Abstract
Objectives: The aim of this study was to estimate the prevalence of anti-microbial resistance (AMR) carriage and its risk factors in hospitalized migrants. Additionally, the prevalence of infectious diseases was evaluated, as well as symptoms of psychological trauma.
Methods: We conducted a retrospective monocentric cross-sectional study including all migrant patients recently arrived and hospitalised over a one-year period.
Results: Among 101 patients, seventy-nine percent originated from Sub-Saharan Africa. The overall AMR carriage rate was 20.7% [95% CI: 12.4; 28.9%]. We isolated 5/92 methicillin-resistant Staphylococcus aureus strains (5.4%) and 15/92 extended-spectrum beta-lactamase-producing Enterobacteriaceae (16.4%). AMR carriage was associated with older age, region of origin and length of migration. Rates of HIV, HBV, and HCV infection were 39.6%, 32.7%, and 5%, reflecting sampling bias linked to reasons for hospitalization. Eleven percent had serological evidence of treponemasis and 7.8% had Chlamydia trachomatis infection. Symptoms of depression or post-traumatic stress disorder were observed for more than half the patients.
Conclusion: It appears essential to offer a systematic and comprehensive post-arrival screening of AMR carriage, infectious diseases and psychological trauma to subjects who experienced migration.
Introduction
Emergence and dissemination of multi-drug resistant (MDR) and extensive drug-resistant (XDR) bacteria are an increasing public health problem, notably for extended-spectrum beta-lactamase producing Enterobacteriaceae (ESBL-E) [1]. International travels in particular play an important part in the worldwide spread of MDR bacteria [2]. According to the United Nations Migration Agency, we are facing a dramatic increase in the number of displaced people across various regions of the world. Since 2015, more than 2 million migrants have entered Europe during the recent refugee crisis [3].
Migrants are exposed to an increased risk of carriage of MDR bacteria and various other infectious diseases due to supposed higher prevalence rates in countries of origin [4], adverse migratory conditions (such as compromised hygiene and sanitation arrangements, overcrowding in containment areas) [5, 6], limited access to healthcare systems [7], and poor living conditions after resettlement [8]. Exposure to violence and trauma during migration, as well as difficult post-migratory living conditions, have been linked to serious psychological disorders in settled migrants [9, 10].
Few studies, summarised in a recent review [11], are available concerning the rate of anti-microbial resistance (AMR) carriage in newly-arrived migrants in Europe. Rates of MDR bacteria (ESBL-E and methicillin-resistant Staphylococcus aureus (MRSA)) carriage range between 20% [12, 13] and 60% [14] in Germany, and between 25% and 30% in Italy [15] and the Netherlands [16], respectively. No such data are available in France. Concerning infectious diseases, high rates of latent tuberculosis and hepatitis B infections have been reported in refugee and asylum seekers in various countries around Europe [17, 18]. In a recent French study performed by Médecins du Monde, rates of positive testing for HIV, HBV and HCV were respectively of 3.6%, 10.9%, and 8.6% in newly-arrived migrants. Syphilis testing was positive for 1.6% of patients and rates of Chlamydiae trachomatis (CT), and Neisseria gonorrhoeae infections were of 6.4% and 1.6%, respectively [19]. The European Centre for Disease Prevention and Control (ECDC) recommends the screening of latent tuberculosis, HIV, HCV, HBV, schistosomiasis, and strongyloidiasis for newly-arrived migrants depending on their country of origin [20]. However, there is likely significant heterogeneity in screening practices across France and in Europe, which emphasises the need for additional data.
Lastly, literature is scarce concerning the mental health of migrants arriving in France. Studies suggest that exposure to traumatic experiences before and during migration and post-migration stress are associated with psychiatric disorders such as depression, anxiety, and post-traumatic stress disorder (PTSD) [9, 21]. In a systematic review performed in 2005, symptoms of PTSD and depression were reported in 9% and 5% of refugees, respectively [10], and more recent data are lacking.
The objectives of this study were 1) to estimate the rate of carriage of MDR and XDR bacteria, 2) to identify factors associated with AMR carriage, 3) to evaluate rates of HIV, HBV, HCV, syphilis, Chlamydia trachomatis (CT), Neisseria gonorrhoeae (NG), and schistosomiasis infections, 4) and to screen for history of physical or sexual abuse and symptoms evocative of depression or PTSD in hospitalised migrants in and out settings.
Methods
Patient Selection and Study Design
We performed a retrospective cross-sectional study that included patients who sought care in the Infectious Diseases department of a university teaching hospital (Saint-Antoine Hospital, Paris, France). Medical records of subjects hospitalised in in-patient and out-patient units from November 2017 to the end of October 2018 were screened for inclusion. All migrants, defined as 1) foreign-born and 2) having arrived in France within 12 months from Eastern Europa, Africa, the Middle-East, Asia or South-America were eligible. Non-inclusion criteria was age inferior to 18 years.
Data Collection
Clinical and biological variables were retrospectively retrieved from our systematic post-arrival survey archived in the medical files (Supplementary Figure S1) and local computer healthcare systems and included [1]: demographic characteristics (age, gender, country of birth and living, marital status, profession, spoken language) [2], history of migration (date of departure and of arrival, countries travelled, means of travel, living conditions during travel (refugee camp, prison), history of violence (physical or sexual), living conditions in France, and administrative status [3]; medical history (including alcohol and tobacco consumption, prior vaccinations, prior antibiotic use, reason for hospitalisation) and symptoms evocative of psychiatric conditions including depression, anxiety, and PTSD using the standardize tool (Mini International Neuropsychiatric Interview (MINI) [4]; microbiological data, which are part of the hospital usual screening policy for migrant patients. Screening for MDR/XDR bacteria were performed with precultures in brain heart infusion broth with 10-µg/ml cefotaxime, 3.3-µg/ml ertapenem, or 3.3-µg/ml vancomycin (to select for ESBL-E, Carbapanemase-producing Enterobacteriaceae (CPE), or Vancomycin-resistant Enterococcus (VRE), respectively) after inoculation from nasal and anal swabs. Each culture were plated on medium for selective isolation (bioMerieux ESBL for ESBL-E). Bacterial colonies were identified using mass spectrometry (MALDI Biotyper; Bruker) and susceptibility testing used Mueller-Hinton agar (Bio-Rad). Serological testing were systematically performed for HIV (HIV-Antibody (Ab), HBV (HBs Antigen (Ag), HBc-Ab, HBs-Ab), HCV (HCV-Ab), syphilis (TPHA-VDRL) (Regent Kits Abbott) as well as PCR testing for CT and NG in urine or vaginal samplings (Roche Diagnostics). Hemoglobin electrophoresis and schistosomiasis serology (ELISA Novatec, Western Blot LDbio diagnostics) were also performed for all patients originating from Sub-Saharan Africa.
Data from de-identified patients were collected in a computerized database with a double data entry check.
Statistical Analyses
As ESBL-E carriage was the most prevalent, statistical analyses focused on it. MRSA was not included because of different modes of transmission and risk factors. Demographic, migration, living conditions in France, clinical, and laboratory characteristics were compared between patients with or without ESBL-E carriage using the chi-squared or Fisher’s exact tests and the Student or Wilcoxon ranked tests for categorical and continuous variables, respectively. The association between ESBL carriage and the covariables was then examined using a multiple logistic regression model. A backward-stepwise process based on the Akaike information criterion was used to select the risk factors. Nine variables were included in this selection process: first, all covariables with a p-value <0.1 in univariate analysis, except the variables “diagnosis” and “time from arrival to sampling” (because of its similarity with the variable “time from arrival to hospitalization” and the absence of significant differences in the time from hospitalization and sampling between both groups) and, second, factors a priori deemed to be possibly significant risk factors (HBV and HIV infections). The final model included the 3 variables shown in the column «Multivariable analysis» of Table 3. ORs, 95% CIs and p-values were calculated. Significance was determined by a p-value <0.05. Statistical analyses were performed using R version 3.6.1.
Results
Over the one-year period, 1023 records were screened, and 101 patients were included in the present analysis after identification of 148 eligible patients and exclusion of 47 (Figure 1). Among these, 71 were male (70.3%), with a median age (IQR [Q1, Q3]) of 30 years (12 [24, 36]). Seventy-nine (78.2%) originated from Sub-Saharan Africa and 30 (30.9%) were asylum seekers. The principal routes of migration were by direct flight (n = 31, 32%), through Libya and Italy (n = 32, 33%), and through Morocco and Spain (n = 24, 24.7%). The median duration of migration (IQR [Q1, Q3]) was 21.7 weeks (70.4 [0.14, 70.5]), and 30.1% of patients had been in at least one refugee camp. In France, 65% lived in poor conditions (homelessness or living in temporary accommodations, including shelters, refugee camps or hostels) (Table 1).
FIGURE 1
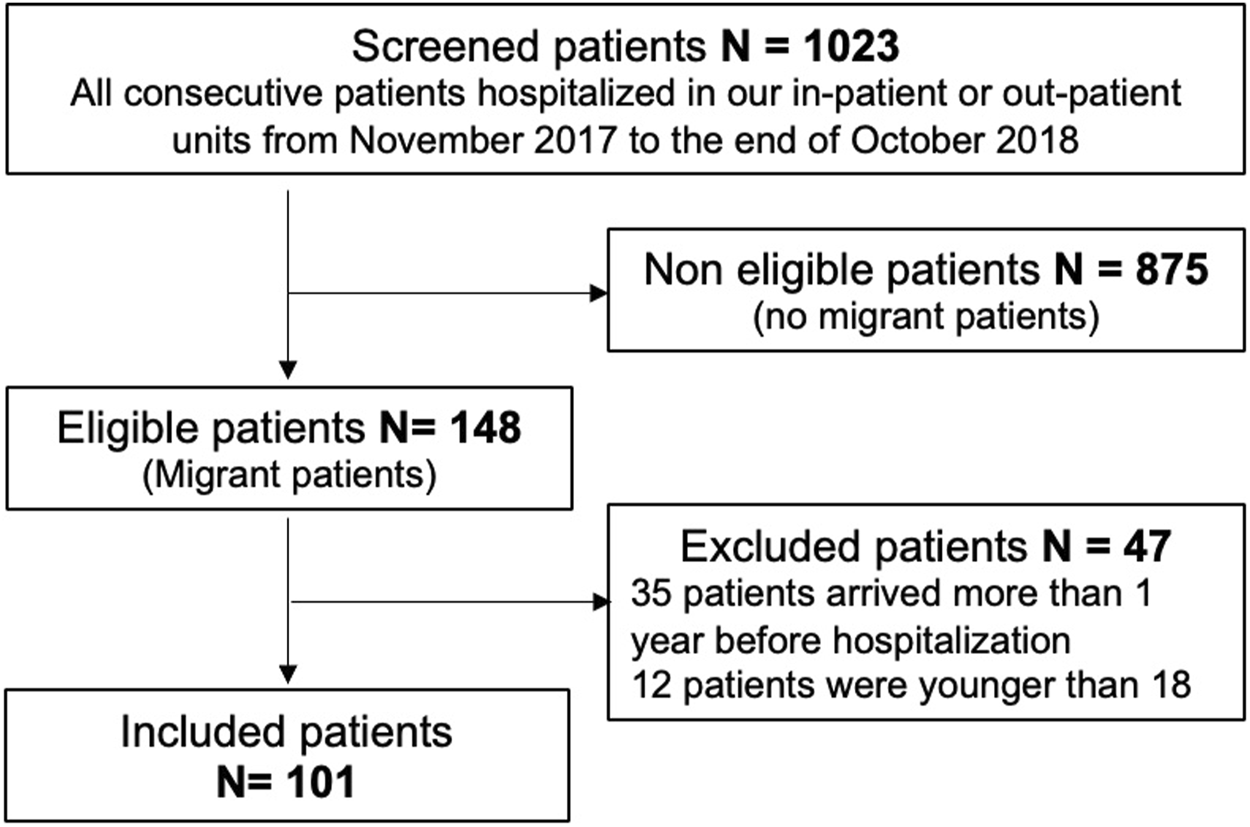
Flow chart (Migrinf study, France, 2018).
TABLE 1
| n | Value | |
|---|---|---|
| Demographics | ||
| Gender, male, n (%) | 101 | 71 (70.3) |
| Age (years), median (IQR) | 101 | 30.0 (12.0) |
| Marital status, married, n (%) | 98 | 24 (24.5) |
| Region of origin, n (%) | 101 | |
| Sub-Saharan Africa | 79 (78.2) | |
| South America | 4 (4.0) | |
| Asia | 4 (4.0) | |
| Eastern Europa | 7 (6.9) | |
| North Africa | 3 (3.0) | |
| Middle-east | 4 (4.0) | |
| Urban area, n (%) | 89 | 26 (29.2) |
| Education level, no higher education, n (%) | 93 | 68 (73.1) |
| Profession, n (%) | 94 | |
| Craftmanship | 36 (38.3) | |
| Higher occupation | 7 (7.4) | |
| Student | 13 (13.8) | |
| Intermediate occupation | 14 (14.9) | |
| No profession | 24 (25.5) | |
| Alcohol use, n (%) | 98 | 15 (15.3) |
| Tobacco use, n (%) | 99 | 19 (19.2) |
| Drug use, n (%) | 96 | 3 (3.1) |
| Recent antibacterial therapy (previous 6 months), n (%) | 84 | 26 (31.0) |
| Migration | ||
| Route of Migration, n (%) | 97 | |
| Direct flight | 31 (32.0) | |
| Through Lybia and Italy | 32 (33.0) | |
| Through Morocco and Spain | 24 (24.7) | |
| Through the Balkans and Greece | 9 (9.3) | |
| Other | 1 (1.0) | |
| Duration of migration (weeks), median (iqr) | 88 | 21.7 (70.4) |
| Refugee camp (at least once), n (%) | 92 | 28 (30.4) |
| Travel by foot (at least one border), n (%) | 94 | 10 (10.6) |
| Physical abuse, n (%) | 96 | 41 (42.7) |
| Sexual abuse, n (%) | 90 | 14 (15.6) |
| Experienced or witnessed a life-threatening event, n (%) | 95 | 40 (42.1) |
| Living conditions in France | ||
| Poor living conditionsa, n (%) | 100 | 65 (65.0) |
| No health insurance coverage, n (%) | 100 | 55 (55.0) |
| Asylum seeker, n (%) | 97 | 30 (30.9) |
| Hospital data | ||
| Reason for admission, n (%) | 96 | |
| Referral by a third party | 68 (70.8) | |
| Own consultation | 5 (5.2) | |
| Emergency consultation | 23 (24.0) | |
| In-patient hospitalisation, n (%) | 101 | 43 (42.6) |
| Diagnosis, n (%) | 100 | |
| Bacterial infection | 12 (12.0) | |
| Viral infection | 62 (62.0) | |
| Tuberculosis | 13 (13.0) | |
| Other | 13 (13.0) | |
Patient characteristics (Migrinf study, France, 2018).
Poor living conditions: homelessness or living in temporary accommodations, including shelters, refugee camps or hostels.
AMR Carriage and Risk Factors for ESBL-E Carriage
The overall rate of carriage of MDR bacteria was 20.7% [95% CI: 12.4; 28.9%]. We isolated 5/92 (5.4%) MRSA strains and 15 (16.3%) ESBL-E, including 11 Escherichia coli, 3 Klebsiella pneumoniae and 1 Enterobacter cloacae (Tables 2, 3). Of the 15 ESBL, 14 were CTX-M-15 enzymes and one was CTX-M-14. Neither carbapenem-resistant Enterobacteriaceae, imipenem-resistant Acinetobacter baumanii nor vancomycin-resistant Enterococci were isolated.
TABLE 2
| Total (N) | Value | Estimated prevalence (%, 95% CI) | |
|---|---|---|---|
| Overall AMR carriage, n (%) | 92 | 19 (20.7) | 20.7 (12.4–28.9) |
| MRSA carriage, n (%) | 92 | 5 (5.4) | 5.4 (0.8–10.0) |
| ESBL carriage, n (%) | 92 | 15 (16.3) | 16.3 (8.7–23.8) |
| IRAB, n (%) | 92 | 0 (0) | — |
| CPE, n (%) | 92 | 0 (0) | — |
| HCV infection, n (%) | 100 | 5 (5.0) | 5.0 (0.73–9.3) |
| HIV infection, n (%) | 101 | 40 (39.6) | 39.6 (30.1–49.1) |
| HBV infection, n (%) | 101 | 33 (32.7) | 32.7 (23.5–41.8) |
| Syphilis, n (%) | 90 | 10 (11.0) | 11.0 (4.6–17.4) |
| Schistosomiasis, n (%) | 73 | 11 (15.1) | 15.1 (6.9–23.3) |
| Chlamydiae trachomatis, n (%) | 77 | 6 (7.8) | 7.8 (1.8–13.8) |
| Neisseria gonorrhoeae, n (%) | 77 | 0 (0) | — |
| Mycoplasma spp, n (%) | 44 | 2 (4.5) | — |
| Haemoglobin electrophoresis, n (%) | 58 | — | |
| Heterozygous sickle cell disease | 6 (10.3) | 10.3 (2.5–18.2) | |
| Normal | 45 (77.6) | 77.6 (66.8–88.3) | |
| Other abnormalities | 7 (12.1) | 12.1 (3.7–20.4) | |
| Symptoms of depressiona, n (%) | 94 | 50 (53.2) | 53.2 (43.1–63.3) |
| Symptoms of anxiety disorderb, n (%) | 91 | 55 (60.4) | 60.4 (50.4–70.5) |
Prevalence of anti-microbial resistance carriage, infectious diseases, and others (Migrinf study, France, 2018).
Sadness, low spirits, lack of willpower.
Excessive irritability, acute anxiety attack, chronic excessive anxiety and revivification episodes.
MRSA, methicillin resistant Staphylococcus aureus; ESBL, Extended Spectrum Beta-lactamase producing Enterobacteriaceae; IRAB, imipenem resistant Acinetobacter Baumanii; CPE, carbapenemase - producing Enterobacteriaceae.
TABLE 3
| Total | ESBL - | ESBL + | Univariable analysis | Multivariable analysis | p-value | |
|---|---|---|---|---|---|---|
| (n) | (n = 77) | (n = 15) | p-value | OR (95% CI)a | ||
| Demographics | ||||||
| Gender, male, n (%) | 92 | 56 (72.7) | 9 (60) | 0.322 | ||
| Age, median (IQR) | 92 | 29.8 (9.9) | 39.9 (12.7) | < 0.001 | 22.2 (3.37–523.0) b | 0.008 |
| Region of origin, n (%) | 92 | 0.050 | ||||
| Sub-Saharan Africa | 62 (80.5) | 10 (66.7) | ||||
| South America | 4 (5.2) | 0 (0) | ||||
| Asia | 3 (3.9) | 0 (0) | ||||
| Eastern Europa | 3 (3.9) | 3 (20) | ||||
| North Africa | 1 (1.3) | 2 (13.3) | ||||
| Middle East | 4 (5.2) | 0 (0) | ||||
| Urban area, n (%) | 80 | 48 (71.6) | 11 (84.6) | 0.496 | ||
| Profession, n (%) | 85 | 0.093 | ||||
| Craftmanship | 26 (36.1) | 5 (38.5) | ||||
| Higher occupation | 6 (8.3) | 1 (7.7) | ||||
| Student | 12 (16.7) | 0 (0) | ||||
| Intermediate occupation | 8 (11.1) | 5 (38.5) | ||||
| No profession | 20 (27.8) | 2 (15.4) | ||||
| Education level, no higher education, n (%) | 84 | 52 (73.2) | 9 (69.2) | 0.765 | ||
| Alcohol use, n (%) | 89 | 12 (16) | 1 (7.1) | 0.683 | ||
| Tobacco use, n (%) | 90 | 15 (19.7) | 1 (7.1) | 0.449 | ||
| Drug use, n (%) | 87 | 2 (2.7) | 1 (7.1) | 0.413 | ||
| Recent antibacterial therapy (previous 6 months) n (%) | 76 | 18 (29) | 6 (42.9) | 0.334 | ||
| Migration | ||||||
| Route of migration, n (%) | 89 | 0.252 | ||||
| Direct by flight | 21 (28) | 8 (57.1) | ||||
| Through Lybia and Italy | 28 (37.3) | 2 (14.3) | ||||
| Through Morocco and Spain | 18 (24) | 3 (21.4) | ||||
| Through the Balkans and Greece | 7 (9.3) | 1 (7.1) | ||||
| Other | 1 (1.3) | 0 (0) | ||||
| Direct route of migration | 89 | 21 (28) | 8 (57.1) | 0.033 | ||
| Duration of migration (weeks), median (IQR) | 79 | 25.3 (73.1) | 0.4 (7.8) | 0.074 | ||
| Refugee camp (at least once), n (%) | 84 | 23 (32.9) | 2 (14.3) | 0.213 | ||
| Travel by foot (at least one border), n (%) | 86 | 9 (12.5) | 1 (7.1) | 1.000 | ||
| Physical violence, n (%) | 87 | 34 (46.6) | 4 (28.6) | 0.214 | ||
| Sexual violence, n (%) | 82 | 10 (14.7) | 2 (14.3) | 1.000 | ||
| Living conditions in France | ||||||
| Poor conditions of living, n (%) | 91 | 48 (63.2) | 11 (73.3) | 0.647 | ||
| No social rights, n (%) | 91 | 38 (50%) | 12 (80%) | 0.064 | ||
| Hospital data | ||||||
| Way of hospital admission, n (%) | 87 | 0.257 | ||||
| Referral by a third party | 52 (72.2) | 9 (60) | ||||
| Own consultation | 5 (6.9) | 0 (0) | ||||
| Emergency consultation | 15 (20.8) | 6 (40) | ||||
| Inpatient hospitalisation, n (%) | 92 | 32 (41.6) | 10 (66.7) | 0.133 | ||
| Time from arrival to sampling (days), median (IQR) | 86 | 139.5 ± 176.8 | 38.0 ± 78.2 | 0.005 | ||
| Time from hospitalization to sampling (days), median (IQR) | 86 | 1.0 ± 7.2 | 1.0 ± 3.5 | 0.612 | ||
| Time from arrival to hospitalisation (days), median (IQR) | 86 | 121.5 ± 153.8 | 35.5 ± 81.2 | 0.007 | 0.991 (0.979–0.999) | 0.108 |
| Diagnosis, n (%) | 91 | 0.011 | ||||
| Bacterial infection | 6 (7.9) | 4 (26.7) | ||||
| Viral infection | 50 (65.8) | 7 (46.7) | ||||
| Tuberculosis | 13 (17.1) | 0 (0) | ||||
| Other | 7 (9.2) | 4 (26.7) | ||||
| HIV infection, n (%) | 92 | 29 (37.7) | 9 (60.0) | 0.108 | 8.75 (0.519–419.5) | 0.182 |
| HCV infection, n (%) | 91 | 2 (2.6) | 3 (20.0) | 0.029 | ||
| HBV infection, n (%) | 92 | 27 (35.1) | 2 (13.3) | 0.132 | ||
Factors associated with extended-spectrum beta lactamase producing Enterobacteriaceae (ESBL-E) carriage (Migrinf study, France, 2018).
Bold values correspond to values <0.1 in the univariate.
Only the variables selected by the backward-stepwise process are shown.
For the multivariate analysis, 86 observations were included. The “age” variable was transformed into a binary variable, using the median age of the global population (i.e., 30 years old) as a threshold, as well as the « region of origin » variable (Sub-Saharan Africa versus other regions). 86 observations.
In univariate analysis, patients with ESBL-E carriage were significantly older (36 years-old vs. 28 years-old, p < 0.001) and originated from Eastern Europe (20% vs. 3.9%, p = 0.05) and North Africa (13.3% vs. 1.3%, p = 0,05). Patients with ESBL-E carriage more often arrived from direct flight (p = 0.033) and after a shorter duration of migration (0.4 weeks vs. 25.3 weeks, p = 0.074). The delay from arrival to hospitalization and sampling was shorter for patients with ESBL-E carriage (35 vs. 121 days, p = 0.007 and 38 vs. 139 days, p = 0.005 respectively). In multivariate analysis, only older age remained independently statistically associated with ESBL-E carriage (p = 0.008).
Older age, direct flight and shorter delay from arrival to sampling were also significantly associated with ESBL-E carriage when considering only patients originated from sub-Saharan Africa (data not shown).
Prevalence of Other Infections and Others
Rates of HIV, HBV, and HCV infection were 39.6%, 32.7%, and 5% respectively. These high rates were reflecting sampling bias linked to reasons for hospital admission as patients were addressed for treatment and/or monitoring of these chronic viral infections (Table 2). Eleven out of 73 patients (15%) had serological evidence of schistosomiasis: nine were male and all originated from Sub-Saharan Africa. Six out of 77 (7.8%) had CT infection corresponding to 3 men and 3 women with a mean age of 28 years old. Hemoglobin electrophoresis performed in patients originating from sub-Saharan Africa showed abnormalities in almost a quarter (22.4%) of cases, including 10.3% of sickle cell disease trait. History of physical abuse during migration was reported in 41 patients (42.7%). Sexual abuse was reported by 12 women (42.9%). Fifty patients presented with symptoms suggesting depression (53.2%), and 55 presented with symptoms consistent with an anxiety disorder (60.4%).
Discussion
In this cross-sectional study of migrant individuals coming to France mainly from Sub-Saharan Africa, MDR bacteria carriage was estimated at 20.7% [95% CI: 12.4; 28.9%]. To our knowledge, this is the first such study to be carried out in France and reporting the prevalence of AMR in migrants. AMR carriage in the general French population has been estimated around 6% in 2011 [22]. Recently-arrived migrants therefore seem to have higher AMR carriage rates than the French population. This higher rate has already been described in other European countries, and mostly ranged between 20 and 30% [12, 15, 16].
E-ESBL were the most frequent MDR bacteria isolated (16.3%), as previously reported [11]. To our knowledge, our study is the first to identify ESBL with all but one enzyme being CTX-M-15, confirming the spread and globalization of CTX-M enzymes and especially CTX-M-15 [23].
One of the most interesting results of this study is the significantly higher risk of ESBL-E carriage in cases of direct migratory trajectory by flight (p = 0.033) and a trend towards a higher risk in cases of shorter duration of migration (p = 0.074). This suggests that the country of origin may be an important marker for AMR carriage in newly-arrived migrants. The importance of the country of origin was previously described in a study in Switzerland, where a higher risk of ESBL-E carriage for patients was reported in patients originating from the Middle East [24]. However, a recent meta-analysis of previous European studies highlighted higher AMR prevalence in high-migrant community settings (refugee centers or outpatient’s clinics), suggesting that AMR carriage was mostly acquired during transit or in migrant settings [11]. Indeed, in the literature, adverse migratory conditions such as compromised hygiene and overcrowding in containment areas have been linked to increasing infectious diseases transmission [6]. Thus, both countries of origin and migratory conditions may have a role in AMR carriage acquisition and transmission.
We also found that older age was significantly associated with ESBL carriage, which to our knowledge has not been previously reported. As the patterns of migration in Europe are likely to evolve over time, with an expected generalization of migration from populations of more diverse age groups, this aspect certainly warrants further consideration.
High rates of venereal diseases such CT infections were found in our study (7.8% [95% CI: 1.8–13.8%]). It should however be noted that this could be confounded by similarly high rates of HIV infection in our population, due to bias caused by reasons for hospital referral. It can also be mentioned that CT infections were screened in vaginal or urinal samples and not in pharyngeal or rectal ones that may have led to underestimate CT prevalence. However, similar rates (6.4%) were previously reported in a study of newly-arrived migrants tested on a voluntary basis [19]. These rates remain high compared to the 3.8% globally observed in 2016 [25]. Screening for venereal diseases is not recommended for newly-arrived migrants. Our data suggest that it should be considered for systematic screening.
Serological evidence for schistosomiasis was found in 15% of patients originating from Sub-Saharan Africa. This high prevalence is similar to the 17% already reported in Italy [26], and strongly suggests the need for systematic screening in these populations. A recent European review confirmed the safety, high effectiveness, and cost-effectiveness of systematic screening of schistosomiasis and praziquantel-based treatment for newly-arrived migrants from endemic countries [27].
Hemoglobin electrophoresis was systematically performed in patients originating from sub-Saharan Africa and showed abnormalities in almost a quarter (22.4%) of cases, including 10.3% of sickle cell disease trait. In France, high-risk population could benefit from early diagnosis in order to prevent complications. Testing for sickle cell disease trait in migrants originated from Sub-Saharan could also lead to information about prenatal diagnosis. No data seemed available on this topic in the literature.
The high rates of psychological symptoms are a significant concern. Indeed, symptoms of depression and anxiety (from excessive irritability to PTSD) were reported in 53.2% [95% CI: 43.1–63.3%] and 60.4% [95% CI: 50.4–70.5%] of patients, respectively. This is higher than was previously reported in the literature: from 5 to 30% for depression and from 10 to 30% for PTSD [10, 28]. Psychological symptoms may be explained by pre-displacement factors, including political persecution, gender, and sexual orientation, and by post-displacement factors, such as social isolation and difficulties in finding employment and housing [29]. Once diagnosed, providing access and continuity to appropriate mental health care for these patients remains a significant challenge, due in part to infrequent recourse to healthcare professionals, lack of social security coverage, and to cultural considerations. Psychiatric symptoms in this setting are however barriers to social integration [30], and are likely to have long-term repercussions on the overall health of migrants. This highlights the urgent need for increased medical awareness of these issues and improvements in the screening and care for mental health in migrants.
The main limitations of our study are the small sample size and the retrospective nature that implies some missing data. Due to the low sample size of our study and the number of missing data for some co-variables, our study may be underpowered and therefore, have underestimated the prevalence of studied conditions and the association between ESBL carriage and some exposure variables. All the screening tests are routinely performed and correspond to the usual practice of our department, which minimizes the risk for recruitment bias and limits the amount of missing data. It is important to notice that the patients included in our study were specifically referred to our department for medical care, and therefore are not representative of the general migrant population. However, reasons for hospitalization were not directly related to the studied conditions which minimizes the risk for recruitment bias. Furthermore, as recommended in France (High Council of Public Health 2019), AMR carriage research was performed as soon as the patients are hospitalized in order to reduce any over risk directly related to hospital settings. Screening patients in first referral medical centers would improve the sensitivity of these analyses.
The European Center for Disease Prevention and Control recently published guidelines on screening for infectious diseases in newly-arrived migrants [20]. This study adds necessary data concerning the health of recently-arrived migrants. As high rates of MDR carriage, of CT infections, and of psychological disorders were observed in our population, the results of this study should argue for the addition of these conditions to a comprehensive screening policy of all newly-arrived migrants.
Finally, more comprehensive data regarding the global prevalence of AMR carriage are required, particularly in low-income countries where increased use of antibiotics is likely to increase the prevalence the prevalence of MDR bacteria. This would allow for a better understanding of the dynamics of dissemination of AMR carriage on a global scale and mitigate the risk of the spreading of an AMR pandemic.
Conclusion
With regards to the high prevalence of AMR, infectious diseases and psychological disorders found in this population of migrants, it appears essential to offer a systematic and comprehensive post-arrival screening of infectious diseases and signs of psychological trauma to all subjects who experienced migration.
Statements
Ethics statement
French legislation on non-interventional studies requires collection of patient non-opposition but does not require written consent. As such, each patient included in the study was informed orally and/or with a written information note translated in the appropriate language, and non-opposition was obtained for the use of their de-identified medical data. This study was authorised by the French Competent Authority because our unit respects the “Méthodologie de réference MR004” and after registration in “Repertoire public des études réalisées sous Méthodologie de Réference“ with the registration number 4914111018.
Author contributions
SS, OP, M-AP, P-MG, KL, and LS: Conception, data collection, data analysis, writing the paper. LD and KL: Statistical analysis, writing the paper. DD and VL: Bacteriological analysis, proofreading the paper.
Acknowledgments
We would like to thank the following people for participating in the care of the patients: Pacanowski J., Meynard J. L., Chopin D., Badoro B., Beaumont A. L., Beron O., Le Pluart D., Roux A., Saada N., Schmidt J., Huriez P., Couture P., Faure G., Tieu A., Cauchois L., Charvet A. L., Colbert C., Combes A., Albert C., Fontaine M., Fourati O., Francon H., Huang A., Joulia H., Lherault G., Lignieres G., Marois K., Benjamin J., Coly M., Cousin O., Demeester A., Dorges P., Esnault V., Gay P., Guilhem Ducleon G., Lahitte A.
Conflict of interest
The authors declare that they do not have any conflicts of interest.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/ijph.2022.1604792/full#supplementary-material
Supplementary Figure S1Example of systematic survey (France, 2018).
References
1.
WHO. Antimicrobial Resistance: Global Report on Surveillance. (2014). [Internet]. WHO. [cité 11 mars 2019] Disponible sur: http://www.who.int/drugresistance/documents/surveillancereport/en/.
2.
van der Bij AK Pitout JDD . The Role of International Travel in the Worldwide Spread of Multiresistant Enterobacteriaceae. J Antimicrob Chemother (2012) 67(9):2090–100. 10.1093/jac/dks214
3.
Migrant EU . Refugee Arrivals by Land and Sea Approach One Million in 2015. Geneva, Switzerland: International Organization for Migration (2015). [Internet]. [cité 11 mars 2019]Disponible sur:https://www.iom.int/news/eu-migrant-refugee-arrivals-land-and-sea-approach-one-million-2015.
4.
World Health Organization. Worldwide Country Situation Analysis: Response to Antimicrobial Resistance. [Internet]. [cité 11 mars 2019] (2015). Disponible sur:http://apps.who.int/iris/bitstream/10665/163468/1/9789241564946_eng.pdf?ua=1&ua=1.
5.
Wilson S . Infectious Diseases of Specific Relevance to Newly Arrived Migrants in the EU EEA. Sweden: European Centre for Disease Prevention and Control (2015). 6.
6.
Maltezou HC Theodoridou M Daikos GL . Antimicrobial Resistance and the Current Refugee Crisis. J Glob Antimicrob Resist (2017) 10:75–9. 10.1016/j.jgar.2017.03.013
7.
Morris MD Popper ST Rodwell TC Brodine SK Brouwer KC . Healthcare Barriers of Refugees post-resettlement. J Community Health (2009) 34(6):529–38. 10.1007/s10900-009-9175-3
8.
Tosas Auguet O Betley JR Stabler RA Patel A Ioannou A Marbach H et al Evidence for Community Transmission of Community-Associated but Not Health-Care-Associated Methicillin-Resistant Staphylococcus Aureus Strains Linked to Social and Material Deprivation: Spatial Analysis of Cross-Sectional Data. Plos Med (2016) 13(1):e1001944. 10.1371/journal.pmed.1001944
9.
Nickerson A Bryant RA Schnyder U Schick M Mueller J Morina N . Emotion Dysregulation Mediates the Relationship between Trauma Exposure, post-migration Living Difficulties and Psychological Outcomes in Traumatized Refugees. J Affect Disord (2015) 173:185–92. 10.1016/j.jad.2014.10.043
10.
Fazel M Wheeler J Danesh J . Prevalence of Serious Mental Disorder in 7000 Refugees Resettled in Western Countries: a Systematic Review. Lancet (2005) 365(9467):1309–14. 10.1016/S0140-6736(05)61027-6
11.
Nellums LB Thompson H Holmes A Castro-Sánchez E Otter JA Norredam M et al Antimicrobial Resistance Among Migrants in Europe: a Systematic Review and Meta-Analysis. Lancet Infect Dis (2018) 18(7):796–811. 10.1016/S1473-3099(18)30219-6
12.
Leistner R Denkel LA Gastmeier P Werner G Layer F Pfeifer Y . Prevalence of MRSA and Gram-Negative Bacteria with ESBLs and Carbapenemases in Patients from Northern Africa at a German Hospital. J Antimicrob Chemother (2015) 70(11):3161–4. 10.1093/jac/dkv219
13.
Heudorf U Albert-Braun S Hunfeld KP Birne FU Schulze J Strobel K et al Multidrug-resistant Organisms in Refugees: Prevalences and Impact on Infection Control in Hospitals. Frankfurt, Germany: German Medical Science GMS Publishing House (2016). [Internet] août [cité 9 août 2017]Disponible sur: http://www.egms.de/en/journals/dgkh/2016-11/dgkh000276.shtml.
14.
Reinheimer C Kempf VAJ Göttig S Hogardt M Wichelhaus TA O’Rourke F et al Multidrug - Resistant Organisms Detected in Refugee Patients Admitted to a University Hospital, Germany, June‒December 2015. Eurosurveillance (2015) 21(2):1560–7917. [Internet]. 14 janv 2016 [cité 9 août 2017]. 10.2807/1560-7917.ES.2016.21.2.30110
15.
Angeletti S Ceccarelli G Vita S Dicuonzo G Lopalco M Dedej E et al Unusual Microorganisms and Antimicrobial Resistances in a Group of Syrian Migrants: Sentinel Surveillance Data from an Asylum Seekers centre in Italy. Trav Med Infect Dis (2016) 14(2):115–22. 10.1016/j.tmaid.2016.03.005
16.
Ravensbergen SJ Lokate M Cornish D Kloeze E Ott A Friedrich AW et al High Prevalence of Infectious Diseases and Drug-Resistant Microorganisms in Asylum Seekers Admitted to Hospital; No Carbapenemase Producing Enterobacteriaceae until September 2015. PLoS One (2016) 11(5):e0154791. 10.1371/journal.pone.0154791
17.
European Centre for Disease Prevention and Control. Rapid Risk Assessment: Communicable Disease Risks Associated with the Movement of Refugees in Europe during the winter Season, 16 November 2015. (2015). [Internet]. [cité 4 oct 2017]Disponible sur: http://ecdc.europa.eu/en/publications-data/rapid-risk-assessment-communicable-disease-risks-associated-movement-refugees.
18.
Eiset AH Wejse C . Review of Infectious Diseases in Refugees and Asylum Seekers-Current Status and Going Forward. Public Health Rev (2017) 38:22. 10.1186/s40985-017-0065-4
19.
Mangin F Sulli L Matra R Dépistage Du Vih, Des Hépatites Et Des Ist Chez Les Personnes Migrantes Primoarrivantes Au Caso De Médecins Du Monde De Saint-Denis, De 2012 À 2016/Screening For Hiv, Hepatitis And Stis Among Recent Migrants At The Healthcare And Advice Clinics (Caso) Of Doctors Of The World In Saint-Denis (France) From 2012 To 2016. (2018). Saint Denis, France: BEH (Bulletin épidémiologique hebdomadaire) (2018). p. 805
20.
European Centre for Disease Prevention and Control. Public Health Guidance on Screening and Vaccination for Infectious Diseases in Newly Arrived Migrants within the EU/EEA. Europa: A European Center foe Disease Prevention and Control (ECDC) publication (2018).
21.
Bogic M Njoku A Priebe S . Long-term Mental Health of War-Refugees: a Systematic Literature Review. BMC Int Health Hum Rights (2015) 15(1):29. [Internet]. déc 2015 [cité 4 oct 2017]. 10.1186/s12914-015-0064-9
22.
Nicolas-Chanoine MH Gruson C Bialek-Davenet S Bertrand X Thomas-Jean F Bert F et al 10-Fold Increase (2006-11) in the Rate of Healthy Subjects with Extended-Spectrum β-lactamase-producing Escherichia coli Faecal Carriage in a Parisian Check-Up centre. J Antimicrob Chemother (2013) 68(3):562–8. 10.1093/jac/dks429
23.
Woerther PL Burdet C Chachaty E Andremont A . Trends in Human Fecal Carriage of Extended-Spectrum β-lactamases in the Community: toward the Globalization of CTX-M. Clin Microbiol Rev (2013) 26(4):744–58. 10.1128/CMR.00023-13
24.
Piso RJ Käch R Pop R Zillig D Schibli U Bassetti S et al A Cross-Sectional Study of Colonization Rates with Methicillin-Resistant Staphylococcus aureus (MRSA) and Extended-Spectrum Beta-Lactamase (ESBL) and Carbapenemase-Producing Enterobacteriaceae in Four Swiss Refugee Centres. PLoS One (2017) 12(1):e0170251. 10.1371/journal.pone.0170251
25.
Rowley J Vander Hoorn S Korenromp E Low N Unemo M Abu-Raddad LJ et al Chlamydia, Gonorrhoea, Trichomoniasis and Syphilis: Global Prevalence and Incidence Estimates, 2016. Bull World Health Organ (2019) 97(8):548–62P. 10.2471/BLT.18.228486
26.
Beltrame A Buonfrate D Gobbi F Angheben A Marchese V Monteiro GB et al The Hidden Epidemic of Schistosomiasis in Recent African Immigrants and Asylum Seekers to Italy. Eur J Epidemiol (2017) 32(8):733–5. 10.1007/s10654-017-0259-6
27.
Agbata EN Morton RL Bisoffi Z Bottieau E Greenaway C Biggs BA et al Effectiveness of Screening and Treatment Approaches for Schistosomiasis and Strongyloidiasis in Newly-Arrived Migrants from Endemic Countries in the EU/EEA: A Systematic Review. Int J Environ Res Public Health (2018) 16(1):11. 10.3390/ijerph16010011
28.
Steel Z Silove D Phan T Bauman A . Long-term Effect of Psychological Trauma on the Mental Health of Vietnamese Refugees Resettled in Australia: a Population-Based Study. Lancet (2002) 360(9339):1056–62. 10.1016/S0140-6736(02)11142-1
29.
Porter M Haslam N . Predisplacement and Postdisplacement Factors Associated with Mental Health of Refugees and Internally Displaced Persons: A Meta-Analysis. JAMA. 3 août (2005) 294(5):602–12. 10.1001/jama.294.5.602
30.
Mollica RF McInnes K Sarajlić N Lavelle J Sarajlić I Massagli MP . Disability Associated with Psychiatric Comorbidity and Health Status in Bosnian Refugees Living in Croatia. JAMA. 4 août (1999) 282(5):433–9. 10.1001/jama.282.5.433
Summary
Keywords
migrants, schistosomiasis, psychological disorders, AMR carriage, ESBL-E, sexual transmitted infections, drepanocytosis
Citation
Stabler S, Paccoud O, Duchesne L, Piot M-A, Valin N, Decré D, Girard P-M, Lalande V, Lacombe K and Surgers L (2022) Prevalence of Antimicrobial Resistance and Infectious Diseases in a Hospitalised Migrant Population in Paris, France, a Retrospective Study. Int J Public Health 67:1604792. doi: 10.3389/ijph.2022.1604792
Received
24 January 2022
Accepted
23 November 2022
Published
15 December 2022
Volume
67 - 2022
Edited by
Lyda Osorio, University of Valle, Colombia
Reviewed by
Jonny Alejandro García Luna, Centro Internacional de Entrenamiento e Investigaciones Medicas, Colombia
Updates
Copyright
© 2022 Stabler, Paccoud, Duchesne, Piot, Valin, Decré, Girard, Lalande, Lacombe and Surgers.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sarah Stabler, sarah.stabler@univ-lille.fr
†These authors have contributed equally to this work
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.