- 1Washington University in St. Louis—Social Policy Institute (SPI), St. Louis, MO, United States
- 2School of Public Health, Faculty of Health Sciences, Ben-Gurion University of the Negev, Be’er-sheva, Israel
- 3The School of Nutrition Science, The Institute of Biochemistry Food Science and Nutrition, The Robert H. Smith Faculty of Agriculture Food and Environment, The Hebrew University of Jerusalem, Rehovot, Israel
- 4Washington University in St. Louis—George Warren Brown School of Social Work, St. Louis, MO, United States
- 5Centene Corporation, St. Louis, MO, United States
Objective: To identify the socioeconomic and demographic factors associated with the prevalence of self-reported long-COVID symptoms.
Method: We examined the association between acute-COVID (SARS-CoV-2) and long-COVID symptoms, by a cross-sectional analysis of data obtained on a prospective online-survey, conducted from November to December 2021 on a nationally-representative sample of the Israeli population (N = 2,246).
Results: Findings suggest that there is a greater likelihood of experiencing long-COVID symptoms among low-income and among marginalized groups. After controlling for demographic and socioeconomic attributes, those who had moderate/severe acute-COVID were 1.3 (p < 0.05) times more likely to experience a long-term symptom and also reported more long-term symptoms (2.2 symptoms) than those who have not been infected (1.4 symptoms; p < 0.01). Among the low-income group, a larger gap in symptom count was found between those who had moderate/severe acute-COVID (3.3 symptoms) and those who had not been infected (1.8 symptoms, p < 0.05).
Conclusion: Our findings highlight the importance of raising awareness of long-COVID among marginalized population groups, and to the therapeutic options available. Such efforts should be tailored and should consider the unique socioeconomic and cultural characteristics, as well as the preexisting low access to healthcare services among these groups.
Introduction
Since the beginning of the coronavirus pandemic, approximately 435 million individuals have been infected worldwide and 5.9 million people have died from COVID-19 related illnesses (1, 2). At the time of writing, in Israel, approximately 3.6 million people out of a total population of 9.3 million have been infected and over 10,000 people have died of the disease (3). Although COVID-19 was initially considered to be primarily a respiratory disease, it is now evident that the virus may harm the pulmonary, cardiovascular, neurologic, psychiatric, gastrointestinal, renal, endocrine, and musculoskeletal systems, in both adult and pediatric populations (4, 5), and more rarely, in children, can lead to a life threatening multisystem inflammatory syndrome (MIS-C) (6). While the acute symptoms of COVID-19 infection typically remit after several weeks, a concerning proportion of individuals experience lingering symptoms that persist for months after infection (1, 7). Symptoms that appear during or after COVID-19 onset, and which persist for one month or more, are referred variably in the literature as post-COVID, post-COVID syndrome, post-acute COVID, long-haul COVID, or simply, “long-COVID”. There is considerable variability with respect to the presentation of long-COVID: some individuals experience a continuation of the same symptoms as when they were first infected; others may experience an asymptomatic period followed by a recurrence of symptoms; and still others present with symptoms that are different from when they were first infected (7). Symptoms and conditions most commonly associated with long-COVID include shortness of breath and fatigue and may also include dizziness, chest and abdominal pain, and mental health problems such as depression, anxiety, and posttraumatic stress disorder (5, 8–12).
Long-COVID is difficult to diagnose and treat, not only because the disease is still an evolving phenomenon but also as a result of its varied presentation, lack of specificity, and temporal separation from the acute infection. Nevertheless, it can significantly degrade quality of life and wellbeing (13, 14). Moreover, there is growing evidence that long-COVID may be related to underlying damage to major organs including the lungs, heart and cardiovascular system, liver, kidneys, and brain (1). Recently, large population studies have shown that individuals who recovered from COVID-19 have significantly increased risk of incident cardiovascular disease (15), mental health disorders (15, 16), and brain anomalies on MRI (17) even among confirmed cases whose acute infection was mild or asymptomatic. Thus, with millions affected worldwide, and as the world transitions to “living with COVID” (18), understanding the nature and determinants of long-COVID is an increasingly urgent public health concern (19–22).
As we have already learned with respect to acute-COVID, social and economic disparities are among the most important predictors of disease severity and outcome and of willingness to accept public health guidance, including on vaccination. It stands to reason that these factors will also be important in determining the outcomes of long-COVID because of the close relationship between the incidence and severity of the acute disease, with disparities in education and income, food insecurity and obesity, as well as vaccine hesitancy among ethnic minorities and other marginalized populations (22–30). However, little is known about the social and economic determinants of long-COVID. Clarifying their role in this chronic and prevalent condition will be necessary if we are to improve clinical care for this condition and develop effective and equitable public health policies to deal with its consequences.
Although still in infancy, a growing set of studies have examined risk factors associated with long-COVID. Older adults and women have been found to be at a heightened risk for onset (31, 32) as have persons with high body mass and those who had reported more than five symptoms when initially infected (31). Co-morbid health (asthma, obesity) and mental health problems prior to the pandemic have also been linked to the onset of long-COVID (32). In light of these studies, we aimed to identify the socioeconomic and demographic factors associated with the prevalence of self-reported long-COVID symptoms using cross-sectional data obtained from our prospective online survey of a nationally-representative sample of the Israeli population.
Methods
Study Design and Population
This study utilized data obtained by a longitudinal online Qualtrics survey of a nationally-representative sample of Israeli adults, which was repeated five times during the COVID-19 pandemic, between June 2020 to November 2021. The objective of the parent study was to evaluate how socioeconomic factors affect resilience during a pandemic for the purpose of policy research and evaluation. For this analysis, we used data from the 5th round of the survey (n = 2,362), which was conducted between 26 November and 21 December 2021. This corresponded to the period in Israel between the fourth wave, dominated by the Delta variant, and the fifth “omicron” wave, which began in early 2022. The sample was constructed from a pool of participants by a local survey company using quota sampling techniques to ensure that the sample represented Israel demographic characteristics with respect to gender, age groups, income groups, and religion/religiosity. The 5th round sample was constructed from returning participants (n = 1,644; 69.6%) whose participation rate was 45.0%, and new participants (n = 718; 30.4%) whose participation rate was 6.4%. We excluded participants who had acute-COVID less than one month before the survey (n = 35) and participants who did not respond to key items, using listwise deletion. Since sample composition was the same as in the parent survey with respect to demographic characteristics and cases of acute-COVID (Table 1), we assumed that the exclusion of records was random. The final analytical sample included all participants with complete responses (n = 2,246).
The survey inquired respondents’ demographic and socioeconomic characteristics and included COVID-19 related questions: having past diagnosis of acute COVID, disease severity, time passed since the diagnosis, and vaccination for COVID-19 including the number of shots received and the time passed since the last one. The survey also inquired whether and how long respondents, regardless of their past infection with COVID-19, currently are suffering from a range of symptoms, including fatigue, shortness of breath, impaired memory and attention, continuous damage to the sense of taste and the sense of smell, muscle aches and joint pains, chest pain, headaches, accelerated heartbeat, hair loss, sore throat and earache, and dizziness (33). Using these reports, we constructed a variable indicating presence of at least one symptom and a variable counting the number of symptoms one suffers from.
For the purpose of this analysis, we considered the frequency of symptoms among uninfected individuals as the background prevalence of these conditions and the prevalence of persistent symptoms among those diagnosed with acute COVID as evidence of long-COVID.
Empirical Model Design
We explored the association of the prevalence of long-COVID with the diagnosis and severity of acute COVID-19 in a cross-sectional design, using three types of models: 1) logistic regression models predicting presence of at least one of the relevant self-reported symptoms; 2) linear models predicting the number of self-reported symptoms, ranging from 0 to 11; and 3) for each symptom
For models 1 and 3, the following logistic model is employed:
For model 2, the following linear model is employed:
where
For a better representation of the regression results, we estimated and plotted the predicted margins—predicted probability (logistic regressions) and predicted count (linear regressions) of long-COVID symptoms—by COVID-19 infection and severity, by income, and by religiosity (see also Supplementary Appendix Table SA1). The data analysis in this study was conducted using Stata (Version 16; StataCorp, 2019), and we used a threshold of p < 0.10 to assess the statistical significance.
Results
Study Sample
Study sample comprises 2,246 individuals of which 89.2% have not had COVID-19, 7.1% have had COVID-19 with mild/minor symptoms, and 3.7% have had COVID-19 with moderate/severe symptoms.
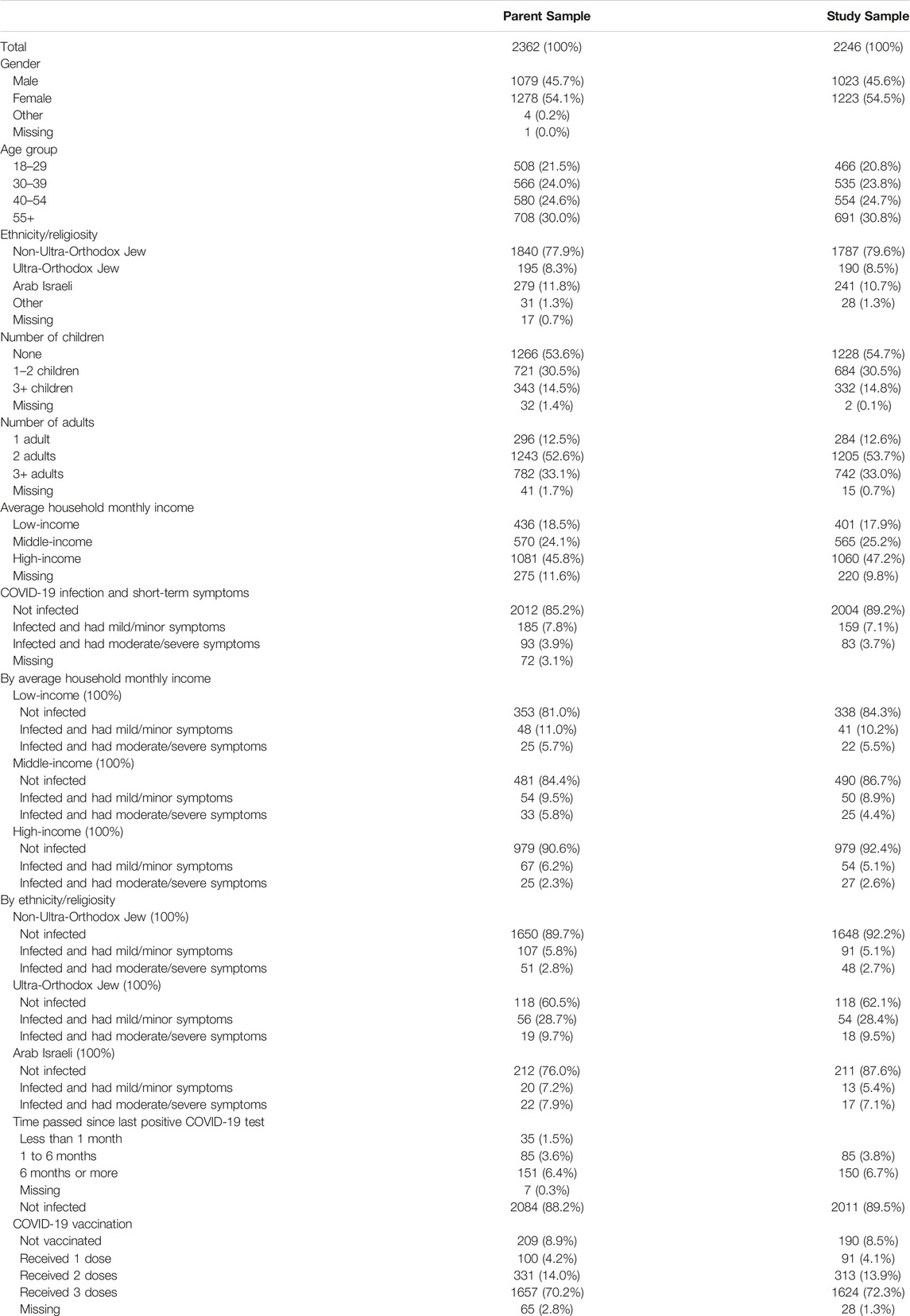
Long-Term COVID-Related Symptoms
Next, we report the results from our multivariate regression models showing how the self-reported COVID-19 long-term symptom (hereafter long-term symptom) prevalence varied with COVID-19 infection and severity of short-term symptoms. On average, 46.7% of our respondents reported one or more long-term symptoms. Also, we found that the long-term symptom prevalence varied with COVID-19 infection as well as its severity. Even after controlling for demographic and socioeconomic attributes, those who suffered from moderate or severe COVID-19 short-term symptoms were 1.3 times more likely to experience a long-term symptom than those who had not been infected (Not infected = 45.6%; Moderate/severe = 61.4%; p < 0.05; Figure 1A). Furthermore, those with moderate/severe COVID-19 reported more long-term symptoms on average (2.2) than those with mild/minor symptoms (1.3, not significant) and those who did not get infected (1.4, p < 0.01; Figure 1B).
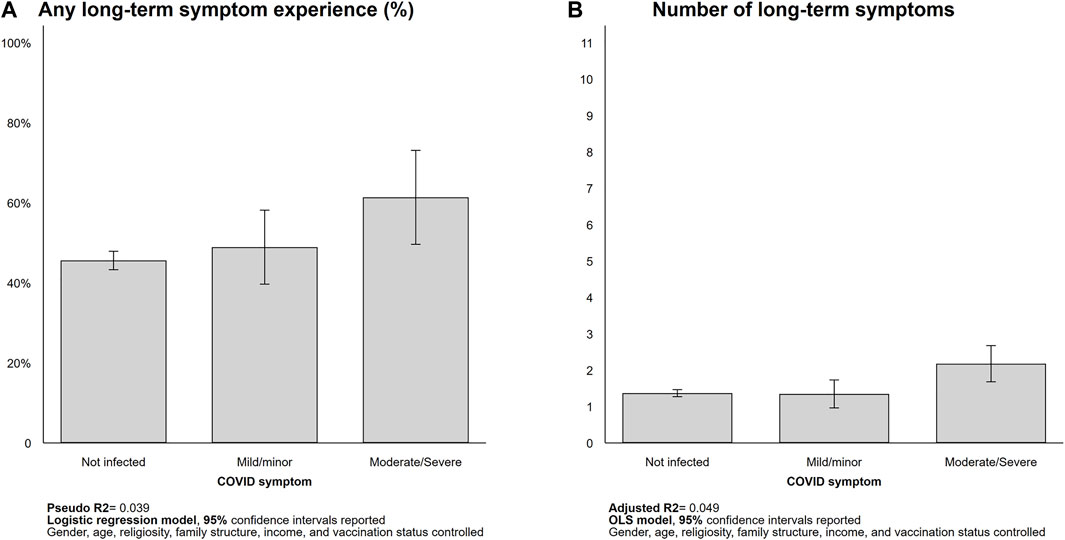
FIGURE 1. Long-term symptom prevalence (Israel, 2021). Predicted probability [(A), logistic regression] and counts of long-term symptom [(B), OLS] reported.
For some symptoms, we observed a greater gap between the moderate/severe group and the mild/minor group than between the mild/minor and not-infected groups: fatigue (not infected = 33.2%; moderate/severe = 56.4%; p < 0.01) and muscle aches and joint pains (not infected = 14.9%; moderate/severe = 32.4%; p < 0.05). Furthermore, in the case of loss of taste/smell functions, regardless of the severity of COVID-19 symptoms, those who had been infected (mild/minor = 10.5%; moderate/severe = 12.4%) were 3.5 and 4.1 times more likely to report this symptom than those who had not been infected (3.0%; p < 0.05 for both comparisons). For other long-COVID symptoms, such as shortness of breath, muscle aches and joint pains, and headaches, we observed similar, though statistically not significant, relationships with acute-COVID disease and severity (Figure 2).
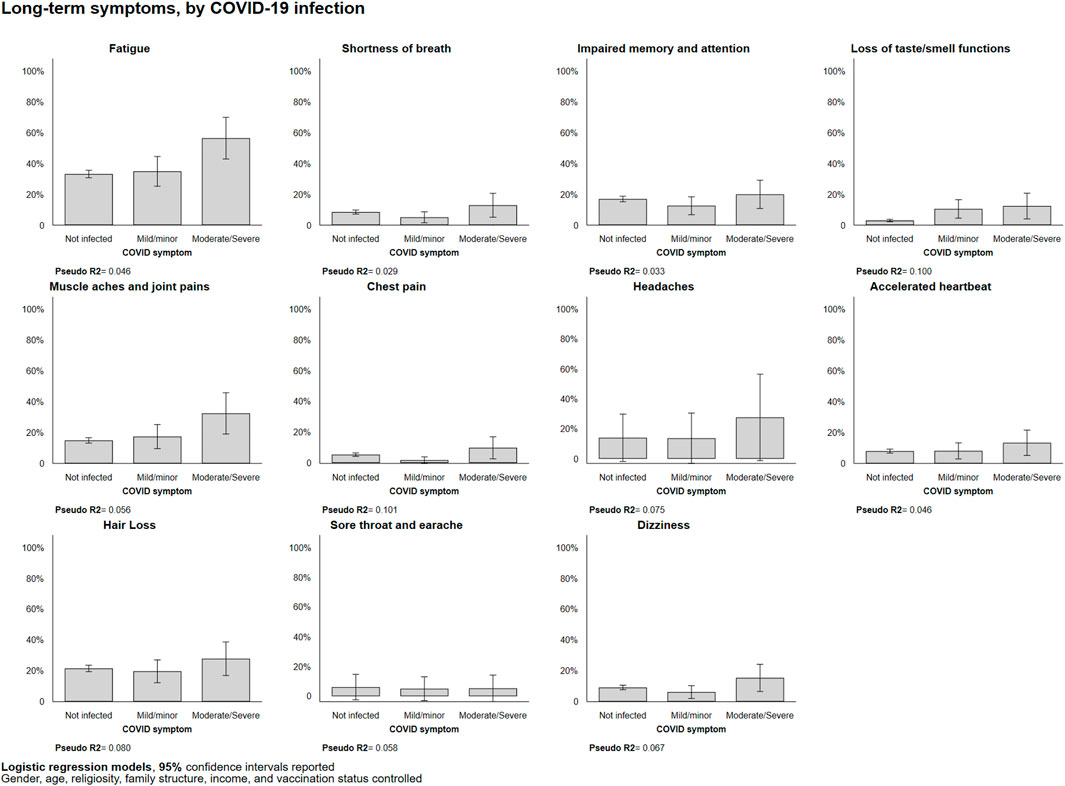
FIGURE 2. Itemized long-term symptom experiences by COVID-19 infection, marginal probabilities (Israel, 2021). Predicted probabilities from logistic regressions reported.
Long-Term COVID-Related Symptoms and Individual Characteristics
Lastly, we utilized the same sets of multivariate regression models to explore how the associations between long-term COVID-19 symptom prevalence and short-term COVID-19 infection/severity varied across respondents’ socioeconomic characteristics (i.e., income and religiosity).
Long-Term Symptoms by Income
We observed a negative association between income and long-term symptom experience in those without COVID-19 infection experience, both in experiencing at least one long-COVID symptom (low-income = 55.5%; high-income = 42.1%; p < 0.01) and in symptom count (low-income = 1.8; high-income = 1.2; p < 0.01). We also observed higher rates of long-term symptom prevalence in both low- and high-income respondents who had moderate/severe COVID-19 symptoms relative to those without COVID-19 infection (low-income = 55.5%–77.0%, p < 0.10; high-income = 42.2%–61.7%, p < 0.10; See Figure 3A). Also, the count of long-term symptoms increased by 1.8 in the low-income group (1.8–3.3, p < 0.05) but not in the other two groups. That is, the count of long-term symptoms of respondents who had moderate/severe COVID-19 symptoms was the highest among low-income respondents (3.3 compared to middle-income = 1.6, p < 0.10; and high-income = 1.8, not significant; Figure 3B).
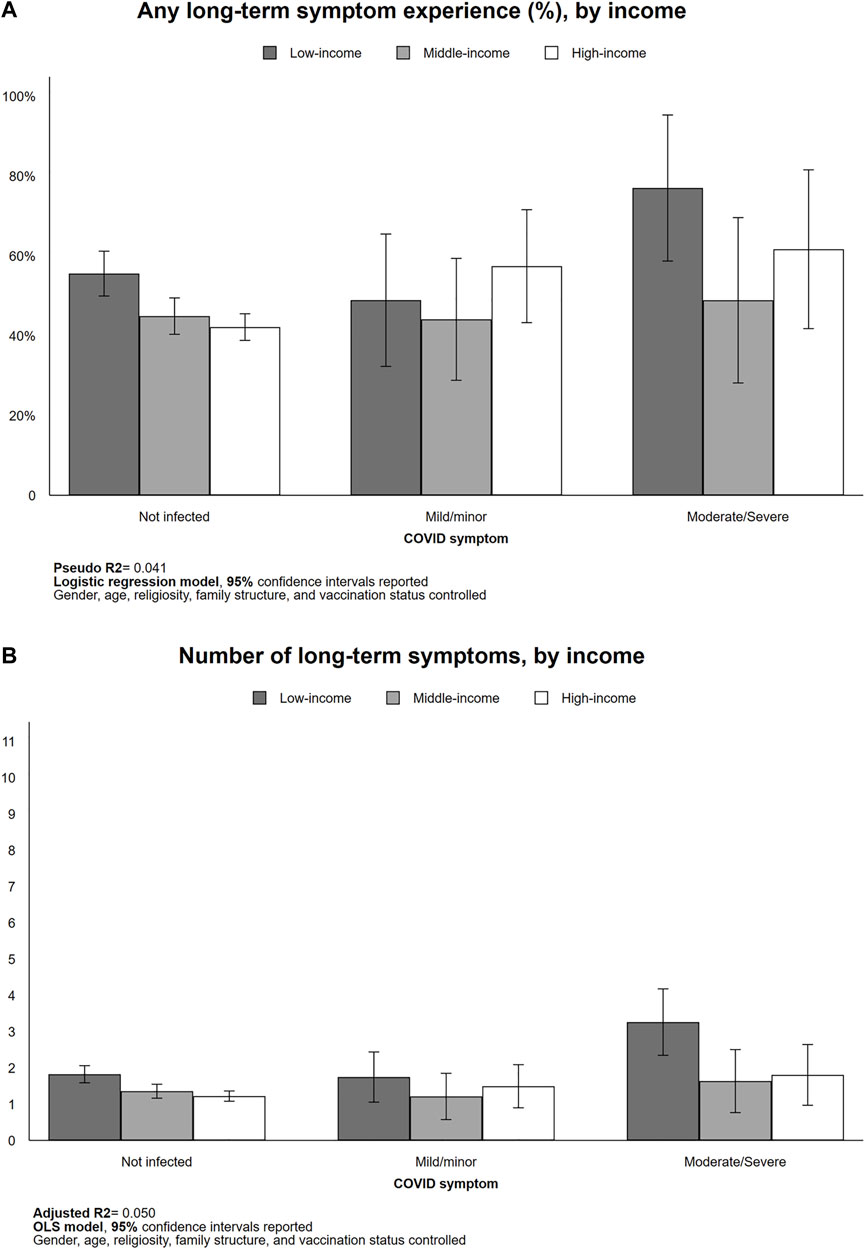
FIGURE 3. Long-term symptom experiences by income (Israel, 2021). Predicted probability [(A), logistic regression] and counts of long-term symptom [(B), OLS] reported.
In the low-income cohorts, we observed a statistically significant higher rate of long-term fatigue (46.6%–58.0%, p < 0.05), muscle aches and joint pains (19.9%–64.1%, p < 0.01). In the high-income group, we observed a statistically significantly higher rate of fatigue (29.0%–58.0%, p < 0.05) and loss of taste/smell functions (1.8%–26.0%, p < 0.05; See Supplementary Appendix Figure SA1).
Long-Term Symptoms by Ethnicity/Religiosity
Each of the three examined population groups comprising the Israeli society experienced more long-term symptoms if they had had moderate/severe COVID-19 disease, relative to those who were uninfected. Nevertheless, there were substantially higher, but not necessarily statistically significant, rates of long-term symptoms among non-Ultra-Orthodox Jews (46.9%–53.3%, not significant), the Ultra-Orthodox Jews (37.5%–76.1%, p < 0.05), and the Arab Israelis (41.2%–58.6%, not significant; see Figure 4A). On the other hand, Arab Israelis exhibited a significantly higher number of long-term symptoms as they suffered moderate/severe COVID-19 symptom in the short-term (1.7–3.2, p < 0.05). Among those who have not been infected with COVID-19, the Arabs Israelis had more long-COVID symptoms than the other group (1.7 symptoms relative to 1.3 (non-Ultra-Orthodox Jew, p < 0.10) and 1.1 (Ultra-Orthodox Jew, p < 0.10); Figure 4B).
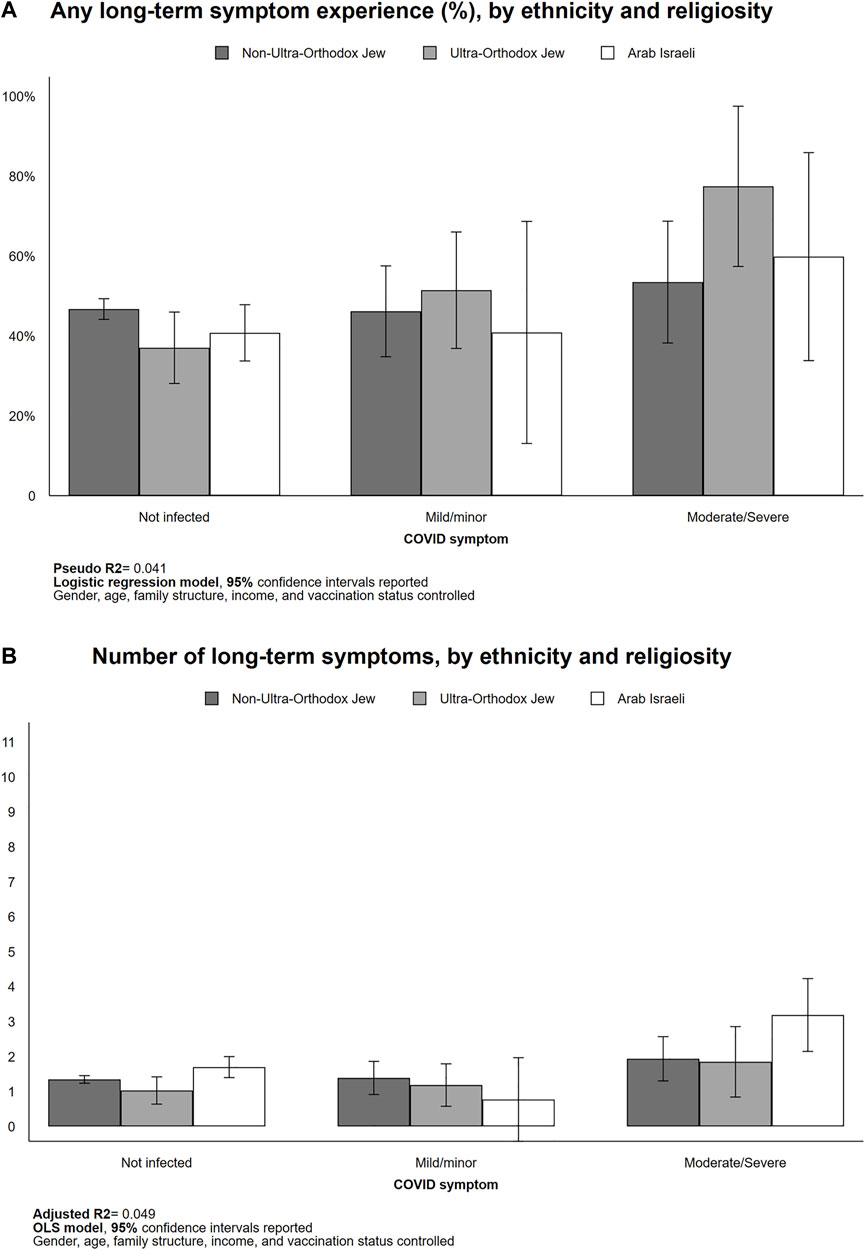
FIGURE 4. Long-term symptom experiences by ethnicity/religiosity (Israel, 2021). Predicted probability [(A), logistic regression] and counts of long-term symptom [(B), OLS] reported.
Non-Ultra-Orthodox Jews exhibited significantly higher rates of certain long-term symptoms, including fatigue (33.9%–53.9%, p < 0.10), loss of taste/smell functions (2.6%–19.3%, p < 0.05), and muscle and joint pains (14.5%–30.6%, p < 0.10) as they experienced moderate/severe short-term COVID-19 (See Supplementary Appendix Figure SA2). Note that the statistically non-significant differences in short-term COVID-19 severity for the two minority groups (Ultra-Orthodox Jews and Arab Israelis) might be related to their small sample sizes (Ultra-Orthodox Jews = 190; Arab Israelis = 241).
Discussion
This study explored the reported prevalence of COVID-19 long-term symptoms and how these symptoms vary with infection and severity of acute-COVID and by demographic and socioeconomic characteristics. The findings indicated that those infected with COVID-19 and who suffered moderate to severe illness were more likely to both experience long-COVID and to suffer more symptoms than those who experienced minor illness or were not infected at all. These findings align with those of a systematic review that found the severity of initial infection or symptom load is associated with a greater likelihood of long-COVID symptomatology (34), as well as with those of a recent German study which reported the intensity of acute phase symptoms as a predictor of post-COVID syndrome (35). Thus, our results further stress the importance of developing proactive and standardized practices for monitoring post-infection symptomatology to combat long-COVID (36, 37). Furthermore, we found that belonging to low-income and/or to a marginalized social or ethnic group was associated with an even greater likelihood of experiencing long-COVID. Our results are consistent with previous findings identifying specific subgroups as more vulnerable to both acute-COVID (38) and several symptoms of long-COVID (39–41). Additionally, recent evidence indicates higher rates of healthcare utilization (e.g., visits with a primary care provider) in the year following the acute COVID infection among socially vulnerable populations (42), highlighting the potential burden on healthcare facilities and staff among marginalized communities. Notably, in the current analysis, individuals from the high-income group that experienced mild or severe acute-COVID symptomatology also reported relatively high rates of long-term symptoms. This finding may reflect the documented association between income levels and COVID awareness (43) and suggest that the mechanisms involved in experiencing long-COVID are complex and warrant further research. Further discussion of these findings, their clinical and social implications, and future research directions are elaborated on below.
The findings relating to specific population groups that were more susceptible to long-COVID raise interesting health and social issues. Individuals of marginalized groups, whether due to ethnicity, social affiliation, low income, or other reasons, are known to be highly vulnerable in emergencies and to be disproportionately affected by them (44). The increased vulnerability stems from various barriers which impede the access of these groups to a variety of resources such as healthcare (45) and education (46), consequently leading to inequalities and blocking life opportunities (47). The COVID-19 pandemic is a stark and ongoing example of the complex ways in which marginalization materializes in adverse outcomes. In Israel, acute-COVID infections and mortality were higher in communities with predominantly Arab and ultra-Orthodox Jewish populations, which also tend to have lower income rates than the general Jewish population (48). Conversely, vaccination was lower among the same populations, despite access to universal healthcare and the rapid rollout of COVID-19 vaccination in Israel (49). The increased vulnerability of these groups has been attributed to various factors such as crowded living conditions, increased dependency on public transportation, employment in occupations that do not allow for the maintenance of social distancing, and a lack of trust in state institutions and their guidelines (50). Our findings provide the first insights into the association between COVID long-term risks and ethnicity, religiosity, and income levels in Israel. The results highlight ultra-Orthodox and Arab Israelis as also highly vulnerable to long-COVID. However, the low vaccine uptake reported above cannot explain these results as we have controlled for vaccination status in our models. The current findings emphasize the importance of raising awareness of long-COVID among these population groups and of the therapeutic options available to those in need. Awareness efforts should be tailored to these groups and should consider their unique socioeconomic and cultural characteristics as well as their preexisting low access to healthcare services (50). For example, several studies suggest using remote home monitoring to manage post-COVID recovery and rehabilitation using telemedicine platforms and devices (51, 52). However, it should be noted that the rate of telemedicine use among marginalized groups is relatively low (53, 54). Thus, close attention should be paid to ensure that the use of telemedicine in this context does not exacerbate existing inequalities.
The challenges of studying long-COVID are considerable (55). It is difficult to attribute the presence of prevalent, persistent, and diffuse or non-specific symptoms to the initial infection with certainty, particularly in cross-sectional and retrospective studies that are susceptible to recall bias. It is important to obtain a diagnosis of the initial infection and to demonstrate that the post-acute symptoms are sequalae of the infection that did not pre-date it. Thus, prospective studies are needed to identify risk factors for incident long-COVID by comparing exposures and outcomes between cases of long-COVID, acute only cases, and healthy controls. The inclusion of questions pertaining to long-COVID in the ongoing phase of our study will allow us to study incident long-COVID in future waves.
The current study has several limitations. First, the study relies on cross-sectional and self-reported data, which may lead to bias and inaccuracy in estimating the phenomenon under investigation, namely long-COVID. Moreover, it is reasonable to assume that a certain proportion of the participants experienced asymptomatic acute-COVID and were not officially diagnosed (56), which may cause additional bias. However, even if this figure turns out to be accurate, it will strengthen the research findings and not weaken them. Second, the issue of sample selection may also be the cause of potential bias: the rate of participants from Arab Israeli households in the current sample (11%) is slightly lower than their actual rate (15%) (57). However, here as well, our findings suggest that increasing their rate will strengthen the findings rather than weaken them. Finally, the current analysis evaluated the direct effects of marginalization indicators (e.g., belonging to a low-income household, ethnicity, etc.) on long-COVID symptom prevalence but did not measure their potential indirect effect. This important issue remains the goal of future research.
Despite these limitations, the results presented here help broaden our understanding of the relatively understudied phenomenon of long-COVID by offering insights into the attributes and predictors of this phenomenon, as well as specific populations that are at risk of experiencing it. As the pandemic continues for the foreseeable future and as the current surge of morbidity has led to more than 27 million new or recurrent acute-COVID cases in the US alone (7), it is of utmost importance to prepare for the aftermath of the infection. The current findings can serve as the basis for future healthcare planning and as a launchpad for future investigations of researchers and public health officials worldwide into how to better cope with the long-term consequences of the pandemic. Finally, as long-COVID is still a phenomenon that needs to be unraveled, further research is needed to better characterize the disease and its effects and to explore effective treatment and rehabilitative interventions.
Ethics Statement
The studies involving human participants were reviewed and approved by the Washington University in St. Louis IRB. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
Conceptualization: OH, YS, and MG-W; data curation: OH, YS, YC, and MG-W; formal analysis: OH and YC; funding acquisition: MG-W; investigation: OH, YS, YC, SS, AT, PM, and MG-W; methodology: OH, YC, SS, AT, and MG-W; discussion: SS, OH, SK, BK, and MG-W; project administration: OH and MG-W; resources: MG-W; software: YC; Writing—original draft: YC, SS, AT, and MA; writing—review and editing: OH, PM, SK, BK, and MG-W.
Funding
The authors declare that this study received funding from Mastercard Center for Inclusive Growth (Grant/Contract number: GR0013430) and Centene Center for Health Transformation (Grant/Contract number: GR0016455). The funder was not involved in the study design, collection, analysis, interpretation of data, the writing of this article, or the decision to submit it for publication.
Conflict of Interest
Authors SK and BK were employed by the Centene Corporation.
The remaining authors declare that they do not have any conflicts of interest.
Acknowledgments
The authors appreciate the contributions from many colleagues at the Social Policy Institute at Washington University in St. Louis who advised on planning and implementation of the study. The authors also thank the individuals who consented to participate in the research surveys and shared their personal experience during the COVID-19 pandemic. The authors acknowledge the funders who made the Socioeconomic Impact of COVID-19 Survey in Israel possible: Mastercard Center for Inclusive Growth and Centene Center for Health Transformation.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/ijph.2022.1605086/full#supplementary-material
References
1. Crook, H, Raza, S, Nowell, J, Young, M, and Edison, P. Long Covid-Mechanisms, Risk Factors, and Management. BMJ (2021) 374:n1648. doi:10.1136/bmj.n1648
2.Reuters. Israel: the Latest Coronavirus Counts, Charts and Maps (2022). Available from: https://graphics.reuters.com/world-coronavirus-tracker-and-maps/countries-and-territories/israel/ (Accessed January 9, 2022).
3. Dong, E, Du, H, and Gardner, L. An Interactive Web-Based Dashboard to Track COVID-19 in Real Time. Lancet Infect Dis (2020) 20(5):533–4. doi:10.1016/S1473-3099(20)30120-1
4. Roberts, C, Levi, M, McKee, M, Schilling, R, Lim, W, and Grocott, M. COVID-19: a Complex Multisystem Disorder. Br J Anaesth 125:238–42. doi:10.1016/j.bja.2020.06.013
5. Jiang, D, Roy, D, Gu, B, Hassett, L, and McCoy, R. Postacute Sequelae of Severe Acute Respiratory Syndrome Coronavirus 2 Infection: A State-Of-The-Art Review. JACC Basic Transl Sci (2021) 6:796. doi:10.1016/j.jacbts.2021.07.002
6. Fainardi, V, Meoli, A, Chiopris, G, Motta, M, Skenderaj, K, Grandinetti, R, et al. Long COVID in Children and Adolescents. Life (Basel) (2022) 12:285. doi:10.3390/life12020285
7.Post-COVID Conditions | CDC. Long COVID or Post-COVID Conditions (2022). Available from: https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html (Accessed January 9, 2022).
8. Fernández-De-las-peñas, C, Palacios-Ceña, D, Gómez-Mayordomo, V, Cuadrado, M, and Florencio, L. Defining Post-COVID Symptoms (Post-Acute COVID, Long COVID, Persistent Post-COVID): An Integrative Classification. Int J Environ Res Public Health 18:2621. doi:10.3390/ijerph18052621
9. Alkodaymi, M, Omrani, O, Fawzy, N, Shaar, B, Almamlouk, R, Riaz, M, et al. Prevalence of post-acute COVID-19 Syndrome Symptoms at Different Follow-Up Periods: A Systematic Review and Meta-Analysis. Clin Microbiol Infect (2022) 28:657–66. doi:10.1016/j.cmi.2022.01.014
10. Badenoch, J, Rengasamy, E, Watson, C, Jansen, K, Chakraborty, S, Sundaram, R, et al. Persistent Neuropsychiatric Symptoms after COVID-19: A Systematic Review and Meta-Analysis. Brain Commun 4:fcab297. doi:10.1093/braincomms/fcab297
11. Nguyen, N, Hoang, V, Dao, T, Dudouet, P, Eldin, C, and Gautret, P. Recurrence of SARS-CoV-2 Viral RNA in Recovered COVID-19 Patients: A Narrative Review. Eur J Clin Microbiol Infect Dis (2022) 40:13–25. doi:10.1007/s10096-020-04088-z
12. Premraj, L, Kannapadi, N, Briggs, J, Seal, S, Battaglini, D, Fanning, J, et al. Mid and Long-Term Neurological and Neuropsychiatric Manifestations of post-COVID-19 Syndrome: A Meta-Analysis. J Neurol Sci (2022) 434:120162. doi:10.1016/j.jns.2022.120162
13. Rubin, R. As Their Numbers Grow, COVID-19 “Long Haulers” Stump Experts. JAMA (2020) 324:1381. doi:10.1001/jama.2020.17709
14. Roth, P, and Gadebusch-Bondio, M. The Contested Meaning of “Long COVID” – Patients, Doctors, and the Politics of Subjective Evidence. Soc Sci Med (2022) 292:114619. doi:10.1016/j.socscimed.2021.114619
15. Xie, Y, Xu, E, Bowe, B, and Al-Aly, Z. Long-term Cardiovascular Outcomes of COVID-19. Nat Med (2022) 28:583–90. doi:10.1038/s41591-022-01689-3
16. Houben-Wilke, S, Goërtz, Y, Delbressine, J, Vaes, A, Meys, R, Machado, F, et al. The Impact of Long COVID-19 on Mental Health: Observational 6-Month Follow-Up Study. JMIR Ment Health (2022) 9(2):e33704. doi:10.2196/33704
17. Tian, T, Wu, J, Chen, T, Li, J, Yan, S, Zhou, Y, et al. Long-term Follow-Up of Dynamic Brain Changes in Patients Recovered from COVID-19 without Neurological Manifestations. JCI Insight (2022) 7:e155827. doi:10.1172/jci.insight.155827
18. Antia, R, and Halloran, M. Transition to Endemicity: Understanding COVID-19. Immunity (2021) 54:2172. doi:10.1016/j.immuni.2021.09.019
19. Auwaerter, P. The Race to Understand Post-COVID-19 Conditions. Ann Intern Med 174:1458–9. doi:10.7326/M21-3072
20. Hacker, K, Briss, P, Richardson, L, Wright, J, and Petersen, R. COVID-19 and Chronic Disease: The Impact Now and in the Future. Prev Chronic Dis (2021) 18:E62. doi:10.5888/pcd18.210086
21. Nuzzo, D, Vasto, S, Scalisi, L, Cottone, S, Cambula, G, Rizzo, M, et al. Post-acute COVID-19 Neurological Syndrome: A New Medical Challenge. J Clin Med (2021) 10:1947. doi:10.3390/jcm10091947
22. van Schalkwyk, M, and McKee, M. Research into Policy: Lessons from the COVID-19 Pandemic. Eur J Public Health (2021) 31:iv3–iv8. doi:10.1093/eurpub/ckab155
23. Ahmed, A, Song, Y, and Wadhera, R. Racial/Ethnic Disparities in Delaying or Not Receiving Medical Care during the COVID-19 Pandemic. J Gen Intern Med (2022) 37:1341–3. doi:10.1007/s11606-022-07406-7
24. Belanger, M, Hill, M, Angelidi, A, Dalamaga, M, Sowers, J, and Mantzoros, C. Covid-19 and Disparities in Nutrition and Obesity. N Engl J Med (2020) 383(11):e69. doi:10.1056/NEJMp2021264
25. Chaudhuri, K, Chakrabarti, A, Chandan, J, and Bandyopadhyay, S. COVID-19 Vaccine Hesitancy in the UK: a Longitudinal Household Cross-Sectional Study. BMC Public Health (2022) 22(1):104. doi:10.1186/s12889-021-12472-3
26. Figueroa, J, Wadhera, R, Mehtsun, W, Riley, K, Phelan, J, and Jha, A. Association of Race, Ethnicity, and Community-Level Factors with COVID-19 Cases and Deaths across U.S. Counties. Healthc (Amst) (2021) 9:100495. doi:10.1016/j.hjdsi.2020.100495
27. Gorman, J, Gorman, S, Sandy, W, Gregorian, N, and Scales, D. Corrigendum: Implications of COVID-19 Vaccine Hesitancy: Results of Online Bulletin Board Interviews. Front Public Health (2021) 10:868438. doi:10.3389/fpubh.2022.868438
28. Heller, O, Chun, Y, Shlomo, Y, Gewirtz-Meydan, A, Acri, M, Kulkarni, S, et al. Public Perceptions and the Willingness to Get Vaccinated against COVID-19: Lessons from Israel. Vaccine (2022) 40:2053. doi:10.1016/j.vaccine.2022.02.031
29. Khetan, A, Yusuf, S, Lopez-Jaramillo, P, Szuba, A, Orlandini, A, Mat-Nasir, N, et al. Variations in the Financial Impact of the COVID-19 Pandemic across 5 Continents: A Cross-Sectional, Individual Level Analysis. EClinicalMedicine (2022) 44:101284. doi:10.1016/j.eclinm.2022.101284
30. Magesh, S, John, D, Li, W, Li, Y, Mattingly-App, A, Jain, S, et al. Disparities in COVID-19 Outcomes by Race, Ethnicity, and Socioeconomic Status: A Systematic-Review and Meta-Analysis. JAMA Netw Open (2021) 4(11):e2134147. doi:10.1001/jamanetworkopen.2021.34147
31. Sudre, C, Murray, B, Varsavsky, T, Graham, M, Penfold, R, Bowyer, R, et al. Attributes and Predictors of Long COVID. Nat Med (2021) 127:626. doi:10.1038/s41591-021-01292-y
32. Thompson, EJ, Williams, DM, Walker, AJ, Mitchell, RE, Niedzwiedz, CL, Yang, TC, et al. Risk factors for long COVID: Analyses of 10 longitudinal studies and electronic health records in the UK. MedRxiv (2021). doi:10.1101/2021.06.24.21259277
33. Raveendran, A. Long COVID-19: Challenges in the Diagnosis and Proposed Diagnostic Criteria. Diabetes Metab Syndr Clin Res Rev (2021) 15(1):145–6. doi:10.1016/j.dsx.2020.12.025
34. Iqbal, F, Lam, K, Sounderajah, V, Clarke, J, Ashrafian, H, and Darzi, A. Characteristics and Predictors of Acute and Chronic post-COVID Syndrome: A Systematic Review and Meta-Analysis. EClinicalMedicine (2021) 36:100899. doi:10.1016/j.eclinm.2021.100899
35. Bahmer, T, Borzikowsky, C, Lieb, W, Horn, A, Krist, L, Fricke, J, et al. Severity, Predictors and Clinical Correlates of Post-COVID Syndrome (PCS) in Germany: A Prospective, multi-centre, Population-Based Cohort Study. eClinicalMedicine (2022) 51:101549. doi:10.1016/j.eclinm.2022.101549
36. Greenhalgh, T, Knight, M, A’Court, C, Buxton, M, and Husain, L. Management of post-acute Covid-19 in Primary Care. BMJ (2020) 370:m3026. doi:10.1136/bmj.m3026
37. O’Connor, R, Preston, N, Parkin, A, Makower, S, Ross, D, Gee, J, et al. The COVID-19 Yorkshire Rehabilitation Scale (C19-YRS): Application and Psychometric Analysis in a post-COVID-19 Syndrome Cohort. J Med Virol (2022) 94:1027. doi:10.1002/jmv.27415
38. Karmakar, M, Lantz, P, and Tipirneni, R. Association of Social and Demographic Factors with COVID-19 Incidence and Death Rates in the US. JAMA Netw Open (2021) 4:e2036462. doi:10.1001/jamanetworkopen.2020.36462
39. Ayoubkhani, D, Khunti, K, Nafilyan, V, Maddox, T, Humberstone, B, Diamond, I, et al. Post-covid Syndrome in Individuals Admitted to Hospital with Covid-19: Retrospective Cohort Study. BMJ (2021) 372:n693. doi:10.1136/bmj.n693
40. Emecen, A, Keskin, S, Turunc, O, Suner, AF, Siyve, N, Basoglu Sensoy, E, et al. The Presence of Symptoms within 6 Months after COVID-19: A Single-center Longitudinal Study. Irish J Med Sci (2022) 17:1. doi:10.1007/s11845-022-03072-0
41. Whitaker, M, Elliott, J, Chadeau-Hyam, M, Riley, S, Darzi, A, Cooke, G, et al. Persistent COVID-19 Symptoms in a Community Study of 606, 434 People in England. Nat Commun (2022) 13:1957. doi:10.1038/s41467-022-29521-z
42. Roth, S, Govier, D, Marsi, K, Cohen-Cline, H, Cook, D, Liu, Y, et al. Differences in Outpatient Health Care Utilization 12 Months after COVID-19 Infection by Race/Ethnicity and Community Social Vulnerability. Int J Environ Res Public Health (2022) 19:3481. doi:10.3390/ijerph19063481
43. Irigoyen-Camacho, M, Velazquez-Alva, M, Zepeda-Zepeda, M, Cabrer-Rosales, M, Lazarevich, I, and Castaño-Seiquer, A. Effect of Income Level and Perception of Susceptibility and Severity of COVID-19 on Stay-At-Home Preventive Behavior in a Group of Older Adults in Mexico City. Int J Environ Res Public Health (2020) 17:7418. doi:10.3390/ijerph17207418
44. Flanagan, B, Gregory, E, Hallisey, E, Heitgerd, J, and Nchhstp, C. A Social Vulnerability Index for Disaster Management. J Homeland Security Emerg Manag (2011) 8. doi:10.2202/1547-7355.1792
45. Lazar, M, and Davenport, L. Barriers to Health Care Access for Low Income Families: A Review of Literature. J Community Health Nurs (2018) 35:28. . doi:10.1080/07370016.2018.1404832
46. Magnuson, K, and Waldfogel, J. Early Childhood Care and Education: Effects on Ethnic and Racial Gaps in School Readiness. Future Child (2005) 15:169. doi:10.1353/foc.2005.0005
47. VinsonTony, T, Rawsthorne, M, Beavis, A, and Ericson, M. Jesuit Social Services, Catholic Social Services Australia. Dropping off the Edge : Persistent Communal Disadvantage in Australia (2015). Canberra: Jesuit Social Services/ Catholic Social Services Australia.
48. Muhsen, K, Na’aminh, W, Lapidot, Y, Goren, S, Amir, Y, Perlman, S, et al. A Nationwide Analysis of Population Group Differences in the COVID-19 Epidemic in Israel, February 2020-February 2021. The Lancet Reg Health Europe (2021) 7:100130. doi:10.1016/j.lanepe.2021.100130
49. Rosen, B, Waitzberg, R, Israeli, A, Hartal, M, and Davidovitch, N. Addressing Vaccine Hesitancy and Access Barriers to Achieve Persistent Progress in Israel’s COVID-19 Vaccination Program. Isr J Health Pol Res 10:43. doi:10.1186/s13584-021-00481-x
50. Waitzberg, R, Davidovitch, N, Leibner, G, Penn, N, and Brammli-Greenberg, S. Israel’s Response to the COVID-19 Pandemic: Tailoring Measures for Vulnerable Cultural Minority Populations. Int J Equity Health 19:71. doi:10.1186/s12939-020-01191-7
51. Contreras, C, Metzger, G, Beane, J, Dedhia, P, Ejaz, A, and Pawlik, T. Telemedicine: Patient-Provider Clinical Engagement during the COVID-19 Pandemic and beyond. J Gastrointest Surg 24:1692–7. doi:10.1007/s11605-020-04623-5
52. Gilmutdinova, I, Kolyshenkov, V, Lapickaya, K, Trepova, A, Vasileva, V, Prosvirnin, A, et al. Telemedicine Platform COVIDREHAB for Remote Rehabilitation of Patients after COVID-19. Eur J Transl Myol 31. doi:10.4081/ejtm.2021.9783
53. Tilden, D, Datye, K, Moore, D, French, B, and Jaser, S. The Rapid Transition to Telemedicine and its Effect on Access to Care for Patients with Type 1 Diabetes during the COVID-19 Pandemic. Diabetes Care (2021) 44:1447. doi:10.2337/dc20-2712
54. Ortega, G, Rodriguez, J, Maurer, L, Witt, E, Perez, N, Reich, A, et al. Telemedicine, COVID-19, and Disparities: Policy Implications. Health Pol Technol (2020) 9(3):368–71. doi:10.1016/j.hlpt.2020.08.001
55. Zimmermann, P, Pittet, L, and Curtis, N. The Challenge of Studying Long COVID: An Updated Review. Pediatr Infect Dis J (2022) 424. doi:10.1097/INF.0000000000003502
56. Yanes-Lane, M, Winters, N, Fregonese, F, Bastos, M, Perlman-Arrow, S, Campbell, JR, et al. Proportion of Asymptomatic Infection Among COVID-19 Positive Persons and Their Transmission Potential: A Systematic Review and Meta-Analysis. Plos One (2020) 15:e0241536. doi:10.1371/journal.pone.0241536
57.Israel Central Bureau of Statistics. Israeli Households – Selected Data [in Hebrew (2021). Available from: https://www.cbs.gov.il/he/subjects/Pages/%D7%9E%D7%A9%D7%A7%D7%99-%D7%91%D7%99%D7%AA.aspx (Accessed August 4, 2022).
Keywords: health inequalites, SARS-CoV-2, Israel, long-COVID, low-income, marginalized groups
Citation: Heller O, Chun Y, Shapira S, Troen A, Shlomo Y, Acri M, Marotta P, Kulkarni S, Kinnison B and Grinstein-Weiss M (2022) Prevalence of Long-COVID Among Low-Income and Marginalized Groups: Evidence From Israel. Int J Public Health 67:1605086. doi: 10.3389/ijph.2022.1605086
Received: 25 May 2022; Accepted: 16 November 2022;
Published: 28 November 2022.
Edited by:
Florencia Borrescio-Higa, Universidad Adolfo Ibañez, ChileReviewed by:
Wojciech Hanke, Nofer Institute of Occupational Medicine, PolandCopyright © 2022 Heller, Chun, Shapira, Troen, Shlomo, Acri, Marotta, Kulkarni, Kinnison and Grinstein-Weiss. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Oren Heller, aG9yZW5Ad3VzdGwuZWR1, b3JjaWQub3JnLzAwMDAtMDAwMi05NTc5LTk4MDk=
 Oren Heller
Oren Heller Yung Chun1
Yung Chun1 Stav Shapira
Stav Shapira