- 1Department of Psychology and Neuroscience, Morrissey College of Arts and Sciences, Boston College, Chestnut Hill, MA, United States
- 2Department of Sociology, Morrissey College of Arts and Sciences, Boston College, Chestnut Hill, MA, United States
Objectives: This study aims to explore the influence of COVID-19 on undergraduate students’ academic performance, social life, and mental health during the pandemic’s early stage, and evaluate potential correlates of stress, anxiety, and depression in relation to COVID-19.
Methods: Participant data was collected as part of a survey that consisted of demographic questions, a DASS-21 questionnaire, and an open-ended question. The final sample consisted of 1077 full-time students in the United States.
Results: 19%, 20%, and 28% of participants met the cutoff for “severe” and “extremely severe” levels of stress, anxiety, and depression according to DASS-21. During COVID-19, a significant increase in hours of sleep, and decrease in hours spent on extracurriculars and studying were observed. While talking to family was significantly associated with stress, anxiety, and depression, engaging in hobbies was only associated with depression.
Conclusion: With the continued spread of COVID-19, it is critical for universities to adapt to the mental health needs of their students. Future institutional advancements should create treatment programs to ensure better academic and social outcomes.
Introduction
In March 2020, the World Health Organization officially declared the rapidly spreading coronavirus outbreak a pandemic [1]. The pandemic has since reshaped almost every facet of modern society. Many schools and universities across the United States closed from March 2020 through the end of the Spring 2020 semester. Consequently, students living in university dormitories were required to return to tumultuous living conditions that likely detracted from learning. Educators were asked to revise, and in some cases completely revamp course standards, expectations, and assessments, all within a matter of weeks.
Despite limited evidence regarding the implications of transitioning to online learning in the context of COVID-19, previous studies have shown that the transition to postsecondary education is itself a source of anxiety [2], stress [3], and depression [2, 4]. This transition can bring about feelings of worthlessness, appetite disturbances, and issues with concentration, all of which adversely affect students’ capability to perform well in demanding environments [5]. Moreover, during the undergraduate years, students are not only immersed in higher education but are also transitioning into other critical social roles [6]. Young adults in this age range, therefore, are forced to deal with identity exploration and adjustment to university life.
Academics are exceptionally fundamental to the life and health of undergraduate students. The amount of time spent studying as well as concerns about examinations have been shown to lead to heightened immune and stress responses [7]. Therefore, coping mechanisms and social support to reduce stress are crucial, as effective coping strategies can potentially ameliorate stress reactivity [8]. In particular, understanding how the learning experience was for undergraduate students is important as online learning will likely be the primary method of instruction during future university closures. Some research has been done to assess early pandemic-related responses associated with undergraduate students’ academic work [9, 10] and mental health [11] in the United States.
Coinciding with the ever-demanding academic burden, mental health among undergraduate students represents an important and growing public health concern [12]. It was found that 12%–18% of college students suffer from a diagnosable mental illness [13]. A mental health crisis may take its toll years after the course of the COVID-19 pandemic [14]. Thus, it is important to investigate the potential factors that have adversely affected students during the pandemic.
Literature to-date is limited on commentary with regards to the effects of online learning on studying quality among undergraduates during the pandemic. The abrupt transition to online learning exploited time better spent in clinical training and internet subscription costs impeded access to effective learning for students studying at home, as did tending to family [15]. A poor internet connection was found to be a leading barrier to online learning [16].
Undergraduates are one of the most sleep-deprived age groups in the United States [17]. Studies that have investigated sleep reported significantly worsened insomnia among students during the pandemic [18, 19]. Specifically, a large cross-sectional study found a marked incidence of insomnia among college-aged students during the lockdown period [20]. Deteriorating sleep quality correlated with depressive symptoms [21].
While previous studies have commented on particular dimensions of the pandemic relating to issues of depression and anxiety [22], there remains a pressing concern to determine precisely which aspects of students’ daily life had been affected. Thus, the aim of the present study was to analyze specific correlates of stress, anxiety, and depression among undergraduate students as they relate to the most intimate issues of the college student’s demanding lifestyle. In particular, we aimed to analyze data from a large sample of students using the Depression, Anxiety, and Stress Scale (DASS-21) to approximate emotional valence. Further questions offered to students in a survey were meant to gauge whether changes in hours spent on extracurricular activities, studying, and sleep before and during the pandemic were related to observed DASS-21 results. This study also aimed to provide a better understanding about COVID-19’s influence in the context of full-time undergraduate students’ academic performance, social life, and mental health in the United States.
Methods
Participants
Participants were undergraduate students at a private university, public university, or community college in the United States. To be included, participants had to be at least 18 years old and enrolled as full-time students as part of class years 2020, 2021, 2022, or 2023. Between April and June 2020, participants were recruited through two channels. First, an email was sent to undergraduate students at Boston College. Second, participants were recruited online via Reddit, a social news platform and online forum.
An invitation to participate in the study was posted on over 20 university-related and survey recruitment subreddits (a subreddit is an online community with user-created threads dedicated to a specific topic). One such subreddit utilized for recruitment in this study was r/SampleSize, a community of over 40,000 users assembled for the express purpose of survey recruitment and participation [23]. Subreddits such as these have been shown to be a good source of diverse and viable participants [23] and are useful for inexpensive participant recruitment and reliable data collection [24, 25]. For the purpose of the current study, face-to-face interviews during this time had to be avoided because of the US lockdown and ongoing public health crisis. The study received 1,734 completed responses. After excluding students younger than 18 (n = 34), part-time students (n = 135), and students with incomplete responses (n = 488) from our analyses, our final sample size was 1,077.
Measures
DASS (Depression, Anxiety, and Stress Scale): The online survey included the 21-item DASS-21 scale on mood and stress [26]. Based on the scores, participants were classified into “normal” (a score of 0–9 for depression, 0–7 for anxiety, and 0–14 for stress), “mild” (10–13, 8–9, 15–18), “moderate” (14–20, 10–14, 19–25), “severe” (21–27, 15–19, 26–33), and “extremely severe” (28+, 20+, 34+) categories. The purpose of these questions was to assess the severity of depression, anxiety, and stress during the COVID-19 pandemic. Previous studies have verified the validity of the DASS-21 scale as a routinely-used clinical and non-clinical self-report scale [27, 28]. One sample statement that participants were to score for depression was “I was unable to become enthusiastic about anything”; one sample statement for anxiety was “I worry about situations in which I might panic and make a fool of myself”; and one sample statement for stress was “I tended to over-react to situations”. Participants were given the option to choose between “once a week or less” (score = 0), “2–3 times a week” (= 1), “4–6 times a week” (= 2) and “7 times a week or more” (= 3). The corresponding sum of scores was used to assess the severity of depression, anxiety, and stress. Cronbach’s α for the items in this test was 0.934, indicating excellent internal consistency in the questionnaire.
COVID-19 Evaluation: The first portion of the survey consisted of a series of questions meant to measure how COVID-19 may have affected students’ social life and mental health. Students were asked about hours of studying per day (“1–2 h,” “3–5 h,” “5–8 h,” and “8+ h”), hours spent on extracurricular activities per week (participants typed in number of hours), and hours of sleep received per night (“4 h or less,” “5–7 h,” “7–8 h,” and “8+ h”) before the pandemic (e.g., “How many hours of sleep did you get per night (BEFORE the COVID-19 pandemic)?”) and during the pandemic (e.g., “How many hours of sleep do you [currently] get per night?”).
Coping Strategies: Participants were asked to select up to three ways they managed their stress. Seven response categories were given: “talk to friends,” “talk to family members,” “home workout/indoor sports,” “meditate,” “do favorite hobbies,” “walk outside,” and “other”. When participants chose “other”, they were asked to specify. Participants were provided with an open-ended question at the end of the survey to further elaborate on experiences that were not captured by previous questions.
Procedure
Before taking the survey, all participants provided informed consent. Participants were made aware of all risks and benefits associated with the survey, confidentiality, and right to withdraw their voluntary participation at any time. The survey, which took 10 min to complete, consisted of four components: social demographics, school adjustments, DASS-21 questions, and an optional open-ended question. As an incentive for participation, participants were entered into a raffle for a chance to win a $10 Amazon gift card (15 participants were awarded a gift card). The survey was accessible online for 9 weeks (from April to June 2020). The procedure was approved by the university’s institutional review board in April 2020, ensuring the protection of human subjects in this research in compliance with US federal law.
Statistical Analysis
Statistical analyses were conducted using R-Studio statistical software (version 1.3.959, 2009–2020 R-Studio, PBC). In the first phase of analysis, descriptive statistics were used to describe the demographics of the sample and the distribution of the three mental health outcomes among students. Next, t-tests were used to test whether moving to remote learning had an effect on stress, anxiety, and depression. Paired t-tests were used to determine differences in the hours of sleep, study, and extracurricular activities before and during the pandemic. Bivariate regression analysis was used to determine whether participants’ responses to moving classes to remote learning were associated with stress, anxiety, and depression. Regression analysis tested whether changes in the hours of sleep and study during COVID-19 were associated with stress, anxiety, and depression. Lastly, a multivariate OLS system was used to determine whether gender, having a family member who tested positive for COVID-19, number of times participants left their homes, school performance after moving to remote learning, and changes in the hours of sleep and studying were associated with stress, anxiety, and depression.
Results
Descriptive Statistics of the Sample
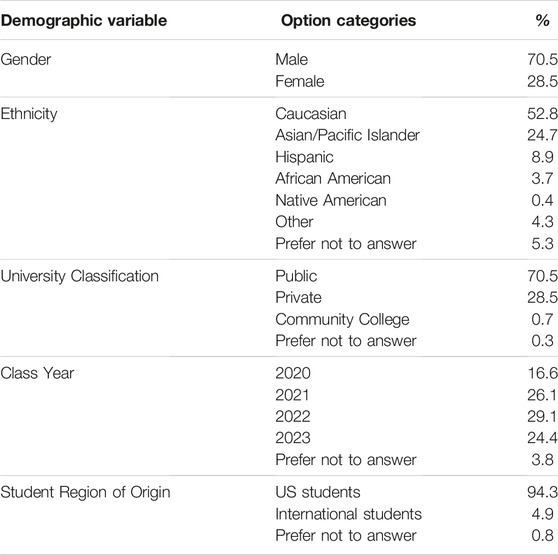
Most participants were students at public universities (70.5%), followed by those from private universities (28.5%) or community colleges (0.7%). 0.3% of participants preferred not to answer this question. Participants were categorized as students in the class of 2020 (16.6%), 2021 (26.1%), 2022 (29.1%), and 2023 (24.4%), respectively. 3.8% of participants preferred not to answer this question (Table 1). Female participants accounted for 51.4% of the sample. Slightly more than half of the participants were Caucasian (52.8%), one fourth were Asian/Pacific Islander (24.7%), about one tenth were Hispanic/Latinx (8.9%), and about 4% were African American (3.7%). 0.4% of participants self-identified as Native American. While the majority of participants were US students (94.3%), some participants were international students (4.9%) and a few participants preferred not to answer (0.8%).
DASS-21
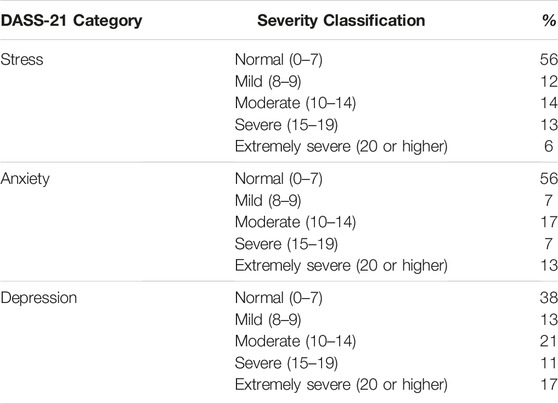
Using DASS-21 scores, 19%, 20%, and 28% of participants were categorized as having “severe” or “extremely severe” levels of stress, anxiety, and depression, respectively (% “severe” + % “extremely severe”) (Figure 1) (Table 2). These results indicate an increase of “severe” and “extremely severe” levels of stress, anxiety, and depression in comparison to a sample baseline, non-pandemic DASS-21 scores, with levels of stress, anxiety, and depression at 11%, 15%, and 11%, respectively [29].
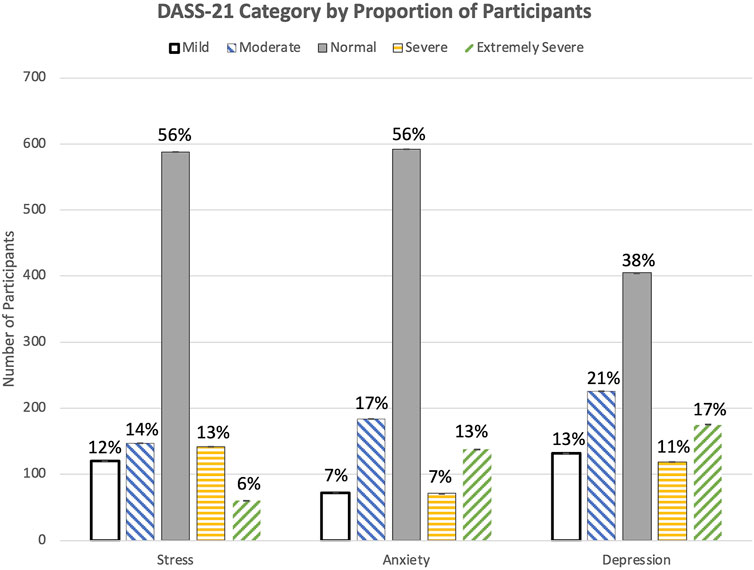
FIGURE 1. Proportion of participants whose answers on the Depression, Anxiety, and Stress Scale-21 indicated a normal, mild, moderate, severe, or extremely severe level of stress, anxiety, and depression (United States. 2020).
Bivariate Relationship Between Academic Performance, Social Life, and Mental Health
COVID-19 disrupted traditional classroom instruction and led to remote learning, as 69.3% of participants claimed that moving to remote learning had a negative impact on their school performance, while 30.7% of participants noted a positive impact of remote learning on school performance. Moreover, in terms of the association between school performance and mental health, a t-test showed that participants who claimed that remote learning had a negative impact on their school performance had significantly higher scores in stress (Figure 2, p < 0.001), anxiety (Figure 2, p < 0.001), and depression (Figure 2, p < 0.001), compared to peers who reported the opposite. A bivariate regression analysis further confirmed that students’ opinions about remote learning were significantly associated with stress (p < 0.001), anxiety (p < 0.001), and depression (p < 0.001). Participants were also asked about changes in hours spent on extracurricular activities, studying, and sleeping before and during COVID-19 comparatively. A paired two-sample t-test showed a significant increase in the hours of sleep (before COVID-19: 6.7 h; during COVID-19: 7.7 h, p < 0.001), a significant decrease in hours spent on extracurricular activities (before COVID-19: 9.4 h; during COVID-19: 6.2 h, p < 0.001), and a significant decrease in hours spent studying (before COVID-19: 4.2 h; during COVID-19: 3.6 h, p < 0.001).
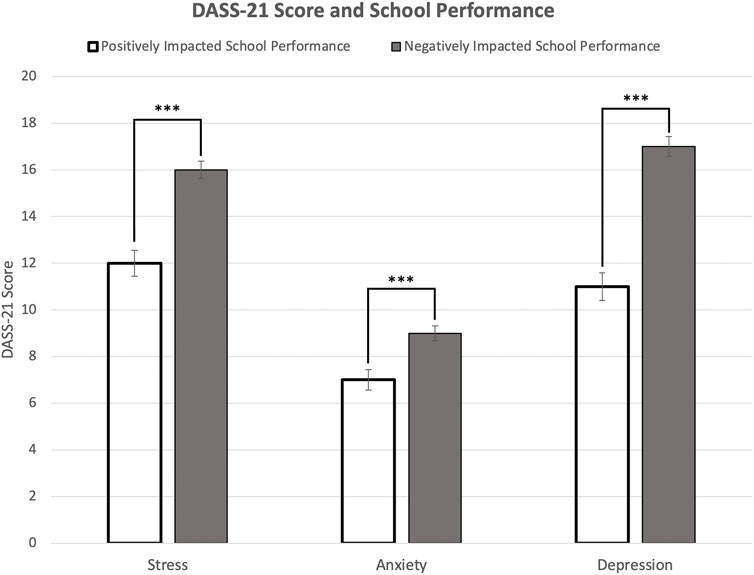
FIGURE 2. Association between stress, anxiety, and depression scores (mean Depression, Anxiety, and Stress Scale-21 score) and self-reported impact of COVID-19 on school performance (United States. 2020). Note: Error bars represent standard errors. Significance levels of Depression, Anxiety, and Stress Scale-21 scores: *p < 0.05, **p < 0.01, ***p < 0.001.
Regression analysis was implemented to find correlates of stress, anxiety, and depression. For survey questions addressed in regard to pre-pandemic conditions, regression analysis showed that hours of sleep was associated with stress (p < 0.001), anxiety (p < 0.001), and depression (p < 0.001), but hours of studying was not associated with stress (p = 0.33), anxiety (p = 0.213), and depression (p = 0.056). However, during COVID-19, regression analysis showed that neither hours of studying nor hours of sleep were associated with stress (p = 0.429 and p = 0.678), anxiety (p = 0.283 and p = 0.506), and depression (p = 0.0517 and p = 0.665).
Multivariate OLS Regression Models
Turning to multivariate OLS regression models, several factors were found to have significant associations with stress and anxiety. Being a male participant (p < 0.001), having a family member who tested positive (p < 0.001), leaving home three times a week (p < 0.05), believing that school performance was affected negatively by moving to remote learning (Figure 2, p < 0.001), and hours of sleep during COVID-19 (“5–6 h” p < 0.05, “7–8 h” p < 0.001, “8+ h” p < 0.001) were significant correlates of stress (Table 3). As for depression, being a male participant (p < 0.01), leaving home once a week (p < 0.05), believing that school performance was affected negatively by moving to remote learning (p < 0.001), hours spent studying (“3–5 h” p < 0.001, “5–8 h” p < 0.05), and hours of sleep during COVID-19 (“5–6 h” p < 0.01, “7–8 h” p < 0.001, “8+ h” p < 0.001) were significant correlates. For stress management, talking to a family member was significantly associated with stress (p < 0.05), anxiety (p < 0.05), and depression (p < 0.05). Engaging in favorite hobbies was only correlated with depression (p < 0.05).
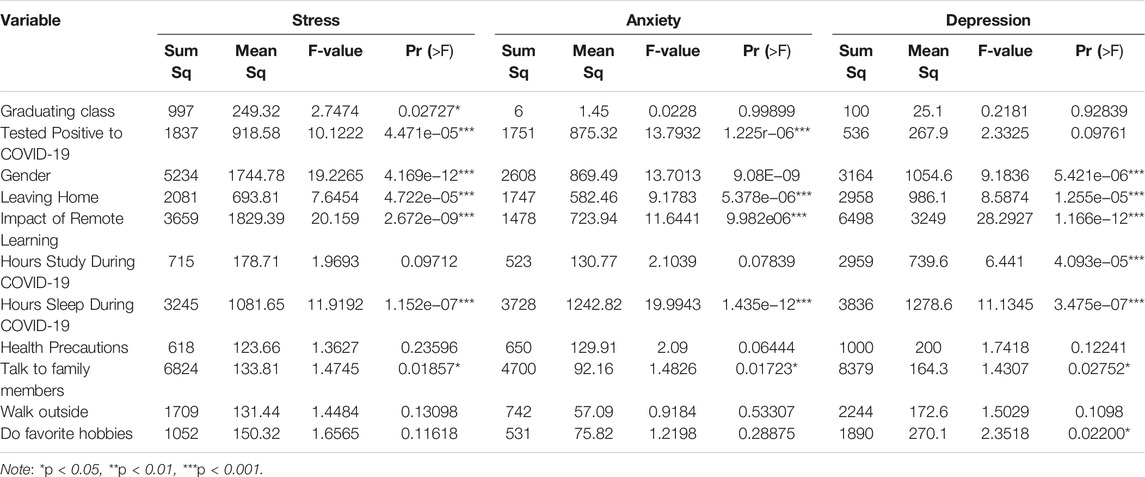
TABLE 3. Multivariate Ordinary Least Squares Models for variables indicative of stress, anxiety, and depression (United States. 2020).
Sex Differences
Female participants showed a larger percentage of severe and extremely severe levels of stress (severe; 16% and extremely severe; 7%), anxiety (8%; 15%), and depression (12%; 18%) in comparison to male participants’ stress (severe; 11% and extremely severe 3%), anxiety (5%; 10%), and depression (11%; 14%) levels (Figure 3). Chi-squared analysis showed being female was associated with severe and extremely severe levels of stress (x-squared = 30.497, df = 4, p < 0.001), anxiety (x-squared = 19.501, df = 4, p < 0.001), and depression (x-squared = 17.59, df = 4, p < 0.01). Two-sample t-test showed that female participants have a higher score in stress (p < 0.001), anxiety (p < 0.001), and depression (p < 0.001) in comparison to male participants. Regression analysis showed that gender is associated with stress (p < 0.001), anxiety (p < 0.001), and depression (p < 0.001).
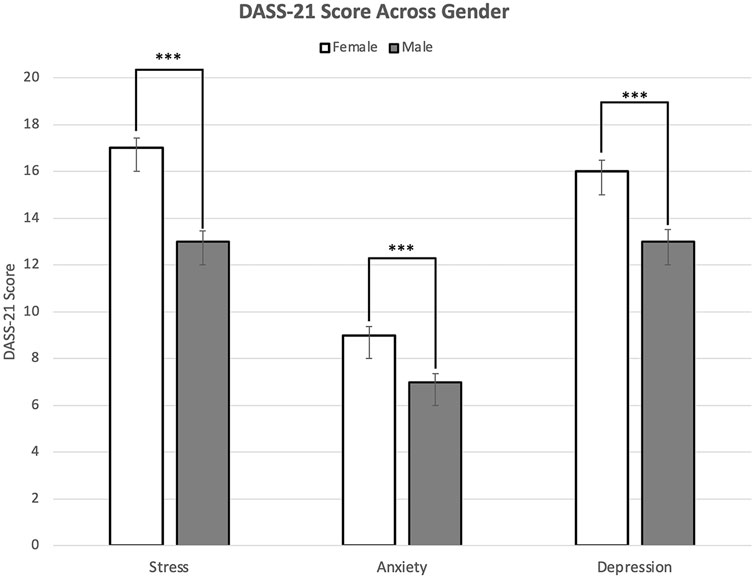
FIGURE 3. Mean Depression, Anxiety, and Stress Scale-21 scores of stress, anxiety, and depression among males and females (United States. 2020). Note: Error bars represent standard errors. Significance levels of Depression, Anxiety, and Stress Scale-21 scores: *p < 0.05, **p < 0.01, ***p < 0.001.
Stress Management
Recall that the survey asked participants to choose up to three ways they managed their stress during the COVID-19 pandemic. Almost half (47.9%) of participants reported that they talked to family members, 76% of participants engaged in their favorite hobbies, and 32.2% of participants walked outside as one of their three choices. Although the vast majority of the open-ended responses included some sentiment of stress, many individuals did have positive experiences to share. Some participants noted that conversing with significant others, in addition to immediate family, was cathartic (“I’ve been [...]reach [ing] out to my boyfriend, at the very least. These things, along with the positive experience of being around a happy family and the safety of our own home, has positively contributed to my mental wellbeing.”). In a simpler sense, some have made the most of their time while at home, with one participant noting that they were “Just staying inside and trying to learn new things.”
Stress During COVID-19
In the open-ended question, one participant from the class of 2021 said the following of their experience during lockdown: “I have been feeling quite depressed. I feel like I have no control over my life ... I cannot plan for the future and my extracurriculars that were going to help me prepare for grad schools have been affected.” Another participant from the class of 2021 said, “Anxious and overwhelmed … I feel like I have less access to academic advising because … professors have not answered my emails. It’s been difficult to focus at home because my parents [are] working over the phone ….”
Many individuals expressed a lack of motivation to perform well on academic tasks noting severe procrastination, loss of direction, and overall dissatisfaction with the progression of the semester. One participant said, “I feel … grateful that I am healthy. However, I also have struggled to find any motivation to do my work or be active. Usually I can get things done because I look forward to having fun or relaxing on weekends, but now it is harder to get things done when it feels like that is all I am doing with nothing fun to look forward to.” Other participants found it challenging to engage with online classes. For example, one participant said, “Online learning is difficult because I feel zero engagement.”
One participant said that they felt suffocated. They said, “I want to leave the house, see new people, go to stores, but I only leave my house about 1–2 times a week.” In addition, leaving home a few times a week may have given students the opportunity to distance themselves from their families and home environment. One participant said, “My parents and I argue, and I feel like my mental health issues are having a negative effect on my family.” Another participant talked about the challenge of staying at home with family, saying, “Being at home with my family has taken a toll on my mental health. [We] do not have a great relationship, and being stuck at home has exacerbated our problems … ” One participant claimed that living temporarily away from family made them “feel great.”
Discussion
This study looked for correlates of stress, anxiety, and depression during COVID-19. Those who reported that school performance was affected negatively by moving to remote learning exhibited significantly heightened levels of stress, as predicted by previous findings [30, 31]. The classroom environment has several advantages over online learning. Teachers, for instance, are able to receive immediate feedback on students’ understanding of key concepts [32]. Furthermore, with remote learning comes some disadvantages; problematic internet use, longer screen time, isolation, and academic pressure are all associated with psychological distress among college students [33–36].
Our results specifically showed that the frequency with which participants left their homes was significantly associated with stress and depression. Participants who left their homes every day had lower DASS-21 scores of stress, anxiety, and depression. Social relationships have been shown to give individuals a sense of purpose and greater appreciation for life, leading to overall reduced stress and bolstered mental health [37–39].
We have identified unique correlates of stress as they relate to the COVID-19 pandemic. In particular, both sleeping hours and having a family member who tested positive for COVID-19 were correlates of stress. Changes in sleep and physical activity during the pandemic were associated with symptoms of high stress [40, 41]. However, while previous studies have shown that patients with suspected COVID-19 (positive COVID-19 test result) demonstrated a significant reluctance to work [42], our study is among the first to identify the contribution of a family member’s positive test result.
This study shows a larger percentage of severe and extremely severe levels of stress, anxiety, and depression among female participants. In agreement with our results, previous studies established that the prevalence of anxiety was higher in women during the COVID-19 pandemic [43–46]. It has also been demonstrated that female students express greater concern for their future careers than do male students [47]. The dissimilarity in the levels of stress, anxiety, and depression between genders may be attributable to women seeking mental health consultation more often than men [48]. Being female was generally shown to be associated with a prominent increase in mental health problems during the pandemic [49].
This study found a significant discrepancy in hours devoted to sleep, extracurricular activities, and studying before and during the pandemic. The increase in hours of sleep could be due to heightened stress and anxiety about the pandemic during lockdown. The lockdown period had a negative impact on mental health by increasing post-traumatic stress symptoms and was associated with irregular sleep patterns [50–52]. Acute and chronic stress have been shown to perturb sleep differentially [53]. The observed decrease in hours spent on extracurricular activities during COVID-19 could be due to a fear of infection, as fear was a definite contributor to a reduction in pursuing activities and to an increase in anxiety during the pandemic [54, 55]. As a whole, engagement in regular routines was also found to lower anxiety irrespective of the kind of stressor one was exposed to [56]. Therefore, one might be able to surmise that a lack of pursuing such activities may lead to greater anxiety. In discussing the motivation to pursue meaningful work, we found that students spent less hours studying when most instruction was conducted online. Although a decrease in hours of studying could be due to changing class syllabi and adjustments to the home environment, hours of studying did not correlate with stress, anxiety, or depression. It could be that students did not feel obligated to study in an environment with less structure or in the midst of a pandemic where students took on more responsibilities at home, such as caring for siblings or supporting their own children [57, 58].
Future research should investigate current methods of mental health management for undergraduate students. The rise of telehealth and online counseling in the age of COVID-19 has provided greater opportunities for students to schedule appointments with a healthcare provider to manage mental health. Future studies might be able to explore the influence of telehealth on DASS-21 scores. Furthermore, it would be important to conduct follow up studies that investigate the impact of increased sleep on stress, anxiety, and depression during COVID-19. The adverse impact of the home environment should also be studied, specifically seeking to answer why students who left their homes less frequently experienced worsened mental health via higher DASS-21 scores (despite not dealing with the stresses of a daily commute, for instance).
Limitations
Because the survey was distributed during the lockdown period, an online convenience sampling method had to have been utilized. This sampling method limited the representativeness and generalizability of the findings reported, as we were necessarily constrained to only those responses from students with access to the Internet. Thus, it is not possible to draw causal inferences due to the nature of this study. The survey also had some duplicate questions and questions that did not provide the capability to select multiple options. For example, one question asked participants about COVID-19 safety precautions taken, where the selection of multiple options could have been appropriate. The term “extracurricular” was also left to the interpretation of participants. A better survey question could have offered participants the option to define extracurricular activities. Furthermore, in addition to DASS-21, the study could have benefited from the utilization of a resilience scale to examine how certain resilience factors could have protected individuals’ mental health from COVID-19 related stress. Allowing participants to evaluate resilience may have permitted greater insight into students’ mental health and wellbeing.
Conclusion
COVID-19 remains a credible threat to undergraduate students, beyond the acute and lingering physical effects of the virus. Students spent less time studying, complemented by the finding that the transition to remote learning hindered the majority of students’ academic experience. Students who left home more frequently may have had a greater opportunity to socialize, which lessened the stress and mental burden of lockdown. The majority of participants also stated that talking to family and engaging in favorite hobbies were beneficial for stress management. As such, these results showed that the pandemic led to significant changes in students’ academic performance, social life, and mental health.
Ethics Statement
The studies involving human participants were reviewed and approved by The Boston College Institutional Review Board (IRB) and Vice Provost for Research. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
JN, MG, and WF contributed to the design, execution, and conceptualization of the study. JN and MG contributed to data management and conducted the literature search. MG contributed to the sample size methodology and carried out the survey distribution and initial data analysis. JN contributed to key elements of statistical analyses and interpretation with additional tests and further interpretation suggested by MG and WF. MG contributed to the essential prose of the manuscript with input from JN and WF. MG and JN prepared the initial draft of the manuscript. MG and JN created the figures and tables with input and suggestions from WF on appropriate edits to be made. All authors approved the final version of the manuscript for submission.
Conflict of Interest
The authors declare that they do not have any conflicts of interest.
References
1. Cucinotta, D, and Vanelli, M. WHO Declares COVID-19 a Pandemic. Acta Biomed (2020) 91(1):157–60. doi:10.23750/abm.v91i1.9397
2. Mounsey, R, Vandehey, M, and Diekhoff, G. Working and Non-working university Students: Anxiety, Depression, and Grade point Average. Coll Student J (2013) 47(2):379.
3. Krieg, D. High Expectations for Higher Education? Perceptions of College and Experiences of Stress Prior to and through the College Career. Coll Student J (2013) 47(4):635.
4. Dyson, R, and Renk, K. Freshmen Adaptation to university Life: Depressive Symptoms, Stress, and Coping. J Clin Psychol (2006) 62(10):1231–44. doi:10.1002/jclp.20295
5. Beck, R, Taylor, C, and Robbins, M. Missing home: Sociotropy and Autonomy and Their Relationship to Psychological Distress and Homesickness in College Freshmen. Anxiety Stress Coping (2003) 16(2):155–66. doi:10.1080/10615806.2003.10382970
6. Reifman, A, Arnett, JJ, and Colwell, MJ. Emerging Adulthood: Theory, Assessment and Application. J Youth Dev (2007) 2(1):37–48. doi:10.5195/jyd.2007.359
7. Murphy, L, Denis, R, Ward, CP, and Tartar, JL. Academic Stress Differentially Influences Perceived Stress, Salivary Cortisol, and Immunoglobulin-A in Undergraduate Students. Stress (2010) 13(4):365–70. doi:10.3109/10253891003615473
8. Doron, J, Stephan, Y, Boiché, J, and Scanff, CL. Coping with Examinations: Exploring Relationships between Students' Coping Strategies, Implicit Theories of Ability, and Perceived Control. Br J Educ Psychol (2009) 79(3):515–28. doi:10.1348/978185409X402580
9. Kecojevic, A, Basch, CH, Sullivan, M, and Davi, NK. The Impact of the COVID-19 Epidemic on Mental Health of Undergraduate Students in New Jersey, Cross-Sectional Study. PloS one (2020) 15(9):e0239696. doi:10.1371/journal.pone.0239696
10. Huckins, JF, DaSilva, AW, Wang, W, Hedlund, E, Rogers, C, Nepal, SK, et al. Mental Health and Behavior of College Students during the Early Phases of the COVID-19 Pandemic: Longitudinal Smartphone and Ecological Momentary Assessment Study. J Med Internet Res (2020) 22(6):e20185. doi:10.2196/20185
11. Wang, X, Hegde, S, Son, C, Keller, B, Smith, A, and Sasangohar, F. Investigating Mental Health of US College Students during the COVID-19 Pandemic: Cross-Sectional Survey Study. J Med Internet Res (2020) 22(9):e22817. doi:10.2196/22817
12. Wyatt, T, and Oswalt, SB. Comparing Mental Health Issues Among Undergraduate and Graduate Students. Am J Health Educ (2013) 44(2):96–107. doi:10.1080/19325037.2013.764248
13. Mowbray, CT, Mandiberg, JM, Stein, CH, Kopels, S, Curlin, C, Megivern, D, et al. Campus Mental Health Services: Recommendations for Change. Am J Orthopsychiatry (2006) 76(2):226–37. doi:10.1037/0002-9432.76.2.226
14. Horesh, D, and Brown, AD. Traumatic Stress in the Age of COVID-19: A Call to Close Critical Gaps and Adapt to New Realities. Psychol Trauma (2020) 12(4):331–5. doi:10.1037/tra0000592
15. Suliman, WA, Abu-Moghli, FA, Khalaf, I, Zumot, AF, and Nabolsi, M. Experiences of Nursing Students under the Unprecedented Abrupt Online Learning Format Forced by the National Curfew Due to COVID-19: A Qualitative Research Study. Nurse Educ Today (2021) 100:104829. doi:10.1016/j.nedt.2021.104829
16. Saha, A, Dutta, A, and Sifat, RI. The Mental Impact of Digital divide Due to COVID-19 Pandemic Induced Emergency Online Learning at Undergraduate Level: Evidence from Undergraduate Students from Dhaka City. J Affect Disord (2021) 294:170–9. doi:10.1016/j.jad.2021.07.045
17. Wolfson, AR, and Carskadon, MA. Understanding Adolescent's Sleep Patterns and School Performance: a Critical Appraisal. Sleep Med Rev (2003) 7(6):491–506. doi:10.1016/s1087-0792(03)90003-7
18. Marelli, S, Castelnuovo, A, Somma, A, Castronovo, V, Mombelli, S, Bottoni, D, et al. Impact of COVID-19 Lockdown on Sleep Quality in university Students and Administration Staff. J Neurol (2021) 268(1):8–15. doi:10.1007/s00415-020-10056-6
19. Blume, C, Schmidt, MH, and Cajochen, C. Effects of the COVID-19 Lockdown on Human Sleep and Rest-Activity Rhythms. Curr Biol (2020) 30(14):R795-R797–7. doi:10.1016/j.cub.2020.06.021
20. Zhang, Y, Wang, D, Zhao, J, Xiao-Yan, CH, Chen, H, Ma, Z, et al. Insomnia and Other Sleep-Related Problems during the Remission Period of the COVID-19 Pandemic: a Large-Scale Survey Among College Students in China. Psychiatry Res (2021) 304:114153. doi:10.1016/j.psychres.2021.114153
21. Evans, S, Alkan, E, Bhangoo, JK, Tenenbaum, H, and Ng-Knight, T. Effects of the COVID-19 Lockdown on Mental Health, Wellbeing, Sleep, and Alcohol Use in a UK Student Sample. Psychiatry Res (2021) 298:113819. doi:10.1016/j.psychres.2021.113819
22. Oh, H, Marinovich, C, Rajkumar, R, Besecker, M, Zhou, S, Jacob, L, et al. COVID-19 Dimensions Are Related to Depression and Anxiety Among US College Students: Findings from the Healthy Minds Survey 2020. J Affect Disord (2021) 292:270–5. doi:10.1016/j.jad.2021.05.121
23. Luong, R, and Lomanowska, AM. Evaluating Reddit as a Crowdsourcing Platform for Psychology Research Projects. Teach Psychol (2021) 49:329–37. doi:10.1177/00986283211020739
24. Jamnik, MR, and Lane, DJ. The Use of Reddit as an Inexpensive Source for High-Quality Data. Pract Assess Res Eval (2017)(1).
25. Lee, JY, Chang, OD, and Ammari, T. Using Social media Reddit Data to Examine foster Families’ Concerns and Needs during COVID-19. Child Abuse Negl (2021) 121:105262. doi:10.1016/j.chiabu.2021.105262
26. Lovibond, PF, and Lovibond, SH. The Structure of Negative Emotional States: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther (1995) 33(3):335–43. doi:10.1016/0005-7967(94)00075-u
27. Henry, JD, and Crawford, JR. The Short-form Version of the Depression Anxiety Stress Scales (DASS-21): Construct Validity and Normative Data in a Large Non-clinical Sample. Br J Clin Psychol (2005) 44(2):227–39. doi:10.1348/014466505X29657
28. Ng, F, Trauer, T, Dodd, S, Callaly, T, Campbell, S, and Berk, M. The Validity of the 21-item Version of the Depression Anxiety Stress Scales as a Routine Clinical Outcome Measure. Acta Neuropsychiatr (2007) 19(5):304–10. doi:10.1111/j.1601-5215.2007.00217.x
29. Beiter, R, Nash, R, McCrady, M, Rhoades, D, Linscomb, M, Clarahan, M, et al. The Prevalence and Correlates of Depression, Anxiety, and Stress in a Sample of College Students. J Affect Disord (2015) 173:90–6. doi:10.1016/j.jad.2014.10.054
30. Lischer, S, Safi, N, and Dickson, C. Remote Learning and Students’ Mental Health during the Covid-19 Pandemic: A Mixed-Method Enquiry. Prospects (2021) 51:589–99. doi:10.1007/s11125-020-09530-w
31. Watermeyer, R, Crick, T, Knight, C, and Goodall, J. COVID-19 and Digital Disruption in UK Universities: Afflictions and Affordances of Emergency Online Migration. High Educ (2021) 81:623–41. doi:10.1007/s10734-020-00561-y
32. Mukhtar, K, Javed, K, Arooj, M, and Sethi, A. Advantages, Limitations and Recommendations for Online Learning during COVID-19 Pandemic Era. Pak J Med Sci (2020) 36(COVID19-S4):S27-S31. doi:10.12669/pjms.36.COVID19-S4.2785
33. Brenneisen Mayer, F, Souza Santos, I, Silveira, PSP, Itaqui Lopes, MH, de Souza, ARND, Campos, EP, et al. Factors Associated to Depression and Anxiety in Medical Students: a Multicenter Study. BMC Med Educ (2016) 16(1):282. doi:10.1186/s12909-016-0791-1
34. Islam, S, Akter, R, Sikder, T, and Griffiths, MD. Prevalence and Factors Associated with Depression and Anxiety Among First-Year university Students in Bangladesh: a Cross-Sectional Study. Int J Ment Health Addict (2020) 20:1289–302. doi:10.1007/s11469-020-00242-y
35. Saeed, H, Saleem, Z, Ashraf, M, Razzaq, N, Akhtar, K, Maryam, A, et al. Determinants of Anxiety and Depression Among university Students of Lahore. Int J Ment Health Addict (2018) 16(5):1283–98. doi:10.1007/s11469-017-9859-3
36. ul Haq, MA, Dar, IS, Aslam, M, and Mahmood, QK. Psychometric Study of Depression, Anxiety and Stress Among university Students. J Public Health (2018) 26:211–7. doi:10.1007/s10389-017-0856-6
37. Cohen, S. Social Relationships and Health. Am Psychol (2004) 59(8):676–84. doi:10.1037/0003-066X.59.8.676
38. Thoits, PA. Mechanisms Linking Social Ties and Support to Physical and Mental Health. J Health Soc Behav (2011) 52(2):145–61. doi:10.1177/0022146510395592
39. Dour, HJ, Wiley, JF, Roy-Byrne, P, Stein, MB, Sullivan, G, Sherbourne, CD, et al. Perceived Social Support Mediates Anxiety and Depressive Symptom Changes Following Primary Care Intervention. Depress Anxiety (2014) 31(5):436–42. doi:10.1002/da.22216
40. Stanton, R, To, QG, Khalesi, S, Williams, SL, Alley, SJ, Thwaite, TL, et al. Depression, Anxiety and Stress during COVID-19: Associations with Changes in Physical Activity, Sleep, Tobacco and Alcohol Use in Australian Adults. Int J Environ Res Public Health (2020) 17(11):4065. doi:10.3390/ijerph17114065
41. Ge, F, Di Zhang, LW, and Mu, H. Predicting Psychological State Among Chinese Undergraduate Students in the COVID-19 Epidemic: a Longitudinal Study Using a Machine Learning. Neuropsychiatr Dis Treat (2020) 16:2111–8. doi:10.2147/NDT.S262004
42. Murat, M, Köse, S, and Savaşer, S. Determination of Stress, Depression and Burnout Levels of Frontline Nurses during the COVID-19 Pandemic. Int J Ment Health Nurs (2021) 30(2):533–43. doi:10.1111/inm.12818
43. Chew, NW, Ngiam, JN, Tan, BY, Tham, SM, Tan, CY, Jing, M, et al. Asian-Pacific Perspective on the Psychological Well-Being of Healthcare Workers during the Evolution of the COVID-19 Pandemic. BJPsych open (2020) 6(6):e116. doi:10.1192/bjo.2020.98
44. Cabarkapa, S, Nadjidai, SE, Murgier, J, and Ng, CH. The Psychological Impact of COVID-19 and Other Viral Epidemics on Frontline Healthcare Workers and Ways to Address it: A Rapid Systematic Review. Brain Behav Immun Health (2020) 8:100144. doi:10.1016/j.bbih.2020.100144
45. Spoorthy, MS, Pratapa, SK, and Mahant, S. Mental Health Problems Faced by Healthcare Workers Due to the COVID-19 Pandemic–A Review. Asian J Psychiatr (2020) 51:102119. doi:10.1016/j.ajp.2020.102119
46. Jafri, L, Ahmed, S, and Siddiqui, I. Impact of COVID-19 on Laboratory Professionals-A Descriptive Cross Sectional Survey at a Clinical Chemistry Laboratory in a Developing Country. Ann Med Surg (2020) 57:70–5. doi:10.1016/j.amsu.2020.07.022
47. Aristovnik, A, Keržič, D, Ravšelj, D, Tomaževič, N, and Umek, L. Impacts of the COVID-19 Pandemic on Life of Higher Education Students: A Global Perspective. Sustainability (2020) 12(20):8438. doi:10.3390/su12208438
48. Andrews, G, Issakidis, C, and Carter, G. Shortfall in Mental Health Service Utilisation. Br J Psychiatry (2001) 179(5):417–25. doi:10.1192/bjp.179.5.417
49. Daly, M, Sutin, AR, and Robinson, E. Longitudinal Changes in Mental Health and the COVID-19 Pandemic: Evidence from the UK Household Longitudinal Study. Psychol Med (2020) 52:2549–58. doi:10.1017/S0033291720004432
50. Brooks, SK, Webster, RK, Smith, LE, Woodland, L, Wessely, S, Greenberg, N, et al. The Psychological Impact of Quarantine and How to Reduce it: Rapid Review of the Evidence. Lancet (2020) 395(10227):912–20. doi:10.1016/S0140-6736(20)30460-8
51. Wang, G, Zhang, Y, Zhao, J, Zhang, J, and Jiang, F. Mitigate the Effects of home Confinement on Children during the COVID-19 Outbreak. Lancet (2020) 395(10228):945–7. doi:10.1016/S0140-6736(20)30547-X
52. Conte, F, Cellini, N, De Rosa, O, Rescott, ML, Malloggi, S, Giganti, F, et al. Dissociated Profiles of Sleep Timing and Sleep Quality Changes across the First and Second Wave of the COVID-19 Pandemic. J Psychiatr Res (2021) 143:222–9. doi:10.1016/j.jpsychires.2021.09.025
53. Lo Martire, V, Caruso, D, Palagini, L, Zoccoli, G, and Bastianini, S. Stress & Sleep: A Relationship Lasting a Lifetime. Neurosci Biobehav Rev (2020) 117:65–77. doi:10.1016/j.neubiorev.2019.08.024
54. de Haas, M, Faber, R, and Hamersma, M. How COVID-19 and the Dutch ‘intelligent Lockdown’change Activities, Work and Travel Behaviour: Evidence from Longitudinal Data in the Netherlands. Transp Res Interdiscip Perspect (2020) 6:100150. doi:10.1016/j.trip.2020.100150
55. Hou, WK, Lai, FT, Ben-Ezra, M, and Goodwin, R. Regularizing Daily Routines for Mental Health during and after the COVID-19 Pandemic. J Glob Health (2020) 10(2):020315. doi:10.7189/jogh.10.020315
56. Hou, WK, Lai, FT, Hougen, C, Hall, BJ, and Hobfoll, SE. Measuring Everyday Processes and Mechanisms of Stress Resilience: Development and Initial Validation of the Sustainability of Living Inventory (SOLI). Psychol Assess (2019) 31(6):715–29. doi:10.1037/pas0000692
57. Driessen, E, Beatty, A, Stokes, A, Wood, S, and Ballen, C. Learning Principles of Evolution during a Crisis: An Exploratory Analysis of Student Barriers One Week and One Month into the COVID-19 Pandemic. Ecol Evol (2020) 10(22):12431–6. doi:10.1002/ece3.6741
Keywords: anxiety, mental health, COVID-19, depression, stress, DASS-21, undergraduate students
Citation: Nano JP, Ghaly MH and Fan W (2022) Lessons From Early COVID-19: Associations With Undergraduate Students’ Academic Performance, Social Life, and Mental Health in the United States. Int J Public Health 67:1604806. doi: 10.3389/ijph.2022.1604806
Received: 28 January 2022; Accepted: 28 November 2022;
Published: 12 December 2022.
Edited by:
Olaf von dem Knesebeck, University Medical Center Hamburg-Eppendorf, GermanyReviewed by:
Jesus Alejandro Aldana Lopez, Instituto Jalisciense de Salud Mental, MexicoCopyright © 2022 Nano, Ghaly and Fan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Joseph P. Nano, am9zZXBoLnAubmFub0BnbWFpbC5jb20=; Mina H. Ghaly, Z2hhbHltYmNAZ21haWwuY29t
†These authors share first authorship
This Original Article is part of the IJPH Special Issue “The Impact of the COVID-19 Pandemic on Mental Health”
 Joseph P. Nano
Joseph P. Nano Mina H. Ghaly
Mina H. Ghaly Wen Fan2
Wen Fan2