. 10.1002/gps.5119
34.
Zielińska-Więczkowska H Sas K . The Sense of Coherence, Self-Perception of Aging and the Occurrence of Depression Among the Participants of the University of the Third Age Depending on Socio-Demographic Factors. Clin Interventions Aging (2020) 15:1481–91. 10.2147/CIA.S260635
35.
Zhou Z Wang P Fang Y . Social Engagement and its Change Are Associated with Dementia Risk Among Chinese Older Adults: A Longitudinal Study. Scientific Rep (2018) 8(1):1551. 10.1038/s41598-017-17879-w
36.
Zhao Y Xu X Dupre ME Xie Q Qiu L Gu D . Individual-level Factors Attributable to Urban-Rural Disparity in Mortality Among Older Adults in China. BMC Public Health (2020) 20(1):1472. 10.1186/s12889-020-09574-9
37.
Liu X Song Z Li Y Yao Y Fang M Bai C et al Integrated Genetic Analyses Revealed Novel Human Longevity Loci and Reduced Risks of Multiple Diseases in a Cohort Study of 15,651 Chinese Individuals. Aging Cell (2021) 20(3):e13323. 10.1111/acel.13323
38.
Yi Z Vaupel J . Association of Late Childbearing with Healthy Longevity Among the Oldest-Old in China. Popul Stud (2004) 58(1):37–53. 10.1080/0032472032000175437
39.
Zeng Y Chen H Shi X Yin Z Yang Z Gu J et al Health Consequences of Familial Longevity Influence Among the Chinese Elderly. J Gerontol A Biol Sci Med Sci (2013) 68:473–82. 10.1093/gerona/gls203
40.
Feng Q Son J Zeng Y . Prevalence and Correlates of Successful Ageing: a Comparative Study between China and South Korea. Eur J Ageing (2014) 12(2):83–94. 10.1007/s10433-014-0329-5
41.
Nunnally JC . Psychometric Theory. Am Educ Res J (1978) 5(3):83.
42.
Lök N Bademli K Selçuk-Tosun A . The Effect of Reminiscence Therapy on Cognitive Functions, Depression, and Quality of Life in Alzheimer Patients: Randomized Controlled Trial. Int J Geriatr Psychiatry (2019) 34(1):47–53. 10.1002/gps.4980
43.
Wu C Zhou D Peter C Fan J Qiao Y . Applicability of Chinese Version of Mini Mental State Examination Form in Rural Areas of China[J]. Chin Ment Health J (2002) 04:242–5. (In China).
44.
Rudman A Gustavsson JP . Burnout during Nursing Education Predicts Lower Occupational Preparedness and Future Clinical Performance: a Longitudinal Study. Inter J Nursing Stud (2012) 49(8):988–1001. 10.1016/j.ijnurstu.2012.03.010
45.
Gao M Kuang W Qiu P Wang H Lv X Yang M . The Time Trends of Cognitive Impairment Incidence Among Older Chinese People in the Community: Based on the CLHLS Cohorts from 1998 to 2014. Age Ageing (2017) 46:787–93. 10.1093/ageing/afx038
46.
Yun EK Lee H Lee JU Park JH Noh YM Song YG et al Longitudinal Effects of Body Mass Index and Self-Esteem on Adjustment from Early to Late Adolescence: A Latent Growth Model. The J Nurs Res : JNR (2019) 27(1):1–7. 10.1097/jnr.0000000000000266
47.
Zhou L Ma X Wang W . Relationship between Cognitive Performance and Depressive Symptoms in Chinese Older Adults: The China Health and Retirement Longitudinal Study (CHARLS). J Affective Disord (2021) 281:454–8. 10.1016/j.jad.2020.12.059
48.
Argano C Catalano N Natoli G Monaco ML Corrao S . GDS Score as Screening Tool to Assess the Risk of Impact of Chronic Conditions and Depression on Quality of Life in Hospitalized Elderly Patients in Internal Medicine Wards. Medicine (2021) 100(26):e26346. 10.1097/md.0000000000026346
49.
Kauppi K Rönnlund M Nordin Adolfsson A Pudas S Adolfsson R . Effects of Polygenic Risk for Alzheimer's Disease on Rate of Cognitive Decline in normal Aging. Translational Psychiatry (2020) 10(1):250. 10.1038/s41398-020-00934-y
50.
Li J Yang R Xia K Wang T Nie B Gao K et al Effects of Stress on Behavior and Resting-State fMRI in Rats and Evaluation of Telmisartan Therapy in a Stress-Induced Depression Model. BMC Psychiatry (2018) 18(1):337. 10.1186/s12888-018-1880-y
51.
Wilson RS Mendes De Leon CF Bennett DA Bienias JL Evans DA . Depressive Symptoms and Cognitive Decline in a Community Population of Older Persons. J Neurol Neurosurg Psychiatry (2004) 75(1):126–9.
52.
Paterniti S Verdier-Taillefer M Dufouil C Alpérovitch A . Depressive Symptoms and Cognitive Decline in Elderly People. Longitudinal Study. Br J Psychiatry : J Ment Sci (2002) 181:406–10. 10.1192/bjp.181.5.406
53.
Henderson AS Korten AE Jacomb PA Mackinnon AJ Jorm B au fnm 1997). The Course of Depression in the Elderly: A Longitudinal Community-Based Study in Australia. Psychol Med, 27(1), 119–29.10.1017/s0033291796004199
54.
Gale CR Allerhand M Deary IJ . Is There a Bidirectional Relationship between Depressive Symptoms and Cognitive Ability in Older People? A Prospective Study Using the English Longitudinal Study of Ageing. Psychol Med (2012) 42(10):2057–69. 10.1017/s0033291712000402
55.
Sun Z Wang Z Xu L Lv X Yu X . Characteristics of Cognitive Deficit in Amnestic Mild Cognitive Impairment with Subthreshold Depression. J Geriatr Psychiatry Neurol (2019) 32(6):344–53. 10.1177/0891988719865943
56.
Vinkers DJ Gussekloo J Stek ML Westendorp RGJ van der Mast RC . Temporal Relation between Depression and Cognitive Impairment in Old Age: Prospective Population Based Study. BMJ (Clinical research ed.) (2004) 329(7471):881. 10.1136/bmj.38216.604664.de
57.
Matyas N Keser Aschenberger F Wagner G Teufer B Auer S Gisinger C et al Continuing Education for the Prevention of Mild Cognitive Impairment and Alzheimer's-type Dementia: a Systematic Review and Overview of Systematic Reviews. BMJ Open (2019) 9(7):e27719. 10.1136/bmjopen-2018-027719
58.
Sánchez JL Torrellas C Martín J Barrera I . Study of Sociodemographic Variables Linked to Lifestyle and Their Possible Influence on Cognitive reserve. J Clin Exp Neuropsychol (2011) 33(8):874–91.
59.
Jia J Wang F Wei C Zhou A Jia X Li F et al The Prevalence of Dementia in Urban and Rural Areas of China. Alzheimer's Demen : J Alzheimer's Assoc (2014) 10(1):1–9. 10.1016/j.jalz.2013.01.012
60.
Park H Park JH Na HR Hiroyuki S Kim GM Jung MK et al Combined Intervention of Physical Activity, Aerobic Exercise, and Cognitive Exercise Intervention to Prevent Cognitive Decline for Patients with Mild Cognitive Impairment: A Randomized Controlled Clinical Study. J Clin Med (2019) 8(7):940. 10.3390/jcm8070940
61.
Angevaren M Aufdemkampe G Verhaar H Aleman L Vanhees L . Physical Activity and Enhanced Fitness to Improve Cognitive Function in Older People without Known Cognitive Impairment. Cochrane Database Syst Rev (2008) 1:CD005381. 10.1002/14651858.CD005381.pub3
62.
Xiao S Lewis M Mellor D McCabe M Byrne L Wang T et al The China Longitudinal Ageing Study: Overview of the Demographic, Psychosocial and Cognitive Data of the Shanghai Sample. J Ment Health (Abingdon, England) (2016) 25(2):131–6. 10.3109/09638237.2015.1124385
Summary
Keywords
longitudinal study, cognitive function, depressive symptoms, latent growth curve model, old adults
Citation
Gao Z, Liu C, Yang L, Mei X, Wei X, Kuang J, Zhou K and Xu M (2022) Longitudinal Association Between Depressive Symptoms and Cognitive Function Among Older Adults: A Latent Growth Curve Modeling Approach. Int J Public Health 67:1605124. doi: 10.3389/ijph.2022.1605124
Received
14 June 2022
Accepted
08 September 2022
Published
23 September 2022
Volume
67 - 2022
Edited by
Nino Kuenzli, Swiss Tropical and Public Health Institute (Swiss TPH), Switzerland
Updates
Copyright
© 2022 Gao, Liu, Yang, Mei, Wei, Kuang, Zhou and Xu.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Li Yang, yang-li81@163.com
†These authors have contributed equally to this work
This Original Article is part of the IJPH Special Issue “Health in all Sustainable Development Goals”
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.