- 1CEISUC - Centre for Health Studies and Research, University of Coimbra, Coimbra, Portugal
- 2ISEG, UL - Lisbon School of Economics and Management, University of Lisbon, Lisbon, Portugal
- 3FEUC - Faculty of Economics, University of Coimbra, Coimbra, Portugal
- 4USF Marquês de Marialva, ACES Baixo Mondego, Coimbra, Portugal
Objectives: This work sets out to find the relationship between taking non-prescribed drugs and predisposing, enabling and need factors. Specifically, our main aim is to find the relationship between taking non-prescribed drugs and the lack of health care.
Methods: We used data from the last 2019 National Health Survey and estimate logistic regressions for the whole sample and stratified by sex.
Results: The most striking finding is that people self-medicating with non-prescribed drugs seem to be replacing health care when this is not used because of financial constraints or distance from provider. This suggests that non-prescribed drugs are a fast, affordable, alternative to health care. Other findings show that income and the financial resources to cope with unexpected expenditure are considerations in taking these drugs. Health and needs are other factors triggering their consumption.
Conclusion: Policy measures need to be aimed at improving access to medical care, providing responses to health needs such as those arising from chronic pain, and improving health literacy.
Highlights
1) People self-medicating with OTC seem to be substituting health care because of financial and distance constraints.
2) Income and the financial capacity to cope with unexpected expenditure are associated with taking OTC drugs.
3) Sleeping problems, chronic pain, and using an emergency contraceptive pill are drivers for taking OTC drugs.
Introduction
A strategic change in the pharmaceutical market that has occurred in recent years is the switch from prescription drugs (Rx) to over-the-counter (OTC) drugs (1). Additionally, the OTC market has been liberalized (in Portugal since 2005) meaning that OTC drugs can be sold by retailers as well as by community pharmacies. These changes have been followed by another social and medical change, namely the promotion of self-medication (SM). This is the selection and use of drugs by an individual to treat self-recognized illnesses or symptoms, without consulting a doctor (2, 3). These symptoms include pain, allergies, migraine, skin conditions, fungal infections, cold symptoms, fever control, heartburn, and dyspepsia (4). However, the practice of SM not only includes the use of OTC but also Rx drugs which people may acquire improperly, without prescription (3). In our work, we focus on OTC, or also referred as nonprescribed drugs, and disregard drugs requiring prescription such as antibiotics, that is, our focus is on drugs which can be bought without prescription. Some of these OTC may be prescribed, such as vitamin D, but this alternative is not covered because this purchase is based on a prescription.
SM with OTC consumption has several advantages. On the one hand it saves the opportunity cost of the time which physicians spend taking care of minor illnesses, and at the same time it saves people having to take time to go to medical appointments, as well as the possible payment for the appointment (5). On the other hand, it gives people power over their health and so it has benefits for their labour productivity (6). Despite these well-recognized advantages, SM poses risks and disadvantages for peoples’ health. These include making a wrong diagnosis, taking the wrong amount of a drug, polypharmacy, adverse reactions and drug interactions, addiction, abuse and overdose, and also delaying correct diagnosis by masking other severe health conditions (4, 5).
In Portugal, the OTC market represents about a quarter of the whole pharmaceutical market (volume), while a quarter of the OTC market involves analgesics and antipyretics, and about 15% to topical application (7). OTC drugs are sold in community pharmacies and other authorized retailers, such as drug outlets and supermarkets; advertising OTC is possible under certain conditions and rules, and buyers must be older than 16 years of age (8). The Portuguese health system is defined as a Beveridge-type national health service, and it is facing some well-identified challenges (9, 10) such as waiting lists, unreasonable time to get an appointment, unavailability of general practitioners, unmet health needs, and high cost-sharing of prescribed pharmaceuticals.
Given this contextual and institutional framework that characterizes the country’s health system, the aim of our analysis is to find the factors associated with self-medication and OTC consumption. More specifically, we aim to test the possible substitutive relationship between the lack of health care and OTC provision, and to understand the role of individual health needs and health in the consumption of OTC drugs in Portugal.
The conceptual model that sustains our analysis is the Behavioral Model of Health Services Use suggested by R. Andersen in 1968 (11). Since then, the model has been updated and adjusted (12), and used to support different empirical studies, including those related to self-care (13–18). Andersen’s model includes three major factors that influence the use of health services at both the individual and contextual levels, namely, 1) predisposing, 2) enabling, and 3) need factors (11, 12, 14) as shown in Figure 1. Predisposing factors mainly include demographic and community characteristics; enabling factors are related to the financing and organizational characteristics which are conditions for enabling and facilitating the use of pharmacies and other shops to sell medicaments OTC; needs are the factors that result in the action to self-medicate and to consume OTC medicines, which are related to the type and duration of illness or symptoms.
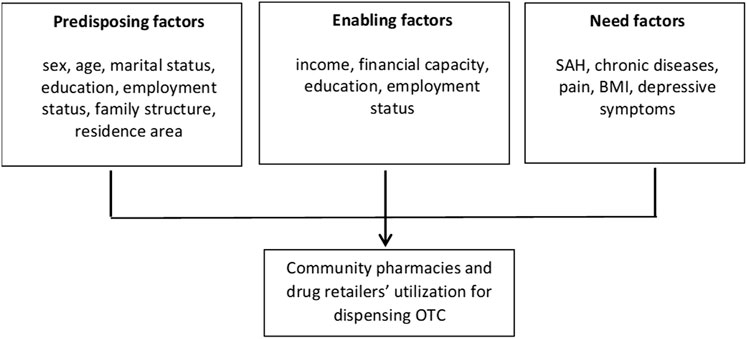
FIGURE 1. Conceptual framework of Anderson’s Behavioral Model of Health Services Use (Portugal, 2022).
A large number of studies on self-medication are focused on low-to-medium-income countries and few of them are aimed at high-income countries (19). Empirical evidence concerning demographic, economic and medical care factors as drivers for OTC use or self-medication in Europe is diversified but some results are aligned. Whereas in Eastern European countries, Austria and in the UK, men tend to self-medicate more often than women (20–22), the opposite is true in Spain (23, 24), and it has no statistical significance in Portugal (25). We find that older people are more likely to take non-prescribed drugs in countries such as Bulgaria, Slovakia and the UK (20, 22), while in others, like Spain (24) and Austria (21), such tendency is not found. In general, better education and higher income are associated with a greater probability of taking OTC drugs (20–25).
This type of concern is more often found in studies for low-to-medium-income countries (19). The influence of medical care on SM has been given little attention in European countries because of the universal coverage of health systems. In Spain and Serbia (24, 26) findings point to a negative relationship between medical consultation and self-medication, but in Austria (21) the opposite happens, and in Portugal (25) no statistical significance is found. From a worldwide perspective (19), difficult access to medical care is an important driver of self-medication.
The importance of health and health needs in SM has captured more attention in European studies. The findings point towards a general association between lower health status and chronic diseases and OTC consumption (20–22).
Methods
Data and Sample
The data used in this analysis were collected by the 2019 National Health Survey. The National Health Survey applied a sampling method based on stratification and multistage data collection to ensure that it is representative of the Portuguese population (27). Data were collected between September 2019 and January 2020. This survey is standardized and regulated at European level (European Parliament and European Council Regulation no 1338/2008; European Commission Regulation no 2018/255). It includes 14,617 non-institutionalized individuals older than 15.
Our sample considers respondents aged over 18, so it includes 14,275 individuals. We excluded 276 minors aged between 15 and 17, because not only do they not have complete autonomy in deciding on the consumption of OTC drugs, but they usually do not have the financial autonomy to buy those drugs either (unless provided by parents). We also excluded 66 pregnant women (of whom only 11 took OTC medicines) because it was assumed that they are only supposed to take OTC under medical supervision.
Outcome Variable
The outcome variable measures the decision to self-medicate and to consume OTC medicines. This variable is obtained from the following question: “In the last 2 weeks, did you take any drug, natural medicine or vitamins which were not prescribed by a physician? (Do not include birth control pills or other birth control hormones).” The answer is binary, meaning, “yes” or “no”. This variable is labelled as “OTC”.
Independent Variables
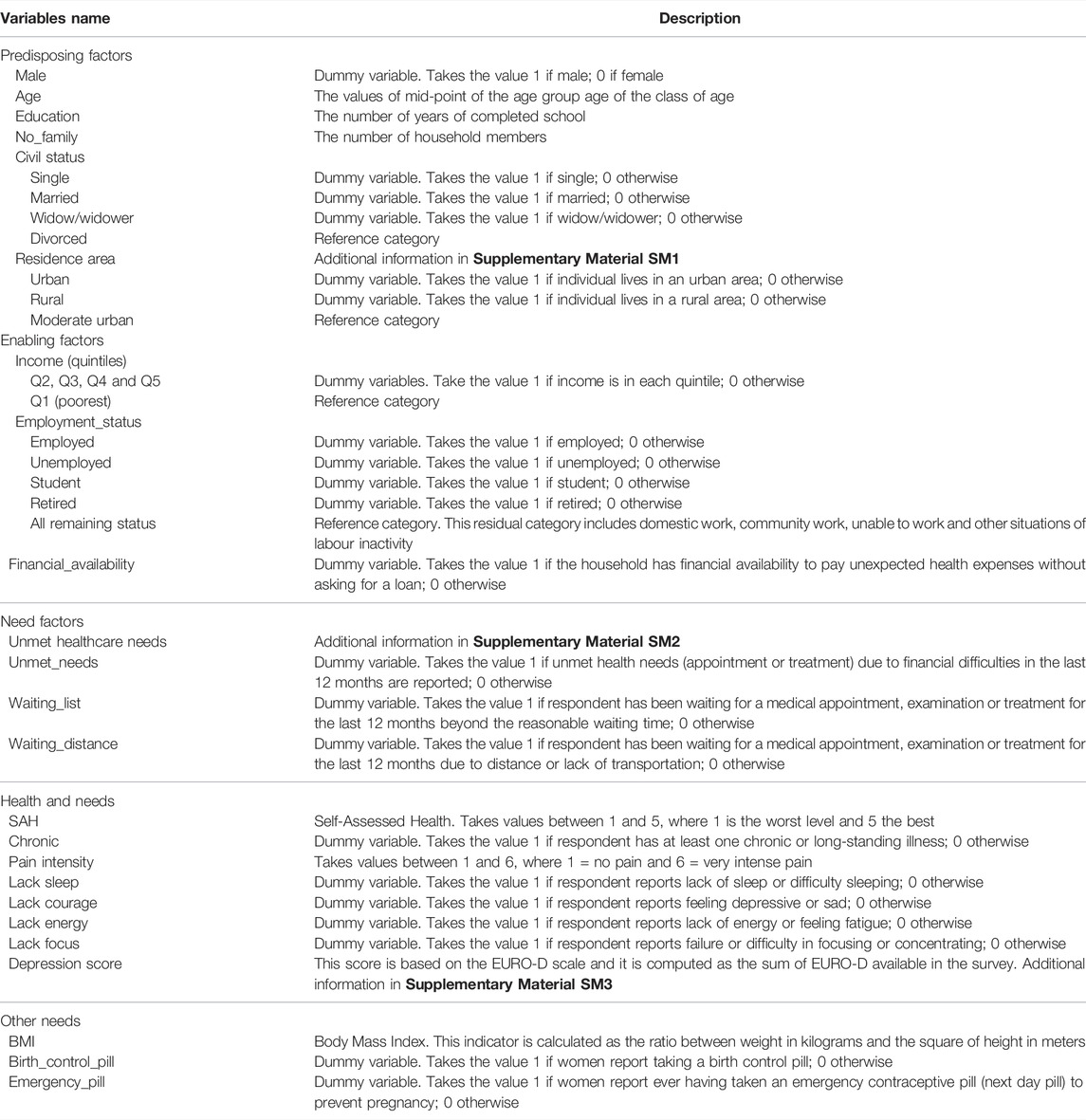
The set of independent variables were divided into three groups: predisposing, enabling, and need according to Anderson’s Behavioral Model of Health Services Use. These variables are listed in Figure 1 and described in Table 1.
Some points about some of the independent variables are worth mentioning.
Firstly, looking at the variable of age, which is collected and provided in age classes, we considered the mid-point value of the age class because when using the factorial variables for age class, the level of multicollinearity exceeds the accepted level for the value of inflated factor (VIF test). The value for the oldest class is taken to be 85 which is the floor value of the age interval.
Secondly, although the question about whether the respondent took OTC medicines clearly excludes the birth control pill and other women’s hormones, we tested a possible relationship between the responses to OTC questions and the responses given by women taking the pill and the emergency contraceptive pill. We consider taking contraceptives as a need to prevent pregnancy. Women taking the pill need to go to the pharmacy more often and those who take the emergency contraceptive pill have a learning experience on accessing OTC drugs in community pharmacies. In this way, women may be more willing to demand OTC, either due to a more frequent relationship with the pharmacist or due to more frequent opportunity to buy drugs.
Thirdly, we have considered BMI in the ‘need factors’ group because high levels of BMI, either measurable or perceived by people, may create an urge to reduce weight, which may motivate a demand for weight-reducing drugs.
Additionally, we have considered other perceived needs which may trigger individuals to seek OTC drugs, needs such as, lack of sleep, lack of courage/well-being, lack of energy, and lack of focus, for which there are specific OTC remedies. Besides these needs, we have also computed a depression score based on EURO-D scale to measure depression in the individual. Our score (“depression_score”) is a sort of reduced EURO-D because it does not include all EURO-D items (28). For a more detailed explanation see Supplementary Material SM2.
Quantitative Analysis
The analysis performed in this work is divided into two main sections. In the first section we present the results obtained from a descriptive statistic.
Next, we estimate a logistic regression for all the sample, for each sex and also for the people aged less than 80. First, we separate women and men because men do not buy or take birth control pills and there are sex differences in the access and utilization of preventive health care services (29). So, we take sex differences as given by previous empirical work and we do not aim to test sex differences (30, 31). Second, we exclude very old seniors (that is, older than 80) to prevent any kind of age bias. We consider an estimation including ‘depression score’ instead of single needs related to mental health.
A VIF test is performed to test multicollinearity across independent variables. The linktest is used for testing specification errors and the Hosmer-Lemeshow is applied for goodness-of-fit test. The reported standard errors are robust to mitigate any heteroscedasticity. Finally, the results are reported using odds-ratios (OR), and 95% confidence intervals (CI) and p-values are also displayed. All the analyses presented in this work are performed in STATA 16.
Results
Descriptive Analysis
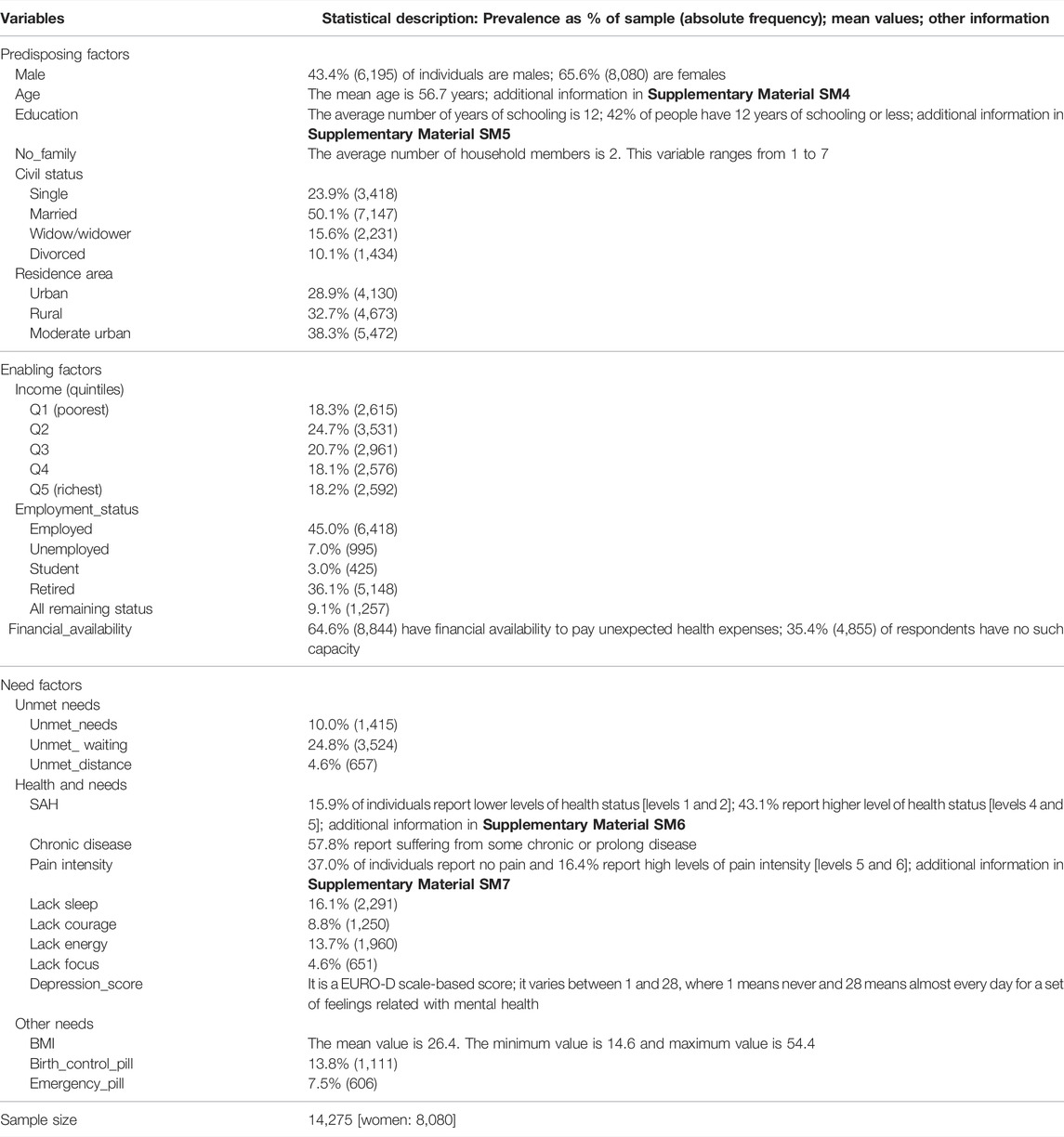
The number of people acknowledging that they took non-prescribed drugs was 3,208, which accounts for about 22.5% of our sample of 14,275 people. Of these, most are women, about 63%.
A statistical description of the set of independent variables is presented in Table 2. Of these, we would like to highlight the statistics showing the lack of health care that people report. More than 4% of people indicate waiting for an appointment, treatment, or medical exam due to long distance or lack of transport as factors; nearly 25% of people report waiting for health care beyond the reasonable time, meaning that they are on a waiting list for too long, and about 10% of people report being unable to cope with their health needs due to financial difficulties.
Estimated Results
The results obtained from the VIF test for testing potential multicollinearity across independent variables is presented in Supplementary Appendix Table SA1. There is no evidence for multicollinearity. The pairwise correlations between non-binary variables are presented in Supplementary Appendix Table SA2.
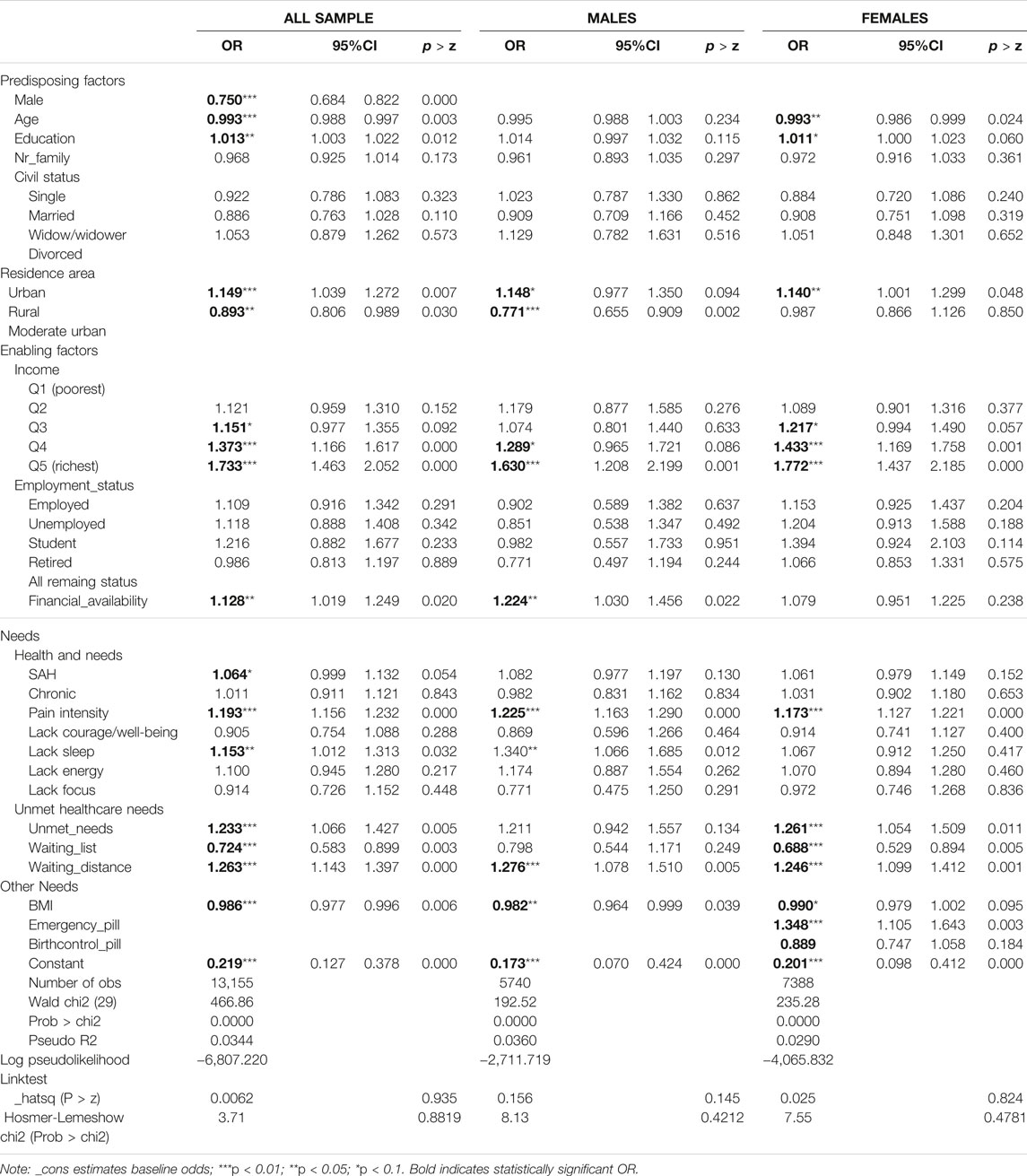
The results for the estimated logistic regression are presented in Table 3, for the whole sample and for women and men separately.
We begin by presenting the results related to need factors, specifically the unmet healthcare needs. The most relevant results show there is a significant correlation between taking OTC medicines and (the lack of) health care. There seems to be a substitution effect between OTC consumption and both unmet health care needs due to financial constraint, and waiting for health care due to long distance; the relationship between waiting for health care on a waiting list has a complementary effect. In other words, people who report unmet healthcare needs because of financial difficulties or experience lack of health care due to distance are more likely to report taking OTC remedies than those who do not report those deficits in health care by a odds ratio (OR) equal to about 1.2.
On the other hand, people reporting waiting for medical care for longer than a reasonable time are less likely to report taking OTC drugs by a OR equal to 0.724. These relationships are found in women, but they are not statistically significant in the estimation for men, except for the case of waiting for health care due to long distance or lack of transport.
Regarding the influence of health and needs on OTC consumption, we found that painkillers are common OTC drugs because of the increasing likelihood of OTC purchases associated with pain intensity, by a OR of 1.193. We also found that the need to sleep motivates a demand for OTC drugs, although this tendency was not found significant for women. We tested the model to include the depression score and we found a positive association between this score and taking OTC medicines (results presented in Supplementary Material SM8), meaning that demand for OTC increases with the number of depression symptoms (OR is equal to 1.036 for p-value less than 0.0001).
Regarding the relevance of other needs, our results show that higher BMI is associated with a lower likelihood of taking OTC products, despite the estimated factor being very close to value 1. In the case of OTC drugs taken by women, we found that women taking an emergency birth-control pill are more likely to take an OTC drug by a OR of 1.348 than women who do not use this type of pill.
With respect to enabling factors, as expected people reporting higher incomes or financial ability to deal with unexpected health expenses are more likely to report buying OTC, except for women, for whom financial ability has no statistical significance.
With reference to the predisposing factors, we found that men and older people are less likely to buy drugs OTC; people with higher levels of education are more likely to choose OTC remedies. Finally, those who live in urban areas are more likely to buy OTC products while those who live in rural areas are less likely to do so than those living in moderate urban areas.
Closing this section, the model specification test (link test) and goodness-of-fit test (Hosmer-Lemeshow) show that the model has a high goodness-of-fit and is well specified. We also tested the model using a sample including people younger than 80 and the results are identical and in line with those presented above (results displayed in Supplementary Material SM8).
Discussion
Self-medication by consuming OTC drugs is a widespread phenomenon in Europe as more Rx drugs are shifted into OTC providers and people are increasingly empowered over their health. There is little empirical evidence about the factors associated with taking non-prescribed drugs in different countries in Europe. Portugal has a specific institutional structure which is characterized by a national health service with universal coverage, but small cost sharing for prescribed pharmaceuticals, and OTC medicines are easily sold in pharmacies and authorized retailers. We aimed to find the predisposing, enabling and need factors associated with the consumption of non-prescription drugs and to test its relationship with the lack of health care.
Key Findings
The most relevant result concerns, first, a substitutive relationship between taking OTC and facing healthcare needs that are not met because of financial constraints and long distance and/or lack of transport. Secondly, we found a complementary relationship between taking OTC remedies and experiencing unmet health care arising from being placed on a waiting list.
Other results show the importance of other need factors, such as pain intensity, lack of sleep, and pregnancy concerns. Additionally, some predisposing and enabling factors may also play a role in an OTC purchasing decision.
Interpretation
Firstly, the main findings concern the correlation between the consumption of OTC drugs and unmet health care needs. We found a substitution relationship between OTC drugs and unmet healthcare needs due to financial difficulties or long distance, and a complementary relationship between OTC drugs and unmet health care due to waiting lists.
These findings show that people may choose to take OTC drugs to replace medical care due to financial and distance/transport constraints, which may indicate that OTC remedies are an affordable and faster alternative for health care. This result has been found before in low-medium income countries and those with weak social welfare (19), and it certainly raises concerns for policymakers and health professionals. Delaying medical care is a serious option as it delays diagnosis and worsens health conditions, which should be prevented. A less expected finding, but one which raises less concern, is the correlation between consuming OTC products and the waiting time for medical care beyond what is reasonable. People seem to stay on hold, expecting a medical assessment of their problem, waiting for a medical intervention or diagnosis. There may be some fear about masking illness conditions, or even speeding up illness. Waiting for a medical appointment is the intrinsic hope for improving health.
Second, regarding the drivers related to health and needs some general results were found in the literature (21, 22, 24, 25) but we have not been able to fully acknowledge. Pain intensity and lack of sleep motivate people to consume OTC drugs according to our results, as well as better reported health. Painkillers are the main class of non-prescribed drugs sold in the OTC market, so this significant result could be expected. This consumption of painkillers might raise concern for potential adverse effects arising from excess consumption, polypharmacy, and pain interactions (32). On the other hand, Portugal faces a mental health problem and it is the European country where most antidepressants are sold (33, 34). So perhaps this high prevalence of mental health issues could be reflected in a high demand for OTC drugs, specifically, for drugs to help with sleep. And in fact, this mental health problem is also observable in the positive correlation found between depression score and OTC demand.
Other needs have also been found to play a part in taking OTC remedies. Women taking emergency contraceptive pills are more likely to self-medicate with OTC drugs. Emergency contraceptive pills can be obtained either with a medical prescription or in a community pharmacy after a licensed pharmacist’s recommendation. Easier access means it is very likely that most women got their emergency pills from a pharmacy. This emergency provides women with a learning experience on accessing and using community pharmacy services, including buying OTC drugs (35). This association has not been found in previous studies, but it may merit future research about the proximity between people and pharmacists within health care.
Third, predisposing factors for taking OTC drugs found in this analysis are being female, young, having education, and living in urban areas. First, men tend to take less care of their health and do so much later than women (23, 33, 36, 37). Second, education is associated with higher individual resources (cognitive, communicative, informative, relational) and so people use their knowledge to exert their empowerment over health (20, 21, 23). Third, younger individuals tend to use more OTC medicines (38), most likely because their opportunity cost for looking for health care is higher and because the illness is not serious enough to motivate them to seek out health care. However, this result may differ, according to different views and analyses (39). Finally, pharmacies and other retailers selling drugs are less available in rural areas, so a lower OTC consumption is quite likely. However, this difference can raise concerns of equity of access to drugs, not only OTC ones, but prescribed drugs too. The greater the distance to a pharmacy means it is accessed less often, and so in cases of mild illness, people may choose to put up with feeling unwell.
Fourthly, significant enabling factors for OTC consumption are in fact of an economic nature. People with higher incomes or with financial resources to deal with unexpected health expenses are more likely to choose OTC products, as suggested by other empirical evidence (12, 21). If one regards an OTC product like any other good in the market, then there is no reason for concern; however, if one believes that an OTC product has relevance for living well, leading a normal life, and being productive in society, then these economic differences may reflect a socioeconomic gradient (40).
Lastly, the statistically significance differences found between women and men for the variables age, education, urban, financial availability, lack of sleep, unmet needs and waiting lists may be explained by several reasons: 1) the size of the men sample is smaller, 2) women and men differ in the expression of health needs, in the use and access to health care, and 3) women have more frequent contact with pharmacist than men due to the birth control need. Nevertheless, for these variables, the direction of the association is the same between men and women.
Strengths and Limitations
There are some limitations to our analysis which should be noted. First, the question concerning self-medication asks people if they took any drug which was not prescribed by a physician. However, people can interpret this question in differently. They might take drugs that were in the bathroom cabinet but were prescribed long before, or take drugs which were prescribed for a family member, neighbour or friend. Nevertheless, the framing of this question in the survey was considered carefully. It comes after a question aimed at prescribed drugs. This will tend to eliminate prescribed drugs from the mind of the respondent in the next question about OTC drugs.
Second, the question about non-prescribed drugs refers to 2 weeks before. The main reason for this time consideration, apart from being general European reference, could be for reasons related to people’s memory. This could be slightly biased, but we believe that this sampling bias is not significant because no matter the time of the year, there are always conditions calling for the consumption of OTC drugs. In the winter people will tend to take flu-related drugs and in the spring/summer people will be more likely to take allergy-related drugs.
Another possible limitation concerns the cross-section analysis which, despite not allowing for causality analysis, nonetheless provides good clues on the associated factors motivating the decision to consume OTC drugs.
The major strength of our work is twofold. Not only does it use recent data for Portugal, which fit with a specific institutional setting for the health system, but it also contributes to the understanding and comparison of the profile of people buying OTC drugs in high-income countries in Europe. This work also provides results with relevant potential policy implications.
Policy Implications
From a policy perspective, our work has brought important insights related to the drivers of self-medication with non-prescribed drugs. First, the substitution effect between consuming OTC drugs and health care due to financial or distance/transport difficulties calls for measures to mitigate these difficulties. Not only for equity reasons, but also for health reasons. People may be delaying medical care and masking symptoms which will become more severe or delay a serious diagnosis, so improving access to medical care is an important policy measure. The widespread trend of health digitalization could be used to decrease distance and transport strains.
Second, pain management and primary care needs to be considered when designing functions of primary care units. Chronic pain impacts peoples’ lives in several ways and it can also lead to mental health problems. General physicians often under-treat pain and are also uncomfortable treating pain because of the various health complexities related to it. However, training or finding specialists in pain management can help to improve people’s quality of life and contribute to a balanced consumption of painkillers.
Third, mental healthcare support has long been recognized as an important policy measure that is still lagging behind. Another related policy is the need to improve citizens’ health literacy so that they are better able to navigate the health system and manage their own health. Taking OTC drugs has advantages and disadvantages, and when people are aware of this trade-off the risks associated with OTC consumption could then be reduced.
Author Contributions
AIT designed the study design, performed the analysis and its interpretation, drafted, and reviewed the manuscript. PLF contributed to the study design, analysis, interpretation of results, and reviewed the manuscript. VC contributed to the analysis, interpretation of results, and reviewed the manuscript.
Acknowledgments
The authors acknowledge CEISUC/CIBB is funded by national funds through FCT—Foundation for Science and Technology, I.P., under the Multiannual Financing of R&D Units 2020–2023.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/ijph.2022.1604852/full#supplementary-material
References
1. Rosenau, PV. Rx-to-OTC Switch Movement. Med Care Rev (1994) 51(4):429–66. doi:10.1177/107755879405100403
2.WHO. The Role of the Pharmacist in Self-Care and Self-Medication: Report of the 4th WHO Consultative Group on the Role of the Pharmacist. Hague: WHO (1998).
3.MSH Management Sciences for Health. MDS-3: Managing Access to Medicines and Health Technologies: Chp 27 Managing for Rational Medicine Use. Arlington,VA: MSH (2012).
4. Noone, J, and Blanchette, CM. The Value of Self-Medication: Summary of Existing Evidence. J Med Econ (2017) 21:201–11. doi:10.1080/13696998.2017.1390473
5.AESGP Foundation. The Economic and Public Health Value of Self-Medication. Brussels: AESGP Foundation (2004).
6. Hughes, CM, McElnay, JC, and Fleming, GF. Benefits and Risks of Self-Medication. Drug Saf (2001) 24:1027–37. doi:10.2165/00002018-200124140-00002
7.INFARMED. Relatorio de Monitorização das vendas fora das farmácias. Medicamentos não sujeitos a receita médica Jan-Dez.2020. (Report on drugs sells outsider pharmacies. Non-prescribed drugs). Lisboa: INFARMED (2021).
8. Oleszkiewicz, P, Krysinski, J, Religioni, U, and Merks, P. Access to Medicines via Non-pharmacy Outlets in European Countries—A Review of Regulations and the Influence on the Self-Medication Phenomenon. Healthcare (2021) 9(2):123. doi:10.3390/healthcare9020123
9. Or, Z, Cases, C, Lisac, M, Vrangbæk, K, Winblad, U, and Bevan, G. Are Health Problems Systemic? Politics of Access and Choice under Beveridge and Bismarck Systems. Health Econ Pol L (2010) 5(03):269–93. doi:10.1017/S1744133110000034
10. Simoes, J, Augusto, GF, Fronteira, I, and Hernández-Quevedo, C. Portugal: Health System Review. Health Syst Transit (2017) 19(2):1–184.
11. Andersen, RM. Families' Use of Health Services: A Behavioral Model of Predisposing, Enabling and Need Components. [dissertation]. West Lafayette, IN: Purdue University (1968).
12. Andersen, R. Revisiting the Behavioral Model and Access to Medical Care: Does it Matter? J Health Soc Behav (1995) 36(1):1–10. doi:10.2307/2137284
13. Babitsch, B, Gohl, D, and von Lengerke, T. Re-revisiting Andersen’s Behavioral Model of Health Services Use: a Systematic Review of Studies from 1998–2011. Psychosoc Med (2012) 9:Doc11. doi:10.3205/psm000089
14. Anderson, R. Self-care Behavior Among the U.S.Population: Analysis of National Data. HHS Project No.04-106. Washington, DC: National Center for Health Services Research (1981).
15. Wilkinson, IF, Darby, DN, and Mant, A. Self-Care and Self-Medication: An Evaluation of Individuals' Health Care Decisions. Med Care (1987) 25(10):965–78. doi:10.1097/00005650-198710000-00005
16. Cho, JH, and Lee, TJ. The Factors Contributing to Expenditures on Over-the-counter Drugs in South Korea. Value Health Reg Issues (2013) 2(1):147–51. doi:10.1016/j.vhri.2013.01.010
17. Chang, J, Wang, Q, and Fang, Y. Socioeconomic Differences in Self-Medication Among Middle-Aged and Older People: Data from the China Health and Retirement Longitudinal Study. BMJ Open (2017) 7:e017306. doi:10.1136/bmjopen-2017-017306
18. Porteousa, T, Wykeb, S, Hannaforda, P, and Bonda, C. Self-care Behaviour for Minor Symptoms: Can Andersen’s Behavioral Model of Health Services Use Help Us to Understand it? Int J Pharm Pract (2015) 23:27–35. doi:10.1111/ijpp.12116
19. Shaghaghi, A, Asadi, M, and Allahverdipour, H. Predictors of Self-Medication Behavior: A Systematic Review. Iran J Public Health (2014) 43:136–46.
20. Green, MA, Little, E, Cooper, R, Relton, C, and Strong, M. Investigation of Social, Demographic and Health Variations in the Usage of Prescribed and Over-the-counter Medicines within a Large Cohort (South Yorkshire, UK). BMJ Open (2016) 6:e012038. doi:10.1136/bmjopen-2016-012038
21. Mayer, S, and Österle, A. Socioeconomic Determinants of Prescribed and Non-prescribed Medicine Consumption in Austria. Eur J Public Health (2015) 25(4):597–603. doi:10.1093/eurpub/cku179
22. Vogler, S, Osterle, A, and Mayer, S. Inequalities in Medicine Use in Central Eastern Europe: an Empirical Investigation of Socioeconomic Determinants in Eight Countries. Int J Equity Health (2015) 14:124–43. doi:10.1186/s12939-015-0261-0
23. Daban, F, Pasarín, MI, Rodríguez-Sanz, M, Garcia-Altes, A, Villalbi, JR, Zara, C, et al. Social Determinants of Prescribed and Non-prescribed Medicine Use. Int J Equity Health (2010) 9:12. doi:10.1186/1475-9276-9-12
24. Jiménez-Rubio, D, and Hernández-Quevedo, C. Explaining the Demand for Pharmaceuticals in Spain: Are There Differences in Drug Consumption between Foreigners and the Spanish Population? Health Policy (2010) 97:217–24. doi:10.1016/j.healthpol.2010.05.003
25. Tavares, AI. Self-medication Model and Evidence from Portugal. Int J Soc Econ (2013) 40(11):990–1009. doi:10.1108/ijse-02-2012-0026
26. Tripkovic, K, Neskovic, A, Jankovic, J, and Odalovic, M. Predictors of Self-Medication in Serbian Adult Population: Cross-Sectional Study. Int J Clin Pharm (2018) 40:627–34. doi:10.1007/s11096-018-0624-x
27.Instituto Nacional de Estatistica/Portugal Statistics. Inquérito Nacional de Saúde/National Health Survey 2019. Lisbon: INE (2020).
28. Prince, MJ, Reischies, F, Beekman, ATF, FuhReR, R, Jonker, C, Kivela, SL, et al. Development of the EURO–D Scale – a European Union Initiative to Compare Symptoms of Depression in 14 European Centres. Br J Psychiatry (1999) 174(04):330–8. doi:10.1192/bjp.174.4.330
29. Vaidya, V, Partha, G, and Karmakar, M. Gender Differences in Utilization of Preventive Care Services in the United States. J Womens Health (2012) 21(2):140–5. doi:10.1089/jwh.2011.2876
30. Loikas, D, Wettermark, B, von Euler, M, Bergman, U, and Schenck-Gustafsson, K. Differences in Drug Utilisation between Men and Women: a Cross-Sectional Analysis of All Dispensed Drugs in Sweden. BMJ Open (2013) 3:e002378. doi:10.1136/bmjopen-2012-002378
31. Hassell, K, Noyce, P, and Rogers, A. A Review of Factors that Influence the Use of Community Pharmacies as a Primary Health Care Resource. Int J Pharm Pract (1999) 7(1):51–9. doi:10.1111/j.2042-7174.1999.tb00948.x
32. Schmiedl, S, Rottenkolber, M, Hasford, J, Rottenkolber, D, Farker, K, Drewelow, B, et al. Self-Medication with Over-the-counter and Prescribed Drugs Causing Adverse-Drug-Reaction-Related Hospital Admissions: Results of a Prospective, Long-Term Multi-Centre Study. Drug Saf (2014) 37(4):225–35. doi:10.1007/s40264-014-0141-3
33. Gusmao, R, Quintao, S, McDaid, D, Arensman, E, Van Audenhove, C, Coffey, C, et al. Antidepressant Utilization and Suicide in Europe: An Ecological MultiNational Study. PLoS ONE (2013) 8(6):e66455. doi:10.1371/journal.pone.0066455
34. Antunes, A, Frasquilho, D, Lopes, SA, Neto, D, Silva, M, Cardoso, G, et al. Disability and Common Mental Disorders: Results from the World Mental Health Survey Initiative Portugal. Eur Psychiatry (2018) 49:56–61. doi:10.1016/j.eurpsy.2017.12.004
35. Atkins, K, Kennedy, CE, Yeh, PT, and Narasimhan, M. Over-the-counter Provision of Emergency Contraceptive Pills: a Systematic Review. BMJ Open (2022) 12:e054122. doi:10.1136/bmjopen-2021-054122
36. Bertakis, KD, Azari, R, Helms, LJ, Callahan, EJ, and Robbins, JA. Gender Differences in the Utilization of Health Care Services. J Fam Pract (2000) 49(2):147–52.
37. Ladwig, KH, Marten-Mittag, B, Formanek, B, and Dammann, G. Gender Differences of Symptom Reporting and Medical Health Care Utilization in the German Population. Eur J Epidemiol (2000) 16:511–8. doi:10.1023/a:1007629920752
38. Johnson, RE, and Reed, LD. OTC Drug Use in an HMO: Comparing the Elderly and Younger Adults. J Aging Health (1996) 8(1):114–35. doi:10.1177/089826439600800106
39. Sujit, S, Sansgiry, MS, and Cady, P. How the Elderly and Young Adults Differ in the Decision Making Process of Nonprescription Medication Purchases. Health Marketing Q (1996) 14(1):3–21. doi:10.1300/j026v14n01_02
Keywords: predictors, non-prescribed drugs, OTC, medical care, Portugal
Citation: Tavares AI, Ferreira PL and Cavadas V (2022) Factors Contributing to Self-Medication and Consumption of Non-Prescribed Drugs in Portugal. Int J Public Health 67:1604852. doi: 10.3389/ijph.2022.1604852
Received: 18 February 2022; Accepted: 17 October 2022;
Published: 07 November 2022.
Edited by:
Olaf von dem Knesebeck, University Medical Center Hamburg-Eppendorf, GermanyReviewed by:
Johan Van Der Heyden, Sciensano, BelgiumCopyright © 2022 Tavares, Ferreira and Cavadas. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Aida Isabel Tavares, YXRhdmFyZXNAaXNlZy51bGlzYm9hLnB0
 Aida Isabel Tavares
Aida Isabel Tavares Pedro Lopes Ferreira
Pedro Lopes Ferreira Veronica Cavadas
Veronica Cavadas