- 1College of Nursing, Research Institute of Nursing Science, Ajou University, Suwon, South Korea
- 2Department of Neurosurgery, Johns Hopkins Medical Institute, Baltimore, MD, United States
- 3Department of Psychology, Morgan State University, Baltimore, MD, United States
Objectives: The global impact of COVID-19 driven by new variants may add to the negative mental health consequences of the prolonged pandemic, including posttraumatic stress symptoms (PTSS). University students may be prone to develop a series of PTSS due to life plan disruptions as well as increased uncertainty caused by the pandemic. The purpose of this study was to assess the associations between pandemic fatigue, anxiety sensitivity (AS), and PTSS among university students in South Korea.
Methods: Using convenience sampling, 400 students participated in this cross-sectional online survey. Descriptive statistics and linear mixed models were used to examine factors associated with PTSS.
Results: About one-third (32.3%) of the participants reported clinically significant levels of PTSS. Multivariate analyses revealed that pandemic fatigue (β = 0.124, p < 0.001) and AS (β = 0.212, p < 0.001) were significantly associated with PTSS while controlling for other study variables.
Conclusion: Young adults who feel more fatigue related to the COVID-19 pandemic and with high AS should be given access to mental health resources to better manage their mental health and reduce PTSS.
Introduction
The novel coronavirus outbreak began in December of 2019, and the Corona virus diseases (COVID-19) pandemic persists worldwide. In January of 2020, the World Health Organization (WHO) declared a public health emergency [1]. Since this time, the number of new cases and deaths from COVID-19 has steadily increased, with 212 billion new cases and 4.4 million deaths as of August 2021 [2]. The global fourth wave of the COVID-19 appears driven by the Delta SARS-CoV-2 variant which was identified as more infectious, and with increased transmissibility even in vaccinated individuals [2].
Extensive consequences of the pandemic have been reported, influencing healthcare [3], education [4], the economy [5], and individuals’ daily lives [6]. Negative consequences of the pandemic on mental health outcomes have been widely studied, including associations with depression, anxiety disorders, stress, panic attacks, and posttraumatic stress symptoms (PTSS) [7, 8]. Young adults, in particular, are at high-risk for the development of mood and anxiety disorders [9] and the disruptions caused by the COVID-19 pandemic on educational and occupational opportunities may have increased their mental health vulnerability [10]. The various pandemic-mitigating strategies of social distancing, university closures, and remote classes have created mental health challenges for university students worldwide [11–17]. Furthermore, the fourth wave of SARS-CoV-2 strains has enhanced the threat toward individuals by extending uncertainty about when the pandemic will end. Having experienced and witnessed the unpredictable and uncontrollable attack of COVID-19 on life and the public policy efforts to control and manage public health emergencies, young adults may prone to develop a series of trauma-relevant psychological symptoms, namely PTSS [18].
Pandemic fatigue is a mental and physical phenomenon that occurs during a pandemic as a consequence of disruptions in individuals’ daily lives, such as lockdown, quarantine, and social distancing [19]. Pandemic fatigue is understood as a natural and expected response to a prolonged public health emergency, recent studies have reported evidence of pandemic fatigue after a few months of the lockdown implementation [20, 21]. Recently, Labrague and Ballad [22] found that a significant proportion of university students experience pandemic fatigue. Fatigue has also been associated with stress, general worries, and COVID-19 specific worries [21]. Inadequate physical/mental self-care among individuals increases fatigue, specifically during the prolonged pandemic, and the negative influence of pandemic fatigue on mental health has been reported [22].
Several personality traits are associated with various aspects of mental health. One such factor is anxiety sensitivity (AS), which is defined as the fear that anxiety symptoms or arousal, can have harmful consequences [23, 24]. The influence of AS on PTSS is of great concern regarding university students [25, 26]. Previous studies revealed that AS is a significant factor associated with PTSS [27, 28], and there are positive relationships between AS and posttraumatic stress disorder (PTSD) severity in military veterans [29], victims of domestic violence [30], and the general population [31]. Elevated trait AS was positively correlated with worry and fear of epidemic outbreaks during the Zika virus and Ebola virus epidemics [32, 33]. Individuals with a tendency to have greater “fear of fear” may experience greater negative feelings during the prolonged COVID-19 pandemic, negatively impacting their mental health.
In South Korea, the fourth wave of COVID-19 began in July of 2021. The number of daily new cases of COVID-19 approached its highest peak since the pandemic began (from 1.02 new cases per million in July 2020 to 29.76 in July 2021), possibly fueled by the increased rate of Delta variant transmission [34, 35]. Activities in universities are restricted during the fourth wave of pandemic in South Korea, and most of the classes are still conducted remotely. COVID-19 full vaccination rate was 12.3% in Mid-July 2021 because vaccines were not sufficiently available by that time in South Korea [36], compared to 48.9% in the United States [37]. Young adults who sought vaccination, especially during the prolonged pandemic, may be frustrated by the unavailability of the vaccines. Low vaccination rates combined with spread of the Delta Variant in South Korea this may exacerbate anxiety and stress associated with the COVID-19 pandemic [38].
Methods
Aim, Design, and Participants
To our knowledge, no current study has focused explicitly on pandemic fatigue, AS, and PTSS related to COVID-19 among university students. The purpose of this study was to describe the status of COVID-19 related pandemic fatigue and PTSS among university students in South Korea. We also examined the associations of pandemic fatigue and AS, along with COVID-19 related factors with PTSS in this population. A descriptive-correlational research design was used. Participants in this study were adults 18 years of age or older who lived in South Korea during the COVID-19 pandemic, were currently attending three or 4-year colleges and were native speakers of the Korean language. The number of study subjects was calculated using the G-Power program, with an effect size of 0.1, a significance level of 0.05, a power of 0.95, and 26 predictors required for multiple regression analysis. As a result, at least 358 subjects were required. Considering the dropout rate of 10%, 406 questionnaires were collected. After excluding 6 insincere questionnaires, 400 were included in the analysis. Participant students were from universities located in a diverse area in South Korea, including Seoul (the capital) and 9 provinces, with most of the participants (95.5%) from the large metropolitan areas of Seoul and K province.
Procedure
We distributed the online survey using Google® Forms between June 2021 and July 2021 to assess pandemic fatigue, AS, and PTSS during the COVID-19 pandemic. The survey link was published on university websites and online community dashboards. The Everytime (https://everytime.kr) is an online anonymous community dashboard for college students belonging to 400 universities in South Korea. It provides general information about college life, such as school life and academic management. Advertised universities include Ajou University, Gachon University, Yonsei University, Seoul National University, Suwon Science College, Dongguk University, Sungkyunkwan University, Hongik University, Korea National University of Arts, Soongsil University, Dongnam Health University, The University of Suwon, Duksung Women’s University, Dankook University, Seoul National University of Science and Technology, and Kookmin University. Information about the study was also posted on institutional homepages or on-campus bulletin boards (e.g., student halls, cafeterias, cafes, libraries, or on the student union hall) for recruitment. The study announcement described the purpose, method, and selection criteria of the study. A detailed explanation of the research was provided in a separate explanatory note, including a clause that there would be no disadvantages due to participation or non-participation in the research. We provided a QR code to access detailed information regarding the study and survey, and potential participants accessed the survey link through the QR code once they agreed to participate. Because of the nature of the online survey, voluntary participation was considered as consent to enroll in the study. Approximately 20–25 min were required to compete the survey; the survey was designed to proceed to the next item when all the previous items were completed to enhance the quality of the responses. Study participants were provided with mobile gift cards ($5) after the completion. The questionnaire consisted of two sections which investigated 1) demographics and COVID-19 related characteristics, 2) pandemic fatigue, AS, and PTSS.
Measures
Posttraumatic Stress Symptoms
We used the Impact of Event Scale-6 (IES-6), which is a 6-item instrument to assess PTSS. This is an abbreviated version of the Impact of Event Scale-revised (IES-R) whose validity has been previously reported [39, 40]. It includes three symptom subscales of posttraumatic stress disorder (PTSD), including intrusion, hyper-arousal, and avoidance. Respondents were asked to report how distressed or bothered they were, over the past 7 days, by trauma-related symptoms ascribed to the COVID-19 pandemic. Each item is scored 0 (not at all) to 4 (extremely). The score was calculated as the average of 6 items, with a higher total score indicating a higher level of PTSS. For this study, the English version of the IES-6 was translated into Korean by two Korean-English bilingual translators. These translators (HJK and JYH) were native Koreans, received a doctoral degree in the US and had practiced in academia in the US. Any differences were reconciled, and the reconciled version was translated back into English by an independent, bilingual translator. The back-translated English version was compared with the original English version to check for any loss of meaning. Cronbach’s alpha [41] for the IES-6 in the current study was 0.82.
Pandemic Fatigue
Pandemic fatigue was measured using the Pandemic Fatigue Scale (PFS) developed by Lilleholt et al. [42]. Translation of the PFS into the Korean language was conducted in the same manner as described above to translate the IES-6. The PFS consists of six items that assess pandemic fatigue, defined as demotivation to engage in recommended COVID-19 protective behaviors (behavioral fatigue) and resistance to receiving information meant to mitigate the spread of the pandemic (information fatigue). Behavioral fatigue items included statements such as “When friends or family members talk about COVID-19, I try to change the subject because I do not want to talk about it anymore.” Information fatigue items include statements such as “I am sick of hearing about COVID-19.” For each statement, participants choose a response score ranging from 1 to 7 to indicate that they “strongly disagree” to “strongly agree” with the statement. The sum of the response scores for all six items provides a measure of participants’ overall pandemic fatigue. The higher the overall PFS score, the greater the pandemic fatigue reported by participants. Cronbach’s alpha for the PFS in the current study was 0.84.
Anxiety Sensitivity
The Anxiety Sensitivity Index (ASI) is a tool to measure the tendency of excessive and persistent responses to anxiety-triggering stimuli [43]. In this study, the Korean version of ASI was used to measure AS. The ASI is an 18-item self-report tool for assessing anxiety-related physical, cognitive, or social concerns. Respondents indicated their level of agreement with each item on a scale ranging from “very little” (coded as 0) to “very much” (coded as 4). The total score is the sum score of all items, with higher scores on the scale representing more severe AS. The Korean version of ASI has been verified for validity and reliability [44]. In this study, Cronbach’s alpha for the ASI was 0.85.
Demographics and COVID-19 Related Characteristics
Demographics collected consisted of questions about age, gender, education, perceived economic status, prescribed or over-the-counter (OTC) medications, frequency of physical activity, tobacco smoking, alcohol consumption, and caffeine intake. COVID-19-related characteristics consisted of questions about COVID-19-related health behaviors (wearing protective equipment, hand washing, social distancing, etc.). Participants were also asked about COVID-19 related symptoms and COVID-19 PCR diagnostic testing, COVID-19 vaccination status, their intention to be vaccinated, and levels of worry related to the vaccine (measured using a 5-point Likert scale where 1 indicates not at all worried and 5 indicates extremely worried) and COVID-19 exposure.
Analysis
Participant demographics and COVID-19-related characteristics, pandemic fatigue, AS, and PTSS levels were analyzed as descriptive statistics (n, %, mean, SD, range). Normality of the data was checked using histograms and normal probability plots, skewness, or kurtosis measures. An independent t-test or a one-way ANOVA was performed for differences in PTSS according to the participants’ demographics and COVID-19-related stressors. Pearson’s correlation coefficients were used to analyze the correlation among study variables, including pandemic fatigue, AS, and PTSS. The Benjamini-Hochberg procedure was used to control the false discovery rate for multiple comparisons in the bivariate analysis.
Linear mixed models nested by location of university were used to examine factors associated with PTSS. All variables designated as associated with PTSS in bivariate analysis were entered into the models along with several demographic characteristics (gender, major, education, and perceived economic status). Given the strong evidence of gender differences in the mental health characteristics during the COVID-19 pandemic [45, 46], we conducted a subgroup analysis by gender. Six out of 406 participants were excluded due to incomplete responses, and there were no missing data in the dataset. Multicollinearity was evaluated using VIF, residuals, and outliers to determine whether the independent variables were suitable for regression analysis. Data were analyzed using the STATA 15.1 (StataCorp, Texas, United States).
Results
Sample Characteristics Related to COVID-19
The average participant age was 21.7 years (SD = 2.6, range: 18–39 years). A majority were female (71.8%, n = 287) and attending a 4-year college (82.8%, n = 331). Fifty-two percent of the participants were attending a university located in Seoul, and 42.5% in K province the location of two metropolitan areas in South Korea. Academic fields of study of participating students were diverse, including basic science and engineering (39.5%), social science, humanities, and education (42.3%), and medical (11.5%). Almost half of the participants reported they were “satisfied” with their economic status (46.5%, n = 186). More than 70% of participants did not take any prescribed (86.0%, n = 344) or OTC medications (74.3%, n = 297), while 12.5% were currently smoking. The percent of participants reporting not consuming alcohol or caffeine was 23.8% and 13.8%, respectively (Table 1).
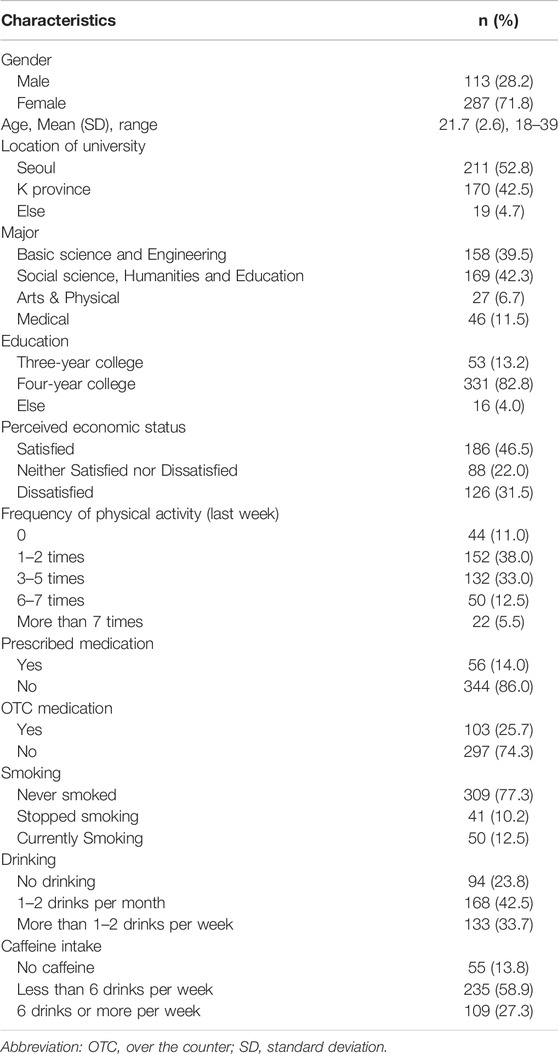
TABLE 1. General characteristics of participants (N = 400) (Mental health status during the COVID-19 pandemic among university students, South Korea, 2021).
Fifty-six percent of participating university students reported staying at home most of the time or always to avoid infection. Most participants (95.9%) always wore a mask when going outside, and KF-94 masks specifically produced to avoid droplet infection were the most commonly used mask (58.2%). Fifty-six percent of participants watched news about COVID-19 for 1, 2 h per week. More than half (55.0%) of the participants had COVID-19-like symptoms in the past week, including coughing, chills, or runny nose. Approximately twenty-five percent of the participants had COVID-19 test, and all were negative. Most participants worried about COVID-19 exposure (75.3%) and going outside (68.8%) at moderate or higher levels. At the time of the survey, only 13% of the participants were vaccinated, but 85.3% of non-vaccinated participants answered they are likely or definitely getting vaccinated when it’s available. About fifty percent of participants were at least moderately worried about side effects of COVID-19 vaccines (Table 2).
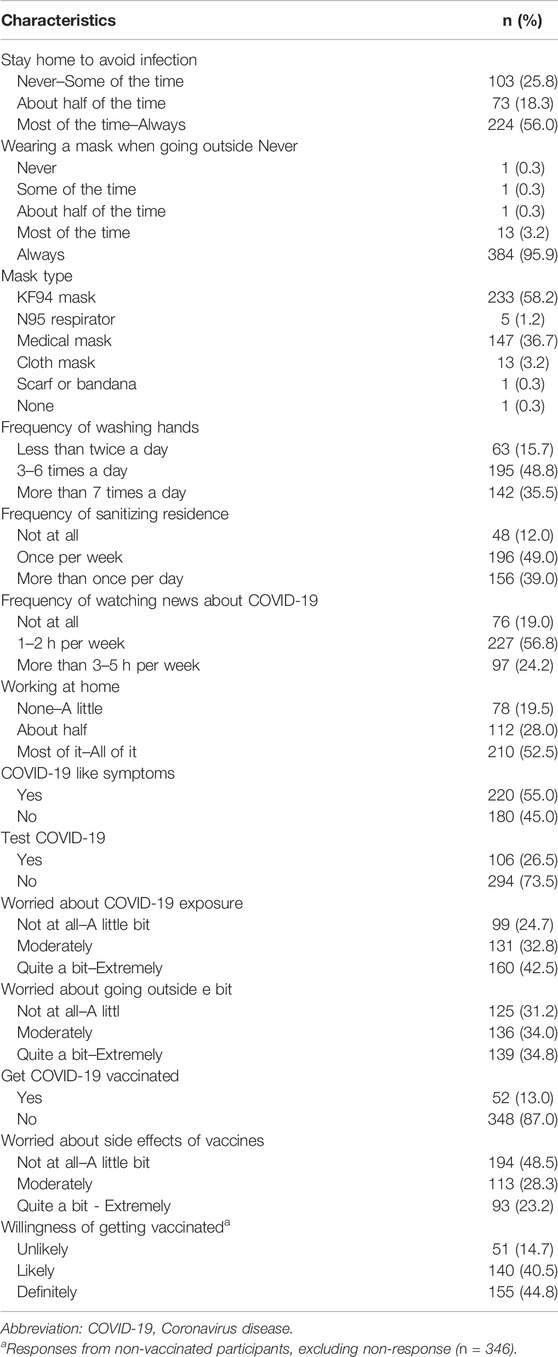
TABLE 2. COVID-19 related characteristics of participants (N = 400) (Mental health status during the COVID-19 pandemic among university students, South Korea, 2021).
Levels of PTSS, Pandemic Fatigue, and Anxiety Sensitivity
The average of PTSS of the participants was 14.06 (SD = 5.04) and ranged from 6 to 29. Using the cutoff score of 10 previously validated for the IES-6 scale [39, 40], 32.3% of the participants self-reported levels of PTSS indicative of PTSD. The average total pandemic fatigue score was 22.27 (SD = 7.41), ranging from 6 to 40. The anxiety sensitivity level of the participants averaged 11.27 (SD = 8.75), ranging from 0 to 52 (Table 3).
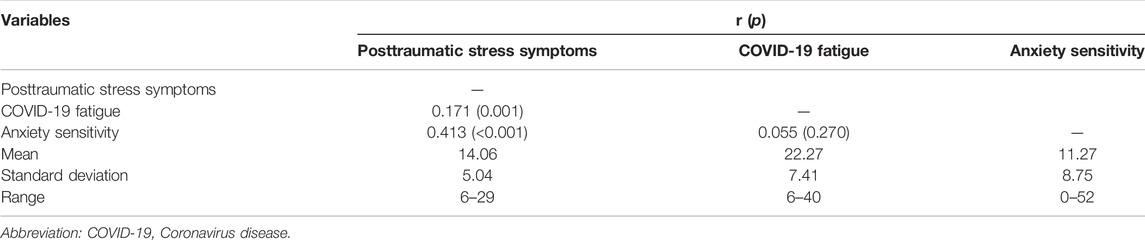
TABLE 3. Correlation among study variables (N = 400) (Mental health status during the COVID-19 pandemic among university students, South Korea, 2021).
Factors Associated With PTSS
Demographic and COVID-19 related factors associated with PTSS in the bivariate analysis included education, having been taking OTC/prescribed medication, staying home to avoid infection, mask type, having had COVID-19 like symptoms, worry about COVID-19 exposure, worry about going outside, and worry about side effects of COVID-19 vaccines (Supplementary S1–S3). Among these variables, mask type was excluded in the final model due to its low level of variance.
The linear mixed model (Table 4), nested by location of university, revealed that staying at home to avoid infection (β = 2.345, p < 0.001, 95% CI = [1.034, 3.656]), being worried about COVID-19 exposure (β = 1.404, p = 0.050, 95% CI = [0.003, 2.805]), COVID-19 fatigue (β = 0.124, p < 0.001, 95% CI = [0.062, 0.186]), and AS (β = 0.212, p < 0.001, 95% CI = [0.158, 0.265]) were significantly associated with PTSS after controlling for other demographic and COVID-19 related factors. Those who stayed at home about half of the time to avoid infection were estimated to be 2.3 units higher in PTSS compared to those who never or sometimes stayed home. Those who worried quite a bit or extremely about COVID-19 exposure were estimated to be 1.4 units higher in PTSS compared to those who worried not at all or a little bit. Higher COVID-19 fatigue and AS was associated with higher PTSS. Subgroup analysis by gender indicated that COVID-19 fatigue (β = 0.237, p < 0.001, 95% CI = [0.113, 0.360]) and AS (β = 0.262, p < 0.001, 95% CI = [0.139, 0.375]) were significantly associated with PTSS in males, while staying at home to avoid infection (β = 2.874, p = 0.001, 95% CI = [1.208, 4.540]), being worried about going outside due to COVID-19 (staying at home to avoid infection (β = 1.988, p = 0.029, 95% CI = [0.207, 3.768]), COVID-19 fatigue (β = 0.086, p = 0.017, 95% CI = [0.015, 0.157]), and AS (β = 0.208, p < 0.001, 95% CI = [0.148, 0.267]) were significantly associated with PTSS in females (Table 4).
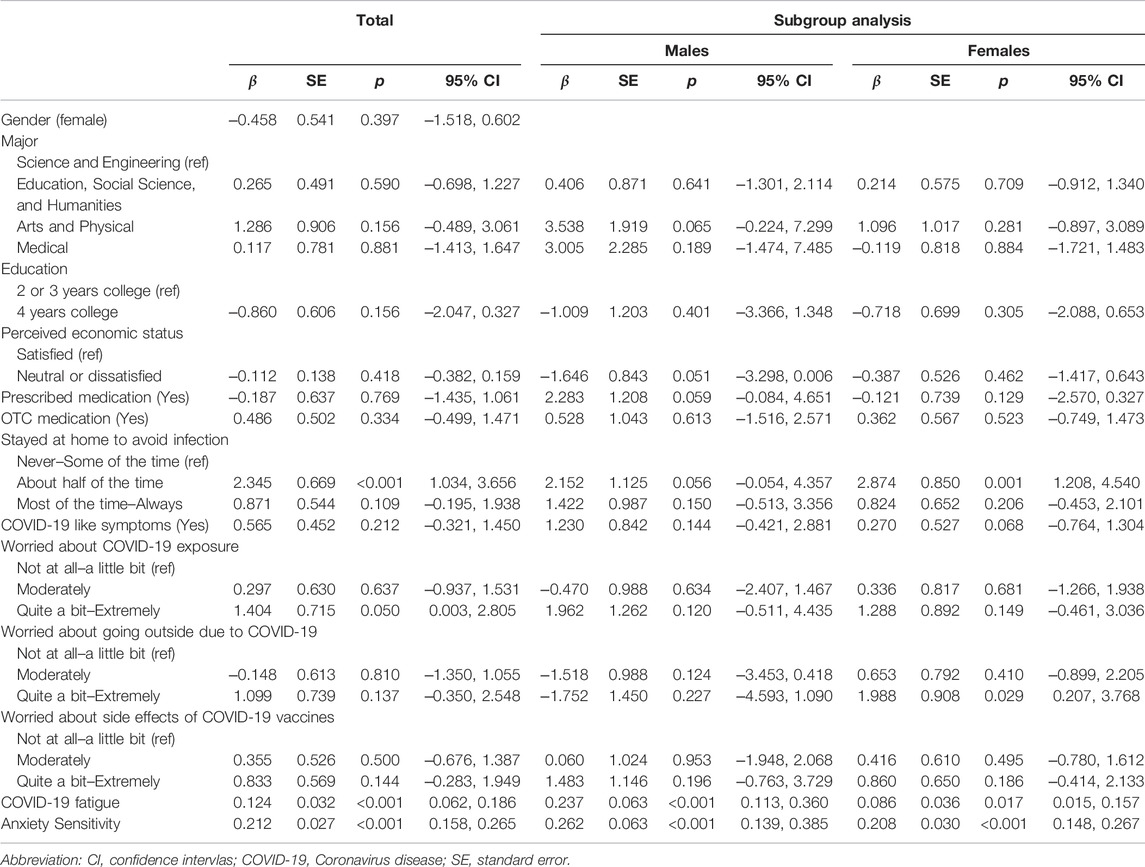
TABLE 4. Linear mixed models to test associated factors to Posttraumatic Stress Symptom (N = 400) (Mental health status during the COVID-19 pandemic among university students, South Korea, 2021).
Discussion
This study examined COVID-19 related PTSS and its associated factors, including demographic characteristics, COVID-19 related factors, pandemic fatigue, and AS among university students in South Korea. The prevalence of PTSS indicative of probable PTSD in our sample was 32.3%, which is relatively high compared to another study in China conducted 1 month after the December 2019 COVID-19 outbreak [11]. A recent study among healthcare workers during the COVID-19 pandemic reported a PTSS prevalence of 26.2% in Italy [47]. Part of the reason for this discrepancy may be the use of different measurements for PTSS between the two studies; the previous studies used PTSD Checklist for DSM-5, whereas the current study used the IES-6 scale. Our results are comparable to a study conducted in the US, reporting 31.8% of prevalence of PTSS indicative of likely PTSD among young adults [11]. These results suggest a relatively high prevalence of PTSD-like symptomatology among young adults during the most recent wave of the COVID-19 pandemic. University students may be particularly distressed in managing their school or work responsibilities, while uncertainty about the end of the COVID-19 pandemic may exacerbate adverse effects on their mental health.
In the linear mixed model analysis, several COVID-19 related factors were associated with PTSS, including staying at home to avoid infection, and worry regarding exposure to SARS-CoV-2 virus. As most participants were living in an urban area where the COVID-19 infection rates were high in South Korea, they may have been worried about viral infection and experienced stress from more restrictive social distancing policies. Interestingly, subgroup analysis revealed some gender differences in those COVID-19 related factors that were associated with PTSS; for male students, the two factors (staying at home to avoid infection and worry regarding exposure to SARS-CoV-2 virus) were not significantly associated with PTSS, whereas staying at home to avoid infection and worry about going outside due to COVID-19 were significantly associated with PTSS in females. These differences suggest that female students are more sensitive to quarantine methods (e.g., staying at home, worrying about going outside) to avoid infection and that these quarantine measures are associated with higher PTSS in females.
The current study revealed that pandemic fatigue and AS were significant factors of PTSS among both male and female university students. Pandemic fatigue is found across cultures and populations [42, 48] as efforts to reduce the spread of COVID-19 are ongoing. The pandemic fatigue phenomena might be related to social and economic factors as well as other pre-existing risks [42, 48, 49]. Morgul et al. [48] for example, reported a significant proportion of participants with less knowledge about COVID-19, general educational attainment, and lower socioeconomic status had greater pandemic fatigue than individuals not belonging to those groups. Furthermore, Lilleholt et al. [42] found greater pandemic fatigue in German and Danish individuals who reported greater worry about the economic consequences of the pandemic. The current study adds to the literature by providing evidence on pandemic fatigue among young adults with relatively self-rated high socio-economic status.
Young adults who feel more fatigue from the COVID-19 pandemic may be more vulnerable to PTSD-like symptoms as their physical and psychological resources are taxed during mandated restrictions on activities to mitigate against viral exposure and spread. The increased psychological burden caused by navigating additional public health safeguards associated with the COVID-19 pandemic is a likely contributing factor exacerbating PTSD-like symptomatology. Previously, pandemic fatigue was found to be an important concern for healthcare workers during the pandemic [50], and the current study results suggests pandemic-related fatigue issues should also be addressed in university students given the associations found between pandemic fatigue and mental health during the COVID-19 pandemic among this population.
AS is a factor for developing PTSD. Previous studies have reported enhanced AS as predictive of development of PTSD symptomatology [28, 51] and positive correlations have been reported between the IES-R and AS [52]. More recent research has shown AS to be related to COVID-19-related anxiety, COVID-19-related worry, overall anxiety severity, depression, psychological impairment in university populations, health care workers and the general population in several countries [52–57].
The current study indicated AS was the factor explaining the amount of highest variance in PTSS among university students during the COVID-19 pandemic. This is consistent with a previous study reporting AS is predictive of COVID-19-related distress and worry among Canadian and American adults [58, 59]. The current study supports the influence of AS on COVID-19 PTSD-like symptomatology among young adults. The results of current study indicate that personality traits, such as AS, influence the PTSS more than demographic characteristics or even COVID-19 specific worries among Korean university students. University students with high AS should be screened and be provided with additional resources to better manage their mental health and to reduce the risk of developing PTSD.
In line with previous findings [11–17], the current study found negative effects of the COVID-19 pandemic on university students’ mental health status. To reduce the damaging mental health influences observed during the pandemic in this population, both local (university) and national level public policies should be developed. At local level, universities may develop and incorporate various online-based wellness programs using telemedicine, boot camps for coping strategies, self-help mindfulness therapy, virtual group exercise and meditation/mindfulness sessions [12, 15]. At the national level, policies to support universities and students are necessary for providing timely and accurate epidemic information and adequate and uniform schooling regulations (e.g., online vs. face-to-face class options, remote management/counseling programs) to avoid any confusion and uncertainty aroused from inconsistent regulations during the pandemic period.
Limitation
One limitation of this study is that we collected data only from South Korean university students in urban areas where relatively high COVID-19 transmission exists. Also, risk of selection bias and response-set bias may have occurred due to the convenience sampling method and data collection using an online/self-reported format. Therefore, generalizability of our results is limited. The scales used to measure AS and pandemic fatigue have not previously been used or validated among South Koreans. However, the undertook a thorough translation process and the internal consistency of the scales from the current sample was adequate. Future studies validating these measures among South Korean population are needed. Other important factors affecting mental health among university students, including self-rated health status, and life-style such as spending times outside or on electronic screens [15] were not captured in this study. Lastly, the incidence, pattern, and mutation of SARS-CoV-2 is dynamic; therefore, it is necessary to longitudinally examine changes in PTSD-like symptomatology related to the COVID-19 pandemic among university students.
Conclusion
Covid-19 pandemic has been prolonged with new variants (e.g., Delta, Omicron), and their impact on mental health should be recognized. Approximately one-third of the university students reported having experienced PTSS related to COVID-19 indicative of clinical PTSD. Pandemic fatigue and AS was significantly associated with PTSS in this population. Based on the results of the current study, we suggest university-wide programs to enhance mental health status among students, including providing platforms of social networking and interactions with peers to share their thoughts and emotions. Using various forms of digital and other interactions, including messaging or calls using social media has been reported to be associated with better mental health among university students [60]. Easily accessible online counseling for students who need the service should be provided, especially during the pandemic. AS was previously reported associated with suicidal ideation and past suicide attempts [24], and more attention should be given regarding this issue among Korean university students during the COVID-19 pandemic. Based on the previous evidence on efficacy of brief cognitive interventions on AS reduction [61], we also suggest providing interventions through convenient therapy platforms, such as video-based intervention [62], online interactions using social media and email/phone calls to foster bonding and social connection [15] to reduce AS among vulnerable university students.
Ethics Statement
Ethics approval for the study was given by the Ajou University Hospital IRB, and all protocols were carried out in accordance with the Declaration of Helsinki. A formal informed consent was waived due to the nature of the online survey. Participants were informed of the purpose of the study, and if they were willing to participate, they accessed the survey link through the QR code provided and fill out the online questionnaire.
Author Contributions
HK, TM, IT, and JM designed and conceptualized the study. HK, SB, and J-HP collected and organized the data. HK organized the whole data collection process and supervised the quality of the data collection. HK and SB analyzed the data and drew all the charts. HK wrote the first draft of the article. All authors participated in the revision of the paper and approved the final manuscript for publication.
Funding
The authors declare that this study received funding from Ajou University School of Medicine (New Faculty Research Fund) and from the National Institutes of Health Research, National Institutes of General Medical Sciences Award #U54MD013376. The funders were not involved in the study design, collection, analysis, interpretation of data, the writing of this article or the decision to submit it for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank all the students who participated in this study.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/ijph.2022.1604552/full#supplementary-material
Supplementary Table S1 | Difference of posttraumatic stress symptoms according to general characteristics of participants (N = 400) (Mental health status during the COVID-19 pandemic among university students, South Korea, 2021).
Supplementary Table S2 | Difference of posttraumatic stress symptoms according to COVID-19 related characteristics of participants (N = 400) (Mental health status during the COVID-19 pandemic among university students, South Korea, 2021).
Supplementary Table S3 | Benjamini-Hochberg procedure results of the bivariate analysis results (N = 400) (Mental health status during the COVID-19 pandemic among university students, South Korea, 2021).
Supplementary Table S4 | Normal probability, histogram of the PTSS (dependent variable), and skewness and kurtosis, VIF of the study variables (Mental health status during the COVID-19 pandemic among university students, South Korea, 2021).
Abbreviations
AS, anxiety sensitivity; IES-6, Impact of Events Scale; PTSS, posttraumatic stress symptoms.
References
1.World Health Organization. Statement on the Second Meeting of the International Health Regulations (2005) Emergency Committee Regarding the Outbreak of Novel Coronavirus (2019-nCoV) (2021). Available from: https://www.who.int/news/item/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov (Accessed Oct 21, 2021).
2.Centers for Disease Control and Prevention. Delta Variant: What We Know about the Science (2021). Available from: https://www.cdc.gov/coronavirus/2019-ncov/variants/delta-variant.html (Accessed Oct 21, 2021).
3. Bigiani, L, Bigiani, S, and Bigiani, A. How to Minimize the Impact of Pandemic Events: Lessons from the COVID-19 Crisis. Int J Health Pol Manag (2020) 9:469–74. doi:10.34172/ijhpm.2020.115
4. Radu, M-C, Schnakovszky, C, Herghelegiu, E, Ciubotariu, V-A, and Cristea, I. The Impact of the COVID-19 Pandemic on the Quality of Educational Process: A Student Survey. Ijerph (2020) 17:7770. doi:10.3390/ijerph17217770
5. Nicola, M, Alsafi, Z, Sohrabi, C, Kerwan, A, Al-Jabir, A, Iosifidis, C, et al. The Socio-Economic Implications of the Coronavirus Pandemic (COVID-19): A Review. Int J Surg (2020) 78:185–93. doi:10.1016/j.ijsu.2020.04.018
6. Di Renzo, L, Gualtieri, P, Pivari, F, Soldati, L, Attinà, A, Cinelli, G, et al. Eating Habits and Lifestyle Changes during COVID-19 Lockdown: An Italian Survey. J Transl Med (2020) 18:229. doi:10.1186/s12967-020-02399-5
7. Hossain, MM, Tasnim, S, Sultana, A, Faizah, F, Mazumder, H, Zou, L, et al. Epidemiology of Mental Health Problems in COVID-19: A Review. F1000Res (2020) 9:F1000Res636. doi:10.12688/f1000research.24457.1
8. Torales, J, O’Higgins, M, Castaldelli-Maia, JM, and Ventriglio, A. The Outbreak of COVID-19 Coronavirus and its Impact on Global Mental Health. Int J Soc Psychiatry (2020) 66(4):317–20. doi:10.1177/0020764020915212
9. Kessler, RC, Berglund, P, Demler, O, Jin, R, Merikangas, KR, and Walters, EE. Lifetime Prevalence and Age-Of-Onset Distributions of DSM-IV Disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry (2005) 62:593–602. doi:10.1001/archpsyc.62.6.593
10. Kujawa, A, Green, H, Compas, BE, Dickey, L, and Pegg, S. Exposure to COVID‐19 Pandemic Stress: Associations with Depression and Anxiety in Emerging Adults in the United States. Depress Anxiety (2020) 37:1280–8. doi:10.1002/da.23109
11. Liu, CH, Zhang, E, Wong, GTF, Hyun, S, and Hahm, HC. Factors Associated with Depression, Anxiety, and PTSD Symptomatology during the COVID-19 Pandemic: Clinical Implications for U.S. Young Adult Mental Health. Psychiatry Res (2020) 290:113172. doi:10.1016/j.psychres.2020.113172
12. Li, Y, Wang, A, Wu, Y, Han, N, and Huang, H. Impact of the COVID-19 Pandemic on the Mental Health of College Students: A Systematic Review and Meta-Analysis. Front Psychol (2021) 12:669119. doi:10.3389/fpsyg.2021.669119
13. Voltmer, E, Köslich-Strumann, S, Walther, A, Kasem, M, Obst, K, and Kötter, T. The Impact of the COVID-19 Pandemic on Stress, Mental Health and Coping Behavior in German University Students - a Longitudinal Study before and after the Onset of the Pandemic. BMC Public Health (2021) 21:1385. doi:10.1186/s12889-021-11295-6
14. Ochnik, D, Rogowska, AM, Kuśnierz, C, Jakubiak, M, Schütz, A, Held, MJ, et al. Mental Health Prevalence and Predictors Among university Students in Nine Countries during the COVID-19 Pandemic: A Cross-National Study. Sci Rep (2021) 11:18644. doi:10.1038/s41598-021-97697-3
15. Browning, MHEM, Larson, LR, Sharaievska, I, Rigolon, A, McAnirlin, O, Mullenbach, L, et al. Psychological Impacts from COVID-19 Among university Students: Risk Factors across Seven States in the United States. PLoS One (2021) 16:e0245327. doi:10.1371/journal.pone.0245327
16. Arsandaux, J, Montagni, I, Macalli, M, Texier, N, Pouriel, M, Germain, R, et al. Mental Health Condition of College Students Compared to Non-students during COVID-19 Lockdown: the CONFINS Study. BMJ Open (2021) 11(8):e053231. doi:10.1136/bmjopen-2021-053231
17. Son, C, Hegde, S, Smith, A, Wang, X, and Sasangohar, F. Effects of COVID-19 on College Students' Mental Health in the United States: Interview Survey Study. J Med Internet Res (2020) 22(9):e21279. doi:10.2196/21279
18. Liu, C, Liu, D, Huang, N, Fu, M, Ahmed, JF, Zhang, Y, et al. The Combined Impact of Gender and Age on post-traumatic Stress Symptoms, Depression, and Insomnia during COVID-19 Outbreak in China. Front Public Health (2020) 8:620023. doi:10.3389/fpubh.2020.620023
19.World Health Organization. Pandemic Fatigue: Reinvigorating the Public to Prevent COVID-19: Policy Framework for Supporting Pandemic Prevention and Management: Revised Version November 2020 (2021). Available from: https://apps.who.int/iris/handle/10665/337574 (Accessed Oct 24, 2021).
20. Brodeur, A, Clark, AE, Fleche, S, and Powdthavee, N. COVID-19, Lockdowns and Well-Being: Evidence from Google Trends. J Public Econ (2021) 193:104346. doi:10.1016/j.jpubeco.2020.104346
21. Nitschke, JP, Forbes, PAG, Ali, N, Cutler, J, Apps, MAJ, Lockwood, PL, et al. Resilience during Uncertainty? Greater Social Connectedness during COVID‐19 Lockdown Is Associated with Reduced Distress and Fatigue. Br J Health Psychol (2021) 26:553–69. doi:10.1111/bjhp.12485
22. Labrague, LJ, and Ballad, CA. Lockdown Fatigue Among College Students during the COVID‐19 Pandemic: Predictive Role of Personal Resilience, Coping Behaviors, and Health. Perspect Psychiatr Care (2021) 57(4):1905–12. doi:10.1111/ppc.12765
23. Reiss, S, Peterson, RA, Gursky, DM, and McNally, RJ. Anxiety Sensitivity, Anxiety Frequency and the Prediction of Fearfulness. Behav Res Ther (1986) 24(1):1–8. doi:10.1016/0005-7967(86)90143-9
24. Allan, NP, Norr, AM, Boffa, JW, Durmaz, D, Raines, AM, and Schmidt, NB. Examining the Unique Relations between Anxiety Sensitivity Factors and Suicidal Ideation and Past Suicide Attempts. Psychiatry Res (2015) 228(3):441–7. doi:10.1016/j.psychres.2015.05.066
25. Boffa, JW, Norr, AM, Raines, AM, Albanese, BJ, Short, NA, and Schmidt, NB. Anxiety Sensitivity Prospectively Predicts Posttraumatic Stress Symptoms Following a Campus Shooting. Behav Ther (2016) 47(3):367–76. doi:10.1016/j.beth.2016.02.006
26. Caulfield, NM, Martin, RL, Norr, AM, and Capron, DW. The Association between Posttraumatic Stress Symptoms and Anxiety Sensitivity in a College Sample. Psychol Rep (2021) 124(4):003329412094822–58. doi:10.1177/0033294120948227
27. Short, NA, Lechner, M, Bell, K, Black, J, Buchanan, J, Ho, J, et al. Anxiety Sensitivity Prospectively Predicts Increased Acute Posttraumatic Stress and Related Symptoms after Sexual Assault. J Traumatic Stress (2020) 33(6):1111–20. doi:10.1002/jts.22613
28. Hensley, L, and Varela, RE. PTSD Symptoms and Somatic Complaints Following Hurricane Katrina: The Roles of Trait Anxiety and Anxiety Sensitivity. J Clin Child Adolesc Psychol (2008) 37(3):542–52. doi:10.1080/15374410802148186
29. Lehman, CL, and Cheung, RC. Depression, Anxiety, post-traumatic Stress, and Alcohol-Related Problems Among Veterans with Chronic Hepatitis C. Am J Gastroenterol (2002) 97(10):2640–6. doi:10.1111/j.1572-0241.2002.06042.x
30. Lang, AJ, Kennedy, CM, and Stein, MB. Anxiety Sensitivity and PTSD Among Female Victims of Intimate Partner Violence. Depress Anxiety (2002) 16(2):77–83. doi:10.1002/da.10062
31. Feldner, MT, Lewis, SF, Leen-Feldner, EW, Schnurr, PP, and Zvolensky, MJ. Anxiety Sensitivity as a Moderator of the Relation between Trauma Exposure Frequency and Posttraumatic Stress Symptomatology. J Cogn Psychother (2006) 20(2):201–13. doi:10.1891/jcop.20.2.201
32. Blakey, SM, and Abramowitz, JS. Psychological Predictors of Health Anxiety in Response to the Zika Virus. J Clin Psychol Med Settings (2017) 24(3-4):270–8. doi:10.1007/s10880-017-9514-y
33. Blakey, SM, Reuman, L, Jacoby, RJ, and Abramowitz, JS. Tracing "Fearbola": Psychological Predictors of Anxious Responding to the Threat of Ebola. Cogn Ther Res (2015) 39(6):816–25. doi:10.1007/s10608-015-9701-9
34. Kim, A. Korea Officially in COVID-19 Fourth Wave (2021). Available from: http://www.koreaherald.com/view.php?ud=20210707000868 (Accessed Feb 14, 2022).
35.Our World in Data. Daily New Confirmed COVID-19 Cases Per Million People (2021). Available from: https://ourworldindata.org/explorers/coronavirus-data-explorer?zoomToSelection=true&facet=none&pickerSort=asc&pickerMetric=location&Metric=Confirmed+ cases&Interval=7-day+rolling+ average&Relative+to+Population=true&Color+by+test+positivity= false&country=∼KOR (Accessed Feb 14, 2022).
36. Fendos, J. The Diplomat. Why South Korea Still Hasn’t Vaccinated Anyone (2021). Available from: https://thediplomat.com/2021/02/why-south-korea-still-hasnt-vaccinated-anyone/(Accessed Feb 14, 2022).
37. Ritchie, H, Mathieu, E, Rodés-Guirao, L, Appel, C, Giattino, C, Ortiz-Ospina, E, et al. Coronavirus Pandemic (COVID-19). Our World in Data (2021). Available from: https://ourworldindata.org/coronavirus (Accessed Feb 14, 2022).
38. Hao, F, Wang, B, Tan, W, Husain, SF, McIntyre, RS, Tang, X, et al. Attitudes toward COVID-19 Vaccination and Willingness to Pay: Comparison of People with and without Mental Disorders in China. BJPsych Open (2021) 7(5):e146. doi:10.1192/bjo.2021.979
39. Hosey, MM, Leoutsakos, J-MS, Li, X, Dinglas, VD, Bienvenu, OJ, Parker, AM, et al. Screening for Posttraumatic Stress Disorder in ARDS Survivors: Validation of the Impact of Event Scale-6 (IES-6). Crit Care (2019) 23(1):276. doi:10.1186/s13054-019-2553-z
40. Thoresen, S, Tambs, K, Hussain, A, Heir, T, Johansen, VA, and Bisson, JI. Brief Measure of Posttraumatic Stress Reactions: Impact of Event Scale-6. Soc Psychiat Epidemiol (2010) 45(3):405–12. doi:10.1007/s00127-009-0073-x
41. Tavakol, M, and Dennick, R. Making Sense of Cronbach's Alpha. Int J Med Education (2011) 2:53–5. doi:10.5116/ijme.4dfb.8dfd
42. Lilleholt, L, Zettler, I, Betsch, C, and Böhm, R. Pandemic Fatigue: Measurement, Correlates, and Consequences. PsyArXiv (2020). doi:10.31234/osf.io/2xvbr
43. Taylor, S, Zvolensky, MJ, Cox, BJ, Deacon, B, Heimberg, RG, Ledley, DR, et al. Robust Dimensions of Anxiety Sensitivity: Development and Initial Validation of the Anxiety Sensitivity Index-3. Psychol Assess (2007) 19(2):176–88. doi:10.1037/1040-3590.19.2.176
44. Lim, Y-J, and Kim, J-H. Korean Anxiety Sensitivity Index-3: Its Factor Structure, Reliability, and Validity in Non-clinical Samples. Psychiatry Investig (2012) 9(1):45–53. doi:10.4306/pi.2012.9.1.45
45. Vloo, A, Alessie, RJM, Mierau, JO, Boezen, MH, Mierau, JO, Franke, L, et al. Gender Differences in the Mental Health Impact of the COVID-19 Lockdown: Longitudinal Evidence from the Netherlands. SSM - Popul Health (2021) 15:100878. doi:10.1016/j.ssmph.2021.100878
46. Tibubos, AN, Otten, D, Ernst, M, and Beutel, ME. A Systematic Review on Sex- and Gender-Sensitive Research in Public Mental Health during the First Wave of the COVID-19 Crisis. Front Psychiatry (2021) 12:712492. doi:10.3389/fpsyt.2021.712492
47. Di Tella, M, Romeo, A, Benfante, A, and Castelli, L. Mental Health of Healthcare Workers during the COVID ‐19 Pandemic in Italy. J Eval Clin Pract (2020) 26(6):1583–7. doi:10.1111/jep.13444
48. Morgul, E, Bener, A, Atak, M, Akyel, S, Aktaş, S, Bhugra, D, et al. COVID-19 Pandemic and Psychological Fatigue in Turkey. Int J Soc Psychiatry (2021) 67(2):128–35. doi:10.1177/0020764020941889
49. Papageorge, NW, Zahn, MV, Belot, M, van den Broek-Altenburg, E, Choi, S, Jamison, JC, et al. Socio-demographic Factors Associated with Self-Protecting Behavior during the Covid-19 Pandemic. J Popul Econ (2021) 34(2):691–738. doi:10.1007/s00148-020-00818-x
50. Labrague, LJ. Pandemic Fatigue and Clinical Nurses' Mental Health, Sleep Quality and Job Contentment during the Covid‐19 Pandemic: The Mediating Role of Resilience. J Nurs Manag (2021) 29(7):1992–2001. doi:10.1111/jonm.13383
51. Marshall, GN, Miles, JNV, and Stewart, SH. Anxiety Sensitivity and PTSD Symptom Severity Are Reciprocally Related: Evidence from a Longitudinal Study of Physical Trauma Survivors. J Abnormal Psychol (2010) 119(1):143–50. doi:10.1037/a0018009
52. Olatunji, BO, and Fan, Q. Anxiety Sensitivity and post-traumatic Stress Reactions: Evidence for Intrusions and Physiological Arousal as Mediating and Moderating Mechanisms. J Anxiety Disord (2015) 34:76–85. doi:10.1016/j.janxdis.2015.06.0010.1016/j.janxdis.2015.06.002
53. Manning, K, Eades, ND, Kauffman, BY, Long, LJ, Richardson, AL, Garey, L, et al. Anxiety Sensitivity Moderates the Impact of COVID-19 Perceived Stress on Anxiety and Functional Impairment. Cogn Ther Res (2021) 45(4):689–96. doi:10.1007/s10608-021-10207-7
54. McKay, D, Yang, H, Elhai, J, and Asmundson, GJG. Anxiety Regarding Contracting COVID-19 Related to Interoceptive Anxiety Sensations: The Moderating Role of Disgust Propensity and Sensitivity. J Anxiety Disord (2020) 73:102233. doi:10.1016/j.janxdis.2020.102233
55. Warren, AM, Zolfaghari, K, Fresnedo, M, Bennett, M, Pogue, J, Waddimba, A, et al. Anxiety Sensitivity, COVID-19 Fear, and Mental Health: Results from a United States Population Sample. Cogn Behav Ther (2021) 50(3):204–16. doi:10.1080/16506073.2021.1874505
56. Karadem, FB, Demirdaş, A, Işık, Ü, and Kılıç, F. Investigation of the Psychiatric Factors that Determine the Fear of COVID-19 in Healthcare Workers and Hospital Staff in a university Hospital in Turkey. J Community Psychol (2021) 2021. doi:10.1002/jcop.22657
57. Rogers, AH, Bogiaizian, D, Salazar, PL, Solari, A, Garey, L, Fogle, BM, et al. COVID-19 and Anxiety Sensitivity across Two Studies in argentina: Associations with COVID-19 Worry, Symptom Severity, Anxiety, and Functional Impairment. Cogn Ther Res (2021) 45(4):697–707. doi:10.1007/s10608-020-10194-1
58. Paluszek, MM, Asmundson, AJN, Landry, CA, McKay, D, Taylor, S, and Asmundson, GJG. Effects of Anxiety Sensitivity, Disgust, and Intolerance of Uncertainty on the COVID Stress Syndrome: A Longitudinal Assessment of Transdiagnostic Constructs and the Behavioural Immune System. Cogn Behav Ther (2021) 50(3):191–203. doi:10.1080/16506073.2021.1877339
59. Schmidt, NB, Morabito, DM, Mathes, BM, and Martin, A. Anxiety Sensitivity Prospectively Predicts Pandemic-Related Distress. J Affective Disord (2021) 292:660–6. doi:10.1016/j.jad.2021.05.124
60. Elmer, T, Mepham, K, and Stadtfeld, C. Students under Lockdown: Comparisons of Students' Social Networks and Mental Health before and during the COVID-19 Crisis in Switzerland. PLoS One (2020) 15(7):e0236337. doi:10.1371/journal.pone.0236337
61. Keough, ME, and Schmidt, NB. Refinement of a Brief Anxiety Sensitivity Reduction Intervention. J Consulting Clin Psychol (2012) 80(5):766–72. doi:10.1037/a0027961
Keywords: COVID-19, university students, pandemic fatigue, anxiety sensitivity, posttraumatic stress symptoms
Citation: Kim HJ, Meeker TJ, Tulloch IK, Mullins J, Park J-H and Bae SH (2022) Pandemic Fatigue and Anxiety Sensitivity as Associated Factors With Posttraumatic Stress Symptoms Among University Students in South Korea During the Prolonged COVID-19 Pandemic. Int J Public Health 67:1604552. doi: 10.3389/ijph.2022.1604552
Received: 26 October 2021; Accepted: 06 April 2022;
Published: 13 May 2022.
Edited by:
Franco Mascayano, Columbia University, United StatesReviewed by:
Kasim Allel, Independent Researcher, Santiago, ChileGonzalo Cuadra-Malinarich, Colegio Médico de Chile, Chile
Copyright © 2022 Kim, Meeker, Tulloch, Mullins, Park and Bae. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sun Hyoung Bae, c2h5b3VuZ0Bham91LmFjLmty
This original research is part of the IJPH Special Issue “The Impact of the COVID-19 Pandemic on Mental Health”
 Hee Jun Kim
Hee Jun Kim Timothy J. Meeker
Timothy J. Meeker Ingrid K. Tulloch
Ingrid K. Tulloch Jake Mullins2
Jake Mullins2 Sun Hyoung Bae
Sun Hyoung Bae