- 1Dialogik (Germany), Stuttgart, Germany
- 2Department of Geography, School of Global Affairs, Faculty of Social Science & Public Policy, King’s College London, London, United Kingdom
- 3Department of Politics and International Relations, University of Edinburgh, Edinburgh, United Kingdom
- 4Department of Safety, Economics and Planning, Faculty of Science and Technology, University of Stavanger, Stavanger, Norway
Objectives: To explore and evaluate the impact of factors including public risk perceptions on COVID-19 protective behaviors across the UK and Germany.
Methods: We used survey data collected from a representative sample for Germany and the UK (total N = 1,663) between April and May 2021. Using a Structural Equation Model, we evaluate the role of personal health risk perceptions, official message quality, source of news, age and political orientation on COVID-19 protective behaviors in the context of German and UK risk communication strategies.
Results: Personal health risk perceptions had a significant positive influence on protective behaviors. Economic risk perceptions had a negative direct influence on protective behaviors, particularly in Germany, as well as a positive indirect influence. Official message quality, use of official news sources and age had positive impacts on risk perceptions and protective behaviors. Left-wing political orientation was linked to greater likelihood of undertaking protective behaviors.
Conclusion: For future pandemics, more attention should be paid to evaluating and conceptualizing different varieties of risk perceptions, risk communication strategies, and demographic variables alongside their impacts on undertaking protective behaviors.
Introduction
On 18 March 2020, Chancellor Angela Merkel emphasized that the COVID-19 pandemic was the greatest challenge Germany faced since World War II. Similar statements were made around the world as COVID-19 became an unprecedented trans-national public health crisis. As a result, a series of regulations, information and interventions have been formulated and rolled out at the national, sub-national and regional government levels, as well as by various health authority-affiliated experts [1].
National and regional governments have responded to COVID-19 virus transmission, hospitalizations and deaths with measures that have often restricted the economy and public liberties [2, 3]. At the same time attempts to minimize the risk COVID-19 have led to extensive demands for societal cooperation [4]. Authorities and different organizations around the world communicated with the public through various channels including TV, radio and newspapers. This has led to demands for the evaluation of impacts on public health or the economy [5]. During the COVID-19 pandemic, many studies have highlighted the need for improved risk communication to heighten and maintain compliance with recommended or required protective behaviors [6–8]. Simultaneously, too little has been said about the actual impact of these interventions, especially from the perspective of the complexity of various underlying patterns of perception that lead individuals to alter their behavior.
As such, this paper aims to evaluate factors that influence likelihood of undertaking relevant COVID-19 protective behaviors, comparing Germany and the UK. Using a structural equation model (SEM), we find that although personal COVID-19 health risk perception positively influences likelihood to undertake protective behaviors in both countries, economic risk perception has a statistically significant negative direct impact on protective behaviors. These findings, alongside impacts of other barriers and drivers on protective behaviors, highlight the importance of evaluating risk perceptions of viruses such as COVID-19 through more than simply the lens of personal health risk.
Germany and the UK: Case Study
Due to the many similarities between Germany and the UK, we selected these two nations to compare government policy and societal behavior during the COVID-19 pandemic. Both nations are members of the World Health Organization and OECD. Both countries are among the world’s largest economies.
The structure of the Federal Republic of Germany is decentralized as a federal state, where 16 federal states have high levels of autonomy from their government [9]. The UK is a parliamentary democracy with three devolved governments of Northern Ireland, Scotland and Wales that have responsibility and power regarding certain policy decisions [10].
In both countries, the share of GDP on healthcare expenditure is over 10%. In Germany healthcare is mandatory for residents and is funded by statutory and private schemes. Around 88% of people hold statutory health insurance and the contribution rate is based on salary. The UK’s National Health Service (NHS) is mainly funded through taxes and free at the point of use for residents.
Before the COVID-19 pandemic, both countries had national pandemic plans for influenza which were tested during the H1N1 pandemic and revised afterward. Germany and the UK have both experienced several communicable disease outbreaks including measles and H1N1 [10].
The first confirmed COVID-19 cases in Germany and UK were announced at the end of January 2020. The first known deaths in the UK and Germany were on the 5 and 9 March respectively. The first and second waves occurred in April and November 2020 in both countries, however from mid-December 2020, the number of confirmed cases in the UK surpassed that of Germany. On 9 January 2021, the incidence rate (7-day rolling average) in the UK was 59,681, almost double as many as Germany. The daily rate of infection in the UK fell dramatically from early March until the end of May 2021, when confirmed cases were lower than seen in Germany [1, 11]. Although the cumulative trends of confirmed deaths were similar in Germany and the UK, the number of deaths in the UK were higher throughout 2020.
Germany
From January 2020, the Robert Koch Institute (RKI) provided information on COVID-19 statistics, situation and some of the regulations daily. The Federal Ministry of Health (Bundesministerium für Gesundheit, BMG), German States, local municipalities and other organizations also provided press conferences and almost daily updates on the guidelines, situation, regulations and German government’s actions in combating the COVID-19 pandemic [12].
In March 2020, the Federal and State Governments attempted better harmonization with joint guidelines. However, after about a month State governments were granted more freedom in self-determination at a local level [9]. Despite many similarities among states’ regulations, implementation varied between different municipalities of the same state across a wide range of NPIs.
Mass gathering restrictions began on 10 March 2020, and from 14 March different states implemented extensive nationwide closures of social spaces. These measures varied in different states, changing several times during the pandemic. Physical distancing of 1.5 m and a “contact ban” (avoiding physical meeting and contact) were announced by Federal and State governments on 22 March, and physical distancing advice continued throughout the pandemic. From 29 April 2020, mask wearing became mandatory in public areas such as shopping centers across Germany [9, 13].
UK
In 2020, COVID-19 communication was mostly devolved and national communication encompassing all devolved regions was only employed in occasional circumstances.
Health information about COVID-19 was provided by the NHS, while detailed statistics about the evolving situation were communicated by public health bodies. Until late June 2020, the UK Government held daily briefings. Later, the Government stated that briefings would only be held when it is required [14]. In the devolved nations daily press briefings continued for different periods of time before reducing. English COVID-19 measures changed at least 64 times between March 2020 and January 2021 [15].
Since March 2020, the government advised physical distancing of 2 m, and during 2020 people could only have close contact with the same household, extended household or bubble. On 23 March 2020 the first lockdown in the UK was announced, coming into force on 26 March 2020 where people were ordered to “stay at home.” Wearing face masks became mandatory on public transport in England on 15 June 2020, becoming mandatory in all four nations by 14 September 2020. Mitigation measures were both centralized and decentralized at different points in the pandemic, and in both Germany and the UK decisions about pandemic measures were made at the national Government level [10].
Although there were differences in the timeline and details of some mitigation measures between Germany and the UK, some of these measures were consistently employed by both authorities since the beginning of the pandemic in 2020. These include handwashing, mask wearing, avoiding physical contact, physical distancing, avoiding public spaces, gatherings, or crowds and staying at home when an individual has symptoms.
Background
Health behavior models, such as Protection Motivation Theory [16] and the Health Belief Model [17–19], have long posited the positive impact of health risk perceptions on likelihood to undertake protective actions. In this context, health risk perceptions can be analyzed in terms of perceived susceptibility, where individuals perceive themselves as at risk of serious impact of a health hazard, or perceived high likelihood of being impacted by said hazard [17, 20].
Risk perceptions can be influenced by factors including the dread and unknown characteristics of the risk itself [21, 22]. Individual characteristics, such as socio-demographic factors, knowledge, trust, values, worldviews and political beliefs and cultural differences also influence risk perceptions [23–27].
In the context of viruses, risk perceptions are consistently found to directly impact on risk-mitigating behaviors. A meta-analysis across several pandemics underscores that severity and perceived risk of serious consequences are strongly linked to behaviors [28]. Other studies also find that public perceptions of severity and likelihood of the impact of H1N1 and H5N1 respectively were significantly related to undertaking relevant protective behaviors [29, 30].
Several studies have found relationships between increased perceived health risks of COVID-19 and greater likelihood to undertake protective behaviors across multiple countries and times during the pandemic [31–35]. Contrastingly, an Indonesian study finds that risk perceptions of COVID-19 significantly influence participants’ beliefs on protective measures, but not their actual behaviour [36]. Similarly, another study finds that health risk perception had no impact on likelihood of wearing a mask in a longitudinal survey [37].
Individuals’ economic situation and distress is also related to likelihood of greater actual exposure to risks, and increased risk severity [38–40]. Social and economic impacts of COVID-19 restrictions have resulted in negative effects on motivation [41]. In a systematic review, the practicability of any non-pharmaceutical intervention (NPI) was found to be often evaluated through the lens of economic barriers to adopting behaviors, both personally and societally [42]. A Swiss study, however, suggests that increased economic risk perceptions would negatively influence likelihood to undertake protective behaviors [35]. Economic concerns about the impact of COVID-19 should therefore be considered as potential influences on probability of undertaking protective behaviors [43].
Throughout the COVID-19 pandemic, officials have justified risk communication through an instrumental perspective [1], where communication is used to achieve specific goals and targets such as policy support or behavioral compliance [44, 45]. Communicating a clear and consistent message is recommended [46], to enhance compliance [27, 47, 48]. For instance, studies undertaken earlier in the pandemic confirm the positive impact that consistency and clarity make on COVID-19 communications [6, 49]. A Vietnamese study found a significant positive relationship between increased experience of media communication and greater engagement in protective behaviors [50]. A study of Iranian respondents found a strong positive relationship between beliefs regarding risk communication and likelihood to undertake public health behaviors [51].
Increased exposure to information sources has long been linked to heightened perceptions across many risks, and news media can amplify risks [52, 53]. Greater engagement with media reporting of the COVID-19 pandemic was linked to increased risk perceptions and protective behaviors, including vaccination intention in the UK and Australia [54, 55]. Those less likely to undertake protective behaviors against COVID-19 are also those who obtained news from official sources less frequently [56]. However, individuals are more likely to obtain COVID-19 information from news media than official sources [55].
Socio-demographic factors can also influence perceptions across a wide range of risks [23, 26]. Although factors such as age are mainly studied as control variables and tend to not be strongly influential on risk perceptions [23, 57], between-group variations in risk perceptions can occur based on the nature of the risk itself [58]. Older individuals are more vulnerable to severe consequences of COVID-19, and so one may expect heightened risk perceptions among older populations because of this. However, findings on differences between age groups’ COVID-19 risk perceptions are mixed. Although a significant relationship between older age and elevated health risk perceptions of COVID-19 has been found in Germany, this is not found among a UK sample [31]. Similarly, two additional studies do not find a relationship between age and heightened health risk perceptions in the UK and Switzerland respectively [33, 34].
Similarly mixed findings are seen in the relationship between age and economic risk perceptions. Although a study of Swiss individuals finds a positive correlation between increased age and worry about the economic situation as a result of the COVID-19 pandemic [33], a US study finds that older age groups reported lower perceived likelihood of suffering personal economic harms as a result of the pandemic [59].
Although findings on variations in COVID-19 risk perceptions between age groups have been mixed and contradictory, many studies clearly show that older individuals are more likely to undertake relevant protective behaviors, while younger people are less likely to comply and display a higher probability of undertaking more risky pandemic-related activities [54, 60–62]. These findings are consistent with past research on pandemic protective behaviors [27, 28].
Political beliefs, ideology and party affiliation are found to significantly influence perceptions and behaviors across many risks, but especially in the context of climate change beliefs [26, 63, 64]. Variation in risk perceptions and behaviors between groups with varying political beliefs is likely context- and risk-dependent [65]. Studies of German respondents found a significant relationship between political ideology and likelihood of accepting or undertaking COVID-19 protective behaviors, with those reporting as more left-wing more likely to undertake behaviors [66, 67]. Similar results are found in Italy and the UK [68, 69]. However, no relationship was found between political ideology and risk perceptions [31] and compliance with government advice [70].
Overall, the main research questions this study is trying to answer are:
(1) What factors influenced the likelihood of society undertaking COVID-19 protective behaviors (PB)?
(2) What factors influence COVID-19 health risk perception (HRP)?
Hypotheses
Building upon the findings, and gaps in research identified above we formulated ten hypotheses that focus on three categories of H1: influential factors on COVID-19 protective behaviors, H2: COVID-19 health risk perception, and H3: COVID-19 economic risk perception.
H1.1 Health risk perception positively influences protective behaviors.
H1.2. Economic risk perception positively influences protective behaviors.
H1.3 Message quality perceptions positively influence protective behaviors.
H1.4 Public use of official news sources positively influences protective behaviors.
H1.5 Left-wing political orientation positively influences protective behaviors.
H1.6 Older age positively influences protective behaviors.
H2.1 Economic risk perception positively influences health risk perception.
H2.2 Message quality perceptions positively influence health risk perception.
H2.3 Public use of official news sources positively influences health risk perception.
H2.4 Older age positively influences health risk perception.
H3 Increasing age negatively influences personal economic risk perception.
Methods
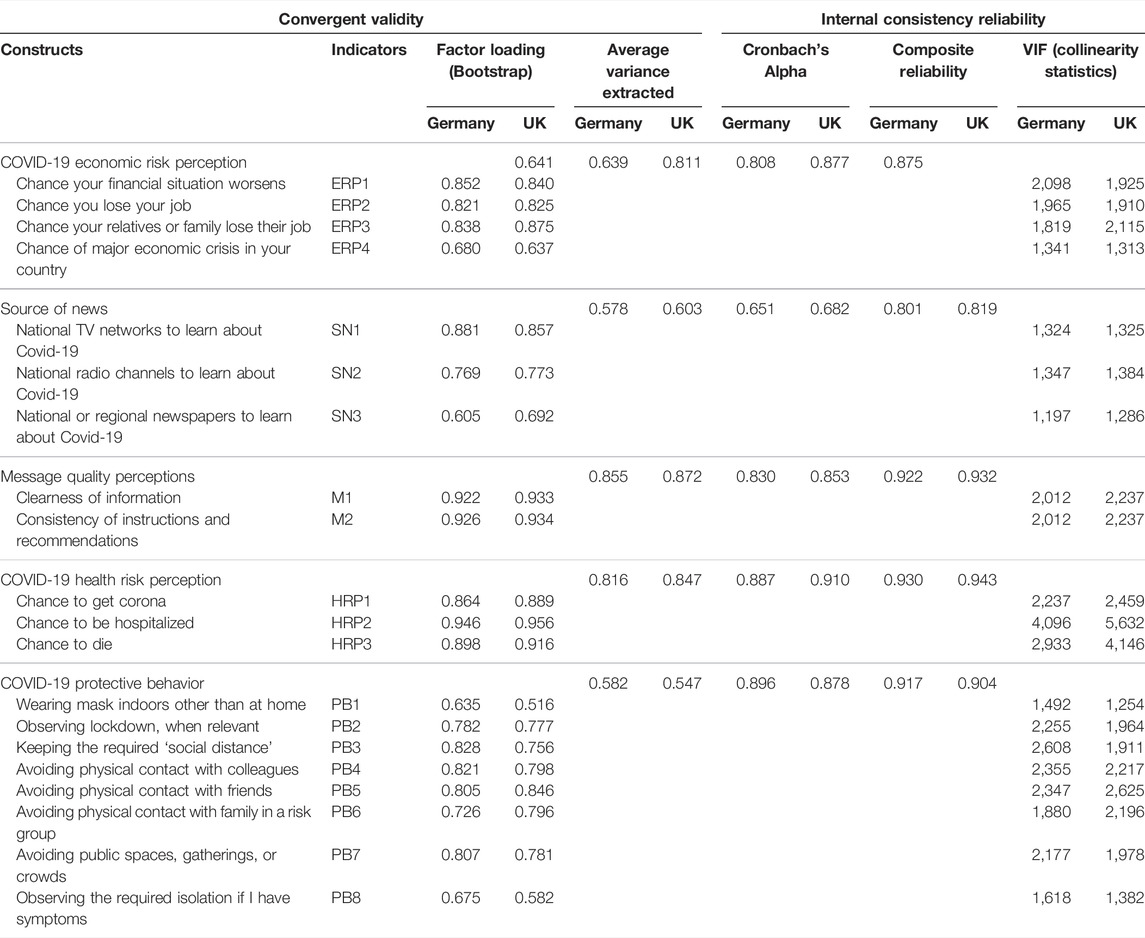
Data were collected via a survey distributed in Germany and the UK, in German and English respectively, between 1 April and 4 May 2021 through the online survey panel provider Qualtrics. Respondents were constrained with quotas based on census data in each nation to represent the population (over 18) based on age, gender, annual household income, and highest educational qualification. Duration of survey completion (at least 2/3 the median completion time) and correct answer to an attention filter in the survey were used as criteria for cleaning the collected data. The number of correctly completed questionnaires was 833 in Germany and 830 in the UK. As shown in Table 1, gender, age, having children at home, and immigration background of respondents were mostly similar in Germany and the UK. Differences between the two countries are seen in the number of respondents in the age range of 60–69, and the ratio of respondents in the at-risk group for COVID-19. The definition of “risk group” in this study is in line with public health authorities (see Table 1).
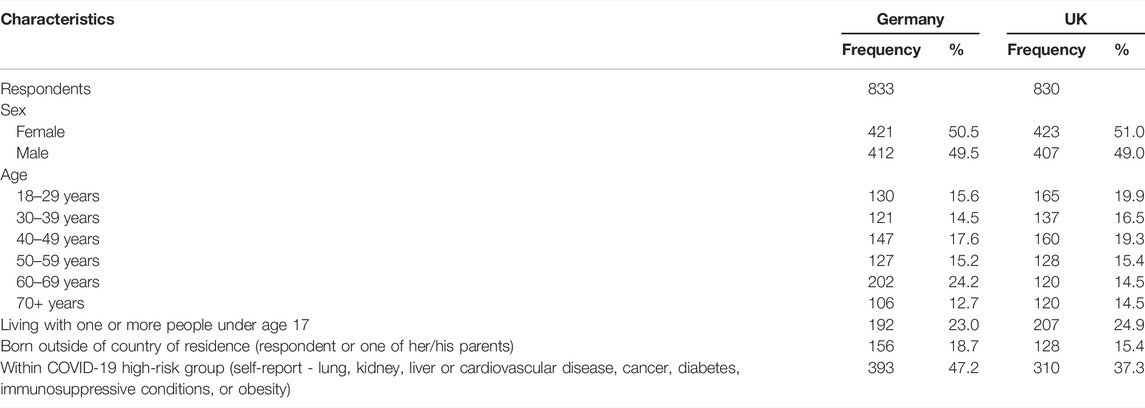
TABLE 1. Demographic distribution of respondents (Germany vs UK. 2021) (PAN-FIGHT, Germany, UK 2020–2022).
To analyze the model, a Structural Equation Model (SEM) was developed using the partial least squares (PLS) method (SmartPLS 3.3.5 program) [71]. The PLS method has the ability to handle single-item measurement, and is considered the most appropriate model for exploratory or prediction modelling [36, 72]. In the model, rectangular variables are directly measured; latent constructs (ovals) are measured by multiple indicators. Separate models were developed for each country and one Multi-Group Analysis (MGA) was undertaken to compare the countries. Figure 1 outlines the hypotheses made for this study. To see the specific question wordings and abbreviations, please refer to Table 2.
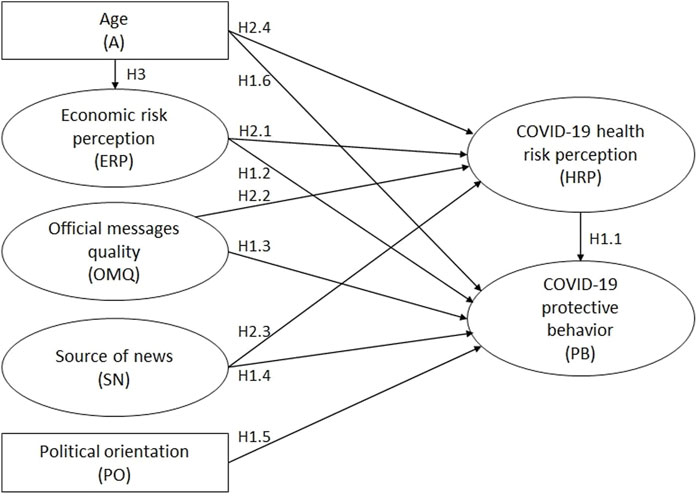
FIGURE 1. Presented model for factors influencing COVID-19 protective behaviour (Germany vs UK. 2021) (PAN-FIGHT, Germany, UK 2020–2022).
For both the German and UK SEM models, convergent validity (see Table 2) was manifest, with most loadings close to or higher than the recommended value of 0.7 [73]. The average of variance extracted exceeded 0.5 for each construct. The thresholds of higher than 0.7 for composite reliability, and higher than 0.6 for Cronbach’s Alpha were set to ensure internal consistency reliability, which the analyses met the requirements [74].
Indicators of COVID-19 health risk perception (HRP) and economic risk perception (ERP) were collected in percentile formats developed from a study of COVID-19 risk perceptions conducted by Bruine de Bruin and Bennett [31]. Official message quality (OMQ), source of news (SN), and COVID-19 protective behaviors (PB) are measured on a 5-point Likert scale. More specifically, OMQ answers ranged from 1 (not at all clear or consistent) to 5 (extremely clear and consistent), SN from 1 (not at all using national TV, radio, and newspaper as information source for COVID-19) to 5 (several times a day) and PB from 1 (never) to 5 (always). Political orientation (PO) is scaled from very left-wing to very right-wing (scale of 1–7). Age in years ranged from 18 to 84. The protective behavior items are based on government measures to mitigate the risk over the course of pandemic outlined above. These measures were also consistently communicated to the public from official platforms. For specific question wording, see the Supplementary Details for the questionnaire.
Results
The SEM analyses revealed similar results for Germany and the UK as expected (Supplementary Figures S1, S2). The results showed the R2 values (effect sizes) of ERP were 0.05 and 0.04, HRP were 0.22 and 0.28, and PB were 0.25 and 0.18 for Germany and the UK respectively. The R2 of HRP was higher in the UK than the Germany, however, PB in Germany was higher than the UK.
To answer the first research question, the results reveal positive significant effects (see Table 3) of HRP, OMQ, SN, PO, and age (A) on PB. In Germany, ERP has a significant effect on PB, while in the UK the effect is not significant (H1.1 – H1.6). Among factors influencing PB, ERP and PO have a negative effect. This means increasing economic risk perception negatively influences likelihood to undertake COVID-19 protective behaviors (H1.2), therefore the hypothesis is not supported, as a positive correlation was expected. People who consider themselves very right-wing are less likely to undertake COVID-19 protective behaviors (H1.5).
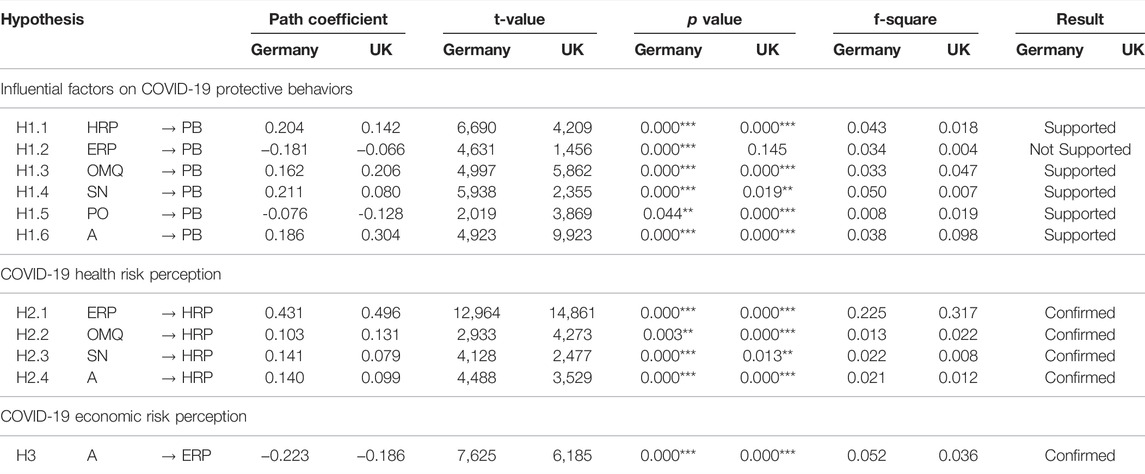
TABLE 3. Verification of proposed hypotheses - Significance level: ***p < 0.001, **p < 0.05 (Germany vs UK. 2021) (PAN-FIGHT, Germany, UK 2020–2022).
For the second research question, in both countries, ERP, OMQ, SN, and A have positive significant effects on HRP (H2.1 – H2.4). The last hypothesis (H3) indicates a significant negative effect of age on ERP, which indicates increasing age is negatively related to ERP.
Indirect effects of all variables on HRP and PB were significant. However, despite the negative significant direct effect of ERP on PB in Germany, ERP has an indirect positive effect on PB through HRP, although the indirect effect is > 0.1. It can be hypothesized that people with high economic risk perception might believe that COVID-19 restrictions damage the economy; therefore, their likelihood of undertaking protective behaviors is comparatively lower. However, as Öhman (2017) argues [75], if people have experienced one type of risk, that reaction can be transferred to other kinds of risk.
Except ERP on HRP, all individual variables had relatively small contributions to R2 values of the endogenous variables (small f2 value) which implies a small but significant contribution of the variables whose hypotheses were supported [74, 76].
MGA is used to explore the statistical differences between the proposed model in Germany and the UK. Despite many similarities between the results of the SEM model for Germany and the UK, Table 4 shows significant differences between these countries on three factors. There is a negative significant relationship of ERP on PB in Germany, but in UK no significant relationship exists. In Germany on average, people followed national sources of news about COVID-19 more than in the UK (2.92 and 2.49 on the scale of 1–5 respectively (Supplementary Table S1), where 1 means not at all and 5 means several times a day). Moreover, in Germany the effect of public use of SN on PB is greater than the UK (however significant in both countries). Finally, despite the significant effect of age on PB in both countries, the impact (beta coefficient) is greater in the UK.
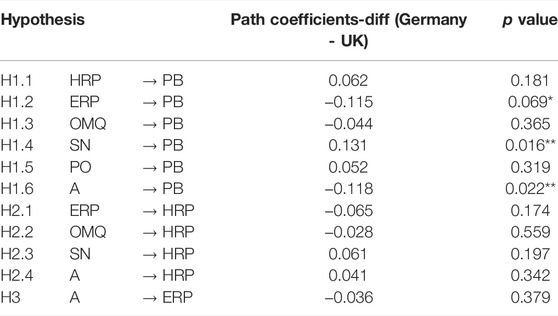
TABLE 4. Partial Least Squares Multi-Group Analyses [77] – Significance level: **p < 0.05, *p < 0.1 (Germany vs. UK. 2021) (PAN-FIGHT, Germany, UK 2020–2022).
Even after the first year of the pandemic, and despite all governments’ efforts, personal health risk perceptions were comparably low in our case study nations. However, people were generally highly likely to undertake protective behaviors (4.36 from 5-point Likert scale in both Germany and the UK). The small differences between the nations were found in PB1 and PB7, which were higher in Germany, while PB5 and PB6 were higher in the UK. In Germany people were more likely to pay greater attention to wearing masks and avoiding crowds, whereas in the UK avoiding physical contact was of the highest priority (Supplementary Table S1).
Discussion
Both Germany and the UK had experiences with previous pandemics and their pandemic plans prior to COVID-19 were tested, however the scale of the pandemic was larger than anticipated and both faced many challenges including high fatalities and infection rates alongside mask shortages.
Average health risk perceptions differed between the two nations (23% in Germany and 19% in the UK) and were slightly lower than economic risk perceptions (26% and 27.5%). In Germany, respondents tended to follow official news sources more than UK respondents (Supplementary Table S1). In general, the content of communicated messages in the two countries were similar, but not exactly the same (Supplementary Table S1). However, public perception of the clearness and consistency of communicated messages were slightly lower among German respondents than in the UK (2.6 and 2.9 respectively out of 5). This could be due to the decentralized system of government in Germany, and points to the potential impact of different states or municipalities having different measures in place at the same time [77, 78]. Long sentences, technical terms and compound words were also found to be contributory reasons why COVID-19 related press releases by the Federal Government in Germany were difficult to understand [79].
Regarding our research questions, our model supported the significant effects of COVID-19 health risk perception, official message quality, source of news, political orientation, and age on COVID-19 protective behaviors. These results are all in line with previous findings. Importantly, the strong significant positive influence of perceptions of message quality on protective behaviors across both nations offers empirical support for theoretical assertions that COVID-19 communicators must ensure clarity and consistency to promote greater compliance [6, 49]. The finding that left-wing political orientation positively influenced likelihood of undertaking protective behaviors is consistent with findings across the UK and Germany [33, 66, 67]. This points to the need for tailored, relevant and salient message frames from trusted and respected messengers when communicating risks to politically diverse groups [80, 81].
Significant positive effects of economic risk perception, official message quality, source of news and age on COVID-19 health risk perception were also discovered. There were no significant differences between the nations (Table 4), emphasizing cross-national validity of these factors’ impact on health risk perceptions. Age positively influencing HRP in both Germany and the UK differs from similar studies [32, 34, 35], highlighting potential context-based differences related to national or temporal experiences of the pandemic. The finding that age positively influences HRP, while negatively influencing economic risk perception, emphasizes the need for measuring and evaluating a range of risk perceptions.
Economic risk perception had a significant but negative direct effect on COVID-19 protective behaviors, therefore we reject this hypothesis (H1.2). This finding varies from Siegrist et al., where no effect of economic risk perceptions on protective behaviors was found [35]. The fact that the relationship is significant in Germany, but not the UK, suggests that care should be taken when considering the impact of economic risk perceptions on COVID-19 protective behaviors across national or regional boundaries. Despite this direct negative relationship in Germany, the existing indirect positive relationship between economic risk perception and protective behaviors, mediated by COVID-19 health risk perception, could have important consequences in the wake of government communicators mainly focusing on health risks associated with COVID-19.
At the beginning of the pandemic, Germany had a lower infection rate than the UK. During the first year of the pandemic, the number of confirmed cases on a 7-day rolling average were usually higher in the UK than in Germany (Supplementary Figure S3). Conversely, the UK had a higher vaccination rate than Germany while this study was conducted (51% vs. 29.5% at least partially vaccinated (Figure 2)). It is important to consider the impact of the vaccination rollout on respondents’ perceptions and optimism regarding the pandemic. According to YouGov data [83], a greater percentage of UK respondents were scared of getting COVID-19 than German counterparts in 2020 and the beginning of 2021. However, this difference narrowed after the UK started the vaccine rollout in early 2021, at a faster rate than in Germany [84]. By the end of March 2021, the rate of people fearful of catching COVID-19 was higher in Germany than in the UK. As the UK had a higher rate of vaccinated individuals than Germany when this study was conducted, this may have changed health and economic risk perceptions, views on government communication, and engagement with communicators compared to a different time in the pandemic. Similarly, German responses may have been comparatively different at a later point in time, when vaccine uptake was at a similar proportion to the UK population.
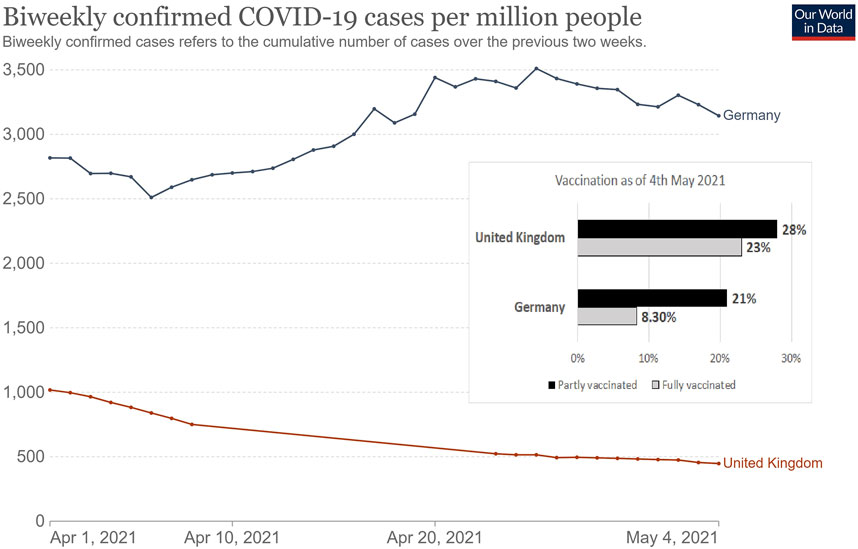
FIGURE 2. COVID-19 confirmed cases between 1st April 2021 to 4th May 2021 when our data was collected and vaccination rate by 4th May 2021 in Germany and the United Kingdom [11, 82]. Data presented by Our World in Data, licensed under the Creative Commons Attribution 4.0 International (CC BY 4.0) by Johns Hopkins University on behalf of its Center for Systems Science in Engineering (Germany vs UK. 2021) (PAN-FIGHT, Germany, UK 2020–2022).
Conclusion and Limitations
Overall, this study finds many key factors positively influencing individuals’ likelihood of undertaking COVID-19 protective behaviors, including personal health risk perceptions, official message quality, the use of official news sources, political orientation and age in both Germany and the UK. However, we discovered a negative and non-significant influence of economic risk perceptions on protective behaviors in Germany and the UK respectively. This underscores the need for a broader evaluation and consideration of risk perceptions past simply personal health risk when communicating to the public about COVID-19. This finding also cautions against applying the same risk communication strategy across multiple nations without consideration for the unique characteristics that influence protective behaviors.
Although the content of relevant COVID-19 messages communicated during the studied period were very similar in Germany and the UK [10, 12], they were not exactly the same, and this may influence public evaluations of official message quality, among other factors. Despite many similarities between Germany and the UK, there are differences in culture, religion, and political ideologies which are not taken into consideration in our evaluation of similarities and differences between the two nations.
For future pandemics, further research focus on influential factors shaping health risk perception, and their impacts on likelihood to undertake protective behaviors, is recommended. Additionally, longitudinal studies of risk perception and protective behaviors are recommended to better understand changing attitudes at different points in the pandemic. Regarding risk communication strategies, Germany could learn from how the UK government communicated to the public regarding physical distancing in the early stages of the pandemic, and the UK could learn from Germany about how to communicate to the public about mask wearing and avoiding public spaces.
The occurrence of future pandemics is inevitable. As a study of beliefs and risk perception by Attema et al. asserts, virus transmission is highly attributable to individual behaviours in the context of a pandemic such as COVID-19 [85]. To minimize virus transmission and the risk of hospitalization or death in the future, it is vital to discover not only the factors such as health risk perception which positively influenced COVID-19 protective behaviors, but also elements that could act as barriers to undertaking such protective behaviors, such as economic risk perception. Although the results of our model presented here are related to Germany and the UK, we argue that the designed model can be applied to any nation to analyze the strength of the factors in creating motivation or barriers to individual pandemic-related protective behaviors.
Author Contributions
FM and GW conceptualized and designed the study, drafted the initial manuscript, and revised the manuscript. DE and FB did some targeted manuscript writing. DE, FB, and GW designed the survey and DE and FB implemented it. FM and DE conducted exploratory data analysis. FM designed and analyzed the SEM model. All authors assisted with reviewing and editing the manuscript.
Funding
This article benefited from the support of the research project “Fighting Pandemics with Enhanced Risk Communication: Messages, Compliance and Vulnerability During the COVID-19 Outbreak” (PAN-FIGHT), which is financed by the Norwegian Research Council (Grant No. 312767).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We would like to thank many colleagues for their support: Kristin Sørung Scharffscher (University of Stavanger - UiS), Siri Wiig (UiS), Mathilde Bourrier (University of Geneva - UNIGE), Mike J. Deml (University of Geneva - UNIGE), Evangelia Petridou (Mid-Sweden University – MIUN), Jörgen Sparf (MIUN), Ole Andreas Hegland Engen (UiS), Emma Comrie (UiS), Sanjana Arora (UiS), Olena Mykolajivna Koval (UiS), Matan Shapiro (UiS).
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/ijph.2022.1604970/full#supplementary-material
References
1. Bourrier, M, Deml, M, and Mahdavian, F. Comparative Report of the Covid-19 Pandemic Responses in Germany, Norway, Sweden, Switzerland, and the United Kingdom. Stavanger: University of Stavanger (2022).
2. Nicola, M, Alsafi, Z, Sohrabi, C, Kerwan, A, Al-Jabir, A, Iosifidis, C, et al. The Socio-Economic Implications of the Coronavirus Pandemic (COVID-19): A Review. Int J Surg (2020) 78:185–93. doi:10.1016/j.ijsu.2020.04.018
3. Witteveen, D, and Velthorst, E. Economic Hardship and Mental Health Complaints during COVID-19. Proc Natl Acad Sci U S A (2020) 117(44):27277–84. doi:10.1073/pnas.2009609117
4. Heinzel, M, and Liese, A. Expert Authority and Support for COVID-19 Measures in Germany and the UK: a Survey experiment. West Eur Polit (2021) 44(5-6):1258–82. doi:10.1080/01402382.2021.1873630
5. Siegrist, M, Luchsinger, L, and Bearth, A. The Impact of Trust and Risk Perception on the Acceptance of Measures to Reduce COVID-19 Cases. Risk Anal (2021) 41(5):787–800. doi:10.1111/risa.13675
6. Abrams, EM, and Greenhawt, M. Risk Communication during COVID-19. J Allergy Clin Immunol Pract (2020) 8(6):1791–4. doi:10.1016/j.jaip.2020.04.012
7. Porat, T, Nyrup, R, Calvo, RA, Paudyal, P, and Ford, E. Public Health and Risk Communication during COVID-19 — Enhancing Psychological Needs to Promote Sustainable Behavior Change. Front Public Health (2020) 8:573397. doi:10.3389/fpubh.2020.573397
8. Warren, GW, and Lofstedt, R. Risk Communication and COVID-19 in Europe: Lessons for Future Public Health Crises. J Risk Res (2021) 1–15. doi:10.1080/13669877.2021.1947874
9. Franzke, J, and Kuhlmann, S. Håndteringen Af Covid-19 I Foråret 2020: Rapport Afgivet Af Den Af Folketingets Udvalg for Forretningsordenen Nedsatte Udredningsgruppe Vedr. Håndteringen Af Covid-19. Copenhagen: Folketinget (2021).
10. Comrie, E. United kingdom of Great Britain and Northern ireland: Country Report. Stavanger, Norway: University of Stavanger (2021).
11. Ritchie, H, Mathieu, E, Rodés-Guirao, L, Appel, C, Giattino, C, Ortiz-Ospina, E, et al. Coronavirus Pandemic (COVID-19). Our World in Data (2020). Available from: https://ourworldindata.org/coronavirus/country/germany#confirmed-deaths (Accessed March 6, 2022).
12. Mahdavian, F. Germany Country Report: Stavanger, Norway. Stavanger: University of Stavanger (2022).
13. Wieler, L, Rexroth, U, and Gottschalk, R. Emerging COVID-19 success story: the challenge of Maintaining Progress (2021). Available from: https://www.exemplars.health/emerging-topics/epidemic-preparedness-and-response/covid-19/germany (Accessed March 6, 2022).
14.BBC. Coronavirus in Wales. Mark Drakeford Gives Last Daily Press Conference: (17/07/2020). BBC News (2020). Available from: https://www.bbc.com/news/uk-wales-53447917 (Accessed June 7, 2022).
15. Syal, RE. Covid Rules Have Changed 64 Times since March, Says Barrister. The Guardian (2021). Available from: https://www.theguardian.com/world/2021/jan/12/england-covid-lockdown-rules-have-changed-64-times-says-barrister (Accessed March 31, 2022).
16. Rogers, RW. A Protection Motivation Theory of Fear Appeals and Attitude Change1. J Psychol (1975) 91(1):93–114. doi:10.1080/00223980.1975.9915803
17. Champion, VL, and Skinner, CS. The Health Belief Model. In: Glanz K, Rimer B, and Viswanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco, CA: Jossey-Bass (2008). p. 45–65.
18. Hochbaum, GM. Public Participation in Medical Screening Programs: A Sociopsychological Study, Public Health Service. Washington, DC: United States Government Printing Office (1958).
19. Rosenstock, IM. The Health Belief Model and Preventive Health Behavior. Health Educ Monogr (1974) 2(4):354–86. doi:10.1177/109019817400200405
20. Brewer, NT, Chapman, GB, Gibbons, FX, Gerrard, M, McCaul, KD, and Weinstein, ND. Meta-analysis of the Relationship between Risk Perception and Health Behavior: The Example of Vaccination. Health Psychol (2007) 26(2):136–45. doi:10.1037/0278-6133.26.2.136
21. Fischhoff, B, Slovic, P, Lichtenstein, S, Read, S, and Combs, B. How Safe Is Safe Enough - A Psychometric Study of Attitudes towards Technological Risks and Benefits. Policy Sci (1978) 9(2):127–52. doi:10.1007/bf00143739
23. Douglas, M, and Wildavsky, A. Risk and Culture: An Essay on the Selection of Technological and Environmental Dangers. Berkeley, CA: University of California Press (1982).
24. Siegrist, M, and Árvai, J. Risk Perception: Reflections on 40 Years of Research. Risk Anal (2020) 40(S1):2191–206. doi:10.1111/risa.13599
25. Siegrist, M, Gutscher, H, and Earle, T. Perception of Risk: the Influence of General Trust, and General Confidence. J Risk Res (2005) 8(2):145–56. doi:10.1080/1366987032000105315
26. Slovic, P, Finucane, ML, Peters, E, and MacGregor, DG. Risk as Analysis and Risk as Feelings: Some Thoughts about Affect, Reason, Risk, and Rationality. Risk Anal (2004) 24(2):311–22. doi:10.1111/j.0272-4332.2004.00433.x
27. van der Linden, S. The Social-Psychological Determinants of Climate Change Risk Perceptions: Towards a Comprehensive Model. J Environ Psychol (2015) 41:112–24. doi:10.1016/j.jenvp.2014.11.012
28. Bish, A, and Michie, S. Demographic and Attitudinal Determinants of Protective Behaviours during a Pandemic: A Review. Br J Health Psychol (2010) 15(4):797–824. doi:10.1348/135910710X485826
29. Rubin, GJ, Amlôt, R, Page, L, and Wessely, S. Public Perceptions, Anxiety, and Behaviour Change in Relation to the Swine Flu Outbreak: Cross Sectional Telephone Survey. BMJ (2009) 339(7713):b2651. doi:10.1136/bmj.b2651
30. Tang, CSK, and Wong, C. An Outbreak of the Severe Acute Respiratory Syndrome: Predictors of Health Behaviors and Effect of Community Prevention Measures in Hong Kong, China. Am J Public Health (2003) 93(11):1887–8. doi:10.2105/ajph.93.11.1887
31. Bruine de Bruin, W, and Bennett, D. Relationships between Initial COVID-19 Risk Perceptions and Protective Health Behaviors: A National Survey. Am J Prev Med (2020) 59(2):157–67. doi:10.1016/j.amepre.2020.05.001
32. Dryhurst, S, Schneider, CR, Kerr, J, Freeman, ALJ, Recchia, G, Bles, A, et al. Risk Perceptions of COVID-19 Around the World. J Risk Res (2020) 23(00):994–1006. doi:10.1080/13669877.2020.1758193
33. Garfin, DR, Fischhoff, B, Holman, EA, and Silver, RC. Risk Perceptions and Health Behaviors as COVID-19 Emerged in the United States: Results from a Probability-Based Nationally Representative Sample. J Exp Psychol Appl (2021) 27(4):584–98. doi:10.1037/xap0000374
34. Schneider, CR, Dryhurst, S, Kerr, J, Freeman, ALJ, Recchia, G, Spiegelhalter, D, et al. COVID-19 Risk Perception: a Longitudinal Analysis of its Predictors and Associations with Health Protective Behaviours in the United Kingdom. J Risk Res (2021) 24(3–4):294–313.
35. Siegrist, M, Luchsinger, L, and Bearth, A. The Impact of Trust and Risk Perception on the Acceptance of Measures to Reduce COVID-19 Cases. Risk Anal (2021) 41(5):787–800.
36. Adiyoso, W, and Wilopo, . Social Distancing Intentions to Reduce the Spread of COVID-19: The Extended Theory of Planned Behavior. BMC Public Health (2021) 21(1):1836. doi:10.1186/s12889-021-11884-5
37. Bearth, A, and Siegrist, M. The Drivers and Barriers of Wearing a Facemask during the SARS-CoV-2 Pandemic in Switzerland. J Risk Res (2022) 1–13.
38. Blaikie, P, Cannon, T, Davis, I, and Wisner, B. At Risk: Natural Hazards, People’s Vulnerability and Disasters. 1st ed. London: Routledge (1994).
39. Fothergill, A, and Peek, LA. Poverty and Disasters in the United States: A Review of Recent Sociological Findings. Nat Hazards (2004) 32(1):89–110. doi:10.1023/b:nhaz.0000026792.76181.d9
40. Van Bavel, JJ, Baicker, K, Boggio, PS, Capraro, V, Cichocka, A, Cikara, M, et al. Using Social and Behavioural Science to Support COVID-19 Pandemic Response. Nat Hum Behav (2020) 4:460–71. doi:10.1038/s41562-020-0884-z
41. Williams, SN, Armitage, CJ, Tampe, T, and Dienes, K. Public Perceptions and Experiences of Social Distancing and Social Isolation during the COVID-19 Pandemic: a UK-based Focus Group Study. BMJ Open (2020) 10(7):e039334. doi:10.1136/bmjopen-2020-039334
42. Teasdale, E, Santer, M, Geraghty, AWA, Little, P, and Yardley, L. Public Perceptions of Non-pharmaceutical Interventions for Reducing Transmission of Respiratory Infection: Systematic Review and Synthesis of Qualitative Studies. BMC Public Health (2014) 14(1):589. doi:10.1186/1471-2458-14-589
43. Siegrist, M, and Bearth, A. Worldviews, Trust, and Risk Perceptions Shape Public Acceptance of COVID-19 Public Health Measures. Proc Natl Acad Sci U S A (2021)(24) 118. doi:10.1073/pnas.2100411118
44. Demeritt, D, and Nobert, S. Models of Best Practice in Flood Risk Communication and Management. Environ Hazards (2014) 13(4):313–28. doi:10.1080/17477891.2014.924897
45. Wardman, JK. The Constitution of Risk Communication in Advanced liberal Societies. Risk Anal (2008) 28(6):1619–37. doi:10.1111/j.1539-6924.2008.01108.x
46. Vaughan, E, and Tinker, T. Effective Health Risk Communication about Pandemic Influenza for Vulnerable Populations. Am J Public Health (2009) 99:S324–32. doi:10.2105/AJPH.2009.162537
47. Mileti, DS, and Sorensen, JH. Communication of Emergency Public Warnings: A Social Science Perspective and State-Of-The-Art Assessment. Oak Ridge, TN: FEMA (1990).
48. Slovic, P. Perceived Risk, Trust, and Democracy. Risk Anal (1993) 13(6):675–82. doi:10.1111/j.1539-6924.1993.tb01329.x
49. Ratzan, SC, Gostin, LO, Meshkati, N, Rabin, K, and Parker, RM. COVID-19: An Urgent Call for Coordinated, Trusted Sources to Tell Everyone what They Need to Know and Do. J Health Commun (2020) 25(10):747–9. doi:10.1080/10810730.2020.1894015
50. Thanh, PT, and Tung, LT. Can Risk Communication in Mass media Improve Compliance Behavior in the COVID-19 Pandemic? Evidence from Vietnam. Int J Sociol Soc Pol (2021). doi:10.1108/ijssp-05-2021-0122
51. Heydari, ST, Zarei, L, Sadati, AK, Moradi, N, Akbari, M, Mehralian, G, et al. The Effect of Risk Communication on Preventive and Protective Behaviours during the COVID-19 Outbreak: Mediating Role of Risk Perception. BMC Public Health (2021) 21(1):54. doi:10.1186/s12889-020-10125-5
52. Combs, B, and Slovic, P. Newspaper Coverage of Causes of Death. Journalism Q (1979) 56(4):837–49. doi:10.1177/107769907905600420
53. Kasperson, RE, Renn, O, Slovic, P, Brown, HS, Emel, J, Goble, R, et al. The Social Amplification of Risk: A Conceptual Framework. Risk Anal (1988) 8(2):177–87. doi:10.1111/j.1539-6924.1988.tb01168.x
54. Allington, D, McAndrew, S, Moxham-Hall, VL, and Duffy, B. Media Usage Predicts Intention to Be Vaccinated against SARS-CoV-2 in the US and the UK. Vaccine (2021) 39(18):2595–603. doi:10.1016/j.vaccine.2021.02.054
55. Faasse, K, and Newby, J. Public Perceptions of COVID-19 in Australia: Perceived Risk, Knowledge, Health-Protective Behaviors, and Vaccine Intentions. Front Psychol (2020) 11:551004. doi:10.3389/fpsyg.2020.551004
56. Kleitman, S, Fullerton, DJ, Zhang, LM, Blanchard, MD, Lee, J, Stankov, L, et al. To Comply or Not Comply? A Latent Profile Analysis of Behaviours and Attitudes during the COVID-19 Pandemic. Plos One (2021) 16(7):e0255268. doi:10.1371/journal.pone.0255268
57. Olofsson, A, and Rashid, S. The white (Male) Effect and Risk Perception: Can equality Make a Difference? Risk Anal (2011) 31(6):1016–32. doi:10.1111/j.1539-6924.2010.01566.x
58. Savage, I. Demographic Influences on Risk Perceptions. Risk Anal (1993) 13(4):413–20. doi:10.1111/j.1539-6924.1993.tb00741.x
59. Bruine de Bruin, W. Age Differences in Covid-19 Risk Perceptions and Mental Health: Evidence from a National u.S. Survey Conducted in March 2020. J Gerontol B Psychol Sci Soc Sci (2021) 76(2):e24–9. doi:10.1093/geronb/gbaa074
60. Gamsızkan, Z, Sungur, MA, and Erdemir, G. How Do Older Age, Gender and Risk Groups Affect Protective Behaviours and Mental Health in the COVID‐19 Pandemic? Int J Clin Pract (2021)(6) 75. doi:10.1111/ijcp.14150
61. Trifiletti, E, Shamloo, SE, Faccini, M, and Zaka, A. Psychological Predictors of Protective Behaviours during the Covid‐19 Pandemic: Theory of Planned Behaviour and Risk Perception. J Community Appl Soc Psychol (2021) 32:382–97. doi:10.1002/casp.2509
62. Wise, T, Zbozinek, TD, Michelini, G, Hagan, CC, and Mobbs, D. Changes in Risk Perception and Self-Reported Protective Behaviour during the First Week of the COVID-19 Pandemic in the United States. R Soc Open Sci (2020) 7(9):200742. doi:10.1098/rsos.200742
63. Choma, B, Hodson, G, Jagayat, A, and Hoffarth, MR. Right‐Wing Ideology as a Predictor of Collective Action: A Test across Four Political Issue Domains. Polit Psychol (2020) 41(2):303–22. doi:10.1111/pops.12615
64. Leiserowitz, AA. Climate Change Risk Perception and Policy Preferences: The Role of Affect, Imagery, and Values. Climatic Change (2006) 77(1–2):45–72. doi:10.1007/s10584-006-9059-9
65. Choma, BL, Hanoch, Y, Gummerum, M, and Hodson, G. Relations between Risk Perceptions and Socio-Political Ideology Are Domain- and Ideology- Dependent. Personal Individual Differences (2013) 54(1):29–34. doi:10.1016/j.paid.2012.07.028
66. Dohle, S, Wingen, T, and Schreiber, M. Acceptance and Adoption of Protective Measures during the COVID-19 Pandemic: The Role of Trust in Politics and Trust in Science. Soc Psychol Bull (2020) 15(4). doi:10.32872/spb.4315
67. Liekefett, L, and Becker, J. Compliance with Governmental Restrictions during the Coronavirus Pandemic: A Matter of Personal Self‐protection or Solidarity with People in Risk Groups? Br J Soc Psychol (2021) 60(3):924–46. doi:10.1111/bjso.12439
68. Rubaltelli, E, Tedaldi, E, Orabona, N, and Scrimin, S. Environmental and Psychological Variables Influencing Reactions to the COVID‐19 Outbreak. Br J Health Psychol (2020) 25(4):1020–38. doi:10.1111/bjhp.12473
69. Schneider, SH, Eger, J, Bruder, M, Faust, J, and Wieler, LH. Does the COVID-19 Pandemic Threaten Global Solidarity? Evidence from Germany. World Development (2021) 140:105356. doi:10.1016/j.worlddev.2020.105356
70. Harper, CA, Satchell, LP, Fido, D, and Latzman, RD. Functional Fear Predicts Public Health Compliance in the COVID-19 Pandemic. Int J Ment Health Addict (2021) 19(5):1875–88. doi:10.1007/s11469-020-00281-5
71. Ringle, CM, Wende, S, and Becker, J-M. SmartPLS 3. Boenningstedt: SmartPLS (2022). Available from: https://www.smartpls.com (Accessed March 31, 2022).
72. Hair, JF, Hult Gt, M, Ringle C, M, Sarstedt, M, Castillo Apraiz, J, Cepeda Carrión, GA, et al. Manual de Partial Least Squares Structural Equation Modeling (PLS-SEM) (Segunda Edición). Terrassa, Spain: OmniaScience (2019).
73. Wong, KK-K. Mastering Partial Least Squares Structural Equation Modeling (PLS-SEM) with SmartPLS in 38 Hours. Bloomington: IUniverse (2019).
74. Dakduk, S, González, Á, and Portalanza, A. Learn about Structural Equation Modeling in SmartPLS with Data from the Customer Behavior in Electronic Commerce Study in ecuador. London: SAGE Publications, Ltd (2017).
75. Öhman, S. Previous Experiences and Risk Perception : The Role of Transference. J Educ Soc Behav Sci (2017) 23(1):1–10. doi:10.9734/JESBS/2017/35101
76. Sarstedt, M, Ringle, CM, and Hair, JF. Partial Least Squares Structural Equation Modeling. In: C. Homburg, M. Klarmann, and A. Vomberg, editors Handbook of Market Research. Cham: Springer (2021). p. 1–47.
77. Henseler, J, Ringle, CM, and Sinkovics, RR. The Use of Partial Least Squares Path Modeling in International Marketing. advances Int marketing (2009) 20:277–319. doi:10.1108/s1474-7979(2009)0000020014
78. Warren, GW, Lofstedt, R, and Wardman, JK. COVID-19: the winter Lockdown Strategy in Five European Nations. J Risk Res (2021) 24(3-4):267–93. doi:10.1080/13669877.2021.1891802
79. Brettschneider, F, and Keller, K. Die (Un-)Verständlichkeit der Corona-Kommunikation: Eine Analyse der Pressemitteilungen der Bundesregierung (Comprehensibility of Corona communication: An analysis of the press releases of the federal government) 2020-2021. Hohenheim: Universität Hohenheim (2021).
80. Slothuus, R, and De Vreese, CH. Political Parties, Motivated Reasoning, and Issue Framing Effects. J Polit (2010) 72(3):630–45. doi:10.1017/s002238161000006x
81. Whitmarsh, L, and Corner, A. Tools for a New Climate Conversation: A Mixed-Methods Study of Language for Public Engagement across the Political Spectrum. Glob Environ Change (2017) 42:122–35. doi:10.1016/j.gloenvcha.2016.12.008
82. Dong, E, Du, H, and Gardner, L. An Interactive Web-Based Dashboard to Track COVID-19 in Real-Time. Lancet Inf Dis (2020) 20(5):533–4. doi:10.1016/S1473-3099(20)30120-1
83.YouGov. COVID-19 Fears. YouGov (2020). Available from: https://yougov.co.uk/topics/international/articles-reports/2020/03/17/fear-catching-covid-19.
84. Warren, GW, and Lofstedt, R. COVID-19 Vaccine Rollout Management and Communication in Europe: One Year on. J Risk Res (2021) 1–20. doi:10.1080/13669877.2021.2001674
Keywords: risk perception, COVID-19, structural equation modelling, risk communication, protective behaviors
Citation: Mahdavian F, Warren GW, Evensen D and Bouder FE (2022) The Relationship Between Barriers and Drivers of COVID-19 Protective Behaviors in Germany and the UK. Int J Public Health 67:1604970. doi: 10.3389/ijph.2022.1604970
Received: 31 March 2022; Accepted: 16 August 2022;
Published: 08 September 2022.
Edited by:
Katharina Jungo, Universität Bern, SwitzerlandReviewed by:
Bako Rajaonah, Université Polytechnique Hauts-de-France, FranceJie Yin, Huaqiao University, China
Wignyo Adiyoso, Ministry of National Development Planning of the Republic of Indonesia, Indonesia
Copyright © 2022 Mahdavian, Warren, Evensen and Bouder. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Frederic E. Bouder, ZnJlZGVyaWMuYm91ZGVyQHVpcy5ubw==
This Review is part of the IJPH Special Issue “Responses to the COVID-19 Pandemic: International Comparisons.”
 Farnaz Mahdavian
Farnaz Mahdavian George W. Warren2
George W. Warren2 Darrick Evensen
Darrick Evensen Frederic E. Bouder
Frederic E. Bouder